Cushing’s Syndrome Case Study (60 min)
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Ms. Smith Is a 33 year old female who presents to her primary care provider for General muscle weakness and low back pain. She reports that this pain has been going on for about 3 months and the weakness has been getting worse over the last 2 weeks and she has been more fatigued with basic physical exertion. She reports getting “steroid injections” in her back previously, but they “didn’t last long at all”.
What further history questions should be asked of Ms. Smith?
- What medical history does she have?
- What medications does she take on a regular basis?
- What has she tried in the past for her back pain? What has worked?
- Is the pain associated with any specific activity or time of day? What makes it worse or makes it better?
Ms. Smith has a history of Type II Diabetes and Asthma, and has been taking inhaled corticosteroids for the past 6 years. She also reports reports having irregular menstrual cycles for the past 2 years accompanied by unexplained weight gain in her abdomen. Her previous provider told her she might have Polycystic Ovarian Syndrome.
What initial nursing assessments should be performed?
- Heart and lung sounds
- Assess skin condition
- Assess strength x 4 extremities
- Abdominal assessment
Ms. Smith’s Vital Signs were as follows:
Temp 98.8°F
The nurse notes purple/pink stretch marks on arms, abdomen, and thighs. Ms. Smith has multiple cuts and bruises on her arms. When asked how she got them, she says “my skin is just so thin these days”. She is obese with noticeable fatty deposits in the midsection and upper back.
What diagnostic testing do you anticipate for Ms. Smith?
- Complete Metabolic Panel – test electrolytes and kidney/liver function
- Hormone levels – estrogen, progesterone, testosterone, cortisol
- Complete Blood Count to evaluate immune system
- ESR and/or CRP to assess for inflammation
Ms. Smith is sent home with a pain reliever for her back pain while the laboratory results are processed. An ultrasound of her kidneys and ovaries is ordered, pending scheduling an appointment for next week. Two days later, lab values result and show the following:
Cortisol 28 mg/dL (H)
Glucose 265 mg/dL
K 3.3 mEq/L
Na 148 mg/dL
Ca 7.8 mg/dL
Testosterone levels elevated
Which finding(s) is/are concerning and need to be reported to the provider? Why?
- Hypokalemia and hypernatremia can be detrimental to the cardiovascular and neurological system and need to be addressed quickly
- The elevated blood sugar and elevated cortisol levels combined with the clinical findings suggest possible Cushing’s Syndrome
What do you believe is going on physiologically with Ms. Smith?
- Ms. Smith likely has developed Cushing’s Syndrome due to chronic use of corticosteroids.
- This causes the Adrenal Glands to over-respond, secreting excess glucocorticoids (hence the hyperglycemia and fat distribution), excess mineralocorticoids (hence the electrolyte abnormalities), and excess androgens (hence the elevated testosterone levels).
- The hypocalcemia can also cause osteoporosis or soft, fragile bones
The provider notifies Ms. Smith that she needs to be seen again ASAP for further diagnostic testing to rule out any cardiac abnormalities. He tells her to stop taking her inhaled corticosteroid and prescribes a different rescue inhaler for her asthma. He also tells her she needs to begin taking some supplements, including calcium and potassium
Why does Ms. Smith need to have her heart checked out? What test would they do?
- The hypokalemia can cause electrical abnormalities or arrhythmias
- She needs an EKG
Why does Ms. Smith need calcium supplements? What caused her hypocalcemia? How might this contribute to her back pain?
- Cushing’s Syndrome causes hypocalcemia
- Hypocalcemia can cause calcium to be pulled from the bones to compensate – this creates an osteoporotic situation
- This may be why her back hurts – it is taking the weight of her body onto the soft, porous bones
Why does Ms. Smith have to stop taking her inhaler?
- The chronic use of the inhaled corticosteroids is the likely culprit – she should refer to her PCP or pulmonologist for other options to manage her asthma
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Endocrine Abstracts
- Issues/Conferences
- Our Services
SFEBES2017 ePoster Presentations Neuroendocrinology and Pituitary (23 abstracts)
Cushing's disease - Case report
Katy chisenga.
University of Cambridge, Cambridge, UK.
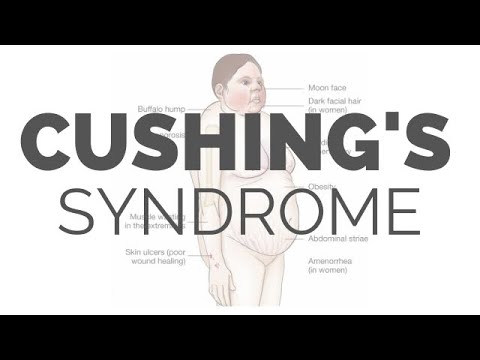
Introduction: Cushing’s syndrome is caused by an extended exposure to increased levels of endogenous or exogenous glucocorticoids. It is a syndrome that can be extremely challenging to diagnose as many symptoms and signs are also indications of other disease processes.
Case: A 76 year old man presented to hospital with a six month history of immobility and falls. Proximal muscle weakness was also noted. The patient then underwent a period of rehabilitation.
The patient had a history of type 2 diabetes mellitus, hypertension, congestive cardiac failure, combined B12 and folate deficiency, longterm suprapubic catheter due to urinary retention, urinary tract infections and a myocardial infarction.
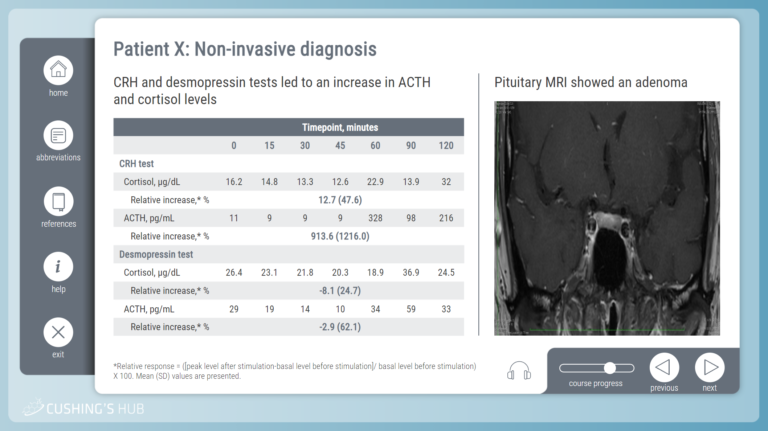
A first set of investigations revealed a 24 hr urinary free cortisol of 206 nmol/24 hr (0–146/24 hr), an overnight dexamethasone suppression test of 1588 nmol/L and a low dose dexamethasone suppression test of 1131 nmol/L (<50 nmol/L). The ACTH level was revealed to be 139 pmol/L and an MRI scan revealed a left-sided pituitary adenoma. As such, a diagnosis of ACTH-dependent Cushing’s disease was made.
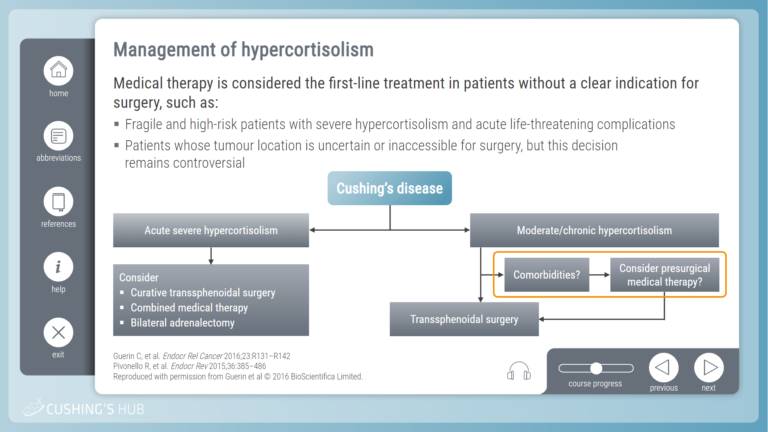
The patient was initially managed with metyrapone with a view to transphenoidal surgery. However the patient developed shortness of breath and worsening peripheral oedema. A chest X ray and echocardiogram revealed left ventricular failure and reduced systolic function, respectively. For this reason it was decided to medically optimize his congestive cardiac failure and hypercortisolaemia as an inpatient with progression to neurosurgery if he were to stabilize.
Discussion: Cushing’s disease is a rarity that can be difficult to diagnose due to the significant number of varied pathologies indicated by its signs and symptoms. This is an interesting case of Cushing’s disease as the levels of cortisol measured in the patient were incredibly high.
Society for Endocrinology BES 2017
Harrogate, UK 06 Nov 2017 - 08 Nov 2017
Browse other volumes
Article tools
My recent searches, my recently viewed abstracts, chisenga katy.

Endocrine Abstracts ISSN 1470-3947 (print) | ISSN 1479-6848 (online) © Bioscientifica 2024 | Privacy policy | Cookie settings
BiosciAbstracts
Bioscientifica Abstracts is the gateway to a series of products that provide a permanent, citable record of abstracts for biomedical and life science conferences.
Early recognition of Cushing's disease: a case study
Affiliation.
- 1 (Nurse Practitioner), Department of Neurosurgery, Pituitary/Neuroendocrine Center, Brigham and Women's Hospital, Boston, Massachusetts (Professor), Department of Neurosurgery, Harvard Medical School, Boston, Massachusetts.
- PMID: 24170635
- DOI: 10.1111/1745-7599.12014
Purpose: To present a case study of a 34-year-old woman with Cushing's disease and provide nurse practitioners (NPs) with the understanding of the clinical presentation needed for early recognition and treatment of the disease.
Data sources: A comprehensive review of published literature on Cushing's disease. Findings from history, physical examination, and diagnostic studies of a woman presenting to primary care NPs, physicians and other healthcare providers with multiple symptoms of Cushing's disease.
Conclusions: Cushing's disease is the result of the pituitary gland producing excess amounts of adrenocorticotropic hormone (ACTH) causing the overproduction of cortisol. The disease is fairly rare and is seen mostly in women. Common chief complaints include increased facial hair, weight gain, amenorrhea, changes in the face, neck, and abdomen, with muscle wasting of the lower extremities. Untreated, diabetes mellitus and hypertension can occur and increase the patient's morbidity and mortality. Early recognition and appropriate referral can reverse the signs and symptoms over time and lead to a significantly improved quality of life.
Implications for practice: This case presented the challenges faced by NPs and physicians in diagnosing patients with Cushing's disease.
Keywords: Diabetes; endocrine; hormone; hypertension; obesity; pituitary; women.
©2013 The Author(s) ©2013 American Association of Nurse Practitioners.
Publication types
- Case Reports
- Pituitary ACTH Hypersecretion / complications
- Pituitary ACTH Hypersecretion / diagnosis*
- Pituitary ACTH Hypersecretion / therapy
Case Studies
Meet the editorial board.

Susan M. Webb
Barcelona, Spain

Iacopo Chiodini
Milan, Italy

Irina Bancos
Rochester, MN, USA
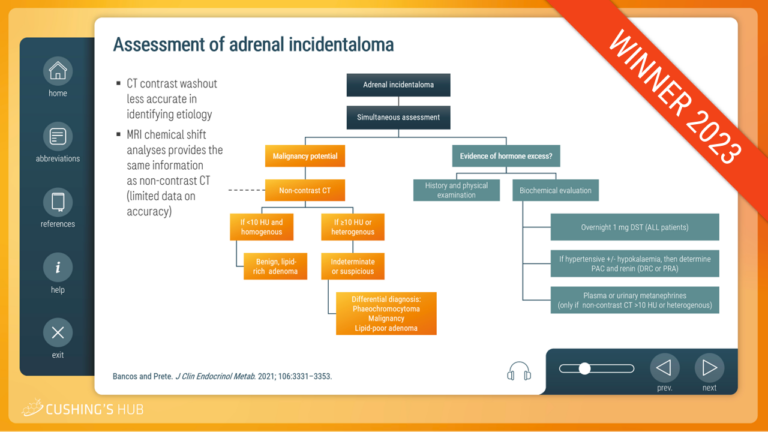
An interactive case study on adrenal incidentalomas and mild autonomous cortisol secretion (MACS)
This case study ꟷ the Cushing’s Hub Clinical Case Competition 2023 winning entry ꟷ looks at the clinical evaluation and management of MACS ranging from the assessment of adrenal incidentalomas to the development of an individual treatment plan.
An interactive case study on ectopic Cushing’s syndrome
This interactive case study describes a case of ectopic Cushing’s syndrome in a middle-aged woman presenting with severe back pain.
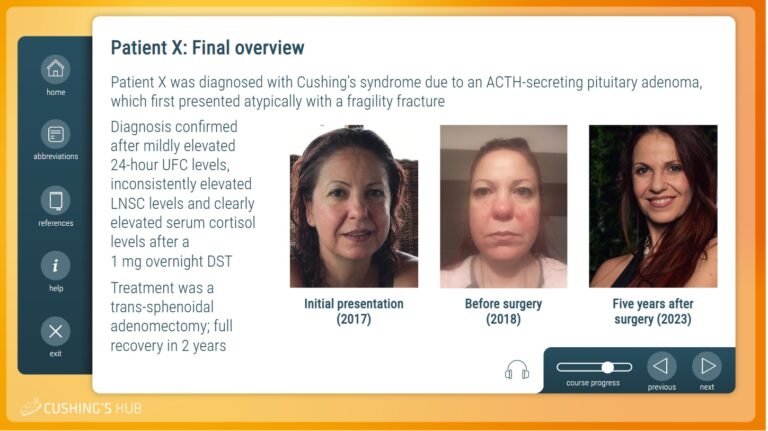
An interactive case study on hidden hypercortisolism
This interactive case study describes an unusual case of Cushing’s syndrome in a largely asymptomatic, female patient presenting with a fragility fracture.
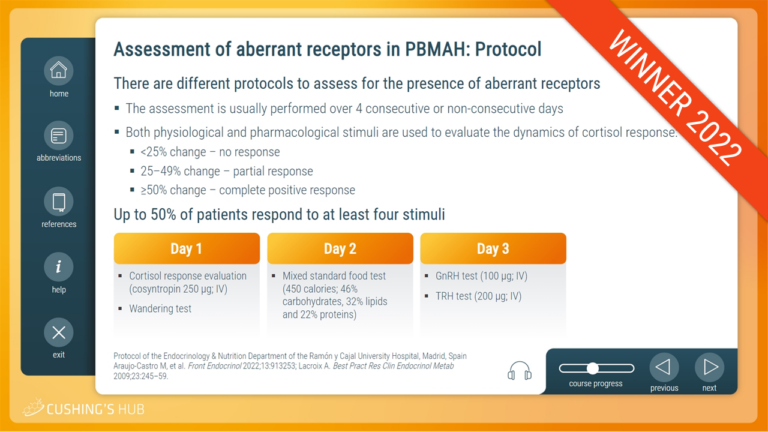

An interactive case study on Cushing´s syndrome due to primary bilateral macronodular adrenal hyperplasia
This case study—the Cushing’s Hub Clinical Case Competition winning entry—looks at primary bilateral macronodular adrenal hyperplasia as a cause of Cushing’s with special emphasis on the role of aberrant receptors.
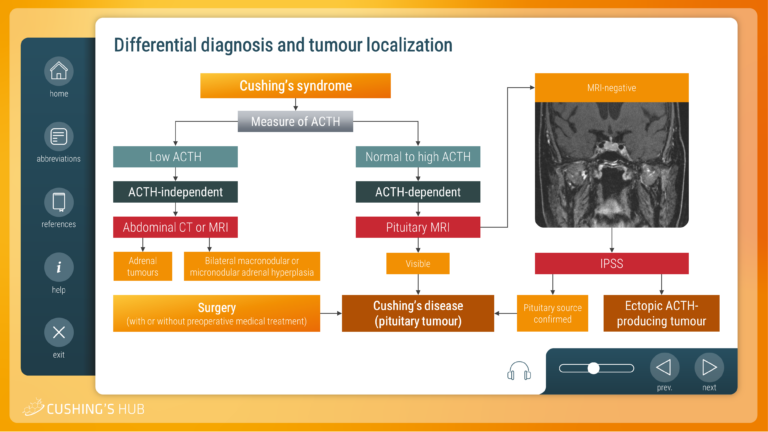
An interactive case study on the differential diagnosis of Cushing’s syndrome
This module looks at the diagnostic strategy required to establish the cause of adrenocorticotrophic hormone (ACTH)-dependent Cushing’s syndrome, when imaging and biochemical results are inconclusive.
An interactive case study on severe hypokalaemia and excessive cortisol secreting Cushing’s disease
This module looks at the optimal way to manage hypercortisolism with associated comorbidities, particularly in patients who are ineligible for surgery.
An interactive case study on screening for Cushing’s syndrome
This module raises questions about who should be screened for Cushing’s syndrome and considers the most suitable diagnostic tests for the avoidance of diagnostic uncertainty.
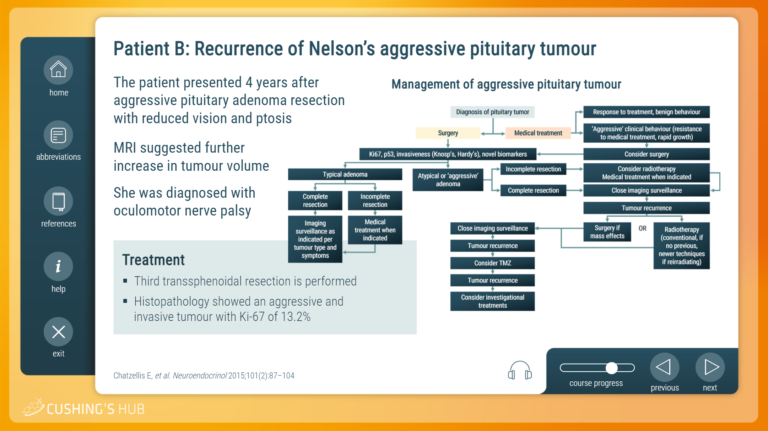
An interactive case study on the management of an aggressive Nelson’s tumour
The third interactive case study describes patient follow-up after bilateral adrenalectomy and explains how to develop a treatment plan for an aggressive Nelson’s tumour.
An interactive case study of relapsing Cushing’s disease in a woman of childbearing age
The second interactive case study explores the management of relapsing Cushing’s disease in a woman of childbearing age with emphasis given to pregnancy planning.
An interactive case study on cortisolemia
This interactive training module uses a case study format to explore the optimal way to assess cortisolemia in patients who have started treatment for Cushing’s syndrome.

© Springer Healthcare, 2024. All rights reserved.
This website is provided by springer healthcare., you are leaving cushings hub.
You are now leaving Cushings Hub and entering a website that we do not control.
Cushings Hub has provided this link for your convenience, but is not responsible for the content, links, privacy policy, or security of this website.
Click agree to proceed or close this window to return to Cushings Hub,
Before you go, why not bookmark Cushings Hub?
- Search Menu
- Volume 8, Issue 6, June 2024 (In Progress)
- Volume 8, Issue 5, May 2024
- Diabetes, Pancreatic and Gastrointestinal Hormones
- Lipids and Cardiovascular
- Obesity and Adipocyte Biology
- Parathyroid, Bone, and Mineral Metabolism
- Pituitary and Neuroendocrinology
- Reproductive Biology and Sex-Based Medicine
- Advance Articles
- Expert Endocrine Consult Articles
- ENDO Meeting Abstracts
- Obesity Research
- Thematic Issues
- Clinical Practice Guidelines
- Endocrine Reviews
- Endocrinology
- Journal of the Endocrine Society
- The Journal of Clinical Endocrinology & Metabolism
- JCEM Case Reports
- Molecular Endocrinology
- Endocrine Society Journals
- Author Guidelines
- Submission Site
- Open Access
- Why Publish with the Endocrine Society?
- Advertising & Corporate Services
- Reprints, ePrints, Supplements
- About Journal of the Endocrine Society
- Editorial Board
- Author Resources
- Reviewer Resources
- Rights & Permissions
- Other Society Publications
- Member Access
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
- < Previous
A Case of Iatrogenic Cushing’s Syndrome
- Article contents
- Figures & tables
- Supplementary Data
Andrea Del Toro Diez, Michelle Marie Mangual Garcia, Jose M Garcia-Mateo, Ernesto Jose Sola Sanchez, A Case of Iatrogenic Cushing’s Syndrome, Journal of the Endocrine Society , Volume 5, Issue Supplement_1, April-May 2021, Page A103, https://doi.org/10.1210/jendso/bvab048.206
- Permissions Icon Permissions
Cushing’s syndrome (CS) is considered a rare disease. The most common cause is the exogenous use of glucocorticoids (GCs), which are often given within a controlled medical setting, but their factitious use is rare. Factitious CS is more common in females, young patients, those with psychiatric disorders, and those with contacts within the medical field. The diagnosis of CS is challenging because some features are non-specific and commonly present in the general population, such as obesity, depression, diabetes, hypertension (HTN), and low bone mineral density (BMD). A high suspicion is warranted. We present the case of a 47-year-old man with HTN, obesity, dyslipidemia, obstructive sleep apnea, and low BMD who complained of increased appetite, significant weight gain, fatigue, sleepiness, muscle weakness, and occasional facial flushing. Medications include Hydrochlorothiazide, Furosemide, Losartan, Atorvastatin, and Teriparatide. Vital signs were normal and body mass index was 41.9 kg/m 2 . He had a round face, central obesity, and wide purple striae in his abdomen. Dual-energy X-ray absorptiometry scan showed low BMD at spine. Laboratories revealed a glycated hemoglobin of 6.1%, late-night salivary cortisol of <0.03 mcg/dL, 24-hour urine free cortisol of 22.5 mcg/24hr, morning cortisol of 0.01 ug/mL, ACTH 23.5pg/mL, and dehydroepiandrosterone sulfate (DHEA-S) 35 mcg/dL. Our patient persistently denied use of exogenous GCs, but a urine synthetic GC screen disclosed a positive result for dexamethasone; levels at 1.1 mcg/dL. After an exhaustive conversation, our patient confessed to using over-the-counter dexamethasone 4mg to treat occasional muscle aches. ACTH is usually suppressed in factitious CS, but this was not our patient’s case, giving the appearance of ACTH-dependent hypercortisolism. This can lead to unnecessary diagnostic and therapeutic approaches. An unsuppressed ACTH could be due to an unreliable ACTH immunoassay or intermittent, instead of continuous, ingestion of GCs. A suppressed DHEA-S level, as seen in our patient, may provide the clue to exogenous GC use as the cause of CS. Our case is also rare because our patient is male, older, and not related to the medical field. Hypercortisolism must be detected and treated early due to its high morbidity and mortality. Several features may be reversed with treatment. The possibility of hypothalamic-pituitary-adrenal (HPA) axis suppression due to prolonged use of GCs, resulting in adrenal insufficiency (AI) should be considered. The prevalence of GC-induced AI ranges from 14–63%, with the highest risk in those with Cushingoid features and those receiving a dose equivalent to prednisone 20mg daily for more than three weeks. Sudden withdrawal of GCs should be avoided to prevent adrenal crisis. A tapering regimen should be adopted with subsequent biochemical testing of the HPA axis once GCs have been reduced to a physiologic dose.
Email alerts
Citing articles via.
- About the Endocrine Society
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 2472-1972
- Copyright © 2024 Endocrine Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Clin Endocrinol Metab

Approach to the Patient: Diagnosis of Cushing Syndrome
Mesut savas.
Department of Internal Medicine, Division of Endocrinology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands
Sonal Mehta
Division of Endocrinology, NYU Langone Medical Center/ Bellevue Hospital Center, New York, NY
Nidhi Agrawal
Elisabeth f c van rossum, richard a feelders, associated data.
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Cushing syndrome results from supraphysiological exposure to glucocorticoids and is associated with significant morbidity and mortality. The pathogenesis includes administration of corticosteroids (exogenous Cushing syndrome) or autonomous cortisol overproduction, whether or not ACTH-dependent (endogenous Cushing syndrome). An early diagnosis of Cushing syndrome is warranted; however, in clinical practice, it is very challenging partly because of resemblance with other common conditions (ie, pseudo-Cushing syndrome). Initial workup should start with excluding local and systemic corticosteroid use. First-line screening tests including the 1-mg dexamethasone suppression test, 24-hour urinary free cortisol excretion, and late-night salivary cortisol measurement should be performed to screen for endogenous Cushing syndrome. Scalp-hair cortisol/cortisone analysis helps in the assessment of long-term glucocorticoid exposure as well as in detection of transient periods of hypercortisolism as observed in cyclical Cushing syndrome. Interpretation of results can be difficult because of individual patient characteristics and hence requires awareness of test limitations. Once endogenous Cushing syndrome is established, measurement of plasma ACTH concentrations differentiates between ACTH-dependent (80%-85%) or ACTH-independent (15%-20%) causes. Further assessment with different imaging modalities and dynamic biochemical testing including bilateral inferior petrosal sinus sampling helps further pinpoint the cause of Cushing’s syndrome. In this issue of “Approach to the patient,” the diagnostic workup of Cushing syndrome is discussed with answering the questions when to screen, how to screen, and how to differentiate the different causes. In this respect, the latest developments in biochemical and imaging techniques are discussed as well.
A 45-year-old woman was referred to the University Medical Center from another hospital for possible Cushing syndrome. She had a weight gain of 6 kg in 18 months, central obesity, moderate muscle weakness, and insomnia. Hypertension had been diagnosed 3 years ago and was treated with nifedipine 30 mg. She consulted a psychiatrist for 14 months because of depressive complaints and there was suspicion of bipolar disorder. For this, she is treated with carbamazepine 200 mg twice daily. There is no alcohol or drug abuse.
At physical examination, a body mass index of 28 kg/m 2 and blood pressure of 150/95 mmHg was measured. The patient had a moderate plethoric facial appearance, supraclavicular fat pads, and some central obesity without striae. There was minimal muscle atrophy of the upper legs, and no ecchymoses, hirsutism, or edema was observed.
In the hospital, an increased urinary free cortisol excretion (UFC) was found of 2 times the upper limit of normal (ULN), a disturbed 1-mg dexamethasone suppression test (DST) with a cortisol value of 5.62 µg/dL (155 nmol/L) and a high-normal ACTH level of 40.9 pg/mL (ULN 50 pg/mL; 9 pmol/L with ULN of 11 pmol/L). Pituitary imaging with magnetic resonance imaging (MRI) showed a small cystic lesion at the left side of the pituitary.
In consultation with the psychiatrist, the carbamazepine was replaced by lithium and psychotherapy was started. Endocrine evaluation at the University Medical Center 6 weeks later revealed a UFC of 1.5 to 2.0 times ULN, a postdexamethasone cortisol dose of 3.05 µg/dL (84 nmol/L), midnight salivary cortisol levels of 0.047 and 0.065 µg/dL (1.3 and 1.8 nmol/L, ULN 0.11 µg/dL or 3.0 nmol/L). In addition, a dexamethasone-corticotropin-releasing hormone (CRH) test was performed showing undetectable cortisol levels after administration of 4 mg dexamethasone for 2 days and no stimulation of cortisol levels after 1 μg/kg CRH IV. A pseudo-Cushing syndrome secondary to her psychiatric disorder and a nonfunctional pituitary lesion was considered the most likely diagnosis. The patient responded well to the psychiatric treatment and 10 months later she felt better with control of depressive symptoms, improvement of her condition, and weight loss of 3 kg. UFC levels were measured and were below the ULN, whereas the DST showed a cortisol level of 1.16 µg/dL (32 nmol/L).
Learning Points
- A pseudo-Cushing syndrome should always be considered in patients with endogenous hypercortisolism
- Patients with a pseudo-Cushing syndrome can have symptoms associated with endogenous hypercortisolism resembling true Cushing syndrome
- The results of first-line screening tests for Cushing syndrome can be influenced by the use of concomitant medication (eg, antiepileptic drugs can cause a false-positive DST)
- Midnight salivary cortisol levels and the second-line dexamethasone-CRH test can be useful to differentiate pseudo-Cushing syndrome from ACTH-dependent Cushing syndrome
A 52-year-old woman was referred by a hospital elsewhere to the University Medical Center for surgical treatment of adrenal Cushing syndrome. The patient presented with nephrolithiasis and on a computed tomography (CT) scan of the abdomen, an enlarged left adrenal gland was found with radiological features compatible with an adenoma (lipid-rich, low Hounsfield units). Six months before the patient was seen at the emergency room because of deep venous thrombosis of the right leg. Then a high blood pressure was measured (210/110 mmHg) for which treatment was started with valsartan. The patient reported weight gain (8 kg in the past 2 years), increased abdominal circumference, hirsutism, easy bruisability, and proximal muscle weakness. At physical examination, she had a cushingoid phenotype with a moon face with plethora and moderate hirsutism, central obesity, proximal muscle atrophy of the extremities, and skin atrophy with some hematomas. A body mass index of 31 kg/m 2 and blood pressure of 170/10 mmHg were measured.
Endocrine evaluation revealed the following results: UFC values of 4.5 to 5.0 times ULN, a DST with a cortisol level of 17.33 µg/dL (478 nmol/L), and an ACTH concentration of 19.07 pg/mL (4.2 pmol/L). After referral, ACTH measurement was repeated and showed values of 12.71 pg/mL (2.8 pmol/L) and 18.16 pg/mL (4.0 pmol/L). Because ACTH levels were not suppressed, an MRI of the sellar region was performed that demonstrated a pituitary adenoma of 7 mm. Additional investigations included measurement of dehydroepiandrosterone-sulfate (DHEAS) and a CRH test. The DHEAS concentration was 2.36 µg/mL or 6.4 µmol/L (reference range, < 2.28 µg/mL or 6.2 µmol/L) and the CRH test showed an ACTH increase of 170% and a cortisol increase of 140% of baseline. Considering these results, the diagnosis pituitary-dependent Cushing syndrome was considered most likely. The patient underwent a transsphenoidal adenomectomy, which resulted in biochemical remission. Pathological examination confirmed a basophilic adenoma with a positive ACTH staining.
- Cushing syndrome is associated with a high risk of venous thromboembolic events which can be a presenting symptom
- Pituitary-dependent Cushing syndrome can be accompanied by unilateral adrenal enlargement
- In Cushing syndrome patients with ACTH levels in the low-normal range and uni- or bilateral adrenal enlargement, measurement of DHEAS levels and a CRH test can be helpful to differentiate between a pituitary and an adrenal cause
Cushing syndrome (CS) results from prolonged exposure to excess glucocorticoids, either from exogenous glucocorticoids or an endogenous source of excess cortisol. The most common cause of CS is iatrogenic, resulting from exogenous pharmacologic doses of corticosteroids. Endogenous CS is caused by ACTH-dependent or ACTH-independent excess of cortisol production ( 1-3 ). The estimated incidence of endogenous CS is 0.2 to 5.0 per million people per year and the estimated prevalence is 39 to 79 per million in various populations ( 2 ). ACTH-dependent CS accounts for 80% to 85% of cases and ACTH-independent accounts for 15% to 20% ( 2 , 4 , 5 ).
CS is a severe disease with often long-lasting effects, yielding a low quality of life ( 6 ). Hypercortisolism is associated with an increase in cardiovascular events (myocardial infarction), cerebrovascular events (stroke), sepsis, and thromboembolism with 3.5 to 5 times increased mortality risk compared with the general population ( 7-11 ). The risk of myocardial infarction is approximately 4.5 times higher in patients with CS compared with the general population ( 8 , 9 ). Surgical remission does not eliminate the risk of complications from systemic comorbidities completely ( 12 , 13 ). The prevalence and pathophysiology of comorbidities in CS ( 5 , 10 , 14-28 ) are shown in Table 1 . Even if improvements occur after successful treatment, recovery often does not seem to be complete, and physical and neuropsychological comorbidities may persist ( 29 ). Therefore, early diagnosis of CS is important, but in clinical practice it is often challenging because there is substantial overlap in signs and symptoms with other (common) conditions.
Comorbidities in Cushing syndrome
In this article, we focus on the diagnostic approach to the patient suspected of (exogenous, endogenous, or cyclic) CS, and take the latest developments in the field of novel diagnostic measurements and technology into account.
Synthetic glucocorticoids (ie, corticosteroids) have the potential to induce similar symptoms as seen in endogenous CS. Glucocorticoid use is in fact the most prevalent cause of CS. The profuse prescription and over-the-counter availability in some countries justify the inclusion of drug history in the initial approach to CS. The net systemic effect of glucocorticoids depends on the bioavailability as well as other pharmacokinetic and the pharmacodynamic properties of the applied drug. Also, the duration of use and the route of administration are important for the development of features of CS. Serious adverse events are in general more likely to occur in systemic corticosteroid users and especially with longer duration and higher dosage of use ( 30 ). Suspected unreported exogenous glucocorticoid administration can be detected with urinary or blood mass spectrometry assays designed to detect exogenous glucocorticoids ( 31 ). Moreover, it is also important to screen for concomitant use of other drugs such as antifungals, protease inhibitors, or estrogens given the potential drug–drug interaction resulting in increased glucocorticoid effect ( 32 , 33 ).
From the patient’s perspective, weight gain has been reported as the most common adverse event followed by skin problems (bruising/thinning) and sleep disturbances ( 34 ). Interestingly, 2 distinct patterns in the occurrence of glucocorticoid-associated adverse events have been described in chronic users. A dose-related pattern was found for clinical features such as cushingoid phenotype, skin thinning, ecchymosis, and sleep disturbances. Although other adverse effects manifested above a certain threshold of daily glucocorticoid dosage (eg, epistaxis and weight gain with daily prednisone equivalent dose of > 5.0-7.5 mg), whereas depression and high blood pressure were especially prevalent with > 7.5 mg/d ( 35 ). With regard to exogenous corticosteroid assessment, administration forms other than the oral types should also be taken into consideration. A meta-analysis on the occurrence of adrenal insufficiency in corticosteroid users has found similar percentages in users of intra-articular injection (52.2% absolute risk) as for oral corticosteroids (48.7%) ( 36 ). Furthermore, the locally applied corticosteroids such as nasal, dermal, and inhaled types were also significantly associated with adrenal insufficiency (4.2%, 4.7%, and 7.8%, respectively), which implies systemic availability of these types. When drugs of different administration routes were combined, which is not uncommon for asthma, eczema, and hay fever, among others, the absolute risk of adrenal insufficiency even increased to 42.7% in this study. In this light, it is of interest that we recently showed associations between use of local corticosteroids, particularly inhaled types, and higher likelihood of metabolic syndrome, higher body mass index, reduced executive cognitive functioning, and a higher likelihood of mood and anxiety disorders ( 37 , 38 ). All these features are also (although nonspecific) characteristics of increased glucocorticoid exposure. These relations between corticosteroid use and cardiometabolic sequelae seemed to be related to glucocorticoid receptor gene variants that are associated with increased or normal glucocorticoid sensitivity. Interestingly, the adverse effects were less pronounced in corticosteroid users harboring gene polymorphisms, which are associated with glucocorticoid receptor resistance ( 39 ). Despite the lower probability of systemic adverse events in locally administered use, it is still of great importance given the fact that the vast majority of corticosteroid use involves the local types ( 37 ). Moreover, in the case of local corticosteroids, also other individual factors that determine glucocorticoid metabolism or can promote absorption and thus systemic adverse events must be considered, such as type of delivery device for inhaled corticosteroids or application of dermal corticosteroids in skin folds or under occlusion.
The clinical presentation of CS can be variable, depending on a patient’s age, sex, severity, and duration of cortisol excess ( Table 2 ) ( 1 , 3 , 5 ). Patients often present with nonspecific features such as (abdominal) obesity and weight gain, rounded (moon) face, menstrual irregularity, and depression ( 1 , 3 , 5 ) as depicted in Figure 1 . The diagnosis is even more complicated if signs and symptoms gradually develop over time and emerge sequentially. It is therefore a challenging task to diagnose endogenous CS at an early stage. There is additionally a large overlap of cushingoid-related features with other conditions associated with relatively mild increased cortisol levels. These pseudo-Cushing states, such as with severe obesity, alcoholism, polycystic ovary syndrome, and neuropsychiatric disorders, are beyond compare more prevalent than endogenous CS ( 40 ) (see also subparagraph “ Pseudo-Cushing’s syndrome ”). Testing is however recommended ( 3 ) in:
Clinical features of Cushing syndrome and prevalence
Features with highest discriminatory value are depicted in bold. Table adapted from Sharma et al ( 5 ).

Clinical features and comorbidities associated with Cushing syndrome. Based on Agrawal et al ( 1 ), Sharma et al ( 5 ), and Pivonello et al ( 27 ).
- Patients with adrenal incidentalomas (adenoma).
- Patients who show Cushingoid-related features which are uncommon for age (such as hypertension, osteoporosis, or female balding).
- Patients who have multiple symptoms, which are progressive over time, in particular when specific cushingoid features are present ( 3 ). Clinical features such as ecchymoses, proximal myopathy, wide reddish-purple striae, facial plethora, recurrent infections, and osteopenia have been found to be more characteristic of CS ( 41 , 42 ) and aid in the decision to perform screening tests.
- Children with a combination of increasing weight and decreasing height percentile.
In addition, screening can be considered in patients with difficult to treat diabetes or hypertension, although it is generally not recommended to perform large-scale screening for CS in populations with diabetes, hypertension, or obesity. In case of pituitary incidentaloma, routine screening for ACTH-hypersecretion is not recommended ( 43 ). It remains a matter of debate whether screening for hypercortisolism in asymptomatic persons is useful for detecting preclinical Cushing disease ( 44 ). Individuals with clinical suspicion of Cushing disease should undergo testing, as mentioned in the next section. Finally, patients with active CS have a high risk of venous thromboembolism (VTE) in comparison to the general population ( 8 , 45 , 46 ). The patient in case 2 presented earlier with VTE, but CS was not recognized yet. The high VTE risk is due to glucocorticoid-induced activation of the coagulation cascade, whereas fibrinolysis is impaired ( 3 , 24 ). Hence, screening for hypercortisolism may be considered in patients with unexplained venous thrombotic events.
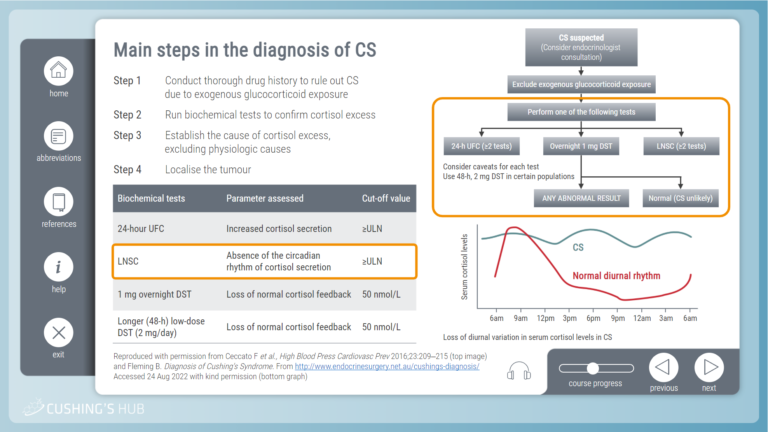
If a patient is suspected of CS and exogenous glucocorticoid use is excluded, it is recommended to start by performing one of the first-line screening tests ( 3 ). Recommended initial tests include:
- overnight 1-mg DST;
- 24-hour UFC; and
- late-night salivary cortisol test (LNSC).
The latter 2 tests should be performed at least twice because of significant day-to-day variations in cortisol production. The pooled diagnostic accuracy of the various tests ( 47 ) is presented in Figure 2 . There is no specific order of screening, but the choice for a specific test can be made based on individual patient characteristics (see also caveats in Figure 2 ). A promising relatively novel test to detect chronic hypercortisolism is measurement of cortisol in scalp hair (see “New developments: potential of hair cortisol measurement as diagnostic tool”).

Diagnostic workup of Cushing syndrome. Flowchart is based on Lacroix et al ( 3 ). The likelihood ratios (LRs) for the first-line screening tests and scalp hair analysis concern pooled data from ( 47 ) and findings from ( 48 ), respectively. LRs take sensitivity and specificity into account and determine the posttest probability given a certain pretest probability (higher LR + = increasing probability of disease with positive test result; lower LR - = decreasing probability of disease with negative test result). Abbreviations: CBG, cortisol-binding globulin; LR-, negative likelihood ratio; LR+, positive likelihood ratio.
CS is unlikely with normal test results; however, referral to an endocrinologist is recommended in patients with a high likelihood. In other cases, a reevaluation in 6 months should be considered if a patient has progressive features. An abnormal test result prompts further evaluation by an endocrinologist. Patients should be subsequently tested again with 1 or 2 first-line screening tests or a second-line screening test (eg, combined dexamethasone-CRH test or midnight serum cortisol) if necessary ( 3 ). The diagnosis of CS is established with concordant abnormal results indicating hypercortisolism. Further evaluation should be focused on identifying the underlying cause. Endogenous CS is unlikely with 2 normal test results and requires no further evaluation unless a cyclical CS or a (rare) glucocorticoid hypersensitivity is suspected. In the rare condition of increased glucocorticoid sensitivity, a clinical picture of CS is present, but laboratory tests show (borderline) low plasma and urinary cortisol values while responsiveness to ACTH (Cortrosyn) or metyrapone stimulation test and/or insulin-induced hypoglycemia is normal ( 31 , 49 ). An ultra-low-dose DST showing suppressed morning serum cortisol levels is also indicative of this rare condition, and functional testing of the glucocorticoid receptor or sequencing of the glucocorticoid receptor gene may be considered in specialized centers ( 31 , 49 , 50 ). In these cases, use of any type of exogenous corticosteroids should be ruled out or only use of low dosages equivalent to hydrocortisone replacement therapy or below with a history of development of cushingoid features after initiation. Primary glucocorticoid resistance, a rare genetic condition resulting mainly from mutations in the glucocorticoid receptor gene, would on the contrary yield abnormal test results ( 51 ). These patients present with symptoms of increased mineralocorticoid and/or androgen action, combined with biochemical hypercortisolism from compensatory overdrive of the hypothalamus-pituitary-adrenal (HPA) axis, but lack of specific cushingoid features. This increased HPA-axis activity from the decreased peripheral glucocorticoid receptor sensitivity should be distinguished from pathological hypercortisolism from CS ( 52 ). In general, follow-up and further evaluation is recommended in the event of discordant results or high clinical suspicion of cyclical CS ( 3 ).
Each of the first-line screening tests has its limitations, the most important factors that can affect the outcome are mentioned in Figure 2 . Regarding the 1-mg DST, it is essential to screen for current drug use, which could alter dexamethasone clearance and/or levels of cortisol-binding globulin. This mainly relates to antiepileptic drugs, as in case 1, and use of estrogen-containing medication; a detailed overview is available elsewhere ( 3 ). In case of positive DST, measurement of serum dexamethasone concentration could be of value in identifying insufficient levels ( 53 ) (eg, from altered dexamethasone metabolism or inadequate test adherence) and in determining in whom a second DST would be useful ( 54 ). As to the LNSC, use of substances containing glycyrrhizic acid (ie, 11beta-hydroxysteroid dehydrogenase type 2 [11β-HSD2] inhibitor) should be avoided. This is because cortisol in the salivary glands is naturally inactivated by 11β-HSD2 and inhibition of this can therefore lead to falsely elevated cortisol levels. Glycyrrhizic acid is among others present in licorice candies and some teas. Other less prevalent 11β-HSD2 inhibitors include the glycyrrhizic acid derivative carbenoxolone, gossypol, and various endocrine disruptors such as phthalates ( 55 ).
One diagnostic challenge in the evaluation of endogenous hypercortisolism is differentiating neoplastic CS from pseudo-CS. Pseudo-CS, or nonneoplastic physiologic hypercortisolism, is a phenomenon that can occur in many medical disorders such as chronic alcoholism, chronic kidney disease, type 2 diabetes mellitus, and psychiatric conditions. Hypercortisolism in these conditions is mainly mediated by activation of the HPA axis through neural pathways without tumorous hypercortisolemia. There is also decreased sensitivity to glucocorticoid negative feedback in the majority of these states which may lead to mild increases in cortisol. Over time, the effects of small increases in cortisol can lead to significant and longitudinal glucocorticoid exposure and can result in pathologic features of hypercortisolism as is also illustrated in case 1 ( 1 , 56 , 57 ). A detailed history and physical examination are important first steps to take in evaluating patients with hypercortisolism and most patients with pseudo-CS will have mild cortisol excess and not have overt clinical manifestations of glucocorticoid excess. When undergoing biochemical testing in patients, if the first-line tests show normal LNSC measurements ( 57 ) and appropriate suppression of cortisol with DST, patients are unlikely to have neoplastic hypercortisolism. However, if there is diagnostic uncertainty, a 48-hour 2 mg/d DST or secondary tests can be performed, including DDAVP stimulation, and dexamethasone-CRH testing ( 1 , 3 , 56-58 ). The latter tests and their interpretation are described in Table 3 .
Secondary testing to differentiate pathologic Cushing syndrome from nonneoplastic physiologic hypercortisolism (pseudo-Cushing syndrome)
Adapted from data from Agrawal et al ( 1 ), Findling et al ( 56 ), Alwani et al ( 57 ), and Yanovski et al ( 58 ).
Abbreviation: CRH, corticotropin-releasing hormone.
A relatively novel method of cortisol measurement in patients suspected of CS is scalp hair analysis, a patient-friendly noninvasive method yielding cortisol values representing long-term cortisol exposure of the past months ( 48 , 59-62 ). This method enables retrospective assessment of glucocorticoid concentrations because both cortisol and its inactive variant cortisone are incorporated in hair ( 63 ). It is often compared with measuring glycosylated hemoglobin, which is used to assess mean blood glucose levels over weeks to months. The routine first-line screening tests capture cortisol exposure for up to several days, whereas hair analysis allows assessment of glucocorticoid concentrations in the past months to years. The growth rate of scalp hair is approximately 1 cm/mo. Depending on the length of the collected hair sample, it is possible to make timelines of past glucocorticoid exposure ( 64 ). This enables to capture (isolated or recurrent) episodes of hypercortisolism, but also to approximate the beginning and course over time of hypercortisolism. Hence, hair analysis possesses unique features which could further aid in the screening of CS ( 60 ). It additionally provides a stable measurement independent of acute stressors that could yield false-positive results with traditional matrices, such as saliva or urine. One of other advantages is that hair sample collection can easily be done at the outpatient clinic at any time of the day.
In the past decade, great progress has been made with the development of scalp hair glucocorticoid analysis, although this method is not yet widely available ( 65 ). Hair cortisol has been shown to differentiate between CS patients and healthy controls with high sensitivity and specificity ( 48 , 66 ). Within CS patients hair cortisol levels have been shown to correlate significantly with UFC ( 61 ). We and others also showed high diagnostic efficacy in screening of CS with hair steroid analysis. In these studies, a 3-cm hair sample per patient was used (corresponding to mean glucocorticoid levels of roughly past 3 months) and hair analysis was performed with either immunoassay ( 59 , 61 ) or liquid chromatography-tandem mass spectrometry ( 48 , 66 ). Interestingly, we found that hair cortisone has a higher differentiating capacity (sensitivity 87%, specificity 90%) than hair cortisol (sensitivity 81%, specificity 88%) ( 48 ). This difference could perhaps be contributed to local metabolism by 11β-HSD enzymes or 5α-reductase; however, further research is needed to confirm those findings ( 67 ).
In addition, hair cortisol and cortisone have been shown to contribute to the identification of patients with mild or subclinical CS ( 66 ). Because hair can be used as a historical timeline, scalp hair cortisol analysis can also be useful in studying the onset of CS (eg, in ectopic CS) or cyclic CS ( 59 , 68 ). Regarding the latter group, those patients periodically secrete excess cortisol and thus are less likely to have abnormal results with traditional tests if not screened at moments of actual hypercortisolism. In our previous study with a set of cyclical CS patients, we created historical timelines using hair and indeed demonstrated dynamic cortisol concentrations over time corresponding with clinical cushingoid features ( 59 ).
Pituitary apoplexy is another (rare) difficulty in diagnosing Cushing disease because this may induce spontaneous remission of the clinical syndrome when it occurs in an ACTH-overproducing adenoma. In these conditions, it is not possible to biochemically confirm this diagnosis at presentation. We recently reported a patient with a clinical picture of Cushing disease presenting with pituitary apoplexy, who was biochemically in remission at admission. In retrospect, the diagnosis of Cushing disease could be confirmed using hair cortisol analysis. This can be important for clinicians because it enables adequate anticipation of remission of Cushing disease, including potential symptoms reflecting a relative hypocortisolism because previous long-term exposure to hypercortisolism, as well as attention for long-term physical and mental complications and disease recurrence ( 69 ).
ACTH-dependent CS
Once CS has been established, plasma ACTH concentrations can help determine whether the cause is ACTH-dependent or ACTH-independent. Because of decreased glucocorticoid negative feedback effects, plasma ACTH levels will be inappropriately normal or elevated (generally > 20 pg/mL) in ACTH-dependent causes and low (generally < 10 pg/mL) in ACTH-independent causes of CS ( 70 , 71 ). Thirty percent of the patients with CS have ACTH levels in the “gray zone” (5-20 pg/mL) and should have repeat testing and consideration of adrenal imaging to detect possible adrenal pathology ( 72 ). ACTH-dependent CS comprises 80% to 85% of all CS cases.
Differentiation Between Cushing disease and Ectopic ACTH Secretion
Cushing disease, the most common cause of ACTH-dependent CS accounting for approximately 80% of cases, occurs when a pituitary adenoma secretes ACTH, which in turn stimulates supraphysiologic secretion of cortisol from the adrenal glands ( 2 , 4 , 5 , 73 ). Ectopic ACTH secretion (EAS) accounts for approximately 20% of ACTH-dependent CS. In these cases, most common sources of ACTH secretion are small cell lung carcinomas or pulmonary carcinoid tumors. Other causes can include pancreatic neuroendocrine tumors, thymic neuroendocrine tumors, gastrinomas, medullary thyroid cancer, and pheochromocytomas, as seen in Figure 3 ( 5 ). Imaging studies can help to differentiate between Cushing disease and ectopic causes. Pituitary MRI is used for detecting pituitary adenomas. Compared with conventional MRI, which can only detect 36% to 63% of pituitary microadenomas in patients with Cushing disease, high-resolution 3T-MRI with 3-dimensional spoiled gradient-echo sequence is characterized by thinner sections and superior soft-tissue contrast and can detect adenomas as small as 2 mm ( 74 ). If a pituitary adenoma > 6 mm is found on MRI, the need for further testing with bilateral inferior petrosal sinus sampling (BIPSS) is not necessary ( 1 , 9 , 74 , 75 ). However, pituitary MRI can be negative in up to 40% to 60% of Cushing disease cases. There can also be false-positive pituitary MRI findings in patients with EAS ( 76 ). BIPSS is the gold standard to differentiate between Cushing disease and EAS. The test, however, cannot be used to establish the diagnosis of ACTH-dependent CS and the presence of hypercortisolism must be confirmed immediately before and at the time of the procedure ( 77 ). During this procedure, plasma ACTH levels are withdrawn simultaneously from each petrosal sinus (venous drainage of the pituitary) and a peripheral vein. Sensitivity can be increased by obtaining ACTH levels under CRH stimulation ( 1 , 76 , 78 ). In ACTH-secreting adenomas, ACTH levels will be higher in the blood samples drawn from the inferior petrosal sinuses (IPS) compared with the periphery and will therefore have elevated IPS-to-peripheral (IPS:P) ACTH ratios: > 2 pre-CRH stimulations or > 3 post-CRH stimulations. A lack of an IPS:P ACTH gradient suggests an ectopic source of ACTH secretion. However, IPS prolactin measurements can be used as a surrogate marker of appropriate catheterization or normal IPS venous efflux to prevent a false-negative result ( 77 ). Studies have also shown how prolactin-adjusted intersinus ACTH ratios can be used for tumor lateralization ( 77 , 79 ). The most common complications of the procedure include groin hematomas and transient headaches. There can also be serious complications, including stroke and subarachnoid hemorrhage, thought to be related to anatomical variations causing transient hypotension and/or vascular injury during the procedure ( 77 ).

Sources of ectopic ACTH secretion. Based on Lacroix et al ( 2 ).
A novel, noninvasive molecular imaging technique that has been described by Walia et al. can help identify corticotroph adenomas using Gallium-68 ( 68 Ga)-tagged CRH combined with positron emission tomography (PET)-CT. 68 Ga-tagged CRH can be used to detect CRH receptors, which are upregulated on corticotroph adenomas and can delineate functionality of adenomas. Although the size of the study population was small, 68 Ga CRH PET-CT scan was able to correctly identify 100% of Cushing disease cases, including culprit lesions less than 6 mm in size, and was able to provide accurate information regarding lateralization and planning for intraoperative navigation, making it useful in both evaluation and management of ACTH-dependent CS ( 80 ). This technique is still investigational and not currently widely available.
Dynamic testing with high-dose DST, CRH test, and desmopressin testing can also be used to help differentiate between Cushing disease and EAS ( 9 , 81 ). In patients with Cushing disease, glucocorticoid receptors at the pituitary level retain the ability to inhibit ACTH secretion in the presence of high dexamethasone doses (8 mg). In contrast, most ectopic ACTH-secreting tumors do not respond to high-dose dexamethasone ( 9 ). The proposed cutoff point for positive response is a decrease in basal cortisol level by 50% or more. The high-dose DST is most often negative in patients with EAS ( 74 ). The CRH test is useful because corticotroph pituitary adenomas express CRH receptors and associated downstream cell-signaling pathway molecules, thereby responding to CRH by releasing excess ACTH compared with ectopic ACTH-secreting tumors ( 81 ). Therefore, most but not all patients with Cushing disease will have an increase in plasma ACTH by more than 50% and cortisol concentrations by more than 20% after CRH stimulation. Patients with EAS are typically unresponsive although some tumors, in particular bronchial carcinoids can express CRH receptors ( 9 , 74 , 81 , 82 ). Desmopressin testing can also be used because type 2 vasopressin receptors, which are generally absent in normal pituitary corticotrophs, have found to be expressed in corticotroph adenomas. Therefore, an increase in plasma ACTH and cortisol can be observed after injection of desmopressin in patients with Cushing disease ( 81 ). On the other hand, an absence of both ACTH and cortisol is expected in patients with EAS, although false-positive results can be seen as EAS tumors may express type 3 vasopressin receptors ( 9 , 74 , 81 ). Individually, none of these tests have 100% specificity because if high false-positive rates, and results can be discordant in up to 65% of patients ( 2 ) because of a number of factors including differences in type of ectopic tumor, patient age, patient sex, and severity of hypercortisolism ( 9 ). In cases of discordant results, BIPSS is needed to determine the disease source ( 2 ). However, using these dynamic tests in combination with pituitary MRI can improve clinical accuracy, decreasing the need for BIPSS ( 9 , 75 ). In cases in which results are inconclusive for Cushing disease, evaluation for EAS should be considered (see also Figure 3 for sources of EAS). Whole-body thin-slice CT scans (cervical, thoracic, abdominal, and pelvic regions) should be performed initially to evaluate for tumors suggestive of EAS ( 9 , 81 ). Second-line tests include functional imaging using 68 Ga-PET/CT or 18 FDG PET/CT scans, which can be used to detect occult tumors, reinforce tumors seen on CT scan as being neuroendocrine, or contribute to the workup of metastatic tumors ( 9 , 81 ).
ACTH-independent CS
ACTH-independent CS is usually caused by an adrenal adenoma and less frequently by bilateral micro- or macronodular adrenal hyperplasia and adrenal carcinoma. Very rare causes include primary pigmented nodular adrenocortical disease, the Carney complex, and McCune-Albright syndrome ( 2 ). If after establishment of endogenous hypercortisolism ACTH concentrations are suppressed (< 10 pg/mL or < 2.2 pmol/L), the next diagnostic step is imaging of the adrenal glands with CT or MRI. If the radiological phenotype has worrisome features (eg, tumor size greater than 4 cm, calcifications, irregular tumor margins, Hounsfield units > 20) and/or the plasma steroid profile shows elevated DHEAS and steroid precursors an additional FDG-PET scan can guide the decision on an (open) adrenalectomy with an oncological approach.
In case of intermediate ACTH values, between 10 and 20 pg/mL (2.2 pmol/L and 4.4 pmol/L), the differentiation between an adrenal and a pituitary cause of CS can be difficult, as is illustrated by case 2. In case of an adrenal cause, mild cortisol overproduction may be accompanied by incomplete ACTH suppression. Conversely, in case of more severe clinical and biochemical hypercortisolism an ACTH-dependent cause of CS is more likely. In addition, a cyclical ACTH secretion pattern may explain ACTH values in the lower range. Measurement of DHEAS concentrations and a CRH test can be helpful to differentiate an adrenal from a pituitary cause. DHEAS secretion is partly ACTH driven and low-normal or suppressed DHEAS levels point to an adrenal cause. Corticotroph tumors are sensitive to CRH stimulation and a substantial ACTH and cortisol increase (> 50% of baseline) are compatible with a pituitary cause ( 83 , 84 ).
Bilateral adrenal hyperplasia, and to a lesser extent adrenal adenomas, is often associated with eutopic or ectopic hormone receptor expression with coupling to steroidogenesis ( 85 ). Examples are the vasopressin receptor, LH receptor, and the glucose-dependent insulinotropic polypeptide receptor. Screening for aberrant hormone receptor expression with specific stimulation tests may offer an option for medical therapy via blockade of the receptor or inhibition of secretion of the endogenous ligand ( 85 ). Screening of family members of patients with bilateral adrenal hyperplasia with a 1 mg DST is recommended ( 85 ).
A subgroup of ACTH-independent hypercortisolism involves patients with uni- or bilateral adrenal incidentaloma(s) and mild autonomous cortisol secretion (MACS). MACS is often accompanied by cushingoid features, in particular, common cardiometabolic and mental complications, such as hypertension, type 2 diabetes, obesity, dyslipidemia, atrial fibrillation, and psychiatric or neurocognitive symptoms ( 86 ). MACS is also associated with an increased risk of frailty, osteoporosis, cardiovascular morbidity, and mortality ( 87 ). The 1-mg DST is the most sensitive test to detect MACS, whereas UFC and LNSC concentrations are frequently normal ( 87 ). It was shown that in patients with adrenal incidentalomas post-DST cortisol levels are related to cardiovascular events and all-cause mortality ( 88 ). A cortisol cutoff of 50 nmol/L is used to differentiate MACS from normal physiology. This 1-mg DST is up to 100% sensitive, so it can be used as an optimal first-line screening test ( 89 ). However, the specificity at the 50 nmol/L cutoff can be as low as ~60%. Use of other methods such as UFC or LNSC can be necessary to confirm the diagnosis of MACS ( 89 ). Low or suppressed ACTH values can further indicate autonomous cortisol production.
Diagnosis of CS in Pregnancy
CS is rarely diagnosed during pregnancy because hypercortisolism inhibits normal follicular development and ovulation. In contrast to nonpregnant patients, the predominant etiology of CS in pregnant patients is adrenal adenomas, found in 40% to 60% of cases ( 90 , 91 ). Early diagnosis and management of CS during pregnancy are important because of associated fetal and maternal morbidity. Fetal morbidity includes rates of spontaneous abortion, perinatal death, premature birth, and intrauterine growth retardation (see Figure 4 ). Maternal morbidity caused by CS includes hypertension, preeclampsia, wound breakdown, diabetes, fractures, and opportunistic infections ( 2 , 92 ).

(Patho)physiologic changes of hypothalamus-pituitary-adrenal axis during pregnancy. Based on Brue et al ( 90 ). Abbreviation: CRH, corticotropin-releasing hormone.
Clinically, the diagnosis of CS during pregnancy can be more challenging because of overlap in features of hypercortisolism and classic features of pregnancy including fatigue, weight gain, hirsutism, acne, and emotional instability. It has been suggested that when pregnant patients have a triad of hypertension, skin ecchymosis, and muscle atrophy, CS should be considered ( 90 , 93 ). The biochemical diagnosis of CS during pregnancy can also be more challenging because of normal physiologic changes that occur during pregnancy, including activation of the HPA axis. Starting in the first trimester, there is an increase in estrogen and CRH produced by the placenta, which can lead to an increase in corticosteroid-binding globulin, a plasma cortisol transport protein. This in combination with the rise in placental CRH and ACTH cause an increase in total plasma cortisol levels. Suppression of serum and plasma cortisol by dexamethasone is blunted during pregnancy; therefore, making the DST difficult to interpret in these patients ( 3 , 90 , 92 ). UFC is often the recommended screening test during pregnancy; however, there are challenges to this as well. During the second trimester, UFC also increases, leading to an approximately 1.4-fold increase during the second trimester and a 1.6-fold increase during the third trimester. Therefore, while 24-hour UFC can be unaffected during the first trimester, it may not be a reliable diagnostic test in the second and third trimesters, unless levels are significantly increased, up to 2- to 3-fold the upper limit of normal ( 3 , 90 , 92 , 93 ). Although there had previously been fewer data on defining LNSC levels during pregnancy, there have been some studies looking at defining normal threshold values in each trimester of pregnancy, which could lead to increased use in screening these patients ( 90 , 94 , 95 ). In the study of Lopes et al ( 95 ), the reference range for the LNSC in each gestational trimester were 0.03 to 0.25 µg/dL (0.8-6.9 nmol/L) in the first trimester, 0.04 to 0.26 µg/dL (1.1-7.2 nmol/L) in the second trimester, and 0.07 to 0.33 µg/dL (1.7-9.1 nmol/L) in the third trimester. The cutoff values for the diagnosis of Cushing disease in the study were 0.255 µg/dL (7.0 nmol/L) for the first trimester, 0.260 µg/dL (7.2 nmol/L) for the second trimester, and 0.285 µg/dL (7.9 nmol/L) for the third trimester ( 90 , 95 ).
CS is multisystemic disease with serious morbidity and mortality and the diagnosis should preferably be made at an early stage considering long-term complications. Increased awareness of CS among physicians who treat comorbidities (family physicians, neurologists, psychiatrists) could be helpful in this respect. First-line screening tests to establish endogenous hypercortisolism include UFC, 1-mg DST, and LNSC. Hair cortisol/cortisone measurement is a relatively new diagnostic tool with a high sensitivity to diagnose CS and can also be helpful to detect cyclical CS in retrospect. All tests have caveats which should be taken into account when test results are interpreted. In patients with (mild) ACTH-dependent CS, a pseudo-CS should always be considered. In patients with ACTH-dependent CS, a pituitary cause should be differentiated from an ectopic origin. BIPSS has a high diagnostic accuracy for this purpose, but recent development of new noninvasive imaging modalities also shows promising results. The diagnostic workup of ACTH-independent CS is usually straightforward but diagnosing a primary adrenal cause of CS can be difficult when ACTH levels are not fully suppressed. Although diagnostic procedures have improved in the past decades with more accurate hormone measurement and improved imaging techniques, the diagnosis and differential diagnosis of CS can still be extremely challenging.
Acknowledgments
Figures 1, 3, and 4 were created by Kristen Dancel-Manning.
Abbreviations
Contributor information.
Mesut Savas, Department of Internal Medicine, Division of Endocrinology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands.
Sonal Mehta, Division of Endocrinology, NYU Langone Medical Center/ Bellevue Hospital Center, New York, NY.
Nidhi Agrawal, Division of Endocrinology, NYU Langone Medical Center/ Bellevue Hospital Center, New York, NY.
Elisabeth F C van Rossum, Department of Internal Medicine, Division of Endocrinology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands.
Richard A Feelders, Department of Internal Medicine, Division of Endocrinology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands.
Disclosures
R.A.F. received consultancy and speakers fees from Recordati. R.A.F. and N.A. received a research grant from Recordati.
Data Availability
Cushing’s Syndrome
Cushing’s syndrome (Cushing’s disease, Hypercortisolism , Adrenal Hyperfunction) is a cluster of clinical abnormalities caused by excessive levels of adrenocortical hormones (particularly cortisol) or related corticosteroids and, to a lesser extent, androgens and aldosterone.
Table of Contents
- What is Cushing’s Syndrome?
Statistics and Incidences
Clinical manifestations, complications, assessment and diagnostic findings, pharmacologic therapy, surgical management, nursing assessment, nursing diagnosis, nursing care planning & goals, nursing interventions, discharge and home care guidelines, documentation guidelines, practice quiz: cushing’s syndrome, what is cushing’s syndrome.
Cushing’s syndrome is a disorder of the endocrine system.
- Cushing’s syndrome (Cushing’s disease, Hypercortisolism, Adrenal Hyperfunction) is a cluster of clinical abnormalities caused by excessive levels of adrenocortical hormones (particularly cortisol) or related corticosteroids and, to a lesser extent, androgens and aldosterone.
- The prognosis depends on the underlying cause; it’s poor in untreated people and in those with untreatable ectopic corticotropin -producing carcinoma.
Incidences of Cushing syndrome are already common worldwide.
- Cushing’s syndrome affects 13 of every 1 million people.
- It is more common in women than in men and occurs primarily between ages 25 and 40.
Causes of Cushing’s syndrome include the following:
- Excess. In approximately 70% of patients, Cushing’s syndrome results from excessive production of corticotropin and consequent hyperplasia of the adrenal cortex.
- Tumor . In the remaining 30% of the patients, Cushing’s syndrome results from a cortisol-secreting adrenal tumor, which is usually benign.
Like other endocrine disorders, Cushing’s syndrome induces changes in multiple body systems, depending on the adrenocortical hormone involved.
- Muscle weakness . Muscle weakness is due to hypokalemia or a loss of muscle mass from increased catabolism.
- Buffalo hump. Buffalo hump is one of the symptoms included in the Cushing’s triad, and these are fat pads over the upper back.
- Moon face. Moon face is a symptom included in the Cushing’s triad and are recognized as excess fats over the face.
- Truncal obesity. Fat pads throughout the trunk refers to truncal obesity, one of the symptoms in Cushing’ triad
- Peptic ulcer . Peptic ulcer results from increased gastric production and pepsin secretion, and decreased gastric mucus.
- Irritability. Irritability and emotional lability ranges from euphoric behavior to depression and psychosis.
- Hypertension . Hypertension occurs due to sodium and water retention.
- Compromised immune system. Increased susceptibility to infection due to decreased lymphocyte production and suppressed antibody formation.
Complications of Cushing’s syndrome include the following:
- Addisonian crisis. The patient with Cushing’s syndrome whose symptoms are treated by withdrawal of corticosteroids, by adrenalectomy, or by removal of a pituitary tumor is at risk for adrenal hypofunction and addisonian crisis.
- Adverse effects of adrenocortical activity. The nurse assesses fluid and electrolyte status by monitoring laboratory values and daily weights.
To detect Cushing’s syndrome, the following are performed:
- Low-dose dexamethasone suppression test. Dexamethasone (1 mg) is administered orally at 11pm, and a plasma cortisol level is obtained at 8am the next morning, and this usually confirms the diagnosis of Cushing’s syndrome.
- Stimulation test. In a stimulation test, administration of metyrapone, which blocks cortisol production by the adrenal glands, tests the ability of the pituitary gland and hypothalamus to detect and correct low levels of plasma cortisol by increasing corticotropin production.
- Imaging studies. Ultrasound, CT scan , or angiography localizes adrenal tumors and may identify pituitary tumors.
- Electrolyte levels. A patient with Cushing’s syndrome include an increase in serum sodium and a decrease in potassium levels.
- Blood studies. Indicators of Cushing’s syndrome include an increase in the blood glucose levels, a reduction in the number of eosinophils, and disappearance of lymphoid tissue.
Medical Management
Treatment to restore hormonal balance and reverse Cushing’s syndrome may necessitate radiation , drug therapy, or surgery .
- Pituitary irradiation. Patients with pituitary-dependent Cushing’s syndrome with adrenal hyperplasia and severe cushingoid symptoms (such as psychosis, poorly controlled diabetes mellitus , osteoporosis , and severe pathologic fractures) may require pituitary irradiation.
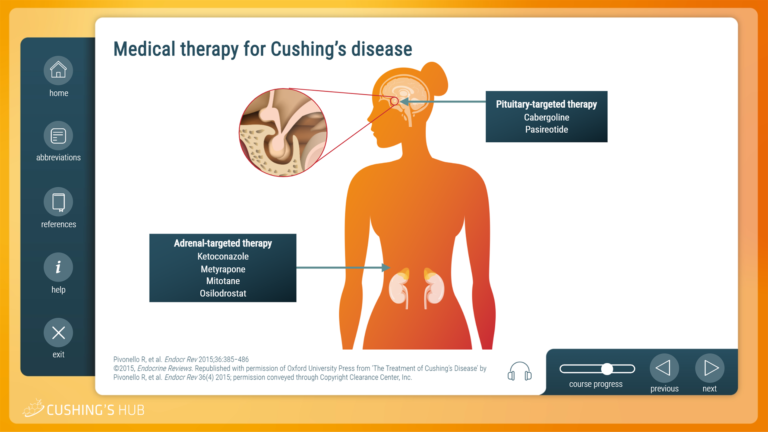
Following the prescribed drug therapy could necessitate recovery.
- Adrenal enzyme inhibitors. Metyrapone , aminoglutethimide , mitotane , and ketoconazole may be used to reduce hyperadrenalism if the syndrome is caused by ectopic ACTH secretion by a tumor that cannot be eradicated.
- Cortisol therapy. Cortisol therapy is essential during and after surgery, to help the patient tolerate the physiologic stress imposed by the removal of the pituitary or adrenals.
Removal of the adrenal or pituitary gland offers a greater success rate for the recovery of the patient.
- Transsphenoidal hypophysectomy. Surgical removal of the tumor by transsphenoidal hypophysectomy is the treatment of choice if Cushing’s syndrome is caused by pituitary tumors and has an 80% success rate.
- Adrenalectomy . Adrenalectomy is the treatment of choice in patients with primary adrenal hypertrophy.
Nursing Management
The nurse must closely monitor the patient with Cushing’s syndrome to avoid complications.
Assessment focus on the effects on the body of high concentrations of adrenal cortex to respond to changes in cortisol and aldosterone levels.
- Health history. The history includes information about the patient’s level of activity and ability to carry out routine and self-care activities.
- Physical exam. The skin is observed and assessed for trauma, infection, breakdown, bruising, and edema .
- Mental function. The nurse assesses the patient’s mental function including mood, responses to questions, awareness of environment, and level of depression.
Based on the assessment data, the major nursing diagnoses of the patient with Cushing’s syndrome include:
- Risk for injury related to weakness.
- Risk for infection related to altered protein metabolism and inflammatory response.
- Self-care deficit related to weakness, fatigue, muscle wasting, and altered sleep patterns.
- Impaired skin integrity related to edema, impaired healing, and thin and fragile skin.
- Disturbed body image related to altered physical appearance, impaired sexual functioning, and decreased activity level.
- Disturbed thought processes related to mood swings, irritability, and depression.
The major nursing goals for the patient include:
- Decrease risk of injury.
- Decrease risk of infection.
- Increase ability to carry out self-care activities.
- Improve skin integrity .
- Improve body image.
- Improve mental function.
Nursing interventions for a patient with Cushing’s syndrome include:
Decreasing Risk of Injury
- Provide a protective environment to prevent falls, fractures, and other injuries to bones and soft tissues.
- Assist the patient who is weak in ambulating to prevent falls or colliding into furniture.
- Recommend foods high in protein, calcium , and vitamin D to minimize muscle wasting and osteoporosis; refer to dietitian for assistance.
Decreasing Risk of Infection
- Avoid unnecessary exposure to people with infections.
- Assess frequently for subtle signs of infections (corticosteroids mask signs of inflammation and infection).
Preparing Patient for Surgery
- Monitor blood glucose levels, and assess stools for blood because diabetes mellitus and peptic ulcer are common problems
Encouraging Rest and Activity
- Encourage moderate activity to prevent complications of immobility and promote self-esteem.
- Plan rest periods throughout the day and promote a relaxing, quiet environment for rest and sleep .
Promoting Skin Integrity
- Use meticulous skin care to avoid traumatizing fragile skin.
- Avoid adhesive tape, which can tear and irritate the skin.
- Assess skin and bony prominences frequently.
- Encourage and assist patient to change positions frequently.
Improving Body Image
- Discuss the impact that changes have had on patient’s self-concept and relationships with others. Major physical changes will disappear in time if the cause of Cushing syndrome can be treated.
- Weight gain and edema may be modified by a low-carbohydrate, low-sodium diet; a high-protein intake can reduce some bothersome symptoms.
Improving Thought Processes
- Explain to patient and family the cause of emotional instability, and help them cope with mood swings, irritability, and depression.
- Report any psychotic behavior.
- Encourage patient and family members to verbalize feelings and concerns.
Monitoring and Managing Complications
- Adrenal hypofunction and addisonian crisis: Monitor for hypotension ; rapid, weak pulse; rapid respiratory rate; pallor; and extreme weakness. Note factors that may have led to crisis (eg, stress, trauma, surgery).
- Administer IV fluids and electrolytes and corticosteroids before, during, and after surgery or treatment as indicated.
- Monitor for circulatory collapse and shock present in addisonian crisis; treat promptly.
- Assess fluid and electrolyte status by monitoring laboratory values and daily weight.
- Monitor blood glucose level, and report elevations to physician.
- Acute adrenal crisis is a life-threatening condition that occurs when there is not enough cortisol, a hormone produced by the adrenal glands.
Teaching Patients Self-Care
- Present information about Cushing syndrome verbally and in writing to patient and family.
- If indicated, stress to patient and family that stopping corticosteroid use abruptly and without medical supervision can result in adrenal insufficiency and reappearance of symptoms.
- Emphasize the need to keep an adequate supply of the corticosteroid to prevent running out or skipping a dose, because this could result in addisonian crisis.
- Stress the need for dietary modifications to ensure adequate calcium intake without increasing risk for hypertension , hyperglycemia, and weight gain .
- Teach patient and family to monitor blood pressure , blood glucose levels, and weight.
- Stress the importance of wearing a medical alert bracelet and notifying other health professionals that he or she has Cushing syndrome.
- Refer for home care as indicated to ensure safe environment with minimal stress and risk for falls and other side effects.
- Emphasize importance of regular medical follow up, and ensure patient is aware of side and toxic effects of medications.
Expected patient outcomes may include the following:
- Improve skin integrity.
The patient and the family should be informed that adrenal insufficiency and underlying symptoms may recur if discharge orders are not complied.
- Medication. Instruct the patient not to stop corticosteroid abruptly and without medical supervision because the syndrome could recur, so the patient should always have an adequate supply of the corticosteroid medication to avoid running out.
- Diet. The nurse stresses the need for dietary modifications to ensure adequate calcium intake without increasing the risk for hypertension, hyperglycemia, and weight gain.
- Monitoring. The patient and family can be taught to monitor blood pressure, blood glucose levels, and weight.
- Follow up appointment. The nurse should emphasize the importance of regular medical follow-ups, the side effects of medications, and the need to wear medical identification with Addison’s and Cushing’s disease.
The focus of documentation should include:
- Client’s/ caregiver ‘s understanding of individual risks and safety concerns.
- Availability and use of resources.
- Recent or current antibiotic therapy.
- Signs and symptoms of infectious process.
- Functional level and specifics of limitations.
- Needed resources and adaptive devices.
- Plan of care and who is involved in planning .
- Teaching plan.
- Individual responses to interventions, teaching, and actions performed.
- Specific actions and changes made.
- Attainment or progress towards desired outcomes.
- Modifications to the plan of care.
Here’s a 5-item quiz about the study guide . Please visit our nursing test bank page for more NCLEX practice questions .
1. A positive diagnosis of Cushing’s syndrome is associated with:
A. The disappearance of lymphoid tissue. B. A reduction in circulating eosinophils. C. An elevated cortisol level. D. All of the above.
2. Clinical manifestations of Cushing’s syndrome may be modified with a diet that is:
A. High in protein. B. Low in carbohydrates. C. Low in sodium. D. All of the above.
3. Confirmatory diagnosis of Cushing’s syndrome is made through:
A. Transsphenoidal hypophysectomy. B. Adrenalectomy. C. Low-dose dexamethasone suppression test. D. Stimulation test.
4. Nursing interventions appropriate for a patient with Cushing’s syndrome include:
A. Monitoring fluid intake and output . B. Administering foods rich in sodium. C. Stopping corticosteroid intake once symptoms have diminished D. All of the above
5. What is included in the Cushing’s triad?
A. Buffalo hump. B. Moonface. C. Truncal obesity. D. All of the above
Answers and Rationale
1. Answer: D. All of the above.
- D: Cushing’s syndrome is associated with the disappearance of lymphoid tissue, reduction in circulating eosinophils, and an elevated cortisol level.
- A, B, C: These laboratory values are present in a patient with Cushing’s syndrome.
2. Answer: D. All of the above.
- D: Weight gain and edema may be modified by a low-carbohydrate, low sodium diet, and a high protein intake may reduce some of the other bothersome symptoms.
- A, B, C: Incorporating the following in the diet could help modify the clinical manifestations of Cushing’s syndrome.
3. Answer: C. Low-dose dexamethasone suppression test.
- C: Dexamethasone (1mg) is administered orally at 11pm, and a plasma cortisol level is obtained at 8am the next morning, and this usually confirms the diagnosis of Cushing’s syndrome.
- A: Transsphenoidal hypophysectomy is the surgical removal of the pituitary tumor.
- B: Adrenalectomy is the treatment of choice in patients with primary adrenal hypertrophy.
- D: In a stimulation test, administration of metyrapone, which blocks cortisol production by the adrenal glands, tests the ability of the pituitary gland and hypothalamus to detect and correct low levels of plasma cortisol by increasing corticotropin production.
4. Answer: A. Monitoring fluid intake and output.
- A: The patient with Cushing’s syndrome retains sodium and water, so careful monitoring of the intake and output should be performed.
- B: Foods that are low in sodium should be given to the patient to further avoid edema.
- C: It is not recommended to stop corticosteroid abruptly and without medical supervision because symptoms may recur.
- D: Not all of the options are correct.
5. Answer: D. All of the above
- D: All of the options are part of the Cushing’s triad
- A, B, C: Cushing’s triad includes buffalo hump, moon face, and truncal obesity.
Related posts:
- Endocrine Medications NCLEX Practice Quiz (20 items)
- Endocrine Disorders NCLEX Practice Quiz 1 (50 Items)
- Hypothyroidism
Leave a Comment Cancel reply

IMAGES
VIDEO
COMMENTS
The diagnosis is often delayed because Cushing's is frequently masked by its overlap with more common medical problems such as diabetes, high blood pressure, obesity, and polycystic ovary syndrome. Cushing's may be more common than previously thought. In this case, a 32-year-old female was ill for at least one and a half years before diagnosis.
Case Study: Addison's Disease. NUR 3219C. Keiser University. Differentiate between Cushing's syndrome and Cushing's disease. Cortisol is a hormone normally made by the adrenal glands and is necessary for life. Cushing's syndrome refers to the condition caused by excess cortisol in the body, regardless of the cause.
A population-based study in Denmark reported the incidence of adrenal adenoma as 0.6 and adrenal carcinoma as 0.2 per million per year . In 1.3 to 8.7 percent of adults AT are discovered incidentally. ... followed by treatment for CS as we did in case 5, while severe Cushing's syndrome, when diagnosed in the 1st trimester of pregnancy, ...
In most case series of Cushing's syndrome, an average of 8% of patients have adrenal carcinoma. 21 If 6 per million is 8% of the group, the total Cushing's syndrome group is 75 persons per ...
BP 156/92. RR 14. Temp 98.8°F. The nurse notes purple/pink stretch marks on arms, abdomen, and thighs. Ms. Smith has multiple cuts and bruises on her arms. When asked how she got them, she says "my skin is just so thin these days". She is obese with noticeable fatty deposits in the midsection and upper back.
Introduction: Cushing's syndrome is caused by an extended exposure to increased levels of endogenous or exogenous glucocorticoids. It is a syndrome that can be extremely challenging to diagnose as many symptoms and signs are also indications of other disease processes. ... Case: A 76 year old man presented to hospital with a six month history ...
Purpose: To present a case study of a 34-year-old woman with Cushing's disease and provide nurse practitioners (NPs) with the understanding of the clinical presentation needed for early recognition and treatment of the disease. Data sources: A comprehensive review of published literature on Cushing's disease. Findings from history, physical examination, and diagnostic studies of a woman ...
An interactive case study on the differential diagnosis of Cushing's syndrome. This module looks at the diagnostic strategy required to establish the cause of adrenocorticotrophic hormone (ACTH)-dependent Cushing's syndrome, when imaging and biochemical results are inconclusive. Go to case study. Posted on October 11, 2022.
Abstract. Cushing's syndrome (CS) is considered a rare disease. The most common cause is the exogenous use of glucocorticoids (GCs), which are often given within a controlled medical setting, but their factitious use is rare. Factitious CS is more common in females, young patients, those with psychiatric disorders, and those with contacts ...
CUSHING SYNDROME (CASE STUDY #2) M. is a 34-year-old male elementary school teacher. He seeks the advice of his HCP because of changes in his appearance over the past year. SUBJECTIVE DAT A: Reports weight gain (mainly through the midsection), easy bruising, and edema of his feet, lower legs, and hands. He has increasing weakness and insomnia.
Definition. Cushing syndrome is an endocrine disease with multiple etiologies and is characterized by a constellation of clinical manifestations that result from excessive concentrations of circulat-ing cortisol (i.e., hypercortisolism). The syndrome is named after Harvey Cushing, an American surgeon who first reported the condition in 1912.
The urinary free cortisol (UFC) test is widely used for the screening of Cushing's syndrome. This case study illustrates the potential failure of the UFC test to correctly diagnose Cushing's disease (CD), indicating that the use of other complementary tests may be necessary to diagnose this disease in some cases.
In one series, Cushing's syndrome occurred in 3 of 16 patients with the multiple endocrine neoplasia syndrome and the Zollinger-Ellison syndrome (16 percent). 8 In these cases, mild Cushing's ...
The study analyzed death data from more than 19,000 patients in 92 studies published through January 2021. "Our results found that death rates have fallen since 2000 but are still unacceptably high," Limumpornpetch said. Cushing's syndrome affects many parts of the body because cortisol responds to stress, maintains blood pressure and ...
Cushing syndrome is a rare disease that rarely presents as acute psychosis. In this case, the patient presented with acute psychosis and agitation as the first manifestations of the disease which led to the admission of the patient to a psychiatry hospital for one month, as it was difficult to restrain her sufficiently for performing appropriate diagnostic tests due to disturbing behavior.
A probabilistic model for Cushing's syndrome screening in at-risk populations: a prospective multicenter study. J Clin Endocrinol Metab. 2016;101(10):3747-3754. doi pubmed; Lindholm J, Juul S, Jorgensen JO, Astrup J, Bjerre P, Feldt-Rasmussen U, Hagen C, et al. Incidence and late prognosis of cushing's syndrome: a population-based study.
Cushing syndrome is the prolonged time of having cortisol in the blood. Cushing disease is when the pituitary gland secreates too much ACTH. CHAPTER 7 ENDOCRINE DISORDERS CASE STUDY 77
Case Study 77 Cushing Syndrome Scenario You graduated 3 months ago and are working with a home care agency. One patient in your caseload is J.S., a 60-year-old man with chronic obstructive pulmonary disease (COPD) related to cigarette smoking. He has been on home oxygen, 2L oxygen by nasal cannula, for several years. Approximately 10 months ago, he started on chronic oral steroid therapy.
Abstract. Cushing syndrome results from supraphysiological exposure to glucocorticoids and is associated with significant morbidity and mortality. The pathogenesis includes administration of corticosteroids (exogenous Cushing syndrome) or autonomous cortisol overproduction, whether or not ACTH-dependent (endogenous Cushing syndrome). An early ...
Case Study 77 Cushings Syndrome.docx - Scenario You... Doc Preview. Pages 5. Identified Q&As 20. Solutions available. Total views 100+ Iowa Western Community College. CIS. ... View Cushing Syndrome Case Study.docx from BIOL 248L at University of New Mexico, Main... CASE STUDY Cushing disease.docx. Taylor College. NUR 2716. Cortisol. digoxin.
Causes and Diagnosis. If Cushing's syndrome is suspected on the basis of the patient's physical appearance, the diagnostic workup should include a thorough medical history, physical exam, and 1 or more of the following tests to establish hypercortisolism: the 24-hour urinary cortisol test, the low-dose dexamethasone suppression test, or the late-night salivary cortisol test.
Cushing's syndrome is a disorder of the endocrine system. Cushing's syndrome (Cushing's disease, Hypercortisolism, Adrenal Hyperfunction) is a cluster of clinical abnormalities caused by excessive levels of adrenocortical hormones (particularly cortisol) or related corticosteroids and, to a lesser extent, androgens and aldosterone.