
- High contrast
- Press Centre

Search UNICEF
- Early childhood nutrition
Preventing malnutrition in infants and young children.

- Available in:
Children need the right foods at the right time to grow and develop to their full potential. The most critical time for good nutrition is during the 1,000-day period from pregnancy until a child’s second birthday.
In the first two years of life, breastfeeding saves lives, shields children from disease, boosts brain development and guarantees children a safe and nutritious food source. UNICEF and the World Health Organization (WHO) recommend that infants begin breastfeeding within one hour of birth, be exclusively breastfed for the first six months, and continue breastfeeding until 2 years of age or beyond.
At the age of 6 months, children need to begin eating their first foods. Young children should be fed frequently and in adequate quantities throughout the day, and their meals must be nutrient-dense and comprised of a variety of food groups. Caregivers should prepare and feed meals with clean hands and dishes, and interact with their child to respond to his or her hunger signals.
What, when and how children eat is more important before age 2 than at any other time in life. Yet, today, many infants and young children are not receiving the nutrition they need to survive and thrive.
Fewer than half of the world’s newborns are benefiting from the life-saving power of breastfeeding during the first hour of life. And only three out of five infants younger than 6 months of age are breastfed exclusively.
Children’s first foods too often lack diversity and are low in energy and nutrients. Globally, one in three children aged 6–23 months is eating the minimum diverse diet needed for healthy growth and development.
Young children’s diets are frequently comprised of grains – with little fruit, vegetables, eggs, dairy, fish or meat. Many are increasingly being fed sugary drinks and packaged snacks high in salt, sugar and fat.
Poor diets in early childhood can lead to deficiencies in essential vitamins and nutrients – such as vitamin A deficiency, which weakens children’s immunity, increases their risk of blindness and can lead to death from common childhood diseases like diarrhoea.
Meeting children’s nutrient needs in early life can be challenging, and many parents face barriers to securing enough nutritious, safe, affordable and age-appropriate food for their children. These challenges are even greater during conflicts, disasters and other humanitarian crises.
UNICEF’s response

Improving the quality of children’s foods and feeding practices in the earliest years of life is the cornerstone of preventing malnutrition in all its forms.
UNICEF early childhood nutrition programmes aim to prevent all forms of malnutrition by:
Protecting, promoting and supporting breastfeeding
UNICEF strengthens breastfeeding counselling and support, and advocates for maternity protection and other protective policies. To protect mothers and babies from marketing practices that undermine breastfeeding, UNICEF works to strengthen national legislation on the International Code of Marketing of Breastmilk Substitutes and related World Health Assembly resolutions. UNICEF also provides specific support on infant feeding to mothers living with HIV and other infections, as well as those facing emergencies.
Together with WHO, UNICEF leads the Global Breastfeeding Collective , a partnership of prominent organizations working to increase political commitment to and investments in breastfeeding.
Improving first foods and feeding practices for infants and young children
UNICEF promotes access to nutritious, safe and affordable foods for children aged 6–23 months. Where nutritious foods are out of reach, UNICEF supports the use of multiple micronutrient powders and fortified foods to improve the quality of children’s diets. We help countries better regulate the labelling and marketing of commercially produced foods and beverages for children, and support caregivers to improve feeding practices through counselling and social and behaviour change communication.
Improving foods and feeding practices for children aged 3–5 years
UNICEF promotes access to nutritious, safe and affordable foods and healthy food environments for children in homes, day care, and early childhood development centres. Where nutritious diets are out of reach, we support the use of multiple micronutrient powders and fortified foods to improve the nutrient quality of children’s diets.
Providing micronutrient supplementation and deworming
UNICEF helps deliver vitamin A supplementation , deworming prophylaxis and iron-containing supplements to children under 5 in areas where nutrient-poor diets prevail, and where micronutrient deficiencies are common. We help align these services with global and national guidelines, and work with governments to provide micronutrient supplementation as part of routine health services for children.
Promoting healthy food environments
UNICEF helps governments adopt policies that foster healthy food environments, improve the availability and affordability of nutritious foods, and safeguard children from consuming unhealthy foods and beverages. This includes ensuring that such policies are free from commercial influence.
More from UNICEF

Global Breastfeeding Collective
Investing in breastfeeding worldwide

Acute hunger remains persistently high in 59 countries with 1 in 5 people assessed in need of critical urgent action - Global Report on Food Crises

Armed violence deepening malnutrition crisis for children in Haiti
Acute malnutrition has doubled in one month in the north of Gaza strip: UNICEF

Healthy Living
Childhood Nutrition

Nearly 1 in 3 children in America is overweight or obese . Despite all the focus on kids being overweight and obese, many parents are still confused, especially when it comes to what kids eat. How much does your child need? Is he getting enough calcium? Enough iron? Too much fat?
Whether you have a toddler or a teen, nutrition is important to his or her physical and mental development. Here's what children need — no matter what the age.
During this stage of life, it's almost all about the milk — whether it's breast milk , formula , or a combination of the two. Breast milk or formula will provide practically every nutrient a baby needs for the first year of life.
At about six months most babies are ready to start solid foods like iron-fortified infant cereal and strained fruits, vegetables, and pureed meats. Because breast milk may not provide enough iron and zinc when babies are around six to nine months, fortified cereals and meats can help breastfed babies in particular.
Once you do start adding foods, don't go low-fat crazy . Although the AAP guidelines state fat restriction in some babies is appropriate, in general, you don't want to restrict fats under age two because a healthy amount of fat is important for babies' brain and nerve development.
Toddlers & Preschoolers
Toddlers and preschoolers grow in spurts and their appetites come and go in spurts, so they may eat a whole lot one day and then hardly anything the next. It's normal, and as long as you offer them a healthy selection, they will get what they need.
Calcium, the body's building block, is needed to develop strong, healthy bones and teeth. Children may not believe or care that milk "does a body good," but it is the best source of much-needed calcium. Still, there's hope for the milk-allergic , lactose-intolerant, or those who just don't like milk. Lactose-free milk, soy milk, tofu, sardines, and calcium-fortified orange juices, cereals, waffles, and oatmeal are some calcium-filled options. In some cases, pediatricians may recommend calcium supplements.
Fiber is another important focus. Toddlers start to say "no" more and preschoolers can be especially opinionated about what they eat. The kids may want to stick to the bland, beige, starchy diet (think chicken nuggets, fries, macaroni), but this is really the time to encourage fruits, vegetables , whole grains, and beans, which all provide fiber. Not only does fiber prevent heart disease and other conditions, but it also helps aid digestion and prevents constipation , something you and your child will be thankful for.
Gradeschoolers
It isn't uncommon for a 6- or 7-year-old to suddenly decide to be a vegetarian once they understand animals and where food comes from. This doesn't mean your child won't get enough protein ; animal tissue isn't the only place we get protein. Rice, beans, eggs, milk, and peanut butter all have protein. So whether your child goes "no-meat" for a week or for life, he or she will likely still get sufficient amounts of protein.
Areas that might be a little too sufficient are sugars, fats, and sodium.
This is a time when kids first go to school and have a little bit more choices in what they eat, especially if they're getting it in the cafeteria themselves. Cakes, candy, chips, and other snacks might become lunchtime staples.
The body needs carbs (sugars), fats, and sodium, but should be eaten in moderation, as too much can lead to unneeded weight gain and other health problems.
Packing your child's lunch or going over the lunch menu and encouraging him or her to select healthier choices can help keep things on track.
Preteens & Teens
As puberty kicks in, young people need more calories to support the many changes they will experience. Unfortunately, for some, those extra calories come from fast food or "junk" foods with little nutritional value.
Some adolescents go the opposite way and restrict calories, fats, or carbs. Adolescence is the time kids start to become conscious of their weight and body image, which, for some, can lead to eating disorders or other unhealthy behaviors. Parents should be aware of changes in their child's eating patterns and make family dinners a priority at least once or twice a week.
Like calories, calcium requirements are higher. Calcium is more important than ever during the tween and teen years because the majority of bone mass is built during this time. Encouraging kids to have milk, milk products, or calcium-rich alternatives, should help them get more calcium.
Your child's gender may play a role in whether he or she needs more of a particular nutrient. For instance, teen girls need more iron than their male counterparts to replace what's lost during menstruation , and males need slightly more protein than girls.
Although getting your child to eat healthy — regardless of his or her age — can be a constant battle, its one well worth fighting. A healthy child becomes a healthy adult, and only with your support and guidance will your child be both.
Water: Drink Up!
Water makes up more than half of kids' body weight and is needed to keep all parts of the body functioning properly.
There's no specific amount of water recommended for children, but it's a good idea to give them water throughout the day — not just when they're thirsty.
Babies generally don't need water during the first year of life.
If your child doesn't like the taste of water, add a bit of lemon or lime for flavor.
Fruits and veggies are also good sources of water.
Kids should drink more water when ill, when it's hot out , or when engaged in physical activity.
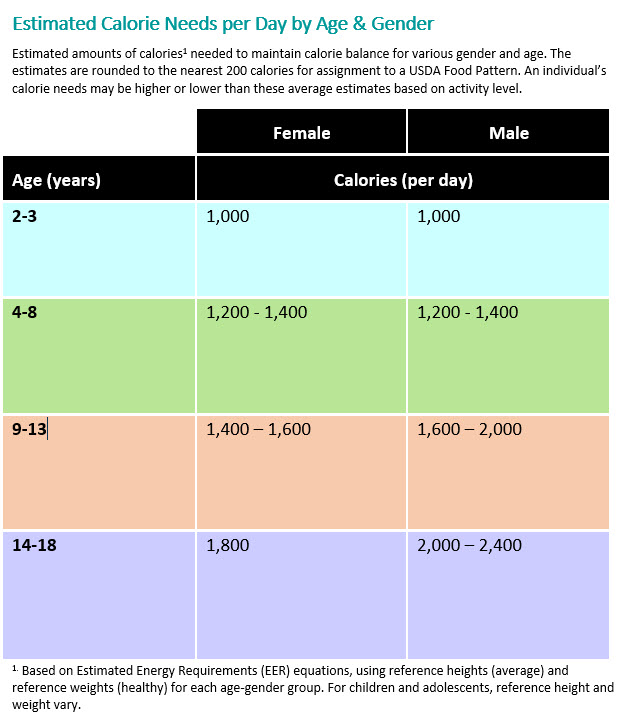
Recommended Amount of Calories
Here's what the United States Department of Agriculture (USDA) recommends kids get calorie-wise and from each food group for a healthy, balanced diet:
Additional Information from HealthyChildren.org:
- Kids Need Fiber: Here's Why and How
- How to Get Your Child to Eat More Fruits and Veggies
- Making Healthy Food Choices
- Healthy and Unhealthy Choices at Fast Food Restaurants

The Importance of Nutrition in Early Childhood Development
by NDFAuthors
- Sep 11, 2016
We all instinctively know from birth that food is essential to our own survival. Studies show that a nutritious diet will make your child healthier and better able to learn.
Children can be picky eaters. For many parents, picturing a toddler stubbornly throwing a piece of broccoli to the floor in disgust is easy – after all, it’s an all too familiar scene. However tiring it might be, it’s important that you find ways to convince your child to eat that piece of broccoli, as studies show that having a balanced and nutritious diet directly impacts all aspects of a child’s growth and development.
Why is Nutrition so Important for Children?
The relationship between nutrition, health and learning is undeniably strong: nutrition is one of the three major factors that impact a child’s development. As genes and environment are the other two factors, eating a certain food cannot guarantee that your child will be smarter, although my mother did successfully teach (trick?) me to eat fish when I was little for that very reason. Nevertheless, research studies show that nutrition in a child’s early years is linked to their health and academic performance in later years.

Copyright: Lana K
Nutrition and Health
However you might personally define it, “a child’s early years” begin before birth when it comes to nutrition. Under-nutrition during pregnancy stunts foetal growth and can lead to poor brain development that result in irreversible chronic illnesses. Under-nutrition of a breastfeeding mother will likewise negatively impact a child’s development, especially in the first 6 months when breast milk is all he/she is consuming. For all soon-to-be and new mothers, it’s worth making sure you’re consuming a healthy and balanced diet full of the vital nutrients that both you and your child need: carbohydrates, protein, calcium, iron and vitamins A, C and D. Although at first glance this list seems overbearing, realistically you probably consume most of these nutrients already – it’s just about following proportions, which the eatwell plate helps to illustrate.
Is it really that important for children to be consuming all of the above nutrients though? The short answer: yes. The benefits of good nutrition to health are endless, but the following few conclusions made by researchers serve to prove my point. Firstly, breastfeeding by mothers following nutritious diets leads to fewer and less severe cases among their children of illnesses including diarrhoea, ear infection and bacterial meningitis. This is because better-nourished children have an enhanced natural ability to fight infection. Secondly, since iron is a vital component of brain tissue, iron deficiency makes nerve impulses move slower and may cause permanent damage to a child’s brain, especially in the first two years of his/her life; iron deficiency during this time is linked to behaviour changes and delayed psychomotor development. However, too much iron also presents problems. As my mother wisely often tells me, “the key is to find the middle way”. Thirdly, under-nutrition has been proven to decrease a child’s activity levels, social interactions, curiosity and cognitive functioning. Although parents everywhere probably harbour the wish that their child wasn’t quite so hyperactively jumping on their bed at 6am, good nutrition remains a must.

Copyright: DeeMPhotography
Nutrition and Academic Performance
It seems bizarre to think that what your child consumes at, say, 4 months will affect their learning ability years later. Research has proven this true. Throughout their early childhood, it’s important to monitor your child’s nutrient intake for the sake of their later performance. For instance, breastfeeding appears to lead to higher IQ, while iron deficiency correlates with reduced cognition and achievement at school age. More obviously to the layman, since under-nourished children get sick more often, they miss more school and fail to keep up with peers. Research has made the link even clearer: school-age children who eat breakfast do better in tests than those that go without.
“Eat up please”
When there’s work to go to, bills to pay and dishes to wash, getting your child to eat what they don’t want to (especially when doing so might cause a much-dreaded tantrum) is oftentimes the least of your worries. But it’s critically important. Following nutrition guidelines is relatively straightforward during pregnancy, as well as at the start of your child’s life. When your child starts to form likes and dislikes, my advice to you is to accept preferences but continue to introduce new foods by making silly faces and playing peek-a-boo until you hear that giggle and see your toddler happily putting the spoon into their mouth themselves. Persevere. I promise he/she will thank you one day.
YOU MIGHT ALSO LIKE

Another Successful Season of Giving: Children from the village of Rvati get their own kindergarten

Participants' impressions from Šabac: The support we provide to the child actually leads to perfection, because each child is perfect in their own way

We distributed New Year's Presents to Children in Banat

Noelle and Luka Bjelic Donated Their Wedding to Novak Djokovic Foundation

Season of Giving Has Started: Let's Build a Better Future for 60 Children in Rural Serbia

Novak Djokovic Foundation Equips "Fawn" Kindergarten in Nis, Creating Spaces for an Additional 110 Children

The Novak Djokovic Foundation has Equipped a Preschool from 175 Children in Beocin

Dr. Gabor Mate - Thank you!

Premiere of the documentary film "Wisdom of Trauma" by Dr. Gabor Maté in Serbia and the region in September

More Stories from "Support, not Perfection Workshops in Petrovac na Mlavi

Family Hobbies and Activities that Improve Health and Well-being

Support, not Perfection: Parent Impressions from Petrovac na Mlavi

A "strange" family

The Power of Play: How Sports and Hobbies Impact Learning and Development
Dr. Gabor Maté is Coming to Our Region

Global Day of Parents
Newsletter preferences, email address*, first name*, language preference.
- Search Menu
- Advance articles
- Editor's Choice
- Supplement Archive
- Article Collection Archive
- Author Guidelines
- Submission Site
- Open Access
- Call for Papers
- Why Publish?
- About Nutrition Reviews
- About International Life Sciences Institute
- Editorial Board
- Early Career Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction, school-age health and nutrition terminology and knowledge gaps, specificities of growth and development in school age, role of nutrition in school age, global status of nutrition in school age, recovery from nutrient deficiencies, growth faltering, and cognition in school-age children, revisiting priorities, acknowledgments.
- < Previous
Nutrition in school-age children: a rationale for revisiting priorities
- Article contents
- Figures & tables
- Supplementary Data
Jose M Saavedra, Andrew M Prentice, Nutrition in school-age children: a rationale for revisiting priorities, Nutrition Reviews , Volume 81, Issue 7, July 2023, Pages 823–843, https://doi.org/10.1093/nutrit/nuac089
- Permissions Icon Permissions
Middle childhood and early adolescence have received disproportionately low levels of scientific attention relative to other life stages, especially as related to nutrition and health. This is partly due to the justified emphasis on the first 1000 days of life, and the idea that early deficits and consequences may not be fully reversible. In addition, these stages of life may superficially appear less “eventful” than infancy or late adolescence. Finally, there has been historical ambiguity and inconsistency in terminology, depending on whether viewing “childhood” through physiologic, social, legal, or other lenses. Nevertheless, this age bracket, which encompasses most of the primary education and basic schooling years for most individuals, is marked by significant changes, inflection points, and sexually driven divergence in somatic and brain growth and development trajectories. These constitute transformative changes, and thus middle childhood and early adolescence represents a major and last opportunity to influence long-term health and productivity. This review highlights the specificities of growth and development in school age, with a focus on middle childhood and early adolescence (5 years–15 years of age, for the purposes of this review), the role of nutrition, the short- and long-term consequences of inadequate nutrition, and the current global status of nutrition in this age group. Adequate attention and emphasis on nutrition in the school-age years is critical: (a) for maintaining an adequate course of somatic and cognitive development, (b) for taking advantage of this last major opportunity to correct deficits of undernutrition and “catch-up” to normal life course development, and (c) for addressing the nutritional inadequacies and mitigating the longer-term consequences of overnutrition. This review summarizes and provides a rationale for prioritizing nutrition in school-age children, and for the need to revisit priorities and focus on this part of the life cycle to maximize individuals’ potential and their contribution to society.
The last three decades of academic and public health efforts have enthusiastically embraced the importance of early life nutrition as a foundational component of lifelong health. The gestational period through the first 2 years of age (the first 1000 d) and early childhood through 5 years of age have received justified attention over the last few decades. However, the ultimate realization of an individual’s potential requires a successful bridging from early childhood to adulthood. The subsequent periods in the life cycle—5 years to 9 years of age, referred to as “middle childhood,” and 10 years–15 years, “early adolescence”—are commonly encompassed in the “school years.”
Middle childhood and early adolescence bridge the period between the relatively steady growth occurring from 2 years to 5 years of age and the final maturation period of late adolescence to adulthood. This period is characterized by multiple dramatic inflection points in the course of growth and development, as well as behavioral and psychosocial events occurring around the arrival of puberty. These inflections represent transformational changes in the brain and cognitive processing, linear bone growth and bone mineralization, body composition, and other organ systems. It is also during this period that major sex-driven inflections and divergences occur in growth and development. The nutrition of children during this period is critical for supporting these changes. In addition, can help overcome early deficits, and may help correct dietary excesses that have been occurring since infancy. Thus, school age constitutes a final major window of opportunity to influence growth and development, and the associated health consequences in mature life.
Unfortunately, relative to other life stages, school-age nutrition has received a disproportionately low level of scientific attention, in part due to a misleading but widespread perception that early deficits in growth and development cannot be rectified. In the last few years, scientific, public health, and other academic voices have been calling attention to this life stage as a critical and potentially last major window of opportunity for intervention in maximizing the potential of individuals as productive members of society. 1–5
This aim of this review was to highlight the critical growth, developmental, and nutritional aspects of these transformative school-age years, and the challenges and gaps in knowledge around these, and to provide arguments for why nutrition during school age deserves greater and more focused attention to maximize individuals’ growth, development, and ultimate productivity.
To achieve this aim, a comprehensive review of the literature was conducted, using PubMed to identify eligible and relevant publications through 2021. Papers were identified by combining the following Medical Subject Heading keywords: children, school age, middle childhood, adolescence, nutrition, nutrients, growth, development (multiple aspects/organ systems), malnutrition, stunting, overweight, and obesity. Literature was selected and prioritized that included information and data for the 5–15-year age group, primarily based on population, cohort, or epidemiologic studies and reviews, as well as literature addressing biologic aspects of specific areas of growth and development for this age group, with a focus on somatic growth, body composition, and neurologic development. Nutrition- and diet-related behavioral, psychologic, or social aspects were not included in the scope of this review.
Compared with the nutrition and health research literature for other life stages, there is a historical neglect of middle childhood and adolescence. Estimates of the published literature describing child health (PubMed sources 2005–2016) show 95.3% of this literature is dedicated to early childhood (<5 y), 3.5% to 5 years–9 years, 0.55% to 10 years–14 years, and 0.61% to 15 years–19 years. 6 The health and nutritional status of school-age children, particularly that during middle childhood, remains the least studied of all life stages.
Public databases of most agencies track rates of malnutrition, stunting, and other health markers for children, but usually do so only until 5 years of age, and only pick up again during adolescence or adulthood. 7 Regional or international databases of nutritional data for middle childhood (5 y–10 y of age) are extremely scarce. Many reviews for this age group rely on extrapolations, eg, using Demographic and Health Surveys (DHS) data for children 4 years–5 years of age 8 or including data of 10-year-olds to 14-year-olds within child surveys. 9 On the other end of school age, most research and data for children 10 years–15 years (early adolescence) is sometimes conflated with the data of adults, eg, Multiple Indicator Cluster Surveys (MICS) and DHS data for females 15 years–19 years. As discussed below, research, particularly concerning child growth and cognition, led to the notion that the consequences of nutritional and environmental insults in the first 2 years of age were irreversible. This may have resulted in reduced interest and research bias, due to underestimating the significant potential for growth and developmental catch-up possible during middle childhood and adolescence.
In part, inadequate research in this age group is also due to ambiguity, inconsistency, and overlapping terminology, resulting from viewing this age group through different lenses: physiologic, reproductive, social, legal, or school system, etc. Terms such as “early childhood,” “middle childhood,” “late childhood,” “school age”, “adolescence,” and “young adulthood” often overlap. From the general physiologic point of view, “middle childhood” (ages 5 y–9 y) is a period of growth and consolidation, followed by an adolescent growth spurt (ages 10 y–14 y), each associated with specific behavioral changes, before a final growth consolidation (ages 15 y to early 20s), and subsequent maturation into adulthood. 1 More broadly speaking, the developmental stages in the life cycle have been classified into 3 main categories: physical growth, cognitive development, and socioemotional/psychosocial development. 10 And while interdependent, the rate of progress for each of these life-stage categories can vary individually, making it hard to propose a purely chronological or age-based approach.
Many organizations and legal systems define “child” as an individual 0 years–18 years. 8 , 11 WHO defines an “adolescent” as aged 10 years to 19 years, “youth” in general as 15 years–24 years, and “young people” covers 10 years–24 years. 2 , 12 More recently, a broader definition for “adolescence” has been advocated as including the entire 10-year-old to 24-year-old group within the term. As explained by the 2016 Lancet Commission on Adolescent Health and elsewhere, 9 , 12 this would support consideration of appropriate social and economic policies, service systems, and legal frameworks for this broad age group. While useful for certain objectives, this approach fails to distinguish the significant differences between the transitional aspects of development (and therefore the distinct difference in needs) of early adolescence versus late adolescence. Others support the use of “young people” (not “adolescents”) as a term for all 10–24-year-olds, distinguishing “adolescents” (10 y–19 y) from “young adults” or “emerging adults” (20 y–24 y). And some suggest that considering people in their early 20s as adolescents could lead to underestimating their competencies and capabilities. 13 Clearly, no definition should be rigid. Approaches to defining “school age” and “adolescence” can vary by setting and should consider the cultural and societal context.
Schools are a significant platform, not always adequately utilized, for delivering nutrition as well as education in nutrition. “Schooling” plays a role as a defining factor in a person’s development, includes what is generally called “primary” and “secondary” schooling, and is quite variable from country to country. Globally, most children in primary school are between 5 years and 14 years of age, and there tends to be late entry into school in low- and middle-income countries. Many consider that “high school” and “preparatory school” fall into this category; others do not. Schooling provides opportunities for promoting nutrition and health. Research and interventions can leverage society’s investment in education and take advantage of the potential synergy between health and education investments. 1 , Figure 1 summarizes the terminology most commonly used for childhood growth and developmental stages. Acknowledging there is no perfect life-stage categorization, given the physiologic and growth changes, most agree that data should be disaggregated for 5 years–9 years (middle childhood), 10 years–14 years (early adolescence), 15 years–20 years (late adolescence), and 20 years–24 years (older adolescents or young adults). 1 , 9 ”School age” defined as comprising “middle childhood” (5 y–9 y) and “early adolescence” (10 y–15 y) will be the age group of focus and the terminology used in this paper.
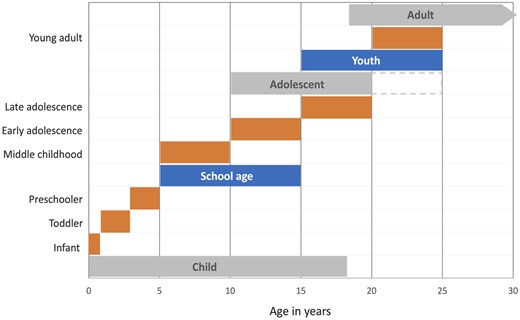
Major developmental life stages (in gray) and commonly used terminology for specific developmental stages as related to age . Modified and adapted from Bundy et al 2017 1 and Sawyer et al 2018 9
What makes school age of particular significance nutritionally is that it encompasses numerous changes in trajectory from the relatively steady growth of the preschool child, through sex differentiation, and into the final consolidation period of late adolescence. These changes are driven by pubertal onset and course, with population variations primarily dependent on genetic, environmental, and nutritional factors. Pubertal sex hormone secretion will also determine changes in growth rate and growth termination. However, much work still remains to be done in understanding the underlying genetics, the timing of puberty (including early-life determining factors), growth variability during puberty, and adiposity and weight gain. 14
Two specific processes contribute to the sex-differentiating physical developmental changes during this period: adrenarche and gonadarche. Adrenarche occurs between 6 years and 8 years of age, earlier in girls and later in boys, and refers to the maturation of the adrenal cortex and increased secretion of adrenal androgens, namely dehydroepiandrosterone. It is involved in the development of pubic hair (pubarche), body odor, skin oiliness, and axillary hair. Gonadarche is initiated by specialized neurons of the hypothalamus that secrete gonadotropin-releasing hormone (GnRH) in a cyclical pattern that regulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) by the anterior pituitary, leading to gonadarche, starting at around 9 years–10 years of age in girls, and around 10 years–12 years in boys. In girls, FSH stimulates estrogen production, follicle formation, and eventually ovulation and menarche. In boys, LH stimulates testosterone production and eventually maturation of spermatozoa.
Finally, these changes during middle childhood and early adolescence are directly related to a differentiated phase of social learning and experimentation, heralding shifts in cognition, motivation, and social behavior, with significant implications for the ultimate development of each child’s personality. These shifts encompass major domains such as the development of independence and decision-making, acquisition of cultural norms, increase in complex moral reasoning, increase in understanding of social hierarchies, increase in sense of gender identity, gender segregation, and romantic attraction, as well as changes in food preferences and dietary habits, the expansion of which are beyond the scope of this paper. 15
These growth and change phenomena and influential factors are interrelated, and nutrition plays a fundamental role. Protein-energy malnutrition is associated with delayed puberty, and subsequently poor growth and development. Secular trends have changed the timing of these processes in different populations, likely reflecting nutrition and health changes in the last century. In Europe and North America, from the early 19th century to the mid 20th century, age at menarche decreased from approximately 17 years to about 12 years–13 years. 16 In China, in just the past 25 years, the mean age of menarche has decreased by 4.5 months per decade. 17 As discussed below, changes in growth patterns, particularly in height and body–mass index (BMI), are interrelated with the onset of puberty. Increases in height and BMI are associated with an earlier onset of puberty, and earlier puberty is associated with an increased rate of later obesity. 14 Obesity, which has risen dramatically in children, is associated with a shift towards earlier onset of puberty, particularly in girls; the situation is less clear in boys. 16
The course of sex hormone secretion will determine the termination of growth during late adolescence into adulthood. The pubertal process is usually complete 2 years to 4 years after physical changes begin to occur. However, physical maturation will continue into the third decade of life. For instance, bone and brain development continues into the 20 s. Hormonal differences during puberty will also affect the size and function of organ systems related to aerobic and anaerobic physical fitness. Heart size and cardiac function, lung size, bone development, muscle volume and strength, erythropoiesis, and substrate utilization will diverge and determine different ultimate fitness and strength levels. 18
Puberty happens in the middle of the school-age years and marks and determines the changes in trajectory and the switch in somatic and brain growth and development rates, which characterize this part of the life cycle. Two significant phenomena arise in this period:
Several inflection points and trajectory changes occur in somatic and brain growth and development, at different time points, for various measures of development (eg, height, adiposity, lean mass accretion, bone mineralization, brain growth and reorganization, with subsequent cognitive development, and secondary sexual characteristics) and social and behavioral changes
Sex divergences appear or become significantly more pronounced in these measures.
The dynamic somatic, cognitive, and behavioral changes that occur during school age underscore the importance of preparing children during middle childhood and facilitating their transition into adolescence during this period. Figure 2 shows the changes in trajectory for key anthropometric changes during the school years.
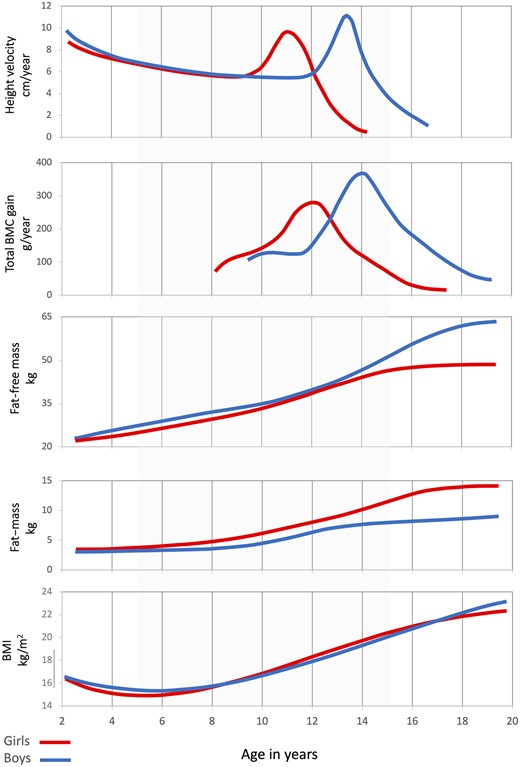
Growth trajectories in school-age years (gray-shaded area) . Fat and fat mass: estimates. All others are medians . Compiled and adapted from Tanner and Davies 1985 24 (height velocity), Weaver et al 2016 33 (BMC gain), Veldhuis et al 2005 21 (fat and fat mass), US CDC 19 (BMI). BMC: bone mineral content; BMI: body–mass index
Body composition
Although height velocity decreases during the preschool years, height gain remains relatively steady, and the amount of body fat remains relatively constant; therefore, most children in middle school will appear slimmer than when they were toddlers. In fact, median BMI will be at its lowest in life at about 5.2 years in girls and at about 5.75 years in boys, ie, just as they enter school age. 19 During this period, a child’s adiposity (corresponding to an increase in number of adipocytes) will rise, giving way to what is called the “adiposity rebound” or second rise in BMI during life. BMI, a reflection of adiposity, is the first anthropometric inflection point to appear in the school-age years. 20
The age at which this inflection happens is inversely proportional to their BMI percentile (children with higher BMI will rebound earlier). Furthermore, an earlier adiposity rebound is associated with a higher risk of later obesity. As mentioned above, secular trends show an interplay between nutritional status and puberty. In addition, overweight and obesity in girls will lead to earlier puberty. Boys, however, show a less clear pattern: overweight boys seem to mature earlier, but obese boys mature later. The mechanisms are not yet clear, and there appears to be a bidirectional influence between puberty and weight gain. 16
Body compositional changes during the school years also mark significant changes in trajectory and sex divergence. Large-scale normative data for body compositional changes for middle childhood and early adolescence are lacking, although some estimations and extrapolations have been done. Fat mass, fat-free mass, and percentage body fat have been estimated by aggregating data from several cross-sectional analyses from European and American populations. 21 During the preschool years, actual fat mass in kilograms is similar in both sexes. Between 5 years and 10 years, girls will accumulate fat mass faster than boys, gaining approximately 6% (2 kg) more than boys. After this, with the onset of puberty, girls will gain about 1.14 kg of fat, while boys will maintain a relatively fixed fat mass. Throughout the school years, until 15 years, girls will have increased their fat mass almost 5-fold, while boys will have increased theirs by around 3-fold. Ultimately, fat mass will increase from 10%–12% of body weight at birth to approximately 15% in young men and approximately 25% in young women. In boys, after a prepubertal increase in percentage body fat, this percentage actually declines with puberty and stabilizes with maturation. 21 The rate of accumulation of fat-free mass (including muscle mass) remains comparable by sex until the onset of puberty. With the onset of puberty, boys will accumulate lean mass significantly faster and for a longer period than girls. Gains in adipose tissue are primarily driven by an increase in the number and size of fat cells, while muscle development happens mainly by an increase in muscle cell mass (hypertrophy). The increase in body weight gain during puberty is mainly attained through an increase in lean tissue in boys.
Skeletal muscle mass, which represents about 25% of body weight at birth, will increase to 40%–45% body weight in late adolescence. 18 , 20 Girls will reach adult stabilization by 15 years–16 years, while boys will do so by 18 years–20 years. 21 Skeletal muscle mass has been estimated for children of school age using appendicular lean tissue mass extracted from dual photon absorptiometry measurements 22 and bioelectrical impedance. 23 Both approaches show that muscle mass and rates of gain are similar in both sexes until middle childhood. At around 5 years of age, boys maintain a slightly higher muscle mass, and girls a higher fat mass, after which trajectories increasingly diverge. This results in an approximately 3.5–5-fold increase in muscle mass in boys and a 3–4-fold increase in muscle mass in girls between 5 years and 15 years, in part depending on the methodology used. Conversely, fat mass will increase more in girls than in boys during this period.
Height and linear bone growth
The increase in height gain is the most noticeable change in trajectory in anthropometric measures of the school years. About 40% of an individual’s linear growth will occur during this time. Based on the United States CDC growth curve medians, by 5 years of age, boys and girls will, on average, be at 61% and 65%, respectively, of their ultimate height. By 15 years, they will be at 96% and 99%, respectively of ultimate height. 19 There are major differences between the first 5 and second 5 years of school age.
During middle childhood, height velocity actually decreases, to the lowest levels of the entire life cycle, only to quickly increase in the middle of the school years to the highest rate of linear gain of all post-infancy years. In North America, CDC growth velocity charts 19 show median height velocity will be at its lowest since birth just before 9 years of age in girls and at approximately 10.5 years in boys. At that point, before the puberty-related acceleration, both girls and boys will have reached ∼80% of their final height. Thus, height at that point will be a strong predictor of ultimate height in most individuals. This speaks to the importance of adequate nutrition and sustained growth between 5 years and 10 years of age.
With the onset of puberty, height velocity rapidly increases. In early adolescence, median peak height velocity in girls reaches its peak at around 11.5 years of age, with growth rates similar to those at 2 years of age (∼8.3 cm/y). In boys, a peak growth rate of about 9.5 cm/year happens at around 13.5 years of age, surpassing the 2 years of age rate of height attainment. 24 In girls, this growth spurt starts earlier (∼9 y in girls vs ∼10.5 y in boys) and ends earlier (∼11.5 y vs ∼13.5 y), lasting at least 0.5 years less than in boys. The ultimate median height in males will be greater due to greater height at the onset of puberty (boys ∼9 cm–10 cm taller than girls), a more prolonged growth spurt period, and a greater increase following pubertal onset (boys gaining ∼3 cm more than girls between the onset and end of the growth spurt). The pubertal growth rate declines rapidly after their gender-specific peak in both sexes, to 1 cm/year or less after 14.5 years in girls and 17 years in boys. 21 , 24
Height gains are dependent on longitudinal bone growth determined by epiphyseal growth plate function. Growth plate chondrocytes proliferate by mitosis, mature, become hypertrophic, lengthen the bone, and ultimately replace osteoblasts to form new calcified bone tissue. Growth hormone and insulin-like growth factor are the key hormonal drivers of this process. Adequate nutrition is critical for providing substrates for epiphysial growth, particularly energy, protein, and zinc. Calcium and vitamin D may play lesser roles in longitudinal bone growth. Very importantly, independent of nutrient provision, bone growth regulation can be blocked by corticosteroids and inflammatory cytokines. Chronic inflammation from infection, environmental factors, autoimmune disease, and the use of corticosteroids can all curtail linear bone growth. In addition, inflammation can lead to insulin and growth hormone resistance, which can further inhibit linear bone growth, thus compounding the effect of undernutrition, as often occurs in underserved populations. 25–27 As discussed below, poor linear growth and stunting (two standard deviations beyond the normal curve median) remain the most prevalent clinical manifestation of undernutrition globally. 28
Bone mineralization
Linear bone growth is followed by increases in bone mass and bone mineralization. Bone matrix becomes mineralized with the deposition of calcium phosphate nanocrystals (carbonated hydroxyapatite). The degree of deposition will determine bone mineral content (BMC), measured in grams, for a specific skeletal location or for the total body. This sequence of events will be similar, with variations by sex.
Total BMC will rapidly increase in early adolescence. Data derived from North American individuals show that by the end of middle childhood, prior to the onset of the growth spurt (2.5 y to 3 y before peak height), children will have achieved 37%–40% of ultimate total body BMC. In the short period between the 2 years before and 2 years after peak height is attained, another 39% of ultimate BMC is accrued. By the end of school age, more than 80% of total body BMC will have been attained, and final total body BMC appears to plateau at around 18 years of age in girls and 20 years in boys. 29 , 30
Similar to height gain, the BMC accretion will increase rapidly with the onset of puberty, and the median peak rate of BMC accretion will occur at around 12.5 years in girls and 14 years in boys. Thus, the peak BMC accretion rate will lag compared with the peak height velocity, which occurs at around 11.5 years and around 13.5 years in girls and boys, respectively. Therefore, there is a transient decrease in bone density relative to height and bone elongation, and consequently an increase in bone fragility lasting about 12 months in girls and 6 months in boys (see Figure 2 ). This may partially explain the higher rate of forearm fractures reported in girls between 8 years and 10 years, and in boys between 10 years and 12 years. 30 , 31
Ultimate bone mass, measured as bone mineral density (BMD) or mineral content divided by bone area, will depend on genetic and environmental factors. Studies in twins suggest that genetics can explain 50%–85% of the variance in peak bone mass, with multiple genes being involved, some of which may interact with environmental factors, including diet. 32 Thus diet and “lifestyle” factors, including exercise, can still significantly influence BMC and BMD. As stated above, middle childhood and early adolescence are the periods of fastest mineral accrual, and more than 90% bone mass is achieved by 18 years–20 years. By the late 20s, bone mass will begin a gradual process of decline, leading to varying degrees of osteoporosis, which can only partially be modified by diet and other environmental factors. It follows that school age becomes a critical age of intervention and “investment” in bone health by maximizing peak bone mass and decreasing the risk of fractures in later life. This includes optimizing nutrition, particularly provision of protein, calcium, and vitamin D, as well as activity and exercise during this life stage. 31 , 33
Brain and cognition
Brain size increases by 4-fold during the preschool years, reaching approximately 90% of adult volume by age 6. 34 However, brain development will be a continuous process with age-specific phases until adulthood. The growth rate of cortical gray matter peaks during school age, by 10 years–12 years of age. Cerebral white matter volume increases through school age until mid-to-late adolescence, peaking by 18 years–20 years. 35 , 36 Total brain size is about 9% greater in males than females, and the difference persists, even if controlling for height and weight. These differences should not be understood as conferring advantage or disadvantage, as they do not represent neuronal or synaptic connectivity or other components of brain architecture and function (see Figure 3 ). 37 , 38
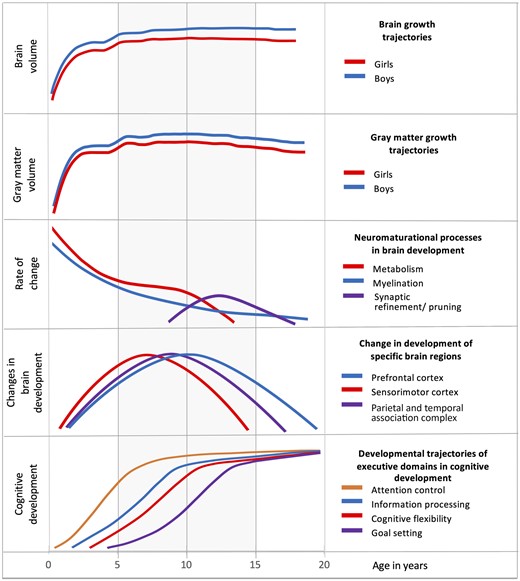
Neuromaturational and cognitive development trajectories in school-age years (gray-shaded area) . Compiled and adapted from Peterson et al 2021 38 (brain and gray matter growth), Tapert and Schweinsburg 2005 114 (neuromaturation process rate), Lee et al 2014 115 (brain region development), and Anderson 2002 46 (cognitive development executive domains)
During the school years, though at a slower rate than during the preschool years, total brain size increases, as does the sex-driven divergence, with boys being faster and peaking by 14.5 years, and girls peaking earlier by 11.5 years. 37 During this period, brain development is also marked by a significant increase in 2 major neuro-maturational processes: continued myelination and an increase in synaptic refinement and pruning, both of which are important for the efficiency of neuronal networks. Dendritic synaptic pruning eliminates unused or weak connections, and a reduction in myelination rates improves connectivity. This fine-tuning within and between brain regions strengthens a number of particular pathways, which increases brain efficiency, critical to the development of cognitive abilities. 39 , 40
School age will be marked by the highest rate of development of specific areas of the brain, particularly the posterior sensorimotor cortex, temporal association complex, and prefrontal cortex, and this development peaks at between 5 years and 15 years of age, in the middle of school age. All these areas are “associative cortices,” which process input from the sensory cortices and ultimately generate behaviors (see Figure 3 ). These structures are the key determinants of higher-order functions, particularly cognitive development (including language, mathematics, and executive function [EF]) and socio-emotional regulation, which among other things, allows for organization of information to serve goal-directed behaviors, decision-making, peer affiliation, and social behaviors. 41 , 42 The parietal and temporal association cortex, responsible for language skills, also develops at a fast rate and this development peaks during school age. For example, language acquisition and proficiency, especially the ability to master a second language as a native speaker, decreases at the end of school age, by 15 years of age. 43
The development of the prefrontal cortex peaks in the middle of the school years and continues to mature into the third decade. The gray matter volume in the frontal cortex peaks at 11 years of age in girls and at just after 12 years in boys. 44 This part of the brain supports higher-level integration and processing, allowing for abstract thinking, problem-solving, understanding others’ thoughts and intentions, and the relating of thoughts temporally, allowing for goal setting. Thus, the prefrontal cortex is generally regarded as the “seat” of EF. EF is a broad term that incorporates a collection of mental processes that (a) enable individuals to hold and recall relevant information (working memory), (b) focus their attention, inhibiting automatic responses to stimuli (inhibitory control), and (c) shift the focus of attention to the managing of problems or multiple-aspect tasks successfully (cognitive flexibility), to yield purposeful, goal-directed behaviors. Ultimately, these processes influence behavior, emotional control, and social interaction. EF is associated with academic performance as well as intelligence quotient (IQ). 42 , 45 , 46
One well-recognized model of EF conceptualizes and maps chronologically 4 distinct and interrelated developmental domains, each of which gathers and processes stimuli from multiple sources: attention control, information processing, cognitive flexibility, and goal setting. Attentional control matures relatively early, by the end of preschool age; information processing and cognitive flexibility are mostly developed by the end of middle childhood; and goal setting is well developed before the end of early adolescence (see Figure 3 ). 46
In addition, the increased synaptic pruning and myelination that occurs during this period significantly reshapes and modifies circuitry and allows malleability and adaptation to environmental experiences, or brain plasticity. There is evidence, eg, that both synaptic pruning and myelination are driven or modified by an individual’s experiences. 47 Thus, behaviors toward the environment are shaped by biologic changes in the brain, which in turn may be shaped by environmental, social, and cultural learning experiences. School age marks a major development of the associative brain regions and the resulting cognitive development and EFs, as well as the maturation of reward and emotional sensitivity areas, which interact with higher function control areas to develop emotional regulation, identity development, and longer-term planning and purpose. Adequate provision of nutrition, healthy social interactions, and cultural experiences, as well as adequate sleep, are all key to physical and psychosocial well-being. 41
The onset of early adolescence will be marked by an increase in social and cultural interactions, and changes in the home, community, and school relationships, which influence behavior. The interaction between behavior resulting from brain functions and external influences appears to be bidirectional. At the onset of puberty, the prefrontal associative brain areas continue to develop, but at a slower pace than some subcortical brain areas. These limbic emotion- and reward-related regions, such as the amygdala, appear to mature earlier than the prefrontal areas, which are responsible for inhibitory control of impulses and regulation of gratification and other emotions. This “mismatch” may in part explain the increase in risk-taking, emotion-driven behaviors seen in adolescence. 48
In summary, between the age of 5 years and 15 years, children go through major accelerations and inflections in their somatic growth, from a prepubertal state in the first 5 years to early adolescence changes in the next 5 years. By the end of school age, and before entering the final stages of “late adolescence,” healthy boys and girls, respectively, will have attained approximately 96% and 95% of their adult height, 19 92% and 77% of their total BMC, 49 89% and 85% of their fat mass, 21 and 84% and 95% of their muscle mass. 22 During this period, neuro-maturational processes will have also undergone significant changes. These include peaks in the development of specific areas of the brain and particularly the prefrontal cortex (implicated in complex cognitive behavior, planning, personality expression, decision-making, and moderation of social behavior) in the middle of the school years. Processes like synaptic pruning, which increase brain efficiency, will also peak by the end of this period, allowing for plasticity and increased brain efficiency. Delaying, altering, or blunting these accelerations and inflection points can significantly affect the ultimate attainment of physical growth, and cognitive, and socioemotional/psychosocial development. The necessity of preparing the child for these changes and supporting them through these accelerations and inflections, leading to the final maturational phase of late adolescence and ultimately adulthood, cannot be overstated.
The number of changes and dynamics of development mentioned above make the school years a particularly sensitive time, especially since most of the final growth and development is attained, which if not achieved will limit physical, cognitive, and social potential. These changes happen against a genetic backdrop expressed in, and dependent upon, multiple environmental and social scenarios that modulate physical and psychosocial development.
All these changes are underpinned by adequate nutrition in this period, as is true for all life cycle phases. Inadequate nutrition will slow or blunt physical and neurocognitive development trajectories during this last period of growth and development, with long-term consequences, inhibiting an individual’s ultimate potential. If environmental conditions, particularly nutrition, are favorable, the growth course and final height and overall body shape will be determined by an individual’s genes. 27 The acceleration and change in growth trajectories discussed above increase the chances for curtailing growth and development if increased nutritional demands are not met. Because of the growth dynamics in this period, the school years become critical for the necessary nutrition (a) to maintain adequate growth trajectories until maturity, or (b) to correct inadequacies and imbalances (deficits and excesses) for a healthy transition to a productive adulthood.
WHO, the US Institute of Medicine, the European Food Safety Authority (EFSA), and other regional authoritative groups all distinguish and define specific energy, macro-, and micro-nutrient requirements for the school-age years (early childhood and early adolescence) distinct from those of other life stages.
Energy and protein
As the child grows, changes in metabolism are directly related to total energy requirements and indirectly to growth, and consist of basal metabolic rate, energy cost of growth, and activity energy expenditure. 50 As a fraction of the total energy requirements, the energy cost of growth is highest in the newborn period, decreases to about 3% at 1 year of age, and goes up again between middle childhood and early adolescence to about 4%. 51 Imbalances between energy intake and expenditure can result in deficits (leading to a decrease in body fat and a deceleration of growth) or excesses (in the form of fat accumulation, increased body weight, and its related consequences).
The factors that affect child energy requirements are growth and body composition (which are sex-dependent), as well as physical activity. Daily energy requirements diverge by sex at the start of school age, and will remain different throughout the life cycle. Sex differences in metabolic rate and energy expenditure are in part driven by differences in body fat and fat-free mass that emerge during school age.
Between 5 years and 15 years of age, physical activity is a particularly important factor in energy balance. In adults, the estimated difference in energy requirements between a sedentary individual and an active individual is below 20%, while in 5-year-olds to 15-year-olds it is around 35%, indicating the need for adequate energy provision—in proportion to the recommended “active” level of physical activity during this period of the life cycle. 51 Energy provision throughout the day is also critical for brain activity, where increased neuronal activity drives increased energy consumption. In addition to all the neurodevelopmental changes occurring during school age mentioned above, the cerebral metabolic rate of glucose utilization is at its highest in middle childhood and early adolescence (apart from during the newborn period), then drops towards the end of adolescence. The mature brain is only approximately 2% of the body weight in adulthood, but is responsible for around 20% of energy consumption. Estimations for 12-year-old children suggest that brain energy consumption is as high as 30%. 52–54 Lastly, this increase in energy requirement and utilization is also dependent on the presence of adequate quantities of several micronutrients. These include riboflavin (vitamin B2), niacin (nicotinamide; vitamin B3), pyridoxine (vitamin B6), cobalamin (vitamin B12), vitamin C, vitamin D, calcium, iron, and phosphorus. They all act as co-factors for key enzymes in the metabolic pathways that generate and use energy.
Protein is the major functional and structural component of every cell in the body. The quality of a source of dietary protein depends on its ability to provide the nitrogen and amino acid requirements necessary for the body’s growth, maintenance, and repair. Through to the end of the growth years, enough protein is required to maintain the nitrogen equilibrium plus protein deposition in tissues. Low consumption of protein, often associated with low protein quality, is strongly associated with stunting, and if marked, other signs of undernutrition. As opposed to requirements for energy and some micronutrients, protein requirements do not change significantly by age or sex during the school years. The United States recommended dietary allowance is 0.95 g/kg/day, representing 10%–30% of total calories, from 4 years to 13 years of age. The recommended dietary allowance decreases slightly after adolescence. In general, proteins from animal sources such as meat, poultry, fish, eggs, milk, cheese, and yogurt provide all indispensable amino acids and are referred to as “complete proteins.” Proteins from plants, legumes, grains, nuts, seeds, and vegetables tend to be deficient in one or more of the indispensable amino acids.Thus, attention needs to be paid to children whose diets are low in animal protein sources to avoid essential amino acid deficiencies. 51
Micronutrients
In the United States, the Estimated Adequate Requirements, and Dietary Reference Intakes for micronutrients are the same for all children up to age 8 years. For the first time, they diverge for boys and girls during the school years: there are small differences (eg, for iron) for 9 years–13 years, and larger differences in requirements for late adolescence, at 14 years–18 years. 51 EFSA has slightly different and more specific age cut-offs for Population Reference Intakes (PRIs) for most vitamins and minerals. 55 Recommendations are made for 4 years–6 years, 7 years–10 years, 11 years–14 years of age, and separately define PRIs for 4 years–10 years and 11 years–17 years for calcium, 1 year–6 years, 7 years–11 years, and 12 years–17 years for iron, and 3 years–9 years and 10 years–17 years for copper, with some differences for sex in these nutrients. EFSA also differentiates requirements in energy and protein for boys and girls starting at 4 years. While specific benefits have been well established in relation to deficiencies for many micronutrients, consensus on optimal doses and combinations of these nutrients for promotion of specific health benefits in otherwise healthy school-age children is not universal and would benefit from further clinical research and substantiation.
Linear growth appears particularly sensitive to restrictions in energy, protein (particularly essential amino acids), zinc, iodine, and phosphorus, as well as some electrolytes. Protein quantity and quality remain fundamental components of adequate growth and function at all ages. Yet, the minimum protein necessary for adequate linear growth remains to be ascertained. Animal proteins, including dairy protein sources, have a selective effect in promoting height gain in undernourished and well-nourished children. In populations with low consumption of foods from animal sources, protein and zinc deficiencies will be more common. While iron and vitamin A are essential for multiple other reasons, intervention studies suggest that their deficiency does not affect linear growth. As discussed further below, calcium is critical for bone mineralization but appears to be of less consequence regarding linear growth. 27
Independent of nutrient provision, as mentioned above, bone growth regulation can be blocked by inflammation, such as recurrent childhood infections, which, if bi-directionally compounded by undernutrition, result in poor growth led to stunting. The term “environmental enteric dysfunction” has been used to refer to chronic and recurrent infections and infestations in areas with poor sanitation, where infection, inflammation, and malabsorption coalesce and perpetuate undernutrition. These conditions may explain why nutrition or dietary interventions alone may not be sufficient to address stunting in children. Current interventions to reduce stunting need to target sanitation and environmental factors as well as nutrition in low- and middle-income country settings. 25 , 27
Calcium is essential for adequate mineralization of bones, and 99% of all calcium in humans is found in bones and teeth. Dietary calcium can be absorbed passively, but the active transport of calcium in the gut is mediated by vitamin D. Both nutrients are inextricably linked in determining BMC. Low calcium intake in young children is associated with low BMC, and sustained low intakes (below 200 mg daily) with radiographic signs of rickets. 56
There is clear evidence suggesting that peak bone mass and risk of fractures in later life are influenced by bone mineral accretion throughout childhood, including school age. As discussed above, peak rates of bone mineralization are reached 6 months–12 months after the peak rate of bone elongation is reached. By the end of school age, median peak height has been achieved in girls (achieved a year later in boys), and more than 80% BMC has been accrued. The exact cessation of mineral accrual varies depending on the skeletal site, but appears to be complete by 18 years in the spine and femoral neck. After peak BMC is reached, the rate of bone mass and mineral content accretion gradually and continually decreases for the rest of an individual’s life. 33 , 57 Therefore, the rate and amount of BMC attained in the school years will greatly determine peak bone mass and be a major contributor to the relative risk of low bone mass and eventual osteoporosis and bone fractures for the rest of an individual’s life. Recent estimates from the United States in adults older than 50 years show a prevalence of low bone mass of 51.5% in women and 33.5% in men, and frank osteoporosis of 19.6% in women and 4.4% in men. 58 Estimates from the International Osteoporosis Foundation indicate that, worldwide, after 50 years of age, 30% of women and 20% of men will have hip, vertebral, or wrist fractures from osteoporosis in the remainder of their lives. 59 Thus, meeting dietary protein and calcium requirements, maintaining adequate vitamin D through diet and sunlight exposure, and physical activity during school-age years constitute critical investments in achieving long-term bone health. 31 , 60
Iron, zinc, polyunsaturated fatty acids (especially docosahexaenoic acid), vitamin B12, and folate have all been specifically identified as critical nutrients for adequate brain growth, cognition, and EF development. However, as for other aspects of life-stage nutrition, most data have been accumulated for these nutrients and their longer-term effects in relation to consumption in the first 5 years of life. They have often not been the primary focus of studies and are poorly investigated in healthy school-age populations. 61
Deficiency in iron deserves highlighting in relation to nutritional consequences for later life, due to its prevalence in and coexistence with all forms of malnutrition. Iron deficiency is the most common nutritional deficit in people worldwide and the most common deficiency in children, whether suffering or not from acute or chronic malnutrition. Anemia, half of which is due to iron deficiency, affects around 33% of the global population. Globally in 2019, iron deficiency was the leading cause of years lived with disability in children and young adults (aged 10 y–24 y), with the highest prevalence in most African and many Asian countries. 62 While its prevalence is higher in low- and middle-income countries, it persists in varying degrees in all socio-economic levels. Iron is a crucial nutrient in maintaining levels of neurotransmitters, including dopamine and serotonin. And its deficiency can decrease brain myelination, alter synaptogenesis, and decrease the functioning of basal ganglia. The consequences in childhood include deficits in motor function and impaired cognitive development, leading to lower cognitive skills, lower school achievement, impaired psychomotor and behavioral development, and ultimately lower work capacity and productivity in adulthood. 63 , 64
The consequences of iron deficiency in childhood, some of which may be irreversible, have been recognized for a long time and have led to global efforts in improving iron status through supplementation in infancy and childhood. 64 , 65 Given the significant changes in brain structure and function that happen during the school years, and the potential long-term consequences of deficiency, iron remains a major nutrient of interest, highlighting the need for adequate preventive interventions as well as treatment of deficiencies during this life stage. There is increasing and robust evidence that improving iron status, particularly in the presence of anemia, significantly affects cognitive performance in school-age children older than 5 years. Interestingly, the evidence for this effect of iron on older children appears stronger than for interventions in children under 2 years of age. 66
Consequences of inadequate nutrition in school age on growth and development
Inadequate nutrition in school age ultimately results from inadequate diets, which in turn are a consequence of multiple factors. On the one hand, food security, availability, and provision are essential. On the other, a healthy diet requires appropriate food choices, which depend on many environmental influences—from home, the community, the school, and broader society. These influences will not only determine the delivery of adequate foods but shape the behavior of children and thus their food choices for the long term. Influences at this age are critical, when cognitive, socioemotional, and psychosocial development are associated with increasing independence, decision-making, and self-image and awareness. Addressing all these factors remains critical for increasing an individual’s chances for long-term health. Discussion of these is beyond the scope of this review.
The immediate and most visible consequences of not meeting nutritional requirements are loss of body weight and adipose tissue (thinness/wasting/low BMI). Prolonged marginal provision of macronutrients, most often accompanied by micronutrient deficits, leads to slowing of linear growth (low height for age). In both cases, infection, or other inflammatory states, coupled with enteropathies related to poor sanitation, can further increase requirement for an effective immune response, lead to a negative nitrogen balance, mobilization of protein from muscle tissues, as well as inhibition of linear bone growth. 25 , 28 Wasting and stunting are often linked and can occur together in the same population, often in the same child. 67 Longitudinal analyses show that wasting is a precursor to stunting. 68 In addition, low BMI and wasting are related to delayed pubertal onset, which in school-age children affects growth trajectories. Globally, stunting (height-for-age greater than 2 standard deviations below the WHO reference) remains by far the most prevalent clinical manifestation of undernutrition, including micronutrient deficiencies. 28
Stunting in early life is associated with poor cognitive development, lower development of EF, lower rates of schooling and school achievement, and ultimately decreased productivity and earning power. These associations, however, do not necessarily infer causality. Stunting is often accompanied by multiple nutrient deficiencies and their consequences, beyond iron deficiency anemia. And the occurrence of stunting due to poor nutrition, and its cognitive and other consequences, cannot be delinked from the effects of the physical and social environments where stunting occurs 69–71 ; nonetheless, it is likely they are causally related. Beyond cognitive impact, not achieving an individual’s height potential can also be associated with higher psychologic dysfunction all the way to late adolescence, with increased chances of developing low self-esteem, anxiety, depressive symptoms, and anti-social behaviors. 72 , 73
Stunting can occur at any age before adulthood, but for most school-age children, it is a continuation of poor growth in early infancy. WHO and World Bank global estimates show that globally, stunting in children under 5 years of age has decreased from 33% (203.6 million children) to 22% (149.2 million children) from 2000 to 2020, 7 with the highest prevalence in Africa and parts of Asia and Latin America. Thus, a great number of children are stunted when entering school age. Stunting prevalence in school age will result from stunting occurring under 5 years, with some “new” cases being added or a decrease in cases from “catch-up” growth. 74 Although most stunting may start in infancy, it can continue or worsen in the school years. As discussed below, given school age is the last and second fastest period of height attainment after infancy, this life stage may offer the last “window of opportunity” for correcting deficits and potentially achieving catch-up growth and catch-up cognitive development, ameliorating its negative consequences for individuals and society.
Lastly, children who remain stunted through school years may be at increased risk for obesity. There is growing evidence that stunted infants and children who gain weight rapidly in later childhood have an increased risk of overweight, obesity, and noncommunicable diseases as adults. 75 , 76 However, stunting at 1 year alone does not seem to raise obesity risk consistently. 77 This is becoming increasingly important, as the secular transition from undernutrition to obesity is accelerating in many populations, as discussed below. The peak incidence of obesity by age has been occurring earlier and earlier in life in many populations (see below). Its consequences (related to metabolic disease, diabetes, cardiovascular disease, and other noncommunicable conditions) constitute the greatest health challenges of this century.
Specific nutrient deficiencies, individually or in combination, and their syndromes are both present and prevalent in school age. The consequences of these in addition to those mentioned above are beyond this review. Suffice it to say that persistent deficiencies such as of iron (and its effects on long-term cognitive function) as well as calcium and vitamin D (and their potential in preventing osteoporosis and fractures well into adult and mature life) are prime examples of the need for maintaining adequacy or correcting deficiencies during school age.
Compared with infant data, apart from some recent increase in data on the adolescent years, there is a serious lack of information on nutritional status and its consequences for middle childhood through adolescence. One analysis showed that, a literature search for 2004–2017 including the terms “health,” “mortality,” or “cause of death in the first 20 years of life” found that about 99% of the publications in Google Scholar and 95% of the publications in PubMed focused on children under age 5 years. 8 Global School-based Student Surveys, a collaboration of WHO, CDC, UNICEF, UNESCO, and UNAIDS, have primarily included only 13-year-olds to 17-year-olds. 78 In addition, data for this age group is often embedded and difficult to disaggregate from “childhood studies” that may include preschool and school-age children, or from studies on “adolescents” that include children of 10 years or 12 years and above. Overall, the ages 5 years–9 years and 10 years–14 years have the least number of research data sources for estimating morbidity and mortality risk factors compared with 0 years–5 years and 15 years–19 years. Another recent large population-based study showed that, within the relatively small amount of available data for height, weight, and BMI in school-age children, 78.9% of studies had data for 15 years–19 years, but only 50.3% had data for 10 years–14 years, and 39.9% for 5 years–9 years of age. 79 In another larger analysis, less than half of the studies included data for middle childhood (5 y–9 y), compared with nearly 90% with data for adolescents (10 y–19 y). Overall, the quantity and quality of data vary significantly by country and region. Still, the relative lack of data for middle childhood is notable across the board, limiting the capacity to compare growth or nutrition outcomes of this age group with earlier or later life stages. 80
A systematic review, one of the few studies focusing on school age (6 y–12 y) in low- and middle-income countries (LMICs), showed underweight and thinness were most prevalent (21%–36%) in South-East Asian and African countries, with lower prevalence in Latin America (8%–6%). The prevalence of overweight and obesity was highest in Latin America (∼26%), compared with 13% in Southeast Asia and 7% in Africa. The mean prevalence of iron deficiency ranged from 29% in Africa to 20% in Southeast Asia, and 14% in Latin America. Iodine, vitamin A, and zinc deficiencies are the most common. The prevalence of vitamin A deficiency was 9% in Latin America (on the lower end), to 54% zinc deficiency prevalence in Africa (on the highest end). 81
Very recently, data from population-based studies supported by the Non-Communicable Disease Risk Factor Collaboration 79 , 80 and the B&M Gates Foundation 82 are shedding light on this global picture. These are the most comprehensive reviews on growth and temporal trends available to date for this age group, and the only available review addressing this age group at a global level. One analysis, NCD RisC 2017, 79 included 31.5 million children from 200 countries aged 5 years–19 years, and estimated trends from 1975 to 2016. The other, NCD RisC 2020, 80 pooled data from 2181 population-based studies, with height and weight measurements for 65 million participants in 200 countries, and estimated trends from 1985 to 2019 in height and BMI for children 5 years–19 years. In this study, data were reported without specific cut-off points for over- or under-nutrition. Data and trends from these studies are summarized immediately below.
Thinness and wasting
From 1975 to 2016, the overall global prevalence of moderate and severe underweight (thinness and wasting) in children 5 years–19 years decreased from 9.2% to 8.4% in girls and from 14.8% to 12.4% in boys, with the expected large variations regionally. The prevalence of moderate and severe underweight remained highest in south Asia, with 22.7% among girls and 30.7% among boys in India. Although the populations increased in most regions, the number of moderately and severely underweight school-age children actually decreased. And while prevalence declined, the relatively small change at the global level was partly due to greater population growth in countries where the prevalence of underweight is higher. 79
Mean BMI trends showed increases in almost every country over the last 30 years, with the greatest increases seen in Sub-Saharan Africa. Low BMI (compared with the WHO reference median in 5-year-old children) persisted primarily in Southeast Asia and Sub-Saharan Africa. In most countries, it decreased as they entered adolescence, and in some countries it disappeared by age 19 years. 80 The trends showed that, globally, the absolute number of underweight children peaked around the year 2000 and has since been decreasing, reaching levels in 2016 close to those in 1975. 79
Data from surveys in 57 LMICs between 2003 and 2013, comprising children 12 years–15 years, showed a global prevalence of stunting of 10%. 75 However, the limited data available on stunting in this age group shows very wide variations. Stunting in adolescent girls (15 y–19 y) in LMICs range from 52% in Guatemala and 44% in Bangladesh to 6% in Brazil. 83
The 2 most extensive global studies including children 5 years–19 years of age 79 , 80 did not report height based on a particular cut-off for stunting. Nevertheless, in age-related trends, most countries showed that height was at or above the WHO median for children at 5 years of age, with girls doing better than boys. Still, in approximately 20% of countries for girls and 30% of countries for boys, the mean height during the school years was significantly below the WHO median. Today, the estimated difference in height of 19-year-olds between countries with the tallest populations (eg, the Netherlands, Denmark) and the shortest populations (eg, Timor-Leste, Laos, Guatemala, Bangladesh) was 20 cm. More concerning is that, in some countries, height adequacy in middle childhood may decrease as children grow older. Children who have optimal height at 5 years of age fall under the WHO median at 19 years by 2 cm or more, particularly in some middle-income countries.
In terms of temporal trends, with rare exceptions, the last 3 decades show significant gains in height in most countries and all regions for boys and girls, except for Sub-Saharan Africa (for both sexes) and Oceania (for boys). The greatest gains have been made in countries with emerging economies, including China and South Korea, and parts of Southeast Asia, the Middle East, and in some countries in North Africa, Latin America, and the Caribbean. 80
Overnutrition
Over the last 40 years, obesity has increased in every country in the world. The NCD-RisC 2017 study 79 showed that, from 1975 to 2016, the global prevalence of obesity in 5-year-olds to 29-year-olds increased from 0.7% to 5.6% in girls, and from 0.9% in 1975 to 7.8% in boys. The number of girls with obesity increased from about 5 million to 50 million in 2016, and the number of boys from about 6 million to 74 million. Trends in mean BMI have continued accelerating, particularly in east and south Asia. Southern African countries had the greatest rise in obesity (∼400% per decade), given the obesity prevalence was minimal 40 years ago.
On the other hand, since about 2000, the increase in prevalence has begun to plateau, and it recently flattened in northwestern Europe, in “high-income English-speaking” and Asia-Pacific regions for both sexes, in southwestern Europe for boys, and in central and Andean Latin America for girls. While not exactly comparable, these findings are consistent with another earlier large study 82 that analyzed 1769 population-based surveys and studies in 19 244 children aged 2 years–19 years (not reporting disaggregated data for school age). These investigators found that, from 1980 to 2013, in developed countries, the prevalence of overweight and obesity for 2-year-old to 19-year-old children (as a group) increased from 16.9% to 23.8% in boys and 16.2% to 22.6% in girls. In the same period, in developing countries, the prevalence of overweight and obesity increased from 8.1% to 12.9% in boys and 8.4% to 13.4% in girls. All studies show that globally, the peak prevalence of obesity is shifting to younger ages. While the prevalence remains higher in developed countries, the great majority of overweight and obese girls and boys (in absolute numbers) are from LIMCs, 79 thus representing a double burden of poor nutrition for the most populous countries in the world.
The NCD RisC 2020 study 80 showed that the difference between the highest mean BMI (eg, Pacific Island countries, the United States, Chile, South Africa) and lowest mean BMI (eg, India, Bangladesh, Ethiopia, and Chad) was 9 kg/m 2 –10 kg/m 2 in girls. Thus, the mean BMI difference, between these countries, was greater than 2 standard deviations in BMI for a 15-year-old girl. Trends by age varied significantly, and they worsened with age in many countries. In some countries (eg, Mexico, South Africa, New Zealand), 5-year-old children with healthy BMI progressively gained more in BMI than in height through the school-age years. Over time, some countries showed too little height gain, and/or too much weight gain for height (eg, Sub-Saharan Africa, New Zealand, the United States, Malaysia, some Pacific Island nations, and Mexico), with some differences by sex.
In summary, though the landscape has changed significantly in the last few decades, undernutrition (wasting/thinness/low BMI) and poor linear growth (low height for age/stunting), as well as overnutrition (elevated BMI with or without low height), remain major nutritional challenges globally. Today, still, despite the increase in overweight and obesity, more school-age children worldwide are moderately or severely underweight than overweight or obese. That said, in most countries, the prevalence increases in overweight and obesity are greater than the declines in prevalence of underweight. So, if current trends continue globally, the prevalence of obesity in school age will be higher than that of moderate and severe underweight before 2025. 80
The considerable global differences in these markers of nutritional adequacy reflect the geographic and socio-economic gaps that also persist globally. While genetics and other factors play a role, a difference of 20 cm in height and 9 kg/m 2 –10 kg/m 2 in BMI between extremes in populations is a partial reflection of the persistence of undernutrition and the large global nutritional and environmental gaps. Lastly, a rapid closing of those gaps may signal a “too rapid” transition from a mostly underweight population to a mostly overweight and obese population, as has occurred in parts of Asia and Latin America, accelerating and increasing the burden of nutrition-related conditions, particularly for LMIC populations.
While trajectories vary regionally, in many countries, based on height and BMI, nutritional status appears to be adequate at 5 years (which may reflect efforts over the last decades in improving early childhood health and nutrition) but deteriorates as children move through the school years. This heightens the relative neglect in attention to school-age nutritional focus, particularly for the 5–10 year-old population.
The global rise in obesity related to socio-economic and other environmental changes, including changes in nutrition, contributes to increases and exacerbations of type 2 diabetes, cardiovascular disease, and other noncommunicable diseases, exacerbating the double burden of disease and of cost to society. Prevention, starting prenatally, remains the most cost-effective and realistic approach. 84 So far, however, no clear or strong regional or national success stories have been demonstrated in the last decades. 82
Micronutrient deficiencies
Micronutrient deficiencies continue to be considered a major contributor to the global burden of disease. Despite this, a recent global report confirms a persistent and wide gap in data and information around micronutrient intake and nutrient status for all ages. 85 Individual deficiencies rarely occur in isolation. As for other indicators of nutrition and health, some school-age micronutrient data is available for some nutrients, and some are available from studies in adolescents and young adults. Still, data in 5-year-old to 15-year-old children is the least available across the board.
Based on the high prevalence of their deficiencies, WHO considers iron, vitamin A, vitamin D, zinc, iodine, and folate the most critical micronutrients globally. It is estimated that 25% of school-age children (around 305 million children) have anemia and that 50% of it is primarily associated with iron deficiency. 86 A 2004 report estimated the prevalence of vitamin A deficiency in school-age children in South Asia to be 23.4% or 83 million children, 9 million of whom had xerophthalmia. 87 In low-income countries, vitamin A deficiency prevalence has been estimated at 20% among early adolescent (10–14-year-old) girls and 18% among late adolescent (15–19-year-old) girls. 83 Worldwide, inadequate zinc intake is estimated at around 17%, with little data disaggregated for school children, 88 90% of which is in Africa and Asia. 89 The prevalence of inadequate iodine intake in 6-year-old to 12-year-old school-age children has been estimated at around 30% (241 million children), ranging from 13% in the Americas to 39% in Africa. 90 Limited data on folate deficiency in females 12 years–49 years (reproductive age) indicate a prevalence of more than 20% in lower-income and less than 5% in higher-income countries. There are no good global estimates of folate deficiency for school-age children. 88 , 91
In one report, vitamin D deficiency in 6-year-old to 12-year-old children ranged from 16% in North America, to 28% in Mexico, to 88% in China. 92 For calcium, as opposed to most other nutrients where adequacy can be measured using biomarkers, there is no universally accepted definition for deficiency. So dietary intake is used as the best proxy for adequacy. In addition, recommended intakes vary significantly by regional or expert groups. For school-age children, EFSA has stated a PRI of 800 mg/day for 4-year-olds to 10-year-olds and 1150 mg/day for 11-year-olds to 17 year-olds. The Institute of Medicine in the United States has stated a recommended dietary allowance of 1000 mg/day for 4-year-olds to 8-year-olds and 1300 mg for 9-year-olds to 13-year-olds. 55 While good estimates are lacking, average calcium intake in the United States for children 1 year to 14 years has been estimated at between 856 mg/day and 993 mg/day, depending on methodology, suggesting that many children fall below recommendations. There are no good global estimations, but from the little data available, it is evident that the great majority of children in developing countries fall far below any current recommendations. 93 Micronutrient deficiencies further compound the total burden of poor nutrition, as they coexist with wasting and obesity.
Studies and systematic reviews of micronutrient supplementation and fortification that include school-age children clearly show that micronutrient status can be improved. The demonstration of clinical effects, including growth and morbidity, varies significantly. The best documented is iron supplementation and fortification, which has been shown to improve iron status and reduce anemia in school-age children 5 years–12 years old. 94 A positive effect of iron supplementation on cognitive development has been shown, and interestingly, effectiveness appears greater for children older than 7 years than for younger ages. 95 Other effects of micronutrient supplementation, including growth and morbidity, are less clear. 81 , 96
Early attention to the significant effect of nutrition until 2 years of age and the assertions, even until recently, that stunting and cognitive delays were irreversible 97 , 98 may have contributed to the lower attention to middle childhood and adolescence as opportunities for recovery, particularly as related to stunting and cognitive deficits. Evidence today suggests this is not the case.
Catch-up growth through the school-age years is possible with the right interventions. Historical reports and observational studies of immigrant populations and adopted children document that in situations where environmental and nutritional conditions change positively, meaningful linear catch-up is possible. 99 Longitudinal observational data from the COHORT multicounty study and longitudinal data from rural Gambia have shown that significant catch-up in height can be achieved between 2 years of age and the end of middle childhood (10 y of age), and between middle childhood and adulthood, even in the absence of any nutrition or health interventions. 2 Catch-up growth is also possible in chronic conditions, including celiac disease and inflammatory bowel disease, with the right medical and nutritional interventions. 100 , 101
Although results are not always consistent, some longitudinal studies that include school-age populations (6 y–11 y old) show linear catch-up is possible with multiple micronutrient supplementation. 102 , 103 A recent systematic review and meta-analysis of the effectiveness of several nutrition-based interventions after 2 years of age (where more than half of the studies included children older than 5 years of age) showed including supplementation of protein, vitamin A, and/or multiple micronutrients, and particularly zinc supplementation, can improve linear growth, especially in children that have experienced early stunting. However, supplementation of other micronutrients, including iodine, iron, calcium, or food-based interventions, did not significantly affect growth, even if resolving anemia or other deficiencies. 96
Although populations and methodologies vary, some studies have not found a correlation between linear growth recovery and cognitive measures in short-term studies over 6 months, 104 while others have. Data from a longitudinal observational cohort in several LMICs found that children who had stunting by 1 year of age with linear growth catch-up by age 8 years had significantly better cognitive outcomes than those who remained stunted. 105 Height catch-up in these children was positively associated with improvements in mathematics achievement, reading comprehension, and receptive vocabulary. Children who remained stunted performed less well, and children who were never stunted remained ahead of the other groups. A subsequent study of the same cohort 74 analyzed catch-up growth between the ages of 8 years and 15 years and showed that more than one third of those stunted at age 8 years caught up to their peers by age 15 years, and also improved their cognitive scores compared with those who did not catch up in height. Notably, linear growth faltering was also accompanied by a decrease in cognitive outcomes in those children who became stunted between 8 years and 15 years. Thus, associations between linear growth and cognitive development vary from country to country and do not always persist from middle childhood through adolescence. 74 , 106 The extent of linear catch-up effect in various studies will vary obviously due to the timing of the initial insult, the timing of the intervention, the duration of the intervention, and other environmental conditions beyond nutrition. Given the obvious genetic, epigenetic, and environmental carryover between young mothers and their offspring, it seems likely also that reversing the cycle of undernutrition will probably require cross-generational catch-up. 107
Inadequate bone mass and mineral accretion in school-age children can have long-term consequences. While no good markers (except assessment of calcium intake and vitamin D) are available, adequate intakes remain important for reducing long-term risks. During the school-age years, a higher milk intake is associated with higher BMC, BMD, and reduced fracture risk in adulthood. Consuming less than one serving of milk a day in childhood was associated with a 2-fold increase in fracture risk as adults. 108 Establishing healthy dietary behaviors with a well-balanced diet that includes adequate calcium and vitamin D, particularly with inclusion of dairy products and regular physical activity, can bring about long-term bone health.
Despite the limited knowledge we have, the nutritional objectives for school-age children appear quite clear: providing energy and protein adequacy (including avoiding excesses), decreasing deficiencies of iron, iodine, vitamin A, vitamin D, calcium, zinc, and folate, and avoiding excesses of simple sugars and sodium. Long-term studies are still lacking, and there appears to be no “magic bullet” for improving dietary intakes and avoiding excesses. However, there is increasing evidence to support school dietary and physical activity–based interventions in schoolchildren to prevent deficiencies and address overweight and obesity. 109–111 The school setting has excellent potential for providing a significant part of daily intake to improve diet quality tailored to the local environment and educate children in nutrition and diet. The potential remains to be tapped.
This can only be accomplished with adequate individual, community, and population education, as well as policies that support these endeavours at multiple levels and by multiple stakeholders—a discussion that is beyond the scope of this review.
Very recently, the last 4 years to 5 years have brought about an increasing level of attention and calls for action to address the health and nutrition of middle childhood and adolescence. In 2017, Bundy et al published a comprehensive volume as part of the World Bank’s Disease Control Priorities series, with support from the Bill and Melinda Gates Foundation, highlighting child and adolescent health, with a focus on ages 5 years–19 years, as “neglected potential” that needs to be realized. 1 They noted an “asymmetry between the public investment in formal education versus health during the age range of 5 years–19 years, and a lack of recognition that the developmental returns from education are themselves dependent on concurrent good health and diet.” This “historical neglect of investments… [beyond the first 1000 d], including the next 7000 days of middle childhood and adolescence… is also reflected in investment in research into the older age-groups.” 1
Around this time, collaborative efforts in population-based studies are finally presenting a more comprehensive and clearer global picture of the nutritional status of children above 5 years of age. 79 , 80 Several research groups have reported on the significant potential that nutrition and health interventions have on improving outcomes during school age, thus constituting a true (and possibly last) major window of opportunity for supporting adequate nutrition, overcoming deficits from earlier life, shaping future dietary behaviors, and improving long-term health and well-being. 2–5
Even more recently, UNICEF’s Nutrition Strategy for 2020–2030 Framework called for “strategic shifts” in upholding children’s right to nutrition and ending child malnutrition in all its forms (as part of the global Sustainable Development Goals). The Strategy includes a comprehensive life cycle approach to nutrition programming, and maternal and child nutrition during the first 1000 days as core to UNICEF programs, and also explicitly states that “nutrition during middle childhood and adolescence is both a right and a window of opportunity for growth, development and learning, particularly for girls, and for breaking the intergenerational cycle of malnutrition.” The 2 first measurable Results areas for the Strategy are 1. Early Childhood Nutrition and 2. Nutrition in Middle Childhood and Adolescence. 112 UNICEF’s Programmatic Guidance for Nutrition in Middle Childhood and Adolescence includes specific priorities of nutritious foods, healthy food environments in schools and beyond, micronutrient supplementation and deworming, nutrition education in school curricula, and healthy dietary practices for school-age children and adolescents. 113
While not neglecting early-life nutrition, a life-cycle approach to nutrition requires increased attention and a re-prioritization of middle childhood and early adolescence. The school-age years provide unique opportunities that will need to be embraced, even more so now, given the added challenges placed on the world by the recent COVID pandemic and climate change.
Nutrition during the formative years remains the foundation for long-term health and productivity of the individuals who make up society. Of these formative years, the first 5, with good reason, have received great attention over the last few decades. Decreasing infant mortality, including the vicious cycle of undernutrition and disease, and a better understanding of health and disease’s developmental origins, have improved our focus and understanding of the critical first few years of life. This, however, was coupled with the poorly documented notion that somatic and cognitive harm or delay in the first 2 years of life were irreversible, and hindered in part the attention given to the rest of childhood, particularly middle childhood and early adolescence. Middle childhood and early adolescence remain the most underrepresented of all life stages in health and nutrition research and clinical, nutritional, and epidemiologic data.
After the first 1000 days, the school-age years represent the most dynamic period of change in somatic and cognitive development before an individual reaches maturity, with multiple changes and inflection points in growth and development trajectories. Figure 4 summarizes key milestones in somatic and brain growth and development and shows how “eventful” this life-cycle period truly is. Deficits in growth, bone health, cognitive development, and alterations in body composition during this period have a life-long impact. It is possible and critical that we intervene during school age (a) to maintain an adequate course of somatic and cognitive development and a bridge to adult life, (b) to correct deficits of undernutrition and “catch-up” to the normal course of growth and development, and (c) to modulate or mitigate inadequacies of overnutrition and avoid longer-term consequences. Middle childhood and adolescence are thus a last major opportunity for investment, to affect growth, nutrition, and ultimate health and cognitive outcomes.
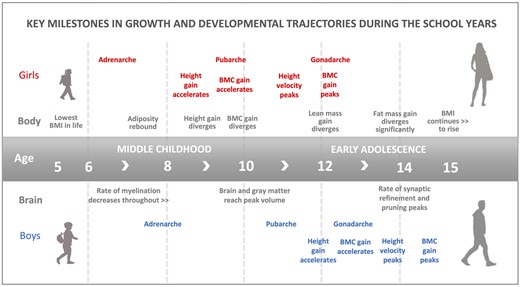
The figure depicts key events in somatic and brain growth and development trajectories occurring in middle childhood and early adolescence. The timing is meant to show sequence, and the ages are best approximations. Divergence relates to differences between sexes. See text for related references. BMC: bone mineral content.
Childhood education, the basis for societal development, is not possible without adequate nutrition. In addition, child education and school systems themselves provide significant tangible opportunities for influencing dietary intake as well as for educating future generations on diet and nutrition. Therefore, it is imperative to improve our understanding of the opportunities presenting themselves during this period of life, and to develop policies and strategies to improve the current level of response to those opportunities. Only very recently has this understanding led to a revisiting of priorities in combating poor nutrition and its long-term consequences. The emphasis on intervention during the school-age years needs to be nurtured and reinforced.
The authors would like to thank Dr Francois-Pierre Martin, Dr Laurence Donato-Capel, and Dr Marie-Claire Fichot for reviewing and providing valuable suggestions regarding the manuscript.
Author contributions . All authors participated in the planning, review, and final approval of the manuscript. The content is solely and entirely the work of the authors.
Funding . The collection of material for this manuscript was partially supported by the Société des Produits Nestlé.
Declaration of interest . J.M.S. is a consultant for Société des Produits Nestlé, and Scaled Microbiomics. A.P. is a board member of the Nestlé Nutrition Institute.
Bundy DAP , Silva ND , Horton AP , et al. Child and adolescent health and development: realizing neglected potential. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017: 1–23.
Google Scholar
Google Preview
Prentice AM , Ward KA , Goldberg GR , et al. Critical windows for nutritional interventions against stunting . Am J Clin Nutr. 2013 ; 97 : 911 – 918 .
Best C , Neufingerl N , van Geel L , et al. The nutritional status of school-aged children: why should we care? Food Nutr Bull. 2010 ; 31 : 400 – 417 .
Akseer N , Al-Gashm S , Mehta S , et al. Global and regional trends in the nutritional status of young people: a critical and neglected age group [published correction appears in Ann N Y Acad Sci . 2017;1396(1):236] . Ann NY Acad Sci. 2017 ; 1393 : 3 – 20 .
Georgiadis A , Penny ME. Child undernutrition: opportunities beyond the first 1000 days . Lancet Public Health. 2017 ; 2 : e399 .
Bundy DAP , de Silva N , Horton S , et al. Annex 1A. Supplemental material. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 :1. Available at: http://www.dcp-3.org/chapter/2754/annexes . Accessed May 11, 2022.
WHO . UNICEF, World Bank, and the Demographic and Health Surveys (DHS)/USAID database. 2021 . Available at: https://dhsprogram.com/data/ . Accessed May 11, 2022.
Galloway R. Global nutrition outcomes at ages 5 to 19. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 : 37 – 45 .
Sawyer SM , Azzopardi PS , Wickremarathne D , et al. The age of adolescence . Lancet Child Adolesc Health. 2018 ; 2 : 223 – 228 .
Alderman H , Behrman JR , Glewwe P , et al. Evidence of impact of interventions on growth and development during early and middle childhood. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 : 79 – 98 .
United Nations Children’s Fund (UNICEF) . Convention on the Rights of the Child. 1990 . Available at: https://www.unicef.org/child-rights-convention/convention-text . Accessed May 11, 2022.
Patton GC , Sawyer SM , Santelli JS , et al. Our future: a Lancet commission on adolescent health and wellbeing . Lancet. 2016 ; 387 : 2423 – 2478 .
McDonagh JE ; European Training Effective Care and Health Faculty . The age of adolescence…and young adulthood . Lancet Child Adolesc Health. 2018 ; 2 : e6 .
Cousminer DL , Berry DJ , Timpson NJ , et al. ; The ReproGen Consortium . Genome-wide association and longitudinal analyses reveal genetic loci linking pubertal height growth, pubertal timing and childhood adiposity . Hum Mol Genet . 2013 ; 22 : 2735 – 2747 .
DelGiudice M. Middle childhood: an evolutionary–developmental synthesis. In: Halfon N , Forrest CB , Lerner RM , Faustman EM , eds. Handbook of Life Course Health Development . Cham (CH ): Springer ; 2017 : 95 – 107 .
Reinehr T , Roth CL. Is there a causal relationship between obesity and puberty? Lancet Child Adolesc Health . 2019 ; 3 : 44 – 54 .
Song Y , Ma J , Wang HJ , et al. Trends of age at menarche and association with body mass index in Chinese school-aged girls, 1985–2010 . J Pediatr. 2014 ; 165 : 1172 – 1177.e1 .
Goswami B , Roy AS , Dalui R , et al. Impact of pubertal growth on physical fitness . Am J Sports Med. 2014 ; 2 : 34 – 39 .
USA Centers for Disease Control and Prevention (CDC): National Center for Health Statistics. CDC Growth Charts . Available at: https://www.cdc.gov/growthcharts/cdc_charts.htm . Accessed May 11, 2022.
Cole TJ. Children grow and horses race: is the adiposity rebound a critical period for later obesity? BMC Pediatr. 2004 ; 4 : 6 .
Veldhuis JD , Roemmich JN , Richmond EJ , et al. Endocrine control of body composition in infancy, childhood, and puberty . Endocr Rev. 2005 ; 26 : 114 – 146 .
Webber CE , Barr RD. Age- and gender-dependent values of skeletal muscle mass in healthy children and adolescents . J Cachexia Sarcopenia Muscle. 2012 ; 3 : 25 – 29 .
McCarthy HD , Samani-Radia D , Jebb SA , et al. Skeletal muscle mass reference curves for children and adolescents . Pediatr Obes. 2014 ; 9 : 249 – 259 .
Tanner JM , Davies PS. Clinical longitudinal standards for height and height velocity for North American children . J Pediatr. 1985 ; 107 : 317 – 329 .
Nijjar JK , Stafford D. Undernutrition and growth in the developing world . Curr Opin Endocrinol Diabetes Obes. 2019 ; 26 : 32 – 38 .
Owino V , Ahmed T , Freemark M , et al. Environmental enteric dysfunction and growth failure/stunting in global child health . Pediatrics . 2016 ; 138 : e20160641 .
Millward DJ. Nutrition, infection and stunting: the roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children . Nutr Res Rev. 2017 ; 30 : 50 – 72 .
Prendergast AJ , Humphrey JH. The stunting syndrome in developing countries . Paediatr Int Child Health. 2014 ; 34 : 250 – 265 .
Baxter-Jones AD , Faulkner RA , Forwood MR , et al. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass . J Bone Miner Res. 2011 ; 26 : 1729 – 1739 .
Maggioli C , Stagi S. Bone modeling, remodeling, and skeletal health in children and adolescents: mineral accrual, assessment and treatment . Ann Pediatr Endocrinol Metab. 2017 ; 22 : 1 – 5 .
Golden NH , Abrams SA ; Committee on Nutrition . Optimizing bone health in children and adolescents . Pediatrics . 2014 ; 134 : e1229 – e1243 .
Ralston SH , de Crombrugghe B. Genetic regulation of bone mass and susceptibility to osteoporosis . Genes Dev. 2006 ; 20 : 2492 – 2506 .
Weaver CM , Gordon CM , Janz KF , et al. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations [published correction appears in Osteoporos Int. 2016;27(4):1387] . Osteoporos Int. 2016 ; 27 : 1281 – 1386 .
Stiles J , Jernigan TL. The basics of brain development . Neuropsychol Rev. 2010 ; 20 : 327 – 348 .
Konrad K , Firk C , Uhlhaas PJ. Brain development during adolescence: neuroscientific insights into this developmental period . Dtsch Arztebl Int. 2013 ; 110 : 425 – 431 .
Mills KL , Goddings AL , Herting MM , et al. Structural brain development between childhood and adulthood: convergence across four longitudinal samples . Neuroimage. 2016 ; 141 : 273 – 281 .
Lenroot RK , Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging . Neurosci Biobehav Rev. 2006 ; 30 : 718 – 729 .
Peterson MR , Cherukuri V , Paulson JN , et al. Normal childhood brain growth and a universal sex and anthropomorphic relationship to cerebrospinal fluid . J Neurosurg Pediatr. 2021 ; 28 : 458 – 468 .
De Bellis MD , Keshavan MS , Beers SR , et al. Sex differences in brain maturation during childhood and adolescence . Cereb Cortex. 2001 ; 11 : 552 – 557 .
Johnson SB , Blum RW , Giedd JN. Adolescent maturity and the brain: the promise and pitfalls of neuroscience research in adolescent health policy . J Adolesc Health. 2009 ; 45 : 216 – 221 .
Immordino-Yang MH , Darling-Hammond L , Krone C. The Brain Basis for Integrated Social, Emotional, and Academic Development. How emotions and social relationships drive learning . Washington, DC: The Aspen Institute National Commission on Social, Emotional, and Academic Development. 2018 . Available at: https://www.aspeninstitute.org/publications . Accessed May 11, 2022.
Dumontheil I. Development of abstract thinking during childhood and adolescence: the role of rostrolateral prefrontal cortex . Dev Cogn Neurosci. 2014 ; 10 : 57 – 76 .
Flege JE , Munro MJ , MacKay IR. Factors affecting strength of perceived foreign accent in a second language . J Acoust Soc Am . 1995 ; 97 : 3125 – 3134 .
Giedd JN , Blumenthal J , Jeffries NO , et al. Brain development during childhood and adolescence: a longitudinal MRI study . Nat Neurosci. 1999 ; 2 : 861 – 863 .
Diamond A. Executive functions . Handb Clin Neurol. 2020 ; 173 : 225 – 240 .
Anderson P. Assessment and development of executive function (EF) during childhood . Child Neuropsychol. 2002 ; 8 : 71 – 82 .
Spear LP. Adolescent neurodevelopment . J Adolesc Health. 2013 ; 52 : S7 – S13 .
Mills KL , Goddings AL , Clasen LS , et al. The developmental mismatch in structural brain maturation during adolescence . Dev Neurosci. 2014 ; 36 : 147 – 160 .
Kelley JC , Crabtree N , Zemel BS. Bone density in the obese child: clinical considerations and diagnostic challenges . Calcif Tissue Int. 2017 ; 100 : 514 – 527 .
Das JK , Salam RA , Thornburg KL , et al. Nutrition in adolescents: physiology, metabolism, and nutritional needs . Ann N Y Acad Sci. 2017 ; 1393 : 21 – 33 .
Trumbo P , Schlicker S , Yates AA , et al. ; Food and Nutrition Board of the Institute of Medicine, The National Academies . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids [published correction appears in J Am Diet Assoc . 2003;103(5):563] . J Am Diet Assoc . 2002 ; 102 : 1621 – 1630 .
Chugani HT. Positron emission tomography scanning: applications in newborns . Clin Perinatol. 1993 ; 20 : 395 – 409 .
Grande Covián F. El metabolismo energético del cerebro en la infancia [Energy metabolism of the brain in children (author’s transl)] . An Esp Pediatr . 1979 ; 12 : 235 – 244 .
Kalhan SC , Kiliç I. Carbohydrate as nutrient in the infant and child: range of acceptable intake . Eur J Clin Nutr. 1999 ; 53 ( suppl 1 ): S94 – S100 .
European Food Safety Authority (EFSA) . Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Summary of Dietary Reference Values – version 4. September 2017 . Available at: https://www.efsa.europa.eu/en/topics/topic/dietary-reference-values. Accessed May 11, 2022.
Branca F , Vatueña S. Calcium, physical activity and bone health–building bones for a stronger future . Public Health Nutr. 2001 ; 4 : 117 – 123 .
Heaney RP , Abrams S , Dawson-Hughes B , et al. Peak bone mass . Osteoporos Int. 2000 ; 11 : 985 – 1009 .
Sarafrazi N , Wambogo EA , Shepherd JA. Osteoporosis or low bone mass in older adults: United States, 2017–2018 . NCHS Data Brief . 2021 ;( 405 ): 1 – 8 .
Fragility Fractures - Epidemiology . Nyon, Switzerland: International Osteoporosis Foundation; 2021 . Available at: https://www.osteoporosis.foundation/health-professionals/fragility-fractures/epidemiology . Accessed May 11, 2022.
Prentice A , Schoenmakers I , Laskey MA , et al. Nutrition and bone growth and development . Proc Nutr Soc. 2006 ; 65 : 348 – 360 .
Georgieff MK , Ramel SE , Cusick SE. Nutritional influences on brain development . Acta Paediatr. 2018 ; 107 : 1310 – 1321 .
GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 . Lancet 2020 ; 396 : 1223 – 1249 .
Camaschella C. Iron deficiency . Blood 2019 ; 133 : 30 – 39 .
Pivina L , Semenova Y , Doşa MD , et al. Iron deficiency, cognitive functions, and neurobehavioral disorders in children . J Mol Neurosci. 2019 ; 68 : 1 – 10 .
Lozoff B. Iron deficiency and child development . Food Nutr Bull. 2007 ; 28 : S560 – S571 .
Larson LM , Phiri KS , Pasricha SR. Iron and cognitive development: what is the evidence? Ann Nutr Metab. 2017 ; 71 ( suppl 3 ): 25 – 38 .
Briend A , Khara T , Dolan C. Wasting and stunting—similarities and differences: policy and programmatic implications . Food Nutr Bull. 2015 ; 36 : S15 – S23 .
Schoenbuchner SM , Dolan C , Mwangome M , et al. The relationship between wasting and stunting: a retrospective cohort analysis of longitudinal data in Gambian children from 1976 to 2016 . Am J Clin Nutr . 2019 ; 110 : 498 – 507 .
Fernald LCG , Prado E , Kariger P , et al. A Toolkit for Measuring Early Childhood Development in Low and Middle-Income Countries. 2017 International Bank for Reconstruction and Development, The World Bank, Washington DC. License: CC BY 3.0 IGO. Available at: https://openknowledge.worldbank.org/handle/10986/29000 . Accessed May 11, 2022.
Crookston BT , Penny ME , Alder SC , et al. Children who recover from early stunting and children who are not stunted demonstrate similar levels of cognition . J Nutr. 2010 ; 140 : 1996 – 2001 .
Sudfeld CR , McCoy DC , Danaei G , et al. Linear growth and child development in low- and middle-income countries: a meta-analysis . Pediatrics . 2015 ; 135 : e1266 – e1275 .
Walker SP , Chang SM , Powell CA , et al. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation . J Nutr . 2007 ; 137 : 2464 – 2469 .
Sánchez A. The structural relationship between early nutrition, cognitive skills and non-cognitive skills in four developing countries . Econ Hum Biol. 2017 ; 27 : 33 – 54 .
Fink G , Rockers PC. Childhood growth, schooling, and cognitive development: further evidence from the Young Lives study . Am J Clin Nutr . 2014 ; 100 : 182 – 188 .
Caleyachetty R , Thomas GN , Kengne AP , et al. The double burden of malnutrition among adolescents: analysis of data from the Global School-Based Student Health and Health Behavior in School-Aged Children surveys in 57 low- and middle-income countries . Am J Clin Nutr. 2018 ; 108 : 414 – 424 .
Schott W , Aurino E , Penny ME , et al. The double burden of malnutrition among youth: trajectories and inequalities in four emerging economies . Econ Hum Biol. 2019 ; 34 : 80 – 91 .
Andersen CT , Stein AD , Reynolds SA , et al. Stunting in infancy is associated with decreased risk of high body mass index for age at 8 and 12 years of age . J Nutr . 2016 ; 146 : 2296 – 2303 .
World Health Organization. Noncommunicable Disease Surveillance, Monitoring and Reporting. Global School-based Student Health Survey . Available at: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-school-based-student-health-survey. Accessed May 11, 2022.
NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body–mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults . Lancet . 2017 ; 390 : 2627 – 2642 .
NCD Risk Factor Collaboration (NCD-RisC) . Height and body–mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants . Lancet . 2020 ; 396 : 1511 – 1524 .
Best C , Neufingerl N , Del Rosso JM , et al. Can multi-micronutrient food fortification improve the micronutrient status, growth, health, and cognition of schoolchildren? A systematic review . Nutr Rev. 2011 ; 69 : 186 – 204 .
Ng M , Fleming T , Robinson M , et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013 [published correction appears in Lancet . 2014;384(9945):746] . Lancet . 2014 ; 384 : 766 – 781 .
Christian P , Smith ER. Adolescent undernutrition: global burden, physiology, and nutritional risks . Ann Nutr Metab. 2018 ; 72 : 316 – 328 .
Darnton-Hill I , Nishida C , James WP. A life course approach to diet, nutrition and the prevention of chronic diseases . Public Health Nutr. 2004 ; 7 : 101 – 121 .
McLean E , Cogswell M , Egli I , et al. Global Nutrition Report . Chapter 3. Development Initiatives Poverty Research Ltd 2018. 2018 . https://globalnutritionreport.org/reports/global-nutrition-report-2018/. Accessed May 11, 2022.
McLean E , Cogswell M , Egli I , et al. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005 . Public Health Nutr. 2009 ; 12 : 444 – 454 .
Singh V , West KP Jr . Vitamin A deficiency and xerophthalmia among school-aged children in Southeastern Asia . Eur J Clin Nutr. 2004 ; 58 : 1342 – 1349 .
Bailey RL , West KP Jr , Black RE. The epidemiology of global micronutrient deficiencies . Ann Nutr Metab. 2015 ; 66 : 22 – 33 .
Kumssa DB , Joy EJ , Ander EL , et al. Dietary calcium and zinc deficiency risks are decreasing but remain prevalent . Sci Rep. 2015 ; 5 : 10974 .
Andersson M , Takkouche B , Egli I , et al. Current global iodine status and progress over the last decade towards the elimination of iodine deficiency . Bull World Health Organ. 2005 ; 83 : 518 – 525 .
Rogers LM , Cordero AM , Pfeiffer CM , et al. Global folate status in women of reproductive age: a systematic review with emphasis on methodological issues . Ann NY Acad Sci. 2018 ; 1431 : 35 – 57 .
Palacios C , Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol. 2014 ; 144 ( Pt A ): 138 – 145 .
Pettifor JM. Calcium and vitamin D metabolism in children in developing countries . Ann Nutr Metab. 2014 ; 64 ( suppl 2 ): 15 – 22 .
De-Regil LM , Jefferds ME , Sylvetsky AC , et al. Intermittent iron supplementation for improving nutrition and development in children under 12 years of age . Cochrane Database Syst Rev 2011 ; 2011 : CD009085 .
Sachdev H , Gera T , Nestel P. Effect of iron supplementation on mental and motor development in children: systematic review of randomised controlled trials . Public Health Nutr. 2005 ; 8 : 117 – 132 .
Roberts JL , Stein AD. The impact of nutritional interventions beyond the first 2 years of life on linear growth: a systematic review and meta-analysis . Adv Nutr. 2017 ; 8 : 323 – 336 .
Martorell R , Khan LK , Schroeder DG. Reversibility of stunting: epidemiological findings in children from developing countries . Eur J Clin Nutr. 1994 ; 48 ( suppl 1 ): S45 – S57 .
Victora CG , Adair L , Fall C , et al. Maternal and child undernutrition: consequences for adult health and human capital [published correction appears in Lancet . 2008;371(9609):302] . Lancet . 2008 ; 371 : 340 – 357 .
Watkins KL , Bundy DAP , Jamison DT , et al. Evidence of impact of interventions on health and development during middle childhood and school age. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 : 99 – 105 .
Gasparetto M , Guariso G. Crohn’s disease and growth deficiency in children and adolescents . World J Gastroenterol. 2014 ; 20 : 13219 – 13233 .
Boersma B , Houwen RH , Blum WF , et al. Catch-up growth and endocrine changes in childhood celiac disease. Endocrine changes during catch-up growth . Horm Res. 2002 ; 58 ( suppl 1 ): 57 – 65 .
Abrams SA , Mushi A , Hilmers DC , et al. A multinutrient-fortified beverage enhances the nutritional status of children in Botswana . J Nutr . 2003 ; 133 : 1834 – 1840 .
Ash DM , Tatala SR , Frongillo EA Jr , et al. Randomized efficacy trial of a micronutrient-fortified beverage in primary school children in Tanzania . Am J Clin Nutr . 2003 ; 77 : 891 – 898 .
Sokolovic N , Selvam S , Srinivasan K , et al. Catch-up growth does not associate with cognitive development in Indian school-age children . Eur J Clin Nutr. 2014 ; 68 : 14 – 18 .
Crookston BT , Schott W , Cueto S , et al. Postinfancy growth, schooling, and cognitive achievement: young lives . Am J Clin Nutr. 2013 ; 98 : 1555 – 1563 .
Georgiadis A , Benny L , Duc LT , et al. Growth recovery and faltering through early adolescence in low- and middle-income countries: determinants and implications for cognitive development . Soc Sci Med. 2017 ; 179 : 81 – 90 .
Golden MH. Is complete catch-up possible for stunted malnourished children? Eur J Clin Nutr . 1994 ; 48 ( suppl 1 ): S58 – S70; discussion S71 .
Kalkwarf HJ , Khoury JC , Lanphear BP. Milk intake during childhood and adolescence, adult bone density, and osteoporotic fractures in US women . Am J Clin Nutr . 2003 ; 77 : 257 – 265 .
Jacob CM , Hardy-Johnson PL , Inskip HM , et al. A systematic review and meta-analysis of school-based interventions with health education to reduce body mass index in adolescents aged 10 to 19 years . Int J Behav Nutr Phys Act. 2021 ; 18 : 1 .
Singhal J , Herd C , Adab P , et al. Effectiveness of school-based interventions to prevent obesity among children aged 4 to 12 years old in middle-income countries: a systematic review and meta-analysis . Obes Rev. 2021 ; 22 : e13105 .
Kyere P , Veerman JL , Lee P , et al. Effectiveness of school-based nutrition interventions in sub-Saharan Africa: a systematic review . Public Health Nutr. 2020 ; 23 : 2626 – 2636 .
United Nations Children’s Fund (UNICEF) . Nutrition, for Every Child: UNICEF Nutrition Strategy 2020–2030 . New York : UNICEF . 2020 . Available at: https://www.unicef.org/media/92031/file/UNICEF%20Nutrition%20Strategy%202020-2030.pdf . Accessed May 11, 2022.
United Nations Children’s Fund (UNICEF) . Programming Guidance: Nutrition in Middle Childhood and Adolescence . New York, NY : UNICEF . 2021 . Available at: https://www.unicef.org/media/106406/file . Accessed May 11, 2022.
Tapert SF , Schweinsburg AD. The human adolescent brain and alcohol use disorders . Recent Dev Alcohol. 2005 ; 17 : 177 – 197 .
Lee FS , Heimer H , Giedd JN , et al. Mental health. Adolescent mental health—opportunity and obligation . Science. 2014 ; 346 : 547 – 549 .
- malnutrition
- science of nutrition
- middle childhood
- school-age child
- growth and development
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1753-4887
- Print ISSN 0029-6643
- Copyright © 2024 International Life Sciences Institute
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Review article, global trends and future prospects of child nutrition: a bibliometric analysis of highly cited papers.

- 1 School of Management, Lanzhou University, Lanzhou, China
- 2 Gansu Provincial Hospital, Lanzhou, China
- 3 Department of Social Medicine and Health Management, School of Public Health, Lanzhou University, Lanzhou, China
- 4 Evidence Based Social Science Research Center, School of Public Health, Lanzhou University, Lanzhou, China
Child nutrition has always been a global concern. This study performed visual analysis of 1,398 child nutrition highly cited papers (HCPs) from 2009 to 2019. The purpose of the study was to evaluate and present the performances of authors, journals, countries, institutions, top cited papers; to explore the hot topics, prospects, and to propose the future research directions on child nutrition. We used bibliometric methods to conduct in-depth statistical analysis of HCPs on child nutrition, showing research progress, trends and hot spots. We included HCPs on child nutrition from the Science Citation Index-Expanded (SCI-E) database February 7, 2020. Two tools, CiteSpace and VOSviewer, were used to conduct the bibliometric analyses. The results showed that, since 2011, the number of HCPs on child nutrition has increased rapidly. The top three contributors in this field were the USA, the UK and Canada. However, the contribution of developing countries was very limited. Intestinal microflora, food allergy, overweight and obesity were the three major research hotspots in this field. Results of this study provide valuable references for ongoing child nutrition related research, which may be interesting and noteworthy to the researchers involved.
Introduction
Child nutrition has always been a global concern. The United Nations International Children's Emergency Fund (UNICEF) released a report in 2019 about children, food and nutrition, entitled “The State of the World's Children in 2019” ( 1 ). The report mentioned that one-third of the world's children under the age of five still cannot get the nutrition they need to grow up currently. At the same time, the burden of malnutrition has become increasingly prominent ( 2 – 4 ). Among the global children under five, there are still 149 million stunted, and nearly 50 million children are in a state of wasting. Three hundred and forty million children face vitamin and mineral deficiencies, which is also known as “hidden hunger” ( 5 ). The problem of overweight is developing rapidly ( 6 ). Lack of necessary nutrients which may weaken the immune system, cause visual and hearing impairments and may also cause obesity. Studies have shown that the average lifetime income loss per child with growth retardation was $ 1,400, and in developed countries, it was as high as $ 30,000 ( 7 ). Overweight and obesity-related diseases, including heart disease, cancer, diabetes, and chronic respiratory diseases, was projected to cost more than $7 trillion in low and middle-income countries between 2011 and 2025 ( 7 – 12 ).
Carrying out scientific research on child nutrition can guide children to take in nutrition reasonably and promote children's healthy growth and development. Black's et al. paper “Global, regional, and national causes of child mortality in 2008: a systematic analysis” conducted a systematic analysis of global causes of child mortality in 2008, and found that nutrition was crucial to guide global efforts to improve child survival ( 13 ). Pries's et al. paper “Snack food and beverage consumption and young child nutrition in low–and middle–income countries: A systematic review” believed that although snacks could provide important nutrients for young children during the complementary feeding period, consumption of energy-dense, nutrient-poor snack foods and sugar-sweetened beverages (SSB) influences undernutrition and overnutrition among young children ( 14 ). Robertson's et al. paper “The Human Microbiome and Child Growth–First 1,000 Days and Beyond” found that an “undernourished” microbiome is intergenerational, thereby perpetuating growth impairments into successive generations, which may contribute to lifelong and intergenerational deficits in growth and development ( 15 ). The results of the above papers have greatly promoted the research on children's health, and have been cited by relevant scholars for many times. Highly cited papers (HCPs) in the Essential Science Indicators database refer to papers with citations in the top 1% of all papers in a research field, and they are considered to be symbols of scientific excellence and top performance of the past 10 years ( 16 ). The identification of HCPs on child nutrition could reflect the research progress and hot topics in this field accurately, which has an important reference to relevant scholars ( 16 , 17 ). Bibliometric analysis is description of the external characteristics of the literature through mathematical and statistical methods, mainly based on the content of published journal papers as the main research object, and descriptive statistics on the academic status, such as journal distribution and main research institutions. Bibliometric analysis is one of the more effective research methods for evaluating the development stage of the discipline and predicting the future development trend ( 18 , 19 ).
Methodology
Data source and search strategy.
We searched the Science Citation Index-Expanded (SCI-E) database on February 7, 2020. The specific retrieval strategy can be found in the Supplementary Material . The initial search yielded a total of 214,264 papers in the period from 1980 to the present. Among them, we chose the selection of “highly cited” in the field. Finally, 1,398 researches were included. There are no limitations on language, publication year, data category, and document type.
Analysis Method
In this research, CiteSpace and VOSviewer tools were used to analyze the publication characteristics, including paper type, language and quantity, active authors, countries and institutions, journals, co-cited journals and co-cited references, co-occurrence keywords and burst keywords, and form social network maps (SNMs) based on the characteristics of the papers published ( 20 – 23 ). Due to the particularity of data format requirements of CiteSpace software, the selected literature was exported in the format of “RefWorks,” the data was saved in the format of “Download_XXX,” and imported into CiteSpace. Set the “Years Per Slice” length to “1,” the “Terms Types” to “Burst Terms,” and the “Pruning” to “Pathfinder.” Meanwhile, the selected literature was downloaded in the format of “TXT” and imported into VOSviewer software. The data type was set to “Create a map based on bibiographic data” and the data source was set to “Read data from bibliographic database files.” Different nodes represent different elements such as authors, countries, institutions, and keywords in a cluster map. The size of nodes indicates the number of publications or co-occurrence times of keywords. The lines between nodes reflects the relations of cooperation, co-occurrence, or co-citations. Nodes and lines of the same color represent the same cluster ( 24 , 25 ). Microsoft Excel 2016 was used to conduct data aggregation and analysis.
Paper Type, Language and Quantity
A total of 1,398 HCPs were retrieved from SCI-E, which includes 944 (67.525%) full-length research articles and 454 (32.475%) reviews. Most of the papers 1,394 (99.714%) were published in English, followed by 2 (0.143%) were published in German and 2 (0.143%) were published in Spanish.
The HCPs on child nutrition were published in 2009 (92 papers) and exceeded 100 papers in 2010 ( Figure 1 ). In 2011, the number of publications decreased (103 papers). Since 2012, the number of publications increased by more than 30 (135 papers) and the growth rate continues slowly and steadily to 2017 (155 papers). The number of publications dropped significantly in 2018 and <100 papers in 2019 (Incomplete statistics). In this study, the relationship between the publication year and the number of publications is described using a polynomial model. There is a significant correlation between the number of studies and the year with a high coefficient of determination ( R 2 = 0.9109).
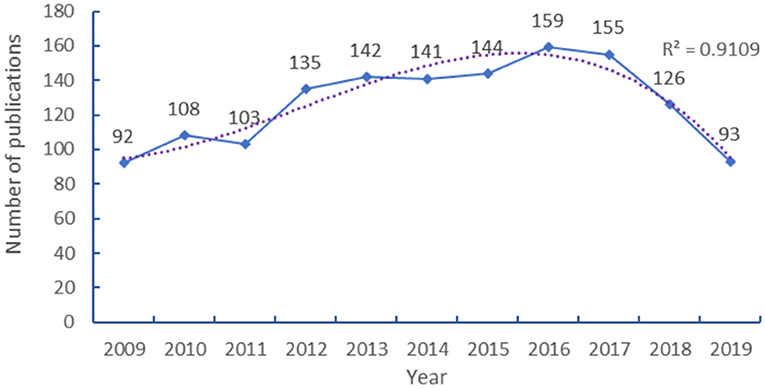
Figure 1 . Publication years for HCPs on child nutrition.

Active Authors, Countries, and Institutions
The HCPs on child nutrition included 7,868 authors. The top 10 authors and co-cited authors were shown in Table 1 . Tremblay has published the most, 17 (1.22%) papers, following Victora with 14 (1.00%) publications. The third were Lawlor and Bhutta both 12 publications (0.86%), following Black 11 publications (0.79%) and Smith 10 publications (0.72%). The other 4 authors all published fewer than 10 publications. The highest co-cited author was World Health Organization (621 co-citations), the remaining co-cited authors were Ogden (183 co-citations), Victora (135 co-citations), Deonis (132 co-citations), Cole (127 co-citations), Sallis (119 co-citations), Flegal (112 co-citations), and Kramer (107 co-citations). Other co-cited authors both 100 co-citations.
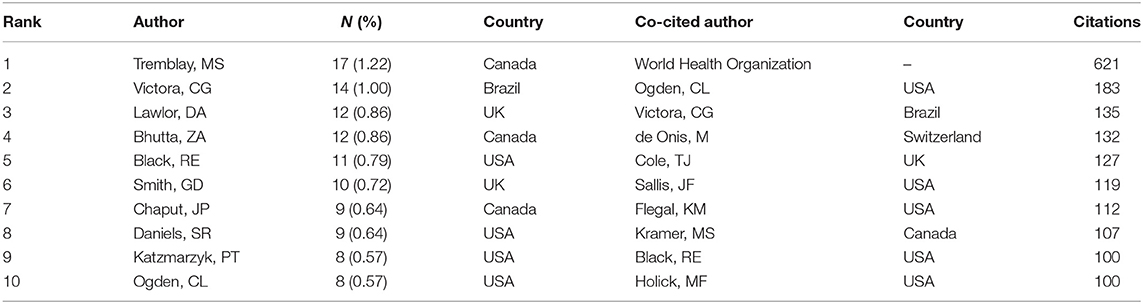
Table 1 . The top 10 authors and co-cited authors [ n (%)].
In total, 113 countries published papers in this study. The top 10 countries and institutions were shown in Table 2 , with the USA ranked first, accounting for 59.87% and the UK ranked second (362 publications, 25.89%), followed by Canada (200 publications, 14.31%), Australia (161 publications, 11.52%), Switzerland (133 publications, 9.51%), Netherlands (127 publications, 9.08%), Germany (113 publications, 8.08%), France (101 publications, 7.22%). The other countries Italy and Spain both published <100 publications. As shown in Figure 2 , the 59 countries with more than 4 papers were divided into 4 categories, with close cooperation among them.
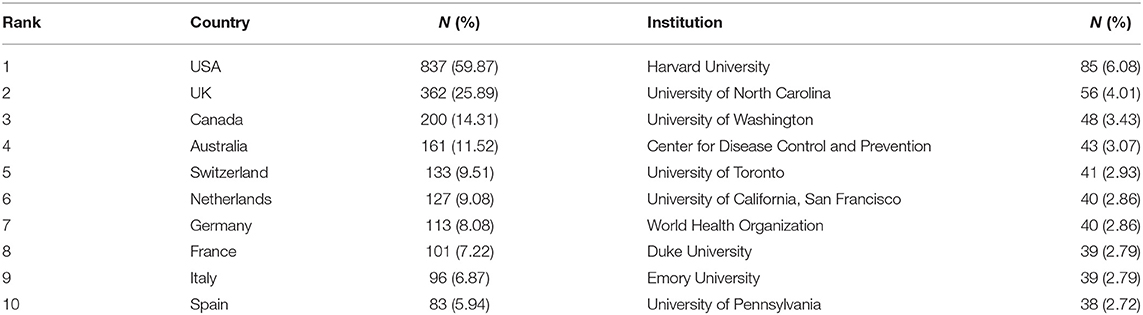
Table 2 . The top 10 countries and institutions [ n (%)].
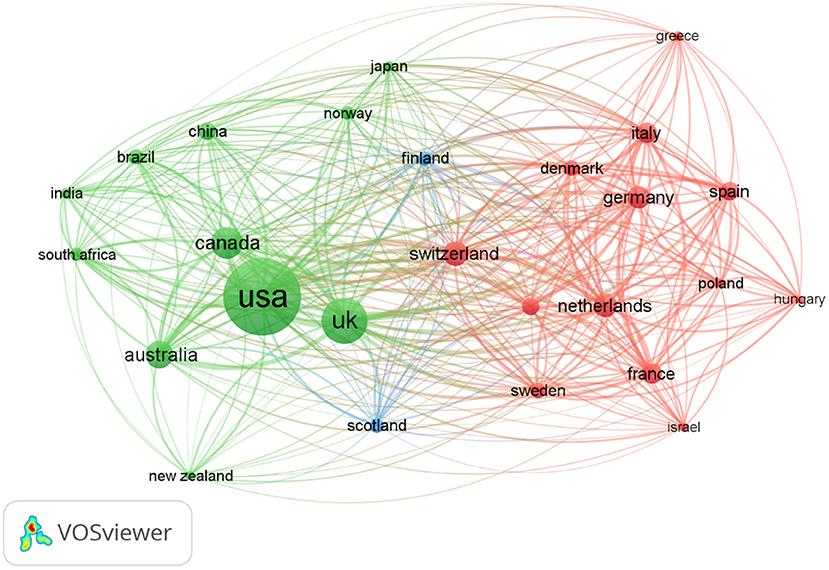
Figure 2 . The network map of countries.
Countries and institutions with greater influence and the status of cooperation could be displayed through the network maps. Two thousand four hundred eighty-two institutions contributed to the publications of this research. Table 3 showed the top 10 institutions. Harvard University ranked first (85 publications, 6.08%), followed by University of North Carolina (56 publications, 4.01%), University of Washington (48 publications, 3.43%), Center for Disease Control and Prevention (43 publications, 3.07%), University of Toronto (41 publications, 2.93%). The University of California, San Francisco and the World Health Organization published the same amount of papers (40 publications, 2.86%). Duke University and Emory University published the same amount of papers (39 publications, 2.79%). The 10th University of Pennsylvania published 38 (2.72%).
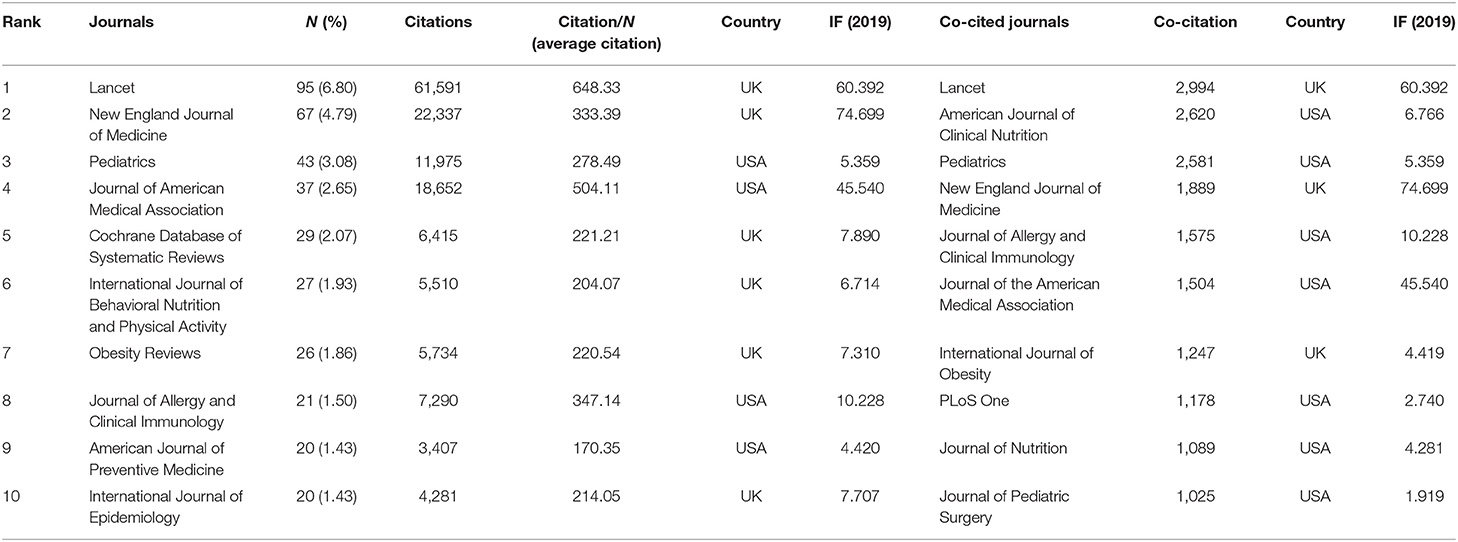
Table 3 . The top 10 journals and co-cited journals [ n (%)].
The cooperation of institutions with more than 10 papers was shown in Figure 3 . Major research institutions were divided into 5 clusters, and close collaboration between the groups.
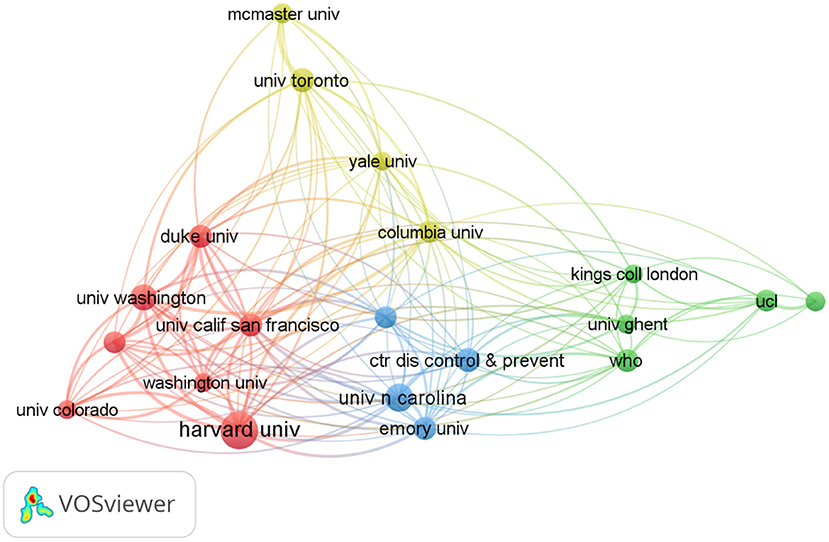
Figure 3 . The network map of institutions.
Journals, Co-cited Journals and Co-cited References
The study was published in 423 journals. The top 10 journals and co-cited journals, as well as the journal citation frequency, publishing countries and impact factor (IF) in 2019 could be seen in Table 3 . The most published journal was Lancet (95 publications, 6.8%), following New England Journal of Medicine (67 publications, 4.79%), Pediatrics (43 publications, 3.08%), Journal of American Medical Association (37 publications, 2.65%), Cochrane Database of Systematic Reviews (29 publications, 2.07%). Six of the top 10 journals were from the UK and others from the USA. “Citation/N” represents the average citations per paper. The Lancet ranked the highest because the average citation frequency of papers published in the journal was 648.33 times.
Lancet was the most co-citation (2,994 co-citations), followed by The American Journal of Clinical Nutrition (2,620 co-citations) and Pediatrics (2,581 co-citations). Among the top 10 co-cited journals, 7 are from the USA. Table 4 shows the top 10 co-cited references related to this research. The co-citation can reflect the researchers' attention. One paper was co-cited more than 60 times ( 26 ). Two papers were co-cited between 35 and 60 times ( 27 , 28 ). Others were co-cited between 30 and 35 times ( 29 – 35 ). The top 20 HCPs are shown in Figure 4 . Papers with a high frequency of citations are represented by red bars, and with a low frequency of citations are represented by green bars. The first reference with citation bursts appeared in 2009, 85.00% were first discovered between 2009 and 2011. After 2009, 3 HCPs were detected with citation burst.
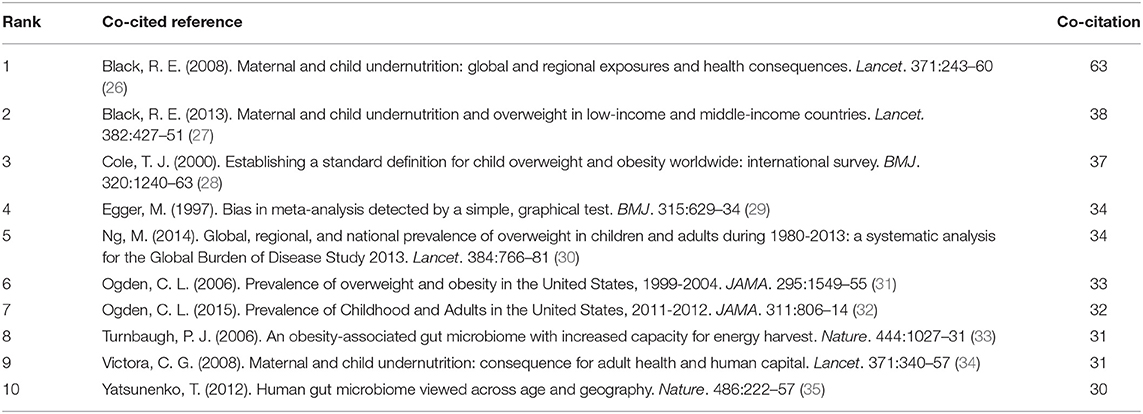
Table 4 . Top 10 co-cited references.
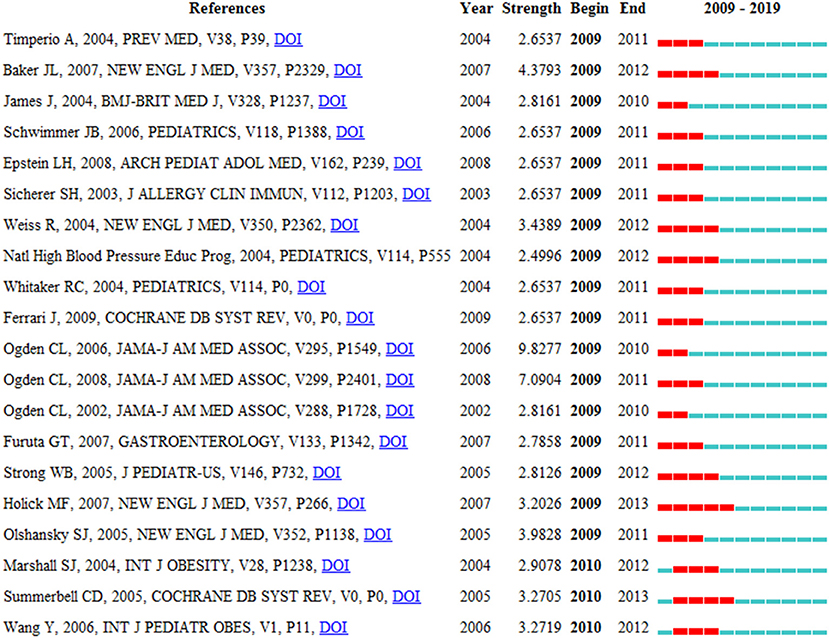
Figure 4 . Top 20 references with the strongest citation burst.
Co-occurrence Keywords and Burst Keywords
We summarized and counted the keywords from the 1,398 HCPs. Figure 5 showed the visualization of color spectral density based on keywords and hotspot intensity, where warm red represents the hot areas and cold blue represents the cold areas. Children, obesity, health, prevalence, risk, risk-factors, metabolic syndrome, united-states, physical-activity, and adolescents were the keywords with the highest density.
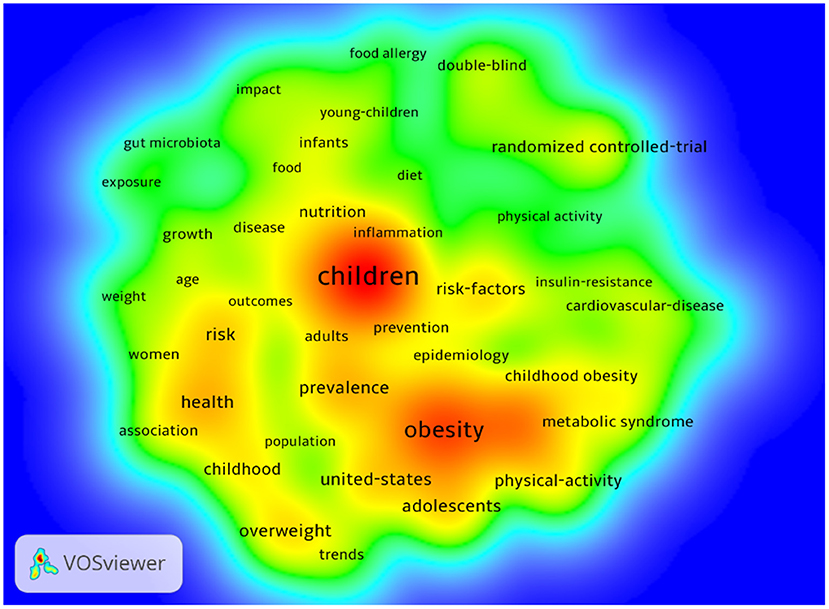
Figure 5 . The density map of keywords.
The cluster map of the main keywords was shown in Figure 6 . Four clusters were formed by these keywords. Cluster 1 was the largest of the four clusters, including 19 keywords, mainly focused on intestinal flora and physical health in children. Cluster 2 included 15 keywords, primarily focused on children's food intake and the prevention of food allergies. Cluster 3 included 14 keywords, mainly focused on the adverse outcomes of children who are overweight or obese. Cluster 4 included 6 keywords, mainly focused on the prevalence of overweight children in the USA.
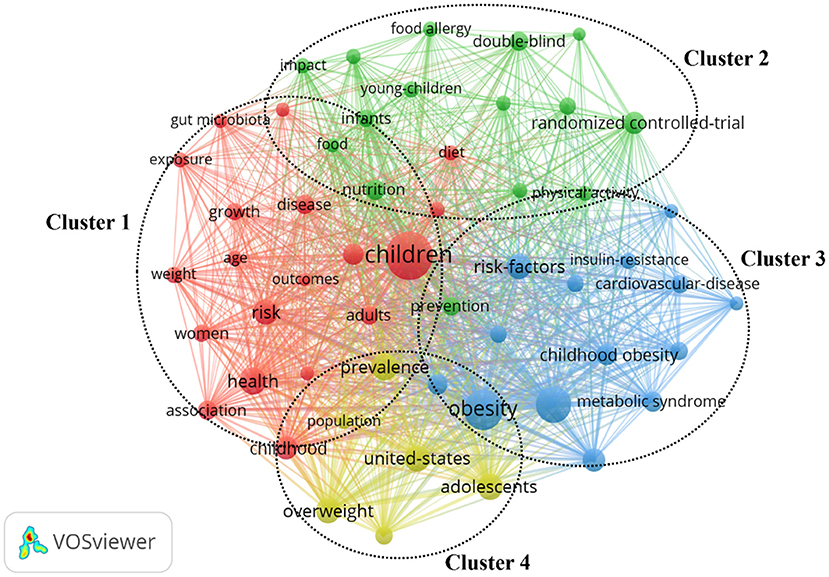
Figure 6 . The network map of keywords.
The map of burst keywords was shown in Figure 7 to identify hot topics. The time period that represents the strongest citation bursts was indicated in red bar. Among them, 8 keywords were detected in 2009. In this period, Vitamin D supplements, obesity-related complications such as diabetes, coronary heart disease, and the National Health and Nutrition Examination Survey (NHANES) findings were hot research topics. From 2010 to 2014, metabolic syndrome, steatohepatitis, insulin resistance, low birth weight and the establishment of models and environments to promote children's health, were major concerns. After 2014, no prominent keywords were detected.
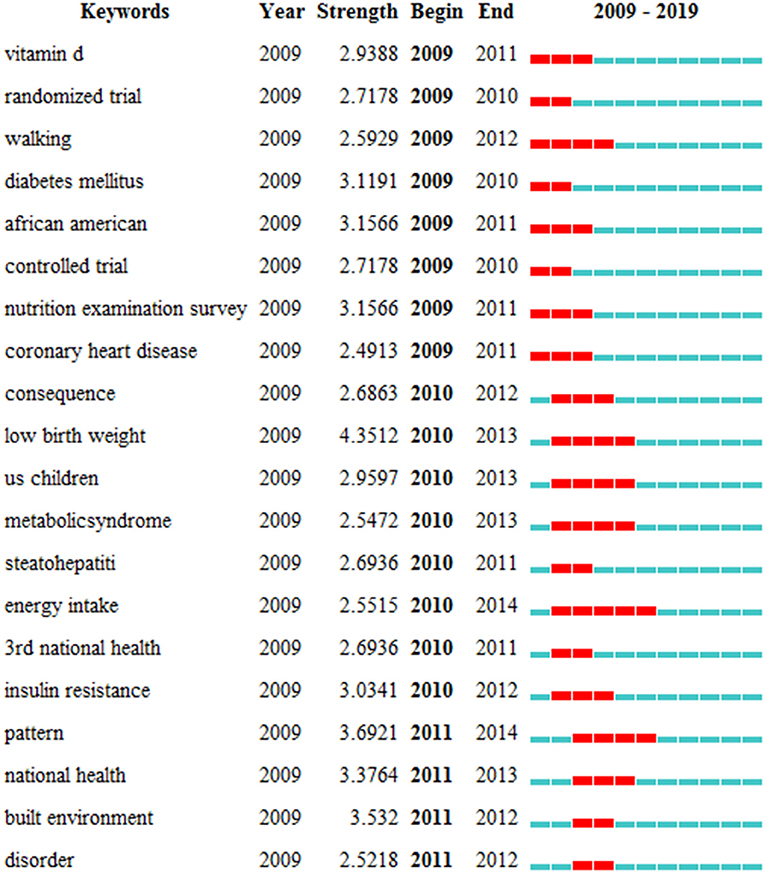
Figure 7 . Top 20 keywords with the strongest citation burst.
Analysis of Paper Types and Publication Year
There were two types of HCPs included in this study, with reviews accounted for 32.475%. This phenomenon means that a lot of summaries and conclusions has been completed by researchers on the basis of existing research. This was undoubtedly great progress. Thus, we were confident that the number of studies on child nutrition will continue to increase, with greater content in the future. This trend will create more awareness and draw attention to children's nutrition and health globally.
The included HCPs were published from 2009 to 2019. Before 2012, the number of published HCPs was in a state of slow growth, and <130, which suggested that the development of child nutrition research was slow during the period, and researchers did not realize the importance of children's nutrition and health. After 2012, HCPs began to growth slowly and reached peak of 159 in 2016. This may be due to the fact that the WHO Child Growth Standards demonstrate that, by the time children reach the age of five, differences are more affected by nutrition, feeding methods, environment, and health care than by genetic or racial characteristics, and the Ninth Global Conference on health promotion focused on global childhood obesity ( 36 , 37 ). After 2016, the number of HCPs has shown a decreasing trend. In general, the number of publications ranged from 90 to 160 annually.
The Geographical Distribution of Research Group
Among 1,398 HCPs included, 7,868 authors involved. But only 6 (0.08%) authors have published more than 10 papers. Sixty-one (0.78%) authors have published more than 5 papers. Statistical results showed that 6,865 (87.25%) authors published only 1 paper. This reflects that few researchers have been committed to child nutrition and health.
Among the top 10 authors, 3 from Canada, Tremblay, Bhutta, and Chaput. They have published 38 HCPs in total. The reason might be that Tremblay, as a leader, has published many papers on the prevalence and long-term changes in overweight and obesity about Canadian children and adolescents. Tremblay and Chaput have been working closely together and have published several papers on children's physical activity to control overweight and obesity. Among them, Systematic review of sedentary behavior and health indicators in school-aged children and youth , published by Tremblay et al. was cited the most ( 38 ), more than 800 times. Among the top 10 co-cited authors, 5 from the USA, and the total number of citations was 614. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012 , published by Ogden et al. ( 32 ); Prevalence and Trends in Obesity Among US Adults, 1999–2008 , published by Flegal et al. ( 39 ); Maternal and child undernutrition and overweight in low-income and middle-income countries , published by Black et al. ( 27 ); Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline , published by Holick et al. ( 40 ) has been cited more than 1,000 times. This shows that the active and influential scholars are from Canada and the USA. Interestingly, neither the top 10 authors nor the co-cited authors have any scholars from China. Probably because: ( 1 ) Chinese scholars pay little attention to child nutrition; ( 2 ) The number and quality of papers published by Chinese scholars on child nutrition were small; ( 3 ) Chinese scholars had low English proficiency and obvious language barriers. Therefore, in the future, it is important for Chinese scholars to strengthen exchanges and cooperation with outstanding foreign scholars to learn advanced research methods, broaden their horizons and ideas.
Although child nutrition deserves global attention, 24.11% of countries have only 1 highly cited paper. Among the top 10 countries with HCP on child nutrition, all included developed countries and no developing countries, which indicates that developing countries are lagging in this field. Among the top 10 institutions, 8 from the USA and 1 from Canada. This phenomenon showed that the USA was in a dominant position and there was a large gap between developing and developed countries in child nutrition research. In short, the global impact of developing countries on child nutrition is limited. There was need for collaborative efforts between high income countries and Low and Middle income countries (LMIC) to improve and carry out more high impact research in the areas of child nutrition especially among children in LMIC.
In terms of cooperation between countries, both the USA and the UK maintain close cooperation with 55 countries, Canada and Switzerland with 54 countries, respectively, followed by Australia and Belgium with 53 and 50 countries, respectively, while Slovakia did not cooperate with any country. It was noteworthy that, China has partnerships with 48 countries, so we are confident that China will be at the forefront on child nutrition in the future.
Analysis of Published Sources
The included 1,398 HCPs were published in 423 journals, each journal should publish an average of 3.30 papers, but in fact, 6.38% of journals published more than 10 papers and 58.16% of journals only published 1 paper. Four major journals published 242 papers, accounting for 17.32%. These journals were as follows: Lancet (6.80%), New England Journal of Medicine (4.79%), Pediatrics (3.08%), Journal of American Medical Association (2.65%). The Lancet was the journal with the most productive and cited researches of HCPs on child nutrition. Among the authors, Black et al. ( 27 ) and Ng et al. ( 30 ) from the USA published many papers, and have been cited 2,568 times and 5,253 times, respectively. The unprecedented World Summit for Children, held at the United Nations headquarters in New York City in 1990, set out 10-year goals for children's health, nutrition and education ( 41 ); the special session on children held in 2002 reviewed the progress made in children's affairs since the 1990 World Summit for Children and reinvigorated the global commitment to children's rights ( 42 ). Through holding these international conferences, scholars have developed great interest on child nutrition, which has also aroused scholars' attention.
Among the top 10 journals, six were from the UK and none from China, which once again confirms the huge gap in scientific research between developing and developed countries. Citation/N is an important index to measure the scientific importance or quality of a paper. It also shows that the quality of the journal is high and the content is attractive. The American Journal of Allergy and Clinical Immunology performed well. This journal were recognized and welcomed by scholars, because although the journal published only 21 HCPs, the citation /N was high, which also shows the high academic influence of the journal.
Analysis of the Main Keywords
Intestinal flora and physical health.
In this study, one of the important research hotspots and directions was the composition and roles of intestinal microbiota in children ( Figure 6 , cluster 1). There are a large number of bacteria in the human gut, which together make up the intestinal flora. In the human body, cells and bacterial cells are symbiotic, and there are 10 times as many bacterial cells as there are human cells ( 43 , 44 ). The effects of intestinal flora on the human body are mainly manifested as nutrient absorption, substance metabolism, and immune defense ( 45 ). Some minerals, such as calcium, iron, and magnesium, are absorbed by the body through the intestinal flora ( 46 ). The intestinal flora is also involved in the metabolism of certain substances by fermenting food, synthesizing exercise fatty acids and vitamin K, which are then absorbed by the body ( 47 ). For children, intestinal bacteria can not only regulate the activity of cytotoxic T cells and natural killer cells, reduce the replication of viruses in cells, but also play an important role in innate immunity, activation of the immune system and the formation of an adaptive immune response ( 48 , 49 ). Probiotics can significantly increase the expression of CD3 + CD4 + in children with severe HFMD caused by EV71, enhance the immune function of T cells and improve the cellular immune response of children. Therefore, intestinal flora plays an important role in children's growth. Gao et al. considered that the diversity of intestinal microflora in obese children was lower than that in normal children, and the relative abundance of intestinal flora at different classification levels was significantly different ( 50 ). Some studies have shown that the mode of delivery affects the bacterial community in the newborn gut. Guarino et al. noted in cesarean delivery, direct contact of the mouth of the newborn with vaginal and intestinal microbiota is replaced by exogenous non-maternally derived bacteria colonizing the infants' intestine producing a less diverse flora ( 51 ). Biasucci et al. believed that intestinal bacterial colonization of infants born by cesarean section is more likely to change ( 52 ). However, Rutayisire et al. considered that the diversity and colonization pattern of intestinal flora were significantly correlated with the mode of delivery 3 months before birth, but the difference disappeared after 6 months ( 53 ). Therefore, the diversity and colonization level of intestinal microflora and the mode of delivery as well as its extensive impact on the health of infants at all stages of life should be further studied.
Prevention of Food Allergies
Food allergies are common and affect about 8% of children in the United States. It brings a huge physiological, economic and social burden to children and families. There is no cure for food allergies ( 54 ). Therefore, the prevention and treatment of food allergy in children is also a key topic in recent years ( Figure 6 , cluster 2). Food allergies can be a variety of symptoms in children, with skin and gastrointestinal symptoms being the most common ( 55 ). Children under the age of 6 are often allergic to high-protein foods such as eggs, milk, peanut, and soy, as children's immune systems are not yet mature and the protective function of the gastrointestinal mucosa in infants is not perfect ( 56 ). Food allergies have a significant impact on the morbidity, living quality of infants and young children, which has become a concern for many parents ( 57 ). Peanut is one of the most common food allergies in children, which is becoming more and more common over time. So far, there is no effective treatment for peanut allergy, only through the use of epinephrine to avoid and alleviate this symptom. The double allergen exposure hypothesis suggested that the dermal sensitization of peanut may be the pathophysiological mechanism of peanut allergy development. In the future, oral and epicutaneous immunotherapy may be used as exciting tools to achieve peanut desensitization in children. In the past, people focused on the treatment of food allergy, but seldom considered the mental health consequences of living with the condition ( 58 , 59 ). Feng et al. found that patients with food allergy may have depression, anxiety, post-traumatic stress, being bullied, and poor overall quality of life. At the same time, the patient's family life will also be disturbed ( 60 ). Parents of children with food allergies, especially mothers, report anxiety, depression, and decreased quality of life ( 61 ). Fong et al. stressed that children and adolescents with food allergies in the Australian population are vulnerable to bullying. It's a significant social problem that requires addressing to positively assist these children ( 62 ).
At present, in the treatment and prevention of food allergies, bacterial therapy has attracted more and more attention from scholars. They believe that one of the effective ways to prevent allergic diseases is fecal flora transplantation ( 63 , 64 ).
Overweight or Obesity in Children
At present, childhood obesity is also widely concerned ( Figure 6 , cluster 3 and cluster 4). In 2017, the WHO announced that the number of obese children and adolescents aged 5 to 19 worldwide has increased ten-fold in the past 40 years. If the current trend continues, the number of obese children and adolescents will exceed the number of moderately or severely underweight by 2022 ( 64 ). American children's obesity rate ranks first in the world. Children with obesity may develop many serious comorbidities. These diseases include musculoskeletal diseases, cardiovascular diseases such as hypertension, insulin resistance and hyperlipidemia, respiratory diseases such as sleep apnea or asthma, and digestive system diseases such as non-alcoholic fatty liver disease ( 65 , 66 ). Childhood obesity has a greater risk of persistence in adulthood. Low socioeconomic status, immigration background, and clinical susceptibility to obesity are the serious risk factors for obesity. However, the individual causes of obesity are quite complex, so it is necessary to make a systematic analysis of individual differences, and to formulate differentiated and realistic treatment plans. In addition to the rare monogenic or syndromic obesity, the treatment of childhood obesity should rely on professional lifestyle intervention programs. In general, a key component of a treatment strategy should include improving nutrition, physical exercise and self-esteem, while reducing stress. Besides, the inclusion of parents in treatment strategies has proved beneficial and necessary. Studies have shown that male children are 1.6 times more likely to be overweight/obesity than female children; children of overweight mothers are 3.34 times more likely to be overweight/obesity than children of normal weight mothers; preschool children's overweight/obesity is related to physical activity, screen time, eating snacks when watching TV, using computers, tablets and mobile phones ( 64 ).
Considering the individual differences between obese children and the complexity of obesity, there is no effective treatment for all groups. The most appropriate intervention method is determined by the age of children and the degree of overweight. The current methods of weight loss include lifestyle change interventions, bariatric surgery and drug use. Lifestyle change is the most widely used way to treat childhood obesity ( 67 ). This approach is designed to improve the quality of diet, increase physical activity and reduce sedentary behavior, usually using behavior change techniques to help maintain positive change and prevent recurrence. Many interventions focus on families, and parents are defined as “agents of change,” especially among children under 12 ( 68 ). Bariatric surgery generally includes gastric shunt, sleeve gastrectomy and gastric banding ( 69 ). Currently, the drugs used to treat obesity include: ( 1 ) Sibutramine, an appetite inhibitor, which is still allowed in Brazil, was suspended by the European drug agency in 2010 due to its adverse cardiovascular effects, and was withdrawn by the US Food and Drug Administration (FDA) in 2010; ( 2 ) Orlistat, a fat absorption inhibitor, has been approved by the FDA, but only for children under the age of 12. Other drugs often used to treat childhood obesity include the antidiabetic drug metformin and the antidepressant fluoxetine ( 67 ). New drugs for appetite regulation are currently under development or evaluation.
Conclusions
At present, more and more researches on child nutrition have been published. The bibliometric method could be used to systematically analyze the characteristics of the papers and show the research status, hot spots, and future development trends. The results showed that 6,865 authors (87.65%) only published 1 paper. Scholars from the UK, the USA, and Canada had a greater academic influence. Scientific research institutions from the USA contributed the most. Strengthening academic exchanges and cooperation is the top priority for future development. Although great progress has been made, further research is needed to understand most of the unknown problems. Combining the above research results, the future development direction of children's nutrition research is put forward:
It has been concluded that the mode of delivery will affect the bacterial community in the intestinal tract of newborns. However, it is still controversial whether the adverse effects will last into childhood or even adulthood. Further research should be carried out in the future, because the results may affect pregnant women's choice of delivery mode.
Food allergies have a significant impact on the morbidity, living quality of children, but there is no effective treatment. The future research should focus on the induction of food allergy in children, the causes of sensitization, clinical manifestations, prognosis, precautions and so on, to solve this scientific problem.
Strengthen the research on the causes, types, prevention and targeted intervention measures of overweight or obesity in children. A large number of studies predict that the number of overweight or obese children will continue to increase in the future. Therefore, we should better understand the source of obesity and control the number and type of obesity children from the source.
Strengths and Limitations
According to our knowledge, this study is the first bibliometric analysis of highly cited articles on child nutrition. Therefore, the study is original. This study not only provide a historical perspective for future research, but also highlight research areas requiring further investigation and development. In addition, before literature search, we read a large number of high-level papers and extracted search terms related to child nutrition. After integration, we formulated the search strategy for this study. Therefore, the search strategy is complete and scientific. Of course, this study also has some shortcomings, the WOS database is considered the most critical data source in bibliometric analysis, so we only searched it ( 70 ), some studies may have been overlooked. Besides, there are many authors in this study, some authors may have the possibility of renaming or having the same author from different institutions. Although we have carefully proofread the process, some mistakes are inevitable.
Author Contributions
JW designed this study. YW, QL, and YC performed search and collected data and wrote the manuscript. YQ rechecked data. BP and QW performed analysis. LG rechecked. JW and GD reviewed the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the National Research Project Development Plan of Gansu Provincial Hospital (19SYPYB-18); Lanzhou Chengguan District Science and Technology Plan Project (2019RCCX0011).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.633525/full#supplementary-material
Abbreviations
HCPs, highly cited papers.
1. Martin CR, Custodio E, Yusuf A, Daniel M, Dominique F, Francois K. Malnutrition and morbidity trends in Somalia between 2007 and 2016: results from 291 cross-sectional surveys. BMJ Open. (2020) 10:e033148. doi: 10.1136/bmjopen-2019-033148
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Bourassa MW, Osendarp SJM, Adu-Afarwuah S, Ahmed S, Ajello C, Bergeron G, et al. Review of the evidence regarding the use of antenatal multiple micronutrient supplementation in low- and middle-income countries. Ann N Y Acad Sci. (2019) 1444:6–21. doi: 10.1111/nyas.14121
3. Zaidi S, Bhutta Z, Hussain SS, Rasanathan K. Multisector governance for nutrition and early childhood development: overlapping agendas and differing progress in Pakistan. BMJ Glob Health. (2018) 10:e000678. doi: 10.1136/bmjgh-2017-000678
4. Cesare MD, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. (2010) 17:212. doi: 10.1186/s12916-019-1449-8
5. Lucas JE, Richter LM, Daelmans B. Care for child development: an intervention in support of responsive caregiving and early child development. Child Care Health Dev. (2018) 44:41–9. doi: 10.1111/cch.12544
6. Ricci G, Tomassoni D, Pirillo I, Sirignano A, Sciotti M, Zaami S, et al. Obesity in the European region: social aspects, epidemiology and preventive strategies. Eur Rev Med Pharmacol Sci. (2018) 22:6930–39. doi: 10.26355/eurrev_201810_16163
7. Bégin F, Aguayo VM. First foods: why improving young children's diets matter. Matern Child Nutr. (2017) 13 (Suppl. 2):e12528. doi: 10.1111/mcn.12528
8. Prentice AM. Stunting in developing countries. World Rev Nutr Diet. (2018) 117:165–75. doi: 10.1159/000484505
9. Shetty P. Nutrition sensitive agriculture to achieve better nutritional outcomes. Eur J Clin Nutr. (2018) 72:1296–9. doi: 10.1038/s41430-018-0208-9
10. Kemps E, Goossens L, Petersen J, Verbeken S, Vervoort L, Braet C. Evidence for enhancing childhood obesity treatment from a dual-process perspective: a systematic literature review. Clin Psychol Rev. (2020) 77:101840. doi: 10.1016/j.cpr.2020.101840
11. Kralick AE, Zemel BS. Evolutionary perspectives on the developing skeleton and implications for lifelong health. Front Endocrinol. (2020) 11:99. doi: 10.3389/fendo.2020.00099
12. Chen XP, Sridevi D. gut microbiome in obesity, metabolic syndrome, and diabetes. Curr Diab Rep. (2018) 18:129. doi: 10.1007/s11892-018-1104-3
13. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. (2010) 375:1969–87. doi: 10.1016/S0140-6736(10)60549-1
14. Pries AM, Filteau S, Ferguson EL. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: a systematic review. Matern Child Nutr. (2019) 15:e12729. doi: 10.1111/mcn.12729
15. Robertson RC, Manges AR, Finlay BB, Prendergast AJ. The human microbiome and child growth - first 1000 days and beyond. Trend Microbiol. (2019) 27:131–47. doi: 10.1016/j.tim.2018.09.008
16. Ma Q, Li Y, Zhang Y. Informetric analysis of highly cited papers in environmental sciences based on essential science indicators. Int J Environ Res Public Health. (2020) 17:3781. doi: 10.3390/ijerph17113781
17. Ring J, Castanov V, McLaren C, Hajjar AEJ, Jeschke MG. Scientific impact and clinical influence: identifying landmark studies in burns. J Burn Care Res . (2020) 41:1240–52. doi: 10.1093/jbcr/iraa083
18. Chen H, Jiang W, Yang Y, Yan Y, Xin M. Global trends of municipal solid waste research from 1997 to 2014 using bibliometric analysis. J Air Waste Manage Assoc. (2015) 65:1161–70. doi: 10.1080/10962247.2015.1083913
19. Chen D, Liu Z, Luo Z, Webber M, Chen J. Bibliometric and visualized analysis of emergy research. Ecol Eng. (2016) 90:285–93. doi: 10.1016/j.ecoleng.2016.01.026
CrossRef Full Text | Google Scholar
20. Chen C M, Dubin R, Kim M C. Orphan drugs and rare diseases: a scientometric review (2000–2014). Expert Opin Orphan Drugs. (2014) 2:709–24. doi: 10.1517/21678707.2014.920251
21. Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci USA. (2004) 101:5303–10. doi: 10.1073/pnas.0307513100
22. Zhang M, Gao M, Yue S, Zheng TL, Gao Z, Ma XY, et al. Global trends and future prospects of food waste research: a bibliometric analysis. Environ Sci Pollut Res. (2018) 25:24600–10. doi: 10.1007/s11356-018-2598-6
23. Ye J, Ding H, Ren J, Xia ZY. The publication trend of neuropathic pain in the world and China: a 20-years bibliometric analysis. J Headache Pain. (2018) 19:110. doi: 10.1186/s10194-018-0941-4
24. Liang YD, Li Y, Zhao J, Wang XY, Zhu HZ, Chen XH, et al. Study of acupuncture for low back pain in recent 20 years: a bibliometric analysis via CiteSpace. J Pain Res. (2018) 10:951–64. doi: 10.2147/JPR.S132808
25. Xie P. Study of international anticancer research trends via coword and document co-citation visualization analysis. Scientometrics. (2015) 105:611–22. doi: 10.1007/s11192-015-1689-0
26. Black RE, Allen LH, Bhutta ZA, Caulfield LE, Onis MD, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
27. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, Onis MD, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
28. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. (2000) 320:1240–63. doi: 10.1136/bmj.320.7244.1240
29. Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
30. Ng M, Fleming T, Robinson M, Blake T, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
31. Ogden CL, Carroll MD, Curtin LR, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. (2006) 295:1549–55. doi: 10.1001/jama.295.13.1549
32. Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. (2015) 219:1–8.
PubMed Abstract | Google Scholar
33. Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. (2006) 444:1027–31. doi: 10.1038/nature05414
34. Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. (2008) 371:340–57. doi: 10.1016/S0140-6736(07)61692-4
35. Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. (2013) 486:222–57. doi: 10.1038/nature11053
36. Perumal N, Gaffey MF, Bassani DG, Roth DE. WHO child growth standards are often incorrectly applied to children born preterm in epidemiologic research. J Nutr. (2015) 145:2429–39. doi: 10.3945/jn.115.214064
37. World Health Organization. Shanghai Consensus on Healthy Cities 2016. Health Promot Int . (2017) 32:603–5. doi: 10.1093/heapro/dax038
38. Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. (2011) 8:98. doi: 10.1186/1479-5868-8-98
39. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. (2012) 307:491–7. doi: 10.1001/jama.2012.39
40. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, 25Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:1911–30. doi: 10.1210/jc.2011-0385
41. Satcher D. From the surgeon general. Sharing an agenda for children: progress and challenges related to the 1990 world summit for Children goals. JAMA. (2001) 286:1305. doi: 10.1016/S0033-3549(04)50028-6
42. Schirnding YV. The world summit on sustainable development: reaffirming the centrality of health. Global Health. (2005) 1:8. doi: 10.1186/1744-8603-1-8
43. Sampson HA. Prevention of atopy and allergic disease: type of infant formula. Nestle Nutr Workshop Ser Pediatr Program. (2012) 57:109–17. doi: 10.1159/000091068
44. Ma Y, Ma S, Chang L, Wang HJ, Ga Q, Ma L, et al. Gut microbiota adaptation to high altitude in indigenous animals. Biochem Biophys Res Commun. (2019) 516:120–6. doi: 10.1016/j.bbrc.2019.05.085
45. Chi X, Gao H, Wu G, Qin W, Song PF, Wang L, et al. Comparison of gut microbiota diversity between wild and captive bharals (Pseudois nayaur). BMC Vet Res. (2019) 15:243. doi: 10.1186/s12917-019-1993-7
46. Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Reddy DN. Role of the normal gut microbiota. World J Gastroenterol. (2015) 21:8787–803. doi: 10.3748/wjg.v21.i29.8787
47. Luo YJ, Chen Y, Liu F, Jiang C, Jiang CH, Gao YQ. Mitochondrial genome sequence of the Tibetan wild ass (Equus kiang). Mitochondrial DNA. (2011) 22:6–8. doi: 10.3109/19401736.2011.588221
48. Schiffrin EJ, Blum S. Interactions between the microbiota and the intestinal mucosa. Eur J Clin Nutr. (2002) 56 (Suppl. 3):S60–4. doi: 10.1038/sj.ejcn.1601489
49. Vrese MD, Schrezenmeir J. Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol. (2008) 111:1–66. doi: 10.1007/10_2008_097
50. Gao XL, Jia RZ, Xie L, Kuang LH, Feng L, Wan C. A study of the correlation between obesity and intestinal flora in school-age children. Sci Rep. (2018) 8:14511. doi: 10.1038/s41598-018-32730-6
51. Guarino A, Wudy A, Basile F, Ruberto E, Buccigrossi V. Composition and roles of intestinal microbiota in children. J Matern Fetal Neonatal Med. (2012)25 (Suppl. 1):63–6. doi: 10.3109/14767058.2012.663231
52. Biasucci G, Rubini M, Riboni S, Morelli L, Bessi E, Retetangos C. Mode of delivery affects the bacterial community in the newborn gut. Early Hum Dev. (2010) 86 (Suppl. 1):13–5. doi: 10.1016/j.earlhumdev.2010.01.004
53. Rutayisire E, Huang K, Liu YH, Tao FB. The mode of delivery affects the diversity and colonization pattern of the gut microbiota during the first year of infants' life: a systematic review. BMC Gastroenterol. (2016) 16:86. doi: 10.1186/s12876-016-0498-0
54. Licari A, Manti S, Marseglia A, Brambilla I, Votto M, Castagnoli R, et al. Food allergies: current and future treatments. Medicina. (2019) 55:120. doi: 10.3390/medicina55050120
55. Patel N, Herbert L, Green TD. The emotional, social, and financial burden of food allergies on children and their families. Allergy Asthma Proc. (2017) 38:88–91. doi: 10.2500/aap.2017.38.4028
56. Martinis MD, Sirufo MM, Viscido A, Ginaldi L. Food allergies and ageing. Int J Mol Sci. (2019) 20:5580. doi: 10.3390/ijms20225580
57. Anagnostou K. Food immunotherapy for children with food allergies: state of the art and science. Curr Opin Pediatr. (2018) 30:798–805. doi: 10.1097/MOP.0000000000000684
58. Chan CJ, Richardo T, Lim RLH. Current trend in immunotherapy for peanut allergy. Int Rev Immunol. (2018) 37:279–90. doi: 10.1080/08830185.2018.1509967
59. Abrams EM, Chan ES, Sicherer S. Peanut allergy: new advances and ongoing controversies. Pediatrics. (2020) 145:e20192102. doi: 10.1542/peds.2019-2102
60. Feng C, Kim JH. Avoidance B. The psychosocial impact of food allergies. Clin Rev Allergy Immunol. (2019) 57:74–82. doi: 10.1007/s12016-018-8708-x
61. Fong AT, Katelaris CH, Wainstein BK. Bullying in Australian children and adolescents with food allergies. Pediatr Allergy Immunol. (2018) 29:740–6. doi: 10.1111/pai.12955
62. Shu SA, Yuen AWT, Woo E, Chu KH, Kwan HS, Yang GX, et al. Microbiota and food allergy. Clin Rev Allergy Immunol. (2019) 57:83–97. doi: 10.1007/s12016-018-8723-y
63. Nance CL, Deniskin R, Diaz VC, Paul M, Anvari S, Anagnostou A. The role of the microbiome in food allergy: a review. Children. (2020) 7:e50. doi: 10.3390/children7060050
64. Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Db Syst Rev. (2019) 7:CD001871. doi: 10.1002/14651858.CD001871.pub4
65. Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA. Child and adolescent obesity: part of a bigger picture. Lancet. (2015) 85:2510–20. doi: 10.1016/S0140-6736(14)61746-3
66. Bass R, Eneli I. Severe childhood obesity: an under-recognised and growing health problem. Postgrad Med J. (2015) 91:639–45. doi: 10.1136/postgradmedj-2014-133033
67. Ells LJ, Rees K, Brown T, Mead E, Al-Khudairy L, Azevedo L, et al. Interventions for treating children and adolescents with overweight and obesity: an overview of cochrane reviews. Int J Obes. (2018) 42:1823–33. doi: 10.1038/s41366-018-0230-y
68. Enright G, Allman-Farinelli M, Redfern J. Effectiveness of family-based behavior change interventions on obesity-related behavior change in children: a realist synthesis. Int J Environ Res Public Health. (2020) 17:4099. doi: 10.3390/ijerph17114099
69. Morales Camacho WJ, Molina Díaz JM, Plata Ortiz S, Plata Ortiz JE, Morales Camacho MA, Patricia Calderón B. Childhood obesity: aetiology, comorbidities, and treatment. Diabetes Metab Res Rev. (2019) 35:e3203. doi: 10.1002/dmrr.3203
70. Gao Y, Ge L, Shi SZ, Sun Y, Liu M, Wang B, et al. Global trends and future prospects of e-waste research: a bibliometric analysis. Environ Sci Pollut Res. (2019) 26:17809–17820. doi: 10.1007/s11356-019-05071-8
Keywords: child nutrition, bibliometric analysis, highly cited papers, intestinal microflora, obesity
Citation: Wang Y, Liu Q, Chen Y, Qian Y, Pan B, Ge L, Wang Q, Ding G and Wang J (2021) Global Trends and Future Prospects of Child Nutrition: A Bibliometric Analysis of Highly Cited Papers. Front. Pediatr. 9:633525. doi: 10.3389/fped.2021.633525
Received: 25 November 2020; Accepted: 16 August 2021; Published: 09 September 2021.
Reviewed by:
Copyright © 2021 Wang, Liu, Chen, Qian, Pan, Ge, Wang, Ding and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiancheng Wang, wangyh2415@126.com
† These authors have contributed equally to this work and share first authorship

CUNY Academic Commons
Hoe does childhood nutrition relate to future health outcomes.
- This Doc can be read by: Anyone
- This Doc can be edited by: The Doc author only
- Comments are visible to: Anyone
- Comments can be posted by: Logged-in Users
- History can be viewed by: Anyone
Janeen Wilson
Professor Benjamin Swett
Writing for Science
25th October 20 21
How does childhood nutrition relate to future health outcomes?
INTRODUCTION
How important is your health as an adult? What changes have you made in your life to better your health status and increase your life expectancy? Cancer, hypertension, diabetes and many other chronic diseases are prematurely killing people. At some point, we must take control of our health to avoid serious health complications. Thanks to a modern advanced medical system, there are ways to medically support people living with chronic diseases. There should be other methods that can prevent or reduce the chances for people to develop a chronic medical condition. The focus in this review would be on childhood nutrition and the effects on future health outcomes. In regards to childhood nutrition there are a few factors that surround it including; the important role parents have concerning their child’s diet, the first foods that is introduced to the child, and the socioeconomic status that determines access to specific foods.
The following articles used in this essay supports the idea that a healthy childhood diet is one method of promoting long term health. This essay also contributes to a bigger mission, that is an evaluation of the effects of a person’s socioeconomic status on their health. All the articles
highlighted the role of parents concerning the nutrition of their child and the importance of their choices of food. These articles share an interest in the importance of childhood nutrition. All the studies promoted healthy eating habits for children and their parents. Obviously, a child can’t be responsible for their own diet. Therefore parents need to know the importance of what they feed their child will affect the child’s health and development in a good or bad way. A low socioeconomic status is the biggest hindrance for families to gain access to good and healthy foods, but there are programs available to provide food assistance.
The role of parents in their child’s nutrition. The purpose of the article “ Parental Self-Efficacy as a Predictor of Children’s Nutrition and the Potential Mediator Effect between the Health Promotion Program “Join the Healthy Boat” and Children’s Nutrition.” was to examine the effects the Parents have concerning the child’s eating habits. A study was done to evaluate the effects of Parent’s self efficacy on fruits and vegetables intake compared to the effects of Parents self efficacy on soft drinks. This study was done in Germany and the participants in the study were kindergarteners and their parents. “The first aim of this study was to show whether parental self-efficacy affects the nutrition behavior of kindergarten children.”( Möhler R, Wartha O, Steinacker JM, Szagun B, Kobel S. ) The article began with the author naming several non communicable diseases and the risk factors of these diseases. A poor diet was mentioned as one of the risk factors for these diseases. “A healthy diet is vital for children…”( Möhler R, Wartha O, Steinacker JM, Szagun B, Kobel S. ) The author continued to explain that a healthy diet is important for children because it contributes to the overall physical health and the cognitive development of the children. The healthy boat organization was implemented to help
increase fruits and vegetables intake in children, while reducing the number of sugary drinks intake. The parents’ self-efficacy on fruits and vegetables intake was a method used to model a healthier eating habit in the presence of the child. This was done hoping that the child will copy the parents behavior. “Parental self-efficacy has been shown to be helpful for a positive parent-child relationship, parental competence, educational quality, and (mental) parental health, as well as child development and adaptability.” ( Möhler R, Wartha O, Steinacker JM, Szagun B, Kobel S. ) The significant findings included that the food the parents eat is usually the food the child would like to eat. Well then, it is vital that all parents expose their child or children to healthy non processed foods. A good practice would be for the child to see their role models making healthy eating habits. This can increase the child’s desire to want healthier foods and decrease the child’s chances of developing future health complications
Introduction to food. “ Impact of a “vegetables first” approach to complementary feeding on later intake and liking of vegetables in infants: a study protocol for a randomised controlled trial” is a study that was done to show that children practice behaviors later on in life that they learnt at an early stage in their life. The goal was to show that children should be fed leafy green vegetables as their first foods instead of bottled baby foods that contain sugar and starch. According to this article, children are encouraged to eat more fruits and veggies, but some children struggle to eat their fruits and veggies. This is why this article recommends that parents should feed their children vegetables as their first foods because it can promote healthier eating habits. “Starting complementary feeding with vegetables, but not with fruits, may promote vegetable acceptance and that liking correlated positively with intake.”( Rapson, J.P., von Hurst, P.R., Hetherington, M.M. et al. ) The leafy green vegetables are recommended for daily
consumption as a healthy meal choice. According to the author, “I ntroducing vegetables at the beginning of complementary feeding may be a promising strategy to promote vegetable intake in children, both immediately and later in life.” The article was good for motivating parents to make smart food choices for their children, but more research is needed because there were no significant findings showing the impact it has on the child’s health. Specimens were collected from each child participant to assess and record their health status. However, the article did not connect the results of veggies as first foods to the health benefits of good childhood nutrition and future health outcomes. However, this study supports the previous article because it highlighted the importance of the parents’ role in providing their children with healthier foods. Also, it is more likely that a child would enjoy eating healthy if it is practiced at an early age and introduced by the parents.
Socioeconomic status affects childhood nutrition . “ Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review” discusses the environment of the child and the effects it has on the child’s diet. Parents have the biggest responsibility to feed their child or children the proper nutritional meals. However, the socioeconomic status of that family sometimes determines how well the family eats. The author was not speaking solely about money, but also background, education, neighborhood and family values. “There is convincing evidence that the family environment is important in influencing the dietary behaviours of young people.”( Pearson, Natalie, et al. ) Just like the healthy boat program article, parents model the behavior and the chances increase for the child to have better eating habits. This article also supports the roles and responsibilities for parents in regards to their children’s diet and health. “Parents believed eating with their children was important in order to model
eating behaviours and also that making food available was likely to influence child’s food consumption.”( Pearson, Natalie, et al. ) The physical factors, sociocultural factors and demographic factors were used to evaluate the correlates of fruits and vegetables intake for children and adolescents. In some studies income levels were shown to have an effect on the amount of fruits and vegetables families have access. Education status was also shown to have an effect on healthier food choices. The parenting style, whether strict or passive, was also a factor used to determine access and intake of fruits and vegetables.
So, how does childhood nutrition affect future health outcomes? According to the articles used in this essay, good childhood nutrition has a positive effect on future health conditions. The foods that people eat are supposed to provide the body with vitamins, minerals and nutrients needed to sustain good health. Then why should people only become health conscious as adults? The idea is to implement and encourage a positive healthy diet in children. The chances increase for that child to continue making healthy food choices as adults to maintain a good health status. All the articles support the idea of children eating more fruits and vegetables daily. The articles also agree that parents have an important role in their children’s diet. The socioeconomic status of a person does affect the diet for the family, especially the children. The realization of socioeconomic status effect on childhood nutrition can be improved with the choices parents make and the environment of the child. It would be amazing to end childhood hunger across the world. However, in the United States of America there are still too many families living in a food shortage crisis. There are still parents who are not concerned about their child’s nutrition and how it connects to their overall health. There is
a need for more outreach programs and public health officials to assist families across the U.S. Using the right medium, the goal of the outreach should be to educate and motivate the parents and children on the connections between childhood nutrition and their future health. The articles didn’t elaborate on the associations between childhood nutrition and future health outcomes, but they certainly share an interest in the importance of fruits and vegetables intake in children’s diet.
Works Cited
Rapson, J.P., von Hurst, P.R., Hetherington, M.M. et al. Impact of a “vegetables first” approach to complementary feeding on later intake and liking of vegetables in infants: a study protocol for a randomised controlled trial. Trials 22, 488 (2021). https://doi.org/10.1186/s13063-021-05374-7
Pearson, Natalie, et al. “Family Correlates of Fruit and Vegetable Consumption in Children and Adolescents: a Systematic Review.” Public Health Nutrition , vol. 12, no. 2, 2009, pp. 267–283., doi:10.1017/S1368980008002589.
Möhler R, Wartha O, Steinacker JM, Szagun B, Kobel S. Parental Self-Efficacy as a Predictor of Children’s Nutrition and the Potential Mediator Effect between the Health Promotion Program “Join the Healthy Boat” and Children’s Nutrition. International Journal of Environmental Research and Public Health. 2020 Dec;17(24). DOI: 10.3390/ijerph17249463. PMID: 33348737; PMCID: PMC7766743 .
Tags: childhood nutrition healthy future outcomes
Need help with the Commons?
Email us at [email protected] so we can respond to your questions and requests. Please email from your CUNY email address if possible. Or visit our help site for more information:

- Terms of Service
- Accessibility
- Creative Commons (CC) license unless otherwise noted

- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Nutrition and health...
Nutrition and health in women, children, and adolescent girls
Read the full collection.
- Related content
- Peer review
- Francesco Branca , director 1 ,
- Ellen Piwoz , senior program officer 2 ,
- Werner Schultink , chief of nutrition 3 ,
- Lucy Martinez Sullivan , executive director 4
- 1 Department of Nutrition for Health and Development, World Health Organization, Avenue Appia 20, 1211 Geneva 27, Switzerland
- 2 Bill and Melinda Gates Foundation, USA
- 3 Unicef, New York, USA
- 4 1000 Days, Washington, DC, USA
- Correspondence to: Francesco Branca brancaf{at}who.int
Urgent action is needed to tackle malnutrition in all forms and to help nutrition unlock the potential of investment in the health of women, children, and adolescents, say Francesco Branca and colleagues
Every year the lives of around 50 million children are put at risk because they are dangerously thin from acute undernutrition, while the long term health of more than 40 million children is threatened because they are overweight. Two billion people suffer from vitamin and mineral deficiencies, but overweight and obesity are key contributors to the non-communicable diseases that account for almost two thirds (63%) of adult deaths globally. These different forms of malnutrition—undernutrition, overweight and obesity, and micronutrient deficiencies—now affect people across the same communities and harm people of all ages. (Unless otherwise cited, the figures given are WHO estimates.)
Improving nutrition therefore presents a key opportunity to improve health. As the UN secretary general launches his second Global Strategy for Women’s, Children’s and Adolescents’ Health in September 2015 a strengthened focus on nutrition is warranted, with special attention to the first 1000 days of life (from pregnancy to the child’s second birthday), pregnant and lactating women, women of reproductive age, and adolescent girls.
This paper highlights nutrition related priority actions to improve the health of women, children, and adolescent girls. It is based on existing policy guidance issued by the World Health Assembly in the form of resolutions or targets; guidelines from the World Health Organization; or the outcome documents of the Second International Conference on Nutrition (ICN2).
The vast majority of the recommended actions proposed in this paper were agreed by the 162 member states attending the ICN2 in Rome in November 2014. 1 These recommendations were developed by the secretariats of the Food and Agriculture Organization of the United Nations and WHO on the basis of current evidence and were subject to extensive consultation. An information note on the ICN2 provides more background information on the recommended actions. 2
Some additional recommendations, specific to women’s, children’s, or adolescents’ nutrition, are based on WHO guidance. Where such a recommendation does not exist, emerging evidence reviewed by the authors is cited.
Problems associated with poor nutrition
Good nutrition is fundamental for optimal health and growth. Through its effect on health and cognitive development it is also vital for academic performance and productivity, and therefore for healthy economies and socioeconomic development.
Health effects of malnutrition
The consequences of malnutrition could hardly be more serious: around 45% of child deaths in 2011 were due to malnutrition (including fetal growth restriction, suboptimal breast feeding, stunting, wasting, and deficiencies of vitamin A and zinc). In 2013 the growth of around 161 million children aged under 5 was stunted by chronic undernutrition, leading to hampered cognitive and physical development, poor health, and an increased risk of degenerative diseases. 3 In the same year 51 million children were wasted (having low weight for height) because of acute undernutrition; severe wasting increases the risk of morbidity, particularly from infectious diseases such as diarrhoea, pneumonia, and measles, and is responsible for as many as two million deaths a year. 4
Meanwhile, deficiencies of vitamin A and zinc cause many deaths (157 000 and 116 000 child deaths, respectively, in 2011), 5 and iodine and iron deficiencies, along with stunting, contribute to children not achieving their full potential. Iron and calcium deficiencies increase the risks associated with pregnancy, particularly maternal mortality. 5
At the same time overweight and obesity in children and adults have been increasing rapidly in all regions of the world, and half a billion adults were affected by obesity in 2010. Dietary risk factors, together with inadequate physical activity, were responsible for 10% of the global burden of disease and disability in 2010. 6
Socioeconomic impact of malnutrition
Malnutrition contributes to an estimated 200 million children failing to attain their full development potential. Stunting is estimated to reduce a country’s gross domestic product by as much as 3%, 7 and eliminating anaemia could increase adult productivity by 5-17%. 8
Every $1 (£0.64; €0.91) invested in tackling undernutrition is estimated to yield around $18 in return—the median benefit:cost ratio from a study modelling the effect of preventing one third of stunting in children up to age 3 in 17 high burden countries. 9 More specifically, a recent study of the benefit:cost ratio of a package of nutrition interventions aimed at averting stunting in 15 countries found that benefits outweighed costs by as much as 42:1, depending on the existing economic and nutritional situation. 10
Box : What do we mean by malnutrition?
Malnutrition: nutritional disorders in all of their forms (including imbalances in energy intake, macronutrient and micronutrient deficiencies, and unhealthy dietary patterns). Conventionally, the emphasis has been on inadequacy, but malnutrition also applies to excess and imbalanced intakes.
Overweight: a situation caused by an excessive, unbalanced intake of energy or nutritional substances (and often combined with a sedentary lifestyle).
Stunting: low height for age (more than two standard deviations below the WHO child growth standard median for children under 5). Stunting is defined by WHO as a public health problem when 20% or more of the population are affected.
Undernutrition: a situation in which the body’s energy and nutrient requirements are not met because of under-consumption or the impaired absorption and use of nutrients. Undernutrition commonly refers to a deficit in energy intake, but it can also refer to deficiencies of macronutrients and micronutrients, and it can be either acute or chronic.
Wasting: low weight for height (more than two standard deviations below the WHO child growth standard median for children under 5). Wasting becomes a public health problem when 5% or more of the population are affected.
Box : Nutrition in recent global initiatives and commitments
Global Strategy for Women’s and Children’s Health : the UN secretary general’s strategy, put into action by the global Every Woman Every Child movement, clearly set out the need to tackle nutrition in young children. 11
Global nutrition targets for 2025: countries are working towards six global targets agreed at the 65th World Health Assembly in 2012 (table 1) ⇓ .
Global Action Plan for the Prevention and Control of Non-communicable Diseases 2013-20 : includes targets to reduce salt intake by a third and to halt the increase in obesity among adolescents and adults.
Second International Conference on Nutrition: in November 2014 the world’s leaders committed to eradicating hunger and preventing all forms of malnutrition worldwide. 12
What progress has been made in tackling malnutrition?
Better understanding of the challenges and solutions.
The root causes of malnutrition and the factors leading to it are complex and multidimensional. Poverty, underdevelopment, and low socioeconomic status are major contributors, along with other social determinants. Current food systems struggle to provide adequate, safe, and diversified foods. The reasons include constraints on access to land, water, and other resources—often aggravated by environmental damage—along with unsustainable production and consumption patterns, food losses and waste, and unequal distribution and access. Malnutrition is often aggravated by poor feeding and care practices for infants and young children, as well as poor sanitation and hygiene. A lack of access to education, quality health systems, and safe drinking water can also have a negative effect, along with infectious disease and the ingestion of harmful contaminants.
In recent years progress has been made in developing knowledge and understanding of the magnitude and scope of nutritional challenges, the increasing contribution of non-communicable diseases, and the complex web of factors that can influence nutrition.
A greater understanding has developed regarding the importance of nutrition at different stages of the life course and the effect of poor nutrition across generations (fig 1 ⇓ ). An intergenerational cycle of malnutrition exists whereby a woman who has anaemia, for example, is likely to have a baby with a reduced birth weight. Low birthweight babies are more likely to be wasted or stunted and to have a higher risk of morbidity and mortality and of developing non-communicable diseases later in life. Conversely, if the mother is obese when she starts her pregnancy she is also at increased risk of complications during pregnancy or delivery, which could result in premature delivery—and, therefore, a low birth weight for her baby. Alternatively, if she carries the baby to full term, her baby is more likely to have a higher birth weight and a higher risk of child and adolescent obesity.
- Download figure
- Open in new tab
- Download powerpoint
Fig Nutrition through the life course—proposed causal links 13
The past two decades have also seen a major shift in understanding of the policy responses required to improve nutrition and promote healthy diets. It is now clear that an enabling environment plays a key role and that policies that change aspects of the food environment are required (such as what foods are available, what levels of fat, sugar, or salt they contain, or how much they cost), as well as nutrition education and information.
Similarly, there is now much greater awareness that effective responses need to come from beyond the health sector and that this must involve other sectors, such as those related to water and sanitation, education, trade, and social protection. Crucially, a radical transformation is needed so that food systems can ensure that everyone has access to a sustainable, balanced, and healthy diet.
Progress towards global nutrition targets
Significant progress has been made in reducing hunger and undernutrition in the past two decades: the percentage of people in developing regions experiencing hunger fell from 24% in 1990-92 to 14% in 2011-13. 14 The 2014 Global Nutrition Report showed, however, that the world is not on track to meet any of the six World Health Assembly nutrition targets (table 1 ⇓ ).
Findings of the 2014 Global Nutrition Report 17
- View inline
What are the priorities for improving nutrition?
Improving women’s, children’s, and adolescents’ nutrition requires a range of policies, programmes, and interventions at different stages of life. And, since we know that malnourished women give birth to malnourished children, it is possible to take action to improve nutrition across generations (fig 2 ⇓ ). Specific recommendations and actions to help put them into practice are shown in tables 2 to 4. ⇓ ⇓ ⇓
Fig Improving nutrition throughout the life course 15
Recommended actions to improve adolescents’ nutrition
Recommended actions to improve child nutrition
Recommended actions to improve women’s nutrition
Actions to improve adolescent girls’ nutrition
Adolescent girls should be at the heart of a life course approach—a young adolescent girl is still a child, but often she will soon become a mother. Adolescent pregnancy is associated with higher risk of maternal mortality and morbidity, stillbirths, neonatal deaths, preterm births, and low birth weight. In addition to actions to prevent adolescent pregnancy and encourage pregnancy spacing, efforts are required to ensure that pregnant and lactating teenage mothers are adequately nourished.
Actions to improve child nutrition
The first 1000 days of life (from pregnancy to the child’s second birthday) present an important window of opportunity to improve child nutrition. The key pillar of any strategy to improve this—in addition to good maternal nutrition and health—is optimal feeding and care for infants and young children. Exclusive breast feeding (defined as the practice of giving an infant only breast milk for the first six months of life, with no other food or water), in particular, has the single largest potential effect on child mortality of any preventive intervention. Timely and adequate complementary feeding, with particular attention to vitamin and mineral content and the nutrient density of foods, is urgently needed.
Actions to improve women’s nutrition
The health and nutrition statuses of women and children are intimately linked. Improving the health of women and children, therefore, begins with ensuring the health and nutritional status of women throughout all stages of life, and it continues with women being providers for their children and families. Thus, a key priority is female empowerment and women’s full and equal access to, and control over, social protection and resources such as income, land, water, and technology. Direct multisectoral actions to tackle critical women’s nutritional challenges, such as iron deficiency anaemia, need to be rolled out on a larger scale to achieve universal coverage.
Improving nutrition across the life course
These targeted recommendations must be supported by a raft of nutrition interventions throughout the life course (see the ICN2 Framework for Action for the full range of recommended actions). Policies are needed, for example, to transform food systems and strengthen health systems. Universal access to functioning and resilient health systems and the scaled-up delivery of interventions can improve nutrition. Governments and international organisations also have a role in developing clear guidelines on healthy diets.
What needs to happen now?
If we want to improve the health of women, children, and adolescents, action to invest in nutrition is needed now. We know what needs to be done—as explained by the recommended actions in tables 2 to 4 ⇑ ⇑ ⇑ —and the clear global commitments to action.
We now need to implement these commitments and ensure the resources to do so (the Addis Ababa Action Agenda refers to the need to scale up efforts to end hunger and malnutrition at paragraph 13 and the need to strengthen national health systems at paragraph 77). 16 In a nutshell, actions are needed to improve the quality of diets; protect, promote, and support breast feeding; ensure that everyone has access to essential nutrition actions; provide adequate water and sanitation; and provide information and education.
To achieve these aims governments and society must join forces and make nutrition a priority. Governments, health services, the food and agriculture industries, schools and universities, and community leaders—along with many others—must work together in a coordinated and coherent way.
The potential human, societal, and economic gains from turning these commitments into action are substantial, and the costs of inaction are high. The time is right to tackle malnutrition in all forms at all ages and to break its intergenerational cycle.
Key messages
Investment in nutrition is crucial to future efforts to improve the health of women, children, and adolescents; the potential human, societal, and economic gains from such investment are substantial.
Clear global commitments to action are in place, backed by targets to measure progress. All contributors, across government and society, must come together to turn these commitments into action.
Specific actions are needed to improve the quality of the diet; to protect, promote, and support breast feeding; to ensure that everyone has access to essential nutrition actions; to provide adequate water and sanitation; and to provide information and education.
Cite this as: BMJ 2015;351:h4173
The authors thank Karen McColl, Lina Mahy, Rebecca Olson, and Shelly Sundberg for their contributions to this paper.
Competing interests: We have read and understood BMJ’s policy on declaration of interests and have no relevant interests to declare.
The authors alone are responsible for the views expressed in this article, which does not necessarily represent the views, decisions, or policies of WHO or the institutions with which the authors are affiliated.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an open access article distributed under the terms of the Creative Commons Attribution IGO License ( https://creativecommons.org/licenses/by-nc/3.0/igo/ ), which permits use, distribution, and reproduction for non-commercial purposes in any medium, provided the original work is properly cited. In any reproduction of this article there should not be any suggestion that WHO or this article endorse any specific organisation or products. The use of the WHO logo is not permitted. This notice should be preserved along with the article's original URL.
- ↵ Second International Conference on Nutrition. Conference outcome document: framework for action. Oct 2014. www.fao.org/3/a-mm215e.pdf .
- ↵ Second International Conference on Nutrition. Information note on the framework for action. 4 Nov 2014. www.fao.org/fileadmin/user_upload/faoweb/ICN2/documents/InfoNote-e.pdf .
- ↵ World Health Organization. WHA global nutrition targets 2025: stunting policy brief. 2014. www.who.int/nutrition/topics/globaltargets_stunting_policybrief.pdf .
- ↵ World Health Organization. WHA global nutrition targets 2025: wasting policy brief. 2014. www.who.int/nutrition/topics/globaltargets_wasting_policybrief.pdf .
- ↵ Black RE, Victora CG, Walker SP, et al; Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low income and middle income countries. Lancet 2013 ; 382 : 427 -51. OpenUrl CrossRef PubMed Web of Science
- ↵ Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012 ;380;2224-60.
- ↵ International Bank for Reconstruction and Development, World Bank. Repositioning nutrition as central to development: a strategy for large scale action. 2006. https://openknowledge.worldbank.org/handle/10986/7409 .
- ↵ World Health Organization. Comprehensive implementation plan on maternal, infant and young child nutrition. 2014. http://apps.who.int/iris/bitstream/10665/113048/1/WHO_NMH_NHD_14.1_eng.pdf?ua=1 .
- ↵ Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S. The economic rationale for investing in stunting reduction. GCC Working Paper Series 2013 ;13-08.
- ↵ Hoddinott J, Horton S. Stunting as a sustainable development goal. SCN News 2015 ; 41 : 59 . www.unscn.org/files/Publications/SCN_News/SCNNEWS41_web_low_res.pdf . OpenUrl
- ↵ United Nations Secretary General. Global strategy for women’s and children’s health. Sept 2010. www.who.int/pmnch/topics/maternal/20100914_gswch_en.pdf .
- ↵ Second International Conference on Nutrition. Conference outcome document: Rome declaration on nutrition. Oct 2014. www.fao.org/3/a-ml542e.pdf .
- ↵ World Health Organization. Global nutrition targets 2025: childhood overweight policy brief (WHO/NMH/NHD/14.6). 2014. www.who.int/nutrition/topics/globaltargets_overweight_policybrief.pdf .
- ↵ United Nations. The millennium development goals report 2014. 2014. www.un.org/millenniumgoals/2014%20MDG%20report/MDG%202014%20English%20web.pdf .
- ↵ World Health Organization. Essential nutrition actions: improving maternal, newborn, infant and young child health and nutrition. 2013. http://apps.who.int/iris/bitstream/10665/84409/1/9789241505550_eng.pdf .
- ↵ United Nations. The Addis Ababa action agenda of the Third International Conference on Financing for Development. July 2015. www.un.org/esa/ffd/ffd3/wp-content/uploads/sites/2/2015/07/Addis-Ababa-Action-Agenda-Draft-Outcome-Document-7-July-2015.pdf .
- International Food Policy Research Institute. Global nutrition report 2014: actions and accountability to accelerate the world’s progress on nutrition. 2014. http://cdm15738.contentdm.oclc.org/utils/getfile/collection/p15738coll2/id/128484/filename/128695.pdf .
- World Health Organization. Healthy diet. Fact sheet no 394. May 2015. www.who.int/mediacentre/factsheets/fs394/en/ .
- World Health Organization. Global recommendations on physical activity for health. 2010. www.who.int/dietphysicalactivity/publications/9789241599979/en/ .
- World Health Organization. Nutrition counselling for adolescents and adults with HIV/AIDS. WHO e-Library of Evidence for Nutrition Actions (eLENA). July 2015. www.who.int/elena/titles/nutrition_hiv/en/ .
- World Health Organization. Guideline: calcium supplementation in pregnant women. 2013. www.who.int/nutrition/publications/micronutrients/guidelines/calcium_supplementation/en/ .

7 Reasons Why Childhood Nutrition Is so Important
C hildhood nutrition has been a focus in our society for some time now, as we’re learning more and more how important it is for children to learn healthy eating habits at a young age. We also know that thousands, if not, millions of children aren’t getting the proper nutrition that they need.
There are seven major reasons why childhood nutrition is so important. Proper nutrition in children…
- Supports the immune system
- Establishes good eating habits
- Provides essential vitamins and minerals
- Ensures proper physical growth and development
- Promotes brain development
- Helps establish sleep patterns
- Affects moods
Childhood nutrition is essential for everyday life. Read on for more information regarding why nutrition is important for your child and to dig deeper into the seven reasons why it is important.
Article Topics
Why is childhood nutrition important.
Children need proper nutrition in the form of healthy, balanced meals each and every day. A child’s meal should consist of fruits, vegetables, dairy, protein, and grains. Each of these foods contains the vitamins and minerals needed to help maintain a healthy life. A child receiving all the nutrients will live a more healthy lifestyle.
Some delivery companies offer a healthy kids menu delivery so you can save your time while your loved youngsters are still getting right foods.
7 Reasons Why Childhood Nutrition Is So Important
There are many reasons why providing a child with proper nutrition is important. Some are more beneficial than others. However, these are more of a general collection of why childhood nutrition is so important.
1. Proper Nutrition Strengthens Immunity
Staying healthy is important. Not just with exercise but also with proper nutrition. Providing a child with proper nutrition can be beneficial for their overall health. Immunity to physically being more healthy can help determine if a child is getting the correct nutrition amount.
Children are around germs every day. For the immune system to be able to provide immunity, the body needs vitamin C and D, zinc, selenium, iron, and protein. The best and natural places to find these are in a food.
This means that a child that has healthy daily nutrition can produce the immunity cells and the antibodies that are needed for any illness or germs that the body needs.
Some foods that are full of immunity support:
- Strawberries
- Red meats such as beef
- Fortified foods such as milk, oatmeal, and tofu
- Meats: chicken, pork, beef
- Pumpkin seeds
Maintaining a good nutritional diet not only provides immunity support but also for overall health. Children need to eat good nutritious meals that are needed for all basic body functions. Having good nutrients in a child’s life will improve their quantity of life and provide relief from the body, attacking itself to gather up all the nutrients that are needed.

2. Promotes Lifelong Healthy Eating Habits
Healthy eating habits ensure that your child can maintain the correct bodyweight for their body types. In some cases, your child may have to be put on an eating schedule or given in certain quantities.
Healthy eating habits can make it easier for your child to adjust to the new eating plan. Some ways to help with proper or good eating habits can be the following:
- Water place of juice or soda. This can cut back on the sugar that is already a part of your child’s nutrition plan.
- Eating slow can help send signals to your brain that you are getting full. It also helps with preventing overeating that can cause tiredness after meals, as well as gastric problems from eating too much too quickly.
- Stick to the serving sizes. Sticking to serving sizes can do wonders to a child’s eating habits. Instead of a whole bowl of mac-n- cheese and six(6) slices of pizza, doing moderations and following the serving sizes, and eating slowly, can increase the feeling full effect and be used as a guide to what is considered healthy.
- Eat fruits and vegetables during meals but also as snacks in place of chips or cakes. Including fruits in snack time can greatly benefit your child’s healthy by replacing good sugars with bad sugars such as those included in soda or snack cakes.
3. Provides Essential Vitamins and Minerals
Parents give their children vitamins in the shape of animals every day, but most don’t realize that proper nutrition gives their children a wide range of the essential vitamins and minerals they need.
Getting the proper nutrition for your child is important. Vitamins and minerals not only help with growth but also helps with bone growth, battle infections, helps our organs such as our eyes to see.
There are a variety of foods that can provide the vitamins and minerals we need. Here are a couple of foods that carry the essential vitamins and minerals needed:
- Nuts and seeds
- Green vegetables
- Dairy products
- Fruits and other vegetables
Here is a complete list of vitamins and minerals and what foods to find them in.
4. Eating the Right Foods Encourages Physical Growth
From infancy to early adulthood, proper nutrition creates many doors for growth, from developing good bones and muscles to maintaining the proper blood supply and organ functions.
If a child is not able to obtain the nutrients that are needed for growth, there are risks. A child that is malnourished will not be able to achieve the physical growth that they are capable of having. This can result in lowered height, weight, and physical performance.
Malnourishment also can contribute to feeling tired more easily. This energy loss can cause different things, from lack of exercise to having problems focusing.
When a child is not obtaining the nutrients needed for energy, the child may seem more relaxed and not interested in games or outdoor play. This can increase the risks of muscle problems due to lack of use. Not using body functions responsible for movement can cause muscles to degenerate or weaken.

5. Childhood Nutrition Enhances Brain Development
From early on, a child needs a certain amount of nutrition for development. When a baby is growing, the proper nutrients aid in the development of brain and organ function. However, some parents are unaware that proper nutrition needs to start during pregnancy.
Throughout childhood, the brain constantly changes and gathers new information. A child will obtain new information daily. This new information is gotten from electronics, parents or other family, friends, and teachers.
A child that lacks proper nutrition can be more relaxed in class or having trouble concentrating. Difficulty concentration can be caused by malnutrition itself or due to the child being hungry. If the child is hungry, they may feel sick or even just be thinking of food itself.
There are many ways to eat healthy and healthy eating habits. It is important to start when your children are smaller and start eating actual food outside of baby or pureed foods.
6. Facilitates Healthy Sleep Patterns
Throughout this article, discussions on moods and child development have been pointed out. What most parents don’t realize is how important nutrition is for sleep. Giving your child the proper nutrition can help regulate sleep patterns. Sleep is a huge part of growing and being able to function throughout the day.
As said before, a child can have a hard time falling asleep due to feeling hungry or lack of food. However, they can also have these problems with too much food.
That’s why making sure your child has had the meals or nutrition they need an hour before bed is always a good idea. It help them run off that excess energy that food can give children, as well as make sure that they have a full belly for a good restful sleep.
Good eating habits also can help with relation to proper nutrition. Giving your child healthy meals and healthy snacks and drinks can prevent a higher sugar intake as well as caffeine intakes that are present in sodas, chocolate, coffee, and teas.

7. Nutrition Directly Affects Children's Moods and Behavior
Your child’s mood is directly affected by food. We all are aware of the phrase “hangry” that people use daily. This is typically meaning that a person is so hungry that they have become or were angry or grumpy.
Usually, when this person that is “hangry” gets the food, they are happy and back to themselves. This can relate to children as well. Parents of toddlers especially can relate to this. Toddlers are still learning how to express themselves. In these cases, sometimes a toddler, or child, may not realize that they are hungry and become irritable or angry.
Usually, after some time and a lot of patience, the parent or guardian will offer a snack or a meal to the child. After the child starts to eat, the irritability goes away.
Poor nutrition or too much nutrition can cause moods other than irritability to occur. Too little or too much food can also cause depression or hyperactivity. Depression can be caused by many different factors other than nutrition, of course.
However, a child that may suffer from malnutrition can become depressed or develop anxiety. Children, in this case, can withdraw into themselves. Feeling hungry or ashamed that they do not have as much food or are considered poor in some cases by others. This can directly affect their mood as well as social interactions and concentration in school.
(Another wonderful thing to teach kids is the art of yoga! It is great for their brain, body, and soul! Learn more about kids yoga teacher training in that amazing article!)
Does Nutrition Affect Learning?
Students tend to focus more after breakfast, lunch, and snack time. This not only allows them to take a small break from learning and for the kids to relax their mind but also provides them with a well-needed boost for energy.
Energy is important to help with tiredness as well as feeling hungry. When a child feels hungry, that’s all they will think about. This can make distractions increase and learning decrease. It can cause the child to be timid and embarrassed among peers because of the social interactions needed for learning.
How Does Nutrition Affect The Growth And Development Of A Child?
Growth and development for a child are based on the nutritional needs each child requires. If a child obtains too much nutrition, or overeating/drinking, it can cause health problems such as obesity, binge eating disorders, and depression or sadness.
However, if a child lacks proper nutrition or is malnourished, they can have stunted growth and developmental delays. This, in turn, can cause things like failure to thrive to occur. This not only affects growth but also psychological development.
Final Thoughts
Proper nutrition is always important for infants, children, teenagers, and young adults to have. Having the nutritional needs met for each child can help them to achieve their full potential in cognitive development as well as physical development.
It is always great as a parent to do healthy eating habits as well as getting proper exercise for themselves as well as helping their children to develop these traits too.
7 Essential Skills for Resilience
Resilience defined: what is it and how do you build it.

Luke Ocean is a writer, self-proclaimed bio-hacker, wellness advocate and yoga expert. Luke grew up on a small ranch in Montana and enlisted in the Navy to study and become a cryptologist. He later graduated from the US Naval Academy with a Minor in Mandarin and a Bachelor's of Science for General Engineering and a Major of English Literature. Luke's interests and career span multiple industries and various disciplines. Luke resides in San Antonio and is a Certified Yoga Instructor, a student of Zen Buddhism, practitioner of Holistic Psychology and has completed his CYT-200 and is studying for his 300-hour yoga teacher training.
Privacy Overview
- Integrative Health
- Mental Health
- Yoga Philosophy
- Positive Psychology
- Personal Development
- Yoga Teacher Training
- Yoga Practice
- Martial Arts
- Relationships
- Spirituality
- Entrepreneurship
- Professional Development
- Energy Healing
- Sound Healing
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: World Health Organization; 2009.

Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals.
Session 1 the importance of infant and young child feeding and recommended practices, 1.1. growth, health and development.
Adequate nutrition during infancy and early childhood is essential to ensure the growth, health, and development of children to their full potential. Poor nutrition increases the risk of illness, and is responsible, directly or indirectly, for one third of the estimated 9.5 million deaths that occurred in 2006 in children less than 5 years of age ( 1 , 2 ) ( Figure 1 ). Inappropriate nutrition can also lead to childhood obesity which is an increasing public health problem in many countries.
Major causes of death in neonates and children under five in the world, 2004. Sources: World Health organization. The global burden of disease: 2004 update . Geneva, World Health organization, 2008; Black R et al. Maternal and child undernutrition: global (more...)
Early nutritional deficits are also linked to long-term impairment in growth and health. Malnutrition during the first 2 years of life causes stunting, leading to the adult being several centimetres shorter than his or her potential height ( 3 ). There is evidence that adults who were malnourished in early childhood have impaired intellectual performance ( 4 ). They may also have reduced capacity for physical work ( 5 , 6 ). If women were malnourished as children, their reproductive capacity is affected, their infants may have lower birth weight, and they have more complicated deliveries ( 7 ). When many children in a population are malnourished, it has implications for national development. The overall functional consequences of malnutrition are thus immense.
The first two years of life provide a critical window of opportunity for ensuring children's appropriate growth and development through optimal feeding ( 8 ). Based on evidence of the effectiveness of interventions, achievement of universal coverage of optimal breastfeeding could prevent 13% of deaths occurring in children less than 5 years of age globally, while appropriate complementary feeding practices would result in an additional 6% reduction in under-five mortality ( 9 ).
1.2. The Global Strategy for infant and young child feeding
In 2002, the World Health Organization and UNICEF adopted the Global Strategy for infant and young child feeding ( 10 ). The strategy was developed to revitalise world attention to the impact that feeding practices have on the nutritional status, growth and development, health, and survival of infants and young children (see also Session 9 ). This Model Chapter summarizes essential knowledge that every health professional should have in order to carry out the crucial role of protecting, promoting and supporting appropriate infant and young child feeding in accordance with the principles of the Global Strategy .
1.3. Recommended infant and young child feeding practices
WHO and UNICEF's global recommendations for optimal infant feeding as set out in the Global Strategy are:
- exclusive breastfeeding for 6 months (180 days) ( 11 );
- nutritionally adequate and safe complementary feeding starting from the age of 6 months with continued breastfeeding up to 2 years of age or beyond.
Exclusive breastfeeding means that an infant receives only breast milk from his or her mother or a wet nurse, or expressed breast milk, and no other liquids or solids, not even water, with the exception of oral rehydration solution, drops or syrups consisting of vitamins, minerals supplements or medicines ( 12 ).
Complementary feeding is defined as the process starting when breast milk is no longer sufficient to meet the nutritional requirements of infants, and therefore other foods and liquids are needed, along with breast milk. The target range for complementary feeding is generally taken to be 6 to 23 months of age, 1 even though breastfeeding may continue beyond two years ( 13 ).
These recommendations may be adapted according to the needs of infants and young children in exceptionally difficult circumstances, such as pre-term or low-birth-weight infants, severely malnourished children, and in emergency situations (see Session 6 ). Specific recommendations apply to infants born to HIV-infected mothers.
1.4. Current status of infant and young child feeding globally
Poor breastfeeding and complementary feeding practices are widespread. Worldwide, it is estimated that only 34.8% of infants are exclusively breastfed for the first 6 months of life, the majority receiving some other food or fluid in the early months ( 14 ). Complementary foods are often introduced too early or too late and are often nutritionally inadequate and unsafe.
Data from 64 countries covering 69% of births in the developing world suggest that there have been improvements in this situation. Between 1996 and 2006 the rate of exclusive breastfeeding for the first 6 months of life increased from 33% to 37%. Significant increases were made in sub-Saharan Africa, where rates increased from 22% to 30%; and Europe, with rates increasing from 10% to 19% ( Figure 2 ). In Latin America and the Caribbean, excluding Brazil and Mexico, the percentage of infants exclusively breastfed increased from 30% in around 1996 to 45% in around 2006 ( 15 ).
Trends in exclusive breastfeeding rates (1996–2006). Source: UNICEF. Progress for children: a world fit for children. Statistical Review, Number 6. new York, UNICEF, 2007.
1.5. Evidence for recommended feeding practices
Breastfeeding.
Breastfeeding confers short-term and long-term benefits on both child and mother ( 16 ), including helping to protect children against a variety of acute and chronic disorders. The long-term disadvantages of not breastfeeding are increasingly recognized as important ( 17 , 18 ).
Reviews of studies from developing countries show that infants who are not breastfed are 6 ( 19 ) to 10 times ( 20 ) more likely to die in the first months of life than infants who are breastfed. Diarrhoea ( 21 ) and pneumonia ( 22 ) are more common and more severe in children who are artificially fed, and are responsible for many of these deaths. Diarrhoeal illness is also more common in artificially-fed infants even in situations with adequate hygiene, as in Belarus ( 23 ) and Scotland ( 24 ). Other acute infections, including otitis media ( 25 ), Haemophilus influenzae meningitis ( 26 ), and urinary tract infection ( 27 ), are less common and less severe in breastfed infants.
Artificially-fed children have an increased risk of long-term diseases with an immunological basis, including asthma and other atopic conditions ( 28 , 29 ), type 1 diabetes ( 30 ), celiac disease ( 31 ), ulcerative colitis and Crohn disease ( 32 ). Artificial feeding is also associated with a greater risk of childhood leukaemia ( 33 ).
Several studies suggest that obesity in later childhood and adolescence is less common among breastfed children, and that there is a dose response effect, with a longer duration of breastfeeding associated with a lower risk ( 34 , 35 ). The effect may be less clear in populations where some children are undernourished ( 36 ). A growing body of evidence links artificial feeding with risks to cardiovascular health, including increased blood pressure ( 37 ), altered blood cholesterol levels ( 38 ) and atherosclerosis in later adulthood ( 39 ).
Regarding intelligence, a meta-analysis of 20 studies ( 40 ) showed scores of cognitive function on average 3.2 points higher among children who were breastfed compared with those who were formula fed. The difference was greater (by 5.18 points) among those children who were born with low birth weight. Increased duration of breastfeeding has been associated with greater intelligence in late childhood ( 41 ) and adulthood ( 42 ), which may affect the individual's ability to contribute to society.
For the mother, breastfeeding also has both short- and long-term benefits. The risk of postpartum haemorrhage may be reduced by breastfeeding immediately after delivery ( 43 ), and there is increasing evidence that the risk of breast ( 44 ) and ovarian ( 45 ) cancer is less among women who breastfed.
Exclusive breastfeeding for 6 months
The advantages of exclusive breastfeeding compared to partial breastfeeding were recognised in 1984, when a review of available studies found that the risk of death from diarrhoea of partially breastfed infants 0–6 months of age was 8.6 times the risk for exclusively breastfed children. For those who received no breast milk the risk was 25 times that of those who were exclusively breastfed ( 46 ). A study in Brazil in 1987 found that compared with exclusive breastfeeding, partial breastfeeding was associated with 4.2 times the risk of death, while no breastfeeding had 14.2 times the risk ( 47 ). More recently, a study in Dhaka, Bangladesh found that deaths from diarrhoea and pneumonia could be reduced by one third if infants were exclusively instead of partially breastfed for the first 4 months of life ( 48 ). Exclusive breastfeeding for 6 months has been found to reduce the risk of diarrhoea ( 49 ) and respiratory illness ( 50 ) compared with exclusive breastfeeding for 3 and 4 months respectively.
If the breastfeeding technique is satisfactory, exclusive breastfeeding for the first 6 months of life meets the energy and nutrient needs of the vast majority of infants ( 51 ). No other foods or fluids are necessary. Several studies have shown that healthy infants do not need additional water during the first 6 months if they are exclusively breastfed, even in a hot climate. Breast milk itself is 88% water, and is enough to satisfy a baby's thirst ( 52 ). Extra fluids displace breast milk, and do not increase overall intake ( 53 ). However, water and teas are commonly given to infants, often starting in the first week of life. This practice has been associated with a two-fold increased risk of diarrhoea ( 54 ).
For the mother, exclusive breastfeeding can delay the return of fertility ( 55 ), and accelerate recovery of pre-pregnancy weight ( 56 ). Mothers who breastfeed exclusively and frequently have less than a 2% risk of becoming pregnant in the first 6 months postpartum, provided that they still have amenorrhoea (see Session 8.4.1 ).
Complementary feeding from 6 months
From the age of 6 months, an infant's need for energy and nutrients starts to exceed what is provided by breast milk, and complementary feeding becomes necessary to fill the energy and nutrient gap ( 57 ). If complementary foods are not introduced at this age or if they are given inappropriately, an infant's growth may falter. In many countries, the period of complementary feeding from 6–23 months is the time of peak incidence of growth faltering, micronutrient deficiencies and infectious illnesses ( 58 ).
Even after complementary foods have been introduced, breastfeeding remains a critical source of nutrients for the young infant and child. It provides about one half of an infant's energy needs up to the age of one year, and up to one third during the second year of life. Breast milk continues to supply higher quality nutrients than complementary foods, and also protective factors. It is therefore recommended that breastfeeding on demand continues with adequate complementary feeding up to 2 years or beyond ( 13 ).
Complementary foods need to be nutritionally-adequate, safe, and appropriately fed in order to meet the young child's energy and nutrient needs. However, complementary feeding is often fraught with problems, with foods being too dilute, not fed often enough or in too small amounts, or replacing breast milk while being of an inferior quality. Both food and feeding practices influence the quality of complementary feeding, and mothers and families need support to practise good complementary feeding ( 13 ).
When describing age ranges, a child 6–23 months has completed 6 months but has an age less than 2 years.
All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob ). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: tni.ohw@snoissimrep ).
- Cite this Page Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: World Health Organization; 2009. SESSION 1, The importance of infant and young child feeding and recommended practices.
- PDF version of this title (2.2M)
In this Page
- Growth, health and development
- The Global Strategy for infant and young child feeding
- Recommended infant and young child feeding practices
- Current status of infant and young child feeding globally
- Evidence for recommended feeding practices
Other titles in this collection
- WHO Guidelines Approved by the Guidelines Review Committee
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- The importance of infant and young child feeding and recommended practices - Inf... The importance of infant and young child feeding and recommended practices - Infant and Young Child Feeding
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Health, Safety and Nutrition for the Young Child Essay
Healthy food ensures the growth of children, their physical and psychological development. It should be balanced and meet all the needs of the child taking into account his age as well as individual peculiarities. Unfortunately, sometimes it is difficult to make children eat healthy food. In this regard, this paper examines how parents are struggling for the healthy food, tips they could apply, and essential nutrients that their body needs.
During the first two years of life, children are developing very quickly. The child begins life as a helpless newborn baby completely depending on his parents. After that, he turns into a person trying to show his parents that he can be very independent. Toddlers could already understand a lot and begin experimenting with words frequently saying the word “no”. By the age of two, the child forms his inclination and rejection of things, especially in relation to food. Therefore, it seems appropriate to consider healthy toddlers’ healthy feeding.
First of all, the majority of parents make the following mistake: they pamper their child by means of food. In other words, the child is eating only what he wants. At that time, it does not matter for parents whether it is useful or harmful. As a result, when the child acquires some digestive problems, it becomes challenging to get him switch to healthy food and limit his favorite sweets. A variety of chronic diseases of the digestive system appears in that age (Brown 277). Moreover, junk food influences the overall physical development and reduced learning ability. Therefore, parents should pay the increased attention to the quantity, quality, composition, and diet of their children.
Second, parents should try to get the child to eat together with the whole family. It is not always easy to implement, in particular, if the child is active and wayward. However, if parents show the child the example of helpfulness of the healthy nutrition, they do a lot of good as it contributes to child’s awareness at the very beginning of his life. Best of all, if eating with family would be a good tradition. It is the time when everyone gathers to eat and talk, a time when everyone could speak and be heard.
Family dinnertime should not leave an unpleasant residue. During the family meal, the child would see what his parents eat and how they act to adopt their demeanor. Children accustomed eating healthy food get a huge benefit. Healthy food provides them with the building blocks of the body, through which they will grow. Proper nutrition helps children to maintain harmony and good health, strengthen their immune system, reduce the risk of different diseases, and even improve their ability to learn (Marotz 516). Therefore, preparation and consumption of healthy food should be an integral part of every family.
What if you want your child’s food to be healthy, but the child refuses to eat it? In order to resolve this problem, one could try various tips. For example, tell your child that his favorite cartoon character always eats healthy food, that is why he is such a strong, courageous, and brave. If the child is old enough and does not believe your story, you can talk to him as with adult carefully explaining why it is important to eat the appropriate food. In the case your daughter refuses to eat worrying about the overweight, make it clear that the proper and healthy eating contributes to the perfect body.
As a matter of fact, it is parents of the toddler who control his feeding as they decide what products should be an essential part of his everyday menu. In order to attract his attention, they might use different strategies. For example, they could garnish healthy food with berries, funny faces made of that food, and your toddler would undoubtedly eat the whole portion. Thus, it is necessary that the dish should be not only tasty and healthy, but also colorfully decorated. Moreover, children like to view products. Hence, you could hang a picture of “healthy food pyramid” in your kitchen. It would describe in detail, what food should make up the daily diet of the toddler. Probably, it would stimulate the child to eat something that is useful.
In addition, parents should not encourage their child to eat more than he wants to. There is no need to feed him forcibly even if you think that he eats little. He eats as much as he needs. Wanting to feed the child to eat properly it must be remembered that the pressure could lead to opposite results (Leung, Marchand and Sauve 455). Consequently, child’s taste preferences should be respected and taken into account.
Tastes of children of this age are not completely predictable. Year-old child, who devoured boiled potatoes with an appetite last week could inexplicably withdraw it this week. Additionally, some children refuse to eat any vegetables for a long period of time. In that case, parents should continue to feed their child with vegetables he likes remembering about fruits, grain products, and lentils that supply the deficiency of vitamins and minerals (“Feeding Toddlers” par. 7). During this period, it is necessary to choose a flexible strategy of communication.
It goes without saying that parents should avoid fast food. Even if you want to eat hamburgers or French fries on weekends or vacation, try not to tempt children. Instead, make sure that the child could always easily take the food that you consider useful for him. Here are a few examples of how to implement it in practice. A tray or dish with fresh or cooked vegetables should always be stored in the refrigerator on child’s eye level. In addition, during breakfast, lunch or dinner, it should be on the table.
It is also very important to point out the fact that planning child’s diet should take into account certain features of his body and behavior. The main difference between children and adults nutrition is the growth of his body. For example, it is obvious that the toddler needs more protein than the adult does.
Products for nutrition of children should be fresh, high quality, delicious, and highly nutritious. As children get older, their food becomes more diverse, denser products replace semi-liquid and liquid food. The original product processing, in particular, removal of defective parts thorough washing and cleaning influences the quality and taste of ready meals. Failure to comply with rules for processing products might contain bacteria that cause food poisoning. In its turn, it might create some hostility to the healthy food.
Speaking of essential nutrients of the child, it seems important to mention milk, fish, meat, fruits, and vegetables. Milk is a valuable product because it saturates the body with animal protein; it is a source of fats, salts, and vitamins. Meat and fish contain complete proteins, vitamins, trace elements along with phosphorus compounds necessary for proper development of the central nervous system. Fish contains very valuable fish oil. Besides, the healthy diet of children making their first steps should include a variety of fresh vegetables, fruits, beans, and whole grains. It is important to include in their diet some sources of vitamin B12 (such as cereals or soy milk, for example) (“Feeding Toddlers” par. 10). Besides, calcium-rich large-leafy green vegetables and beans fortified with calcium are also essential.
In order to structure the paper, it seems appropriate to consider characteristics of adequate children nutrition in relation to their body and activities.
- High mobility. In contrast to adults, children are very mobile. The high mobility of the body of the child helps to normalize his or her metabolism. The limitation of movements of the child would provoke insufficient secretion of growth hormone and, as a result, the development gap. Carbohydrates are the main supplier of energy for muscles and other organs (Samela 14). The more the child is active, the more energy is consumed by his organism. Various cereals, vegetables, honey, and milk contains the essential carbohydrates.
- Eating sweets. Due to the high metabolism intensity, children could absorb more sweets than adults without much harm. However, there should be some restrictions. Although, sweet products of natural origin such as dates or raisins are very useful for the child. The child might appeal some sweet vegetables such as carrots or baked beets as well.
- Cholesterol . As a major component of the membrane that surrounds the cells of the whole organism, it is extremely important for the health of the child. The child grows up, and his organism produces plenty of new cells. It should also be mentioned that fat cells formed during the first years of life influence the perspective possibility of overweight. Therefore, adult’s health in many respects is connected with nutrition in childhood.
- Water . Because of their high mobility, children loss noticeable amount of water, so they cannot be restricted to drink. Nevertheless, parents should not compensate the lack of water by means of sweet compotes or juices, as it leads to the appetite suppression.
- Regulatory mechanisms . It is the most important feature of child food. In the body of the child, there are perfectly functioning regulatory mechanisms that control power consumption. However, if there is an abundance of spiced, fried, fatty, and sweet dishes, the physiological function might be disrupted.
- General development. This feature requires an adequate nutrition, too. The lack of adequate nutrition might cause “poor mental health and lower IQ in children” (Parletta par. 3). It is important for the child to receive sufficient unsaturated fatty acids many of which are found in olive, linseed, and sunflower oil.
Thus, the healthy nutrition of children requires taking into account features of the body of the child as well as the knowledge of some rules and principles of healthy eating. It should be stressed that providing a healthy diet for children, parents ensure the all-round development, strengthen the immune system of the child, and protect him from diseases generally improving his quality of life.
Works Cited
Brown, Judith E. Nutrition through the Life Cycle . 5th ed. New York: Cengage Learning, 2013. Print.
“Feeding Toddlers.” Parenting and Child Health . n.d.
Leung, Alexander, Valérie Marchand, and Reginald Sauve. “The ‘picky Eater’: The Toddler or Preschooler Who Does Not Eat.” Paediatr Child Health 17.8 (2012): 455-57. Print.
Marotz, Lynn R. Health, Safety, and Nutrition for the Young Child . 9th ed. New York: Cengage Learning, 2015. Print.
Parletta, Natalie. “ Health Check: How to Get Kids to Eat Healthy Food. ” The Conversation . Web.
Samela, Kate. Give Peas a Chance: A Foolproof Guide to Feeding Your Picky Toddler , New York: Cengage Learning, 2013. Print.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, April 12). Health, Safety and Nutrition for the Young Child. https://ivypanda.com/essays/health-safety-and-nutrition-for-the-young-child/
"Health, Safety and Nutrition for the Young Child." IvyPanda , 12 Apr. 2024, ivypanda.com/essays/health-safety-and-nutrition-for-the-young-child/.
IvyPanda . (2024) 'Health, Safety and Nutrition for the Young Child'. 12 April.
IvyPanda . 2024. "Health, Safety and Nutrition for the Young Child." April 12, 2024. https://ivypanda.com/essays/health-safety-and-nutrition-for-the-young-child/.
1. IvyPanda . "Health, Safety and Nutrition for the Young Child." April 12, 2024. https://ivypanda.com/essays/health-safety-and-nutrition-for-the-young-child/.
Bibliography
IvyPanda . "Health, Safety and Nutrition for the Young Child." April 12, 2024. https://ivypanda.com/essays/health-safety-and-nutrition-for-the-young-child/.
- Uber Eats App: Success Stories
- Nutritional Practices for Infants and Toddlers
- “What the World Eats” Book by Menzel and D’Aluisio
- "Ali: Fear Eats the Soul" Film Cinematography
- Importance of Nutrition During the Infancy and Toddler-Hood Period
- Observing the Motor Skill Development of a Toddler
- Teaching in Action for Toddlers
- Description of a Toddler’s Room
- Toddlers and Tiaras: Have Parents Gone Too Far
- Monitoring Toddlers and Technology
- Withdrawing Products with High Sugar Contents
- Healthy Food: Lesson Plan
- Hispanic Patients and Dietary Approaches (DASH)
- Obesity in the US Population
- Childhood Obesity Policy Actions

IMAGES
VIDEO
COMMENTS
Globally, one in three children aged 6-23 months is eating the minimum diverse diet needed for healthy growth and development. Young children's diets are frequently comprised of grains - with little fruit, vegetables, eggs, dairy, fish or meat. Many are increasingly being fed sugary drinks and packaged snacks high in salt, sugar and fat.
Parents should be aware of changes in their child's eating patterns and make family dinners a priority at least once or twice a week. Like calories, calcium requirements are higher. Calcium is more important than ever during the tween and teen years because the majority of bone mass is built during this time. Encouraging kids to have milk, milk ...
It is crucial to begin practicing healthy eating habits early on in your child's life. One of the most important conversations to have with your child is the power of healthy eating. The Benefits of Healthy Eating. As children grow and develop, they need important nutrients to be strong and healthy. Some of the benefits of healthy eating include:
Importance of Nutrition During the Infancy and Toddler-Hood Period Essay. As Woody (2007, pp.6-7) argues, occurrences in a child's early stages of life are primary determinants of developments in a child's later stages of life. That is, because of the developments and refinement of abilities associated with childhood, occurrences in a child ...
Effectiveness of Integrated Early Child Development and Nutrition Interventions. In the last 2 years, systematic reviews and meta-analyses have examined the effectiveness of ECD and nutrition interventions separately and integrated on early child development outcomes.Aboud et al. reviewed interventions conducted since 2000 and found that psychosocial-stimulation interventions (n = 21) had a ...
Throughout their early childhood, it's important to monitor your child's nutrient intake for the sake of their later performance. For instance, breastfeeding appears to lead to higher IQ, while iron deficiency correlates with reduced cognition and achievement at school age. More obviously to the layman, since under-nourished children get ...
The present Special Issue of Nutrients aims to host scientific articles contributing to enriching the knowledge in the field of nutritional habits and intervention in childhood. The role of the diet in the achievement and maintenance of a healthy status is well recognized. This is especially important in the pediatric age since children need an adequate intake of energy and nutrients for ...
This is especially important since children are at an increased risk for eating disorders (EDs) [26,27,28]. Emotional eating, i.e., eating in response to emotional cues rather than physiological hunger, has been associated with developing obesity and eating disorders in childhood [29,30,31,32]. Food is often used as an emotional regulator ...
Nutrition in Middle Childhood and Adolescence. 112 UNICEF's Programmatic Guidance for Nutrition in Middle Childhood and Adolescence includes specific priorities of nutritious foods, healthy food environments in schools and beyond, micronutrient supplementation and deworming, nutrition education in school curricula, and healthy dietary ...
Child nutrition has always been a global concern. This study performed visual analysis of 1,398 child nutrition highly cited papers (HCPs) from 2009 to 2019. The purpose of the study was to evaluate and present the performances of authors, journals, countries, institutions, top cited papers; to explore the hot topics, prospects, and to propose the future research directions on child nutrition.
This essay also contributes to a bigger mission, that is an evaluation of the effects of a person's socioeconomic status on their health. ... These articles share an interest in the importance of childhood nutrition. All the studies promoted healthy eating habits for children and their parents. Obviously, a child can't be responsible for ...
Actions to improve child nutrition. The first 1000 days of life (from pregnancy to the child's second birthday) present an important window of opportunity to improve child nutrition. The key pillar of any strategy to improve this—in addition to good maternal nutrition and health—is optimal feeding and care for infants and young children.
The study included 896 children: 53% were male, 9% had high nutritional risk, and 17% were vulnerable on the EDI. A 1-SD increase in NutriSTEP total score was associated with 1.54 times increased odds of being vulnerable on the EDI among children in year 2 of kindergarten ( P = 0.001).
One consequence has been the absence of an integrated perspective on adolescent growth and development, and the role that nutrition plays. Through late childhood and early adolescence, nutrition has a formative role in the timing and pattern of puberty, with consequences for adult height, muscle, and fat mass accrual, as well as risk of non ...
There are seven major reasons why childhood nutrition is so important. Proper nutrition in children…. Supports the immune system. Establishes good eating habits. Provides essential vitamins and minerals. Ensures proper physical growth and development. Promotes brain development.
The purpose of this special issue is to highlight important contributions from previously published articles in Maternal & Child Nutrition to the field of nutrition and ECD. The collection of papers presented in this special issue collectively indicates that although nutrition‐specific interventions are essential for child development, they ...
Nutrition is very important during childhood. The reason for this is that children require more energy than adults. The macronutrients and micronutrients that the body needs are absorbed according to the body size. The smaller the body size the more nutrients the body will need. Children also have a higher growth rate.
The Importance a Good Earlychildhood Nutrition Essay. As a parent, you want to provide the best nourishment available to ensure your toddler's early physical growth. Early childhood nutrition is crucial for development in the first two years, not only to protect health and support growth, but it can also introduce and reinforce beneficial ...
1784 Words. 8 Pages. Open Document. Child Nutrition. Fueling Growth. Children come in a variety of shapes and sizes. Their genetic blueprints determine how fast and how big they will grow. Some children are destined to grow slowly while others make rapid leaps in development. Genetic, environmental, hormonal, nutritional and behavioral factors ...
Proper nutrition is crucial to consider when you care for kids, as it protects against malnourishment, maintains a healthy immune system, prevents obesity and reduces the risk of chronic disease. Some important nutrients for children include: Calcium strengthens bones. Found in milk, yoghurt and seeds. Protein builds muscles.
Adequate nutrition during infancy and early childhood is essential to ensure the growth, health, and development of children to their full potential. Poor nutrition increases the risk of illness, and is responsible, directly or indirectly, for one third of the estimated 9.5 million deaths that occurred in 2006 in children less than 5 years of age (1,2) (Figure 1). Inappropriate nutrition can ...
The child might appeal some sweet vegetables such as carrots or baked beets as well. Cholesterol. As a major component of the membrane that surrounds the cells of the whole organism, it is extremely important for the health of the child. The child grows up, and his organism produces plenty of new cells.
The right nutrition makes our immune system strong. We will not get sick because we have a strong immunity against different types of diseases or illness. Our body height and weight is also affected by the nutrition. If we do not have the right nutrition the growth in our height and weight gets hampered.