- Research article
- Open access
- Published: 24 April 2019

Priorities and challenges for health leadership and workforce management globally: a rapid review
- Carah Alyssa Figueroa ORCID: orcid.org/0000-0002-8825-7796 1 ,
- Reema Harrison 1 ,
- Ashfaq Chauhan 1 &
- Lois Meyer 1
BMC Health Services Research volume 19 , Article number: 239 ( 2019 ) Cite this article
208k Accesses
23 Altmetric
Metrics details
Health systems are complex and continually changing across a variety of contexts and health service levels. The capacities needed by health managers and leaders to respond to current and emerging issues are not yet well understood. Studies to date have been country-specific and have not integrated different international and multi-level insights. This review examines the current and emerging challenges for health leadership and workforce management in diverse contexts and health systems at three structural levels, from the overarching macro (international, national) context to the meso context of organisations through to the micro context of individual healthcare managers.
A rapid review of evidence was undertaken using a systematic search of a selected segment of the diverse literature related to health leadership and management. A range of text words, synonyms and subject headings were developed for the major concepts of global health, health service management and health leadership. An explorative review of three electronic databases (MEDLINE®, Pubmed and Scopus) was undertaken to identify the key publication outlets for relevant content between January 2010 to July 2018. A search strategy was then applied to the key journals identified, in addition to hand searching the journals and reference list of relevant papers identified. Inclusion criteria were independently applied to potentially relevant articles by three reviewers. Data were subject to a narrative synthesis to highlight key concepts identified.
Sixty-three articles were included. A set of consistent challenges and emerging trends within healthcare sectors internationally for health leadership and management were represented at the three structural levels. At the macro level these included societal, demographic, historical and cultural factors; at the meso level, human resource management challenges, changing structures and performance measures and intensified management; and at the micro level shifting roles and expectations in the workplace for health care managers.
Contemporary challenges and emerging needs of the global health management workforce orient around efficiency-saving, change and human resource management. The role of health managers is evolving and expanding to meet these new priorities. Ensuring contemporary health leaders and managers have the capabilities to respond to the current landscape is critical.
Peer Review reports
Health systems are increasingly complex; encompassing the provision of public and private health services, primary healthcare, acute, chronic and aged care, in a variety of contexts. Health systems are continually evolving to adapt to epidemiological, demographic and societal shifts. Emerging technologies and political, economic, social, and environmental realities create a complex agenda for global health [ 1 ]. In response, there has been increased recognition of the role of non-state actors to manage population needs and drive innovation. The concept of ‘collaborative governance,’ in which non-health actors and health actors work together, has come to underpin health systems and service delivery internationally [ 1 ] in order to meet changing expectations and new priorities. Seeking the achievement of universal health coverage (UHC) and the Sustainable Development Goals (SDGs), particularly in low- and middle-income countries, have been pivotal driving forces [ 2 ]. Agendas for change have been encapsulated in reforms intended to improve the efficiency, equity of access, and the quality of public services more broadly [ 1 , 3 ].
The profound shortage of human resources for health to address current and emerging population health needs across the globe was identified in the World Health Organization (WHO) landmark publication ‘Working together for health’ and continues to impede progress towards the SDGs [ 4 ]. Despite some improvements overall in health workforce aggregates globally, the human resources for health challenges confronting health systems are highly complex and varied. These include not only numerical workforce shortages but imbalances in skill mix, geographical maldistribution, difficulty in inter-professional collaboration, inefficient use of resources, and burnout [ 2 , 5 , 6 ]. Effective health leadership and workforce management is therefore critical to addressing the needs of human resources within health systems and strengthening capacities at regional and global levels [ 4 , 6 , 7 , 8 ].
While there is no standard definition, health leadership is centred on the ability to identify priorities, provide strategic direction to multiple actors within the health system, and create commitment across the health sector to address those priorities for improved health services [ 7 , 8 ]. Effective management is required to facilitate change and achieve results through ensuring the efficient mobilisation and utilisation of the health workforce and other resources [ 8 ]. As contemporary health systems operate through networks within which are ranging levels of responsibilities, they require cooperation and coordination through effective health leadership and workforce management to provide high quality care that is effective, efficient, accessible, patient-centred, equitable, and safe [ 9 ]. In this regard, health leadership and workforce management are interlinked and play critical roles in health services management [ 7 , 8 ].
Along with health systems, the role of leaders and managers in health is evolving. Strategic management that is responsive to political, technological, societal and economic change is essential for health system strengthening [ 10 ]. Despite the pivotal role of health service management in the health sector, the priorities for health service management in the global health context are not well understood. This rapid review was conducted to identify the current challenges and priorities for health leadership and workforce management globally.
This review utilised a rapid evidence assessment (REA) methodology structured using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [ 11 ]. An REA uses the same methods and principles as a systematic review but makes concessions to the breadth or depth of the process to address key issues about the topic under investigation [ 12 , 13 , 14 ]. An REA provides a balanced assessment of what is already known about an issue, and the strength of evidence. The narrower research focus, relative to full systematic reviews, make REAs helpful for systematically exploring the evidence around a particular issue when there is a broad evidence base to explore [ 14 ]. In the present review, the search was limited to contemporary literature (post 2010) selected from leading health service management and global health journals identified from exploring major electronic databases.
Search strategy
An explorative review of three core databases in the area of public health and health services (MEDLINE®, Pubmed and Scopus) was undertaken to identify the key publication outlets for relevant content. These databases were selected as those that would be most relevant to the focus of the review and have the broadest range of relevant content. A range of text words, synonyms and subject headings were developed for the major constructs: global health, health service management and health leadership, priorities and challenges. Regarding health service management and health leadership, the following search terms were used: “healthcare manag*” OR “health manag*” OR “health services manag*” OR “health leader*”. Due to the large volume of diverse literature generated, a systematic search was then undertaken on the key journals that produced the largest number of relevant articles. The journals were selected as those identified as likely to contain highly relevant material based on an initial scoping of the literature.
Based on the initial database search, a systematic search for articles published in English between 1 January 2010 and 31 July 2018 was undertaken of the current issues and archives of the following journals: Asia-Pacific Journal of Health Management; BMC Health Services Research; Healthcare Management Review; International Journal of Healthcare Management; International Journal of Health Planning and Management; Journal of Healthcare Management; Journal of Health Organisation and Management; and, Journal of Health Management. Hand-searching of reference lists of identified papers were also used to ensure that major relevant material was captured.
Study selection and data extraction
Results were merged using reference-management software (Endnote) and any duplicates removed. The first author (CF) screened the titles and abstracts of articles meeting the eligibility criteria (Table 1 ). Full-text publications were requested for those identified as potentially relevant. The inclusion and exclusion criteria were then independently applied by two authors. Disagreements were resolved by consensus or consultation with a third person, and the following data were extracted from each publication: author(s), publication year, location, primary focus and main findings in relation to the research objective. Sixty-three articles were included in the final review. The selection process followed the PRISMA checklist [ 11 ] as shown in Fig. 1 .
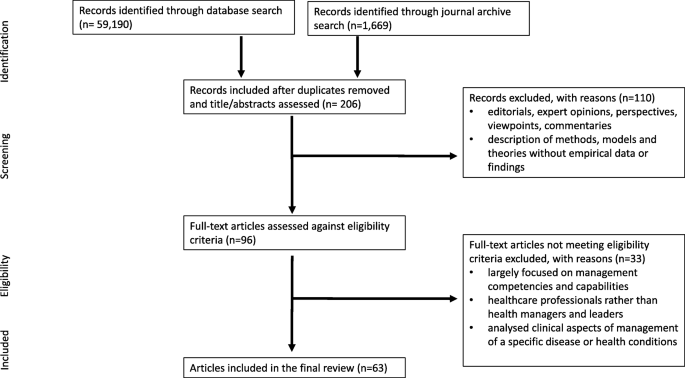
PRISMA flow chart of the literature search, identification, and inclusion for the review
Data extraction and analysis
A narrative synthesis was used to explore the literature against the review objective. A narrative synthesis refers to “an approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis” [ 15 ]. Firstly, an initial description of the key findings of included studies was drafted. Findings were then organised, mapped and synthesised to explore patterns in the data.
Search results
A total of 63 articles were included; Table 2 summarizes the data extraction results by region and country. Nineteen were undertaken in Europe, 16 in North America, and one in Australia, with relatively fewer studies from Asia, the Middle East, and small island developing countries. Eighteen qualitative studies that used interviews and/or focus group studies [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 ] were identified. Other studies were quantitative [ 33 , 34 , 35 , 36 , 37 , 38 , 39 ] including the use of questionnaires or survey data, or used a mixed-method approach [ 40 , 41 , 42 , 43 , 44 ]. Other articles combined different types of primary and secondary data (key informant interviews, observations, focus groups, questionnaire/survey data, and government reports). The included literature also comprised 28 review articles of various types that used mixed data and bibliographic evidence.
Key challenges and emerging trends
A set of challenges and emerging trends were identified across healthcare sectors internationally. These were grouped at three levels: 1) macro, system context (society, demography, technology, political economy, legal framework, history, culture), 2) meso, organisational context (infrastructure, resources, governance, clinical processes, management processes, suppliers, patients), and 3) micro context related to the individual healthcare manager (Table 3 ). This multi-levelled approach has been used in previous research to demonstrate the interplay between different factors across different levels, and their direct and indirect reciprocal influences on healthcare management policies and practices [ 45 ].
Societal and system-wide (macro)
Population growth, ageing populations, and increased disease burdens are some of the common trends health systems are facing globally. Developing and developed countries are going through demographic and epidemiological transitions; people are living longer with increasing prevalence of chronic diseases requiring health managers and leaders to adjust to shifting healthcare needs at the population level, delivering preventative and long-term care beyond acute care. Countries in Africa, Europe, the Pacific Islands, Middle East, Asia and Caribbean are seeing an increase in number of patients with non-communicable diseases and communicable diseases [ 21 , 46 , 47 , 48 , 49 , 50 , 51 , 52 ].
Although many countries have similar emerging health system concerns, there are some differences in the complexities each country faces. For many small countries, outmigration, capacity building and funding from international aid agencies are affecting how their health systems operate, while in many larger countries, funding cuts, rise in private health insurance, innovations, and health system restructuring are major influences [ 21 , 34 , 50 , 53 , 54 ]. In addition, patients are increasingly health literate and, as consumers, expect high-quality healthcare [ 34 , 53 , 54 ]. However, hospitals and healthcare systems are lacking capacity to meet the increased demand [ 16 , 34 , 43 ].
Scientific advances have meant more patients are receiving care across the health system. It is imperative to have processes for communication and collaboration between different health professionals for high-quality care. However, health systems are fragmented; increasing specialisation is leading to further fragmentation and disassociation [ 31 , 54 , 55 ]. Adoption of technological innovations also require change management, hospital restructure, and capacity building [ 56 , 57 , 58 ].
Changes in health policies and regulations compound the challenge faced by healthcare managers and leaders to deliver high quality care [ 53 , 54 , 59 ]. Political reforms often lead to health system restructuring requiring change in the values, structures, processes and systems that can constrain how health managers and leaders align their organisations to new agendas [ 24 , 28 , 31 , 60 ]. For example, the distribution of health services management to local authorities through decentralisation has a variable impact on the efficacy and efficiency of healthcare delivery [ 24 , 27 , 35 , 59 ].
Governments’ decisions are often made focusing on cost savings, resulting in budgetary constraints within which health systems must operate [ 16 , 19 , 53 , 61 ]. Although some health systems have delivered positive results under such constraint [ 53 ], often financial resource constraints can lead to poor human and technical resource allocation, creating a disconnect between demand and supply [ 23 , 27 , 40 , 47 , 57 ]. To reduce spending in acute care, there is also a push to deliver health services in the community and focus on social determinants of health, though this brings further complexities related to managing multiple stakeholder collaborations [ 27 , 32 , 34 , 38 , 40 , 49 , 55 ].
Due to an increase in demand and cost constraints, new business models are emerging, and some health systems are resorting to privatisation and corporatisation [ 22 , 48 , 62 ]. This has created competition in the market, increased uptake of private health insurance and increased movement of consumers between various organisations [ 22 , 48 ]. Health managers and leaders need to keep abreast with continuously changing business models of care delivery and assess their impact [ 59 , 62 ]. The evolving international health workforce, insufficient numbers of trained health personnel, and maintaining and improving appropriate skill mixes comprise other important challenges for managers in meeting population health needs and demands (Table 3 ).
Organisational level (meso)
At the organisation level, human resource management issues were a central concern. This can be understood in part within the wider global human resources for health crisis which has placed healthcare organisations under intense pressure to perform. The evidence suggests healthcare organisations are evolving to strengthen coordination between primary and secondary care; there is greater attention to population-based perspectives in disease prevention, interdisciplinary collaboration, and clinical governance. These trends are challenged by the persistence of bureaucratic and hierarchical cultures, emphasis on targets over care quality, and the intensification of front-line and middle-management work that is limiting capacity.
Healthcare managers and leaders also face operational inefficiencies in providing primary health and referral services to address highly complex and shifting needs which often result in the waste of resources [ 49 , 63 , 64 ]. Considering the pace of change, organisations are required to be flexible and deliver higher quality care at lower cost [ 21 , 53 , 65 ]. To achieve this, many organisations in developing and developed countries alike are adopting a lean model [ 17 , 21 ]. However, there are challenges associated with ensuring sustainability of the lean system, adjusting organisational hierarchies, and improving knowledge of the lean model, especially in developing countries [ 17 , 21 ].
Healthcare organisations require various actors with different capabilities to deliver high quality care. However, a dominant hierarchical culture and lack of collaborative and distributed culture can limit the performance of healthcare organisations [ 22 , 36 , 54 ]. In addition, considering high turnover of executive leadership, healthcare organisations often rely on external talent for succession management which can reduce hospital efficiency [ 44 , 66 ]. Other contributors to weakened hospital performance include: the lack of allocative efficiency and transparency [ 24 , 30 , 64 , 67 ]; poor hospital processes that hamper the development of effective systems for the prevention and control of hospital acquired infections (HAIs) [ 53 , 68 ]; and, payment reforms such as value-based funding and fee-for-service that encourage volume [ 18 , 23 , 24 , 61 , 62 , 69 , 70 ].
Managerial work distribution within organisations is often not clearly defined, leading to extra or extreme work conditions for middle and front-line managers [ 29 , 42 , 53 , 70 ]. Unregulated and undefined expectations at the organisation level leads to negative effects such as stress, reduced productivity, and unpredictable work hours, and long-term effects on organisational efficiency and delivery of high quality care [ 22 , 28 , 29 , 37 , 42 , 51 , 71 ]. Furthermore, often times front-line clinicians are also required to take the leadership role in the absence of managers without proper training [ 20 ]. Despite this, included studies indicate that the involvement of middle and front-line managers in strategic decision-making can be limited due to various reasons including lack of support from the organisation itself and misalignment of individual and organisational goals [ 16 , 26 , 31 , 72 ].
Individual level (micro)
Worldwide, middle and front-line health managers and leaders are disproportionately affected by challenges at the system and organisational level, which has contributed to increasing and often conflicting responsibilities. Some countries are experiencing a growth in senior health managers with a clinical background, while in other countries, the converse is apparent. Indistinct organisational boundaries, increasing scope of practice, and lack of systemic support at policy level are leaving healthcare managers with undefined roles [ 28 , 59 ]. Poorly defined roles contribute to reduced accountability, transparency, autonomy, and understanding of responsibilities [ 24 , 30 , 31 , 67 ]. Studies also indicate a lack of recognition of clinical leaders in health organisations and inadequate training opportunities for them as such [ 20 , 67 ].
The number of hybrid managers (performing clinical and managerial work concurrently) in developed countries is increasing, with the perception that such managers improve the clinical governance of an organization. In contrast, the number of non-clinical managers in many developing countries appears to be increasing [ 63 , 73 , 74 , 75 ]. Included studies suggest this approach does not necessarily improve manager-clinical professional relationships or the willingness of clinicians becoming managers, limiting their participation in strategic decisions [ 28 , 70 , 71 , 74 ].
This rapid review highlights the current global climate in health service management, the key priority areas, and current health management approaches being utilised to address these. The multitude of issues emerging demonstrate the complex and evolving role of health service management in the wider complex functioning of health systems globally in a changing healthcare landscape. Key themes of achieving high quality care and sustainable service delivery were apparent, often evidenced through health reforms [ 5 ]. The influence of technological innovation in both its opportunities and complexities is evident worldwide. In the context of changing healthcare goals and delivery approaches, health management is seeking to professionalise as a strategy to build strength and capacity. In doing so, health managers are questioning role scope and the skills and knowledge they need to meet the requirements of the role.
Global challenges facing health management
Understanding how the features of the macro, meso and micro systems can create challenges for managers is critical [ 19 ]. With continual healthcare reform and increasing health expenditure as a proportion of GDP, distinct challenges are facing high-income Organisation for Economic Co-operation and Development (OECD) countries, middle-income rapidly-developing economies, and low-income, resource-limited countries. Reforms, especially in OECD countries, have been aimed at controlling costs, consolidating hospitals for greater efficiencies, and reconfiguring primary healthcare [ 1 , 76 ]. The changing business models for the delivery of care have wider implications for the way in which health managers conceptualise healthcare delivery and the key stakeholders [ 59 ], for example, the emerging role of private healthcare providers and non-health actors in public health. Changes to the business model of healthcare delivery also has implications for the distribution of power amongst key actors within the system. This is evident in the evolved role of general practitioners (GPs) in the UK National Health Service as leaders of Clinical Commissioning Groups (CCGs). Commissioning requires a different skill set to clinical work, in terms of assessing financial data, the nature of statutory responsibilities, and the need to engage with a wider stakeholder group across a region to plan services [ 77 ]. With new responsibilities, GPs have been required to quickly equip themselves with new management capabilities, reflecting the range of studies included in this review around clinician managers and the associated challenges [ 18 , 28 , 53 , 63 , 70 , 71 , 74 , 75 ].
Central to the role of healthcare managers is the ability to transition between existing and new cultures and practices within healthcare delivery [ 59 ]. Bridging this space is particularly important in the context of increasingly personalized and technologically-driven healthcare delivery [ 54 ]. While advances in knowledge and medical technologies have increased capability to tackle complex health needs, the integration of innovations into existing healthcare management practices requires strong change management [ 73 ]. Health leaders and managers need to be able to rapidly and continually assess the changes required or upon them, the implications, and to transform their analysis into a workable plan to realise change [ 10 ]. Focusing only on the clinical training of health professionals rather than incorporating managerial and leadership roles, and specifically, change management capability may limit the speed and success of innovation uptake [ 22 ].
Implications
Our findings highlight the implications of current priorities within the health sector for health management practice internationally; key issues are efficiency savings, change management and human resource management. In the context of efficiency approaches, health system and service managers are facing instances of poor human and technical resource allocation, creating a disconnect between demand and supply. At the service delivery level, this has intensified and varied the role of middle managers mediating at two main levels. The first level of middle-management is positioned between the front-line and C-suite management of an organisation. The second level of middle-management being the C-suite managers who translate regional and/or national funding decisions and policies into their organisations. Faced with increasing pace of change, and economic and resource constraints, middle managers across both levels are now more than ever exposed to high levels of stress, low morale, and unsustainable working patterns [ 29 ]. Emphasis on cost-saving has brought with it increased attention to the health services that can be delivered in the community and the social determinants of health. Connecting disparate services in order to meet efficiency goals is a now a core feature of the work of many health managers mediating this process.
Our findings also have implications for the conceptualisation of healthcare management as a profession. The scale and increasing breadth of the role of health leaders and managers is evident in the review. Clarifying the professional identity of ‘health manager’ may therefore be a critical part of building and maintaining a robust health management workforce that can fulfil these diverse roles [ 59 ]. Increasing migration of the healthcare workforce and of population, products and services between countries also brings new challenges for healthcare. In response, the notion of transnational competence among healthcare professionals has been identified [ 78 ]. Transnational competence progresses cultural competence by considering the interpersonal skills required for engaging with those from diverse cultural and social backgrounds. Thus, transnational competence may be important for health managers working across national borders. A key aspect of professionalisation is the education and training of health managers. Our findings provide a unique and useful theoretical contribution that is globally-focused and multi-level to stimulate new thinking in health management educators, and for current health leaders and managers. These findings have considerable practical utility for managers and practitioners designing graduate health management programs.
Limitations
Most of the studies in the field have focused on the Anglo-American context and health systems. Notwithstanding the importance of lessons drawn from these health systems, further research is needed in other regions, and in low- and middle-income countries in particular [ 79 ]. We acknowledge the nuanced interplay between evidence, culture, organisational factors, stakeholder interests, and population health outcomes. Terminologies and definitions to express global health, management and leadership vary across countries and cultures, creating potential for bias in the interpretation of findings. We also recognise that there is fluidity in the categorisations, and challenges arising may span multiple domains. This review considers challenges facing all types of healthcare managers and thus lacks discrete analysis of senior, middle and front-line managers. That said, managers at different levels can learn from one another. Senior managers and executives may gain an appreciation for the operational challenges that middle and front-line managers may face. Middle and front-line managers may have a heightened awareness of the more strategic decision-making of senior health managers. Whilst the findings indicate consistent challenges and needs for health managers across a range of international contexts, the study does not capture country-specific issues which may have consequences at the local level. Whilst a systematic approach was taken to the literature in undertaking this review, relevant material may have been omitted due to the limits placed on the rapid review of the vast and diverse health management literature. The inclusion of only materials in English language may have led to further omissions of relevant work.
Health managers within both international and national settings face complex challenges given the shortage of human resources for health worldwide and the rapid evolution of national and transnational healthcare systems. This review addresses the lack of studies taking a global perspective of the challenges and emerging needs at macro (international, national and societal), meso (organisational), and micro (individual health manager) levels. Contemporary challenges of the global health management workforce orient around demographic and epidemiological change, efficiency-saving, human resource management, changing structures, intensified management, and shifting roles and expectations. In recognising these challenges, researchers, management educators, and policy makers can establish global health service management priorities and enhance health leadership and capacities to meet these. Health managers and leaders with adaptable and relevant capabilities are critical to high quality systems of healthcare delivery.
Abbreviations
Clinical Commissioning Groups
General practitioners
Hospital acquired infections
Organisation for Economic Co-operation and Development
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Rapid evidence assessment
Sustainable Development Goals
Universal health coverage
World Health Organization
Senkubuge F, Modisenyane M, Bishaw T. Strengthening health systems by health sector reforms. Glob Health Action. 2014;7(1):23568.
Article Google Scholar
World Health Organization, Global Health Workforce Alliance. Human resources for health: foundation for universal health coverage and the post-2015 development agenda. Report of the Third Global Forum on Human Resources for Health, 2013 November 10–13. Recife, Brazil: WHO; 2014.
Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, et al. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387(10020):811–6.
World Health Organisation. Working together for health: the world health report 2006: policy briefs. Geneva: World Health Organisation; 2006.
Google Scholar
West M, Dawson J. Employee engagement and NHS performance. London: King's Fund; 2012.
World Health Organization. Global strategy on human resources for health: workforce 2030. Geneva: World Health Organisation; 2016.
Reich MR, Javadi D, Ghaffar A. Introduction to the special issue on “effective leadership for health systems”. Health Syst Reform. 2016;2(3):171–5.
Waddington C, Egger D, Travis P, Hawken L, Dovlo D, World Health Organization. Towards better leadership and management in health: report of an international consultation on strengthening leadership and management in low-income countries, 29 January-1 February. Ghana: Accra; 2007.
World Health Organization. Quality of care: a process for making strategic choices in health systems. Manila: WHO Regional Office for the Western Pacific; 2006.
Ginter PM, Duncan WJ, Swayne LE. The strategic management of health care organizations: John Wiley & Sons; 2018.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Int Med. 2009;151(4):264–9.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(2):91–108.
Varker T, Forbes D, Dell L, Weston A, Merlin T, Hodson S, et al. Rapid evidence assessment: increasing the transparency of an emerging methodology. J Eval Clin Pract. 2015;21(6):1199–204.
Tricco AC, Langlois EV, Straus SE. Rapid reviews to strengthen health policy and systems: a practical guide. Geneva, Switzerland: World Health Organization; 2017.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1:b92.
Taylor A, Groene O. European hospital managers’ perceptions of patient-centred care: a qualitative study on implementation and context. J Health Organ Manag. 2015;29(6):711–28.
Costa LBM, Rentes AF, Bertani TM, Mardegan R. Lean healthcare in developing countries: evidence from Brazilian hospitals. Int J Health Plann Manage. 2017;32(1).
Chreim S, Williams BE, Coller KE. Radical change in healthcare organization: mapping transition between templates, enabling factors, and implementation processes. J Health Organ Manag. 2012;26(2):215–36.
Greenwald HP. Management challenges in British Columbia’s healthcare system. J Health Organ Manag. 2017;31(4):418–29.
Mercer D, Haddon A, Loughlin C. Leading on the edge: the nature of paramedic leadership at the front line of care. Health Care Manag Rev. 2018;43(1):12–20.
Reijula J, Reijula E, Reijula K. Healthcare management challenges in two university hospitals. Int J Healthc Tech Manag. 2016;15(4):308–25.
Srinivasan V, Chandwani R. HRM innovations in rapid growth contexts: the healthcare sector in India. Int J Hum Res Manage. 2014;25(10):1505–25.
Afzali HHA, Moss JR, Mahmood MA. Exploring health professionals' perspectives on factors affecting Iranian hospital efficiency and suggestions for improvement. Int J Health Plann Manag. 2011;26(1):e17–29.
Jafari M, Rashidian A, Abolhasani F, Mohammad K, Yazdani S, Parkerton P, et al. Space or no space for managing public hospitals; a qualitative study of hospital autonomy in Iran. Int J Health Plann Manag. 2011;26(3):e121–e37.
Lapão LV, Dussault G. From policy to reality: clinical managers' views of the organizational challenges of primary care reform in Portugal. Int J Health Plann Manag. 2012;27(4):295–307.
Andreasson J, Eriksson A, Dellve L. Health care managers' views on and approaches to implementing models for improving care processes. J Nurs Manag. 2016;24(2):219–27.
Maluka SO, Hurtig AK, Sebastián MS, Shayo E, Byskov J, Kamuzora P. Decentralization and health care prioritization process in Tanzania: from national rhetoric to local reality. Int J Health Plann Manag. 2011;26(2):e102–e20.
Taytiwat P, Briggs D, Fraser J, Minichiello V, Cruickshank M. Lessons from understanding the role of community hospital director in Thailand: clinician versus manager. Int J Health Plann Manag. 2011;26(2):e48–67.
Buchanan DA, Parry E, Gascoigne C, Moore C. Are healthcare middle management jobs extreme jobs? J Health Organ Manag. 2013;27(5):646–64.
Longenecker CO, Longenecker PD. Why hospital improvement efforts fail: a view from the front line. J Healthc Manag. 2014;59(2):147–57.
Reyes DJ, Bekemeier B, Issel LM. Challenges faced by public health Nurs leaders in Hyperturbulent times. Public Health Nurs. 2014;31(4):344–53.
Louis CJ, Clark JR, Gray B, Brannon D, Parker V. Service line structure and decision-maker attention in three health systems: implications for patient-centered care. Health Care Manag Rev. 2017. https://doi.org/10.1097/HMR.0000000000000172 .
Oppel EM, Winter V, Schreyogg J. Evaluating the link between human resource management decisions and patient satisfaction with quality of care. Health Care Manag Rev. 2017;42(1):53–64.
Ramanujam P. Service quality in health care organisations: a study of corporate hospitals in Hyderabad. J Health Manag. 2011;13(2):177–202.
Diana A, Hollingworth SA, Marks GC. Effects of decentralisation and health system reform on health workforce and quality-of-care in Indonesia, 1993–2007. Int J Health Plann Manag. 2015;30(1):e16–30.
Prenestini A, Lega F. Do senior management cultures affect performance? Evidence from Italian public healthcare organizations. J Healthc Manag. 2013;58(5):336–51.
Giauque D. Stress among public middle managers dealing with reforms. J Health Organ Manag. 2016;30(8):1259–83.
Jennings JC, Landry AY, Hearld LR, Weech-Maldonado R, Snyder SW, Patrician PA. Organizational and environmental factors influencing hospital community orientation. Health Care Manag Rev. 2017. https://doi.org/10.1097/HMR.0000000000000180 .
Tasi MC, Keswani A, Bozic KJ. Does physician leadership affect hospital quality, operational efficiency, and financial performance? Health Care Manag Rev. 2017. https://doi.org/10.1097/HMR.0000000000000173 .
Hall W, Williams I, Smith N, Gold M, Coast J, Kapiriri L, et al. Past, present and future challenges in health care priority setting: findings from an international expert survey. J Health Organ Manag. 2018;32(3):444–62.
Nelson SA, Azevedo PR, Dias RS, de Sousa SdMA, de Carvalho LDP, Silva ACO, et al. nursing work: challenges for health management in the northeast of Brazil. J Nurs Manag 2013;21(6):838–849.
Ireri S, Walshe K, Benson L, Mwanthi MA. A qualitative and quantitative study of medical leadership and management: experiences, competencies, and development needs of doctor managers in the United Kingdom. J Manag Marketing Healthc. 2011;4(1):16–29.
Powell M. The snakes and ladders of National Health Service management in England. Int J Health Plann Manag. 2014;29(3):260–79.
Groves KS. Examining the impact of succession management practices on organizational performance: A national study of U.S. hospitals. Health Care Manage Rev. 2017; doi: https://doi.org/10.1097/hmr.0000000000000176 .
Syed J, Özbilgin M. A relational framework for international transfer of diversity management practices. Int J Hum Res Manage. 2009;20(12):2435–53.
Adindu A. The need for effective management in African health systems. J Health Manag. 2013;15(1):1–13.
Greaves DE. Health management/leadership of Small Island developing states of the English-speaking Caribbean: a critical review. J Health Manag. 2016;18(4):595–610.
Khan MI, Banerji A. Health Care Management in India: some issues and challenges. J Health Manag. 2014;16(1):133–47.
Moghadam MN, Sadeghi V, Parva S. Weaknesses and challenges of primary healthcare system in Iran: a review. Int J Health Plann Manag. 2012;27(2):e121–e31.
Taylor R. The tyranny of size: challenges of health administration in Pacific Island states. Asia Pac J Health Manag. 2016;11(3):65.
Jooste K, Jasper M. A south African perspective: current position and challenges in health care service management and education in nursing. J Nurs Manag. 2012;20(1):56–64.
Sen K, Al-Faisal W. Reforms and emerging noncommunicable disease: some challenges facing a conflict-ridden country—the case of the Syrian Arab Republic. Int J Health Plann Manag. 2013;28(3):290–302.
Carney M. Challenges in healthcare delivery in an economic downturn, in the Republic of Ireland. J Nurs Manag. 2010;18(5):509–14.
Bowden DE, Smits SJ. Managing in the context of healthcare's escalating technology and evolving culture. J Health Organ Manag. 2012;26(2):149–57.
Meijboom BR, Bakx SJWGC, Westert GP. Continuity in health care: lessons from supply chain management. Int J Health Plann Manag. 2010;25(4):304–17.
Lega F, Calciolari S. Coevolution of patients and hospitals: how changing epidemiology and technological advances create challenges and drive organizational innovation. J Healthc Manag. 2012;57(1):17–34.
Kim Y, Kang M. The performance management system of the Korean healthcare sector: development, challenges, and future tasks. Public Perform Manag. 2016;39(2):297–315.
CAS Google Scholar
Hernandez SE, Conrad DA, Marcus-Smith MS, Reed P, Watts C. Patient-centered innovation in health care organizations: a conceptual framework and case study application. Health Care Manag Rev. 2013;38(2):166–75.
Briggs D, Isouard G. The language of health reform and health management: critical issues in the management of health systems. Asia Pac J Health Manag. 2016;11(3):38.
Zuckerman AM. Successful strategic planning for a reformed delivery system. J Healthc Manag. 2014;59(3):168–72.
Gantz NR, Sherman R, Jasper M, Choo CG, Herrin-Griffith D, Harris K. Global nurse leader perspectives on health systems and workforce challenges. J Nurs Manag. 2012;20(4):433–43.
Jeurissen P, Duran A, Saltman RB. Uncomfortable realities: the challenge of creating real change in Europe’s consolidating hospital sector. BMC Health Serv Res. 2016;16(2):168.
Kirkpatrick I, Kuhlmann E, Hartley K, Dent M, Lega F. Medicine and management in European hospitals: a comparative overview. BMC Health Serv Res. 2016;16(2):171.
Akbulut Y, Esatoglu AE, Yildirim T. Managerial roles of physicians in the Turkish healthcare system: current situation and future challenges. J Health Manag. 2010;12(4):539–51.
Naranjo-Gil D. The role of top management teams in hospitals facing strategic change: effects on performance. Int J Healthc Manag. 2015;8(1):34–41.
Ford EW, Lowe KB, Silvera GB, Babik D, Huerta TR. Insider versus outsider executive succession: the relationship to hospital efficiency. Health Care Manag Rev. 2018;43(1):61–8.
Leggat SG, Balding C. Achieving organisational competence for clinical leadership: the role of high performance work systems. J Health Organ Manag. 2013;27(3):312–29.
Baylina P, Moreira P. Healthcare-associated infections – on developing effective control systems under a renewed healthcare management debate. Int J Healthc Manag. 2012;5(2):74–84.
Jha R, Sahay B, Charan P. Healthcare operations management: a structured literature review. Decis. 2016;43(3):259–79.
Kuhlmann E, Rangnitt Y, von Knorring M. Medicine and management: looking inside the box of changing hospital governance. BMC Health Serv Res. 2016;16(2):159.
Spehar I, Frich JC, Kjekshus LE. Clinicians’ experiences of becoming a clinical manager: a qualitative study. BMC Health Serv Res. 2012;12(1):421.
Rodriguez CA. Challenges to effectiveness in public health organizations: the case of the Costa Rican health ministry. J Bus Res. 2016;69(9):3859–68.
Cinaroglu S. Complexity in healthcare management: why does Drucker describe healthcare organizations as a double-headed monster? Int J Healthc Manag. 2016;9(1):11–7.
Rotar A, Botje D, Klazinga N, Lombarts K, Groene O, Sunol R, et al. The involvement of medical doctors in hospital governance and implications for quality management: a quick scan in 19 and an in depth study in 7 OECD countries. BMC Health Serv Res. 2016;16(2):160.
Edmonstone JD. Whither the elephant?: the continuing development of clinical leadership in the UK National Health Services. Int J Health Plann Manag. 2014;29(3):280–91.
Naylor C, Ross S, Curry N, Holder H, Marshall L, Tait E. Clinical commissioning groups: supporting improvement in general practice? London: The King's Fund; 2013.
Holder H, Robertson R, Ross S, Bennett L, Gosling J, Curry N. Risk or reward? The changing role of CCGs in general practice. London: Kings Fund/Nuffield Trust; 2015.
Koehn PH, Rosenau JN. Transnational competence in an emergent epoch. Int Stud Perspect. 2002;3(2):105–27.
Antunes V, Moreira JP. Skill mix in healthcare: an international update for the management debate. Int J Healthc Manag. 2013;6(1):12–7.
Seitio-Kgokgwe OS, Gauld R, Hill PC, Barnett P. Understanding human resource management practices in Botswana’s public health sector. J Health Organ Manag. 2016;30(8):1284–300.
Miners C, Hundert M, Lash R. New structures for challenges in healthcare management. Healthc Manage Forum. 2015;28(3):114–7.
Hopkins J, Fassiotto M, Ku MC, Mammo D, Valantine H. Designing a physician leadership development program based on effective models of physician education. Health Care Manag Rev. 2017. https://doi.org/10.1097/hmr.0000000000000146 .
Miranda R, Glenn SW, Leighton JA, Pasha SF, Gurudu SR, Teaford HG, et al. Using hybrid change strategies to improve the patient experience in outpatient specialty care. J Healthc Manag. 2015;60(5):363–76.
Download references
Acknowledgements
Not applicable
The rapid review is part of a larger study on global health management priorities and qualities, supported by the University of New South Wales, Sydney.
Availability of data and materials
The data that support the findings of this review are included in this published article.
Author information
Authors and affiliations.
School of Public Health and Community Medicine, University of New South Wales, UNSW, Sydney, 2052, Australia
Carah Alyssa Figueroa, Reema Harrison, Ashfaq Chauhan & Lois Meyer
You can also search for this author in PubMed Google Scholar
Contributions
CF conducted the database searches and identification of relevant literature. RH and AC assessed the selected literature. RH and LM conceived the design of the review and contributed to the interpretation of the review results. CF drafted the initial manuscript while RH, AC and LM reviewed and revised subsequent drafts of the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Carah Alyssa Figueroa .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Figueroa, C.A., Harrison, R., Chauhan, A. et al. Priorities and challenges for health leadership and workforce management globally: a rapid review. BMC Health Serv Res 19 , 239 (2019). https://doi.org/10.1186/s12913-019-4080-7
Download citation
Received : 08 March 2019
Accepted : 09 April 2019
Published : 24 April 2019
DOI : https://doi.org/10.1186/s12913-019-4080-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health service management
- Health leadership
- Global health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Mapping the literature of health care management: an update
Affiliations.
- 1 [email protected], Southern Illinois University Carbondale, Carbondale, IL.
- 2 [email protected], Southern Illinois University Carbondale, Carbondale, IL.
- 3 [email protected], Southern Illinois University Carbondale, Carbondale, IL.
- PMID: 34629976
- PMCID: PMC8485946
- DOI: 10.5195/jmla.2021.1121
Objective: This study aims to identify the core journals cited in the health care management literature and to determine their coverage in the foremost bibliographic databases used by the discipline.
Methods: Using the methodology outlined by the Medical Library Association's Nursing and Allied Health Resource Section (NAHRS) protocol for "Mapping the Literature of Nursing and Allied Health Professions," this study updates an earlier study published in 2007. Cited references from articles published in a three-year range (2016-2018) were collected from five health care management journals. Using Bradford's Law of Scattering, cited journal titles were tabulated and ranked according to the number of times cited. Eleven databases were used to determine coverage of the most highly cited journal titles for all source journals, as well as for a subset of practitioner-oriented journals.
Results: The most highly cited sources were journals, followed by government documents, Internet resources, books, and miscellaneous resources. The databases with the most complete coverage of Zone 1 and 2 were Scopus, Web of Science Core Collection, and PubMed, while the worst performing databases were Health Business Elite, ABI/Inform, and Business Source Complete.
Conclusions: The literature of health care management has expanded rapidly in the last decade, with cumulative citations increasing by 76.6% and the number of cited journal titles increasing by nearly 70% since the original study. Coverage of the core journals in popular databases remains high, although specialized health care management and business databases did not perform as well as general or biomedical databases.
Copyright © 2021 Amber T. Burtis, Susan M. Howell, Mary K. Taylor.
- Abstracting and Indexing*
- Bibliometrics
- Databases, Bibliographic
- Delivery of Health Care
- Publications*
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Keeping pace with the healthcare transformation: a literature review and research agenda for a new decade of health information systems research
Nadine ostern, guido perscheid, caroline reelitz, jürgen moormann.
- Author information
- Article notes
- Copyright and License information
Responsible Editor: Shengnan Han
Corresponding author.
Received 2020 Dec 11; Accepted 2021 May 26; Issue date 2021.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Accelerated by the coronavirus disease 2019 (Covid-19) pandemic, major and lasting changes are occuring in healthcare structures, impacting people's experiences and value creation in all aspects of their lives. Information systems (IS) research can support analysing and anticipating resulting effects.
The purpose of this study is to examine in what areas health information systems (HIS) researchers can assess changes in healthcare structures and, thus, be prepared to shape future developments.
A hermeneutic framework is applied to conduct a literature review and to identify the contributions that IS research makes in analysing and advancing the healthcare industry.
We draw an complexity theory by borrowing the concept of 'zooming-in and out', which provides us with a overview of the current, broad body of research in the HIS field. As a result of analysing almost 500 papers, we discovered various shortcomings of current HIS research.
Contribution
We derive future pathways and develop a research agenda that realigns IS research with the transformation of the healthcare industry already under way.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12525-021-00484-1.
Keywords: Healthcare, Health information systems research, Research agenda
Introduction
Particularly since the last decade, IT has opened up new opportunities for ‘ehealth’ through telemedicine and remote patient monitoring, alongside potential improvements in the cost-effectiveness and accessibility of health care (Chiasson & Davidson, 2004 ). Accordingly, health information systems (HIS) research has come to focus on how healthcare organizations invest in and then assimilate HIS, looking in particular at the impact of digitalization on healthcare costs, healthcare quality, and patient privacy (Chen et al., 2019 ; Park, 2016 ).
Less attention has been paid to issues such as mobile health, health information interchange, digital health communities, and services that change customer expectations and may lead to major disruptions (Chen et al., 2019 ; Park, 2016 ). These topics, however, are becoming increasingly important due to the penetration of the user and health market by external players, especially tech companies, providing services such as fitness trackers, and surveillance software for patient monitoring in hospitals (Gantori et al., 2020 ). Modern IT, thus, becomes a catalyst to provide greater operational efficiency, offering new possibilities for tech companies to build new health-centred business models and services (Park, 2016 ).
The ways in which tech companies are entering the healthcare industry can be seen amid the spread of coronavirus disease 2019 (Covid-19), which is pushing healthcare systems to the edge of their capacities (Worldbank, 2020 ). In this extraordinary condition, the pandemic has provided an additional opportunity for tech companies that were hitherto not active or not allowed to enter the healthcare industry (Gantori et al., 2020 ).
We are currently seeing how entering the healthcare market is actually taking place, particularly in the USA, where tech companies are increasingly offering services to help address some of the problems associated with Covid-19. Google’s subsidiary Verily, for instance, facilitates the automation of coronavirus symptom screening and provides actionable, up-to-date information that supports community-based decision-making (Landi, 2020 ). Although the collaboration with Verily assists the US government in tracking cases to identify the spread of the virus, it is reasonable to suggest that Verily probably did not launch the screening tool out of altruism. In fact, to receive preliminary screening results via the Verily app, citizens have to log into their personal Google account (Greenwood, 2020 ). This allows Verily to gain immense value by aggregating huge, structured data sets and analyse them to come up with new health services, such as better tools for disease detection, new data infrastructures, and insurance offerings that – for better or for worse – may outplay current healthcare providers and even disrupt whole healthcare ecosystems (CB Insights, 2018 ). Similarly, Amazon has started to provide cloud space through Amazon Web Services to store health surveillance data for the Australian government’s tracing app (Tillett, 2020 ), and Amazon Care, a division initially responsible for handling internal staff care needs, now cooperates with the Bill and Melinda Gates Foundation to distribute Covid-19 testing kits to US residents (Lee & Nilsson, 2020 ).
Looking at information systems (IS) researchers’ previous assessments of state-of-the-art healthcare-related IS literature reveals that most scholars seem to have little or no concern for the beginning of those potentially long-lasting changes that are occurring in the healthcare industry (Chen et al., 2019 ). This is worrying, considering that it is already apparent that the years ahead will be marked by economic volatility and social upheaval as well as direct and indirect health consequences, including sweeping transformations in many of the world’s healthcare systems.
While it is clear that recent developments and the push of tech and platform companies into the healthcare sector can significantly improve the quality of life for billions of people around the world, it will be accompanied by serious challenges for healthcare industries, governments, and individuals (Park, 2016 ). Technological advances are, for instance, giving rise to a plethora of smart, connected products and services, combining sensors, software, data, analytics, and connectivity in all kinds of ways, which in turns leads to a restructuring of health industry boundaries and the empowerment of novel actors, especially tech and platform companies such as IBM, Google, and Amazon (Park, 2016 ).
Observing those changes, we need to develop a general understanding of long-term trends such as digitalization and blurring industry boundaries. As the pandemic is only an amplifier of longer-lasting trends, it is likely that the consequences and exogenous effects on the healthcare industry will go far beyond the time of the current pandemic. Given these observations, we wonder whether the IS research domain is ready to capture, understand, and accompany these developments, which require a holistic view of the healthcare industry, its structures, and the interdependencies between incumbents and new entrants. Thus, we argue that it is now time to develop a more comprehensive understanding of these developments and to determine the role that IS research can play by asking: How can we prepare HIS research to capture and anticipate current developments in the healthcare industry?
To find answers to this question, our paper provides a literature overview of HIS research by ‘zooming in and zooming out’ (Gaskin et al., 2014 ) and by drawing on complexity theory (Benbya et al., 2020 ). Since a healthcare system, like the industry as a whole, can be understood as a complex, digital socio-technical system (Kernick & Mitchell, 2009 ; Therrien et al., 2017 ), zooming in and zooming out is a way to view, capture, and theorize the causes, dynamics, and consequences of a system’s complexity. Complex systems are characterized by adaptiveness, openness (Cilliers, 2001 ), and the diversity of actors and their mutual dependency in the system, meaning that outcomes and research span various levels within these systems, although the boundaries of socio-technical systems are elusive. Assuming that HIS research is just as complex as the socio-technical system investigated, we first zoom in, focusing on concrete research outcomes across levels (i.e., what we can actually observe). Zooming in is followed by zooming out, which means abstracting from the concrete level and embracing the strengths and disparities of overall HIS research on a higher level in which concrete research outcomes are embedded (Benbya et al., 2020 ). Using this approach, we can capture and understand the complexity of HIS research without losing sight of concrete research issues and topics that drive research in this field.
To do this, we chose a hermeneutic framework to guide us in a thorough review and interpretation of HIS literature and lead us to the following overarching observations: (i) The literature review determines the unique contribution that IS research plays in analysing and advancing the healthcare industry. However, it also shows that we are hardly prepared to take up current developments and anticipate their consequences. (ii) The reason for this unpreparedness is that we currently neglect the ecosystem perspective and thus ignore holistic approaches to resolve the striking number of interrelated issues in HIS research. (iii) Based on the unique insights of this literature review, our paper provides a research agenda in which we use complexity theory to discuss the consequences of current developments. This theory assists IS researchers not only to better understand developments and implications thereof for the healthcare industry (and thus HIS research) but also to create a meaningful impact on the future of this industry. Since we have limited our research explicitly to the IS domain, our results may not be generally applicable to other healthcare research domains and we do not claim to provide an overview of the literature in the field of HIS research. However, while IS researchers cannot solve the pandemic directly, preparing them by providing a new research agenda will support them in developing concepts and applications, thereby helping them to overcome the negative effects of the pandemic. In our opinion, it is particularly important that IS research, and especially HIS-related research, obtains a deeper understanding of the needed transformation that is caused by digitalization and the emergence of new players catalysed by the current pandemic.
The remainder of this paper is structured as follows. The next section is concerned with the hermeneutic framework used to conduct the systematic literature review. After explaining the hermeneutic approach and the research steps, we elaborate on the key findings by zooming in; that is, we focus on the key results that emerge from analysing and interpreting the literature for each of the phases defined in the course of the literature sorting process. We then concentrate on zooming out, emphasizing the patterns and interdependencies across phases, which helps us determine the state of HIS research. The results of both parts of the literature review – i.e., zooming in and zooming out (Benbya et al., 2020 ; Gaskin et al., 2014 ) – support us in identifying strengths, as well as drawbacks, in HIS research. On this basis, we develop a research agenda that provides future directions for how HIS research can evolve to anticipate the impending transformation of the healthcare industry.
Literature review: a hermeneutic approach
To answer our research question, we conducted a literature review based on hermeneutic understanding. In particular, we followed Boell and Cecez-Kecmanovic ( 2014 ). They proposed a hermeneutic philosophy as a theoretical foundation and methodological approach that focuses on the inherently interpretive processes in which a reader engages in an ever-expanding and deepening understanding of a relevant body of literature. Adopting a comprehensive literature review approach that addresses well-known issues resulting from applying structured literature review approaches (e.g., Webster & Watson, 2002 ), we strive toward the dual purpose of hermeneutic analysis – i.e., to synthesize and critically assess the body of knowledge (Boell & Cecez-Kecmanovic, 2014 ). We would like to emphasize that the hermeneutic approach to literature reviews is not in opposition to structured approaches. Rather, it addresses the weaknesses of structured approaches (i.e., that they view engagement with the literature as a routine task rather than as a process of intellectual development) and complements them with the hermeneutic perspective to create a holistic approach for conducting literature reviews.
Theoretical underpinning and research method
A methodological means for engaging in reciprocal interpretation of a whole and its constituent elements is the hermeneutic cycle (Bleicher, 2017 ), which consists of a mutually intertwined search and acquisition circle (Circle 1 in Fig. 1 ) and the wider analysis and interpretation circle (Circle 2 in Fig. 1 ) (Boell & Cecez-Kecmanovic, 2014 ). Figure 1 depicts the steps associated with the hermeneutic literature review. The search and acquisition circle is shown on the left of the figure, while the analysis and interpretation circle containing steps of meta and content analysis is depicted on the right. The two circles should be understood as an iterative procedure, the nature of which will be explained in the following.
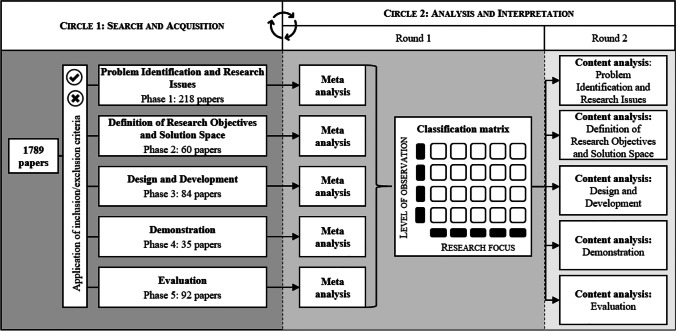
Hermeneutic procedure applied to the literature review
Circle 1: Search and acquisition
The hermeneutic literature review starts with the search and acquisition circle, which is aimed at finding, acquiring, and sorting relevant publications. In line with holistic thinking, we began with the identification of a rather small set of highly relevant literature (Boell & Cecez-Kecmanovic, 2014 ) and went on to identify further literature on the basis of progressively emerging keywords. This step is central to the hermeneutic approach and addresses a criticism on structured literature reviews, namely that they downplay the importance of reading and dialogical interaction between the literature and the reader in the literature search process, reducing it to a formalistic search, stifling academic curiosity, and threatening quality and critique in scholarship and research (Boell & Cecez-Kecmanovic, 2014 ; MacLure, 2005 ). Thus, while the search process remains formalized, as in pure structured approaches, the hermeneutic approach allows us to acquire more information about the problem at hand and to identify more relevant sources of information (Boell & Cecez-Kecmanovic, 2014 ).
Given our initial research question and the scope of the review, we began by searching for papers in the Association for Information System’s (AIS’s) eLibrary over a period of 30 years (1990 to 2019). We consider this database to be a source of the most significant publications in the field of HIS research with a focus on the IS research domain. Using the keywords ‘digital health’ and ‘digital healthcare service’, we identified an initial set of 54 papers based on the title, abstract, and keyword search. Engaging in a first round of the hermeneutic search and acquisition circle, we extended and refined these keywords by identifying emerging topics within the literature, as well as using backward and forward search (Webster & Watson, 2002 ). In particular, with each additional paper identified through backward and forward search, we compared keyword references in the papers to our list of keywords and added them if there was sufficient content delimitation. The decision to add a keyword was discussed with all authors until consensus was reached. This led us to a set of 12 keywords, including ‘electronic health’, ‘ehealth’, ‘mobile health’, ‘mhealth’, ‘health apps’, ‘tech health’, ‘healthcare services’, ‘healthcare informatics’, ‘medical informatics’, and ‘health data’.
The selection of publications being considered for our research comprised all journals belonging to the AIS eLibrary, the Senior Scholars’ Basket of Eight Journals (e.g., European Journal of Information Systems, Information Systems Research , and MIS Quarterly ), well-regarded journals following the analyses of Chiasson and Davidson ( 2004 ) and Chen et al. ( 2019 ) (e.g., Business & Information Systems Engineering , Communications of the ACM, and Decision Support Systems ), and the proceedings of the major AIS conferences (e.g., Americas Conference on Information Systems (AMCIS), International Conference on Information Systems (ICIS)). An overview of the selected journals and proceedings is provided in Appendix 1 .
Using our set of keywords, we searched for each keyword individually in the AIS eLibrary and the databases of the respective journals. Subsequently, we created a dataset and filtered out the duplicates, yielding a total number of 1,789 papers to be screened in the search and acquisition circle (Circle 1 in Fig. 1 ). Figure 2 provides an overview of this process by listing the total number of articles identified for each journal individually.
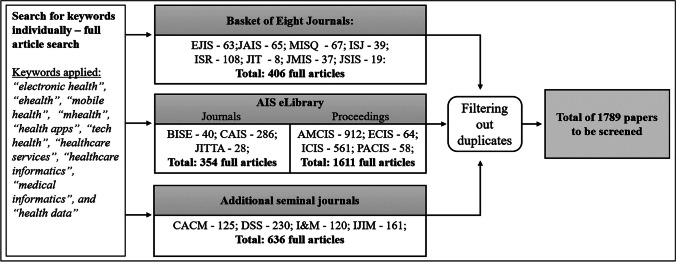
Steps of the search process to create the data set
The resulting 1,789 papers progressively passed through the intertwined hermeneutic circles. Because of the large number, we divided the papers at random into four equally sized groups and assigned them to each of the authors. Each author then screened the paper in his or her group. In the course of several rounds of discussion, decisions on the inclusion of keywords and articles in the literature review were made by all authors, based on the original recommendations of the author responsible for the respective group. To ensure rigor and transparency of the analysis and results, we kept a logbook in which all decisions of the authors and steps of the literature review were recorded (Humphrey, 2011 ).
Given the abundance of topics that were already apparent from titles and abstracts, we began to sort the publications (Boell & Cecez-Kecmanovic, 2014 ). The process of sorting proved to be challenging, as HIS research is diverse and tends to be eclectic (Agarwal et al., 2010 ). This is why researchers have developed frameworks for clustering and analysing HIS research (LeRouge et al., 2007 ). So far, however, no consent on a unified framework has emerged, and sorting is often strongly influenced by the authors’ views on HIS research (Agarwal et al., 2010 ; Fichman et al., 2011 ). For instance, Agarwal et al. ( 2010 ) predetermined health IT adoption and health IT impact as major themes associated with health ITs, acknowledging that this pre-categorization of research topics made a systematic review of the growing and increasingly complex HIS literature unfeasible. Consequently, we decided to sort the articles we had identified into groups inspired by and loosely related to the phases of design science research (DSR) (Peffers et al., 2008 ), which is an essential step in hermeneutics – i.e., defining guidelines to facilitate interpretive explication (Cole & Avison, 2007 ). DSR can be understood as a cumulative endeavour and, therefore, we understood HIS research as accumulative knowledge that can be reconstructed and consolidated using DSR phases as guidance (vom Brocke et al., 2015 ; vom Brocke et al., 2009 ). In particular, this helped us to sort the articles without prejudice to expected HIS research topics and clusters (Grondin, 2016 ).
In the past, researchers have used the DSR process in the context of literature reviews to identify advances in design science-related research outcomes (Offermann et al., 2010 ). In this paper, we use the DSR phases – in the sense of a rough guideline – as a neutral lens to classify articles according to their research outcomes. We thereby assume that HIS literature can be seen as an overall process, where research results and progress are built upon each other and can be classified into phases of problem identification and research issues , definition of research objectives and possible solution space , design and development of solutions , demonstration of research effectiveness, innovativeness and acceptance , and evaluation . These phases served as a guide to achieve an outcome-oriented, first-hand sorting of articles, while this approach also gave us the opportunity to take a bird's-eye view on HIS research. Note that we intentionally omitted the last step of DSR – i.e., communication – as we regard communication as present in all published articles. Based on our initial reading, we assigned all 1,789 papers to the phases and discussed this sorting in multiple rounds until all authors agreed on the assignments.
Simultaneously, we applied criteria for the inclusion and exclusion of articles. We included full papers published in the journals and conference proceedings belonging to our selection. We excluded articles that were abstract-only papers, research-in-progress papers, panel formats, or workshop formats, as well as papers without direct thematic reference to our research objective. Additionally, during the acquisition stage we stored selected papers in a separate database whenever they fulfilled certain quality criteria (e.g., for separate studies using the same dataset, such as a conference publication and a subsequent journal publication, we only used the articles with the most comprehensive reporting of data to avoid over-representation).
The authors read the resulting 489 papers to identify new core terms and keywords that were used in subsequent searches, which not only provided the link to the analysis and interpretation circle but also informed the literature search. For this purpose, each author read the papers and kept notes in the logbook that supported us in systematically recording the review process and allowed us to shift from concentrating on particular papers to focusing on scientific concepts (Boell & Cecez-Kecmanovic, 2014 ; Webster & Watson, 2002 ).
Circle 2: Analysis and interpretation
The search and acquisition circle formed part of the iterative procedure of analysis and interpretation, whereby the reading of individual papers was the key activity linking Circle 1 to the steps of Circle 2 (Boell & Cecez-Kecmanovic, 2014 ). Through orientational reading we gained a general understanding of the literature, thus laying the foundation for the subsequent steps of analysis and interpretation (Boell & Cecez-Kecmanovic, 2014 ).
Within the analysis and interpretation circle, two types of reviews were conducted for all identified and sorted articles: in a first round a meta-review, and in a second round a content analysis of the papers was performed. Meta-reviews are a useful tool for capturing and analysing massive quantities of knowledge using systematic measures and metrics. We followed Palvia et al. ( 2015 ), who proposed a structured method that is integrated into the hermeneutic approach. In particular, having identified and sorted the relevant research articles, we applied proposed review features, including methodological approach, level of observation, sample size, and research focus (Humphrey, 2011 ; Palvia et al., 2015 ) to map, classify, and analyse the publications (Boell & Cecez-Kecmanovic, 2014 ). In doing so, we slightly adapted the classic meta-analysis by focusing on meta-synthesis, which is similar to meta-analysis but follows an interpretive rather than a deductive approach. Whereas a classic meta-analysis tries to increase certainty in cause-and-effect conclusions, meta-synthesis seeks to understand and explain the phenomena of mainly qualitative work (Walsh & Downe, 2005 ). The results of the meta-synthesis provided the basis for our subsequent critical assessment of content. Furthermore, we created a classification matrix based on particularly salient features of the meta-review (i.e., levels of observation and research foci), which facilitated and standardized the content analysis.
Within the matrix, the levels of observation comprised infrastructure (e.g., information exchange systems, electronic health records), individuals (patients and users of digital health services), professionals (e.g., nurses and general practitioners), organizations (hospitals and other medical institutions), and an ecosystem level. The latter is defined as individuals, professionals, organizations, and other stakeholders integrated via a digital infrastructure and aiming to create a digital environment for networked services and organizations with common resources and expectations (Leon et al., 2016 ). To identify the most important concepts used by researchers, we discussed a variety of approaches to the derivation of research foci – i.e., areas containing related or similar concepts that are frequently used in research on HIS. Finally, six research focus areas emerged, covering all relevant research areas. To describe the core HIS research issues addressed by these foci, we used the following questions:
HIS strategy: What are the prerequisites for configuring, implementing, using, maintaining, and finding value in HISs?
HIS creation: How are HISs composed or developed?
HIS implementation: How are HISs implemented and integrated?
HIS use and maintenance: How can HISs be used and maintained once in place?
Consequences and value of HIS: What are the consequences and the added value of HISs?
HIS theorization: What is the intellectual contribution of HIS research?
We used the classification matrix as a tool for assigning publications and finding patterns across research articles and phases. In particular, we used open, axial, and selective coding (Corbin & Strauss, 1990 ) to analyse the content of articles in a second round of the analysis and interpretation circle. Each author individually assigned open codes to text passages while reading the identified research articles, noting their thoughts in the shared digital logbook that was used for constant comparative analysis. Once all authors had agreed on the open codes, axial coding – which is the process of relating the categories and subcategories (including their properties) to each other (Wolfswinkel et al., 2013 ) – was conducted by each author and then discussed until consent on codes was reached. Next, we conducted selective coding and discussed the codes until theoretical saturation was achieved (Corbin & Strauss, 1990 ; Matavire & Brown, 2008 ). For the sake of consistent terminology, we borrowed terms from Chen et al. ( 2019 ), who used multimethod data analysis to investigate the intellectual structure of HIS research. In particular, they proposed 22 major research themes, which we assigned to the initial codes whenever possible. In two rounds of discussion in which we compared the assignment of codes, two additional codes emerged, which left us with a total of 24 theme labels (Appendix 2 ). By discussing the codes at all stages of coding, theoretical saturation emerged, which is the stage at which no additional data are being found or properties of selective codes can be developed (Glaser & Straus, 1968 ; Saunders et al., 2018 ). In fact, independent from each other, all authors saw similar instances occurring over and over again, resulting in the same codes, making us confident that we had reached theoretical saturation (Saunders et al., 2018 ).
Finally, we entered the codes into the classification matrix, which allowed us to identify patterns based on the meta and content analysis. This enabled us to provide insights into the strengths and weaknesses of current HIS research; these are presented in the following section.
Zooming-in: key findings of the phase-based literature analysis
In the following, we ‘zoom in’ (Gaskin et al., 2014 ) by presenting key findings of the literature review for each phase, illustrated by means of the classification matrices. We assigned selective codes that emerged from the content analysis to the fields of the matrices, with the numbers in brackets indicating the frequency with which codes emerged. Note that, for the sake of clarity, we displayed only the most relevant research themes in the matrices and indicated the number of further papers using the reference ‘other themes.’ A complete list of research themes for each phase can be found in the appendix (Appendix 2 ). In the following, each table shows the classification matrix and selective codes that resulted from the meta and content analysis of papers in the respective phase. The shaded areas in the matrix show focused research themes (i.e., selective codes) and characteristics of research articles that gave way to clusters (i.e., collections of themes that appear frequently and/or characteristically for the respective focus).

Phase 1: Problem identification and research issues
Within the first phase, a large body of literature was found (218 articles). This phase encompasses articles that identify problems and novel research issues as a main outcome, with the aim of pointing out shortcomings and provoking further research. For instance, besides behavioural issues such as missing user acceptances or trust in certain HISs, the design and effectiveness of national health programs and/or HIS is a frequently mentioned topic. It should be noted, however, that literature assigned to this phase is extremely diverse in terms of research foci, levels of observation, and research themes, and hardly any gaps can be identified (Table 1 ).
HIS publications assigned to the phase of problem identification and research issues
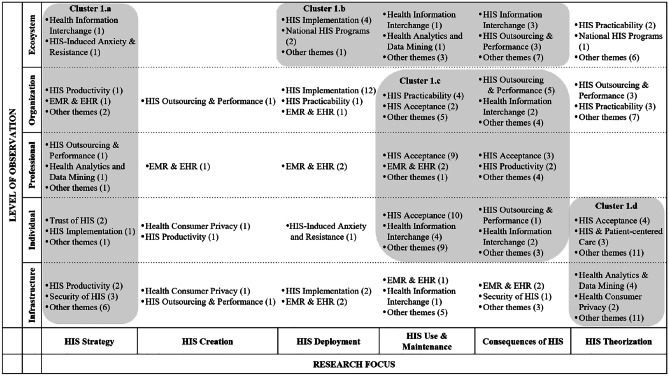
The first cluster (1a) encompasses the research focus of HIS strategy, spanning all levels of observation and totalling 24 publications. HIS strategy appears to be of particular relevance to the levels of organization and infrastructure. Content-wise, the theme of health information interchange is of particular interest, referring, for example, to the development of a common data infrastructure (Ure et al., 2009 ), consumer-oriented health websites (Fisher et al., 2007 ), and security risks of inter-organizational data sharing (Zhang & Pang, 2019 ). HIS productivity and HIS security are the second most salient themes, focusing, for example, on measuring the effectiveness of fitness apps (Babar et al., 2018 ) and presenting challenges with regard to the interoperability of medical devices (Sametinger et al., 2015 ).
The second cluster (1b), comprising 25 publications, represents the ecosystem level and focuses mainly on national and cross-national HIS-related issues such as the relation between ICT penetration and access to ehealth technologies across the European Union (Currie & Seddon, 2014 ), as well as on the collaboration and involvement of different stakeholders (Chang et al., 2009 ; King, 2009 ). Most important here is health information interchange – e.g., the provision, sharing, and transfer of information (Bhandari & Maheshwari, 2009 ; Blinn & Kühne, 2013 ).
Cluster 1c covers the research focus of HIS use and maintenance, as well as the consequences of HIS. Whereas most papers addressing the HIS acceptance theme focus on professionals’ or patients’ acceptance of specific technological solutions, such as telemedicine (Djamsbi et al., 2009 ) or electronic health records (Gabel et al., 2019 ), papers assigned to health information interchange focus on topics related to information disclosure, such as self-tracking applications (Gimpel et al., 2013 ). Finally, the HIS outsourcing and performance theme concentrates on financial aspects in organizations, including potential for quality improvements and cost reductions (Setia et al., 2011 ; Singh et al., 2011 ).
Finally, the fourth cluster (1d) focuses on HIS theorizing with respect to the individual and infrastructure levels of observation. Although this cluster represents a range of theme labels (15), those addressing HIS acceptance, HIS patient-centred care, as well as health analytics and data mining predominate. Papers within the theme label HIS acceptance cover a wide range of topics, such as the acceptance of telehealth (Tsai et al., 2019 ) up to the usage intentions of gamified systems (Hamari & Koivisto, 2015 ). The same applies to the papers assigned to the theme labels of health analytics and data mining. Focusing on the infrastructure level of observation, the identified papers mostly review academic research on data mining in healthcare in general (Werts & Adya, 2000 ), through to the review of articles on the usage of data mining with regard to diabetes self-management (Idrissi et al., 2019 ). Papers on HIS patient-centred care mostly address the challenges and opportunities of patient-centred ehealth applications (Sherer, 2014 ).
Apart from these clusters, quite a few research articles refer to the infrastructure level of observation, addressing information sharing in general (Li et al., 2008 ), electronic medical records (George & Kohnke, 2018 ; Wessel et al., 2017 ), and security and privacy issues (Zafar & Sneha, 2012 ).
Most common in terms of research methods within this phase are case studies (57), followed by quantitative data analyses (50), theoretical discussions (29), and literature studies (14). In particular, case studies dominate when referring to the ecosystem or infrastructure level of observation, whereas quantitative analyses are conducted when individuals or professionals are at the centre of the discussion. However, and unsurprisingly given the considerable diversity of research themes within this phase, the variety of research methods is also quite large, ranging from field studies (Paul & McDaniel, 2004 ), to interviews (Knight et al., 2008 ), to multimethod research designs (Motamarri et al., 2014 ).
Phase 2: Definition of research objectives and solution space
The second phase of HIS research yielded a lower number of articles (45) compared to the phase of problem identification and research issues. The second phase comprises articles that focus on proposing possible solutions to existing problems – i.e., introducing theory-driven, conceptual designs of health ecosystems including health information interchange, as well as scenario analyses anticipating the consequences of HIS implementation on an organizational level. Based on the research foci and levels of observation, we identified three specific thematic clusters, as shown in Table 2 .
HIS publications assigned to the definition of research objectives and solution space
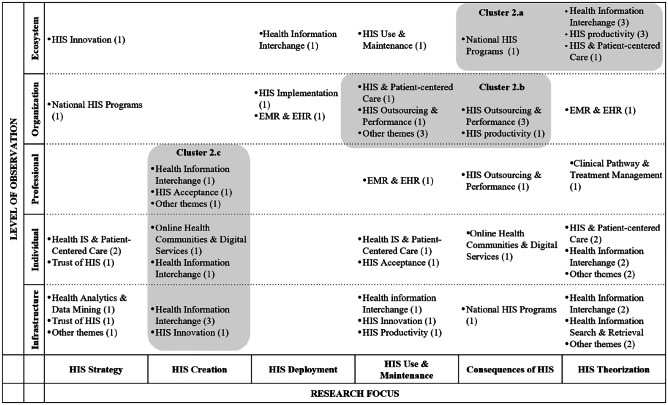
The first cluster (2a) comprises the ecosystem level of observation and encompasses eight publications. Besides a strong tendency toward theory-driven research, health information interchange is the most common theme. We found that the need to enable cooperation within networks and to ensure accurate data input was addressed in most of the literature. While a majority of studies focus on the application of HIS in networks within specific boundaries, such as medical emergency coordination (Sujanto et al., 2008 ) or Singapore’s crisis management in the fight against the SARS outbreak in 2003 (Devadoss & Pan, 2004 ), other studies, such as that by Aanestad et al. ( 2019 ), take an overarching perspective, addressing the need to break down silo thinking and to start working in networks. Following the question of why action research fails to persist over time, Braa et al. ( 2004 ) highlighted the role of network alignment, criticizing action research projects for failing to move beyond the prototyping phase and, therefore, failing to have any real impact.
Cluster 2b, encompassing nine publications, was derived from the observation that studies within the organizational level concentrated strongly on HIS use and maintenance and the consequences of HIS research. Herein, a vast array of topics was observed, such as the potential for cost reduction through HIS (Byrd & Byrd, 2009 ), the impact of HIS on product and process innovation in European hospitals (Arvanitis & Loukis, 2014 ), and the perceived effectiveness of security risk management in healthcare (Zafar et al., 2012 ). Moreover, we found that practice-oriented methods, such as mixed-method approaches, surveys, data analyses, and case studies, are used predominantly within this cluster. Focusing on the latter, most studies analyse particular scenarios by using a rather small sample of cases, for instance, Al-Qirim ( 2003 ) analysed factors influencing telemedicine success in psychiatry and dermatology in Norway.
The third cluster (2c) was derived from analysis of the HIS creation research focus (nine publications). Although health information interchange is the most represented in this cluster, a large number of further themes can be observed. Studies within this cluster predominantly address design aspects of system interoperability, focusing on data processing and data interchange between the actors. HISs mostly serve as a tool for the development or enhancement of decision support systems, such as for real-time diagnostics combining knowledge management with specific patient information (Mitsa et al., 2007 ) or clinical learning models incorporating decision support systems in the dosing process of initial drug selection (Akcura & Ozdemir, 2008 ).
Phase 3: Design and development
The design and development phase comprises 84 research articles concerned with the creation of novel IS artefacts (e.g., theories, models, instantiations). We thereby refer to Lee et al.’s ( 2015 ) definition of the IS artefact – i.e., the information, technology, and social artefact that forms an IS artefact by interacting. We assigned to this phase papers that are explicitly concerned with developing solutions for information exchange (e.g., design of messaging systems or knowledge systems in hospitals), technological artefacts (e.g., hardware or software used for generating electronic health records), and social artefacts that relate to social objects (e.g., design of national or international institutions and policies to control specific health settings and patient-centred solutions). Within the design and development phase, the analysis revealed two clusters (Table 3 ).
HIS publications assigned to the design and development phase
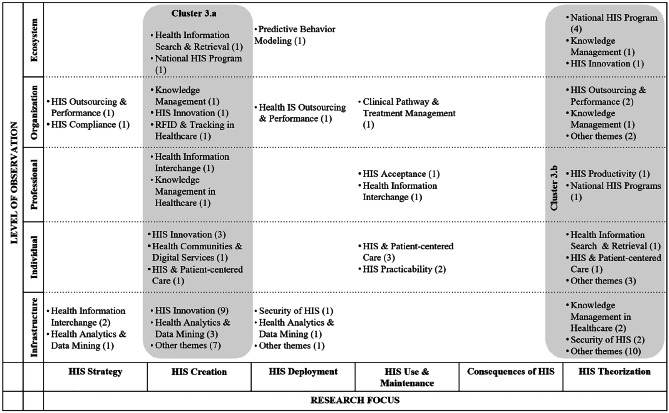
The first cluster (3a) was identified in the research focus of HIS creation (31 articles). Here, the most frequent research theme is HIS innovation followed by HIS and patient-centred care, HIS productivity, and health analytics and data mining. The focus is on specific contexts, mostly medical conditions and artefacts developed for their treatment, such as in the context of mental health/psychotherapy (Neben et al., 2016 ; Patel et al., 2018 ), diabetes (Lichtenberg et al., 2019 ), or obesity (Pletikosa et al., 2014 ). Furthermore, information infrastructures or architectures – for instance, for the process of drug prescription (Rodon & Silva, 2015 ), or for communication between healthcare providers and patients (Volland et al., 2014 ) – are represented.
The second aggregation of research articles is found in cluster 3b, focusing on theoretical aspects of HIS (32 articles). Again, these studies span all levels of observation (including infrastructure, individual, professional, organization, and ecosystem). Topics in this theme are diverse, ranging from HIS on a national level (Preko et al., 2019 ), to knowledge management in healthcare (Wu & Hu, 2012 ) to security of HIS (Kenny & Connolly, 2016 ).
Beyond both clusters, it is evident that during design and development, researchers do not deal with the consequences of HIS, nor does HIS strategy play an important role. Furthermore, only in the research focus of theorization is the ecosystem level of some relevance to other levels (e.g., the individual level). It should be noted that ecosystems are mostly referred to in terms of nations or communities, without any transnational or global perspective. Furthermore, the term ‘ecosystem’ has not been used in research, and within the other research focus areas, the ecosystem level is barely represented. Moreover, articles combining different perspectives of the single levels of observation on HIS – namely individuals (i.e., patients), professionals (i.e., medical staff), and organizations (e.g., hospitals) – are rare. During design and development, potential users are not typically integrated, whereas it is quite common to derive requirements and an application design from theory, only involving users afterwards – e.g., in the form of a field experiment (e.g., Neben et al., 2016 ).
Surprisingly, theoretical papers outweigh papers on practical project work, whereby the latter mostly focus on a description of the infrastructure or artefact (e.g., Dehling & Sunyaev, 2012 ; Theobalt et al., 2013 ; Varshney, 2004 ) or are based on (mostly single) case studies (e.g., Hafermalz & Riemer, 2016 ; Klecun et al., 2019 ; Ryan et al., 2019 ). Within the design and development phase, the generation of frameworks, research models, or taxonomies is prevalent (e.g., Preko et al., 2019 ; Tokar et al., 2015 ; Yang & Varshney, 2016 ).
Phase 4: Demonstration
This phase includes 35 articles related to presenting and elaborating on proposed solutions – e.g., how HIS can be implemented organization-wide (e.g., via integration into existing hospital-wide information systems), proposed strategies and health policies, as well as novel solutions that focus on health treatment improvements. Within the demonstration phase, we identified two clusters that emerged from the meta and content analyses (Table 4 ).
HIS publications assigned to the demonstration phase
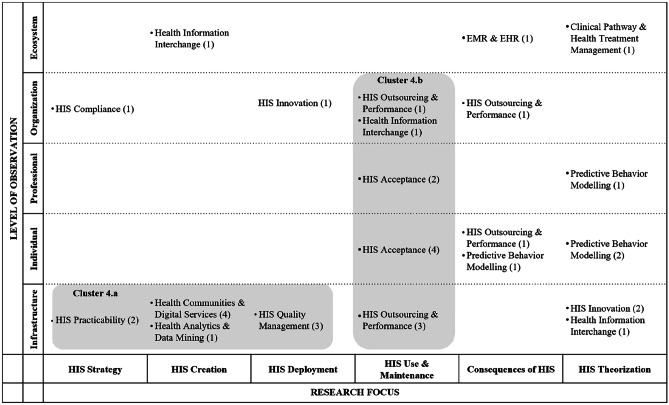
Cluster 4a (10 articles) is characterized by articles that focus on HIS issues related to the infrastructure level, spanning the research foci of HIS strategy, creation, and deployment. Content-wise, the cluster deals mainly with technical feasibility and desirability of HISs, including topics such as the configuration of modular infrastructures that support a seamless exchange of HISs within and between hospitals (Dünnebeil et al., 2013 ). Moreover, papers in this cluster address HIS practicability by determining general criteria that are important for the design of health information systems (Maheshwari et al., 2006 ) or conduct HIS application tests by carrying out prototypical implementations of communication infrastructures. In particular, the latter are tested and proven to meet specific technical standards to guarantee the frictionless transmission of health information data (Schweiger et al., 2007 ). In contrast, Heine et al. ( 2003 ) upscaled existing HIS solutions and tested the infrastructure in large, realistic scenarios.
Conversely, cluster 4b (11 articles) is mainly concerned with HIS use and maintenance, spanning several levels of observation – i.e., infrastructure, individuals, professionals, and organizations. Interestingly, papers in this cluster aim at efficiency and added value when looking at the infrastructure and organizational levels, whereas researchers are more interested in acceptance when focusing on the individual and professional use of HISs. Overall, cluster 4b is primarily concerned with organizational performance (e.g., increases in efficiency due to better communication and seamless transfer of patient health information) as well as user acceptance of new HISs.
Although the two clusters constitute a diverse set of literature and themes, it is apparent that research taking an ecosystem perspective is very rarely represented. Across the papers, only three are concerned with issues related to the ecosystem level. In particular, Lebcir et al. ( 2008 ) applied computer simulations in a theoretical demonstration as a decision support system for policy and decision-makers in the healthcare ecosystem. Abouzahra and Tan ( 2014 ) used a mixed-methods approach to demonstrate a model that supports clinical health management. Findikoglu and Watson-Manheim ( 2016 ) addressed the consequences of the implementation of electronic health records (EHR) systems in developing countries.
Phase 5: Evaluation
The fifth phase includes 92 publications with a focus on assessing existing or newly introduced HIS artefacts – i.e., concepts, policies, applications, and programs – thereby proving their innovativeness, effectiveness, or user acceptance. As Table 5 shows, three clusters were identified.
HIS publications assigned to the evaluation phase
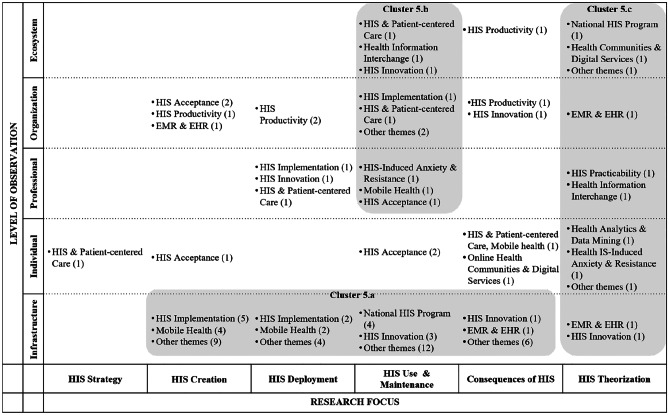
The main focus of publications in the evaluation phase is on the infrastructure level, where most papers are related to HIS creation and HIS use and maintenance. Therefore, together with the publications pigeonholed to HIS deployment and consequences of HIS, these articles were summarized as the first cluster (5a, comprising 53 articles). The assessment of national HIS programs, as well as mobile health solutions, are a frequent focus (10 papers). Articles on HIS use and maintenance are largely related to the professional, organizational, and ecosystem levels and were thus grouped as cluster 5b (10 articles). A third cluster (5c – 11 articles) emerged from research articles in HIS theorization. Here, papers at all levels of observation were found. Research focusing on areas such as HIS strategy and consequences of HIS are, with a few exceptions, not covered in the evaluation phase. Methods used include interviews, focus groups, and observations (e.g., Romanow et al., 2018 ). Experiments and simulation are rarely applied (e.g., Mun & Lee, 2017 ). The number of interviews shows a huge spread, starting with 12 and reaching a maximum of 150 persons interviewed.
Under the evaluation lens, the ecosystem perspective is covered by seven articles, but only three papers look at cases, while the others focus on theorization or consequences in terms of costs. Overall, popular topics in the evaluation phase include mobile health and the fields of electronic medical records (EMR) and EHR, e.g., Huerta et al. ( 2013 ); Kim and Kwon ( 2019 ). The authors cover these themes mostly from an HIS creation perspective; thus, they deal with concrete concepts, prototypes, or even implemented systems. In the evaluation phase, just nine papers deal with HIS innovation – a good example being Bullinger et al. ( 2012 ), who investigated the adoption of open health platforms. We may conclude that, in most cases, evaluation is related to more established technologies of HIS. As expected, most articles in this phase rely on practice-oriented/empirical work (as opposed to theory-driven/conceptual work). Just two papers (Ghanvatkar & Rajan, 2019 ; Lin et al., 2017 ) deal with health analytics and data mining, one of the emerging topics of HIS.
Zooming out: key findings of the literature analysis across phases
Having elaborated on the key findings within each phase of HIS research, we now ‘zoom out’ (Benbya et al., 2020 ; Gaskin et al., 2014 ) to recognize the bigger picture. Thereby, we ‘black-box’ the concrete research themes (e.g., HIS implementation, health analytics, HIS innovation) to focus on clusters across phases, highlighting the breadth that HIS research encompasses (Leroy et al., 2013 ). In particular, while we focused on analysing the main topics within the different phases of HIS research in the zoom-in section, we now abstract from those to perform a comparative analysis of emerging clusters across those phases by zooming out. We do so by comparing the different clusters, taking into account the aspects of the level of observation and the research foci, which gave us the opportunity to identify areas of strong emphasis and potential gaps.
In particular, each author first conducted this comparative analysis on their own and then discussed and identified the potential weaknesses together. This was done in two rounds of discussion. In particular, it became obvious which areas hold immense potential for further research in healthcare (especially the penetration of new, initially non-healthcare actors, such as tech companies or other providers pushing into the industry). We summarize these potentials for research by proposing four pathways that can help HIS research to broaden its focus so that we can better understand and contribute to current developments. Notably, we expect that these insights will help to assess the state-of-the-art of HIS research and its preparedness for dealing with the consequences of Covid-19 and further pandemics, as well as for coping with associated exogenous shocks.
In zooming out, we identified discrepancies between phase 1 (problem identification and research issues) and the subsequent phases. In particular, the diversity of topics was considerably lower when it came to how researchers determined strategies; created, demonstrated, used, and maintained HISs; and coped with the consequences thereof. We observed that researchers pointed to a diverse set of issues that span all levels of observation, especially in HIS theorization, focusing on topics such as trust in HIS, data analytics, and problems associated with the carrying out of national health programs. Surprisingly, although we can assume that researchers recognized the multidimensionality of issues as a motivation to conduct HIS research, they did not seem to approach HIS research issues in a comprehensive and consistent way.
To illustrate this assertion, we point to the ‘shift of clusters’ that can be observed when comparing the single phases, from problem identification to the evaluation of HIS. We note that clusters increasingly migrate ‘downwards’ (i.e., from the ecosystem level down to the infrastructure level) and become even fewer. In line with Braa et al. ( 2004 ), we suggest that extant HIS research has identified a multitude of interrelated issues but has faced problems in translating these approaches into concrete and holistic solutions. This is reflected in the lower number of, and reduced diversity in, clusters across research themes when we move through the HIS research phases. Thus, we conclude that future HIS research can be broadened by taking into account the following pathway:
HIS research is well-prepared and able to identify and theorize on systemic problems related to the healthcare industry. Nonetheless, it has the potential to address these problems more thoroughly – i.e., to find solutions that are as diverse as the problems and, thus, suitable for coping with issues in the healthcare industry characterized by the involvement of multiple actors, such as governments, healthcare providers, tech companies, and their interactions in diverse ecosystems (pathway 1).
As we have seen, HIS research has tended to focus on important but incremental improvements to existing infrastructures, particularly in the phases of demonstration and evaluation, with the aim of presenting new IS artefacts and conceptual or practical solutions. For instance, Choi and Tulu ( 2017 ) considered improvements in user interfaces to decrease the complexity of mobile health applications using incremental interface design changes and altering touch techniques. Similarly, Roehrig and Knorr ( 2000 ) designed patient-centred access controls that can be implemented in existing infrastructures to increase the privacy and security of EHRs and avoid malicious access and misuse of patient health information by third parties.
While we sincerely acknowledge these contributions and wish to emphasize the multitude of papers that are concerned with enhancements to existing infrastructures, we would like to shift the view to the major challenges in HIS research. These challenges include combating global and fast-spreading diseases (e.g., malaria, tuberculosis, Covid-19) and tracking health statuses accurately and efficiently, especially in developing countries. All of these challenges necessitate global and comprehensive solutions, spanning individuals, organizations, and nations, and have to be embedded in a global ecosystem (Winter & Butler, 2011 ). Such grand challenges are, by nature, not easy to cope with, and the intention to develop a comprehensive solution from the perspective of IS researchers seems almost misguided. However, HIS research is currently missing the opportunity to make an impact, despite the discipline’s natural intersection with essential aspects of the healthcare industry (i.e., its infrastructures, technologies, and stakeholders, and the interdependencies between these components). Thus, we assert that:
HIS research has often focused on necessary and incremental improvements to existing IS artefacts and infrastructures. We see potential in shifting this focus to developing solutions that combine existing IS artefacts to allow for exchange of information and the creation of open systems, which will enhance support for and understanding of the emergence of ecosystems (pathway 2).
By focusing on incremental improvements, HIS research has become extraordinarily successful in solving isolated issues, especially in relation to the problems of patients and health service providers (e.g., hospitals and general practitioners). However, we observed during our analysis that spillover effects were seldom investigated. When, for example, a new decision support system in a hospital was introduced, positive consequences for patients, such as more accurate diagnoses, were rarely of interest to the research. In fact, our meta-analysis revealed that the level of observation for the majority of papers matched the level of analysed effects. While it is valid to investigate productivity and efficiency gains by introducing a hospital-wide decision support system, we are convinced that spillover effects (for instance, on patients) should also be within the focus of HIS research. Therein, we suggest that HIS research has not focused primarily on patients and their well-being but on IS infrastructures and artefacts. However, patient well-being is the ultimate direct (or indirect) goal of any HIS research (by increasing the accuracy and shortening the time of diagnosis, improving treatment success rates, etc.). Thus, we propose that:
HIS research is experienced in solving isolated issues related to the daily processes of healthcare providers; however, we see much potential in considering the value that is delivered by focusing on patient-centricity (pathway 3).
Putting the patient at the centre of HIS research implies shifting the focus of researchers to the patient’s own processes. The question remains as to how HIS researchers can support patient-centricity. While this is only possible by understanding patients’ processes, we also see the need to understand the whole system – i.e., the ecosystem in which patients’ processes are embedded. The ecosystem perspective needs to consider networked services and organizations, including resources and how they interact with stakeholders of the healthcare industry (including patients). To date, we observe, across phases the ecosystem perspective has largely been neglected. To be precise, although HIS research seems to be aware of the multilevel aspects of healthcare issues in the problem identification phase, researchers appear to stop or are hindered from developing solutions that go beyond the development of prototypes (Braa et al., 2004 ). Thus, we find that:
HIS research is capable of theorizing on an ecosystem level (i.e., capturing the complexity of the socio-technical health system), but would benefit from increasing the transfer of these insights into research so as to develop holistic solutions (pathway 4).
Looking at the strengths of HIS research, the reviewed papers accentuate the unique contribution that IS researchers can make to better understand and design IS artefacts for the healthcare context. This has been achieved by analysing empirical data and exploring contextual influences through the application and elaboration of IS theories (LeRouge et al., 2007 ). At the same time, our literature review shows the incredible diversity and high level of complexity of issues related to HISs, indicating that we need solutions characterized by holism and the inclusion of multiple actors (i.e., an integrative ecosystem perspective). So far, by concentrating on incremental improvements to existing infrastructures HIS research has widely failed to reach the necessary holistic level.
We would like to emphasize that we recognize the value of all previous approaches. Yet, it is necessary to ask whether we as IS researchers are in a position to identify current developments in the healthcare industry and to anticipate the consequences triggered by pandemics or other waves of disease. We acknowledge that this will be difficult unless we take a more holistic view and try to understand connections in the health ecosystems. Regarding whether HIS research is in a position to capture and anticipate consequences of the current push of tech companies in the healthcare industry catalysed, for example, by Covid-19, we assert that this is hardly the case, even if IS research is well-placed to interpret the expected socio-technical changes and adaptations within healthcare. Given the enormous potential for disruption caused by, for instance, pandemics and its consequences, such as the intrusion of technology companies into the market, it is now time to question and redefine the role of HIS research so that it can generate decisive impacts on the developments in this industry.
Research agenda
To support HIS research for the transformation of the healthcare industry, we develop a research agenda that is informed by complexity theory. This theory implies that complex, socio-technical systems such as the healthcare industry can fluctuate between different states, ranging from homogenous forms of coevolution (i.e., a state where emergent structures and processes become similar to each other) to chaotic systems that are characterized by increasing levels of tension, which might result in extreme outcomes such as catastrophes or crises (Benbya et al., 2020 ).
While coevolution and chaos represent possible extreme states, the current situation – i.e., the penetration of tech companies into the healthcare industry – is best described by the dynamic process of emergence. Emergence is characterized by a disequilibrium, which implies unpredictability of outcomes that may lead to new structures, patterns, and properties within a system characterized by self-organization and bursts of amplification (Benbya et al., 2020 ; Kozlowski et al., 2013 ). Given the dynamics resulting from this, it seems impossible to predict the future; however, it is not impossible to prepare for it.
In particular, the current dynamics within the healthcare industry necessitate an understanding of exponential progress, not as the ability to foresee well-defined events in space and time, but as an anticipation of the consequences of emerging states and dynamic adaptive behaviours within the industry (Benbya et al., 2020 ). The following research agenda for HIS research is thus structured along three key issues: anticipating the range of actors’ behaviours, determining boundaries and fostering collaboration in the healthcare industry, and creating sustainable knowledge ecosystems.
According to these key issues, Table 6 offers guiding questions for HIS researchers. Addressing all issues will contribute to an understanding of the entire healthcare industry and the development of holistic solutions for a multitude of health issues by involving different actors (e.g., patients, hospitals, professionals, governments, NGOs). However, we propose approaching the agenda stepwise, in the order of the key issues, first looking at the range of behaviours and consequences of current developments for actors, then focusing on the blurring lines of the healthcare industry, and finally investigating the dissemination and sharing of knowledge, which we see as the ultimate means to connect actors and infrastructures to create a joint ecosystem. Table 6 thereby provides key guiding statements and exemplary research questions for future HIS research that support researchers in taking one of the aforementioned pathways. We structured guiding statements along three major areas of improvement. In addition, we offer exemplary research questions to these statements, as well as inspiring studies from other industries that have faced similar challenges and have been studied and supported by researchers.
Agenda for a comprehensive research approach for future HIS-research
Area of improvement 1: Anticipating the range of actor behaviours
As healthcare systems are becoming more open – for example, through the penetration of new market actors and the use of increasingly comprehensive and advanced health technologies – accurately determining the boundaries of an industry and its key actors is becoming more difficult. To model these systems, we must carefully model every interaction in them (Benbya et al., 2020 ), which first requires HIS researchers to identify potential actors in the ecosystem rather than predetermining assumed industry boundaries. As actors are not always evident, we follow Benbya et al. ( 2020 ) in proposing Salthe’s ( 1985 ) three-level specification, assisting researchers in identifying actors at the focal level of what is actually observed (e.g., hospitals, patients, and general practitioners) and its relations with the parts described at the lower level (e.g., administrators and legal professionals), taking into account entities or processes at a higher level in which actors at the focal level are embedded (e.g., national health system structures and supporting industries, such as the pharmaceutical or tech industries). These examples are only illustrative, and criteria for levels have to be suggested and discussed for each research endeavour.
To anticipate future developments in the healthcare industry, we also need to analyse the strategies and interests of actors for joining or staying in the healthcare industry. This is especially important because, like other complex socio-technical systems, the healthcare industry is made up of large numbers of actors that influence each other in nonlinear ways, continually adapting to internal or external tensions (Holland et al., 1996 ). If tension rises above a certain threshold, we might expect chaos or extreme outcomes. As these are not beneficial for the actors in the system, the eventual goal is to align actors’ interests and strategies across a specific range of behaviour to foster coevolution. This allows for multi-layered ecosystems that encourage joint business strategies in competitive landscapes, as well as the alignment of business processes and IT across actors (Lee et al., 2013 ).
Area of improvement 2: Determining boundaries and fostering collaboration
Actors build the cornerstones of the healthcare industry. Thus, if we want to understand and capture its blurring boundaries, there is a need to understand the complex causality of interactions among heterogeneous actors. In particular, scholars have emphasized that, in complex systems, outcomes rarely have a single cause but rather result from the interdependence of multiple conditions, implying that there exist multiple pathways from an input to an output (Benbya et al., 2020 ). To capture interaction, we follow Kozlowski et al. ( 2013 ), who envisioned a positive feedback process including bottom-up dynamic interaction among lower-level actors (upward causation), which over time manifests at higher, collective levels, while higher-level actors influence interaction at lower levels (downward causation). As these kinds of causalities shape interaction within healthcare ecosystems as well as at their boundaries, HIS researchers need to account for multi-directional causality in the form of upward, downward, and circular causality (Benbya et al., 2020 ; Kim, 1992 ).
Understanding casualties among actors in the healthcare industry is important for harnessing the advantages of the blurring of boundaries – e.g., by making use of the emergent ecosystem for launching innovation cycles (Hacklin, 2008 ). However, first, HIS researchers increasingly need to consider the ecosystem perspective by investigating interactions among actors and the role of IS infrastructures in fostering collaborative health innovations. We propose a focus on radical innovation, which is necessary to address the diversity and interdependence of issues present in the healthcare industry by putting the patient at the core of all innovation efforts. HIS researchers, however, need to break down the boundaries between different innovation phases and innovation agencies, including a higher level of unpredictability and overlap in their time horizons (Nambisan et al., 2017 ). Notably, this requires actors in the healthcare industry to discover new meaning around advanced technologies and IS infrastructures whose design needs to facilitate shared meaning among a diverse set of actors, thereby fuelling radical digital innovations (Nambisan et al., 2017 ).
Area of improvement 3: Creating sustainable knowledge ecosystems
We define knowledge dissemination and sharing as the ultimate means of connecting actors and aligning actions within common frameworks to shape an inclusive healthcare ecosystem. Paving the way for inclusive healthcare ecosystems is thus necessary to address the current shortcomings of HIS research as elaborated in the previous section.
Addressing knowledge dissemination and sharing is thereby of the utmost importance as we look at the healthcare industry in the current phase of emergence. This means that the industry might go through several transition phases in which existing actors, structures, and causal relationships dissipate and new ones emerge, resulting in a different set of causal relationships and eventually altering knowledge claims (Benbya et al., 2020 ). Creating a permeable and sustainable knowledge management system is necessary to ensure the transfer of knowledge for the best outcomes for the patient while securing the intellectual property rights and competitive advantages of diverse actors such as hospitals and other healthcare providers.
To be precise, we argue that to design sustainable knowledge management systems, HIS researchers need to implement systems with structures that create mutual benefits – i.e., encourage knowledge dissemination and sharing (e.g., open innovation) by actors in the healthcare industry. In a comprehensive and sustainable knowledge management system, however, not only corporations but also patients should be encouraged to share knowledge. Using this information, researchers and health service providers will be enabled to create optimized infrastructures, processes, and products (e.g., for predictive algorithms that improve treatment accuracy, or for assessing the likelihood of the occurrence of certain diseases and even of pandemics). At the same time, the trustworthiness of predictions and the anonymity of health information (and thus privacy) must be ensured. Bridging this duality of data sharing and knowledge dissemination, on the one hand, and protection of health information, on the other, is therefore essential for future HIS research.
This paper analyses the HIS literature within the IS research domain, prompted by the question of whether IS researchers are prepared to capture and anticipate exogenous changes and the consequences of current developments in the healthcare industry. While this review is limited to insights into the IS research domain and does not claim to offer insights into the health literature in general or related publications (e.g., governmental publications), we disclose several shortcomings and three key issues. Based on these, we provide initial guidance on how IS research can develop so that it is prepared to capture the expected large and long-lasting changes from current and possible future pandemics as well as the necessary adaptation of global healthcare industries affecting human agencies and experiences in all dimensions. Thus, while adaptations in the healthcare industry are already emerging, IS researchers have yet to develop a more comprehensive view of the healthcare industry. For this purpose, we provide a research agenda that is structured in terms of three areas of improvement: anticipating the range of actors’ behaviours, determining boundaries and fostering collaborations among actors in the healthcare industry, and creating sustainable knowledge management systems. In particular, addressing these areas will assist IS researchers in balancing the shortcomings of current HIS research with the unique contribution that IS research plays in analysing, advancing, and managing the healthcare industry. We are confident that IS research is not only capable of anticipating changes and consequences but also of actively shaping the future of the healthcare industry by promoting sustainable healthcare ecosystems, cultivating structures of mutual benefit and cooperation between actors, and realigning IS research to face the imminent transformation of the healthcare industry. IS research cannot contribute directly to solving the current pandemic problems; however, it can contribute indirectly triggering timely adaptations of novel technologies in global health systems, and proposing new processes, business models, and systematic changes that will prepare health systems to cope with increasing digitalization and emerging players whose push into the market enabled by the exogenous effects triggered by the pandemic.
While we are confident that the proposed research agenda based on the analysis of HIS literature provides fruitful arrays for being prepared in anticipating the future role of IS research for the healthcare industry, our results need to be reflected in light of their shortcomings. First and foremost, we recognize that the selection of literature, which is limited to the IS research domain, excludes other contextual factors that are not primarily considered by IS researchers. Thus, we cannot assume completeness, providing instead a broad overview of current issues in HIS research. In addition, possible biases may have arisen due to the qualitative analysis approach used. By independently coding and discussing codes to the point of theoretical saturation, we are confident that we largely eliminated biases in the thematic analysis. However, data saturation could not be achieved. This means that further insights could have emerged through the addition of other database searches and journals with a broader scope. Additionally, the initial sorting of papers into single defined phases of DSR research restricted multiple assignments that could have led to different results. However, we consider sorting as a necessary step of abstraction, especially given the large number of papers analysed.
We deliberately considered IS research, for which we have developed an agenda for potential future research avenues. For each of those avenues, researchers should go deeper into the subject matter in order to examine the complexity of the paths shown and to include them in the analysis (e.g., through in-depth case studies). However, it is also clear from the issues identified that IS researchers cannot solve current challenges by working on the pathways alone. In fact, the issues identified in the research agenda are only the starting point for further research, which should address the proposed issues step by step and in cooperation with other research disciplines. The latter is likely to generate further and deeper-rooted problems, as well as, in turn, future paths for research. Nevertheless, we are confident that this paper provides an important first step in opening up HIS research to better understand current developments in the healthcare industry. Further, by following and enhancing the proposed research pathways, we believe that HIS research can contribute to and support changes already taking place in the healthcare industry.
Below is the link to the electronic supplementary material.
Open Access funding enabled and organized by Projekt DEAL.
The original online version of this article was revised: In this article the affiliation of authors are incorrect. Given here are the correct affiliations.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
A Correction to this paper has been published: 10.1007/s12525-021-00518-8
Contributor Information
Nadine Ostern, Email: [email protected].
Guido Perscheid, Email: [email protected].
Caroline Reelitz, Email: [email protected].
Jürgen Moormann, Email: [email protected].
- Aanestad M, Vassilakopoulou P, Ovrelid E. Collaborative Innovation in Healthcare: Boundary Resources for Peripheral Actors. International Conference on INformation Systems. 2019;1:1–17. [ Google Scholar ]
- Abouzahra, M., & Tan, J. (2014). The multi-level impact of clinical decision support system: a framework and a call for mixed methods. Pacific Asia Conference on Information Systems (PACIS), 1–17.
- Agarwal R, Gao G, DesRoches C, Jha AK. Digital Transformation of Healthcare: Current Status and the Road Ahead. Information Systems Research. 2010;21(4):796–809. doi: 10.1287/isre.1100.0327. [ DOI ] [ Google Scholar ]
- Akcura, M. T., & Ozdemir, Z. D. (2008). Physician learning and clinical decision support systems. Americas Conference on Information Systems (AMCIS) , 1–10.
- Akkerman SF, Bakker A. Boundary crossing and boundary objects. Review of Educational Research. 2011;81(2):132–169. doi: 10.3102/0034654311404435. [ DOI ] [ Google Scholar ]
- Al-Qirim, N. (2003). Championing telemedicine in New Zealand: the case of utilizing video conferencing in psychiatry and dermatology. Americas Conference on Information Systems (AMCIS), 1–10.
- Arvanitis, S., & Loukis, E. (2014). An empirical investigation of the impact of ICT on innovation in European hospitals. European Conference on Information Systems (ECIS), 1–13.
- Babar, Y., Chan, J., & Choi, B. (2018). "Run Forrest Run!": measuring the impact of app-enabled performance and social feedback on running performance. Pacific Asia Conference on Information Systems (PACIS 2018), 160.
- Benbya, H., Nan, N., Tandriverdi, H., & Yoo, Y. (2020). Complexity and information systems research in the emerging digital world. MIS Quarterly , 44 (1), 1–17. 10.25300/MISQ/2020/13304
- Bhandari, G., & Maheshwari, B. (2009). Toward an integrated health information system for collaborative decision making and resource sharing: findings from a Canadian study. Americas Conference on Information Systems (AMCIS), 648.
- Bleicher J. Contemporary Hermeneutics: Hermeneutics as method, philosophy, and critique. 2. Routledge; 2017. [ Google Scholar ]
- Blinn N, Kühne M. Health Information on the Internet - State of the Art and Analysis. Business & Information Systems Engineering. 2013;5(4):259–274. doi: 10.1007/s12599-013-0274-4. [ DOI ] [ Google Scholar ]
- Boell S, Cecez-Kecmanovic D. A Hermeneutic Approach for Conducting Literature Reviews and Literature Searches. Communication of the Association for Information Systems. 2014;34(12):257–286. [ Google Scholar ]
- Braa J, Monteiro E, Sahay S. Networks of action: Sustainable health information systems across developing countries. MIS Quarterly. 2004;28(3):337–362. doi: 10.2307/25148643. [ DOI ] [ Google Scholar ]
- Bullinger, A., Rass, M., & Moeslein, K. (2012). Towards open innovation in health care. European Conference on Information Systems (ECIS), 1–13.
- Byrd, L., & Byrd, T. (2009). Examining the effects of healthcare technology on operational cost. Americas Conference on Information Systems (AMCIS), 1–10.
- CB Insights. (2018). How Google Plans to Use AI to Reinvent the $3 Trillion US Healthcare Industry . https://www.distilnfo.com/lifesciences/files/2018/11/CB-Insights_Google-Strategy-Healthcare.pdf
- Chang IC, Hwang HG, Hung MC, Kuo KM, Yen DC. Factors affecting cross-hospital exchange of electronic medical records. Information & Management. 2009;46(2):109–115. doi: 10.1016/j.im.2008.12.004. [ DOI ] [ Google Scholar ]
- Chen, L., Baird, A., & Straub, D. (2019). An analysis of the evolving intellectual structure of health information systems research in the information systems discipline. Journal of the Association for Information Systems , 20 (8), 1023–1074. 10.17705/1jais.00561
- Chiasson MW, Davidson E. Pushing the contextual envelope: Developing and diffusing IS theory for health information systems research. Information and Organization. 2004;14(3):155–188. doi: 10.1016/j.infoandorg.2004.02.001. [ DOI ] [ Google Scholar ]
- Choi, W., & Tulu, B. (2017). Effective use of user interfaces and user experience in an mHealth application. Hawaii International Conference on System Sciences (HICSS), 3803–3812. 10.24251/HICSS.2017.460
- Cole M, Avison D. The potential of hermeneutics in information systems research. European Journal of Information Systems. 2007;16(6):820–833. doi: 10.1057/palgrave.ejis.3000725. [ DOI ] [ Google Scholar ]
- Cilliers P. Boundaries, Hierarchies and Networks in Complex Systems. International Journal of Innovation Management. 2001;5(2):135–147. doi: 10.1515/9781501502590-009. [ DOI ] [ Google Scholar ]
- Corbin JM, Strauss A. Grounded theory research: Procedures, canons, and evaluative criteria. Qualitative Sociology. 1990;13(1):3–21. doi: 10.1007/BF00988593. [ DOI ] [ Google Scholar ]
- Currie WL, Seddon JJ. A cross-national analysis of eHealth in the European Union: Some policy and research directions. Information & Management. 2014;51(6):783–797. doi: 10.1016/j.im.2014.04.004. [ DOI ] [ Google Scholar ]
- Dehling, T., & Sunyaev, A. (2012). Architecture and design of a patient-friendly eHealth web application: patient information leaflets and supplementary services. Americas Conference on Information Systems (AMCIS), 1–8.
- Devadoss, P., & Pan, S. L. (2004). Leveraging eGovernment infrastructure for crisis management: lessons from managing SARS outbreak in Singapore. Americas Conference on Information Systems (AMCIS), 1–10.
- Djamsbi S, Fruhling A, Loiacono E. The Influence of Affect, Attitude and Usefulness in the Acceptance of Telemedicine Systems. Journal of Information Technology Theory and Application. 2009;10(1):1–38. [ Google Scholar ]
- Dünnebeil S, Krcmar H, Sunyaev A, Leimeister J, M. Modular Architecture of Value-Added Applications for German Healthcare Telematics. Business & Information Systems Engineering. 2013;5:3–16. doi: 10.1007/s12599-012-0243-3. [ DOI ] [ Google Scholar ]
- Enkel E, Gassmann O. Creative imitation: Exploring the case of cross-industry innovation. R&d Management. 2010;40(3):256–270. doi: 10.1111/j.1467-9310.2010.00591.x. [ DOI ] [ Google Scholar ]
- Fichman RG, Kohli R, Krishnan R. The Role of Information Systems in Healthcare: Current Research and Future Trends. Information Systems Research. 2011;22(3):419–428. doi: 10.2307/23015587. [ DOI ] [ Google Scholar ]
- Findikoglu M, Watson-Manheim MB. Linking macro-level goals to micro-level routines: EHR-enabled transformation of primary care services. Journal of Information Technology. 2016;31(4):382–400. doi: 10.1057/s41265-016-0023-5. [ DOI ] [ Google Scholar ]
- Fisher, J., Burstein, F., Lynch, K., Lazarenko, K., & McKemmish, S. (2007). Health information websites: is the health consumer being well-served? Americas Conference on Information Systems (AMCIS), 1–10.
- Fisman, R., Branstetter, L. G., & Foley, C. F. (2004). Do stronger intellectual property rights increase international technology transfer? Empirical evidence from US firm-level panel data . The World Bank, Washington, DC. 10.1596/1813-9450-3305
- Gabel, M., Foege, J. N., & Nuesch, S. (2019). The (In)Effectiveness of incentives - a field experiment on the adoption of personal electronic health records. International Conference on Information Systems (ICIS), 1–17.
- Gantori, S., Issel, H., Donovan, P., Rose, B., Kane, L., Dennean, K., Ganter R., Sariyska, A., Wayne, G., Hyde, C., & Lee, A. (2020). Future of the Tech Economy . https://www.ubs.com/global/en/wealth-management/chief-investment-office/investment-opportunities/investing-in-the-future/2020/future-of-tech-economy.html
- Gaskin, J., Berente, N., Lyytinen, K., & Yoo, Y. (2014). Toward generalizable sociomaterial inquiry. MIS Quarterly , 38 (3), 849–872. 10.25300/MISQ/2014/38.3.10
- George, J. F., & Kohnke, E. (2018). Personal health record systems as boundary objects. Communication of the Association for Information Systems , 42 (1), 21–50. 10.17705/1CAIS.04202
- Ghanvatkar, S., & Rajan, V. (2019). Deep recurrent neural networks for mortality prediction in intensive care using clinical time series at multiple resolution. International Conference on Information Systems (ICIS), 1–18.
- Gimpel, H., Nißen, M., & Görlitz, R. A. (2013). Quantifying the quantified self: a study on the motivation of patients to track their own health. International Conference on Information Systems (ICIS), 1–17.
- Glaser BG, Strauss AL, Strutzel E. The discovery of grounded theory; strategies for qualitative research. Nursing Research. 1968;17(4):364. doi: 10.1097/00006199-196807000-00014. [ DOI ] [ Google Scholar ]
- Greenwood, F. (2020, March). Google Want Your Data in Exchange for a Coronavirus Test. Foreign Policy. https://foreignpolicy.com/2020/03/30/google-personal-health-data-coronavirus-test-privacy-surveillance-silicon-valley/
- Grondin, J. (2016). What is the hermeneutical cycle? In N. Keane & C. Lawn (Eds.), The Blackwell Companion to Hermeneutics, 299–305. Oxford, UK: Blackwell Publishing.
- Hacklin, F. (2008). Management of Convergence in Innovation: Strategies and Capabilities for Value Creation Beyond Blurring Industry Boundaries . Zurich, Switzerland: Physica.
- Hafermalz, E., & Riemer, K. (2016). Negotiating distance: "presencing work” in a case of remote telenursing. International Conference on Information Systems(ICIS), 1–13.
- Hamari J, Koivisto J. Why do people use gamification services? International Journal of Information Management. 2015;35(4):419–431. doi: 10.1016/j.ijinfomgt.2015.04.006. [ DOI ] [ Google Scholar ]
- Heine, C., Herrler, R., Petsch, M., & Anhalt, C. (2003). ADAPT: Adaptive Multi-Agent Process Planning and Coordination of Clinical Trials. Americas Conference on Information Systems (AMCIS), 1823–1834.
- Holland S, Phimphachanh C, Conn C, Segall M. Impact of economic and institutional reforms on the health sector in Laos: Implications for health system management. IDS Publications, Institute of Development Studies. 1996;28:133–154. [ Google Scholar ]
- Huerta TR, Thompson MA, Ford EW, Ford WF. Electronic health record implementation and hospitals' total factor productivity. Decision Support Systems. 2013;55(2):450–458. doi: 10.1016/j.dss.2012.10.004. [ DOI ] [ Google Scholar ]
- Humphrey SE. What does great meta-analysis look like? Organizational Psychology Review. 2011;1(2):99–103. doi: 10.1177/2041386611401273. [ DOI ] [ Google Scholar ]
- Idrissi TE, Idri A, Bakkoury Z. Systematic map and review of predictive techniques in diabetes self-management. International Journal of Information Management. 2019;46:263–277. doi: 10.1016/j.ijinfomgt.2018.09.011. [ DOI ] [ Google Scholar ]
- Kenny, C., & Connolly, R. (2016). Drivers of health information privacy concern: a comparison study. Americas Conference on Information Systems (AMCIS), 1–10.
- Kernick D, Mitchell A. Working with lay people in health service research: A model of co-evolution based on complexity theory. Journal of Interprofessional Care. 2009;24(1):31–40. doi: 10.3109/13561820903012073. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kim SH, Kwon J. How Do EHRs and a Meaningful Use Initiative Affect Breaches of Patient Information? Information Systems Research. 2019;30(4):1107–1452. doi: 10.1287/isre.2019.0858. [ DOI ] [ Google Scholar ]
- Kim, S. (1992). Downward causation in emergentism and non-reductive physicalism. In A. Beckermann, H. Flohr, & J. Kim (Eds.). Emergence or Reduction. Essays on the Prospects of Nonreductive Physicalism (118–138). Berlin, Germany: de Gryuter.
- King, N. (2009). An initial exploration of stakeholder benefit dependencies in ambulatory ePrescribing. Americas Conference on Information Systems (AMCIS), 1–10.
- Klecun E, Zhou Y, Kankanhalli A, Wee YH, Hibberd R. The dynamics of institutional pressures and stakeholder behavior in national electronic health record implementations: A tale of two countries. Journal of Information Technology. 2019;34(4):292–332. doi: 10.1177/0268396218822478. [ DOI ] [ Google Scholar ]
- Knight, J., Patrickson, M., & Gurd, B. (2008). Towards understanding apparent South Australian GP resistance to adopting Health Informatics systems. Australasian Conference on Information Systems (ACIS), 492–501.
- Kozlowski SWJ, Chao GT, Grand JA, Braun MT, Kulijanin G. Advancing Multilevel Research Design: Capturing the Dynamics of Emergence. Organizational Research Methods. 2013;16(4):581–615. doi: 10.1177/1094428113493119. [ DOI ] [ Google Scholar ]
- Landi, H. (2020, April). Alphabet’s Verily rolls out COVID screening tool for health systems . FierceHealthcare. https://www.fiercehealthcare.com/tech/alphabet-s-verily-rolls-out-covid-screening-tool-for-health-systems
- Lebcir, R. M., Choudrie, J., Atum, R. A., & Corker, R. J. (2008). Examining HIV and tuberculosis using a decision support systems computer simulation model: the case of the Russian Federation. Americas Conference on Information Systems (AMCIS), 1–18.
- Lee, D., & Nilsson, P. (2020, March). Amazon auditions to be “the new Red Cross” in Covid-19 crisis . Financial Times. https://www.ft.com/content/220bf850-726c-11ea-ad98-044200cb277f
- Lee AS, Thomas M, Baskerville RL. Going back to basics in design science: From the information technology artifact to the information systems artifact. Information Systems Journal. 2015;25(1):5–21. doi: 10.1111/isj.12054. [ DOI ] [ Google Scholar ]
- Lee CH, Venkatraman N, Tanriverdi H, Iyer B. Complementary-based Hypercompetition in the Software Industry. Strategic Management Journal. 2013;31(13):1431–1356. doi: 10.1002/smj.895. [ DOI ] [ Google Scholar ]
- Leon MC, Nieto-Hipolito JI, Garibaldi-Beltran J, Amaya-Parra G, Luque-Morales P, Magana-Espinoza P, Aquilar-Velazco J. Designing a model of a digital ecosystem for healthcare and wellness using the BM canvas. Journal of Medical Systems. 2016;40(6):144–154. doi: 10.1007/s10916-016-0488-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- LeRouge C, Mantzana V, Wilson EV. Healthcare information systems research, revelations and visions. European Journal of Information Systems. 2007;16(6):669–671. doi: 10.1057/palgrave.ejis.3000712. [ DOI ] [ Google Scholar ]
- Leroy J, Cova B, Salle R. Zooming in VS zooming out on value co-creation: Consequences for BtoB research. Industrial Marketing Management. 2013;42(7):1102–1111. doi: 10.1016/j.indmarman.2013.07.006. [ DOI ] [ Google Scholar ]
- Li L, Jeng L, Naik HA, Allen T, Frontini M. Creation of environmental health information system for public health service: A pilot study. Information Systems Frontiers. 2008;10(5):531–542. doi: 10.1007/s10796-008-9108-1. [ DOI ] [ Google Scholar ]
- Lichtenberg, S., Greve, M., Brendel, A. B., & Kolbe, L. M. (2019). Towards the design of a mobile application to support decentralized healthcare in developing countries – The case of diabetes care in eSwatini. Americas Conference on Information Systems (AMCIS), 1–10.
- Lin, Y.-K., Chen, H., Brown, R. A., Li, S.-H., & Yang, H.-J. (2017). Healthcare predictive analytics for risk profiling in chronic care: a Bayesian multitask learning approach. MIS Quarterly , 41 (2), 473–495. 10.25300/MISQ/2017/41.2.07
- MacLure M. Clarity Bordering on Stupidity: Where’s the Quality in Systematic Review? Journal of Education Policy. 2005;20(4):393–416. doi: 10.4324/9780203609156. [ DOI ] [ Google Scholar ]
- Maheshwari, M., Hassan, T., & Chatterjee, S. (2006). A framework for designing healthy lifestyle management information system. Americas Conference on Information Systems (AMCIS), 2811–2817.
- Matavire, R., & Brown, I. (2008). Investigating the use of “Grounded Theory” in information systems research. Proceedings of the 2008 annual research conference of the South African Institute of Computer Scientists and Information Technologists on IT research in developing countries, 139–147. 10.1145/1456659.1456676
- Mitsa, T., Fortier, P. J., Shrestha, A., Yang, G., & Dluhy, N. M. (2007). Information systems and healthcare XXI: a dynamic, client-centric, point-of-care system for the novice nurse. Communication of the Association for Information Systems , 19 , 740–761. 10.17705/1CAIS.01936
- Motamarri, S., Akter, S., Ray, P., & Tseng, C.-L. (2014). Distinguishing “mHealth” from other healthcare services in a developing country: a study from the service quality perspective. Communication of the Association for Information Systems , 34 (1), 669–692. 10.17705/1CAIS.03434
- Mun, C., & Lee, O. (2017). Integrated supporting platform for the visually impaired: using smart devices. International Conference on Information Systems (ICIS), 1–18.
- Nambisan, S., Lyytinen, K., Majchrzak, A., & Song, M. (2017). Digital innovation management: reinventing innovation management research in a digital world. MIS Quarterly , 41 (1), 223–238. 10.25300/MISQ/2017/41:1.03
- Neben, T., Seeger, A. M., Kramer, T., Knigge, S., White, A. J., & Alpers, G. W. (2016). Make the most of waiting: theory-driven design of a pre-psychotherapy mobile health application. Americas Conference on Information Systems (AMCIS), 1–10.
- Nicholls-Nixon CL, Jasinski D. The blurring of industry boundaries: An explanatory model applied to telecommunications. Industrial and Corporate Change. 1995;4(4):755–768. doi: 10.1093/icc/4.4.755. [ DOI ] [ Google Scholar ]
- Offermann, P., Blom, S., Schönherr, M., & Bub, U. (2010). Artifact types in information systems design science – a literature review. International Conference on Design Science Research in Information Systems, 77–92. 10.1007/978-3-642-13335-0_6
- Palvia, P., Kakhki, M. D., Ghoshal, T., Uppala, V., & Wang, W. (2015). Methodological and topic trends in information systems research: a meta-analysis of IS journals. Communication of the Association for Information Systems , 37 (30), 630–650. 10.17705/1CAIS.03730
- Park, H. A. (2016). Are we ready for the fourth industrial revolution? Yearbook of Medical Informatics , (1), 1–3. 10.15265/IY-2016-052 [ DOI ] [ PMC free article ] [ PubMed ]
- Patel, M., Shah, A., Shah, K., & Plachkinova, M. (2018). Designing a mobile app to help young adults develop and maintain mental well-being. Americas Conference on Information Systems (AMCIS), 1–10.
- Paul LD, McDaniel RRJ. A Field Study of the Effect of Interpersonal Trust on Virtual Collaborative Relationship Performance. MIS Quarterly. 2004;28(2):183–227. doi: 10.2307/25148633. [ DOI ] [ Google Scholar ]
- Peffers K, Tuunanen T, Rothenberger MA, Chatterjee S. A Design Science Research Methodology for Information Systems Research. Journal of Management Information Systems. 2008;24(3):45–78. doi: 10.2753/MIS0742-1222240302. [ DOI ] [ Google Scholar ]
- Pletikosa, I., Kowatsch, T., Büchter, D., Brogle, B., Dintheer, A., Wiegand, D., Durrer, D., l'Allemand-Jander, D., Schutz, Y., Maass, W. (2014). Health information system for obesity prevention and treatment of children and adolescents. European Conference on Information Systems (ECIS), 1–13.
- Preko, M., Boateng, R., & Effah, J. (2019). Health informatics and brain drain mitigation in Ghana. Americas Conference on Information Systems (AMCIS), 1–10.
- Rivard, P. E., Rosen, A. K., & Carroll, J. S. (2006). Enhancing patient safety through organizational learning: are patient safety indicators a step in the right direction? Health Services Research , 41(4p2), 1633–1653. 10.1111/j.1475-6773.2006.00569.x [ DOI ] [ PMC free article ] [ PubMed ]
- Rodon J, Silva L. Exploring the Formation of a Healthcare Information Infrastructure: Hierarchy or Meshwork? Journal of the Association for Information System. 2015;16(5):394–417. doi: 10.17705/1JAIS.00395. [ DOI ] [ Google Scholar ]
- Roehrig, S., & Knorr, K. (2000). Toward a secure web based health care application. European Conference on Information Systems (ECIS), 1–8. 10.4018/978-1-930708-13-6.ch007
- Romanow, D., Rai, A., & Keil, M. (2018). CPOE-Enabled Coordination: appropriation for deep structure use and impacts on patient outcomes. MIS Quarterly , 42 (1), 189–212. 10.25300/MISQ/2018/13275
- Ryan, J., Doster, B., Daily, S., & Lewis, C. (2019). Seeking operational excellence via the digital transformation of perioperative scheduling. Americas Conference on Information Systems (AMCIS), 1–10.
- Rycroft RW, Kash DE. Self-organizing innovation networks: Implications for globalization. Technovation. 2004;24(3):187–197. doi: 10.1016/S0166-4972(03)00092-0. [ DOI ] [ Google Scholar ]
- Salthe SN. Evolving Hierarchical Systems. Columbia University Press; 1985. [ Google Scholar ]
- Samentinger J, Rozenblit J, Lysecky R, Ott P. Security Challenges for Medical Devices. Communications of the Association for Information Systems. 2015;58(4):74–82. [ Google Scholar ]
- Saunders B, Sim J, Kingstone T, Baker S, et al. Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity. 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schweiger, A., Sunyaev, A., Leimeister, J. M., & Krcmar, H. (2007). Information systems and healthcare XX: toward seamless healthcare with software agents. Communications of the Association for Information Systems , 19 (33), 392–710. 10.17705/1CAIS.01933
- Schwetschke S, Durugbo C. How firms synergise: Understanding motives and management of co-creation for business-to-business services. International Journal of Technology Management. 2018;76(3–4):258–284. doi: 10.1504/IJTM.2018.091289. [ DOI ] [ Google Scholar ]
- Setia, P., Setia, M., Krishnan, R., & Sambamurthy, V. (2011). The effects of the assimilation and use of IT applications on financial performance in healthcare organizations. Journal of the Association for Information System , 12 (Special Issue), 274–298. 10.17705/1jais.0060
- Shahmoradi L, Safadari R, Jimma W. Knowledge management implementation and the tools utilized in healthcare for evidence-based decision making: A systematic review. Ethiopian Journal of Health Sciences. 2017;27(5):541–558. doi: 10.4314/ejhs.v27i5.13. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sherer, S. A. (2014). Patients are not simply health it users or consumers: the case for “e Healthicant” applications. Communications of the Association for Information systems , 34(1), 17. 10.17705/1CAIS.03417.
- Singh, R., Mathiassen, L., Stachura, M. E., & Astapova, E. V. (2011). Dynamic capabilities in home health: IT-enabled transformation of post-acute care. Journal of the Association for Information System , 12 (2), 163–188. 10.17705/1jais.00257
- Sujanto, F., F., B., Ceglowski, A., & Churilov, L. (2008). Application of domain ontology for decision support in medical emergency coordination. Americas Conference on Information Systems (AMCIS), 1–10.
- Theobalt, A., Emrich, A., Werth, D., & Loos, P. (2013). A conceptual architecture for an ICT-based personal health system for cardiac rehabilitation. Americas Conference on Information Systems (AMCIS), 1–10.
- Therrien M-C, Normandin J-M, Denis J-L. Bridging complexity theory and resilience to develop surge capacity in health systems. Journal of Health Organisation and Management. 2017;31(1):96–109. doi: 10.1108/JHOM-04-2016-0067. [ DOI ] [ PubMed ] [ Google Scholar ]
- Tillett, A. (2020, April). Amazon to store data from virus tracing app. Financial Review. https://www.afr.com/politics/federal/amazon-to-store-data-from-virus-tracing-app-20200424-p54mwq
- Tokar, O., Batoroev, K., & Böhmann, T. (2015). A framework for analyzing patient-centered mobile applications for mental health. Americas Conference on Information Systems (AMCIS), 1–15.
- Tsai JM, Cheng MJ, Tsai HH, Hung SW, Chen YL. Acceptance and resistance of telehealth: The perspective of dual-factor concepts in technology adoption. International Journal of Information Management. 2019;49:34–44. doi: 10.1016/j.ijinfomgt.2019.03.003. [ DOI ] [ Google Scholar ]
- Ure, J., Procter, R., Lin, Y. W., Hartswood, M., Anderson, S., Lloyd, S., Wardlaw, J., Gonzalez-Velez, H., & Ho, K. (2009). The development of data infrastructures for eHealth: a socio-technical perspective. Journal of the Association for Information Systems , 10 (5), 415–429. 10.17705/1jais.00197
- Varshney, U. (2004). Using wireless networks for enhanced monitoring of patients. Americas Conference on Information Systems (AMCIS), 1–10. 10.1504/IJHTM.2005.007009
- Volland, D., Korak, K., & Kowatsch, T. (2014). A health information system that extends healthcare professional-patient communication. European Conference on Information Systems (ECIS), 1–10.
- vom Brocke J, Simons A, Reimer K, Niehaves B, Plattfaut R, Cleven A. Standing on the Shoulders of Giants: Challenges and Recommendations of Literature Search in Information Systems Research. Communications of the Association for Information Systems. 2015;37(1):205–224. [ Google Scholar ]
- vom Brocke, J., Simons, A., Niehaves, B., Reimer, K., Plattfaut, R., & Cleven, A. (2009): Reconstructing the giant: on the importance of rigour in documenting the literature search process. European Conference on Information Systems (ECIS) , 1–12.
- Walsh D, Downe S. Meta-synthesis method for qualitative research: A literature review, methodological issues in nursing. Journal of Advanced Nursing. 2005;50(2):204–211. doi: 10.1111/j.1365-2648.2005.03380.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Webster J, Watson RT. Analyzing the past to prepare for the future: Writing a literature review. MIS Quarterly. 2002;26(2):13–23. doi: 10.2307/4132319. [ DOI ] [ Google Scholar ]
- Werts, N., & Adya, M. (2000). Data mining in healthcare: issues and a research agenda. Americas Conference on Information Systems (AMCIS), 98.
- Wessel L, Gersch M, Harloff E. Talking Past Each Other - A Discursive Approach to the Formation of Societal-Level Information Pathologies in the Context of the Electronic Health Card in Germany. Business & Information Systems Engineering. 2017;59(1):23–40. doi: 10.1007/s12599-016-0462-0. [ DOI ] [ Google Scholar ]
- Winter SJ, Butler BS. Creating bigger problems: Grand challenges as boundary objects and the legitimacy of the information systems field. Journal of Information Technology. 2011;26(2):99–108. doi: 10.1057/jit.2011.6. [ DOI ] [ Google Scholar ]
- Wolfswinkel JF, Furtmueller E, Wilderom CPM. Using grounded theory as a method for rigorously reviewing literature. European Journal of Information Systems. 2013;22(1):45–55. doi: 10.1057/ejis.2011.51. [ DOI ] [ Google Scholar ]
- Malpass, D., (2020, March). Coronavirus highlights the need to strengthen health systems. Worldbank Blogs. https://blogs.worldbank.org/voices/coronavirus-covid19-highlights-need-strengthen-health-systems
- Wu, I.-L., & Hu, Y.-P. (2012). Examining knowledge management enabled performance for hospital professionals: a dynamic capability view and the mediating role of process capability. Journal of the Association for Information System , 13 (12), 976–999. 10.17705/1jais.00319
- Yang, A., & Varshney, U. (2016). A taxonomy for mobile health implementation and evaluation. Americas Conference on Information Systems (AMCIS), 1–10.
- Zafar, H., & Sneha, S. (2012). Ubiquitous healthcare information system: toward crossing the security chasm. Communication of the Association for Information Systems , 31 (9), 193–206. 10.17705/1CAIS.03109
- Zhang, L., & Pang, M. S. (2019). Does sharing make my data more insecure? An empirical study on health information exchange and data breaches. International Conference on Information Systems (ICIS), 1–14.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- PDF (3.1 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The Management Perspective in Digital Health Literature: Systematic Review
Alfred angerer , prof dr, johanna stahl , msc, egzona krasniqi , msc, stefan banning , msc.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: Alfred Angerer [email protected]
Corresponding author.
Contributed equally.
Received 2022 Feb 28; Revision requested 2022 Mar 30; Revised 2022 Oct 7; Accepted 2022 Oct 14; Collection date 2022 Nov.
This is an open-access article distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR mHealth and uHealth, is properly cited. The complete bibliographic information, a link to the original publication on https://mhealth.jmir.org/ , as well as this copyright and license information must be included.
New digital health technologies are considered one solution to challenges in the health sector, which include rising numbers of chronic diseases and increased health spending. As digitalization in health care is still in its infancy, there are many unanswered questions about the impact of digital health on management.
This paper assesses the current state of knowledge in the field of digital health from a management perspective. It highlights research gaps within this field to determine future research opportunities.
A systematic review of digital health literature was conducted using 3 databases. The chosen articles (N=38) were classified according to a taxonomy developed for the purpose, and research gaps were identified based on the topic areas discussed.
The literature review revealed a slight prevalence of practical (n=21, 55%) over theoretical (n=17, 45%) approaches. Most of the papers (n=23, 61%) deal with information technology (IT) and are, therefore, focused more on technology and less on management. The research question in most of the papers (n=31, 82%) deals with the creation of concepts, and very few (n=4, 11%) evaluate or even question existing solutions. Most consider the main reason for digitalization to be the optimization of operational processes (n=26, 68%), and 42% (n=16) deal with new business models. The topic area discussed most frequently was found to be eHealth (n=30, 79%). By contrast, the field of tech health with topics such as sensors receives the least attention (n=3, 8%), despite its significant potential for health care processes and strategy.
Conclusions
Three main research propositions were identified. First, research into digital health innovation should not focus solely on the technology aspects but also on its implications for strategic and operational management. Second, the research community should target other domains besides eHealth. Third, we observed a lack of quantitative research on the real impact of digital health on organizations and their management. More quantitative evidence is required regarding the expected outcome and impact of the implementation of digital health solutions into our health care organizations.
Keywords: digital health, management, health care management, literature review, health technology, eHealth, data health, trend health, tech health
Introduction
Any list of the significant trends that influence the way we manage our organizations will certainly include digitalization. It is not surprising, therefore, that digital health is a major area of interest in the health care sector. Public health literature, popular media, and health care services all increasingly focus on this topic [ 1 ]. At the same time, a uniform definition of the term ‘digital health’ has yet to be established [ 2 ]. Furthermore, when discussing digitalization in the health care sector, the terms Medicine 4.0, Health 2.0, and ‘connected health’ are used alongside and sometimes interchangeably with digital health.
It should be emphasized that digital health has the potential to radically change the strategy, operations, and culture of health care providers. In particular, it can offer cost-effective, patient-centered solutions [ 3 ], which could drastically simplify access to data as well as the exchange and generation of data for the benefit of patients and health care professionals [ 4 ].
Furthermore, digital health can add value not only at the level of the overall health care sector but also to individual organizations; therefore, it also has a significant management perspective.
When discussing digital health solutions and taking advantage of the great potential associated with them, individual health care organizations and their managers are confronted with major decisions. In order to be able to continue to compete in the health care market, health care managers need guiding frameworks and sound advice from scientific sources on how to exploit the potential of digital health and how to cope with the associated changes in the best possible way. We felt it was important, as a result, to assess the impact that digital health has on the field of health care management. The reverse effect, the impact of management on digital health, is beyond the scope of this study.
Previous Research and Research Gap
Limited information is currently available on the impact of digital health from a management perspective. In a literature review of digital transformation cases by Ivančić et al [ 5 ], only 2 out of 29 papers analyzed addressed the health care sector. A literature review by Henriette et al [ 6 ] on digital transformation identified just one paper about the health sector. Admittedly, these reviews have the following limitations: (1) they were not targeted at the health care sector specifically, and (2) they had a very narrow focus on the transformative aspect of digitization.
Research Problem, Questions, and Methods
This study addresses the lack of health care–related data in the literature on digital transformation identified above. In particular, it discusses the results of a literature review we conducted on the impact of digital health on health care management.
To this end, we followed the recommendations of Tranfield et al [ 7 ]. In addition to a comprehensive overview of digital health in the health care sector, we wanted to incorporate a broader, ‘big picture’ view of the impact of digital health on health care management. According to Thompson et al [ 8 ], health care managers and their tasks can be defined as follows:
The profession that provides leadership and direction to organizations that deliver personal health services, and to divisions, departments, units or services within those organizations [ 8 ].
Since there are many definitions of digital health, we used the following broad definition of digital health:
Digital health is the utilization of modern information and communication technologies (ICT) in the health care sector to improve the quality, the efficiency, and the focus on patients’ needs [ 9 ].
This holistic definition includes, for example, the many existing digital devices and apps used to diagnose and treat disease, simplify the self-treatment of chronic diseases, and monitor health parameters and daily behavior patterns. The definition also encompasses completely different technologies such as software used by health care providers to optimize their daily operations and train their staff.
The objective of this systematic review was to provide health care managers with an overview of digital health literature from a management perspective and uncover any potential research gaps in this field.
The literature review we conducted is based on the approach by Tranfield et al [ 7 ] and is depicted in Multimedia Appendix 1 . In the following section, the study design is presented in more detail.
Search Strategy
In March 2019, two researchers were tasked with searching the 3 databases ABI/Inform Global, WISO, and PubMed for studies published between 2000 and 2019. The search was limited to freely available full-text articles published in English. To take into account the management perspective of digital health, the search terms “digital,” “health,” and “manage*” were used in different combinations.
Reference lists of systematic reviews were searched for additional studies not captured by our initial systematic research. Once the search was complete, duplicates were removed, and the citations were uploaded to a secure internet-based platform.
Selection Criteria and Data Collection
Multimedia Appendix 2 defines the specific inclusion criteria for each database and shows the documentation of the search terms with the corresponding hits per database.
Studies were included according to the following inclusion criteria: (1) studies were published between January 1, 2000, and December 31, 2019, on Web of Science Core collection; (2) studies were published between 2009 and 2019 on ABI/Inform Global or PubMed; (3) studies were published in English; (4) full-text articles were freely available; and (5) studies were relevant to our subject.
Exclusion criteria included the following: (1) a lack of thematic focus (eg, ‘health’ or ‘digital’ were not the main topic or digital health was only discussed in passing); (2) studies focusing on digitalization as a means to transforming customer experience; and (3) unpublished literature, conference abstracts, and letters or editorials. Since our goal was to provide a first and extensive overview of digital health literature from a management perspective, there were no restrictions on the type of study designs reviewed.
The 2 reviewers each selected studies for possible inclusion based on title and the content of the abstract. Studies deemed to fulfill the inclusion criteria were analyzed in full-text review. Any disagreements were discussed between the reviewers, and a third party was involved to help reach consensus if necessary. Full data extraction, including characteristics of included articles, was completed by one reviewer and verified by the second reviewer.
Analysis Framework
To analyze the literature we had identified as relevant, we developed a taxonomy with the following 6 dimensions:
Research approach. Publications can derive their knowledge from real implementations or theoretical thinking. In line with Brandao de Souza [ 10 ], we classified the articles as ‘case-based’ or ‘conceptual.’ This classification is relevant since, from the distribution of both types, we can derive statements on the maturity level of the overall implementation of digital health in the health care market.
Research question type. Wytrzens et al [ 11 ] defined 5 basic types of research question that categorize articles according to their primary objective, as follows: description, explanation, creation or concept, evaluation or criticism, and forecasting or prediction. This differentiation permits statements on the focus and core objective of a study.
Management discipline. The objective of this category was to assess whether various business management disciplines are treated in a balanced way. To do so, we used the same catalog that Harvard Business Publishing [ 12 ] uses to structure their publications. Since some of the articles were also in the legal and public health fields, these two dimensions were added to the Harvard Business Publishing categorization. The dimension ‘general management’ is used for any residual topic that does not fit well into the Harvard taxonomy.
Reason for digitalization. Like any other organization, health care organizations should always ask themselves why they want to introduce digital health solutions into their operations. In line with the message in Simon Sinek’s popular management book, “Start With Why” [ 13 ], we tried to understand the rationale for digitalization. We differentiated between the two goals of improving operational processes and creating new business models. This is a concept used by the Massachusetts Institute of Technology Center for Digital Business [ 14 ]. Their research has shown that it is primarily the business process, business model, or customer experience that can improve overall business outcomes. For our literature research, we wanted to focus on the management aspect, so we excluded all ‘customer experience’ publications.
Content domain. To analyze the content of the papers chosen, we used the following 4 digital health subcategories created by Angerer et al [ 2 ]: trend health (lifestyle), eHealth (exchange of data), tech health (hardware), and data health (software). During the coding, we added a fifth additional domain that we called ‘overarching challenges,’ where the focus was on the challenges in the implementation and use of different technologies found in practice.
Implementation approach. To answer the question of how the health care sector implements its digitalization initiatives, the examples of practices, principles, and tools from Angerer et al [ 2 ] were taken and supplemented with new elements discovered during the screening process.
The search resulted in 133 unique citations, which were screened by our researchers. Based on the articles’ titles and abstracts, 31 were excluded, resulting in 102, which were subjected to a full-text screening. This process left us with 38 papers that met the inclusion criteria for our review ( Figure 1 ). Their reference lists were searched, but no additional studies were added. Multimedia Appendix 3 shows all publications eventually included in this study.
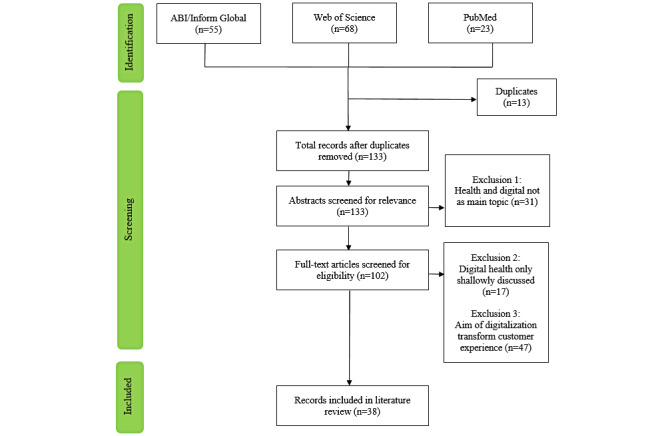
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of literature research procedure [ 15 ].
Analysis Based on Research Approach
Table 1 outlines the distribution of papers by research approach. Of the 38 papers included, 21 (55%) papers are case based, and 17 (45%) papers are theory based. This led us to conclude that this subject area is well balanced in terms of theory-based versus practice-based articles.
Number of papers by research approach (N=38).
Analysis Based on Research Question Type
As depicted in Table 2 , the objective of 31 (82%) papers was to design new digital concepts to overcome practical problems in health care. The second most pursued goal in 7 (18%) papers was to predict future health care scenarios. As frequently stated, the health care sector is still in its digital infancy; therefore, it seems highly plausible that the most popular research questions will deal with future, hypothetical situations, or concepts. We found it surprising that only 4 (11%) papers were (critical) evaluation papers, since they have one of the most vital roles of the scientific management community.
Number of papers by objective of the research question (N=38) a .
a One paper can include more than one category; therefore, the sum can be larger than 100%.
Analysis Based on Management Discipline
As shown in Table 3 , the discipline most frequently addressed in 23 (61%) papers is IT management. This finding is consistent with the findings of a literature review by Reis et al [ 16 ] on digital transformation in general and shows that IT is still the main driver of digital health (ie, technology push). From a management perspective, strategy should lead the way (ie, technology pull), yet only 4 (11%) reviewed papers addressed this underresearched topic. In a hospital setting, for example, this could imply that the IT department with its technological perspective is in the driver’s seat. Yet this can be problematic, as the digital health strategy should support the overall organizational strategy. Another indication that digital health is still primarily a result of technology push is that people-focused disciplines, such as human resources, ethics, and organizational behavior, are underrepresented.
Number of papers by management discipline (N=38) a .
a One paper can include more than one discipline; therefore, the sum can be larger than 100%.
Analysis Based on Reason for Digitalization
The digitalization of the health care system is discussed in just over two-thirds (n=26, 68%) of all papers ( Table 4 ). This comes as no surprise, since increasing the efficiency and effectiveness of health care today seems to be the primary focus of the majority of stakeholders [ 17 ]. Transforming business models through digitalization is much more radical and challenging, which may explain the comparatively low number of articles addressing this (n=16, 42%).
Number of papers by the reason for digitalization (N=38) a .
a One paper can include several dimensions; therefore, the sum can be larger than 100%.
Analysis Based on Content Domain
The vast majority of the papers (n=30, 79%) deal with different issues related to eHealth ( Table 5 ). This is consistent with a survey published by the World Health Organization [ 18 ], which revealed that 58% of its member countries already have an eHealth strategy. Arak and Wójcik [ 19 ] held that eHealth is the key to addressing the challenges of modern health care systems. Electronic health records are a very popular subtopic of the eHealth papers reviewed (n=11, 29%).
Distribution of publications by content domain (N=38) a .
a One paper can be part of several dimensions, so the sum can be larger than 100%.
The second most frequently mentioned dimension is data health (n=12, 32%). The majority of the papers in this category (n=7, 18%) deal with methods to analyze data. This digital health dimension is relatively close to the next dimension—overarching challenges (n=7, 18%)—where the focus is on challenges related to the implementation and use of different technologies found in practice. The biggest issue, by far, is personal data privacy. Both dimensions being so close to each other is not unusual, since data analysis always touches on security issues as well.
The dimensions occurring least frequently in the literature reviewed are trend health (n=5, 13%) and tech health (n=3, 8%). The latter is in line with our expectations for 2 reasons. First, we focused on management literature, and highly technical papers—where the hardware itself plays a major role—are unlikely to be published in business-oriented journals. Second, many of the technologies within the domain, such as 3D printing or robotics, are not yet widely spread in a health care context. More remarkable, however, is the low number of just 5 papers for trend health–related publications. From a business perspective, lifestyle solutions can be significant revenue drivers, as seen in the success of activity tracking devices. A possible explanation for this low count might be the bias of researchers to focus their activities on more ‘serious’ digital health aspects closer to conventional medicine.
Figure 2 is a summary graphical representation of the content findings from our digital health literature search. The innermost (white) layer of the circle represents the ‘why’ and shows that operational processes are the main reason for digital transformation in the papers analyzed. The second layer represents the ‘where’ and shows clearly that eHealth is addressed most often in scientific articles. The outermost layer illustrates the ‘what’; it shows that electronic health records and IT systems are the topics mentioned most frequently.
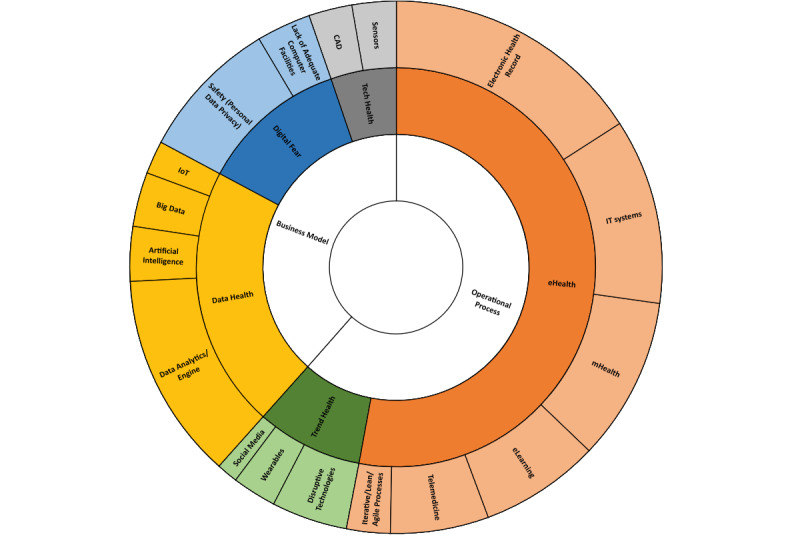
Distribution of reviewed publications. CAD: computer-aided design; IoT: internet of things; IT: information technology.
Main Findings
This literature review provides an overview of digital health literature from a management perspective and uncovers research gaps. In general, it shows that digitalization in the health care sector is still in its infancy, and therefore, there are still significant knowledge gaps concerning health care management. In the following section, we present the 3 important avenues for future research derived from our literature review.
The first finding regarding the ‘management discipline’ is that most papers analyzed focus on the IT domain and its technological aspects. Understanding technology is certainly key, as new IT solutions can enable management practices that were not previously possible. However, the technological perspective alone is not sufficient, as we strongly agree with Henriette et al [ 6 ] that “digital transformation is more than just a technological shift.” The implementation of digital health solutions could have major implications in many areas, such as for the senior management of a hospital [ 20 ]. For them, an innovation that would create the ability to track material and persons with sensors in real time could revolutionize the daily operational processes in larger hospitals. Consequently, we need more initiatives in which technology and management experts work together through all the development and implementation phases. True innovations can only happen when digital health technology is successfully integrated into daily operations and day-to-day management processes. Our first research proposition is hence to take more into consideration the implications for the management and leading of health care organizations, as follows:
Future digital health research should not merely focus on the technology aspects. Instead, it should have a more holistic approach and further study the implications the technology has for the strategic and operational management of health care organizations.
The second research proposition refers to ‘content domains.’ We identified a strong focus on eHealth topics, as this has been the domain with the longest implementation history (eg, telemedicine was introduced to Australia back in the 1980s). Nevertheless, other fields could be of equal or greater importance when their implementation becomes more widespread. We base these expectations on the many publications forecasting a radical transformation of health care owing to different developing technologies (eg, in the field of big data, as in the review by Kruse et al [ 21 ]). Therefore, we advocate a more balanced examination of the 5 content domains presented in this paper, as follows:
Explore the management perspective of all the different content dimensions of digital health in appropriate depth.
A final imbalance was found in the distribution of ‘research questions.’ An overwhelming number of papers create concepts for a possible digital health future. From a business perspective, these provide mostly anecdotal descriptions of the impact such solutions might have on the management of health care organizations. We suggest this is due to the relative youth of digital health in our current systems and a lack of widespread real-life application and experience. However, as more and more concepts become a reality, we would encourage the scientific community to take further steps. Future research should analyze in greater detail the real value of implementation. Practitioners and academics alike need more evidence regarding the expected outcome and impact of digital health on our health care organizations. Future research initiatives could, for example, examine the input and outcomes of digital health implementation by employing a quantitative study design. The quantification of the impact of digital health solutions on clinical outcomes has been the focus of many studies (eg, [ 22 , 23 ]). We encourage scholars to conduct methodologically similar pre-post studies, analyzing the effect on management process and business performance. A solid foundation is needed to result in meaningful recommendations for managers. Therefore, our last research avenue for exploration is the following:
Broaden the research focus to include quantitative analysis of the impact of digital health on health care management and organizational design.
This study presents contributions to an underresearched area of digital health from a management viewpoint. Within the scope of our review, we examined the most relevant publications to access the impact of digital health on health care management. All of the available publications were published between 2010 and 2019, with more literature published from 2016 to 2019 emphasizing the growing interest in digital health. The findings of our systematic review are the first step toward giving health care practitioners an overview of digital health in the field of health care management and enabling them to handle the ongoing digital transformation in the best possible way. By unveiling the actual status of digitalization in the health care sector and showing significant knowledge gaps, we set the stage for further research on how best to support health care practitioners through the process of digital transformation. To achieve this in the best possible way, we conducted three research proposals for future research avenues based on the research gaps identified.
Limitations
It is important to note some limitations associated with the study design. The researchers have a background in health care management and are based in Europe. We did not control for the geographical location of the papers analyzed, but our assumption is that most of the papers dealt with findings from North American and European organizations. A potential concern is therefore the generalization of the findings to other parts of the world. Furthermore, we focused on 3 specific databases as part of our systematic search. Therefore, it cannot be ruled out that the inclusion of further databases, such as Embase, might have yielded additional relevant publications. However, the studies published on Embase often coincide with those on PubMed, which was included in our search strategy. A final limitation is that no unpublished literature was reviewed or evaluated. However, due to the inclusion of various databases, we assume that the noninclusion of further publications is rather low. We therefore believe that with our approach, we have nevertheless achieved our aim to provide a first overview for practitioners.
To our knowledge, this study is the first overview of the impact of digital health from the health care management viewpoint. This paper relies on a systematic literature review of both conceptual and case-based papers on digital health. As our main contribution, we have developed three research proposals for future research avenues based on the research gaps identified. The big question is not whether further developments in digital health will have an impact on our health care organizations but how prepared managers are to deal with these changes. We note that most publications are still concerned with possibilities, but as more and more of these possibilities become a reality, managers need to be able to be proactive and, what is more, shape their organizations accordingly. We believe this paper has created some insights for the digital health research community on how best to support health care practitioners through the process of digital transformation.
Abbreviations
information technology
Literature review stages.
The specific inclusion criteria for each database.
All publications eventually included in this study.
Authors' Contributions: AA and EK designed the study. EK wrote the first manuscript draft. AA, JS, and SB wrote the final manuscript. All authors were involved in preparing the manuscript, and they all read and approved the final manuscript. This paper has not been published elsewhere.
Conflicts of Interest: None declared.
- 1. Santha A. Deborah Lupton: digital health. critical and cross-disciplinary perspectives. Acta Univ Sapientiae Soc Anal. 2018;8:109–112. doi: 10.2478/aussoc-2018-0007. [ DOI ] [ Google Scholar ]
- 2. Angerer A, Moll C, Strunk L, Brügger U. Digital Health - Die Zukunft des Schweizer Gesundheitswesens. 2017. [2022-10-20]. https://digitalcollection.zhaw.ch/bitstream/11475/1458/1/Digital%20Health%20Report_DC_2017_11_08.pdf .
- 3. Powell J, Newhouse N, Boylan A, Williams V. Digital health citizens and the future of the NHS. Digit Health. 2016 Oct 10;2:2055207616672033. doi: 10.1177/2055207616672033. https://journals.sagepub.com/doi/10.1177/2055207616672033?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2055207616672033 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Lupton D. Digital health now and in the future: Findings from a participatory design stakeholder workshop. Digit Health. 2017 Nov 09;3:2055207617740018. doi: 10.1177/2055207617740018. https://journals.sagepub.com/doi/10.1177/2055207617740018?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2055207617740018 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Bosilj Vukšić V, Ivančić L, Suša Vugec D. A preliminary literature review of digital transformation case studies. IJCEIT. 2018;12(9):737–742. doi: 10.5281/zenodo.1474581. [ DOI ] [ Google Scholar ]
- 6. Henriette E, Feki M, Boughzala I. The shape of digital transformation: a systematic literature review. MCIS 2015 Proceedings; MCIS; Oct 3-5; Samos, Greece. 2015. Oct, pp. 1–13. https://tinyurl.com/yc2hjud8 . [ Google Scholar ]
- 7. Tranfield D, Denyer D, Smart P. Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br J Management. 2003 Sep;14(3):207–222. doi: 10.1111/1467-8551.00375. [ DOI ] [ Google Scholar ]
- 8. Thompson JM, Buchbinder SB, Shanks NH. An overview of health care management. Introduction to Health Care Management Second Edition. 2012. Jan 06, [2022-10-22]. https://samples.jbpub.com/9780763790868/90868_ch01_final_withoutcropmark.pdf .
- 9. Angerer A, Russ C, Ultsch S. Digital health - revolution or evolution?: strategic options in healthcare. Zürcher Hochschule für Angewandte Wissenschaften. 2019 Oct; doi: 10.21256/zhaw-18267. https://digitalcollection.zhaw.ch/bitstream/11475/18267/1/2019_Digital%20Health%20Report.pdf . [ DOI ] [ Google Scholar ]
- 10. Brandao de Souza L. Trends and approaches in lean healthcare. Leadersh Health Serv. 2009 May;22(2):121–139. doi: 10.1108/17511870910953788. [ DOI ] [ Google Scholar ]
- 11. Wytrzens H, Schauppenlehner-Kloyber E, Sieghardt M, Gratzer G. Wissenschaftliches Arbeiten: eine Einführung. Wien: Facultas; 2017. [ Google Scholar ]
- 12. Harvard Business Publishing. [2022-10-04]. https://hbsp.harvard.edu/catalog/
- 13. Sinek S. Start With Why: How Great Leaders Inspire Everyone to Take Action. Westminster, England: Penguin; 2009. [ Google Scholar ]
- 14. Westerman G, Calméjane C, Bonnet D, Feraris P, McAfee A. Digital transformation: a roadmap for billion-dollar organizations. MIT Center for Digital Business and Capgemini Consulting. 2011. [2022-10-20]. https://www.capgemini.com/wp-content/uploads/2017/07/Digital_Transformation__A_Road-Map_for_Billion-Dollar_Organizations.pdf .
- 15. PRISMA Flow Diagram. [2022-10-04]. https://prisma-statement.org/prismastatement/flowdiagram.aspx .
- 16. Reis J, Amorim M, Melão N, Matos P. Digital Transformation: A Literature Review Guidelines for Future Research. New York City, NY: Springer International Publishing; 2018. [ Google Scholar ]
- 17. Chin W, Hamermesh R, Huckman R, McNeil B, Newhouse J. 5 imperatives for addressing health care's innovation challenge. Forum on Health Care Innovation. 2012. [2022-10-20]. https://www.hbs.edu/healthcare/Documents/Forum-on-Healthcare-Innovation-5-Imperatives.pdf .
- 18. Global diffusion of eHealth: making universal health coverage achievable. World Health Organization. 2017. [2022-10-20]. https://www.who.int/publications/i/item/9789241511780 .
- 19. Arak P, Wójcik A. Transforming eHealth into a political and economic advantage. Polityka Insight. 2017. [2022-10-20]. https://www.politykainsight.pl/_resource/multimedium/20111291 .
- 20. Windeck P, Förster S, Mummert R. IT und Technik: Digitalisierung und Führungskräfte. Was für Geschäftsführungen jetzt anders wird. Das Kraunkenhaus. [2022-10-22]. https://daskrankenhaus.de/thema/detail/it-und-technik-digitalisierung-und-fuehrungskraefte-was-fuer-geschaeftsfuehrungen-jetzt-anders-wird/
- 21. Kruse CS, Goswamy R, Raval Y, Marawi S. Challenges and opportunities of big data in health care: a systematic review. JMIR Med Inform. 2016 Nov 21;4(4):e38. doi: 10.2196/medinform.5359. https://medinform.jmir.org/2016/4/e38/ v4i4e38 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Wang J, Howell D, Shen N, Geng Z, Wu F, Shen M, Zhang X, Xie A, Wang L, Yuan C. mHealth supportive care intervention for parents of children with acute lymphoblastic leukemia: quasi-experimental pre- and postdesign study. JMIR Mhealth Uhealth. 2018 Nov 19;6(11):e195. doi: 10.2196/mhealth.9981. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Bollyky JB, Melton ST, Xu T, Painter SL, Knox B. Theeffect of a cellular-enabled glucose meter on glucose control for patients with diabetes: prospective pre-post study. JMIR Diabetes. 2019 Oct 7;4(4):e14799. doi: 10.2196/14799. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

COMMENTS
The literature of health care management has expanded rapidly in the last decade, with cumulative citations increasing by 76.6% and the number of cited journal titles increasing by nearly 70% since the original study.
This literature review identified a variety of interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy.
Health Care Management Review (HCMR) disseminates state-of-the-art knowledge about management, leadership, and administration of health care systems, organizations, and agencies.
This article describes a step-by-step process to systematically review the literature along with links to key resources. An example of a graduate program using systematic literature reviews to link research and quality improvement practices is also provided.
Literature reviews related to Health Management. How to successfully implement population health management: a scoping review. Article. Full-text available. Aug 2023. A. F. T. M. van Ede....
This review examines the current and emerging challenges for health leadership and workforce management in diverse contexts and health systems at three structural levels, from the overarching macro (international, national) context to the meso context of organisations through to the micro context of individual healthcare managers.
Health Care Management Review (HCMR) disseminates state-of-the-art knowledge about management, leadership, and administration of health care systems, organizations, and agencies.
The literature of health care management has expanded rapidly in the last decade, with cumulative citations increasing by 76.6% and the number of cited journal titles increasing by nearly 70% since the original study.
Accelerated by the coronavirus disease 2019 (Covid-19) pandemic, major and lasting changes are occuring in healthcare structures, impacting people's experiences and value creation in all aspects of their lives. Information systems (IS) research can support analysing and anticipating resulting effects.
The findings of our systematic review are the first step toward giving health care practitioners an overview of digital health in the field of health care management and enabling them to handle the ongoing digital transformation in the best possible way.