- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
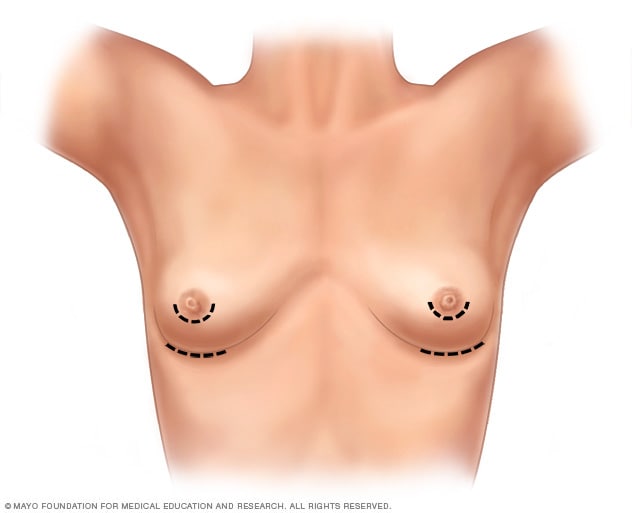
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
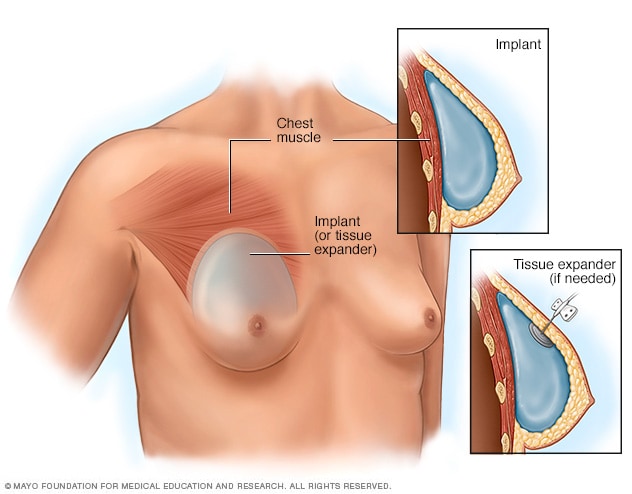
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
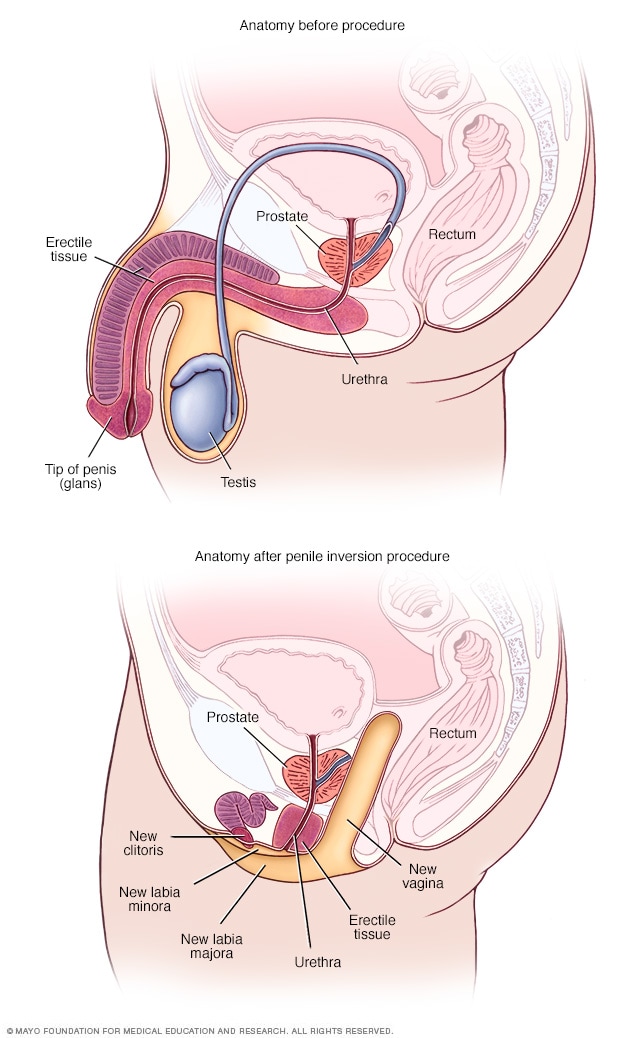
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
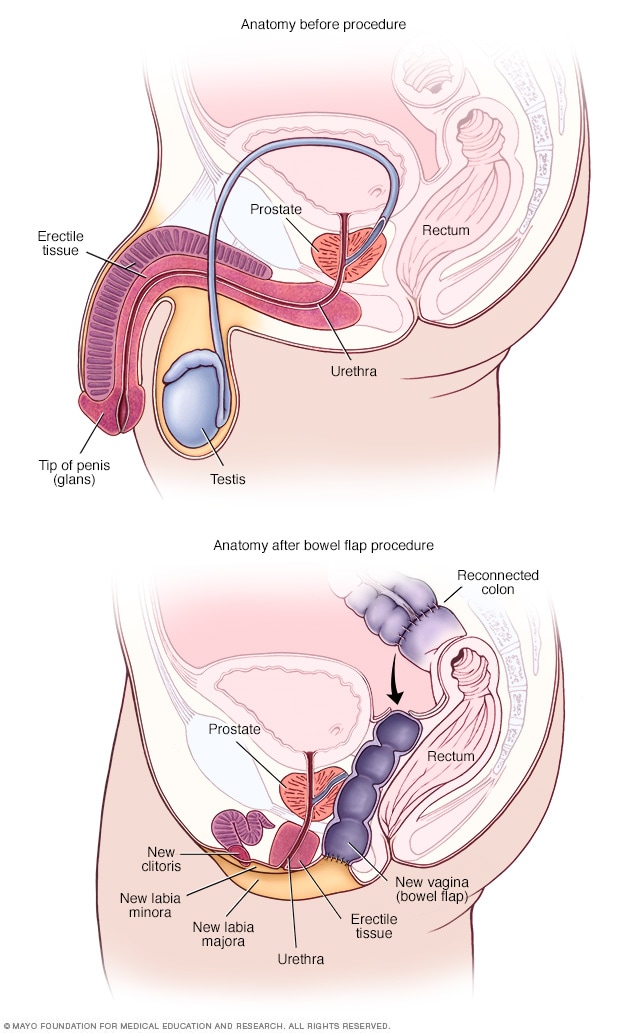
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.

Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Transgender Health Program
- Enter keyword Search
Gender-Affirming Surgery
OHSU surgeons are leaders in gender-diverse care. We provide specialized services tailored to the needs and goals of each patient. We offer:
- Specialists who do hundreds of surgeries a year.
- Plastic surgeons, urologists and other specialists who are leading experts in bottom surgery, top surgery and other gender-affirming options.
- Vocal surgery with a highly trained ear, nose and throat doctor.
- Peer volunteers who can provide support during visits.
- Welcoming care for every patient, every gender and every journey.
Our surgical services
We offer many gender-affirming surgery options for transgender and nonbinary patients, including options within the following types. We also welcome you to request a procedure that isn’t listed on our pages.
Top surgery:
- Gender-affirming mastectomy
- Gender-affirming breast augmentation
Bottom surgery:
- Phalloplasty and metoidioplasty , including vagina-preserving options
- Vaginoplasty and vulvoplasty , including penile-preserving options
Hysterectomy
Nullification surgery, oophorectomy, orchiectomy.
Bottom surgery options also include:
- Scrotectomy
- Scrotoplasty
- Urethroplasty
- Vaginectomy
Additional gender-affirming options:
- Adam’s apple surgery
Vocal surgery
Face and body surgery, preparing for surgery.
Please see our patient guide page to learn about:
- Steps to surgery
- WPATH standards of care
- The letter of support needed for some surgeries
For patients
Request services.
Please fill out an online form:
- I am seeking services for myself.
- I am seeking services for someone else.
Other questions and concerns
Contact us at:
- 503-494-7970
- [email protected]
Refer a patient
- Please complete our Request for Transgender Health Services referral form and fax with relevant medical records to 503-346-6854 .
- Learn more on our For Health Care Professionals page.
At OHSU, our gynecologic surgeon, Dr. Lishiana Shaffer, specializes in hysterectomies (uterus and cervix removal; often combined with oophorectomy, or ovary removal) for gender-diverse patients. She does more than 150 a year.
We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Some patients choose hysterectomy to:
- More closely align their bodies with their gender identity.
- With ovary removal, to remove a main source of the hormone estrogen.
- To end pain caused by testosterone therapy that shrinks the uterus.
- To end the need for some gynecologic exams, such Pap smears.
Preparation: We usually recommend a year of hormone therapy first, to shrink the uterus. We don’t require a year of social transition.
Most often, we use a minimally invasive laparoscope and small incisions in the belly. We usually recommend removing fallopian tubes as well, to greatly reduce the risk of ovarian cancer.
Most patients spend one night in the hospital. Recovery typically takes about two weeks. You’re encouraged to walk during that time but to avoid heavy lifting or strenuous exercise.
Hysterectomy is usually safe, and we have a low rate of complications. Risks can include blood clots, infection and scar tissue. Because of a possible link between hysterectomy and higher risk of cardiovascular disease, your doctors may recommend regular tests.
Removing the uterus also ends the ability to carry a child. OHSU fertility experts offer options such as egg freezing before treatment, and connecting patients with a surrogacy service.
OHSU offers nullification surgery to create a gender-neutral look in the groin area.
Nullification surgery may include:
- Removing the penis (penectomy)
- Removing the testicles (orchiectomy)
- Reducing or removing the scrotum (scrotectomy)
- Shortening the urethra
- Removing the uterus (hysterectomy)
- Removing the vagina (vaginectomy)
The procedure takes several hours. Patients can expect to spend one to two nights in the hospital. Recovery typically takes six to eight weeks. Patients are asked to limit walking and to stick to light to moderate activity for four weeks. They should wait three months before bicycling or strenuous activity.
Nullification surgery cannot be reversed. Risks can include:
- Changes in sensation
- Dissatisfaction with the final look
- Healing problems
Removing the penis and testicles or the uterus also affects the ability to conceive a child. OHSU fertility experts offer options such as freezing eggs and connecting patients with a surrogacy service.
Having a gynecologic surgeon remove one or both ovaries is often done at the same time as a hysterectomy. We do nearly all these surgeries with a minimally invasive laparoscope and small incisions in the belly.
Most patients spend one night in the hospital and return to their regular routine in about two weeks.
The ovaries produce estrogen, which helps prevent bone loss and the thickening of arteries. After removal, a patient should be monitored long-term for the risk of osteoporosis and cardiovascular disease.
We encourage patients to keep at least one ovary to preserve fertility without egg freezing. This also preserves some hormone production, which can avoid early menopause.
At OHSU, expert urologists do orchiectomies (testicle removal). Patients may choose this option:
- To remove the body’s source of testosterone
- As part of a vaginoplasty or vulvoplasty (surgeries that create a vagina and/or vulva)
- To relieve dysphoria (some patients choose only this surgery)
Removing the testicles usually means a patient can stop taking a testosterone blocker. Patients may also be able to lower estrogen therapy.
The surgeon makes an incision in the scrotum. The testicles and the spermatic cord, which supplies blood, are removed. Scrotal skin is removed only if the patient specifically requests it. The skin is used if the patient plans a vaginoplasty or vulvoplasty.
You will probably go home the same day. Patients can typically resume normal activities in a week or two.
Reducing testosterone production may increase the risk of bone loss and cardiovascular disease, so we recommend regular tests. Without prior fertility treatment, orchiectomy also ends the ability to produce children. Serious risks are uncommon but include bleeding, infection, nerve damage and scarring.
Adam’s apple reduction (laryngochrondoplasty)
Dr. Joshua Schindler, an ear, nose and throat doctor who does Adam’s apple and vocal surgeries, completed his training at Johns Hopkins University.
Laryngochrondoplasty is also known as Adam’s apple reduction or a tracheal shave (though the trachea, or windpipe, is not affected).
A surgeon removes thyroid cartilage at the front of the throat to give your neck a smoother appearance. This procedure can often be combined with facial surgery.
Thin incision: At OHSU, this procedure can be done by an ear, nose and throat doctor (otolaryngologist) with detailed knowledge of the neck’s anatomy. The surgeon uses a thin incision, tucked into a neck line or fold. It can also be done by one of our plastic surgeons, typically with other facial surgery.
In an office or an operating room: Our team can do a laryngochrondoplasty in either setting, which may limit a patient’s out-of-pocket expenses.
OHSU also offers Adams’ apple enhancement surgery.
Many patients find that hormone therapy and speech therapy help them achieve a voice that reflects their identity. For others, vocal surgery can be added to raise the voice’s pitch.
Voice therapy: Patients have voice and communication therapy before we consider vocal surgery. Your surgeon and your speech therapist will assess your voice with tests such as videostroboscopy (allowing us to see how your vocal cords work) and acoustic voice analysis.
Effective surgery: We use a surgery called a Wendler glottoplasty. It’s done through the mouth under general anesthesia. The surgeon creates a small controlled scar between the two vocal cords, shortening them to increase tension and raise pitch. Unlike techniques that can lose effectiveness over time, this surgery offers permanent results.
Hormone therapy can bring out desired traits, but it can’t change the underlying structure or remove hair follicles. Our highly trained surgeons and other specialists offer options. Patients usually go home the same day or spend one night in a private room.
Face options:
- Browlift (done with the forehead)
- Cheek augmentation
- Chin surgery (genioplasty), including reductive, implants or bone-cut options
- Eyelid surgery
- Face-lift, neck lift
- Forehead lengthening
- Forehead reduction, including Type 3 sinus setback and orbital remodeling
- Hairline advancement (done with the forehead)
- Jawline contouring
- Lip lift and/or augmentation
- Lipofilling (transferring fat using liposuction and filling)
- Nose job (rhinoplasty)
Body options:
Hormone treatment may not result in fat distribution consistent with your gender. We offer liposuction and fat grafting to reshape areas of the body.
