Nutritional Status: An Overview of Methods for Assessment
- First Online: 02 April 2017

Cite this chapter

- Catherine M. Champagne PhD (RDN, LDN, FADA, FAND, FTOS) 6 &
- George A. Bray M.D. 7
Part of the book series: Nutrition and Health ((NH))
2417 Accesses
This chapter focuses on the whole area of nutritional assessment and explores the wide spectrum of testing available that can aid in determining the health of an individual. This process typically includes in-depth evaluation of both subjective data and objective evaluations of an individual’s food and nutrient intake, components of lifestyle, and medical history. A nutritional assessment provides an overview of nutritional status; it focuses on nutrient intake analysis of the diet, which is then compared with blood tests and physical examination.
With comprehensive data on diet and biological information, the physician can make an accurate estimate of that person’s nutritional status. Decisions can then be made on an appropriate plan of action to either maintain current health status or referral to counseling or other interventions that may enable the individual to reach a more healthy state. Only with sufficient anthropometric, biochemical, clinical, and dietary information can a plan be drafted.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

The Nutrition Assessment of Metabolic and Nutritional Balance

Nutritional Status Evaluation: Body Composition and Energy Balance
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14.
Article CAS PubMed PubMed Central Google Scholar
Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8.
Google Scholar
Flegal KM, Panagiotou OA, Graubard BI. Estimating population attributable fractions to quantify the health burden of obesity. Ann Epidemiol. 2015;25:201–7.
Article PubMed Google Scholar
Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA automated multiple-pass method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136:2594–9.
CAS PubMed Google Scholar
Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7:121–34.
Article PubMed PubMed Central Google Scholar
Bray GA. Review of: good calories, bad calories by Gary Taubes. New York: AA Knopf; 2007. Obes Rev. 2008;9:251–63.
Article Google Scholar
Archer E, Hand GA, Blair SN. Validity of U.S. nutritional surveillance: National Health and Nutrition Examination Survey caloric energy intake data, 1971–2010. PLoS One. 2013;8:e76632.
Tooze JA, Vitolins MZ, Smith SL, et al. High levels of low energy reporting on 24-hour recalls and three questionnaires in an elderly low-socioeconomic status population. J Nutr. 2007;137:1286–93.
Shaneshin M, Jessri M, Rashidkhani B. Validity of energy intake reports in relation to dietary patterns. J Health Popul Nutr. 2014;32:36–45.
PubMed PubMed Central Google Scholar
Scagliusi FB, Ferriolli E, Lancha Jr AH. Underreporting of energy intake in developing nations. Nutr Rev. 2006;64(7 Pt 1):319–30.
Balkau B, Deanfield JE, Despres JP, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation. 2007;116:1942–51.
Bray GA. Contemporary diagnosis and management of obesity. 3rd ed. Newtown: Handbooks in Health Care Co; 2003.
Rothney MP, Brychta RJ, Schaefer EV, Chen KY, Skarulis MC. Body composition measured by dual-energy x-ray absorptiometry half-body scans in obese adults. Obesity. 2009;17:1281–6.
Lazzer S, Bedogni G, Agosti F, De Col A, Mornati D, Sartorio A. Comparison of dual-energy x-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br J Nutr. 2008;18:1–7.
Shypailo RJ, Butte NF, Ellis KJ. DXA: can it be used as a criterion reference for body fat measurements in children? Obesity (Silver Spring). 2008;16:457–62.
Nichols J, Going S, Loftin M, Stewart D, Nowicki E, Pickrel J. Comparison of two bioelectrical impedance analysis instruments for determining body composition in adolescent girls. Int J Body Compos Res. 2006;4:153–60.
CAS PubMed PubMed Central Google Scholar
Volgyi E, Tylavsky FA, Lyytikainen A, Suominen H, Alen M, Cheng S. Assessing body composition with DXA and bioimpedance: effects of obesity, physical activity, and age. Obesity (Silver Spring). 2008;16:700–5.
Chen Z, Wang Z, Lohman T, et al. Dual-energy x-ray absorptiometry is a valid tool for assessing skeletal muscle mass in older women. J Nutr. 2007;137:2775–80.
Neovius M, Hemmingsson E, Freyschuss B, Udden J. Bioelectrical impedance underestimates total and truncal fatness in abdominally obese women. Obesity (Silver Spring). 2006;14:1731–8.
Drewnowski A. Obesity and the food environment. Dietary energy density and diet costs. Am J Prev Med. 2004;27(3S):154–62.
Kant AK, Graubard BI. Energy density of diets reported by American adults: association with food group intake, nutrient intake, and body weight. Int J Obes. 2005;29:950–6.
Article CAS Google Scholar
Champagne CM, Casey PH, Connell CL, Lower Mississippi Delta Nutrition Intervention Research Initiative, et al. Poverty and food intake in rural America: diet quality is lower in food insecure adults in the Mississippi Delta. J Am Diet Assoc. 2007;107:1886–94.
Stuff JE, Casey PH, Connell CL, et al. Household food insecurity and obesity, chronic disease, and chronic disease risk factors. J Hunger Environ Nutr. 2006;1:43–62.
Hoy KM, Goldman JD. Fiber intake of the U.S. population: what we eat in America, NHANES 2009–2010. Food Surveys Research Group, Dietary Data Brief No. 12; 2014.
Guenther PM, Casavale KO, Reedy J, et al. Healthy Eating Index 2010. Center for Nutrition Policy and Promotion. CNPP Fact Sheet No. 2. 2013. http://www.cnpp.usda.gov/sites/default/files/healthy_eating_index/CNPPFactSheetNo2.pdf . Accessed 22 Mar 2016.
Suggested Further Reading
Bray GA, Bouchard C. Handbook of obesity. Clinical applications. 4th ed. Boca Raton: CRC Press; 2014.
Book Google Scholar
Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey (NHANES). Laboratory methods. http://www.cdc.gov/nchs/nhanes/nhanes2011-2012/lab_methods_11_12.htm .
Food and Nutrition Board, Institute of Medicine—FNB. http://www.healthfinder.gov/orgs/HR0139.htm .
Mahan LK, Raymond JL, Escott-Stump S, editors. Krause’s food & the nutrition care process. 13th ed. Philadelphia: W.B. Saunders; 2011.
Schlenker E, Gilbert JA. Williams’ essentials of nutrition & diet therapy. 11th ed. Maryland Heights: Mosby; 2014.
USDA, National Agricultural Library, Food and Nutrition Information Center. https://fnic.nal.usda.gov/ .
Download references
Author information
Authors and affiliations.
Department of Nutritional Epidemiology, Pennington Biomedical Research Center, Louisiana State University, 6400 Perkins Road, Baton Rouge, LA, 70808, USA
Catherine M. Champagne PhD (RDN, LDN, FADA, FAND, FTOS)
Pennington Biomedical Research Center, Louisiana State University, Baton Rouge, LA, USA
George A. Bray M.D.
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Catherine M. Champagne PhD (RDN, LDN, FADA, FAND, FTOS) .
Editor information
Editors and affiliations.
Athabasca University Centre for Science, Athabasca, Alberta, Canada
Norman J. Temple
Winona State University Department of Biology, Winona, Minnesota, USA
Louisiana State University Pennington Biomedical Research Center, Baton Rouge, Louisiana, USA
George A. Bray
Rights and permissions
Reprints and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Champagne, C.M., Bray, G.A. (2017). Nutritional Status: An Overview of Methods for Assessment. In: Temple, N., Wilson, T., Bray, G. (eds) Nutrition Guide for Physicians and Related Healthcare Professionals. Nutrition and Health. Humana Press, Cham. https://doi.org/10.1007/978-3-319-49929-1_35
Download citation
DOI : https://doi.org/10.1007/978-3-319-49929-1_35
Published : 02 April 2017
Publisher Name : Humana Press, Cham
Print ISBN : 978-3-319-49928-4
Online ISBN : 978-3-319-49929-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
SYSTEMATIC REVIEW article
Nutritional status and dietary intake of school-age children and early adolescents: systematic review in a developing country and lessons for the global perspective.

- 1 Division of Women and Child Health, Aga Khan University Hospital, Karachi, Pakistan
- 2 Institute of Global Health and Development, Aga Khan University, Karachi, Pakistan
- 3 Policy and Strategic Planning Unit, Ministry of Health, Government of Punjab, Lahore, Pakistan
- 4 Faculty of Health and Medical Sciences, Robinson Research Institute, The University of Adelaide, Adelaide, SA, Australia
- 5 Centre for Global Child Health, The Hospital for Sick Children (SickKids), Toronto, ON, Canada
- 6 Government Services Hospital, Karachi, Pakistan
- 7 Ministry of Health, Government of Sindh, Karachi, Pakistan
Background: The prevalence of double burden of malnutrition (DBM) is high in low- and middle-income countries (LMICs). Data on malnutrition trends is present for children <5 years of age, however the data for school-going children and adolescents aged 5–15 years is scarce.
Objective: This systematic review presents the pooled prevalence of nutritional status and dietary intake among school-going children and adolescents (5–15 years of age) in an LMIC of Pakistan and the perspective for broader global nutrition in this age group.
Methods: An electronic search of databases was run on Pubmed and Medline (via Ovid) along with gray literature and archives of local scientific journals till 2nd January 2021. Studies meeting the eligibility criteria were included and relevant data were extracted, and a pooled proportional analysis was performed.
Results: A total of 51 studies including 62,148 children of 5–15 years met the inclusion criteria, of which 30 studies reported on anthropometric indices alone, eight on dietary intake patterns while 13 reported both. All of the included studies had a cross-sectional study design. There were 20 studies from the province of Punjab, 15 from Sindh, eight from Khyber Pakhtoonkhwa, two from Balochistan, and three from multiple cities across Pakistan. The pooled proportional analysis showed that the proportion of underweight children and adolescents was 25.1% (95% CI 17.3–33.7%); stunting 23% (95% CI 11.8–36.7%); wasting 24% (95% CI 15.2–34%); thinness 12.5% (95% CI 9.4–16.1%); overweight 11.4% (95% CI 7.2–16.3%); and obesity 6.9% (95% CI 3–12%). A relatively high intake of carbohydrates, soft drinks, and sweets/chocolates; and a low intake of protein-rich foods, fruits, and vegetables, compared to the recommended daily allowance (RDA), was reported.
Conclusion: The limited data suggests the presence of DBM amongst children aged 5–15 years and also identified that dietary intake patterns are not meeting the recommended allowance. This review highlights the gaps and the need for larger, well-designed studies for this age group with the representation of different contexts and the need for similar studies in various LMICs, so that appropriate actions be deliberated and appropriate programs should be designed focusing on this vital population.
Introduction
Populations in which there is co-existence of under- and over-nutrition are known to be facing the double burden of malnutrition (DBM) ( 1 ). According to Global Nutrition Reports 2018, one in three people suffer from malnutrition, one in 20 children complain of hunger, and one in every five deaths around the world is attributed to poor diet ( 2 ). DBM is more prevalent in low- and middle-income countries (LMIC), with a higher prevalence in poorer LMICs ( 3 ). It is especially prevalent in sub-Saharan Africa, South-East Asia, and the Pacific ( 3 ). The progress in the reduction of the burden of malnutrition worldwide has been slow and it is therefore advised to collect population-specific data to better understand the nutrition dynamics across the world and to allow the nutritional needs of communities to be addressed adequately ( 2 , 4 ).
An issue being ignored is malnutrition trends in children over the age of 5 years. The World Health Organization (WHO) reports 1.8 billion children to be in the age bracket of 5–15 years worldwide, with 90% of this population residing in LMICs ( 5 ). There is no consistent terminology used to describe children age 5–15 years which proves the narrow focus on younger children and neglect of this age group, however, children age 5–10 years are often referred to as school-going children ( 6 ), while adolescent has been defined by the WHO as children aged 10–19 years, with early adolescent defined to be in an age bracket of 10–14 years and late adolescent between 15 and 19 years ( 7 ). Whether DBM exists in this age bracket and to what extent is a query that is yet to be adequately explored.
In 2011, the United Nations Children's Fund (UNICEF) published a report stating that adolescence provides a second window of opportunity to improve the nutritional status of children and prevent future health consequences of malnourishment ( 8 ). However, nutritional challenges occur throughout the life cycle of an individual, therefore, nutritional needs through each phase must be assessed and addressed adequately ( 7 ), especially school-going children and adolescents age 5–15 years. Mental and physical development continues through this age bracket and it gives individuals a chance to improve their nutritional deficiencies, thereby preventing impairment of growth, development, and cognitive achievement ( 8 ). It is known that major developmental and physical changes occur within the early adolescence phase. This includes growth spurt, development of sex organs, secondary sexual characteristics, and, according to recent neuroscientific research, significant increase and reorganization in the neuronal network ( 8 ). A relatively newer concept referred to as developmental origins of adult health and disease (DOHaD) postulates that poor nutrition during the early phases of life is associated with chronic illnesses in adulthood ( 9 ). The current scarcity of data on school-going children and adolescents and now, with the increase in child survival rates, the number of children entering their second decade is increasing and their health and nutritional needs compel attention.
The WHO proposes strategic guidance and planning on actions for child health in the South-East Asian Region (SEAR), however, it is limited to adolescents alone ( 10 ). It has been reported that 20% of the population in the South-East Asian Region comprises of adolescents, which make up to a total of 360 million adolescents in the region ( 11 ). The process used by WHO in developing strategic guidance for improving adolescent health was by first conducting relevant reviews under national, regional, or global categories, followed by surveys in those regions to identify lessons learned and proposals for future actions. They also took input from experts in the field and then finally developed the guidance ( 10 ). This process should be adopted by other LMICs to identify the gaps and make the necessary interventions for improvement.
It is imperative that children above 5 years of age be assessed for undernutrition, overnutrition, and nutritional deficiencies, and therefore this systematic review aims to present a narrative on the trends of nutritional status and dietary intake patterns among school-going children and adolescents 5–15 years of age across Pakistan with a broader commentary related to global nutrition status, and challenges in this age group across other LMICs. This systematic review can be used as an example to synthesize the available literature and identify gaps in nutritional status and dietary intake patterns amongst school-going children and early adolescents aged 5–15 years in other LMICs.
Materials and Methods
Types of studies and participants.
We included observational studies (prospective and retrospective cohort, and cross-sectional studies) reporting data on nutritional status and dietary intake and their association to gender, locale (urban vs. rural), school type (government vs. private), family income, and lifestyle (sedentary vs. active) amongst school-going children and early adolescents aged 5–15 years in Pakistan. We also included studies reporting nutrition trends in children affected by natural disasters or employed as laborers. Studies that assessed dietary intake and prevalence of malnutrition amongst children were included, as long as data on our age group of interest was also present. Studies exclusively assessing children with known co-morbidities or on Pakistani children living abroad were excluded. We included studies that were published during and after the year 2000 to ensure we get information on current trends, with the last date of the search conducted on the 2nd of January 2021.
Types of Outcomes
We included studies that met our eligibility criteria and reported outcomes on anthropometric indices or dietary intake, such as underweight [weight-for-age Z (WAZ) score < −2 SD], stunting [height-for-age Z (HAZ) score < −2 SD], wasting [weight-for-height Z (WHZ) score< −2 SD], thinness (BMI-for-age < −2 SD), overweight (BMI-for-age > +1 SD), obesity (BMI-for-age > +2 SD), macro/micronutrient deficiencies, food, and nutrient intake. We also extracted the associations of these outcomes, such as gender, socio-economic status, private vs. government schools, family income, and sedentary lifestyles.
Search Methods
We conducted an electronic literature search until 2nd January 2021 using Pubmed, Medline (via Ovid), and Google Scholar. Gray literature search was conducted on databases from the WHO, UNICEF, Food and Agriculture Organization (FAO), World Food Programme (WFP), Global Alliance for Improved Nutrition (GAIN), Scaling Up Nutrition (SUN), Action Against Hunger, International Food Policy Research Institute (IFPRI), and Google web. We also searched the archives of local journals [Journal of Pakistan Medical Association (JPMA) and Journal of Ayub Medical College (JAMC)] separately and went through the reference lists of included studies. We included articles that provided data on nutritional status and dietary intake patterns and their associations amongst school-aged children and early adolescents aged 5–15 years in Pakistan. Nutritional status was defined as “a physiological state of an individual, which results from the relationship between nutrient intake and requirements, and from the body's ability to digest, absorb and use these nutrients” ( 12 ).
The completed search strategy used for Pubmed and Medline (via Ovid) is presented as Supplementary Tables 1a,b ). The following MeSH terms and their variants were used for our search strategy: “Nutritional Status” OR “Nutrition Assessment” OR “Diet” OR “Micronutrients” AND (“Schools” OR “Child” OR “Child/education” OR “Adolescent”) AND (“Pakistan” OR “South Asia”). Studies conducted by the same author on the same population were scrutinized for overlapping data and the studies with the inclusion of more relevant variables were chosen. There were no language restrictions placed while screening articles.
Data Collection and Analysis
Two reviewers (DSK and JKD) screened titles and abstracts for eligibility using EndNote X8 ( 13 ). We retrieved full texts of the remaining articles and examined them based on our eligibility criteria. Studies that fulfilled the inclusion and exclusion criteria were selected for this review. Any conflicts regarding article selection were resolved through mutual consensus. We extracted data on Microsoft Excel from the included studies on variables including study background (province, city), population, age group, sample size, setting (rural vs. urban, school vs. community, government vs. private schools), socioeconomic status, anthropometric indices (underweight, stunting, wasting, thinness, overweight and obesity), dietary intake patterns and associations ( 14 ).
Data were analyzed and pooled prevalence was performed on the Joanna Briggs Institute (JBI) SUMARI software ( 15 ). The meta-analysis pooled overall prevalence using Dersimonian and Laird random-effect meta-analysis after transforming data using Freeman-Tukey transformation arcsine square root transformation. The review pooled overall means and proportion for the age group of 5–15 years and reported their 95% confidence intervals (CI) and the percentage of variation across studies that is due to heterogeneity rather than chance using I 2 statistics. Studies with participants of age 0–19 years, from which data specifically for 5–15 years age group could not be extracted, were placed in the age category of either 5–19 years or 0–19 years; and pooled separately. We also pooled performed subgroup analysis based on gender, geographic setting i.e., urban/rural, provinces, natural disaster, special population i.e., children who were laborers, school attended (private or government), and socio-economic class, for children age 5–15 years.
We used the National Institute of Health (NIH)—National Heart, Lung, and Blood Institute (NHLBI) quality assessment tool for cross-sectional studies to assess the quality and potential risk of bias for all the included studies ( 16 ). This tool helps evaluate the internal validity of a study, hence ensuring that the results are truly due to the exposure being evaluated.
This systematic review follows the guidelines recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) ( 17 ). The PRISMA checklist is presented in Supplementary Table 2 .
Our electronic search for all databases yielded a total of 11,539 articles that underwent title and abstract screening. A total of 276 articles were selected for full-text review, of which 39 met the eligibility criteria. Through cross-referencing of included articles and local journals, another 12 articles were added, leading to a total of 51 studies being selected for inclusion as depicted in Figure 1 . Results were reported according to two categories, namely “anthropometry” and “dietary intake”.
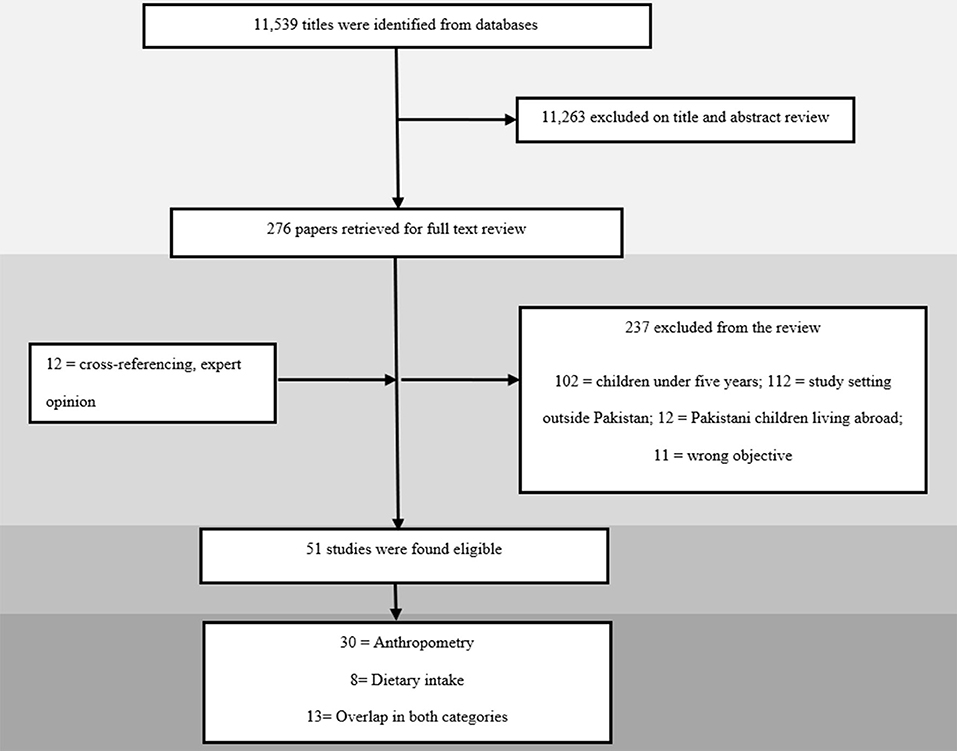
Figure 1 . Search flow diagram.
Description of Included Studies
A total of 51 studies were included, all of which had a cross-sectional study design ( 18 – 68 ). The studies were conducted between the years 2002 and 2020 in different cities across Pakistan. Twenty-eight studies reported data specifically on children between 5 and 15 years of age ( 19 , 21 – 23 , 25 – 29 , 31 , 32 , 35 , 38 , 44 , 45 , 47 – 50 , 52 , 54 , 55 , 59 , 60 , 62 – 64 , 67 ). The remaining 23 studies had children in our age group of interest but beyond it too, with seven reporting data on children between 0 and 19 years of age ( 24 , 34 , 51 , 56 , 58 , 61 , 65 ) and 16 reporting on children 5 and 19 years of age ( 18 , 20 , 30 , 33 , 36 , 37 , 39 – 43 , 46 , 53 , 57 , 66 , 68 ). There were only five studies that reported data specifically on children in the 5 to 10 age group ( 29 , 34 , 64 – 66 ) and only three studies in the 10 to 15 years age group ( 21 , 24 , 47 ). Province wise; 20 studies were conducted in Punjab ( 19 , 22 , 24 , 28 , 29 , 31 , 39 , 40 , 44 , 46 , 52 – 54 , 58 , 65 , 67 ), 15 in Sindh ( 18 , 20 , 21 , 23 , 30 , 32 , 36 – 38 , 43 , 45 , 49 , 55 , 63 ), eight in Khyber Pakhtoonkhwa (KP) ( 26 , 34 , 35 , 47 , 48 , 50 , 61 , 64 ), two in Balochistan ( 25 , 51 ), four from the federal capital ( 27 , 42 , 66 , 68 ), and three from multiple cities across Pakistan ( 41 , 56 , 57 ). The remaining three studies failed to report their location ( 33 , 59 , 62 ).
A total of 35 studies were conducted in urban areas ( 18 – 46 , 52 , 63 , 65 – 68 ), while five were conducted in rural areas ( 47 – 51 ), six in both ( 53 – 58 ), and the remaining five did not report their setting ( 59 – 62 , 64 ). Forty studies were carried out in a school setting ( 15 , 16 , 19 – 22 , 24 – 40 , 42 , 44 – 52 , 55 , 58 , 59 , 61 , 63 – 65 ), nine in community setting ( 21 , 27 , 45 , 47 , 57 , 58 , 60 , 61 , 66 ), and two studies did not specify ( 22 , 64 ). Of the forty conducted in schools, 22 studies were conducted across both government and private schools ( 18 , 20 , 23 , 24 , 26 , 28 , 29 , 31 , 35 , 37 , 38 , 40 , 43 , 44 , 48 , 52 – 54 , 56 , 62 , 67 , 68 ), seven in private schools exclusively ( 19 , 25 , 30 , 36 , 39 , 41 , 65 ), and five were carried out in government schools ( 32 , 33 , 49 , 50 , 55 ). Six studies did not specify their study setting ( 34 , 42 , 46 , 51 , 59 , 63 ). There were two studies which reported nutritional status amongst children affected by natural disasters ( 47 , 50 ) and two on child laborers ( 45 , 68 ). For the age group of 5–15 years particularly, 17 studies reported anthropometric indices with respect to gender ( 19 , 21 – 23 , 26 , 28 , 29 , 32 , 35 , 38 , 44 , 48 , 49 , 54 , 60 , 62 , 63 ), 18 with respect to geographic setting; urban or rural ( 19 , 21 – 23 , 26 – 29 , 32 , 35 , 38 , 44 , 48 , 49 , 52 , 63 , 67 ), three with respect to socioeconomic status ( 29 , 35 , 52 ) and eight with respect to school attended; private or government ( 19 , 26 , 28 , 32 , 44 , 49 , 62 , 65 ).
The included studies in this review targeted 62,148 individuals. Two studies had a sample size of >10,000 ( 56 , 57 ), 14 studies had a sample size of 1,000–9,999 individuals ( 21 , 24 , 28 , 29 , 31 , 37 , 42 , 47 – 49 , 51 , 54 , 55 , 58 ), six had a sample size of 500–999 ( 18 , 30 , 33 , 38 , 53 , 60 ), 27 studies between 100 and 499 ( 19 , 20 , 22 , 23 , 25 – 27 , 32 , 34 – 36 , 39 – 41 , 43 – 46 , 50 , 52 , 59 , 62 , 64 – 68 ), and two studies with a sample size of <100 individuals ( 61 , 63 ).
Of the selected 51 studies, 30 reported data on anthropometric indices only ( 18 , 23 , 26 – 29 , 33 – 35 , 37 – 39 , 43 – 45 , 47 – 52 , 54 , 56 , 60 – 66 ), eight reported data on dietary intake alone ( 20 , 25 , 31 , 41 , 53 , 55 , 57 , 68 ), while 13 reported both, anthropometric indices and dietary intake patterns across our population of interest ( 19 , 21 , 22 , 24 , 30 , 32 , 36 , 40 , 42 , 46 , 58 , 59 , 67 ). The characteristic of each included study is presented briefly in Table 1 below with a detailed version included as Supplementary Table 3 .
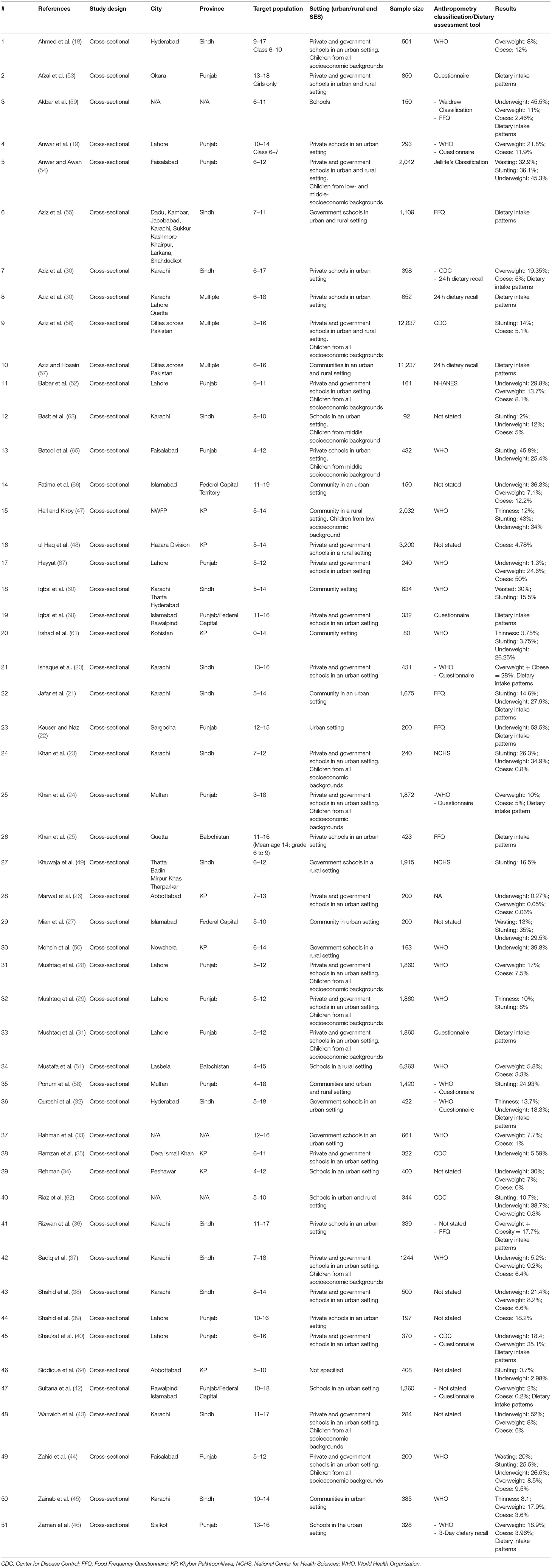
Table 1 . Brief overview of characteristics of included studies.
Quality of Studies
Quality assessment using NHLBI tool for cross-sectional studies, as presented in Supplementary Table 4 and briefly as Table 2 , showed that all studies had clearly stated their objective and had a participation rate of >50%, with all the subjects selected from the same population. 88.2% of studies had specified and defined their population, while only 33.3% had justified sample size calculation. Since all the studies were cross-sectional, exposure was not measured prior to outcomes, studies were assessed at one point in time and therefore had no follow-ups. Outcomes were defined by 74.5% of the studies, while none of the studies reported outcomes to be blinded to assessors. 25.5% of studies measured confounding variables and adjusted them statistically to assess associations to the outcomes.
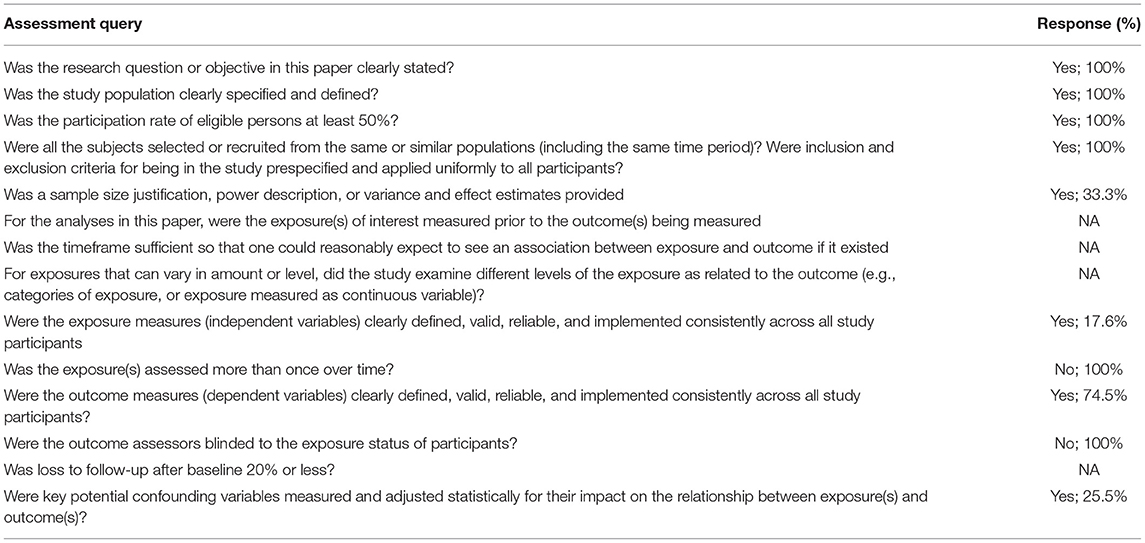
Table 2 . Summary of NHLBI quality assessment.
Anthropometric Indices
We identified 43 studies reporting data on anthropometric indices ( 18 , 19 , 30 , 32 – 40 , 42 – 52 , 54 , 56 , 58 , 59 , 61 – 68 ). Our focus was to report the prevalence of malnutrition for the age group 5–15 years, however, some studies reported data beyond our age group of interest due to which an overall analysis, with overlapping data from 5 to 15 years age group, was also conducted for age groups zero to 19 and 5–19 years as depicted in Table 3 , Supplementary Figures 1–3 . The age group 5–19 was also separately reported to understand the overall malnutrition trends in children above 5 years of age. Anthropometric indices reported amongst school-going children and early adolescents age 5–15 years across provinces in Pakistan are depicted in Table 4 , Figure 2 , however, no data amongst children from Balochistan in this age group was available. Anthropometric indices with respect to gender, geographic setting (urban or rural), and type of school attended (private or government), along with indices of children affected by natural disasters (e.g., flood, earthquake, etc.) and child laborers in this age group have also been reported in Table 4 , Supplementary Figures 4–9 .
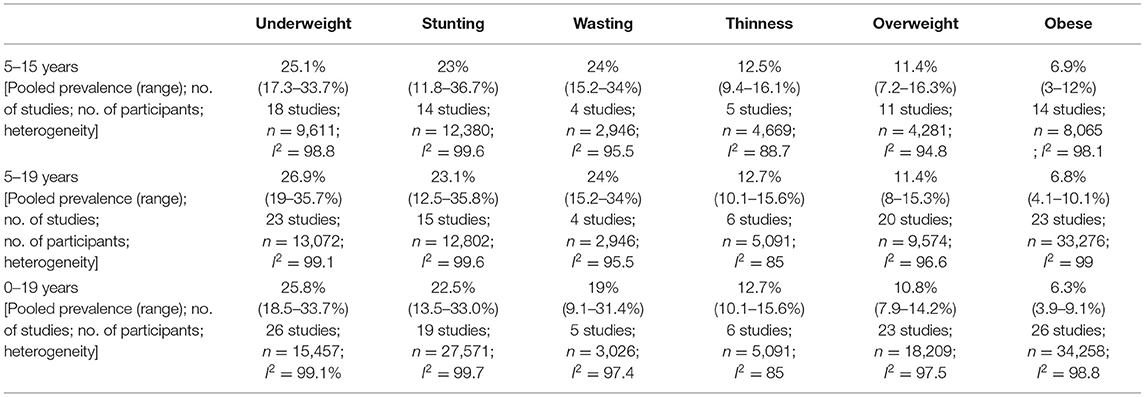
Table 3 . Prevalence of Anthropometric Measures in Pakistan according to age groups.
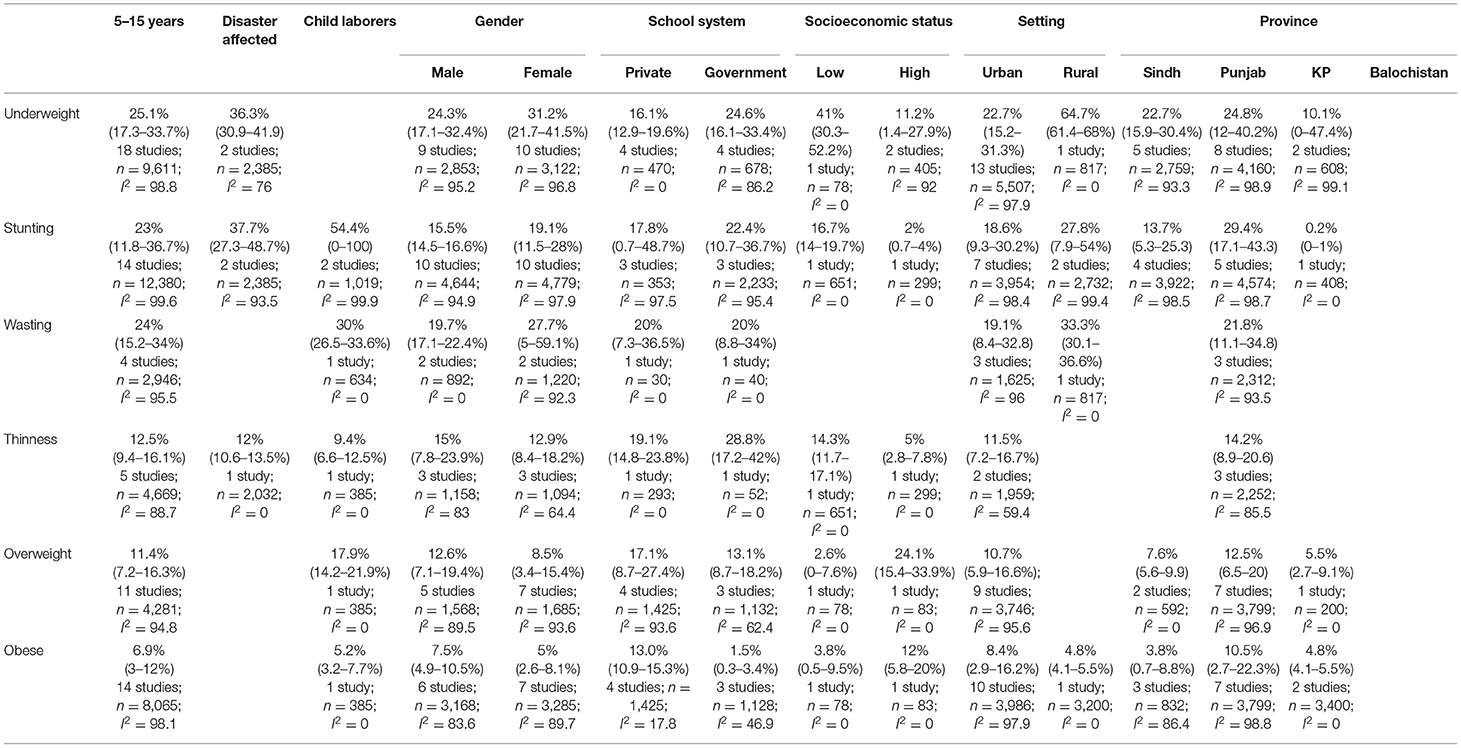
Table 4 . Setting specific anthropometric indices in children age 5–15 years.
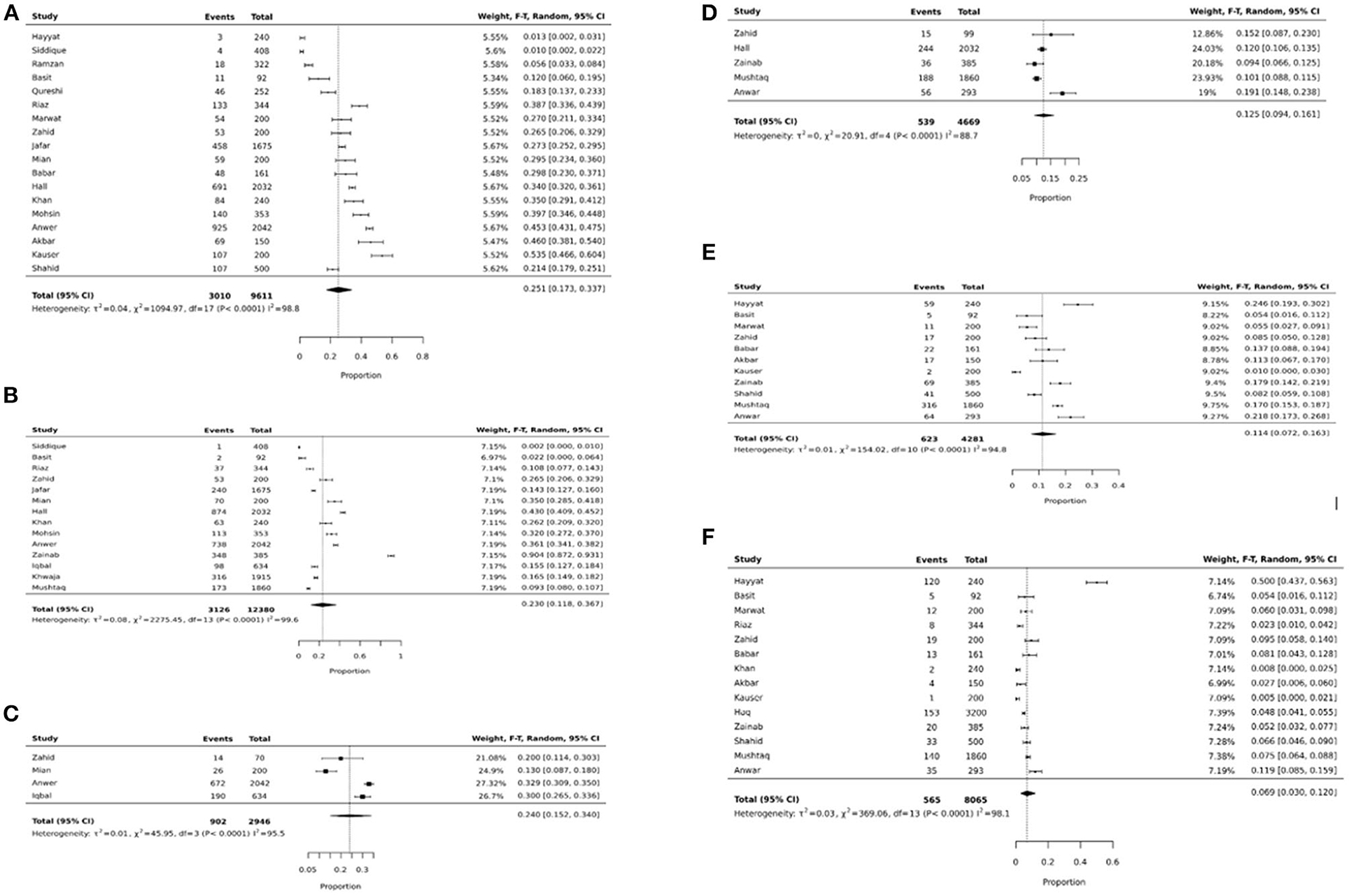
Figure 2. (A) Underweight pooled prevalence in 5–15 years. (B) Stunting pooled prevalence in 5–15 years. (C) Wasting pooled prevalence in 5–15 years. (D) Thinness pooled prevalence in 5–15 years. (E) Overweight pooled prevalence in 5–15 years. (F) Obese pooled prevalence in 5–15 years.
We noticed similar trends of pooled prevalence for children age 0–19 and 5–19 across all anthropometric indices as shown in Table 3 . This could be because of the overlap in data across all three age groups.
The pooled prevalence of underweight amongst school-going children and adolescents age 5 to 15 years was 25.1% (95% CI: 17.3–33.7%; 18 studies; 9,611; I 2 : 98.8) ( Table 4 , Figure 2A ). The prevalence was found to be higher amongst females (31.2%; 95% CI: 21.7–41.5%), children from government schools (24.6%; 95% CI: 16.1–33.4%), belonged to low SES (41%; 95% CI: 30.3–52.2%), from the province of Punjab (24.8% 95% CI: 12–40.2%), and Sindh (22.7%; 95% CI: 15.9–30.4%), and from disaster striken areas (36.3%; 95% CI: 30.9–41.9%) ( Supplementary Figure 4 ).
The overall pooled prevalence of stunting in school-going children and adolescents age 5–15 years was 23% (95% CI: 11.8–36.7%; 14 studies; 12,380 participants; I 2 : 99.6) ( Figure 2B ). The prevalence was was higher amongst females (19.1%; 95% CI: 11.5–28%), children going to government schools (22.4%; 95% CI: 10.7–36.7%), those from a low SES (16.7%; 95% CI: 14–19.7%), and those who lived in rural areas (27.8%; 95% CI: 7.9–54%) ( Table 4 ). The highest stunting pooled prevalence was noted to be amongst children from the province of Punjab (29.4%; 95% CI: 17.1–43.3%), those who were laborers (54.4%; 95% CI: 0–100%), and disaster striken areas (37.7%; 95% CI: 27.3–48.7%) ( Supplementary Figure 5 ).
The pooled prevalence of wasting amongst school-going children and adolescents age 5–15 years was 24% (95% CI: 15.2–34%; 4 studies; 2,946 participants; I 2 : 95.5) ( Figure 2C ). Wasting was reported to be higher amongst females (27.7%; 95% CI: 5–59.1%), and those who lived in rural areas (33.3%; 95% CI: 30.1–36.6%). Data on wasting prevalence was only available for the province of Punjab with a pooled prevalence of 21.8% (95% CI: 11.1–34.8%) ( Supplementary Figure 6 ).
The overall prevalence of thinness was 12.5% (95% CI: 9.4–16.1; 4 studies; 4,669 participants; I 2 : 88.7) ( Figure 2D ). Thinness was reported to be higher amongst males (15%; 95% CI: 7.8–23.9%), those attending government schools (28.8%; 95% CI: 17.2–42%), and those from a low SES (14.3% 95% CI: 11.7–17.1%) ( Table 4 ). Data on thinness prevalence was only available for the province of Punjab with a pooled prevalence of 14.2% (95% CI: 8.9–20.6). For children from disaster-affected regions and child laborers, the pooled prevalence of thinness was reported to be 12% (95% CI: 10.6–13.5%) and 9.4% (95% CI: 6.6–12.5%), respectively ( Supplementary Figure 7 ).
The overall overweight pooled prevalence for school-going children and adolescents age 5–15 years was 11.4% (95% CI: 7.2–16.3%; 11 studies; 4,281 participants; I 2 : 94.8) ( Figure 2E ). Overweight pooled prevalence was noted to be higher amongst males (12.6%; 95% CI: 7.1–19.4%), children going to private schools (17.1%; 95% CI: 8.7–27.4%), and those from a high SES (24.1%; 95% CI: 15.4–33.9%) ( Table 4 ). Between provinces, the highest overweight prevalence was amongst children from Punjab (12.5%; 95% CI: 6.5–20%), followed by Sindh (7.6%; 95% CI: 5.6–9.9%) and the least in KP (5.5%; 95% CI: 2.7–9.1%) ( Supplementary Figure 8 ).
The pooled prevalence on obesity was 6.9% (95% CI: 3–12%; 14 studies; 8,065 participants; I 2 : 98.1) ( Figure 2F ). The pooled prevalence of obesity was noted to be higher amongst males (7.5%; 95% CI: 4.9–10.5%), children attending private schools (13%; 95% CI: 10.9–15.3%), those from high SES (12%; 95% CI: 5.8–20%), and those living in urban areas (8.4%; 95% CI: 2.9–16.2%) ( Table 4 ). The highest obesity pooled prevalence was reported amongst children from Punjab (10.5%; 95% CI: 2.7–22.3%), followed by KP (4.8%; 95% CI: 4.1–5.5%), and least in Sindh (3.8%; 95% CI: 0.7–8.8%). Only 5.2% (95% CI: 3.2–7.7%) obesity pooled prevalence was reported amongst child laborers ( Supplementary Figure 9 ).
For the age group of 5–10 years, we could only calculate pooled prevalence for underweight which was 6.5% (95% CI: 2–13.1%; 5 studies, 1,569 participants, I 2 : 94.7%) and stunting at 4% (95% CI: 0 to 12.7%; 4 studies, 1,044 participants, I 2 :96%) ( Supplementary Figure 10 ). While for the age group 10–15 years, pooled prevalence was only calculated for overweight at 5.9% (95% CI: 3.4 to 8.9%; 2 studies, 678 participants, I 2 : 56.8%) and obesity at 2.5% (95% CI: 0.5–5.8%; 2 studies, 678 participants, I 2 :79.3%) ( Supplementary Figure 11 ). This is due to lack of data on anthropometric indices for these age groups specifically.
Dietary Intake
Our systematic review includes 21 studies which reported dietary intake trends amongst school-going children and adolescents aged 5 to 15 years ( 19 – 22 , 24 , 25 , 30 – 32 , 36 , 40 – 42 , 46 , 53 , 55 , 57 – 59 , 67 , 68 ). The tools used to assess dietary intake patterns are presented in Table 1 .
The recommended percentage of daily energy contribution, according to the Acceptable Macrnonutrient Distribution Ranges (AMDR), for carbohydrates, proteins, and fats in children age 4–18 years is 45–65%, 10–30%, and 25–35%, respectively ( 69 ). Aziz 2014 reported that children from schools across Pakistan had an overall increased daily intake of carbohydrates (60–75%) ( 57 ). Two separate studies conducted in different cities across Pakistan reported the highest carbohydrate consumption amongst children from Balochistan ( 41 , 57 ). Aziz et al. ( 30 ) conducted a study on children from Karachi and reported they have an upper limit of carbohydrate consumption ( 30 ).
Aziz et al. ( 41 ) reports children generally had the lowest consumption of protein compared to the recommended daily allowance (RDA) ( 41 ). Sultana et al. ( 42 ) conducted a study on children from Punjab and reported they have the highest protein intake (12%) when compared to other provinces ( 57 ). A study assessing lunch box contents amongst 1,360 students noticed meals to be low in proteins and fiber but high in fat ( 42 ). Aziz et al. ( 41 ) and Aziz and Hosain ( 57 ) conducted two studies assessing fat intake and it was noted that fat intake amongst children across Pakistan was below the recommended daily standards ( 41 , 57 ).
For micronutrients , Kausar 2018 reported girls to have inadequate dietary intake with their daily consumption being less than the Recommended Daily Allowance (RDA) ( 22 ). This was seconded by Zaman et al. ( 46 ), reporting female participants to have an overall lower energy intake and failure to meet the recommended intake of vitamins A, C, D, E, folic acid, phosphorus, zinc, sodium, potassium, iron, and magnesium as compared to the RDA ( 46 ). Males on the other hand were found to have a higher carbohydrate, sugar, fiber, and fat consumption ( 46 ). Children from high socioeconomic status settings were observed to have a higher vitamin and supplements intake ( 68 ).
Aziz et al. ( 55 ) reported breakfast consumption varied with socioeconomic status as children from rural areas or squatter settlements were more likely to skip breakfast. However, Shaukat et al. ( 40 ) reported 29% of their population from an urban setting skipped breakfast. A single study reported 8% of their population skipped breakfast and were more likely to be overweight or obese ( p < 0.002) ( 31 ). Qureshi et al. ( 32 ), on the other hand, reports 82.2% of their population had insufficient breakfast and found a higher prevalence of thinness and stunting amongst them.
There are 11 studies included in our systematic review that reported dietary intake in children according to food groups. Table 5 below gives an overview of the dietary intake patterns. It can be noted that children have suboptimal vegetable and fruit intake while consumption of soft drinks and sweets/chocolates is high.
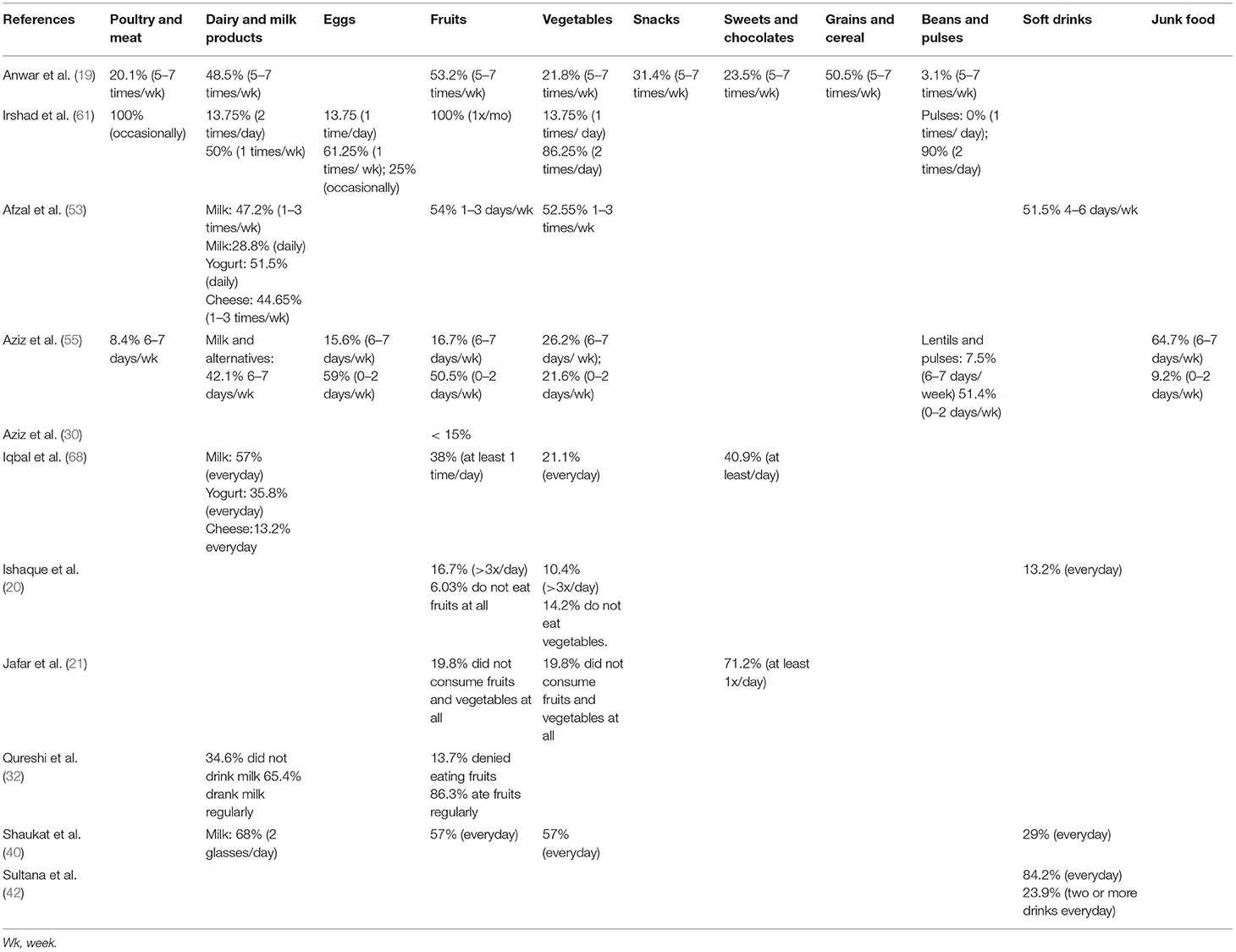
Table 5 . Dietary intake frequency.
In the present systematic review targeting 62,148 individuals, the limited evidence suggests the presence of DBM among school-going children and adolescents age 5 to 15 years. Our pooled analyses have found that approximately one-quarter of these children are underweight (25.1%), stunted (23%), wasted (24%); while 12.5% have thinness, 11.4% are overweight and 6.9% are obese. Dietary intake patterns in school-going children and adolescents aged 5–15 years show relatively high carbohydrate intake and low intake of protein-rich foods, compared to RDA, with suboptimal consumption of fruits and vegetables and increased intake of soft drinks and sweets/chocolates.
In the 1990s, using data on children <5 years of age, Pakistan was only dealing with a high prevalence of undernutrition. However, in the 2010s, this rhetoric changed and Pakistan emerged as a country facing DBM with >30% overweight prevalence ( 3 ). A similar transition was noted amongst countries within the lower quartile Gross Domestic Product (GDP) per capita purchasing power parity. This change has been associated with the concept of nutritional transition, which is about changes in the dietary patterns, physical activity, and tendency toward a sedentary lifestyle affecting body composition, fat distribution, and nutritional problems thereby leading to a rapid increase in overweight, obesity, and nutritional related non-communicable diseases ( 70 ). Pakistan has also been experiencing this nutritional transition with the rapid urbanization and change in diets. This trend is observed in our systematic review with children reporting an increased intake of carbohydrates, soft drinks, and sweets/chocolates.
The subgroup analysis ( Table 4 ) revealed a higher prevalence of undernutrition (underweight, stunting, and wasting), except thinness, amongst girls, while overweight, obesity, and thinness were higher amongst boys. This disparity highlights the issue of gender inequality which has been embedded in the Pakistani culture, with parents having a strong preference for sons, leading to girls being neglected ( 54 ). The National Nutrition Survey (NNS) 2018 of Pakistan, on the other hand, reports higher prevalence of underweight and obesity in adolescent boys and higher overweight prevalence in adolescent girls age 10–19 years ( 71 ). 78.4% of the studies were conducted in a school setting and according to Pakistan Annual Report 2016 by UNICEF, 22.6 million children age 5–16 years in Pakistan are out of school ( 72 ), hence, more data is needed from communities and rural areas to generalize trends of different anthropometric indices for children across Pakistan ( 71 ). Although this is a region-specific finding, even globally there is limited data on school-going children and early adolescents 5–15 years of age ( 6 ).
Higher undernutrition prevalence was also noted amongst children attending government schools, children from low socioeconomic backgrounds, and children living in rural areas. This could be attributed to poor living standards and food insecurity coupled with poor dietary practices amongst individuals living in poverty ( 26 ). The NNS 2018 survey reports 36.7% households in Pakistan to be facing food insecurity ( 71 ). A higher prevalence of overnutrition (overweight and obesity) was noted amongst children attending private schools, children from high socioeconomic backgrounds, and children living in urban areas. This trend is most likely due to the rapid urbanization and change in diet to higher consumption of carbohydrate rich foods, fast foods and carbonated/energy drinks with high sugar content along with a change to a more sedentary lifestyle.
Best 2010 conducted a review to assess the nutritional status of children age 5–12 years from Latin America, Africa, Asia, and the Eastern Mediterranean region and reported high underweight and thinness prevalence in South-East Asia and Africa while overweight prevalence was reported to be below 15% ( 73 ). In 2010, East Africa, the Pacific, and sub-Saharan Africa were reported to have a greater overweight prevalence (26.5 and 22.2%, respectively) than that of underweight (7.9 and 12.1%, respectively) ( 74 ). A cross-sectional study conducted in Lebanon also reported coexistence of under- and over-nutrition manifested as an overall prevalence of stunting to be 13.7% and overweight to be 7.2% amongst 153 5–14 years ( 75 ). On the other hand, a more recent analysis by Caleyachetty 2018 of data from global school-based student health surveys on children age 12–15 years from 57 LMICs and reported an overall 10.2% stunting prevalence, 5.5% thinness, and 21.4% overweight and obesity prevalence ( 76 ).
Dietary studies of school-aged children in Pakistan depict relatively high carbohydrate intake and low intake of protein-rich foods, fruits, and vegetables ( 46 , 57 , 77 , 78 ). The culture, myths, and misconceptions about dietary habits are different in every region and hence cannot be used to generalize this trend across Pakistan. Two studies have reported the highest carbohydrate intake amongst children from Quetta and Balochistan ( 41 , 55 ), however, more evidence is needed as not many studies have reported data specifically from these regions. There is a need to develop context-specific behavior change messages for school-aged children to encourage consumption of easily available, accessible, and affordable protein- and vitamin-rich foods such as lentils, seasonal fruits, and vegetables, as well as milk and its derivatives. An increase in consumption of a healthy, balanced diet will also help support the agrarian economy and encourage the utilization of local products to boost immunity and reduce chances of chronic diseases and, therefore, a reduction in the burden on the health sector ( 79 ).
Ochola 2014 conducted a systematic review on dietary intake habits of children age 6–12 years from different LMICs. They reported limited diversity and availability of food groups for children and reported children to have a higher intake of plant-based food sources, but an overall low fruit and vegetable intake and limited animal foods, thereby many being deficient in micronutrients. In Kuala Lumpur, 20% of school-going children and adolescents skipped at least one meal a day, with the most commonly skipped meal being breakfast (12.6%) while 32% of adolescents rarely consumed breakfast in Ghana. An increasing trend of processed and fast-food consumption was noted amongst children living in urban areas, with a greater preference for foods high in sugar, salt, and saturated fats. Ochola and Masibo ( 80 ) highlighted the need for nutrition education, not only for the school management, children, and parents but also the community at large, to spread awareness and sensitize the people about healthy eating habits ( 80 ).
The limitations identified in this review included that (i) studies used different tools and standards, such as the WHO or CDC criteria or did not specify, to categorize anthropometric indices, which led to lack of uniformity and possibility of over-or under-estimation of anthropometric measures, (ii) majority of the studies were conducted in urban setting with most of the data collected from the cities of Lahore and Karachi alone, (iii) majority of the studies had a sample size <500 ( n = 27), (iv) poor assessment of macro-and micronutrient consumption amongst children and (v) overall poor quality assessment of the included studies with 88.2% studies clearly specified and defined their population, while only 33.3% provided justification for sample size calculation with outcomes defined by 74.5% of the studies, no study had outcomes blinded to assessors and only 25.5% of the studies measured confounding variables and adjusted them statistically to assess associations to the outcomes. We could not measure publication bias for this review using SUMARI, as the estimates were proportions. It is recommended that good quality, large-scale cross-sectional surveys should be conducted for this age group especially in LMICs, along with micronutrient assessment as a component of future research for a better understanding of the problems and to help design specific programs to ameliorate the specific needs.
This systematic review identifies the burden of malnutrition and dietary patterns in school-going children and early adolescents from Pakistan and highlights the gaps that need to be addressed. Large-scale population-representative studies are still required, with standardized tools for anthropometry and dietary assessment. As the prevalence of DBM for school-going children and early adolescents age 5–15 years in other LMICs is not known, similar reviews from each region also need to be conducted. Such reviews will allow epidemiologists to first assess the availability of data in this age group, then identify their malnutrition trends, and thereby allow them to recognize the gaps and formulate interventions that can better tackle the issue of DBM in this age group globally. Notwithstanding, the need for more evidence; the recent review identifies the high burden of both under- nutrition and over- nutrition in this age group and the relevant mult-sectoral stakehlders should a take a note and plan for programs for this specific and very important age goup.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material , further inquiries can be directed to the corresponding author/s.
Author Contributions
DK and JD: formed the search strategy, identified relevant articles, extracted data, and analyzed it. They also conducted a quality assessment for all included studies. ZB and JD: conceptualized and designed this study. ZL: performed the analysis. ZB, JD, and ZL: guided other authors throughout the process. SZ, AS, MR, AD, and AK: reviewed, provided critical inputs, and revised the manuscript. All authors contributed to the article and approved the submitted version.
This systematic review was funded by SCANS consortium including the Trust for Vaccines & Immunizations (Pakistan) and the Aga Khan University (Karachi, Pakistan). The authors declare that this study also received funding from Mother & Child Care & Research Inc. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.739447/full#supplementary-material
Abbreviations
DBM, Double Burden of Malnutrition; LMIC, Low- and middle-income country; NWFP, North West Frontier Province; RDA, Recommended Daily Allowance.
1. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet . (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Hawkes C. Global Nutrition Report 2018. Shining a Light to Spur Action on Nutrition. 28–51 p. Available online at: https://globalnutritionreport.org/50bff8#section-2-1 (accessed January 28, 2021).
Google Scholar
3. Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. (2020) 395:65–74. doi: 10.1016/S0140-6736(19)32497-3
4. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet . (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
5. World Heal Organ. Obesity Overweight Factsheet From the WHO. Health 2018. World Heal Organ. (2018). Available online at: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed June 12, 2021).
6. Bundy DAP, de Silva N, Horton S, Patton GC, Schultz L, Jamison DT. Child and adolescent health and development. In: Disease Control Priorities, Third Edition (Volume 8): Child and Adolescent Health and Development. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK525240/ (accessed June 23, 2020).
7. World Health Organization Regional Office for South-East Asia. Adolescent nutrition: a review of the situation in selected South-East Asian Countries. World Health Organization, Regional Office for South-East Asia. (2006). Available online at: https://apps.who.int/iris/handle/10665/204764 (accessed January 28, 2021).
8. United Nation Children Fund (UNICEF),. The State of the World's Children 2011: Adolescence an age of Opportunity. UNICEF (2011). Available online at: https://data.unicef.org/resources/the-state-of-the-worlds-children-2011-adolescents-an-age-of-opportunity/ (accessed October 12, 2020).
9. Mandy M, Nyirenda M. Developmental origins of health and disease: the relevance to developing nations. Int Health. (2018) 10:66–70. doi: 10.1093/inthealth/ihy006
10. World Health Organization Regional Office for South-East Asia. Strategic Guidance on Accelerating Actions for Adolescent Health in South-East Asia Region 2018–2022. (2018). Available online at: https://apps.who.int/iris/bitstream/handle/10665/274312/9789290226475-eng.pdf (accessed July 02, 2021).
11. World Health Organization. Regional Office for South-East Asia. Adolescent Health in the South-East Asia Region . Available online at: https://www.who.int/southeastasia/health-topics/adolescent-health (accessed January 28, 2021).
12. Food Agric Organ. Nutritional Status Food Security. Food Agric Organ. (2007). Available online at: https://elearning.fao.org/course/view.php?id=189 (accessed October 12, 2020).
13. EndNote. Available online at: https://endnote.com (accessed June 13, 2020).
14. University of Cambridge. DAPA Measurement Toolkit. University of Cambridge (2015). Available online at: https://dapa-toolkit.mrc.ac.uk (accessed January 28, 2021).
15. Piper C. System for the Unified Management, Assessment, and Review of Information (SUMARI). J Med Libr Assoc. (2019) 107:634–6. doi: 10.5195/jmla.2019.790
16. U.S. Department of Health and Human Services. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Bethesda, MD: Natl Institutes Heal Dep Heal Hum Serv. (2014). Available online at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed February 28, 2021).
17. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med . (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
18. Ahmed J, Laghari a, Naseer M, Mehraj V. Prevalence of and factors associated with obesity among Pakistani schoolchildren: a school-based, cross-sectional study. East Mediterr Health J. (2013) 19:242–7. doi: 10.26719/2013.19.3.242
19. Anwar A, Anwar F, Joiya HU, Ijaz A, Rashid H, Javaid A, et al. Prevalence of obesity among the school-going children of lahore and associated factors. J Ayub Med Coll Abbottabad. (2010) 22:27–32. Available online at: https://pubmed.ncbi.nlm.nih.gov/22455255/
PubMed Abstract | Google Scholar
20. Ishaque A, Ahmad F, Zehra N, Amin H. Frequency of and factors leading to obesity and overweight in school children. J Ayub Med Coll Abbottabad. (2012) 24:34–8. Available online at: https://www.ayubmed.edu.pk/JAMC/24-2/Aiesha.pdf
21. Jafar TH, Hatcher J, Bhutta ZA. Rapidly rising rates of overweight and obesity coupled with persistently high rates of undernutrition among school aged children in an urban Indo-Asian population: Authors' response. Arch Dis Child. (2008) 93:1000–01. doi: 10.1136/adc.2007.125641
22. Kausar T, Naz A. Assessment of nutritional status of school going girls in Sargodha. Int J Food Nutr Sci. (2018) 5:81–5. Available online at: https://www.ommegaonline.org/article-details/Assessment-of-Nutritional-Status-of-School-Going-Girls-in-Sargodha/185
23. Khan K, Khanzada S, Qazi WA, Khalid S, Mawani A, Khalid F. Anthropometric measurement of primary school going children in Karachi. Int J Physiother. (2016) 3:214–7. doi: 10.15621/ijphy/2016/v3i2/94894
CrossRef Full Text | Google Scholar
24. Khan S, Abbas A, Ali I, Arshad R, Tareen MB, Shah MI. Prevalence of overweight and obesity and lifestyle assessment among school-going children of Multan, Pakistan. Isra Med J. (2019) 11:230–3. Available online at: http://www.imj.com.pk/wp-content/uploads/2019/10/7.-OA-634-Prevalence-of-overweight-and-obesity-and-lifestyle-assessment.pdf
25. Khan Z, Khan SA, Kumar R, Qureshi MA, Rehman R, Safdar RM. Behaviour towards healthy food among students of private schools in Quetta, Pakistan. Pakistan J Public Heal. (2015) 5:1–5. Available online at: https://www.researchgate.net/publication/281522127_Eating_behaviour_towards_healthy_food_among_students_of_Private_Schools_in_Quetta_Pakistan
26. Marwat ZI, Nawaz S, Wazir AK, Afzal E, Gul C, Khan MJ, et al. Nutritional assessment of school going children in district Abbottabad, K.P. Pakistan. Int J Sci Rep . (2019) 5:59–65. doi: 10.18203/issn.2454-2156.IntJSciRep20190253
27. Mian RMA, Ali M, Ferroni PA, Underwood P. The nutritional status of school-aged children in an urban squatter settlement in Pakistan. Pakistan J Nutr . (2002) 1:121–3. doi: 10.3923/pjn.2002.121.123
28. Mushtaq MU, Gull S, Abdullah HM, Shahid U, Shad MA, Akram J. Prevalence and socioeconomic correlates of overweight and obesity among Pakistani primary school children. BMC Public Health. (2011) 11:724. doi: 10.1186/1471-2458-11-724
29. Mushtaq M, Gull S, Khurshid U, Shahid U, Ma S, Am S. Prevalence and socio-demographic correlates of stunting and thinness among Pakistani primary school children. BMC Public Health . (2011) 11:790. doi: 10.1186/1471-2458-11-790
30. Aziz S, Noorulain W, Zaidi UER, Hossain K, Siddiqui IA. Prevalence of overweight and obesity among children and adolescents of affluent schools in Karachi. J Pak Med Assoc. (2009) 59:35–8. Available online at: https://pubmed.ncbi.nlm.nih.gov/19213375/
31. Mushtaq MU, Gull S, Mushtaq K, Shahid U, Shad MA, Akram J. Dietary behaviors, physical activity and sedentary lifestyle associated with overweight and obesity, and their socio-demographic correlates, among Pakistani primary school children. Int J Behav Nutr Phys Act . (2011) 8:130. doi: 10.1186/1479-5868-8-130
32. Qureshi MF, Rathore A, Seerani N, Qureshi S, Faisal B, Kumar R. Nutritional status among primary school going children living in urban area of Sindh, Pakistan. Pakistan J Public Heal. (1970) 7:62–5. doi: 10.32413/pjph.v7i1.27
33. Rahman AJ, Qamar FN, Ashraf S, Khowaja ZA, Tariq SB, Naeem H. Prevalence of hypertension in healthy school children in Pakistan and its relationship with body mass index, proteinuria and hematuria. Saudi J Kidney Dis Transplant. (2013) 24:408–12. doi: 10.4103/1319-2442.109619
34. Rehman ZU, Ishtiaq M, Naeem M, Gul R, Amjad M, et al. Prevalence of malnutrition among school going children of university campus Peshawar. J Saidu Med Coll Swat. (2013) 4:434–7. doi: 10.52206/jsmc.2014.4.1.434-437
35. Ramzan M, Ali I, Ramzan F, Ramzan F. Nutritional status of affluent school children of Dera Ismail Khan: Is under nutrition common. Pakistan J Nutr. (2010) 9:1002–5. doi: 10.3923/pjn.2010.1002.1005
36. Rizwan A, Akhter J, Jafar TH. The association of sugar-sweetened beverage consumption and inadequate physical activity with overweight and obesity in school-going children and adolescents in Pakistan. Arch Dis Child. (2011) 96:109–11. doi: 10.1136/adc.2010.193383
37. Sadiq S, M F, Farooq L, Mohammad D, Lakhani M, et al. Reference percentile for height, weight and BMI among children/adolescents of Karachi, Pakistan. Integr Res J . (2019) 4:90–6. Available online at: https://www.researchgate.net/publication/337818529_Reference_percentile_for_height_weight_and_BMI_among_childrenadolescents_of_Karachi_Pakistan
38. Shahid A, Ramzan A, Mustufa MA, Nasim S, Pirzada AG, Memon A. Blood pressure, Body Mass Index and Waist circumference of school going children of Karachi. Pakistan J Med Res Pak J Med Res. (2010) 49:116–20. Available online at: https://www.researchgate.net/publication/216022160_Blood_Pressure_Body_Mass_Index_and_Waist_Circumference_of_School_going_Children_of_Karachi
39. Shahid B, Jalal MA, Waseem M, Shahid H, Mehboob-ur-Rehman M. Prevalence of obesity in school going adolescents and its association with hypertension. Pakistan J Med Heal Sci. (2017) 11:1082–4. Available online at: https://www.pjmhsonline.com/2017/july_sep/pdf/1082.pdf
40. Shaukat F, Ahmad F, Zehra N. Association of bmi and life style: a comparative study on school going children (Aged 6-16 Years) of Lahore. Annals. (2013) 19:297–304. Available online at: https://www.annalskemu.org/journal/index.php/annals/article/viewFile/531/393
41. Aziz S, Noorulain W, Majid R, Hosain K, Siddiqui IA, et al. Dietary pattern, height, weight centile and BMI of affluent school children and adolescents from three major cities of Pakistan. J Coll Phys Surg Pakistan. (2010) 20:10–16. Available online at: https://pubmed.ncbi.nlm.nih.gov/20141686/
42. Sultana F, Abdullah Z, Farrukh Z. Magnitude of obesity and its contributory factors in school going children of affluent families of Rawalpindi and Islamabad, Pakistan. J Rehman Med Inst. (2017) 3:25–8. Available online at: http://jrmi.pk/article/view/103
43. Warraich HJ, Javed F, Faraz-ul-Haq M, Khawaja FB, Saleem S. Prevalence of obesity in school-going children of Karachi. PLoS One. (2009) 4:e4816. doi: 10.1371/journal.pone.0004816
44. Zahid S, Masood Z, Fayyaz R, Itrat N, Hussain SJ. Assessment of nutritional status of school children in public and private sector schools by anthropometry. J Univ Med Dent Coll. (2017) 8:52–61. Available online at: https://www.jumdc.com/index.php/jumdc/article/view/155
45. Zainab S, Kadir M. Nutritional status and physical abuse among the children involved in domestic labour in Karachi Pakistan: a cross-sectional survey. J Pak Med Assoc . (2016) 66:1243–8. Available online at: https://pubmed.ncbi.nlm.nih.gov/27686297/
46. Zaman R, Iqbal Z, Ali U. Dietary intakes of urban adolescents of sialkot, Pakistan do not meet the standards of adequacy. Pakistan J Nutr. (2013) 12:460–7. doi: 10.3923/pjn.2013.460.467
47. Hall A, Kirby H. The numbers, educational status and health of enrolled and non-enrolled school-age children in the Allai Valley, Northwest Frontier Province, Pakistan. Soc Sci Med. (2010) 70:1131–40. doi: 10.1016/j.socscimed.2009.12.021
48. ul Haq I, Siddiqui TS, Jan MA. Prevalence of obesity in school children of Hazara division. J Ayub Med Coll Abbottabad. (2010) 22:50–2. Available online at: https://pubmed.ncbi.nlm.nih.gov/22455260/
49. Khuwaja S, Selwyn BJ, Shah SM. Prevalence and correlates of stunting among primary school children in rural areas of southern Pakistan. J Trop Pediatr. (2005) 51:72–7. doi: 10.1093/tropej/fmh067
50. Mohsin SN, Fatima M, Aasim M, Ghous R. Comparison of nutritional status among, flood affected and unaffected school aged children. Pakistan J Med Res Pak J Med Res. (2017) 56:39–43. Available online at: https://www.researchgate.net/publication/318686514_Comparison_of_the_Nutritional_Status_among_Flood_Affected_and_Unaffected_School_Aged_Children
51. Mustufa MA, Jamali AK, Sameen I, Burfat FM, Baloch MY, Baloch AH, et al. Malnutrition and poor oral health status are major risks among primary school children at Lasbela, Balochistan, Pakistan. J Health Popul Nutr. (2017) 36:17. doi: 10.1186/s41043-017-0100-6
52. Babar NF, Muzaffar R, Khan MA, Imdad S. IImpact of socioeconomic factors on nutritional status in primary school children. J Ayub Med Coll Abbottabad. (2010) 22:15–18. Available online at: https://pubmed.ncbi.nlm.nih.gov/22455252/
53. Afzal N, Khan AU, Iqbal MA, Tahir S khan. Nutritional status, dietary practices and physical activities among female adolescents: a cross sectional study in district Okara, Pakistan. J Nutr Food Sci. (2018) 8:8–11. doi: 10.4172/2155-9600.1000650
54. Anwer I, Awan JA. Nutritional status comparison of rural with urban school children in Faisalabad District, Pakistan. Rural Remote Health. (2003) 3:130. doi: 10.22605/RRH130
55. Aziz A, Pervaiz M, Khalid A, Khan AZ, Rafique G. Dietary practices of school children in Sindh, Pakistan. Nutr Health. (2018) 24:231–40. doi: 10.1177/0260106018791859
56. Aziz S, Noor-ul-ain W, Majeed R, Khan MA, Qayum I, Ahmed I, et al. Growth centile charts (anthropometric measurement) of Pakistani pediatric population. J Pakistan Med Assoc. (2012) 62:367–77. Available online at: https://pubmed.ncbi.nlm.nih.gov/22755283/
57. Aziz S, Hosain K. Carbohydrate (CHO), Protein and fat intake of healthy Pakistani school children in a 24 hour period. J Pak Med Assoc. (2014) 64:1255–9. Available online at: https://pubmed.ncbi.nlm.nih.gov/25831641/
58. Ponum M, Khan S, Hasan O, Mahmood MT, Abbas A, Iftikhar M, et al. Stunting diagnostic and awareness: impact assessment study of sociodemographic factors of stunting among school-going children of Pakistan. BMC Pediatr. (2020) 20:232. doi: 10.1186/s12887-020-02139-0
59. Akbar NF, Lodhi A, Mahmood S, Mueen-ud-Din G, Murtaza MA. Nutritional status of school going children in relation to their dietary intake at mid-morning. Pak J Nutr . (2015) 14:150–4. doi: 10.3923/pjn.2015.150.154
60. Iqbal M, Fatmi Z, Khan K, Jumani Y, Amjad N, Nafees A. Malnutrition and food insecurity in child labourers in Sindh, Pakistan: a cross-sectional study. East Mediterr Heal J. (2020) 26:1087–1096. doi: 10.26719/emhj.20.040
61. Irshad R, Khan A, Mustafa A, Farooq U. Nutritional assessment focusing on women and children in palas valley-kohistan. J Ayub Med Coll Abbottabad. (2018) 30:258–63. Available online at: https://pubmed.ncbi.nlm.nih.gov/29938431/
62. Riaz R, Sultana A, Hameed S, Tehseen I, Sabir SA. Nutritional status of school going children. J Rawalpindi Med Coll. (2010) 14:51–4. Available online at: https://www.journalrmc.com/jrmc/volumes/1394531627.pdf
63. Basit A, Hakeem R, Hydrie MZI, Ahmedani MY, Masood Q. Relationship among fatness, blood lipids, and insulin resistance in Pakistani children. J Heal Popul Nutr. (2005) 23:34–43. Available online at: https://pubmed.ncbi.nlm.nih.gov/15884750/
64. Siddique S, Ayub M, Shore N, Tariq U, Zaman S. Nutritional status of primary school children in Abbottabad. J Ayub Med Coll Abbottabad. (2013) 25:123–6. Available online at: https://pubmed.ncbi.nlm.nih.gov/25098074/
65. Batool S, Shaheen A, Rehman R, Qamar S, Raza SMA, Jabeen R, et al. To assess the nutritional status of primary school children in an urban school of faisalabad. Pakistan J Med Heal Sci. (2012) 6:776–9. Available online at: https://www.pjmhsonline.com/2012/july_sep/pdf/776%20%20%20To%20Assess%20the%20Nutritional%20Status%20of%20Primary%20School%20Children%20in%20an%20Urban%20School%20of%20Faisalabad.pdf
66. Fatima F, Hafeez A, Yaqoob A. Nutritional assessment of adolescent girls living in Cherah union council. J Pak Med Assoc. (2014) 64:1220–4. Available online at: https://pubmed.ncbi.nlm.nih.gov/25831634/
67. Hayyat MU. Assessing the nexus of fast food consumption and childhood obesity in Lahore Metropolitan City of Pakistan. Int J Biosci . (2019) 14:95–102. doi: 10.12692/ijb/14.4.95-102
68. Iqbal TA, Maiken ZH, Bajwa SG, Malik SN, Qazi W. Nutritional imbalance and physical activity, a comparison among students belonging to different socioeconomic status in metropolitan city of Pakistan. Pakistan J Public Heal. (2017) 7:146–52. doi: 10.32413/pjph.v7i3.67
69. Melinda MM. Exercise and the Institute of Medicine recommendations for nutrition. Curr Sports Med Rep. (2005) 4:193–8. doi: 10.1097/01.CSMR.0000306206.72186.00
70. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. (2012) 70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x
71. Government of Pakistan & UNICEF. National Nutrition Survey 2018: Key Finding Report. Gov Pakistan UNICEF Pakistan. (2018). Available online at: https://www.unicef.org/pakistan/reports/national-nutrition-survey-2018-key-findings-report (accessed October 12, 2020).
72. UNICEF. Pakistan Annual Report 2016. (2016). Available online at: https://www.unicef.org/pakistan/reports/annual-report-2016 (accessed February 28, 2021).
73. Best C, Neufingerl N, van Geel L, van den Briel T, Osendarp S. The nutritional status of school-aged children: why should we care? Food Nutr Bull. (2010) 31:400–17. doi: 10.1177/156482651003100303
74. Winichagoon P, Margetts B. The double burden of malnutrition in low- and middle-income countries. Int Agency Res Cancer. (2017). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK565820/
75. El-Kassas G, Ziade F. The dual burden of malnutrition and associated dietary and lifestyle habits among lebanese school age children living in orphanages in North Lebanon. J Nutr Metab. (2017) 2017:1–12. doi: 10.1155/2017/4863431
76. Caleyachetty R, Thomas GN, Kengne AP, Echouffo-Tcheugui JB, Schilsky S, Khodabocus J, et al. The double burden of malnutrition among adolescents: analysis of data from the Global School-Based Student Health and Health Behavior in School-Aged Children surveys in 57 low- and middle-income countries. Am J Clin Nutr. (2018) 108:414–24. doi: 10.1093/ajcn/nqy105
77. Jafar TH, Qadri Z, Islam M, Hatcher J, Bhutta ZA, Chaturvedi N. Rise in childhood obesity with persistently high rates of undernutrition among urban school-aged Indo-Asian children. Arch Dis Child. (2008) 93:373–8.
78. Mahmood R, Khan R, Saleem S. Association of anaemia with dietary practices in adolescent girls. Pakistan J Physiol. (2018) 14:41–45. Available online at: http://www.pps.org.pk/PJP/14-3/Rabia.pdf
79. Government of Pakistan. National Food Security Policy. Available online at: http://mnfsr.gov.pk/userfiles1/file/NationalFoodSecurityPolicy2018(1).pdf (accessed October 12, 2021).
80. Ochola S, Masibo PK. Dietary intake of schoolchildren and adolescents in developing countries. Ann Nutr Metab. (2014) 64:24–40. doi: 10.1159/000365125
Keywords: malnutrition, dietary intake, school-going children, adolescents, double burden of malnutrition
Citation: Khan DSA, Das JK, Zareen S, Lassi ZS, Salman A, Raashid M, Dero AA, Khanzada A and Bhutta ZA (2022) Nutritional Status and Dietary Intake of School-Age Children and Early Adolescents: Systematic Review in a Developing Country and Lessons for the Global Perspective. Front. Nutr. 8:739447. doi: 10.3389/fnut.2021.739447
Received: 11 July 2021; Accepted: 23 December 2021; Published: 02 February 2022.
Reviewed by:
Copyright © 2022 Khan, Das, Zareen, Lassi, Salman, Raashid, Dero, Khanzada and Bhutta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zulfiqar A. Bhutta, zulfiqar.bhutta@sickkids.ca
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Research gaps and opportunities in precision nutrition: an NIH workshop report
Affiliations.
- 1 Health Policy and Management, City University of New York Graduate School of Public Health and Health Policy, New York, NY, USA.
- 2 USDA-Human Nutrition Research Center on Aging at Tufts University, Boston, MA, USA.
- 3 Nutrition and Exercise Physiology, University of Missouri School of Medicine, MO, USA.
- 4 Public Health, University of California, San Diego, San Diego, CA, USA.
- 5 Network Science Institute and Department of Physics, Northeastern University, Boston, MA, USA.
- 6 The Ohio State University, Columbus, OH, USA.
- 7 Keck School of Medicine, University of Southern California, Los Angeles, CA, USA.
- 8 Allied Health Sciences, University of Connecticut, Storrs, CT, USA.
- 9 Novo Nordisk Foundation, Hellerup, Denmark, Copenhagen, Denmark, and Lund University Diabetes Center, Sweden.
- 10 The Lund University Diabetes Center, Malmo, SwedenInsert Affiliation Text Here.
- 11 National Institutes of Health, Office of Behavioral and Social Sciences Research, Bethesda, MD, USA.
- 12 Computer Science, Northwestern University McCormick School of Engineering, IL, USA.
- 13 Department of Medicine, The University of Chicago, Chicago, IL, USA.
- 14 Epidemiology and Clinical Research, Stanford University, Stanford, CA, USA.
- 15 Public Health and Human Sciences, Linus Pauling Institute, Oregon State University, Corvallis, OR, USA.
- 16 Information Sciences Institute, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, USA.
- 17 Neurology, Weill Cornell Medical College, New York, NY, USA.
- 18 HealthPartners Institute, Bloomington, MN, USA.
- 19 Rory Meyers College of Nursing, New York University, New York, NY, USA.
- 20 Ingestive Behavior Laboratory, Pennington Biomedical Research Center, Baton Rouge, LA, USA.
- 21 Nutrition, Harvard TH Chan School of Public Health, Boston, MA, USA.
- 22 Epidemiology and Population Health, Stanford University, Stanford, CA, USA.
- 23 Fred Hutchinson Cancer Center, Seattle, WA, USA.
- 24 Grossman School of Medicine, New York University, New York, NY, USA.
- 25 UCD Conway Institute, School of Public Health, Physiotherapy, and Sports Science, University College Dublin, Dublin, Ireland.
- 26 Johns Hopkins University, Baltimore, MD, USA.
- 27 Brigham and Women's Hospital, Boston, MA, USA.
- 28 Medicine and Neurology, Harvard Medical School, Boston, MA, USA.
- 29 Computer Science and Applied Math, Weizmann Institute of Science, Rehovot, Israel.
- 30 Twin Research and Genetic Epidemiology, King's College London, London, United Kingdom.
- 31 Preventive Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL, USA.
- 32 Kinesiology and Nutrition, University of Illinois at Chicago, Chicago, IL, USA.
- 33 Nutrition and Nutrition Research Institute, Gillings School of Public Health, The University of North Carolina, Chapel Hill, NC, USA.
- PMID: 36055772
- PMCID: PMC9761773
- DOI: 10.1093/ajcn/nqac237
Precision nutrition is an emerging concept that aims to develop nutrition recommendations tailored to different people's circumstances and biological characteristics. Responses to dietary change and the resulting health outcomes from consuming different diets may vary significantly between people based on interactions between their genetic backgrounds, physiology, microbiome, underlying health status, behaviors, social influences, and environmental exposures. On 11-12 January 2021, the National Institutes of Health convened a workshop entitled "Precision Nutrition: Research Gaps and Opportunities" to bring together experts to discuss the issues involved in better understanding and addressing precision nutrition. The workshop proceeded in 3 parts: part I covered many aspects of genetics and physiology that mediate the links between nutrient intake and health conditions such as cardiovascular disease, Alzheimer disease, and cancer; part II reviewed potential contributors to interindividual variability in dietary exposures and responses such as baseline nutritional status, circadian rhythm/sleep, environmental exposures, sensory properties of food, stress, inflammation, and the social determinants of health; part III presented the need for systems approaches, with new methods and technologies that can facilitate the study and implementation of precision nutrition, and workforce development needed to create a new generation of researchers. The workshop concluded that much research will be needed before more precise nutrition recommendations can be achieved. This includes better understanding and accounting for variables such as age, sex, ethnicity, medical history, genetics, and social and environmental factors. The advent of new methods and technologies and the availability of considerably more data bring tremendous opportunity. However, the field must proceed with appropriate levels of caution and make sure the factors listed above are all considered, and systems approaches and methods are incorporated. It will be important to develop and train an expanded workforce with the goal of reducing health disparities and improving precision nutritional advice for all Americans.
Keywords: data science; food; genomics; nutrigenomics; precision nutrition.
© The Author(s) 2022. Published by Oxford University Press on behalf of the American Society for Nutrition.
PubMed Disclaimer
Precision nutrition. Factors associated with…
Precision nutrition. Factors associated with interindividual variability in responses to diet.
How a systems approach can…
How a systems approach can utilize technology to iteratively better understand complex systems.…
Similar articles
- Precision nutrition for prevention and management of type 2 diabetes. Wang DD, Hu FB. Wang DD, et al. Lancet Diabetes Endocrinol. 2018 May;6(5):416-426. doi: 10.1016/S2213-8587(18)30037-8. Epub 2018 Feb 9. Lancet Diabetes Endocrinol. 2018. PMID: 29433995 Review.
- Precision Nutrition: A Review of Personalized Nutritional Approaches for the Prevention and Management of Metabolic Syndrome. de Toro-Martín J, Arsenault BJ, Després JP, Vohl MC. de Toro-Martín J, et al. Nutrients. 2017 Aug 22;9(8):913. doi: 10.3390/nu9080913. Nutrients. 2017. PMID: 28829397 Free PMC article. Review.
- Precision (Personalized) Nutrition: Understanding Metabolic Heterogeneity. Zeisel SH. Zeisel SH. Annu Rev Food Sci Technol. 2020 Mar 25;11:71-92. doi: 10.1146/annurev-food-032519-051736. Epub 2020 Jan 13. Annu Rev Food Sci Technol. 2020. PMID: 31928426 Review.
- Precision Nutrition 4.0: A Big Data and Ethics Foresight Analysis--Convergence of Agrigenomics, Nutrigenomics, Nutriproteomics, and Nutrimetabolomics. Özdemir V, Kolker E. Özdemir V, et al. OMICS. 2016 Feb;20(2):69-75. doi: 10.1089/omi.2015.0193. Epub 2016 Jan 19. OMICS. 2016. PMID: 26785082
- Opportunities to advance implementation science and nutrition research: a commentary on the Strategic Plan for NIH Nutrition Research. Nicastro HL, Vorkoper S, Sterling R, Korn AR, Brown AGM, Maruvada P, Oh AY. Nicastro HL, et al. Transl Behav Med. 2023 Jan 20;13(1):1-6. doi: 10.1093/tbm/ibac066. Transl Behav Med. 2023. PMID: 36370119 Free PMC article.
- Western diets and chronic diseases. Adolph TE, Tilg H. Adolph TE, et al. Nat Med. 2024 Jul 31. doi: 10.1038/s41591-024-03165-6. Online ahead of print. Nat Med. 2024. PMID: 39085420 Review.
- Contribution of Nucleotide-Binding Oligomerization Domain-like (NOD) Receptors to the Immune and Metabolic Health. Apaza CJ, Días M, García Tejedor A, Boscá L, Laparra Llopis JM. Apaza CJ, et al. Biomedicines. 2024 Feb 1;12(2):341. doi: 10.3390/biomedicines12020341. Biomedicines. 2024. PMID: 38397943 Free PMC article. Review.
- Emerging mechanisms of obesity-associated immune dysfunction. Shaikh SR, Beck MA, Alwarawrah Y, MacIver NJ. Shaikh SR, et al. Nat Rev Endocrinol. 2024 Mar;20(3):136-148. doi: 10.1038/s41574-023-00932-2. Epub 2023 Dec 21. Nat Rev Endocrinol. 2024. PMID: 38129700 Review.
- Precision Nutrition: The Hype Is Exceeding the Science and Evidentiary Standards Needed to Inform Public Health Recommendations for Prevention of Chronic Disease. Bailey RL, Stover PJ. Bailey RL, et al. Annu Rev Nutr. 2023 Aug 21;43:385-407. doi: 10.1146/annurev-nutr-061021-025153. Annu Rev Nutr. 2023. PMID: 37603433 Free PMC article. Review.
- Perspective: Challenges and Future Directions in Clinical Research with Nuts and Berries. Zuelch ML, Radtke MD, Holt RR, Basu A, Burton-Freeman B, Ferruzzi MG, Li Z, Shay NF, Shukitt-Hale B, Keen CL, Steinberg FM, Hackman RM. Zuelch ML, et al. Adv Nutr. 2023 Sep;14(5):1005-1028. doi: 10.1016/j.advnut.2023.07.010. Epub 2023 Aug 2. Adv Nutr. 2023. PMID: 37536565 Free PMC article.
- US Burden of Disease Collaborators, Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany Eet al. . The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–72. - PMC - PubMed
- Phillips JA. Dietary guidelines for Americans, 2020–2025. Workplace Health Safety. 2021;69(8):395. - PubMed
- Maruvada P, Lampe JW, Wishart DS, Barupal D, Chester DN, Dodd Det al. . Perspective: dietary biomarkers of intake and exposure—exploration with omics approaches. Adv Nutr. 2020;11(2):200–15. - PMC - PubMed
- Lewontin R. The genetics of human diversity. New York (NY): Freeman Press; 1980.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review the Process to Update the Dietary Guidelines for Americans . Redesigning the process for establishing the Dietary Guidelines for Americans. Washington (DC): National Academies Press (US); 2017. Available from: https://www.ncbi.nlm.nih.gov/books/NBK469837/ - DOI - PubMed
Publication types
- Search in MeSH
Related information
- Cited in Books
Grants and funding
- F32 HD008686/HD/NICHD NIH HHS/United States
- U54 TR004279/TR/NCATS NIH HHS/United States
- 5T32HL151323-02/HL/NHLBI NIH HHS/United States
- T32 HL151323/HL/NHLBI NIH HHS/United States
LinkOut - more resources
Full text sources.
- Elsevier Science
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
- Silverchair Information Systems

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 10 August 2024
Changes in nutritional status and associations with physical and clinical outcomes in acute myeloid leukemia patients during intensive chemotherapy
- Rianne van Lieshout ORCID: orcid.org/0000-0002-1456-7820 1 ,
- Lidwine W. Tick 2 ,
- Erik A. M. Beckers 3 ,
- Willemijn Biesbroek 4 ,
- Jeanne P. Dieleman 5 ,
- Myrthe Dijkstra 6 ,
- Wanda Groenesteijn 7 ,
- Harry R. Koene 8 ,
- Suzanne Kranenburg 9 ,
- Debbie van der Lee 1 ,
- Liesbeth van der Put - van den Berg 9 ,
- Nicky Rademakers 10 ,
- Josien C. Regelink 11 ,
- Claudia J. van Tilborg 12 ,
- Peter E. Westerweel 12 ,
- Sandra de Zeeuw 12 ,
- Harry C. Schouten 3 &
- Sandra Beijer 13 , 14
European Journal of Clinical Nutrition ( 2024 ) Cite this article
20 Accesses
Metrics details
- Malnutrition
Background/Objectives
Patients with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) often receive medical nutrition therapy (MNT) during intensive remission-induction treatment. Since little is known about changes in nutritional status, specifically body composition, in this patient population, these changes and their associations with physical and clinical outcomes were assessed.
Subjects/Methods
In this multicenter prospective observational study, newly diagnosed AML/MDS patients who received intensive remission-induction chemotherapy, routine dietary counseling by a dietician and MNT immediately upon inadequate nutritional intake, were included. At treatment initiation and discharge, nutritional status, including Patient-Generated Subjective Global Assessment (PG-SGA)-scores and body composition, physical outcomes and fatigue were assessed. Associations of nutritional status/body composition with physical outcomes, fatigue, fever duration, number of complications, time to neutrophil engraftment and hospital length of stay (LOS) (collected from medical records) were examined using multiple regression analysis.
In >91% of the 126 AML/MDS patients included, nutritional intake was adequate, with 61% receiving MNT. Nevertheless, body weight decreased significantly ( p < 0.001) and mainly consisted of a loss of muscle/fat-free mass (FFM) ( p < 0.001), while fat mass (FM) remained unchanged ( p -value range = 0.71–0.77). Body weight and waist circumference showed significant negative associations with fever duration and/or number of complications. Significant positive associations were found between mid-upper arm muscle circumference (MUAMC) and physical functioning and between PG-SGA-scores and fatigue. Body weight and MUAMC were also negatively associated with LOS.
Despite MNT in AML/MDS patients undergoing intensive chemotherapy, muscle/FFM decreased while FM remained unchanged. Maintenance of nutritional status was associated with improved physical and clinical outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Increases in adipose tissue and muscle function are longitudinally associated with better quality of life in colorectal cancer survivors
Body weight, body composition and survival after 1 year: follow-up of a nutritional intervention trial in allo-HSCT recipients
Improving nutritional status after allogeneic stem cell transplantation: results of phase 2 ALLONUT clinical trial
Data availability.
Data analyzed in this study are available from the corresponding author on reasonable request.
Comprehensive Cancer Center the Netherlands. The Netherlands Cancer Registry 2023. www.iknl.nl/nkr-cijfers . Accessed February 21, 2024.
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140:1200–28.
Article PubMed PubMed Central CAS Google Scholar
The Hemato Oncology Foundation for Adults in The Netherlands (HOVON), Leukemia Working Group. Treatment guideline AML (Dutch only). 2021. https://hovon.nl/en/treatment-guidelines/leukemia . Accessed February 21, 2024.
Walrath M, Bacon C, Foley S, Fung HC. Gastrointestinal side effects and adequacy of enteral intake in hematopoietic stem cell transplant patients. Nutr Clin Pr. 2015;30:305–10.
Article Google Scholar
Baumgartner A, Bargetzi A, Zueger N, Bargetzi M, Medinger M, Bounoure L, et al. Revisiting nutritional support for allogeneic hematologic stem cell transplantation-a systematic review. Bone Marrow Transpl. 2017;52:506–13.
Article CAS Google Scholar
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11–48.
Article PubMed Google Scholar
Campelj DG, Timpani CA, Rybalka E. Cachectic muscle wasting in acute myeloid leukaemia: a sleeping giant with dire clinical consequences. J Cachexia Sarcopenia Muscle. 2022;13:42–54.
Nakamura N, Ninomiya S, Matsumoto T, Nakamura H, Kitagawa J, Shiraki M, et al. Prognostic impact of skeletal muscle assessed by computed tomography in patients with acute myeloid leukemia. Ann Hematol. 2019;98:351–9.
Ando T, Fujisawa S, Teshigawara H, Ogusa E, Ishii Y, Miyashita K, et al. Impact of treatment-related weight changes from diagnosis to hematopoietic stem-cell transplantation on clinical outcome of acute myeloid leukemia. Int J Hematol. 2019;109:673–83.
Jung J, Lee E, Shim H, Park JH, Eom HS, Lee H. Prediction of clinical outcomes through assessment of sarcopenia and adipopenia using computed tomography in adult patients with acute myeloid leukemia. Int J Hematol. 2021;114:44–52.
Article PubMed CAS Google Scholar
Brauer D, Backhaus D, Pointner R, Vucinic V, Niederwieser D, Platzbecker U, et al. Nutritional Status at Diagnosis and Pre-transplant Weight Loss Impact Outcomes of Acute Myeloid Leukemia Patients Following Allogeneic Stem Cell Transplantation. Hemasphere. 2021;5:e532.
Article PubMed PubMed Central Google Scholar
Baumgartner A, Zueger N, Bargetzi A, Medinger M, Passweg JR, Stanga Z, et al. Association of Nutritional Parameters with Clinical Outcomes in Patients with Acute Myeloid Leukemia Undergoing Haematopoietic Stem Cell Transplantation. Ann Nutr Metab. 2016;69:89–98.
Horsley P, Bauer J, Gallagher B. Poor nutritional status prior to peripheral blood stem cell transplantation is associated with increased length of hospital stay. Bone Marrow Transpl. 2005;35:1113–6.
Morishita S, Kaida K, Tanaka T, Itani Y, Ikegame K, Okada M, et al. Prevalence of sarcopenia and relevance of body composition, physiological function, fatigue, and health-related quality of life in patients before allogeneic hematopoietic stem cell transplantation. Support Care Cancer. 2012;20:3161–8.
Anderson LJ, Yin C, Burciaga R, Lee J, Crabtree S, Migula D, et al. Assessing Cachexia Acutely after Autologous Stem Cell Transplant. Cancers. 2019;11:1300.
Qin Z, Lu K, Jiang T, Wang M, Weng Y, Tang X, et al. Evaluating Sarcopenia by Using the Bioelectrical Impedance Analysis in Patients with Acute Myeloid Leukemia After Chemotherapy. Int J Gen Med. 2022;15:1261–9.
van Lieshout R, Tick LW, Dieleman JP, Custers S, van Dongen MS, van der Lee D, et al. Changes in body weight and serum liver tests associated with parenteral nutrition compared with no parenteral nutrition in patients with acute myeloid leukemia during remission induction treatment. Support Care Cancer. 2020;28:4381–93.
Deluche E, Girault S, Jesus P, Monzat S, Turlure P, Leobon S, et al. Assessment of the nutritional status of adult patients with acute myeloid leukemia during induction chemotherapy. Nutrition. 2017;41:120–5.
Iversen PO, Ukrainchenko E, Afanasyev B, Hulbekkmo K, Choukah A, Gulbrandsen N, et al. Impaired nutritional status during intensive chemotherapy in Russian and Norwegian cohorts with acute myeloid leukemia. Leuk Lymphoma. 2008;49:1916–24.
Eriksson KM, Cederholm T, Palmblad JE. Nutrition and acute leukemia in adults: relation between nutritional status and infectious complications during remission induction. Cancer. 1998;82:1071–7.
Cederholm T, Eriksson K, Palmblad J. Nutrition and acute leukemia in adults: relation to remission rate and survival. Haematol. 2002;32:405–17.
Google Scholar
Esfahani A, Ghoreishi Z, Abedi Miran M, Sanaat Z, Ostadrahimi A, Eivazi Ziaei J, et al. Nutritional assessment of patients with acute leukemia during induction chemotherapy: association with hospital outcomes. Leuk Lymphoma. 2014;55:1743–50.
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9.
Baumgartner A, Schuetz P. Nutritional Support. In: Carreras E, Dufour C, Mohty M, Kroger N, editors. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies [ https://www.ebmt.org/education/ebmt-handbook ]. Cham (CH): Springer; 2019. Chapter 24, p. 171–6.
Charlson ME, Carrozzino D, Guidi J, Patierno C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother Psychosom. 2022;91:8–35.
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Pt-Global, Innovation in nutritional care. Patient-Generated Subjective Global Assessment (PG-SGA). Standard Operating Procedure and link to relevant literature on the PG-SGA, including: Jager-Wittenaar H, Ottery FD. Assessing nutritional status in cancer: role of the Patient-Generated Subjective Global Assessment. Curr Opin Clin Nutr Metab Care. 2017;20:322–9. https://pt-global.org/ .
World Health Organisation BMI Categories. 2010. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi . Accessed February 21, 2024.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM, et al. Bioelectrical impedance analysis-part I: review of principles and methods. Clin Nutr. 2004;23:1226–43.
Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C. Single prediction equation for bioelectrical impedance analysis in adults aged 20-94 years. Nutrition. 2001;17:248–53.
Frisancho AR. New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr. 1981;34:2540–5.
Landi F, Russo A, Liperoti R, Pahor M, Tosato M, Capoluongo E, et al. Midarm muscle circumference, physical performance and mortality: results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Clin Nutr. 2010;29:441–7.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177–89.
Gonzalez MC, Mehrnezhad A, Razaviarab N, Barbosa-Silva TG, Heymsfield SB. Calf circumference: cutoff values from the NHANES 1999-2006. Am J Clin Nutr. 2021;113:1679–87.
Thompson E, Subar AF. Dietary Assessment Methodology. In: Coulston AM, Boushey CJ, Ferruzzi MG, Delahanty LM, editors. Nutrition in the Prevention and Treatment of Disease 4th ed. London: Elsevier Inc.; 2017. p. 5–44.
Kruizenga HM, Hofsteenge GH, Weijs PJ. Predicting resting energy expenditure in underweight, normal weight, overweight, and obese adult hospital patients. Nutr Metab. 2016;13:85.
Weijs PJ, Sauerwein HP, Kondrup J. Protein recommendations in the ICU: g protein/kg body weight - which body weight for underweight and obese patients? Clin Nutr. 2012;31:774–5.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Langius J, Visser W, Kruizenga H, Reijven N. Measuring protocol handgrip strength with Hand Dynanometer. Standard Operating Procedures, Nutritional Assessment Platform. Version 2. 2016. https://nutritionalassessment.nl/standard-operating-procedures-sops/ . Accessed June 10, 2024.
Norman K, Stobaus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr. 2011;30:135–42.
Dang A. Real-World Evidence: A Primer. Pharm Med. 2023;37:25–36.
National Cancer Institute, U.S. Department of Health and Human Services. Common Terminology Criteria of Adverse Events (CTCAE) version 5.0. 2017. http://ctep.cancer.gov , Accessed February 21, 2024.
Peseski AM, McClean M, Green SD, Beeler C, Konig H. Management of fever and neutropenia in the adult patient with acute myeloid leukemia. Expert Rev Anti Infect Ther. 2021;19:359–78.
Buffa R, Mereu E, Comandini O, Ibanez ME, Marini E. Bioelectrical impedance vector analysis (BIVA) for the assessment of two-compartment body composition. Eur J Clin Nutr. 2014;68:1234–40.
Malihi Z, Kandiah M, Chan YM, Hosseinzadeh M, Sohanaki Azad M, Zarif Yeganeh M. Nutritional status and quality of life in patients with acute leukaemia prior to and after induction chemotherapy in three hospitals in Tehran, Iran: a prospective study. J Hum Nutr Diet. 2013;26:123–31.
Brooks N, Cloutier GJ, Cadena SM, Layne JE, Nelsen CA, Freed AM, et al. Resistance training and timed essential amino acids protect against the loss of muscle mass and strength during 28 days of bed rest and energy deficit. J Appl Physiol. 2008;105:241–8.
Matsui R, Rifu K, Watanabe J, Inaki N, Fukunaga T. Impact of malnutrition as defined by the GLIM criteria on treatment outcomes in patients with cancer: A systematic review and meta-analysis. Clin Nutr. 2023;42:615–24.
Sucak GT, Suyani E, Baysal NA, Altindal S, Cakar MK, Aki SZ, et al. The role of body mass index and other body composition parameters in early post-transplant complications in patients undergoing allogeneic stem cell transplantation with busulfan-cyclophosphamide conditioning. Int J Hematol. 2012;95:95–101.
van Lieshout R, Lize N, Tick LW, van Deursen J, Driessen E, Janssen T, et al. Nutrition-related problems, nutritional support practices and barriers to adherence to nutritional guidelines during intensive treatment for acute myeloid leukemia: Patients’ and hematology nurses’ perspectives and experiences. Clin Nutr ESPEN. 2022;48:446–55.
Download references
Acknowledgements
We thank the Departments of Dietetics and Nutrition, the Departments of Physiotherapy and the Hematology Departments of the following hospitals for their participation in the current study: Albert Schweitzer Hospital, Dordrecht; Maxima MC, Veldhoven; Meander Medical Center, Amersfoort; and Sint Antonius Hospital, Nieuwegein. Furthermore, we thank Mara Lam, Aniek Schuurbiers, Mandy van Gils, Laura Boots, Dana Verhoeven and Eske Ruijters for their help in reviewing and entering the data.
This work was partially supported by the Vrienden Integrale Oncologische Zorg Foundation, Utrecht, The Netherlands (2017); Baxter B.V., Utrecht, The Netherlands (GHOL6759, 2018); Fresenius Kabi Nederland B.V., Huis ter Heide, The Netherlands (2019), Albert Schweitzer Hospital’s Research Fund, Dordrecht, The Netherlands (2019). These funding sources did not play any role in the design of the study, the collection, analysis and interpretation of data, in writing of the report nor in the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of Dietetics and Nutrition, Maxima MC, De Run 4600, 5504 DB, Veldhoven, The Netherlands
Rianne van Lieshout & Debbie van der Lee
Department of Internal Medicine, Maxima MC, De Run 4600, 5504 DB, Veldhoven, The Netherlands
Lidwine W. Tick
Department of Internal Medicine, Division Hematology, Maastricht University Medical Center, P. Debyelaan 25, 6229 HX, Maastricht, The Netherlands
Erik A. M. Beckers & Harry C. Schouten
Department of Dietetics and Nutrition, Meander Medical Center, Maatweg 3, 3813 TZ, Amersfoort, The Netherlands
Willemijn Biesbroek
Department of Research, Maxima MC, De Run 4600, 5504 DB, Veldhoven, The Netherlands
Jeanne P. Dieleman
Department of Physiotherapy, Sint Antonius Hospital, Koekoekslaan 1, 3435 CM, Nieuwegein, The Netherlands
Myrthe Dijkstra
Department of Physiotherapy, Meander Medical Center, Maatweg 3, 3813 TZ, Amersfoort, The Netherlands
Wanda Groenesteijn
Department of Internal Medicine, Sint Antonius Hospital, Koekoekslaan 1, 3435 CM, Nieuwegein, The Netherlands
Harry R. Koene
Department of Dietetics and Nutrition, Sint Antonius Hospital, Koekoekslaan 1, 3435 CM, Nieuwegein, The Netherlands
Suzanne Kranenburg & Liesbeth van der Put - van den Berg
Department of Physiotherapy, Maxima MC, De Run 4600, 5504 DB, Veldhoven, The Netherlands
Nicky Rademakers
Department of Internal Medicine, Meander Medical Center, Maatweg 3, 3813 TZ, Amersfoort, The Netherlands
Josien C. Regelink
Department of Internal Medicine, Albert Schweitzer Hospital, Albert Schweitzerplaats 25, 3318 AT, Dordrecht, The Netherlands
Claudia J. van Tilborg, Peter E. Westerweel & Sandra de Zeeuw
Department of Research and Development, Netherlands Comprehensive Cancer Organization, Godebaldkwartier 419, 3511 DT, Utrecht, The Netherlands
Sandra Beijer
Department of Dietetics and Nutrition, Maastricht University Medical Center, P. Debyelaan 25, 6229 HX, Maastricht, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
Rianne van Lieshout contributed to the conception of the study. Rianne van Lieshout and Sandra Beijer contributed to the design of the study. Rianne van Lieshout, Willemijn Biesbroek, Wanda Groenesteijn, Suzanne Kranenburg, Debbie van der Lee, Liesbeth van der Put, Nicky Rademakers, Claudia J. van Tilborg and Sandra de Zeeuw contributed to the acquisition of the data. Analysis of the data was performed by Rianne van Lieshout. Rianne van Lieshout, Lidwine W. Tick, Prof. Erik A.M. Beckers, Jeanne P. Dieleman, Harry R. Koene, Josien C. Regelink, Peter E. Westerweel, Em. Prof. Harry C. Schouten and Sandra Beijer contributed to the interpretation of the data. Rianne van Lieshout drafted the manuscript. All authors critically revised the manuscript for important intellectual content and approved the final version to be submitted.
Corresponding author
Correspondence to Rianne van Lieshout .
Ethics declarations
Competing interests.
RvL has received unrestricted research grants from the Vrienden Integrale Oncologische Zorg Foundation, Utrecht, The Netherlands, Baxter B.V. Utrecht, The Netherlands (Grand reference number: GHOL6759) (Category 1), and Fresenius Kabi Nederland B.V., Huis ter Heide, The Netherlands (Category 1). C.J.v.T., S.d.Z. and P.E.W. have received an unrestricted research grant from the Albert Schweitzer Hospital’s Research Fund, Dordrecht, The Netherlands. The other authors have nothing to disclose.
Ethical approval
The study protocol was reviewed and exempted from ethics approval by the Medical Ethics Committee Maxima MC (N17025). The study procedures were in accordance with the rules of the European Personal Data Protection Act and the Code of Ethics of the World Medical Association (Helsinki Declaration). The study was registered at The Dutch Trial Register (NTR) with trial number NL8505. Written informed consent was obtained from all patients prior to enrollment in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Supplementary information
Supplementary material, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
van Lieshout, R., Tick, L.W., Beckers, E.A.M. et al. Changes in nutritional status and associations with physical and clinical outcomes in acute myeloid leukemia patients during intensive chemotherapy. Eur J Clin Nutr (2024). https://doi.org/10.1038/s41430-024-01488-8
Download citation
Received : 21 December 2023
Revised : 30 July 2024
Accepted : 30 July 2024
Published : 10 August 2024
DOI : https://doi.org/10.1038/s41430-024-01488-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Research article
- Open access
- Published: 23 February 2021
Assessment of nutritional status and associated factors among adolescent girls in Afar, Northeastern Ethiopia: a cross-sectional study
- Gebrehiwot Hadush 1 ,
- Oumer Seid 2 &
- Abel Gebre Wuneh 3
Journal of Health, Population and Nutrition volume 40 , Article number: 2 ( 2021 ) Cite this article
19k Accesses
10 Citations
6 Altmetric
Metrics details
A body of evidences showed that adolescent undernutrition is a serious public health problem in developing countries including Ethiopia. Adolescence period is the last chance for curbing the consequences of undernutrition and breaking the intergenerational cycle of malnutrition and poor health. Despite this fact, they have been considered as a low-risk group for poor health and nutrition problems than the young children or the very old. This study aimed to assess prevalence of nutritional status and associated factors among adolescent girls in Afar, Northeastern Ethiopia, 2017.
A school-based cross-sectional study design was conducted among 736 adolescent girls from February15 to March 05, 2017 in Afar, Northeastern Ethiopia, 2017. Multi-stage sampling technique was used to select study participants. A pretested and structured interviewer-administered questionnaire and anthropometric measurements was used to collect the data. The collected data were entered in to Epi Data version 3.1 and exported to SPSS version 20.0 for further statistical analysis. Body Mass Index for age (thinness) and height for age (stunting) was used to assess undernutrition of adolescent girls by using the new 2007 WHO Growth Reference. Data were analyzed using bivariate and multivariable logistic regression. The degree of association between dependent and independent variables were assessed using odds ratio with 95% confidence interval, and variables with p value < 0.05 were considered significant.
The study revealed that the prevalence of thinness and stunting were 15.8% (95% CI 13.3–18.5%) and 26.6% (95% CI 23.5–29.9%), respectively. Being at an early adolescent age (AOR = 2.89, 95% CI 1.23–6.81) for thinness and being at an early adolescent age (AOR = 1.96, 95% CI 1.02–3.74), household food insecure (AOR = 2.88, 95% CI 1.15–7.21), menstruation status (AOR = 2.42, 95% CI 1.03–5.71), and availability of home latrine (AOR = 3.26, 95% CI 1.15–4.42) for stunting were the independent predictors among the adolescent girls.
Conclusions
The prevalence of thinness and stunting is above the public health importance threshold level. Thus, Multi-sector-centered nutrition interventions to improve nutritional status of disadvantaged adolescent girls through providing comprehensive nutritional assessment and counseling services at community, school, and health facility levels, and creating household’s income-generating activities are recommended before they reach conception to break the intergenerational cycle effect of malnutrition.
World Health Organization (WHO) defined adolescence as a period of life ranging from 10 to 19 years old which is the transition from dependent childhood to independent adulthood [ 1 ]. Worldwide, there are about 1.2 billion adolescents, representing more than 18% of the global population. Nearly 90% of them live in developing countries, and approximately 600 million are female [ 2 ]. In Ethiopia, 20–26% of the population are adolescents [ 3 ].
Adolescence is a period of rapid growth and development by which up to 45% of skeletal growth takes place, and 15 to 25% of adult height is achieved [ 4 ]. Throughout this period, risk of nutrition inadequacies and other health issues are of great concern due to rapid growth in stature, muscle mass, and fat mass. As a result of these serious nutritional challenges, adolescents would be negatively affected by this rapid growth spurt as well as their health as adults [ 5 ].
Malnutrition in all its forms, particularly undernutrition including underweight for age, too short for age (stunted), too thin relative to height (wasted), and functionally deficient in vitamins and minerals, is a global issue, but in the developing countries, it is catastrophic [ 6 , 7 ]. Adolescents are in a vulnerable group for malnutrition and its consequences, because it is a dynamic period of physical growth and mental development. Undernutrition starts before birth, goes into adolescence and adult life, and can span into generations and results in short stature, lean body mass, and is associated with deficiencies in muscular strength. In addition, it can reduce resistance to infection and other debilitating conditions that reduce productivity [ 8 , 9 , 10 ].
A body of evidence showed that globally, adolescent undernutrition is a serious public health problem in both developed and developing countries, but is disproportionally keeping sever in developing countries, especially in Asia (32–65%) and Africa (4–30%), making them more vulnerable to low productivity, poor health, and early deaths. In Sub-Saharan Africa, the prevalence of adolescent undernutrition is 15–58%, which is higher from other African countries [ 7 , 11 , 12 , 13 ]. According to WHO, the recommended indicator to assess the nutrition status of adolescents are thinness (low body mass index for age) and stunting (low height for age), where the former is a result of mainly acute (short term), and the latter shows chronic (long term) nutritional deficiency [ 14 , 15 , 16 ].
Evidences showed that adolescent girls in many contexts are a marginalized and disempowered group and consequently face diminished opportunities and choices [ 17 ]. They are a nutritionally vulnerable group for their high requirements for growth, their eating patterns and lifestyles, and their risk-taking behaviors; their susceptibility to environmental influences and hard physical work, as commonly observed in low-income countries, may impose additional physiological stress and nutritional requirements in adolescence. In certain cultures, from infancy onwards including adolescents, girls are at particularly high risk because of gender discrimination [ 9 , 18 , 19 , 20 ]. On top of this, adolescents have been considered a low-risk group for poor health and nutrition and often receive little attention. This results in lack of information regarding the nutritional status of adolescents especially from the developing world [ 20 , 21 ].
There are few studies done in Ethiopia regarding the level of adolescent undernutrition in the country. The Ethiopian nutrition baseline report revealed that the prevalence of stunting and thinness in adolescent girls was 23 and 14%, respectively [ 22 ]. The other community-based studies done in different parts of Ethiopia such as Somali, Oromia, and Tigray indicated that the prevalence of both stunting and thinness were high in some rural parts of the country which were 22.9% stunted and 11.5% thin [ 23 ], 27.5% thin and 15.6% stunted [ 24 ], and 21.4% thin and 26.5% stunted [ 4 ], respectively.
Even though the few existing studies done on the nutritional status of adolescent girls in some parts Ethiopia and other developing world [ 10 , 14 , 19 , 20 ] indicated that adolescent undernutrition is a major public health problem in developing countries including our country, data on adolescent girl’s nutritional status in pastoral societies are scarce. Despite the fact that having adequate evidences and information on nutritional status among adolescent girls do have a paramount step for intervention programs to break the intergenerational cycle of malnutrition, to the best of our knowledge, there was no previous study with this objective on adolescent girls in Afar regional state where pastoral communities live particularly in the study area. Therefore, this study aimed to assess the prevalence of nutritional status (thinness, stunting) and associated factors among adolescent girls in Megale district, Afar regional state, Northeastern Ethiopia.
Study design and setting
This study employed a school-based cross-sectional study design from February 15, to March 05, 2017 in selected schools found at Megale district, Afar National Regional State, North East Ethiopia. The district is located at a distance 325 km away to the west of the regional capital, Semera and 765 km northern east of the capital of Ethiopia, Addis Ababa. The district is typically rural and organized into 8 administrative kebeles (the smallest administrative units), and the community is characterized by pastoral livelihood.
According to the Megale district health office report, the total population of the district, in the year 2016, is estimated to be 34,692 (19,220 males and 15,473 females) and children aged 6 months to 59 years old are 3962. Currently, the district has 21 governmental primary schools in the academic year of 2016/2017. The district has 3 health centers, 7 health posts, one private drug store, and one pharmacy. The topography is 60% mountainous, 20% flat, and 20% inclined. The annual rainfall is 500–600 ml, and the temperature is 35–40 °C [ 25 ].
Study populations
All adolescent girls (10–19 years) found in the governmental primary school of Megale district were the targets for the study, where the study population consisted of a sample of all regular adolescent girls found residing in the randomly selected governmental primary schools during the study period. Those adolescent girls who had physical deformity that hinder height measurements, self-reported pregnancy status, and residents of the study area for less than 6 months in the family at the time of interview were excluded from the study.
Sample size and sampling procedure
The required sample size for the first objective of this study (to determine the prevalence of thinness and stunting) was determined using a single population proportion with the following assumptions: The level of confidence ( α ) 95% ( Z 1-α /2 = 1.96), margin of error ( d ) 5%, design effect of 2 and the proportions ( p ) of adolescents’ girls who had thinness and stunting were 22.9 and 11.5% respectively taken from previous study done in Somalia region, Ethiopia [ 23 ], and the higher prevalence (22.9%) was taken and calculated using z 2 × p × q / d 2 . Therefore, the final sample size by considering the non-response rate of 10% was 298.
The required sample size for the second objective of this study (for the factors associated with thinness and stunting) was determined using Open Epi menu online software program with the following assumptions: The level of confidence (α) is taken to be 95%, power 80; and ratio (unexposed: exposed) was taken only once (Table 1 ).
At the end, out of two objectives, the prevalence (290) and associated factors (379), the largest sample 379 was used for this study. Considering a design effect of 2 (379 × 2 = 758), the final sample size calculated was 758.
Study participants were selected by multistage random sampling method. First, out of the twenty one governmental primary schools (grade 4–grade 8), eight schools were selected randomly. Second, the total sample size was allocated in to each randomly selected school using proportion to population size (PPS). Finally, after taking a list of an identification number for each adolescent girl student in the randomly selected schools from each school’s administrators (from their roster) as a sampling frame (list of students between 10 and 19 years), study participants were selected using simple random sampling technique randomly by computer-generated random numbers.
Data collection tools and process
A structured questionnaire was developed from the Ethiopian national nutrition survey report for the national nutrition program of Ethiopia [ 22 ] and other relevant literatures and contextualized to the local situation. The questionnaire was composed of sociodemographic and economic factors, health- and environment-related factors, dietary habits, and anthropometrics. Concerning the dietary diversity, individuals were asked about their past 24-h dietary recall method (from sunrise to sunrise), while for the dietary food frequency, individuals were asked about their past 7 days of food frequency practice using the WHO nine food groups. The minimum dietary diversity score of four or more out of the nine groups of foods was considered as adequate [ 26 ].
Anthropometric measurements such as body weight and height were measured, the former by using a weighing scale in light clothing with no jackets or coats, shoes, and additional clothing to the nearest 0.1 kg on a new calibrated portable scale and the latter by using a portable stadiometer with no shoes; shoulders, buttocks, and heels touching the vertical stand; and the head in Frankfurt position to the nearest 0.1 cm, respectively. Mid upper arm circumference (MUAC) was measured by marking midway between shoulder tip and the elbow tip on the vertical axis of the upper arm with the arm bent at right angle and between the lateral and medial surface of the left arm. Four diploma female nurses as data collectors and two BSc nursing professionals as supervisors were recruited. For each participant from the eight primary schools, direct face-to-face interviews were conducted during their break time before noon.
Data quality control
English version questionnaire was translated into the local language, “Afaraff”, and then back to English to maintain its consistency. Pretest was conducted among 37 students (5% of the sample) in a non-selected school in the district for necessary modification. A two-day training was given to the data collectors and supervisors before the actual data collection. Continuous supervision was done by the supervisors and the principal investigator on a daily basis.
Statistical analysis
All raw data with the exception of anthropometric data were entered and cleaned in EPI data software version 3.1 and then exported to SPSS for analysis; whereas the anthropometric data were entered and converted to height-for-age and BMI-for-age Z scores by using the Antro Plus software. Adolescent girls with BMI-for-age below −2 Z scores and height-for-age below −2 Z scores of the 2007 WHO reference population were classified as thin and stunted, respectively [ 27 ]. Descriptive statistical measures such as percentage, mean, and standard deviation of variables were computed to summarize the data.
Binary logistic regression model was used to assess the association between the two dependent and independent variables using odds ratio with 95% confidence interval. To identify independent variables which have statistically significant association with the outcome variable (thinness and stunting), first, bivariate analysis was computed for each independent variable, and the outcome variables and crude odds ratio (COR) and 95% confidence interval (CI) were obtained.
Then, all variables observed to be significant in the bivariate logistic analysis (at p value < 0.25) were subsequently included in the multivariable logistic regression model to identify the independent predictor variable after controlling the effects of confounders and adjusted odds ratio (AOR) with 95% CI was calculated. Multicollinearity between the independent variables was checked using standard error and excluded the variables that had standard error of > 2, and Goodness of fit was checked by the Hosmer & Lemeshow test with p value > 0.05. All tests were two-sided, and p values of less than 0.05 were considered to be predictive for each outcome variable. Results were described and presented using narrative text, graphs, and tables.
Operational definitions
Adolescents are individuals in the age group of 10–19 years of age. It is categorized as early (adolescents in the age group of 10–13 years of age), middle (adolescents in the age group of 14–16 years of age), and late adolescents (adolescents in the age group of 17–19 years of age) [ 28 ].
Stunting is if the height-for-age Z score is found to be below −2 SD of the 2007 WHO growth reference. Severe stunting is diagnosed if it is below −3 SD [ 27 , 29 ].
Thinness is if the BMI-for-age Z score < −2 SD of the WHO growth reference 2007. Severe thinness is diagnosed if it was below −3 SD [ 27 , 29 ].
Body mass index (BMI) is defined as weight in kilograms divided by height in meters squared = Weight (kg)/Height (m 2 )—normal weight if 18.5 kg/m 2 < BMI < 25 kg/m 2 , underweight if BMI < 18.5 kg/m 2 , and overweight if BMI > 25 kg/m 2 [ 27 , 29 ].
Mid upper arm circumference (MUAC) < 18 cm is classified as severe acute malnutrition, MUAC of 18–21 as moderate acute malnutrition, and MUAC > 21 is classified as normal [ 27 , 29 ].
Household food security was assessed using the four-item module, and the sum of affirmative responses to the six questions in the module was taken. The food security status of households with raw score 0–1 was described as food secure and food insecure [ 23 ].
Adequate dietary diversity score is defined as adolescent girls with dietary diversity score of the median and above the median values ( > 4 food groups), whereas inadequate dietary diversity score is when adolescent girls with dietary diversity score is below the median value (< 4 food groups) [ 26 ].
Ethical considerations
Ethical clearance was obtained from Mekelle University, College of Health Sciences, Research and Community Service Unit Ethical Review Committee. A support letter was also obtained from Afar regional education Bureau, Megale district health and education offices and kebele administrations. Again, informed consent was obtained from the commandant of the schools, participant, participant’s parent/ guardian before being enrolled, and they were assured about the confidentiality of the information. The aims of study and any possible risk of the study were explained to study participants using their own local language.
Demographic and socioeconomic characteristics
A total of 736 adolescent girls participated in this study with a response rate of 97.4%. The mean ± SD age of study participants were 14.28 ± 2.79 years where around two fifth, 286 (38.9%), of them were in the early adolescence period, while 178 (24.2%) were in the late adolescence period. Slightly below three fourths, 270(73.4%), of participants were rural residents. Majority, 714 (97.0%) and 712 (96.7%), of the participants were Muslims in religion and Afar in ethnicity, respectively. Moreover, 628(85.3%) of them were single, while the remaining 108 (14.7%) were currently married (Table 2 ).
The educational distribution of the students’ parents showed that 704 (95.7%) and 674 (91.6%) of their mothers and fathers did not attend formal education, whereas the least percent have joined college or university, 14(1.9%) for mothers and 12 (1.6%) for fathers. Regarding the occupation of parents, majority of the fathers’ occupation were pastoral/herding livestock, 514 (69.8%) and followed by government employee, 168 (22.8%). Majority of mothers’ occupation were housewife, 672 (91.3%) and followed by government employee, 58 (7.9%). Around 702 (95.4%) of households were headed by males and 34 (4.6%) were by females (Table 2 ).
Health and household environment-related characteristics
Slightly below one third, 168 (22.8%) of the participants reported that they have a home latrine, and 162 (96.4%) of them were using a latrine. Concerning school latrine utilization, 154 (20.9%) of the participants do not use the school latrine. Regarding the source of drinking water, 276 (37.5%) of them obtained from a protected or safe water source. Again in terms of waste disposal method, 702 (95.4%) of the participants use the open-field waste disposal method (Table 3 ). About 206 (28.0%) of adolescent girls started menstruation, and the mean ± SD age of menarche was 13.86 + 1.84 years. Moreover, 112 (15.2%) had history of illness in the past 2 weeks prior to the data collection.
Dietary intake-related characteristics
Eating behavior and dietary diversity score of adolescent girls.
Based on the 24-h dietary recalls, the overall proportion of adolescent girls with minimum dietary diversity score (at least consumed four food groups out of nine food groups) was 98 (13.3%). The dietary diversities consumed out of nine food groups were 640 (87.0%), 80 (10.9%), and 16 (2.1%), for low, medium, and high scores, respectively (Table 4 ).
Among the participants, 736 (100 %) consumed starchy staple food (cereals) followed by milk & milk products 452 (61.4%), flesh meat 232 (31.5%), and legumes/nuts 190 (25.8%). Consumption of dark green leafy vegetables, vitamin a-rich fruits and vegetables, and animal source foods (like organ meat, others fruits and vegetables, and eggs) were relatively low (Fig. 1 ).
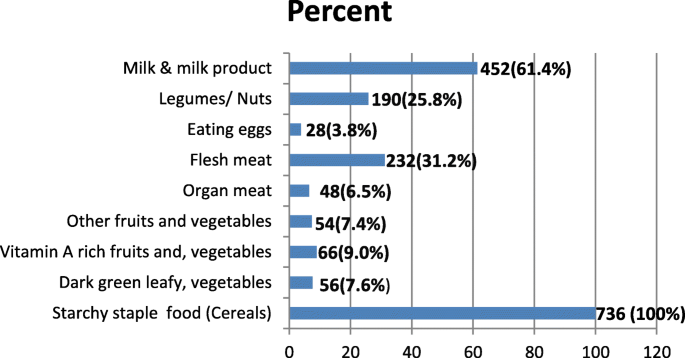
Types of food groups consumed over a 24-h period by school adolescents girls in Megale district, Afar Regional state, Northeastern Ethiopia, April, 2017 ( n = 736)
Past 7-day food frequency of adolescent girls
Based on the 7-day food frequency report, 736 (100%) of them consumed starchy staple food (cereals), three or more times per week, followed by milk & milk products 604 (82.1%) and legumes/nuts 330 (44.8%), whereas dark-green leafy vegetables, vitamin-A rich fruits and vegetables, and animal source foods (like organ, flesh meat, & eggs) were relatively least consumed (Table 5 ).
Prevalence of thinness and stunting of adolescent girls
The mean ± SD overall height and weight of the participants was 145.8 ± 10.3 cm and 39.1 ± 9.3 kg, respectively. In this study, the overall prevalence of thinness (BAZ < − 2 SD) was 116 (15.8%) (95% CI 13.3–18.5%), the overall prevalence of stunting (HAZ < − 2 SD) was 196 (26.6%) (95% CI 23.5–29.9%), while the prevalence of overweight was 6 (0.8%). The prevalence of severe thinness (BAZ < − 3 SD) and stunting (HAZ < − 3 SD) were 3.8 and 7.6%, respectively. The nutritional status of the adolescent girls according to the body mass index (BMI) showed that 198 (26.9%) of them were underweight. Moreover, according to their mid upper arm circumference (MUAC), 336 (45.7%) of the adolescent girls were found to have moderate acute malnutrition (MUAC 18–21 cm) (Table 6 ).The anthropometric measurements indicated that early age of adolescent girls were more stunted 102 (13.9%) and thin 74 (10.1%) than late adolescents 40 (5.4%) and 16 (2.2%), respectively (Fig. 2 ).
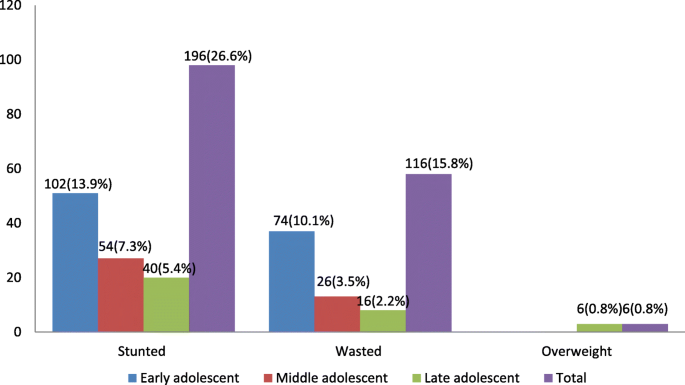
Overall anthropometric status of school adolescent girls in Megale district, Afar Regional state, Northeastern Ethiopia, April, 2017 ( N = 736)
Factors associated with thinness and stunting of adolescent girls
Factors associated with thinness.
In the first logistic regression model, the variables significantly associated with adolescent girls’ thinness were being early adolescent age, eating snacks, grade level, marital status, menarche, and dietary diversity have association at p value < 0.25. In the final multivariable analysis after examining the effect of confounders, the independent predicators for thinness were being early adolescent age (AOR = 2.89, 95% CI 1.23–6.81). The odds of thinness were around 2.89 times higher among adolescent girls who were early adolescent girls than those who were late adolescents. However, the other determinant factors did not show an association with thinness in multivariable analysis (Table 7 ).
Factors associated with stunting
In the first logistic regression model, the variables significantly associated with adolescent girls’ stunting were being early adolescent age, menarche, availability of home latrine, household food insecurity, grade level, family monthly income level, dietary diversity, source of water, and eating snack. Finally, those variables were taken to the final multivariable logistic regression to identify the variables significantly associated with stunting after controlling the effect of confounders. Hence, in the multivariable logistic regression analysis models, being early adolescent age (AOR = 1.96, 95% CI 1.02–3.74), household food insecure (AOR = 2.88, 95% CI 1.15–7.21), menstruation status (AOR = 2.42, 95% CI 1.03–5.71), and availability of home latrine (AOR = 3.26, 95% CI 1.15–4.42) were the independent predictors for stunting.
The odds of stunting were around 1.96 times higher among adolescent girls who were early adolescent girls than those who were of late adolescent age. Those adolescent girls whose households were food insecure were around 2.88 times more likely to get stunted as compared with those whose households were food secure, and those who had not had home latrine were 3.26 times more likely to get stunted as compared with those who had home latrine. Adolescent girls who did not start menstruation were 2.42 times more likely to be stunted as compared with adolescent girls who started menstruation (Table 8 ).
Discussions
Adolescents have specific health and development needs, and many of them face challenges that hinder their well-being especially on adolescent girls such as adverse reproductive outcomes, pregnancy outcomes, and birth weight [ 26 , 30 ]. Despite this fact, many studies in Ethiopia are still carried out focusing on the vulnerable groups like infant, pregnant and lactating women, and limited on adolescent girls. Hence, this study aimed to assess prevalence of nutritional status and associated factors among adolescent girls in primary schools of Megale district, Afar region, North East Ethiopia.
This study revealed that the overall prevalence of thinness among the adolescent girls was 15.8% (95% CI 13.3–18.5%), and this finding is almost similar using the same cutoff point with study done in Asembo and Mumias, Kenya (15.6%) [ 31 ], Kavre District, Nepal (14.94%) [ 32 ], Burkina Faso (13.7%) [ 33 ], and west Bengal (16%) [ 34 ]. It is consistent with the prevalence reported in Addis Ababa (13%) and Mekele (14%) [ 26 , 35 ] but lower than the study done in Adwa town (21.4%) [ 4 ], Ambo (27.5%) [ 36 ], and Eastern Tigray, Ethiopia (33.7%) [ 8 ]. Again, it is much lower when we compared with the study done in Kolar District, Garhwal, India, rural community of Tigray, Ethiopia, and Northern Nigeria where 54.8, 43.47, 58.3, and 58.7% of the adolescent girls were thin [ 30 , 37 , 38 , 39 ], respectively, but higher than study conducted in Tamale Metropolis, Ghana (10%) [ 40 ].
Other studies conducted in Addis Ababa city, Ethiopia (6.2%) [ 41 ] and Tunisia (1.3%) [ 42 ] have been reported much lower prevalence than the current study. These findings indicated that thinness is a major public health problem in majority of Ethiopian and other communities. The possible explanation for this difference could be due to difference in the study group and urban–rural difference between the study subjects and settings. Unlike this study, some studies done in Tunisia considered adolescents the middle and late stages which are less likely to be thin because of less possibility of height growth than early adolescents. The other possible variation could also be due to socioeconomic and cultural difference in dietary habit and care practices of study populations.
The overall prevalence of stunting in this study was also found to be 26.6% (95% CI 23.5–29.9%). This finding was consistent with other studies done in the rural community of Tigray, Ethiopia which reported that prevalence of stunting were 26.5% [ 39 ]. It is also consistent with study done in Nepal (21.08%) [ 32 ] and Seychelles (23%) [ 43 ]. Other previous studies in adolescent Ethiopians girls also reported that much lower levels of stunting. These include studies in Somali, Ethiopia (11.5%) [ 23 ], Adama zone (15.6%) [ 24 ], and Adwa Ethiopia (12.1%) [ 4 ].
Nonetheless, in northern Ethiopia, the prevalence of childhood chronic malnutrition is very high which may have an impact on the level of adolescent stunting [ 44 ]. A number of studies in other African countries including Burkina Faso (8.8%) [ 33 ] and Kenya (12.1%) [ 31 ] have been reported a lower prevalence of stunting. However, a high prevalence of stunting in adolescent girls has been reported in Bangladesh (32%) [ 45 ] and Garhwali, India (30.43%) [ 30 ].The variation could be due to socioeconomic and cultural difference in food access, nutrition information, dietary habit, and care practices of the communities.
In this study among the variables moved to the final multivariable logistic regression analysis model, being of early adolescent age was found to be the independent predictor for thinness. Hence, the odds of thinness were around 2.89 times higher among adolescent girls who were in the early stage of adolescents than those who were in late adolescent age. This might be due to the increased growth spurt during the early adolescent stage as compared to late adolescent stage with a sudden increase of height in the early adolescents than late adolescents. Findings from Tigray, Ethiopia [ 4 , 39 , 46 ] and Belgaum and Karnataka, India [ 47 , 48 ] have reported similar results with the present study.
Regarding stunting, the odds of stunting was around 1.96 times higher among adolescent girls who were in the early stage of adolescent period than those who were late adolescents. This finding is consistent with other studies conducted in five districts of Amhara region, Ethiopia [ 49 ], the baseline national nutrition survey [ 22 ], and rural community of Tigray, Ethiopia [ 39 ], which showed that prevalence and severity of stunting have been found to decrease with age. This might be due to the fact that inadequate nutrient intake besides increased requirement during early adolescent’s faster growth period and those early adolescents might be more affected by undernutrition than the older adolescents in the current study. However, a contradict finding that has been reported from Somalia region, Ethiopia was the present result [ 23 ].
The odds of stunting among adolescent girls who did not start menstruation early were 2.42 times more likely to be stunted as compared with adolescent girls who started menstruation late. This result is in line with the findings of studies done in Adwa, Ethiopia [ 4 ], Goba town, Ethiopia [ 50 ], and Western Kenya [ 31 ] which indicated a negative association between stunting with sexual maturity. This might be explained by the fact that starting menstruation coincides with the adolescent growth spurt. Delay in menstruation in stunted adolescents shows the opportunity for catch-up growth as stunting delay menarche [ 4 , 39 ].
The odds of stunting among adolescent girls who had no home latrine were 3.26 times more likely to be stunted as compared with those adolescent girls who had had home latrine. This might be explained by the fact that those who have home latrine may have used it properly and they could not be affected by communicable diseases easily; as a result, they become healthy. Whereas those who do not have home latrine, they may defecate in the opened field and may be easily affected by communicable diseases; as a result growth will be interrupted and leads to stunting. Previous studies done in the rural community of Tigray, Ethiopia [ 39 ] and Tehuledere District, Ethiopia [ 51 ] showed that lack of home latrine was a predictor of stunting in adolescents.
The odds of stunting among adolescent girls from food-insecure households were 2.88 times more likely to be stunted than adolescent girls from food secured households. This indicate that the presence of chronic food insecurity leads to stunting because of chronic undernutrition and might be one of the important determinant of chronic nutritional insult in adolescent girls. The finding was in agreement with other studies conducted in Mini EDHS report and Tigray, Ethiopia [ 4 , 44 ] and five districts of Amhara region, Ethiopia [ 49 ] where food insecurity is negatively associated with the linear growth of adolescents.
Limitations of the study
The study involved a single cross-sectional design. Hence, causal inference might not be strong.
Recall and reporting bias might also affect for dietary diversity & food frequency questions. Therefore, further studies combined both quantitative and qualitative approach might be necessary for better understanding of undernutrition in the community.
This study revealed that the overall prevalence of thinness and stunting were found to be 15.8% (95% CI 13.3–18.5%) and 26.6% (95% CI 23.5–29.9%) in the study area, respectively. This result indicated that thinness and stunting among the adolescent girls are public health problems in the study area according to the WHO, cutoff values for public health significance.
The independent predictor significantly associated with thinness was being early adolescents’ age while the independent predictors significantly associated with stunting were being early adolescents’ age, household food insecure, menstruation status, and availability of home latrine. A comprehensive strategy such as nutrition education, improving household economy through income-generating activities, personal and environmental hygiene practices are recommended. Interventions are also needed to improve the nutritional status of disadvantaged adolescent girls through providing comprehensive and routine nutritional assessment and counseling services at community, school, and health facility levels before they reach conception period to break the intergenerational cycle effect of malnutrition.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
Adjusted odds ratio
achelor of Science
Mid upper arm circumference
Proportion to population size
Standard deviation
World Health Organization
WHO (2005) World Health Organization. Nutrition in adolescence-issues and challenges for the health sector: issues in adolescent health and development. Geneva: WHO; 2005.
Google Scholar
WHO. World Health Organization. Monitoring, evaluation and review of national health strategies: a country led platform for information and accountability; 2011. p. 1–34.
Eu T, States M, Programme NN, Assembly WH, Nutrition WHA, Stunting I, et al. Ethiopia Nutr Country Fiche; 2015. p. 2012–4.
Gebregyorgis T, Tadesse T, Atenafu A. Prevalence of thinness and stunting and associated factors among adolescent school girls in Adwa town, North Ethiopia. Int J Food Sci. 2016;2016.
WHO. The management of nutrition in major emergencies. 2nd ed. Geneva: World Health Organization; 2000. p. 236.
Effectiveness D. Addressing child undernutrition: evidence review. 2014;(March).
World Health Organization(WHO). Essential nutrition actions; improving maternal, newborn, infant and young child health and nutrition. 2013.
Weres ZG, Yebyo HG, Miruts KB, Gesesew HA, Woldehymanot TE. Assessment of adolescents' under nutrition level among school students in Eastern Tigray, Ethiopia: a cross-sectional study. J Nutr Food Sci. 2015;5(5):1.
Hanson MA, Bardsley A, De-Regil LM, Moore SE, Oken E, Poston L, et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “think Nutrition First.”. Int J Gynecol Obstet. 2015;131(October):S213–53.
Article Google Scholar
USAID, Multi-sectoral nutrition strategy global learning and evidence exchange, east and southern Africa regional meeting. 2010. https://www.fantaproject.org/sites/default/files/MultiSectoral-Nutrition-Strategy-2014-2025.pdf .
PMNCH. Knowledge summary: women’s & children’s health. Partnersh Matern Newborn CHhild Heal Knowledge Summ. 2012;18:1–4.
WHO. World Health Statistics [Internet]. Vol. 27, WHO World Health Organization; 2012. p. 171.
Sci JNF, State R. Journal of Nutrition & Food Sciences Prevalence and Associated Factors of Stunting Among Schoolchildren , in Debre Markos Town and Gozamen Woreda , East Gojjam Zone , Amhara; 2014.
Radu E, CIOTARU LO. Adolescent malnutrition from anthropological perspective. InProc Rom Acad, Series B. 2007;2:155–8.
Rosen JE. Adolescent health and development ( AHD ) a resource guide for world bank operations staff and government counterparts. Hnp Discussion Paper; 2004. p. 78.
De Onis M, Onyango AW, Borghi E, Siyam A, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents, vol. 43497; 2007. p. 660–7.
Save the Children. Adolescent nutrition policy and programming in SUN+ countries. 2015;
Miah MS, Rahman N, Prodhan U, Linkon M, Rahman S. Prevalence of iron deficiency anemia among adolescent girls and its risk factors in tangail region of Bangladesh. Int J Eng Technol. 2014;3(06):613–9.
Story M, Stang J. Chapter 3 Nutrition needs of adolescents; Mary Story and Jamie Stang; 2005. p. 21–34.
Omobuwa O, Alebiosu CO, Olajide FO, Adebimpe WO. Assessment of nutritional status of in-school adolescents in Ibadan. Nigeria. South African Fam Pract. 2014;56(4):246–50.
Damie TD, Wondafrash M, Nigussie A. Nutritional status and associated factors among school adolescents in Chiro Town. Ethiopia: West Hararge; 2013.
Health E. for the National Nutrition Program of; 2009.
Awel AA, Lema TB, Hebo HJ. Nutritional status and associated factors among primary school adolescents of pastoral and agro- pastoral communities, Mieso Wored, Somali Region. Ethiopia: a comparative cross-sectional study. 2016;8(November):297–310.
KT R, M A. Nutritional status and its associated factors among school adolescent girls in Adama City, Central Ethiopia. J Nutr Food Sci. 2016;6(3):4–11.
Megale district profile from the annual report, for the Year Ended 2016.
Telake DS. Undernutrition among women in Ethiopia. 2010;(77).
WHO, Anthro plus for personal computers manual: software for assessing growth of the world’s children and adolescents, WHO, Geneva, Switzerland, 2009.
Yasin MA. Nutritional status and associated risk factors among adolescents girls in Agarfa High School, Bale Zone, Oromia Region, South East Ethiopia. Int J Nutr Food Sci. 2015;4(4):445.
Amanu W, Mekonnin D. Nutr Status Adolesc Girls Living in Southwest of, vol. 34; 2014. p. 58–65.
BO R, Zia S. Internet Journal of Medical Update ( Biannual Electronic Journal ). J Med Updat. 2012;6(2):2012.
Leenstra T, Petersen LT, Kariuki SK, Oloo AJ, Kager PA, ter Kuile FO. Prevalence and severity of malnutrition and age at menarche; cross-sectional studies in adolescent school girls in western Kenya. Eur J Clin Nutr. 2005;59(1):41–8.
Article CAS PubMed Google Scholar
Di M, Mk H, Sharma K, Dk M, Shakya R. Prevalence of underweight, stunting and thinness among adolescent girls in Kavre District. 2015;35(2):129–135.
Daboné C, Delisle HF, Receveur O. Poor nutritional status of schoolchildren in urban and peri-urban areas of Ouagadougou (Burkina Faso). Nutr J. 2011;10(1):34.
Article PubMed PubMed Central Google Scholar
Sarkar M, Manna N, Sinha S. Eating habits and nutritional status among adolescent school girls: an experience from rural area of West Bengal. 2015;14(12):6–12.
Gebremariam H. Assessment of nutritional status and associated factors among school going adolescents of Mekelle City, Northern Ethiopia. Int J Nutr Food Sci. 2015;4(1):118.
Yetubie M, Haidar J, Kassa H, Fallon F. Socioeconomic and demographic factors affecting body mass index of adolescent students aged 10-19 in Ambo (a Rural Town) in Ethiopia. Int J Biomed Sci. 2010;6(4):321–6.
PubMed PubMed Central Google Scholar
Shivaramakrishna HR, Deepa AV, Sarithareddy M. Nutritional status of adolescent girls in rural area of Kolar District -a cross-sectional study. Al Ame en J Med Sci. 2011;4(3):243–6.
Mijinyawa MS, Yusuf SM, Gezawa ID, Musa BM, Uloko AE. Prevalence of thinness among adolescents in Kano. Northwestern Nigeria. 2014;11(1):24–9.
Mulugeta A, Hagos F, Stoecker B, Kruseman G, Linderhof V, Abraha Z. Nutritional status of adolescent girls from rural communities of Tigray, Northern Ethiopia 2009;(August).
Book Google Scholar
Danquah AO, Amoah AN, Opare-obisaw C. Nutritional status of upper primary school pupils in a rural setting in Ghana. 2013;2(6):320–326.
Gebreyohannes Y. Nutritional status of adolescents in selected government and private secondary schools of Addis Ababa, Ethiopia. Int J Nutr Food Sci. 2014;3(6):504.
Aounallah-skhiri H, Romdhane H Ben, Traissac P, Eymard-duvernay S, Delpeuch F, Achour N, et al. Nutritional status of Tunisian adolescents: associated gender, environmental and socio-economic factors. 2017;11(12):1306–1317.
Bovet P, Kizirian N, Madeleine G, Blössner M, Chiolero A. Prevalence of thinness in children and adolescents in the Seychelles: comparison of two international growth references. Nutr J. 2011;10(1):65.
Central Statistical Agency [Ethiopia]. Ethiopia mini demographic and health survey 2014. Addis Ababa, Ethiop. 2014;(August).
Alam N, Roy SK, Ahmed T, Ahmed AMS. Nutritional status, dietary intake, and relevant knowledge of adolescent girls in rural Bangladesh. J Heal Popul Nutr. 2010;28(1):86–94.
Melaku YA, Gordon Alexander Zello GA, Robert JA, Zumin S. Prevalence and factors associated with stunting and thinness among adolescent students in Northern Ethiopia: A comparison to World Health Organization standards. Archiv Public Health. 2015;73:44.
Baliga SS, Naik VA, Mallapur MD. A commmunity based cross sectional study. Nutritional status of adolescents in rural area, India. J Sci Soc. 2014;41:22–5.
Karnataka N, Rajaretnam T, Hallad JS. Nutritional status of adolescents in Karnataka, India. 2012;58(1):55–67.
Wassie MM, Gete AA, Melkie Edris Yesuf ME, Alene GD, Belay A, Moges T. Predictors of nutritional status of Ethiopian adolescent girls: a community based cross sectional study. BMC Nutrition. 2015;1:20. https://doi.org/10.1186/s40795-015-0015-9 .
Mekonnen T, Semere S, Tesfaye A, Abdurrahman K. Nutritional status and associated factors of adolescent school girls, Goba Town, Southeast Ethiopia. Volume 16 Issue 1 Version 1.0 Year; 2016.
Woday A, Menber Y, Tsegaye D. Prevalence of and associated factors of stunting among adolescents in Tehuledere District, North East Ethiopia, 2017. J Clin Cell Immunol. 2018;9:546. https://doi.org/10.4172/2155-9899.1000546 .
Download references
Acknowledgements
Authors would like to thank Mekelle University, Megale district Administrative Office, Megale district, Education Office and respective school administrations, study participants, data collectors, and supervisors for their cooperation in the study.
Not applicable
Author information
Authors and affiliations.
Afar Region Health Bureau, Semera, Ethiopia
Gebrehiwot Hadush
School of Public Health, College of Health Sciences, Mekelle University, Mekelle, Ethiopia
Department of Public Health, College of Medical and Health Sciences, Samara University, Samara, Ethiopia
Abel Gebre Wuneh
You can also search for this author in PubMed Google Scholar
Contributions
GH has designed the study and was involved in data collection. GH, SO, and AG have cleaned and analyzed the data, interpreted the results, and drafted the manuscript. All authors have critically reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Abel Gebre Wuneh .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from Mekelle University, College of Health Sciences, Institutional Review Board (IRB). An informed consent was obtained from the commandant of the schools, participants, participant’s parent/guardian before being enrolled in the study. In addition, participants were assured about the aim, possible risk if any, and confidentiality of the study using their own local language (Afaraff language).
Consent for publication
This manuscript has not been published elsewhere by another journal.
Competing interests
The authors declared no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hadush, G., Seid, O. & Wuneh, A.G. Assessment of nutritional status and associated factors among adolescent girls in Afar, Northeastern Ethiopia: a cross-sectional study. J Health Popul Nutr 40 , 2 (2021). https://doi.org/10.1186/s41043-021-00227-0
Download citation
Received : 30 October 2018
Accepted : 14 February 2021
Published : 23 February 2021
DOI : https://doi.org/10.1186/s41043-021-00227-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescent girls
- Northeast Ethiopia
Journal of Health, Population and Nutrition
ISSN: 2072-1315
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Nutrition and ageing
Nutrition to achieve and maintain optimal health throughout life is one of the primary research themes within the chair group Nutritional Biology at the Division of Human Nutrition and Health. Our aim is to identify dietary strategies that optimize nutritional status to slow down or reverse stages preceding ageing related pathologies (cognitive decline, sarcopenia, osteoporosis, anorexia of ageing).
Research topics
A major cause of frailty and disability is sarcopenia. Resistance-type exercise training and nutritional supplementation are considered promising strategies to treat and/or postpone sarcopenia. Well-designed trials have been performed defining new leads for nutritional and exercise interventions. Our research concentrates on nutritional strategies to prevent or treat the progressive loss of muscle mass, strength and physical performance with ageing, using novel, sensitive and specific assessment methods.
Cognitive decline
One of the major age-related changes is a decline in cognitive functioning. Our intervention and observational studies have focused on the role of omega-3 fatty acids, B-vitamins, vitamin D, glucose and protein in the prevention of cognitive decline and dementia. Our current research acknowledges the interactions between nutrients and foods by assessing the role of prebiotics, multi-nutrients and dietary patterns. We further aim to explore the biological effects of nutrition in relationship to lifestyle, across the microbiota-gut-brain axis and in relationship to biomarkers of cognitive ageing and neurodegeneration.
Bone health
Osteoporosis is a multifactorial disease increasing bone fragility and susceptibility to fractures. Dietary therapies including vitamin D and calcium have beneficial effects on bone mass, density and turnover and a reduced risk of fractures. Evidence for associations between B-vitamin intake and bone health is diverse. In the B-PROOF trial we studied the effect of 2-year daily supplementation with vitamin B12 and folate on the reduction of fracture incidence. Current research links bone and muscle health concurrently studying the efficacy of protein nutrition and exercise.
Public health practice
An important step is to translate scientific evidence on nutrition, exercise and physical activity in relation to nutritional, functional and health status of elderly people to practice. Based on these scientific insights effective public health interventions will be developed in response to sustainability issues, practical needs and in close collaboration with local authorities and stakeholders.
Our projects

Project Muscle Health and Function

Project Lifestyle research into maintaining optimal cognitive function in ageing (MOCIA)

Project ProMuscle in Practice: Resistance exercise training and increased protein intake to improve physical functioning in community-dwelling elderly people

Project B-vitamins in the prevention of osteoporotic fractures in elderly people

Project NU-AGE - New dietary strategies addressing the specific needs of elderly population for an healthy ageing in Europe

Project Development of protein-enriched meal concepts tailored to the needs of elderly people

Project Telemonitoring for the prevention of undernutrition in community-dwelling elderly

Project FOCOM Cognition Test

Project 4xD: Vitamin D for preventing Dementia and Depression in Diabetes

Project E-learning ‘Older adults and malnutrition’ aimed at caregivers

Project Gut-brain health effects of PREbiotics in older adults with suspected COgnitive Decline: the PRECODE study
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Food Nutr Res

Assessment of nutritional status in the elderly: a proposed function-driven model
There is no accepted or standardized definition of ‘malnutrition’. Hence, there is also no definition of what constitutes an adequate nutritional status. In elderly people, assessment of nutritional status is complex and is complicated by multi-morbidity and disabilities combined with nutrition-related problems, such as dysphagia, decreased appetite, fatigue, and muscle weakness.
We propose a nutritional status model that presents nutritional status from a comprehensive functional perspective. This model visualizes the complexity of the nutritional status in elderly people.
Design and results
The presented model could be interpreted as the nutritional status is conditional to a person’s optimal function or situation. Another way of looking at it might be that a person’s nutritional status affects his or her optimal situation. The proposed model includes four domains: (1) physical function and capacity; (2) health and somatic disorders; (3) food and nutrition; and (4) cognitive, affective, and sensory function. Each domain has a major impact on nutritional status, which in turn has a major impact on the outcome of each domain.
Conclusions
Nutritional status is a multifaceted concept and there exist several knowledge gaps in the diagnosis, prevention, and optimization of treatment of inadequate nutritional status in elderly people. The nutritional status model may be useful in nutritional assessment research, as well as in the clinical setting.
The prevalence of malnutrition is reported to be 18–30% in different populations of elderly people in need of health care services ( 1 – 6 ). As yet, there is no established or accepted definition of ‘malnutrition’ although several definitions have been used in the scientific literature ( 3 , 7 , 8 ) and several proposals have been presented ( 9 – 12 ). Hence, there is also no definition of what constitutes an adequate nutritional status.
This article will not attempt to define malnutrition but will elaborate on nutritional status, as a condition, from a comprehensive functional perspective. Impaired nutritional status (as in malnutrition) may not itself be a subjective problem or discomfort, unless it affects the persons’ capacities or contributes to their impairments or disease progression. We propose a function-driven nutritional status model in order to visualize the diversity of the situation and also to analyze and discuss nutritional status.
The proposed nutritional status model, as well as the associated nutritional assessment, is developed from questions concerning how nutritional status affects, and is affected by, health or disease. In a young or adult population, the importance of an adequate nutritional status in supporting a long and healthy life is well established. But what about older people who are already in need of health care and social services? Is the aim still to lead a long and, depending on individual circumstances, relatively healthy life? Or is the aim to enable them to live an independent life? And how does the approach to nutritional status in old age affect practice in health care? Populations in geriatric care are heterogeneous, which further complicates the application of scientific research to individuals’ needs in health care.
Need for personalized nutritional care
There is a need for an effective, personalized, and scientifically based model for the assessment and evaluation of nutritional status in old people. Today, most countries and communities are facing a geriatric challenge ( 13 ), with an increasing proportion of older people in the population ( 14 ). A geriatric nutritional assessment is complicated by multi-morbidity, injuries, and disabilities in combination with nutrition-related problems such as dysphagia, decreased appetite, fatigue, and muscle weakness. Old age is the most dominant risk factor for acute and chronic disease, as well as reduced physical, cognitive, affective, and social function. This functional decline may be the main reason for high risk of malnutrition ( 8 , 15 , 16 ), but the risk of malnutrition increases even further in the case of multi-morbidity, and such disease-related malnutrition is common in old people ( 17 ). The increased risk of malnutrition found in research may, however, be due to the method used for nutritional assessment, as some methods are based on parameters such as the number of drugs used, living arrangements (e.g. living at home vs. living in the nursing home), and diagnoses (e.g. dementia), indicating an increased risk of malnutrition according to the screening method. A minimum age, or definition of elderly people, for the proposed approach on nutritional status is not defined, as each individual situation has to be taken into concern. The concept of ‘frailty’ has been proposed to make a distinction between biological and chronological ages and is therefore applicable in this proposed model as it highlights the challenges of geriatric nutrition. Nutritional assessments require knowledge, qualified personnel, and scientifically based methods to evaluate and meet the nutritional needs of people at old age.
A comprehensive perspective is needed to adequately assess and interpret nutritional status in elderly people, as visualized in the proposed model for assessment of nutritional status ( Fig. 1 ). The model takes account of the heterogeneity of the elderly population, with various symptoms, disorders, and treatments affecting their nutritional status. Nutritional research, as well as the clinical methodology of nutritional assessment, has to explore associations between nutritional status and its predictors, exposures, and outcomes. In clinical practice and also in research we need a personalized approach, taking into account the heterogeneity of the population and the complex nature of nutritional status ( 18 ). Too often research including nutritional assessments ignores the complexity of nutritional status in elderly people and uses a single parameter such as low body mass index or low energy intake, or else it is based on simple screening methods such as the Mini Nutritional Assessment or Subjective Global Assessment. Also, most instruments aim to evaluate the presence of malnutrition rather than to adequately assess nutritional status.

Individualized model for assessment of nutritional status, including an obligatory examination of each of four domains, namely, (1) physical function and capacity; (2) health and somatic disorders; (3) food and nutrition; and (4) cognitive, affective, and sensory function. Each domain contributes to nutritional status. Optimal function (defined for each person) is the most important factor in analyzing nutritional status and at the same time is the overall goal of any actions and treatment.
In the proposed nutritional status model, the goal for actions and treatment in the clinical setting is to identify and achieve optimal function (and the optimal situation) for each person or patient. The model describes the complex interaction between four domains contributing to the overall goal – the optimal function.
Aim of the nutritional status model
The proposed model aims to visualize the interplay between the main components of nutritional status from an aging perspective. It is intended to be used in nutritional assessments in research as well as in clinical settings.
The four domains included in the proposed model of nutritional status were identified by two background questions: ‘What constitutes adequate nutritional status in old people?’ and ‘How do health care professionals perceive nutritional status in elderly people?’ The model should be applied flexibly, as the domains are interrelated and these interrelations are individually specific. The model may also require that in specific cases domains should be added or rebuilt.
The complexity of nutrition is highlighted within this research, as food has nutritional, social, biomedical, and functional implications. In the proposed model, we use four domains, overall categories or blocks in a comprehensive framework, to facilitate a fruitful discussion as part of the process of assessing nutritional status.
- Physical function and capacity: comprising muscle strength, activities of daily living (ADL) functioning, physical activity, body composition, etc.
- Health and somatic disorders: comprising prescribed pharmaceuticals, physical symptoms, current diseases, health-related quality of life, inflammation, etc.
- Food and nutrition: comprising intake of energy and nutrients, mealtime habits, fluid intake, dietary patterns, etc.
- Cognitive, affective, and sensory function: comprising cognitive decline, depression, mood, sense of taste and smell, etc.
In practical use, the model encourages transdisciplinary competence. No specific speciality has precedence of any area or domain, and no specific area or domain has precedence over any other area or domain, in the model.
The model could be interpreted as indicating that nutritional status is conditional to a person’s optimal function (as defined by themselves), where each of the four domains contributes to the final goal (of optimal function). Also, the model could be interpreted as showing that nutritional status affects each domain and, consequently, the individual’s optimal function. Each domain has a great impact on nutritional status, which has a great impact on the outcome of the domains, as explained below. In each individual case, each domain is more or less important for achieving optimal function, as the optimal function is defined by each person and each particular situation or setting.
In the following, the four domains are described and presented from this perspective.
Physical function and capacity
In the framework of this article, ‘physical function’ mainly comprises muscle, cardiovascular, and pulmonary function. Physical function is not necessarily related to physical capacity. The muscle function of leg muscles (measured using leg press) may be adequate, but when it comes to the capacity of performing household chores, the physical (i.e. muscle) function (e.g. strong legs) has to be transformed to physical capacity (e.g. walking, standing, bending, and keeping the balance). In general, loss of muscle mass is associated with loss of functional capacity and also with the risk of developing chronic metabolic disease ( 19 ).
Change in body weight is often used as a primary outcome measure in nutritional interventions in the elderly, in research, as well as in clinical practice. As an isolated biomarker, the individual’s physical capacity will probably matter more than body weight. The ability to perform ADL is highly relevant in this context, as loss of muscle cell mass is related to loss of ADL function ( 20 ), and malnutrition is correlated with dependence on other people for ADLs ( 21 ). Nutritional interventions (dietary advice and nutritional supplementation) with the goal to improve ADL functions are most useful for people at risk of malnutrition ( 22 ).
Body composition is strongly related to nutritional status. Body fat mass and fat-free mass are associated with physical ability, morbidity, and mortality ( 23 , 24 ) . Body composition changes in old age, even in individuals with a stable body weight, and is characterized by increased fat mass and reduced fat-free mass ( 25 ). This change, probably due to hormonal changes, inadequate nutritional intake, increased morbidity, and less physical activity and exercise, among other reasons, causes sarcopenia and impaired physical function ( 7 , 26 ).
Older people, especially those with multi-morbidity, have increased levels of systemic inflammatory markers, such as C-reactive protein (CRP) ( 26 ), and chronic inflammation also denoted as ‘inflammaging’. Increased levels of inflammatory activity impair the anabolic processes in the body, as an anabolic block ( 27 ). The inflammatory condition may also decrease the intake of energy through loss of appetite, a condition also called ‘anorexia of ageing’ ( 28 ). Nutritional interventions in such a catabolic state are complicated and should not focus merely on achieving a positive energy balance, as this will result in increased body weight, meaning predominantly increased body fat. This may, in turn, stimulate the systemic inflammatory activity and hamper the anabolic processes even further ( 28 ).
In summary, physical function and capacity affect nutritional status in a bidirectional fashion. Changes in body weight as an indicator of a person’s nutritional status have to be measured in terms of various body function indicators, as a complement. Physical function and capacity may be measured as muscle strength, ADL function, physical activity, body composition, etc.
Health and somatic disorders
Disease may negatively affect appetite, which can, in turn, lead to impairment of nutritional status and functional performance. As described previously in this article, old age is associated with chronic systemic inflammation (inflammaging), which substantially affects morbidity and mortality ( 29 ). Physical exercise has been discussed as preventive action ( 30 ), but its effect has not been clearly proven. The presence of this systemic inflammatory activity also disqualifies the use of serum albumin concentrations as a valid indicator of nutritional status. Because of its characteristic as a negative acute phase protein, it reflects inflammatory status rather than indicating adequate protein intake in particular, or nutritional status in general ( 31 ).
Acute or somatic disorders, and their treatment and the resulting functional impairments, may negatively affect the ability to ingest and/or digest a meal, as well as to absorb macro- and micronutrients, hence negatively affecting nutritional status. A poor nutritional status also impairs the immune function, increasing the risk of disease and contributing to a negative trend. Disease and multi-morbidity have traditionally been considered as a confounder (or just ignored) in the research on nutritional status and malnutrition. However, in the model presented here, this is an essential part of and contributor to nutritional status. Classification of disease status could not only be achieved by diagnosis or a combination of diagnoses, but also the number or category of pharmaceuticals can be an indicator of disease status.
The presence of physical or psychological symptoms, due to disorders, may affect not only dietary intake but also other components of lifestyle, such as physical activity and social interactions. Conversely, poor nutritional status may have an impact on physical capacity and social interaction and consequently will affect the quality of life.
In summary, the presence of disease and multi-morbidity, and the inflammation and symptoms they may cause, closely affect the nutritional status in a bidirectional fashion. The domain of health and somatic disorders may be measured as prescribed or used pharmaceuticals, physical symptoms, current diseases, health-related quality of life, inflammation, etc.
Food and nutrition
Old age per se does not cause reduced dietary intake. However, if functions required for habitual activities (such as shopping, cooking, and eating) are compromised due to disease or reduced capacity, then the intake of energy and nutrients will be decreased ( 32 – 35 ). The changes in food habits, in combination with the ongoing disease, challenge the health practitioners to provide individualized care and achieve a comprehensive view of the person’s nutritional status.
The Nordic Nutrition Recommendations (NNR) ( 36 ) include dietary reference values for nutrients, foods, food patterns, physical activity, and sustainable food, with the aim to help prevent illnesses and chronic diseases. The reference values are adapted to different age groups, from infants to older adults, in good health. The use of reference values in frail elderly people, or those at immediate risk of frailty or malnutrition, is complicated and, hence, determining adequate nutritional intake on an individual basis in these elderly individuals is cumbersome and not evidence based. Therefore, more research in needed for this specific group of people. On an individual level, the care needs to be based on, among others, a comprehensive examination of energy need, body composition, physical function, and biomarkers.
The intake of fluids is rarely included in the analysis of dietary intake, although it is an essential contributor to optimal metabolic function and nutritional status. An impaired ability to achieve essential hydration status in combination with decreased fluid intake is common in old age ( 36 , 37 ), and overt dehydration has been reported in old people in need of health and social care ( 38 – 40 ). However, the importance of fluid intake is probably underestimated in clinical practice ( 41 ). Low fluid intake is not synonymous with dehydration, as the risk of dehydration is also affected by the presence of diseases, and their treatment, as well as by the person’s general physical condition. Unfortunately, the impact of dehydration and insufficient fluid intake in old age is insufficiently studied, although confusion and cognitive impairment have been reported as symptoms ( 42 , 43 ). Impaired cognitive performance may occur with dehydration matching only 2% of the person’s body weight ( 44 ), and older people may reach this level of dehydration earlier than younger people, as body water volume decreases with age ( 45 ). The NNR ( 36 ) presents a guiding value of water and fluid intake (in addition to water from foods) at 1–1.5 L/day for adults. There is no specific recommendation for older people, but it is concluded that elderly people should have a broader safety margin due to less capacity to concentrate urine and often impaired feelings of thirst.
Food and nutrition is probably the domain most obviously associated with nutritional status, but it is complex as it comprises aspects such as adequate intake of macro- and micronutrients, dietary patterns, mealtime situation, mealtime habits, surrounding environment, and social interaction during meals. Food intake may be perceived as a pleasant event, but can also be a medical treatment, as well as a necessity for survival. Hence, the solution to an individual nutritional problem needs to be more than a recommendation of a specific dietary intake ( 8 ), and nutritional intervention studies should include a functional perspective in the nutritional assessments or outcomes.
In summary, food and nutrition, as the most obvious of the domains included, affect nutritional status in a bidirectional fashion. The food and nutrition domain should be analyzed from a broader perspective.
Cognitive, affective, and sensory function
Adequate cognitive function is crucial for most activities in daily living, including planning and preparing meals, food intake, physical exercise, and other factors contributing to adequate nutritional status. In the care of people with dementia, the importance of creating a dining environment based on each and every person has been emphasized ( 46 ), as the physical environment has a major impact on the food and meal experience and, hence, the person’s nutritional status.
The definition of ‘cognitive function’ may comprise mood, regulation of anxiety, concentration, memory, and motivation or initiative. Most available scientific reports on the interaction between nutritional status and cognitive function deal with the hydration issue, or with the impact of dementia. Malnutrition is more common in people with dementia ( 47 ), with difficulties handling mealtimes during the progression of the disease ( 48 ). The identified increase in risk may also be due to the methods used for nutritional assessment.
An association between impaired nutritional status and depression has been observed, but the causal relationship is complex and it can be questioned whether depression is the cause or consequence of impaired nutritional status ( 49 ).
Impairment of olfactory function worsens with age, and the prevalence is higher in malnourished and multi-morbid people ( 50 ). This may negatively affect dietary intake, and it may cause specific micronutrient deficiencies that may, in turn, deteriorate olfactory function. However, the association between malnutrition and olfactory function has not been widely investigated and can be questioned ( 51 ).
In summary, cognitive, affective, and sensory functions affect nutritional status in a bidirectional fashion. To assess this domain, measurements of cognitive function or decline, depression, mood, and sensory function such as taste and smell can be used.
A model for assessing nutritional status is presented. We argue that nutritional status is a multi-faceted concept and the presented model highlights the complexity. Several knowledge gaps exist in each domain, leading to uncertainty and lack of evidence on how to diagnose, prevent, and optimize nutritional status in an individual and personalized setting.
The proposed nutritional status model has been used in a research setting but not in regular clinical setting. The model should, therefore, be implemented in various settings in order to generate experience. In research setting, it has supported the understanding of the complex role of nutrition in the health and well-being of the elderly, at a group level as well as at an individual level, supporting comprehensive geriatric assessment.
Acknowledgement
S.E. is financially supported by the Foundation Olle Engkvist Byggmästare.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.

COMMENTS
Assessing nutritional status is vital for understanding and managing patients' clinical conditions. Controlling Nutritional Status (CONUT) score is one of the most frequently used scores that evaluate caloric status, protein reserve, and immunological ...
NHANES is conducted by NCHS, in part to monitor the overall nutritional status of the U.S. population through health and medical histories, dietary interviews, physical examinations, and laboratory measurements. Information is obtained about many medical conditions, including nutrition-related disorders.
Food and nutrition are basic indispensable needs of humans. Nutrition plays a critical role in maintaining the health and well-being of individuals and is also an essential component of the healthcare delivery system. The nutritional status of individuals affects the clinical outcomes. Essential nutrients are classified into six groups, namely carbohydrates, proteins, lipids, minerals ...
Reliable information about the nutritional status is essential to identify potential critical nutrients and the population groups at risk of deficiency, as well as to develop effective public health policies to counteract unfavorable nutrition patterns that contribute to morbidity and mortality. In this review, the important role of biomarkers in the assessment of nutritional status is ...
The NIH nutrition research portfolio includes extramural and intramural research as well as research training. In F Y 21, 81 percent of the nutrition research portfolio was extramural research, conducted by hundreds of institutions in the United States and in . several countries across the world.
State of the body in relation to the consumption and utilization of nutrients. | Explore the latest full-text research PDFs, articles, conference papers, preprints and more on NUTRITIONAL STATUS ...
Food and nutrition are basic indispensable needs of humans. Nutrition plays a critical role in maintaining the health and well-being of individuals and is also an essential component of the healthcare delivery system. The nutritional status of individuals affects the clinical outcomes. Essential nut …
The Concept of Nutritional Status and Its Measurement Nutritional status is a component of health status that represents the bodily state resulting from the intake, absorption, utilization, and metabolism of dietary intake. It has an impact on all nutrition-related facets of health including growth, development, immunity, and risk of diet-related disease. Nutritional status is assessed by a ...
Nutrition plays a pivotal role in human health and overall well-being, serving as the foundation for life-sustaining physiological functions. A robust understanding of the various indicators that accurately reflect an individual's nutritional status is instrumental in addressing global health challenges. In recent years, there has been growing recognition of the utility and necessity of ...
For a number of medical conditions as well as weight status, an assessment of nutritional status can provide valuable information to direct treatment efforts. In the context of the seemingly constant increase in obesity, it is more important than ever to assess these...
Research examples are presented showing how biological anthropologists study nutritional status in order to examine human variation, adaptation, and adaptability, and the social determinants of ...
For a number of medical conditions as well as weight status, an assessment of nutritional status can provide valuable information to direct treatment efforts. In the context of the seemingly ...
A nutritional assessment provides an overview of nutritional status; it focuses on nutrient intake analysis of the diet, which is then compared with blood tests and physical examination. With comprehensive data on diet and biological information, the physician can make an accurate estimate of that person's nutritional status.
Background: Although nutritional status is influenced by multidimensional aspects encompassing physical factors, there is limited research on this complex relationship. Objectives: This study aimed to examine the interaction between physical activity level indicators and the nutritional status of ...
The New Concept of Integrative Nutritional Biomarkers. In terms of nutrition, health biomarkers are the cornerstone of research that establishes the functional effects of nutrition on the health-disease relationship. Currently, given the complex relationship between food intake and health/disease status, a more integrative understanding of the ...
A variety of questionnaires, equations and tools were found with ability to assess nutritional status for metabolic care or clinical nutrition purposes, but apparently there is no optimal, universal and reliable nutritional status screening system for all metabolic conditions. Novel assessment instr …
Objective: This systematic review presents the pooled prevalence of nutritional status and dietary intake among school-going children and adolescents (5-15 years of age) in an LMIC of Pakistan and the perspective for broader global nutrition in this age group.
On 11-12 January 2021, the National Institutes of Health convened a workshop entitled "Precision Nutrition: Research Gaps and Opportunities" to bring together experts to discuss the issues involved in better understanding and addressing precision nutrition. The workshop proceeded in 3 parts: part I covered many aspects of genetics and ...
Associations of nutritional status/body composition with physical outcomes, fatigue, fever duration, number of complications, time to neutrophil engraftment and hospital length of stay (LOS ...
Nutritional Status Evaluation (NSE) should provide a prognostic evaluation of the nutritional risk; an early diagnosis of malnutrition (either over- or undernutrition); the identification of nutritional requirements; the detection of patients needing total or partial nutritional support (diet, supplementation, artificial nutrition); the ...
2. Assessment of Nutritional Status Knowing the current micronutrient status is an important pre-requisite while developing concepts to improve nutrition in general. Food intake surveys are widely used to assess nutritional status and are available for many countries.
The screening of nutritional status is crucial in the treatment of RLPS. Various nutritional screening tools, such as the nutritional risk index (NRI), prognostic nutritional index (PNI) and Nutrition Risk Screening 2002 (NRS-2002) have been explored in various type of cancers.
Despite this fact, they have been considered as a low-risk group for poor health and nutrition problems than the young children or the very old. This study aimed to assess prevalence of nutritional status and associated factors among adolescent girls in Afar, Northeastern Ethiopia, 2017.
Nutrition, Nutritional Status and Functionality. A good quality of life means obtaining adequate nutrition and regular physical activity. This combination also reduces the risk of developing many chronic diseases while increasing one's level of physical performance. These aspects are critical for the population.
This study aimed at determining the influence of nutrition knowledge and dietary practices on the nutritional status of non-academic staff at the Tamale campus of University for Development Studies (UDS). The question was, does poor nutrition knowledge result into poor dietary practices and nutritional status?
The purpose of this study was to examine the effect of nutritional status and parental income on students' physical fitness. This research was an experimental research aimed to examine the ...
Nutrition to achieve and maintain optimal health throughout life is one of the primary research themes within the chair group Nutritional Biology at the Division of Human Nutrition and Health. Our aim is to identify dietary strategies that optimize nutritional status to slow down or reverse stages preceding ageing related pathologies (cognitive decline, sarcopenia, osteoporosis, anorexia of ...
Conclusions Nutritional status is a multifaceted concept and there exist several knowledge gaps in the diagnosis, prevention, and optimization of treatment of inadequate nutritional status in elderly people. The nutritional status model may be useful in nutritional assessment research, as well as in the clinical setting.