Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Asthma articles from across Nature Portfolio
Asthma is a form of bronchial disorder caused by inflammation of the bronchi. It is characterized by spasmodic contraction of airway smooth muscle, difficulty breathing, wheezing and coughing.
Latest Research and Reviews

Association of factors with childhood asthma and allergic diseases using latent class analysis
- Cornelia M. Borkhoff
- Jingqin Zhu
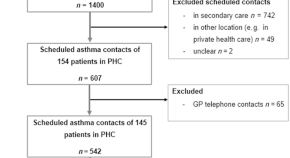
Documentation of comorbidities, lifestyle factors, and asthma management during primary care scheduled asthma contacts
- Jaana Takala
- Iida Vähätalo
- Hannu Kankaanranta
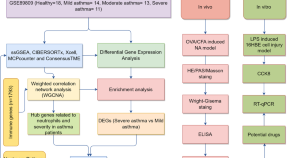
Bronchial epithelial transcriptomics and experimental validation reveal asthma severity-related neutrophilc signatures and potential treatments
Transcriptomic analysis of the airway epithelia in asthma patients identifies several neutrophilic signatures and targets associated with asthma severity, and highlights the potential therapeutic value of Reperixin in managing deteriorating asthma.
- Xinxin Zhang
- Xiufang Huang

Genomic attributes of airway commensal bacteria and mucosa
Systematic culture and genome sequencing of thoracic airway commensal bacteria finds many potential influences on lung health and disease. Polyomics of differentiated airway epithelium also suggest pathways that may sustain host-microbial interactions.
- Leah Cuthbertson
- Ulrike Löber
- William. O. C. Cookson
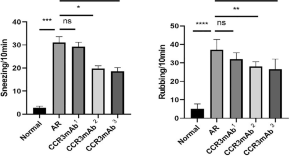
The study of the role of purified anti-mouse CD193 (CCR3) antibody in allergic rhinitis mouse animal models
- Yating Xiao
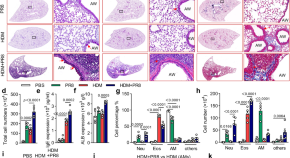
Cullin5 drives experimental asthma exacerbations by modulating alveolar macrophage antiviral immunity
Asthma may be exacerbated by respiratory viral infection, but the cellular and molecular mechanisms are still unclear. Here the authors show, using mouse models of asthma with influenza infection, that asthma-induced cullin5 in alveolar macrophages suppresses IFN-β production to promote neutrophilic inflammation but dampens antiviral immunity.
- Haibo Zhang
News and Comment
Jak1 hits a nerve.
- Stephanie Houston
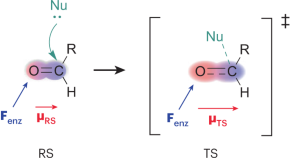
Boosted electrostatic biocatalysis
- Jan-Stefan Völler

Vitamin B-reath easier: vitamin B6 derivatives reduce IL-33 to limit lung inflammation
- Hēth R. Turnquist
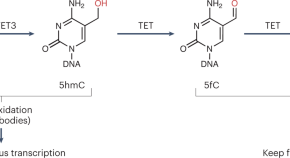
5-hydroxymethylcytosine stabilizes transcription by preventing aberrant initiation in gene bodies
5-hydroxymethylcytosine (5hmC) accumulates in transcribed gene regions (called ‘gene bodies’) and near enhancers, but its biological role has remained mysterious. A new study demonstrates that 5hmC serves to counteract inappropriate, spurious intragenic transcription in airway smooth muscle cells and by doing so, this DNA base functions in the prevention of chronic inflammation in the lung and an asthma-like phenotype.
- Gerd P. Pfeifer

Natural mouse microbes transiently block innate responses to allergens
Cohousing pet-store mice with laboratory mice leads to the natural transfer of microbes and subsequent inflammation in laboratory mice. Lung group 2 innate lymphoid cells — rapid responders to airway allergens — are transiently inhibited by inflammatory signals, but their activity recovers once the active infection subsides.

Asthma treatment for those who need it most
A biologic therapy reduces asthma exacerbations in Black and Hispanic children living in urban areas — a group with a disproportionately high asthma burden.
- Karen O’Leary
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Search by keyword
- Search by citation
Page 1 of 2
Psychological distress and associated factors among asthmatic patients in Southern, Ethiopia, 2021
There is an increased prevalence of psychological distress in adults with asthma. Psychological distress describes unpleasant feelings or emotions that impact the level of functioning. It is a significant exac...
- View Full Text
Retrospective assessment of a collaborative digital asthma program for Medicaid-enrolled children in southwest Detroit: reductions in short-acting beta-agonist (SABA) medication use
Real-world evidence for digitally-supported asthma programs among Medicaid-enrolled children remains limited. Using data from a collaborative quality improvement program, we evaluated the impact of a digital i...
Nonadherence to antiasthmatic medications and its predictors among asthmatic patients in public hospitals of Bahir Dar City, North West Ethiopia: using ASK-12 tool
Globally, adequate asthma control is not yet achieved. The main cause of uncontrollability is nonadherence to prescribed medications.
The hen and the egg question in atopic dermatitis: allergy or eczema comes first
Atopic dermatitis (AD) as a chronic inflammatory systemic condition is far more than skin deep. Co-morbidities such as asthma and allergic rhinitis as well as the psychological impact influence seriously the q...
Medication regimen complexity and its impact on medication adherence and asthma control among patients with asthma in Ethiopian referral hospitals
Various studies have found that medication adherence is generally low among patients with asthma, and that the complexity of the regimen may be a potential factor. However, there is no information on the compl...
Monoclonal antibodies targeting small airways: a new perspective for biological therapies in severe asthma
Small airway dysfunction (SAD) in asthma is characterized by the inflammation and narrowing of airways with less of 2 mm in diameter between generations 8 and 23 of the bronchial tree. It is now widely accepte...
Level of asthma control and its determinants among adults living with asthma attending selected public hospitals in northwestern, Ethiopia: using an ordinal logistic regression model
Asthma is a major public health challenge and is characterized by recurrent attacks of breathlessness and wheezing that vary in severity and frequency from person to person. Asthma control is an important meas...
Static lung volumes and diffusion capacity in adults 30 years after being diagnosed with asthma
Long-term follow-up studies of adults with well-characterized asthma are sparse. We aimed to explore static lung volumes and diffusion capacity after 30 + years with asthma.
Over-prescription of short-acting β 2 -agonists and asthma management in the Gulf region: a multicountry observational study
The overuse of short-acting β 2 -agonists (SABA) is associated with poor asthma control. However, data on SABA use in the Gulf region are limited. Herein, we describe SABA prescription practices and clinical outcom...
A serological biomarker of type I collagen degradation is related to a more severe, high neutrophilic, obese asthma subtype
Asthma is a heterogeneous disease; therefore, biomarkers that can assist in the identification of subtypes and direct therapy are highly desirable. Asthma is a chronic inflammatory disease that leads to change...
Adherence to inhalers and associated factors among adult asthma patients: an outpatient-based study in a tertiary hospital of Rajshahi, Bangladesh
Adherence to inhaler medication is an important contributor to optimum asthma control along with adequate pharmacotherapy. The objective of the present study was to assess self-reported adherence levels and to...
The link between atopic dermatitis and asthma- immunological imbalance and beyond
Atopic diseases are multifactorial chronic disturbances which may evolve one into another and have overlapping pathogenetic mechanisms. Atopic dermatitis is in most cases the first step towards the development...
The effects of nebulized ketamine and intravenous magnesium sulfate on corticosteroid resistant asthma exacerbation; a randomized clinical trial
Asthma exacerbation is defined as an acute attack of shortness of breath with more than 25% decrease in morning peak flow compared to the baseline on 2 consecutive days, which requires immediate standard thera...
Determinants of asthma in Ethiopia: age and sex matched case control study with special reference to household fuel exposure and housing characteristics
Asthma is a chronic inflammatory disorder characterized by airway obstruction and hyper-responsiveness. Studies suggest that household fuel exposure and housing characteristics are associated with air way rela...
Feasibility and acceptability of monitoring personal air pollution exposure with sensors for asthma self-management
Exposure to fine particulate matter (PM 2.5 ) increases the risk of asthma exacerbations, and thus, monitoring personal exposure to PM 2.5 may aid in disease self-management. Low-cost, portable air pollution sensors...
Biological therapy for severe asthma
Around 5–10% of the total asthmatic population suffer from severe or uncontrolled asthma, which is associated with increased mortality and hospitalization, increased health care burden and worse quality of lif...
Treatment outcome clustering patterns correspond to discrete asthma phenotypes in children
Despite widely and regularly used therapy asthma in children is not fully controlled. Recognizing the complexity of asthma phenotypes and endotypes imposed the concept of precision medicine in asthma treatment...
Positive change in asthma control using therapeutic patient education in severe uncontrolled asthma: a one-year prospective study
Severe asthma is difficult to control. Therapeutic patient education enables patients to better understand their disease and cope with treatment, but the effect of therapeutic patient education in severe uncon...
Asthma and COVID-19: a dangerous liaison?
The coronavirus disease 2019 (COVID-19) pandemic, caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), provoked the most striking international public health crisis of our time. COVI...
Knowledge, attitude, and practice towards COVID-19 among chronic disease patients at Aksum Hospital, Northern Ethiopia, 2020: a cross-sectional study
The Coronavirus disease 2019 outbreak is the first reported case in Wuhan, China in December 2019 and suddenly became a major global health concern. Currently, there is no vaccine and treatment have been repor...
Self-reported vs. objectively assessed adherence to inhaled corticosteroids in asthma
Adherence to inhaled corticosteroids (ICS) in asthma is vital for disease control. However, obtaining reliable and clinically useful measures of adherence remains a major challenge. We investigated the associa...
Association between prevalence of obstructive lung disease and obesity: results from The Vermont Diabetes Information System
The association of obesity with the development of obstructive lung disease, namely asthma and/or chronic obstructive pulmonary disease, has been found to be significant in general population studies, and weig...
Changes in quantifiable breathing pattern components predict asthma control: an observational cross-sectional study
Breathing pattern disorders are frequently reported in uncontrolled asthma. At present, this is primarily assessed by questionnaires, which are subjective. Objective measures of breathing pattern components ma...
The role of leukotriene modifying agent treatment in neuropsychiatric events of elderly asthma patients: a nested case control study
In March 2020, the US Food and Drug Administration decided that the dangers related to neuropsychiatric events (NPEs) of montelukast, one of the leukotriene modifying agents (LTMAs), should be communicated thr...
Asthma and stroke: a narrative review
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation, bronchial reversible obstruction and hyperresponsiveness to direct or indirect stimuli. It is a severe disease causing a...
Comparison of dental caries (DMFT and DMFS indices) between asthmatic patients and control group in Iran: a meta-analysis
The association between caries index, which is diagnosed by Decayed, Missing, and Filled Teeth (DMFT), and asthma has been assessed in several studies, which yielded contradictory results. Meta-analysis is the...
ICS/formoterol in the management of asthma in the clinical practice of pulmonologists: an international survey on GINA strategy
The treatment with short-acting beta-2 agonists (SABA) alone is no longer recommended due to safety issues. Instead, the current Global Initiative for Asthma (GINA) Report recommends the use of the combination...
Sustainability of residential environmental interventions and health outcomes in the elderly
Research has documented that housing conditions can negatively impact the health of residents. Asthma has many known indoor environmental triggers including dust, pests, smoke and mold, as evidenced by the 25 ...
Non-adherence to inhaled medications among adult asthmatic patients in Ethiopia: a systematic review and meta-analysis
Medication non-adherence is one of a common problem in asthma management and it is the main factor for uncontrolled asthma. It can result in poor asthma control, which leads to decreased quality of life, incre...
The outcome of COVID-19 among the geriatric age group in African countries: protocol for a systematic review and meta-analysis
According to the World Health Organization (WHO), the outbreak of coronavirus disease in 2019 (COVID-19) has been declared as a pandemic and public health emergency that infected more than 5 million people wor...
Correction to: A comparison of biologicals in the treatment of adults with severe asthma – real-life experiences
An amendment to this paper has been published and can be accessed via the original article.
The original article was published in Asthma Research and Practice 2020 6 :2
Disease control in patients with asthma and respiratory symptoms (wheezing, cough) during sleep
The Global Initiative for Asthma ( GINA)-defined criteria for asthma control include questions about daytime symptoms, limitation of activity, nocturnal symptoms, need for reliever treatment and patients’ satisfac...
The burden, admission, and outcomes of COVID-19 among asthmatic patients in Africa: protocol for a systematic review and meta-analysis
Coronavirus disease 2019 outbreak is the first reported case in Wuhan, China in December 2019 and suddenly became a major global health concern. According to the European Centre for Disease Prevention and Cont...
The healthcare seeking behaviour of adult patients with asthma at Chitungwiza Central Hospital, Zimbabwe
Although asthma is a serious public health concern in Zimbabwe, there is lack of information regarding the decision to seek for healthcare services among patients. This study aimed to determine the health care...
Continuous versus intermittent short-acting β2-agonists nebulization as first-line therapy in hospitalized children with severe asthma exacerbation: a propensity score matching analysis
Short-acting β2-agonist (SABA) nebulization is commonly prescribed for children hospitalized with severe asthma exacerbation. Either intermittent or continuous delivery has been considered safe and efficient. ...
Patient perceived barriers to exercise and their clinical associations in difficult asthma
Exercise is recommended in guidelines for asthma management and has beneficial effects on symptom control, inflammation and lung function in patients with sub-optimally controlled asthma. Despite this, physica...
Asthma management with breath-triggered inhalers: innovation through design
Asthma affects the lives of hundred million people around the World. Despite notable progresses in disease management, asthma control remains largely insufficient worldwide, influencing patients’ wellbeing and...
A nationwide study of asthma correlates among adolescents in Saudi Arabia
Asthma is a chronic airway inflammation disease that is frequently found in children and adolescents with an increasing prevalence. Several studies are linking its presence to many lifestyle and health correla...
A comparison of biologicals in the treatment of adults with severe asthma – real-life experiences
Anti-IgE (omalizumab) and anti-IL5/IL5R (reslizumab, mepolizumab and benralizumab) treatments are available for severe allergic and eosinophilic asthma. In these patients, studies have shown beneficial effects...
The Correction to this article has been published in Asthma Research and Practice 2020 6 :10
Determinants of Acute Asthma Attack among adult asthmatic patients visiting hospitals of Tigray, Ethiopia, 2019: case control study
Acute asthma attack is one of the most common causes of visits to hospital emergency departments in all age groups of the population and accounts for the greater part of healthcare burden from the disease. Des...
Determinants of non-adherence to inhaled steroids in adult asthmatic patients on follow up in referral hospital, Ethiopia: cross-sectional study
Asthma is one of the major non-communicable diseases worldwide. The prevalence of asthma has continuously increased over the last five decades, resulting in 235 million people suffering from it. One of the mai...
Development of a framework for increasing asthma awareness in Chitungwiza, Zimbabwe
Asthma accounts for significant global morbidity and health-care costs. It is still poorly understood among health professionals and the general population. Consequently, there are significant morbidity and mo...
Epidemiology and utilization of primary health care services in Qatar by asthmatic children 5–12 years old: secondary data analysis 2016–2017
Childhood asthma is a growing clinical problem and a burden on the health care system due to repetitive visits to children’s emergency departments and frequent hospital admissions where it is poorly controlled...
Is asthma in the elderly different? Functional and clinical characteristics of asthma in individuals aged 65 years and older
The prevalence of chronic diseases in the elderly (> 65 years), including asthma, is growing, yet information available on asthma in this population is scarce.
Factors associated with exacerbations among adults with asthma according to electronic health record data
Asthma is a chronic inflammatory lung disease that affects 18.7 million U.S. adults. Electronic health records (EHRs) are a unique source of information that can be leveraged to understand factors associated w...
What is safe enough - asthma in pregnancy - a review of current literature and recommendations
Although asthma is one of the most serious diseases causing complications during pregnancy, half of the women discontinue therapy thus diminishing the control of the disease, mostly due to the inadequate educa...
Biomarkers in asthma: state of the art
Asthma is a heterogenous disease characterized by multiple phenotypes driven by different mechanisms. The implementation of precision medicine in the management of asthma requires the identification of phenoty...
Exhaled biomarkers in childhood asthma: old and new approaches
Asthma is a chronic condition usually characterized by underlying inflammation. The study of asthmatic inflammation is of the utmost importance for both diagnostic and monitoring purposes. The gold standard fo...
Assessment of predictors for acute asthma attack in asthmatic patients visiting an Ethiopian hospital: are the potential factors still a threat?
Recurrent exacerbations in patients with moderate or severe asthma are the major causes of morbidity, mortality and medical expenditure. Identifying predictors of frequent asthma attack might offer the fertile...
Effect of adjusting the combination of budesonide/formoterol on the alleviation of asthma symptoms
The combination of budesonide + formoterol (BFC) offers the advantages of dose adjustment in a single inhaler according to asthma symptoms. We analyzed the relationship between asthma symptoms in terms of peak...
Asthma Research and Practice
ISSN: 2054-7064
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Advertisement
Asthma History, Current Situation, an Overview of Its Control History, Challenges, and Ongoing Management Programs: An Updated Review
- Published: 11 November 2022
- Volume 93 , pages 539–551, ( 2023 )
Cite this article
- Anandi Kapri ORCID: orcid.org/0000-0002-8254-2676 1 ,
- Swati Pant ORCID: orcid.org/0000-0001-9872-2463 1 ,
- Nitin Gupta ORCID: orcid.org/0000-0002-8093-7295 2 ,
- Sarvesh Paliwal ORCID: orcid.org/0000-0002-5247-2021 1 &
- Sumitra Nain ORCID: orcid.org/0000-0001-8238-3145 1
4051 Accesses
2 Citations
4 Altmetric
Explore all metrics
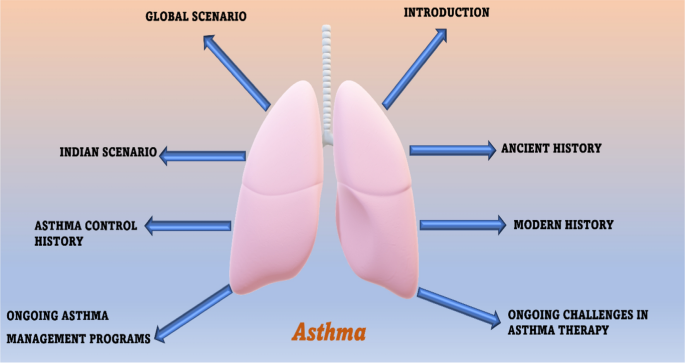
Asthma is a disease of the airways that is characterized by chronic inflammation and disordered airway function. The purpose of writing the current review paper is to review the history, current situation, control history, challenges, and ongoing management programs of asthma. Some official websites of known respiratory professional bodies were consulted for asthma guidelines, and information from Google Scholar® and PubMed® was also consulted. We reviewed around two hundred eight papers, and then, inclusion and exclusion criteria were applied to prepare this manuscript. Out of these papers, thirty papers, factsheets, and some official websites were used to prepare this manuscript. Physicians should follow already existing asthma guidelines in order to manage asthma. All prescribed medications should be continued. The government should make and adopt more strategies to promote the rational use of anti-asthmatic drugs and healthcare facilities and also make plans to disseminate more awareness among people about the schemes and programs made for safeguarding people against this life-threatening disease. We have done so much advancement to fight against this deadly disease, and we still need time to make the globe asthma-free. The number of people suffering from asthma is more than the number of people suffering from HIV infection and tuberculosis. Understanding the recommendations of professional bodies will assist in medical decision-making in asthma management. The individual needs of patients should be considered by healthcare professionals.
Graphical Abstract
Similar content being viewed by others

Asthma epidemiology and risk factors
Jessica Stern, Jennifer Pier & Augusto A. Litonjua
Safety of Biological Therapies for Severe Asthma: An Analysis of Suspected Adverse Reactions Reported in the WHO Pharmacovigilance Database
Paola Maria Cutroneo, Elena Arzenton, … Gianluca Trifirò

The 2023 GOLD Report: Updated Guidelines for Inhaled Pharmacological Therapy in Patients with Stable COPD
Paul D. Terry & Rajiv Dhand
Avoid common mistakes on your manuscript.
Introduction
Asthma is one of the most ancient diseases of the airways, characterized by chronic inflammation and disordered airway function [ 1 ]. Despite numerous advancements in the treatment and diagnosis of asthma, unfortunately, a large population is still suffering, and worldwide it becomes one of the top infectious diseases. Approximately 10% of children and 5% of adults are suffering from this disease. A WHO key facts dated May 3, 2021, on asthma stated that approximately 262 million people are affected by this life-threatening disease in 2019 and the number will be expected to hike in the future. It is also characterized by some other symptoms like epithelial rupture, hypertrophy of airway smooth muscles, hypersecretion of mucous in lungs bronchial walls, wheezing, coughing, and dyspnea (Fig. 1 ). Although there is no proper treatment available for asthma, it can be controlled with proper management and help asthmatics to live in a better way [ 2 ]. The primary preventive measure taken by WHO (world health organization) for asthma and disease management is reducing tobacco smoke exposure, and the initiative MPOWER and Mtobacco cessation is enabling progress in this area of tobacco control.
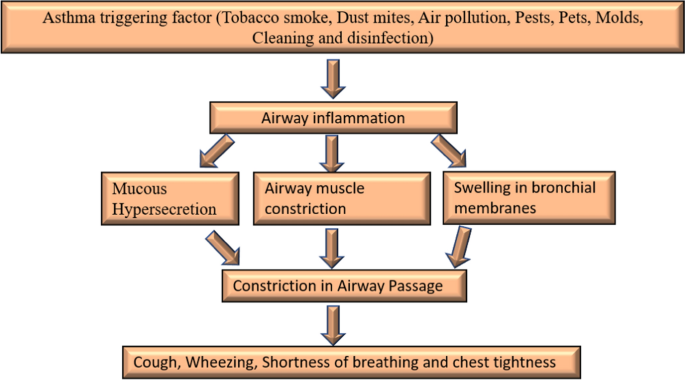
Flowchart of asthma
The use of bronchodilators is the principal therapy used in asthma but a greater understanding of the chief role of inflammation in asthma has led to the conclusion of the use of anti-allergic or anti-inflammatory agents for the management of asthma and is an internationally recognized strategy for its cure. The ICS (Inhaled corticosteroids) can provide ideal disease control but not as monotherapy. They need additional therapies such as SABA (Short-acting β2 agonists), LABA (Long-acting β2 agonists), LTRA (Leukotriene receptor antagonist therapy), and theophylline to achieve adequate control [ 3 ]. The primary aim of writing this review paper is to provide a brief understanding of asthma by critically assessing articles related to asthma.
Material and Methods
We performed an electronic search to find out the existing literature on asthma. Initially, the search was conducted on search engines like Google Scholar® and PubMed® to gather updated information about asthma. In addition, the search was conducted on the official websites of professional organizations such as GINA (Global initiative for asthma), WHO, MOHFW (Government of India-ministry of health and family welfare), and CDC (Centers for disease control and prevention) to get relevant guidelines for asthma control, anti-asthmatic drugs, challenges, prevention, and control management programs. Approximately 10 months were completely used to compile data for this manuscript. The key terms used during the search were “Asthma,” “history of asthma” “current situation of asthma,” “asthma control history,” “challenges in asthma,” and “ongoing asthma management programs.” Two hundred eight papers were screened, and then, inclusion and exclusion criteria were applied to prepare this manuscript. Out of these papers, thirty papers were used to prepare this manuscript. The last search was conducted on October 30, 2021.
Inclusion and Exclusion Criteria
Resources that were targeted at healthcare professionals and articles with a thorough understanding of asthma were included. All those papers which do not have original data and studies targeting the general public and patients were excluded.

Ancient History
For the very first-time, respiratory distress was recorded in China in 2600BC. The evidence was found in the form of “noisy breathing.” Shen nong in 2700BC was the first person to taste ephedra which was popularly known as anti-asthmatic herbal medicine around 5000 years ago [ 2 , 3 ]. The ancient Egyptians in 3000–1200BC believed respiration was one of the most crucial functions of the human body. Greco-roman (1000BC–200AD), both believe that asthma was produced due to demonic possession. Hippocrates was the first person who found that people suffering from asthma may have a hunch back. He also tried to understand the correlation between environment and respiratory problems. He also recommended ephedra along with red wine for the treatment of asthma [ 4 ].
Modern History
In the modern period, the understanding of the root cause of asthma began. In Europe 1500s, tobacco was introduced for the treatment of asthma, expectorate mucus and induce coughing. In 1579–1644, one of the chemists and physicians from Belgium Jean Baptiste Van Helmont said, “asthma was developed in the pipes of the lungs.” In (1633–1714), Bernardino Ramazzini found for the first-time exercise-induced asthma. He also acknowledged the correlation between organic dust and asthma. In the year 1873, Charles Blackley discovered the main cause of “hay asthma” and found that pollen was related to it. He rubbed pollen on different body parts to reproduce the symptoms [ 5 ]. In the 1900s, selective beta-2 adrenoceptors agonists were used for asthma treatment. In 1916, a physician and allergist named Francis Minot Rackemann reported that not all asthma is related to allergies. In 1920s, the deaths from asthma were related to airway structural changes and extensive inflammation but the information on why this happened and how it is responsible for bronchospasm was not known. For some decades, the treatment of asthma was done as episodic exacerbations [ 6 ]. Kustner and Prausnitz in the year 1921 noticed that asthmatics suffer from allergy symptoms due to indoor and outdoor irritants. In 1960s–1970s, technological advancements led to the use of peak flow meters to measure obstruction in airways and arterial blood gasses [ 7 ]. After the 1970s, inhaled corticosteroids were used for asthma cure. In 1980s, a depth understanding of how an allergen exposure, affect the release of a chemical mediator from mast cell which results in allergic asthmatic response [ 8 ].
Global Scenario
According to WHO information, asthma is included among (NCD) non-communicable diseases which is prevalent in children and adults. Generally, the deaths related to this disease mostly occur in countries with the economy in creeping and walking stage. The top fifteen countries with the largest asthmatic patients are Myanmar, Kiribati, Laos, Sri Lanka, New Guinea, Mali, Nepal, Fiji, Lesotho, Indonesia, Solomon Island, Sierra Leone, Timor-Leste, Philippines, and Vanuatu ( https://www.worldlifeexpectancy.com/cause-of-death/asthma/by-country/ ). In 2010, according to the data provided by National Hospital Ambulatory Medical Care Survey, approximately 1.3 million patients hospital visits were due to asthma [ 9 ]. In 2011–2012, the national survey for children’s health reported that around 3.4% of children have used emergency hospital visits due to this life-threatening disease [ 5 , 8 ]. Around 10.1 million physician office visits were reported for the year 2015. In 2017, around 43.12 million asthma cases were recorded whereas 272.68 asthma prevalence (prevalence 3.57%) and 0.49 million deaths (mortality rate 0.006%). More than 1.6 million asthmatic patient emergency visits were reported for the year 2018. According to the 2019 data by WHO, this disease is considered one of the top ten deadliest diseases. It cannot be completely cured but proper management with inhaled medications can help to control the disease and thereby help people to lead normal life [ 10 ]. Around 262 million people were affected by this deadly disease in 2019 which caused 461,000 deaths. Globally, this disease is ranked 16th among the leading causes of years lived with a disability as well as 28th among the leading causes of burden of disease as calculated by DALY (disability-adjusted life years). It is estimated that around 300 million people were suffering from asthma worldwide and by 2025 around 100 million people were affected. There is a huge geographical variation in asthma severity, prevalence, and mortality. The prevalence is extremely high in high-income countries whereas the mortality rate is high in low-middle-income countries. As per the Lancet, the asthma statistics worldwide for 2020 reported that more than 339 million people were suffering from asthma and globally approx. four million children develop asthma each year. In North America, approx. 8% population has been diagnosed with asthma. The estimated prevalence of severe asthma is 5–10% of the global asthma population. It is more common in Puerto Rican Hispanic (13.3%) and Black (8.7%) than in white people (7.6%). The mortality rate is higher in black 25.4 than in whites 8.8 per million annually. The treatment options available for asthma are discussed as follows:
Bronchodilators or relievers act by quickly opening the airways and improving the rate of breathing. They also remove mucous from the lungs. As the airways get dilated, the mucous can be coughed with more ease. These act by targeting the β-2 adrenergic receptors in the airways. Activation of this receptor may relax the airway smooth muscles, thereby ensuring better airflow in the lungs [ 11 ]. Furthermore, they also help in inhibiting the parasympathetic nervous system receptors from functioning. As the parasympathetic nervous system increases the bronchial secretions and constriction in airways, inhibiting the nervous system should result in bronchodilation and lesser bronchial secretion [ 12 ] (Fig. 2 ). Bronchodilators are subdivided into the following parts (Fig. 3 ), Inhaled rapid-acting β-2 agonists: Fenoterol (1), Salbutamol (2), Isoproterenol (3), Metaproterenol (4), Terbutaline (5), Albuterol (6), Glucocorticoids (systemic): Beclomethasone (7), Prednisone (8), Triamcinolone (9), Budesonide (10), Flunisonide (11), Anticholinergics: Tiotropium bromide (12), Ipratropium bromide (13), Atropine methonitrate (14), Oxitropium bromide (15), Xanthine derivatives: Caffeine (16), Theobromine (17), Theophylline (18), Aminophylline (19), Hydroxyethyl theophylline (20), Choline theophyllinate (21), Doxophylline (22), Deriphylline (23), Diprophylline (24), Theophylline ethanolate of piperazine (25), Oral SABA: Salbutamol (2), Terbutaline (5), Bitolterol (26), Fenoterol (27), Rimiterol (28), Levalbuterol (29), and Pirbuterol (30).
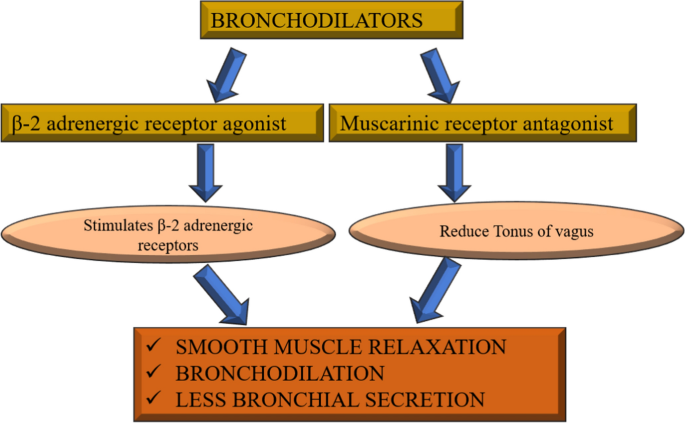
Mechanism of action of bronchodilators in asthma
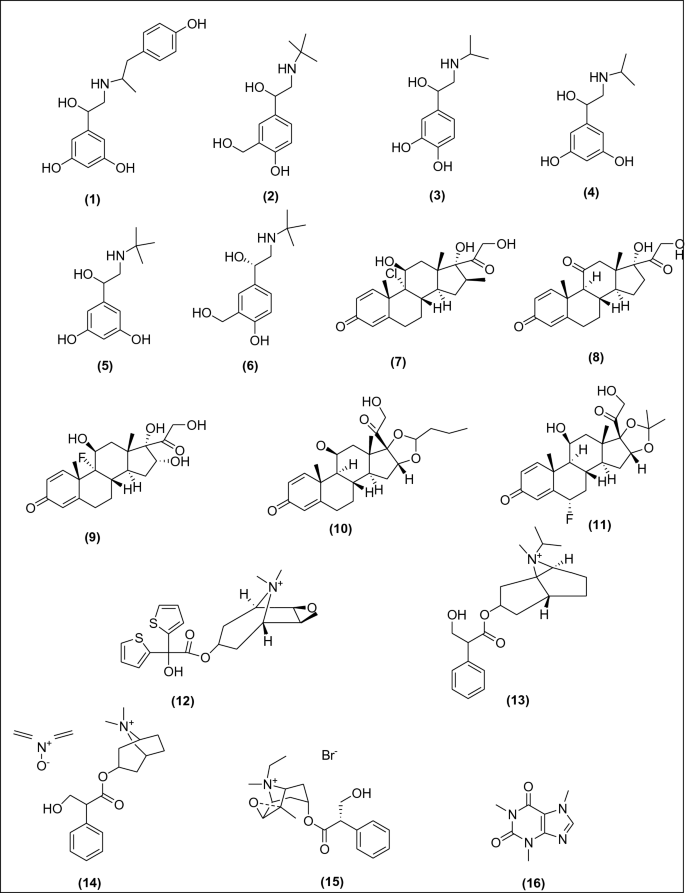
Anti-asthmatic drugs used as bronchodilators
Anti-inflammatory agents reduce inflammation, swelling, and mucus production in the airways. The most important anti-inflammatory treatments are given by inhalation. Their mode of action is not completely understood, but they are likely to act in several different ways to produce an anti-inflammatory effect. The glucocorticoids act by inhibiting transcription factors that help in the regulation of pro-inflammatory mediators such as eosinophils, macrophages, dendritic cells, mast cells, and lymphocytes [ 13 ]. The steroids also act on mast cells and exert their anti-allergic action by inhibiting the signaling pathways in mast cells [ 14 ]. Furthermore, they also reduce plasma exudation in the airways and inhibit mucus glycoprotein secretion (Fig. 4 ). Anti-inflammatory agents are further classified into (Fig. 5 ), Inhaled or systemic corticosteroids: Triamcinolone (31), Mometasone (32), Budesonide (33), Prednisolone (34), Hydrocortisone (35), Beclomethasone (36), Fluticasone (37), Ciclesonide (38), Flunisolide (39), prednisone (40), Methylprednisolone (41), LABA: Formoterol (42), Salmeterol (43), Anti-IgE: Omalizumab, Leukotriene antagonist: Zafirlukast (44), Montelukast (45), Pranlukast (46), Iralukast (47), Oral anti-allergic compounds: Tranilast (48), Mast cell stabilizer: Sodium cromoglycate (49), Nedocromil Sodium (50), and Ketotifen (51).
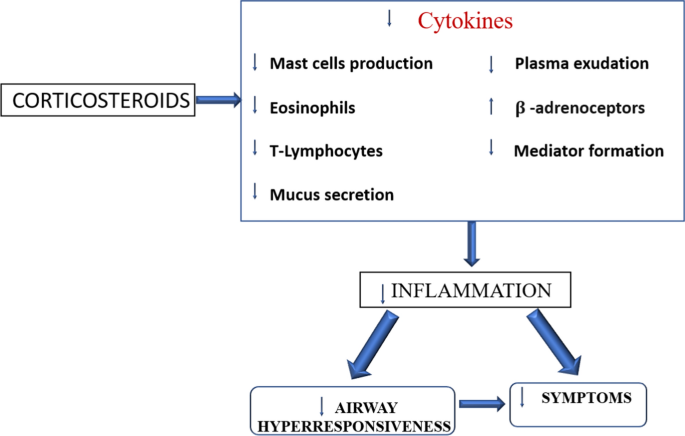
Mechanism of action of corticosteroids on airway inflammation, symptoms and airway hyper-responsiveness
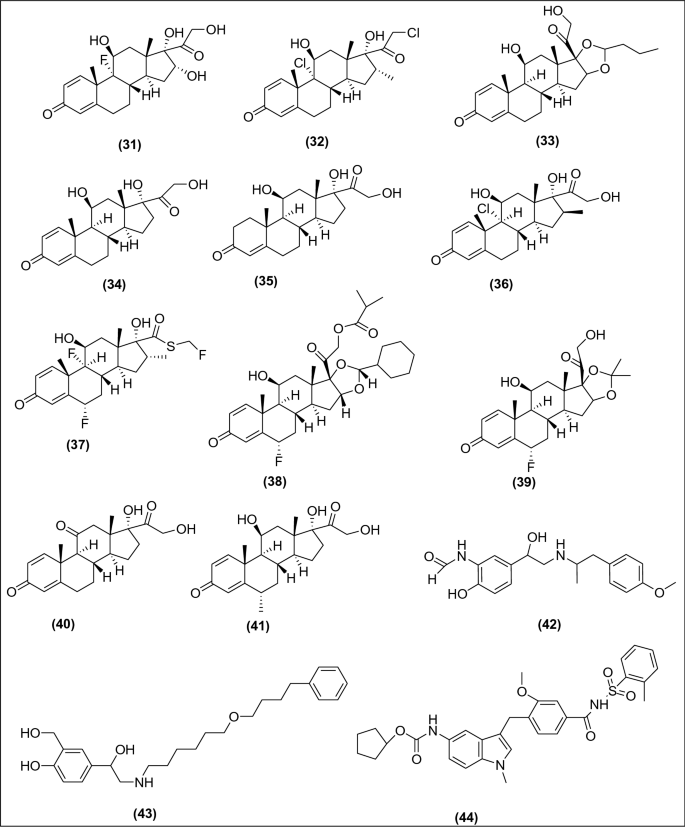
Anti-inflammatory drugs used for asthma
Indian Scenario
The Indians ayurveda believe that asthma results due to the imbalance between three doshas: (a) pitta (bile), (b) Kapha (phlegm), and (c) vata (wind). A person stays healthy if these three humors were balanced. The first book Ayurveda Materia medica from India ‘Charaka Samhita’ has a good clinical description of this life-threatening disease. A recent study on respiratory symptoms and chronic bronchitis performed on 85,105 men and 84,470 women from eleven rural and twelve urban areas in India estimated the prevalence rate of asthma is 2.05% among those aged above 15 years with an estimated national burden causing 18 million asthmatics [ 15 ]. Despite enormous advancements in the treatment and management of this disease, it becomes a major public health issue in India.
Asthma Control History
The early period of asthma control.
In 1500BC, the inhalation of the smoke of herbs is recommended for use as the treatment therapy for asthmatic patients in Egypt. In ancient China around 5000 years ago, the treatment was done by using ma-huang (Ephedra sinica), a type of Chinese herb which was later examined to have ephedrine (muscle relaxant), and these agents work as bronchodilators [ 6 , 13 ]. For a prolonged period, bronchodilators were used as the first-line drugs for the management of asthma which indicates contraction of airways as the chief pathology involved in the treatment. In 1900, the avoidance of allergens was used as the foremost therapy for asthma [ 5 ]. The use of a pressurized metered-dose inhaler in the mid-1950 has been developed for the administration of adrenaline and isoproterenol and was later used as a β2-adrenergic agonist. Later salbutamol and terbutaline were introduced as SABA. Recently, LABA is used as the principal drug incorporated into the inhaled corticosteroids in Japanese guidelines for asthma. Furthermore, LTRA and theophylline were used as the first-line drugs along with LABA and inhaled corticosteroids. The American thoracic society in the year 1962 describes asthma as a disease identified by the presence of airway hyper-responsiveness as well as reversible airway constriction [ 12 ]. Moreover, chronic airway inflammation was finally found as the clinical etiology involved in the pathogenesis of asthma and inhaled corticosteroids and the use of anti-inflammatory drugs became the first-line therapy for asthmatic patients [ 16 ]. In the early twentieth century, inhalation and intravenous administration of anticholinergic drugs were regarded as the principal therapy for asthma [ 2 ].
Current WHO-Aided Asthma Control Program
For the prevention and control of asthma, this disease has been incorporated in the WHO global action plan as well as the UN (United Nations) 2030 agenda for the sustainable development. WHO has taken several actions to extend the diagnosis and treatment of this disease. The PEN (package of essential non-communicable) disease intervention was developed by WHO to support people with non-communicable diseases with the help of UHC (universal health coverage) [ 17 ]. The PEN includes rules for assessment, diagnosis, and management of asthma and (COPD) chronic obstructive pulmonary disease and includes modules on healthy lifestyles (Fig. 6 ) [ 18 ]. The primary preventive measure taken for asthma and disease management is reducing tobacco smoke exposure, and the initiative MPOWER and Mtobacco cessation is enabling progress in this area of tobacco control. MPOWER is the WHO framework convention on tobacco control, and its guidelines were meant for countries working toward tobacco control. These guidelines were introduced in the year 2008 to manage tobacco control at the country level.
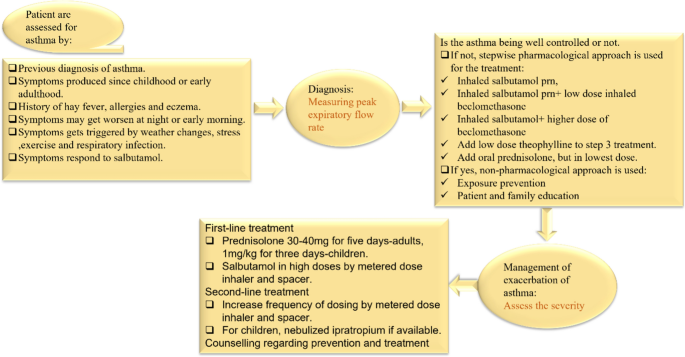
Assessment of asthma as per WHO PEN
WHO Global Action Plan 2013–2020
The goal of this action plan is to reduce the number of morbidities, mortality, and disability due to NCD by using multisectoral cooperation and collaboration at distinct levels (national, regional, and global), so that the population will remain at the highest standard of health and productivity at all ages as well as those diseases will no longer act as a barrier to well-being. As per the WHO, the total number of deaths due to NCD may increase to 55 million by 2030. The scientific knowledge demonstrates that the prevalence of non-communicable diseases is greatly decreased if cost-effective preventive and curative action, as well as interventions for prevention and control of NCD which are already available, are implemented in a balanced and effective manner [ 19 ].
GINA Global Strategy for Asthma 2021
On Nov 1, 2021, the GINA published an executive summary of an updated evidence-based summary for the treatment and prevention of asthma. On Oct 18, 2021, the summary was published online. The GINA science committee was developed in the year 2002 to review published research on asthma. This GINA report is updated every year and approx. 500,000 copies of GINA reports were downloaded each year by one hundred countries [ 20 ]. GINA report has been updated in the year 2020 with some modifications such as interim guidance about asthma and Covid-19, additional information for the new as well as existing therapies; additional documents have been added in supporting the use of ICS (Inhaled corticosteroid)—formoterol in mild asthma; assessment of symptom control and new data have been incorporated for the initial treatment of newly diagnosed asthma; information related to a maximum daily dose of ICS-Formoterol has been added; additional documents for the support of the use of ICS and addition of minimum and maximum doses of ICS have been incorporated in the treatment recommendation for asthma, and new additional information about the management of asthma in children has also been added [ 21 ].
India Asthma Report
As per demographics, around 6% of children and 2% of adults were suffering from this disease. A maximum number of people in India have no health insurance, and there is a big gap in healthcare facilities for the poor and the rich people. Most of the medications available in India (inhaled corticosteroids, combination inhalers, and β-2 agonists) are too expensive compared to oral formulations [ 22 ]. According to the data compiled from 1990 to 2005, the mortality rate in India decreased mainly in areas where healthcare facilities were better (urban areas and prosperous states). It was documented that Rajasthan and Uttar Pradesh have the highest mortality rate. The Rajasthan government had provided free access to medicines to all the asthmatic patients of the state at government hospitals since 2011 and around 15,000 pharmacies had been opened by the state government across the state along with a free supply of metered-dose inhalers, nebulizer solutions, and dry powder inhaler capsules to asthmatic patients. In 2018, the Indian government planned to provide health insurance at no cost to 100 million low-income families, to cover their treatment costs [ 23 ].
Ongoing Challenges in Asthma Therapy
The problem of asthma is a global burden affecting more than 300 million people and causing around 2,50,000 deaths per year. Despite several effective treatments available, the control of this disease in the population remains inadequate. The advancement in treatments for children is lesser as compared to the adults due to the varying immunopathology, respiratory pathology, need for a child, parent education, and communication barrier. As most of the asthma research work was performed on adult asthma, thus this seems to be one of the principal barriers to managing the therapy childhood asthma [ 16 ]. The data on LABA use for the treatment of asthma in adults are widely available while the data available for LABA use in children are limited. Since then, several studies have been conducted to complete the gap for LABA use in children and adolescents resulting in several regulatory approvals for LABA inhalers, and inhaled corticosteroids such as fluticasone + salmeterol, budesonide + formoterol have been approved as maintenance treatment for children and adolescents in the USA and Europe [ 24 , 25 ]. Asthma management in children is a complex process due to variability in asthma severity, control, and difficulty in measuring lung function as well as airway inflammation. The primary challenge in the management of pediatric asthma is treating the symptoms of asthma rather than treating the root cause, i.e., inflammation, and switching to controller therapy when the problem worsens. The prevalence of childhood asthma increased in the 1980s–1990s, and the rate kept on increasing over the past decade; it seems to be one of the greatest global economic burdens in terms of direct and indirect costs.
Furthermore, the healthcare providers, as well as patients, are dealing with several types of challenges such as challenges in diagnosis, treatment, and follow-up challenges. As poor healthcare facilities are provided in rural areas, poverty, lack of awareness, and the high price of anti-asthmatic drugs are some of the routinely faced challenges of patients [ 26 ]. The diagnosis of asthma seems to be challenging work, both in terms of underdiagnosis and overdiagnosis. The underdiagnosis of asthma is familiar and was documented in epidemiological as well as clinical studies while the data on overdiagnosis are new [ 27 ]. Physicians are entirely dependent on asthma guidelines for the diagnosis and management of this disease. The NIH (National Institute of health) released latest updates to the national guidelines meant for the diagnosis, management, and treatment of asthma. The guidelines were made to upgrade patient care and to support decision-making about asthma management in a clinical setting.
In India, the national rural health mission (NRHM) was implemented to improve primary healthcare facilities in rural areas, to improve the health status and quality of life of people living in rural areas, and to prevent and control communicable and non-communicable diseases. The diagnosis of asthma is a difficult process because for some reasons: (a) The signs and symptoms might not show during routine analysis, (b) unavailability of the standard diagnostic test—in clinical practice, spirometry and peak expiratory flow assessment are done to check the signs and symptoms, and (c) The guideline recommendation is not always compatible with the working systems in primary care. Some of the other treatment options which might help in improving asthma management and control are switching from relievers SABA to LABA along with a combination of inhaled corticosteroids as per the recommendation of GINA to make sure that the person with asthma receives an inhaled corticosteroid to get symptomatic relief whenever possible.
Ongoing Asthma Management Programs
The problem of asthma is prevalent among children and elderly people. In UK 1 in 14 adults are affected by this alarming condition. The national public health agency of the USA, i.e., CDC has made a self-management education (SME) program “Breathe well, live well” that helps those people with prevailing health conditions to feel better. The SME program helps people to strategize and develop the skills and confidence to tackle ongoing health conditions efficiently and help in dealing with the following conditions: cope with symptoms, communicate with doctors, manage fatigue, handle stress, manage medication, eat healthy, reduce depression, and be active. These strategies can help the patients to make good decisions about health and makes them feel better [ 28 ].
The 2020 focused updates to the asthma management guidelines were published for the diagnosis and management of asthma. These guidelines help the clinician integrate the new recommendation into clinical care. These are meant for individual patient management [ 29 ]. The Alameda County public health department (ACPHD) enabled community health services asthma start programs that help families of children with asthma by providing in-home case management studies. They provide education, support, and assistance in developing an action plan to address the needs of families where the child has asthma thereby helping in regulating it. The services provided by them is as follows: (a) education to families about the disease, several types of triggers, prevention of attacks, treatments, etc., (b) collaborating with daycare providers and schools to make sure asthma medication is accessible to every child, and moreover, supplying asthma-related education to all the school staff as well as daycare providers, (c) assistance with health insurance, housing, and employment, and (d) remote home inspections to find the triggers and causes of asthma [ 30 ].
Results and Discussion
Generally, the recommendations from different professional bodies suggest that physicians should follow the already existing guidelines for the proper management of this disease. The key points are as follows: bronchodilators were considered a principal therapy for the treatment of asthma in early times, but after the advent of inhaled corticosteroids, the therapeutic history gets drastically changed. The use of bronchodilators is the principal therapy used in asthma but a greater understanding of the chief role of inflammation in the pathogenesis of asthma has led to the conclusion of the use of anti-allergic or anti-inflammatory agents for the management of asthma. The ICS can provide ideal disease control but not as monotherapy. They need additional therapies such as SABA, LABA, LTRA, and theophylline to achieve adequate control.
It is very much clear from the above discussion that we have done so much advancement to fight against this deadly disease and we still need time to make the globe asthma-free. The number of people suffering from asthma is more than the number of people suffering from HIV infection and tuberculosis.
Understanding the recommendations of professional bodies will assist in medical decision-making in asthma management. Healthcare professionals should consider the individual needs of patients. In conclusion, the main problem in the management of this disease is improper use of healthcare facilities, lack of knowledge about anti-asthmatic drugs, poverty, and the cost of drugs. The government should make and adopt more strategies to promote the rational use of anti-asthmatic drugs and make plans to spread more awareness among people about the schemes and programs made for safeguarding people against this life-threatening disease.
Löwhagen O (2015) Diagnosis of asthma–new theories. J Asthma 67(6):713–717. https://doi.org/10.3109/02770903.2014.991971
Article CAS Google Scholar
Stein SW, Thiel CG (2017) The history of therapeutic aerosols: a chronological review. J Aerosol Med Pulm Drug Deliv 30(1):20–41. https://doi.org/10.1089/jamp.2016.1297
Article PubMed PubMed Central Google Scholar
Bergmann KC (2014) Asthma. Chem Immunol Allergy 100:69–80. https://doi.org/10.1159/000358575
Article PubMed Google Scholar
Rothe TA (2018) Century of “intrinsic asthma.” Allergo J 27:19–23. https://doi.org/10.1007/s15007-018-1719-3
Article Google Scholar
Sanders MJ (2017) Guiding inspiratory flow: development of the in-check DIAL G16, a tool for improving inhaler technique. Pulm Med. https://doi.org/10.1155/2017/1495867
Beasley R, Harper J, Bird G et al (2019) Inhaled corticosteroid therapy in adult asthma: time for a new therapeutic dose terminology. Am J Respir Crit Care Med 199(12):1471–1477. https://doi.org/10.1164/rccm.201810-1868ci
Article CAS PubMed Google Scholar
Silverman RA, Hasegawa K, Egan DJ et al (2017) Multicenter study of cigarette smoking among adults with asthma exacerbations in the emergency department, 2011–2012. Respir Med 125:89–91. https://doi.org/10.1016/j.rmed.2017.02.004
Quirt J, Hildebrand KJ, Mazza J et al (2018) Asthma. Allergy Asthma Clin Immunol 14:15–30. https://doi.org/10.1186/s13223-018-0279-0
Centers for Disease Control and Prevention (2018) Usual place for medical care among children, pp 13–17. https://www.cdc.gov/nchs/data/nhis/earlyrelease/EarlyRelease201803_02.pdf . Accessed 8 April 2021
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1204–1222. Erratum in: Lancet. 2020; 396(10262):1562. https://doi.org/10.1016/s0140-6736(20)30925-9
Matera MG, Page CP, Calzetta L et al (2020) Pharmacology and therapeutics of bronchodilators revisited. Pharmacol Rev 72(1):218–252. https://doi.org/10.1124/pr.119.018150
Harma S, Hashmi MF, Chakraborty RK (2021) Asthma medications. StatPearls Publishing, Treasure Island
Google Scholar
Williams DM (2018) Clinical pharmacology of corticosteroids. Respir Care 63(6):655–670. https://doi.org/10.4187/respcare.06314
Oppong E, Flink N, Cato ACB (2013) Molecular mechanisms of glucocorticoid action in mast cells. Mol Cell Endocrinol 380(1–2):119–126. https://doi.org/10.1016/j.mce.2013.05.014
Joshi KS, Nesari TM, Dedge AP et al (2016) Dosha phenotype specific Ayurveda intervention improves asthma symptoms through cytokine modulations: results of whole system clinical trial. J Ethnopharmacol 197:110–117. https://doi.org/10.1016/j.jep.2016.07.071
Barcik W, Boutin RCT, Sokolowska M, Finlay BB (2020) The role of lung and gut microbiota in the pathology of asthma. Immunity 52(2):241–255. https://doi.org/10.1016/j.immuni.2020.01.007
Article CAS PubMed PubMed Central Google Scholar
World Health Organization (2021) factsheet: Asthma. https://www.who.int/news-room/fact-sheets/detail/asthma . Accessed 17 April 2021
World Health Organization (2020) package of essential non communicable (PEN) disease interventions for primary healthcare. https://www.who.int/publications/i/item/who-package-of-essential-noncommunicable-(pen)-disease-interventions-for-primary-health-care . Accessed 24 April 2021
World Health Organization (2013) Global action plan for the prevention and control of non-communicable diseases 2013–2020. https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1 . Accessed 2 May 2021
Global Initiative for Asthma (GINA) (2021) Global strategy for asthma management and prevention. https://ginasthma.org/wp-content/uploads/2021/07/GINA-2021_Methodology_20210523.pdf . Accessed 12 May 2021
Global Initiative for Asthma (GINA) (2020) Pocket guide for asthma management and prevention for adults and children (updated 2020). https://ginasthma.org/wp-content/uploads/2020/04/Main-pocket-guide_2020_04_03-final-wms.pdf . Accessed 17 June 2021
The Global Asthma Report (2018) http://globalasthmareport.org/management/india.php . Accessed 22 June 2021
Centers for Disease Control and Prevention (2019) Most recent national asthma data. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm . Accessed 8 Aug 2021
Szefler SJ, Chipps B (2018) Challenges in the treatment of asthma in children and adolescents. Ann Allergy Asthma Immunol 120(4):382–388. https://doi.org/10.1016/j.anai.2018.01.003
Pearlman DS, Eckerwall G, McLaren J et al (2017) Efficacy and safety of budesonide/formoterol pMDI vs budesonide pMDI in asthmatic children (6–<12years). Ann Allergy Asthma Immunol 118:489–499. https://doi.org/10.1016/j.anai.2017.01.020
Bakirtas A (2017) Diagnostic challenges of childhood asthma. Curr Opin Pulm Med 23(1):27–33. https://doi.org/10.1097/MCP.0000000000000338
Aaron SD, Boulet LP, Reddel HK, Gershon A (2018) Under-diagnosis and over-diagnosis of asthma. Am J Respir Crit Care Med 198(8):1–25. https://doi.org/10.1164/rccm.201804-0682ci
Centers for Disease Control and Prevention. Managing asthma. https://www.cdc.gov/learnmorefeelbetter/programs/asthma.htm . Accessed 15 Aug 2021
2020 Focused updates to the asthma management guidelines (2020) Briefly guide. https://www.nhlbi.nih.gov/sites/default/files/publications/AsthmaClinicians-At-a-Glance-508.pdf . Accessed 10 Sept 2021
Alameda County Public Health Department. Asthma Start program. https://acphd.org/asthma/ . Accessed 30 Oct 2021
Download references
Acknowledgements
The authors are thankful to the Honorable Vice-Chancellor, Banasthali Vidyapith, Banasthali, Rajasthan, for providing essential facilities.
There was no funding provided for the preparation of the manuscript.
Author information
Authors and affiliations.
Department of Pharmacy, Banasthali Vidyapith, Banasthali, Rajasthan, 304022, India
Anandi Kapri, Swati Pant, Sarvesh Paliwal & Sumitra Nain
Agilent Technologies Pvt. Ltd., 181/46, Industrial Area, Phase-1, Chandigarh, 160002, India
Nitin Gupta
You can also search for this author in PubMed Google Scholar
Contributions
Nitin Gupta contributed to Conception and design of study, Swati Pant contributed to literature collection and Anandi Kapri contributed to Drafting the manuscript and Sumitra Nain & Sarvesh Paliwal contributed to Overall supervision.
Corresponding author
Correspondence to Sumitra Nain .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Significance Statement: This review paper aims to spread awareness among the general public about the scenario of Asthma. The physicians should prescribe bronchodilators and anti-inflammatory agents to manage asthma symptoms.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Kapri, A., Pant, S., Gupta, N. et al. Asthma History, Current Situation, an Overview of Its Control History, Challenges, and Ongoing Management Programs: An Updated Review. Proc. Natl. Acad. Sci., India, Sect. B Biol. Sci. 93 , 539–551 (2023). https://doi.org/10.1007/s40011-022-01428-1
Download citation
Received : 23 January 2022
Revised : 03 August 2022
Accepted : 31 August 2022
Published : 11 November 2022
Issue Date : September 2023
DOI : https://doi.org/10.1007/s40011-022-01428-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Respiratory
- Healthcare professionals
- Anti-asthmatic drugs
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 15 August 2020
Treatment strategies for asthma: reshaping the concept of asthma management
- Alberto Papi 1 , 7 ,
- Francesco Blasi 2 , 3 ,
- Giorgio Walter Canonica 4 ,
- Luca Morandi 1 , 7 ,
- Luca Richeldi 5 &
- Andrea Rossi 6
Allergy, Asthma & Clinical Immunology volume 16 , Article number: 75 ( 2020 ) Cite this article
44k Accesses
51 Citations
4 Altmetric
Metrics details
Asthma is a common chronic disease characterized by episodic or persistent respiratory symptoms and airflow limitation. Asthma treatment is based on a stepwise and control-based approach that involves an iterative cycle of assessment, adjustment of the treatment and review of the response aimed to minimize symptom burden and risk of exacerbations. Anti-inflammatory treatment is the mainstay of asthma management. In this review we will discuss the rationale and barriers to the treatment of asthma that may result in poor outcomes. The benefits of currently available treatments and the possible strategies to overcome the barriers that limit the achievement of asthma control in real-life conditions and how these led to the GINA 2019 guidelines for asthma treatment and prevention will also be discussed.
Asthma, a major global health problem affecting as many as 235 million people worldwide [ 1 ], is a common, non-communicable, and variable chronic disease that can result in episodic or persistent respiratory symptoms (e.g. shortness of breath, wheezing, chest tightness, cough) and airflow limitation, the latter being due to bronchoconstriction, airway wall thickening, and increased mucus.
The pathophysiology of the disease is complex and heterogeneous, involving various host-environment interactions occurring at various scales, from genes to organ [ 2 ].
Asthma is a chronic disease requiring ongoing and comprehensive treatment aimed to reduce the symptom burden (i.e. good symptom control while maintaining normal activity levels), and minimize the risk of adverse events such as exacerbations, fixed airflow limitation and treatment side effects [ 3 , 4 ].
Asthma treatment is based on a stepwise approach. The management of the patient is control-based; that is, it involves an iterative cycle of assessment (e.g. symptoms, risk factors, etc.), adjustment of treatment (i.e. pharmacological, non-pharmacological and treatment of modifiable risk factors) and review of the response (e.g. symptoms, side effects, exacerbations, etc.). Patients’ preferences should be taken into account and effective asthma management should be the result of a partnership between the health care provider and the person with asthma, particularly when considering that patients and clinicians might aim for different goals [ 4 ].
This review will discuss the rationale and barriers to the treatment of asthma, that may result in poor patient outcomes. The benefits of currently available treatments and the possible strategies to overcome the barriers that limit the achievement of asthma control in real-life situations will also be discussed.
The treatment of asthma: where are we? Evolution of a concept
Asthma control medications reduce airway inflammation and help to prevent asthma symptoms; among these, inhaled corticosteroids (ICS) are the mainstay in the treatment of asthma, whereas quick-relief (reliever) or rescue medicines quickly ease symptoms that may arise acutely. Among these, short-acting beta-agonists (SABAs) rapidly reduce airway bronchoconstriction (causing relaxation of airway smooth muscles).
National and international guidelines have recommended SABAs as first-line treatment for patients with mild asthma, since the Global Initiative for Asthma guidelines (GINA) were first published in 1995, adopting an approach aimed to control the symptoms rather than the underlying condition; a SABA has been the recommended rescue medication for rapid symptom relief. This approach stems from the dated idea that asthma symptoms are related to bronchial smooth muscle contraction (bronchoconstriction) rather than a condition concomitantly caused by airway inflammation. In 2019, the GINA guidelines review (GINA 2019) [ 4 ] introduced substantial changes overcoming some of the limitations and “weaknesses” of the previously proposed stepwise approach to adjusting asthma treatment for individual patients. The concept of an anti-inflammatory reliever has been adopted at all degrees of severity as a crucial component in the management of the disease, increasing the efficacy of the treatment while lowering SABA risks associated with patients’ tendency to rely or over-rely on the as-needed medication.
Until 2017, the GINA strategy proposed a pharmacological approach based on a controller treatment (an anti-inflammatory, the pillar of asthma treatment), with a SABA as an additional rescue intervention. The reliever, a short-acting bronc hodilator, was merely an addendum , a medication to be used in case the real treatment (the controller) failed to maintain disease control: SABAs effectively induce rapid symptom relief but are ineffective on the underlying inflammatory process. Based on the requirement to achieve control, the intensity of the controller treatment was related to the severity of the disease, varying from low-dose ICS to combination low-dose ICS/long-acting beta-agonist (LABA), medium-dose ICS/LABA, up to high-dose ICS/LABA, as preferred controller choice, with a SABA as the rescue medication. As a result, milder patients were left without any anti-inflammatory treatment and could only rely on SABA rescue treatment.
Poor adherence to therapy is a major limitation of a treatment strategy based on the early introduction of the regular use of controller therapy [ 5 ]. Indeed, a number of surveys have highlighted a common pattern in the use of inhaled medication [ 6 ], in which treatment is administered only when asthma symptoms occur; in the absence of symptoms, treatment is avoided as patients perceive it as unnecessary. When symptoms worsen, patients prefer to use reliever therapies, which may result in the overuse of SABAs [ 7 ]. Indirect evidence suggests that the overuse of beta-agonists alone is associated with increased risk of death from asthma [ 8 ].
In patients with mild persistent disease, low-dose ICS decreases the risk of severe exacerbations leading to hospitalization and improves asthma control [ 9 ]. When low-dose ICS are ineffective in controlling the disease (Step 3 of the stepwise approach), a combination of low-dose ICS with LABA maintenance was the recommended first-choice treatment, plus as-needed SABA [ 3 , 10 ]. Alternatively, the combination low-dose ICS/LABA (formoterol) was to be used as single maintenance and reliever treatment (SMART). The SMART strategy containing the rapid-acting formoterol was recommended throughout GINA Steps 3 to 5 based on solid clinical-data evidence [ 3 ].
The addition of a LABA to ICS treatment reduces both severe and mild asthma exacerbation rates, as shown in the one-year, randomized, double-blind, parallel-group FACET study [ 11 ]. This study focused on patients with persistent asthma symptoms despite receiving ICS and investigated the efficacy of the addition of formoterol to two dose levels of budesonide (100 and 400 µg bid ) in decreasing the incidence of both severe and mild asthma exacerbations. Adding formoterol decreased the incidence of both severe and mild asthma exacerbations, independent of ICS dose. Severe and mild exacerbation rates were reduced by 26% and 40%, respectively, with the addition of formoterol to the lower dose of budesonide; the corresponding reductions were 63% and 62%, respectively, when formoterol was added to budesonide at the higher dose.
The efficacy of the ICS/LABA combination was confirmed in the post hoc analysis of the FACET study, in which patients were exposed to a combination of formoterol and low-dose budesonide [ 12 ]. However, such high levels of asthma control are not achieved in real life [ 5 ]. An explanation for this is that asthma is a variable condition and this variability might include the exposure of patients to factors which may cause a transient steroid insensitivity in the inflammatory process. This, in turn, may lead to an uncontrolled inflammatory response and to exacerbations, despite optimal controller treatment. A typical example of this mechanism is given by viral infections, the most frequent triggers of asthma exacerbations. Rhinoviruses, the most common viruses found in patients with asthma exacerbations, interfere with the mechanism of action of corticosteroids making the anti-inflammatory treatment transiently ineffective. A transient increase in the anti-inflammatory dose would overcome the trigger-induced anti-inflammatory resistance, avoiding uncontrolled inflammation leading to an exacerbation episode [ 13 , 14 , 15 ].
Indeed, symptoms are associated with worsening inflammation and not only with bronchoconstriction. Romagnoli et al. showed that inflammation, as evidenced by sputum eosinophilia and eosinophilic markers, is associated with symptomatic asthma [ 16 ]. A transient escalation of the ICS dose would prevent loss of control over inflammation and decrease the risk of progression toward an acute episode. In real life, when experiencing a deterioration of asthma control, patients self-treat by substantially increasing their SABA medication (Fig. 1 ); it is only subsequently that they (modestly) increase the maintenance treatment [ 17 ].
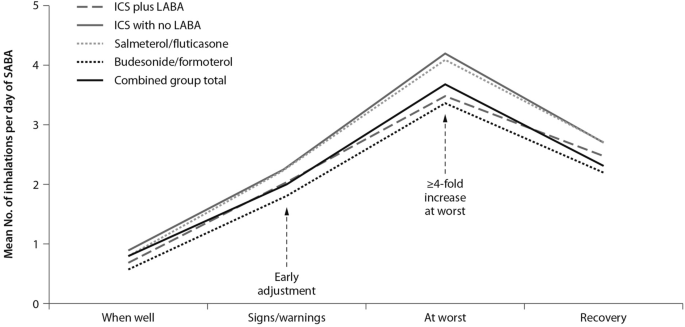
Mean use of SABA at different stages of asthma worsening. Patients have been grouped according to maintenance therapy shown in the legend. From [ 17 ], modified
As bronchodilators, SABAs do not control the underlying inflammation associated with increased symptoms. The “as required” use of SABAs is not the most effective therapeutic option in controlling a worsening of inflammation, as signaled by the occurrence of symptoms; instead, an anti-inflammatory therapy included in the rescue medication along with a rapid-acting bronchodilator could provide both rapid symptom relief and control over the underlying inflammation. Thus, there is a need for a paradigm shift, a new therapeutic approach based on the rescue use of an inhaled rapid-acting beta-agonist combined with an ICS: an anti-inflammatory reliever strategy [ 18 ].
The symptoms of an exacerbation episode, as reported by Tattersfield and colleagues in their extension of the FACET study, increase gradually before the peak of the exacerbation (Fig. 2 ); and the best marker of worsening asthma is the increased use of rescue beta-agonist treatment that follows exactly the pattern of worsening symptomatology [ 19 ]. When an ICS is administered with the rescue bronchodilator, the patient would receive anti-inflammatory therapy when it is required; that is, when the inflammation is uncontrolled, thus increasing the efficiency of the anti-inflammatory treatment.
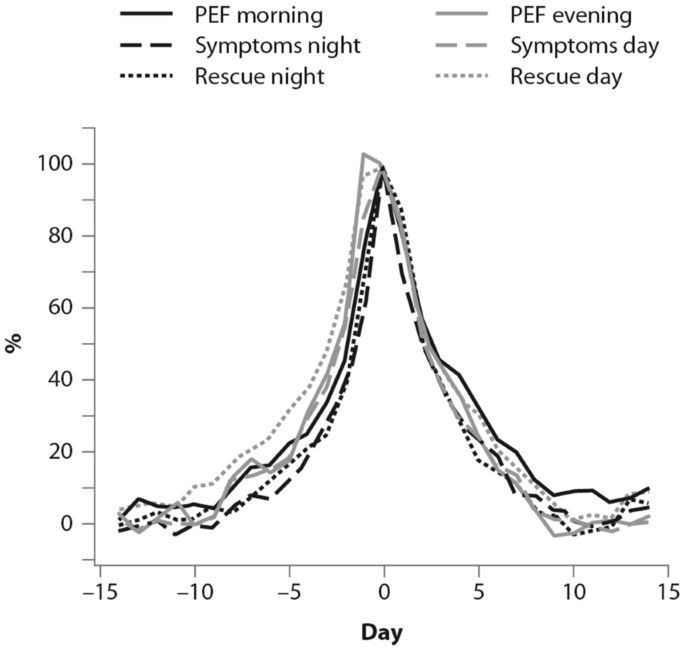
(From [ 19 ])
Percent variation in symptoms, rescue beta-agonist use and peak expiratory flow (PEF) during an exacerbation. In order to allow comparison over time, data have been standardized (Day-14 = 0%; maximum change = 100%)
Barriers and paradoxes of asthma management
A number of barriers and controversies in the pharmacological treatment of asthma have prevented the achievement of effective disease management [ 20 ]. O’Byrne and colleagues described several such controversies in a commentary published in 2017, including: (1) the recommendation in Step 1 of earlier guidelines for SABA bronchodilator use alone, despite asthma being a chronic inflammatory condition; and (2) the autonomy given to patients over perception of need and disease control at Step 1, as opposed to the recommendation of a fixed-dose approach with treatment-step increase, regardless of the level of symptoms [ 20 ]. Other controversies outlined were: (3) a difficulty for patients in understanding the recommendation to minimize SABA use at Step 2 and switch to a fixed-dose ICS regimen, when they perceive SABA use as more effective; (4) apparent conflicting safety messages within the guidelines that patient-administered SABA monotherapy is safe, but patient-administered LABA monotherapy is not; and (5) a discrepancy as to patients’ understanding of “controlled asthma” and their symptom frequency, impact and severity [ 20 ].
Controversies (1) and (2) can both establish an early over-dependence on SABAs. Indeed, asthma patients freely use (and possibly overuse) SABAs as rescue medication. UK registry data have recently suggested SABA overuse or overreliance may be linked to asthma-related deaths: among 165 patients on short-acting relievers at the time of death, 56%, 39%, and 4% had been prescribed > 6, > 12, and > 50 SABA inhalers respectively in the previous year [ 21 ]. Registry studies have shown the number of SABA canisters used per year to be directly related to the risk of death in patients with asthma. Conversely, the number of ICS canisters used per year is inversely related to the rate of death from asthma, when compared with non-users of ICS [ 8 , 22 ]. Furthermore, low-dose ICS used regularly are associated with a decreased risk of asthma death, with discontinuation of these agents possibly detrimental [ 22 ].
Other barriers to asthma pharmacotherapy have included the suggestion that prolonged treatment with LABAs may mask airway inflammation or promote tolerance to their effects. Investigating this, Pauwels and colleagues found that in patients with asthma symptoms that were persistent despite taking inhaled glucocorticoids, the addition of regular treatment with formoterol to budesonide for a 12-month period did not decrease asthma control, and improved asthma symptoms and lung function [ 11 ].
Treatment strategies across all levels of asthma severity
Focusing on risk reduction, the 2014 update of the GINA guidelines recommended as-needed SABA for Step 1 of the stepwise treatment approach, with low-dose ICS maintenance therapy as an alternative approach for long-term anti-inflammatory treatment [ 23 ]. Such a strategy was only supported by the evidence from a post hoc efficacy analysis of the START study in patients with recently diagnosed mild asthma [ 24 ]. The authors showed that low-dose budesonide reduced the decline of lung-function over 3 years and consistently reduced severe exacerbations, regardless of symptom frequency at baseline, even in subjects with symptoms below the then-threshold of eligibility for ICS [ 24 ]. However, as for all post hoc analyses, the study by Reddel and colleagues does not provide conclusive evidence and, even so, their results could have questionable clinical significance for the management of patients with early mild asthma. To be effective, this approach would require patients to be compliant to regular twice-daily ICS for 10 years to have the number of exacerbations reduce by one. In real life, it is highly unlikely that patients with mild asthma would adhere to such a regular regimen [ 25 ].
The 2016 update to the GINA guidelines lowered the threshold for the use of low-dose ICS (GINA Step 2) to two episodes of asthma symptoms per month (in the absence of any supportive evidence for the previous cut-off). The objective was to effectively increase the asthma population eligible to receive regular ICS treatment and reduce the population treated with a SABA only, given the lack of robust evidence of the latter’s efficacy and safety and the fact that asthma is a variable condition characterized by acute exacerbations [ 26 ]. Similarly, UK authorities recommended low-dose ICS treatment in mild asthma, even for patients with suspected asthma, rather than treatment with a SABA alone [ 10 ]. However, these patients are unlikely to have good adherence to the regular use of an ICS. It is well known that poor adherence to treatment is a major problem in asthma management, even for patients with severe asthma. In their prospective study of 2004, Krishnan and colleagues evaluated the adherence to ICS and oral corticosteroids (OCS) in a cohort of patients hospitalized for asthma exacerbations [ 27 ]. The trend in the data showed that adherence to ICS and OCS treatment in patients dropped rapidly to reach nearly 50% within 7 days of hospital discharge, with the rate of OCS discontinuation per day nearly double the rate of ICS discontinuation per day (− 5.2% vs. − 2.7%; p < 0.0001 respectively, Fig. 3 ), thus showing that even after a severe event, patients’ adherence to treatment is suboptimal [ 27 ].

(From [ 27 ])
Use of inhaled (ICS) and oral (OCS) corticosteroids in patients after hospital discharge among high-risk adult patients with asthma. The corticosteroid use was monitored electronically. Error bars represent the standard errors of the measured ICS and OCS use
Guidelines set criteria with the aim of achieving optimal control of asthma; however, the attitude of patients towards asthma management is suboptimal. Partridge and colleagues were the first in 2006 to evaluate the level of asthma control and the attitude of patients towards asthma management. Patients self-managed their condition using their medication as and when they felt the need, and adjusted their treatment by increasing their intake of SABA, aiming for an immediate relief from symptoms [ 17 ]. The authors concluded that the adoption of a patient-centered approach in asthma management could be advantageous to improve asthma control.
The concomitant administration of an as-needed bronchodilator and ICS would provide rapid relief while administering anti-inflammatory therapy. This concept is not new: in the maintenance and reliever approach, patients are treated with ICS/formoterol (fast-acting, long-acting bronchodilator) combinations for both maintenance and reliever therapy. An effective example of this therapeutic approach is provided in the SMILE study in which symptomatic patients with moderate to severe asthma and treated with budesonide/formoterol as maintenance therapy were exposed to three different as-needed options: SABA (terbutaline), rapid-onset LABA (formoterol) and a combination of LABA and ICS (budesonide/formoterol) [ 28 ]. When compared with formoterol, budesonide/formoterol as reliever therapy significantly reduced the risk of severe exacerbations, indicating the efficacy of ICS as rescue medication and the importance of the as-needed use of the anti-inflammatory reliever.
The combination of an ICS and a LABA (budesonide/formoterol) in one inhaler for both maintenance and reliever therapy is even more effective than higher doses of maintenance ICS and LABA, as evidenced by Kuna and colleagues and Bousquet and colleagues (Fig. 4 ) [ 29 , 30 ].
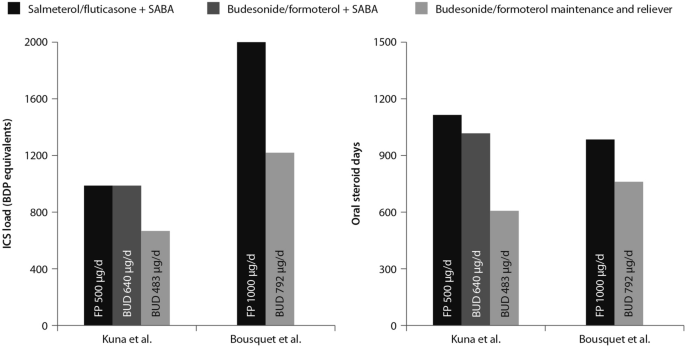
(Data from [ 29 , 30 ])
Comparison between the improvements in daily asthma control resulting from the use of budesonide/formoterol maintenance and reliever therapy vs. higher dose of ICS/LABA + SABAZ and steroid load for the two regimens
The effects of single maintenance and reliever therapy versus ICS with or without LABA (controller therapy) and SABA (reliever therapy) have been recently addressed in the meta-analysis by Sobieraj and colleagues, who analysed 16 randomized clinical trials involving patients with persistent asthma [ 31 ]. The systematic review supported the use of single maintenance and reliever therapy, which reduces the risk of exacerbations requiring systemic corticosteroids and/or hospitalization when compared with various strategies using SABA as rescue medication [ 31 ].
This concept was applied to mild asthma by the BEST study group, who were the first to challenge the regular use of ICS. A pilot study by Papi and colleagues evaluated the efficacy of the symptom-driven use of beclomethasone dipropionate plus albuterol in a single inhaler versus maintenance with inhaled beclomethasone and as-needed albuterol. In this six-month, double-blind, double-dummy, randomized, parallel-group trial, 455 patients with mild asthma were randomized to one of four treatment groups: an as-needed combination therapy of placebo bid plus 250 μg of beclomethasone and 100 μg of albuterol in a single inhaler; an as-needed albuterol combination therapy consisting of placebo bid plus 100 μg of albuterol; regular beclomethasone therapy, comprising beclomethasone 250 μg bid and 100 μg albuterol as needed); and regular combination therapy with beclomethasone 250 μg and albuterol 100 μg in a single inhaler bid plus albuterol 100 μg as needed.
The rescue use of beclomethasone/albuterol in a single inhaler was as efficacious as the regular use of inhaled beclomethasone (250 μg bid ) and it was associated with a lower 6-month cumulative dose of the ICS [ 32 ].
The time to first exacerbation differed significantly among groups ( p = 0.003), with the shortest in the as-needed albuterol and placebo group (Fig. 5 ). Figure 5 also shows equivalence between the as-needed combination therapy and the regular beclomethasone therapy. However, these results were not conclusive since the study was not powered to evaluate the effect of the treatment on exacerbations. In conclusion, as suggested by the study findings, mild asthma patients may require the use of an as-needed ICS and an inhaled bronchodilator rather than a regular treatment with ICS [ 32 ].
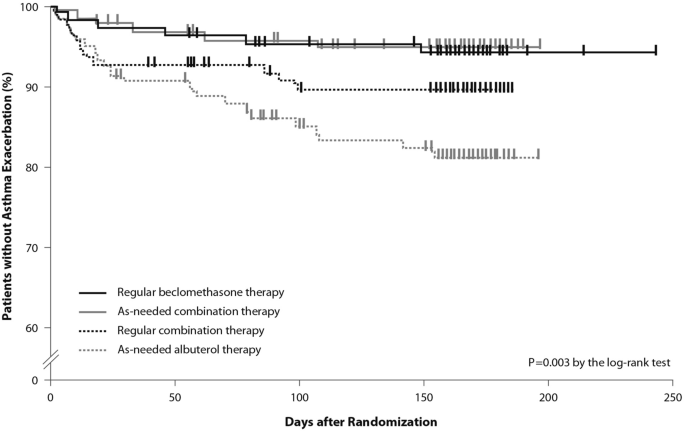
(From [ 32 ])
Kaplan Meier analysis of the time to first exacerbation (modified intention-to-treat population). First asthma exacerbations are shown as thick marks. As-needed albuterol therapy = placebo bid plus 100 μg of albuterol as needed; regular combination therapy = 250 μg of beclomethasone and 100 μg of albuterol in a single inhaler bid plus 100 μg of albuterol as needed; regular beclomethasone therapy = 250 μg of beclomethasone bid and 100 μg of albuterol as needed; as-needed combination therapy = placebo bid plus 250 μg of beclomethasone and 100 μg of albuterol in a single inhaler as needed
Moving forward: a new approach to the management of asthma patients
Nearly a decade after the publication of the BEST study in 2007, the use of this alternative therapeutic strategy was addressed in the SYGMA 1 and SYGMA 2 trials. These double-blind, randomized, parallel-group, 52-week phase III trials evaluated the efficacy of as-needed use of combination formoterol (LABA) and the ICS budesonide as an anti-inflammatory reliever in patients requiring GINA Step 2 treatment, with the current reliever therapy (e.g. as-needed SABA) or with low-dose maintenance ICS (inhaled budesonide bid ) plus as-needed SABA, administered as regular controller therapy [ 33 , 34 ].
The SYGMA 1 trial, which enrolled 3849 patients, aimed to demonstrate the superiority of the as-needed use of the combination budesonide/formoterol over as-needed terbutaline, as measured by the electronically-recorded proportion of weeks with well-controlled asthma [ 34 ]. The more pragmatic SYGMA 2 trial enrolled 4215 patients with the aim to demonstrate that the budesonide/formoterol combination is non-inferior to budesonide plus as-needed terbutaline in reducing the relative rate of annual severe asthma exacerbations [ 33 ]. Both trials met their primary efficacy outcomes. In particular, as-needed budesonide/formoterol was superior to as-needed SABA in controlling asthma symptoms (34.4% versus 31.1%) and preventing exacerbations, achieving a 64% reduction in exacerbations. In both trials, budesonide/formoterol as-needed was similar to budesonide maintenance bid at preventing severe exacerbations, with a substantial reduction of the inhaled steroid load over the study period (83% in the SYGMA 1 trial and 75% in the SYGMA 2 trial). The time to first exacerbation did not differ significantly between the two regimens; however, budesonide/formoterol was superior to SABA in prolonging the time to first severe exacerbation [ 33 , 34 ].
The double-blind, placebo-controlled design of the SYGMA trials does not fully address the advantages of anti-inflammatory reliever strategy in patients who often rely on SABAs for symptom relief, so to what extent the study findings could apply to real-life practice settings was unclear.
These limitations were overcome by the results of the Novel START study, an open-label, randomized, parallel-group, controlled trial designed to reflect real-world practice, which demonstrated the effectiveness in mild asthma of budesonide/formoterol as an anti-inflammatory reliever therapy [ 35 ].
In real-world practice, mild asthma patients are treated with an as-needed SABA reliever or with daily low-dose ICS maintenance therapy plus a SABA reliever. In the Novel START study, 668 patients with mild asthma were randomized to receive either as-needed albuterol 100 µg, two inhalations (SABA reliever as a continuation of the Step 1 treatment according to the 2017 GINA guidelines), budesonide 200 µg (ICS maintenance treatment) plus as-needed albuterol (Step 2 therapy of the GINA 2017 guidelines), or 200 µg/6 µg budesonide/formoterol as anti-inflammatory reliever therapy taken as-needed for a 52-week study period.
In this study, the rate of asthma exacerbations for budesonide/formoterol was lower compared with albuterol (51%) and similar to the twice-daily maintenance budesonide plus albuterol, despite a 52% reduction in the mean steroid dose with the single combination inhaler treatment [ 35 ]. In addition, severe exacerbation rate was lower with budesonide/formoterol as compared with as-needed albuterol and regular twice-daily budesonide. These data support the findings of the SYGMA 1 and 2 trials, highlighting the need for a critical re-examination of current clinical practice. Along with the results of the SYGMA trials, they provide convincing evidence of the advantages of the anti-inflammatory reliever strategy, particularly in real-life settings.
The SYGMA 1, SYGMA 2 and the novel START studies complete the picture of the treatment strategies for asthma at any degree of severity, including mild asthma. A growing body of evidence shows that an anti-inflammatory reliever strategy, when compared with all other strategies with SABA reliever, consistently reduces the rate of exacerbations across all levels of asthma severity (Fig. 6 ) [ 28 , 29 , 34 , 36 , 37 , 38 , 39 ].
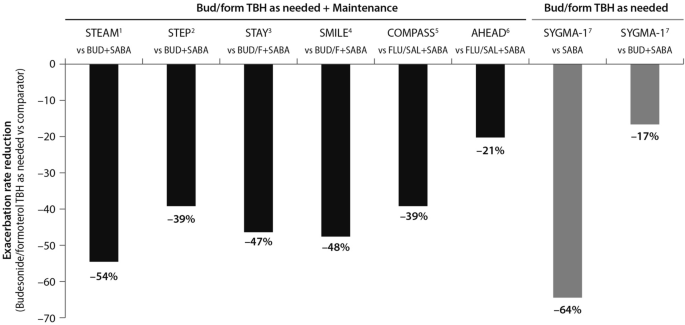
(Data source: [ 39 ])
Risk reduction of severe asthma attack of anti-inflammatory reliever versus SABA across all levels of asthma severity. Bud = budesonide; form = formoterol; TBH = turbohaler. Data from: 1: [ 36 ]; 2: [ 37 ]; 3: [ 38 ]; 4: [ 28 ]; 5: [ 29 ]; 6: [ 30 ]; 7: [ 34 ]
This evidence set the ground (Fig. 7 ) for the release of the 2019 GINA strategy updates. The document provides a consistent approach towards the management of the disease and aims to avoid the overreliance and overuse of SABAs, even in the early course of the disease. The 2019 GINA has introduced key changes in the treatment of mild asthma: for safety reasons, asthmatic adults and adolescents should receive ICS-containing controller treatment instead of the SABA-only treatment, which is no longer recommended.
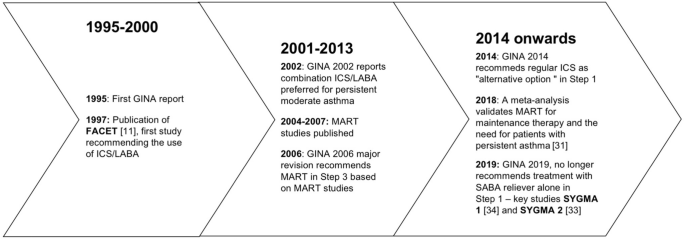
Timeline of key randomized controlled trials and meta-analyses providing the supporting evidence base leading to the Global Initiative for Asthma (GINA) 2019 guidelines. GINA global initiative for asthma, MART maintenance and reliever therapy, SMART single inhaler maintenance and reliever therapy
In Step 1 of the stepwise approach to adjusting asthma treatment, the preferred controller option for patients with fewer than two symptoms/month and no exacerbation risk factors is low-dose ICS/formoterol as needed. This strategy is indirectly supported by the results of the SYGMA 1 study which evaluated the efficacy and safety of budesonide/formoterol as needed, compared with as-needed terbutaline and budesonide bid plus as-needed terbutaline (see above). In patients with mild asthma, the use of an ICS/LABA (budesonide/formoterol) combination as needed provided superior symptom control to as-needed SABA, resulting in a 64% lower rate of exacerbations (p = 0.07) with a lower steroid dose (17% of the budesonide maintenance dose) [ 34 ]. The changes extend to the other controller options as well. In the 2017 GINA guidelines, the preferred treatment was as-needed SABA with the option to consider adding a regular low-dose ICS to the reliever. In order to overcome the poor adherence with the ICS regimen, and with the aim to reduce the risk of severe exacerbations, the 2019 GINA document recommends taking low-dose ICS whenever SABA is taken, with the daily ICS option no longer listed.
Previous studies including the TREXA study in children and adolescents [ 40 ], the BASALT study [ 41 ] and research conducted by the BEST study group [ 32 ] have already added to the evidence that a low-dose ICS with a bronchodilator is an effective strategy for symptom control in patients with mild asthma. A recently published study in African-American children with mild asthma found that the use of as-needed ICS with SABA provides similar asthma control, exacerbation rates and lung function measures at 1 year, compared with daily ICS controller therapy [ 42 ], adding support to TREXA findings that in children with well controlled, mild asthma, ICS used as rescue medication with SABA may be an efficacious step-down strategy [ 40 ].
In Step 2 of the stepwise approach, there are now two preferred controller options: (a) a daily low-dose ICS plus an as-needed SABA; and (b) as-needed low-dose ICS/formoterol. Recommendation (a) is supported by a large body of evidence from randomized controlled trials and observations showing a substantial reduction of exacerbation, hospitalization, and death with regular low-dose ICS [ 7 , 8 , 9 , 24 , 43 ], whereas recommendation (b) stems from evidence on the reduction or non-inferiority for severe exacerbations when as-needed low-dose ICS/formoterol is compared with regular ICS [ 33 , 34 ].
The new GINA document also suggests low-dose ICS is taken whenever SABA is taken, either as separate inhalers or in combination. This recommendation is supported by studies showing reduced exacerbation rates compared with taking a SABA only [ 32 , 40 ], or similar rates compared with regular ICS [ 32 , 40 , 41 ]. Low-dose theophylline, suggested as an alternative controller in the 2017 GINA guidelines, is no longer recommended.
Airway inflammation is present in the majority of patients with asthma, and although patients with mild asthma may have only infrequent symptoms, they face ongoing chronic inflammation of the lower airways and risk acute exacerbations. The GINA 2019 strategy recognizes the importance of reducing the risk of asthma exacerbations, even in patients with mild asthma (Steps 1 and 2) [ 4 ]. In this regard, the new recommendations note that SABA alone for symptomatic treatment is non-protective against severe exacerbation and may actually increase exacerbation risk if used regularly or frequently [ 4 ].
The reluctance by patients to regularly use an ICS controller means they may instead try and manage their asthma symptoms by increasing their SABA reliever use. This can result in SABA overuse and increased prescribing, and increased risk of exacerbations.
As part of the global SABINA (SABA use IN Asthma) observational study programme, a UK study examined primary care records to describe the pattern of SABA and ICS use over a 10-year period in 373,256 patients with mild asthma [ 44 ]. Results showed that year-to-year SABA prescribing was more variable than that of ICS indicating that, in response to fluctuations in asthma symptom control, SABA use was increased in preference to ICS use. Furthermore, more than 33% of patients were prescribed SABA inhalers at a level equivalent to around ≥ 3 puffs per week which, according to GINA, suggests inadequate asthma control.
The problem of SABA overuse is further highlighted by two studies [ 45 , 46 ], also as part of the SABINA programme. These analysed data from 365,324 patients in a Swedish cohort prescribed two medications for obstructive lung disease in any 12-month period (HERA).
The first study identified SABA overuse (defined as ≥ 3 SABA canisters a year) in 30% of patients, irrespective of their ICS use; 21% of patients were collecting 3–5 canisters annually, 7% were collecting 6–10, and 2% more than 11 [ 45 ]. Those patients who were overusing SABA had significantly more asthma exacerbations relative to those using < 3 canisters (20.0 versus 12.5 per 100 patient years; relative risk 1.60, 95% CI 1.57–1.63, p < 0.001). Moreover, patients overusing SABA and whose asthma was more severe (GINA Steps 3 and 4) had greater exacerbation risk compared with overusing patients whose asthma was milder (GINA Steps 1 and 2).
The second study found those patients using three or more SABA reliever canisters a year had an increased all-cause mortality risk relative to patients using fewer SABA canisters: hazard ratios after adjustment were 1.26 (95% CI 1.14–1.39) for 3–5 canisters annually, 1.67 (1.49–1.87) for 6–10 canisters, and 2.35 (2.02–2.72) for > 11 canisters, relative to patients collecting < 3 canisters annually [ 46 ].
The recently published PRACTICAL study lends further support to as-needed low-dose ICS/formoterol as an alternative option to daily low-dose ICS plus as-needed SABA, outlined in Step 2 of the guidelines [ 47 ]. In their one-year, open-label, multicentre, randomized, superiority trial in 890 patients with mild to moderate asthma, Hardy and colleagues found that the rate of severe exacerbations per patient per year (the primary outcome) was lower in patients who received as-needed budesonide/formoterol than in patients who received controller budesonide plus as-needed terbutaline (relative rate 0.69, 95% CI 0.48–1.00; p < 0.05). Indeed, they suggest that of these two treatment options, as-needed low-dose ICS/formoterol may be preferred over controller low-dose ICS plus as-needed SABA for the prevention of severe exacerbations in this patient population.
Step 3 recommendations have been left unchanged from 2017, whereas Step 4 treatment has changed from recommending medium/high-dose ICS/LABA [ 3 ] to medium-dose ICS/LABA; the high-dose recommendation has been escalated to Step 5. Patients who have asthma that remains uncontrolled after Step 4 treatment should be referred for phenotypic assessment with or without add-on therapy.
To summarise, the use of ICS medications is of paramount importance for optimal asthma control. The onset and increase of symptoms are indicative of a worsening inflammation leading to severe exacerbations, the risk of which is reduced by a maintenance plus as-needed ICS/LABA combination therapy. The inhaled ICS/bronchodilator combination is as effective as the regular use of inhaled steroids.
The efficacy of anti-inflammatory reliever therapy (budesonide/formoterol) versus current standard-of-care therapies in mild asthma (e.g. reliever therapy with a SABA as needed and regular maintenance controller therapy plus a SABA as-needed) has been evaluated in two randomized, phase III trials which confirmed that, with respect to as-needed SABA, the anti-inflammatory reliever as needed is superior in controlling asthma and reduces exacerbation rates, exposing the patients to a substantially lower glucocorticoid dose.
Conclusions
A growing body of evidence shows that anti-inflammatory reliever strategy is more effective than other strategies with SABA reliever in controlling asthma and reducing exacerbations across all levels of asthma severity. A budesonide/formoterol therapy exposes asthma patients to a substantially lower glucocorticoid dose while cutting the need for adherence to scheduled therapy.
Availability of data and materials
Not applicable.
Abbreviations
Global Initiative for Asthma
Inhaled corticosteroids
Long-acting beta-agonists
Oral corticosteroids
Short-acting beta-agonists
Single inhaler maintenance and reliever treatment
World Health Organization. Asthma. 2017. https://www.who.int/news-room/fact-sheets/detail/asthma . Accessed 9 April 2019.
Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391(10122):783–800.
Article PubMed Google Scholar
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2017. http://www.ginasthma.org . Accessed 1 June 2019.
Global Initiative for Asthma. Pocket guide for asthma management and prevention. 2019, pp. 1–32. www.ginasthma.org . Accessed 1 June 2019.
Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000;16(5):802–7.
Article CAS PubMed Google Scholar
Price D, Fletcher M, Molen V. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009.
Article PubMed Central PubMed Google Scholar
Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax. 2002;57(10):880–4.
Article CAS PubMed Central PubMed Google Scholar
Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. New Engl J Med. 2000;343(5):332–6.
Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen YZ, Ohlsson SV, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet. 2003;361(9363):1071–6.
Healthcare Improvement Scotland and British Thoracic Society. SIGN 153: British guideline on the management of asthma. 2016. https://www.sign.ac.uk/sign-153-british-guideline-on-the-management-of-asthma.html .
Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O’Byrne P, Barnes PJ, Ullman A. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med. 1997;337(20):1405–11.
O’Byrne PM, Naya IP, Kallen A, Postma DS, Barnes PJ. Increasing doses of inhaled corticosteroids compared to adding long-acting inhaled β2-agonists in achieving asthma control. Chest. 2008;134(6):1192–9.
Johnston SL, Pattemore PK, Sanderson G, Smith S, Lampe F, Josephs L, et al. Community study of role of viral infections in exacerbations of asthma in 9–11 year old children. BMJ. 1995;310(6989):1225–9.
Corne JM, Marshall C, Smith S, Schreiber J, Sanderson G, Holgate ST, Johnston SL. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet. 2002;359(9309):831–4.
Papi A, Contoli M, Adcock IM, Bellettato C, Padovani A, Casolari P, et al. Rhinovirus infection causes steroid resistance in airway epithelium through nuclear factor κb and c-Jun N-terminal kinase activation. J Allergy Clin Immunol. 2013;132(5):1075–85.
Romagnoli M, Vachier I, Tarodo de la Fuente P, Meziane H, Chavis C, Bousquet J, et al. Eosinophilic inflammation in sputum of poorly controlled asthmatics. Eur Respir J. 2002;20(6):1370–7.
Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006;6:13.
Papi A, Caramori G, Adcock IM, Barnes PJ. Rescue treatment in asthma. More than as-needed bronchodilation. Chest. 2009;135(6):1628–33.
PubMed Google Scholar
Tattersfield AE, Postma DS, Barnes PJ, Svensson K, Bauer CA, Byrne PM, et al. Exacerbations of asthma: a descriptive study of 425 severe exacerbations The FACET International Study Group. Am J Respir Crit Care Med. 1999;160(2):594–9.
O’Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? Eur Respir J. 2017. https://doi.org/10.1183/13993003.01103-2017 .
Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD). Confidential Enquiry report. London: RCP; 2014.
Google Scholar
Suissa S, Ernst P, Boivin JF, Horwitz RI, Habbick B, Cockroft D, et al. A cohort analysis of excess mortality in asthma and the use of inhaled β-agonists. Am J Respir Crit Care Med. 1994;149(3 Pt 1):604–10.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2014. https://ginasthma.org/wp-content/uploads/2019/01/2014-GINA.pdf .
Reddel HK, Busse WW, Pedersen S, Tan WC, Chen YZ, Jorup C, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: a post hoc efficacy analysis of the START study. Lancet. 2017;389(10065):157–66.
Papi A, Fabbri LM. Management of patients with early mild asthma and infrequent symptoms. Lancet. 2017;389(10065):129–30.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2016. https://ginasthma.org/wp-content/uploads/2016/04/GINA-Appendix-2016-final.pdf .
Krishnan JA, Riekert KA, McCoy JV, Stewart DY, Schmidt S, Chanmugam A, et al. Corticosteroid use after hospital discharge among high-risk adults with asthma. Am J Respir Crit Care Med. 2004;170(12):1281–5.
Rabe KF, Atienza T, Magyar P, Larsson P, Jorup C, Lalloo UG. Effect of budesonide in combination with formoterol for reliever therapy in asthma exacerbations: a randomised controlled, double-blind study. Lancet. 2006;368(9537):744–53.
Kuna P, Peters MJ, Manjra AI, Jorup C, Naya IP, Martínez-Jimenez NE, Buhl R. Effect of budesonide/formoterol maintenance and reliever therapy on asthma exacerbations. Int J Clin Pract. 2007;61(5):725–36.
Bousquet J, Boulet LP, Peters MJ, Magnussen H, Quiralte J, Martinez-Aguilar NE, Carlsheimer A. Budesonide/formoterol for maintenance and relief in uncontrolled asthma vs. high-dose salmeterol/fluticasone. Respir Med. 2007;101(12):2437–46.
Sobieraj DM, Weeda ER, Nguyen E, Coleman CI, White CM, Lazarus SC, et al. Association of inhaled corticosteroids and long-acting β-agonists as controller and quick relief therapy with exacerbations and symptom control in persistent asthma a systematic review and meta-analysis. JAMA. 2018;319(14):1485–96.
Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, BEST Study Group, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. New Engl J Med. 2007;356(20):2040–52.
Bateman ED, Reddel HK, O’Byrne PM, Barnes PJ, Zhong N, Keen C, et al. As-needed budesonide–formoterol versus maintenance budesonide in mild asthma. New Engl J Med. 2018;378(20):1877–87.
O’Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zhong N, Keen C, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. New Engl J Med. 2018;378(20):1865–76.
Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, Novel START Study Team, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. New Engl J Med. 2019;380(21):2020–30.
Rabe K, Pizzichini E, Ställberg B, Romero S, Balanzat AM, Atienza T, et al. Budesonide/formoterol in a single inhaler for maintenance and relief in mild-to-moderate asthma: a randomized, double-blind trial. Chest. 2006;129(2):246–56.
Scicchitano R, Aalbers R, Ukena D, Manjra A, Fouquert L, Centanni S, et al. Efficacy and safety of budesonide/formoterol single inhaler therapy versus a higher dose of budesonide in moderate to severe asthma. Curr Med Res Opin. 2004;20(9):1403–18.
O’Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med. 2005;171(2):129–36.
Pavord ID, Beasley R, Agusti A, Anderson GP, Bel E, Brusselle G, et al. After asthma: redefining airways diseases. Lancet. 2017;391(10118):350–400.
Martinez FD, Chinchilli VM, Morgan WJ, Boehmer SJ, Lemanske RF Jr, Mauger DT, et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): a randomised, double-blind, placebo-controlled trial. Lancet. 2011;377(9766):650–7.
Calhoun WJ, Ameredes BT, King TS, Icitovic N, Bleecker ER, Castro M, et al. Comparison of physician-, biomarker-, and symptom-based strategies for adjustment of inhaled corticosteroid therapy in adults with asthma: the BASALT randomized controlled trial. JAMA. 2012;308(10):987–97.
Sumino K, Bacharier LB, Taylor J, et al. A pragmatic trial of symptom-based inhaled corticosteroid use in African-American children with mild asthma. J Allergy Clin Immunol Pract. 2020;8(176–85):e2.
Byrne PM, Barnes PJ, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, Tattersfield A. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164(8):1392–7.
Article Google Scholar
Bloom C, Quint J, Cabrera C. SABA and ICS prescriptions among mild asthma patients in UK primary care. Poster presented at the European Respiratory Society International Congress; 2019 Sep 28–Oct 2; Madrid, Spain.
Janson C, Nwaru B, Hasvold P, Wicklund F, Telg G, Ekstrom M. Use of short-acting beta-2 agonists (SABA) and exacerbations in a nationwide Swedish asthma cohort (HERA). Poster presented at the European Respiratory Society International Congress; 2019 Sep 28–Oct 2; Madrid, Spain.
Janson C, Nwaru B, Hasvold P, Wicklund F, Telg G, Ekstrom M. SABA overuse and risk of mortality in a nationwide Swedish asthma cohort (HERA). Late Breaker abstract at the European Respiratory Society International Congress; 2019 Sep 28–Oct 2; Madrid, Spain.
Hardy J, Baggott C, Fingleton J, Reddel HK, Hancox RJ, Harwood M, et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet. 2019;394(10202):919–28.
Download references
Acknowledgements
The Authors thank Maurizio Tarzia and Gayle Robins, independent medical writers who provided editorial assistance on behalf of Springer Healthcare Communications. The editorial assistance was funded by AstraZeneca.
No funding was received for this study. The editorial assistance was funded by AstraZeneca.
Author information
Authors and affiliations.
Section of Cardiorespiratory and Internal Medicine, Department of Morphology, Surgery and Experimental Medicine, University of Ferrara, Ferrara, Italy
Alberto Papi & Luca Morandi
Internal Medicine Department, Respiratory Unit and Adult Cystic Fibrosis Center, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy
Francesco Blasi
Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy
Personalized Medicine Asthma & Allergy Clinic, Humanitas University & Istituto Clinico Humanitas, Milan, Italy
Giorgio Walter Canonica
Università Cattolica del Sacro Cuore, Fondazione Policlinico A. Gemelli IRCCS, Rome, Italy
Luca Richeldi
Respiratory Section, Department of Medicine, University of Verona, Verona, Italy
Andrea Rossi
Respiratory Unit, Emergency Department, University Hospital S. Anna, Via Aldo Moro 8, 44124, Ferrara, Italy
You can also search for this author in PubMed Google Scholar
Contributions
AP, FB, GWC, LM, LR and AR contributed to writing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Alberto Papi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
AP reports grants, personal fees, non-financial support and payment for advisory board membership, consultancy, payment for lectures, grants for research, and travel expenses reimbursement from Chiesi, AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Mundipharma and Teva, and personal fees and non-financial support from Menarini, Novartis, Zambon and Sanofi.
FB reports having received in the last three years research grants as well as lecture or advisory board fees from: Alk-Abelló, AstraZeneca, Boehringer Ingelheim, Chiesi, Guidotti, Glaxo Smith Kline, Grifols, Menarini, Novartis, Sanofi, Valeas, Zambon.
GWC reports having received in the last 3 years research grants as well as lecture or advisory board fees from: A. Menarini, Alk-Abelló, AstraZeneca-Medimmune, Boehringer Ingelheim, Chiesi Farmaceutici, Genentech, Guidotti-Malesci, Glaxo Smith Kline, Hal Allergy, Merck Sharp & Dohme, Mundipharma, Novartis, Orion, Sanofi-Aventis, Sanofi Genzyme/Regeneron, Stallergenes-Greers, UCB Pharma, Uriach Pharma, Valeas.
LR Receipt of grants/research supports: Roche, Boehringer Ingelheim.
Receipt of honoraria or consultation fees: Boehringer Ingelheim, Roche, Biogen, FibroGen,
Sanofi-Aventis, Anthera, Promedior, ImmuneWorks, Asahi-Kasei, Bayer, Celgene, RespiVant,
Nitto, Bristol Myers Squibb, Prometic, Pliant Therapeutics, Toray, Global Blood Therapeutics,
Zambon, Veracyte, Acceleron, CSL Behring.
LM and AR reports no conflicts of interest in the last 3 years.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Papi, A., Blasi, F., Canonica, G.W. et al. Treatment strategies for asthma: reshaping the concept of asthma management. Allergy Asthma Clin Immunol 16 , 75 (2020). https://doi.org/10.1186/s13223-020-00472-8
Download citation
Received : 18 March 2020
Accepted : 05 August 2020
Published : 15 August 2020
DOI : https://doi.org/10.1186/s13223-020-00472-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Anti-inflammatory treatment
- Disease control
- Patient outcomes
Allergy, Asthma & Clinical Immunology
ISSN: 1710-1492
- Submission enquiries: [email protected]
- General enquiries: [email protected]
The pharmacological management of asthma in adults: 2023 update
Affiliations.
- 1 Unit of Pharmacology, Department of Experimental Medicine, University of Campania "Luigi Vanvitelli", Naples, Italy.
- 2 Pharmacy Unit, "Luigi Vanvitelli" University Hospital, Naples, Italy.
- 3 Unit of Respiratory Medicine, Department of Experimental Medicine, University of Rome "Tor Vergata", Rome, Italy.
- PMID: 38497368
- DOI: 10.1080/14656566.2024.2332627
Introduction: The pharmacotherapy of asthma is a dynamic process that changes as our knowledge of the underlying pathophysiology and treatment of this disease continues to evolve. This implies the need for continuous revision of the recommendations of asthma guidelines and strategies.
Areas covered: This review summarizes the latest key practical information on the pharmacological management of asthma in adults. We provide the background to the 2023 update of the GINA strategy report, focusing on changes and discussing areas of uncertainty. We review current and emerging pharmacotherapy for uncontrolled asthma, including synthetic agents and new biologics, and provide expert perspectives and opinions on the treatment of uncontrolled asthma.
Expert opinion: The current pharmacological treatment of asthma, based on a step-by-step, control-based approach, with ICSs, LABAs and LAMAs being the mainstay generally provides good symptom control. Biologic therapies are often effective in treating T2 high severe asthma. However, there is still room for improvement, such as the discovery of new molecules that specifically target chronic inflammation and, most importantly, the ability to provide solutions to the various areas of uncertainty that still exist. Also finding solutions to improve the accessibility and affordability of rescue ICS in resource-constrained settings is critical.
Keywords: Asthma; Global initiative for asthma; biologics; biomarkers; guidelines; pharmacotherapy; treatable traits.
Publication types
- Help & Support
- Lung Health & Diseases
- Lung Disease Lookup
- Learn About Asthma
Asthma Research
Why we need research.
Asthma research helps us understand how the disease is caused, how it develops and how it is best treated. Research can also help us understand who is at high risk for developing asthma, certain triggers, and ways to avoid getting asthma.
Our Asthma Research Program
The American Lung Association is committed to funding asthma research. Our Awards and Grants Program funds top-notch researchers at important career crossroads to gain long-term commitment to lung health and disease research. Without the life-long dedication of lung researchers, important and much-needed discoveries would not be possible. In addition to the Awards and Grants Program, the Lung Association funds the Airways Clinical Research Centers (ACRC) Network , which implements patient-centered clinical trials, and has helped to change the nature of asthma patient care since its inception in 2000.
What Research Is Being Done?
Some of the current topics American Lung Association funded researchers are investigating include understanding the immune system’s role in asthma, using mobile technology to reach young African Americans with asthma, and better defining subtypes of asthma. Together, studies like these lead to improved therapy, quality of life, and access to care for all people with asthma.
Thanks to the medical breakthroughs led by Lung Association researchers and their colleagues, we have made significant contributions to improve our understanding of asthma.
Currently funded Lung Association researchers are:
- Studying asthma that is resistant to steroid treatments
- Boosting the immune system to reduce allergic inflammation in airways
- Understanding which genes are responsible for severe asthma
- Finding new genetic targets in lung tissue for new asthma therapy and prevention
- Improve our understanding of the challenges in access to asthma medication in schools
- Evaluating asthma management policy in Chicago schools
- Providing asthma education to children in the hospital and at home
Asthma Researchers
Visit our Meet the Researchers section to view our asthma researchers and their studies.
Asthma Clinical Trials
- See our Lung Association listing of current trials .
- View ACRC clinical trials that are currently recruiting as well as outcomes from completed studies.
Airways Clinical Research Centers (ACRC) Network
The ACRC is the nation's largest not-for-profit network of clinical research centers dedicated to asthma and chronic obstructive pulmonary disease (COPD) treatment research, attracting some of the best investigators nationwide. The ACRC Network conducts large clinical trials that will directly impact patient care for COPD and asthma.
Meet our Principal Investigators, see where our centers are located and learn more about some of the important research findings at Lung.org/acrc .
Page last updated: April 19, 2023
A Breath of Fresh Air in Your Inbox
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- ERJ Open Res
- v.8(2); 2022 Apr

Prevalence, time trends and treatment practices of asthma in India: the Global Asthma Network study
Sheetu singh.
1 Dept of Pulmonary Medicine, Rajasthan Hospital, Jaipur, India
Sundeep Salvi
2 Pulmocare Research and Education Foundation, Pune, India
Daya Krishan Mangal
3 Dept of Public Health, IIHMR University, Jaipur, India
Meenu Singh
4 Dept of Pediatrics, Postgraduate Institute of Medical Education and Research, Changdigarh, India
Shally Awasthi
5 Dept of Pediatrics, King George's Medical University, Lucknow, India
Padukudru Anand Mahesh
6 Dept of Respiratory Medicine, Jagadguru Sri Shivarathreeshwara Medical College, JSSAHER, Mysuru, India
Sushil K. Kabra
7 Dept of Pediatrics, All India Institute of Medical Sciences, New Delhi, India
Sabir Mohammed
8 Dept of Pulmonary Medicine, Kothari Medical College and Research Institute, Bikaner, India
Thevaruparambil U. Sukumaran
9 Dept of Pediatrics, Caritas Hospital, Thellakom, Kottayam, India
Aloke G. Ghoshal
10 National Allergy Asthma Bronchitis Institute, Kolkata, India
Monica Barne
Sanjeev sinha.
11 Dept of Medicine, All India Institute of Medical Sciences, New Delhi, India
Sanjay K. Kochar
Nishtha singh.
12 Dept of Respiratory Medicine, Asthma Bhawan, Jaipur, India
Udaiveer Singh
13 Division of Research, Asthma Bhawan, Jaipur, India
Kamalesh Kumar Patel
Arvind kumar sharma.
14 Dept of Community Medicine, Mahatma Gandhi Medical College and Hospital, Jaipur, India
Bhushan Girase
15 Family Health, PATH, New Delhi, India
Anil Chauhan
16 Dept of Telemedicine, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Niranjan Sit
Jayaraj b. siddaiah, virendra singh.
The objective of this subanalysis of data from centres across urban areas in India of the Global Asthma Network (GAN) was to study 1) the prevalence of symptoms of asthma in children and adults, 2) the change in prevalence of asthma and its trigger factors since the International Study of Asthma and Allergies in Childhood (ISAAC), and 3) current asthma treatment practice.
In this cross-sectional, multicentre, school-based and self-administered questionnaire, responses from children aged 6–7 years and 13–14 years, and their respective parents, were analysed.
The GAN Phase I study included 20 084 children in the 6–7-year age group, 25 887 children in the 13–14-year age group and 81 296 parents. The prevalence of wheeze in the previous 12 months was 3.16%, 3.63% and 3.30% in the three groups, respectively. In comparison to the ISAAC studies, there was a significant reduction in the prevalence of current wheeze (p<0.001). Bivariate analysis revealed a significant reduction in the prevalence of trigger factors. Almost 82% of current wheezers and 70% of subjects with symptoms of severe asthma were not clinically diagnosed as having asthma. The daily use of inhaled corticosteroids (ICS) was less than 2.5% in subjects with current wheeze and those with symptoms of severe asthma but less than 1% used daily ICS when asthma remained undiagnosed.
The prevalence of current wheeze and its causal factors showed a significant reduction compared to previous ISAAC studies. Among subjects with current wheeze and symptoms of severe asthma, the problem of under-diagnosis and under-treatment was widespread.
Short abstract
Data from Indian centres that participated in the multicentre Global Asthma Network showed a significant decline in symptoms of asthma compared to previous studies. The study highlighted under-diagnosis and under-treatment in children and adults with asthma. https://bit.ly/3thevot
Introduction
The prevalence of asthma varies widely among countries/geographical regions and also within countries with different geographies and socioeconomic strata [ 1 , 2 ]. The Indian Study on Epidemiology of Asthma, Respiratory Symptoms and Chronic Bronchitis in Adults (INSEARCH) estimated the national burden of asthma at 17.23 million with an overall prevalence of 2.05% [ 3 ]. The recent Global Burden of Disease (GBD, 1990–2019) estimated the total burden of asthma in India as 34.3 million, accounting for 13.09% of the global burden [ 4 ]. It also attributed that there were 13.2 per thousand deaths due to asthma in India [ 4 ]. Asthma accounted for 27.9% of disability-adjusted life years (DALYs) in the Indian population [ 4 ]. On the whole, India has three times higher mortality and more than two times higher DALYs compared to the global proportion of asthma burden. The disproportionate mortality and morbidity can be explained by global studies with uniform methodology.
The International Study of Asthma and Allergy in Childhood (ISAAC) Phase I (1995) and Phase III (2001–03) are the largest multicentre global studies to be conducted with uniform methodology worldwide [ 5 , 6 ]. The studies showed around 6% of children in India had current wheezing and identified several environmental factors associated with asthma globally, including environmental tobacco smoke [ 7 ], cooking with firewood [ 8 ], exposure to heavy truck traffic [ 9 ], obesity [ 10 ], fast-food consumption [ 11 ], dampness in homes [ 12 ] and paracetamol/antibiotic use [ 13 ].
Over the past two decades there has been a change in the economy, industrialisation, air pollution levels, and environmental and socio-cultural factors in India. Apart from the ISAAC studies, no other worldwide multicentre studies have been conducted to analyse the impact of these changes on the prevalence and severity of asthma. The ISAAC study group was resurrected in 2012 in the form of the Global Asthma Network (GAN), to estimate the current prevalence of symptoms of asthma and allergies [ 14 ].
The GAN study included certain aspects that were not covered in the ISAAC studies, including the prevalence of asthma symptoms amongst parents of children and the medications used for control [ 14 ]. The objective of this paper was to analyse the GAN Phase I data from Indian centres for 1) the prevalence of asthmatic symptoms in children (aged 6–7 years and 13–14 years) and their adult parents; 2) the change in prevalence of asthmatic symptoms in children compared to previous ISAAC studies and associated environmental factors, and 3) the current use of medicines among children and adults with asthma.
Materials and methods
The GAN Phase I study was a cross-sectional, multi-country, multicentre and questionnaire-based epidemiological research study conducted in schools. The study protocol and methodology were similar to the previous ISAAC Phase III study, details of which are explained in an earlier publication [ 14 ]. The GAN Phase I study included seven centres that participated in ISAAC Phase III and two new centres. The new centres (Mysuru and Kolkata, representing south and east India, respectively) were included to better represent all geographical areas. The survey was conducted across nine centres in India (Bikaner, Chandigarh, Delhi, Jaipur, Kolkata, Kottayam, Mysuru, Lucknow and Pune) in the 13–14-year age group and eight centres in the 6–7-year age group of children (Kolkata did not participate in the younger age group). The study was approved by the ethics committee from the respective local centres and was registered in the Clinical Trial Registry, India (CTRI/2018/02/011758).
Schools were randomly selected from a pool of total schools in the selected centres ( figure 1 ), with the help of the Indian Institute of Health Management and Research (IIHMR), Jaipur. The geographic boundary was defined for each city and it was divided into four zones. A fraction of schools was randomly selected from each zone. Invitations were sent to the principals of the schools and consenting schools were enrolled in the study. If a school in the randomised list refused to participate, the next school was approached. Passive consent was obtained from the participants. The option of refusal to participate was communicated either by a phone call to the field worker from the parents/guardians or written/verbal refusal by the child to participate.

Flow chart depicting recruitment into the Global Asthma Network study.
Two age groups of schoolchildren (13–14 years and 6–7 years) and their parents/guardians were given written questionnaires. The heights and weights of the children were recorded on the day the questionnaires were administered. The adolescent group (13–14 years) had to complete a questionnaire about themselves at school and were asked to take the adult questionnaires home for their parents/guardians to complete about their own health. The younger age group (6–7 years) took the questionnaires home for parents/guardians to complete the questionnaire about the health of their wards and themselves. Codes assigned to the children and their respective parents were the same.
The questionnaire used in the study was similar to the previously validated core questionnaire used in ISAAC for both age groups of children. The questionnaire had 70, 50 and 47 questions for the 6–7 years, 13–14 years and the adult groups, respectively (there were an additional two questions for the children and five questions for the adults in the questionnaire used in Indian centres compared to the questionnaire used globally). The items in the questionnaires pertained to demography; symptoms of asthma, rhinoconjunctivitis and atopic eczema; environment and use of medications. The adult questionnaire was derived from the questionnaire used in ISAAC and the European Community Respiratory Health Survey. The questionnaire was available in different languages (English, Hindi, Bengali, Marathi, Punjabi, Kannada and Malayalam). The language translation of the questionnaire was validated by back-translating the questionnaire to the English language according to standard protocols.
A meeting was convened for all principal investigators of their respective centres at the National Data Coordinating Center (NDCC, Asthma Bhawan, Jaipur) to delineate the study pathway. Field investigators and data entry operators received training at IIHMR, Jaipur.
Ten per cent of the data were uploaded online, and the data entry errors were kept below 2% by entering the data twice, first at the site and then the second time by the statistical team at IIHMR, Jaipur. The statistical team consolidated the entire data at IIHMR University, Jaipur, and sent it to the GAN global centre (Auckland, New Zealand) and subsequently to the main data centre (London, UK), where the data were cleaned for consistency and duplicity ( figure 1 ).
Coding of the data was done as per the GAN protocol. Current wheeze was defined as the presence of wheeze in the past 12 months (WHEZ12); this variable was then used to calculate the prevalence of asthma. The other variables were: ever diagnosed as asthma (ASTHMAEV) and wheeze ever (WHEZEV). Dry cough in the night during the past 12 months apart from infection (COUGH12) was termed as nocturnal cough. Severe asthma was defined as a current wheeze with more than four attacks per year or wheeze affecting speech or sleep.
Data management and statistical analysis
The sample size targeted for each age group was 3000 participants, and potentially 6000 adults per centre. This sample size could detect a 5% difference between the two centres with 99% certainty (at a 1% level of significance) [ 14 ]. The missing data were not included in the analysis. Statistical tests such as Chi-squared were carried out for bivariate analysis to estimate the distribution and association of current wheeze and severe asthma in different predictors. If the cell frequency was less than 5, the Fisher exact probability test was used. The quantitative data were analysed using STATA version 12 (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP). Prevalence of current wheeze as reported in ISAAC Phase I, III and GAN Phase I studies were compared using Chi-squared test.
In this study, questionnaires were received from 20 084 children in the 6–7-year age group, 25 887 children in the 13–14-year age group and 81 296 adults ( table 1 ). The average response rates were 83.9%, 96.6% and 99.4% for 6–7 years, 13–14 years and adults, respectively. There were 48.0%, 51.1% and 50.2% females in the 6–7 years, 13–14 years and adults, respectively. The mean age of the adults was 37.6±6.4 years.
Prevalence of symptoms of asthma, severe asthma, asthma ever and doctor-diagnosed asthma in children and adults across both genders
# : sex not defined for 13 adults. ¶ : Chi-squared test. + : questions not included in adult questionnaire. § : severe asthma is defined as more than four attacks of wheezing in previous 12 months or wheeze affecting sleep or speech in previous 12 months.
The prevalence of current wheeze was 3.16%, 3.63% and 3.30% among the 6–7 years, 13–14 years and adults, respectively ( table 1 ) with no significant difference between the age groups (p>0.05). A significantly higher prevalence of current wheeze, wheeze ever, asthma ever, doctor-diagnosed asthma and nocturnal cough in the last 12 months was noted in boys in both the age groups of children (p<0.05) ( table 1 ). However, in adults, the prevalence of asthma ever and doctor-diagnosed asthma were significantly higher in women than in men (p<0.001). Severe asthma was prevalent in 1.59%, 1.60% and 1.16% in the 6–7 years, 13–14 years and adults (parents), respectively ( table 1 ). The prevalence of current wheeze, nocturnal cough in the past 12 months and severe asthma varied markedly across centres ( supplementary tables 1, 2 and 3 ).
Across ISAAC Phase III and GAN Phase I, in both age groups, there was a significant decrease in the prevalence of current wheeze (p<0.001) and asthma ever (p<0.001), but there was a significant increase in the prevalence of the symptom nocturnal cough (p<0.001, figure 2 , supplementary table 4 ). Bivariate analysis of comparison of various causal factors of current wheeze among children during GAN from ISAAC showed a significant reduction in paracetamol use, maternal smoking, farm exposure, pets in the house and trucks passing outside the house. There was a significant increase in the usage of fresh fruits ( table 2 ).
Time trends in known environmental trigger factors through the International Study of Asthma and Allergies in Childhood (ISAAC) Phase III and Global Asthma Network (GAN) in the two age groups of children
Data are presented as n (%), unless otherwise stated. # : Chi-squared test. ¶ : questions included in the 6–7-year age group questionnaire only.

Time trends in various aspects of asthma including current wheeze, wheeze ever, nocturnal cough, severe asthma and asthma ever through the International Study of Asthma and Allergies in Childhood (ISAAC) Phase I and Phase III, and the Global Asthma Network (GAN) Phase I, in the two age groups of children. # : severe asthma is defined as more than four attacks of wheezing in previous 12 months or wheeze affecting sleep or speech in previous 12 months. *: p<0.05; **: p<0.01; ***: p<0.001 when ISAAC Phase I compared to ISAAC Phase II. ¶¶¶ : p<0.001 when ISAAC Phase III compared to GAN Phase I.
In the 6–7-year age group absenteeism due to wheeze was noted in 66.1% and 2.5% of children with current wheeze, with and without a concomitant doctor diagnosis of asthma, respectively ( table 3 ). In the 13–14-year age group these numbers were 52.7% and 24.0%, respectively. Hospitalisations at least once in the past year because of breathing problems were noted in 44.3% of children with current wheeze with a concomitant doctor diagnosis of asthma and 1.2% of children with current wheeze without a doctor diagnosis ( table 3 ). In the 13–14-year age group these numbers were 25.5% and 8.7%, respectively. Similarly, exercise-induced wheeze and visits to an emergency department due to breathing trouble were also higher in subjects with doctor-diagnosed asthma.
School absenteeism, exercise-induced wheeze and medical assistance required among children and adults with current wheeze with or without doctor-diagnosed asthma, and healthy subjects
Data are presented as n (%), unless otherwise stated. # : Chi-squared test.
In all groups both inhaled and oral medicines were used in almost equal proportion. However, in subjects in any of the three groups with current wheeze or with symptoms of severe asthma, less than 2.5% of subjects were using daily ICS and less than 2% of subjects used inhaled beta-agonist daily ( table 4 ).
Treatment undertaken for current wheeze and severe asthma in children and adults
ICS: inhaled corticosteroid; LABA: long-acting β-agonist. # : severe asthma is defined as current wheeze with more than four attacks per year or wheeze affecting speech or activity.
Among subjects with current wheeze, 75–82% remained clinically undiagnosed ( table 5 ). Among subjects with severe asthma, 68–70% of subjects were never clinically diagnosed with asthma ( table 5 ). Among subjects with current wheeze who had undiagnosed asthma, less than 1% took daily ICS ( table 5 ). In subjects with current wheeze who were clinically diagnosed with asthma, use of daily ICS increased to 2–8% in different age groups; this difference was statistically significant (p<0.001). A similar trend was noted in subjects with symptoms of severe asthma ( table 5 ). Almost 40% of doctor-diagnosed patients used beta-agonist inhaled treatment whenever they had symptoms, but less than 7% used it when asthma was not clinically confirmed by a doctor ( table 5 ).
Use of various types of medicines in subjects with current wheeze and severe asthma with or without doctor-diagnosed asthma
Data are presented as n (%), unless otherwise stated. ICS: inhaled corticosteroid; LABA: long-acting β-agonist. # : the Chi-squared test is used when all expected cell frequencies are ≥5. If expected cell frequency was <5 the Fisher exact probability test was used. ¶ : severe asthma is defined as current wheeze with more than four attacks per year or wheeze affecting speech or activity.
The GAN Phase I study was the largest multicentre study since the ISAAC Phase III to analyse the prevalence of asthma symptoms in children and adults in India. The prevalence of current wheeze was 3.16%, 3.63% and 3.30% in the 6–7 years, 13–14 years and adults, respectively. The comparison of prevalence of current wheeze across Indian centres in ISAAC Phase I and Phase III, and GAN Phase I, showed a significantly lower prevalence in both the age groups of children in the GAN study (p<0.001), but a higher prevalence for nocturnal cough (p<0.001). Most subjects with symptoms of asthma were not diagnosed clinically with asthma. A significantly higher number of current wheezers/symptoms of severe asthma with a doctor's diagnosis of asthma were taking either inhaled medications or inhaled steroids or oral medications in all three groups (p<0.001) compared to those without a doctor's diagnosis of asthma.
The time trends of prevalence of asthma from our study are contrary to the widely held belief that asthma is increasing in recent decades. However, our study reveals a significant reduction in the prevalence of current wheeze, which has been considered a symptom of asthma. The methodology, recruitment sites and investigators were the same in the ISAAC and GAN studies, thereby allowing for a reasonable comparison of data to assess the time trends. A significant reduction was also noted in the GAN study in the prevalence of most of the causal factors of current wheeze as compared to the previous ISAAC studies, such as paracetamol use, maternal smoking, farm exposure, pets in house, trucks passing outside the house and antibiotic use during the first year of life ( table 2 ). In India strict vehicle emission norms have also been implemented during this period. Conversely, use of factors such as fruit consumption and child ever breastfed were increased significantly in the GAN Phase I study as compared to the ISAAC Phase III study, which are considered as protective factors for asthma [ 11 ]. National asthma guidelines were also formulated and initiated, which would have also resulted in better outcomes [ 15 ]. The change in aforementioned environmental factors may be a possible explanation for reduction in the prevalence of current wheeze.
Nevertheless, there is a wide variation in the prevalence of wheeze in comparative studies. A questionnaire-based study in adults in India revealed the prevalence of asthma as 2.05% [ 3 ]. Another multicentre research study has reported a prevalence of asthma as 2.38% in adults [ 16 ]. An ISAAC questionnaire-based study reported the prevalence of bronchial asthma as 13.1% in children aged between 11 and 16 years (n=927). The prevalence of current subjects with asthma (defined as asthma episode(s) in the past 12 months) was 10.2% [ 17 ]. P al et al . [ 18 ] profiled 15 epidemiological studies related to asthma in children and reported the prevalence of asthma as 2.74%. Significant time has elapsed since these studies were conducted and published. These studies also had varied methodology, time frames and study population, which could be possible reasons for this difference. The recently published GBD data estimated 34.3 million cases in an Indian population of 1330 million, almost comparable to our study [ 4 ].
The GAN Phase I global data also show significant changes as per centre, age and income in prevalence of asthma across the world [ 19 ]. The world total data showed a significant decline in current wheeze, with both increase and decrease noted as per individual centre. Preliminary data from few other global centres have shown mixed results regarding time trends in the prevalence of current wheeze [ 20 – 22 ]. Data from a single centre in Mexico showed a 7.9% increase in the prevalence of current wheeze in both age groups compared with ISAAC Phase III [ 20 ]. On the other hand, the GAN Phase I study conducted in Bangkok suggests a similar prevalence of current wheeze in the younger age group and slightly lower prevalence in the older age group when compared with ISAAC Phase III [ 21 ]. Interestingly, lower prevalence of current wheeze was reported from the centres from low-income group countries while it did not change for high-income countries in either age group. However, prevalence of current wheeze was increased in upper middle-income countries [ 19 ]. There have been changes in the micro-environment and macro-environment between the phases of studies across the centres, but the exact cause of the trend would be difficult to identify.
The prevalence of current wheeze varied from centre to centre and was consistent with the previous ISAAC studies. Similar heterogeneity was documented in previous ISAAC studies, with intercontinental, intercountry, inter-regional and intra-regional variations [ 2 , 5 , 6 ]. The various cities across India have varying geography, climate, environment and socioeconomic conditions. The lowest prevalence of current wheeze was documented in Bikaner (0.35%) and the highest in Chandigarh (8.54%) in the 6–7-year age group. Bikaner is a desert area located in the western part of India and it experiences dry and hot weather associated with dust storms. Chandigarh, on the other hand, has a cooler and humid climate, situated in the northern part of the country. In the 13–14-year age group, the lowest prevalence was in New Delhi (0.89%) and the highest in Jaipur (6.62%) ( supplementary tables 1 and 2 , supplementary figure 1 ). Among adults, New Delhi (0.88%) reported the lowest prevalence and Kottayam (6.02%) the highest prevalence ( supplementary table 3 ). The findings are contradictory as Jaipur is located in western India and has a dry and arid desert climate while New Delhi is situated in the northern part of the country, with poor air quality. Kottayam is situated in southern India with a warm and tropical climate. Such variation is also observed in global data, which is difficult to explain. After ISAAC Phase III, compressed natural gas (CNG) replaced petrol and diesel in nearly all public vehicles in New Delhi in December 2002, including truck traffic [ 23 ]. Diesel exhaust particles have been associated with an increase in Th2 and Th17 cytokines, which are responsible for the asthmatic response [ 24 ]. Reduction in diesel exhaust particles may in turn have been a contributing factor for a decrease in prevalence in New Delhi. The INSEARCH study also reported variation in the prevalence of bronchial asthma (adults) among the 12 participating centres (from 0.4% in Secunderabad to 4.8% in Kolkata) [ 3 ].
The self-reported prevalence of wheeze was significantly more common in boys in both age groups (p<0.001) [ 25 ]. It is unclear why there is this gender difference in children; possible explanations are variations in sex hormone levels [ 26 ], bronchial lability [ 27 ] and allergen sensitivities [ 28 ]. Interestingly, among adults this difference was not noted for current wheeze and a significantly higher prevalence of asthma ever and doctor-diagnosed asthma were seen in women, which is consistent with previous reports in adults. Previous health surveys conducted from 2005 to 2006 in adults in India have reported a prevalence of wheeze of 1.8% (95% CI 1.6–2.0) and 1.9% (95% CI 1.8–2.0) in men and women, respectively [ 29 ].
Nocturnal cough is a symptom of asthma that has increased in prevalence during GAN Phase I compared to ISAAC Phase I and Phase III. However, nocturnal cough can be attributed to other causes also such as gastro-oesophageal reflux disease, post-nasal drip, bronchiectasis and medication-induced [ 30 ]. It is a non-specific symptom and all nocturnal cough would not be due to bronchial asthma. Nonetheless, it is worth noting the significant increase in the prevalence of nocturnal cough; a similar increase was also noted in both the age groups in the worldwide GAN Phase I data, a trend that is difficult to explain [ 19 ].
Our study reveals a gap in the diagnosis of asthma. Almost 82% of current wheezers and 70% of subjects with symptoms of severe asthma were not clinically diagnosed as having asthma by a doctor. This gap in diagnosis is high compared to a similar study that reported almost a third of the subjects remained undiagnosed [ 31 ]. Under-treatment is another problem; among doctor-diagnosed subjects with wheeze and with symptoms of severe asthma, daily ICS were used in less than 9% among different age groups of subjects ( table 5 ). Under-diagnosis and under-treatment may be attributed to lack of medical facilities, poverty, illiteracy, ignorance on the part of patients, improper techniques of medication intake, non-adherence and poor communication skills of medical personnel [ 32 – 34 ]. Apart from these factors an interesting aspect worth discussing is disease terminology used by asthmatic patients and their treating doctors. When an asthmatic patient consults a doctor, only 71% of doctors refer to “asthma” as the name of their disease and 29% use other terminology. The problem is worse at patient level; only 23% of asthmatic patients call their disease “asthma” while the rest use terminology like swas, dama or cold and cough [ 35 ]. Asthma is considered to be a stigma and many parents conceal the disease and therefore avoid medications or give only when a patient is symptomatic or unable to tolerate symptoms. Incorrect notions such as that inhalers are harmful and habit-forming also play a role in treatment non-adherence. Regular use of ICS among undiagnosed current wheezers was thereby very low; under-treatment may account for high school absenteeism, urgent medical consultation to a doctor and emergency department visits ( table 3 ). Even hospitalisation due to breathing problems was significantly high. Similarly, indexes of uncontrolled asthma such as exercise-related wheeze in children and restriction of usual activities were also significantly higher in current wheezers than healthy subjects ( table 3 ). These findings suggest high morbidity and use of hospital resources among current wheezers.
Untreated children with asthma have been found to have higher school absenteeism in similar studies [ 36 ]. Exercise-induced asthma, emergency visits, hospitalisation and school absenteeism are markers of uncontrolled asthma [ 37 ]. However, all these markers were more significantly affected in subjects having a clinical diagnosis of asthma, probably indicating that more severely affected persons consult a doctor more frequently and thereby have a higher chance of getting clinically diagnosed with asthma. However, earlier studies show that more than half of asthmatic subjects discontinue asthma medications once they tolerate symptoms and this tendency of symptom tolerance persists in more than a third of patients, even after education [ 32 , 33 ]. This issue needs to be addressed in asthma education programmes as it leads to significant clinical implications in the form of non-compliance.
Our study thus highlights an unmet need in terms of diagnosis and treatment of symptoms of asthma, thereby leading to significant morbidity resulting from the disease. Lack of patient education, concerns about medication side-effects and the stigma associated with inhalation devices might also contribute to this skewed treatment approach [ 32 , 34 ].
Underdiagnoses, delayed treatment, under-treatment or no treatment may be responsible for increased morbidity due to asthma in terms of DALYs and disproportionately high mortality [ 1 , 4 ]. These findings emphasise the need for national-level health programmes to address better strategies to diagnose and manage asthma, and also the need to communicate a diagnosis of asthma to the patient.
The GAN Phase I study was a self-reported, questionnaire-based study; objective measures of assessment of asthma and its severity, such as spirometry, were not used for diagnosis of the disease. Conducting spirometry for every child across all centres would not have been logistically feasible and would not have allowed for comparison with earlier studies. Because it was a questionnaire-based study, answers were subject to the understanding of the children and adults. Adolescents may have a poor perception of their symptoms; thus questionnaire-based assessment tools may underestimate the actual prevalence of the illness. Cough is a common symptom in subjects with asthma, especially children. Although wheeze is more specific for a diagnosis of asthma, its sensitivity is low and may therefore underestimate the prevalence of asthma. However, the previous ISAAC studies have used this particular question to calculate the prevalence of asthma [ 2 , 5 , 6 ]. The validated ISAAC questionnaire is the most authentic means of collecting childhood asthma prevalence globally [ 14 , 38 ]. Furthermore, because the study aimed to compare the current prevalence of wheeze with the previous ISAAC data, a similar questionnaire was used to maintain consistency. The study was limited by the fact that the centres participated voluntarily, and were not randomly selected. Although the participating centres were voluntary they represented the various geographies including north, south, east, west and central. Further, each centre was divided into four zones, and a fraction of schools were randomly selected from each zone to ensure appropriate representation. This same methodology was adopted by the GAN Phase I study worldwide and the previous ISAAC studies as well. The study population was representative of the population of school-going children of the respective nine centres. Despite these steps to strive for equal representation from across centres, the prevalence of asthma varies across rural and urban areas, and within cities itself due to differences in socioeconomic conditions, thus to generalise the results to the entire country or the world would not be appropriate. Potential bias could exist as some children may have refused to participate and all children may not be attending school. Furthermore, not all schools across the country were covered. Recall bias could also exist, as exposures in the first year of life could have been forgotten or incorrectly remembered. However, the same protocol was used in the previous ISAAC studies, thereby allowing for valid comparison of time trends. Prevalence of current wheeze in adults could be obtained for only those adults (age group 31–44 years) whose children were in a particular age group and were attending the participating schools; thus, a selection bias may exist.
Conclusions
The prevalence of current wheeze in the 6–7 years, 13–14 years and adults was 3.16%, 3.63% and 3.30%, respectively. There was a significant reduction in current wheeze in GAN Phase I compared with the previous ISAAC Phase III study. It was also associated with a significant reduction in the frequency of exposure to causal factors such as paracetamol use, maternal smoking, farm exposure, pets in the house and trucks passing outside the house. The problem of under-diagnosis and under-treatment of asthma was noted. Up to 82% of subjects with current wheeze and up to 70% of subjects with symptoms of severe asthma remain undiagnosed and less than 1% of undiagnosed subjects take the recommended daily ICS. Even among current wheezers with a clinical diagnosis of asthma, use of daily ICS was relatively low. The study provides valuable insights into changing trends in the prevalence of current wheeze in India and highlights under-diagnosis and under-treatment. The findings could help in planning management strategies for this non-communicable disease.
Acknowledgements
We are thankful to the children, parents and school staff who contributed to the study. We would like to thank the team at the Chest Research Foundation for their relentless efforts as partners in the coordination and execution of this study across centres. We would like to thank Dr K.R. Jat, Dr Pankaj Jorwal, Dr Rakesh Lodha, Dr Rashmi Yadav and Dr Tuhina Verma for valuable data collection at various sites. Ms Deepika Chaudhary, Ms Divya Sharma, Ms Gazala Parveen, Ms P. Lingambika, Ms Nek Parveen, Ms Pallavi, Ms Pooja, Ms Preeti Bala, Ms Monika, Ms Priya Chugh, Ms Puja, Ms Rashmi Mundada, Ms Shivani Sharma, Ms N. Vidyashree, Mr Aadi Kumar, Mr Ajil, Mr A. Akhil, Mr Anil Kumar, Mr Ankit, Mr Balaji, Mr Dushyant Acharya, Mr Hasib Rehman, Mr Jitendra Kumar, Mr Kamlesh Kumar, Mr Mohd. Javed, Mr Pankaj Rathore, Mr Prafful, Mr Rahul Kumar, Mr M. Raju, Mr Rakesh, Mr P. Ravi Kumar, Mr Ravinder Duggal, Mr Ravindra, Mr Saizan, Mr Samir, Mr Sandeep, Mr Sanjeev, Mr Sathish Chandran, Mr Sumanta Ghata, Mr Suvajit Das, Mr Treedeep, Mr Vedprakash, Mr Vishnu and Mr B. Vyshakh have been instrumental in collecting data and its entry across various sites in India. We would also like to thank Ms Sushmeeta Chhowala for valuable coordination between centres and supervision in manuscript preparation.
Provenance: Submitted article, peer reviewed.
This study was registered in the Clinical Trial Registry, India (CTRI/2018/02/011758).
Conflict of interest: There is no conflict of interest to report by any of the authors.
Support statement: This study was supported by the Cipla Foundation, Mumbai, India. Funding information for this article has been deposited with the Crossref Funder Registry .

IMAGES
COMMENTS
Background. Asthma, a major global health problem affecting as many as 235 million people worldwide [], is a common, non-communicable, and variable chronic disease that can result in episodic or persistent respiratory symptoms (e.g. shortness of breath, wheezing, chest tightness, cough) and airflow limitation, the latter being due to bronchoconstriction, airway wall thickening, and increased ...
The prevalence of asthma in adults in the United States is approximately 7.7%. 1 It is one of the most common chronic, noncommunicable diseases in the country and worldwide. 1,2 Among U.S. adults ...
According to an EAACI position paper in 2019, biomarkers for the clinical and inflammatory phenotype of asthma were summarized as follows (1) type 2 asthma: (a) ... Asthma research produces up to 9000 publications per year and represents one of the most rapidly developing areas. Most of the novel developments of the last year focus in the areas ...
Around 5-10% of the total asthmatic population suffer from severe or uncontrolled asthma, which is associated with increased mortality and hospitalization, increased health care burden and worse quality of life. In the last few years, new drugs have been launched and several asthma phenotypes according to definite biomarkers have been identified. In particular, therapy with biologics has ...
Asthma articles from across Nature Portfolio. Asthma is a form of bronchial disorder caused by inflammation of the bronchi. It is characterized by spasmodic contraction of airway smooth muscle ...
Long-term follow-up studies of adults with well-characterized asthma are sparse. We aimed to explore static lung volumes and diffusion capacity after 30 + years with asthma. Conrad Uldall Becker Schultz, Oliver Djurhuus Tupper and Charlotte Suppli Ulrik. Asthma Research and Practice 2022 8 :4.
Asthma is one of the most common chronic non-communicable diseases worldwide and is characterised by variable airflow obstruction, causing dyspnoea and wheezing. Highly effective therapies are available; asthma morbidity and mortality have vastly improved in the past 15 years, and most patients can attain good asthma control. However, undertreatment is still common, and improving patient and ...
Asthma is the most common chronic respiratory disease affecting millions of people of all ages across the globe ( 1-6 ). The average global prevalence ranges between 5-10% ( 2 ). Traditionally, asthma diagnosis was based on the history and the response to a trial of various treatments, but emerging evidence shows that under the umbrella of ...
Asthma, a chronic inflammatory airway disease, is one of the most common long-term conditions worldwide and can affect people of all ages. The Global Burden of Disease study estimated that 262 million people were living with asthma in 2019. Asthma accounts for about half a million deaths per year and is a major global economic burden in terms of both direct and indirect costs.1,2
Asthma is a disease of the airways that is characterized by chronic inflammation and disordered airway function. The purpose of writing the current review paper is to review the history, current situation, control history, challenges, and ongoing management programs of asthma. Some official websites of known respiratory professional bodies were consulted for asthma guidelines, and information ...
Abstract. Asthma is a disorder characterized by chronic airway inflammation, airway hypersensitivity to a variety of stimuli, and airway obstruction. It is at least partially reversible, either ...
Asthma is a common chronic disease characterized by episodic or persistent respiratory symptoms and airflow limitation. Asthma treatment is based on a stepwise and control-based approach that involves an iterative cycle of assessment, adjustment of the treatment and review of the response aimed to minimize symptom burden and risk of exacerbations. Anti-inflammatory treatment is the mainstay of ...
Conclusion. Asthma is a disease of the airways, characterised by inflammation and associated. with airway hyper-responsiveness, which can. result in episodes of breathlessness, chest. tightness ...
Introduction: The pharmacotherapy of asthma is a dynamic process that changes as our knowledge of the underlying pathophysiology and treatment of this disease continues to evolve. This implies the need for continuous revision of the recommendations of asthma guidelines and strategies. Areas covered: This review summarizes the latest key practical information on the pharmacological management ...
Asthma is characterized by wheezing, coughing, recurring episodes of airflow obstruction, and shortness of breath (Kumar et al., 2009). Causative agents of asthma can be allergic (pollens, molds ...
The American Lung Association is committed to funding asthma research. Our Awards and Grants Program funds top-notch researchers at important career crossroads to gain long-term commitment to lung health and disease research. Without the life-long dedication of lung researchers, important and much-needed discoveries would not be possible.
Bronchial asthma is a chronic inflammatory disease of the airways characterized by bronchial hyperreactivity and a variable degree of airway obstruction. It is diagnosed on the basis of the clinical history, physical examination, and pulmonary function tests, including reversibility testing and measurement of bronchial reactivity.
Information paper Quick reference guide: asthma in adults. Download PDF. The National Asthma Council Australia has released a quick reference guide for the diagnosis and management of asthma in adults. ... The Asthma Experts eNews is circulated monthly and includes all the latest news, views and research from the asthma world.
Introduction. The prevalence of asthma varies widely among countries/geographical regions and also within countries with different geographies and socioeconomic strata [1, 2].The Indian Study on Epidemiology of Asthma, Respiratory Symptoms and Chronic Bronchitis in Adults (INSEARCH) estimated the national burden of asthma at 17.23 million with an overall prevalence of 2.05% [].