ORIGINAL RESEARCH article
The impact of perspective taking on obesity stereotypes: the dual mediating effects of self-other overlap and empathy.

- School of Psychology, Inner Mongolia Normal University, Hohhot, China
Previous studies have indicated that obese people face many forms of severe prejudice and discrimination in various settings, such as education, employment, and interpersonal relationships. However, research aimed at reducing obesity stereotyping is relatively rare, and prior studies have focused primarily on negative stereotypes. Based on the empathy-altruism hypothesis and self-other overlap hypothesis, this study investigates the impact of perspective taking (PT) on both positive and negative obesity stereotypes and examines the mediating effects of empathy and self-other overlap. A sample of 687 students (191 males and 496 females) at Chinese universities participated by completing self-report questionnaires on trait tendency and evaluation toward obese people. Structural equation modeling and the bootstrap method revealed that self-other overlap (but not empathy) mediated the relationship between PT and negative obesity stereotypes. While self-other overlap and empathy both mediated the relationship between PT and positive obesity stereotypes. These findings address the importance of PT for improving positive and negative obesity stereotypes: specifically, PT promotes psychological merging, and produces empathic concern (EC).

Introduction
Obese people are severely stigmatized because of their weight. An intensive review by Puhl and Heuer (2009) shows that they confront prejudice and discrimination in many forms. In educational settings, obese students are less likely than normal-weight students to obtain a college degree ( Fowler-Brown et al., 2010 ) or be accepted as graduate students after an interview ( Burmeister et al., 2013 ). As regards interpersonal relationships, obese individuals tend to have poor relationships with their peers in school ( Puhl and Latner, 2007 ) and have fewer close friends relative to thinner individuals ( Sarlio-Lähteenkorva, 2001 ). Further, in employment settings, obese applicants are sometimes not hired because of discrimination based on their weight ( Puhl et al., 2008 ). Individuals experiencing the stigma of obesity are vulnerable to psychological disorders such as depression, low self-esteem, and anxiety ( Puhl and King, 2013 ). This stigma derives partly from negative stereotypes ( Tiggemann and Anesbury, 2000 ) that obese people are lazy, unintelligent, and lacking in self-discipline and willpower ( Puhl and Heuer, 2009 ). Although there is a lot of evidence about the adverse consequences of the stigma of obesity, relatively few studies have explored strategies to reduce obesity stereotypes and prejudices ( Gloor and Puhl, 2016 ). It is, therefore, necessary to take measures to improve attitudes toward this group.
Perspective Taking (PT) and Stereotypes
Corrigan and O'Shaughnessy (2007) propose three main avenues to change stereotypes and stigma, namely protest, education, and contact. However, the protest may provoke rebound effects, arouse resistance, and ultimately fail to induce more positive attitudes ( Corrigan et al., 2001 ). Furthermore, the magnitude and duration of education to improve attitudes may be restricted ( Corrigan et al., 2002 ). For contact to be effective, some optimal conditions are required, such as shared goals and cooperation ( Pettigrew and Tropp, 2006 ). Different from these aforementioned approaches (e.g., PT will not cause the rebound effects), PT has become an effective stereotype-improvement strategy ( Galinsky, 2002 ; Todd and Galinsky, 2014 ; Sun et al., 2016 ; Wang et al., 2018 ; Huang et al., 2020 ) because of its unique advantages. Specifically, its positive effect can be generalized from specific individuals to the groups they belong to Shih et al. (2009) for a relatively long time ( Batson et al., 1997 ) at both the explicit and implicit levels ( Todd and Burgmer, 2013 ). The limited existing work applied this strategy to anti-fat bias found that taking the perspective of obese persons who experienced discrimination did produce reduced implicit bias among overweight participants ( Teachman et al., 2003 ). There are two main theoretical hypotheses to explain the mechanisms underlying PT.
PT, Empathy, and Stereotypes
The first is the empathy-altruism hypothesis ( Batson et al., 1997 ), focused on the emotional level, which holds that taking the perspective of a member of a stigmatized group will increase the empathic feelings of an individual, such as sympathy and compassion for that individual. These feelings will evoke altruistic motivation and generalize to the whole stigmatized group, thus increasing the positive evaluation and attitude of an individual toward the group. The theory that PT indirectly reduces stereotyping through the mediating effect of empathy has been tested in many groups, such as people with AIDS ( Li, 2017 ), drug addicts ( Batson et al., 2002 ), African Americans ( Vescio et al., 2003 ), homosexuals ( Wang, 2018 ), and the elderly ( Bian, 2015 ). However, few studies have applied this method to attempt to tackle obesity stereotyping. As far as the author knows, only Cheng and Zhang (2017) have examined the direct impact of PT on implicit obesity stereotypes in China; they found significant attenuation of stereotyping but did not explore the underlying mechanism. To address this deficiency, the present study draws on the empathy-altruism hypothesis to test the mediating role of empathy between PT and obesity stereotypes. Another limitation in the literature is that many studies have shown the role of PT in reducing negative stereotypes ( Galinsky and Moskowitz, 2000 ; Ku et al., 2010 ; Todd et al., 2011 ) but few have considered positive stereotypes ( Wang et al., 2014 ). Obesity stereotypes include not only negative qualities but also positive characteristics, such as warmth and friendliness ( Tiggemann and Rothblum, 1988 ). Does PT weaken or enhance positive obesity stereotypes? The current study will answer this question.
PT, Self-Other Overlap, and Stereotypes
The second explanation mechanism is the self-other overlap hypothesis ( Davis et al., 1996 ; Galinsky and Moskowitz, 2000 ), focused on the cognitive level, which holds that PT can activate self-concept and lead perspective takers to attribute a greater proportion of their self-traits to the other. With perspective takers perceiving that they share more common characteristics with the target, they merge their mental representations of self and others, which changes their evaluation of the target group. Galinsky and Ku (2004) indirectly tested the self-other overlap hypothesis by examining the moderating role of self-esteem on the effect of PT on prejudice toward the elderly. They reasoned that because perspective takers change their attitude by applying the self to the target, the positive self will be activated and applied to the target group when the perspective takers have high self-esteem, thereby improving their attitude toward target group members; conversely, when perspective takers feel negative about themselves, there is no reduction in prejudice against the target group. As expected, Galinsky and Ku (2004) found that perspective takers with high self-esteem evaluated the elderly more positively than did those with low self-esteem. However, the studies of Bian (2015) , Li (2017) , and Wang (2018) , did not produce this result. The three researchers suggested that the inconsistent findings may be caused by a cultural difference in self-esteem between East and West. Todd et al. (2012) found that automatic self–Black associations, measured by IAT, mediated the effect of PT on perceptions of racial discrimination. Additionally, there are multiple measures to assess self–other overlap, such as Adjective Checklist Overlap, Absolute Difference in Attribute Ratings, and the Inclusion of Others in Self Scale (IOS; Aron et al., 1992 ). Myers and Hodges (2012) comprehensively analyzed these measures and identified perceived closeness (e.g., IOS) as the most effective way to measure the quality of the relationship between two people. For the above reasons, the present study does not take the indirect approaches but, instead, uses the IOS to directly measure self-other overlap. The aim is to test whether the influence of PT on obesity stereotypes is realized through the mediating effect of self-other overlap.
In summary, based on the empathy-altruism hypothesis and self-other overlap hypothesis, this study investigates the impact of PT on positive and negative obesity stereotypes and examines the underlying mechanism of this relationship, namely the mediating effects of empathy, and self-other overlap.
Participants
The participants were 687 undergraduates recruited from three universities in Hebei, Shandong, and Jiangxi Province, China, comprising 191 males and 496 females. The average age of participants was 19.91 years (SD = 1.14, age-range = 17~24). Among the participants, 151 students majored in Chinese language and literature, 378 students majored in pharmacy, and 158 students majored in education. Six hundred forty eight students were Han and the rest were ethnic minorities. In terms of self-reported body weight, 141 participants were underweight, 389 participants were moderate, and 157 participants were overweight.
A teacher from each University conducted the questionnaire survey in class. The teachers first explained to the students their rights as participants, including the option to withdraw and assured them that their anonymity and the confidentiality of their responses were guaranteed. Written informed consent was obtained from all participants; for underage participants, consent was obtained from parents. Teachers then distributed the questionnaire to participants, who were seated separately and not permitted to interact with one another while completing the questionnaire. Each participant received a small reward for their contribution to the study.
PT and Empathy
Following Wang et al. (2014) , this study used the PT and empathic concern (EC) subscales of the Chinese version of Zhan (1986) of the Interpersonal Reactivity Index ( Davis, 1980 ) to respectively measure the PT and empathy tendency of students. The PT subscale contains five items, such as “I sometimes try to understand my friends better by imagining how things look from their perspective”; the EC subscale includes six items, such as “I often have tender, concerned feelings for people less fortunate than me.” All items are measured using a 5-point Likert scale of agreement, with response options ranging from 0 (“does not describe me well”) to 4 (“describes me very well”). Cronbach's alphas for each subscale were α PT = 0.84, α EC = 0.52, consistent with the previous study (e.g., Zhang et al., 2010 ).
Self-Other Overlap
Self-other overlap was measured by the IOS. The scale comprises seven pairs of circles with an increasing degree of overlap. One circle represents the self and the other represents obese group members. Participants were asked to select which pair of circles best described their relationship with the obesity group. The scale is scored from 1 (no overlap) to 7 (nearly complete overlap). The higher the overlapping degree of circles, the greater the self-other overlap.
Obesity Stereotypes
Obesity stereotypes were selected from the studies of Vartanian et al. (2015) and Cheng (2017) . Specifically, this study included five negative stereotypes (lazy, sloppy, self-indulgent, lacking in self-discipline, and clumsy) and five positive stereotypes (kind, warm, optimistic, simple and honest, and generous). Participants were asked to rate the extent to which each stereotype fitted the characteristics of obese people. The response options ranged from 1 = strongly disagree to 5 = strongly agree. Cronbach's alphas for the overall scale and each subscale were α overall = 0.77, α positivestereotypes = 0.84, and α negativestereotypes = 0.90.
Analytic Strategy
Descriptive statistics were performed using SPSS 22. The hypothesized relationships were tested through a series of structural equation models and the bootstrap method in AMOS. Studies using structural equation modeling usually set several thresholds for goodness-of-fit indexes, such as root mean square error of approximation (RMSEA) ≤ 0.08 ( Williams et al., 2009 ), CFI ≥ 0.90, and 2 ≤ χ 2 /df ≤ 5 ( Hair et al., 2010 ). Before the data analysis, all variables were standardized. The items of PT, empathy, self-other overlap, and obesity stereotypes were used as analysis indicators. Self-other overlap was considered as a manifest variable, while PT, empathy, and obesity stereotypes were considered as latent variables.
Control for Common Method Bias
Through precautions such as protecting anonymity and using various response formats (5- and 7-point scales), the data collection process was designed to minimize the common method bias of data obtained from the self-report questionnaire. Following data collection, Harman's single-factor test ( Podsakoff et al., 2003 ) was conducted to control for common method bias. The results revealed five factors with eigenvalues >1, of which the first factor accounted for 20.16% of the total variance (below the critical standard of 40%). Therefore, common method bias was not a significant problem in this study.
Descriptive Statistics
The ranges, means, SDs, and correlations of the research variables are reported in Table 1 . All the variables were significantly correlated, except empathy–negative stereotypes and negative–positive stereotypes. In addition, the age and gender of participants were not significantly correlated with either dependent variable [negative ( r age < −0.01, p = 0.95; r gender = 0.05, p = 0.20] and positive ( r age = 0.04, p = 0.25; r gender <0.01, p = 0.99) obesity stereotypes; for simplicity, these results are not presented in the Table. The body weight of participants was significantly correlated with the positive obesity stereotypes ( r = 0.10, p < 0.05), so body weight was controlled for in the subsequent analysis.
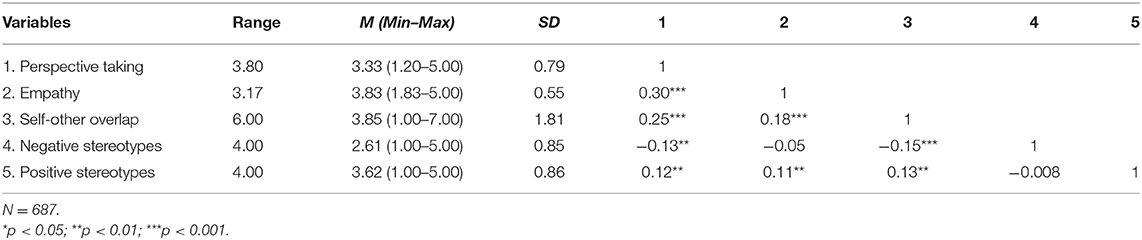
Table 1 . Descriptive statistics of the sample.
Analysis of Mediating Effect
First, the influence of PT on the negative obesity stereotypes and the mediating mechanism of this relationship were examined. Step 1 tested the direct effect of PT on negative obesity stereotypes. The results showed that the direct path was significant (β = −0.15, p < 0.001) but the model fit was poor (RMSEA = 0.10, χ 2 / df = 7.95). Step 2 then assessed the mediating role of empathy between PT and negative obesity stereotypes. As reported above, the correlation between empathy and negative obesity stereotypes was not significant, meaning that PT could not affect the negative obesity stereotypes through the mediating role of empathy. The mediation model analysis also supported this result: Although the indirect path from PT to empathy was significant (β = 0.59, p < 0.001), the indirect path from empathy to negative obesity stereotypes did not reach statistical significance (β = 0.001, p > 0.05). Next, step 3 examined the mediating role of self-other overlap in the effect of PT on negative obesity stereotypes. Model analysis showed that each path reached a significant level (as shown in Figure 1 ) and the model fitted well (RMSEA = 0.07, goodness of fit index (GFI) = 0.96, incremental fit index (IFI) = 0.95, comparative fit index (CFI) = 0.95, tucker-lewis index (TLI) = 0.94, chi-square/degree of freedom (the minimum discrepancy divided by degrees of freedom) χ 2 / df = 4.23). The mediating effect was tested by the bootstrap method. The results showed that the mediating effect of self-other overlap was significant with an indirect effect of 0.03 and a 95% confidence interval (CI) of [−0.06, −0.01]. Then pwrSEM was used to conduct a power analysis ( Wang and Rhemtulla, 2021 ). Results suggested that the study had 0.81 power to detect an indirect effect of 0.03 in the model. The above results indicate that PT has a negative effect on negative obesity stereotypes through the mediating effect of self-other overlap. However, empathy appears not to play a mediating role.
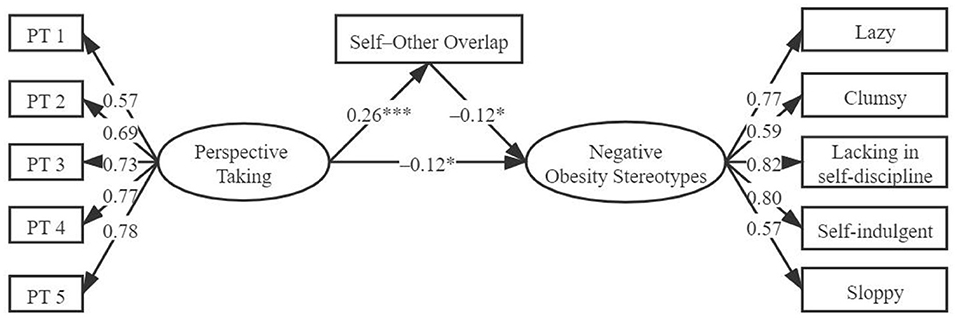
Figure 1 . The mediating role of self-other overlap between perspective taking and negative obesity stereotypes. * p < 0.05; *** p < 0.001.
Second, the influence of PT on positive obesity stereotypes and the mediating mechanism of this relationship were examined. The body weight of participants was treated as a control variable because it was identified earlier as being significantly correlated with positive obesity stereotypes. Step 1 tested the direct effect of PT on positive obesity stereotypes. The results indicated that the direct path was significant (β = 0.15, p < 0.001) and the model fitted well (RMSEA = 0.07, GFI = 0.95, IFI = 0.96, CFI = 0.96, TLI = 0.95, χ 2 / df = 4.22). Step 2 then assessed the mediating role of empathy between PT and positive obesity stereotypes. The model analysis showed that after adding the mediating variable empathy, the direct path from PT to positive obesity stereotypes became insignificant, while the indirect path from PT to empathy (β = 0.59, p < 0.001) and from empathy to positive obesity stereotypes (β = 0.17, p = 0.01) reached a significant level. The model fit indexes were RMSEA = 0.07, GFI = 0.92, IFI = 0.91, CFI = 0.91, χ 2 / df = 4.49, suggesting that the mediating model acceptably fitted the data. The mediating effect was (0.59 × 0.17)/0.15 = 0.67.
Next, step 3 assessed the mediating role of self-other overlap between PT and positive obesity stereotypes. The results showed that after adding the mediating variable self-other overlap, the direct path from PT to positive obesity stereotypes (β = 0.13, p < 0.01) and the indirect path from PT to self-other overlap (β = 0.26, p < 0.001) and from self-other overlap to positive obesity stereotypes (β = 0.10, p < 0.05) were all significant. The measurement model showed acceptable fit: RMSEA = 0.06, GFI = 0.95, IFI = 0.96, CFI = 0.96, χ 2 / df = 3.80. The mediating effect was (0.26 × 0.10)/0.15 = 0.17. In step 4, the mediating variables empathy and self-other overlap were combined to construct and test an integrated mediating model. The bootstrap method was used to test multiple mediating effects ( Lau and Cheung, 2012 ). Model analysis indicated that the direct path from PT to positive obesity stereotypes became insignificant when the two mediating variables were added simultaneously. The direct effect was 0.03 and the 95% CI (−0.10, 0.16) contained zero. All the other paths were significant: from PT to empathy [CI: (0.51, 0.67)], from empathy to positive obesity stereotypes [CI: (0.02, 0.31)], from PT to self-other overlap [CI: (0.19, 0.35)], from self-other overlap to positive obesity stereotypes [CI: (0.01, 0.310)]. Finally, a dual mediating model was obtained, with an indirect effect of 0.12, a 95% CI of (0.04, 0.22), and good model fit to the data (as shown in Figure 2 , which excludes the control variable for simplicity; RMSEA = 0.07, GFI = 0.92, IFI = 0.91, CFI = 0.91, TLI = 0.90, χ 2 / df = 4.16). Then pwrSEM was used to run a power analysis ( Wang and Rhemtulla, 2021 ). Results suggested that the study had 0.85 power to detect an indirect effect of 0.12 in the model. These results suggest that self–other overlap and empathy both play a mediating role between PT and positive obesity stereotypes.
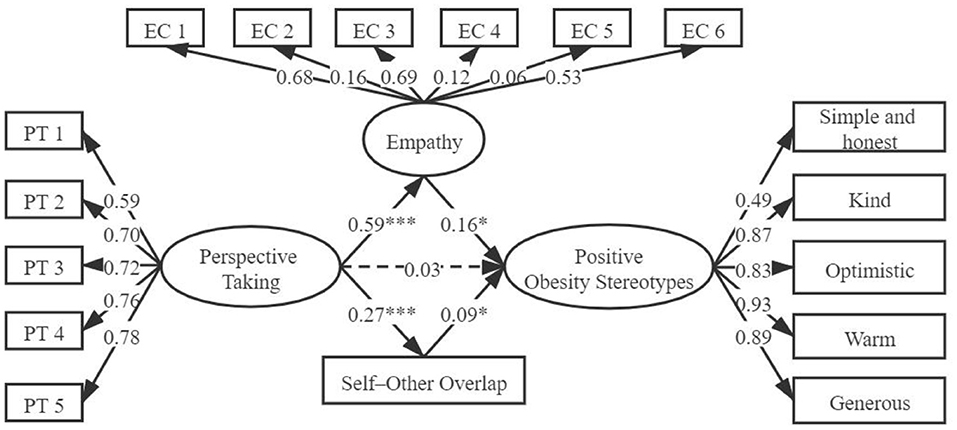
Figure 2 . The mediating role of empathy and self-other overlap between perspective taking and positive obesity stereotypes (The dotted line means that the path is not significant). * p < 0.05; *** p < 0.001.
This research aimed to discover the influence of PT on positive and negative obesity stereotypes among University students. Based on the self-other overlap hypothesis (cognitive level) and empathy-altruism hypothesis (emotional level), this study tested the mediating role of self-other overlap and empathy in the relationship between PT and obesity stereotypes. The results will be discussed in detail below.
First, analysis of the mechanism through which PT influences negative obesity stereotypes revealed that self-other overlap, but not empathy, played a mediating role. Although PT can predict empathy, empathy did not significantly affect negative obesity stereotypes. This is consistent with the findings of previous studies that empathy cannot effectively reduce obesity prejudice ( Teachman et al., 2003 ; Gapinski et al., 2006 ). In this regard, studies suggest that empathy inadvertently emphasizes or evokes the negative aspects of obesity ( Daníelsdóttir et al., 2010 ), which may offset the sympathy and compassion that empathy generates for stigmatized groups in negative evaluations. The mean score of the negative obesity stereotypes in this study was 2.61 (median = 3), indicating that the University students did not consider the negative traits to be characteristic of obese people. If this truly reflects the perception of participants about obese people, then they would feel no need to sympathize. However, the responses of participants may have been affected by social desirability bias, such that even in an anonymous context they did not report their true attitudes with respect to negative obesity stereotypes. Future research will benefit from directly measuring social desirability, to quantify and separate its impact. Another consideration is that this study used a trait tendency measurement, rather than taking a specific perspective for the obese group. This may have prevented participants from putting themselves in the position of obese people to feel the challenges they encounter. Future studies could address this limitation by using experimental methods to manipulate participants into taking the perspective of and empathizing with obese people. It would be valuable to discover whether this approach further verifies the hypotheses and results of this research. Additionally, from the perspective of the common ingroup identity model ( Gaertner et al., 1993 ), recategorizing two separate groups as one group could improve negative evaluations toward outgroup members. By promoting self-other overlapping, the attitudes of perspective takers toward former outgroup members (i.e., obese group) become more positive through processes involving pro-ingroup bias.
Second, this study found that self-other overlap and empathy both mediated the relationship between PT and positive obesity stereotypes. Individuals usually view themselves positively ( Taylor and Brown, 1988 ). Through PT that enhances the psychological merging between self and target, individuals apply the positive description of themselves to obese people, thereby enhancing positive evaluation. This is consistent with the findings of Laurent and Myers (2011) but contrary to the result of Wang et al. (2014) , who found that PT reduces the positive stereotypes of doctors through self-other overlap. These different findings may be attributed to the different contents of the stereotype: whereas the traits examined by Laurent and Myers (e.g., attractive, wholesome) and in this study (e.g., kind, warm) mainly focus on the “warmth” dimension, Wang et al. (2014) examined positive characteristics of the “competence” dimension (e.g., analytical, smart).
Although empathy did not mediate the relationship between PT and negative obesity stereotypes, this study supported the empathy-altruism hypothesis by showing that empathy played a mediating role between PT and positive obesity stereotypes. This seems to indicate the positive trait bias of the hypothesis in the obese group. In other words, empathy generates altruistic motivation to help obese people escape unfavorable situations by enlarging their positive traits. However, Gloor and Puhl (2016) found that although PT increases empathy, it also increases fat phobia. This may be related to the attitudes of participants toward obese people. The mean score of the positive obesity stereotypes in this study was 3.62 (median = 3), meaning that participants consider the positive traits to be fairly characteristic of obese people. Skorinko and Sinclair (2013) pointed out that when the characteristics of the target group are consistent with the stereotypes, PT will cause stereotyping to increase.
Finally, the shortcomings of this study must be acknowledged. Obesity stereotypes were measured through a self-report questionnaire. In some prior studies, participants who did not show explicit obesity prejudice were found to have strong implicit negative obesity stereotypes ( Teachman et al., 2003 ). Therefore, future research should use implicit measurement to test whether University students truly hold a neutral attitude toward negative obesity stereotypes. Considering the group specificity of PT, measuring individual tendency through a questionnaire may have weakened the empathy of participants toward the obese group and, consequently, their attitudes toward obesity stereotypes. Future research should, therefore, seek to verify the results of this study by using experimental methods to manipulate PT. Furthermore, the correlational method makes reverse causality an underlying issue. The application of experimental design will help to establish causal links between variables. Despite these limitations, this study makes valuable contributions to the literature by finding that self-other overlap and empathy both mediated the relationship between PT and positive obesity stereotypes among University students. Yet, for negative obesity stereotypes, self-other overlap emerged as the only mediator.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Inner Mongolia Normal University. Written informed consent to participate in this study was provided by the participants and underage participants' parents.
Author Contributions
YW conceived the original idea, organized the data collection, performed the statistical analyses, and drafted the manuscript. YZ critically revised the manuscript. All the authors read and approved the final draft of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.643708/full#supplementary-material
Aron, A., Aron, E. N., and Smollan, D. (1992). Inclusion of other in the self scale and the structure of interpersonal closeness. J. Pers. Soc. Psychol. 63, 596–612. doi: 10.1037/0022-3514.63.4.596
CrossRef Full Text | Google Scholar
Batson, C. D., Chang, J., Orr, R., and Rowland, J. (2002). Empathy, attitudes, and action: can feeling for a member of a stigmatized group motivate one to help the group. Pers. Soc. Psychol Bull. 28, 1656–1666. doi: 10.1177/014616702237647
Batson, C. D., Polycarpou, M. P., Harmon-Jones, E., Imhoff, H. J., Mitchener, E. C., Bednar, L. L., et al. (1997). Empathy and attitudes: can feeling for a member of a stigmatized group improve feelings toward the group? J. Pers. Soc. Psychol. 72, 105–118. doi: 10.1037/0022-3514.72.1.105
PubMed Abstract | CrossRef Full Text | Google Scholar
Bian, N. (2015). The effect of perspective taking on the college students' elderly stereotype . [master's thesis]. Wuhan, Hubei: Central China Normal University.
Burmeister, J. M., Kiefner, A. E., Carels, R. A., and Musher-Eizenman, D. R. (2013). Weight bias in graduate school admissions. Obesity 21, 918–920. doi: 10.1002/oby.20171
Cheng, L. (2017). A study on the influence of obese body shape stereotype to employment intention . [master's thesis]. Hohhot, Inner Mongolia: Inner Mongolia Normal University.
Cheng, L., and Zhang, Y. Z. (2017). Research on the influence of perspective taking on implicit obesity stereotype. J. Inner Mongo. Norm. Univ. 30, 73–77. doi: 10.3969/j.issn.1671-0916.2017.02.012
Corrigan, P. W., David, R., Amy, G., Robert, L., Philip, R., Kyle, U. W., et al. (2002). Challenging two mental illness stigmas: personal responsibility and dangerousness. Schizophr. Bull. 28, 293–309. doi: 10.1093/oxfordjournals.schbul.a006939
Corrigan, P. W., and O'Shaughnessy, J. R. (2007). Changing mental illness stigma as it exists in the real world. Aust. Psychol. 42, 90–97. doi: 10.1080/00050060701280573
Corrigan, P. W., River, L., Lundin, R. K., Penn, D. L., Uphoff-Wasowski, K., Campion, J., et al. (2001). Three strategies for changing attributions about severe mental illness. Schizophr. Bull. 27, 187–195. doi: 10.1093/oxfordjournals.schbul.a006865
Daníelsdóttir, S., O'Brien, K. S., and Ciao, A. (2010). Anti-fat prejudice reduction: a review of published studies. Obes. Facts 3, 47–58. doi: 10.1159/000277067
Davis, M. H. (1980). A multidimensional approach to individual differences in empathy. JSAS Cat. Sel. Doc. Psychol. 10:85.
Davis, M. H., Conklin, L., Smith, A., and Luce, C. (1996). Effect of perspective taking on the cognitive representation of persons: a merging of self and other. J. Pers. Soc. Psychol. 70, 713–726. doi: 10.1037/0022-3514.70.4.713
Fowler-Brown, A. G., Ngo, L. H., Phillips, R. S., and Wee, C. C. (2010). Adolescent obesity and future college degree attainment. Obesity 18, 1235–1241. doi: 10.1038/oby.2009.463
Gaertner, S. L., Dovidio, J. F., Anastasio, P. A., and Bachman, B. A. (1993). The common ingroup identity model: Recategorization and the reduction of intergroup bias. Eur. Rev. Soc. Psychol. 4, 1–26. doi: 10.1080/14792779343000004
Galinsky, A. D. (2002). “Creating and reducing intergroup conflict: the role of perspective-taking in affecting out-group evaluations,” in Toward Phenomenology of Groups and Group Membership , ed. H. Sondak (New York, NY: Elsevier), 85–113. doi: 10.1016/S1534-0856(02)04005-7
Galinsky, A. D., and Ku, G. (2004). The effects of perspective-taking on prejudice: The moderating role of self-evaluation. Pers. Soc. Psychol. Bull. 30, 594–604. doi: 10.1177/0146167203262802
Galinsky, A. D., and Moskowitz, G. B. (2000). Perspective-taking: decreasing stereotype expression, stereotype accessibility, and in-group favoritism. J. Pers. Soc. Psychol. 78, 708–724. doi: 10.1037/0022-3514.78.4.708
Gapinski, K. D., Schwartz, M. B., and Brownell, K. D. (2006). Can television change anti-fat attitudes and behavior? J. Appl. Biobehav. Res. 11, 1–28. doi: 10.1111/j.1751-9861.2006.tb00017.x
Gloor, J. L., and Puhl, R. M. (2016). Empathy and perspective-taking: examination and comparison of strategies to reduce weight stigma. Stigma Health 1, 269–279. doi: 10.1037/sah0000030
Hair, J. F., Black, W. C., Babin, B. J., and Anderson, R. E. (2010). Multivariate Data Analysis, 7th Edn. New York, NY: Pearson Prentice Hall.
Google Scholar
Huang, Q., Peng, W., and Simmons, J. V. (2020). Assessing the evidence of perspective taking on stereotyping and negative evaluations: a p-curve analysis. Group Process. Intergroup Relat. doi: 10.1177/1368430220957081. [Epub ahead of print].
Ku, G., Wang, C. S., and Galinsky, A. D. (2010). Perception through a perspective-taking lens: differential effects on judgment and behavior. J. Exp. Soc. Psychol. 46, 792–798. doi: 10.1016/j.jesp.2010.04.001
Lau, R. S., and Cheung, G. W. (2012). Estimating and comparing specific mediation effects in complex latent variable models. Organ. Res. Methods 15, 3–16. doi: 10.1177/1094428110391673
Laurent, S. M., and Myers, M. W. (2011). I know you're me, but who am I? Perspective taking and seeing the other in the self. J. Exp. Soc. Psychol. 47, 1316–1319. doi: 10.1016/j.jesp.2011.05.018
Li, P. F. (2017). A study of the impact ofPT on the college students' HIV/AIDS Prejudice . [master's thesis]. (Chengdu, Sichuan): Sichuan Normal University.
Myers, M. W., and Hodges, S. D. (2012). The structure of self-other overlap and its relationship to perspective taking. Pers. Relat. 19, 663–679. doi: 10.1111/j.1475-6811.2011.01382.x
Pettigrew, T. F., and Tropp, L. R. (2006). A meta-analytic test of intergroup contact theory. J. Pers. Soc. Psychol. 90, 751–783. doi: 10.1037/0022-3514.90.5.751
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., and Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 88, 879–903. doi: 10.1037/0021-9010.88.5.879
Puhl, R. M., Andreyeva, T., and Brownell, K. D. (2008). Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int. J. Obes. 32, 992–1000. doi: 10.1038/ijo.2008.22
Puhl, R. M., and Heuer, C. A. (2009). The stigma of obesity: a review and update. Obesity 17, 941–964. doi: 10.1038/oby.2008.636
Puhl, R. M., and King, K. M. (2013). Weight discrimination and bullying. Best Pract. Res. Clin. Endocrinol. Metab. 27, 117–127. doi: 10.1016/j.beem.2012.12.002
Puhl, R. M., and Latner, J. D. (2007). Stigma, obesity, and the health of the nation's children. Psychol. Bull. 133, 557–580. doi: 10.1037/0033-2909.133.4.557
Sarlio-Lähteenkorva, S. (2001). Weight loss and quality of life among obese people. Soc. Indic. Res. 54, 329–354. doi: 10.1023/A:1010939602686
Shih, M., Wang, E., Trahan Bucher, A., and Stotzer, R. (2009). Perspective taking: reducing prejudice towards general outgroups and specific individuals. Group Process. Intergroup Relat. 12, 565–577. doi: 10.1177/1368430209337463
Skorinko, J. L., and Sinclair, S. A. (2013). Perspective taking can increase stereotyping: the role of apparent stereotype confirmation. J. Exp. Soc. Psychol. 49, 10–18. doi: 10.1016/j.jesp.2012.07.009
Sun, S., Zuo, B., Wu, Y., and Wen, F. (2016). Does perspective taking increase or decrease stereotyping? The role of need for cognitive closure. Pers. Individ. Differ. 94, 21–25. doi: 10.1016/j.paid.2016.01.001
Taylor, S. E., and Brown, J. (1988). Illusion and well-being: a social psychological perspective on mental health. Psychol. Bull. 103, 193–210. doi: 10.1037/0033-2909.103.2.193
Teachman, B. A., Gapinski, K. D., Brownell, K. D., Rawlins, M., and Jeyaram, S. (2003). Demonstrations of implicit anti-fat bias: the impact of providing causal information and evoking empathy. Health Psychol. 22, 68–78. doi: 10.1037/0278-6133.22.1.68
Tiggemann, M., and Anesbury, T. (2000). Negative stereotyping of obesity in children: the role of controllability beliefs. J. Appl. Soc. Psychol. 30, 1977–1993. doi: 10.1111/j.1559-1816.2000.tb02477.x
Tiggemann, M., and Rothblum, E. D. (1988). Gender difference in social consequences of perceived overweight in the United States and Australia. Sex Roles 18, 75–86. doi: 10.1007/BF00288018
Todd, A. R., Bodenhausen, G. V., and Galinsky, A. D. (2012). Perspective taking combats the denial of intergroup discrimination. J. Exp. Soc. Psychol. 48, 738–745. doi: 10.1016/j.jesp.2011.12.011
Todd, A. R., Bodenhausen, G. V., Richeson, J. A., and Galinsky, A. D. (2011). Perspective taking combats automatic expressions of racial bias. J. Pers. Soc. Psychol. 100, 1027–1042. doi: 10.1037/a0022308
Todd, A. R., and Burgmer, P. (2013). Perspective taking and automatic intergroup evaluation change: testing an associative self-anchoring account. J. Pers. Soc. Psychol. 104, 786–802. doi: 10.1037/a0031999
Todd, A. R., and Galinsky, A. D. (2014). Perspective-taking as a strategy for improving intergroup relations: evidence, mechanisms, and qualifications. Soc. Pers. Psychol. Compass 8, 374–387. doi: 10.1111/spc3.12116
Vartanian, L. R., Trewartha, T., and Vanman, E. J. (2015). Disgust predicts prejudice and discrimination toward individuals with obesity. J. Appl. Soc. Psychol. 46, 369–375. doi: 10.1111/jasp.12370
Vescio, T. K., Sechrist, G. B., and Paolucci, M. P. (2003). Perspective taking and prejudice reduction: the mediational role of empathy arousal and situational attributions. Eur. J. Soc. Psychol. 33, 455–472. doi: 10.1002/ejsp.163
Wang, C. S., Ku, G., Tai, K., and Galinsky, A. D. (2014). Stupid doctors and smart construction workers:PT reduces stereotyping of both negative and positive targets. Soc. Psychol. Pers. Sci. 5, 430–436. doi: 10.1177/1948550613504968
Wang, C. S., Lee, M., Ku, G., and Leung, A. K. (2018). The cultural boundaries of Perspective-taking: when and why Perspective-taking reduces stereotyping. Pers. Soc. Psychol. Bull. 44, 928–943. doi: 10.1177/0146167218757453
Wang, L. L. (2018). A study on the influence of perspective taking on homosexual stigma among the college students . [master's thesis]. [Chengdu, Sichuan]: Sichuan Normal University.
Wang, Y. A., and Rhemtulla, M. (2021). Power analysis for parameter estimation in structural equation modeling: a discussion and tutorial. Adv. Methods Pract. Psychol. Sci. 4, 1–17. doi: 10.31234/osf.io/pj67b
Williams, L. J., Vandenberg, R. J., and Edwards, J. R. (2009). 12 structural equation modeling in management research: a guide for improved analysis. Acad. Manag. Ann. 3, 543–604. doi: 10.5465/19416520903065683
Zhan, Z. Y. (1986). The relationship between grade, sex-role, human relationship orientation and empathy . [master's thesis]. [Taipei, Taiwan]: National Chengchi University.
Zhang, F. F., Dong, Y., Wang, K., Zhan, Z. Y., and Xie, L. F. (2010). Reliability and validity of the Chinese version of the interpersonal reactivity index-C. Chi. J. Clin. Psychol. 18, 25–27. doi: 10.16128/j.cnki.1005-3611.2010.02.019
Keywords: obesity stereotypes, perspective taking, empathy, self-other overlap, dual mediating effects
Citation: Wu Y and Zhang Y (2021) The Impact of Perspective Taking on Obesity Stereotypes: The Dual Mediating Effects of Self-Other Overlap and Empathy. Front. Psychol. 12:643708. doi: 10.3389/fpsyg.2021.643708
Received: 18 December 2020; Accepted: 12 July 2021; Published: 12 August 2021.
Reviewed by:
Copyright © 2021 Wu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuzhu Zhang, nsdzyz@163.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
The Impact of Perspective Taking on Obesity Stereotypes: The Dual Mediating Effects of Self-Other Overlap and Empathy
Affiliation.
- 1 School of Psychology, Inner Mongolia Normal University, Hohhot, China.
- PMID: 34456781
- PMCID: PMC8387714
- DOI: 10.3389/fpsyg.2021.643708
Previous studies have indicated that obese people face many forms of severe prejudice and discrimination in various settings, such as education, employment, and interpersonal relationships. However, research aimed at reducing obesity stereotyping is relatively rare, and prior studies have focused primarily on negative stereotypes. Based on the empathy-altruism hypothesis and self-other overlap hypothesis, this study investigates the impact of perspective taking (PT) on both positive and negative obesity stereotypes and examines the mediating effects of empathy and self-other overlap. A sample of 687 students (191 males and 496 females) at Chinese universities participated by completing self-report questionnaires on trait tendency and evaluation toward obese people. Structural equation modeling and the bootstrap method revealed that self-other overlap (but not empathy) mediated the relationship between PT and negative obesity stereotypes. While self-other overlap and empathy both mediated the relationship between PT and positive obesity stereotypes. These findings address the importance of PT for improving positive and negative obesity stereotypes: specifically, PT promotes psychological merging, and produces empathic concern (EC).
Keywords: dual mediating effects; empathy; obesity stereotypes; perspective taking; self-other overlap.
Copyright © 2021 Wu and Zhang.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 20 December 2021
Behavior, Psychology and Sociology
Weight-based stereotype threat in the workplace: consequences for employees with overweight or obesity
- Hannes Zacher ORCID: orcid.org/0000-0001-6336-2947 1 &
- Courtney von Hippel 2
International Journal of Obesity volume 46 , pages 767–773 ( 2022 ) Cite this article
9170 Accesses
4 Citations
6 Altmetric
Metrics details
- Patient education
Background/Objectives
Employees with overweight or obesity are often stereotyped as lazy, unmotivated, and less competent than employees with normal weight. As a consequence, employees with overweight or obesity are susceptible to stereotype threat, or the concern about confirming, or being reduced to, a stereotype about their group. This survey study examined whether employees with overweight or obesity experience stereotype threat in the workplace, whether it is associated with their perceived ability to meet their work demands (i.e., work ability), and whether high levels of knowledge about one’s self (i.e., authentic self-awareness) can offset a potential negative association.
Subjects/Methods
Using a correlational study design, survey data were collected from N = 758 full-time employees at three measurement points across 3 months. Employees’ average body mass index (BMI) was 26.36 kg/m² (SD = 5.45); 34% of participants were employees with overweight (BMI between 25 and <30), and 18% of participants were employees with obesity (BMI > 30).
Employees with higher weight and higher BMI reported more weight-based stereotype threat ( r s between 0.17 and 0.19, p < 0.001). Employees who experienced higher levels of weight-based stereotype threat reported lower work ability, while controlling for weight, height, and subjective weight ( β = −0.27, p < 0.001). Authentic self-awareness moderated the relationship between weight-based stereotype threat and work ability ( β = 0.14, p < 0.001), such that the relationship between stereotype threat and work ability was negative among employees with low authentic self-awareness ( β = −0.25, p < 0.001), and non-significant among employees with high authentic self-awareness ( β = 0.08, p = 0.315).
Conclusions
The findings of this study contribute to the literature by showing that weight-based stereotype threat is negatively associated with employees’ perceived ability to meet their work demands, particularly among those employees with low authentic self-awareness.
Similar content being viewed by others

A qualitative exploration of individual differences in wellbeing for highly sensitive individuals
Becky A. Black & Margaret L. Kern
Weight biases, body image and obesity risk knowledge in the groups of nursing students from Poland and Nigeria
Wojciech Styk, Marzena Samardakiewicz & Szymon Zmorzynski

Sport–gender stereotypes and their impact on impression evaluations
Zhiyuan Liu, Menglu Shentu, … Weiqi Zheng
People with overweight or obesity face prejudice and discrimination in various aspects of their lives, such as healthcare, education, and interpersonal relationships [ 1 ]. Unfortunately, the employment context is no exception. Employees with overweight or obesity are stereotyped to lack self-discipline, self-control, and willpower [ 2 , 3 ], and are seen as less competent and conscientious [ 4 ]. In light of these stereotypes, it is not surprising that cross-sectional surveys, population-based research, and experimental studies demonstrate that people with overweight or obesity experience bias with regard to a variety of workplace outcomes [ 1 ]. For example, compared to people with normal weight, people with overweight or obesity are less likely to be hired [ 5 , 6 ], receive lower pay [ 7 ], and are less likely to receive promotions [ 8 ]. Employees with overweight or obesity also report being the subject of derogatory comments and other uncivil behaviors from their supervisors and co-workers [ 9 ]. In short, employees with overweight or obesity are stigmatized and discriminated against in the workplace [ 1 ], raising the clear possibility that these employees will be susceptible to stereotype threat.
According to stereotype threat theory [ 10 ], concerns about being stereotyped based on one’s group membership can lead people to psychologically distance themselves from domain-relevant activities and performance. That is, stereotype threat can lead to disidentification—or disengagement—from the task domain. Although the majority of stereotype threat research has taken place in a laboratory setting [ 11 ], a growing body of research demonstrates that stereotype threat is also important in the workplace [ 12 , 13 ]. Research in organizational contexts demonstrates that stigmatized groups (e.g., older employees; women in male-dominated fields) disengage from work when they experience stereotype threat [ 12 , 14 ]. Given the growing percentage of people with overweight or obesity worldwide [ 15 ], it is important to examine whether employees with overweight or obesity experience stereotype threat in the workplace, whether it is associated with their perceived ability to meet their work demands, and whether other psychological factors can offset a potential negative association.
Although the stereotypes about employees with overweight or obesity are varied, many focus on the notion that they are less capable [ 4 ]. Over time, people from stereotyped groups can internalize the stigma about their group [ 16 ]. If employees with overweight or obesity internalize the stigma that they are less capable at work than their colleagues with normal weight, then feelings of stereotype threat should lead to lowered perceptions of work ability, or the perceived capacity to continue working in their current job given their perceptions of their physical, cognitive, and interpersonal job demands and their ability to meet these demands [ 17 , 18 ]. In short, employees’ experience of weight-based stereotype threat should lead them to believe they are less capable of meeting the demands of their job.
The moderating role of authentic self-awareness
Scholarly interest in employee authenticity, or “being your true self at work,” has rapidly increased over the past few years [ 19 ]. Authentic self-awareness is the extent of knowledge (and trust in that knowledge) about various aspects of one’s self and the motivation to expand that knowledge [ 20 ]. Employees with high levels of authentic self-awareness consider their self as a whole (e.g., physical appearance, internal states including cognitions and emotions, motives and intentions, social commitments) and are invested in understanding and learning more about their “true self” [ 21 ]. Research has shown that employees’ authentic self-awareness is empirically distinct from, but moderately and positively associated with self-insight (i.e., clarity of understanding various aspects of one’s self), self-acceptance (i.e., positive attitude to one’s self), and self-esteem (i.e., confidence in one’s own worth), and negatively associated with anxiety, cognitive and emotional strain, and ill-health [ 21 ].
We predict that weight-based stereotype threat generally is negatively related to work ability, but that high (vs. low) levels of authentic self-awareness may buffer this negative association. This prediction is based on theorizing that employees who better understand themselves are less likely to comply with unwanted social and situational pressures in their work environment and react less strongly to others’ demands and workplace stressors [ 21 ]. Thus, authentic self-awareness may constitute a coping mechanism that helps employees deal with the stressor of weight-based stereotype threat [ 22 , 23 ]. Consistent with this possibility, experimental work has shown that people who have a more stable sense of self—a trait that is associated with greater self-concept clarity [ 24 ] and greater integration of positive and negative information [ 25 ]—are more likely to treat negative feedback as a challenge rather than a hindrance [ 26 ]. Clarity and stability of the self-concept, as well as integration of positive and negative information into the self-concept, are all important components of authentic self-awareness [ 20 , 27 ].
Additionally, employees who possess a holistic and differentiated understanding of their self and who are motivated to continuously improve their self-understanding should have a broader and more effective set of psychological coping strategies (e.g., positive reframing, reappraisal) at their disposal when they feel stereotyped [ 28 , 29 ]. That is, when faced with weight-based stereotype threat, they should be more capable of restoring a sense of themselves as capable employees through consideration of numerous other aspects of their self-concept. In contrast, employees with low authentic self-awareness do not adopt a broad perspective on their self and are less interested in learning more about its elements. With less self-knowledge at their disposal, these employees should be more susceptible to the negative effects of weight-based stereotype threat. Consistent with this possibility, inauthenticity has been hypothesized to result in employees who are more likely to comply with stereotypes [ 30 ]. Thus, employees’ authentic self-awareness should moderate the negative relationship between weight-based stereotype threat and work ability, such that weight-based stereotype threat is associated with greater deficits in work ability when authentic self-awareness is low than when authentic self-awareness is high.
Participants and procedure
We conducted a correlational survey study with three measurement points over a period of 3 months, incorporating an initial survey with demographic and control variables (Time [T] 1) as well as two subsequent surveys (T2 and T3) that included measures of weight-based stereotype threat, work ability, and authentic self-awareness. We used a time lag of four weeks between measurement points in an effort to ensure that participants could recall their concerns and experiences at work. Data for this study were collected as part of a larger data collection effort, and so far two other studies based on the same dataset, but with completely different research questions and completely different substantive variables, have been published [ 31 , 32 ]. In Germany, correlational studies are exempt from institutional review board approval. The research was conducted in line with the ethical guidelines and requirements of the German Psychological Society. Participation in the study was voluntary and anonymous, and informed consent was obtained from all participants.
We commissioned a professional and ISO 26362 certified panel provider to recruit participants from a nationally representative online panel in Germany. To be eligible for inclusion, participants had to be at least 18 years old and working full-time. Approximately 3500 participants were initially contacted with a request to participate in the first measurement wave (T1). This number of initial participants was determined based on the panel provider’s recommendations to obtain a final sample size of 750 participants or more at T3, which is sufficient to detect small correlational effect sizes (i.e., r ≥ 0.10) with high (i.e., ≥0.80) statistical power [ 33 ]. Of those 3500 contacted, 1522 responded and were eligible to participate according to our selected inclusion criteria. Of these 1522 who qualified, 758 consented to participate and provided complete data on all three measurement occasions.
The sample was comprised of 438 (57.8%) men and 320 women (42.2%). Participants’ age ranged from 21 to 74 years with a mean age of 43.83 years (SD = 10.70). Most participants held either a lower-secondary school degree (228; 30.1%), a higher-secondary school degree (137; 18.1%), or a college/university degree (241; 31.8%). Participants worked across 21 different industries, with the public administrative sector (12.7%), manufacturing (12.8%), and healthcare (10.3%) most represented.
Overall, body mass index (BMI) values of participants at T1 ranged from 16.71 to 60.22, with an average BMI of 26.36 kg/m² (SD = 5.45). More specifically, only 17 participants (2%) were employees with underweight (BMI < 18.5), whereas 346 participants (46%) were employees with normal weight (BMI between 18.5 to <25), 260 participants (34%) were employees with overweight (BMI between 25 and <30), and 135 participants (18%) were employees with obesity (BMI > 30).
Weight-based stereotype threat
We assessed weight-based stereotype threat by self-report at T2 and T3 using an adapted version of a 5-item stereotype threat scale [ 34 , 35 ], which was itself adapted from a scale to measure stereotype threat in a laboratory context [ 36 ]. We adapted the items by referring to participants’ weight instead of their gender or age as in previous studies. Participants were asked to report on their feelings of weight-based stereotype threat within the last 4 weeks. The items followed the introductory statement “Last month (in the last 4 weeks) I worried that…,” and were: “…some people at my workplace felt I have less ability because of my weight,” “…people at my workplace drew conclusions about my ability based on my weight,” “…some people at my workplace felt that I’m not committed to my work because of my weight,” “…some people at my workplace felt that I have less to contribute at work because of my weight,” “…my behavior caused people in my workplace to think that stereotypes about people of my weight are true.” Responses were provided on a five-point scale from 1 (never) to 5 (always). Reliability for the scale was high at both T2 (Cronbach’s α = 0.97) and T3 ( α = 0.98).
Authentic self-awareness
We measured employees’ authentic self-awareness at T2 using a four-item scale [ 21 ]. Specifically, we asked participants to think about the last 4 weeks when responding to the following items on a five-point scale ranging from 1 (not true at all) to 5 (completely true): “I understood why I thought about myself as I did,” “For better or worse, I knew who I really was,” “I understood well why I behaved like I did,” and “I felt like I didn’t know myself particularly well” (reverse coded). Alpha for the scale was 0.71.
Work ability
We measured employees’ perceived work ability at T2 and T3 using a four-item measure [ 17 ], which was based on three items from the work ability index [ 37 ] and one additional item on interpersonal demands adapted from the work ability index [ 38 ]. Participants were asked, “Please evaluate your ability in the last month (the last 4 weeks) to meet the following demands of your work.” The first three items were, “Thinking about the [physical, mental, interpersonal] demands of your work, how do your rate your ability to meet those demands?” and the fourth item was, “How many points would you give your overall ability to work?” Responses were provided on a scale from 0 (was unable to work at all) to 10 (my work ability was at its lifetime best). Reliability for the scale was α = 0.92 at T2 and α = 0.92 at T3.
Control variables
At T1, we assessed employees’ age (in years), gender (1 = male, 2 = female), highest level of education (1 = some high school to 7 = college/university degree), weight (in kilograms), height (in cms), and subjective weight. We measured subjective weight with a single item: “How would you describe your weight?” Responses were provided on a scale ranging from 1 (severely underweight) to 5 (severely overweight). We did not control for BMI, as it was highly correlated with objective and subjective weight (see Table 1 ).
Table 1 shows the means, standard deviations (SD), and correlations of all study variables. Weight, subjective weight, and BMI were positively related to weight-based stereotype threat, whereas age, authentic self-awareness, and work ability were negatively associated with weight-based stereotype threat. An exploratory analysis revealed that weight and BMI did not have curvilinear relationships with weight-based stereotype threat, suggesting that stereotype threat was generally lower among employees with lower weight and lower BMI and higher among employees with higher weight and higher BMI.
Table 2 reports the results of the regression analyses. A Kolmogorov–Smirnov test indicated that our main outcome variable, T3 work ability, was not normally distributed, D (758) = 0.108, p < 0.001. However, given our large sample size, the fact that there were more than 75 observations per predictor variable, and the sizeable SD (SD = 1.82; see Table 1 ), this violation of the normality assumption of regression analysis is not a primary concern for this study [ 39 ]. Consistent with expectations, weight-based stereotype threat was negatively related to work ability. As shown in Table 2 (Model 1), T2 weight-based stereotype threat was negatively associated with T3 work ability above and beyond the T1 control variables ( β = −0.27, p < 0.001), suggesting that employees who felt higher levels of stereotype threat subsequently perceived lower work ability. Together, weight-based stereotype threat and the control variables explained 11 percent of the variance in work ability. An additional analysis showed that the interaction between gender and weight-based stereotype threat was not significantly associated with work ability ( β = −0.03, p = 0.346), suggesting that the relationship between stereotype threat and work ability is consistent for men and women. The relationship between weight-based stereotype threat and work ability was similar when considering only employees with overweight (i.e., BMI between 25 and <30; β = −0.20, p = 0.003), only employees with obesity (i.e., BMI > 30; β = −0.31, p < 0.001), or both of these groups combined in the analysis ( β = −0.25, p < 0.001).
Next, we tested the prediction that authentic self-awareness moderates the relationship between weight-based stereotype threat and work ability. As shown in Table 2 (Model 2), a significant interaction emerged between weight-based stereotype threat and authentic awareness ( β = 0.14, p < 0.001) which, together with the main effect of authentic self-awareness, explained an additional eight percent of the variance in work ability. This interaction is graphically shown in Fig. 1A . Simple slope analyses showed that the relationship between weight-based stereotype threat and work ability was negative and significant at low (−1 SD) levels of authentic self-awareness ( B = −0.46, SE = 0.08, β = −0.25, t = −5.80, p < 0.001) and weak and non-significant at high (+1 SD) levels of authentic self-awareness ( B = 0.14, SE = 0.14, β = 0.08, t = 1.01, p = 0.315). An additional analysis showed that a three-way interaction between gender, weight-based stereotype threat, and authentic self-awareness (while controlling for the respective main effects and two-way interaction terms) was not associated with work ability ( β = −0.03, p = 0.413). The interaction between weight-based stereotype threat and authentic self-awareness was also significant when only considering employees with overweight in the analysis (i.e., BMI between 25 and <30; β = 0.15, p = 0.034), whereas it was not significant when considering only employees with obesity (i.e., BMI > 30; β = −0.02, p = 0.843) or both of these groups combined in the analysis ( β = 0.07, p = 0.163). Overall, these findings suggest that weight-based stereotype threat was negatively associated with work ability among employees with obesity, as well as among those employees with normal weight or overweight who had low levels of authentic self-awareness. In contrast, weight-based stereotype threat was not significantly associated with work ability among employees with normal weight or overweight who had high levels of authentic self-awareness.
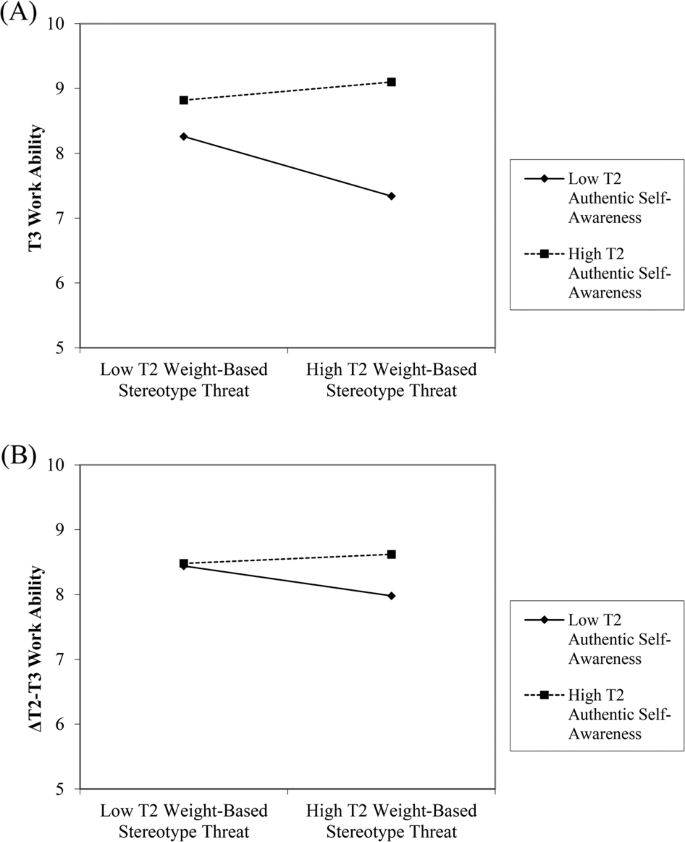
Effects of T2 weight-based stereotype threat on ( A ) T3 work ability (without controlling for T2 work ability) and ( B ) T3 work ability (controlling for T2 work ability) moderated by T2 authentic self-awareness.
Supplemental analyses
We conducted a supplemental analysis in which we additionally controlled for baseline (T2) work ability (Model 3, Table 2 ). The patterns of results of this lagged endogenous change model [ 40 , 41 ] did not differ substantially from the results reported above. In particular, results suggest that the interaction between weight-based stereotype threat and authentic self-awareness was associated with change in work ability from T2 to T3 ( β = 0.07, p = 0.039). The significant interaction effect is shown in Fig. 1B . Simple slope analyses showed that the relationship between weight-based stereotype threat and change in work ability was negative and significant at low (−1 SD) levels of authentic self-awareness ( B = −0.23, SE = 0.07, β = −0.13, t = −3.22, p = 0.001) and weak and non-significant at high (+1 SD) levels of authentic self-awareness ( B = 0.07, SE = 0.12, β = 0.04, t = 0.55, p = 0.585). Again, a three-way interaction between gender, weight-based stereotype threat, and authentic self-awareness was not significantly associated with work ability ( β = 0.02, p = 0.659). Additional analyses with only employees with overweight ( β = 0.05, p = 0.378), only employees with obesity ( β = −0.03, p = 0.729), or both of these groups combined ( β = 0.01, p = 0.852) did not yield significant interaction effects. However, T2 weight-based stereotype threat still had a negative main effect when only considering employees with obesity in this analysis ( β = −0.20, p = 0.026).
To test whether the temporal order of variables we proposed represents the best fit to the data, we also estimated a reverse temporal order model in which we regressed T3 weight-based stereotype threat on the control variables, baseline (T2) weight-based stereotype threat, work ability, authentic self-awareness, and the interaction of work ability and authentic self-awareness (Model 4, Table 2 ). As shown in Model 4 (Table 2 ), age ( β = −0.07, p = 0.004) and authentic self-awareness ( β = −0.06, p = 0.044) were weakly and negatively associated with change in weight-based stereotype threat. In contrast, T2 work ability and the interaction between work ability and authentic self-awareness were not significantly associated with change in weight-based stereotype threat. An additional analysis showed that a three-way interaction between gender, work ability, and authentic self-awareness was not significantly associated with change in weight-based stereotype threat ( β = −0.04, p = 0.154). The interaction between work ability and authentic self-awareness was also non-significant when considering only employees with overweight ( β = 0.06, p = 0.092), only employees with obesity ( β = −0.08, p = 0.293), or both of these groups combined ( β = 0.01, p = 0.659).
Consistent with expectations, our correlational survey study showed that the experience of weight-based stereotype threat was associated with lower levels of work ability, and this relationship was qualified by authentic self-awareness. Specifically, the relationship between weight-based stereotype threat and work ability was non-significant among employees with higher authentic self-awareness, whereas employees with lower authentic self-awareness reported lower work ability when they experienced weight-based stereotype threat. This interaction effect was weaker, but still significant, when baseline levels of work ability were controlled, suggesting that the interaction between weight-based stereotype threat and authentic self-awareness is associated with mean-level changes in work ability across 1 month.
These findings, albeit correlational and not causal, advance research on stereotype threat, work ability, and authenticity. Most research on stereotype threat has been conducted in the laboratory, and stereotype threat research in a work context has neglected weight-based stereotype threat [ 12 ]. The current results demonstrate that employees with overweight or obesity experience weight-based stereotype threat and this concern, in turn, can diminish their sense of work ability. Work ability is associated with increased absenteeism, disability leave, and early retirement [ 17 ], suggesting that weight-based stereotype threat might be indirectly related to these outcomes. Indeed, this has been shown for other forms of stereotype threat in the workplace [ 42 ]. Additionally, if stereotype threat is negatively associated with work ability it might create a vicious cycle whereby diminished work ability fuels the stereotypes about people with overweight or obesity, thereby making these employees even more susceptible to stereotype threat.
Our findings are consistent with prior research suggesting that high authentic self-awareness constitutes a psychological resource and coping mechanism [ 19 , 20 , 21 ], as it seems to make employees less susceptible to the detrimental consequences of weight-based stereotype threat. It is important to note, however, that authentic self-awareness did not moderate the association between weight-based stereotype threat and work ability when only employees with obesity were considered in the analysis. Due to the fact that these employees are the most overweight and hence the most easily identified as such, it is not surprising that they were also found to be more susceptible to weight-based stereotype threat than employees with overweight or normal weight (i.e., we found positive linear relationships of weight and BMI with weight-based stereotype threat). Thus, it seems likely that authentic self-awareness may only serve a protective function among employees who experience relatively lower levels of stereotype threat (in the current case, employees with overweight, but not those with obesity).
Finally, the bivariate correlations showed that older employees weighed more and had higher BMIs, but nonetheless experienced less weight-based stereotype threat than younger employees. While the former finding is consistent with the literature on work and health [ 43 ], a potential explanation for the latter finding is that older employees have accumulated more work and life experience and may, therefore, be less concerned that other people at work reduce them to weight-based stereotypes. Moreover, the positive relationship between age and authentic self-awareness suggests that older employees possess greater knowledge about various aspects of their selves and, thus, may be less susceptible to experiencing weight-based stereotype threat.
Limitations and future research
This study integrates psychological theorizing on stereotype threat with the literature on obesity and weight stigma to examine the consequences of weight-based stereotype threat in the workplace. Most weight-stigma research focuses on women with overweight [ 44 , 45 ], whereas our sample includes men and women. Additional analyses showed that two- and three-way interactions of gender with weight-based stereotype threat and authentic self-awareness were not significantly associated with work ability. Nevertheless, examining both genders continues to be important in light of the inconsistent associations of weight stigma with potential outcome variables in a workplace context, with some research showing men to be more susceptible and other research showing women to be more susceptible to weight-based prejudice and discrimination (see [ 1 ]). Thus, further research is needed that addresses the issue of intersectionality, or how the combination of gender, weight, and other relevant characteristics may be associated with potential detrimental consequences in the workplace [ 46 , 47 ].
Nonetheless, this study has a number of limitations that should be addressed in future research. First, all of the constructs in our study were assessed using self-report, which may raise concerns about artificially inflated associations due to common method bias. However, following methodological recommendations [ 48 ], we temporally separated measurements of our predictor and outcome variables. Additionally, our predictor, moderator and outcome variables used different response scales, helping to further combat common method variance [ 49 ]. Perhaps most importantly, methodologists have demonstrated that interaction effects are not inflated by common method bias [ 50 ]. Nonetheless, research demonstrates that self- and other-reports of authentic self-awareness are weak and non-significant [ 21 ], suggesting there may be limitations in the accessibility of self-knowledge or that self-presentation biases people’s judgements [ 51 ]. To address this possibility, future research could supplement self-report measures of authentic self-awareness with reports obtained from other people (e.g., co-workers, family members).
Second, although work ability is an important outcome, future studies should examine the associations of weight-based stereotype threat with additional engagement- and disengagement-related work outcomes. Research with employees from other stigmatized groups demonstrates that stereotype threat is associated with more negative job attitudes and increased intentions to quit [ 12 ]. Lower work ability also relates to more negative attitudes and intentions to quit [ 17 ], raising the possibility that work ability may play a mediating role between the experience of stereotype threat and these outcomes.
Previous research has neglected the potential consequences of weight-based stereotype threat in the work context. Consistent with stereotype threat theory, we found a negative relationship between employees’ experiences of weight-based stereotype threat and work ability, which was weaker among those with higher levels of authentic self-awareness. Thus, organizations should identify ways to enhance authentic self-awareness, particularly among employees who may be susceptible to the negative effects of weight-based stereotype threat.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–64.
Article PubMed Google Scholar
Bellizzi JA, Norvell DW. Personal characteristics and salesperson’s justifications as moderators of supervisory discipline in cases involving unethical salesforce behavior. J Acad Mark Sci. 1991;19:11–6.
Article Google Scholar
Brochu PM, Esses VM. What’s in a name? The effects of the labels “fat” versus “overweight” on weight bias. J Appl Soc Psychol. 2011;41:1981–2008.
Rudolph CW, Wells CL, Weller MD, Baltes BB. A meta-analysis of empirical studies of weight-based bias in the workplace. J Vocat Behav. 2009;74:1–10.
Campos-Vazquez RM, Gonzalez E. Obesity and hiring discrimination. Econ Hum Biol. 2020;37:100850.
Klarenbach S, Padwal R, Chuck A, Jacobs P. Population‐based analysis of obesity and workforce participation. Obesity. 2006;14:920–7.
Judge TA, Cable DM. When it comes to pay, do the thin win? The effect of weight on pay for men and women. J Appl Psychol. 2011;96:95–112.
Lindeman MI, Crandall AK, Finkelstein LM. The effects of messages about the causes of obesity on disciplinary action decisions for overweight employees. J Psychol. 2017;151:345–58.
Sliter KA, Sliter MT, Withrow SA, Jex SM. Employee adiposity and incivility: establishing a link and identifying demographic moderators and negative consequences. J Occup Health Psychol. 2012;17:409–24.
Steele CM. A threat in the air: How stereotypes shape intellectual identity and performance. Am Psychol. 1997;52:613–29.
Article CAS PubMed Google Scholar
Spencer SJ, Logel C, Davies PG. Stereotype threat. Annu Rev Psychol. 2016;67:415–37.
Kalokerinos EK, Von Hippel C, Zacher H. Is stereotype threat a useful construct for organizational psychology research and practice? Ind Organ Psychol. 2014;7:381–402.
von Hippel C. Stereotype threat in the workplace. In: Paludi M, editor. Managing diversity in today’s workplaces. Santa Barbara, CA: ABC-CLIO; 2012.
Roberson L, Kulik CT. Stereotype threat at work. Acad Manag Perspect. 2007;21:24–40.
World Health Organization. Obesity and overweight. 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight .
Guardabassi V, Tomasetto C. Does weight stigma reduce working memory? Evidence of stereotype threat susceptibility in adults with obesity. Int J Obes. 2018;42:1500–7.
McGonagle A, Fisher GG, Barnes‐Farrell JL, Grosch J. Individual and work factors related to perceived work ability and labor force outcomes. J Appl Psychol. 2015;100:376–98.
Ilmarinen J. Work ability: a comprehensive concept for occupational health research and prevention. Scand J Work Environ Health. 2009;35:1–5.
Cha SE, Hewlin PF, Roberts LM, Buckman BR, Leroy H, Steckler EL, et al. Being your true self at work: Integrating the fragmented research on authenticity in organizations. Acad Manag Ann. 2019;13:633–71.
Kernis MH, Goldman BM. A multicomponent conceptualization of authenticity: theory and research. Adv Exp Soc Psychol. 2006;38:283–357.
Knoll M, Meyer B, Kroemer NB, Schröder-Abé M. It takes two to be yourself: an integrated model of authenticity, its measurement, and its relationship to work-related variables. J Individ Differ. 2015;36:38–53.
Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity. 2006;14:1802–15.
Himmelstein MS, Puhl RM, Quinn DM. Weight stigma and health: the mediating role of coping responses. Health Psycho. 2018;37:139–47.
Campbell JD, Trapnell PD, Heine SJ, Katz IM, Lavallee LF, Lehman DR. Self-concept clarity: measurement, personality correlates, and cultural boundaries. J Pers Soc Psychol. 1996;70:141–56.
Zeigler-Hill V, Showers CJ. Self-structure and self-esteem stability: the hidden vulnerability of compartmentalization. Pers Soc Psychol Bull. 2007;33:143–59.
Seery MD, Blascovich J, Weisbuch M, Vick SB. The relationship between self-esteem level, self-esteem stability, and cardiovascular reactions to performance feedback. J Pers Soc Psychol. 2004;87:133–45.
Sheldon KM, Ryan RM, Rawsthorne LJ, Ilardi B. Trait self and true self: cross-role variation in the Big-Five personality traits and its relations with psychological authenticity and subjective well-being. J Pers Soc Psychol. 1997;73:1380–93.
Hayward LE, Vartanian LR, Pinkus RT. Coping with weight stigma: development and validation of a brief coping responses inventory. Obes Sci Pract. 2017;3:373–83.
Article CAS PubMed PubMed Central Google Scholar
Himmelstein MS, Puhl RM, Pearl RL, Pinto AM, Foster GD. Coping with weight stigma among adults in a commercial weight management sample. Int J Behav Med. 2020;27:576–90.
Avolio BJ, Gardner WL. Authentic leadership development: getting to the root of positive forms of leadership. Leadersh Q. 2005;16:315–38.
Weiss M, Zacher H. Why and when does voice lead to increased job engagement? The role of perceived voice appreciation and emotional stability. J Vocat Behav. 2022;132:103662.
Zacher H, Rudolph CW. Strength and vulnerability: indirect effects of age on changes in occupational well-being through emotion regulation and physiological disease. Psychol Aging. 2021; https://doi.org/10.1037/pag0000671 .
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum; 1988.
Google Scholar
von Hippel C, Issa M, Ma R, Stokes A. Stereotype threat: antecedents and consequences for working women. Eur J Soc Psychol. 2011;41:151–61.
von Hippel C, Kalokerinos EK, Henry JD. Stereotype threat among older employees: relationships with job attitudes and turnover intentions. Psychol Aging. 2013;28:17–27.
Steele CM, Aronson J. Stereotype threat and the intellectual test performance of African Americans. J Pers Soc Psychol. 1995;69:797–811.
Tuomi K, Ilmarinen JA, Jahkola A, Katajarinne L, Tulkki A. Work ability index. 2nd ed. Helsinki, Finland: Finnish Institute of Occupational Health; 1998.
Barnes-Farrell JL, Bobko N, Fischer F, Iskra-Golec I, Kaliterna L, Tepas D. Comparisons of work ability for health care workers in five nations. In: Ilmarinen J, Lehtinen S, editors. Past, present and future of work ability: Proceedings of the 1st International Symposium on Work Ability. Helsinki, Finland: Finnish Institute of Occupational Health; 2004. p. 76–82.
Schmidt AF, Finan C. Linear regression and the normality assumption. J Clin Epidemiol. 2018;98:146–51.
Finkel SE. Linear panel analysis. In: Menard S, editor. Handbook of longitudinal research: design, measurement, and analysis. New York: Academic Press; 2008. p. 475–504.
Aickin M. Dealing with change: using the conditional change model for clinical research. Perm J. 2009;13:80–4.
Article PubMed PubMed Central Google Scholar
Von Hippel C, Kalokerinos EK, Haanterä K, Zacher H. Age-based stereotype threat and work outcomes: stress appraisals and rumination as mediators. Psychold Aging. 2019;34:68–84.
Ng TWH, Feldman DC. Employee age and health. J Vocat Behav. 2013;83:336–45.
Major B, Eliezer D, Rieck H. The psychological weight of weight stigma. Soc Psychol Personal Sci. 2012;3:651–8.
Schvey NA, Puhl RM, Brownell KD. The impact of weight stigma on caloric consumption. Obesity. 2011;19:1957–62.
Smith CA. Intersectionality and sizeism: implications for mental health practitioners. Women Ther. 2019;42:59–78.
Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied framework for addressing weight stigma. Am J Prev Med. 2017;53:421–31.
Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendation on how to control it. Annu Rev Psychol. 2012;63:539–69.
Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88:879–903.
Siemsen E, Roth A, Oliveira P. Common method bias in regression models with linear, quadratic, and interaction effects. Organ Res Methods. 2010;13:456–76.
Nisbett RE, Wilson TD. Telling more than we can know: Verbal reports on mental processes. Psychol Rev. 1977;84:231–59.
Download references
Acknowledgements
This research is funded by the Australian Research Council (ARC DP DP190100546) and Volkswagen Foundation (Az. 96 849, “The role of work in the development of civilization diseases”).
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Wilhelm Wundt Institute of Psychology, Leipzig University, Leipzig, Germany
Hannes Zacher
School of Psychology, The University of Queensland, Brisbane, QLD, Australia
Courtney von Hippel
You can also search for this author in PubMed Google Scholar
Contributions
HZ and CvH conceived and designed the study. HZ collected the data and performed the analyses. HZ and CvH wrote the original draft and contributed to the revision of the manuscript.
Corresponding author
Correspondence to Hannes Zacher .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zacher, H., von Hippel, C. Weight-based stereotype threat in the workplace: consequences for employees with overweight or obesity. Int J Obes 46 , 767–773 (2022). https://doi.org/10.1038/s41366-021-01052-5
Download citation
Received : 10 June 2021
Revised : 29 November 2021
Accepted : 10 December 2021
Published : 20 December 2021
Issue Date : April 2022
DOI : https://doi.org/10.1038/s41366-021-01052-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Culture, Obesity Stereotypes, Self-Esteem, and the “Thin Ideal”: A Social Identity Perspective
- Published: August 2004
- Volume 33 , pages 307–317, ( 2004 )
Cite this article
- Paul A. Klaczynski 1 ,
- Kristen W. Goold &
- Jeffrey J. Mudry 2
6443 Accesses
96 Citations
Explore all metrics
Recent concerns with the increasing prevalence of overweight and obesity among children and adults indicate the need to better understand the psychosocial correlates of weight. We examined the relationships among negative stereotypes of obesity, “thin ideal” beliefs, perceptions of the causes of obesity and of control over weight, body esteem, and global self-esteem. A negative correlation between beliefs in control over one's weight and self-esteem was mediated by both negative attitudes toward obesity and thin idealization. Additionally, body esteem and gender were related but this relationship was mediated by beliefs in control over weight and valuation of the thin ideal. Central to the theoretical foundation of this research, however, was the observed negative correlation between negative attitudes toward obesity and self-esteem. This relationship was mediated primarily by the belief that obesity is caused by personality shortcomings. This last finding is explained from a social identity perspective.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Body Image, Eating, and Weight. Some Cultural Differences
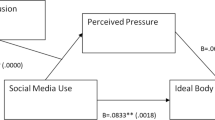
Am I thin enough? Social media use and the ideal body stereotype: The mediating role of perceived socio-cultural pressure and the moderating role of cognitive fusion
Alexandra Maftei & Ioan-Alex Merlici
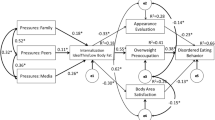

An exploration of the tripartite influence model of body image in Lithuanian sample of young adults: does body weight make a difference?
Rasa Jankauskiene & Migle Baceviciene
Archibald, A., Graber, J., and Brooks-Gunn, J. (1999). Associations among parent–adolescent relationships, pubertal growth, dieting, and body image in young adolescent girls: A short-term longitudinal study. J. Res. Adolescence , 9: 427-453.
Google Scholar
Baumeister, R. F., and Leary, M. R. (1995). The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 117: 497-527.
Bell, S. K., and Morgan, S. B. (2000). Children's attitudes and behavioral intentions toward a peer presented as obese: Does a medical explanation for obesity make a difference? J. Pediatr. Psychol. 25: 137-145.
Bigler, R. S., Jones, L. C., and Lobliner, D. B. (1997). Social categorization and intergroup attitudes in children. Child Dev. 68: 530-543.
Boyer, E. (1986, December). Transition from school to college. Phi Delta Kappan , 293-297.
Centers for Disease Control (2002). Prevalence of overweight among children and adolescents: United States, 1999 . Retrieved from www.cdc.gov/nccdphp/dnpa/obesity/trend/index.htm
Crandall, C. S. (1994). Prejudice against fat people: Ideology and self-interest. J. Pers. Soc. Psychol. 66: 882-894.
Crandall, C. S., and Biernat, M. R. (1990). The ideology of anti-fat attitudes. J Appl. Soc. Psychol. 20: 227-243.
Crandall, C. S., D'Anello, S. D., Sakalli, N., Wieczorkowski, G., and Feather, N. T. (2001). An attribution model of prejudice: Anti-fat attitudes in six nations. Pers. Soc. Psychol. Bull. 27: 30-37.
Crocker, J., Cornwell, B., and Major, B. (1993). The stigma of overweight: Affective consequences of attributional ambiguity. J. Pers. Soc. Psychol. 64: 60-70.
Crystal, D. S., Watanabe, H., and Chin, W. (1997). Intolerance of human differences: A cross-cultural and developmental study of American, Japanese, and Chinese children. J. Appl. Dev. Psychol. 18: 149-167.
Crystal, D. S., Watanabe, H., and San Chen, R., (2000). Reactions to morphological deviance: A comparison of Japanese and American children and adolescents. Soc. Dev. 9: 40-62.
Friedman, M. A., and Brownell, K. D. (1995). Psychological correlates of heavyweight: Moving to the next generation of research. Psychol. Bull. 117: 3-20.
Gable, S., and Lutz, S. (2000). Household, parent, and child contributions to childhood obesity. Fam. Relat. 49: 293-300.
Harter, S. (1985). Competence as a dimension of self-evaluation: Toward a comprehensive model of self-worth. In Leahy, R. (ed.), The Development of Self. Academic Press, New York, pp. 55-122.
Harter, S. (1993). Causes and consequences of low self-esteem in children and adolescents. In Baumeister, R. F. (ed.), Self-Esteem: The Puzzle of Low Self-Regard. Plenum, NY, pp. 87-116.
Heinberg, L. J., Thompson, J. K., and Stormer, S. (1995) Development and validation of the Sociocultural Attitudes Towards Appearance Questionnaire (SATAQ). Int. J. Eat. Disord. 17: 81-89.
Hewstone, M., Islam, M. R., and Judd, C. M. (1993). Models of crossed categorization and intergroup relations. J Pers. Soc. Psychol. 64: 779-793.
Hewstone, M., Jaspars, J., and Lalljee, M. (1982). Social representations, social attribution, and social identity: The intergroup images of “public” and “comprehensive” schoolboys. Eur. J. Soc. Psychol. 12: 241-269.
Jessor, R., Van Den Bos, J., Vanderryn, J., Costa, F., and Turbin, M. (1995). Protective factors in adolescent problem behavior: Moderating effects and developmental change, Dev. Psychol. 31: 923-933.
Klaczynski, P. A. (1991). Sociocultural myths and occupational attainment: Educational influences on adolescents' perceptions of social status. Youth Soc. 22: 448-467.
Klaczynski, P. A. (2000). Motivated scientific reasoning biases, epistemological beliefs, and theory polarization: A two-process approach to adolescent cognition. Child Dev. 71: 1347-1366.
Klaczynski, P. A., and Aneja, A. (2002). The development of quantitative reasoning and gender biases. Dev. Psychol. 38: 208-221.
Lerner, R. M., and Korn, S. J. (1972). The development of body-build stereotypes in males. Child Dev. 43: 908-920.
Lewis, R. J., Cash, T. F., Jacobi, L., and Bubb-Lewis, C. (1997). Prejudice toward fat people: The development and validation of the Antifat Attitudes Test. Obes. Res. 5: 297-307.
Mendelson, B. K., White, D. R., and Balfour, L. (1995). The Body-Esteem Scale for Adolescents and Adults . Unpublished manuscript, Concordia University, Montreal, Quebec.
Mendelson, B. K., White, D. R., and Mendelson, M. J. (1996). Self-esteem and body esteem: Effects of gender, age, and weight. J. Appl. Dev. Psychol. 17: 321-346.
Miller, C. T., and Downey, K. T. (1999). A meta-analysis of heavyweight and self-esteem. Pers. Soc. Psychol. Rev. 3: 68-84.
Nestle, M. (2002). Food Politics . University of California Press, Los Angeles, CA.
Osgood, D. W., Wilson, J., O'Malley, P., Bachman, J., and Johnston, L. (1996). Routine activities and individual deviant behavior. Am. Sociol. Rev. 61: 635-655.
Peterson, A. (1988). Adolescent development. Annu. Rev. Psychol. 39: 583-607.
Pettigrew, T. F. (1979). The ultimate attribution error: Extending Allport's cognitive analysis of prejudice. Pers. Soc. Psychol. Bull. 5: 461-476.
Pierce, J., and Wardle, J. (1997). Cause and effect beliefs and self-esteem of overweight children. J. Child Psychol. Psychiatry , 38: 645-650.
Quinn, D. M., and Crocker, J. (1999). When ideology hurts: Effects of belief in the Protestant ethic and feeling overweight on the psychological well-being off women. J. Pers. Soc. Psychol. 77: 402-414.
Rosenburg, M. (1979). Conceiving the Self . Basic Books, NY.
Simmons, R. G., and Rosenberg, M. (1971). Functions of children's perceptions of the stratification system. Am. Sociol. Rev. 36: 235-249.
Simon, B., and Brown, R. (1987). Perceived intragroup homogeneity in minority-majority contexts. J. Pers. Soc. Psychol. 53: 703-711.
Staffieri, J. R. (1967). A study of social stereotype of body image in children. J. Pers. Soc. Psychol. 7: 101-104.
Steinberg, L. (2002). Adolescence (6th edn.) . McGraw-Hill, Boston, MA.
Tajfel, H. (1982). Social psychology of intergroup relations. Annu. Rev. Psychol. 33: 1-39.
Tajfel, H., and Turner, J. C. (1979). An integrative theory of intergroup conflict. In Austin, W. G., and Worchel, S. (eds.), The Social Psychology of Intergroup Relations. Brooks/Cole, Monterey, CA, pp. 33-47.
Taylor, D. M., Moghaddam, F. M., and Bellerose, J. (1989). Social comparison in an intergroup context. J. Soc. Psychol. 129: 499-515.
Tesser, A. (1986). Some effects of self-evaluation maintenance on cognition and action. In Sorrentino, R. M., and Higgins, E. T. (eds.), Handbook of Motivation and Cognition. Guilford, NY, pp. 435-464.
Thompson, J. K., and Stice, E. (2001). Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Curr. Dir. Psychol. Sci. 10: 181-183.
Thurstone, T. G. (1962). Primary Mental Abilities for Grades 9–12. Science Research Associates, Chicago.
Turner, R. H. (1960). Sponsored and contest mobility and the school system. Am. Sociol. Rev. 25: 855-867.
Weiner, B., Perry, R. P., and Magnusson, J. (1988). An attributional analysis of reactions to stigmas. J. Pers. Soc. Psychol. 55: 738-748.
Willis, S., and Schaie, K. W. (1996). Psychometric intelligence and aging. In Blanchard-Fields, F., and Hess, T. M. (eds.), Perspectives on Cognitive Change in Adulthood and Aging . McGraw-Hill, New York, pp. 293-322.
Wing, R. R., and Jeffrey, R. W. (1999). Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J. Consulting Clin. Psychol. 67: 132-138.
Download references
Author information
Authors and affiliations.
The Pennsylvania State University, USA
Paul A. Klaczynski ( Associate Professor at )
The Pennsylvania State University's Psychology Department, USA
Jeffrey J. Mudry ( Undergraduate )
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Paul A. Klaczynski .
Rights and permissions
Reprints and permissions
About this article
Klaczynski, P.A., Goold, K.W. & Mudry, J.J. Culture, Obesity Stereotypes, Self-Esteem, and the “Thin Ideal”: A Social Identity Perspective. Journal of Youth and Adolescence 33 , 307–317 (2004). https://doi.org/10.1023/B:JOYO.0000032639.71472.19
Download citation
Issue Date : August 2004
DOI : https://doi.org/10.1023/B:JOYO.0000032639.71472.19
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- obesity stereotypes
- social identity
- thin idealization
- personal control over weight
- Find a journal
- Publish with us
- Track your research

- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story

Educate medics about weight stigma to reduce UK’s obesity rate
10 August 2022
To help tackle the UK’s obesity crisis, we must better educate medical professionals on weight stigma, according to the conclusions of a large-scale review led by UCL researchers.

It is widely accepted that people living with obesity are negatively affected by weight stigma, often referred to as weight-blaming; this is a form of discrimination, across all settings, based on stereotypes and prejudices about people who are either obese or overweight.
In healthcare, the negative biases associated with weight stigma are known to limit both access to health services and treatments. This has recently been the focus of a joint international consensus statement, published in Nature *, aiming to end weight stigma in healthcare globally.
Published in Obesity Reviews , researchers at UCL conducted a review to evaluate weight stigma reduction strategies in healthcare practice and healthcare education, with a view to provide recommendations for interventions, learning, and research.
Lead author, Dr Anastasia Kalea (UCL Division of Medicine) said: “Sadly healthcare, including general practice, is one of the most common settings for weight stigmatisation and we know this acts as a barrier to the services and treatments that can help people manage weight.
“A common misconception among medics and others, is that obesity is caused by factors within a person’s control, focusing on diet and exercise without recognition of, for instance, social and environmental determinants.
“In this review, it was clear more needs to be done to educate healthcare professionals and medical students on the complex range of factors regulating body weight, and to address weight stigma, explicitly emphasising its prevalence, origins, and impact.”
In the largest study of its kind, researchers undertook a systematic review** of 3,773 international research articles. This included 25 weight stigma interventional initiatives, comprising a total of 3,554 participants.
Through this analysis, researchers identified that weight-inclusive approaches to education in healthcare were effective in challenging stereotypes and improving attitudes. Such methods included ethics seminars discussing patient experiences, embedding virtual story-telling of patient case studies, or empathy evoking activities in the curriculum, such as following a calorie restricted diet or participation in clinical encounters with patients living with overweight and obesity. However, other methods such as video presentations and short lectures were not equally effective in improving attitudes in the long term.
Researchers are now calling on medical schools in both the UK and globally to ensure effective and sustained weight-inclusive teaching is embedded in medical doctor training and is added to the continuing professional development of clinicians.
Dr Kalea said: “Weight stigma needs to be addressed early on and continuously throughout healthcare education and practice, by teaching the genetic and socioenvironmental determinants of weight, by discussing the sources, impact and recognising the implications of stigma on treatment. We need to move away from a solely weight-centric approach to healthcare to a health-focussed weight-inclusive one. And it is equally important to assess the effects of weight stigma in epidemiological research.”
Obesity is one of the UK Government’s health priorities. Almost two-thirds (63%) of adults in England are overweight or living with obesity – and one in three children leave primary school overweight or obese, with obesity-related illnesses costing the NHS £6 billion a year***. The urgency of tackling the obesity and overweight has been brought to the fore by evidence of the link to an increased risk from COVID-19.
Dr Kalea added: “Stigma reduction interventions are a current research priority. Improving the ways we educate healthcare professionals early on is a starting point, keeping the focus on our patients; we need to communicate better, listen carefully to our patients needs and let these inform our teaching and research agendas.”
Weight stigma is also known to cause ‘internalised weight bias’ (IWB), which is when a person applies negative societal or cultural beliefs about body weight to themselves. This can lead to psychological distress, depression, anxiety, low self-esteem and often leads to decreased health motivation and maladaptive coping such as avoidance of timely healthcare, social isolation, reduced physical activity and disordered eating behaviours.
Weight stigma has also been shown to increase risk of developing obesity, and healthcare is one of the most common contexts where weight stigmatisation occurs. Physicians have been reported as the second most common source of weight stigma and discrimination.
Senior author, Professor Rachel Batterham OBE (UCL Division of Medicine), who leads the Centre for Obesity Research at UCL and the UCLH Centre for Weight Management said: “Identifying widely applicable ways to effectively reduce healthcare related weight stigma is urgently needed. In addition to improving healthcare provision, and the health and well-being of patients with obesity, healthcare that not only avoids, but actively addresses and reduces internalised weight bias may help patients better cope with and reduce the effects of stigma until it minimised in society. Not surprisingly, whilst stigmatising does the opposite, empathetic, non-stigmatising weight-related communication can increase patients’ health motivation and intention to comply with health professionals’ advice.”
Weight stigma programme launched by UCL
Two years ago the UCL Division of Medicine designed a new MSc Obesity and Clinical Nutrition for healthcare professionals. This applied the evidence in practice to improve obesity management and adopted a weight-inclusive approach.
* Joint international consensus statement, published in Nature , co-authored by Professor Rachel Batterham OBE at UCL.
**A systematic review carefully identifies all the relevant published and unpublished studies, rates them for quality and bias.
*** UK Government: Tackling Obesity
- Research paper published in Obesity Reviews
- Dr Anastasia Kalea's academic profile
- Professor Rachel Batterham's academic profile
- UCL Division of Medicine
- 'Man talking to the doctor at office', credit AnnaStills on iStock
Media contact
Henry killworth.
Tel: +44 7881 833274
E: h.killworth [at] ucl.ac.uk

Introduction
Participants and methods, disclosure statement, examining perceived stereotype threat among overweight/obese adults using a multi-threat framework.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Robert A. Carels , Sarah E. Domoff , Jacob M. Burmeister , Afton M. Koball , Nova G. Hinman , Alan K. Davis , Marissa Wagner Oehlhof , Michelle Leroy , Erin Bannon , Debra A. Hoffmann; Examining Perceived Stereotype Threat among Overweight/Obese Adults Using a Multi-Threat Framework. Obes Facts 1 June 2013; 6 (3): 258–268. https://doi.org/10.1159/000352029
Download citation file:
- Ris (Zotero)
- Reference Manager
Objective: The Multi-Threat Framework accounts for potentially different forms of stereotype threat that differ in target (i.e., the individual or the group) and source (i.e., the self or others). This investigation examined how these different forms of perceived stereotype threat were related to concepts, such as group identity, stereotype endorsement, stigma consciousness, etc., among overweight and obese individuals. Method: 216 adults completed an online survey. Participants' mean age was 23.6 (SD 10.1; range 18-64) years and mean BMI was 31.6 (SD 7.5) kg/m 2 . Results: Participants reported a history of feeling threatened by stereotypes related to weight. When reflecting on past experiences of perceived stereotype threat, participants reported greater levels of self/own stereotype threat compared to group stereotype threat. Level of stereotype threat was related to a number of personal characteristics (i.e., sex, BMI) and individual factors (i.e., group identity, stigma consciousness, fear of fat). Conclusion: Individuals who are overweight report a history of being threatened by negative stereotypes. The findings support the Multi-Threat Framework for stereotype threat based on body weight. Overweight individuals' susceptibility to stereotype threat may vary systematically depending on several factors. Future research should examine weight-related stereotypes' impact on cognitive and behavioral outcomes.
The experience of weight bias is pervasive and results in a variety of negative physical and psychological consequences [ 1,2,3,4 ]. A component of weight bias is the set of negative stereotypes about obese persons. Some of the most common stereotypes include the belief that obese individuals are lazy, unmotivated, and lack self-discipline [ 4,5 ]. Given the strength and ubiquity of these stereotypes, it is plausible that obese individuals, similar to other stereotyped groups, may experience disrupted performance on relevant tasks when their actions could be seen as confirming negative stereotypes associated with being overweight. This experience is commonly referred to as stereotype threat [ 6,7 ].
Over the past decade, stereotype threat has become one of the most widely studied topics in social psychology [ 8 ]. Previous research has consistently shown that individuals often perform poorly on stereotype-relevant tasks when they are reminded of the stereotype beforehand [ 7,8,9 ]. Although a large body of work confirms the reliability of stereotype threat effects (e.g., underperformance for women in math or science and racial/ethnic minorities in academics), questions remain about whether the phenomenon occurs for other stereotyped groups (e.g., obese individuals) and about the form that stereotype threat might take among these groups. Preliminary research suggests that stereotype threat can impact the behavioral intentions of overweight/obese adults [ 10 ].
Once conceptualized as a unitary construct, recent research indicates that stereotype threat may be a set of several distinct processes and phenomena [ 11 ]. To address this variability, Shapiro and Neuberg [ 6 ] proposed a Multi-Threat Framework consisting of multiple, qualitatively discrete forms of stereotype threat. See Shapiro and Neuberg [ 6 ] and Shapiro [ 11 ] for a detailed description of the Multi-Threat Framework. The Multi-Threat Framework accounts for potentially different forms of stereotype threat that differ in target (i.e., to whom one's actions will reflect upon: the self or group) and source (i.e., who will judge these actions: the self or others). To explain further, when the target of the threat is the group, group concept threat is the fear that poor performance will confirm (in the individual's own mind) that negative stereotypes about obese individuals are true in general (target: other; source: self). group reputation threat is the fear that poor performance will confirm (in the minds of others) that negative stereotypes about obese individuals are true in general (target: other; source: group). For example, if an obese individual is asked to complete a task requiring effort and motivation, she or he may fear that she or he might confirm a negative stereotype (i.e., being lazy) about obese people. In contrast, when the target of the threat is the self, self-concept threat is the fear that poor performance will confirm (in the individual's own mind) that negative stereotypes about obese individuals are true, specifically of the individual (target: self; source: self). Own-reputation threat is the fear that poor performance will confirm (in the minds of others) that negative stereotypes about obese individuals are true, specifically of the individual (target: self; source: group). For example, if an obese individual is asked to complete a task requiring effort and motivation, she or he may fear that others see her or him as lazy (i.e., she or he confirmed a negative stereotype about obesity targeted toward the self).
With the development of the Multi-Threat Framework, Shapiro [ 11 ] proposed that a number of factors are associated with the emergence of stereotype threat. One such factor is group identification, which is apparent when individuals perceive themselves as similar to other in-group members [for review see [ 12 ]. Generally speaking, the stronger an individual identifies with his or her group (i.e., other obese individuals), the more likely the individual is to fear confirming and supporting the negative stereotype about obese persons.
Similarly, the Multi-Threat Framework suggests that stereotype endorsement is a critical factor in the emergence of stereotype threat [ 11 ]. The more an individual believes (or trusts that others believe) that a stereotype is true (stereotype endorsement), the more likely he or she will be to experience stereotype threat. For example, if an obese individual believes that obese people are lazy and lack self-discipline, then he or she would be categorized as high in stereotype endorsement and would be expected to be more fearful of confirming that obese individuals are lazy through their actions (stereotype threat).
In support of the Multi-Threat Framework, Shapiro [ 11 ] demonstrated that group identification, stereotype endorsement, and the perceived target of threat varied across different stigmatized groups. For example, individuals who are members of racial/ethnic or religious minorities have greater group identification and less stereotype endorsement compared to individuals who are overweight or have a mental illness. In a subsequent study, Shapiro [ 11 ] demonstrated that individuals in high stereotype-endorsing as well as low identifying groups (i.e., overweight, mental illness) were more likely to view themselves, rather than their group, as the target of the threat. Finally, when individuals who were blind at birth (likely high group identifiers) were compared to those who became blind later in life (likely low group identifiers), those who became blind later in life were more likely to report that the self rather than the group was the target of the threat.
Consistent with the Multi-Threat Framework [ 11 ], the current investigation sought to further examine the different forms of stereotype threat that present in individuals who are overweight/obese. Preliminary findings show that individuals who are overweight or obese have lower group identification and greater stereotype endorsement than other stigmatized groups, such as racial or religious minorities [ 11 ]. As a result, they are more likely to perceive the self as a target of threat compared to the group. Thus, hypothesis one was that this sample of individuals who are overweight or obese would endorse perceiving threat from situations in which they themselves are the target of the stereotype more so than when their group (overweight people in general) was the target of the threat.
In addition, we intended to examine the relationship between perceived stereotype threat and factors that hypothetically could be associated with perceived stereotype threat among overweight/obese individuals. Hypothesis two is multi-faceted, examining factors that included the participants' level of group identity and stereotype endorsement, their BMI and gender, their level of awareness of negative stereotypes about the group (i.e., stigma consciousness), and their own anti-fat attitudes and self-esteem. Given earlier findings related to perceived stereotype threat and weight status, it was hypothesized that individuals' level of identification with overweight/obese as a group (group identification) would be related to higher levels of perceived stereotype threat. Similarly, it was hypothesized that participants' level of belief that stereotypes about overweight people are true (stereotype endorsement) would also be related to higher levels of perceived stereotype threat.
In addition, an individual, who embodies characteristics that are representative of a stigmatized group (i.e., higher BMI) or who possesses an attribute that increases the likelihood that they will be a target of weight-based bias and discrimination (i.e., female gender), may be exposed to more circumstances where stereotyped evaluations occur [ 4,13 ]. Similarly, research suggests that discrimination may occur at lower weight levels for women than for men [ 4 ]. Therefore, we hypothesized that females and individuals with higher BMIs would be more likely to report experiencing stereotype threat.
Furthermore, the more an individual is aware about his or her stigmatized status (i.e., stigma consciousness [ 14 ]), the more susceptible he or she may be to experiencing stereotype threat. For example, Brown and Pinel [ 15 ] showed that inducing stereotype threat in a group of women, who also reported high levels of stigma consciousness, resulted in domain-specific performance deficits (i.e., lower scores on math tests). Therefore, we hypothesized that overweight persons who were more self-conscious about their stigmatized status would be more likely to report stereotype threat.
Additionally, two potentially relevant factors to perceptions of stereotype threat are weight bias and self-esteem. First, contrary to other stigmatized groups, who are less likely to accept with-in group stereotypes, previous research suggests that overweight and obese people frequently hold strong anti-fat (i.e., anti-group) attitudes and, as indicated above, express higher levels of stereotype endorsement [ 4,11 ]. Therefore, we hypothesized that the more likely that an overweight/obese person is to make negative judgments about other obese individuals, the more likely they are to be aware that others are making stereotyped judgments against them. Second, self-esteem [ 16 ] has been found to be negatively associated with more frequent stigmatizing encounters [ 3 ]. A similar decrease in self-esteem might be found among individuals who believe that evaluations of their behaviors are based on their weight. Therefore, we hypothesized that individuals who report higher levels of perceived stereotype threat will report lower self-esteem.
Finally, because overweight/obese individuals are more likely to endorse stereotype threat where the target of the threat is the individual rather than the group, hypothesis three proposed correlates of stereotype threat indicated above (e.g., level of group identity, stereotype endorsement) would be more strongly associated with stereotype threat when the self is the target than for when the group is the target.
Participants
216 adults were recruited from psychology classes at a large Midwestern university (n = 155; 71.8% of the sample) and the community via the internet (e.g., Facebook and health-related web forums; n = 61; 28.1%). Participants met the study inclusion criteria if they were 18 years or older and were (or perceived themselves to be) overweight or obese. Psychology students were compensated with course credit, and community sample participants received a chance to win a USD 50 or USD 25 Amazon.com gift card. This investigation was approved by the University's institutional review board.
Participants' mean age was 23.6 (SD 10.1; range 18-64) years. The majority of the participants were Caucasian (81.3%) and female (76.1%). Regarding socioeconomic status, 22.2% of the sample reported having a high school diploma (n = 48), 64.4% reported having some college education (n = 139), 6.9% reported receiving a college diploma (n = 15), and 6.5% of the sample had a master's degree or higher (n = 14). Most of the sample earned an annual household income of less than USD 30,000 (n = 97, 45.5%), with 15.0% reporting an income between USD 30,000 and USD 45,000 (n = 32), 13.1% earning between USD 45,000 and USD 60,000 (n = 28), 8.9% earning between USD 60,000 and USD 75,000 (n = 19), and 17.1% earning greater than USD 75,000 annually (n = 37). Mean BMI was 31.6 ±7.5 kg/m 2 (normal weight (BMI < 25 kg/m 2 ) n = 26; overweight (BMI ≥25 and <30 kg/m 2 ) n = 73; class I obesity (BMI >30 and <40 kg/m 2 ) n = 94; class II obesity (BMI > 40 kg/m 2 ) n = 21). Perception of overweight was assessed with the question: ‘Do you consider yourself to be: i) underweight, ii) normal/average weight, iii) overweight, iv) or obese?'. Given that people who perceive themselves as overweight/obese (even if their actual weight is not in the overweight/obese category) may be concerned with confirming negative stereotypes, this investigation included individuals who perceived themselves to be overweight. The vast majority (92%, n = 199) of this sample perceived themselves to be overweight or obese and had BMIs ≥ 25. Of those who perceived themselves to be overweight or obese, 26 (13.7% of this subsample) did not have a BMI that fell within the overweight or obese categories. However, the findings did not change when participants who perceived themselves to be overweight or obese (but who were not based on their self-reported height and weight) were excluded. Therefore, these participants were included in the analyses. Additionally, a minority of participants (8%, n = 17) reported that they perceived themselves to be normal weight, but were in fact overweight according to their BMI. Findings did not change when these participants were excluded from analyses and so they were included in analyses.
Perceived Stereotype Threat
To measure perceived stereotype threat, participants were first asked to identify a negative stereotype associated with obesity that has had an influence on their life by either endorsing one of the six most common stereotypes described by Puhl and Brownell (e.g., laziness, lacking willpower/self-discipline [ 22 ]) or generating their own. Next, participants were asked to imagine a situation in which their actions had the potential to confirm the negative stereotype they had just endorsed. Participants were provided a brief example based on the specific negative stereotypes they chose, for example, ‘Imagine that you are walking with some acquaintances to a different floor of a building. If you decide to take the elevator instead of the stairs, you may confirm the stereotype that overweight/fat people are lazy.' They were then asked to write a short description of a situation they had personally experienced.
Next, participants completed a 12-item self-report scale designed to measure four types of stereotype threat developed by Shapiro [ 10 ]. On a 4-point scale (i.e., not at all; a little; somewhat; a lot), participants reported the extent to which they were concerned that their actions indicated self-concept threat (concern that their actions imply negative things about their own abilities in their own mind, e.g., ‘To what extent are you concerned that your actions will lead you to see yourself as actually possessing the negative stereotype that others have about people who are overweight/fat?'), own reputation threat (concern of showing that one's group possesses the negative stereotype, e.g., ‘To what extent are you concerned that your actions could lead you to be judged negatively by others because you are overweight/fat?'), group-concept threat (concern about confirming negative stereotypes about the overweight/obese group in their own mind, e.g., ‘To what extent are you concerned that your actions will confirm, in your own mind, that the negative stereotypes are true about people who are overweight/fat?'), and group reputation threat (concern of reinforcing other's negative stereotypes of one's group or representing one's group poorly, e.g., ‘To what extent are you concerned that your actions will reinforce the negative stereotypes, to others, about people who are overweight/fat?').
We collapsed the categories to simplify analyses and because for this stereotyped group, the source of the threat (self vs. other) is much less relevant than the target of the threat. This is consistent with Shapiro's [ 11 ] findings that individuals in low identifying and high stereotype-endorsing groups, such as overweight, were more likely to view themselves, rather than their group, as the target of the threat. Thus, we chose to combine the self-concept and own reputation threat measures to create an overall self/own threat score (6 items; α = 0.88). Similarly, the group-concept and group reputation threat measures were combined to create an overall group threat score (6 items; α = 0.87) with higher scores indicating greater threat. The self/own and group threats were correlated at r = 0.72 (p < 0.01).
Group Identification
Group identification was measured with eight items modified from the Multigroup Ethnic Identity Measure [ 17 ] using a 9-point Likert scale ranging from very strongly agree to very strongly disagree. Factor analyses suggest that the measure has two subscales (affirmation, belonging, and commitment; ethnic search identity). Affirmation, belonging, and commitment were assessed with items, such as ‘I have a strong sense of belonging with overweight/fat individuals' and ‘I have strong attachment to other overweight/fat individuals'. Group (i.e., ethnic) search identity was assessed with items such as, ‘I am active in organizations or social groups that include mostly overweight/fat individuals' and ‘I think a lot about how my life is/will be impacted by being an overweight/fat individual'. A total score was calculated with higher scores reflecting higher group identity. Cronbach's α was 0.79. The sample mean was 29.7 ± 7.4.
Stereotype Endorsement
To measure stereotype endorsement participants were asked to report the extent to which they believe six common stereotypes about overweight/fat people identified by Puhl and Brownell [ 22 ] (e.g., I am lazy, I lack willpower/self-discipline) were true of themselves using a 7-point scale ranging from strongly agree to strongly disagree. Higher scores reflected higher stereotype endorsement Cronbach's α was 0.78 for these items. The sample mean was 17.8 ± 6.2.
Stigma Consciousness
Stigma consciousness was measured using a modified version of the Stigma Consciousness Questionnaire [ 14 ]. Items were modified to reflect overweight/fat people rather than women. Participants were asked to report the extent to which they agree with ten statements about overweight/fat people (e.g., ‘Stereotypes about overweight/fat people have not affected me personally') using a 6-point scale ranging from strongly agree to strongly disagree. Higher scores reflected higher stigma consciousness. Cronbach's α was 0.78 and the mean 3.9 ± 0.7.
Anti-Fat Attitudes
Crandall's Anti-Fat Attitudes Questionnaire [ 18 ] was used to assess participant's attitudes toward obesity. This measure contains three subscales: the evaluation and dislike of individuals who are fat (7 items; α = 0.84), the controllability of weight/fat (3 items; α = 0.74), and personal concerns and distress about weight or the prospect of becoming overweight (fear of fat; 3 items; α = 0.83) that are measured on a 10-point Likert scale (0 = very strongly disagree; 9 = very strongly agree) with higher scores indicating stronger anti-fat attitudes. The means for the dislike, controllability of weight, and distress over becoming overweight scales for this sample were 2.4 ± 1.0, 4.3 ± 1.3, and 5.2 ± 1.6, respectively.
Self-Esteem
Rosenberg's Self Esteem Scale [ 19 ] was used to assess participants' self-esteem. Self-esteem is rated with ten self-report items using a 4-point scale ranging from strongly disagree to strongly agree. Higher scores indicating more positive self-evaluation. Cronbach's α was 0.82 for this study, with a sample mean of 26.3 ± 5.6.
Statistical Analyses
Multivariate analyses of variance were conducted to determine if demographic variables (gender, education, and income) significantly predicted perceived stereotype threat. Bivariate correlations were examined between age and perceived stereotype threat as well. The primary analyses consisted of two parts: examining the level of perceived stereotype threat and evaluating a priori predictors of stereotype threat. For hypothesis one that participants would perceive higher levels of self/own stereotype threat compared to group stereotype threat, a paired samples t-test was conducted. For hypothesis two, the association between stereotype threat and hypothesized predictors were examined using bivariate correlations. For hypothesis three that the predictor variables would be more strongly related to self/own stereotype threat compared to group stereotype threat, dependent r comparisons were conducted [ 20 ]. Finally, two additional post-hoc exploratory hierarchical linear regressions were conducted with self/own stereotype threat and group stereotype threat as the dependent variables. For both regressions, gender was entered into step 1 and the following variables were entered into step 2: BMI, group identity, stereotype endorsement, stigma consciousness, fear of fat, and self-esteem.
Preliminary Analyses
For demographic variables, MANOVA indicated a significant effect for gender only (F (2, 195) = 8.32, p < 0.01). As hypothesized, females endorsed significantly higher levels of perceived self/own stereotype threat (5.80 ± 3.93) compared to males (3.28 ± 3.12). Similarly, females endorsed significantly higher levels of perceived group stereotype threat (4.50 ± 3.60) compared to males (2.52 ± 2.71). Neither education level nor income was significantly associated with perceived stereotype threat. Age was not significantly correlated with either self/own or group stereotype threat. Therefore, gender was entered as a covariate into subsequent analyses.
Participants had been asked to choose one negative stereotype about people with obesity upon which they would base an imagined threatening situation. They chose unattractiveness (44%), laziness (23%), lack of willpower (16%), always binge eats (14%), unintelligence (1%), poor hygiene (1%), or did not respond (1%). ANOVA indicated that there was a significant difference in self/own threat scores among participants who chose different stereotypes, F (5,209) = 4.77, p < 0.001. Using a Bonferroni post-hoc test, participants who chose the unattractiveness stereotype had higher self/own threat scores (5.9) compared to those who chose the always binge eats stereotype (3.8) or the laziness stereotype (3.7).
Main Analyses
Hypothesis 1: As expected, average self/own perceived stereotype threat (5.2 ± 3.9) was higher than group stereotype threat (4.0 ± 3.5; t (209) = -6.08, p < 0.001). These results support the hypothesis that overweight and obese individuals would perceive stereotype threat as an attack against their own reputation or self-concept more so than as a threat against their group.
Hypothesis 2: Most of the predictor variables (group identity, stereotype endorsement, stigma consciousness, fear of fat, and self-esteem) were significantly correlated with self/own and group perceived stereotype threat (table 1 ).
Significantly different correlations among threat targets and related variables
Hypothesis 3: To compare the strength of the associations between self/own stereotype threat and predictor variables as well as group stereotype threat and predictor variables, dependent r comparisons were conducted [ 20 ]. These indicated a stronger correlation between the predictor variables and self/own threat compared to group stereotype threat (significant differences in strengths of associations are indicated in table 1 ). For example, the correlation between group identity and self/own threat (r = 0.40, p < 0.01) was greater than the correlation between group identity and group threat (r = 0.29, p < 0.01). This pattern of results was found for stereotype endorsement, stigma consciousness, fear of fat, and self-esteem as well.
In addition, post-hoc analyses using regression to examine predictors of self/own stereotype threat, gender emerged as significant predictor (β = 0.28, p < 0.01), accounting for 8% of the variance in self/own stereotype threat (F (1, 203) = 16.98, p < 0.01) in step 1. The variables entered in step 2 explained an additional 30% of the variance (F (7, 197) = 16.67, (p < 0.01). Of the variables entered, gender (β = 0.12, p < 0.05), BMI (β = 0.12, p < 0.05), stigma consciousness (β = 0.21, p < 0.01), fear of fat (β = 0.19, p < 0.01), and self-esteem (β = -0.16, p < 0.05) were statistically significant.
Similarly, a hierarchical linear regression was conducted to examine significant predictors of perceived group stereotype threat. In step 1, gender emerged as a significant predictor (β = 0.24, p < 0.01) of perceived group stereotype threat, explaining 6% of the variance (F (1, 203) = 12.75, p < 0.01). The variables in step 2 explained an additional 14% of the variance (F (7, 197) = 7.16, p < 0.01). Of the variables entered, only gender was statistically significant (β = 0.15, p < 0.05), with stigma consciousness showing a trend towards significance (β = 0.17, p = 0.05).
Consistent with the Multi-Threat Framework [ 11 ], this investigation sought to examine how different forms of stereotype threat were related to group identity and stereotype endorsement among overweight/obese individuals and those who perceived themselves to be. In addition, we examined the relationship between perceived stereotype threat and factors that hypothetically could be associated with perceived stereotype threat among overweight/obese individuals and those who perceived themselves to be.
As predicted, findings revealed that individuals who are overweight or obese reported a significant history of being threatened by stereotypes related to weight. This is not surprising, given that weight bias is pervasive and increasing [ 1,2,3,4 ]. Whether real or imagined, the fear that one's actions could lead to harsh judgment or the confirmation of negative stereotypes is a real concern for overweight and obese individuals.
Participants reflecting on past experiences of perceived stereotype threat reported greater levels of self/own stereotype threat compared to group stereotype threat. This is consistent with previous research indicating that the kind of stereotype threat (i.e., self/own versus group) most commonly experienced can vary among stigmatized groups [ 11 ]. Specifically, individuals with excess weight are less likely to show an in-group positive bias [ 18 ], are less likely to identify with being a part of an overweight group, and thus may be more vulnerable to experiencing threats on the personal or individual level compared to other stigmatized groups [ 11 ]. In other words, an obese individual would be generally less concerned that she or he might confirm a negative stereotype about obese people being lazy, and more concerned about having others see him or her as being a lazy person just because they have visible excess weight. Unlike other stigmatized groups with stronger group identity, such as racial minorities, overweight/obese individuals are more concerned that their behaviors will reflect poorly on him- or herself than on obese people in general.
The results of the present study support two of the primary tenets of the Multi-Threat Framework: that the emergence of stereotype threat is strongly associated with group identification (a perceived similarity to other in-group members) and stereotype endorsement (a belief that the stereotype is true). The findings of the present study suggest that, among overweight/obese individuals, those individuals identifying as part of the ‘overweight' group and who believe in common stereotypes about overweight individuals were more likely to perceive that stereotype threat had occurred in stigmatizing situations. Interestingly, stronger group identity was associated with greater self/own threat than group threat. At first glance, this finding might appear counterintuitive because it would seem natural for group identity to lead to seeing the group as the target of the threat. However, group identity is both a necessary precondition for threat as well as a factor that influences the perceived target of the threat [ 6,11 ]. In other words, an individual has to perceive him- or herself as obese and have some level of group identity to experience stereotype threat in the first place. However, it is likely that considerably higher group identity, such as those levels found in racial and religious minorities, would be necessary before an individual was concerned about their group's reputation more than his or her own.
As expected, female participants and participants with higher BMIs reported a greater likelihood of experiencing stereotype threat. As indicated earlier, individuals with higher BMIs and women are more likely to be targets of prejudice and discrimination [ 4 ]. In addition, weight may hold more self-relevance for females than men. Therefore, women may not only fear but may also be targets of stereotyped evaluations more than men. However, the findings did not change when participants who perceived themselves to be overweight or obese (but who were not based on their self-reported height and weight) were excluded. These findings are consistent with research that revealed few psychological differences in body image, eating/dieting behaviors, and psychosocial well-being between persons as a function of their perceived versus actual weight [ 21 ].
Being aware of and believing their stereotyped status (i.e., stigma consciousness) was also related to higher levels of perceived stereotype threat. Not surprisingly, as stigma consciousness increased, participants reported a greater perception that they had experienced self/own stereotype threat compared to group stereotype threat. These findings are consistent with previous research examining stigma consciousness and stereotype threat among women in the math domain. Brown and Pinel [ 15 ] showed that inducing stereotype threat in a group of women, who also endorsed high levels of stigma consciousness, resulted in domain-specific performance deficits (i.e., lower scores on math tests). These findings would appear to generalize to overweight/obese individuals. The more individuals are aware of stereotypes, believe in them, and find that they pervade their life experiences, the more likely they are to experience stereotype threat.
Additionally, possessing a fear of being fat was related to higher levels of perceived stereotype threat. Previous research suggests that overweight and obese people frequently hold strong anti-fat (i.e., anti-group) attitudes [ 4,11 ] which is in contrast to other stigmatized groups who are less likely to endorse within-group stereotypes. It is likely that the heightened sensitivity to being overweight/obese contributed to a greater fear of judgment. Overweight/obese individuals who feared their overweight group status were more likely to perceive stereotyped judgments were directed against them.
Finally, experiencing low self-esteem was related to higher levels of stereotype threat. Self-esteem has been found to be negatively related to the greater frequency of stigmatizing situations [ 3 ]. People with more frequent past experiences with weight-based discrimination may be more vigilant to having their behaviors judged relative to their weight. Therefore, low self-esteem may be a consequence of experiencing stereotype threat. Future research will be important in answering this question.
Taken together, the results from this investigation provide support for the Multi-Threat Framework for stereotype threat broadly, but also specifically related to overweight and obese individuals. Both self/own and group stereotype threat were reported by overweight individuals (and as expected, self/own stereotype threat was reported to a greater extent). Additionally, the two types of stereotype threat are related to a number of personal characteristics (i.e., gender, BMI) and individual factors (i.e., group identity, stigma consciousness, fear of fat). However, there are some limitations of the present study, along with implications for future research that are important to note. First, although the primary focus of the study related to participants' weight and perceptions of weight-related stereotype threat, some participants endorsed belonging to a variety of other stigmatized groups (e.g., gender, racial/ethnic, etc.). However, given that the current sample was composed primarily of Caucasians (81.3%) and members of a religious majority (76.1%), inadequate statistical power limited our ability to examine interactions between identification with another stigmatized group and weight-related stereotype threat.
A second limitation of the present study is that findings are based on participants' self-reports of perceived stereotype threat; behavioral outcomes of being threatened with negative stereotypes (i.e., performance deficits) were not measured. With this method, we were not able to assess the direct outcomes of experiencing weight-related stereotype threat on domain-specific functioning. However, prior research has found participants' self-reported stereotype threat experiences to parallel performance outcomes. In particular, individuals' self-reports of stereotype threat in other stigmatized groups (e.g., race) are associated with negative implications for related performance outcomes []e.g., [ 24,25,26,27 ]. Finally, although the findings from this investigation are consistent with theoretical predictions from the Multi-Threat Framework, we cannot rule out the possibility that the instructions to the participants ‘to identify a negative stereotype associated with obesity that has had an influence on their life' differentially favored their selection of a threat for which self rather than others were the source of the target.
The current findings provide a base on which to build future research designed to measure the direct effects of experiencing weight-related stereotype threat through experimental manipulation of each type of threat (e.g., threats to the self vs. the group). This research will be necessary to definitively say that weight-based stereotype threat is a valid phenomenon. Future research could examine how performance on tasks related to health decision-making or physical activity effort is affected by the presentation of negative weight-related stereotypes. Burgess, et al. [ 28 ] outlined a number of ways in which patients' experience of stereotype threat in clinical settings and encounters may contribute to health care disparities. To our knowledge only one study has examined stereotype threat among obese adults. Seacat and Mickelson [ 10 ] found that overweight women who were exposed to negative weight-related stereotypes reported fewer healthy dietary and exercise intentions compared to a control. Additionally, in similar research on social identity threat, Major et al. [ 29 ] found that overweight women who were exposed to appearance related evaluations (i.e., rated on a speech on why they would make a good dating partner) and who believed that they were being videotaped, exhibited increased blood pressure, diminished executive control, and more stress-related emotions compared to average-weight women.
The present study provides an important evaluation of the Multi-Threat Framework [ 6,11 ] for stereotype threat in overweight and obese individuals. This research adds to the understanding of how stereotypes may affect overweight individuals, a group known to experience a high degree of stigma and weight bias [ 4 ]. A greater understanding of how stereotype threat affects individuals who are overweight could lead to the development of interventions to ameliorate likely negative psychosocial and health behavior outcomes.
The authors declare no conflict of interests.

Email alerts
Citing articles via, suggested reading.
- Online ISSN 1662-4033
- Print ISSN 1662-4025
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Contact: Front Office
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Weight Stigma
What we do Our Policy Priorities Weight Stigma
- Obesity as a disease
- Commercial determinants of obesity
- Childhood Obesity
- Obesity in Universal Health Coverage
- The ROOTS of Obesity
Weight stigma refers to the discriminatory acts and ideologies targeted towards individuals because of their weight and size. Weight stigma is a result of weight bias. Weight bias refers to the negative ideologies associated with obesity.
Changing the global obesity narrative
A position statement on weight stigma from World Obesity
These can include laziness, lack of will power, a lack of moral character, bad hygiene, low level of intelligence and unattractiveness. Stigmatising beliefs and ideologies can lead to stigmatising acts. These acts can manifest themselves in various different ways. People with obesity may experience negative verbal commentaries, teasing, or physical assault.
Additionally, subtle behavioural slights such as eye rolling and tutting frequently occur. The environment also plays a part - for example, seating in cinemas or airlines are not designed to accommodate people with obesity. This is commonly reported in medical settings in particular, where seating, gowns and examination tables are unable to accommodate people with obesity.
The school and education environment is renowned for bullying and weight is one of the primary reasons for victimisation. Weight bias in education settings can come from a variety of different sources - students are not just victimised by their peers. It has been documented that even their teachers (particularly, but not exclusively physical education teachers) can be common perpetrators of stigma.
Weight stigma can prevent students from progressing into higher education. Students with obesity are significantly less likely to be accepted to college or university and those that do are likely to receive less financial support than their healthy-weight peers.
There is consistent evidence of weight discrimination at every stage of employment including; career counselling, interviews and hiring processes, salary disparities, fewer promotions, harsher disciplinary actions and higher contract termination rates. People with obesity are also significantly less likely to be put into a sales or customer-facing position. It has also been shown that people with obesity can be paid less than their healthy-weight counterparts for the same work. This is more pronounced for women with obesity, who can receive up to 6% less for the same work, whilst men with obesity may tend to sort themselves into lower-paying jobs.
Close relationship partners, including spouses/partners, parents, siblings and children, are documented as being the most common source of stigmatising comments, and in some cases, generate the most harmful stigmatising encounters.
Weight bias persists into healthcare settings. Physicians, nutritionists, dietitians, fitness professionals and exercise science students have all shown a propensity to ascribe stereotypical characteristics such as lazy, weak- willed, and noncompliant. Physicians generally have lower levels of respect for patients with higher BMI and generally spend less time providing consultations to patients with obesity compared to their healthy-weight counterparts. Physicians can also be a direct source of stigmatising comments. In one study by Puhl and Brownell 53% of people with overweight and obesity reported to have received inappropriate comments from their doctor about their weight.
In addition to stigma arising from the physician-patient relationship, many people with obesity report a stigmatising physical environment. This can include gowns, chairs, and examination tables that cannot accommodate people with obesity.
Weight prejudice exists in almost all sections of the media, from children's shows where characters with obesity are stereotyped as clumsy, lazy, and without friends, through to news reports which have apportioned blame for global warming and rising fuel prices to people with obesity.
In terms of representation, underweight characters are significantly over-represented and overweight characters under-represented compared to the general population; something particularly true for women.
Marketing for weight loss products regimes is overwhelmingly focused on personal responsibility for weight, further perpetuating the belief that weight gain or loss is entirely in the hands of the individual. This framing of obesity as a purely personal-level responsibility can also be seen in public-health campaigns that solely focus on behaviour changes in their efforts to lower obesity levels.
Overtly discriminatory language is a predominant aspect of the obesity media narrative and will often be accompanied by equally stigmatising images that perpetuate the many false stereotypes attributed to people with obesity.

The consequences of stigma
Stigma can result in a variety of adverse emotional responses such as depression, low self-esteem and anxiety. Obesity itself is typically blamed for these potential consequences. However, it is weight stigma, rather than obesity, which has been proven to mediate the greater likelihood of depressive and anxiety disorders in individuals that have or have formally had obesity. Focus tends to be placed on the emotional effects of stigma. However, in addition to emotional health, weight stigma can also have social and physical effects.
Due to the numerous social contexts in which weight stigma can and does occur, the effects it can have on an individual’s social life can be extensive. It has been proven to weaken social relationships. In an effort to evade stigma, individuals have reported engaging in selective social isolation, which refers to avoiding social situations in an effort to remain unnoticed through fear of being stigmatised.

Stigma and the fear of stigma can affect physical health in a multitude of ways;
- Fear of stigma can lead to avoidance of seeking medical care which creates barriers to obesity prevention and treatment strategies.
- Weight stigma has been positively correlated with a variety of disordered eating patterns such as binge eating, emotional eating, restrictive eating, weight cycling and eating anxiety.
- There are many scientific studies associating obesity to a variety of serious medical conditions. However, more recently there have been studies with results which indicate that weight stigma plays a fundamental role in the development of some of these medical conditions. For example, it has been found that weight stigma, independent of adiposity positively correlates with increased stress hormone levels. Stress has been found to impact multiple areas of health such as, blood pressure, cardiac health, visceral fat levels and insulin resistance.
- Finally, in some cases weight stigmatisation is so severe that it has been directly associated with suicidal ideations and acts.
The drivers of stigma
The drivers of stigma are primarily based around a misunderstanding of the complex causes of obesity, with people attributing weight gain to personal responsibility, and failing to grasp the complex mix of genetics, environment, and biological factors that drive it. The focus on personal responsibility results in blaming people with obesity for their condition, and enables the stereotyping of people with obesity as lazy and lacking in willpower.
It is argued by some that stigmatisation of people with obesity will incentivise them to lose weight. However, evidence shows that this is a counterintuitive approach to weight loss motivation. Therefore, in addition to crossing moral boundaries, bias and stigma contribute considerably towards the globally rising obesity levels. Addressing weight stigma is essential in order to meet obesity reduction and prevention targets.

Tackling stigma
We are working in four distinct areas to tackle the stigma experienced by people with obesity, and encourage others to join us in this.
To tackle stigma in healthcare settings we are calling for better obesity education for healthcare professionals, as well as running our own e-learning platform SCOPE . Many healthcare professionals say they do not feel equipped to treat patients with obesity, and patients with obesity have self-reported their doctors as being a key source of stigmatising remarks. We believe that by providing and advocating for healthcare professional education on obesity we can reduce stigma amongst this group, leading to better treatment for people with obesity, as well as instilling a compassion for people with obesity that will trickle into the rest of our society.
Whilst changing attitudes for healthcare professionals is vital if we're going to reduce stigma, it's not enough to do only that. Wider societal attitudes need to be adjusted too. Our World Obesity Day 2018 Campaign aims to shed light on the ubiquity and seriousness of stigma. Improving awareness about obesity amongst the general public and challenging the assumption that obesity is purely an issue of personal responsibility is paramount to successfully reducing stigma.
Obesity is one of the last diseases where society has failed to implement people first language. People-first language puts the person before their disease, emphasising that an individual is not defined by their condition. For example, it is now very uncommon to see someone referred to as a disabled person ; you'll more likely see reference to a person with a disability . The person comes first, and their disability is a characteristic rather than a defining feature. Unfortunately, this is not yet the norm with obesity, and the language used around the condition remains a major contributor towards stigmatisation. It is still usual to see obese people and a key part of our fight for people-first language is to change this to people with obesity. Language is integral to affording people with obesity the dignity they deserve.
Images used to accompany online or print news stories frequently depict people with obesity from unflattering angles, often inactive or consuming unhealthy food. This portrayal creates an environment where there is a lack of understanding and even a desire to shame individuals who have obesity. They invariably exploit the “shock value” of focusing on abdomens or lower bodies, and excluding heads from the frame of view. We are advocating for a fair portrayal of people with obesity in the media. We maintain a free to use image bank depicting people with obesity in various settings which we are encouraging media outlets to make use of.
Related Resources
World obesity day 2018: toolkit, world obesity day 2018: press releases, world obesity day 2018: mind map, world obesity day 2018: media report, our image bank.
One of the simplest ways to start fighting weight stigma is to use non stigmatising imagery. You can find a whole host of non stigmatising imagery on our image bank, freely available using the link below.
Share this page
Training & Events
SCOPE E-Learning
We offer the only internationally recognised course on obesity management. Read more here.
Global Obesity Observatory
We offer various statistics, maps and key data around the topic of obesity. You can find all that and more here.
Policy & Advocacy
Our Policy Priorities
We have developed five key areas of policy that are a priority to us. Want to know more? Check them out here!
- Our Members
- Partnerships
- Patient Portal
- Membership Application Form
- Member Benefits
- Finance Committee
- Annual Report and Financials
- Prevalence of Obesity
- Causes of Obesity
- Obesity Classification
- Prevention of Obesity
- World Obesity Day
- Healthy Venues
- Reinventing the Food System: A Report
- The Spotlight Project
- SCOPE Examination
- Guide to SCOPE Certification
- SCOPE Schools
- Accreditation
- SCOPE Fellows
- Leadership Programme
- SCOPE Pricing
- SCOPE Accredited Events
- Event Archive
- International Congress on Obesity
Sign up for notifications
- ConscienHealth
- Advocacy Organizations
- Affiliates & Advocates
- Service Partners
- Publications
- LATEST NEWS
Brozempic, Gender Stereotypes, and Obesity Care

It can be awkward.
The cultural baggage of seeking help with obesity for men is certainly different and arguably more daunting for men. Nurse practitioner Chace Franks from Owensboro, KY, explains:
“Men are slower to ask for help. There’s some shame in the society and media about taking medication for weight management. The comments I get about taking ‘the easy way out’ — most of those come from men.”
Media studies professor Emily Contois is more blunt about it:
“Weight loss has been understood as feminine and feminizing, not just in the U.S. but in similar Western countries.”
Clearly, telehealth startups aimed at men want to change this. “We’re not mommying you,” says the founder of Fella Health. “We’re a mechanic. You’re bringing a car in that needs to get fixed.” Cue the male grunt.
Mostly Women in Obesity Trials
In the pivotal SURMOUNT-1 study of tirzepatide for treating obesity, two-thirds of the people who enrolled were women. If anything, this was less lopsided in favor of women than most clinical trials of obesity treatment. Three-quarters of the subjects in the STEP-1 trial for semaglutide were women.
It is a simple fact that women with obesity face more pressure or feel more strongly about dealing with it.
But Then There’s Heart Health
However, when it comes to the bias in heart health, the situation is exactly the opposite. Men are overrepresented. Gender bias in the cardiovascular care is unmistakable . And this showed up in the landmark SELECT study of preventing major cardiovascular events by treating obesity. This study enrolled 84% white men.
When President Dwight Eisenhower had a heart attack, it created a teachable moment that framed cardiac health as a legitimate issue for powerful men. The rest is history. Weight management in cardiac rehabilitation became a key entry point for men into obesity care.
Will the rise of advanced obesity medicines change the gender dynamic in obesity care? Or reinforce it? We can see both scenarios as credible.
Click here for more on this from the New York Times. For a more scholarly view of gender and obesity, click here .
The Man with the Monocle, painting by Amedeo Modigliani / WikiArt
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.
Your email:
April 19, 2024
Leave a Reply
Search this blog.
- access to care
- anti-obesity medicines
- bariatric surgery
- childhood obesity
- evidence based medicine
- food industry
- food policy
- health disparities
- health economics
- health insurance
- health outcomes
- health reporting
- Obesity Action Coalition
- obesity care
- obesity causes
- obesity prevention
- obesity statistics
- obesity treatment
- physical activity
- public health
- scientific integrity
- scientific rigor
- semaglutide
- The Obesity Society
- weight bias
- weight discrimination
- weight loss
- weight stigma
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- February 2012
- January 2012
- October 2011
- February 2011
- January 2011
- December 2010
- October 2010
- September 2010
- October 2009
- August 2009
- Consumer Trends
- Food & Nutrition
- Food Industry
- Health & Obesity
- Health Policy
- Scientific Meetings & Publications

outstanding advocacy
Recognized by The Obesity Society & Obesity Action Coalition
©2009-2013 ConscienHealth. All rights reserved. | Website Design by Mariela Antunes | Hosting by DTS
Advertisement
Supported by
Sleep Apnea Reduced in People Who Took Weight-Loss Drug, Eli Lilly Reports
The company reported results of clinical trials involving Zepbound, an obesity drug in the same class as Novo Nordisk’s Wegovy.
- Share full article

By Gina Kolata
The pharmaceutical manufacturer Eli Lilly announced on Wednesday that its obesity drug tirzepatide, or Zepbound, provided considerable relief to overweight or obese people who had obstructive sleep apnea, or episodes of stopped breathing during sleep.
The results, from a pair of yearlong clinical trials, could offer a new treatment option for some 20 million Americans who have been diagnosed with moderate to severe obstructive sleep apnea. Most people with the condition do not realize they have it, according to the drug manufacturer. People with sleep apnea struggle to get enough sleep, and they face an increased risk for high blood pressure, heart disease, diabetes, strokes and dementia.
The study’s findings have not been published in a peer-reviewed medical journal. Eli Lilly provided only a summary of its results — companies are required to announce such findings that can affect their stock price as soon as they get them. Dr. Daniel M. Skovronsky, Eli Lilly’s chief scientific officer, said the company was still analyzing the data and would provide detailed results at the American Diabetes Association’s 84th Scientific Sessions in June.
But experts not affiliated with Eli Lilly or involved in its studies were encouraged by the summary.
“That’s awesome,” said Dr. Henry Klar Yaggi, director of the Yale Centers for Sleep Medicine in New Haven, Conn.
He added that the most common treatment, a CPAP machine that forces air into the airway, keeping it open during sleep, is effective. About 60 percent of patients who use continuous positive airway pressure continue to use it, he said.
Dr. Eric Landsness, a sleep medicine researcher at Washington University in St. Louis, said the Lilly results were “phenomenal.”
They suggest, he said, that tirzepatide “is a great alternative for people who are obese and can’t use CPAP or are on CPAP and want to improve the effect.”
He added that unlike current treatments that address only the symptoms of sleep apnea, cessation of breathing, tirzepatide goes after the underlying cause, the blockages in the airway that make a person stop breathing.
Tirzepatide, sold under the brand name Zepbound, was approved by the Food and Drug Administration for weight loss in November. The agency previously approved the drug for diabetes under the name Mounjaro. Tirzepatide is part of the class of GLP-1 drugs that includes Ozempic and Wegovy, which are sold by Novo Nordisk.
Patients who participated in these Eli Lilly trials were overweight or obese and had moderate to severe obstructive sleep apnea, with moderate defined as stopped breathing at least 15 times an hour during sleep. The trials did not involve those with central sleep apnea, a type that occurs because the brain stops signaling the muscles that control breathing.
One of the Lilly studies involved about 200 people with obesity who could not or were unwilling to use a CPAP machine. Half were randomly assigned to tirzepatide, a weekly injection. The others got a placebo.
Those who got tirzepatide had an average of 27.4 fewer apnea events per hour compared with an average reduction of 4.8 events per hour for placebo.
The other Lilly trial involved about 200 people with obesity who used a CPAP machine and were encouraged to continue using it except for the assessments of their apnea episodes. Those who took tirzepatide had an average of 30.4 fewer events per hour after a year of the drug, compared with an average reduction of six events per hour for participants who got a placebo.
In both studies, participants who took tirzepatide lost about 20 percent of their weight. Dr. Skovronsky of Eli Lilly attributed the results to the loss of fat deposits in the tongue and airway.
Many people with obesity, Dr. Landsness explained, have fat deposits in the tongue and in the back of the throat. The neck gets larger with fat that narrows the airway, and the tongue gets larger in all directions, “like blowing up a balloon,” he said. During sleep, the tongue obstructs the flow of oxygen, repeatedly waking the person.
Researchers assumed that losing weight would reduce obstructive sleep apnea episodes. But before the new drugs like tirzepatide, significant and permanent weight loss was all but impossible for most people with obesity unless they had bariatric surgery.
Marishka Brown, director of the federally funded National Center on Sleep Disorders Research, said it had been difficult to know how much of an effect weight loss would have on people with sleep apnea.
“Sometimes the sleep apnea goes away, but not always,” Dr. Brown said.
For that reason, she added, when asked if weight loss is an effective treatment, “the research community has been a bit cautious about saying yes or no.”
Now, with the new results, that tentativeness may change, researchers said.
Of course, everyone in the study was eligible for tirzepatide anyway — it is approved for people with obesity, meaning those with a body mass index of at least 30, or for those with a body mass index of at least 27 and with obesity-related medical conditions.
But insurance companies do not always pay for tirzepatide for weight loss. The drug’s list price is about $1,000 a month, but insurers pay much less . Eli Lilly sells the drug to people without insurance for $550 a month.
Dr. Skovronsky said that Eli Lilly planned to submit an application to the F.D.A. and to drug regulatory agencies around the world requesting that tirzepatide be approved for the reduction of sleep apnea in people with obesity or who are overweight.
“The goal is for insurance to cover it,” Dr. Skovronsky said.
Gina Kolata reports on diseases and treatments, how treatments are discovered and tested, and how they affect people. More about Gina Kolata
A Close Look at Weight-Loss Drugs
Ozempic’s Inescapable Jingle: The diabetes drug has become a phenomenon, and “Oh, oh, oh, Ozempic!” — a takeoff of the Pilot song “Magic” — has played a big part in its story.
The Era of ‘Brozempic’: Some telehealth start-ups are playing up masculine stereotypes to market GLP-1s — the revolutionary class of drugs like Ozempic — which have been more widely associated with women.
Taking on Weight Stigma: Oprah Winfrey, a prominent figure in the conversation about dieting and weight bias, tackled the rise of weight loss drugs in a new prime-time special . In December, she shared that she was taking a medication to manage her weight.
Beyond Weight Loss: Wegovy is now approved for a new use: reducing the risk of heart attacks , strokes and cardiovascular-related death in adults who have heart disease and are overweight
Pregnancy: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus .
Muscle Loss: As drugs like Ozempic become increasingly popular for weight loss, more doctors and patients are looking for ways to counteract the muscle loss that can happen on these medications. Companies are racing to meet that demand .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley-Blackwell Online Open

Impact of weight bias and stigma on quality of care and outcomes for patients with obesity
1 Division of Health Care Policy and Research, Mayo Clinic, Rochester, Minnesota, USA
2 Center for Chronic Disease Outcomes Research, Minneapolis Veterans Affairs Medical Center, Minneapolis, Minnesota, USA
3 Department of Medicine, University of Minnesota, Twin Cities, Minneapolis, Minnesota, USA
4 Department of Family Medicine and Community Health, University of Minnesota, Twin Cities, Minneapolis, Minnesota, USA
WL Hellerstedt
5 Division of Epidemiology and Community Health, University of Minnesota, Twin Cities, Minneapolis, Minnesota, USA
The objective of this study was to critically review the empirical evidence from all relevant disciplines regarding obesity stigma in order to (i) determine the implications of obesity stigma for healthcare providers and their patients with obesity and (ii) identify strategies to improve care for patients with obesity. We conducted a search of Medline and PsychInfo for all peer-reviewed papers presenting original empirical data relevant to stigma, bias, discrimination, prejudice and medical care. We then performed a narrative review of the existing empirical evidence regarding the impact of obesity stigma and weight bias for healthcare quality and outcomes. Many healthcare providers hold strong negative attitudes and stereotypes about people with obesity. There is considerable evidence that such attitudes influence person-perceptions, judgment, interpersonal behaviour and decision-making. These attitudes may impact the care they provide. Experiences of or expectations for poor treatment may cause stress and avoidance of care, mistrust of doctors and poor adherence among patients with obesity. Stigma can reduce the quality of care for patients with obesity despite the best intentions of healthcare providers to provide high-quality care. There are several potential intervention strategies that may reduce the impact of obesity stigma on quality of care.
Introduction
The goal of primary care is to improve patients' health, longevity and quality of life through the provision of patient-centred care. To do so, healthcare providers must identify modifiable behaviours that increase disease risk, and help patients change them. Recent US Preventive Services Task Force guidelines recommend screening adults for obesity and offering behavioural interventions to those with a body mass index (BMI) over 30 kg m −2 ( 1 ). However, obesity is a stigmatized condition; thus, one side effect of increased focus on body weight in health care may be the alienation and humiliation of these patients. The term ‘stigma’ describes physical characteristics or character traits that mark the bearer as having lower social value ( 2 ). A stigmatized trait can lead to experiences of discrimination, and the feeling of being stigmatized can put one at risk for low self-esteem ( 3 ), depression ( 4 – 6 ) and lower quality of life ( 7 – 10 ). However, the empirical evidence on stigma overall and obesity stigma in particular is scattered across diverse disciplines and lines of research, making it difficult to get a clear picture of the implication of obesity stigma for healthcare providers and their patients.
In order to address this gap, we critically reviewed literature related to the impact of obesity stigma on interpersonal encounters and decision-making. We discuss potential implications, including several mechanisms whereby stigma may affect patient-centred communication and care, defined by the Institute of Medicine ( 11 ) as ‘care that establishes a partnership among practitioners, patients, and their families (when appropriate) to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care’ (p. 7). We also suggest several strategies that may help healthcare providers and clinics reduce the impact of stigma on patients with obesity.
Obesity is a commonly and strongly stigmatized characteristic ( 12 , 13 ). There is substantial empirical evidence that people with obesity elicit negative feelings such as disgust, anger, blame and dislike in others ( 14 – 16 ). Despite the high prevalence of obesity (approximately one-third of the US adult population ( 17 ) ), individuals with obesity are frequently the targets of prejudice, derogatory comments and other poor treatment in a variety of settings, including health care ( 12 , 18 ). Furthermore, there is a growing body of evidence that physicians and other healthcare professionals hold strong negative opinions about people with obesity ( 19 – 27 ).
We conducted a narrative review of this literature to highlight the ways that the obesity stigma may interrupt the healthcare process and impede many healthcare providers' goal of providing equitable high-quality care. We reviewed all original studies in the fall of 2014 on topics related to obesity stigma in medical care and/or the impact of stigma on interpersonal encounters and decision-making in PubMed and PsychInfo, with the majority of studies found in health communication, social psychology and health disparities research. We then selected papers relevant to the potential impact of obesity stigma on healthcare provider behaviour, patient healthcare outcomes and healthcare encounters.
Impact on providers
Primary care providers and health promotion specialists, who typically demonstrate a commitment to providing care for underserved populations, are unlikely to flagrantly and intentionally discriminate against their patients. Nevertheless, there are several ways that their attitudes about obesity may cause their patients with obesity to feel disrespected, inadequate or unwelcome, thus negatively affecting the encounter quality and their willingness to seek needed care (see Fig. Fig.1). 1 ). Behaviours that emanate from negative attitudes about a stigmatized group are known as enacted stigma ( 28 ). Enacted stigma on the part of the provider affects the patient in both measurable and immeasurable ways. It can reduce the quality, and even the quantity, of patient-centred care, and can signal to the patient that he or she is being perceived in terms of his or her stigmatized identity, which, in turn, may affect patient perception of, and compliance with, provider recommendations.

A conceptual model of hypothesized pathways whereby the associations between obesity and health outcomes are partially mediated by healthcare providers' attitudes and behaviours about obese patients, and patients' response to feeling stigmatized.
The negative attitudes underlying enacted stigma can be explicit or implicit. Explicit attitudes are conscious and reflect a person's opinions or beliefs about a group. Implicit attitudes are automatic and often occur outside of awareness and in contrast to explicitly held beliefs ( 29 ). The response to some stigmatized groups, such as racial minorities among egalitarian Caucasians, often consists of negative implicit attitudes, but neutral or positive explicit ones ( 30 ). In contrast, explicit negative attitudes about people with obesity are more socially acceptable than explicit racism: e.g. it is acceptable in many Western cultures that people with obesity are the source of derogatory humour and may thus be openly – and unquestionably – portrayed as lazy, gluttonous and undisciplined. Primary care providers, medical trainees, nurses and other healthcare professionals hold explicit as well as implicit negative opinions about people with obesity ( 21 , 31 – 33 ). This has important implications for communication in the clinical interview, because explicit attitudes influence verbal behaviours as well as decisions that are within conscious control, whereas implicit negative attitudes predict non-verbal communication and decisions under cognitive burden ( 29 , 34 – 36 ). There is evidence that providers' communication is less patient-centred with members of stigmatized racial groups ( 37 – 43 ), and other stigmatized groups including patients with obesity ( 44 ), and that provider attitudes contribute to this disparity ( 45 – 47 ). Implicit attitudes have also been found to be associated with lower patient ratings of care ( 46 ). The combination of implicit and explicit negative obesity attitudes may elevate the potential for impaired patient-centred communication, which is associated with a 19% higher risk of patient non-adherence, as well as mistrust, and worse patient weight loss, recovery and mental health outcomes ( 48 – 53 ).
There are several mechanisms by which provider attitudes may affect the quality of, or potential for, patient-centred care. First, primary care providers engage in less patient-centred communication with patients they believe are not likely to be adherent ( 54 ). A common explicitly endorsed provider stereotype about patients with obesity is that they are less likely to be adherent to treatment or self-care recommendations ( 23 , 24 , 55 , 56 ), are lazy, undisciplined and weak-willed ( 12 , 55 , 57 – 59 ). Second, primary care providers have reported less respect for patients with obesity compared with those without ( 59 , 60 ), and low respect has been shown to predict less positive affective communication and information giving ( 61 ). Third, primary healthcare providers may allocate time differently, spending less time educating patients with obesity about their health ( 62 ). For example, in one study of primary care providers randomly assigned to evaluate the records of patients who were either obese or normal weight, providers who evaluated patients who were obese were more likely to rate the encounter as a waste of time and indicated that they would spend 28% less time with the patient compared with those who evaluated normal-weight patients ( 59 ). Finally, physicians may over-attribute symptoms and problems to obesity, and fail to refer the patient for diagnostic testing or to consider treatment options beyond advising the patient to lose weight. In one study involving medical students, virtual patients with shortness of breath were more likely to receive lifestyle change recommendations if they were obese (54% vs. 13%), and more likely to receive medication to manage symptoms if they were normal weight (23% vs. 5%) ( 23 ).
Impact on patients
Experiences of discrimination and awareness of stigmatized social status can cause patients to experience stress and have other acute reactions that may reduce the quality of the encounter, regardless of their provider's attitudes and behaviour. Three conceptually overlapping processes – identity threat, stereotype threat and felt stigma – describe the stigmatized patient's reaction to being stigmatized. Identity threat occurs when patients experience situations that make them feel devalued because of a social identity. Social identities are the categories, roles, and social groups that define each person and give a sense of self ( 63 , 64 ). Each social identity, be it a professional identity, a gender identity, or identity as a person who is obese, has emotional significance for the individual, is closely tied to self-esteem, and can empower or make one vulnerable. Obesity is stigmatized, and thus is more likely to make the individual aware of the possibility for rejection or derogation than make him/her feel confident and empowered. Stereotype threat occurs when an individual is aware that he or she may be viewed as a member of a stigmatized group, and becomes preoccupied with detecting stereotyping on the part of the provider and monitoring his or her own behaviour to ensure that it does not confirm group stereotypes ( 65 ). Felt stigma is a term used to describe the expectation of poor treatment based on past experiences of discrimination ( 28 ).
The effects of stigma are both immediate and long-term. The direct effects of provider attitudes on patient-centred care may reduce the quality of the patient encounter, harming patient outcomes and reducing patient satisfaction. Patients with obesity who experience identity/stereotype threat or felt/enacted stigma may experience a high level of stress which can contribute to impaired cognitive function and ability to effectively communicate ( 66 ). Accumulated exposure to high levels of stress hormones (allostatic load) has several long-term physiological health effects, including heart disease, stroke, depression and anxiety disorder, diseases that disproportionately affect obese individuals and have been empirically linked to perceived discrimination ( 67 – 69 ). Indeed, stress pathways may present an alternate explanation for some proportion of the association between obesity and chronic disease ( 70 ).
Other effects include avoidance of clinical care if patients perceive that their body weight will be a source of embarrassment in that setting ( 71 , 72 ). For example, there is evidence that obese women are less likely to seek recommended screening for some cancers ( 72 – 76 ). The long-term result of avoidance and postponement of care is that people with obesity may present with more advanced, and thus more difficult to treat, conditions. Individuals who are stigmatized, or are vigilant for evidence of stigma, may withdraw from full participation in the encounter. Because of this, they may not recall advice or instructions given by the provider, reducing adherence to prescribed treatment or self-care. Experiencing stereotype threat may also cause patients to discount feedback provided by the source of the threat ( 77 ), which in turn may affect adherence. Patients who report feeling judged by their primary care provider are less likely to seek or achieve successful weight loss ( 78 , 79 ). Patients who have tried to lose weight and failed may ‘dis-identify’, or reduce their efforts to lose weight, in order to disconnect their self-esteem from achievement in a domain with which they have not had success ( 65 ), and may feel shame for failing to lose weight or maintain weight loss ( 78 ). Along similar lines, individuals who experience more obesity stigma report less health utility, or place lower value on health ( 80 ).
Setting factors
Felt stigma and identity/stereotype threat can be triggered by experiences in the healthcare clinical setting that signal to the patient that his/her identity as a person who is obese is salient and possibly devalued. A typical primary care clinical encounter has many such signals, including weight measurement, dietary assessment, and queries about physical activity. Providers are also encouraged to provide unsolicited weight loss counsel as well as to assess patients' willingness to alter behaviours that are associated with obesity. There is evidence that many providers dislike treating obesity, feel underprepared to do so, and have little hope that their patients will make lifestyle changes ( 55 , 81 – 84 ), which may be detectable in their tone of voice or language. They may also signal overly simplified assumptions about the causes of obesity, by suggesting, for example, that their patients cut back on fast food or consider taking the stairs instead of elevators. These assumptions ignore the complexity of energy balance and propagate a common misunderstanding that weight loss is as simple as ‘calories in < calories out’ ( 85 ). Such counsel, despite its positive intentions to optimize patient health, may create unrealistic expectations about the effects of small lifestyle changes, which may lead to disappointment and recidivism. This counsel can also have unintended side effects if it signals to patients that they are seen solely in terms of their stigmatized identity. This could create a state of threat that may affect the patient's emotional state, ability to communicate effectively, and attitude towards medical advice ( 86 ).
Clinic equipment may also promote identity threat for patients with obesity ( 87 , 88 ). Waiting room chairs with armrests can be uncomfortable or too small. Equipment such as scales, blood pressure cuffs, examination gowns and pelvic examination instruments are often designed for use with smaller patients. When larger alternatives are not available, or are stored in a place that suggests infrequent use, it can signal to patients that their size is unusual and that they do not belong. These experiences, which are not delivered with malicious intent, can be humiliating.
Potential strategies to address obesity stigma in clinical care
Promising strategies to reduce stigma in the primary care setting include improving provider attitudes about patients with obesity and/or reducing the likelihood that negative attitudes influence provider behaviour; altering the clinic environment or procedures to create a setting where patients with obesity feel accepted and less threatened; and empowering patients to cope with stigmatizing situations and attain high-quality health care ( 86 , 89 ). Here we focus on strategies that clinics or healthcare organizations might implement to improve the experience of patients with obesity or overweight. Some of the studies discussed here are firmly rooted in research evidence, but some are untested strategies that will require research to test their effectiveness.
Our intent was to highlight the salience of obesity stigma in health care and the potential to re-frame and optimize provider–patient encounters. Our work recognizes the contributions of interdisciplinary scholars, in fat studies and elsewhere, who have raised awareness of how cultures conceptualize body size, and consequently, how body size itself can inform identity. Such scholars have thus set much of the theoretical foundation for our work, even though our suggestions are not consistent with their advocacy for a weight-inclusive approach to medical care, in which obesity is seen as independent of health and weight reduction is not a focus of medical care ( 90 , 91 ). While there is evidence supporting this viewpoint, we focus on interventions that are more consistent with the dominant medical and nursing paradigms of obesity as a risk factor.
Reducing weight stigma in clinical care is a shared responsibility of healthcare providers and other clinic staff, as well as the healthcare systems/organizations that have the power to implement intervention strategies broadly. Many of the strategies we discuss here can be implemented by providers or clinics, but any of these strategies could be implemented more efficiently, and have a wider influence, if uptake was required of providers and clinic staff by healthcare organizations.
Strategies that clinics can implement to improve provider attitudes about people with obesity include the following. (i) Increase provider empathy through perspective-taking exercises. Perspective-taking exercises have improved provider attitudes towards stigmatized groups ( 92 ), although findings are mixed about its effectiveness in reducing obesity stigma ( 93 , 94 ). (ii) Alter perceived norms regarding negative attitudes and stereotypes about people with obesity. In one study, researchers reduced explicit bias against obese people by providing individuals information and evidence that their peers did not hold negative attitudes ( 95 ). To minimize the perception that anti-fat bias is the norm, one untested strategy could include implementing a zero-tolerance policy for comments or humour that stereotypes or degrades anyone based on a physical identity or attribute. (iii) Encourage provider instruction and practice in emotion regulation techniques that foster positive affect. High cognitive load and time pressure, characteristic of clinical care settings, impair judgments and decision-making ( 96 ). Furthermore, frustration that providers may feel towards ‘difficult’ or ‘complex’ patients or patients who they perceive are harming their own health, may elicit strong negative emotions. Although no studies have directly tested their effect on weight bias, evidence from one study of prejudice reduction suggests that emotion regulation tools such as meditation or deep breathing may help providers overcome these negative emotions and improve compassion and other pro-social emotions ( 97 , 98 ). (iv) An untested strategy to build awareness of weight bias and a felt need to address it might include encouraging providers to examine their explicit beliefs and stereotypes about obese people, and complete an assessment of implicit attitudes (e.g. the online Implicit Association Test at http://www.implicit.harvard.edu ). Provide information about the automatic nature of these attitudes and encourage providers to consciously strive to behave in ways consistent with helping and egalitarian values. And lastly, (v) educate providers on the genetic, environmental, biological, psychological and social contributors to weight gain and loss ( 99 , 100 ). Providers who understand this complex web of causality have more positive attitudes about patients with obesity ( 101 ). This information is likely less threatening for their patients than over-simplified messages like ‘eat less, move more’, or ‘calories in, calories out’ ( 102 ).
There are several strategies for providing a welcoming and less threatening healthcare environment to patients with obesity. (i) Reduce focus on body weight. Instead, focus on screening for the diseases and conditions for which obesity is a risk factor and encourage feasible behaviours that will improve health and well-being. This could be accomplished by weighing patients less frequently – for example, restricting weigh-ins to well-visit checkups and forgoing weigh-ins when visits are not associated with a weight-related reason. Increasing patients' knowledge of the health effects of obesity has shown little effect on weight loss ( 103 , 104 ). However, encouraging patients to not focus on weight or weight loss, but rather on the other benefits of physical activity and healthy eating, may reduce the threat of conversations about these behaviours, and thus increase the likelihood of behaviour change and maintenance ( 102 , 105 ). (ii) Adopt patient-centred communication strategies, such as motivational interviewing, which may be less threatening for patients and are associated with patient adherence and positive outcomes ( 48 , 51 – 53 , 106 – 108 ). (iii) Although its impact on felt stigma is not tested, one could ensure that the clinic environment is welcoming by providing chairs and medical equipment that are usable by patients of all sizes and by keeping specialized instruments for patients with obesity readily available to clinical staff. (iv) Convey a sense of identity safety by providing evidence that diversity is valued ( 109 ). Although untested, this could be accomplished by posting a mission statement that stresses the value of body size diversity or by using positive and non-stereotypical images of overweight and obese people in clinic advertisements, pamphlets or artwork. (v) Healthcare systems could ensure that the continuum of care includes adequate referral resources for behaviour change counselling, including providers or clinics specializing in weight loss strategies and remove barriers (e.g. requirement for a secondary diagnosis, long wait times for an appointment) to accessing these resources ( 78 ). Study is needed in this area to determine whether shifting the threat of discussing weight loss strategies from the primary care setting to a specialty care setting may improve utilization of primary health care. These providers may also be more skilled at using communication strategies that are not threatening.
Healthcare providers strive to provide the highest quality health care for their patients. This effort may be hindered by interpersonal and environmental cues that convey that patients with obesity are not welcome or by behaviours that lower the quality of communication in the encounter. Attitudes towards obesity as a health risk factor can exacerbate and mask negative attitudes towards individuals with obesity. Healthcare providers often view obesity as an avoidable risk factor that impedes their ability to treat and prevent disease. As this is a largely unchallenged perspective on obesity , healthcare providers may be less self-aware of their propensity to, and feel less pressure (internally or from external sources) to, behave in a non-prejudicial way towards people with obesity .
A great deal more research is needed to understand the impact of stigma on care for people with obesity. Much of the extant research involves small or convenience samples and requires replication with more generalizable populations. There are several important gaps in the literature on weight bias and health care. While several studies have found high levels of explicit bias in healthcare providers, there is a need for more research on weight stigma using measures of implicit bias. More research is also needed to identify the impact of those attitudes on aspects of the medical encounter, including decision-making and communication, as well as the differential effects of those attitudes by gender, race, socioeconomic status, sexual orientation, and other characteristics. The development and testing of novel interventions is also needed to reduce bias or its impact on behaviour in medical trainees, practicing physicians, other healthcare providers, and other staff members of healthcare organizations.
It is important to note the tension between obesity stigma literature or literature advocating a weight-inclusive approach ( 91 ) and the body of literature that supports increased provider attention to body weight and weight loss as a strategy to encourage behaviour change. We believe that the strategies and perspectives reviewed here are not contrary to this evidence, but may inform the refinement of interventions in order to avoid unintended consequences brought on by stigma, and maximize the effectiveness of patient behaviour change intervention.
Acknowledgments
Dr. Phelan is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K01DK095924. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement
Drs. Burgess, Hellerstedt, Griffin, and van Ryn do not report any potential conflicts of interest. Dr. Phelan and Dr. Yeazel report grants from the National Institutes of Health during the conduct of the study.

IMAGES
VIDEO
COMMENTS
Obesity stereotypes were selected from the studies of Vartanian et al. and Cheng . Specifically, this study included five negative stereotypes (lazy, sloppy, self-indulgent, lacking in self-discipline, and clumsy) and five positive stereotypes (kind, warm, optimistic, simple and honest, and generous). Participants were asked to rate the extent ...
Obesity stereotypes were selected from the studies of Vartanian et al. (2015) and Cheng (2017). Specifically, this study included five negative stereotypes (lazy, sloppy, self-indulgent, lacking in self-discipline, and clumsy) and five positive stereotypes (kind, warm, optimistic, simple and honest, and generous).
Introduction to obesity stigma. Obesity is a complex, chronic disease characterised by abnormal excess body fat that negatively affects physical 1 and mental 2 health. It has also been associated with significant financial burdens in developed and developing countries. 3 According to the World Health Organization (WHO), obesity is rising worldwide, and its global prevalence almost doubled ...
However, research aimed at reducing obesity stereotyping is relatively rare, and prior studies have focused primarily on negative stereotypes. Based on the empathy-altruism hypothesis and self-other overlap hypothesis, this study investigates the impact of perspective taking (PT) on both positive and negative obesity stereotypes and examines ...
1 INTRODUCTION. Social stigma is a fundamental driver of population health inequalities. 1 Although this has been recognized for decades, 2 detrimental effects of the stigma of body size and weight have gained wider acknowledgement only recently. 3 Societal weight stigma is pervasive 4, 5 and suggested to be in part driven by the increased blame and shame framing of obesity in media and public ...
Based on the empathy-altruism hypothesis and self-other overlap hypothesis, this study investigates the impact of perspective taking (PT) on both positive and negative obesity stereotypes and ...
Obesity stigmatisation has become a major topic of research, with empirical evidence showing negative consequences for people who are stigmatised. 1. With research showing that obesity stigmatisation is widespread and that antifat attitudes are strong, 2. there have been not only calls for intervention but also criticism of sources that seem to ...
Forty-two percent of U.S. adults say they have faced some form of weight stigma, such as being teased about their weight or treated unfairly because of it, with physicians and coworkers listed as some of the most common sources (Lee, K. M., et al., International Journal of Obesity, Vol. 45, 2021; Puhl, R. M., et al., International Journal of ...
with obesity (e.g., type II diabetes, heart disease, high blood pressure, stroke) have pushed obesity to the fore as a public and national health concern (Ernsberger & Koletsky, 1999). The belief that people with obesity are unhealthy is another nega-tive aspect of an already negative and deeply discrediting stereotype because it too
Authentic self-awareness moderated the relationship between weight-based stereotype threat and work ability (β = 0.14, p < 0.001), such that the relationship between stereotype threat and work ...
We then performed a narrative review of the existing empirical evidence regarding the impact of obesity stigma and weight bias for healthcare quality and outcomes. Many healthcare providers hold strong negative attitudes and stereotypes about people with obesity. There is considerable evidence that such attitudes influence person-perceptions ...
Recent concerns with the increasing prevalence of overweight and obesity among children and adults indicate the need to better understand the psychosocial correlates of weight. We examined the relationships among negative stereotypes of obesity, "thin ideal" beliefs, perceptions of the causes of obesity and of control over weight, body esteem, and global self-esteem. A negative correlation ...
The PDG submitted a series of questions which cover two key aspects of obesity and its management: weight bias and stigma and the effectiveness and impact of weight management ... as the negative attitudes or stereotypes people hold against the obese and any subsequent prejudice or discrimination. ... Since this review several more papers have ...
To help tackle the UK's obesity crisis, we must better educate medical professionals on weight stigma, according to the conclusions of a large-scale review led by UCL researchers. ... based on stereotypes and prejudices about people who are either obese or overweight. In healthcare, the negative biases associated with weight stigma are known ...
Abstract. Objective: The Multi-Threat Framework accounts for potentially different forms of stereotype threat that differ in target (i.e., the individual or the group) and source (i.e., the self or others). This investigation examined how these different forms of perceived stereotype threat were related to concepts, such as group identity, stereotype endorsement, stigma consciousness, etc ...
The focus on personal responsibility results in blaming people with obesity for their condition, and enables the stereotyping of people with obesity as lazy and lacking in willpower. It is argued by some that stigmatisation of people with obesity will incentivise them to lose weight. However, evidence shows that this is a counterintuitive ...
This essay will focus on the obesity stereotype among adults in the United Kingdom. The aspects of obesity stereotype that will be discussed include some background, how the stereotype occurs, the impacts of stereotyping, how to promote inclusiveness, and a personal reflection that focuses on how various aspects of my life have shaped my ...
Brozempic, Gender Stereotypes, and Obesity Care. Perhaps it was inevitable. Last week, the Times plunged into stereotypes about obesity care and gender, asking "Is the era of 'Brozempic' upon us?" The spark for the story comes from the efforts of telehealth businesses trying to crack the code for reaching men with concerns about obesity.
In a study, people with sleep apnea who were randomly assigned to take the weight-loss drug Zepbound had an average of about 30 fewer apnea episodes per hour. Brendan Mcdermid/Reuters. By Gina ...
We conducted a search of Medline and PsychInfo for all peer-reviewed papers presenting original empirical data relevant to stigma, bias, discrimination, prejudice and medical care. ... Many healthcare providers hold strong negative attitudes and stereotypes about people with obesity. There is considerable evidence that such attitudes influence ...