- Case report
- Open access
- Published: 10 March 2023

A 14-year-old boy with multiple trauma and bilateral basal ganglia hemorrhage due to coronavirus disease 2019: a case report
- Payman Asadi 1 , 2 , 4 ,
- Saba Maleki 1 , 2 , 3 ,
- Seyyed Mahdi Zia Ziabari 1 , 3 , 4 &
- Nazanin Noori Roodsari 1 , 2 , 3
Journal of Medical Case Reports volume 17 , Article number: 88 ( 2023 ) Cite this article
1420 Accesses
1 Citations
1 Altmetric
Metrics details
In December 2019, coronavirus disease 2019 spread worldwide, causing acute respiratory distress syndrome. Coronavirus disease 2019 presents from an asymptomatic infection to severe disease causing multiorgan failure. Neurological manifestations were observed in some patients, including intracerebral hemorrhage. Bilateral basal ganglia hemorrhage is rare due to trauma.
Case presentation
Our patient was a 14-year-old Iranian boy with multiple trauma and loss of consciousness who tested positive for coronavirus disease 2019. The brain computed tomography scan reported bilateral basal ganglia hemorrhage. Bilateral ground glass opacity was reported through a chest computed tomography scan.
Discussion and conclusions
In this study, we reported a 14-year-old boy referred to the emergency room due to multiple trauma. Through the medical interventions, bilateral basal ganglia hemorrhage was discovered incidentally. Coronavirus disease 2019 was detected in this patient on the basis of findings in chest computed tomography scan and positive real reverse transcription polymerase chain reaction test. Several clinical reports and series exploring the relationship between coronavirus disease 2019 and ischemic strokes have been published. Coronavirus disease 2019, like other acute respiratory syndromes, can invade the central nervous system through hematogenous and neuronal dissemination or it can be an immune response to the cytokine storm. In conclusion, it is vital to know the pathophysiology of the neurological manifestations of coronavirus disease 2019 and prevent the mild neurological manifestations leading to severe conditions.
Peer Review reports
Introduction
Severe acute respiratory syndrome–coronavirus-2 (SARS–CoV-2) caused coronavirus disease 2019 (COVID-19) in Wuhan, China in December 2019. COVID-19 is a contagious respiratory disease spreading worldwide [ 1 ]. COVID-19 can appear from an asymptomatic situation to acute respiratory distress syndrome (ARDS) and eventually multiorgan damage [ 2 ]. The central nervous system (CNS) can be involved in COVID-19. Some neurological manifestations of COVID-19 include dizziness, headache, hypogeusia, hyposmia, ataxia, seizure, ischemic stroke, cerebral hemorrhage, encephalopathy, encephalitis, meningitis, seizure, cerebral vein thrombosis, and Guillain–Barre syndrome [ 3 ]. Intracranial hemorrhage (ICH) is an uncommon situation due to COVID-19. This may happen because of some risk factors such as arterial hypertension or anticoagulant therapy [ 2 ]. Expression of angiotensin-converting enzyme 2 (ACE2) in glial cells and neurons may be a possible etiology for the neurological manifestation of COVID-19 [ 4 ]. In this case study, we will report bilateral basal ganglia hemorrhage in a 14-year-old boy who tested positive for COVID-19 and denied any past medical history or anticoagulant consumption.
The case is a 14-year-old Iranian boy with no past medical history presenting with multiple trauma from a motorcycle accident who was transferred to the Poursina hospital emergency room (ER) in Rasht on 9 June 2020. In addition, he had an extensive laceration on his right knee and a star-shaped laceration on his parietal region. O 2 saturation was 93%, temperature was 38.5 °C, and the other vital signs were stable. In the ER, his Glasgow Coma Scale (GCS) score was 3/15 (E1V1M1). No free fluid in the abdomen and pelvic cavity in focused assessment with sonography for trauma was reported. A right bundle branch block was observed in his electrocardiogram (ECG). Echocardiography was performed and reported as normal. He was then referred to the neurosurgery ward and was hospitalized for almost 40 days.
He had no signs and symptoms related to COVID-19. However, during hospitalization, spiral high-resolution computed tomography (HRCT) scan of his lung without contrast revealed patchy ground-glass opacity in both lungs (mostly in the right lung) (Fig. 1 ). These findings suggested that the patient was infected by COVID-19. Finally, the COVID-19 infection was confirmed by consecutive positive reverse transcription polymerase chain reaction (RT-PCR) test.

Patchy ground-glass opacities in both lungs, especially in the right lung, propounded by COVID-19 infection. Heart size is normal. Pleural effusion is not seen. Chest wall is normal
Following a brain CT scan, a deep intracranial hemorrhage in the thalamus was found (Fig. 2 A). The contusion of the right parietal lobe without hydrocephalus and midline shifts were reported (Fig. 2 B). Furthermore, no spinal fractures and displacements were reported in his cervical spine CT scan. Abdominal and pelvic CT scan were also normal.
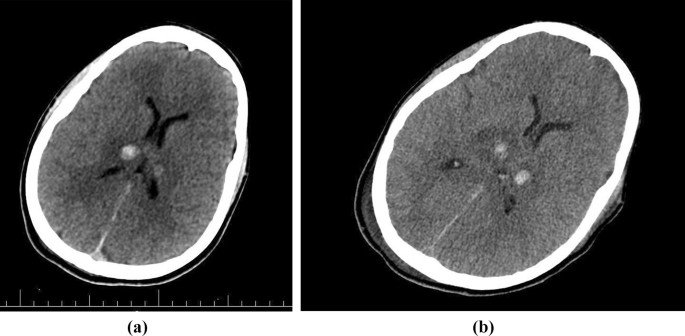
A CT scan of the brain at the ER showing two hyperdense lesions in the thalamus and parenchymal edema. B Brain CT scan taken after a few days, showing no midline shift, and ventricular edema less than previous CT scan
His laceration of the parietal region was repaired by surgery. In addition, the repair and debridement of the right knee laceration were carried out. Afterward, he was intubated and a collar fixed his cervical spine. He was treated with lasix and mannitol because of raised intracranial pressure. After supportive therapy for almost 40 days, he was discharged after educating his parents about his care at home, while his GCS was 6/15 (E2V1M3).
In this study, we reported a 14-year-old boy referred to the ER due to multiple trauma. He had no history of coagulopathy or anticoagulant consumption. In this case, trauma precipitated parietal contusion. Through medical interventions, bilateral basal ganglia hemorrhage was discovered incidentally.
Several clinical reports and series exploring the relationship between COVID-19 and ischemic strokes have been published [ 5 ].
Neurologic symptoms in COVID-19 can be divided into several categories, ranging from nonspecific symptoms such as a headache to severe forms such as cerebrovascular disease [ 6 ].
Basal ganglia hemorrhage due to traumatic events is rare [ 7 ].
Systemic and metabolic disease, neurodegenerative disease, and vascular disease can involve basal ganglia and thalamus [ 8 , 9 ].
COVID-19, like other acute respiratory syndromes, can invade the central nervous system (CNS) through hematogenous and neuronal dissemination, or it can be an immune response to the cytokine storm [ 10 , 11 ].
There is not enough data about the underlying mechanisms of neurological disorders caused by COVID-19. A total of 2% of patients have neurological symptoms. One of the ways in which COVID-19 can invade the neurological system is through the mucous layer of the nose that contains the olfactory receptor cells. Olfactory nerves might deliver viruses and infections to the brain. On the other hand, COVID-19 causes respiratory infection and the level of oxygen in blood may decrease. Brain function can be impaired through hypoxemia (Fig. 3 ) [ 12 ].
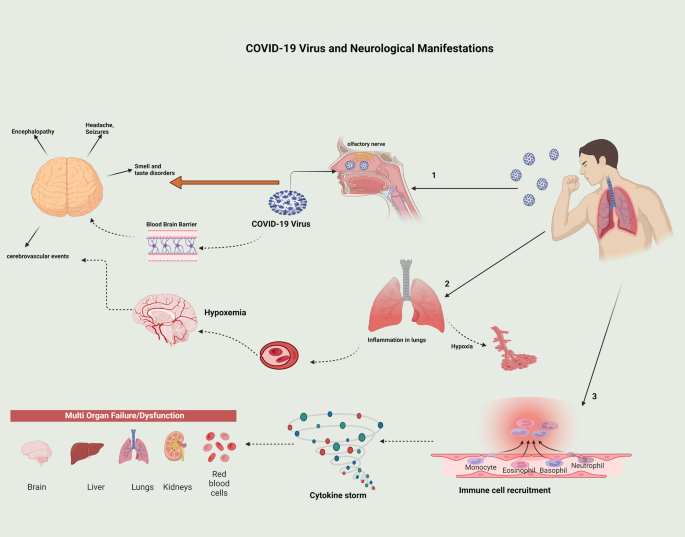
Representation of how COVID-19 can cause neurological manifestations such as headache, seizure, smell and taste disorders, encephalopathies, and cerebrovascular events
Some other pathophysiology of ischemic stroke in COVID-19 are hypoperfusion of the brain, hypertension leading to posterior reversible encephalopathy syndrome, and septic embolization in patients with bacterial superinfection (Fig. 3 ) [ 13 ].
ACE2 serves important roles in various parts of the body, such as the lung, kidney, brain, liver, and endothelial cells. COVID-19 decreases the expression of ACE2. Due to reduced ACE2 levels, the renin–angiotensin–aldosterone system (RAAS) will deteriorate and cause multiorgan damage. Diminished ACE2 can cause intracerebral hemorrhage through several mechanisms. For instance, increasing the blood pressure, endothelial dysfunction, damage to the brain vessels, and finally depression of angiotensin-(1-7) and Mas receptor [Ang (1-7)/MasR] signaling, which has a neuroprotective, antifibrotic, and vasodilatory effect [ 14 , 15 ].
Immune response to the cytokine storm and chemokines can disrupt the blood–brain barrier and neuroinflammation. The breakdown of the blood–brain barrier and inflammation both have a main role in ischemic stroke [ 16 , 17 ].
Intracranial hemorrhage was documented in some cases as a complication of COVID-19. Some risk factors are arterial hypertension and anticoagulation therapy (pretreatment of unrelated disease to COVID-19 thromboprophylaxis) [ 2 ].
Hyperinflammatory state may be the main cause of complication in patients with diabetes mellitus (DM) as well as COVID-19. A case series was reported in October 2020 that included three patients with COVID-19 and ICH. All three patients had risk factors for ICH such as hypertension and DM. DM and ICH are associated through some mechanisms. High blood glucose can cause endothelial dysfunction. Dysfunction of the brain’s small vessel endothelial can lead to ICH [ 14 ].
There is a hypothesis that the state of hyperinflammation in diabetic patients is related to higher mortality in these patients [ 18 ]. High C-reactive protein (CRP) levels are a risk factor for stroke. High CRP levels may lead to ICH in patients with COVID-19 [ 19 ].
We reported a 14-year-old boy with bilateral basal ganglia hemorrhage and documented COVID-19. Our patient had no special past medical history of hypertension, DM, and other diseases. There is no evidence that he consumed anticoagulant agents before. There is some research that ICH is propounded as a complication of COVID-19. Basal ganglia hemorrhage related to trauma is rare [ 7 ].
The underlying pathophysiology for COVID-19 related ICH can involve hyperinflammatory state due to increased cytokine production. Although a few case series and case reports were published on some patients COVID-19 as well as ICH, more investigation and research regarding the association between COVID-19 and ICH are needed.
Conclusions
It is essential to discover the pathophysiology of neurological manifestations of COVID-19. Neurological findings of COVID-19 range from mild conditions such as headache to severe conditions such as stroke. Therefore, acknowledgement as to the causes and prevention of the situations leading to critical events should be considered in treatments of COVID-19.
Availability of data and materials
The datasets obtained and analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
Coronavirus disease 2019
Computed tomography scan
- Intracranial hemorrhage
Glasgow Coma Scale
Electrocardiogram
Reverse transcription polymerase chain reaction
Central nervous system
Diabetes mellitus
C-reactive protein
Emergency room
Acute respiratory distress syndrome
Angiotensin-converting enzyme 2
High-resolution CT scan
Renin–angiotensin–aldosterone system
Angiotensin-(1-7) and Mas receptor
Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al . A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–9.
Article CAS PubMed PubMed Central Google Scholar
Margos NP, Meintanopoulos AS, Filioglou D, Ellul J. Intracerebral hemorrhage in COVID-19: a narrative review. J Clin Neurosci. 2021;89:271–8.
Sharifi-Razavi A, Sedaghat Z, Baziboroun M, Karimi N. COVID-19 accompanied with intracerebral hemorrhage: a case series. Arch Clin Infect Dis. 2020;15(4): e104877.
Article CAS Google Scholar
Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–8.
Article CAS PubMed Google Scholar
Benger M, Williams O, Siddiqui J, Sztriha L. Intracerebral haemorrhage and COVID-19: clinical characteristics from a case series. Brain Behav Immun. 2020;88:940.
Abboud H, Abboud FZ, Kharbouch H, Arkha Y, El Abbadi N, El Ouahabi A. COVID-19 and SARS-Cov-2 infection: pathophysiology and clinical effects on the nervous system. World Neurosurg. 2020;140:49–53.
Article PubMed PubMed Central Google Scholar
Kankane VK, Gupta TK, Jaiswal G. Traumatic bilateral basal ganglia bleed: a report of rare two cases and review of the literature. Asian J Neurosurg. 2016;11(4):457.
Ghoshal S, Gokhale S, Rebovich G, Caplan LR. The neurology of decreased activity: abulia. Rev Neurol Dis. 2011;8(3–4):e55-67.
PubMed Google Scholar
Bao Y, Lin SY, Cheng ZH, Xia J, Sun YP, Zhao Q, et al . Clinical features of COVID-19 in a young man with massive cerebral hemorrhage—case report. SN Compr Clin Med. 2020;2(6):703–9.
Haddadi K, Ghasemian R, Shafizad M. Basal ganglia involvement and altered mental status: a unique neurological manifestation of coronavirus disease 2019. Cureus. 2020;12(4): e7869.
PubMed PubMed Central Google Scholar
Alqahtani A, Alaklabi A, Kristjansson S, Alharthi H, Alam H. Acute necrotic hemorrhagic leukoencephalitis related to COVID-19: a report of 2 cases. Radiol Case Rep. 2021;16(9):2393–8.
Ahmadirad N, Ghasemi Z. COVID-19 and central nervous system: entry routes and. Basic Clin Neurosci. 2020;11(2):217.
Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al . SARS-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51(7):2002–11.
Pavlov V, Beylerli O, Gareev I, Torres Solis LF, Solís Herrera A, Aliev G. COVID-19-related intracerebral hemorrhage. Front Aging Neurosci. 2020;12:352.
Article Google Scholar
Steardo L, Steardo L Jr, Zorec R, Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol. 2020;229: e13473.
Liu R, Pan M-X, Tang J-C, Zhang Y, Liao H-B, Zhuang Y, et al . Role of neuroinflammation in ischemic stroke. Neuroimmunol Neuroinflamm. 2017;4:158–66.
Yang C, Hawkins KE, Doré S, Candelario-Jalil E. Neuroinflammatory mechanisms of blood–brain barrier damage in ischemic stroke. Am J Physiol Cell Physiol. 2019;316(2):C135–53.
Tadic M, Cuspidi C, Sala C. COVID-19 and diabetes: is there enough evidence? J Clin Hypertens. 2020;22(6):943–8.
Liu Y, Wang J, Zhang L, Wang C, Wu J, Zhou Y, et al . Relationship between C-reactive protein and stroke: a large prospective community based study. PLoS ONE. 2014;9(9): e107017.
Download references
Acknowledgements
The author would like to thank Parnian Shobeiri for commenting on this manuscript.
This research did not receive any specific grant from funding agencies.
Author information
Authors and affiliations.
School of Medicine, Guilan University of Medical Sciences (GUMS), Rasht, Guilan Province, Iran
Payman Asadi, Saba Maleki, Seyyed Mahdi Zia Ziabari & Nazanin Noori Roodsari
Roud Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
Payman Asadi, Saba Maleki & Nazanin Noori Roodsari
Clinical Research Development Unit of Poursina Hospital, Department of Emergency Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
Saba Maleki, Seyyed Mahdi Zia Ziabari & Nazanin Noori Roodsari
Department of Emergency Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
Payman Asadi & Seyyed Mahdi Zia Ziabari
You can also search for this author in PubMed Google Scholar
Contributions
PA, NN, and MZ treated the patient. SM and PA wrote the manuscript. All authors revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nazanin Noori Roodsari .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the institutional board review at Guilan University of Medical Sciences with the ethics code of IR.GUMS.1401.276.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Asadi, P., Maleki, S., Zia Ziabari, S.M. et al. A 14-year-old boy with multiple trauma and bilateral basal ganglia hemorrhage due to coronavirus disease 2019: a case report. J Med Case Reports 17 , 88 (2023). https://doi.org/10.1186/s13256-023-03824-1
Download citation
Received : 15 September 2022
Accepted : 15 February 2023
Published : 10 March 2023
DOI : https://doi.org/10.1186/s13256-023-03824-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Basal ganglia hemorrhage
- Neurological manifestations
- Neuroimaging
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

International Emergency Medicine Education Project
We promote emergency medicine and provide free, reusable education resources for medical students and educators
Multiple Trauma
by Pia Jerot and Gregor Prosen
Case Presentation
A 28-year old male was a restrained driver in a head-on motor vehicle collision. He was entrapped and extricated from the vehicle. Transient loss of consciousness was reported. He complains of severe chest pain, abdominal pain, and right upper leg pain.
Critical Bedside Actions and General Approach
Multiple trauma patients are primarily stabilized by the ambulance crew on the field according to Prehospital Trauma Life Support (PHTLS) or International Trauma Life Support (ITLS) algorithm. This chapter is about the approach to multiple trauma patients in the resuscitation room and mainly focuses primary survey.
Preparing For Patient Arrival
The ambulance service has to provide information to the trauma center for the arrival of the seriously injured patient. The trauma team puts on protective clothing (rubber latex gloves, plastic aprons, eye protection, etc.). A team leader should brief the team and make sure that every member knows his role and all necessary equipment is ready.
Primary Survey
In the first few minutes, a primary survey has to be done. The primary survey is a structured assessment in which we identify and immediately treat conditions that are life-threatening. The primary survey should always be the same, following the ABCDE algorithm listed below.
A: airway and cervical spine control B: breathing C: circulation D: disability E: exposure
In case of massive external hemorrhage, “C” takes advantage over A and B. When the bleeding is controlled, we can continue with A and B.
A – Airway and cervical spine control
When the patient arrives at the trauma center, talk to the patient and quickly asses his consciousness and airway. If the patient is conscious and talking with a normal voice, his airway is adequate for a period. If it is obstructed, the airway has to be secured. While securing the airway, C-spine has to be protected, especially when we are dealing with a patient with neck pain, focal neurological signs, coma, suspected head injury or a history of high-speed impact.
Do not delay C-spine and vertebra stabilization in a trauma patient with proper size of c-collar, side pads, and trauma board ..

The airway can be temporarily opened with a jaw thrust or basic adjuncts such as nasopharyngeal or oropharyngeal airway. If the patient’s airway is still compromised, it should be secured by endotracheal intubation or surgical airway. Indications for endotracheal intubation are listed in Table 1 . Intubated patients should be monitored by continuous capnography.
B – Breathing
All trauma patients should be given 15 L O2 via non-rebreather mask. The respiratory rate has to be evaluated. Expose the chest, and inspect for any deformities, wounds, bruising, asymmetrical movement or flail chest. The chest has to be palpated for any crepitus or subcutaneous emphysema. The lungs should be auscultated to assess the presence of breathing sounds bilaterally.
Chest injuries that can impair breathing have to be identified and treated. Life-threatening thoracic conditions are tension pneumothorax, massive haemathorax, cardiac tamponade, open chest wound, flail chest. If any of those conditions are found, immediate action is needed.
We can also use ultrasound at this moment to identify pneumothorax, haemathorax, and cardiac tamponade.
C – Circulation and hemorrhage control
The main objective of this step is to identifying shock situation in the patients. If there is massive external hemorrhage, it should be controlled before we proceed with A and B assessment. Radial pulses, heart rate and blood pressure (BP) should be assessed at that stage. The patient should be attached to the monitor. If we are dealing with a major trauma patient, at least two large bore (14G or 16 G) IVs have to be established. As an alternative, intraosseous line can be used.
“Permissive hypotension” with systolic BP 80-90 mmHg should be maintained when bleeding is not controlled (internal bleeding). If the patient is hemodynamically unstable, fluid resuscitation should begin with 1 L of warm isotonic fluid, either normal saline or lactated Ringer’s. At this moment, it is better to keep in your mind that normal vitals are considered stage I shock which patients could lose up to 750 cc blood. So, starting fluid support to patients suspected multiple trauma is a standard approach regardless of their vital signs. If the patient is still unstable after 1 Liter of fluid or is having ongoing blood loss, we should administer a transfusion of O-negative blood and order type-specific blood. The patients who have an identified bleeding source will usually require surgical intervention. Do not delay surgery departments’ involvement. Internal bleeding in the thorax, abdomen, pelvis or around fractures of long bones (particularly femur) should also be evaluated. For identifying bleeding into abdominal, pleural, or pericardial cavities, we can use the bedside ultrasound ( e-FAST exam). In the hemodynamically unstable patient with normal e-FAST , one should think pelvic injuries.
What is your opinion about eFAST sample below in a patient with trauma and hypotension?

D – Disability
In the primary survey pupil size, symmetry and reactivity should be assessed. To detect the level of consciousness, the patient has to be assessed by AVPU scale. It stands for A: Awake, V: responds to voice or verbal commands, P: responds to painful stimuli, U: unresponsive.
If there is time, Glasgow Coma Scale (GCS) can be used to assess the level of consciousness. Otherwise, GCS is assessed in the secondary survey. GCS is listed in Table 2 .
And finally, patients should be evaluated for any lateralized motor deficits which motor part of the GCS may help for this. An important clue, the patients can not move their extremities because of focal injuries.
In this stage, blood glucose and body temperature should also be checked.
E – Exposure
All clothes have to be removed from the patient so that hidden injuries and bleeding can be identified. The patient has to be log-rolled. In a log-roll, back of the head, neck, posterior chest, lower back should be inspected, palpated and auscultated as appropriate. If necessary, the rectal examination can be applied at this moment. We have to avoid hypothermia during this stage.
Secondary Survey
The secondary survey can be done after the primary survey and when the patient is responding to resuscitation. It consists of taking history (see “SAMPLE” mnemonic below), head to toe assessment (including log-roll), interpreting results of investigations, formulating a management plan for the patient and documenting all findings.
S: symptoms – social A: allergies M: medications P: past medical history L: last meal E: environment and events
Differential Diagnoses
There are critical conditions which should have been diagnosed during the primary survey. These are;
- A: Airway obstruction caused by c-spine injury, foreign body, etc.
- B: Tension pneumothorax, flail chest, massive haematothorax, chest wound
- C: Shock because of cardiac tamponade, intra-abdominal, intrathoracic, intrapelvic hemorrhage, external hemorrhage
- D: Head injury
- E: Fractures, dislocations and small wounds
History and Physical Examination Hints
History and physical examination hints to help “rule in or rule out” differential diagnoses are listed in Tables 3 . As an example, any patients with head, neck, facial injury or having abnormal breath sounds should be suspected of an obstructed airway. Any patients with severe shortness of breath, decreased or absent breath sounds on the lung, and hypotension is a tension pneumothorax until proven otherwise.
Emergency Diagnostic Tests and Interpretation
Laboratory tests.
Laboratory evaluation of the trauma patient is used for assessing the adequacy of resuscitation, for determining the proper transfusion products and the onset of coagulopathy and for baseline values for follow-up studies.
When IV access has been established, 20 mL of blood should be taken for a full blood count, urea, electrolytes and for blood group type or full cross-match. An arterial blood should also be taken for blood gas and pH analysis, but it can be taken at the end of the primary survey. If there is a very limited amount of blood taken, blood group type and cross-match should be the only test for the patient.
The e-FAST (Extended Focused Assessment with Sonography for Trauma) should ideally be a part of the primary survey, especially for unstable patients. It can be used for evaluating pneumothorax, free fluid in thorax and abdomen and to identify cardiac tamponade.
What is your diagnosis and next action for a trauma patient with below eFAST view?
A trauma patient should be radiographically evaluated with chest and pelvic radiographs. C-spine X-ray was traditionally used. Nowadays, any low-risk criteria violation is considered for computerised tomographic evaluation for the cervical spine. Cervical spine imaging can be delayed if there are no neurologic findings or persistent moderate hypotension. For assessing C-spine and other injuries, CT scan is the best choice in the acute setting, when the patient is stable.
What is your diagnosis and next action for a trauma patient with below CT scan?

Imaging studies of the thoracolumbar spine and extremities can be delayed until higher priority assessments and interventions are complete.
Emergency Treatment Options
Initial stabilization.
Initial stabilization should be done during primary survey. The algorithm is shown in Figure 1 . The goal is every abnormality detected during the primary survey should be fixed.
Medications
Drugs needed for rsi.
For RSI, you will need a pretreatment agent (mainly fentanyl), induction agent (mainly ketamine or etomidate) and paralytic agent (mainly rocuronium). Dosages and characteristics of drugs are listed in Table 4 . Doses must be adjusted in the hypotensive or shocked patient.
For analgesia, opioids or ketamine can be used. Dosages and characteristics of drugs are listed in Table 4 .
All procedures for initial stabilization should be done in the primary survey.
Airway: If the patient’s airway is compromised after a jaw thrust, nasopharyngeal or oropharyngeal tube placement, then orotracheal intubation is indicated. Rapid sequence intubation should be done. If it is unsuccessful, the surgical airway should be established.
Breathing: If tension pneumothorax is found in the primary survey, it should be decompressed immediately. Tube thoracostomy should be followed this procedure. If massive haemathorax is found, thoracostomy should be performed. However, in this situation, please make sure that the patient was supplied with enough volume and blood. Informing trauma surgery or thoracic surgery for potential thoracotomy risk is a wise approach.
Circulation: If massive bleeding is found, it should be controlled immediately. If cardiac tamponade is found, it should be treated with pericardiocentesis.
Pediatric, Geriatric, and Pregnant Patient Considerations
Pediatric patient considerations.
Airway: Airway should be checked the same as in an adult patient. When positioned flat on a stretcher, the occiput can flex the neck and the floppy upper airway which can result in occlusion of the airway. To prevent this, place a pad under the torso of children younger than eight years.
Breathing: Normal respiratory rates vary in different ages. Newborn respirates 25-50 breath per minute while 6 months to 12 year kids respirate 15-30 breath per minute.
Circulation: Brachial and femoral pulses are usually easy to feel. A weak, rapid pulse with a rate over 130 is a sign of shock in children all ages except neonates. Children have a strong compensatory mechanism in early shock and later deteriorate very quickly. When giving fluid resuscitation, give 20 mL/kg in each bolus.
Disability: When evaluating an injured child, the care provider should remember that children of various ages have different cognitive skills and interact differently. For assessing child`s neurological status, special GCS is used.
Geriatric Patient Considerations
The geriatric patient should be assessed and treated by ATLS protocol for adults. Because of multiple comorbidities in this age group, the patients may need special considerations such as medications which affect vital signs and basal laboratory results which affect the decision on imaging modalities (high kidney functions). However, life-threatening situations have priority, and immediate actions should be taken as with normal adults.
Pregnant Patient Considerations
Primary survey is the same for the pregnant patient as for other patients.
The normal heart rate of a pregnant patient is 10-15 beats faster than usual, and the blood pressure is 10-15 mmHg lower; so, normal vital signs can be mistaken for a shock. A blood loss of 30-35% can occur before there is a significant fall in blood pressure.
Disposition Decisions
Admission criteria.
The majority of patients will be admitted to the hospital following major trauma for the management of their injuries. Some of them need operation while other just need observation.
Admission criteria for ICU are cardiovascular resuscitation, airway protection and mechanical ventilation, invasive monitoring, severe head injury, organ support and correct coagulopathy.
Discharge criteria
The discharge decisions of trauma patients differ between institutions and systems. However, below list are cover the general agreement about the patients who can discharge after trauma.
- Minor blunt trauma, hemodynamically stable on serial assessments.
- Negative e-FAST and CT scans for free fluid in body cavities.
- Minimal head injury with GCS 15 and normal CT scans without other body injuries and with normal neurologic status (with instructions to return for any changes in mental status, vomiting, or worsening headaches).
- Uncomplicated rib or sternal fractures.
Multiple trauma patients who do not need admission for opetaion or observation are usually referred to a surgeon for the follow-up or management of their injuries.
References and Further Reading
- Driscoll AP, Skinner VD. Initial Assessment and Management: Primary Survey and Resuscitation. In: Driscoll AP, Skinner VD, editors. ABC of Major Trauma, fourth edition. Oxford: Blackwell Publishing Ltd; 2013: 1-7.
- Bhangu A, Lee C, Porter K. Principles of trauma management. In: Bhangu A, Lee C, Porter K, editors. Emergencies in Trauma. New York: Oxford University Press Inc; 2010: 3-11.
- Betz ME, Tibbles CD, Rosen CL. Initial approach to trauma. In: Legmone E, Shockley LW, editors. Trauma: a comprehensive emergency medicine approach. Cambridge: Cambridge University Press; 2011: 1-9.
- Ilgen JS. Trauma in Adults. In: Tintalli JE, editor. Tintinalli’s Emergency Medicine. New York: McGraw-Hill Companies, 2010: Chapter 156.
- Bailitz J, Bokhari F, Scaletta TA, Schaider J. STABILIZATION: Airways, Breathing and Circulations (ABCs). In: Bailitz J, Bokhari F, Scaletta TA, Schaider J., editors. Emergent Manegement of Trauma. New York: The McGraw-Hill Companies, Inc; 2011: 11-12.
- Gross EA, Martel ML. Multiple Trauma. In: Marx JA, Hockberger JS, Walls RM, et al. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Philadelphia: Saunders, an imprint of Elsevier Inc; 2010: 287-295.
- Nickson C. Intubation, Hypotension and Shock. Life in the Fastlane [serial on the Internet]. 2015 Nov. http://lifeinthefastlane.com/ccc/rapid-sequence-induction-of-the-shock-patient/ . Accessed April 27, 2016. – Link
- Lafferty KA. Medications used in Tracheal Intubation. Medscape. [serial on the Internet]. 2016 Feb. http://emedicine.medscape.com/article/109739-overview#a1 . Accessed April 27, 2016. – Link
- Kupnik D. Zdravila v nujni medicini. In: Grmec Š. Nujna stanja. Ljubljana: Macula Lunea, 2008: 447-470.
- J Trauma Acute Care Surg. Pediatric Trauma. In: J Trauma Acute Care Surg. ATLS-Advanced Trauma Life Support. Chicago: American College of Surgeons, 2008: 246-270.
- Fernandez J, Rifenbark M. Trauma Principles. In: Schindlbeck MA, Sherman SC, Weber JM, Patwari RG, Clinical Emergency Medicine. New York: McGraw-Hill Education; 2014: 358-362.
- Schindlbeck MA, Sherman SC, Weber JM, et al. Clinical Emergency Medicine. New York: McGraw-Hill Education; 2014.
Links To More Information
- Trauma! Initial Assessment and Management by Chris Nickson (2017) – Link
- Trauma! Major Haemorrhage, by Chris Nickson (2016) – Link
- Trauma! Are you prepared?, by Chris Nickson (2014) – Link
- Initial Trauma Assessment, by Chris Nickson (2016) – Link
- EM Fundementals – Trauma – Link
Sharing is caring
- Click to share on Twitter (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

- Browse Topics
- Earn CME Credits Stroke Cardiac Trauma Pediatric Trauma Urgent Care All CME Tests
- Pathways New!
- Resources For Emergency Physicians Urgent Care Clinicians Emergency PAs & NPs Residents Groups & Hospitals

Management of Multiply Injured Pediatric Trauma Patients in the Emergency Department
*new* quick search this issue.
When children with multiple serious injuries present to the ED, how do you ensure that you identify and address all of their injuries? This issue provides a systematic approach to the management of pediatric patients with multiple traumatic injuries, with specific attention to commonly missed injuries and injuries that may cause significant morbidity or mortality. You will learn:
Recommendations for initial field management and evaluation that will aid in early recognition and stabilization of injuries, critical elements of the primary survey that will help identify and address life-threatening injures, which diagnostic imaging modalities are warranted, and which is the best choice, based on presentation, evidence-based recommendations for a systematic approach to managing pediatric patients with multiple traumatic injuries, case presentations, introduction, critical appraisal of the literature.
- Common Mechanisms of Injury
- Difficulties in Assessing Pediatric Patients
- Commonly Missed Injuries
- Traumatic Brain Injuries
- Differential Diagnosis
- Initial Stabilization and Communication With Field Emergency Medical Technicians
- Cervical Spine Immobilization
- Splinting Orthopedic Injuries
- Airway Management
- Circulation
- Exposure and Environmental Control
- Focused Assessment With Sonography in Trauma (FAST) Examination
- Pediatric Airway Management
- Management of Closed Head Injuries
- Open Fractures
- Tetanus Vaccination
- Compartment Syndrome
- Fluid Resuscitation
- Radiographic Studies
- Computed Tomography
- Magnetic Resonance Imaging
- Laboratory Studies
- Pregnant Teenagers
- Severe Traumatic Brain Injury
- Transportation of Pediatric Trauma Patients
- Disposition
- Risk Management Pitfalls in the Management of Pediatric Patients With Multiple Injuries
- Case Conclusions
- Time and Cost-Effective Strategies
- Clinical Pathway for the Management of a Pediatric Patient With Multiple Traumatic Injuries
- Table 1. Differential Diagnosis for Pediatric Trauma Patients
- Table 2. Pediatric Glasgow Coma Scale Scoring
- Figure 1. Primary Survey Evaluation for Trauma Patients
- Figure 2. Differences in the Pediatric Airway Compared to the Adult Airway
- Figure 3. AVPU System for Infant Neurologic Assessment
Management of the child with multiple traumatic injuries can be challenging, and important injuries may not be readily recognized. Early recognition of serious injuries, initiation of appropriate diagnostic studies, and rapid stabilization of injuries are key to decreasing morbidity and mortality in the multiply injured pediatric trauma patient. The differential diagnosis for these patients is wide, and treatment is targeted to the specific injuries. In this issue, a systematic approach to the multiply injured pediatric patient will be reviewed, with specific attention to commonly missed injuries and those injuries that may cause significant morbidity or mortality.
A 12-year-old previously healthy boy presents to the ED via EMS for a visible deformity of his right arm. His 18-year-old brother was pulling him around in an inner tube that was attached by a long rope to a truck traveling about 40 miles per hour through a lightly wooded area. His brother made a sharp turn, and the patient went flying off the inner tube and hit a tree. The brother said that the patient did not lose consciousness, but that he was “stunned” for a few seconds, then started complaining about his right arm. The patient said he was not wearing any personal protective equipment. He has multiple abrasions to his face, trunk, and extremities. He denies pain anywhere except in his arm. He requests to have his neck brace removed because it is “annoying.” He denies vomiting but reports feeling nauseous after receiving morphine from the paramedics en route to the hospital. Because this was a severe mechanism, though the patient appears to have an isolated injury, you begin to consider how much you should do. Should you “pan-scan” the patient and draw labs because of the mechanism? What other imaging studies do you need to obtain besides an x-ray of the arm? Is the patient at risk for internal bleeding due to this blunt impact? Should you consult the surgeons or just call the orthopedist to reduce the obvious fracture?
A 16-month-old previously healthy girl presents to the ED via EMS after a seemingly accidental fall out of a third-story apartment window. Onlookers said the girl fell into a bush and appeared stunned but did not lose consciousness. The mother says when she got downstairs, the child was crying but easily consoled. The girl has multiple abrasions all over her body and a bloody nose, but otherwise seems fine. She cries throughout the primary and secondary surveys. Is the crying merely developmentally appropriate stranger anxiety? Does this patient need labs drawn? What type of imaging is warranted? If no other injuries are identified, what is the appropriate disposition for this patient?
Trauma is the leading cause of morbidity and mortality in children aged > 1 year. 1,2 When pediatric patients present with multiple traumatic injuries, life- or limb-threatening injuries in 2 or more organ systems are not uncommon; 1,3,4 traumatic brain injuries (TBIs) and orthopedic/musculoskeletal injuries are frequent. 5 Death occurs in up to 27% of pediatric patients with multiple traumatic injuries and is mainly dependent upon the severity of the TBI. 4
Typically, major issues with airway, breathing, and circulation are recognized and stabilized in a timely fashion. Problems occur when TBIs and orthopedic injuries are not identified early, as they can lead to long-term disabilities in pediatric patients. 2,6 In one study, 9% of injuries were initially missed in pediatric trauma patients, with 46% of those injuries being missed fractures. Earlier identification of these injuries can greatly decrease the rates of morbidity and mortality. Other organ systems in which certain missed injuries can lead to serious morbidity in multiple-trauma patients include the gastrointestinal and respiratory systems. 6 Less common pathologies, such as abdominal compartment syndrome, 3 if not recognized early, can lead to a decline in respiratory status and decreased cardiac output. Blunt chest trauma can cause morbidity primarily from lung contusions or hemothorax/pneumothorax or secondarily as a result of a systemic inflammatory response syndrome leading to acute lung injury.
This issue of Pediatric Emergency Medicine Practice will discuss evidence-based recommendations for early recognition of TBI during the primary survey, initiation of the proper imaging to diagnose injuries, expedient stabilization of injuries, and utilization of a systematic approach to manage pediatric patients with multiple trauma.
A literature search was performed in PubMed using the search terms: multiple trauma , pediatrics , emergency room , trauma , children , polytrauma , imaging , FAST , permissive hypotension , transfusion , airway , tranexamic acid , and ATLS . A total of 193 articles from 1997 to the present were reviewed. The Cochrane Database of Systematic Reviews and the National Guideline Clearinghouse were searched for systematic reviews using the key term multiple trauma pediatrics . Approximately 70 articles were found, most of them being from the view of surgical management. The ninth edition of the Advanced Trauma Life Support (ATLS) guidelines, 7 released by the American College of Surgeons Committee on Trauma, were also reviewed. While ATLS is not pediatric-specific, it is a system based on both best available evidence and expert consensus. These guidelines are widely considered the standard approach to all injured patients. Very few guidelines or policy statements were found specifically on pediatric trauma. The American Academy of Pediatrics (AAP) issued a policy statement in August 2016 that demonstrated the importance of a diverse trauma team when caring for pediatric trauma patients. 8
The search of the literature revealed few case reports on multiple trauma in pediatric patients; there were also few studies on the emergency medical management of these cases. There were more studies that focused on the surgical management of multiple trauma patients, including emergency surgical procedures and early involvement of surgical specialties in resuscitation. The studies were retrospective, with very few prospective or randomized double-blinded studies.
Tables and Figures

Evidence-based medicine requires a critical appraisal of the literature based upon study methodology and number of patients. Not all references are equally robust. The findings of a large, prospective, randomized, and blinded trial should carry more weight than a case report.
To help the reader judge the strength of each reference, pertinent information about the study is included in bold type following the reference, where available. In addition, the most informative references cited in this paper, as determined by the author, are highlighted .
- Schalamon J, Bismarck SV, Schober PH, et al. Multiple trauma in pediatric patients. Pediatr Surg Int. 2003;19(6):417-423. (Retrospective review; 70 patients)
- Kay RM, Skaggs DL. Pediatric polytrauma management. J Pediatr Orthop. 2006;26(2):268-277. (Review article)
- Letts M, Davidson D, Lapner P. Multiple trauma in children: predicting outcome and long-term results. Can J Surg. 2002;45(2):126-131. (Retrospective case series; 149 patients)
- Dereeper E, Ciardelli R, Vincent JL. Fatal outcome after polytrauma: multiple organ failure or cerebral damage? Resuscitation. 1998;36(1):15-18. (Retrospective review; 98 patients)
- van der Sluis CK, Kingma J, Eisma WH, et al. Pediatric polytrauma: short-term and long-term outcomes. J Trauma. 1997;43(3):501-506. (Retrospective study; 74 patients)
- Miele V, Di Giampietro I, Ianniello S, et al. Diagnostic imaging in pediatric polytrauma management. Radiol Med. 2015;120(1):33-49. (Review article)
- ATLS Subcommittee, American College of Surgeons' Committee on Trauma. Chapter 10: Pediatric Trauma. Advanced Trauma Life Support Student Course Manual. 9th ed: American College of Surgeons; 2013. (Textbook)
- Committee on Pediatric Emergency Medicine, Council on Injury Violence, and Poison Prevention, Section on Critical Care, Section on Orthopaedics, Section on Surgery, Section on Transport Medicine, et al. Management of pediatric trauma. Pediatrics. 2016;138(2). (AAP policy statement)
- Tracy ET, Englum BR, Barbas AS, et al. Pediatric injury patterns by year of age. J Pediatr Surg. 2013;48(6):1384-1388. (Review article)
- Lallier M, Bouchard S, St-Vil D, et al. Falls from heights among children: a retrospective review. J Pediatr Surg. 1999;34(7):1060-1063. (Retrospective review; 64 patients)
- Wang MY, Kim KA, Griffith PM, et al. Injuries from falls in the pediatric population: an analysis of 729 cases. J Pediatr Surg. 2001;36(10):1528-1534. (Retrospective review; 729 patients)
- Thompson EC, Perkowski P, Villarreal D, et al. Morbidity and mortality of children following motor vehicle crashes. Arch Surg. 2003;138(2):142-145. (Retrospective review; 191 patients)
- Wetzel RC, Burns RC. Multiple trauma in children: critical care overview. Crit Care Med. 2002;30(11 Suppl):S468-S477. (Review article)
- Furnival RA, Woodward GA, Schunk JE. Delayed diagnosis of injury in pediatric trauma. Pediatrics. 1996;98(1):56-62. (Retrospective review; 1175 patients)
- Gaines BA, Ford HR. Abdominal and pelvic trauma in children. Crit Care Med. 2002;30(11 Suppl):S416-S423. (Review article)
- Werner C, Engelhard K. Pathophysiology of traumatic brain injury. Br J Anaesth. 2007;99(1):4-9. (Review article)
- Sundstrom T, Asbjornsen H, Habiba S, et al. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31(6):531-540. (Review article)
- Hadley MN, Walters BC, Grabb PA, et al. Management of pediatric cervical spine and spinal cord injuries. Neurosurgery. 2002;50(3 Suppl):S85-S99. (Literature review)
- Pandya NK, Upasani VV, Kulkarni VA. The pediatric polytrauma patient: current concepts. J Am Acad Orthop Surg. 2013;21(3):170-179. (Review article)
- Nau C, Jakob H, Lehnert M, et al. Epidemiology and management of injuries to the spinal cord and column in pediatric multiple-trauma patients. Eur J Trauma Emerg Surg. 2010;36(4):339-345. (Retrospective analysis; 35 patients)
- Meier R, Krettek C, Grimme K, et al. The multiply injured child. Clin Orthop Relat Res. 2005(432):127-131. (Retrospective case study; 925 patients)
- Avarello JT, Cantor RM. Pediatric major trauma: an approach to evaluation and management. Emerg Med Clin North Am. 2007;25(3):803-836. (Review article)
- Reilly PL, Simpson DA, Sprod R, et al. Assessing the conscious level in infants and young children: a paediatric version of the Glasgow Coma Scale. Childs Nerv Syst . 1988;4(1):30-33. (Retrospective review)
- Holmes JF, Gladman A, Chang CH. Performance of abdominal ultrasonography in pediatric blunt trauma patients: a meta-analysis. J Pediatr Surg. 2007;42(9):1588-1594. (Meta-analysis; 25 studies, 3838 patients)
- Fox JC, Boysen M, Gharahbaghian L, et al. Test characteristics of focused assessment of sonography for trauma for clinically significant abdominal free fluid in pediatric blunt abdominal trauma. Acad Emerg Med. 2011;18(5):477-482. (Prospective study; 357 patients)
- Calder BW, Vogel AM, Zhang J, et al. Focused assessment with sonography for trauma in children after blunt abdominal trauma: a multi-institutional analysis. J Trauma Acute Care Surg. 2017;83(2):218-224. (Prospective study; 2188 patients)
- Holmes JF, Kelley KM, Wootton-Gorges SL, et al. Effect of abdominal ultrasound on clinical care, outcomes, and resource use among children with blunt torso trauma: a randomized clinical trial. JAMA . 2017;317(22):2290-2296. (Randomized controlled trial; 925 patients)
- Stafford PW, Blinman TA, Nance ML. Practical points in evaluation and resuscitation of the injured child. Surg Clin North Am. 2002;82(2):273-301. (Review article)
- Esposito TJ, Sanddal ND, Dean JM, et al. Analysis of preventable pediatric trauma deaths and inappropriate trauma care in Montana. J Trauma. 1999;47(2):243-251. (Retrospective chart review; 138 patients)
- Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59(3):165-175. (Review)
- Abdelgadir IS, Phillips RS, Singh D, et al. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev. 2017;5:CD011413. (Systematic review; 12 studies, 803 patients)
- Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. (Prospective cohort; 42,412 patients)
- Bae DS, Kadiyala RK, Waters PM. Acute compartment syndrome in children: contemporary diagnosis, treatment, and outcome. J Pediatr Orthop. 2001;21(5):680-688. (Retrospective chart review; 33 patients)
- Ziolkowski NI, Zive L, Ho ES, et al. Timing of presentation of pediatric compartment syndrome and its microsurgical implication: a retrospective review. Plast Reconstr Surg. 2017;139(3):663-670. (Retrospective review; 35 patients)
- Greene N, Bhananker S, Ramaiah R. Vascular access, fluid resuscitation, and blood transfusion in pediatric trauma. Int J Crit Illn Inj Sci. 2012;2(3):135-142. (Review article)
- Hughes NT, Burd RS, Teach SJ. Damage control resuscitation: permissive hypotension and massive transfusion protocols. Pediatr Emerg Care. 2014;30(9):651-656. (Review)
- Kannan N, Wang J, Mink RB, et al. Timely hemodynamic resuscitation and outcomes in severe pediatric traumatic brain injury: preliminary findings. Pediatr Emerg Care. 2018;34(5):325-329. (Retrospective review; 234 patients)
- Zebrack M, Dandoy C, Hansen K, et al. Early resuscitation of children with moderate-to-severe traumatic brain injury. Pediatrics. 2009;124(1):56-64. (Retrospective review; 299 patients)
- Hendrickson JE, Shaz BH, Pereira G, et al. Implementation of a pediatric trauma massive transfusion protocol: one institution’s experience. Transfusion . 2012;52(6):1228-1236. (Prospective cohort; 102 patients)
- Hwu RS, Spinella PC, Keller MS, et al. The effect of massive transfusion protocol implementation on pediatric trauma care. Transfusion. 2016;56(11):2712-2719. (Retrospective review; 11,995 patients)
- Whittaker B, Christiaans SC, Altice JL, et al. Early coagulopathy is an independent predictor of mortality in children after severe trauma. Shock. 2013;39(5):421-426. (Retrospective review; 803 patients)
- Smith SA, Livingston MH, Merritt NH. Early coagulopathy and metabolic acidosis predict transfusion of packed red blood cells in pediatric trauma patients. J Pediatr Surg. 2016;51(5):848-852. (Retrospective review; 96 patients)
- Rossaint R, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care . 2016;20:100. (Guidelines)
- Kozek-Langenecker SA, Afshari A, Albaladejo P, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol . 2013;30(6):270-382. (Guidelines)
- Eckert MJ, Wertin TM, Tyner SD, et al. Tranexamic acid administration to pediatric trauma patients in a combat setting: the pediatric trauma and tranexamic acid study (PED-TRAX). J Trauma Acute Care Surg. 2014;77(6):852-858. (Retrospective review; 766 patients)
- Baker N, Woolridge D. Emerging concepts in pediatric emergency radiology. Pediatr Clin North Am. 2013;60(5):1139-1151. (Review article)
- Jakob H, Lustenberger T, Schneidmuller D, et al. Pediatric polytrauma management. Eur J Trauma Emerg Surg. 2010;36(4):325-338. (Review article)
- Frank JB, Lim CK, Flynn JM, et al. The efficacy of magnetic resonance imaging in pediatric cervical spine clearance. Spine (Phila Pa 1976). 2002;27(11):1176-1179. (Retrospective chart review)
- Asimos A. The trauma panel: laboratory test utilization in the initial evaluation of trauma patients. Emergency Medicine Reports. February 1997. (Review)
- Capraro AJ, Mooney D, Waltzman ML. The use of routine laboratory studies as screening tools in pediatric abdominal trauma. Pediatr Emerg Care . 2006;22(7):480-484. (Retrospective medical record review; 382 patients)
- Keller MS, Coln CE, Trimble JA, et al. The utility of routine trauma laboratories in pediatric trauma resuscitations. Am J Surg . 2004;188(6):671-678. (Retrospective study; 240 children)
- Mathieson S, Whalen D, Dubrowski A. Infant trauma management in the emergency department: an emergency medicine simulation exercise. Cureus. 2015;7(9):e316. (Simulation exercise report)
- Morrissey K, Fairbrother, HE. Pediatric trauma: pearls and pitfalls. emDocs.net . Available at: http://www.emdocs.net/pediatric-trauma-pearls-pitfalls/. Accessed May 15, 2018. (Online resource)
- Murphy NJ, Quinlan JD. Trauma in pregnancy: assessment, management, and prevention. Am Fam Physician. 2014;90(10):717-722. (Review article)
- Nesiama JA, Pirallo RG, Lerner EB, et al. Does a prehospital Glasgow Coma Scale score predict pediatric outcomes? Pediatr Emerg Care. 2012;28(10):1027-1032. (Retrospective chart review; 185 patients)
- Kochanek PM, Carney N, Adelson PD, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents--second edition. Pediatr Crit Care Med. 2012;13 Suppl 1:S1-S82. (Guidelines)
- Andrews PJ, Sinclair HL, Rodriguez A, et al. Hypothermia for intracranial hypertension after traumatic brain injury. N Engl J Med. 2015;373(25):2403-2412. (Randomized controlled trial; 387 patients)
- Widdel L, Winston KR. Prognosis for children in cardiac arrest shortly after blunt cranial trauma. J Trauma. 2010;69(4):783-788. (Retrospective chart review; 40 patients)
- Missios S, Bekelis K. Transport mode to level I and II trauma centers and survival of pediatric patients with traumatic brain injury. J Neurotrauma. 2014;31(14):1321-1328. (Retrospective cohort; 15,704 patients)
- Macnab AJ, Wensley DF, Sun C. Cost-benefit of trained transport teams: estimates for head-injured children. Prehosp Emerg Care. 2001;5(1):1-5. (Retrospective chart review; 43 patients)
- Acierno SP, Jurkovich GJ, Nathens AB. Is pediatric trauma still a surgical disease? Patterns of emergent operative intervention in the injured child. J Trauma. 2004;56(5):960-964. (Retrospective study)
- Amini R, Lavoie A, Moore L, et al. Pediatric trauma mortality by type of designated hospital in a mature inclusive trauma system. J Emerg Trauma Shock. 2011;4(1):12-19. (Retrospective chart review; 11,503 patients)
Publication Information
Andria Tatem, MD; Rupa Kapoor, MD, FAAP

Peer Reviewed By
Michelle Hughes, DO, FAAP; Lara Zibners, MD, MMEd
Publication Date
June 2, 2018
Get Permission
Content You Might Be Interested In
Emergency Department Assessment and Management of Pediatric Acute Mild Traumatic Brain Injury and Concussion (Trauma CME)
Severe Traumatic Brain Injury in Children: An Evidence-Based Review of Emergency Department Management (Trauma CME and Pharmacology CME)
Content you might be interested in

Price: $497/year
140+ Credits!
Get A Sample Issue Of Emergency Medicine Practice
1-678-366-7933, [email protected].
Connect With Us
Who We Serve
Accredited By

Endorsed By

Our Partners
A case study of a multiply injured patient
Affiliation.
- 1 Department of Surgery, Division of Trauma and Surgical Critical Care, Medical College of Wisconsin, Milwaukee, WI 53226, USA.
- PMID: 23153888
- DOI: 10.1016/j.suc.2012.08.016
Initial evaluation of severely injured patients requires an organized, rapid, and thorough evaluation of the patient where life-threatening injuries are identified and treated simultaneously. A case study provides the basis for discussion of the management of the multiply injured trauma patient. The ultimate goal in rehabilitation of a multiply injured patient is to return each patient to as much independent function and ability to contribute to society as possible.
Copyright © 2012. Published by Elsevier Inc.
Publication types
- Accidents, Traffic
- Advanced Trauma Life Support Care*
- Chest Tubes
- Decision Making
- Head Injuries, Closed / diagnosis
- Head Injuries, Closed / therapy
- Multiple Trauma / complications
- Multiple Trauma / diagnosis*
- Multiple Trauma / rehabilitation
- Multiple Trauma / therapy*
- Peptic Ulcer / etiology
- Peptic Ulcer / prevention & control
- Respiration, Artificial
- Spleen / injuries
- Thoracic Injuries / diagnosis
- Thoracic Injuries / therapy
- Venous Thromboembolism / etiology
- Venous Thromboembolism / prevention & control
CASE STUDY: Repatriating a multiple trauma patient
Dr marjan basmenji shares marm assistance’s experience in case management and repatriation of a critical patient suffering from multiple trauma, from kayseri, turkey, to barcelona, spain..
The patient was a 72-year-old lady who sustained multiple trauma due to an accident while on a trip to Cappadocia, Central Turkey. She was found unconscious at the scene of the accident, and had difficulty in breathing, and stridor. She was haemodynamically unstable and immediately transferred to the closest well-equipped hospital. The patient was evaluated: she showed signs of shock, and was diagnosed with a left upper palpebral laceration; foreign bodies in her cornea; a comminuted fracture of the tympanic part of left temporal bone; tympanic membrane laceration in left ear; traumatic hemothorax in the right hemithorax; and lung contusion in the thorax.
Fracture lines were also detected at costas number 2, 3, 4, 5, 6, 7 and 8, bilaterally, while abdominal computed tomography (CT) scans revealed fluids in the abdominal fossa and findings suggestive of traumatic liver injury. Finally, the patient was diagnosed with displaced right femur shaft fracture; left humerus displaced diaphysis fracture; right clavicle fracture; and lumbar vertebrae transverse process fractures – bilateral at L1, L2, and L3, and unilateral at L4 and L5.
Ensuring the best medical provision
The patient was immediately taken to the operation room for a diagnostic laparoscopy. During the surgery, an aspiration of haemorrhagic fluids and repair of liver capsule laceration was carried out. The patient was transferred to an intensive care unit (ICU) postoperation, intubated, and ventilated with a high dose inotropic infusion. One day after admission, due to the patient’s severe condition, marm assistance medical team decided to transfer the patient to a better equipped hospital in Kayseri – 80 kilometres away. Upon approval by the insurance company and family, a medical doctor from marm assistance visited the patient and other victims of the tragic accident, supervised the transfer process, and evaluated clinical condition of all patients with treating teams in hospital.
Elective surgical operations for treatment of femur, humerus and tympanic segment of temporal bone fractures were carried out in the second hospital. A litre of haemorrhagic fluid was evacuated from the right hemithorax, via chest tube thoracostomy. The patient was followed in ICU and ventilated for one week, prior to weaning and non-invasive ventilation trial. Her general condition improved, while treatment for pan-resistant klebsiella growth on patient’s tracheal aspirations continued.
A sudden deterioration
Unfortunately, news that the patient’s condition had suddenly deteriorated complicated the situation, leading to re-intubation. A CT scan on the 13th day since admission revealed massive bilateral emboli, despite the fact the patient was receiving anti-thrombosis prophylaxis. Anti-thrombotic treatment was initiated. The patient was extubated after two days, and had spontaneous respiration – however, inotropic infusion and high flow nasal oxygen at 10 litre/minute continued.
Four days after pulmonary emboli diagnosis – on the 17th day of admission – the patient was discharged from İCU and was transferred to internal disease service, with spontaneous respiration and 6 litre/minute high flow oxygen support, with a saturation percentage of 97 per cent. During close follow-ups assessments, the marm assistance medical team evaluated the best time and means of repatriating the patient to her home country of Spain. Arrangements for readmission were carried out by the insurance company.
Careful consideration required
Considerations for the patient’s repatriation were both medical and logistical. Logistically, a direct transfer from Kayseri to Barcelona was only possible via air ambulance. Medically, the patient was stable, and her general condition was improving day by day – due to the complications of the massive bilateral pulmonary emboli, it was foreseen she may need a minimum 8 litre/minute of high-flow oxygen during the flight. Supplying this amount of oxygen on a plane, for the duration of a four-hour flight to Barcelona, could be problematic. The patient’s pain and delicate condition also favoured an air ambulance repatriation.
Considering the various factors, an air ambulance transfer from Kayseri to Barcelona was arranged, and the patient was successfully transported home on 23rd day of her admission, escorted by marm medical escorts.
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Introduction
Mike, a 35 year-old male, is presented to the emergency department with multiple puncture wounds to the right arm and bruising on the face. He arrived at the hospital via emergency medical services after calling 911.
Mike was playing with his dog, a German Shepherd, in front of his hoe one day when all of the sudden, his dog decides to bit his right arm and punch him in the face. He immediately takes off his jacket and notices blood all over his arm and calls 911. calling 911, Mike states that he has been bitten on his arm and punched in the face by his dog. The operator tells Mike that EMS will be there in 10 minutes and to clean the wounds with soap and water and to cover the wounds if possible.
On route to the hospital, EMS performs a primary assessment using the ABCDE approach.
- A irway: Patent
- B reathing: tachypneic with labored breath and breath sounds normal
- C irculation: pulses rapid and weak
- D isability (LOC): awake, alert, responds to pain and voice. GCS: 15
- E xposure: Site of wound exposed. Wounds on right arm and bruising on face noted
C-Spine Stabilization is not indicated.
Upon admission to the ED, the secondary assessment was performed. The patient’s vital signs were a BP: 92/54, HR: 120, RR: 22, T 100.7F, O2: 96% on room air, and a pain of 9/10. Performing a full head-to-toe assessment revealed:
- Neurological: Awake, alert and oriented x 4, GCS 15, full PERRLA
- Cardiovascular: Normal s1s2, pulses rapid and weak, cap refill <2 secs
- Respiratory: Tachypneic, labored breathing, normal breath sounds
- GI: Nondistended, soft, non-tender, bowel sounds active
- GU: No complaints of urinary problems
- Integumentary: Multiple right arm puncture wounds. Bruising on face. Site of wound warm and swollen. Skin is cool and pale.
- Musculoskeletal: weakness and pain in right arm
- Psychological: Possible PTSD
The patient’s medical history was gathered using the mnemonic device, AMPLE:
- A llergies: Latex
- M edications: Atorvastatin, metoprolol
- P ast medical history: Splenectomy 19 years ago
- L ast oral intake: a glass of water
- E vent leading to injury: playing with dog. Dog overexcited
Question 1: After reviewing the findings in the secondary assessment, what are some notable concerns to address in the assessment?
Question 2: Based on the secondary assessment, what interventions should the nurse expect to be ordered?
Question 3: After performing these interventions, should the patient be admitted into the hospital or discharged and given a follow up visit? Why?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Trauma Case 1: Stab to Left Chest
Boston medical center – trauma case of the month, case #1: diagnostic laparoscopy in penetrating chest trauma.
by Rie Aihara, M.D. and Wayne LaMorte, M.D., Ph.D., M.P.H.
Pre-Hospital Data
A 17 year-old male from Michigan was visiting his cousins and friends in Boston, when he became a victim of a stabbing. This all began when the victim confronted an old friend about a personal conflict which occurred between them years ago. What started out as a verbal argument eventually resulted in physical violence. The victim sustained a single stab wound to the left chest in the mid axillary line, just below the level of the nipple. He was transported to our emergency department by Boston EMS. He was noted to be awake and alert throughout the entire transport.
Past Medical/Surgical History: Asthma Family History: Non-significant Medications: Inhalers as needed Allergy: No Known Drug Allergy (NKDA)
Trauma Room Assessment:
The patient was moved from the stretcher onto the examination table, and the only complaint obtained from the patient was shortness of breath.
Cardiac monitors, blood pressure-cuff and oxygen saturation probes were then placed on the patient.
Vital signs:
Heart rate- 90/min Blood Pressure- 130/70 Respiratory rate 25 Temperature- 97 F
Primary Survey:
Airway- patent airway as demonstrated by his ability to talk. Breathing- decreased breath sounds at the left base.
- Oxygen mask with 100% FiO2 was placed; & an oxygen saturation of 100% was obtained
Circulation – no active external bleeding Deficits – neurological exam grossly intact Exposure – the patient’s clothes were removed to throughly examine for other injuries Secondary survey: HEENT: no lacerations, no hematomas, no fractures palpated Neck: midline trachea, no JVD, no crepitus Chest: clear on right, single stab wound to the left chest in the mid-axillary line in the 4 th intercostal space, no crepitus, no bleeding, decreased breath sounds at the left base Cardiac: regular rate and rhythm (RRR), normal S1 and S2 Abdomen: present bowel sounds, soft, non-tender, non-distended Extremities: warm, present distal pulses Neuro: awake, GCS 15, no focal deficits
Radiological Survey:
Chest X-ray: left sided hemopneumothorax
- An upright CXR was obtained. We were able to sit the patient up because he had an isolated penetrating injury to the chest, and the mechanism of injury did not warrant spinal precautions. A pelvis and lateral C-spine films were also not obtained because of the isolated nature of the injury.
Other Pertinent Studies:
Transthoracic Echocardiogram: no pericardial effusion
- Because the weapon can be aimed at any direction (medially, superiorly, inferiorly), the heart can be potentially injured. A pericardial tamponade is lethal unless discovered and treated quickly.
Blood Work Ordered:
- Type and screen
- Coagulation panel
- Complete blood count (CBC)
- Arterial blood gas
- Toxicology screen
ER Procedures:
Chest tube placement: drained 300cc of frank blood
Change in status:
The patient at this time began complaining of a new subscapular pain, or pain between the shoulder blades. This was alarming to the trauma team for the following reasons.
- Patients with diaphragmatic injuries and irritation from the blood frequently exhibit referred pain in this distribution. If the knife wound had projected inferiorly penetrating the diaphragm, there was also a high likelihood of intraabdominal injuries. Therefore, it was decided that the patient required surgical exploration, and the patient was taken to the operating room.
Operating Room:
The surgical team performed a diagnostic laparoscopy in order to determine whether or not the diaphragm had been penetrated. The laparoscopy demonstrated an obvious defect in the diaphragm, as shown here.

Inspection within the abdomen demonstrated blood clots on the anterior surface of the stomach and the left lateral segment of the liver. In order to more carefully assess the extent of intra-abdominal injuries and carry out repair, the procedure was converted to an open laparotomy.
Upon exploration, there were three lacerations on the surface of the liver which required suture closure. There was also a 2 cm perforation of the anterior surface of the stomach which was closed primarily in two layers.
In order to assess the extent of intrathoracic injuries more closely, the laparoscope was advanced from the abdomen into the thorax through the diaphragmatic defect.
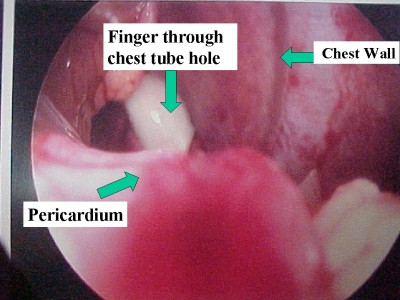
Examination of the pericardium showed no evidence of bleeding, contusion, or penetration.
We therefore proceeded to close the diaphragmatic perforation with interrupted Ethibond suture with pledgets.

Upon completion of the procedure the patient recovered without complications and was discharged to home in four days.
Major Teaching Points:
- Arterial blood gas is a better indicator of hemorrhage than hematocrit for the reasons described above.
- The peritoneal cavity can extend into the thoracic cavity as high as the 4th intercostal space. Any penetrating chest injury at or below that level has the potential to injure intra-abdominal organs.
- The presence of subscapular pain in a patient with a penetrating injury to the chest strongly suggests penetration of the diaphragm and a high risk of associated intra-abdominal injuries. This situation warrants surgical evaluation of the abdomen in the operating room.
Surgical exploration can be undertaken in one of two ways: a) the conventional approach is to perform an open laparotomy, and b) the alternate approach is to do a diagnostic laparoscopy. The primary purpose of the laparoscopy is to determine the presence of diaphragmatic perforation. If the diaphragm is intact, then there should be no intra-abdominal injuries. In this case, a midline incision can be avoided, and the recovery period will be shortened significantly. This can be beneficial to high risk patients such as those with pulmonary disease, cardiac disease and morbid obesity where a long midline incision can be a source of morbidity such as infection and respiratory compromise
Share this:
- Publisher Home

- About the Journal
- Editorial Team
- Article Processing Fee
- Privacy Statement
- Crossmark Policy
- Copyright Statement
- GDPR Policy
- Open Access Policy
- Publication Ethics Statement
- Author Guidelines
- Announcements
Reeducation of the Upper Limb: A Case Study of a Multiple Trauma Patient, Who Suffered a Car Accident
- Inês Rodrigues de Oliveira
Inês Rodrigues de Oliveira
Search for the other articles from the author in:
- Joana Filipa Ganhão Palma
Joana Filipa Ganhão Palma
Abstract Views 284
Downloads 73
##plugins.themes.bootstrap3.article.sidebar##
##plugins.themes.bootstrap3.article.main##
The hand and the forearm are the main defensive organs and more than often they suffer serious traumatism in car accidents. Guiding these patients to rehabilitation areas is essential for the success of the process.
The present case refers to a multiple trauma patient who suffered a car accident which had great impact on his upper left limb. The patient was treated at Hospital de São José, and later transferred for the Centro de Medicina e Reabilitação do Sul to start his rehabilitation. The complete description of the process in Occupational Therapy/Hand Therapy starts here, with the intention of evaluating the impact of this type of intervention on a multiple trauma patient, by assessing the evolution of the open wound, scar, edema, sensitiveness, joint range, muscular activation, limb functionality as well as Instrumental and Daily Life Activities.
Despite improvements at motor and sensory levels, these were not as expected, as a result of the severity of the injuries and the late rehabilitation beginning. Nonetheless, at the functionality level the patient was able to achieve improvement levels that allowed a greater independence and a return to his job. A timely reference for treatment, in this case of multiple trauma in the upper limb, could have allowed for a greater success in the rehabilitation, at the same time, a more effective communication among all the structures involved in the case since the moment of the accident until rehabilitation would also have led to a faster closing of the wound, which would have a positive influence in the results. Although, and even with the late start, the Hand Therapy intervention was paramount for the patient’s independence.


Management of the Geriatric Trauma Patient
Authors: Jonathan Henricks, MD, Hussam Salhi, MD PhD, and Lauren T. Southerland, MD
Edited By: Angel Li MD; Shan Liu, SD
Updated: 9/24/2021
Abbreviations Table:
TLS: Advanced Trauma Life Support GCS: Glasgow Coma Score MVC: Motor vehicle collision EMS: Emergency medical services HR: Heart Rate CAD: Coronary artery disease COPD: Chronic obstructive pulmonary disease IVC: Inferior Vena Cava FAST: Focused Assessment of Sonography in Trauma
Case Study: A 77 year-old female is brought to the emergency department by EMS for evaluation after a single-car MVC which occurred just prior to arrival. The patient was driving down a back road when she “couldn’t lift the foot off of the gas” and accelerated into a tree with airbag deployment. She is alert and talking to you, currently reporting a headache, neck pain, and left hip pain. Per EMS, vitals are notable for an irregularly irregular heart rate but otherwise “within normal limits.” Per EMS, the patient stated that she takes Coumadin, Metoprolol, Lisinopril, and Hydrochlorothiazide. She is unsure of the year or her current location. The patient’s daughter is en-route to the ED at this time.
By the end of this module, the student will be able to:
- Describe a focused rapid assessment of the geriatric trauma patient using an organized primary and secondary survey.
- Discuss the criteria for trauma activation.
- Discuss concerns for geriatric pathology that can occur in each domain of the primary survey and recommend treatment/stabilization measures.
- Describe geriatric considerations for the secondary survey.
- Describe how to stabilize a trauma patient and prioritize resuscitative measures.
Introduction
Trauma in the older patient, otherwise known as geriatric trauma, is important to delineate because despite a lower rate of unintentional injuries, these patients have significantly higher mortality and poorer functional outcomes when compared with their younger counterparts (2). Like all trauma patients, the basic ATLS (Advanced Trauma Life Support) algorithm serves as the framework patient evaluation, treatment, and disposition, however geriatric patients are often more complicated than younger adults, presenting a unique set of challenges to the emergency physician.
Currently, there is no standard definition of the term “geriatric trauma,” however in this discussion, we are referring to patients ages 65 and older. The US Census Bureau projects that the population of Americans greater than or equal to 65 years old will increase from 15% in 2016 to 21% in 2030, due to the aging of the “Baby Boomer” generation (1).. Currently, unintentional injury (trauma) is the seventh leading cause of morbidity and mortality in the geriatric population, and, amongst these, falls are the leading cause (2, 3). Geriatric patients represent roughly 30.75% of all trauma patients in the US (4) and these patients have worse clinical outcomes when compared with younger patients (5). The case fatality rate of those aged 75 to 84 (6.66%) is roughly double that of younger adults between the ages of 35 and 44, and even in cases where immediate mortality does not occur, geriatric patients who experience traumatic injuries have increased mortality within the next 12 months (6).
Initial Actions and Primary Survey
Trauma Activation
While in some cases, the decision to “activate a trauma” is relatively straightforward (eg. A multi-vehicle MVC with loss of consciousness, a fall from significant height, and a GSW to the abdomen), trauma in the geriatric patient may not be quite as obvious. As mentioned earlier, falls, even from standing height, are a leading cause of morbidity and mortality in the geriatric population, highlighting the dramatic physical and physiologic differences that a few decades can make to trauma patients. Multiple studies have demonstrated both the tendency to under-triage geriatric trauma patients to facilities with insufficient trauma capabilities, requiring early transfer to better-equipped facilities (7-9) A study of 2009-2014 Medicare claims data found that nearly half of older adults with a final injury severity score of 16 or higher (moderately-to-severely injured patients) were under-triaged to a non-trauma center (10). This delays necessary care and may be unsafe for patients, prompting the state of Ohio to derive a set of geriatric-specific prehospital triage criteria that has increased the sensitivity for severe injury in geriatric patients by 32%. These criteria can be found below. Always ask about your hospital’s trauma triage criteria and whether it includes additional parameters for older adults. (11)
Figure 1: Ohio Trauma Triage Criteria for older adults
Modifications to the Trauma Assessment of Older Adults
In general, older adults in good states of health have sufficient reserves to accomplish normal activities of daily living. When stressed by acute trauma or illness, however, their decreased physiologic reserves can result in a rapid progression of tissue hypoperfusion and organ failure, a common cause of death in older patients. Beware of this combination of decreased physiologic reserve and impaired resistance to stressors, also known as “frailty.” Frailty indices may be more predictive of death from trauma than initial injuries or vital signs in this population (12).
Primary Survey
The initial systemic trauma assessment (ABCDE’s) and secondary surveys should be conducted according to traditional ATLS principles as discussed in Chapter “Approach to Trauma.” However, there are special considerations in the approach in geriatric trauma, owing to changes in physiology with aging as well as increased rates of medical comorbidities and medication interactions. Additionally, while rapid assessment and effective resuscitation is generally the goal in managing the acutely ill, it is important to be aware of your patient’s advanced directives or other care-planning documents, as certain treatments may go against their medical wishes, which should be respected. The following are special considerations in each step of the trauma primary survey.
Conduct a systemic airway assessment, focusing on the ability to mask-ventilate, intubate via endotracheal tube, and possible surgical airway (cricothyroidotomy). Older patients have a higher rate of edentulousness than younger patients. Bagging them with the dentures in facilitates ventilation but remember to remove all dentures prior to intubation to improve first pass success. Additionally, due to underlying arthritic and degenerative changes, or prior surgical fixation, these patients often have reduced cervical mobility and a stiffer TMJ, complicating airway assessment and laryngoscopy. One should not use excessive force when adjusting the patient’s head, as this may worsen, or cause, cervical spine injury. Cervical kyphosis, preexisting neck malignancies or prior surgeries/radiation may distort the normal cervical anatomy, which may make obtaining a surgical airway more challenging. Lastly, post-intubation hypotension is more likely in older adults. Consider volume resuscitation prior to or concurrent with securing an airway.
Older patients have many physiologic changes to their pulmonary system including reduced chest wall compliance (due to degenerative disk disease, intercostal narrowing and kyphosis), weakened diaphragm/accessory muscles, loss of lung elastic recoil with increased residual volume, and decreased cough reflex/mucociliary function. In non-intubated patients, it is important to follow respiratory rate closely, as these patients are more likely to tire and decompensate as a result of pulmonary injury (eg. contusion) or aggressive fluid resuscitation. Just the act of immobilizing an older patient flat on the gurney can impair respiration. Consider ramping or elevating the head of the bed (if safe) to limit dependent atelectasis and maximize available lung tissue. Ask if the patient needs multiple pillows to breath easily at night, because this suggests that leaving them flat on the gurney for an hour could result in significant discomfort and difficulty oxygenating.
If an older adult has difficulty breathing due to injuries, use of non-invasive mechanical ventilation (CPAP/BiPAP, HFNC) may improve respiratory parameters and temporize the patient to enable goals of care discussions with patients/surrogates. A trial of positive airway pressure is recommended by the EAST trauma guidelines for pulmonary contusions or flail chest (13) End-tidal capnography is highly recommended for older adults if there is concern for underlying lung disease (COPD, pulmonary fibrosis, or pulmonary hypertension), thoracic injury (rib fractures or pulmonary contusions), or if analgesia and sedatives are provided.
Circulation
The cardiovascular system is significantly affected by aging. Over time, there are physiologic and pathologic changes to the heart including gradual stiffening of the ventricles with diastolic dysfunction, cardiac damage from coronary artery disease (CAD)/myocardial infarction, cardiomyopathy, heart failure, and valvular disease (14, 15). Decreased cardiac receptor responsiveness to circulating catecholamines limits the augmentation of stroke volume in response to increased demand (15). As a result, increasing heart rate may be a primary mechanism of increasing cardiac output to compensate for blood loss. Unfortunately, this too may be impaired due to existing conduction system abnormalities, loss of pacemaker cells with aging, and commonly used negative chronotropic agents (beta-blockers, calcium channel blockers). Ultimately, these changes culminate with a “pseudo-normal” physical exam and vital signs that do not reliably reflect the severity of systemic illness that face our geriatric trauma patients. Because “normal” vital signs are not definitively reassuring in the geriatric population, adjusted parameters for heart rate and blood pressure (HR >90, SBP <110 mmHg) have been posited to avoid relative hypotension and “occult” hypoperfusion, a finding associated with double the odds of death (16). In addition to trending vital signs and reviewing past medical records for baseline levels, trending lactates to assess adequacy of perfusion and resuscitative efforts can serve as a useful adjunct in the medical management of these patients (17). For a summary of vital sign pearls and pitfalls in the elderly, please see Table 1:
Adapted from Clare D, Zink, K, Geriatric Trauma. Special considerations impacting vital signs in the elderly trauma patient (18).
Table 1: A summary of vital signs in older adults that are concerning for significant injury in geriatric trauma patients and warrant intervention.
Regarding steps in resuscitation, identify and treat all life-threatening bleeding first, per ATLS guidelines. The FAST ultrasound exam can serve as a valuable adjunct in rapid assessment for shock from blood loss, and the subxiphoid view of the heart can give a quick gross assessment of contractility. Volume resuscitation cannot fully compensate for poor cardiac output, whether from baseline illness or injury, so any older adult trauma patient who is hypotensive should have a quick ultrasound assessment of contractility. Resuscitate with isotonic crystalloid or blood as needed. If no clear source of hemorrhage is identified, fluid resuscitation with 500cc aliquots of warmed isotonic crystalloid is recommended, with frequent reassessment to avoid pulmonary edema and fluid overload (19). Point-of-care ultrasound to assess IVC collapsibility or pulmonary B-lines may be useful in guiding fluid resuscitation and assessing fluid status, in conjunction with other physical exam findings. If significant bleeding, hemodynamic instability, or significant injury (eg. unstable pelvis), transfusion with blood products is indicated.
Finally, the number of older adults who are medicated with warfarin or other oral anticoagulants is increasing (20). These medications increase the likelihood of morbidity and mortality when compared to younger patients with similar initial injury severity scores. Be aware of your institution’s anticoagulation reversal policies. Vitamin K with 3- or 4 Factor Prothrombin Complex Concentrates for Warfarin, Protamine Sulfate for Lovenox, and the novel reversal agents Praxbind and Andaxanet Alfa for Dabigatran and Factor-Xa inhibitors may be life-saving. Fresh Frozen Plasma is an alternative to 3-4 factor PCCs, but requires longer infusion times and significant infusion volumes, which may not be tolerated in older adults with congestive heart failure, renal disease, or liver disease.
A Glasgow Coma Scale is documented as a part of ATLS protocol. However, GCS is not as good a predictor for severity of injury in older adults as in younger adults, as a good GCS (14-15) does not correlate with severity of injury on CT for older adults (21). In addition, baseline neurological function can be complicated by comorbid conditions such as underlying dementia or acute delirium from the injury. As such, all depressed neurological function, including amnesia to the event or confusion should be evaluated as a potentially traumatic brain injury. After immediate stabilization/evaluation, we recommend a delirium screening tool such as the CAM-ICU to test for altered mentation even in a patient with a GCS of 15.
Exposure is a key step in the primary survey to assess for other injuries. Remember to do a full skin exam as bruising and lacerations can be easily missed, as can pressure ulcers from prolonged backboard/Cervical collar use. Also, the skin exam can give insight into the cause of a fall or inform concern about elder abuse/neglect as causes of injury (see Chapter “Elder Abuse”). After exposure exam, keep the patient warm. Many older adults experience an age-related decline in thermoregulatory capacity and muscle mass. Oral and axillary temperatures can be less reliable (artificially low) in older adults, especially if the person is mouth breathing due to altered mental status, pulmonary disease, or acute injury. If you have an older adult who is confused or has a low GCS, check a rectal temperature.
Table 2: Summary of key points in the initial trauma assessment for older adults
CASE PART 2: Secondary Survey
On primary survey, the patient’s airway, breathing, and circulation appear intact. She is confused but opens eyes and moves all extremities spontaneously. She has no open wounds but does have a moderate hematoma to her left forehead and some contusions to her left knee. She has no evidence of basilar skull fracture but does have cervical spinal tenderness on evaluation. She has pain with passive range of motion of the left hip. Her right lower extremity is noticeably weak on examination.
Geriatric Considerations in the Secondary Evaluation
The stable geriatric trauma patient requires a thorough secondary assessment for both causes of the injury and concomitant medical conditions that may contribute to their current presentation. A special consideration in the older adult is to corroborate the patient’s baseline functional status and living arrangements which may help in final disposition planning for these patients. It is essential to screen all older trauma patients for substance and elder abuse, which are rare but can’t-miss diagnoses in this population (22).
Suggested labs include complete blood count, comprehensive metabolic panel, coagulation studies, lactic acid, urinalysis, cardiac enzymes, and a serum or urine toxicology screen. Obtain an electrocardiogram and place the patient on cardiac monitoring to evaluate for cardiac causes/complications of trauma. Imaging should include plain radiographs of the chest and pelvis at minimum, with computerized tomography being the imaging modality of choice in the stable geriatric trauma patient. The FAST exam has not been studied extensively in this population, but should be included as part of the initial evaluation and repeated as part of ongoing hemodynamic monitoring.
Presentation, Diagnostics, and Management based on System
Closed Head Injury
Traumatic brain injury in the elderly has significantly more morbidity and mortality than in younger patients. Due to underlying comorbidities and polypharmacy, traumatic events including falls are more likely to occur, and the prevalence of anticoagulant/antiplatelet agent use increase the risk of severe intracerebral hemorrhage. Several anatomic changes in the elderly are responsible for an increased risk of subdural hematoma and intraparenchymal hemorrhage vs younger adults. Increased adherence of the dura to the skull along with cerebral atrophy decreases the tortuosity of bridging veins across the subdural space, increasing the risk of tearing when exposed to shearing forces in trauma. Increased subdural space due to cerebral atrophy leads to delayed onset of symptoms, which may lead to delayed presentations to the emergency department, up to 17-74 days in one case series (23). This delay in presentation contributes to the higher morbidity and mortality in the elderly. For more information about the various presentations and management of closed head injury, please refer to the chapter, “Closed Head Injury.”

Figure 1: 74 year old patient fall from standing without neurological deficits found to have minor subdural hemorrhage on initial evaluation. If not evaluated, geriatric patients are at risk for delayed presentation for chronic subdural hematoma.
The diagnostic approach to the closed head injury in geriatric trauma differs from the average standard. Because clinical variables are not sensitive enough to rule out injury and clinical decision rules (such as Nexus and Canadian Head CT rules) are not validated or applicable in the geriatric population, the threshold for obtaining CT head imaging is much lower regardless of neurological presentation. Any older adult with physical signs of head trauma or altered mentation should receive brain imaging to evaluation for intracranial bleeding. The treatment of traumatic brain injury involves rapid anticoagulation reversal, evaluation for need for surgical decompression, and early neurosurgical consultation. Supportive care with glucose control, avoiding hypoxia with supplemental oxygen, head of bed elevation, and BP monitoring/control are also critical initial actions. Patients with moderate to severe TBI will require ICU level disposition with frequent neuro-checks and neurosurgical consultation. Those with normal mental status, no neuro deficits, and a small bleed may be amenable to observation or short stay units for 12-24 hours of neuro monitoring. It is recommended that any geriatric patient with confusion or neurological deficits at minimum has 24 hours of observation with continued evaluation for concussion or evolving intracranial pathology.
Vertebral/Spinal Cord Injury
Osteopenia and age-related changes to disks and the spinal canal place elderly at greater risk of vertebral fractures and spinal cord injury (SCI). A fourth of geriatric patients have cervical stenosis, and 90% of patients older than 60 years have degenerative changes in the C-spine (19). This increases leverage on the spinal column when force is applied, causing increased fracture risk. Three injuries constitute the majority of spinal injuries in the elderly population: central cord syndrome, cervical distraction injuries, and odontoid injuries.
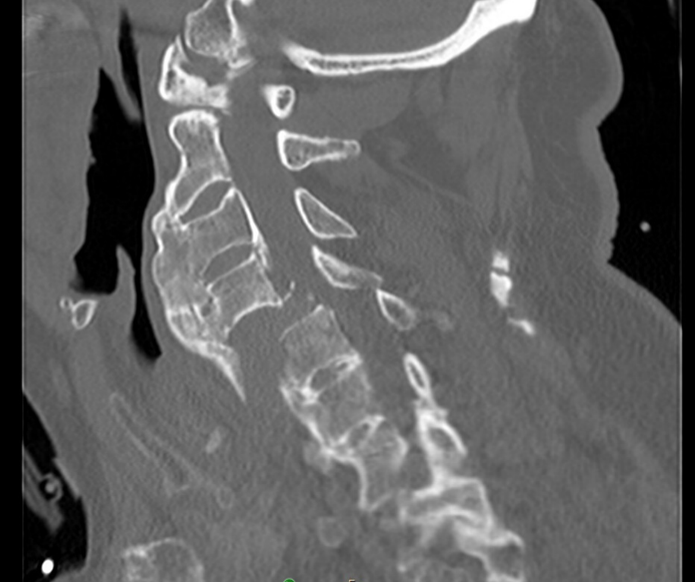
Figure 2: 85 year old male with bilateral jumped facet dislocation, a cervical distraction injury with high morbidity occurred as fall backwards off tipped stool with impact onto neck in flexed position.
As with closed head injury, spinal injuries in geriatric trauma are more difficult rule in or out with physical exam and risk stratification tools (24). Up to 20% of older adults with cervical spine fractures do not report neck pain (25). The location of pain on exam also often does not correlate to the level of injury, and often times a fracture in one section of spine is accompanied by a fracture in another. In fact, up to 26% of geriatric patients with a cervical fracture have been found to have a concomitant thoracolumbar fracture. Therefore, identification of a vertebral fracture in older adults should prompt whole spine imaging. Given the variability in clinical presentation and decreased sensitivity of decision tools for spine imaging in geriatric trauma, liberal CT imaging of the spine is recommended for older adults with spine trauma. In cases of suspected fracture or spinal cord injury, immobilization, spinal surgery consultation, and admission are indicated. Be cautious when empirically placing a cervical collar on an older adult, as they are at higher risk of complications including difficulty breathing, pressure ulcers from poorly fitting collars, and delirium.
Thoracic Trauma
Please refer to Chapter “Chest Trauma” for review of mechanisms of injury, initial management and various presentations of traumatic thoracic injuries. Due to increased rates of osteoporosis and osteopenia, rib and sternal fractures are more common in geriatric patients that suffer chest trauma and can be occult on chest xray. Pulmonary contusions are also very common with minimal trauma, even in the absence of rib fractures. The pain associated with this leads to splinting and atelectasis, which decreases pulmonary clearance and increases the risk of post-traumatic pneumonia, a more common complication in the geriatric population (26).
Chest xray and extended FAST examination, even when combined, have proven inadequate to diagnose thoracic injury in blunt thoracic trauma (27). Thus, CT chest is recommended for all older patients with chest trauma or respiratory complications following a traumatic mechanism. Continuous evaluation and airway monitoring, and early intubation xin anticipation of declining clinical course can be considered. Early pain control with opioid or paravertebral analgesic (rib block) can be instrumental in preventing post-traumatic pneumonia. Chest wall compliance, respiratory muscle atrophy, and capacity for oxygen are decreased with age and cause reductions in VC, FRC, and FEV, limiting the elderly patient’s response to hypoxia and compensation during chest injury. As a result, the threshold for ICU monitoring in elderly patients is lower upon admission with thoracic injuries, especially in the case of multiple rib fractures, pulmonary contusions, and flail chest. In one case series of 401 older adults with rib fractures cared for at University of California-Davis, 63% were admitted to an ICU and a third of those required a critical care intervention or had an adverse event.
Abdominal Trauma
Refer to Chapter “Abdominal Trauma” for review of differential diagnoses, approach, and management of general blunt and penetrating abdominal injuries. Although physical examination helps guide imaging evaluation on secondary survey, the abdominal examination in a significant proportion of geriatric patients can be unreliable. Peritoneal signs may be absent, and reliance on physical examination may lead to missed injuries. There should be a high suspicion for intrabdominal solid organ injury in patients with lower rib fractures or pelvic fractures. As such, CT with contrast is an ideal imaging modality in hemodynamically stable patients to assess the extent of injury. Carefully-selected older adults are candidates for non-operative management (eg. low grade splenic injury) (22). The FAST exam should be part of the initial exam, and can detect large volumes of intraperitoneal fluid and be repeated as a part of hemodynamic monitoring. However, the FAST exam can be “fooled” if the patient has chronic ascites from CHF, liver failure, or ESRD. In these cases, CT with IV contrast can determine if there is active bleeding vs chronic ascites fluid.
Digital rectal exam to assess for intestinal injury, a high-riding prostate (urethral trauma) or spinal cord injury was a part of ATLS secondary exam for many years and is still mentioned in many textbooks. However, this exam has low sensitivity and can also return a false positive in older adults, who have higher likelihood of non traumatic causes of bleeding such as hemorrhoids, diverticulosis, and colonic polyps (28). Rectal tone also is decreased with age and digital rectal exam has a high false negative rate. Unless there is concern for rectal or urethral trauma externally, this exam is unnecessary.
Extremity Injury
Because the geriatric population has a higher rate of decreased bone mineral density and malnutrition with age, they are more prone to extremity injury with lower intensity mechanisms of trauma. The morbidity associated with this can be grave. Isolated traumatic hip fractures in the geriatric population have been found to lead to a 8-30% 1-year mortality (29). Early surgical management of extremity fractures is associated with better outcomes (30). Thus, transfer of hemodynamically stable patients to a center for orthopedic consultation and management is indicated for older patients with traumatic extremity fractures.
Extremity injuries also require different management as compared to younger adults. Older adults may have more difficulties with mobility and activities of daily living if an arm or leg is injured and may require additional support services at home. For example, a younger adult with a distal radius fracture not requiring operative repair can typically be discharged to home safely, but with an older adult you must consider whether the splint will unbalance them, whether they can bathe with only one arm, and whether they use a cane in that hand to walk safely. An older adult with a minor fracture who lives alone can struggle significantly and has a high risk of returning to the ED. In one series, older adults discharged home with isolated forearm fractures had a 10% chance of returning to the ED within 72 hours of discharge (31).
Pharmaceutical Considerations in the Geriatric Trauma Patient
While pharmaceuticals can result in the changes to heart rate and blood pressure, as mentioned above, there are many other classes of medications that may result in impaired primary/secondary evaluations in trauma patients. A list of commonly used agents and their effects on the trauma exam can be seen below:
Table 3: Summary of medication classes complicating the trauma evaluation and care
Medical Evaluation
Geriatric trauma and falls requiring ED care are sentinel events. While in some cases, these occurrences are truly an accident (eg. Passenger in an MVC or pushed down at a stadium), injuries may be preceded by a medical emergency such as myocardial infarction, stroke, dehydration, pulmonary embolism, sepsis, and intentional- or accidental-pharmacologic overdose. It is important to consider these precipitants when evaluating these trauma patients to appropriately stabilize and treat them in the hospital, as well as in preventing future falls and injuries. Bedside electrocardiogram, cardiac enzymes, urinalysis, and drug screen can be included in the typical trauma workup when deemed necessary to evaluate for these causes. Treatment for these concurrent medical emergencies such as MI and stroke should be made in consultation with appropriate specialists.
Disposition
Once the acute injuries have been identified and treated, a gait assessment and review of fall risk factors should be conducted for all older adult trauma patients whether the mechanism was a fall or not. Combination care provided by trauma and a geriatrics team has been shown to improve care, reduce hospital length of stay, and reduce admission to skilled nursing facilities after a hospital stay for geriatric trauma (32, 33). An observation unit or short stay for physical therapy, geriatrician evaluation, and home safety assessment can also identify and address medical and environmental issues that contributed to their presentation (34, 35). All geriatric trauma patients should be screened for evidence of abuse/neglect, as well as substance use and depression/suicidal ideation as precipitants for their trauma.
Table 4: Special considerations in the safe discharge of geriatric trauma patients. Adapted from Clare, D, Zink, K. Geriatric Trauma. Emergency Medicine Clinics of North America, 2021-05-01, Volume 39, Issue 2, Pages 257-271, Copyright © 2021 Elsevier Inc
Case Resolution
The patient’s workup is completed. FAST exam negative. CXR negative, and pelvic XR suggests a posteriorly-dislocated left hip with femoral neck fracture. CT head, chest, and abdomen/pelvis are negative for hemorrhage. Spinal imaging suggesting of non-displaced cervical spinous process fracture and concomitant lumbar vertebral compression fracture. A CT Perfusion study was obtained given the patient’s right-sided weakness, showing a left-sided ACA infarct. Labs notable for lactate of 5, hct of 11, and an INR of 2.8. Her anticoagulation was reversed with 4-factor PCC, and she was admitted to the neuro-icu where she received treatment with a mechanical thrombectomy for her stroke, followed by hip reduction and replacement. Due to residual right-sided weakness and new left-sided immobility, she was sent to inpatient rehabilitation for intensive therapy and medical monitoring. She recovered well and was able to return home with support (but no more driving!) 6 weeks later.
- Bureau, U.S.C. Projections of the size and composition of the U.S. population: 2014 to 2060 population estimates and projections current population reports. 2017; https://www-census-gov.proxy.lib.ohio-state.edu/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
- Trends in causes of death among older persons in the United States, S. National Center for Health, Editor. 2005: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- Stevens, J.A., et al., Self-reported falls and fall-related injuries among persons aged>or=65 years--United States, 2006. J Safety Res, 2008. 39(3): p. 345-9.
- Chang, M.C., National Trauma Data Bank Annual Report. American College of Surgeons, 2016.
- Eagles, D., et al., A systematic review and meta-analysis evaluating geriatric consultation on older trauma patients. J Trauma Acute Care Surg, 2020. 88(3): p. 446-453.
- von Friesendorff, M., et al., Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int, 2016. 27(10): p. 2945-53.
- Garwe, T., et al., Out-of-hospital and Inter-hospital Under-triage to Designated Tertiary Trauma Centers among Injured Older Adults: A 10-year Statewide Geospatial-Adjusted Analysis. Prehosp Emerg Care, 2017. 21(6): p. 734-743.
- Garwe, T., et al., Survival Benefit of Treatment at or Transfer to a Tertiary Trauma Center among Injured Older Adults. Prehosp Emerg Care, 2020. 24(2): p. 245-256.
- Fröhlich, M., et al., Do elderly trauma patients receive the required treatment? Epidemiology and outcome of geriatric trauma patients treated at different levels of trauma care. Eur J Trauma Emerg Surg, 2020. 46(6): p. 1463-1469.
- Uribe-Leitz, T., et al., National Study of Triage and Access to Trauma Centers for Older Adults. Ann Emerg Med, 2020. 75(2): p. 125-135.
- Werman, H.A., et al., Development of statewide geriatric patients trauma triage criteria. Prehosp Disaster Med, 2011. 26(3): p. 170-9.
- Maxwell, C.A., et al., Frailty and Prognostication in Geriatric Surgery and Trauma. Clin Geriatr Med, 2019. 35(1): p. 13-26.
- Simon, B., et al., Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg, 2012. 73(5 Suppl 4): p. S351-61.
- Cheitlin, M.D., Cardiovascular physiology-changes with aging. Am J Geriatr Cardiol, 2003. 12(1): p. 9-13.
- Strait, J.B. and E.G. Lakatta, Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail Clin, 2012. 8(1): p. 143-64.
- Heffernan, D.S., et al., Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma, 2010. 69(4): p. 813-20.
- Salottolo, K.M., et al., A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med, 2013. 21: p. 7.
- Clare, D. and K.L. Zink, Geriatric Trauma. Emerg Med Clin North Am, 2021. 39(2): p. 257-271.
- Walls, R., et al., Rosen's Emergency Medicine: Concepts and Clinical Practice. Ninth ed. 2018.
- Barnes, G.D., et al., National Trends in Ambulatory Oral Anticoagulant Use. Am J Med, 2015. 128(12): p. 1300-5.e2.
- Garza, N., et al., The Increasing Age of TBI Patients at a Single Level 1 Trauma Center and the Discordance Between GCS and CT Rotterdam Scores in the Elderly. Front Neurol, 2020. 11: p. 112.
- Schuur, J.C., Z., Geriatric Trauma, in Rosen's Emergency Medicine: Concepts and Clinical Practice. 2017.
- Chan, D.Y.C., et al., Chronic subdural haematoma during the COVID-19 lockdown period: late presentation with a longer interval from the initial head injury to the final presentation and diagnosis. Chin Neurosurg J, 2021. 7(1): p. 4.
- Goode, T., et al., Evaluation of cervical spine fracture in the elderly: can we trust our physical examination? Am Surg, 2014. 80(2): p. 182-4.
- Healey, C.D., et al., Asymptomatic cervical spine fractures: Current guidelines can fail older patients. J Trauma Acute Care Surg, 2017. 83(1): p. 119-125.
- Battle, C.E., H. Hutchings, and P.A. Evans, Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury, 2012. 43(1): p. 8-17.
- Schellenberg, M., et al., The combined utility of extended focused assessment with sonography for trauma and chest x-ray in blunt thoracic trauma. J Trauma Acute Care Surg, 2018. 85(1): p. 113-117.
- Ahl, R., L. Riddez, and S. Mohseni, Digital rectal examination for initial assessment of the multi-injured patient: Can we depend on it? Ann Med Surg (Lond), 2016. 9: p. 77-81.
- Martinez-Reig, M., L. Ahmad, and G. Duque, The orthogeriatrics model of care: systematic review of predictors of institutionalization and mortality in post-hip fracture patients and evidence for interventions. J Am Med Dir Assoc, 2012. 13(9): p. 770-7.
- Simunovic, N., et al., Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ, 2010. 182(15): p. 1609-16.
- Southerland, L.T., et al., Emergency department recidivism in adults older than 65 years treated for fractures. Am J Emerg Med, 2014. 32(9): p. 1089-92.
- Southerland, L.T., et al., Early geriatric consultation increases adherence to TQIP Geriatric Trauma Management Guidelines. J Surg Res, 2017. 216: p. 56-64.
- Saha, S., et al., Integration of Geriatrician Consultation for Trauma Admissions May Benefit Patient Outcomes. Gerontol Geriatr Med, 2019. 5: p. 2333721419858735.
- Southerland, L.T., et al., An Emergency Department Observation Unit Is a Feasible Setting for Multidisciplinary Geriatric Assessments in Compliance With the Geriatric Emergency Department Guidelines. Acad Emerg Med, 2018. 25(1): p. 76-82.
- Caspers, C.G., Care of Traumatic Conditions in an Observation Unit. Emerg Med Clin North Am, 2017. 35(3): p. 673-683.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Case Rep

Severe Traumatic Brain Injury: A Case Report
Clinton g. nelson.
1 Department of Trauma Surgery, HonorHealth John C. Lincoln Medical Center, Phoenix, AZ, U.S.A.
2 Department of Neurocritical Care, HonorHealth John C. Lincoln Medical Center, Phoenix, AZ, U.S.A
Jeanette Bannister
James dzandu, alicia mangram, victor zach.
Patient: Male, 28
Final Diagnosis: Closed head injury
Symptoms: Bilateral mydriasis • coma
Medication: —
Clinical Procedure: Ventriculostomy and hemicraniectomy
Specialty: Neurology
Unusual clinical course
Background:
Traumatic brain injury remains a challenging and complicated disease process to care for, despite the advance of technology used to monitor and guide treatment. Currently, the mainstay of treatment is aimed at limiting secondary brain injury, with the help of multiple specialties in a critical care setting. Prognosis after TBI is often even more challenging than the treatment itself, although there are various exam and imaging findings that are associated with poor outcome. These findings are important because they can be used to guide families and loved ones when making decisions about goals of care.
Case Report:
In this case report, we demonstrate the unanticipated recovery of a 28-year-old male patient who presented with a severe traumatic brain injury after being in a motorcycle accident without wearing a helmet. He presented with several exam and imaging findings that are statistically associated with increased mortality and morbidity.
Conclusions:
The care of severe traumatic brain injuries is challenging and dynamic. This case highlights the unexpected recovery of a patient and serves as a reminder that there is variability among patients.
In the United State alone, there are approximately 1.5 million traumatic brain injuries (TBI) per year, and TBI is the leading cause of death among individuals under the age of 45 [ 1 , 2 ]. Annually, these injuries result in approximately 50 000 deaths and about 80 000–90 000 cases of debilitating head injuries [ 2 ]. In the US, the estimated annual economic cost of TBIs is $76.5 billion, and we must not forget the emotional and physical toll that disability inflicts on patients and their families [ 3 ]. In many cases, patients are left without the ability to work or to perform activities of daily living (ADLs) [ 4 ]. Initial management of TBI is the most critical time period because it will have the greatest effect on mortality and degree of debility that surviving patients will experience.
In TBI, the most important tool used to assess degree of brain injury and prognosis is exam findings. According to the guideline Early Indicators of Prognosis in Severe Traumatic Brain Injury , on average, 88% of patients who presented with bilaterally un-reactive pupils became vegetative or died, and 4% had good recovery or moderate disability [ 5 ]. The Glasgow Coma Scale (GCS) uses exam findings to quantify level of consciousness following TBI, with 3 being the worst, defined as deep coma or death, and 15 being the best, a fully awake person. In a study by Fearnside et al., out of 315 patients with severe TBI, 65% with initial GCS of 3 died [ 6 ]. In a larger study by Marshall et al., out of 746 patients, 78.4% with initial GCS 3 died and 7.2% had mild to moderate disability [ 7 ].
Radiographic findings can also be used be used to predict morbidity and mortality, and can be used to guide surgical intervention. A review of 753 computed tomography (CT) studies that revealed abnormal mesencephalic cisterns, midline shift, and subarachnoid hemorrhage were associated with an increased risk of elevated intracranial pressure (ICP) and death [ 8 ]. Here, we describe a patient who had all of the above CT findings, and who presented with a GCS of 3 and bilaterally dilated and fixed pupils.
Case Report
Bystanders found a 28-year-old, unhelmeted, white male prone and unconscious after he had lost control of his motorcycle and went off the road. He was brought to the Emergency Department via ambulance intubated as a Level 1 Trauma activation. The physical examination revealed a GCS of 3T, 4 mm bilaterally fixed pupils, negative corneal response, right parietal cephalohematoma, and cerebral spinal fluid (CSF) otorrhea on the right. CT of the head showed subarachnoid hemorrhage with left frontal and temporal subdural hemorrhage ( Figure 1 ), effacement of the suprasellar cistern ( Figure 2 ), and effacement of the 3 rd and 4 th ventricles ( Figure 3 ). In addition, CT studies showed a left frontal/temporal and parietal hematoma with mass effect and cerebral edema causing a 5.38-mm left to right midline shift ( Figure 4 ), a frontal skull base fracture, and a complex non-displaced comminuted fracture of the right temporal bone. He was bradycardic, with his lowest heart rate recorded at 28 bpm, and hypertensive with an initial blood pressure of 172/118 mmHg and markedly elevated blood pressure of 221/105 mm Hg 30 min after his arrival at our facility. He required atropine push and nicardipine infusion. An arterial line and central venous catheters were placed for fluid and medication administration. Emergent treatment for herniation syndrome included endotracheal intubation, 30 grams of IV Mannitol, hypertonic solution of 23% (weight/volume) sodium chloride (NaCl), and left-sided decompressive craniectomy. Postoperatively, an external ventricular drain (EVD) was placed; the initial intracranial pressure (ICP) was 14 mmHg. The patient was examined postoperatively and also after EVD placement. His GCS was 5T, with bilaterally reactive pupils, and positive corneal reflex in the left eye. CT of his head showed improvement of midline shift ( Figure 5 ) and the ventriculostomy catheter tip was found to be in the proper location in the frontal horn of the right lateral ventricle ( Figure 6 ). The patient was then started on 3% NaCl continuous infusion. ICP and cerebral perfusion pressure (CPP) displayed normal values at 3–4 and 70–75 mm Hg, respectively, for the first 24 h with the EVD open at 10 cm H 2 O.

10/30/14 Presenting Head CT showing traumatic subarachnoid hemorrhage in sylvian fissure and left frontal and temporal subdural hemorrhage.

10/30/14 Presenting Head CT showing effaced suprasellar cistern and left temporal subdural hemorrhage.

10/30/14 Presenting Head CT showing cerebral edema with effacement of third ventricle, bilateral traumatic subarachnoid hemorrhage, and left frontal/temporal subdural hematoma.

10/30/14 Presenting Head CT showing left frontal and parietal subdural hematoma, bilateral traumatic subarachnoid hemorrhage, and cerebral edema worse in left hemisphere with 5.38 mm of left to right midline shift.

10/30/14 CT head after left craniectomy for decompression showing improved midline shift and evolving bilateral traumatic subarachnoid hemorrhage.

10/30/14 Head CT after ventriculostomy showing catheter tip in frontal horn of right lateral ventricle.
On hospital day (HD) 2 the patient’s ICP was elevated in the upper 20s in the setting of shivering, hypertension, and fever, which were controlled with increased sedation, nicardipine infusion, and targeted temperature management, respectively. Repeat CT revealed cerebral edema in evolution, with no worsening midline shift or hemorrhage.
On HD 3 his GCS improved from 6T to 8T, with intact brain stem reflexes. The next day, HD 4, the patient’s oxygen saturation dropped from 96% to 87% requiring an increase in fraction of inspired oxygen (FIO2) from 50% to 80% and positive end-expiratory pressure (PEEP). Respiratory cultures were obtained and a chest x-ray revealed worsening bibasilar opacities ( Figure 7 ); therefore, he was empirically started on IV vancomycin.

11/1/14 Chest x-ray showing bilateral interstitial infiltrate and left base atelectasis and pleural effusion.
On HD 5, the patient’s GCS deteriorated from 8T to 3T in the setting of elevated ICP. During bronchoscopy, his ICP was noted to be markedly elevated at 46; therefore, 23% NaCl was administered intravenously over a period of 10 min. Subsequently, a repeat CT of the head was obtained that showed cerebral edema in evolution and no change in midline shift or hemorrhage. Respiratory cultures on HD 6 revealed methicillin-sensitive staphylococcus aureus (>10 000 cfu/ml) and pseudomonas aeruginosa (>10 000cfu/ml). Repeat chest x-ray showed worsening infiltrates and bilateral pleural effusions ( Figure 8 ). The antibiotic was switched from vancomycin to IV levofloxacin and IV cefepime.

11/4/14 Chest x-ray showing worsening interstitial and alveolar infiltrates and pleural effusions bilaterally.
Examination on HD 8 revealed an improved GCS of 6T. His ICP was controlled during an EVD clamp trial, and the EVD was then removed. There were also copious amounts of thick, tan endotracheal secretions; therefore, another bronchoscopy was performed using saline lavage. The patient was started on IV Zosyn and cefepime was discontinued. ICP was controlled by administering 23% NaCl. During a sedation vacation, his oxygen saturation decreased from 95% to 70% and the ventilator settings were therefore changed to airway pressure release ventilation (APRV) mode.
On HD 14, his oxygenation was improving and remained stable at 97%. The ventilator mode was weaned from APRV to continuous mandatory ventilation (CMV). The patient was taken off sedation. His GCS was 10T and he was started on amantadine. He was started on oral metronidazole due to multiple loose stools positive for Clostridium difficile toxin B.
On HD 15, he began blinking to threat, with a GCS of 10T. A CT of his head showed improvement in diffuse cerebral edema and effacement of basal cisterns ( Figure 9 ). He underwent a percutaneous tracheostomy with video-assisted bronchoscopy, and open gastrostomy tube placement by trauma surgery. The patient remained neurologically unchanged on HD 16, but repeat chest x-ray revealed an interval increase in right-sided infiltrates with resolution of left lung opacity. On HD 17, he continued to maintain adequate oxygen saturation at 97% and was started on continuous positive airway pressure (CPAP).

11/14/14 New left occipital horn intraventricular hemorrhage, increased external herniation of left frontal contusion, and resolving diffuse cerebral edema with decreased effacement of third ventricle.
On HD 18 the patient developed tachypnea and he was placed back on CMV. The antibiotics were changed from Zosyn to levofloxacin and nebulized tobramycin due to piperacillin/tazobactam-resistant Pseudomonas pneumonia. On HD 19 his neurologic status was unchanged and he was started on Provigil. He was also given a protective helmet. Two days later, on HD 21, the patient’s neurologic status remained unchanged and he was discharged to a long-term care facility.
A follow-up visit three months later revealed the patient was living at home with his mother. In the interim his tracheostomy and gastrostomy tube had been removed. His major neurologic sequelae were transcortical motor aphasia and mood disorder. His GCS was 13 (E4, V3, M6). His GOS, on a 5-point scale, was 3, with severe injury and permanent need for help with daily living. His Modified Rankin Scale was 3 with moderate disability, requiring some help, but able to walk without assistance. His Lawton Instrumental Activities of Daily Living Scale was 4/8. Barthel Index was 95/100, and National Institutes of Health Stroke Scale was 5. Eleven months after the accident, he had similar outcome scores and had developed a seizure disorder; however, his speech was markedly improved with speech therapy. A repeat CT of the head showed improved external herniation ( Figure 10 ).

8/3/15 Improved external herniation and increase in hydrocephalus secondary to prior brain injury.
When predicting mortality and unfavorable outcome following TBI, exam, laboratory, and imaging findings can be used together by utilizing the CRASH and IMPACT calculators [ 9 , 10 ]. Unfavorable outcome is described as death, vegetative state, or severe disability. Here, we describe a patient who presented with a GCS of 3, bilaterally fixed pupils, and CT findings of subarachnoid bleeding, midline shift, subdural hematoma, effaced 3rd ventricle, effaced 4 th ventricle, and effaced basal cisterns. Therefore, according to the CRASH calculator, which takes into account country, age, GCS, pupil reactivity, and CT findings, he had a 14-day mortality risk of 91.8% and a 95.7% chance of unfavorable outcome at 6 months [ 9 ]. His pertinent laboratory studies, which are utilized along with exam and imaging findings in the IMPACT calculator, revealed an initial glucose concentration of 260 mg/dL and a hemoglobin concentration of 15.4 g/dL. Using the IMPACT calculator, at 6 months, the patient’s predicted probability of mortality was 62% and the probably of unfavorable outcome was 77%. He left our facility bedbound, ventilator- and tube feed-dependent, and in a minimally conscious state with a GCS 10T. Yet despite all this, he had a favorable recovery. Within 1 year of discharge he was able to live at home, interact, and go shopping with his mother, walk, feed himself, and perform simple chores and ADLs.
This is a poignant reminder that variability between individual patients makes prognosticating after traumatic brain injury difficult and uncertain.
Conclusions
Our case shows that severe caution should be taken when using prior studies to make medical decisions about individual patients. Treatment of traumatic brain injuries is complex, and should continue to evolve with evidence-based medicine. Improvement in outcome is not based on 1 intervention; rather, it is the additive effect of multiple interventions. It is possible that the addition of multimodality monitoring could have further changed his outcome, and more studies need to be done to answer this. In addition, daily multidisciplinary rounds with Neurocritical Care, Trauma Critical Care, Infectious Disease, Pharmacy, Respiratory Therapy, Physical Therapy, Occupational Therapy, Social Services, Chaplain Services, and Dietary Services provided optimal medical management in a team-based approach. Further studies need to be conducted to explore the effect that daily multidisciplinary rounds have on the outcome of severe TBIs.
Abbreviations
The authors whose names are listed within this manuscript certify they have no affiliations with any organization or group with any financial or non-financial interest in this report.
References:

IMAGES
COMMENTS
Background The mortality rate is very high for patients with severe multiple trauma with massive pulmonary contusion containing intrapulmonary hemorrhage. Multiple treatment modalities are needed not only for a prevention of cardiac arrest and quick hemostasis against multiple injuries, but also for recovery of oxygenation to save the patient's life. Case presentation A 48-year-old Japanese ...
In this study, we reported a 14-year-old boy referred to the ER due to multiple trauma. He had no history of coagulopathy or anticoagulant consumption. In this case, trauma precipitated parietal contusion. Through medical interventions, bilateral basal ganglia hemorrhage was discovered incidentally.
In addition, the occurrence of multiple trauma around the world is an important issue, and the process of management of these patients is still a challenge from medical, logistic, social, and economic points of view. In accordance to the report of Institute for Health Metrics and Evaluation (IHME), multiple trauma could cause acute inability of ...
A diagnosis of "multiple trauma" implies the presence of two or more separate injuries, at least one or a combination of which endangers the patient's life. ... one study reported a reduction in the rate of death within 1 h after arrival at the hospital from 24.2% to 0% . ... in the case of negative FAST, extra-abdominal bleeding sources ...
This article presents an overview of complex trauma and a case study describing the evidence-informed treatment of a 25-year-old woman with chronic complex trauma symptoms resulting from childhood sexual, physical, and psychological ... 34.5% had been exposed to multiple, chronic trauma by a caregiver (Kisiel, Fehrenbach, Small, & Lyons, 2009 ...
by Pia Jerot and Gregor Prosen Case Presentation A 28-year old male was a restrained driver in a head-on motor vehicle collision. He was entrapped and extricated from the vehicle. Transient loss of consciousness was reported. He complains of severe chest pain, abdominal pain, and right upper leg pain. Critical Bedside Actions and General Approach Multiple … Continue reading Multiple Trauma
Go to: 1. Introduction. The management of polytrauma patients with orthopaedic injuries is a complex and dynamic process that requires a robust understanding of the pathophysiology of the response to trauma and indicators of patient status. There has been a significant evolution in our understanding of these concepts and therefore many changes ...
The search of the literature revealed few case reports on multiple trauma in pediatric patients; there were also few studies on the emergency medical management of these cases. There were more studies that focused on the surgical management of multiple trauma patients, including emergency surgical procedures and early involvement of surgical ...
Trauma Anesthesia. Published online: 18 January 2010. Chapter. Advanced neuroimaging techniques in children with traumatic brain injury. Stephen Ashwal , Karen A. Tong , Andre Obenaus and Barbara A. Holshouser. Pediatric Traumatic Brain Injury.
A case study provides the basis for discussion of the management of the multiply injured trauma patient. The … Initial evaluation of severely injured patients requires an organized, rapid, and thorough evaluation of the patient where life-threatening injuries are identified and treated simultaneously.
The patient was a 72-year-old lady who sustained multiple trauma due to an accident while on a trip to Cappadocia, Central Turkey. She was found unconscious at the scene of the accident, and had difficulty in breathing, and stridor. She was haemodynamically unstable and immediately transferred to the closest well-equipped hospital.
Abstract. This qualitative instrumental collective case study explores how adults with a history of complex trauma experience online learning and their unique needs in the adult/postsecondary ...
Chest and Abdominal Trauma Case Studies Case #1 Scenario: EMS is dispatched to a 2-car MVC with head on collision. The posted speed limit is marked at 40 MPH. Upon EMS arrival to the scene an unrestrained adult driver is found inside the vehicle with noted + steering wheel deformity. The patient is A & O X 3 but appears restless and agitated.
Trauma Case Study: Mike. 35. Case Study Summary: Michelle Audrey Guila Overdose. 36. End of Life care. 37. Trauma Case Study: Johnny Tsunami. 38. End of Life Care. ... Mike, a 35 year-old male, is presented to the emergency department with multiple puncture wounds to the right arm and bruising on the face. He arrived at the hospital via ...
Trauma Case 1: Stab to Left Chest Boston Medical Center - Trauma Case of the Month Case #1: Diagnostic Laparoscopy in Penetrating Chest Trauma. by Rie Aihara, M.D. and Wayne LaMorte, M.D., Ph.D., M.P.H. Pre-Hospital Data. A 17 year-old male from Michigan was visiting his cousins and friends in Boston, when he became a victim of a stabbing.
In this case, the diagnosis was delayed for 11 days. It is the opinion of the authors that without intervention the patient would have continued to deteriorate, and this injury would have resulted in mortality. On review of the case some salient features come to light. It is clear that multiple trauma played a role in the delay of diagnosis.
The hand and the forearm are the main defensive organs and more than often they suffer serious traumatism in car accidents. Guiding these patients to rehabilitation areas is essential for the success of the process. The present case refers to a multiple trauma patient who suffered a car accident which had great impact on his upper left limb.
Case Study. Case Study: A 77 year-old female is brought to the emergency department by EMS for evaluation after a single-car MVC which occurred just prior to arrival. ... highlighting the dramatic physical and physiologic differences that a few decades can make to trauma patients. Multiple studies have demonstrated both the tendency to under ...
Poole et al. (Citation 2017) outlined many different terms related to TIC, with multiple descriptive titles such as trauma-specific and, or informed services, trauma-informed approaches, and, or practice. Many of these terms address different contexts within a specialised trauma service, ... This scoping study aims to identify, collate and ...
jazmine brown november 18, 2020 professor mccrae trauma case study case study 112 multiple trauma: gunshot wound difficulty: advanced setting: emergency
An exploratory multiple-case study design was used to examine the phenomenon of nurses' trauma care and education within their bounded system and context. This approach captured multiple perspectives and generated an in-depth understanding of this phenomenon (Cope, 2015). Further, the purposive sampling approach was used, as particular ...
The client needs multiple diagnostic studies and must be seen within 10 minutes. ... Trauma team members must be prepared to deal with any type o@ injury. Understanding the mechanism o@ injury can assist with predicting the types and combinations o@ injuries sustained. Mechanism o@ injury describes the circumstances and energy @orces that ...
Severe Traumatic Brain Injury: A Case Report is a paper that describes the clinical course and outcome of a young man who suffered a devastating head injury in a motorcycle crash. The paper highlights the challenges and controversies in the management of such patients, as well as the potential for recovery despite poor prognostic indicators. The paper also compares and contrasts the case with ...
Multi-Concept Case Study # Multiple Organ Dysfunction from Trauma and Shock. Related Concepts: Fluid & Electrolytes, Acid-Base Balance, Respiration, Hormonal Regulation, Tissue Integrity, Movement, Ventilator Management, Cardiac Arrest, and Critical Care Medications.