

Breast Cancer Clinical Presentation
- Author: Pavani Chalasani, MD, MPH; Chief Editor: John V Kiluk, MD, FACS more...
- Sections Breast Cancer
- Practice Essentials
- Pathophysiology
- Epidemiology
- Physical Examination
- Approach Considerations
- Breast Cancer Screening
- Ultrasonography
- Magnetic Resonance Imaging
- Imaging Studies for Staging
- Accuracy of Breast Imaging Modalities
- Breast Biopsy
- HER2 Testing
- Breast Cancer Staging
- Additional Testing
- Tumor Molecular Testing
- Treatment of Invasive Breast Cancer
- Systemic Adjuvant Therapy for Breast Cancer
- Treatment of Carcinoma in Situ
- Treatment of Locally Advanced and Inflammatory Breast Cancer
- Systemic Treatment of Metastatic Breast Cancer
- Surgical Treatment of Metastatic Breast Cancer
- Pharmacologic Reduction of Breast Cancer Risk
- Prophylactic Mastectomy
- Long-Term Monitoring
- Integrative Therapy
- Medication Summary
- Antineoplastics, Alkylating
- Antineoplastics, Anthracycline
- Calcium Metabolism Modifiers
- Antineoplastics, Antimetabolite
- Antineoplastics, Vinca Alkaloid
- Monoclonal Antibodies
- Tyrosine Kinase Inhibitors
- Antineoplastics, Antimicrotubular
- Aromatase Inhibitors
- CDK Inhibitors
- Antineoplastics, PARP Inhibitors
- Antineoplastics, Estrogen Receptor Antagonist
- PD-1/PD-L1 Inhibitors
- PI3K Inhibitors
- AKT Inhibitors
- Questions & Answers
- Media Gallery
Many early breast cancers are asymptomatic, particularly if they were discovered during a breast-screening program. Larger tumors may present as a painless mass. Pain or discomfort is not usually a symptom of breast cancer; only 5% of patients with a malignant mass present with breast pain.
Often, the purpose of the history is not diagnosis but risk assessment. A family history of breast cancer in a first-degree relative is the most widely recognized breast cancer risk factor.
The US Preventive Services Task Force (USPSTF) guidelines on risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women are as follows [ 89 ] :
Women who have family members with breast, ovarian, tubal, or peritoneal cancer should be screened to identify a family history that may be associated with an increased risk for mutations in the breast cancer susceptibility genes BRCA1 or BRCA2
Women who have positive screening results should receive genetic counseling and then BRCA testing if warranted
Women without a family history associated with an increased risk for mutations should not receive routine genetic counseling or BRCA testing
If the patient has not noticed a lump, then signs and symptoms indicating the possible presence of breast cancer may include the following:
- Change in breast size or shape
- Skin dimpling or skin changes (eg, thickening, swelling, or redness)
- Recent nipple inversion or skin change or other nipple abnormalities (eg, ulceration, retraction, or spontaneous bloody discharge)
- Nipple discharge, particularly if bloodstained
- Axillary lump
To detect subtle changes in breast contour and skin tethering, the examination must include an assessment of the breasts with the patient upright with arms raised. The following findings should raise concern:
- Lump or contour change
- Skin tethering
- Nipple inversion
- Dilated veins
- Redness or eczemalike rash involving nipple or surrounding area ( mammary Paget disease )
- Edema or peau d’orange
The nature of palpable lumps is often difficult to determine clinically, but the following features should raise concern:
- Irregularity
- Focal nodularity
- Asymmetry compared with the other breast
- Fixation to skin or muscle (assess fixation to muscle by moving the lump in the line of the pectoral muscle fibers with the patient bracing her arms against her hips)
A complete examination includes assessment for lymphatic and distant metastases; in descending order of frequency, distant metastases are to bone, lung, liver, and brain. [ 90 ] Thus, the assessment should include the axillae and supraclavicular fossae, the chest and sites of skeletal pain, and abdominal and neurologic examinations. The clinician should be alert to symptoms of metastatic spread, such as the following:
- Symptoms of hypercalcemia
- Breathing difficulties
- Abdominal distention
- Localizing neurologic signs
- Altered cognitive function
The clinical evaluation should include a thorough assessment of specific risk factors for breast cancer (see Breast Cancer Risk Factors ).
Breast Cancer Signs and Symptoms. American Cancer Society. Available at https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/breast-cancer-signs-and-symptoms.html . January 14, 2022; Accessed: May 6, 2024.
Breast Cancer Screening and Diagnosis. National Comprehensive Cancer Network. Available at https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf . Version 2.2024 — April 9, 2024; Accessed: May 6, 2024.
American Cancer Society Recommendations for the Early Detection of Breast Cancer. American Cancer Society. Available at https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html . January 14, 2022; Accessed: August 17, 2023.
[Guideline] Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ, Clinical Guidelines Committee of the American College of Physicians., et al. Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians. Ann Intern Med . 2019 Apr 16. 170 (8):547-560. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] American Cancer Society Recommendations for the Early Detection of Breast Cancer. American Cancer Society. Available at https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html . December 19, 2023; Accessed: May 6, 2024.
PDQ Adult Treatment Editorial Board. Breast Cancer Treatment (Adult) (PDQ®): Health Professional Version. January 19, 2024. [QxMD MEDLINE Link] . [Full Text] .
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin . 2021 May. 71 (3):209-249. [QxMD MEDLINE Link] . [Full Text] .
Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin . 2024 Jan-Feb. 74 (1):12-49. [QxMD MEDLINE Link] . [Full Text] .
The Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature . 2012 Oct 4. 490(7418):61-70. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Recht A, Edge SB, Solin LJ, Robinson DS, Estabrook A, Fine RE, et al. Postmastectomy radiotherapy: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol . 2001 Mar 1. 19 (5):1539-69. [QxMD MEDLINE Link] .
Wen HY, Brogi E. Lobular Carcinoma In Situ. Surg Pathol Clin . 2018 Mar. 11 (1):123-145. [QxMD MEDLINE Link] . [Full Text] .
Surveillance Epidemiology and End Results (SEER). Cancer Stat Facts: Female Breast Cancer. National Cancer Institute. Available at http://seer.cancer.gov/statfacts/html/breast.html#incidence-mortality . Accessed: May 6, 2024.
Jatoi I, Anderson WF, Rosenberg PS. Qualitative age-interactions in breast cancer: a tale of two diseases? doi: 10.1097/COC.0b013e3181844d1c. Am J Clin Oncol . 2008 Oct. 31(5):504-6. [QxMD MEDLINE Link] .
Allott EH, Shan Y, Chen M, Sun X, Garcia-Recio S, Kirk EL, et al. Bimodal age distribution at diagnosis in breast cancer persists across molecular and genomic classifications. Breast Cancer Res Treat . 2020 Jan. 179 (1):185-195. [QxMD MEDLINE Link] . [Full Text] .
Michailidou K, Lindström S, Dennis J, Beesley J, Hui S, et al. Association analysis identifies 65 new breast cancer risk loci. Nature . 2017 Oct 23. [QxMD MEDLINE Link] .
Milne RL, Kuchenbaecker KB, Michailidou K, Beesley J, Kar S, et al. Identification of ten variants associated with risk of estrogen-receptor-negative breast cancer. Nat Genet . 2017 Oct 23. [QxMD MEDLINE Link] .
FDA authorizes, with special controls, direct-to-consumer test that reports three mutations in the BRCA breast cancer genes. U.S. Food & Drug Administration. Available at https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm599560.htm?utm_campaign=03062018_PR_23andme_BRCA&utm_medium=email&utm_source=Eloqua . March 6, 2018; Accessed: May 6, 2024.
Kelsey JL, Bernstein L. Epidemiology and prevention of breast cancer. Annu Rev Public Health . 1996. 17:47-67. [QxMD MEDLINE Link] .
Colditz GA, Rosner B. Cumulative risk of breast cancer to age 70 years according to risk factor status: data from the Nurses' Health Study. Am J Epidemiol . 2000 Nov 15. 152(10):950-64. [QxMD MEDLINE Link] .
Deligeoroglou E, Michailidis E, Creatsas G. Oral contraceptives and reproductive system cancer. Ann N Y Acad Sci . 2003 Nov. 997:199-208. [QxMD MEDLINE Link] .
Colditz GA, Rosner BA, Chen WY, Holmes MD, Hankinson SE. Risk factors for breast cancer according to estrogen and progesterone receptor status. J Natl Cancer Inst . 2004 Feb 4. 96(3):218-28. [QxMD MEDLINE Link] .
Pike MC, Pearce CL, Peters R, Cozen W, Wan P, Wu AH. Hormonal factors and the risk of invasive ovarian cancer: a population-based case-control study. Fertil Steril . 2004 Jul. 82(1):186-95. [QxMD MEDLINE Link] .
Eliassen AH, Missmer SA, Tworoger SS, Spiegelman D, Barbieri RL, Dowsett M, et al. Endogenous steroid hormone concentrations and risk of breast cancer among premenopausal women. J Natl Cancer Inst . 2006 Oct 4. 98(19):1406-15. [QxMD MEDLINE Link] .
Hankinson SE, Eliassen AH. Circulating sex steroids and breast cancer risk in premenopausal women. Horm Cancer . 2010 Feb. 1(1):2-10. [QxMD MEDLINE Link] . [Full Text] .
Cuzick J, DeCensi A, Arun B, Brown PH, Castiglione M, Dunn B, et al. Preventive therapy for breast cancer: a consensus statement. Lancet Oncol . 2011 May. 12(5):496-503. [QxMD MEDLINE Link] .
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst . 2005 Nov 16. 97(22):1652-62. [QxMD MEDLINE Link] . [Full Text] .
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA . 2006 Jun 21. 295(23):2727-41. [QxMD MEDLINE Link] .
Key T, Appleby P, Barnes I, Reeves G. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst . 2002 Apr 17. 94(8):606-16. [QxMD MEDLINE Link] .
Santen RJ, Boyd NF, Chlebowski RT, Cummings S, Cuzick J, Dowsett M, et al. Critical assessment of new risk factors for breast cancer: considerations for development of an improved risk prediction model. Endocr Relat Cancer . 2007 Jun. 14(2):169-87. [QxMD MEDLINE Link] .
Endogenous Hormones and Breast Cancer Collaborative Group. Free estradiol and breast cancer risk in postmenopausal women: comparison of measured and calculated values. Cancer Epidemiol Biomarkers Prev . 2003 Dec. 12(12):1457-61. [QxMD MEDLINE Link] .
Marchbanks PA, McDonald JA, Wilson HG, Folger SG, Mandel MG, Daling JR, et al. Oral contraceptives and the risk of breast cancer. N Engl J Med . 2002 Jun 27. 346(26):2025-32. [QxMD MEDLINE Link] .
Garbe E, Levesque L, Suissa S. Variability of breast cancer risk in observational studies of hormone replacement therapy: a meta-regression analysis. Maturitas . 2004 Mar 15. 47(3):175-83. [QxMD MEDLINE Link] .
Reeves GK, Beral V, Green J, Gathani T, Bull D. Hormonal therapy for menopause and breast-cancer risk by histological type: a cohort study and meta-analysis. Lancet Oncol . 2006 Nov. 7(11):910-8. [QxMD MEDLINE Link] .
Schairer C, Lubin J, Troisi R, Sturgeon S, Brinton L, Hoover R. Menopausal estrogen and estrogen-progestin replacement therapy and breast cancer risk. JAMA . 2000 Jan 26. 283(4):485-91. [QxMD MEDLINE Link] .
Speroff L. The Million Women Study and breast cancer. Maturitas . 2003 Sep 25. 46(1):1-6. [QxMD MEDLINE Link] .
Collaborative Group on Hormonal Factors in Breast Cancer. Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet . 2019 Sep 28. 394 (10204):1159-1168. [QxMD MEDLINE Link] . [Full Text] .
Anderson GL, Chlebowski RT, Aragaki AK, Kuller LH, Manson JE, Gass M, et al. Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: extended follow-up of the Women's Health Initiative randomised placebo-controlled trial. Lancet Oncol . 2012 May. 13(5):476-86. [QxMD MEDLINE Link] . [Full Text] .
Holmberg L, Anderson H. HABITS (hormonal replacement therapy after breast cancer--is it safe?), a randomised comparison: trial stopped. Lancet . 2004 Feb 7. 363(9407):453-5. [QxMD MEDLINE Link] .
Loprinzi CL, Michalak JC, Quella SK, O'Fallon JR, Hatfield AK, Nelimark RA, et al. Megestrol acetate for the prevention of hot flashes. N Engl J Med . 1994 Aug 11. 331(6):347-52. [QxMD MEDLINE Link] .
Bordeleau L, Pritchard K, Goodwin P, Loprinzi C. Therapeutic options for the management of hot flashes in breast cancer survivors: an evidence-based review. Clin Ther . 2007 Feb. 29(2):230-41. [QxMD MEDLINE Link] .
Page DL, Jensen RA. Evaluation and management of high risk and premalignant lesions of the breast. World J Surg . 1994 Jan-Feb. 18(1):32-8. [QxMD MEDLINE Link] .
Kollias J, Ellis IO, Elston CW, Blamey RW. Clinical and histological predictors of contralateral breast cancer. Eur J Surg Oncol . 1999 Dec. 25(6):584-9. [QxMD MEDLINE Link] .
Page DL, Schuyler PA, Dupont WD, Jensen RA, Plummer WD Jr, Simpson JF. Atypical lobular hyperplasia as a unilateral predictor of breast cancer risk: a retrospective cohort study. Lancet . 2003 Jan 11. 361(9352):125-9. [QxMD MEDLINE Link] .
Page DL. Breast lesions, pathology and cancer risk. Breast J . 2004 Jan-Feb. 10 Suppl 1:S3-4. [QxMD MEDLINE Link] .
Ashbeck EL, Rosenberg RD, Stauber PM, Key CR. Benign breast biopsy diagnosis and subsequent risk of breast cancer. Cancer Epidemiol Biomarkers Prev . 2007 Mar. 16(3):467-72. [QxMD MEDLINE Link] .
Degnim AC, Visscher DW, Berman HK, Frost MH, Sellers TA, Vierkant RA, et al. Stratification of breast cancer risk in women with atypia: a Mayo cohort study. J Clin Oncol . 2007 Jul 1. 25(19):2671-7. [QxMD MEDLINE Link] .
Dupont WD, Page DL, Parl FF, Vnencak-Jones CL, Plummer WD Jr, Rados MS, et al. Long-term risk of breast cancer in women with fibroadenoma. N Engl J Med . 1994 Jul 7. 331(1):10-5. [QxMD MEDLINE Link] .
Henderson BE, Bernstein L. The international variation in breast cancer rates: an epidemiological assessment. Breast Cancer Res Treat . 1991 May. 18 Suppl 1:S11-7. [QxMD MEDLINE Link] .
Kaaks R. Nutrition, hormones, and breast cancer: is insulin the missing link?. Cancer Causes Control . 1996 Nov. 7(6):605-25. [QxMD MEDLINE Link] .
Stoll BA. Breast cancer and the western diet: role of fatty acids and antioxidant vitamins. Eur J Cancer . 1998 Nov. 34(12):1852-6. [QxMD MEDLINE Link] .
Holmes MD, Liu S, Hankinson SE, Colditz GA, Hunter DJ, Willett WC. Dietary carbohydrates, fiber, and breast cancer risk. Am J Epidemiol . 2004 Apr 15. 159(8):732-9. [QxMD MEDLINE Link] .
Holmes MD, Willett WC. Does diet affect breast cancer risk?. Breast Cancer Res . 2004. 6(4):170-8. [QxMD MEDLINE Link] . [Full Text] .
van den Brandt PA, Schulpen M. Mediterranean diet adherence and risk of postmenopausal breast cancer: results of a cohort study and meta-analysis. Int J Cancer . 2017 Mar 5. [QxMD MEDLINE Link] . [Full Text] .
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult weight change and risk of postmenopausal breast cancer. JAMA . 2006 Jul 12. 296(2):193-201. [QxMD MEDLINE Link] .
Han D, Nie J, Bonner MR, McCann SE, Muti P, Trevisan M, et al. Lifetime adult weight gain, central adiposity, and the risk of pre- and postmenopausal breast cancer in the Western New York exposures and breast cancer study. Int J Cancer . 2006 Dec 15. 119(12):2931-7. [QxMD MEDLINE Link] .
Kaaks R. Nutrition, insulin, IGF-1 metabolism and cancer risk: a summary of epidemiological evidence. Novartis Found Symp . 2004. 262:247-60; discussion 260-68. [QxMD MEDLINE Link] .
Lukanova A, Lundin E, Zeleniuch-Jacquotte A, Muti P, Mure A, Rinaldi S, et al. Body mass index, circulating levels of sex-steroid hormones, IGF-I and IGF-binding protein-3: a cross-sectional study in healthy women. Eur J Endocrinol . 2004 Feb. 150(2):161-71. [QxMD MEDLINE Link] .
Baer HJ, Colditz GA, Rosner B, Michels KB, Rich-Edwards JW, Hunter DJ, et al. Body fatness during childhood and adolescence and incidence of breast cancer in premenopausal women: a prospective cohort study. Breast Cancer Res . 2005. 7(3):R314-25. [QxMD MEDLINE Link] . [Full Text] .
Ruder EH, Dorgan JF, Kranz S, Kris-Etherton PM, Hartman TJ. Examining breast cancer growth and lifestyle risk factors: early life, childhood, and adolescence. Clin Breast Cancer . 2008 Aug. 8(4):334-42. [QxMD MEDLINE Link] . [Full Text] .
Fuemmeler BF, Pendzich MK, Tercyak KP. Weight, dietary behavior, and physical activity in childhood and adolescence: implications for adult cancer risk. Obes Facts . 2009. 2(3):179-86. [QxMD MEDLINE Link] . [Full Text] .
Coyle YM. The effect of environment on breast cancer risk. Breast Cancer Res Treat . 2004 Apr. 84(3):273-88. [QxMD MEDLINE Link] .
Gammon MD, Eng SM, Teitelbaum SL, Britton JA, Kabat GC, Hatch M, et al. Environmental tobacco smoke and breast cancer incidence. Environ Res . 2004 Oct. 96(2):176-85. [QxMD MEDLINE Link] .
Smith-Bindman R. Environmental causes of breast cancer and radiation from medical imaging: findings from the Institute of Medicine report. Arch Intern Med . 2012 Jul 9. 172(13):1023-7. [QxMD MEDLINE Link] .
Smith-Warner SA, Spiegelman D, Yaun SS, van den Brandt PA, Folsom AR, Goldbohm RA, et al. Alcohol and breast cancer in women: a pooled analysis of cohort studies. JAMA . 1998 Feb 18. 279 (7):535-40. [QxMD MEDLINE Link] .
Alcohol Use and Cancer. American Cancer Society. Available at https://www.cancer.org/cancer/risk-prevention/diet-physical-activity/alcohol-use-and-cancer.html . June 9, 2020; Accessed: May 6, 2024.
Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol . 2006 Feb. 7 (2):149-56. [QxMD MEDLINE Link] .
Carmichael A, Sami AS, Dixon JM. Breast cancer risk among the survivors of atomic bomb and patients exposed to therapeutic ionising radiation. Eur J Surg Oncol . 2003 Jun. 29(5):475-9. [QxMD MEDLINE Link] .
Clemons M, Loijens L, Goss P. Breast cancer risk following irradiation for Hodgkin's disease. Cancer Treat Rev . 2000 Aug. 26(4):291-302. [QxMD MEDLINE Link] .
Hill DA, Gilbert E, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, et al. Breast cancer risk following radiotherapy for Hodgkin lymphoma: modification by other risk factors. Blood . 2005 Nov 15. 106(10):3358-65. [QxMD MEDLINE Link] . [Full Text] .
Li CI, Daling JR. Changes in breast cancer incidence rates in the United States by histologic subtype and race/ethnicity, 1995 to 2004. Cancer Epidemiol Biomarkers Prev . 2007 Dec. 16(12):2773-80. [QxMD MEDLINE Link] .
Glass AG, Lacey JV Jr, Carreon JD, Hoover RN. Breast cancer incidence, 1980-2006: combined roles of menopausal hormone therapy, screening mammography, and estrogen receptor status. J Natl Cancer Inst . 2007 Aug 1. 99(15):1152-61. [QxMD MEDLINE Link] .
Jemal A, Ward E, Thun MJ. Recent trends in breast cancer incidence rates by age and tumor characteristics among U.S. women. Breast Cancer Res . 2007. 9(3):R28. [QxMD MEDLINE Link] . [Full Text] .
Ravdin PM, Cronin KA, Howlader N, Berg CD, Chlebowski RT, Feuer EJ, et al. The decrease in breast-cancer incidence in 2003 in the United States. N Engl J Med . 2007 Apr 19. 356(16):1670-4. [QxMD MEDLINE Link] .
Katalinic A, Rawal R. Decline in breast cancer incidence after decrease in utilisation of hormone replacement therapy. Breast Cancer Res Treat . 2008 Feb. 107(3):427-30. [QxMD MEDLINE Link] .
Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet . 2003 Aug 9. 362(9382):419-27. [QxMD MEDLINE Link] .
Anderson WF, Reiner AS, Matsuno RK, Pfeiffer RM. Shifting breast cancer trends in the United States. J Clin Oncol . 2007 Sep 1. 25(25):3923-9. [QxMD MEDLINE Link] .
Evidence-based assessment of the impact of the WHI on women’s health. doi: 10.3109/13697137.2012.655564. Burger HG, MacLennan AH, Huang KE, Castelo-Branco C. Climacteric . 2012 Jun. 15(3):281-7.
American Cancer Society. Breast Cancer Facts & Figures 2022-2024. Available at https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/2022-2024-breast-cancer-fact-figures-acs.pdf . Accessed: May 6, 2024.
Xu S, Murtagh S, Han Y, Wan F, Toriola AT. Breast Cancer Incidence Among US Women Aged 20 to 49 Years by Race, Stage, and Hormone Receptor Status. JAMA Netw Open . 2024 Jan 2. 7 (1):e2353331. [QxMD MEDLINE Link] . [Full Text] .
Stringer-Reasor EM, Elkhanany A, Khoury K, Simon MA, Newman LA. Disparities in Breast Cancer Associated With African American Identity. Am Soc Clin Oncol Educ Book . 2021 Jun. 41:e29-e46. [QxMD MEDLINE Link] . [Full Text] .
Johnson JA, Moore BJ, Syrnioti G, Eden CM, Wright D, Newman LA. Landmark Series: The Cancer Genome Atlas and the Study of Breast Cancer Disparities. Ann Surg Oncol . 2023 Oct. 30 (11):6427-6440. [QxMD MEDLINE Link] .
[Guideline] NCCN Clinical Practice Guidelines in Oncology. Breast Cancer. National Comprehensive Cancer Network. Available at http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf . Version 2.2024 — March 11, 2024; Accessed: May 6, 2024.
Nassar H, Wallis T, Andea A, Dey J, Adsay V, Visscher D. Clinicopathologic analysis of invasive micropapillary differentiation in breast carcinoma. Mod Pathol . 2001 Sep. 14(9):836-41. [QxMD MEDLINE Link] .
Rayson D, Adjei AA, Suman VJ, Wold LE, Ingle JN. Metaplastic breast cancer: prognosis and response to systemic therapy. Ann Oncol . 1999 Apr. 10(4):413-9. [QxMD MEDLINE Link] .
Chao TC, Wang CS, Chen SC, Chen MF. Metaplastic carcinomas of the breast. J Surg Oncol . 1999 Aug. 71(4):220-5. [QxMD MEDLINE Link] .
Chaudary MA, Millis RR, Lane EB, Miller NA. Paget's disease of the nipple: a ten year review including clinical, pathological, and immunohistochemical findings. Breast Cancer Res Treat . 1986. 8(2):139-46. [QxMD MEDLINE Link] .
Kollmorgen DR, Varanasi JS, Edge SB, Carson WE 3rd. Paget’s disease of the breast: a 33-year experience. J Am Coll Surg . 1998 Aug. 187(2):171-7.
Mehta LS, Watson KE, Barac A, et al. Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. Circulation . 2018 Feb 20. 137 (8):e30-e66. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Moyer VA. Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA-Related Cancer in Women: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med . 2013 Dec 24. [QxMD MEDLINE Link] .
Xiao W, Zheng S, Yang A, Zhang X, Zou Y, Tang H, et al. Breast cancer subtypes and the risk of distant metastasis at initial diagnosis: a population-based study. Cancer Manag Res . 2018. 10:5329-5338. [QxMD MEDLINE Link] . [Full Text] .
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med . 2005 Oct 27. 353(17):1784-92. [QxMD MEDLINE Link] .
Elmore JG, Armstrong K, Lehman CD, Fletcher SW. Screening for breast cancer. JAMA . 2005 Mar 9. 293(10):1245-56. [QxMD MEDLINE Link] . [Full Text] .
Moss SM, Wale C, Smith R, Evans A, Cuckle H, Duffy SW. Effect of mammographic screening from age 40 years on breast cancer mortality in the UK Age trial at 17 years' follow-up: a randomised controlled trial. Lancet Oncol . 2015 Jul 20. [QxMD MEDLINE Link] .
Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ . 2014 Feb 11. 348:g366. [QxMD MEDLINE Link] . [Full Text] .
García-Albéniz X, Hernán MA, Logan RW, Price M, Armstrong K, Hsu J. Continuation of Annual Screening Mammography and Breast Cancer Mortality in Women Older Than 70 Years. Ann Intern Med . 2020 Feb 25. [QxMD MEDLINE Link] .
Brawley OW. On Mammography Screening for Women Older Than 70 Years. Ann Intern Med . 2020 Feb 25. [QxMD MEDLINE Link] .
[Guideline] Siu AL, U.S. Preventive Services Task Force. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med . 2016 Feb 16. 164 (4):279-96. [QxMD MEDLINE Link] . [Full Text] .
Nyström L, Andersson I, Bjurstam N, Frisell J, Nordenskjöld B, Rutqvist LE. Long-term effects of mammography screening: updated overview of the Swedish randomised trials. Lancet . 2002 Mar 16. 359(9310):909-19. [QxMD MEDLINE Link] .
Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet . 2003 Apr 26. 361(9367):1405-10. [QxMD MEDLINE Link] .
Noble M, Bruening W, Uhl S, Schoelles K. Computer-aided detection mammography for breast cancer screening: systematic review and meta-analysis. Arch Gynecol Obstet . 2009 Jun. 279(6):881-90. [QxMD MEDLINE Link] .
Kleinknecht JH, Ciurea AI, Ciortea CA. Pros and cons for breast cancer screening with tomosynthesis - a review of the literature. Med Pharm Rep . 2020 Oct. 93 (4):335-341. [QxMD MEDLINE Link] . [Full Text] .
Santos Aragon LN, Soto-Trujillo D. Effectiveness of Tomosynthesis Versus Digital Mammography in the Diagnosis of Suspicious Lesions for Breast Cancer in an Asymptomatic Population. Cureus . 2021 Mar 11. 13 (3):e13838. [QxMD MEDLINE Link] . [Full Text] .
Chiarelli AM, Edwards SA, Prummel MV, Muradali D, Majpruz V, Done SJ, et al. Digital compared with screen-film mammography: performance measures in concurrent cohorts within an organized breast screening program. Radiology . 2013 May 14. [QxMD MEDLINE Link] .
Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L. Effectiveness of Breast Cancer Screening: Systematic Review and Meta-analysis to Update the 2009 U.S. Preventive Services Task Force Recommendation. Ann Intern Med . 2016 Feb 16. 164 (4):244-55. [QxMD MEDLINE Link] .
Ward E, Jemal A, Thun M. Regarding "Increase in breast cancer incidence in middle-aged women during the 1990s". Ann Epidemiol . 2005 Jul. 15(6):424-5; author reply 426-7. [QxMD MEDLINE Link] .
[Guideline] US Preventive Services Task Force, Nicholson WK, Silverstein M, Wong JB, Barry MJ, Chelmow D, et al. Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement. JAMA . 2024 Apr 30. 164 (4):279-96. [QxMD MEDLINE Link] . [Full Text] .
Smith RA, Saslow D, Sawyer KA, Burke W, Costanza ME, Evans WP 3rd, et al. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin . 2003 May-Jun. 53(3):141-69. [QxMD MEDLINE Link] .
[Guideline] Oeffinger KC, Fontham ETH, Etzioni R, et al. Breast Cancer Screening for Women at Average Risk: 2015 Guideline Update From the American Cancer Society. JAMA . October 20, 2015. 314: [Full Text] .
Expert Panel on Breast Imaging:., Mainiero MB, Moy L, Baron P, Didwania AD, diFlorio RM, et al. ACR Appropriateness Criteria ® Breast Cancer Screening. J Am Coll Radiol . 2017 Nov. 14 (11S):S383-S390. [QxMD MEDLINE Link] . [Full Text] .
Alsheik N, Blount L, Qiong Q, Talley M, Pohlman S, Troeger K, et al. Outcomes by Race in Breast Cancer Screening With Digital Breast Tomosynthesis Versus Digital Mammography. J Am Coll Radiol . 2021 Jul. 18 (7):906-918. [QxMD MEDLINE Link] . [Full Text] .
Bernardi D, Macaskill P, Pellegrini M, Valentini M, Fantò C, Ostillio L, et al. Breast cancer screening with tomosynthesis (3D mammography) with acquired or synthetic 2D mammography compared with 2D mammography alone (STORM-2): a population-based prospective study. Lancet Oncol . 2016 Aug. 17 (8):1105-13. [QxMD MEDLINE Link] .
Kerlikowske K, Zhu W, Tosteson AN, Sprague BL, Tice JA, Lehman CD, et al. Identifying women with dense breasts at high risk for interval cancer: a cohort study. Ann Intern Med . 2015 May 19. 162 (10):673-81. [QxMD MEDLINE Link] . [Full Text] .
ACR Practice Parameter for the Performance of a Diagnostic Breast Ultrasound Examination. American College of Radiology. Available at https://www.acr.org/-/media/ACR/Files/Practice-Parameters/US-Breast.pdf . 2021; Accessed: April 7, 2022.
Sood R, Rositch AF, Shakoor D, Ambinder E, Pool KL, Pollack E, et al. Ultrasound for Breast Cancer Detection Globally: A Systematic Review and Meta-Analysis. J Glob Oncol . 2019 Aug. 5:1-17. [QxMD MEDLINE Link] . [Full Text] .
Mann RM, Cho N, Moy L. Breast MRI: State of the Art. Radiology . 2019 Sep. 292 (3):520-536. [QxMD MEDLINE Link] .
Breast MRI. American Cancer Society. Available at https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/breast-mri-scans.html . January 14, 2022; Accessed: May 6, 2024.
[Guideline] Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast Cancer Screening in Women at Higher-Than-Average Risk: Recommendations From the ACR. J Am Coll Radiol . 2018 Mar. 15 (3 Pt A):408-414. [QxMD MEDLINE Link] .
Buist DSM, Abraham L, Lee CI, Lee JM, Lehman C, O'Meara ES, et al. Breast Biopsy Intensity and Findings Following Breast Cancer Screening in Women With and Without a Personal History of Breast Cancer. JAMA Intern Med . 2018 Feb 12. [QxMD MEDLINE Link] . [Full Text] .
Comstock CE, Gatsonis C , Newstead GM, et al. Comparison of Abbreviated Breast MRI vs Digital Breast Tomosynthesis for Breast Cancer Detection Among Women With Dense Breasts Undergoing Screening. JAMA . 2020 Mar 24. 323 (12):1194. [QxMD MEDLINE Link] . [Full Text] .
Taillefer R. Clinical applications of 99mTc-sestamibi scintimammography. Semin Nucl Med . 2005 Apr. 35(2):100-15. [QxMD MEDLINE Link] .
[Guideline] Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol . 2007 Jan 1. 25(1):118-45. [QxMD MEDLINE Link] .
[Guideline] Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol . 2018 Jul 10. 36 (20):2105-2122. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Wolff AC, Somerfield MR, Dowsett M, Hammond MEH, Hayes DF, McShane LM, et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: ASCO-College of American Pathologists Guideline Update. J Clin Oncol . 2023 Aug 1. 41 (22):3867-3872. [QxMD MEDLINE Link] . [Full Text] .
Chen AC, Paulino AC, Schwartz MR, Rodriguez AA, Bass BL, Chang JC, et al. Prognostic markers for invasive micropapillary carcinoma of the breast: a population-based analysis. Clin Breast Cancer . 2013 Apr. 13(2):133-9. [QxMD MEDLINE Link] .
Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, et al. Breast Cancer-Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin . 2017 Mar 14. [QxMD MEDLINE Link] . [Full Text] .
Hortobagyi GN, Connolly JL, D'Orsi CJ, et al. Breast. Amin MB, Edge SB, Greene FL, et al, eds. AJCC Cancer Staging Manual . Eighth ed. New York: Springer; 2017. 589-636.
[Guideline] Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE. Sentinel Lymph Node Biopsy for Patients With Early-Stage Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol . 2017 Feb 10. 35 (5):561-564. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Brackstone M, Baldassarre FG, Perera FE, Cil T, Chavez Mac Gregor M, Dayes IS, et al. Management of the Axilla in Early-Stage Breast Cancer: Ontario Health (Cancer Care Ontario) and ASCO Guideline. J Clin Oncol . 2021 Sep 20. 39 (27):3056-3082. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Duffy MJ, Harbeck N, Nap M, Molina R, Nicolini A, Senkus E, et al. Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM). Eur J Cancer . 2017 Apr. 75:284-298. [QxMD MEDLINE Link] . [Full Text] .
Sparano JA, Gray RJ, Makower DF, et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. N Engl J Med . 2018 Jul 12. 379 (2):111-121. [QxMD MEDLINE Link] . [Full Text] .
Sparano JA, Gray RJ, Makower DF, et al. Clinical Outcomes in Early Breast Cancer With a High 21-Gene Recurrence Score of 26 to 100 Assigned to Adjuvant Chemotherapy Plus Endocrine Therapy: A Secondary Analysis of the TAILORx Randomized Clinical Trial. JAMA Oncol . 2019 Sep 30. [QxMD MEDLINE Link] . [Full Text] .
Kalinsky K, Barlow WE, Gralow JR, et al. 21-Gene Assay to Inform Chemotherapy Benefit in Node-Positive Breast Cancer. N Engl J Med . 2021 Dec 16. 385 (25):2336-2347. [QxMD MEDLINE Link] .
Jacobson A. Benefits of Adjuvant Chemotherapy Differ by Menopausal Status in Women with HR+/HER2- Early Breast Cancer, 1-3 Positive Nodes, and a Low Recurrence Score. Oncologist . 2022 Mar 28. 27 (Suppl 1):S15-S16. [QxMD MEDLINE Link] . [Full Text] .
Piccart M, van 't Veer LJ, Poncet C, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol . 2021 Apr. 22 (4):476-488. [QxMD MEDLINE Link] . [Full Text] .
Dowsett M, Sestak I, Lopez-Knowles E, Sidhu K, Dunbier AK, Cowens JW, et al. Comparison of PAM50 risk of recurrence score with oncotype DX and IHC4 for predicting risk of distant recurrence after endocrine therapy. J Clin Oncol . 2013 Aug 1. 31 (22):2783-90. [QxMD MEDLINE Link] .
Gnant M, et al; Austrian Breast and Colorectal Cancer Study Group. Predicting distant recurrence in receptor-positive breast cancer patients with limited clinicopathological risk: using the PAM50 Risk of Recurrence score in 1478 postmenopausal patients of the ABCSG-8 trial treated with adjuvant endocrine therapy alone. Ann Oncol . 2014 Feb. 25 (2):339-45. [QxMD MEDLINE Link] .
Liu S, Chapman JA, Burnell MJ, Levine MN, Pritchard KI, Whelan TJ, et al. Prognostic and predictive investigation of PAM50 intrinsic subtypes in the NCIC CTG MA.21 phase III chemotherapy trial. Breast Cancer Res Treat . 2015 Jan. 149 (2):439-48. [QxMD MEDLINE Link] .
Martin M, Brase JC, Ruiz A, Prat A, Kronenwett R, Calvo L, et al. Prognostic ability of EndoPredict compared to research-based versions of the PAM50 risk of recurrence (ROR) scores in node-positive, estrogen receptor-positive, and HER2-negative breast cancer. A GEICAM/9906 sub-study. Breast Cancer Res Treat . 2016 Feb. 156 (1):81-9. [QxMD MEDLINE Link] .
Sestak I, Cuzick J, Dowsett M, Lopez-Knowles E, Filipits M, Dubsky P, et al. Prediction of late distant recurrence after 5 years of endocrine treatment: a combined analysis of patients from the Austrian breast and colorectal cancer study group 8 and arimidex, tamoxifen alone or in combination randomized trials using the PAM50 risk of recurrence score. J Clin Oncol . 2015 Mar 10. 33 (8):916-22. [QxMD MEDLINE Link] .
Dubsky P, Filipits M, Jakesz R, Rudas M, Singer CF, Greil R, et al. EndoPredict improves the prognostic classification derived from common clinical guidelines in ER-positive, HER2-negative early breast cancer. Ann Oncol . 2013 Mar. 24 (3):640-7. [QxMD MEDLINE Link] .
Martin M, Brase JC, Calvo L, Krappmann K, Ruiz-Borrego M, Fisch K, et al. Clinical validation of the EndoPredict test in node-positive, chemotherapy-treated ER+/HER2- breast cancer patients: results from the GEICAM 9906 trial. Breast Cancer Res . 2014 Apr 12. 16 (2):R38. [QxMD MEDLINE Link] .
Filipits M, et al; EP Investigators. A new molecular predictor of distant recurrence in ER-positive, HER2-negative breast cancer adds independent information to conventional clinical risk factors. Clin Cancer Res . 2011 Sep 15. 17 (18):6012-20. [QxMD MEDLINE Link] .
Sanft T, Aktas B, Schroeder B, Bossuyt V, DiGiovanna M, Abu-Khalaf M, et al. Prospective assessment of the decision-making impact of the Breast Cancer Index in recommending extended adjuvant endocrine therapy for patients with early-stage ER-positive breast cancer. Breast Cancer Res Treat . 2015 Dec. 154 (3):533-41. [QxMD MEDLINE Link] .
[Guideline] Korde LA, Somerfield MR, Carey LA, Crews JR, Denduluri N, Hwang ES, et al. Neoadjuvant Chemotherapy, Endocrine Therapy, and Targeted Therapy for Breast Cancer: ASCO Guideline. J Clin Oncol . 2021 May 1. 39 (13):1485-1505. [QxMD MEDLINE Link] . [Full Text] .
Jones V, Schroeder MC, Roberson ML, De Andrade J, Lizarraga IM. Differential response to neoadjuvant endocrine therapy for Black/African American and White women in NCDB. Breast Cancer Res Treat . 2024 Jan. 203 (1):125-134. [QxMD MEDLINE Link] . [Full Text] .
Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol . 2014 Nov. 15 (12):1303-10. [QxMD MEDLINE Link] . [Full Text] .
Haviland JS, Owen JR, Dewar JA, et al, on behalf of the START Trialists' Group. The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol . 2013 Sep 18. [QxMD MEDLINE Link] .
[Guideline] Moran MS, Schnitt SJ, Giuliano AE, Harris JR, Khan SA, Horton J, et al. Society of Surgical Oncology-American Society for Radiation Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Stages I and II Invasive Breast Cancer. Int J Radiat Oncol Biol Phys . 2014 Mar 1. 88(3):553-64. [QxMD MEDLINE Link] .
[Guideline] American Society of Breast Surgeons. Consensus Guideline on Accelerated Partial Breast Irradiation. Available at https://www.breastsurgeons.org/about/statements/PDF_Statements/APBI.pdf . June 5, 2018; Accessed: January 17, 2019.
Smith GL, Jiang J, Buchholz TA, Xu Y, Hoffman KE, Giordano SH, et al. Benefit of adjuvant brachytherapy versus external beam radiation for early breast cancer: impact of patient stratification on breast preservation. Int J Radiat Oncol Biol Phys . 2014 Feb 1. 88(2):274-84. [QxMD MEDLINE Link] .
Kuske RR, Young SS. Breast brachytherapy versus whole-breast irradiation: reported differences may be statistically significant but clinically trivial. Int J Radiat Oncol Biol Phys . 2014 Feb 1. 88(2):266-8. [QxMD MEDLINE Link] .
Vaidya JS, Wenz F, Bulsara M, Tobias JS, Joseph DJ, Keshtgar M, et al. Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet . 2013 Nov 8. [QxMD MEDLINE Link] .
Veronesi U, Orecchia R, Maisonneuve P, Viale G, Rotmensz N, Sangalli C, et al. Intraoperative radiotherapy versus external radiotherapy for early breast cancer (ELIOT): a randomised controlled equivalence trial. Lancet Oncol . 2013 Nov 8. [QxMD MEDLINE Link] .
[Guideline] Recht A, Comen EA, Fine RE, Fleming GF, Hardenbergh PH, Ho AY, et al. Postmastectomy Radiotherapy: An American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology Focused Guideline Update. Pract Radiat Oncol . 2016 Nov - Dec. 6 (6):e219-e234. [QxMD MEDLINE Link] . [Full Text] .
Ebctcg Early Breast Cancer Trialists' Collaborative Group. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet . 2014 Mar 19. [QxMD MEDLINE Link] .
Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet . 2015 Jul 23. [QxMD MEDLINE Link] . [Full Text] .
Narod SA, Iqbal J, Giannakeas V, Sopik V, Sun P. Breast Cancer Mortality After a Diagnosis of Ductal Carcinoma In Situ. JAMA Oncol . 2015 Aug 20. [QxMD MEDLINE Link] . [Full Text] .
Esserman L, Yau C. Rethinking the Standard for Ductal Carcinoma In Situ Treatment. JAMA Oncol . 2015 Aug 20. [QxMD MEDLINE Link] .
Allred DC, Anderson SJ, Paik S, Wickerham DL, Nagtegaal ID, Swain SM, et al. Adjuvant tamoxifen reduces subsequent breast cancer in women with estrogen receptor-positive ductal carcinoma in situ: a study based on NSABP protocol B-24. J Clin Oncol . 2012 Apr 20. 30(12):1268-73. [QxMD MEDLINE Link] . [Full Text] .
Phillips KA, Milne RL, Rookus MA, Daly MB, Antoniou AC, Peock S, et al. Tamoxifen and Risk of Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. J Clin Oncol . 2013 Sep 1. 31(25):3091-3099. [QxMD MEDLINE Link] .
Margolese RG, Cecchini RS, Julian TB, Ganz PA, Costantino JP, Vallow LA, et al. Anastrozole versus tamoxifen in postmenopausal women with ductal carcinoma in situ undergoing lumpectomy plus radiotherapy (NSABP B-35): a randomised, double-blind, phase 3 clinical trial. Lancet . 2016 Feb 27. 387 (10021):849-56. [QxMD MEDLINE Link] . [Full Text] .
Gianni L, Pienkowski T, Im YH, Roman L, Tseng LM, Liu MC, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol . 2012 Jan. 13(1):25-32. [QxMD MEDLINE Link] .
Gianni L, Pienkowski T, Im YH, Tseng LM, Liu MC, Lluch A, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol . 2016 Jun. 17 (6):791-800. [QxMD MEDLINE Link] . [Full Text] .
Tutt ANJ, Garber JE, Kaufman B, Viale G, et al. Adjuvant Olaparib for Patients with BRCA1 - or BRCA2 -Mutated Breast Cancer. N Engl J Med . 2021 Jun 24. 384 (25):2394-2405. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Giordano SH, Temin S, Chandarlapaty S, Crews JR, Esteva FJ, Kirshner JJ, et al. Systemic Therapy for Patients With Advanced Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol . 2018 Sep 10. 36 (26):2736-2740. [QxMD MEDLINE Link] . [Full Text] .
Bear HD, Anderson S, Smith RE, Geyer CE Jr, Mamounas EP, Fisher B, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer:National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol . 2006 May 1. 24(13):2019-27. [QxMD MEDLINE Link] .
[Guideline] Partridge AH, Rumble RB, Carey LA, Come SE, Davidson NE, Di Leo A, et al. Chemotherapy and Targeted Therapy for Women With Human Epidermal Growth Factor Receptor 2-Negative (or unknown) Advanced Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol . 2014 Sep 2. [QxMD MEDLINE Link] .
[Guideline] Burstein HJ, Somerfield MR, Barton DL, Dorris A, Fallowfield LJ, Jain D, et al. Endocrine Treatment and Targeted Therapy for Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Metastatic Breast Cancer: ASCO Guideline Update. J Clin Oncol . 2021 Dec 10. 39 (35):3959-3977. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Burstein HJ, DeMichele A, Somerfield MR, Henry NL, Biomarker Testing and Endocrine and Targeted Therapy in Metastatic Breast Cancer Expert Panels. Testing for ESR1 Mutations to Guide Therapy for Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Metastatic Breast Cancer: ASCO Guideline Rapid Recommendation Update. J Clin Oncol . 2023 Jun 20. 41 (18):3423-3425. [QxMD MEDLINE Link] . [Full Text] .
Mehta RS, Barlow WE, Albain KS, Vandenberg TA, Dakhil SR, Tirumali NR, et al. Combination anastrozole and fulvestrant in metastatic breast cancer. N Engl J Med . 2012 Aug 2. 367(5):435-44. [QxMD MEDLINE Link] . [Full Text] .
Robertson JFR, Bondarenko IM, Trishkina E, Dvorkin M, Panasci L, Manikhas A, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): an international, randomised, double-blind, phase 3 trial. Lancet . 2016 Dec 17. 388 (10063):2997-3005. [QxMD MEDLINE Link] . [Full Text] .
Bidard FC, Kaklamani VG, Neven P, Streich G, Montero AJ, Forget F, et al. Elacestrant (oral selective estrogen receptor degrader) Versus Standard Endocrine Therapy for Estrogen Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: Results From the Randomized Phase III EMERALD Trial. J Clin Oncol . 2022 Oct 1. 40 (28):3246-3256. [QxMD MEDLINE Link] . [Full Text] .
Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol . 2015 Jan. 16(1):25-35. [QxMD MEDLINE Link] .
Turner NC, Ro J, André F, Loi S, Verma S, Iwata H, et al. Palbociclib in Hormone-Receptor-Positive Advanced Breast Cancer. N Engl J Med . 2015 Jul 16. 373 (3):209-19. [QxMD MEDLINE Link] . [Full Text] .
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol . 2018 Jul 1. 29 (7):1541-1547. [QxMD MEDLINE Link] . [Full Text] .
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Ribociclib as First-Line Therapy for HR-Positive, Advanced Breast Cancer. N Engl J Med . 2016 Nov 3. 375 (18):1738-1748. [QxMD MEDLINE Link] .
Dickler MN, Tolaney SM, Rugo HS, Cortés J, Diéras V, Patt D, et al. MONARCH 1, A Phase II Study of Abemaciclib, a CDK4 and CDK6 Inhibitor, as a Single Agent, in Patients with Refractory HR + /HER2 - Metastatic Breast Cancer. Clin Cancer Res . 2017 Sep 1. 23 (17):5218-5224. [QxMD MEDLINE Link] . [Full Text] .
Sledge GW Jr, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. MONARCH 2: Abemaciclib in Combination With Fulvestrant in Women With HR+/HER2- Advanced Breast Cancer Who Had Progressed While Receiving Endocrine Therapy. J Clin Oncol . 2017 Sep 1. 35 (25):2875-2884. [QxMD MEDLINE Link] . [Full Text] .
Goetz MP, et al. MONARCH 3: Abemaciclib As Initial Therapy for Advanced Breast Cancer. J Clin Oncol . 2017 Nov 10. 35 (32):3638-3646. [QxMD MEDLINE Link] . [Full Text] .
Modi S, Saura C, Yamashita T, and the, DESTINY-Breast01 Investigators. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Breast Cancer. N Engl J Med . 2019 Dec 11. [QxMD MEDLINE Link] .
Tukysa (tucatinib) [package insert]. Bothell, WA: Seattle Genetics, Inc. April 2020. Available at [Full Text] .
O'Shaughnessy J. Gemcitabine combination chemotherapy in metastatic breast cancer: phase II experience. Oncology (Williston Park) . 2003 Dec. 17(12 Suppl 14):15-21. [QxMD MEDLINE Link] .
Perez EA, Hillman DW, Stella PJ, Krook JE, Hartmann LC, Fitch TR, et al. A phase II study of paclitaxel plus carboplatin as first-line chemotherapy for women with metastatic breast carcinoma. Cancer . 2000 Jan 1. 88(1):124-31. [QxMD MEDLINE Link] .
Jones SE, Savin MA, Holmes FA, O'Shaughnessy JA, Blum JL, Vukelja S, et al. Phase III trial comparing doxorubicin plus cyclophosphamide with docetaxel plus cyclophosphamide as adjuvant therapy for operable breast cancer. J Clin Oncol . 2006 Dec 1. 24(34):5381-7. [QxMD MEDLINE Link] .
Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med . 2007 Dec 27. 357(26):2666-76. [QxMD MEDLINE Link] .
Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im SA, et al. Phase III Randomized Study of Ribociclib and Fulvestrant in Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: MONALEESA-3. J Clin Oncol . 2018 Aug 20. 36 (24):2465-2472. [QxMD MEDLINE Link] . [Full Text] .
O'Shaughnessy J, Miles D, Vukelja S, Moiseyenko V, Ayoub JP, Cervantes G, et al. Superior survival with capecitabine plus docetaxel combination therapy in anthracycline-pretreated patients with advanced breast cancer: phase III trial results. J Clin Oncol . 2002 Jun 15. 20(12):2812-23. [QxMD MEDLINE Link] .
Biganzoli L, Martin M, Twelves C. Moving forward with capecitabine: a glimpse of the future. Oncologist . 2002. 7 Suppl 6:29-35. [QxMD MEDLINE Link] .
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med . 2001 Mar 15. 344(11):783-92. [QxMD MEDLINE Link] .
Marty M, Cognetti F, Maraninchi D, Snyder R, Mauriac L, Tubiana-Hulin M, et al. Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: the M77001 study group. J Clin Oncol . 2005 Jul 1. 23(19):4265-74. [QxMD MEDLINE Link] .
Burstein HJ, Kuter I, Campos SM, Gelman RS, Tribou L, Parker LM, et al. Clinical activity of trastuzumab and vinorelbine in women with HER2-overexpressing metastatic breast cancer. J Clin Oncol . 2001 May 15. 19(10):2722-30. [QxMD MEDLINE Link] .
Geyer CE, Forster J, Lindquist D, Chan S, Romieu CG, Pienkowski T, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med . 2006 Dec 28. 355(26):2733-43. [QxMD MEDLINE Link] .
Albain KS, Nag SM, Calderillo-Ruiz G, Jordaan JP, Llombart AC, Pluzanska A, et al. Gemcitabine plus Paclitaxel versus Paclitaxel monotherapy in patients with metastatic breast cancer and prior anthracycline treatment. J Clin Oncol . 2008 Aug 20. 26(24):3950-7. [QxMD MEDLINE Link] .
André F, Ciruelos E, Rubovszky G, Campone M, Loibl S, Rugo HS, et al. Alpelisib for PIK3CA-Mutated, Hormone Receptor-Positive Advanced Breast Cancer. N Engl J Med . 2019 May 16. 380 (20):1929-1940. [QxMD MEDLINE Link] .
FDA approves first treatment for breast cancer with a certain inherited genetic mutation. U.S. Food & Drug Administration. Available at https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm592347.htm . January 12, 2018; Accessed: May 7, 2024.
Robson M, Im SA, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N Engl J Med . 2017 Aug 10. 377 (6):523-533. [QxMD MEDLINE Link] .
Litton JK, Rugo HS, Ettl J, Hurvitz SA, Gonçalves A, Lee KH, et al. Talazoparib in Patients with Advanced Breast Cancer and a Germline BRCA Mutation. N Engl J Med . 2018 Aug 23. 379 (8):753-763. [QxMD MEDLINE Link] .
Turner NC, Oliveira M, Howell SJ, and the, CAPItello-291 Study Group. Capivasertib in Hormone Receptor-Positive Advanced Breast Cancer. N Engl J Med . 2023 Jun 1. 388 (22):2058-2070. [QxMD MEDLINE Link] .
[Guideline] Giordano SH, Franzoi MAB, Temin S, Anders CK, Chandarlapaty S, Crews JR, et al. Systemic Therapy for Advanced Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer: ASCO Guideline Update. J Clin Oncol . 2022 Aug 10. 40 (23):2612-2635. [QxMD MEDLINE Link] . [Full Text] .
Schmid P, et al, for the IMpassion130 Trial Investigators. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N Engl J Med . October 20, 2018. [Full Text] .
Tecentriq (atezolizumab) [package insert]. South San Francisco, CA: Genentech, Inc. April 2024. Available at [Full Text] .
FDA alerts health care professionals and oncology clinical investigators about efficacy and potential safety concerns with atezolizumab in combination with paclitaxel for treatment of breast cancer. U.S. Food & Drug Administration. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-alerts-health-care-professionals-and-oncology-clinical-investigators-about-efficacy-and . September 8, 2020; Accessed: May 6, 2024.
FDA grants regular approval to sacituzumab govitecan for triple-negative breast cancer. U.S. Food & Drug Administration. Available at https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-regular-approval-sacituzumab-govitecan-triple-negative-breast-cancer . April 7, 2021; Accessed: May 7, 2024.
Khan SA, Zhao F, Goldstein LJ, Cella D, Basik M, Golshan M, et al. Early Local Therapy for the Primary Site in De Novo Stage IV Breast Cancer: Results of a Randomized Clinical Trial (EA2108). J Clin Oncol . 2022 Mar 20. 40 (9):978-987. [QxMD MEDLINE Link] . [Full Text] .
Goss PE, Ingle JN, Alés-Martínez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, et al. Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med . 2011 Jun 23. 364(25):2381-91. [QxMD MEDLINE Link] . [Full Text] .
Cuzick J, Sestak I, Forbes JF, Dowsett M, Cawthorn S, Mansel RE, et al. Use of anastrozole for breast cancer prevention (IBIS-II): long-term results of a randomised controlled trial. Lancet . 2020 Jan 11. 395 (10218):117-122. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Visvanathan K, Fabian CJ, Bantug E, Brewster AM, Davidson NE, DeCensi A, et al. Use of Endocrine Therapy for Breast Cancer Risk Reduction: ASCO Clinical Practice Guideline Update. J Clin Oncol . 2019 Nov 20. 37 (33):3152-3165. [QxMD MEDLINE Link] . [Full Text] .
Surgery to Reduce the Risk of Breast Cancer. National Cancer Institute. Available at https://www.cancer.gov/types/breast/risk-reducing-surgery-fact-sheet . August 12, 2013; Accessed: May 7, 2024.
[Guideline] NCCN Clinical Practice Guidelines in Oncology. Breast Cancer Risk Reduction. National Comprehensive Cancer Network. Available at https://www.nccn.org/professionals/physician_gls/pdf/breast_risk.pdf . Version 2.2024 — March 11, 2024; Accessed: May 7, 2024.
Carbine NE, Lostumbo L, Wallace J, Ko H. Risk-reducing mastectomy for the prevention of primary breast cancer. Cochrane Database Syst Rev . 2018 Apr 5. 4 (4):CD002748. [QxMD MEDLINE Link] .
Boughey JC, Attai DJ, Chen SL, Cody HS, Dietz JR, Feldman SM, et al. Contralateral Prophylactic Mastectomy (CPM) Consensus Statement from the American Society of Breast Surgeons: Data on CPM Outcomes and Risks. Ann Surg Oncol . 2016 Oct. 23 (10):3100-5. [QxMD MEDLINE Link] . [Full Text] .
Lancellotti P, Nkomo VT, Badano LP, Bergler J, Bogaert J, Davin L, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging . 2013 Aug. 14(8):721-40. [QxMD MEDLINE Link] .
[Guideline] Greenlee H, Balneaves L, Carlson M, et al. Clinical Practice Guidelines on the Use of Integrative Therapies as Supportive Care in Patients Treated for Breast Cancer. J Natl Cancer Inst . 2014. 50:346-358. [Full Text] .
Maia LO, Beaussant Y, Garcia ACM. The Therapeutic Potential of Psychedelic-assisted Therapies for Symptom Control in Patients Diagnosed With Serious Illness: A Systematic Review. J Pain Symptom Manage . 2022 Jun. 63 (6):e725-e738. [QxMD MEDLINE Link] .
Lehto RH, Miller M, Sender J. The Role of Psilocybin-Assisted Psychotherapy to Support Patients With Cancer: A Critical Scoping Review of the Research. J Holist Nurs . 2022 Sep. 40 (3):265-280. [QxMD MEDLINE Link] .
Olsson Möller U, Beck I, Rydén L, Malmström M. A comprehensive approach to rehabilitation interventions following breast cancer treatment - a systematic review of systematic reviews. BMC Cancer . 2019 May 20. 19 (1):472. [QxMD MEDLINE Link] . [Full Text] .
Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, et al. Cancer screening in the United States, 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin . 2019 May. 69 (3):184-210. [QxMD MEDLINE Link] . [Full Text] .
Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin . 2007 Mar-Apr. 57 (2):75-89. [QxMD MEDLINE Link] .
[Guideline] Practice Bulletin Number 179: Breast Cancer Risk Assessment and Screening in Average-Risk Women. Obstet Gynecol . 2017 Jul. 130 (1):e1-e16. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Schünemann HJ, Lerda D, Quinn C, et al, European Commission Initiative on Breast Cancer (ECIBC) Contributor Group. Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines. Ann Intern Med . 2019 Nov 26. [QxMD MEDLINE Link] . [Full Text] .
Visvanathan K, Hurley P, Bantug E, Brown P, Col NF, Cuzick J, et al. Use of pharmacologic interventions for breast cancer risk reduction: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol . 2013 Aug 10. 31 (23):2942-62. [QxMD MEDLINE Link] .
[Guideline] US Preventive Services Task Force., Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, et al. Medication Use to Reduce Risk of Breast Cancer: US Preventive Services Task Force Recommendation Statement. JAMA . 2019 Sep 3. 322 (9):857-867. [QxMD MEDLINE Link] .
[Guideline] Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J Clin Oncol . 2020 Jan 13. JCO1902309. [QxMD MEDLINE Link] .
[Guideline] Morrow M, Van Zee KJ, Solin LJ, Houssami N, Chavez-MacGregor M, Harris JR, et al. Society of Surgical Oncology-American Society for Radiation Oncology-American Society of Clinical Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Ductal Carcinoma in Situ. Pract Radiat Oncol . 2016 Sep-Oct. 6 (5):287-95. [QxMD MEDLINE Link] . [Full Text] .
Moran MS, Schnitt SJ, Giuliano AE, Harris JR, Khan SA, Horton J, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Int J Radiat Oncol Biol Phys . 2014 Mar 1. 88 (3):553-64. [QxMD MEDLINE Link] .
[Guideline] Smith BD, Bellon JR, Blitzblau R, et al. Radiation therapy for the whole breast: Executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Practical Radiation Oncology . 2018. [Full Text] .
[Guideline] Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, et al. Adjuvant Endocrine Therapy for Women With Hormone Receptor-Positive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update on Ovarian Suppression. J Clin Oncol . 2016 May 10. 34 (14):1689-701. [QxMD MEDLINE Link] . [Full Text] .
Burstein HJ, Temin S, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: american society of clinical oncology clinical practice guideline focused update. J Clin Oncol . 2014 Jul 20. 32 (21):2255-69. [QxMD MEDLINE Link] .
[Guideline] Harris LN, Ismaila N, McShane LM, Andre F, Collyar DE, Gonzalez-Angulo AM, et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women With Early-Stage Invasive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol . 2016 Apr 1. 34 (10):1134-50. [QxMD MEDLINE Link] .
[Guideline] Paluch-Shimon S, Pagani O, Partridge AH, Abulkhair O, Cardoso MJ, Dent RA, et al. ESO-ESMO 3rd international consensus guidelines for breast cancer in young women (BCY3). Breast . 2017 Oct. 35:203-217. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J Clin . 2016 Jan-Feb. 66 (1):43-73. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Freedman RA, Minami CA, Winer EP, et al. Individualizing Surveillance Mammography for Older Patients After Treatment for Early-Stage Breast Cancer: Multidisciplinary Expert Panel and International Society of Geriatric Oncology Consensus Statement. JAMA Oncol . 2021 Jan 28. [QxMD MEDLINE Link] .
[Guideline] Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol . 2019 Aug 1. 30 (8):1194-1220. [QxMD MEDLINE Link] . [Full Text] .
- Anatomy of the breast.
- Intrinsic subtypes of breast cancer.
- Breast cancer. Intraductal carcinoma, comedo type. Distended duct with intact basement membrane and central tumor necrosis.
- Breast cancer. Intraductal carcinoma, noncomedo type. Distended duct with intact basement membrane, micropapillary, and early cribriform growth pattern.
- Breast cancer. Lobular carcinoma in situ. Enlargement and expansion of lobule with monotonous population of neoplastic cells.
- Breast cancer. Infiltrating ductal carcinoma. Low-grade carcinoma with well-developed glands invading fibrous stroma.
- Breast cancer. Colloid (mucinous) carcinoma. Nests of tumor cells in pool of extracellular mucin.
- Breast cancer. Papillary carcinoma. Solid papillary growth pattern with early cribriform and well-developed thin papillary fronds.
- Anatomy of the breast. Courtesy of Wikimedia Commons (Patrick J Lynch, medical illustrator).
- Table 1. Accuracy of Breast Imaging Modalities
- Table 2. Grading System in Invasive Breast Cancer (Modified Bloom and Richardson)
- Table 3. Ductal Carcinoma in Situ Subtypes
- Table 4. TNM Classification for Breast Cancer
- Table 5. Histologic grade
- Table 6. Anatomic stage/prognostic groups
- Table 7. Clinical prognostic stage
- Table 8. Pathological prognostic stage
- Table 9. Hormone Agents Used in Breast Cancer
- Table 10. Targeted Chemotherapy for Metastatic Breast Cancer
- Table 11. Combination Regimens for Metastatic Breast Cancer
- Table 12. Follow-up Recommendations for Breast Cancer Survivors
|
|
|
|
|
Mammography | 63-95% (>95% palpable, 50% impalpable, 83-92% in women older than 50 y; decreases to 35% in dense breasts) | 14-90% (90% palpable) | 10-50% (94% palpable) | Initial investigation for symptomatic breast in women older than 35 y and for screening; investigation of choice for microcalcification |
Ultrasonography | 68-97% palpable | 74-94% palpable | 92% (palpable) | Initial investigation for palpable lesions in women younger than 35 y |
MRI | 86-100% | 21-97% (< 40% primary cancer) | 52% | Scarred breast, implants, multifocal lesions, and borderline lesions for breast conservation; may be useful in screening high-risk women |
Scintigraphy | 76-95% palpable, 52-91% impalpable | 62-94% (94% impalpable) | 70-83% (83% palpable, 79% impalpable) | Lesions >1 cm and axilla assessment; may help predict drug resistance |
PET | 96% (90% axillary metastases) | 100% |
| Axilla assessment, scarred breast, and multifocal lesions |
MRI = magnetic resonance imaging; PET = positron emission tomography; PPV = positive predictive value. | ||||
|
| ||
|
|
|
|
A. Tubule formation | >75% | 10-75% | < 10% |
B. Mitotic count/HPF (microscope- and field-dependent) | < 7 | 7-12 | >12 |
C. Nuclear size and pleomorphism | Near normal; little variation | Slightly enlarged; moderate variation | Markedly enlarged; marked variation |
Grade I cancer if total score (A + B + C) is 3-5 | |||
Grade II cancer if total score (A + B + C) is 6 or 7 | |||
Grade III cancer if total score (A + B + C) is 8 or 9 | |||
HPF = high-power field. | |||
|
|
|
Nuclear grade | High | Low |
Estrogen receptor | Often negative | Positive |
Distribution | Continuous | Multifocal |
Necrosis | Present | Absent |
Local recurrence | High | Low |
Prognosis | Worse | Better |
DCIS = ductal carcinoma in situ. | ||
| |
TX | Primary tumor cannot be assessed |
T0 | No evidence of primary tumor |
Tis | Carcinoma in situ |
Tis (DCIS) | Ductal carcinoma in situ |
Tis (Paget) | Paget disease of the nipple NOT associated with invasive carcinoma and/or carcinoma in situ (DCIS) in the underlying breast parenchyma. Carcinomas in the breast parenchyma associated with Paget disease are categorized on the basis of the size and characteristics of the parenchymal disease, although the presence of Paget disease should still be noted |
T1 | Tumor ≤ 20 mm in greatest dimension |
T1mi | Tumor ≤ 1 mm in greatest dimension |
T1a | Tumor > 1 mm but ≤ 5 mm in greatest dimension (round any measurement >1.0-1.9 mm to 2 mm) |
T1b | Tumor > 5 mm but ≤ 10 mm in greatest dimension |
T1c | Tumor > 10 mm but ≤ 20 mm in greatest dimension |
T2 | Tumor > 20 mm but ≤ 50 mm in greatest dimension |
T3 | Tumor > 50 mm in greatest dimension |
T4 | Tumor of any size with direct extension to the chest wall and/or to the skin (ulceration or skin nodules), not including invasion of dermis alone |
T4a | Extension to chest wall, not including only pectoralis muscle adherence/invasion |
T4b | Ulceration and/or ipsilateral satellite nodules and/or edema (including peau d’orange) of the skin, which do not meet the criteria for inflammatory carcinoma |
T4c | Both T4a and T4b |
T4d | Inflammatory carcinoma |
| |
| |
cNX | Regional lymph nodes cannot be assessed (eg, previously removed) |
cN0 | No regional lymph node metastasis (on imaging or clinical examination) |
cN1 | Metastasis to movable ipsilateral level I, II axillary lymph node(s) |
cN1mi | Micrometastases (approximately 200 cells, larger than 0.2 mm, but none larger than 2.0 mm) |
cN2 | Metastases in ipsilateral level I, II axillary lymph nodes that are clinically fixed or matted; in ipsilateral internal mammary nodes in the absence of clinically evident axillary lymph node metastases |
cN2a | Metastases in ipsilateral level I, II axillary lymph nodes fixed to one another (matted) or to other structures |
cN2b | Metastases only in ipsilateral internal mammary nodes and in the absence of axillary lymph node metastases |
cN3 | Metastases in ipsilateral infraclavicular (level III axillary) lymph node(s), with or without level I, II axillary node involvement, in ipsilateral internal mammary lymph node(s) with level I, II axillary lymph node metastasis; metastases in ipsilateral supraclavicular lymph node(s), with or without axillary or internal mammary lymph node involvement |
cN3a | Metastasis in ipsilateral infraclavicular lymph node(s) |
cN3b | Metastasis in ipsilateral internal mammary lymph node(s) and axillary lymph node(s) |
cN3c | Metastasis in ipsilateral supraclavicular lymph node(s) |
Note: (sn) and (f) suffixes should be added to the N category to denote confirmation of metastasis by sentinel node biopsy or fine needle aspiration/core needle biopsy, respectively. | |
| |
pNX | Regional lymph nodes cannot be assessed (for example, previously removed, or not removed for pathologic study) |
pN0 | No regional lymph node metastasis identified histologically, or isolated tumor cell clusters (ITCs) only. ITCs are defined as small clusters of cells ≤ 0.2 mm, or single tumor cells, or a cluster of < 200 cells in a single histologic cross-section; ITCs may be detected by routine histology or by immunohistochemical (IHC) methods; nodes containing only ITCs are excluded from the total positive node count for purposes of N classification but should be included in the total number of nodes evaluated |
pN0(i) | No regional lymph node metastases histologically, negative IHC |
pN0(i+) | ITCs only in regional lymph node(s) |
pN0(mol-) | No regional lymph node metastases histologically, negative molecular findings (reverse transcriptase polymerase chain reaction [RT-PCR]) |
pN0(mol+) | Positive molecular findings by RT-PCR; no ITCs detected |
pN1 | Micrometastases; or metastases in 1-3 axillary lymph nodes and/or in internal mammary nodes; and/or in clinically negative internal mammary nodes with micrometastases or macrometastases by sentinel lymph node biopsy |
pN1mi | Micrometastases (200 cells, > 0.2 mm but none > 2.0 mm) |
pN1a | Metastases in 1-3 axillary lymph nodes (at least 1 metastasis > 2.0 mm) |
pN1b | Metastases in ipsilateral internal mammary lymph nodes, excluding ITCs, detected by sentinel lymph node biopsy |
pN1c | Metastases in 1-3 axillary lymph nodes and in internal mammary sentinel nodes (ie, pN1a and pN1b combined) |
pN2 | Metastases in 4-9 axillary lymph nodes; or positive ipsilateral internal mammary lymph nodes by imaging in the absence of axillary lymph node metastases |
pN2a | Metastases in 4-9 axillary lymph nodes (at least 1 tumor deposit > 2.0 mm) |
pN2b | Clinically detected* metastases in internal mammary lymph nodes with or without microscopic confirmation; with pathologically negative axillary lymph nodes |
pN3 | Metastases in ≥ 10 axillary lymph nodes; in infraclavicular (level III axillary) lymph nodes; or positive ipsilateral internal mammary lymph nodes by imaging in the presence of one or more positive level I, II axillary lymph nodes; in > 3 axillary lymph nodes and micrometastases or macrometastases by sentinel lymph node biopsy in clinically negative ipsilateral internal mammary lymph nodes; or in ipsilateral supraclavicular lymph nodes |
pN3a | Metastases in ≥ 10 axillary lymph nodes (at least 1 tumor deposit > 2.0 mm); metastases to the infraclavicular (level III axillary lymph) nodes |
pN3b | pN1a or pN2a in the presence of cN2b (positive internal mammary nodes by imaging) pN2a in the presence of pN1b |
pN3c | Metastases in ipsilateral supraclavicular lymph nodes |
*"Clinically detected" is defined as detected by imaging studies (excluding lymphoscintigraphy) or by clinical examination and having characteristics highly suspicious for malignancy or a presumed pathologic macrometastasis on the basis of FNA biopsy with cytologic examination. | |
| |
M0 | No clinical or radiographic evidence of distant metastasis |
cM0(i+) | No clinical or radiographic evidence of distant metastases in the presence of tumor cells or deposits no larger than 0.2 mm detected microscopically or by molecular techniques in circulating blood, bone marrow, or other nonregional nodal tissue in a patient without symptoms or signs of metastase |
cM1 | Distant metastases detected by clinical and radiographic means |
pM1 | Any histologically proven metastases in distant organs; or if in non-regional nodes, metastases > 0.2 mm |
| |
GX | Grade cannot be assessed |
G1 | Low combined histologic grade (favorable) |
G2 | Intermediate combined histologic grade (moderately favorable) |
G3 | High combined histologic grade (unfavorable) |
|
|
|
|
0 | Tis | N0 | M0 |
IA | T1 | N0 | M0 |
IB | T0 | N1mi | M0 |
| T1 | N1mi | M0 |
IIA | T0 | N1 | M0 |
| T1 | N1 | M0 |
| T2 | N0 | M0 |
IIB | T2 | N1 | M0 |
| T3 | N0 | M0 |
IIIA | T0 | N2 | M0 |
| T1 | N2 | M0 |
| T2 | N2 | M0 |
| T3 | N1 | M0 |
| T3 | N2 | M0 |
IIIB | T4 | N0 | M0 |
| T4 | N1 | M0 |
| T4 | N2 | M0 |
IIIC | Any T | N3 | M0 |
IV | Any T | Any N | M1 |
|
|
|
|
|
|
Tis N0 M0 | Any | Any | Any | Any | 0 |
T1 N0 M0 T0 N1mi M0 T1 N1mi M0 | G1 | Positive | Positive | Positive | IA |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | IB | ||||
G2 | Positive | Positive | Positive | IA | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | IB | ||||
G3 | Positive | Positive | Positive | IA | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | IB | ||||
Negative | Positive | ||||
Negative | |||||
T0 N1 M0 T1 N1 M0 T2 N0 M0 | G1 | Positive | Positive | Positive | IB |
Negative | IIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IB | ||
Negative | IIA | ||||
Negative | Positive | ||||
Negative | |||||
G2 | Positive | Positive | Positive | IB | |
Negative | IIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IB | ||
Negative | IIA | ||||
Negative | Positive | ||||
Negative | IIB | ||||
G3 | Positive | Positive | Positive | IB IIA | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
T2 N1 M0 T3 N0 M0 | G1 | Positive | Positive | Positive | IB |
Negative | IIA | ||||
Negative | Positive | ||||
Negative | IIB | ||||
Negative | Positive | Positive | IIA | ||
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
G2 | Positive | Positive | Positive | IB | |
Negative | IIA | ||||
Negative | Positive | ||||
Negative | IIB | ||||
Negative | Positive | Positive | IIA | ||
Negative | IIB | ||||
Negative | Positive | ||||
Negative | IIIB | ||||
G3 | Positive | Positive | Positive | IB | |
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | IIIB | ||||
T0 N2 M0 T1 N2 M0 T2 N2 M0 T3 N1 M0 T3 N2 M0 | G1 | Positive | Positive | Positive | IIA |
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IIA | ||
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | IIIB | ||||
G2 | Positive | Positive | Positive | IIA | |
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IIA | ||
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | IIIB | ||||
G3 | Positive | Positive | Positive | IIB | |
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | IIIC | ||||
T4 N0 M0 T4 N1 M0 T4 N2 M0 Any T N3 M0 | G1 | Positive | Positive | Positive | IIIA |
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | IIIC | ||||
G2 | Positive | Positive | Positive | IIIA | |
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | IIIC | ||||
G3 | Positive | Positive | Positive | IIIB | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | IIIC | ||||
Negative | Positive | ||||
Negative | |||||
Any T Any N M1 | Any | Any | Any | Any | IV |
ER=estrogen receptor; PR=progesterone receptor | |||||
|
|
|
|
|
|
Tis N0 M0 | Any | Any | Any | Any | 0 |
T1 N0 M0 T0 N1mi M0 T1 N1mi M0 | G1 | Positive | Positive | Positive | IA |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | |||||
G2 | Positive | Positive | Positive | ||
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | IB | ||||
G3 | Positive | Positive | Positive | IA | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | |||||
Negative | Positive | ||||
Negative | IB | ||||
T0 N1 M0 T1 N1 M0 T2 N0 M0 | G1 | Positive | Positive | Positive | IA |
Negative | IB | ||||
Negative | Positive | ||||
Negative | IIA | ||||
Negative | Positive | Positive | IA | ||
Negative | IB | ||||
Negative | Positive | ||||
Negative | IIA | ||||
G2 | Positive | Positive | Positive | IA | |
Negative | IB | ||||
Negative | Positive | ||||
Negative | IIA | ||||
Negative | Positive | Positive | IA | ||
Negative | IIA | ||||
Negative | Positive | ||||
Negative | |||||
G3 | Positive | Positive | Positive | IA IIA | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IB | ||
Negative | IIA | ||||
Negative | Positive | ||||
Negative | |||||
T2 N1 M0 T3 N0 M0 | G1 | Positive | Positive | Positive | IA |
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IA | ||
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
G2 | Positive | Positive | Positive | IB | |
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IB | ||
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
G3 | Positive | Positive | Positive | IB | |
Negative | IIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IIA | ||
Negative | IIB | ||||
Negative | Positive | ||||
Negative | IIIA | ||||
T0 N2 M0 T1 N2 M0 T2 N2 M0 T3 N1 M0 T3 N2 M0 | G1 | Positive | Positive | Positive | IB |
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IB | ||
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
G2 | Positive | Positive | Positive | IB | |
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IB | ||
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | IIIB | ||||
G3 | Positive | Positive | Positive | IIA | |
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IIA | ||
Negative | IIIA | ||||
Negative | Positive | ||||
Negative | IIIC | ||||
T4 N0 M0 T4 N1 M0 T4 N2 M0 Any T N3 M0 | G1 | Positive | Positive | Positive | IIIA |
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IIIA | ||
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | |||||
G2 | Positive | Positive | Positive | IIIA | |
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | IIIA | ||
Negative | IIIB | ||||
Negative | Positive | ||||
Negative | IIIC | ||||
G3 | Positive | Positive | Positive | IIIB | |
Negative | |||||
Negative | Positive | ||||
Negative | |||||
Negative | Positive | Positive | |||
Negative | IIIC | ||||
Negative | Positive | ||||
Negative | |||||
Any T Any N M1 | Any | Any | Any | Any | IV |
ER=estrogen receptor; PR=progesterone receptor | |||||
|
|
| |
Tamoxifen | 20 mg PO every day |
| Elacestrant | 345 mg PO every day |
| |
Aromatase inhibitor | |
Anastrozole | 1 mg PO every day |
Letrozole | 2.5 mg PO every day |
Exemestane | 25 mg PO every day |
| |
Fulvestrant | 500 mg IM on days 1, 15, 29, and once monthly thereafter |
| |
Megestrol | 40 mg PO 4 times a day |
| |
Tamoxifen | 20 mg PO every day |
| |
Aromatase inhibitor + LHRH* | |
Leuprolide | 7.5 mg IM depot q28d 22.5 mg IM q3mo 30 mg IM q4mo |
Goserelin | 3.6 mg SC depot q28d 10.8 mg SC q3mo |
Megestrol | 40 mg PO 4 times a day |
*LHRH = luteinizing hormone–releasing hormone. | |
|
|
|
|
|
| Abemaciclib | CDK inhibitor | 200 mg PO BID continue until disease progression | 19.7% | Diarrhea, fatigue, neutropenia and nausea |
| Alpelisib | PI3K inhibitor | 300 mg PO qDay continue until disease progression | 26.6% | Hypersensitivity, diarrhea, cutaneous adverse reactions, hyperglycemia |
Capecitabine | Oral fluoro-pyrimidine | 1250 mg/m²/d PO for 2 weeks with 1 wk off | 30% | Rash, hand-foot syndrome, diarrhea, mucositis |
Docetaxel | Antimicrotubule | 75-100 mg/m² IV q3wk or 40 mg/m²/wk X IV for 6 wk with 2 wk off | 30-68% | Myelosuppression, alopecia, skin reaction, mucositis, and fluid retention |
Doxorubicin | Anthracycline (antitumor antibiotic) | 45-60 mg/m² IV q3wk or 20 mg/m² IV qwk (not to exceed a cumulative dose of 450-500 mg/m²) | 35-50% | Myelosuppression, nausea/ vomiting, mucositis, diarrhea cardiotoxicity, alopecia |
Doxil (liposomal encapsulated doxorubicin) | Anthracycline | 20 mg/m² IV q2wk or 35-40 mg/m² IV q4wk |
| Less cardiotoxicity, neutropenia, alopecia, stomatitis, hand-foot syndrome |
Epirubicin | Anthracycline | 90 mg/m² IV q3wk (not to exceed cumulative dose of 900 mg/m²) | 35-50% | Myelosuppression, mucositis, nausea, vomiting, cardiotoxicity |
| Everolimus | mTor kinase inhibitor | 10 mg PO qDay continue until disease progression | 12.6% | Stomatitis, constipation, infection, asthenia, fatigue, cough |
Gemcitabine | Antimetabolite | 725 mg/m²/wk IV for 3 wk then 1 wk off or 1 g/m²/wk IV X 2 then 1 wk off |
| Myelosuppression, nausea/ vomiting, flulike syndrome, elevated LFTs |
Nab-paclitaxel | Antimicrotubule | 80-100 mg/m²/wk IV X 3 then 1 wk off or 260 mg/m² IV q3wk | 58-62% 33% | Less neuropathy, and allergic reaction |
| Olaparib | PARP inhibitor | 300 mg PO BID | 59.9% | Anemia, fatigue, nausea, and vomiting |
Paclitaxel | Antimicrotubule | 80 mg/m²/wk IV or 175 mg/m² IV over 3 hours q3wk | 25-50% | Myelosuppression, alopecia, neuropathy, allergic reaction |
Pertuzumab | Monoclonal antibody | 840 mg IV loading dose, then 420 mg q3wk Give with trastuzumab and docetaxel | 80.2% (objective response rate) | Fever, allergic reaction, cardiotoxicity/congestive heart failure |
Palbociclib | CDK inhibitor | 125 mg/day PO for 3 weeks with 1 wk off Give with letrozole | Data are not available for ORR Mean PFS was 10.2 months in the letrozole group and 20.2 months for palbociclib plus letrozole group | Neutropenia, leukopenia, thrombocytopenia, anemia, stomatitis |
| Ribociclib | CDK inhibitor | 600 mg/day PO for 3 weeks with 1 wk off Give with letrozole | Mean PFS was 16 months in the letrozole group and 25.3 months for ribociclib | QT prolongation, hepatobiliary toxicity, neutropenia, alopecia, diarrhea, vomiting, constipation, fatigue, anorexia |
| Sacituzumab govitecan | Monoclonal antibody | 10 mg/kg IV on Days 1 and 8 with 2 wk off | 33.3% | Nausea, neutropenia, diarrhea, fatigue, anemia, vomiting |
| Talazoparib | PARP inhibitor | 1 mg PO qDay | 62.6% | Fatigue, anemia, nausea, neutropenia, headache, thrombocytopenia, vomiting, alopecia, diarrhea, and decreased appetite |
Trastuzumab or biosimilars of trastuzumab | Monoclonal antibody | Combination therapy: 4 mg/kg IV once, then 2 mg/kg weekly for 12-18 weeks, then 6 mg/kg q3weeks to total 52 weeks Single agent: 8 mg/kg IV once, then 6 mg/kg q3weeks to total 52 weeks | 10-15% | Fever, allergic reaction, cardiotoxicity/congestive heart failure |
| Trastuzumab deruxtecan ] | Monoclonal antibody conjugate | 5.4 mg/kg IV q3weeks | 60.3% | Interstitial lung disease and pneumonitis; neutropenia; left ventricular dysfunction |
| Tucatinib ] | Tyrosine kinase inhibitor of HER2 | 300 mg PO BID | 40.6% | Diarrhea, hand-foot syndrome, nausea, fatigue, hepatotoxicity |
Vinorelbine | Vinca alkaloid | 20 mg/m²/wk IV | 35-45% | Myelosuppression, nausea/ vomiting, constipation, fatigue, stomatitis, anorexia |
|
|
|
| ||
Capecitabine Docetaxel | 1250 mg/m² bid days 1-14 75 mg/m² day 1 | Repeat cycle every 21 days May decrease capecitabine dose to 850-1000 mg/m² to reduce toxicity risk |
| ||
Capecitabine Paclitaxel | 825 mg/m² bid days 1-14 175 mg/m² day 1 | Repeat cycle every 21 days |
| ||
Capecitabine Navelbine | 1000 mg/m² bid days 1-14 25 mg/m² days 1 and 8 | Repeat cycle every 21 days |
Gemcitabine ] Paclitaxel | 1250 mg/m² days 1 and 8 175 mg/m² day 1 | Repeat cycle every 21 days |
Carboplatin ] Paclitaxel | AUC of 6 day 1 200 mg/m² day 1 | Repeat cycle every 21 days |
Carboplatin ] Docetaxel | AUC of 6 day 1 75 mg/m² day 1 | Repeat cycle every 21 days |
Palbociclib ] Letrozole | 125 mg PO once daily days 1-21 2.5 mg PO once daily days 1-28 | Repeat cycle every 28 days |
Palbociclib Fulvestrant | 125 mg PO once daily days 1-21 500 mg IM on days 1, 15, 29 and once monthly thereafter | Repeat cycle every 28 days |
Ribociclib ] Letrozole | 600 mg PO once daily days 1-21 2.5 mg PO once daily days 1-28 | Repeat cycle every 28 days |
Paclitaxel ] | 90 mg/m² day 1, 8, and 15 | Repeat cycle every 28 days |
Abemaciclib Fulvestrant ] | 150 mg PO BID 500 mg IM on Days 1, 15 and 29 and once monthly thereafter | Repeat cycle every 28 days |
Ribociclib ] Fulvestrant | 600 mg PO once daily days 1-21 500 mg IM on Days 1, 15 and 29 and once monthly thereafter | Repeat cycle every 28 days |
| ||
Trastuzumab Paclitaxel | 4 mg/kg loading dose then 2 mg/kg weekly 80 mg/m² IV weekly |
|
Trastuzumab Docetaxel | 8 mg/kg loading dose then 6 mg/kg day 1 100 mg/m² IV day 1 | Repeat cycle every 21 days |
Pertuzumab/trastuzumab/hyaluronidase Docetaxel | Loading dose of 1,200 mg pertuzumab/600 mg trastuzumab SC x 1 dose followed by 600 mg pertuzumab/600 mg trastuzumab SC Docetaxel is 75 mg/m IV, may escalate to 100 mg/m | Repeat cycle every 3 week; continue until disease recurrence or unmanageable toxicity, whichever occurs first |
Trastuzumab Vinorelbine | 4 mg/kg loading dose then 2 mg/kg weekly 25 mg/m² day 1 weekly |
|
Trastuzumab Capecitabine Tucatinib ] | 8 mg/kg loading dose then 6 mg/kg weekly 1000 mg/m2 PO BID days 1-14 300 mg PO BID | Repeat cycle every 21 days |
Lapatinib Capecitabine | 1250 mg PO daily 2000 mg/m² daily days 1-14 | Repeat cycle every 21 days |
Paclitaxel Lapatinib | 175 mg/m 1500 mg/d | Repeat cycle every 3 weeks |
AUC = area under the curve (systemic exposure) References for chemotherapy regimens: XT, ] XP, ] XN, ] HER2-positive metastatic breast cancer regimens , , , ] | ||
|
|
|
History and physical examination | Year 1, every 3-4 mo Year 2, every 4 mo Year 3-5, every 6 mo Year 6+, annually | Year 1-3, every 3-6 mo Year 4-5, every 6-12 mo Year 6+, annually |
Breast self-examination | No recommendation | Counseled to perform monthly breast self-examination |
Mammography | 6 mo after post-BCS radiation therapy Annually thereafter | 6 mo after definitive radiation therapy Every 6-12 mo for surveillance of abnormalities Annually if stability of abnormalities is achieved |
Pelvic examination | Annually, for women on tamoxifen Annual exam if uterus present | Regular gynecologic follow-up Patients on tamoxifen should be advised to report any vaginal bleeding |
Routine blood tests | Not recommended | Not recommended |
Imaging studies | Not recommended | Not recommended |
Tumor marker testing | Not recommended | Not recommended |
Women aged ≥65 years |
Woman aged 60-64 years with ≥1 of the following: 1. Family history of osteoporosis 2. Low body weight 3. Prior nontraumatic fracture 4. Other risk factors (eg, smoking, sedentary lifestyle) |
Postmenopausal women on aromatase inhibitors |
Premenopausal women who develop treatment related premature menopause |
Contributor Information and Disclosures
Pavani Chalasani, MD, MPH Professor of Medicine, Director, Division of Hematology and Oncology, Leader, Breast Cancer Clinical Research Team, Co-Program Leader, Clinical and Translational Oncology Program, George Washington Cancer Center, George Washington University School of Medicine and Health Sciences Pavani Chalasani, MD, MPH is a member of the following medical societies: American Association for Cancer Research , American College of Physicians , American Society of Clinical Oncology , American Society of Hematology , Hemostasis and Thrombosis Research Society , SWOG Disclosure: Serve(d) as a director, officer, partner, employee, advisor, consultant or trustee for: Bayer, Heron, Amgen, Athenex, Novartis, Eisai, Eli Lilly, Zentalis <br/>Received research grant from: Pfizer.
Abigail Camenisch, BS, MPH MD Candidate, University of Arizona College of Medicine Disclosure: Nothing to disclose.
John V Kiluk, MD, FACS Associate Professor, Department of Oncologic Sciences, Department of Surgery (Joint Appointment), University of South Florida Morsani College of Medicine; Clinical Director, Breast Surgical Oncology, Associate Member, Comprehensive Breast Program, Department of Women's Oncology, H Lee Moffitt Cancer Center and Research Institute John V Kiluk, MD, FACS is a member of the following medical societies: American College of Surgeons , American Society of Breast Surgeons , Moretz Surgical Society, Society of Surgical Oncology , Southeastern Surgical Congress Disclosure: Nothing to disclose.
Alison T Stopeck, MD Professor of Medicine, Arizona Cancer Center, University of Arizona Health Sciences Center; Director of Clinical Breast Cancer Program, Arizona Cancer Center; Medical Director of Coagulation Laboratory, University Medical Center; Director of Arizona Hemophilia and Thrombosis Center Alison T Stopeck, MD is a member of the following medical societies: American Association for Cancer Research , American College of Physicians , American Society of Hematology , SWOG , American Society of Clinical Oncology , Hemophilia and Thrombosis Research Society Disclosure: Received honoraria from Genentech for speaking and teaching; Received honoraria from AstraZeneca for speaking and teaching; Received grant/research funds from AstraZeneca for other.
Patricia A Thompson, PhD Assistant Professor, Department of Pathology, University of Arizona College of Medicine Disclosure: Nothing to disclose.
Leona Downey, MD Assistant Professor of Internal Medicine, Section of Oncology and Hematology, University of Arizona, Arizona Cancer Center
Leona Downey, MD is a member of the following medical societies: American Geriatrics Society , American Society of Clinical Oncology , and Southwest Oncology Group
Disclosure: Nothing to disclose.
Manjit Singh Gohel, MD, MRCS, MB, ChB Specialist Registrar, Division of Breast and Endocrine Surgery, Northwick Park Hospital
Harold Harvey, MD Professor, Department of Medicine, Pennsylvania State University
Kanchan Kaur, MBBS, MS (General Surgery), MRCS (Ed) Consulting Breast and Oncoplastic Surgeon, Medanta, The Medicity, India
Julie Lang, MD Assistant Professor of Surgery and the BIO5 Institute, Director of Breast Surgical Oncology, University of Arizona College of Medicine
Julie Lang, MD is a member of the following medical societies: American College of Surgeons , American Society of Breast Surgeons, American Society of Clinical Oncology , Association for Academic Surgery , and Society of Surgical Oncology
Disclosure: Genomic Health Grant/research funds Speaking and teaching; Agendia Grant/research funds Speaking and teaching; Surgical Tools Grant/research funds Research; Sysmex Grant/research funds Research
Robert B Livingston, MD Professor of Clinical Medicine and Director, Clinical Research Shared Services, Arizona Cancer Center
Robert B Livingston, MD is a member of the following medical societies: American Association for Cancer Research , American Federation for Clinical Research, and American Society of Clinical Oncology
Hanan Makhoul, MD Staff Physician, Department of Internal Medicine, University of Arkansas School of Medicine
Issam Makhoul, MD Associate Professor, Department of Medicine, Division of Hematology/Oncology, University of Arkansas for Medical Sciences
Issam Makhoul, MD is a member of the following medical societies: American Society of Clinical Oncology and American Society of Hematology
Robert C Shepard, MD, FACP Associate Professor of Medicine in Hematology and Oncology at University of North Carolina at Chapel Hill; Vice President of Scientific Affairs, Therapeutic Expertise, Oncology, at PRA International
Robert C Shepard, MD, FACP is a member of the following medical societies: American Association for Cancer Research , American College of Physician Executives , American College of Physicians , American Federation for Clinical Research, American Federation for Medical Research , American Medical Association , American Medical Informatics Association , American Society of Hematology , Association of Clinical Research Professionals , Eastern Cooperative Oncology Group , European Society for Medical Oncology , Massachusetts Medical Society , and Society for Biological Therapy
Hemant Singhal, MD, MBBS, FRCSE, FRCS(C) Senior Lecturer, Director of Breast Service, Department of Surgery, Imperial College School of Medicine; Consultant Surgeon, Northwick Park and St Marks Hospitals, UK
Hemant Singhal, MD, MBBS, FRCSE, FRCS(C) is a member of the following medical societies: Royal College of Physicians and Surgeons of Canada and Royal College of Surgeons of Edinburgh
Carl V Smith, MD The Distinguished Chris J and Marie A Olson Chair of Obstetrics and Gynecology, Professor, Department of Obstetrics and Gynecology, Senior Associate Dean for Clinical Affairs, University of Nebraska Medical Center
Carl V Smith, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Association of Professors of Gynecology and Obstetrics , Central Association of Obstetricians and Gynecologists , Council of University Chairs of Obstetrics and Gynecology , Nebraska Medical Association , and Society for Maternal-Fetal Medicine
Wiley Souba, MD Chairman, Professor, Department of General Surgery, Pennsylvania State College of Medicine; Chief Surgeon, The Milton S Hershey Medical Center
Rachel Swart, MD, PhD Assistant Professor of Medicine, Department of Hematology and Oncology, Arizona Cancer Center, University of Arizona
Rachel Swart, MD, PhD is a member of the following medical societies: American Association for Cancer Research , American Society of Clinical Oncology , Arizona Medical Association , and Southwest Oncology Group
Disclosure: Roche Grant/research funds Other
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Simon Thomson, MB, BCh, MD, FRCS Specialist Registrar, Department of Breast and Endocrine Surgery, Northwick Park Hospital, UK
Simon Thomson, MB, BCh, MD, FRCS is a member of the following medical societies: British Medical Association
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Breast Cancer Histology
- Breast Cancer
- Male Breast Cancer Imaging
- Fast Five Quiz: Unusual Breast Cancer Presentations
- Breast Cancer Survivorship in Veterans
- Breast Cancer Ultrasonography
- Patient Simulation: A 63-Year-Old Woman With Metastatic Breast Cancer
- A Benefit to Add-On Abemaciclib in Advanced Breast Cancer?
- Could Aspirin Help Treat Breast Cancer?
- Intermediate Endpoints Predict Breast Cancer Survival

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2010/viewarticle/942912 Fast Five Quiz: What to Know About Early-Stage Breast Cancer

- 2001/viewarticle/1000633 ASCO 2024: Addressing Unmet Needs in Early Breast Cancer
- 2001/viewarticle/1000586 ASCO 2024: Anticipating Advancements in Metastatic Breast Cancer

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Breast cancer case study
Published by Gianna Herbertson Modified over 10 years ago
Similar presentations
Presentation on theme: "Breast cancer case study"— Presentation transcript:
This short questionnaire will help to determine whether there may be a gene in your family connected to an increased risk of the development of bowel.
What Do We Do? Cancer Genetics Service for Wales.
What if the patient wants answers... (and you don’t have them) Dr Geraldine Swift and Dr Sonia Mangwana.
Hereditary GI Cancer Syndromes: Keys to identify high risk patients

HEALTHY PEOPLE. Aims Interpret evidence about a screening programme and decide whether it is worthwhile – for individuals or groups Demonstrate an.
Which of the following increases a women’s risk for Breast Cancer? A.Starting her menses at age 14 or older B.Breastfeeding C.Extremely dense breast tissue.
Genetics and genomics for healthcare © 2014 NHS National Genetics and Genomics Education Centre Why is genetics relevant to.
Level 8 - undergraduate students Breast cancer case study Enter resource.
Princess Alexandra Hospitals NHS Trust Breast Unit Family History Clinic.
10 November 2011 Genetic counseling for breast cancer risk Aichu Huang, MS. CGC. Department of Medical Genetics National Taiwan University Hospital.
The Genetics of Breast and Ovarian Cancer Susceptibility Patricia Tonin, PhD Associate Professor Depts. Medicine, Human Genetics & Oncology McGill University.
Breast Cancer Risk and Risk Assessment Models
1 Development of Hereditary Cancer Prevention Measures in Pskov Region Asoc. Prof. Edvīns Miklaševičs, Riga Stradins University 16 November 2011, St.Petersburg,
Cancer Genetics for Primary Care Sara Levene Registered Genetic Counsellor.
Few more cases Cancer and cholesterol. Cancer and genetic testing Available guidance (NICE) Familial breast cancer /colonic/ovarian Familial Hypercholesteremia.
Breast Cancer 101 Barbara Lee Bass, MD, FACS Professor of Surgery
Breast Cancer By Kajal Haghmoradi.
The Facts about Breast Cancer
Promoting Excellence in Family Medicine Enabling Patients to Access Electronic Health Records Guidance for Health Professionals.

Ovarian Cancer Awareness In the Community. Facts about Ovarian Cancer 80% of cases occur in women over th most common cancer in women Almost 7000.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Patient Mrs. B.C. is a 56 year old female who is presenting to her WHNP for her annual exam. She had to cancel her appointment two months ago and didn’t reschedule until now. Her last pap smear and mammogram were normal. Today, while performing her breast exam, her nurse practitioner notices dimpling in the left breast as the patient raises her arms over her head. When the NP mentions it to Mrs. B.C. she is surprised and denies noticing it before today. A firm, non-tender, immobile nodule is palpated in the upper quadrant of her breast . The NP then asks Mrs. B.C. how frequently she is performing breast self-exams, she admits to only doing them randomly when she remembers, which is about every few months. She reports no recent or abnormal drainage from her breast. Further examination reveals palpable axillary lymph nodes.
Mrs. B.C. is about 30 pounds overweight and walks her dog around her neighborhood every morning before work and every evening when she gets home. She reports drinking a glass of white wine before bed each night. She denies any history of tobacco use. She reports use of a combination birth control pill on and off for 25 years until she reached menopause. She is not currently taking any prescription medications.
Past Medical History
- Menarche (Age 10)
- Post-menopausal (Age 53)
- No other pertinent medical history
Family History:
- Father George- deceased from stroke (75 years old), history of hypertension, CAD, HLD
- Mother Maryanne alive- 76 years old, history of dementia, osteoporosis
- Brother Michael- alive, 57 years old, history of hypertension, CAD and cardiac stent placement (54 years old)
- Sister, Michelle- alive 53 years old, history of GERD, Asthma
- Brother- Jimmy- alive 50 years old, no past medical history
Social History:
Mrs. B.C. works Monday-Friday 8am-5pm at the local dentist’s office at the front desk as a schedule coordinator. She is planning to retire in a few years. In her spare time, she is involved in various community efforts to feed the homeless and helps to prepare dinners at her local church one night a week. She also enjoys cooking and baking at home, gardening, and nature photography.
Mrs. B.C. has two children. Her oldest son, Patrick, is 21 years old and is in his final year of pre-med. He is attending a public university about 2 hours away from home where he lives year-round. As an infant, Patrick was breastfed until 18 months when he self-weaned. Her daughter, Veronica, is 19 years old and lives at home while attending the local branch campus of a state university. She is in her second year of a business degree and then plans to transfer to the main campus next year. When Veronica was an infant she had difficulty latching onto the breast due to an undiagnosed tongue and lip ties resulting in Mrs. BC exclusively pumping and bottle feeding for six months. After six months, Mrs. B.C. was having a hard time keeping up while working and her found her supply diminished. Veronica had begun eating solid foods so Mrs. B.C. switched to supplemental formula, which was a big relief.
Mrs. B.C. was married to her now ex-husband Kent for 26 years. They divorced two years ago when Veronica was a senior in high school. They have remained friends and Kent lives 25 minutes away in a condo with his girlfriend. She also has two brothers who live nearby and a sister who lives out of state. Her 7 nieces and nephews range in age from 9 years old to 26 years old. Her father, George, passed away from a sudden stroke 4 years ago. Her mother, Maryanne, has dementia and is living in a nearby memory care facility. She also has many close friends.
- Pop Culture
- Family Feud
- Father’s Day
Breast Cancer Powerpoint Templates and Google Slides Themes
Discover a collection of beautifully designed presentation templates tailored to raise awareness and support for Breast Cancer initiatives.
- Agenda (25)
- Background (21)
- Creative (24)
- Feminine (16)
- Solid Color (18)
- Business (17)
- Creative Agency (15)
- Education (18)
- Marketing (18)
- Medical (17)
- Nonprofit (34)
Explore Free Breast Cancer Presentation Templates

Doodle Cancer Awareness Social Media Campaign Slides
Immerse your audience in an engaging, creative journey with this PowerPoint and Google Slides template specifically designed for marketing professionals. ... Read more
Retro Illustrated Breast Cancer Brochure Slides
Take your awareness campaign to the next-level with our vibrant Powerpoint and Google Slides templates. Geared towards marketers, our unique, ... Read more
Illustrated Breast Cancer Case Slides
Bring your awareness campaign to life with our pink, geometric style awareness slides template. Tailored for marketing teams, it’s a ... Read more

Illustrated Breast Cancer Healthcare Center Slides
Brighten up your message with our Pink Vibrancy Healthcare Awareness PowerPoint Template. This modern, clean design is perfect for marketing ... Read more

Cute Breast Cancer Information Brochure Slides
Grab your audience’s attention with our retro-styled, power-packed Powerpoint templates specifically designed for campaigning. Hues of pink and purple and ... Read more

Illustrated Breast Cancer Prevention Campaign Slides
The Vibrant Breast Cancer Campaign Slides template is a tastefully illustrated, pop art-inspired deck. Perfect for marketing professionals, this eye-catching ... Read more

Elegant Minimal Breast Cancer Awareness Slides
Embark on your Breast Cancer Awareness campaign with our dignified and sophisticated Powerpoint and Google Slides templates. Crafted in a ... Read more
Minimal Breast Cancer Awareness Month Slides
Revamp your marketing strategies with this highly customizable, photo-centric PowerPoint and Google Slides template. Perfectly tailored for marketers aiming to ... Read more

Illustrated Breast Cancer Treatment Breakthrough Slides
Boost the visibility of your visionary breast cancer therapy with our Powerpoint and Google Slides templates. Specifically designed for marketers, ... Read more
Bold World Breast Cancer Newsletter Slides
Make an impact with your next breast cancer awareness event with our dynamic Powerpoint and Google Slides template. Catering specifically ... Read more

Pink and Beige Breast Cancer Awareness Slides
Vibrant and soothing, these breast cancer awareness slides are easy to use as a Google Slides template, PowerPoint theme or ... Read more

Pastel Illustrative Floral Doodles Prenatal Healthcare Education Slides
Help your audience stay healthy and informed with these prenatal healthcare slides, easy to use as a Google Slides template, ... Read more

Pastel Illustrations and Doodles Healthcare Center Slides
Make your message easy on the eyes with these pastel healthcare center slides, perfect as a Google Slides template, PowerPoint ... Read more

Blue Simple Gradient Professional Medical Center Slides
Spread the word about your business with these professional medical center slides, easy to use as a Google Slides template, ... Read more
Pink and Purple Colorblock Geometric Bold Floral Resume Slides
Time to switch jobs? Make it a smooth process with a floral resume template, simple to use as a Google ... Read more
Professional designs for your presentations
SlidesCarnival templates have all the elements you need to effectively communicate your message and impress your audience.
Suitable for PowerPoint and Google Slides
Download your presentation as a PowerPoint template or use it online as a Google Slides theme. 100% free, no registration or download limits.
- Google Slides
- Editor’s Choice
- All Templates
- Frequently Asked Questions
- Google Slides Help
- PowerPoint help
- Who makes SlidesCarnival?
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Case Presentation on Locally Advanced breast Cancer

Related Papers
European Respiratory Journal
Annelies Rappaport
International Journal of Women's Health
Nicole Sandhu
Although much emphasis has been placed on the primary presentations of breast cancer, little focus has been placed on how systemic illnesses may affect the breast. In this article, we discuss systemic illnesses that can manifest in the breast. We summarize the clinical features, imaging, histopathology, and treatment recommendations for endocrine, vascular, systemic inflammatory, infectious, and hematologic diseases, as well as for the extramammary malignancies that can present in the breast. Despite the rarity of these manifestations of systemic disease, knowledge of these conditions is critical to the appropriate evaluation and treatment of patients presenting with breast symptoms.
Diagnostic Histopathology
Sarah Pinder
IOSR Journals
Background: Benign breast ds (BBD) are common disease affecting woman mainly. These can be diagnosed by triple assessment including clinical examination, radiological imagings, and a pathological examination. Majority of the benign lesions are not associated with an increased risk for subsequent breast cancer but some may have increased risk of malignancy like atypical hyperplasia. The main problem from women’s patient of view is fear that such a lump may be a cancer. Unlike breast cancer, benign breast diseases have often been difficult to understand, in part due to variety of names that have been used to describe the various conditions. So that clinician requires in-depth knowledge to give clear explanation about breast diseases. Making an early diagnosis and planning the treatment during initial consultations, helps in alleviating unnecessary anxiety about breast cancer and unnecessary long term follow up can be avoided. So, the need for study is to analyze the spectrum of benign breast disease. Method: A total 85 patients diagnosing as benign breast diseases under the inclusion criteria were studied during the period of Oct 2014 to March 2016; in the Dept of Surgery at People’s hospital of People’s college of medical science and research center, Bhopal. Our study objectives were A. To describe the spectrum of Benign Breast Diseases with Respect to Age of incidence, Social Demography, Duration of Symptoms, Site of lumps, Clinical features specific to conditions. B. To diagnose clinically and cytologically (FNAC) Suitable patients with benign breast disease and provide either conservative or operative treatment. C. To do histopathological examination of excised specimen for the comparisons and confirmation of cytological and clinical diagnosis. Result: Fibro adenoma was the most common benign lesion encountered (65.9%) followed by Breast Abscess 18.8% disease. Fibro adenoma was presented most often in the second and third decade (75%). Lump in the breast was the commonest presentation of BBD, Lump and Mastalgia was the second commonest symptom of BBD. There was a slight preponderance of lesions in the right breast (45.9%) as compared to left breast (44.7%), shown to be significant. Most of patients belong to middle class. 100% 0f the patients were in pre menopausal group. Majority (45.9%) of lesions were of the size 2-5 cms, 31.8% were between 6-10 cms FNAC highly reliable for fibro adenoma than for other lesions. All fibro adenomas willing for surgical procedure were managed by simple excision than follow up. All 16 cases of Breast Abscess underwent incision and drainage and simple mastectomy was done in phylloide tumors. Conclusion: In the present study BBD occupy majority of total breast diseases. Fibro adenoma was the most common benign lesion (65.9%). FNAC was highly accurate and was highly reliable for fibro adenoma than for other lesions. Triple test is a prerequisite for determining management. However all fibro adenomas willing for surgical procedure were managed by simple excision than follow up. Conservative approach is acceptable in young patients, who choose conservative management, need to be informed about the limitation of the test, advised for proper follow up, and must be assessed properly if there are symptoms and clinical changes. Breast self examination should be emphasized as a part of female adult education.
Siniša Franjić
In most women, breast pain is not severe and disappears very quickly on its own. Severe pain, which is rare, can be relieved with medication. Benign breast diseases are common in young and older women, and malignant breast diseases most commonly occur around and after menopause. Although much rarer than benign changes, breast cancers are the most common cancers in women and represent a significant health problem. When she feels pain in her breast, the woman immediately thinks she has got breast cancer. Pain is not always a symptom of cancer. This paper discusses breast cancer, as the most common type of cancer in women, but also some other breast diseases that are not so common.
The Western journal of medicine
william goodson
Sushil Kachewar
Purpose: Cystic breast lesions are a common finding in young as well as elderly females. Although, mostly benign; they can at times be malignant too. Timely diagnosis is possible with help of Fine needle aspiration cytology (FNAC). This study was carried out with the aim of studying the panorama of various cystic breast lesions on FNAC in our setup. Materials and Methods: This was a four year prospective study carried out from May 2010 to January 2014. Cystic nature of breast mass was confirmed by palpation and by sonomammography. FNAC was then performed and the smears were stained with MGG and Papanicolaou stain. Results: Out of the 72 cases that were diagnosed to be cystic breast lesions clinically or on sonomammography, 64 were found to be benign and 08 were found to be malignant on FNAC. Retrospective imaging correlation of the 08 cystic cases revealed that they were of complex cystic nature and had either thick septae(03), solid areas (04) or dense contents (01) within. This in...
Scholar Science Journals
Background: Study of pattern of benign breast disease is a challenge due to variants in occurrence and presentation in different age groups and different geographical areas. The objective is to study the clinical profile and pattern of benign breast disease and its pathological correlation. Methods: This is a prospective study of females with breast disease presenting to surgery department over a period of one year. This survey was mainly meant for studying the age distribution, to evaluate the different types of benign diseases of the breast, their mode of clinical presentation and pathology and to evaluate the various modes of management for different types of Benign Breast Diseases. Patients with obvious malignancy and males were excluded from the study. Results: A total of 100 females were included in the study. Fibroadenoma (37%) and fibroadenosis (23%) were the commonest diseases,both presenting mostly at 21-30years of age. Left side involvement was most common. The commonest presentation was breast lump which comprised 84 (84%) cases, out of which 26 (26%) had associated complaints like breast pain and nipple discharge. Conclusion: Benign breast diseases are common problems of 2nd and 3 rd decade in females and raises considerable fear of malignancy. The patients of BBDs generally present with one or more of these complaints – breast lump, breast pain or nipple discharge. All the patients with discrete breast lumps should undergo a triple assessment to make an early diagnosis.
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Yonsei Medical Journal
Journal of Mammary Gland Biology and Neoplasia
Corinne Balleyguier
European Journal of Cancer Care
Yazan Masannat
ANZ Journal of Surgery
Melek Yavuz
International Surgery Journal
Poonam Shingade
Tushar Ahir
International Journal of Surgery Case Reports
Cristovam Neto
Diagnostic Pathology
Arshad Malik
Advances in Dermatology and Allergology
Laboratory Investigation
Mônica Maria Ágata Stiepcich
Reports — Medical Cases, Images, and Videos
Zois Margelis
Journal of Rawalpindi Medical College
Usman Qureshi
Faruk Skenderi
The Breast Journal
Nasim Ahmadiyeh
International Journal of Reproduction, Contraception, Obstetrics and Gynecology
Mayank Kapoor
RadioGraphics
Sofia Torrubia
Mayo Clinic Proceedings
Aziza Nassar
Archives of pathology & laboratory medicine
Richard Cote
Kathryn Malherbe
Spyridon Marinopoulos
Mojtaba Sepandi
European Journal of Radiology Extra
Jeanie Choi
Nature Clinical Practice Oncology
Mukesh Harisinghani
Breast Care
Katsuyuki Kiura
The Oncologist
Merih Guray
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Case Study 63: Cancer of the Female Breast
Dec 21, 2019
170 likes | 242 Views
Case Study 63: Cancer of the Female Breast. By Robyn Schwartz. Case Background. 46, premenopausal Dense breasts Has noticed cysts in the past Noticed new lump in upper right quadrant Did not resolve Got bigger Denied lumps in axillary. Patient history. Happily married for 21 years
Share Presentation

Presentation Transcript
Case Study 63: Cancer of the Female Breast By Robyn Schwartz
Case Background • 46, premenopausal • Dense breasts • Has noticed cysts in the past • Noticed new lump in upper right quadrant • Did not resolve • Got bigger • Denied lumps in axillary
Patient history • Happily married for 21 years • 3 kids (3, 8, and 10) • Does breast self exams • Normal pap 2 years ago • Has Asthma and hypertension • Exercises • No tobacco, alcohol or illegal drugs
Risk Factors • All 3 kids born after the age of 35 • First period at 11yr old • Dense breasts • Cysts already develop regularly • Family history of breast cancer • Paternal grandmother diagnosed at age 45 before menopause • Mother diagnosed at age 45 before menopause. Died at age 73 from reoccurrence of breast cancer
Breast Cancer: What is it? • Uncontrolled division of abnormal cells in the breast • Caused by specific mutations • BRCA1 and BRCA2 • TP53
Our patient: Mammogram • 2.3cm x 2.9cm x 3.2cm mass • Irregular borders • Skin thickening • Enlarged axillary lymph node • 6 Y-shaped microcalcifications extended toward nipple • Abnormal mass into pectoral muscle
Grading vs Staging • How far the cancer has spread • I, II, III, IV • Based on • Size of tumor • Invasive vs non invasive • Spread to lymph nodes • Spread to other parts of the body • How abnormal the cells are • 1, 2, 3,4 • Based on • Tubule formation • Size and shape of cells • Mitotic division • Measures the likely aggressiveness of the cells
Grading tumors Nuclear (size/shape) Score 1: little variation in size Score 2: moderate variability, open vesicular nuclei Score 3: lots of variability open nuclei Mitotic Score 1: <7 mitoses Score 2: 8-14 mitoses Score 3: >14 mitoses Tubular differentiation Score 1: > 75% glandular/tubular Score 2: 10-75% glandular/tubular Score 3: < 10% Glandular/ tubular
Staging Cancer • agrdjdytydstasf Stage 0: No Cancer Stage I: IA: Cancer is small, low grade and localized IB: Cancer is large, low grade and localized Stage II: IIA: Tumor is 2-5cm but has not spread IIB: Tumor is 2-5cm but has spread to lymph nodes Stage III: Tumor is larger than 5cm and has spread to multiple lymph nodes Stage IV: Cancer has spread to other parts of the body
Our Patient: Biopsy and ultrasound • Ultrasound: • Non-cystic mass, solid appearing • Abnormal vascularity • Some skin thickening and mild tissue edema • Biopsy: • Consistent with infiltrating breast cancer • 3-5 divisions per high power field • Mild pleomorphism • Positive for estrogen and progesterone receptors
Grade and Stage • Grade 1 • Mitotic score: 1 (<7 divisions) • Glandular Score: 1 (75% glandular) • Nucleic Score: 1 (not much change) • Total score: 3 • 10 year survival rate 90% • Stage IIB • Small • Spread to 1 lymph node • 5 year survival rate of 71%
Our Patient: Treatment • Breast conservation therapy • Lump removal • Radiation • Lymph node biopsy • Tamoxifen • Estrogen receptor blocker • Helps stop growth of cancer cells
Our Patient: Follow Up • 6.5 years cancer free • 80 months later, complained of • bone pain in lower back • Headache
Test Results • Bone scan • Lesions in lumbar spine without fracture • Chest X-Ray • 3 small nodules in upper lobe of left lung • Brain MRI • Small mass in right frontal lobe • Abdominal CT • Negative • Blood tests • CEA elevated by 2-fold • CA27-29 concentration elevated by 2-fold
Diagnosis, Outlook, and Treatment • Stage IV Breast cancer • 13% 10-year survival rate • Treatments • Chemotherapy • taxanes • Hormone Therapy • Targeted therapy • HER2 targeted therapy • Slow growth • Manage Bone Metastasis • Biophosphonates • Slow destruction
How to Prevent cancer • Exercise • Eat well • Don’t smoke • Do regular breast self exams • Report anything suspicious immediately • Check family history
- More by User

Breast Cancer, BRCA2 Gene
Breast Cancer, BRCA2 Gene Breast Cancer Breast cancer specifically refers to a cancer that forms in tissues of the breast Usually in the ducts – which are the tubes that carry milk to the nipple Or the lobules – glands that make milk It occurs in both men and women
1.47k views • 39 slides
BREAST CANCER STUDY
BREAST CANCER STUDY A STUDY OF ISSUES INVOLVING THE DIAGNOSIS OF BREAST CANCER THAT RESULT IN MEDICAL MALPRACTICE CLAIMS 2002 Breast Cancer Study Focus 450 cases involving paid claims with resolution dates no earlier than January 1, 1995 were analyzed.
753 views • 32 slides
ACP: Breast Cancer Update
ACP: Breast Cancer Update. Elaine A. Muchmore, M.D. UC San Diego 10/20/07. Breast Cancer. Breast cancer affects more than 150,000 women each year, with a lifetime incidence of greater than 10%.
632 views • 19 slides
Breast cancer screening
[email protected]. 2. . Breast cancer screening. Early detection is an important factor in the success of breast cancer treatment. The earlier breast cancer is found, the more easily and successfully it can be treated. The three methods commonly used for early detection are: Breast self-exam (BSE). Clinical breast exam (CBE).Mammogram..
1.35k views • 32 slides
Ambi Journal Club June 14th 2006 Breast Cancer
ACADEMIC APPROACH TO BREAST CANCER IN LITERATUREDrug Therapy: Treatment of Breast Cancer Hortobagyi G. N. N Engl J Med 1998; 339:974-984, Oct 1, 1998. Review ArticlesPrimary Care: Assessing the Risk of Breast Cancer Armstrong K., Eisen A., Weber B.
931 views • 49 slides
THE REGISTRATION OF BREAST CANCER
2. FIVE FACTS ABOUT BREAST CANCER. Incidence:1 in 9 women in the TCR area develop breast cancer during their lifetime.0.5% of breast cancer cases occur in men.Survival:Now improving. Depends on stage at diagnosis.90% at 5yrs for localised disease, 77% at 5 yrs if lymph nodes involved.Most
424 views • 24 slides
Breast & Prostate Cancer
Breast & Prostate Cancer. Wednesday, October 17 2007. Introduction. Who we are Why we’re here today What is breast cancer What is prostate cancer Statistics How this affects you Prevention or Living with it. Breast Cancer. What is Breast Cancer?.
758 views • 31 slides
Breast Cancer
Breast Cancer. Kristi McIntyre M.D. Resident’s lecture. Breast cancer. Risk factors Hereditary breast cancer Detection Staging Surgical intervention Prognostic factors Management of early stage breast cancer. Breast cancer risk factors. Age/race
1.43k views • 59 slides

Weight Control for Breast Cancer Prevention
Outline. Weight control and breast cancer: BackgroundEvidence for primary breast cancer riskEvidence for breast cancer survivalPlanning of a national trial in weight control2. Practical aspects of weight control3. Proposed pilot study of weight control in newly diagnosed women though
899 views • 79 slides

Cancer Breast
Cancer Breast . * Epidemiology:. The most common malignant tumor in female. Accounts for 32% of all female cancer.
450 views • 18 slides
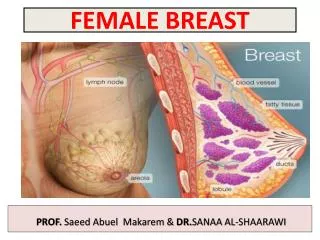
FEMALE BREAST
FEMALE BREAST. PROF. Saeed Abuel Makarem & DR. SANAA AL-SHAARAWI. OBJECTIVES. By the end of the lecture, the student should be able to : Describe the shape and position of the female breast. Describe the structure of the mammary gland. List the blood s upply of the female breast.
1.31k views • 17 slides
R5 洪逸平 SUPERVISOR 趙大中醫師
R5 洪逸平 SUPERVISOR 趙大中醫師. Breast Cancer. The most prevalent cancer in female Mortality 4 th in Taiwan. Treatment of Breast Cancer. Breast Cancer. When to change regimen? Unacceptable toxicity Progression disease. Current Tools for Follow-up. Radiologic image Standard serologic test
411 views • 27 slides
Breast cancer
Breast cancer. PPT 22 nd November 2012 Introduction: Dr B K Jindal Mr A Haq Consultant Surgeon . Aims and Objectives: . To understand the prevalence of breast cancer To receive the trends in survivability from breast cancer To consider the outcome of 2 week wait referrals
763 views • 26 slides
Physical Activity & Breast Cancer
Physical Activity & Breast Cancer. By Janet Foote, PhD. Educational Objectives. Discuss the role of movement in: 1. Prevention of breast cancer onset 2. Appropriateness for breast cancer survivors 3. Prevention of Breast Cancer recurrence.
506 views • 25 slides
Neoadjuvante Therapy of Breast Cancer
Neoadjuvante Therapy of Breast Cancer. Cancer statistics Genesis of cancer Cancer in detail Treatment of cancer Prevention Follow-up NEWS Research. INCIDENCE OF CANCER. Colorectal cancer Breast cancer Lung Cancer Prostate cancer Cervix carcinoma Meaning of
1.04k views • 55 slides
Breast Cancer. Kathrina Calulut Alison Saechao. Breast Cancer. Cancer of tissues of the breast Ductal carcinoma Lobular carcinoma. Risk Factors. 1 in 8 women Age and Gender Family History Substance Abuse Childbirth Obesity. Early Symptoms. New lump or mass
778 views • 15 slides
Development of laboratory models to study Breast Cancer
Section of Pathology and Tumour Biology. Development of laboratory models to study Breast Cancer. Deborah Holliday Breast Research Group Section of Pathology & Tumour Biology. Outline. Introduction to the cells found in breast tissue Changes in breast cells during breast cancer
359 views • 20 slides
HER-2 Positive Breast Cancer Market in the US 2015-2019
Breast cancer is characterized by uncontrolled growth of cancerous cells in the breast. It occurs in both males and females, however, the incidence of breast cancer in males is rare. Histologically, breast cancer can be classified into ductal carcinoma, lobular carcinoma, nipple cancer, and other undifferentiated carcinoma. Breast cancer is the second most common form of cancer in women. HER-2 is a protein that affects the growth of malignant cells and is usually found on the surface of normal breast cells. Sometimes, a large number of HER-2 receptors are found on the surface of breast cancer cells. Get full report & TOC @: http://www.researchbeam.com/her-2-positive-breast-cancer-in-the-us-2015-2019-market
303 views • 6 slides
Latest Study on Global Breast Biopsy Devices Consumption with Investment Feasibility Analysis and Market Research on Maj
A breast biopsy is a procedure in which part or all of a suspicious area in the breast is removed and examined, usually for the presence of cancer. Breast cancer is the most common cancer affecting women and accounts for the second highest incidence of cancer-related death, after lung cancer.
274 views • 7 slides

Breast Cancer Therapeutics in Asia-Pacific Markets to 2021
Breast cancer, a malignant neoplasm, is the second-most common cancer and the most common cancer in women worldwide, accounting for 16% of all female cancers, making the disease exceedingly prevalent. For More Information: http://bit.ly/1NnH1v0
267 views • 8 slides

How Breast Cancer Prevent With Cancer Treatment Centers?
If cells of breast spread out of control and forms a tumor it is the sign of Breast cancer with the help of X-ray we seen this changes. Many Cancer Treatment Centers are providing awareness for breast cancer because in this case, less symptoms are happening. There are 4 stages of breast cancer it can depend on changes in the breast. Houston Cancer Specialist are offered many therapies to stop breast cancer and also get success. If any treatment of Houston cancer hospital does not give the best result of treatment then also take the second opinion for cancer sometimes it shows best result.
726 views • 11 slides
Breast Cancer : Overview of symptoms, causes, diagnosis, risk factor and treatment
Breast cancer is a disorder in women, which starts in the inner lining of milk ducts or the lobules that supply them milk. Breast cancer may include lump in the breast, a change in breast or red scaly patch on skin. Breast cancer usually builds up with the age or it can be genetics.
488 views • 14 slides
Breast Cancer Case

How to download the Breast Cancer Case template for Powerpoint
How to download the template breast cancer case in google slides, description.

Enchanted Fortress

Soft Notebook Design

Clean and Elegant Black & White Design
Home Collections Medical Cancer Breast Cancer PowerPoint Presentation
Free - Editable Breast Cancer PowerPoint Presentation Slides
Create Awareness Using This Template:
Features of this template:.
- 100% customizable slides and easy to download
- Slides are available in different nodes & colors.
- The slides contained 16:9 and 4:3 format.
- Easy to change the slide colors quickly.
- Well-crafted Template with instant download facility.
- Crisp and elegant font style.
- The best Template with attractive nodes
- Cancer Infographics
- Cancer Disease
- Breast Cancer
- Breast Cancer Infographics
- Breast Cancer Awareness

677+ Templates
-594.webp)
124+ Templates

Science & Research
182+ Templates

Telemedicine
40+ Templates

327+ Templates

86+ Templates
117+ Templates

44+ Templates
46+ Templates

191+ Templates
You May Also Like These PowerPoint Templates


- Allergy & Immunology
- Anesthesiology
- Critical Care
- Dermatology
- Diabetes & Endocrinology
- Emergency Medicine
- Family Medicine
- Gastroenterology
- General Surgery
- Hematology - Oncology
- Hospital Medicine
- Infectious Diseases
- Internal Medicine
- Multispecialty
- Ob/Gyn & Women's Health
- Ophthalmology
- Orthopedics
- Pathology & Lab Medicine
- Plastic Surgery
- Public Health
- Pulmonary Medicine
- Rheumatology
- Transplantation
- Today on Medscape
- Business of Medicine
- Medical Lifestyle
- Science & Technology
- Medical Students
- Pharmacists
ASCO 2024: How to Best Use New Breast Cancer Data
Kevin Kalinsky, MD, MS; Sara Hurvitz, MD
Authors and Disclosures

Disclosure: Kevin M. Kalinsky, MD, MS, has disclosed no relevant financial relationships
Disclosure: Sara A. Hurvitz, MD, has disclosed the following relevant financial relationships: Serve(d) as a consultant or advisor for: Briacell; Boehringer-Ingelheim; Bristol Myers Squibb; Gilead; Luminate (all paid to institution) Received research grant from: Ambrx; Amgen; Arvinas; AstraZeneca; Bayer; Celcuity; Cytomx; Daiichi-Sankyo; Dantari; Dignitana; Genentech/Roche; G1-Therapeutics; Gilead; Greenwich Life Sciences Inc; GSK; Immunomedics; Eli Lilly; LOXO; Macrogenics; Novartis; OBI Pharma; Orinove; Orum; Pfizer; Phoenix Molecular Designs; Ltd.; Pieris; PUMA; Radius; Samumed; Sanofi; Seattle Genetics/Seagen; Zymeworks/Jazz
This transcript has been edited for clarity.
Kevin M. Kalinsky, MD, MS: Hi. I'm Kevin Kalinsky. I'm the division director of Medical Oncology at Winship Cancer Institute in Atlanta, Georgia. I am very pleased and happy to be joined by my colleague, Dr Sara Hurvitz, who's the senior vice president of the clinical research division at Fred Hutchinson Cancer Center, and head of the Division of Hematology and Oncology at the University of Washington Department of Medicine. Dr Hurvitz, good to see you.
Sara A. Hurvitz, MD: Great to see you, Kevin.
Kalinsky: We've seen some exciting data that we have been awaiting. In particular, I would say the most anticipated data were from the DB-06 , the DESTINY-Breast06 study. Maybe we can talk through that study. I'm curious about your perception of that study and how we will best utilize that study when we're taking care of our patients with hormone receptor–positive disease.
Hurvitz: It was a really interesting clinical trial looking at trastuzumab -deruxtecan (T-DXd) in patients with hormone receptor–positive metastatic breast cancer that was HER2- low or -ultralow expressing. They allowed patients who had HER2 immunohistochemistry (IHC) 0, as long as there was up to 10% of faint staining for HER2. Patients were allowed on if they had exhausted endocrine therapy options, so they had to have had endocrine therapy, most cyclin-dependent kinase (CDK)–4/6 inhibitors, but no chemo yet.
This is like a frontline chemo, but not a frontline study, comparing T-DXd to treatment of physician's choice, which was essentially capecitabine or taxane. Capecitabine was had by about 60% of patients in the treatment of physician's choice arm. They reported a very significant improvement in progression-free survival (PFS), a very impressive hazard ratio, and about a 5-month delta, if I'm remembering correctly, 8-13 months with T-DXd.
The survival data were immature, of course, but this now places T-DXd, not after chemo but in front of chemo. I think many things are important to consider. First of all, being that many of our community oncologists are incredibly busy and are treating multiple tumor types, you can hear top-line results like this and misinterpret and think we should be replacing T-DXd in the frontline setting and skipping over endocrine therapy and CDK4/6 inhibitors. That's not the message from this trial.
We should be exhausting endocrine therapy options first. I do think these data are very important and do, especially if they end up showing survival benefits, place T-DXd earlier in front of chemotherapy. I don't know. What do you think? I mean, capecitabine is so well tolerated, and it's oral.
Kalinsky: Definitely. I think the first point that you made is a critical point, that these are patients with hormone receptor–positive disease. This is a marathon, right? We want patients to be able to utilize endocrine-based treatments for as long as they can with targeted therapy , ideally, before we need to utilize something where they have to spend more time with us at the infusion center. It's a really important point. When I was a fellow, 1000 years ago, we used to give our patients chemotherapy in that front line. We've really moved away from that, where we give doublet endocrine therapy and CDK4/6 inhibition. That should remain the case.
For those patients, when they become endocrine-resistant, then it's a question of whether we should be using T-DXd vs something like capecitabine. For me, my clinical interpretation of the data is if a patient has a slow-growing tumor, maybe it remains bone-only and I'm not concerned about their pace of disease, capecitabine is still a reasonable option. If I have somebody who I'm concerned about, I feel like I need to get a response — like those were some additional notable data where the response rate was over 60% in that population, so it's an active drug, T-DXd — then, I would consider giving T-DXd.
The other thing is that there were no additional safety signals beyond what we know. We're now very familiar with what we should be checking and making sure that we're looking for interstitial pneumonitis, given that is a potential toxicity.
Hurvitz: The one thing that was a little bit different, I believe, from the written abstract than what was presented was there were five deaths from interstitial lung disease, underscoring the importance of us stopping therapy and watching, with even grade 1, and utilizing steroids aggressively to mitigate that.
The other point that somebody made that I thought was salient is that only 20% of the patients who were on the treatment of physician's choice went on and received T-DXd at progression. We don't know if having T-DXd at first-line chemo or at second-line chemo makes a difference. That's something I think we're going to have to wait and see as the survival data mature.
Kalinsky: For sure. Two things. One, for the survival data, there were some patients, I think it was about 20% or so, who crossed over. We'll see how this looks, and the point's very well taken in terms of what patients received subsequent lines of treatment. Then, that HER2-ultralow population — I believe there were maybe like 700 or so patients who were HER2-low, and 150 or so who were HER2-ultralow.
Hurvitz: Yes.
Kalinsky: The question is: What do we do with those patients? During that session, I was texting my pathologist, asking, "Well, how are we going to report this?" We don't report it in a spectrum like that. It's 0, 1, 2, or 3. It raises the question of, well, should we be thinking about utilizing this just in all patients, regardless of HER2 score? Though that's not what the indication is right now. It just raises the question. Then, just working with our pathologists of how we're going to be determining that someone actually has HER2-ultralow disease.
Hurvitz: Absolutely. Quantification of HER2 is going to be so important. I know there are a number of groups working on new assays because IHC was never meant to be a quantitative assay. I agree with you. It's going to be very difficult for us if the FDA expands the label for this drug, including HER2-ultralow. We don't have a companion diagnostic. It's going to be very interesting.
Kalinsky: For sure. I'm going to switch topics because we were talking about endocrine-sensitive disease. The other day, we saw the results of postMONARCH . This was a study where we'd seen some phase 2 trials that demonstrated some inconsistent findings, though the phase 2 data that we had were suggesting maybe there was a benefit of switching.
In this particular study, patients had endocrine therapy with an aromatase inhibitor and a CDK4/6 inhibitor — it could have been any of them — and then they were switched to fulvestrant plus placebo vs fulvestrant plus abemaciclib .
It was a randomized phase 3 trial. It was a true second-line study. Patients did not have chemotherapy in the advanced setting. I'm curious about your interpretation of those data.
Hurvitz: Well, it's the only phase 2 trial to address whether continuing a CDK4/6 inhibitor after progression on one is beneficial. I think these are very important data, just based on the fact that the trial was done, to confirm the findings of MAINTAIN , which were very compelling, interesting phase 2 data that you presented.
It met its primary endpoint. It did have a good hazard ratio, showing the benefit by continuing the CDK4/6 inhibitor. It's really interesting, though, because we're treating it as though abemaciclib is just a CDK4/6 inhibitor, and it's a different drug. It's far more potent, it is far less selective, and it's hitting other kinases that may be implicated in the development of resistance to CDK4/6 inhibitors.
As you mentioned, like 60% of the patients enrolled in that trial had received palbociclib first then went to abemaciclib. That, on the forest plot, seems to be where most of the benefit is coming from. The 30% or so patients who went from ribociclib to abemaciclib, what do you think of those results?
Kalinsky: I think that this was the largest population that we have of post-ribociclib so far. We'll see other datasets that should read out, hopefully in the next year or so, looking at post-ribociclib and how patients with endocrine therapy with or without a CDK4/6 inhibitor do, like the upcoming EMBER-3 trial .
That hazard ratio, as you mentioned, was 1. That confidence interval was wide. There were less than 100 events and the interaction P value was not statistically significant. It is interesting. We will see if that signal continues. There is this question, and as you mentioned, I don't think that all the CDK4/6 inhibitors are the same.
When I think about those data that were presented for postMONARCH, the patients that I would think about continuing CDK4/6 inhibitor, in this case, abemaciclib, would be those that did not have visceral metastasis. Though we did see, if you had liver metastasis, that the hazard ratio was about the same in those who were on their CDK4/6 inhibitor for greater than or equal to 12 months.
The other thing is that about 30% did not have an ESR1 mutation or a PI3 kinase (PI3K) pathway signaling alteration. For those patients, where we don't have specific targeted therapies, this offers one to those potential patients. Would you think about utilization any differently?
Hurvitz: No. I completely agree with you. I think what we will be doing in that setting is testing circulating tumor DNA at the time to figure out if there is a more targeted, selective way to go with our treatment. If there's a PI3 mutation or an AKT mutation, we're probably going to choose a different regimen. I completely agree with you.
Kalinsky: Along that topic, another thing that we saw during the session was updates on some of the studies that we've seen previously, including the INAVO120 study , where we saw recently that inavolisib got breakthrough status. We anticipate that this will be something that we have in our clinic. Talk me through the design of that study, and where you think the utilization of inavolisib will be?
Hurvitz: This was first presented at San Antonio, sort of as a late-breaker Friday session before we all got on the plane. There was this last-minute added session looking at this phase 3 clinical trial of inavolisib combined with fulvestrant and palbociclib, compared to fulvestrant palbociclib. Inavolisib is a PI3K inhibitor. This study actually demonstrated a very compelling PFS benefit and a strong trend toward overall survival. What was most compelling, I think, was the safety didn't appear to have the level of grade 3 diarrhea or hypoglycemia that we all contend with by hitting the PI3 kinase pathway.
These were very impressive data. Here at ASCO, they presented some updated adverse events as well as PFS2. The efficacy data continue to look compelling. What is really surprising is the relative lack of grade 3 events when you're looking at rash, diarrhea, and hyperglycemia. One thing to note is that these were highly, highly selected patients. The A1c levels at entry were very restrictive. I believe it was 6 or 6.5 to get on this study. Other studies have used 8.
These are data that I think are going to have to be confirmed by real-world evidence to see really how well it's tolerated when we get it out into a general patient population who may not have been fit for this clinical trial.
Kalinsky: I agree. The population, as you mentioned, was this endocrine-resistant population. These patients had tumor progression within 12 months of their endocrine therapy, so it's a very select population. With the doublet, they did not do well at all. That's why these data, I think, were so compelling for this population.
When you think about when you would be checking circulating tumor DNA, do you think that it would be just those patients that you would be checking circulating tumor DNA earlier? Or is your practice now, even at the time of metastatic diagnosis, doing next-generation sequencing?
Hurvitz: I think if this regimen is approved, we're going to be compelled to test and do next-generation sequencing on our patients at the time of diagnosis of metastatic disease, especially if their disease is behaving in a more aggressive manner, as you said. Do you agree?
Kalinsky: I do. This is great. Anything else that was on your radar?
Hurvitz: No. I think this was an exciting conference, with a large amount of data out. I think those three abstracts were pretty much top.
Kalinsky: Yeah, I agree. It's been great chatting with you, as always. Enjoy the rest of your meeting.
Hurvitz: You too.
Kalinsky: Thank you for joining me. This is Kevin Kalinsky, speaking from the 2024 ASCO Annual Meeting in Chicago.
TOP PICKS FOR YOU
- Perspective
- Drugs & Diseases
- Global Coverage
- Additional Resources
- SABCS 2023 Highlights Breast Cancer De-Escalation
- Breast Cancer Exacts High Financial Toll Worldwide
- Pfizer to Sell All Its Drugs in Low-Income Countries at Nonprofit Price
- Fast Five Quiz: What to Know About Early-Stage Breast Cancer
- ASCO 2024: Addressing Unmet Needs in Early Breast Cancer
- ASCO 2024: Anticipating Advancements in Metastatic Breast Cancer
- Conference Coverage ESMO Breast Cancer 2024
- Breast Cancer Histology
- Breast Cancer
- Male Breast Cancer Imaging
- Fast Five Quiz: Unusual Breast Cancer Presentations
- Breast Cancer Survivorship in Veterans
- Patient Simulation: A 63-Year-Old Woman With Metastatic Breast Cancer
- Metastatic Breast Cancer: A Review of 3 Cases and Palliative Care
- A Benefit to Add-On Abemaciclib in Advanced Breast Cancer?
- Intermediate Endpoints Predict Breast Cancer Survival
- Is Vaginal Estrogen Safe in Breast Cancer Survivors?
WebMD Network
Breast Cancer

Breast cancer starts in the cells of the breast and can spread to other parts of the body. There are several types of breast cancer including ductal carcinoma in situ, invasive ductal carcinoma, inflammatory breast cancer, and metastatic breast cancer. Risk factors include being a woman, aging, family history and genetic factors, personal history of breast cancer, reproductive history. Screening tests include mammograms, clinical breast exams, and breast self-exams. Treatment involves surgery to remove the tumor, chemotherapy, radiation therapy, and hormone therapy. Prevention focuses on maintaining a healthy weight, physical activity, breastfeeding, diet and avoiding hormone therapy when possible. Read less

Recommended
More related content, what's hot, what's hot ( 20 ), viewers also liked, viewers also liked ( 20 ), similar to breast cancer, similar to breast cancer ( 20 ), more from abdullatif al-rashed, more from abdullatif al-rashed ( 20 ), recently uploaded, recently uploaded ( 20 ).
- 1. Case 7.1 Breast Cancer BY: Abdullatiff Sami AL-Rashed 1
- 2. Objectives 2 1. What Is Breast Cancer. 2. Types of Breast Cancer. 3. Etiology of breast cancer. 4. Risk factors. 5. Signs and symptoms. 6. Investigations. 7. Treatment. 8. Prevention. 9. Screening. 10. Question asked by my colleagues.
- 3. What Is Breast Cancer Breast cancer is a malignant tumor that starts in the cells of the breast. A malignant tumor is a group of cancer cells that can grow into (invade) surrounding tissues or spread (metastasize) to distant areas of the body. The disease occurs almost entirely in women, but men can get it, too. 3
- 4. What Is Breast Cancer Most commonly from the inner lining of milk ducts or the lobules that supply the ducts with milk. Cancers originating from ducts are known as ductal carcinomas, while those originating from lobules are known as lobular carcinomas. 4 Breast cancer showing an inverted nipple, lump and skin dimpling. Author: Hic et nunc
- 5. Types of Breast Cancer 5 There are many types of breast cancer 1. Ductal carcinoma in citu (DCIS) 2. Invasive Ductal Carcinoma. 3. Inflammatory Breast Cancer 4. Metastatic Breast Cancer 5. Some other specific types.
- 6. Types of Breast Cancer 6 1. Ductal carcinoma in citu (DCIS) is a non-invasive cancer where abnormal cells have been found in the lining of the breast milk duct. The atypical cells have not spread outside of the ducts into the surrounding breast tissue. Ductal carcinoma In situ is very early cancer that is highly treatable, but if it’s left untreated or undetected, it can spread into the surrounding breast tissue.
- 7. Types of Breast Cancer 7 2. INVASIVE DUCTAL CARCINOMA: The abnormal cancer cells that began forming in the milk ducts have spread beyond the ducts into other parts of the breast tissue. IDC is the most common type of breast cancer, making up nearly 70- 80% of all breast cancer diagnoses. IDC is also the type of breast cancer that can most commonly affects men
- 9. Types of Breast Cancer 9 3. Inflammatory Breast Cancer Inflammatory Breast Cancer is an an aggressive and fast growing breast cancer in which cancer cells infiltrate the skin and lymph vessels of the breast. It often produces no distinct tumor or lump that can be felt and isolated within the breast. But when the lymph vessels become blocked by the breast cancer cells, symptoms begin to appear.
- 10. Types of Breast Cancer 10 4. Metastatic Breast Cancer: The cancer has spread to other parts of the body. This usually includes the lungs, liver, bones or brain.
- 12. Etiology 12 When you're told that someone have breast cancer, it’s natural to wonder what may have caused the disease. But no one knows the exact causes of breast cancer. Doctors seldom know why one woman develops breast cancer and another doesn’t, and most women who have breast cancer will never be able to pinpoint an exact cause. What we do know is that breast cancer is always caused by damage to a cell's DNA.
- 13. Etiology Cont.. 13 But doctors have known some risk factors that increase the chance to get a breast cancer. Women with certain risk factors are more likely than others to develop breast cancer.
- 14. Risk Factors There are some risk factors for the breast cancer: 1. Gender. 2. Age. 3. Genetics related. 4. Family history. 5. Personal history of breast cancer. 6. Menstrual periods. 7. Having children. 8. Birth control. 9. Breastfeeding 14
- 15. Risk Factors 1. Gender: Being a woman is the main risk for breast cancer. While men also get the disease, it is about 100 times more common in women than in men. 15
- 16. Risk Factors 2. Age: The chance of getting breast cancer goes up as a woman gets older. About 2 of 3 women with invasive breast cancer are 55 or older when the cancer is found. 16
- 17. Risk Factors 3. Genetic risk factors: About 5% to 10% of breast cancers are thought to be linked to inherited changes (mutations) in certain genes. 3. The most common changes are those of the BRCA1 and BRCA2 genes. Women with these gene changes have up to an 80% chance of getting breast cancer during their lifetimes17
- 18. Risk Factors 4. Family history: Breast cancer risk is higher among women whose close blood relatives have this disease. The relatives can be from either the mother’s or father’s side of the family. Having a mother, sister, or daughter with breast cancer about doubles a woman’s risk. It’s important to note that most (over 85%) women who get breast cancer do not have a family history of this disease, so not having a relative with breast cancer doesn’t mean you won’t get it. 18
- 19. Risk Factors 5. Personal history of breast cancer: A woman with cancer in one breast has a greater chance of getting a new cancer in the other breast or in another part of the same breast. This is different from a return of the first cancer (called a recurrence). 19 MRI screening recommended for women with a history of breast cancer
- 20. Risk Factors 6. Menstrual periods: Women who began having periods early (before age 12) or who went through the change of life (menopause) after the age of 55 have a slightly increased risk of breast cancer. The increase in risk may be due to a longer lifetime exposure to the hormones estrogen and progesterone. 20
- 21. Risk Factors 21 7. Having Children: Women who have had no children or who had their first child after age 30 have a slightly higher breast cancer risk. Having many pregnancies and becoming pregnant at a young age reduce breast cancer risk.
- 22. Risk Factors 22 8. Birth control: Studies have found that women using oral contraceptives (birth control pills) have a slightly greater risk of breast cancer than women who have never used them.
- 23. Risk Factors 23 9. Breastfeeding: Some studies suggest that breastfeeding may slightly lower breast cancer risk, especially if breastfeeding is continued for 1½ to 2 years.
- 24. 24 Sings and Symptoms:
- 25. Investigations 25 Doctors can investigate the breast cancer by doing: 1. Mammography: The goal of mammography is the early detection of breast cancer. 2. Breast ultrasound. 3. Magnetic resonance imaging mammogram
- 26. Investigations 26 4. Breast Biopsy: A breast biopsy is a small needle sample of tissue taken from your breast. Several samples may be taken and sent to a laboratory for testing to find out if the lump is cancerous or not.
- 27. Treatment 27 The treatment of breast cancer has certain steps: 1. Surgery. 1. Chemotherapy. 2. Radiotherapy 3. Hormonal therapy
- 28. Treatment Cont.. 28 1. Surgery: The first step and most common form of treatment for breast cancer is surgery. Surgery involves removing the tumor and nearby margins.
- 29. Treatment Cont.. 29 There are certain procedures in surgery: 1. Lumpectomy: removal of cancerous tumor without removing the entire breast. 2. mastectomy: removal of the entire breast.
- 30. 30 lumpectom y Total mastectomy
- 31. Treatment Cont.. 31 2. Chemotherapy : is a breast cancer treatment method that uses a combination of drugs to either destroy cancer cells or slow down the growth of cancer cells. 3. Radiotherapy: uses high-energy rays to kill cancer cells.
- 32. Treatment Cont.. 32 4. Hormonal therapy: If the cancer cells have hormone receptors, you may be prescribed hormone therapy drugs, such as blockers or inhibitors. Both types of drugs help to destroy cancer cells by cutting off their supply of hormones.
- 33. Prevention 33 Breast cancer prevention begins with various factors you can control. For example: 1. Control the weight 2. Get plenty of physical activity 3. Breast-feed. 4. Healthy diet. 5. Discontinue hormone therapy 6. Avoid exposure to environmental pollution
- 34. Screening 34 Breast cancer screening means checking a woman's breasts for cancer before there are signs or symptoms of the disease. Three main tests are used to screen the breasts for cancer. 1. Mammogram. 2. Clinical breast exam. A clinical breast exam is an examination by a doctor or nurse 3. Breast self-exam.
- 35. Why women are more common to have breast cancer than men? 35 there are several factors that could explain why breast cancer is more common in women: 1. more breast tissue in women. 2. different hormone levels: estrogen and testosterone are present in both men and women, but at different levels. 3. menstruation. 4. lactation.
- 36. How we can repair the breast after mastectomy? 36 doctors can repair the breast after mastectomy by breast reconstruction. Breast reconstruction is a type of surgery for women who have had a breast removed (mastectomy). The surgery rebuilds the breast mound so that it is about the same size and shape as it was before.
- 37. 37 Breast reconstruction
- 38. References http://www.cancer.org/Cancer/BreastCancer/Detailed Guide/breast-cancer-what-is-breast-cancer http://www.nationalbreastcancer.org http://www.cancer.org/cancer/breastcancer/moreinfor mation/breastreconstructionaftermastectomy/breast- reconstruction-after-mastectomy-what-is-br-recon 38
- Open access
- Published: 18 June 2024
Measurement properties of the Iranian version of the breast cancer perception scale (BCPS) according to the COSMIN checklist
- Sepideh Mashayekh-Amiri 1 ,
- Mohammad Asghari Jafarabadi 2 , 3 , 4 ,
- Mina Hosseinzadeh 5 ,
- Elham seyed Kanani 6 &
- Mojgan Mirghafourvand 7 , 8
BMC Cancer volume 24 , Article number: 743 ( 2024 ) Cite this article
55 Accesses
Metrics details
Breast cancer is a prevalent cancer characterized by its aggressive nature and potential to cause mortality among women. The rising mortality rates and women’s inadequate perception of the disease’s severity in developing countries highlight the importance of screening using conventional methods and reliable scales. Since the validity and reliability of the breast cancer perception scale (BCPS) have not been established in the Iranian context. Therefore, this study aimed to determine the measurement properties of the BCPS in women residing in Tabriz, Iran.
The present study comprised a cross-sectional design, encompassing a sample of 372 Iranian women. The participants were selected through a multi-stage cluster random sampling technique conducted over a period spanning from November 2022 to February 2023. The measurement properties of the Iranian version of BCPS were assessed following the guidelines outlined in the COSMIN checklist. This involved conducting various steps, including the translation process, reliability testing (internal consistency, test-retest reliability, and measurement error), and methodological tests for validity (content validity, face validity, construct validity, and hypothesis testing). The study also investigated the factors of responsiveness and interpretability. The presence of floor and ceiling effects was assessed.
The internal consistency of the scale was assessed using Cronbach’s alpha, yielding a satisfactory value of 0.68. Additionally, McDonald’s omega (95% CI) was computed, resulting in a value of 0.70 (0.66 to 0.74). Furthermore, the test-retest reliability was evaluated, revealing a high intraclass correlation coefficient (ICC) of 0.97 (95% CI: 0.94 to 0.99). The CVI, CVR, and impact scores of the BCPS were determined to be 0.98, 0.95, and 3.70, respectively, indicating favorable levels of content and face validity. To assess construct validity, an examination of the Exploratory Factor Analysis (EFA) was conducted on a set of 24 items. This analysis revealed the presence of six distinct factors, which collectively accounted for 52% of the cumulative variance. The fit indices of the validity model (CFI = 0.91, NFI = 0.96, RFI = 0.94, TLI = 0.90, χ 2 /df = 2.03, RMSEA = 0.055 and SRMR = 0.055) were confirmed during the confirmatory factor analysis (CFA). The overall score of BCPS exhibited a ceiling effect of 0.3%. The floor effect observed in the overall score (BCPS) was found to be 0.5%. Concerning the validation of the hypothesis, Spearman’s correlation coefficient of 0.55 was obtained between the BCPS and the QLICP-BR V2.0. This correlation value signifies a statistically significant association. Furthermore, it is worth noting that the minimum important change (MIC) of 3.92 exhibited a higher value compared to the smallest detectable change (SDC) of 3.70, thus suggesting a satisfactory level of response.
Conclusions
The obtained findings suggest that the Iranian version of the BCPS demonstrates satisfactory psychometric properties for assessing the perception of breast cancer among Iranian women. Furthermore, it exhibits favorable responsiveness to clinical variations. Consequently, it can serve as a screening instrument for healthcare professionals to comprehend breast cancer and as a reliable tool in research endeavors.
Peer Review reports
Breast cancer is a significant global health issue [ 1 ], accounting for approximately 30% of cancer cases among women [ 2 ]. It is recognized as the second-leading cause of mortality in developed nations and the third-leading cause of mortality in less developed nations [ 3 ]. Based on the findings of the Global Cancer Incidence, Mortality and Prevalence (GLOBOCAN) report in 2020, it was determined that there were an estimated 2,261,419 million new cases (1 in 4 new cancer cases) (11.7%), and 684,996 (1 in 6 deaths) (6.9%) fatalities [ 4 ]. It is also predicted that these figures will reach 2,964,197 in 2040 (31% rise from 2018) [ 5 ], and 4.4 million in 2070 (110% rise from 2018) [ 6 ]. According to the report of the American Cancer Society in 2024, the number of new cases of female breast cancer in the United States was 310,720 and the number of deaths was 42,250 [ 7 ]. Approximately two-thirds of these fatalities are documented in regions with lower levels of development [ 4 ]. Alternatively, based on the projection provided by the World Health Organization (WHO), it is anticipated that by 2050, approximately 2.3 million women will receive a diagnosis of breast cancer [ 8 ]. Breast cancer is recognized as a highly costly form of cancer on a global scale, with an estimated annual expenditure of approximately 88 billion dollars. Failing to promptly diagnose and conduct screening examinations, coupled with the consequential impact on the entire family unit, imposes substantial financial burdens on society [ 9 ].
Breast cancer exhibits the highest prevalence and mortality rates among women in the Eastern Mediterranean region (EMR), encompassing Iran when compared to other forms of cancer. Breast cancer is widely recognized as the predominant form of cancer in Iran, ranking as the fifth-highest cause of mortality among women in the country [ 10 ]. The Age-standardized rate (ASR) incidence rate is approximately 28 per 100,000 individuals, exhibiting a recent upward trend [ 11 ]. Based on a systematic review, it has been documented that the incidence rate of breast cancer in Iran stands at 23.6% [ 12 ]. The reported prevalence of this cancer in the United States (US) is approximately 13%, indicating that one out of every eight individuals is affected [ 13 ].
Breast cancer is correlated with numerous risk factors, a significant proportion of which remain unidentified. The findings of a systematic review conducted in 2020 in Iran reveal various risk factors associated with breast cancer. These factors include family history, hormone replacement therapy (HRT), exposure to passive smoking, advanced maternal age during pregnancy, history of abortion, consumption of sweets, and possession of the Arg/Arg genotype. These factors have been found to potentially elevate the risk of developing breast cancer. Conversely, certain factors such as the late onset of menstruation, nulliparity, breastfeeding for a duration of 13 to 24 months, regular physical exercise, and consumption of vegetables have been observed to have a protective effect against the incidence of breast cancer [ 14 ].
It is noteworthy that the incidence of breast cancer among Iranian women occurs at an age approximately 10 years earlier compared to women in other developed nations. According to various studies, there has been a documented increase in the prevalence of breast cancer among women under the age of 40 in recent years [ 15 ]. The rise in its occurrence in developing nations is primarily attributed to alterations in lifestyle and reproductive behaviors [ 16 ]. The majority of female individuals afflicted with breast cancer receive a diagnosis during the later stages of the ailment, thereby correlating with an elevated mortality rate. Hence, it has been observed that early detection of breast cancer leads to a significant improvement in both survival rates and treatment outcomes, with a reported increase of 90% [ 17 ].
The United States Office of Disease Prevention and Health Promotion’s Healthy People 2020 initiative has as its goals the improvement of breast cancer diagnostic procedures for women, a decrease in the prevalence of cases of end-stage cancer, and a reduction in breast cancer mortality rates. Conversely, in the case of cancers that exhibit both genetic and environmental risk factors, it is imperative to adopt strategies that prioritize modifiable risk factors and early detection. Hence, the implementation of a preventive strategy aimed at early detection, which incorporates the evaluation of knowledge on breast cancer and its associated risks, assumes paramount significance [ 18 ].
The perception of breast cancer is a crucial subjective psychological phenomenon that is associated with the evaluation of potential threats. This evaluation is linked to an individual’s assessment of their susceptibility to the disease and the probability of gaining advantages from engaging in preventive measures [ 15 ]. Various studies have indicated that risk perception is a significant determinant of preventive health-related behaviors, such as screening. The motivation to undergo screening tests can be influenced by individuals’ perceptions of the risk associated with breast cancer [ 16 ]. According to the literature, screening tests play a crucial role in mitigating complications and mortality associated with breast cancer [ 17 ].
Various studies have documented divergent findings regarding the correlation between the perception of breast cancer risk and the utilization of screening tests, such as mammography [ 18 ]. Research findings indicate that the implementation of mammography screening during the age range of 40 to 49 years has been associated with a reduction in mortality rates of approximately 15 to 20% [ 19 ].
According to a study conducted on families to assess their perception of breast cancer risk, the rate of adherence to screening tests in Germany was found to be 83% [ 20 ]. Conversely, a research study conducted in Iran examined the adherence rate of women aged 35 to 69 years to mammography, as recommended by screening programs. The findings revealed that in urban areas, the adherence rate was 8.3%, while in rural areas, it was 3.16% [ 1 ]. Therefore, the perception level that women possess regarding breast cancer has the potential to influence their subsequent actions, such as seeking medical evaluation and undergoing screening procedures like breast self-examination (BSE), clinical breast examination (CBE), and mammography. Therefore, it is imperative to assess the perception of breast cancer in women using a multidimensional approach [ 20 ].
Numerous methodologies have been suggested for assessing the perception of breast cancer risk, which can be categorized into two distinct types: evaluation of the objective perception of risk (i.e., actual risk) and evaluation of the subjective perception of risk [ 21 ]. Currently, Gill’s model predominantly serves as a tool for conducting quantitative risk assessments. This approach aims to objectively evaluate the actual risk by considering the attributes of risk factors [ 22 ]. The second method entails the assessment of self-perceived risk, which can be anticipated by gauging individuals’ mental perceptions using a visual analog scale (VAS). Despite the presence of a multitude of tools within this domain, their practicality appears to be limited as they do not provide comprehensive coverage of all the factors that influence behaviors related to the diagnosis of breast cancer [ 23 ].
Taylan et al. (2021) developed the BCPS in Turkey, considering the health belief model for the first time. This scale encompasses various domains, including Perceived knowledge, Perceived treatment belief, Perceived need for health check, Perceived stigma, Perceived fear and Perceived risk. The utilization of this scale offers several benefits in assessing women’s perceptions regarding the factors influencing breast cancer diagnostic behavior comprehensively. Furthermore, it is worth noting that the extent of women’s perceived knowledge of breast cancer has not been quantitatively evaluated thus far. Consequently, this tool serves as a distinctive scale specifically designed to measure women’s knowledge regarding cancer. Additionally, it quantifies the dimensions of the breast [ 23 ].
The Health Belief Model (HBM) was initially formulated by Becker et al., in 1974 to comprehend health-related protective behaviors [ 24 ]. The evaluation of perceived risk, employing the HBM, has been validated in various studies examining screening behaviors, such as those related to breast cancer diagnostics [ 25 , 26 , 27 ]. The model encompasses various dimensions, namely perceived sensitivity, perceived severity, perceived benefits, perceived barriers, self-efficacy, and guidance for action. Based on the presented model, individuals’ healthcare behaviors can be subject to influence from factors such as perception, beliefs, values, and attitudes. By identifying and modifying an individual’s perceptions, beliefs, and attitudes, the effectiveness of healthcare education or treatment can be enhanced [ 26 ].
However, it is crucial to assess the methodological rigor of studies that evaluate the measurement properties of instruments used to measure health-related patient-reported outcomes (HR-PROs) [ 28 ]. The Consensus-Based Standards for the Selection of Health Status Measurement Instruments (COSMIN) checklist was developed by Mokkink et al. in 2010 through a consensus-based approach utilizing the Delphi method [ 28 ]. The COSMIN list is widely regarded as a highly comprehensive set of criteria for selecting an appropriate tool. It serves as a valuable guide for researchers, offering a range of logical indicators that aid in the process of tool selection [ 29 ].
Given the rising incidence of breast cancer, the significance of early screening, and the potential influence of risk perception on women’s adoption of preventive behaviors, such as breast screening methods, it is pertinent to assess the level of knowledge regarding breast cancer when devising interventions aimed at modifying health behaviors. It is worth noting that the validity and reliability of the aforementioned assessment tool have not been established in Iran. The present study was undertaken to conduct a measurement propertice of the BCPS in women residing in Tabriz city-Iran, by using the COSMIN checklist.
The present study was conducted with the aim of determining the measurement properties of the breast cancer risk perception scale (BCPS) in according to COSMIN checklist in women in Tabriz, Iran.
Validity procedure
The measurement properties of the Iranian version of BCPS were assessed following the guidelines outlined in the COSMIN checklist [ 29 ]. This involved conducting various steps, including the translation process, reliability testing (internal consistency, test-retest reliability, and measurement error), and methodological tests for validity (content validity, face validity, construct validity, and hypothesis testing). The study also investigated the factors of responsiveness and interpretability. The presence of floor and ceiling effects was assessed.
Translation process
Initially, permission to use the BCPS was obtained by sending an email from the original designer of the instrument (Taylan et al.) [ 23 ]. Efforts were made to maintain the integrity of the original intent during the translation process. Following the recommendations made by the WHO, EORTC Quality of Life Group Translation Procedure Guidelines and expert panel review, this was performed [ 30 ]. The translation process involves the utilization of two distinct methods. The two methods utilized in this study are the Forward-Backward method (FB) and the Dual Panel method (DP), which were implemented throughout four distinct stages. The process consisted of four stages: forward translation, backward translation, pre-testing and cognitive interviewing, and the final version.
During the initial phase of translation, the original English version of the instrument was administered to two individuals who were native Persian speakers, proficient in English, and possessed expertise in the development of the instrument as well as knowledge in the field of breast cancer. Translators were subsequently instructed to translate the tool in a fully autonomous and individual manner, with a focus on conceptual rather than literal translations. Additionally, they were encouraged to use language that would be comprehensible to the majority of the target audience. Ultimately, two translators looked into the discrepancies between the two translated versions, which led to a reconciled translation. Subsequently, the identified issues were addressed, leading to the presentation of a unified version [ 31 ]. Subsequently, the backward translation method was employed to guarantee a comprehensive correspondence between the Persian translation and the original version. The translated questionnaire from the preceding stage was administered to two individuals who are native English speakers. These individuals were not involved in the forward translation process and had no prior exposure to the original version of the questionnaire. They were instructed to retranslate the questionnaire back into English. The concluding report at the culmination of this phase encompassed the following components: two forward translations from the English language to Farsi, a reconciled translation, two backward translations from Farsi to English, and the incorporation of any supplementary remarks regarding the translations provided by the panel of experts. Ultimately, before implementing the tool in the intended population, it is imperative to conduct a pilot study. To achieve the intended objective, a questionnaire was administered to a sample of ten qualified female participants. Based on the feedback received from these participants regarding the ease of completing the instrument, grammar, comprehensibility, and writing style, modifications were made to the Persian version, and the revised version was finalized and presented [ 31 ].
Validation study
This cross-sectional study aimed to assess the measurement properties of the Iranian version of the BCPS among a sample of 372 Iranian women who sought healthcare services at Tabriz health centers affiliated with Tabriz University of Medical Sciences in two separate secondary samples (172 participants via exploratory factor analysis and 200 participants via confirmatory factor analysis). The study was conducted following the approval of the Ethics Committee of Tabriz University of Medical Sciences (ref: IR.TBZMED.REC.1401.390) from November 2022 to February 2023. It is important to acknowledge that informed consent was obtained from all participants. The study was conducted in adherence to the applicable regulations of the Ethics Committee of the University of Medical Sciences and the Declaration of Helsinki.
Among the 410 women, it was found that 16 participants did not satisfy the predetermined eligibility criteria, leading to their exclusion from the research investigation. Out of the remaining 394 participants who met the eligibility criteria, a total of 22 participants expressed their unwillingness to participate in the study. Ultimately, a total of 372 participants were incorporated into the research investigation. The response rate for the study was 94%, (372/394). In the sampling procedure, the cluster method was employed to randomly select a quarter of the 92 health centers in Tabriz City. The selection process was facilitated through the utilization of the website ( www.random.org ). In addition to their contact information, which was obtained from the SIB system (integrated health system), women were selected at random from the compiled list. To clarify, the selection of women from each center was determined based on the proportional sampling method, and the process of randomly selecting women was carried out utilizing the aforementioned website. Following a telephone conversation with the participants, wherein the researcher offered a concise overview of the research, the researcher proceeded to invite the women to attend the designated health center within the specified timeframe. The purpose of this visit was to provide additional explanations and administer the questionnaires. Upon conducting a visit and assessing the fundamental aspects such as basic information and inclusion and exclusion criteria, the individual proceeded to furnish the concerned parties with extensive details related to the research, its advantages, outcomes, and the confidentiality of the data. It is important to acknowledge that the random selection of participants was conducted before the assessment of their eligibility criteria. Following their visit to the health center, participants underwent a comprehensive evaluation to gather baseline data and determine their eligibility. Full information regarding the research objectives and methodology was exclusively provided to individuals who satisfied the predetermined eligibility criteria, and only they were extended an invitation to participatein the study. After agreeing to participate in the study, the participants proceeded to complete the informed consent form, the questionnaire of socio-demographic characteristics, and the BCPS.
The study’s inclusion criteria encompassed women who were at least 20 years old, exhibited no indications of abnormal breast lesions during clinical examination, and possessed the necessary literacy skills to complete the questionnaire. The study excluded individuals who met the following criteria: a confirmed diagnosis of breast cancer as documented in medical records, a history of cosmetic breast surgery, and impairment in communication skills related to hearing and speaking, and an inability to physically, cognitively, or mentally respond to questions.
Socio-demographic questionnaire
The questionnaire included questions regarding socio-demographic factors such as age, spouse age, marital status, educational level, job, income, breast cancer history, history of hormone therapy, family history of breast cancer and menopause status.
Breast cancer perception scale
Taylan et al. (2021) in Turkey [ 23 ] developed the BCPS. The present tool is grounded in the theoretical framework of the HBM and comprises a set of 24 items designed to assess women’s perceptions of breast cancer. The construct comprises six sub-dimensions, including Perceived knowledge, Perceived treatment belief, Perceived need for health check, Perceived stigma, Perceived fear and Perceived risk, which are assessed using a five-point Likert scale. The responses span a spectrum from strongly disagree (1) to strongly agree (5). The scale’s validity and reliability have been empirically established within the specific demographic of Turkish women in 2021. The lower bound of the scoring range for this questionnaire is 24, while the upper bound is set at 120. A positive correlation exists between higher scores and a greater level of women’s perception of breast cancer [ 23 ].
Sample size determination
It is imperative to ascertain the appropriate sample size to conduct the factor analysis procedure. According to a rule of thumb, the classification of sample size for EFA is as follows: a sample size of 50 is considered very poor, 100 is poor, 200 is fair, 300 is good, 500 is very good, and 1000 is excellent [ 32 ]. To ensure the reliability and validity of the results, it is necessary to have an appropriate sample size when conducting factor analysis. This study incorporated the guidelines proposed by Nunnally [ 33 ], which recommend a sample size of 5 to 10 samples for each instrument question to facilitate the generalizability of the findings to the broader community. Under these guidelines, it was deemed appropriate to utilize a sample size of 10 samples for each case, taking into account that the tool consisted of 24 items. Therefore, initially, a minimum of 240 samples were considered necessary. Nevertheless, it is imperative to take into account the effectof the cluster sampling technique employed in the research. The cluster sampling method introduces a factor of intra-cluster correlation that necessitates its inclusion in the calculation of the sample size [ 33 ]. To address this issue, a design effect of 1.5 was employed to modify the sample size. Due to a 10% attrition rate, the sample size has consequently expanded to encompass a total of 372 participants.
Statistical analysis
The statistical analysis was conducted using the SPSS software package (version 16, IBM Corp., Armonk, NY, USA), STATA14 (Statcorp, College Station, Texas, USA), and R software 4.2 (Psych package). To examine socio-demographic data, descriptive statistics were employed, including frequency (percentage) for qualitative variables, minimum and maximum values, and mean ± standard deviation (SD) for quantitative variables. The evaluation encompassed methodological testing, which involved the assessment of reliability, validity, and responsiveness. Exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) techniques were employed to assess construct validity on a larger scale. The direct oblimin method was employed in the EFA. Bartlett’s test for sphericity and KMO’s test for assessing the adequacy of scale content and sample size were conducted. The CFA methodology was employed to assess the factor structure and factor loadings of the scale. In conclusion, an assessment was conducted to evaluate the reliability of the study, specifically focusing on internal consistency, test-retest reliability, and measurement error. Finally, the presence of ceiling and floor effects was assessed.
Methodological testing according to the COSMIN checklist
- Reliability
Reliability refers to the extent to which a measurement is devoid of any errors that may arise during the measurement process. The evaluation of reliability primarily involves the assessment of three key characteristics: internal consistency, test-retest reliability, and measurement error [ 29 ].
Internal consistency
Internal consistency refers to the extent of interconnectedness among items. It serves as an estimation of the correlation level between the variables that constitute the intended structure or instrument [ 29 ]. The internal consistency of the instrument as a whole and its six subscales was assessed using both Cronbach’s alpha coefficient and McDonald’s omega coefficient. A minimum threshold of 0.7 was deemed necessary for both Cronbach’s alpha and MacDonald’s Omega coefficients to establish satisfactory internal consistency [ 34 ].
Test–retest reliability
Test-retest reliability refers to the extent to which the outcomes of a patient with identical health conditions remain consistent over a while [ 29 ]. Following the guidelines outlined in the COSMIN manual, a test-retest procedure was conducted with a minimum interval of two weeks. This time frame was chosen to prevent participants from recalling their previous responses and to account for any potential changes in their health status [ 29 ]. To achieve the intended objective, a survey was administered to a cohort of 30 female participants on two separate occasions, with a 14-day gap between each administration. The resulting scores were subsequently utilized to assess the reliability of the survey instrument through the application of the intraclass correlation coeficient (ICC). A reliability coefficient greater than 0.7 was deemed advantageous [ 34 ].
Measurement error
Measurement error is considered one of the key indicators of measurement and test reliability. In essence, it refers to the presence of both systematic and random errors in the patient’s score, which cannot be attributed to genuine variations in the construct under consideration. The calculation of the standard error of measurement (SEM) involves the use of the formula (SEM = SD√1-ICC), where SD represents the standard deviation [ 34 ]. The concept of the smallest detectable change (SDC) pertains to the minimum magnitude of an individual score change that can be accurately interpreted as a genuine change. The calculation of the SDC is determined by employing the formula (SDC = SEM*1.96*√2). A reduced level of the SDC corresponds to an increased level of measurement sensitivity [ 34 ].
Validity refers to the extent to which a given instrument accurately measures the specific characteristic it is designed to assess [ 29 ].
Face validity
Face validity is a concept that pertains to the extent to which the items within an instrument, specifically the HR-PRO, accurately represent the underlying construct that is intended to be measured [ 29 ]. The researchers conducted an assessment of face validity using both qualitative and quantitative methods. To conduct a qualitative assessment of face validity, a sample of 10 women from health centers in Tabriz City was selected using a convenience sampling method. This sample then examined the initial questionnaire. The participants assessed the quality, level of difficulty, lack of relevance, and degree of ambiguity of the items. To evaluate the face validity, item impact scores were quantitatively computed. During this phase, the aforementioned participants assessed each item on a 5-point Likert scale, ranging from “completely important” to “not at all important,” with scores ranging from 5 to 1 (representing “completely important,” “important,” “moderately important,” “slightly important,” and “not important,” respectively). The impact score is calculated by multiplying the Frequency (expressed as a percentage) by the Importance (Impact Score = Frequency (%) × Importance). Items with an impact score exceeding 1.5 were deemed appropriate and were subsequently retained for further stages of analysis [ 35 ].
Content validity
The degree to which the content of an HR-PRO instrument effectively represents the construct that is intended to be assessed [ 29 ]. Both qualitative and quantitative methods were used to examine the validity of the content of the questionnaire. To assess the credibility of the qualitative content, a group of ten experts, including three experts in reproductive health, two specialists in midwifery, three specialists in medical-surgical nursing, and two specialists in community health nursing, were invited to provide their insights and opinions on topics considering grammar, vocabulary choice, item arrangement, and scoring.
The inclusion criteria of the experts to determine content validity include voluntary participation, faculty members with the rank of assistant professor and above, PhDs of midwifery/nursing and individuals with clinical experience in breast cancer. The process of assessing quantitative content validity involves the calculation of two measures: the content validity ratio (CVR) and the content validity index (CVI) [ 36 ]. To fulfill the objective, a questionnaire comprising questions organized into two overarching categories was distributed to each expert. In the initial phase, the participants assessed the items using a 3-point Likert scale (necessary, useful but not necessary, not necessary) to ascertain the CVR, which was computed using the following mathematical expression:
CVR= (Ne-N/2)/ (N/2).
Where, “Ne” represents the count of experts who have chosen the “necessary” option, and N denotes the total number of experts. Regarding Lawshe table, a CVR > 0.62 for a sample size of 10 individuals, confirms the essentiality of the items under investigation [ 37 ].
Subsequently, the CVI review underwent evaluation by an identical group of 10 experts. Concerning this matter, questions have been raised regarding the three criteria of relevance, clarity, and simplicity for each item. These criteria have been assessed using a four-point Likert scale, which includes options such as irrelevant, somewhat relevant, relevant, and completely relevant. The assessment is based on the content validity index [ 38 ] developed by Waltz and Basel. The level of relevance, clarity, and simplicity was assessed by experts based on their subjective evaluation, and then the CVI was computed using the following formula:
CVI = number of experts giving a rating of 3 and 4 / total number of experts.
CVIs higher than 0.79, between 0.70 and 0.79, and less than 0.70 were considered acceptable, in need of correction, and unacceptable, respectively [ 39 ].
Construct validity
The concept of construct validity pertains to the extent to which the scores obtained from an HR-PRO instrument align with the anticipated hypotheses. This alignment can be observed in terms of internal relationships, relationships with scores obtained from other instruments, or differences between relevant groups. This assessment is contingent upon the assumption that the HR-PRO instrument possesses validity. The concept of validity pertains to the extent to which a given measure accurately assesses the construct it is intended to measure. The three aspects encompassed in this study are as follows: structural validity, which pertains to the internal relationships within the construct; hypothesis testing; and cross-cultural validity, which focuses on the relationships with scores on other instruments or differences between relevant groups [ 29 ].
Structural validity
The suitability of the data for EFA was assessed by employing the Kaiser-Meyer Olkin (KMO) criterion and Bartlett’s test of sphericity. The KMO test is a statistical measure that quantifies the proportion of variance in the questions that can be attributed to the primary factors. Typically, values falling within the range of 0.8–1 are indicative of adequate data sampling to conduct factor analysis. However, when the value of the statistic falls below 0.7, it indicates that the sample size is insufficient, necessitating the implementation of corrective actions [ 40 ].
Bartlett’s test of sphericity is a frequently employed statistical test to assess the appropriateness of data for factor analysis. The significance of this test serves as an indicator of the suitability of the data for factor analysis [ 40 ]. The process of extracting factors from the 24 items of the questionnaire was conducted using the principal component analysis method, employing varimax rotation (direct oblimin). The determination of the number of factors was based on the criterion of an Eigenvalue greater than 1 and the examination of the Scree plot. In this analysis, a minimum factor loading threshold of 0.3 was utilized for the extraction of factors. In contrast, CFA employs the maximum likelihood method to estimate the model’s fit indices, and a range of indices are utilized to assess the appropriateness of the model. This study assessed the adequacy of the model by employing the indicators outlined below [ 41 ]:
Root mean score error of approximation (RMSEA < 0.08), standardized root mean square residual (SRMR < 0.10), normed Chi 2 (x 2 / df) < 5, comparative fit indices including comparative fit index (CFI > 0.90), Bentler-Bonett Normed Fit Index (NFI) > 0.90, Relative fit index (RFI) > 0.90 and Tucker-Lewis Index (TLI) > 0.90.
Hypothesis testing
The process of hypothesis testing is characterized by its continuous and iterative nature. Hypotheses serve as a means to express the anticipated direction and magnitude of correlations or differences between the construct under investigation and other constructs. As the number of hypotheses tested regarding the alignment between the data and pre-existing hypotheses increases, a greater amount of evidence supporting construct validity is accumulated [ 29 ]. To assess construct validity, an analysis of the hypotheses that were previously formulated was conducted. In this study, it was postulated that the BCPS would exhibit a strong correlation with other subjective scales, such as quality-of-life instruments for cancer patients (QLICP-BR V2.0). Hence, confirmation of the desired hypothesis can be achieved when the Pearson correlation coefficient exceeds 0.5. Furthermore, the study computed the floor and ceiling effect (F/C) as well as the proportion of women who achieved the minimum and maximum scores. F/C effects refer to the percentage of individuals who achieve the highest (ceiling) or lowest (floor) possible scores within a specific domain. These effects serve as indicators of a questionnaire’s sensitivity and coverage at the extreme ends of the scale. In the context of this study, a problematic scenario is defined as a situation where 15% or more of the respondents fall into either the ceiling or floor category [ 42 ].
Responsiveness
Measurement instruments should possess a high degree of sensitivity to detect and accurately capture changes, while also demonstrating a responsive nature to promptly reflect these changes. According to the COSMIN checklist, responsiveness refers to the capacity of an HR-PRO instrument to accurately identify alterations in the construct being assessed over a while [ 29 ]. Terwee et al. [ 34 ] argue that responsiveness can be assessed by examining the relationship between the smallest detectable change (SDC) and the minimally important change (MIC). If the value of SDC is less than MIC, then the responsiveness is confirmed.
Interpretability
Interpretability refers to the extent of qualitative significance, specifically the minimally important changes (MIC) within the instrument. The extent to which quantitative instrument scores or changes in scores can be attributed to qualitative meaning, such as clinical or commonly understood meanings, has been discussed [ 29 ]. The estimation of the minimum important change (MIC) was conducted by dividing the standard deviation (SD) by two, as outlined in the study conducted by Norman et al. [ 43 ].
Descriptive characteristics of participants
This study involved the participation of 372 women. The participants were randomly split into two groups, one group of 172 participants for EFA and another group of 200 participants for CFA. The average age was 52.7 and 52.3 years with a standard deviation of 9.5 and 8.5 years in EFA and CFA group, respectively. A significant majority of the individuals surveyed were married (78.5%, 80.5% in EFA and CFA group, respectively), and 73.8%, 61.0% of them identified themselves as housewives in EFA and CFA group, respectively. Table 1 provides a summary of the additional socio-demographic characteristics of the two groups of participants.
In the present study, the mean (SD) of the entire BCPS scale was 61.66 (8.44), with a range of obtainable scores from 24 to 120. The mean (SD) for the six extracted factors, namely Perceived fear, Perceived knowledge, Perceived treatment belief, Perceived risk, Perceived need for a health check, and Perceived stigma, were respectively 8.28 (4.02), 11.63 (3.79), 10.5 (2.41), 9.37 (2.12), 10.19 (3.22), and 12.15 (2.65).
The values of Cronbach’s alpha and McDonald’s omega (95% CI) were found to be 0.68 and 0.70 (0.66 to 0.74), respectively. These results suggest that the questionnaire exhibits satisfactory internal consistency. Also, the ICC (95% CI) gave a value of 0.97 (0.94 to 0.99). Standard error of measurment is a statistical metric utilized to assess the accuracy and consistency of a given measurement. The SEM value in this study was determined to be 1.36. This implies that upon conducting multiple iterations of the measurement, it is anticipated that the recorded values will fall within a range of ± 1.36 units with the actual score. Moreover, the SDC denotes the smallest detectable change that can be consistently detected by the measuring apparatus. Within the given framework, the value of SDC was ascertained to be 3.73 units. This implies that any deviation in the measured quantity that is less than 3.73 units may not be discernible due to measurement errors and can be regarded as insignificant (Table 2 ).
The tool’s content and face validity were assessed using the CVI (CVI range: 0.87–1.00), CVR (CVR range: 0.75–1.00), and impact scores (3.06–4.00), which yielded values of 0.98, 0.95, and 3.70, respectively.
The construct validity investigation involved conducting an EFA on a set of 24 items. The resulting Kaiser-Meyer-Olkin (KMO) value of 0.71 was obtained at a statistically significant level of less than 0.001, indicating that the sample size in the current study was sufficient. Furthermore, the statistical analysis revealed that Bartlett’s test of sphericity yielded a significant result ( p ≤ 0.001), indicating that factor analysis was appropriately conducted based on the correlation matrix in the sample under investigation.
The scree plot displayed the results of EFA, revealing six factors with eigenvalues > 1. These factors collectively accounted for 52% of the variance (Fig. 1 ). Table 3 presents the extracted components alongside the corresponding items associated with each factor. The initial factor examined in this study was Perceived fear, comprising a set of four questions that contributed to 13.60% of the overall variance. The second factor, referred to as Perceived knowledge, comprises a set of four questions that collectively account for 11.00% of the overall variance. The third and fourth factors were Perceived treatment belief and Perceived risk, respectively. These factors consisted of four and two questions, respectively, and accounted for 8.9% and 6.4% of the variance. The fifth factor, referred to as Perceived need for a health check, consists of four questions with a variance of 6.3%. Additionally, the sixth factor, known as “Perceived stigma,” comprises four questions that account for 5.8% of the total variance (Fig. 2 ). After preliminary psychometric testing, 24 items were factor-analysed providing a 22-item, six-factor scale. It is important to highlight that, in the original instrument, questions 9 and 23, respectively addressed the notions that “Breast cancer treatment does not change the outcome” and “The risk for breast cancer is higher in those with a family history of breast cancer,” were excluded from the EFA in the present study due to their factor loadings being less than 0.3. Consequently, there was a reduction in the number of instrument questions from 24 items in the original instrument to 22 items.

Factor load scree plot of the items for determining the number of extracted factors of the Iranian version of BCPS

Factor structure model of the BCPS based on CFA. All factor-item relationships were significant ( P < 0.05). Fc1: Perceived fear, Fc2: Perceived knowledge, Fc3: Perceived treatment belief, Fc4: Perceived risk, Fc5: Perceived need for health check, Fc6: Perceived stigma
CFA was employed to examine the six factors that were derived from EFA. The findings indicate that the model has attained a level of fit that is considered optimal, thereby providing support for confirming the factor structure. The indicator \(\raisebox{1ex}{${x}^{2}$}\!\left/ \!\raisebox{-1ex}{$df$}\right.\) is found to be 2.029 (χ2 = 393.781, df = 194, P-value < 0.001). Additionally, the fit indexes TLI, CFI, NFI, and RFI all exceed the threshold of 0.9. Furthermore, the RMSEA and SRMR index values are both equal to 0.055, indicating a valid model.
Hypothesis testing, responsiveness and interpretability
The hypothesis confirmation involved the computation of Spearman’s correlation coefficient between the BCPS and QLICP-BR V2.0, and the resulting coefficient of 0.55 indicated a statistically significant correlation. To assess the feasibility of the tool, the ceiling effect in the overall score of BCPS was found to be 0.3%. In the sub-domains, the ceiling effects for Perceived fear, Perceived knowledge, Perceived treatment belief, Perceived risk, Perceived need for a health check, and Perceived stigma were determined to be 2.2%, 0.4%, 0.3%, 1.1%, 0.3%, and 0.8%, respectively. The floor effect in the overall score of BCPS was observed to be 0.5%, while in the specific subdomains, it was found to be 26.9%, 3.5%, 3.2%, 1.3%, 4.6%, and 0.8%, respectively. It is noteworthy to mention that the MIC refers to a specific threshold value that delineates the smallest alteration in the measured parameter that holds clinical or practical significance. In this particular instance, the MIC was determined to be 3.92 units. Specifically, the study reveals that the MIC value surpasses the SDC value by 3.73 units. This observation indicates that the Iranian version of the measurement tool is sufficiently responsive. Put simply, the measurement tool can accurately identify and assess changes that hold significance or relevance within the given measurement framework. SEM of this study’s findings generally implies that the measuring device used exhibits a satisfactory level of precision. The comparison between the SDC and the MIC values further demonstrates the instrument’s capacity to consistently identify significant variations in the measured variable (Table 2 ).
The aim of this study was to assess the measurment properties of the Breast Cancer Perception Scale (BCPS) in Iranian women, according to the COSMIN checklist for the first time. The findings of the research substantiate the validity, reliability, responsiveness, and interpretability of the BCPS, which is grounded in the health belief model (HBM) when applied to Iranian women.
The HBM has been widely employed in the study of breast cancer diagnostic behaviors for an extended period [ 25 , 26 , 27 ]. The BCPS is a novel screening tool for breast cancer that has been developed utilizing the HBM [ 23 ]. Despite the presence of various tools in this domain, such as “belief in mammography” and “breast self-examination,” “perceived sensitivity toward breast cancer,” “perceived benefits and obstacles of mammography usage,” “fear of breast cancer (FBC)”, and “fatalism regarding cancer “, these instruments appear to lack practicality as they assess factors individually and fail to encompass all relevant domains. The BCPS demonstrates utility in its comprehensive coverage of various domains, particularly in assessing previously unmeasured aspects such as perceived knowledge, and mental measurements, including the perceived need for a health check, perceived stigma, perceived fear, and perceived risk [ 23 ].
Breast cancer perception is one of the most important indicators for preventing breast cancer and adopting protective behaviors against breast cancer. Proper perception of breast cancer serves as a motivator for women to adhere to breast cancer prevention methods. Despite the existence of various preventive and diagnostic methods for breast cancer, none of these methods will be effective until there is a proper perception of breast cancer. Therefore, the BCPS scale, considering important dimensions such as Perceived knowledge, Perceived treatment belief, Perceived need for health check, Perceived stigma, Perceived fear and Perceived risk, can play an important role in creating preventive behaviors against breast cancer [ 23 ].
In the current investigation, EFA was conducted on a set of 24 items of the instrument. The analysis yielded six factors, namely Perceived fear, Perceived knowledge, Perceived treatment belief, Perceived risk, Perceived need for a health check, and Perceived stigma. These factors aligned with the original instrument and collectively accounted for approximately 52% of the variance, while in the original instrument, they accounted for 74.36% of the variance [ 23 ]. To assess the validity of the instrument, the KMO measure was computed, yielding a value of 0.71. Additionally, the adequacy of the model was verified through Bartlett’s test, which yielded a significance level of 0.77 in the original study [ 23 ]. Furthermore, the reliability of the instrument was obtained ranging from 0.64 to 0.94 by using Cronbach’s alpha, and these values align with the original study’s reported range of 0.81 to 0.95 [ 23 ].
In the present study, the initial factor extracted during the exploratory EFA was identified as perceived fear. The influence of perceived fear on women’s adoption of protective behaviors against breast cancer can be observed. The findings of various studies indicate that a significant majority of women encounter fear regarding the potential diagnosis of breast cancer and the subsequent possibility of undergoing a mastectomy, either unilaterally or bilaterally, at some point in their lives [ 44 , 45 ]. In a similar vein, a separate study indicated that women who exhibited a heightened FBC were found to undergo mammograms less frequently within a one-year timeframe in comparison to their counterparts [ 46 ]. In the study conducted by Aguirre et al., it was observed that young Spanish women exhibited a notable level of fear towards breast cancer, despite not expressing a general sense of concern regarding the disease. According to the study [ 47 ], it was found that 25.3% of the participants reported above-average FBC, while 59.7% reported high FBC. This finding implies that breast cancer may elicit a particularly strong sense of fear, even among young women who do not have significant health issues and have a low objective risk. This observation aligns with the findings of previous research [ 48 , 49 ]. Furthermore, when comparing the findings of this study to previous research conducted within the past two decades, it becomes evident that the extent of fear induced by breast cancer has remained relatively stable despite favorable epidemiological advancements such as reduced mortality rates and enhanced treatment options [ 50 ].
The second factor that was extracted in this study related to perceived knowledge. Perceived knowledge encompasses biases, such as unrealistic optimism and implicit confidence [ 51 ]. The concept of perceived knowledge pertains to an individual’s level of knowledge and is not directly associated with one’s knowledge, specifically regarding breast cancer. The WHO has advocated for the adoption of breast cancer knowledge and awareness as a viable medical strategy for the management of breast cancer. This approach is deemed essential and should be universally implemented, irrespective of financial constraints. In this regard, Izanloo et al. demonstrated that a significant majority of the participants, totaling over 84%, exhibited a lack of knowledge regarding breast cancer and screening tests among 14- to 84-year-old Iranian women. The primary factors cited by women as barriers to undergoing screening tests were the absence of discernible symptoms or issues and their perception of the test’s necessity. A significant difference was observed in the level of women’s knowledge of breast cancer and screening tests concerning factors such as employment status, education level, and family history of breast cancer. However, no significant difference was found in the level of knowledge among women based on their marital status or income level [ 52 ]. Moreover, a study conducted by Mehejabin et al. sought to examine the level of knowledge regarding various aspects of breast cancer among women in Bangladesh. The findings revealed that a majority of the participants, exceeding 50%, possessed a limited understanding of the risk factors associated with breast cancer, indicating a significant lack of knowledge [ 53 ].
Perceived treatment beliefs constituted an additional factor. Perceived belief in treatment can be influenced by various factors, including women’s spiritual and religious beliefs, familial history of breast cancer treatment, and prior experiences with breast cancer treatment [ 45 ]. Concerning this matter, individuals’ perceptions of their treatment beliefs have the potential to influence their engagement in protective behaviors. The findings of the study conducted by Mehejabin et al. indicate that a considerable proportion of women hold the belief that breast cancer can be detected at a young age. Furthermore, the participants held the belief that early diagnosis of the disease could lead to its potential cure [ 53 ]. The aforementioned findings align with the results obtained from a research study carried out at Dhaka Medical College Hospital in Bangladesh, wherein 51.43% of female participants indicated that early detection of breast cancer leads to a potential cure [ 54 ]. Suwankhong and Liamputtong have posited that religious belief significantly influences individuals’ decision-making processes concerning treatment options and risk factors associated with breast cancer [ 55 ]. Yew et al., found a significant difference in the perceptions of breast cancer risk with religious affiliations, specifically between the Muslim and Buddhist cohorts. The impact of Islam and Buddhism on individuals’ lifestyles and health-related behaviors has been significant. Muslim women exhibited a profound conviction in the authority of God (Allah), whereas Buddhist women commonly invoked their karma [ 56 ].
Perceived risk, identified as an additional extracted factor, holds a significant influence over breast cancer protective behavior [ 45 ]. Observing the challenges and distress experienced by our beloved individuals throughout breast cancer treatment amplifies both the perceived fear and the perceived risk of breast cancer [ 57 ]. The primary determinant of health behaviors for breast cancer prevention, diagnosis, and control is the perceived risk. Conversely, establishing concordance between the perceived risk and the objective risk of developing breast cancer results in a more accurate and actual perception of the risk. Consequently, it can serve as motivation for fostering suitable health behaviors [ 58 ]. Hajian et al. [ 59 ], examined the perceived risk of breast cancer among 800 Iranian women about the actual risk. The findings of the study revealed that both women with a low and high risk of breast cancer exhibited a significantly higher perceived risk of the disease compared to their actual risk. This finding suggests a significant inclination towards pessimism in the assessment of breast cancer risk, consistent with previous research conducted in this domain [ 60 , 61 ].
The results of this study also identified the perceived need for a health check as an additional extracted factor. One of the main obstacles to breast cancer screening among women is a diminished perception of the necessity for health screening. Women typically do not perceive the necessity of seeking medical attention unless they possess knowledge regarding the specific symptoms associated with a particular ailment [ 62 ]. Research findings indicate that women residing in developing nations often tend to decline the notion of early diagnosis and screening for breast cancer, primarily influenced by their cultural and personal beliefs. The aforementioned factor has a detrimental impact on the implementation of preventive measures aimed at mitigating the risk of breast cancer [ 63 ]. Therefore, variations in the perceived need for health screening can potentially impact individuals’ engagement in breast cancer protective behaviors. The scoping review study conducted by Omidi et al. examined the current status of breast cancer screening strategies and indicators among Iranian women. The study findings revealed that the prevalence rates of screening methods, including BSE, CBE, and mammography, among Iranian women were reported as 0-79.4%, 4.1–41.1%, and 1.3–45%, respectively [ 64 ].
Based on the HBM theory, Darvishpour et al. [ 25 ] posited that the decision of women to engage in breast cancer screening is influenced by factors such as self-efficacy and perceived benefits. Conversely, the presence of perceived barriers diminishes the likelihood of self-examination. According to Khazir et al., individuals who perceive fewer barriers are more likely to engage in breast cancer screening programs [ 65 ]. Abdel-Aziz et al. conducted a study utilizing EFA to examine the perceived barriers faced by women with breast cancer. Their findings indicate that personal fears, specifically fear of doctors/examiners, fear of screening results, and fear of the hospital environment, are the primary obstacles preventing women from utilizing free screening. These fears were identified as the main barriers based on their eigenvalue values, which exceeded 3.335, representing 30.4% of the barriers identified [ 66 ].
The final factor that was extracted pertains to the concept of perceived stigma. The symbolic significance of breasts for women stems from their association with childbirth, breastfeeding, childrearing, and sexual desires. Consequently, the symbolic significance associated with this phenomenon may impede women from accessing necessary healthcare services, interventions, or diagnostic procedures [ 67 ]. Furthermore, the absence of discussion regarding breast cancer and screening behaviors may be associated with societal stigmatization and cultural taboos surrounding the topic of breasts [ 68 ]. It is well known that stigma plays a significant role in the psychological distress that breast cancer-diagnosed women experience. The occurrence of rejection, blame, or devaluation is what defines the social phenomenon known as stigma. This arises from the personal experience, perception, or rational expectation of an unfavorable social evaluation directed toward an individual or a collective entity [ 69 ]. It was found that around 76.7% and 8.7% of breast cancer survivors reported moderate and high levels of stigma, respectively [ 70 ]. Based on prior research, it has been established that the perceived stigma among individuals diagnosed with breast cancer has significant adverse consequences for their overall well-being and health-related outcomes. These repercussions encompass various aspects such as sexual dysfunction, depressive symptoms, compromised sleep quality, reduced inclination to seek medical assistance, and diminished quality of life [ 71 ].
In terms of clinical application, the use of this scale is considered to save time and enable early detection of breast cancer during assessment. Utilizing this screeninig tool by health care providers improves a quick and comprehensive attitude toward breast cancer perception among women. The main advantage of BCPS is that it helps more subjective measurements compared to other scales in this area. In addition, its goal is to evaluate the relationship between breast cancer and diagnostic behaviors for breast cancer (such as maintaining healthy behaviors like diet, physical activity, mammography, breast self-examination, and clinical breast examination), knowledge about breast cancer, and family history of breast cancer [ 23 ].
Strength and limitation
The present study possesses several notable strengths. Firstly, it is the first study to assess BCPS among Iranian women. Secondly, the study adheres to the COSMIN checklist, ensuring methodological rigor. Additionally, the study incorporates both the DP and FB methods for the translation process, effectively addressing the limitations associated with the FB method. Lastly, the study includes a comparative analysis of BCPS with other versions.
However, it is important to acknowledge the limitations of the current study. These limitations include the lack of criterion validity calculations due to the lack of a gold standard, the lack of an assessment of cross-cultural validity and the possibility of bias from participants’ tendency to give socially desirable answers when using self-reported measures. As we conducted this study in Tabriz-Iran, should be cautious about the generalizability of findings. In conclusion, it is recommended that future research endeavors employ a larger sample sizeand assess the measurment properties in diverse contexts.
The obtained findings suggest that the Iranian version of the BCPS demonstrates satisfactory measurment properties for assessing the perception of breast cancer among Iranian women. Furthermore, it exhibits favorable responsiveness to clinical variations. The assessment of women’s perceptions of breast cancer is imperative for the advancement of preventive behaviors against this disease. The present scale can be employed for the assessment of the association between breast cancer and behaviors related to breast cancer diagnosis, including breast self-examination, clinical breast examination, mammography, and the adoption of healthy behaviors such as diet and exercise. Finally, it can be utilized to investigate the correlation between breast cancer knowledge and family history.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the limitations of ethical approval involving the patient data and anonymity, but are available from the corresponding author upon reasonable requests.
Abbreviations
Breast Cancer Perception Scale
Consensus-Based Standards for the Selection of Health Status Measurement Instruments
Breast Cancer
Global Cancer Incidence Mortality and Prevalence
World health organization
Eastern Mediterranean Region
Age-standardized rate
Hormone replacement therapy
Visual Analouge Scale
Health Belief Model
Breast self-examination
Clinical Breast Examination
Health related-patient reported outcomes
Dual pannel
Forward-backward
Exploratory factor analysis
Confirmatory factor analysis
Intra-class Correlation Coefficient
standard deviation
Content validity index
Content validity ratio
Standard error of measurment
Smallest detectable change
Minimal important change
Degree of freedom
Average variance extracted
Kaiser-Meyer-Olkin
Root mean squared error of approximation
Comparative fit index
Tucker–Lewis index
Ferlay J, Soerjomataram I, Ervik M, Dikshit S, Eser C, Mathers M, et al. V1. 0, cancer incidence and mortality worldwide: IARC CancerBase No. 11. 2013. Lyon, France: International Agency for Research on Cancer; 2012.
Google Scholar
Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, et al. The global burden of Cancer 2013. JAMA Oncol. 2015;1(4):505–27.
Article PubMed Google Scholar
Parkin DM, Läärä E, Muir CS. Estimates of the worldwide frequency of sixteen major cancers in 1980. Int J Cancer. 1988;41(2):184–97.
Article CAS PubMed Google Scholar
Sung H, Ferlay J, Siegel RL, Global Cancer S. 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209 – 49.
Sedeta ET, Jobre B, Avezbakiyev B. Breast cancer: global patterns of incidence, mortality, and trends. J Clin Oncol. 2023;41(16).
Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol. 2021;18(10):663–72.
Siegel RL, Giaquinto AN. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):12–49.
Hortobagyi GN, de la Garza Salazar J, Pritchard K, Amadori D, Haidinger R, Hudis CA, et al. The global breast cancer burden: variations in epidemiology and survival. Clin Breast Cancer. 2005;6(5):391–401.
Sharif Nia H, Behmanesh F, Kwok C, Firouzbakht M, Ebadi A, Nikpour M. Breast cancer screening beliefs questionnaire: psychometric properties of the Persian version. BMC Womens Health. 2020;20(1):184.
Article PubMed PubMed Central Google Scholar
Akbari M, Abachizadeh K, Tabatabaei S, Ghanbari Motlagh A, Majd Jabari Z, Khayamzadeh M. Cancer in Iran. Qom: Darolfekr; 2008.
Razi S, Salehiniya H, Dizaji M. Epidemiology of prevalent cancer among Iranian women and its incidence trends from 2003–2009 in Iran. AMUJ. 2015;18(2):17–24.
Kazeminia M, Salari N, Hosseinian-Far A, Akbari H, Bazrafshan M-R, Mohammadi M. The prevalence of breast cancer in Iranian women: a systematic review and meta-analysis. Indian J Gynecol Oncol. 2022;20(1):14.
Article Google Scholar
Giaquinto AN, Sung H, Miller KD, Kramer JL, Newman LA, Minihan A, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72(6):524–41.
Shamshirian A, Heydari K. Breast cancer risk factors in Iran: a systematic review & meta-analysis. Horm Mol Biol Clin Investig. 2020;41(4).
Weinstein ND. What does it mean to understand a risk? Evaluating risk comprehension. J Natl Cancer Inst Monogr. 1999(25):15–20.
Osei E, Osei Afriyie S, Oppong S, Ampofo E, Amu H. Perceived breast Cancer risk among female undergraduate students in Ghana: a cross-sectional study. J Oncol. 2021;2021:8811353.
Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. Wiley; 2008.
Rakhshkhorshid M, Navaee M. The Association of Health Literacy with breast Cancer knowledge, perception and screening behavior. Eur J Breast Health. 2018;14(3):144–7.
PubMed PubMed Central Google Scholar
Fletcher SW, Elmore JG. Clinical practice. Mammographic screening for breast cancer. N Engl J Med. 2003;348(17):1672–80.
Vetter L, Keller M, Bruckner T, Golatta M, Eismann S, Evers C, et al. Adherence to the breast cancer surveillance program for women at risk for familial breast and ovarian cancer versus overscreening: a monocenter study in Germany. Breast Cancer Res Treat. 2016;156(2):289–99.
Brinton LA, Brown SL, Colton T, Burich MC, Lubin J. Characteristics of a population of women with breast implants compared with women seeking other types of plastic surgery. Plast Reconstr Surg. 2000;105(3):919–27. discussion 28 – 9.
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81(24):1879–86.
Taylan S, Özkan İ. Breast Cancer Perception Scale: Psychometric Development Study. Eur J Breast Health. 2021;17(2):95–102.
Becker MH. The health belief model and personal health behavior. Health Educ Monogr. 1974;2:324–473.
Darvishpour A, Vajari SM, Noroozi S. Can Health Belief Model predict breast Cancer screening behaviors? Open Access Maced J Med Sci. 2018;6(5):949–53.
Fouladi N, Pourfarzi F, Mazaheri E, Asl HA, Rezaie M, Amani F, et al. Beliefs and behaviors of breast cancer screening in women referring to health care centers in northwest Iran according to the champion health belief model scale. Asian Pac J Cancer Prev. 2013;14(11):6857–62.
MASOUDI YL, Dashtbozorgi B, Gheibizadeh M, SAKI MA, Moradi M. Applying the health belief model in predicting breast cancer screening behavior of women. Jundishapur J Chronic Dis Care. 2015;4(4):e30234.
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19(4):539–49.
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. COSMIN checklist manual. Amsterdam: University Medical Center; 2012.
World Health Organization. Process of translation and adaptation of instruments. 2010.
Kalfoss M. Translation and adaption of questionnaires: a nursing challenge. SAGE Open Nurs. 2019;5:2377960818816810.
Comrey A, Lee H. A first course in factor analysis: psychology press. Taylor and Francis Group New York, NY; 2013.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGrawHill; 1994.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
Seyf AA. Measurement, test and educational evaluation. 7th ed. Tehran: Douran; 2016.
Yang Z, Sun Y, Wang H, Zhang C, Wang A. A scale for measuring home-based cardiac rehabilitation exercise adherence: a development and validation study. BMC Nurs. 2023;22(1):259.
Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–75.
Waltz CF, Bausell BR. Nursing research: design statistics and computer analysis. Davis Fa; 1981.
Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–67.
Harerimana A, Mtshali NG. Using exploratory and Confirmatory Factor Analysis to understand the role of technology in nursing education. Nurse Educ Today. 2020;92:104490.
Schreiber J, Nora A, Stage F, Barlow L, King J. Confirmatory factor analyses and structural equations modeling: an introduction and review. J Educ Res. 2006;99(6).
Gulledge CM, Smith DG, Ziedas A, Muh SJ, Moutzouros V, Makhni EC. Floor and Ceiling effects, Time to Completion, and question burden of PROMIS CAT domains among shoulder and knee patients undergoing nonoperative and operative treatment. JB JS Open Access. 2019;4(4).
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92.
George TO, Allo TA, Amoo EO, Olonade O. Knowledge and attitudes about breast Cancer among women: a Wake-Up call in Nigeria. Open Access Maced J Med Sci. 2019;7(10):1700–5.
Kardan-Souraki M, Moosazadeh M, Khani S, Hamzehgardeshi Z. Factors related to breast Cancer screening in women in the Northern Part of Iran: a cross-sectional study. Open Access Maced J Med Sci. 2019;7(4):637–42.
Sohbet R, Karasu F. Investigation of the knowledge, behavior and applications of their women towards breast cancer. Gumushane Univ J Health Sci. 2017;6(4):113–21.
Aguirre-Camacho A, Hidalgo B, González-Cuevas G. Fear of breast cancer among young Spanish women: factor structure and psychometric properties of the Champion breast cancer fear scale. PLoS ONE. 2021;16(4):e0249562.
Article CAS PubMed PubMed Central Google Scholar
Berry TR, Curtin KD, Courneya KS, McGannon KR, Norris CM, Rodgers WM, et al. Heart disease and breast cancer perceptions: ethnic differences and relationship to attentional bias. Health Psychol Open. 2016;3(2):2055102916657673.
Vraga EK, Stefanidis A, Lamprianidis G, Croitoru A. Cancer and Social Media: a comparison of traffic about breast Cancer, prostate Cancer, and other Reproductive cancers on Twitter and Instagram. J Health Commun. 2018;23(2):181–9.
Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends–An Update. Cancer Epidemiol Biomarkers Prev. 2016;25(1):16–27.
Pohl R, Pohl RF. Cognitive illusions: a handbook on fallacies and biases in thinking. judgement and memory: Psychology; 2004.
Izanloo A, Ghaffarzadehgan K, Khoshroo F, Erfani Haghiri M, Izanloo S, Samiee M, et al. Knowledge and attitude of women regarding breast cancer screening tests in Eastern Iran. Ecancermedicalscience. 2018;12:806.
Mehejabin F, Rahman MS. Knowledge and perception of breast cancer among women of reproductive age in Chattogram, Bangladesh: a cross-sectional survey. Health Sci Rep. 2022;5(5):e840.
Chowdhury S, Sultana S. Awareness on breast cancer among the women of reproductive age. JFRH. 2011;5(4).
Suwankhong D, Liamputtong P. Experiences of living with HIV: social stigma and discrimination among HIV-positive mothers in Southern Thailand. Malays J Med Health Sci. 2021;17:36–42.
Yew WC, Awang AH, Selvadurai S, Mohd Noor M, Chang PK. A Comparative Study of Islam and Buddhism: a Multicultural Society Perspective. Religions. 2021;12(12):1098.
Hashemi-Ghasemabadi M, Taleghani F, Kohan S, Yousefy A. Living under a cloud of threat: the experience of Iranian female caregivers with a first-degree relative with breast cancer. Psychooncology. 2017;26(5):625–31.
Katapodi MC, Dodd MJ, Facione NC, Humphreys JC, Lee KA. Why some women have an optimistic or a pessimistic bias about their breast cancer risk: experiences, heuristics, and knowledge of risk factors. Cancer Nurs. 2010;33(1):64–73.
Hajian-Tilaki K, Nikpour M. Accuracy of self-perceived risk perception of breast cancer development in Iranian women. BMC Womens Health. 2021;21(1):93.
Aduayi VA, Onayade AA, Aduayi OS, Odu OO. Relating self-perceived with objective risk for breast cancer among women in rural and urban communities in southwestern Nigeria. Int J Med Sci Public Health. 2015;4(10):1.
Ceber E, Soyer MT, Ciceklioglu M, Cimat S. Breast cancer risk assessment and risk perception on nurses and midwives in Bornova Health District in Turkey. Cancer Nurs. 2006;29(3):244–9.
Kwok C, Endrawes G, Lee CF. Cultural beliefs and attitudes about breast Cancer and Screening practices among Arabic women in Australia. Cancer Nurs. 2016;39(5):367–74.
Donnelly TT, Khater AH, Al-Bader SB, Al Kuwari MG, Al-Meer N, Malik M, et al. Arab women’s breast cancer screening practices: a literature review. Asian Pac J Cancer Prev. 2013;14(8):4519–28.
Omidi Z, Koosha M, Nazeri N, Khosravi N, Zolfaghari S, Haghighat S. Status of breast cancer screening strategies and indicators in Iran: a scoping review. J Res Med Sci. 2022;27:21.
Khazir Z, Morrowati Sharifabad MA, Vaezi AA, Enjezab B, Fallahzadeh H, Yari F. Predictors of mammography based on Health Belief Model in Khorramabad women. J Educ Health Promot. 2019;8:180.
Abdel-Aziz SB, Amin TT, Al-Gadeeb MB, Alhassar AI, Al-Ramadan A, Al-Helal M, et al. Perceived barriers to breast cancer screening among Saudi women at primary care setting. J Prev Med Hyg. 2018;59(1):E20–9.
CAS PubMed PubMed Central Google Scholar
Banning M, Hafeez H. A two-center study of muslim women’s views of breast cancer and breast health practices in Pakistan and the UK. J Cancer Educ. 2010;25(3):349–53.
Sheppard VB, Christopher J, Nwabukwu I. Breaking the silence barrier: opportunities to address breast cancer in African-born women. J Natl Med Assoc. 2010;102(6):461–8.
PubMed Google Scholar
Lebel S, Devins GM. Stigma in cancer patients whose behavior may have contributed to their disease. Future Oncol. 2008;4(5):717–33.
Jin R, Xie T, Zhang L, Gong N, Zhang J. Stigma and its influencing factors among breast cancer survivors in China: a cross-sectional study. Eur J Oncol Nurs. 2021;52:101972.
Wang Q-X, Bai Y, Lu G-F, Zhang C-Y. Perceived health-related stigma among patients with breast cancer. Chin Nurs Res. 2017;4(4):158–61.
Download references
Acknowledgements
We should thank the Vice-chancellor for Research of Tabriz University of Medical Sciences for their financial support and the invaluable participation of women would be appreciated.
This Study is funded by Tabriz University of Medical Sciences (grant number: 69930). The funding source had no role in the design and conduct of the study, and decision to this manuscript writing and submission.
Author information
Authors and affiliations.
Students Research Committee, Midwifery Department, Faculty of Nursing and Midwifery, Tabriz University of Medical sciences, Tabriz, Iran
Sepideh Mashayekh-Amiri
Cabrini Research, Cabrini Health, Melbourne, VIC, 3144, Australia
Mohammad Asghari Jafarabadi
School of Public Health and Preventative Medicine, Faculty of Medicine, Nursing and Health Sciences, Monash University, VIC 3800, Melbourne, Australia
Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Department of Community Health Nursing, Nursing and Midwifery Faculty, Tabriz University of Medical Sciences, Tabriz, Iran
Mina Hosseinzadeh
Department of Community Health Nursing, Faculty of Nursing and Midwifery, Tabriz University of Medical sciences, Tabriz, Iran
Elham seyed Kanani
Social Determinants of Health Research Center, Department of Midwifery, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran
Mojgan Mirghafourvand
Medical Philosophy and History Reseach Center, Tabriz University of Medical Sciences, Tabriz, Iran
You can also search for this author in PubMed Google Scholar
Contributions
MM, SMA, MH contributed to the design of the study. SMA, ESK, MM has written the first draft of this article and MAJ Analyzed and data. All authors have critically read the text and contributed with inputs and revisions, and all authors read and approved the final manuscript.
Corresponding author
Correspondence to Mojgan Mirghafourvand .
Ethics declarations
Ethics approval and consent to participate.
The current study was approved by the Ethics Committee of Tabriz University of Medical Sciences [ref: IR.TBZMED.REC.1401.390]. Written Informed consent to participate in the study was obtained from all the participants before enrolment. Permission to use the BCPS was obtained by sending an email from the original designer of the instrument. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Mashayekh-Amiri, S., Jafarabadi, M.A., Hosseinzadeh, M. et al. Measurement properties of the Iranian version of the breast cancer perception scale (BCPS) according to the COSMIN checklist. BMC Cancer 24 , 743 (2024). https://doi.org/10.1186/s12885-024-12493-2
Download citation
Received : 16 July 2023
Accepted : 10 June 2024
Published : 18 June 2024
DOI : https://doi.org/10.1186/s12885-024-12493-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Psychometric
- Patient-reported outcome (PRO)
- COSMIN checklist
- Iranian validation
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
60 Effective PowerPoint Presentation Tips & Tricks (Giant List)
Here's a PowerPoint presentation tips and tricks guide that takes you through how to make a good PowerPoint presentation.

The best PowerPoint presentations shouldn’t be remembered. Instead, they should fall into the background to support you and the message you’re trying to get across.
Unlike good PowerPoint presentations , bad PowerPoint presentations are a distraction. You may remember them, but not in a good way.
You’ve seen them before. They might have millions of lines of text. Or a disjointed flow to the slides. Even worse, some slides feature ugly photos and poor design that detract from the message you’re trying to get across. That can even hurt your credibility as a professional or speaker.

This article will take you from finding your initial topic to learning how to make a great PowerPoint presentation. Our guide covers everything in between so that you learn how to present a PowerPoint like a pro.
These Microsoft PowerPoint presentation tips and guidelines are organized into sections. So cut straight to the advice you need and come back when you’re ready for the next steps.
Guide to Making Great Presentations (Free eBook Download)

Also, download our Free eBook: The Complete Guide to Making Great Presentations . It’s the deepest resource for learning effective presentation skills for a PPT.
This eBook covers the complete presentation process. It takes the PowerPoint tips and tricks you learn in this article further. Learn how to write your presentation, design it like a pro, and prepare it to present powerfully. It’s another great source for presentation design tips.
Master PowerPoint (Free Course): 15 Essential Tips
This article is full of helpful tips so you can build a powerful presentation. You can also find more PowerPoint tips in this video lesson:
To learn even more about how to make a PowerPoint look good, review the huge list of tips below.
What Makes a PowerPoint Presentation Effective?
Knowing how to use PowerPoint and work within it quickly is helpful. But more important is making a good presentation that hits all your goals. A great PowerPoint presentation is:
- Prepared to Win . Research, plan, and prepare your presentation professionally. It helps you deliver an effective message to your target audience.
- Designed Correctly . Your visual points should stand out without overwhelming your audience. A good PowerPoint visual shouldn’t complicate your message.
- Practiced to Perfection . Rehearse your timing and delivery so that your points land as practiced with a live audience.
- Delivered With Poise . Present with a relaxed inner calm and confident outward projection. Give your audience warmth, excitement, and energy.
- Free From Mistakes . Avoid typos, cheesy clip art, and mistakes like reading directly from your slides.
Consider this your all-inclusive guide to how to make a good presentation. We’ll look at preparing your presentation and explore how to design it in PowerPoint. Plus, we’ll cover how to practice and nail your delivery successfully come presentation time.
We’ll also address what not to do in these tips for PowerPoint presentations—so you can sidestep any big mistakes. Now let’s dig into these tips for effective PowerPoint presentations.
Killer Presentation Preparation Tips to Get Started Right
Before even opening PowerPoint, start by addressing these things. These Microsoft PowerPoint tips and tricks will ensure that you’re prepared for your presentation:
1. Know Your Stuff
Your presentation isn’t about your slides alone. It’s about the message you want to get across. Before filling in stats, facts and figures, think about the narrative that’ll be discussed, why, and in what order.
2. Write It Out
Start in a Word or Google doc, and storyboard or script the entire presentation. This will give you an idea of how the information presented will flow and how viewers will see it in sequence. Learn the complete writing process .
3. Highlight What’s Most Important
A presentation covers the most crucial pieces only. Whatever you’ve been working on that led to this—a paper, a work project, a new product design—doesn’t need to be shared in its entirety. Pick key points and put the rest in an “Appendix” to refer to during the Q&A session at the end.
4. Know Your Audience
How you talk to a room full of medical professionals should be different from the way you address a room full of young entrepreneurs. Everything, in fact, is different: your topic selection, the language you use, the examples you give to illustrate points. The little bits of humor you include should be tailored specifically with your target audience in mind.
Understand your audience’s needs to create a successful PowerPoint presentation. Customize your content to meet their specific requirements.
5. Rehearse! (Yes, Already)
It’s never too early to get used to the rhythm of your presentation and take note of points you want to emphasize. While saying it out loud, you’ll start to develop a “feel” for the material. You’ll notice that some things work well, while others don’t and might need to be worked around.
6. Rewrite After You Rehearse
As you’re rehearsing your presentation, you’re bound to stumble over sections that don’t quite flow naturally. Instead of reworking your delivery, it might be time to consider the content and rewrite the areas that served as stumbling blocks.
“Editing is hard. ‘It’s good enough,’ is a phrase wannabes use. Leaders take editing seriously.” – Anthony Trendl
The most important part of creating a great presentation is the writing stage. The second most important stage is rewriting.
7. Share With a Friend
If the stakes are high for your presentation, it’s never too early to get feedback from those that you trust. Here’s an article that helps you collaborate as a team on a PowerPoint presentation. Get PowerPoint design tips from those that you trust when you collaborate.
Simple Tips to Design Your PowerPoint Presentation Better
Second only to you (the information you bring and how you present it) is your PowerPoint slides. If not designed well, a PowerPoint can be disengaging or distracting (regardless of the content quality). Here are some presentation design tips to make sure this doesn’t happen to you:
8. Keep Your Slides Simple
This is one of the most important PowerPoint presentation tips to follow when designing your slides. Keep in mind that less is more (effective.) A cluttered slide is distracting. It causes confusion for an audience: Which part of the slide should I focus on? Should I read the slide or pay attention to the presenter?
A simple, visually appealing slide will engage your audience, keeping them on track with your main points. Here’s an example of a simple slide that serves its purpose perfectly:

Minimalist slide templates like Nook can help you resist the urge to clutter your slides.
9. Limit Words on Your Slides
Piggybacking on the last point, less is more effective. If possible, avoid bullets altogether. Otherwise cut them to just a few simple words. The audience should be listening, not reading.
10. Use High-Quality Photos and Graphics
One of the most important tips for quality PowerPoint presentations is to use high-quality photos and graphics.
Earlier in this tutorial, you saw Envato Elements, an all-you-can-download service with PPT tips inside of templates. Those pre-built designs are a beginner’s best friend. They’re even better when paired with Elements’ unlimited library of stock photos .
People are more likely to take you seriously if your presentation is visually appealing. Users view attractive design as more usable. Similarly, they’ll view a more attractive PowerPoint as more effective.
11. Use Accurate and Relevant Charts and Graphs
Charts and graphs can also be distracting if they’re not used right. Make sure your information design is simple and clean so that the audience doesn’t spend the entire time trying to decipher what your X axis says. Learn more about PPT data presentation .
12. Use High-Quality, Fresh Templates
Have you seen the old PowerPoint template that looks like worn paper and uses ink splashes? Yeah, so has your audience. Templates can be distracting if they’re too basic or if the design feels dated. You need one with great design options.
Costs are always a concern. But when you use Envato Elements, you’ve got everything you need to create a great PowerPoint presentation . That’s thanks to the incredible all-you-can-download subscription package.
The best PowerPoint tips and tricks can hardly compare to the value of using a template while building your presentation.
On Envato Elements, there are thousands of PowerPoint design templates that are ready to use. Instead of designing a presentation from scratch, start with a template! Just add your specifics to the placeholders.

Templates like Galaxi are impressively designed and waiting for your slide specifics.
The best PowerPoint design tips save you time. And there’s no tip more powerful than this one: use a pre-built template . It helps you master how to present a PowerPoint without spending all your time in the app.
13. Choose Appropriate Fonts
Fonts are an important part of engaging your audience. Fonts and typography choices have a subconscious effect on viewers. They can characterize your company’s presentation and brand either positively or negatively. Make sure that you’re choosing fonts that are professional and modern.
14. Choose Color Well
Like font choice, colors cause specific subconscious reactions from viewers. Choosing an outdated color combination for your presentation will render it ineffective.
Below is an example of the Popsicle PowerPoint template , which has a modern presentation color choice:

The Popsicle PowerPoint template highlights how harmonized color palettes can create beautiful slides.
15. Clean + Simple Formatting Makes All the Difference!
We’ve got a full tutorial on how to make a good presentation slide . Give it a read through and review the accompanying video. Just remember, less is more. The focus is you and your message , not your slides.
16. Make Sure All Objects Are Aligned
A simple way to create a well-designed presentation is to make sure all items on a slide are intentionally aligned. To do this, hold down Shift and select all the objects you want to include. Then choose Arrange in the options bar and apply Alignment Type .
17. Limit Punctuation
This isn’t the place for exclamation points. Emphasize your points (while speaking). Don’t enlist punctuation to do this for you. (Leave these at home!!!)
18. Avoid Over-Formatting Your Points
This PowerPoint presentation tip is simple. There’s no need to have every word of every bullet point capitalized, or to have all your bullet points in title case. If possible, drop bullets altogether. Again, the simpler, the better!
Limit your text formatting, including reducing the use of bullets, underline, and other effects. Compare the before example on the left to the revised version on the right.

19. Combine Information With Graphics in PowerPoint
One of the most powerful presentation skills for PPT is using infographics. With the right type of visuals, slides come to life and reduce the text in favor of graphics.
Infographics help combine information with graphics. It’s easier to explain complex ideas when you use visual formats that are intuitive.
Practice Presentation Tips: Rehearse, Rehearse, Rehearse!
Delivery is probably more important than the actual content. Here’s how to become more aware of your own unique ticks, and how to present like a polished pro:
20. I’ll Say It Again, Rehearse!
Just do it. Again and again. Experiment with pauses, gestures, and body language. Practice around one hour for every minute of your speech.
21. Practice With a Timer
Consistency is key to an effective PowerPoint presentation. The timing should be similar (ideally the same) each time you rehearse. This one will especially pay off when it’s time to present in front of your audience.
22. Slow It Down
Many of the best speakers today intentionally speak slowly. You’ll have the chance to emphasize, appear more thoughtful, and make your information easier to digest.
23. Pause More Often
Like the prior tip, pausing more often allows your main points to be emphasized and gives time for information to sink in. You need to let key points breathe a little before rushing into the next section.
24. Record Yourself
Use your phone’s voice recorder. Assess and critique yourself. Consider:
- Are your pauses too short or too long?
- Are you speaking slowly enough? Too slow?
- When you’re nervous, does your voice get high like the mice in Cinderella?

It’s always weird to hear your own voice recorded; don’t stress it. Use this as a time to adjust.
25. Choose Three Focal Points in the Room
If you stare at the same spot (or even creepier, the same person) the entire time, your presentation will be ineffective (and awkward.) People will be distracted by you, wondering what you’re staring at.
Try this: pick three points in the room (typically: left, center, right). Take time to direct your delivery toward each physical focal point in the room. Also, focus on the center when making your primary points.
26. Vary Your Sentence Length
This makes you sound more interesting, and it’s easier for your audience to follow. Think short and punchy. Or go long and complex for dramatic effect.
27. Modulate!
Don’t speak in monotone for your whole presentation. Be conscious of raising and lowering your voice tone. Otherwise, people will tune you out, and you’ll come across like the teacher in Charlie Brown.
28. Practice in Front of a Mirror
What you look like is as important as how you sound. Pretend you’re having a normal conversation, and allow your hands to move with your speech to emphasize your points. Just don’t get carried away! (I’m thinking Brene Brown or President Obama , not your Aunt Jamie after a few gin and tonics.)
29. Use “Present Mode” When Rehearsing
When you finally are ready to hit the Present button in PowerPoint, make sure you use the Present Mode option. This allows you (and only you) to view extra notes about each slide—just in case you forget something!
30. Practice With New Audiences
If possible, try doing a few real live test runs as a webinar or even at a local Toastmasters organization to get some feedback from a live audience.
31. Engage the Audience by Asking Questions
There’s no reason that a presentation should be one-sided. Why not invert the format and ask your audience a question?
To learn how to create a slide that kicks off a Q&A, use this article . These PowerPoint design tips help you create an engaging and exciting discussion.
Helpful Tips to Step Up and Deliver Come Presentation Time
When the actual day arrives, there are only a few last PowerPoint presentation tips and guidelines to keep in mind:
32. Take a Deep Breath
Deep breathing is proven to relieve stress. It’s simple, and it’ll help you remain calm and in the moment, even up to the last minute before starting.
33. Lighten Up Your Mood
Tell yourself a joke or watch a funny video clip. Do this before the presentation, of course. Research concludes that happy people are more productive. More productive is more focused and able to perform better.
34. Remind Yourself to Take It Slow
When we’re stressed or nervous (or both), we tend to speak faster. Consciously, take yet another deep breath and remind yourself to take it slow!
35. Read the Room
Every presentation room has a temperature. It’s your job as a speaker to gauge it and tailor your presentation to it.
Here’s a great example. Layoffs are coming at a company, and you’re asked to speak to an audience. Even if the audience isn’t personally affected by the actions, you’ve got to consider the morale of the workforce.

Skilled speakers have a knack for reading the energy of the room and adjusting their presentation on the fly.
The last thing that group will want to hear is how strong the economy is and why the company is the best place to work. That doesn’t mean that you’ve got to align to their uncertainty, but don’t go too far against the grain while presenting.
Robert Kennedy III is a master of bringing energy and aligning a speech to the audience. Here’s his advice for adjusting:
“It can be hard to wake up a “dead” crowd but go for it. Most of all, don’t take their energy personally. Focus on serving them with every bit of your fiber then leave empty.”
36. Fake It ‘Til You Make It!
Go forward with confidence. If you act confident, you’ll start to feel more confident. Move slowly with grace, speak clearly, smile, wear something nice. You’ll appear confident to all attendees (no matter how you feel internally).
PowerPoint Presentation Tips and Tricks to Help Avoid Mistakes (What Not to Do)
Most importantly, focus on what you can do to make your presentation better. There are a few important things not to do that we’ve got to address. Here are a handful of PowerPoint presentation tips and tricks to help you avoid missteps.
37. Stop With the Sound Effects
Sound effects are distracting and outdated. In most cases, avoid them. Add audio or music to your presentation to inject interest or highlight an important point, but it’s something to take extra care with. If you insert audio, then make sure your use really connects with your audience and has a fresh approach. Otherwise, it’s best to leave it out.
38. Don’t Use Flashy Slide Transitions
Again, this is distracting and outdated. Use transitions and subtle animations in your PowerPoint presentation. But you need to take care and do it right .
39. Beware of Clip Art
This PowerPoint presentation tip shouldn’t even have to be said. But please, please don’t use clip art. Use professional graphics instead.
40. Don’t Be Afraid to Be Afraid
The fear of public speaking is a real one. Many beginners think that if they’re feeling nervous that a presentation won’t go well or succeed. That might lead them to cancel the presentation.
Here’s a tip from expert Sandra Zimmer, who leads The Self-Expression Center on conquering your fears before you take the stage:
“Get out of your head and into your body. I do this through a grounding exercise that really works to calm nerves and bring you present in the moment.”
If you think that public speaking fears aren’t normal, you might never give your award-winning presentation. So don’t be afraid to be afraid, and acknowledge it’s part of the process!
41. Don’t Read Directly During Your PowerPoint Presentation
If you spend your entire presentation looking at the screen or your note cards, you’re sure to lose your audience’s attention. They’ll disengage from what you’re saying, and your presentation will fall flat.
Reading from your paper or screen also makes it look like you’re not prepared. Many people do it, but no one should. As a general rule, only present something you know well and have, at least mostly, memorized the main points of.
42. Don’t Miss Out on PowerPoint Customizations
Many new PowerPoint users often make significant mistakes when using Envato Elements designs.
The best way to see how to make a good presentation PPT is to start with designs from others. That means using a template, but that doesn’t mean you can’t customize them!

Don’t forget that PowerPoint templates are infinitely customizable. Think of them as guides with built-in presentation design tips.
To see more presentation tips that show you what not to do, make sure to check out our guide .
Work in PowerPoint More Effectively (Tips & Tricks to Level Up Your PPT Skills)
These PowerPoint tips will help you get the most out of the application to level up your next presentation. Let’s dive in.
43. Use the Visual Guides
When you’re designing your next PowerPoint presentation, it helps to create a sense of visual rhythm. Slides that have objects aligned and centered are more likely to resonate with an audience.
44. Use a Few Animations (Tastefully)
Animations in effective PowerPoint presentations are a slippery slope. We’ve all sat through presentations where there were so many objects in motion that it was easy to lose focus on the key ideas in the presentation.
But that’s why animations get an unfairly bad reputation. Use animations to create motion and hold an audience’s attention. Use them sparingly and on key elements on your slide, and you’ll capture that attention properly.
45. Stage Key Content With Animations
You just learned that animations should avoid being distracting. But there’s an important principle to using animations properly. It’s called staging content.
Staging content means that the content appears step by step. There’s nothing worse than overwhelming an audience with all your content at once. But when you stage content, bring it on step by step.
Take it from presentation pro Suzannah Baum :
“If you’re sharing a slide with lots of different points on it, using the animation to reveal those points one at a time is a way to keep the presenter’s content flowing smoothly.”
For more animation presentation tips and tricks, follow our guide .
46. Add a Video to Your PowerPoint
When you’re sharing a big idea in your presentation, it helps to share your perspective from a few different angles. Adding a video to supplement your content can do just that. Luckily, it’s easy to add and embed a YouTube video in your next PowerPoint presentation.
47. Add Charts & Graphs
Charts and graphs can help you tell stories with data. It’s easy for an audience to zone out when you throw a big data table or set of statistics at them.
instead, convert those to charts and graphs. Try out our tutorial to learn how to edit those graphs.
48. Build Your Own Infographics With SmartArt
Earlier in this tutorial, we gave you one of my favorite PowerPoint design tips: use infographic templates.
Here’s another. One of my favorite PowerPoint features is SmartArt, which allows you to build infographics right inside the app.
You don’t have to use another graphic design app like Photoshop or Illustrator to add visuals. Instead, try out SmartArt to help you build graphics that are easy to update.
49. Use Presenter View
Remember that when you use the PowerPoint, you’ re the presentation. The slides are just there to reinforce what you’ve got to say and support your speaking points.
That’s why I always recommend using Presenter view. More often than not, you’re going to have several displays. Presenter view shows your content on your screen, while your presentation is displayed on another screen.
50. Track Your PowerPoint Changes
One of my favorite PowerPoint design tips is to collaborate. Those who know you best will suggest compelling changes that are sure to help you succeed.
As you start collaborating on your presentation, it helps to keep track of proposed and included PowerPoint changes. Use this article to track changes made by others.
10 More Advanced PowerPoint Tips & Tricks
Really need to wow an audience with a good PowerPoint presentation? Give these tips a try to make an unforgettable impression:
51. Engage With an Interactive Quiz
A good PowerPoint presentation gets your audience involved. One of the best PowerPoint tricks is to do that with a quiz. By engaging audiences, a quiz makes your slides memorable.

By adding trivia, you’ll see how to present a PowerPoint in a way that people will love. Channel your inner game-show host today. MIDTEST is a good PowerPoint presentation with quiz slides.
52. Illustrate With Custom Image Masks
One of the top PowerPoint tips is to illustrate your slides. But you can go beyond simple, rectangular images on each slide.

The Burte template is full of PowerPoint tricks , including custom image masks. Image masks shape photos into unique works of art. And thanks to premium templates, you can style photos just like this. Masks overlay your photos onto geometric shapes, instantly elevating your style.
53. Print Handouts With Extra Notes
Wonder how to give a good presentation PPT that audiences will remember? Give them a piece of it to take home.
PowerPoint makes it easy to print handouts with room for notes on the page. This way, audiences can keep copies of your slides, along with their own notes. This is the perfect way to ensure everyone engages with and retains your content.
54. Make Bulk Edits With Master Slides
When you think about how to present a PowerPoint, consider your branding. That means keeping your logo front and center in the eyes of an audience. But if you’re working with a lengthy slide deck, this could seem daunting.
That’s where master slides come in. They’re common in premium layouts, and they’re a leading example of presentation skills for PPT. Master slides let you make bulk edits fast.
55. Shrink File Sizes for Sharing
Many of the top presentation tips involve making your slides more accessible. Often, that involves sharing them with audiences online.
You’ll often find that email clients and cloud services limit the size of files that you share. This can be a problem with large PPT slide decks. But there are a few quick steps you can take to reduce PPT file size. Cut graphics, scale down photos, and more.
56. Map Processes With Flowcharts
As you consider how to do a good PowerPoint presentation, think of ease of understanding. After all, you’re trying to explain something to your audience.

The Flowcharts in Infographics template seamlessly illustrates ideas and processes. A flowchart maps out a process in a visual way. Instead of resorting to endless narration, try a quick illustration like this. It saves you time and effort, and your audience is sure to thank you.
57. Use Brand-Specific Colors
Using presentation skills for PPT helps form an association between your message and branding. There’s no better way to do that than with your brand colors.
PowerPoint makes it easy to change color themes, adding your brand colors and logo to each slide. This is one of the top PowerPoint tricks for marketing presentations.
58. Build Social Media Posts in PPT
A good PowerPoint presentation doesn’t have to be shared through a projector. Use the app and templates to build amazing illustrations to use anywhere.

A template like Soffee helps you learn how to present a PowerPoint easily with a pre-built design.
Try using PowerPoint to create social media posts. It helps you engage with your audience, with no need to design custom layouts from scratch.
59. Be Industry-Specific
One of the top presentation tips in 2024 is to be industry-specific. That means avoiding generic layouts and choosing something more customized.
This offers two key advantages. First, you save time by having layouts built for you. Second, you gain design inspiration for your specific topic. Themed templates are truly the best of both worlds.

The Medical and Health template is a good PowerPoint presentation with a set theme.
60. Design for Online (Virtual) Sharing
Last but not least in our list of PowerPoint tips comes virtual presenting. More and more often, slides will be shared with online audiences around the globe.
Why not design your slides for that very purpose? And then learn how to share flawlessly with a global team? It’s one of the top presentation tips for 2024. Embrace it today.
More Great PowerPoint Tutorial Resources
We’ve built a resource for Microsoft PowerPoint that you’re sure to want to try. It includes countless PowerPoint tips and tricks. It’s called How to Use PowerPoint (Ultimate Tutorial Guide) and has all the PowerPoint design tips you need.
Discover More Top PowerPoint Template Designs From Envato Elements for 2024
You’ve just seen our favorite powerful PowerPoint presentation tips and guidelines to help you improve your speaking. We’ve also mentioned Envato Elements, an incredible all-you-can-download source for top PowerPoint designs .
Here are five of the best PowerPoint templates that you can use to create your best presentation yet:
1. Galaxi PowerPoint Template
Blast off to success with the help of this PowerPoint template! Think of the pre-built slide designs as pro PowerPoint design tips. They’re built by professional graphic designers. All the popular and modern slide styles that are perfect for your next presentation. Use Galaxi’s five styles and 30 designs to create a great presentation.
2. Masmax PowerPoint Template

We selected templates for this article that match the PowerPoint tips and tricks provided. Masmax fits the bill perfectly across its 234 unique slide designs. These slide designs are sure to align with the latest in design expectations.
3. STYLE Multipurpose PowerPoint Template V50

Style is subjective, but we can all agree that this template is stunning! The light and airy slide designs are built with fashion-focused designs in mind. But that doesn’t mean that it’s not perfect for most presentations. When learning to present a PowerPoint, remember that templates can be customized to suit your purpose.
4. Peachme Creative PowerPoint Template

Peachme has image-focused slides with splashy designs. The slides are colorful and perfect for a modern presentation. Don’t worry about remembering all the PowerPoint design tips because they’re included in the pre-built slides. Use Peachme’s designs for your presentation today.
5. Buizi Office Building Rent PowerPoint Template

Buizi markets itself as a real estate focused template. It’s ideal for that purpose because of the minimal, image-focused slide designs. But that also makes it a perfect choice for presentations in many fields.
We’ve just scratched the surface of PowerPoint design tips with these five options. Here are many more, bundled inside of the best roundups on Envato Tuts+:
How to Build a Good PowerPoint Presentation Quickly (In 2024)
You’ve already seen effective presentation skills PPT techniques. But you may be wondering exactly how to do a good PowerPoint presentation. It only takes a few clicks. Let’s learn how in just five steps.
For this mini-tutorial, we’ll use the Enjoy PowerPoint Template from Envato Elements. You’ll see that it’s a beautiful template that helps you learn how to present a PowerPoint by giving you every object and layout you need.

Let’s get started:
1. Choose Your Slides
As you can see, a template like Enjoy has dozens of unique slides inside. The key to how to give a good presentation PPT is to choose only the slides that you need.

One of the best PowerPoint tricks is to start by selecting slides you wish to use from your template.
In PowerPoint, scroll through the sidebar on the left to view different slide layouts. Right-click and choose Delete to remove unwanted designs. Plus, you can click and drag slide thumbnails to reorder them in the deck.
2. Add Text
Consider how to do a good PowerPoint presentation without investing a ton of time. That’s where premium templates come in.

One of our top presentation tips when working with a PPT is to lean on the pre-built text boxes for your content.
To add custom text, simply click and select the contents of any text box on your slide. Then, type in your own words. Repeat as needed throughout your slide deck.
3. Customize Fonts
With text selected, it’s easy to customize fonts on each slide. Find the Font section on PowerPoint’s Home tab. From there, you’ve got a variety of dropdown options.

Another of our top tips for presentation tricks is to use a custom font setting in your template.
Click to change the font, font size, and more. You can also use the buttons on the left to add bolds, italics, and more.
Need more custom font styles? As an Envato Elements subscriber, you’ve got instant access to thousands of custom fonts . Use them in your presentation with ease.
4. Insert Images
Slides like this one contain an image placeholder. That’s another advantage found only with premium templates. These make adding images a breeze.

Add images to your PPTX template for more visually interesting slides.
To get started, find an image file stored on your computer. Then, drag and drop it over the placeholder. PowerPoint will import it, sized and scaled for a perfect fit.
5. Change Colors
One of the top effective presentation skills is changing shape colors. This helps you control the look and feel of each slide.

With a shape selected, find the Shape Format tab on PowerPoint’s ribbon. Then, click on the Shape Fill dropdown. You’ll see a color chooser menu appear. Click on any thumbnail to apply it to the shape or browse through the Gradient and Texture options.
Start Putting These PowerPoint Presentation Tips & Tricks Into Use Today!
Learning to write, design, and present a PowerPoint presentation is an invaluable skill, no matter where you use it. If you’re a good communicator of important messages, you’ll never go hungry.
Luckily, improving PowerPoint presentations isn’t as hard as it seems. Follow these tips for PowerPoint presentations to design and deliver with greater confidence.
Remember: Less is more (effective) . Use PowerPoint presentation templates for better design and more effective visual impact. And you can customize a PPT template quickly , with the right workflow.
Related Articles

Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

education technology
239 templates
computer technology
306 templates

ai technology
186 templates

cyber security
10 templates

meet the teacher
30 templates

first day of school
70 templates
Breast Cancer Infographics
It seems that you like this template, free google slides theme, powerpoint template, and canva presentation template.
Allow us to help you spread useful information about breast cancer, its symptoms, treatment and more. Download this template and edit any of the designs included so that you have the data represented with images and other visual resources, which is always a good addition if you really want your audience to pay attention to what you're showing.
Features of these infographics
- 100% editable and easy to modify
- 30 different infographics to boost your presentations
- Include icons and Flaticon’s extension for further customization
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint and Keynote
- 16:9 widescreen format suitable for all types of screens
- Include information about how to edit and customize your infographics
How can I use the infographics?
Am I free to use the templates?
How to attribute the infographics?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access


Oncology's largest annual meeting brings 40,000 to Chicago to discuss cancer advances

The 60th Annual Meeting of the American Society of Clinical Oncology 2024 (ASCO 2024) became the venue for global oncology professionals to discuss groundbreaking scientific discoveries and practice-changing novel therapies that are poised to change the landscape of cancer care. More than 40,000 oncology professionals convened at McCormick Place in Chicago from May 31 to June 4.
The ASCO 2024 Annual Meeting Program featured more than 200 sessions complementing the President’s theme, “The Art and Science of Cancer Care: From Comfort to Cure.” The University of Chicago Medicine Comprehensive Cancer Center (UCCCC) faculty and trainees presented the latest clinical research data and discussed groundbreaking research in various education sessions, clinical science symposia, oral abstract sessions, case report panels, publications and posters.
Honors and awards
Two faculty members from the UCCCC, Fay J. Hlubocky, PhD, MA, and Mitchell C. Posner, MD , were recognized as new Fellows of the ASCO organization. This distinction recognizes members for their extraordinary volunteer service, engagement, dedication and commitment to ASCO.
Additionally, Siddhi Ramesh, a resident at the University of Chicago Pritzker School of Medicine, received an ASCO Annual Meeting Merit Award for recognition of research in high-quality abstracts submitted to an ASCO Meeting.
UCCCC highlights at ASCO 2024
Everett Vokes, MD , John E. Ultmann Distinguished Service Professor and Chair of Medicine, introduced and presented the 2024 Science of Oncology Award to Jennifer A. Pietenpol, PhD, of Vanderbilt University Medical Center in recognition of her groundbreaking discoveries in triple-negative breast cancer and the p53 family-signaling network.
Alexander Pearson, MD, PhD , Associate Professor, Department of Medicine, discussed two abstracts in a clinical science symposium session titled, " Using 'Artificial' Intelligence to Achieve 'Real' Improvements in Cancer Care. " Both abstracts were on analyzing the existing clinical and imaging data using multi-modal AI models to estimate distant metastasis in HR+ HER2- breast cancer and to estimate immunotherapy response in advanced non-small cell lung cancer. In an oral presentation session, Pearson presented data from PATHWay study – a multi-site, randomized, placebo-controlled trial testing neoadjuvant pembrolizumab in high-risk head and neck squamous cell cancer (HNSCC) patients.
Ari Rosenberg, MD , Assistant Professor of Medicine, presented the updated results demonstrating the safety profile of HB-200, arenavirus-based immunotherapy in combination with pembrolizumab in recurrent/metastatic HPV16+, PD-L1+ HNSCC patients. In an educational session, Rosenberg reviewed the data of novel therapies such as antibody-drug conjugates, bispecific antibodies, fusion proteins, and multikinase inhibitors that were tested in the management of metastatic head and neck squamous cell carcinoma.
Evgeny G Izumchenko, PhD , Assistant Professor of Medicine, presented a poster on developing saliva-based, non-invasive diagnostic tests for HPV-positive oropharyngeal cancers.
Fred Howard, MD , Assistant Professor of Medicine, presented a poster demonstrating the increased use of artificial intelligence tools like ChatGPT to generate oncology scientific abstracts from 2021 -2023. This high impact work was simultaneously published in the ASCO journal, JCO Clinical Cancer Informatics .
Ardaman Shergill, MD , Assistant Professor of Medicine, presented results from an ongoing clinical trial evaluating the combination of FOLFOX6 and binimetinib that improve overall survival of patients with advanced biliary tract cancer with MAPK mutations in comparison with FOLFOX6 alone in second-line therapy. She also chaired a clinical symposium session on circulating biomarkers where clinical studies discussed circulating tumor cells and tumor DNA as diagnostic and prognostic markers for various cancers.
Justin Kline, MD, Professor of Medicine, chaired an oral presentation session, “Hematologic Malignancies—Lymphoma and Chronic Lymphocytic Leukemia.” In the same session, Peter Riedell, MD , Associate Professor of Medicine, discussed three abstracts focused on current treatment approaches in Diffuse Large B-Cell Lymphoma. Riedell also presented a poster with updated results from EV-103 study evaluating neoadjuvant enfortumab vedotin monotherapy in muscle-invasive bladder cancer patients who were ineligible for cisplatin therapy.
In a rapid oral abstract session, Marina Chiara Garassino, MD , Professor of Medicine, presented updated results from KEYNOTE-671 study with data supporting the perioperative pembrolizumab as a new standard of care for early-stage non-small-cell lung cancer (NSCLC).
In an oral abstract session, Ami V Desai, MD, MSCE , Associate Professor of Pediatrics, presented the results of a feasibility study testing chemoimmunotherapy after autologous stem cell transplantation in newly diagnosed high-risk neuroblastoma patients. In another session, she joined two panelists on a case-based panel of “Transplant in Neuroblastoma: When Do We Go Off-Script?” The panelists discussed how response to induction therapy is defined for patients with high-risk neuroblastoma. The panel suggested the appropriate timing of transplant based on data for bridging therapy in North America.
John W. Moroney, MD , Associate Professor of Obstetrics and Gynecology, reviewed four abstracts in a “Highlights of the Day” session.
In a clinical science symposium session, Ben Derman, MD , presented results from a prospective study “MRD2STOP” demonstrating lack of disease progression in multiple myeloma (MM) patients after discontinuation of maintenance therapy with a high rate of sustained MRD-negativity, suggesting MRD negativity as a potential biomarker in MM.
Jessica Donington, MD, MSCR , Professor of Surgery, discussed three abstracts in an oral abstract session, “Lung Cancer—Non–Small Cell Local-Regional/Small Cell/ Other Thoracic Cancers.” It highlighted the need for broader inclusion criteria and improved screening infrastructure for lung cancer screening and peri-adjuvant “sandwich” immunotherapy for locally advanced non-small-cell lung cancer.
Tara Henderson, MD, MPH , Arthur and Marian Edelstein Professor of Pediatrics, and Director of the Childhood, Adolescent and Young Adult Survivorship Center, presented results from the ENGAGE Study: Childhood Cancer Survivor Study (U24 CA55727) Ancillary Study, highlighting the potential barriers that are associated with lower rates of genetic counseling/testing in the cancer survivor community.
Daniel Olson, MD , Assistant Professor of Medicine, discussed three abstracts in an oral abstract session, “Developmental Therapeutics—Immunotherapy,” stressing the need for the development of novel, engineered cell therapies beyond antigen targeting to enhance safety and efficacy of emerging cell therapies.
In total, our faculty and trainees participated in more than 50 oral, rapid oral, poster and educational sessions. A full list of presentations at ASCO 2024 can be found here .
The next ASCO Annual Meeting will take place in Chicago May 30 - June 3, 2025.

UChicago Medicine Comprehensive Cancer Center
UChicago Medicine is designated as a Comprehensive Cancer Center by the National Cancer Institute, the most prestigious recognition possible for a cancer institution. We have more than 200 physicians and scientists dedicated to defeating cancer.

IMAGES
VIDEO
COMMENTS
Case study breast cancer. Jan 28, 2013 • Download as PPTX, PDF •. 75 likes • 95,337 views. AI-enhanced description. Nilesh Kucha. This case study describes a 37-year-old female patient who presented with a breast mass. Diagnostic tests performed included a mammogram, biopsy, and right modified radical mastectomy which revealed invasive ...
This case study summarizes a 38-year old female patient presenting with breast pain, nipple tenderness, and bloody discharge. Her medical history includes a diagnosis of tennis elbow. Laboratory tests and cytology reports were conducted. She was diagnosed with breast cancer and prescribed a treatment plan including Aceclofenac, Pantoprazole ...
Breast cancer ppt. Breast cancer is the second leading cause of death and second most common cancer in women. It occurs when abnormal cells in the breast grow in an uncontrolled way and form tumors. The breasts contain lobes and lobules which produce milk, connected by ducts. The two main types are ductal carcinoma, originating in the ducts ...
The typeface that you'll find in body text, on the other hand, is a sans-serif one, and has semi-rounded details. Start customizing this template in Google Slides or PowerPoint and share what you have to say about a breast cancer clinical case. Features of this template. A clinical case presentation with pink colors and health-related fill icons
Increasing Mortality in Korean Patients With Breast Cancer: High Mortality Rate in Elderly Breast Cancer Population Due to Suboptimal Treatment and Other Diseases, Cancer Control, 28 ...
Breast Cancer Case Presentations 11/11/2021. Patient Case 1: Early Stage Her2neu+ disease •55 yo post menopausal female presented after self palpating a right breast mass •FH: maternal aunt breast cancer •Gyn Hx: menarche 13, G2P2 first live birth at 30, breastfed, menopause at ... PowerPoint Presentation
History. Many early breast cancers are asymptomatic, particularly if they were discovered during a breast-screening program. Larger tumors may present as a painless mass. Pain or discomfort is not usually a symptom of breast cancer; only 5% of patients with a malignant mass present with breast pain. Often, the purpose of the history is not ...
8 Breast Cancer case study - Part I. Mollie Jenkins a 45-year-old lady has been admitted to the surgical ward for a left breast lumpectomy and removal of axillary glands. She discovered a lump in her breast about a month ago and was referred to the breast clinic.
Patient Case Presentation. Patient Mrs. B.C. is a 56 year old female who is presenting to her WHNP for her annual exam. She had to cancel her appointment two months ago and didn't reschedule until now. Her last pap smear and mammogram were normal. Today, while performing her breast exam, her nurse practitioner notices dimpling in the left ...
Discover our Pink Geometric Illustrated Breast Cancer Case Presentation. A creative, retro marketing tool perfect for catalogues, posters, and social media. Fully customizable and 100% free to use. ... it's a fresh and creative alternative for Powerpoint and Google Slides presentations. Use it for crafting intricate marketing proposals ...
960 likes | 5.23k Views. BREAST CANCER CASE STUDY. FRAZER BELL STUDENT BMS BSc APPLIED BIOMEDICAL SCIENCE. PATIENT HISTORY. 70 YEAR OLD FEMALE PRESENTED AT GP SURGERY 02/OCT/2012 EXAMINATION: RIGHT NIPPLE DRAWING IN & FIRM PALPABLE LUMP REFERRED TO THE BREAST CLINIC. BREAST CLINIC.
Download your presentation as a PowerPoint template or use it online as a Google Slides theme. 100% free, no registration or download limits. Use these breast cancer templates to create informative presentations that spread awareness and inspire hope. No Download Limits Free for Any Use No Signups.
Fibroadenoma (37%) and fibroadenosis (23%) were the commonest diseases,both presenting mostly at 21-30years of age. Left side involvement was most common. The commonest presentation was breast lump which comprised 84 (84%) cases, out of which 26 (26%) had associated complaints like breast pain and nipple discharge.
Download the Female Reproductive System Case Report: Breast Cancer presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there's a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it's great news ...
Presentation Transcript. Case Study 63: Cancer of the Female Breast By Robyn Schwartz. Case Background • 46, premenopausal • Dense breasts • Has noticed cysts in the past • Noticed new lump in upper right quadrant • Did not resolve • Got bigger • Denied lumps in axillary. Patient history • Happily married for 21 years • 3 kids ...
A. ahmedalgzali1. This case study describes a 72-year-old retired female teacher who presented with a lump in her right breast and was diagnosed with invasive lobular carcinoma. She had a previous history of left breast cancer in 1986 and family history of various cancers. She underwent lumpectomy of the right breast followed by 16 fractions of ...
2. Click on the button below the presentation features that says 'Download Breast Cancer Case as a Free PowerPoint template'. 3. Once done it will start downloading a .pptx file that you can edit in PowerPoint. 4. If we do not have the powerpoint file we will direct you to the original source so you can download it. 5.
For example, machines help with surgeries that require lots of precision. That is the case with breast surgery to treat cancer, robots have been helping doctors for a couple years, and the results are astonishing! Speak about a clinical case that shows the benefits of these techniques with this creative template for health proffesionals.
Create Awareness Using This Template: Present your details about breast cancer and create awareness among your audience and to your desired people. You can find the four nodes which are inserted in this template that are colorful and informative with the captions and the node space. The diagram which is presented in the center looks highlighted ...
What is Breast Cancer.Ppt - Free download as Powerpoint Presentation (.ppt / .pps), PDF File (.pdf), Text File (.txt) or view presentation slides online. Breast cancer begins in the breast tissue and may start in the ducts or lobes. It occurs when breast cells divide uncontrollably and form a lump or tumor. Most breast lumps are benign, but some are cancerous.
Here at ASCO, they presented some updated adverse events as well as PFS2. The efficacy data continue to look compelling. What is really surprising is the relative lack of grade 3 events when you ...
Breast Cancer. Breast cancer starts in the cells of the breast and can spread to other parts of the body. There are several types of breast cancer including ductal carcinoma in situ, invasive ductal carcinoma, inflammatory breast cancer, and metastatic breast cancer. Risk factors include being a woman, aging, family history and genetic factors ...
Background Women with dense breasts benefit from supplemental cancer screening with US, but US has low specificity. Purpose To evaluate the performance of breast US tomography (UST) combined with full-field digital mammography (FFDM) compared with FFDM alone for breast cancer screening in women with dense breasts. Materials and Methods This retrospective multireader multicase study included ...
That is why the World Health Organization itself established the month of October as the month of awareness about breast cancer to raise awareness about this disease, to get more support for women who suffer from it and more funds for early detection. In Slidesgo we join the cause and we have designed this template for you to talk about breast ...
Breast cancer is a prevalent cancer characterized by its aggressive nature and potential to cause mortality among women. The rising mortality rates and women's inadequate perception of the disease's severity in developing countries highlight the importance of screening using conventional methods and reliable scales. Since the validity and reliability of the breast cancer perception scale ...
A great PowerPoint presentation is: Prepared to Win. Research, plan, and prepare your presentation professionally. It helps you deliver an effective message to your target audience. Designed Correctly. Your visual points should stand out without overwhelming your audience. A good PowerPoint visual shouldn't complicate your message.
Free Google Slides theme, PowerPoint template, and Canva presentation template. Allow us to help you spread useful information about breast cancer, its symptoms, treatment and more. Download this template and edit any of the designs included so that you have the data represented with images and other visual resources, which is always a good ...
" Both abstracts were on analyzing the existing clinical and imaging data using multi-modal AI models to estimate distant metastasis in HR+ HER2- breast cancer and to estimate immunotherapy response in advanced non-small cell lung cancer. In an oral presentation session, Pearson presented data from PATHWay study - a multi-site, randomized ...
However, currently, female breast cancer superseded lung cancer worldwide. Female breast cancer is reported to have a high incidence among all cancers, with 2.3 million newly diagnosed cases becoming the most reported malignancy. By the very end of this decade, breast cancer will become the most prevalent cancer worldwide . In 2020 ...