An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Subst Abuse
- PMC10176789

The Impact of Recreational Cannabis Legalization on Cannabis Use and Associated Outcomes: A Systematic Review
Kyra n farrelly.
1 Department of Psychology, York University, Toronto, ON, Canada
2 Peter Boris Centre for Addictions Research, St. Joseph’s Healthcare Hamilton, McMaster University, Hamilton, ON, Canada
Jeffrey D Wardell
3 Institute for Mental Health Policy Research, Centre for Addiction and Mental Health, Toronto, ON, Canada
4 Department of Psychiatry, University of Toronto, Toronto, ON, Canada
Emma Marsden
Molly l scarfe, peter najdzionek, jasmine turna.
5 Michael G. DeGroote Centre for Medicinal Cannabis Research, McMaster University & St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
James MacKillop
6 Homewood Research Institute, Guelph, ON, Canada
Background:
Recreational cannabis legalization has become more prevalent over the past decade, increasing the need to understand its impact on downstream health-related outcomes. Although prior reviews have broadly summarized research on cannabis liberalization policies (including decriminalization and medical legalization), directed efforts are needed to synthesize the more recent research that focuses on recreational cannabis legalization specifically. Thus, the current review summarizes existing studies using longitudinal designs to evaluate impacts of recreational cannabis legalization on cannabis use and related outcomes.
A comprehensive bibliographic search strategy revealed 61 studies published from 2016 to 2022 that met criteria for inclusion. The studies were predominantly from the United States (66.2%) and primarily utilized self-report data (for cannabis use and attitudes) or administrative data (for health-related, driving, and crime outcomes).
Five main categories of outcomes were identified through the review: cannabis and other substance use, attitudes toward cannabis, health-care utilization, driving-related outcomes, and crime-related outcomes. The extant literature revealed mixed findings, including some evidence of negative consequences of legalization (such as increased young adult use, cannabis-related healthcare visits, and impaired driving) and some evidence for minimal impacts (such as little change in adolescent cannabis use rates, substance use rates, and mixed evidence for changes in cannabis-related attitudes).
Conclusions:
Overall, the existing literature reveals a number of negative consequences of legalization, although the findings are mixed and generally do not suggest large magnitude short-term impacts. The review highlights the need for more systematic investigation, particularly across a greater diversity of geographic regions.
Introduction
Cannabis is one of the most widely used substances globally, with nearly 2.5% of the world population reporting past year cannabis use. 1 Cannabis use rates are particularly high in North America. In the U.S., 45% of individuals reported ever using cannabis and 18% reported using at least once annually in 2019. 2 , 3 In Canada, approximately 21% of people reported cannabis use in the past year use in 2019. 4 In terms of cannabis use disorder (CUD), a psychiatric disorder defined by clinically significant impairment in daily life due to cannabis use, 5 ~5.1% of the U.S. population ages 12+ years met criteria in 2020, with ~13.5% of individuals ages 18 to 25 years meeting criteria. 6
Overall, rates of cannabis use have shown long-term increasing trends among several age groups in North America. 7 - 9 Moreover, research has revealed recent cannabis use increases in at risk populations, such as individuals with depression and pregnant women. 10 , 11 Parallel to increased cannabis use over time, rates of cannabis-related consequences have also increased across Canada and the U.S., including cannabis dependence and CUD, 8 , 12 crime rates (eg, increased possession charges), 8 and cannabis-impaired driving (and, lower perception of impairment and risk from cannabis use). 11 , 13 , 14 Further, cannabis use poses a risk for early-onset or use during adolescence as there is evidence that cannabis use in adolescence is linked with poorer cognitive performance, psychotic disorders, and increased risk of mood and addictive disorders. 15 With the rates of negative consequences from cannabis use increasing, particularly in North America where cannabis has become legal in many parts of the US and all of Canada, understanding the role of cannabis legalization in these changes is crucial to inform ongoing changes in cannabis policies worldwide.
The legal status of cannabis varies widely across countries and regions. Although cannabis is largely illegal at the global level, policies surrounding cannabis use are becoming steadily liberalized. Decriminalization (reduced penalties for self-use but not distribution) is more widespread worldwide, including in the Netherlands, Portugal, and parts of Australia. Medical legalization is also seen in Peru, Germany, New Zealand, the Netherlands and across many U.S. states. To date, Canada, Uruguay, and Malta are the only 3 countries to legalize recreational cannabis use at the national level. Further, individual U.S. states began legalizing recreational cannabis in 2012, with nearly half of U.S. states having legalized recreational cannabis by 2023. As national and subnational recreational legalization continues to gain support and take effect, understanding the consequences of such major regulatory changes is crucial to informing ongoing policy changes.
There are arguments both for and against recreational cannabis legalization (RCL). Common pro-legalization arguments involve increasing regulatory control over product distribution, weakening organized crime, reducing burden and inequality in the criminal justice system, and generating economic benefits such as tax revenues and commercial activity. 16 Furthermore, as cannabis obtained from illicit markets is of varying and unknown potency, 17 cannabis legalization may help better regulate the potency and quality of cannabis products. 18 On the other hand, there are anti-legalization arguments such as the possibility of legalization leading to increased use among youth and increased cannabis-impaired driving. 16 A nationally representative survey in the U.S. found that pro-legalization arguments were perceived to be more persuasive than public health anti-legalization arguments in a U.S. nationally representative survey, 19 suggesting policymaker concerns regarding RCL do not seem to hold as much weight in the general public. However, while research may be increasing surrounding the impacts of RCL, the general consensus of if RCL leads to more positive or negative consequences is unclear.
With RCL becoming more prevalent globally, the impacts it may have on a variety of health-related outcomes are of critical importance. Prevalence of cannabis use is of course a relevant issue, with many concerned that RCL will cause significant spikes in rates of cannabis use for a variety of groups, including youth. However, current studies have revealed mixed evidence in the U.S., 20 , 21 thus there is a need to synthesize the extant literature to better understand the balance of evidence and potential impacts of RCL across different samples and more diverse geographic areas. Another common question about RCL is whether it will result in changes in attitudes toward cannabis. These changes are of interest as they might forecast changes in consumption or adverse consequences. Similarly, there are concerns surrounding RCL and potential spill-over effects that may influence rates of alcohol and other substance use. 22 Thus, there remains a need to examine any changes in use of other substance use when studying effects of RCL.
Beyond changes in cannabis and other substance use and attitudes, health-related impacts of RCL are important to consider as there are links between cannabis use and adverse physical and mental health consequences (eg, respiratory and cardiovascular diseases, psychosis). 23 Additionally, emergency service utilization associated with cannabis consumption is a frequent concern associated with RCL, particularly due to the spikes in admissions following RCL in Colorado. 24 However, the rates of cannabis-related emergency service admissions more globally (eg, in legal countries like Canada and Uruguay) have not been fully integrated into summaries of the current literature. Finally, another health-related consequence of RCL is potential impacts on opioid use. While opioid-related outcomes can fall into substance use, they are considered health-related for this review as much of the discussion surrounding RCL and opioids involve cannabis substituting opioid use for medicinal reasons or using cannabis as an alternate to prescription opioids in the healthcare system. The current opioid crisis is a global public health problem with serious consequences. While there is evidence that medicinal cannabis may reduce prescription opioid use 25 and that cannabis may be a substitute for opioid use, 26 the role of recreational cannabis legalization should also be examined as the 2 forms of cannabis use are not interchangable 27 and have shown unique associations with prescription drug use. 28 Thus, there is a need to better understand how and if RCL has protective or negative consequences on opioid-related outcomes.
Due to the impairing effects of cannabis on driving abilities and the relationship with motor vehicle accidents, 29 another important question surrounding RCL is how these policy changes could result in adverse driving-related outcomes. An understanding of how RCL could influence impaired driving prevalence is needed to give insight into how much emphasis jurisdictions should put on impaired driving rates when considering RCL implementation. A final consequence of RCL that is often debated but requires a deeper understanding is how it impacts cannabis-related arrest rates. Cannabis-related arrests currently pose a significant burden on the U.S. and Canadian justice system. 30 , 31 Theoretically, RCL may ease the strain seen on the justice system and have positive trickle-down effects on criminal-related infrastructure. However, the overall implications of RCL on arrest rates is not well understood and requires a systematic evaluation. With the large number of RCL associated outcomes there remains a need to synthesize the current evidence surrounding how RCL can impact cannabis use and other relevant outcomes
Present review
Currently, no reviews have systematically evaluated how RCL is associated with cannabis-use changes across a variety of age groups as well as implications on other person- or health-related outcomes. The present review aims to fill an important gap in the literature by summarizing the burgeoning research examining a broad range of consequences of RCL across the various jurisdictions that have implemented RCL to date. Although previous reviews have considered the implications of RCL, 32 , 33 there has recently been a dramatic increase in studies in response to more recent changes in recreational cannabis use policies, requiring additional efforts to synthesize the latest research. Further, many reviews focus on specific outcomes (eg, parenting, 34 adolescent use 35 ). There remains a need to systematically summarize how RCL has impacted a variety of health-related outcomes to develop a more comprehensive understanding of the more negative and positive outcomes of RCL. While a few reviews have examined a broad range of outcomes such as cannabis use, related problems, and public health implications, 32 , 33 some reviews have been limited to studies from a single country or published in a narrow time window. 32 Thus, a broader review is necessary to examine multiple types of outcomes from studies in various geographic regions. Additionally, a substantial amount of the current literature examining the impact of RCL relies on cross-sectional designs (eg, comparing across jurisdictions with vs without recreational legalization) which severely limit any conclusions about causal associations. Thus, given its breadth, the current systematic review is more methodologically selective by including only studies with more rigorous designs (such as longitudinal cohort studies), which provide stronger evidence regarding the effects of RCL. In sum, the aim of the current review was to characterize the health-related impacts of RCL, including changes in these outcomes in either a positive or negative direction.
The review is compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 36 ). Full-text extraction was initiated immediately following article search, therefore the protocol was not registered with PROSPERO. Relevant articles on cannabis legalization were principally identified using the Boolean search terms (“cannabis” OR “marijuana” OR “THC” OR “marihuana”) AND “legalization” AND (“recreational” OR “non-medical” OR “nonmedical”) AND (“longitudinal” OR “pre-post” OR “prospective” OR “timeseries” OR “cohort”). The search was conducted using PubMed/MEDLINE, EMBASE, and PsycINFO through November 2022. Relevant studies identified through secondary means (eg, prior knowledge of a relevant publication, articles brought to the authors’ attention) were also included for screening. Titles and abstracts resulting from the initial search were screened in Covidence (Veritas Health Innovation Inc) by 2 reviewers for suitability for full-text review and final inclusion. Conflicts were discussed by both reviewers and a final decision was made by consensus. Following screening, reviewers read and extracted relevant data. To be included, an article was required to meet the following criteria: (i) an original empirical research article published in a peer-reviewed journal; (ii) written in (or available in) English; (iii) RCL serves as an independent variable; (iv) quantitative study design that clearly permitted the evaluation of the role of RCL with a more rigorous non-cross-sectional study design (eg, pre- vs post-legalization, longitudinal, cohort, interrupted time series, etc.); and (v) reports on health-related outcomes (ie, changes in consumption or attitudes, as opposed to changes in price or potency).
RCL related outcomes that were considered were those specifically involving the behavior, perceptions, and health of individuals. Population-level outcomes (eg, health-care utilization or impaired driving) were considered eligible for inclusion as they involve the impacts that legalization has on individual behavior. Thus, economic- or product-level outcomes that do not involve individual behavior (eg, cannabis prices over time, changes in cannabis strain potency) were considered out of scope. The outcome groups were not decided ahead of time and instead 5 main themes in outcomes emerged from our search and were organized into categories for ease of presentation due to the large number of studies included.
Studies that examined medicinal cannabis legalization or decriminalization without recreational legalization, and studies using exclusively a cross-sectional design were excluded as they were outside the scope of the current review. The study also excluded articles that classified RCL as the passing of legal sales rather than implementation of RCL itself as RCL is often distinct from introduction of legal sales, or commercialization. Thus, we excluded studies examining commercialization as they were outside the scope of the current review.
Characteristics of the literature
The search revealed 65 relevant articles examining RCL and related outcomes (see Figure 1 ). There were 5 main themes established: cannabis use and other substance use behaviors ( k = 28), attitudes toward cannabis ( k = 9), health-related outcomes ( k = 33), driving related impacts ( k = 6), and crime-related outcomes ( k = 3). Studies with overlapping themes were included in all appropriate sections. Most studies (66.2%) involved a U.S. sample, 32.3% examined outcomes in Canada, and 1.5% came from Uruguay. Regarding study design, the majority (46.2%) utilized archival administrative data (ie, hospital/health information across multiple time points in one jurisdiction) followed by cohort studies (18.5%). The use of administrative data was primarily used in studies examining health-related outcomes, such as emergency department utilization. Studies examining cannabis use or attitudes over time predominantly used survey data. Finally, both driving and crime related outcome studies primarily reported findings with administrative data.

Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) study flow diagram.
Changes in cannabis and other substance use
Cannabis and other substance use changes represented the second largest number of studies, with 28 articles identified. Studies examining changes in cannabis use behaviors were divided by subpopulation (ie, adolescents, young adults, general population adults, clinical populations, and maternal use; see Table 1 ). Finally, we separately summarized studies reporting changes in concurrent use of other substances, and routes of cannabis administration.
Studies investigating the role of recreational cannabis legalization on cannabis and other substance consumption.
Author, author of article; Year, publication year of article; Location, jurisdiction article data was collected in; Date of Legalization, year legalization was enacted in jurisdiction; Sample, total N of article sample; RCL, Recreational Cannabis Legalization.
Cannabis use changes in adolescents (~12-17)
Ten studies examined changes in cannabis use among adolescents and found that changes in the rates of use were inconsistent following RCL. Gunadi et al 37 found an association between RCL and more pronounced transition from non-use to cannabis use when compared to states with no legalization and those with medical cannabis legalization ( P ⩽ .001) combined, but not when compared to states with medical cannabis legalization only. Another study found that in states with RCL adolescents who never used cannabis but used e-cigarettes were more likely to use cannabis at follow-up than those living in states without RCL (aOR = 18.39, 95% CI: 4.25-79.68vs aOR = 5.09, 95% CI: 2.86-9.07, respectively) suggesting a risk of cannabis initiation among legal states. 38 Among adolescents reporting recent alcohol and cannabis co-use, one study found a significant increase in the frequency of past 30-day cannabis use following RCL ( b = 0.36, SE = 0.07, P ⩽ .001). 39 In a Canadian study using a repeated cross-sectional design as well as a longitudinal design to examine changes in cannabis use, results revealed that adolescents had increased odds of ever using cannabis in the year following RCL in the cross-sectional data ( P = .009). 40 However, the longitudinal sample revealed no significant differences in the odds of ever use, current use, and regular use of cannabis post-legalization. There is also evidence of RCL impacts on adolescent cannabis use consequences, as a Washington study found a significant indirect effect of RCL on cannabis consequences through perceived risk as a mediator ( B = 0.37, P ⩽ .001). 41
On top of the above evidence, there were multiple studies examining cannabis use changes over time among adolescents in Washington and Oregon that found higher rates of cannabis use associated with cohorts examined during RCL compared to non-legal cohorts, 42 - 44 although the differences across legal cohorts were not significant in all cases. 42 Furthermore, in another study, RCL did not impact initiation of use, but for current users the RCL group had significantly greater increased rates of cannabis use compared to the pre-RCL group (RR = 1.26, 95% CI = 1.10, 1.45). 43 For the final study, cannabis use increased in the post-RCL group but patterns of use (frequency; daily vs weekly use) were similar across groups. 44 Overall, the preceding 8 studies reveal some evidence that RCL was associated with increasing rates of cannabis use in adolescent. However, 5 studies point to some inconsistent associations of RCL and cannabis use and suggest that overall relationship of RCL and adolescent cannabis as mixed.
Three studies add to these inconsistent findings and point to lack of an association between RCL and changes in cannabis use among adolescents. Two studies found no significant increase in the frequency of or prevalence of cannabis use following RCL. 41 , 45 Finally, a study examining trends of adolescent cannabis use and associations with period effects (ie, external world events that could influence use) suggests laws and regulations associated with RCL were not associated with cannabis use changes. 46 The current research reveals conflicting evidence about the role of RCL on adolescent cannabis use.
Cannabis use changes in young adults (~18-25)
Young adulthood, typically defined as ages 18 to 25 and also known as emerging adulthood, is commonly associated with decreased parental supervision, increased availability of substances, and greater substance experimentation making it a key developmental period for the onset of cannabis use. 47 Four studies examined the impact of RCL on cannabis use among young adults, 2 of which found significant associations between RCL and increased cannabis use in college students. 47 , 48 Barker and Moreno 48 found the rate of students ever using cannabis did not change. However, in those who had used cannabis prior to RCL, the proportion of students using in the past 28-days increased faster following RCL in Washington (legal-state) when compared with the rate of increase in Wisconsin (non-legal state; P ⩽ .001). 48 Further, in college students from Oregon, rates of cannabis use increased significantly from before to after RCL ( P = .0002). 47 Another study looked at changes in cannabis use in a sample of young adults from the U.S. who had never vaped cannabis at the time of recruitment. 49 Results revealed that cannabis use in the past year did not differ in states with or without RCL, although, those living in states with RCL did show a larger increase in rates of cannabis vaping across time, compared to those in non-RCL states. Finally, in a sample of youth from Oregon and Washington, RCL predicted a higher likelihood of past-year cannabis use ( P = .001). 50 In contrast to the adolescent literature, studies examining cannabis use in young adult samples fairly consistently point to an association between RCL and increasing rates of cannabis use.
Cannabis use changes in general population adults
Five studies examined changes in cannabis use in adults (without further age subclassification) associated with RCL. Four of these studies suggested higher rates of cannabis use in adults for RCL jurisdictions compared to non-legal states post-RCL, or increased use following RCL. 37 , 45 , 51 , 52 Past 30-day cannabis use increased significantly 1-month post-RCL and remained elevated 6-months post-RCL (ps = 0.01) in a sample of adults from California. 51 Another study found an association between RCL and transition from non-users to cannabis users and non-users to weekly users when compared to states with no medical legalization or RCL ( P ⩽ .001) and states with no legalization combined with those with medical cannabis legalization ( P ⩽ .001). 37 Meanwhile, in Canada, a significant increase in prevalence of cannabis use was observed following RCL. 45 Additionally, in those reporting no cannabis use prior to RCL in Canada, there were significant increases in cannabis use frequency, quantity of cannabis used, and severity of cannabis misuse following RCL. 52 The opposite pattern was seen for those reporting cannabis use prior to RCL, with significant decreases in frequency of use, quantity, and misuse. 52 However, not all studies found RCL was associated with increased cannabis use. For instance, a repeated cross-sectional study of adult in the U.S. found no association between RCL and frequency of cannabis use. 53
A benefit of the extant literature examining general population cannabis use is that it covers a variety of jurisdictions and study designs, albeit with some heterogeneity and mixed findings. On balance, the evidence within the current literature, generally suggests an increase in cannabis use for adults in the general population following RCL with 80% of the reviewed studies supporting this conclusion.
Maternal use
Three studies examined whether rates of cannabis use during pregnancy have increased following RCL. Two studies suggested increased cannabis use during pregnancy associated with RCL. In one study urine screen-detected cannabis use during pregnancy increased from 6% to 11% following RCL in California ( P = .05). 54 Another study in a sample of women participating in an intensive case management program for heavy alcohol and/or drug use during pregnancy, examined cannabis use among those exiting from the program before versus after RCL. Findings revealed women exiting after RCL were more likely to report using cannabis in the 30 days prior to exit compared to those pre-RCL (OR = 2.1, P ⩽ .0001). 55 One study revealed no significant difference in cannabis or alcohol use associated with RCL in women living with HIV during pregnancy or the postpartum period. 56 Overall, the evidence from these three studies suggests there may be increases in perinatal cannabis use following RCL, but the small number of studies and unique features of the samples suggests a need for more research.
Clinical populations use
Six studies examined cannabis use in clinical populations. One study investigated use and trauma admissions for adults and pediatric patients in California. 57 Results showed an increase in adult trauma patients with THC+ urine tests from pre- to post-RCL (9.4% to 11.0%; P = .001), but no difference for pediatric trauma patients. A study based in Colorado and Washington, found that cannabis use rates in inflammatory bowel disease patients significantly increased from 107 users to 413 ( P ⩽ .001) pre to post-RCL. 58 A Canada-based study of women with moderate-to-severe pelvic pain found an increase in the prevalence of current cannabis use following RCL (13.3% to 21.5%; P ⩽ .001). 59 Another Canadian study showed an increase in the prevalence of current cannabis use after RCL among cancer patients (23.1% to 29.1%; P ⩽ .01). 60 Finally, two studies examined changes in cannabis use among individuals receiving treatment for a substance use disorder. In a sample of Canadian youth in an outpatient addictions treatment program, there was no change in the rate of cannabis use following RCL. 61 Further, in a sample of individuals receiving treatment for opioid use disorder, cannabis use was compared for those recruited 6 months before or after RCL with no significant changes in the prevalence or frequency of self-reported ( P = .348 and P = .896, respectively) or urine screen-detected ( P = .087 and P = .638, respectively) cannabis use following RCL. 62 Although these studies only represent a small number of observations, their findings do reveal associations between RCL and increasing cannabis use within some clinical samples.
Changes in polysubstance and other substance use
One study examined simultaneous cannabis and alcohol use among 7th, 9th, and 11th grade students in the U.S. 39 This study found that RCL was associated with a 6% increase in the odds of past 30-day alcohol and cannabis co-use. The association was even stronger in students with past 30-day alcohol use and heavy drinking. However, among past 30-day cannabis users, RCL was associated with a 24% reduction in co-use. This study suggests at least a modest association between RCL and concurrent cannabis and alcohol use among adolescents.
Numerous studies examined changes of alcohol and other substance use pre to post RCL. With regard to alcohol, one study from Colorado and Washington found a decrease in alcohol consumption among adolescents following RCL, 42 whereas another Washington study found RCL predicted a higher likelihood of alcohol use among youth. 50 A Canadian study also found no significant effect of RCL on rates of alcohol or illicit drug use among youth. 61 Finally, in a sample of trauma patients in California the findings around changes in substance use were mixed. 57 In adult patients, the rates of positive screens for alcohol, opiates, methamphetamine, benzodiazepine/barbiturate, and MDMA did not change following RCL, but there was an increase in positive screens for cocaine. In pediatric patients, increases were seen in positive screens for benzodiazepine/barbiturate, but positive screens for alcohol, opiates, methamphetamine, and cocaine did not change. 57 The current evidence is divided on whether RCL is associated with increased alcohol and other substance use, with 40% of studies finding an association and 60% not observing one or finding mixed results.
In the case of cigarettes, Mason et al 42 did find significant cohort effects, where the post-RCL cohort was less likely to consume cigarettes compared to the pre-RCL one (Coefficient: − 2.16, P ⩽ .01). However, these findings were not echoed in more recent studies. Lack of an effect for cigarette use is supported by an Oregon study that found RCL was not associated with college student’s cigarette use. 47 Similarly, RCL was not significantly associated with past-year cigarette use in a sample of young adults from Oregon and Washington. 50 On balance, there is little evidence that RCL is linked with changes in cigarette smoking.
Route of administration
The increase in smoke-free alternative routes of cannabis administration (eg, vaping and oral ingestion of edibles) 63 , 64 make method of cannabis consumption an important topic to understand in the context of RCL. Two studies examined differences in route of cannabis consumption as a function of cannabis policy. One study examined changes in the number of different modes of cannabis use reported by high school students in Canada. 65 Results showed that from pre-to-post RCL 31.3% of students maintained a single mode of use, 14.3% continued to use cannabis in multiple forms, while 42.3% expanded from a single mode to multiple modes of administration and 12.1% reduced the number of modes they used. Another study found that smoking, vaping, and edibles (in that order) were the most frequent modes of cannabis use pre- and post-RCL in California, suggesting minimal impact of RCL on mode of cannabis use. 51 However, the least common mode of cannabis use was blunts, which did decline following RCL (13.5%-4.3%). 51 Overall, the evidence suggests RCL may be associated with changes in modes of cannabis consumption, but as the evidence is only from two studies there still remains a need for more studies examining RCL and cannabis route of administration.
Nine studies examined RCL and cannabis attitudes (see Table 2 ). Regarding cannabis use intentions, one U.S. study found that for both a non-RCL state and a state that underwent RCL, intention to use in young adults significantly increased post-RCL, suggesting a lack of RCL specific effect, 48 and that aside from the very first time point, there were no significant differences between the states in intention to use. Further, attitudes and willingness to use cannabis, between the RCL and non-RCL state remained similar overtime ( P s ⩾ .05), although both states reported significantly more positive attitudes toward cannabis following RCL ( P ⩽ .001). 48 However, another study U.S. from found differences in adolescent use intentions across RCL, whereby those in the RCL cohort in jurisdictions that allowed sales were less likely to increase intent to use cannabis ( P = .04), but the RCL cohort without sales were more likely to increase intent to use ( P = .02). 43 The pre-RCL cohort in communities that opted out of sales were also less likely to increase willingness to use compared to the cohort with legal sales ( P = .02). 43 Both studies reveal contrasting findings surrounding RCL’s relationship with cannabis use intentions and willingness to use.
Studies examining recreational cannabis legalization and attitudes surrounding cannabis.
Looking at cannabis use motives, one study found a non-significant increase in recreational motives for cannabis use post-RCL. 60 Similarly following RCL in Canada, 24% of individuals previously reporting cannabis use exclusively for medical purposes declared using for both medical and non-medical purposes following RCL, and 24% declared use for non-medical purposes only, 66 suggesting RCL can influence recreational/nonmedicinal motivations for cannabis use among those who previously only used for medical reasons.
In studies examining perceived risk and perceptions of cannabis use, one U.S. study found an indirect effect between RCL and increased consequences of use in adolescents through higher perceived risk ( P ⩽ .001), but no association with frequency of use. 41 Another U.S. study revealed mixed results and found that RCL was not associated with perceived harm of use in youth. 50 Further, youth in one study did not report differences in perceptions of safety of cannabis, ease of accessing cannabis use or on concealing their use from authority, 61 which contrasts with another study finding increased reports of problems accessing cannabis post-RCL ( P ⩽ .01). 60 Regarding health perceptions, a California study found that cannabis use was perceived as more beneficial for mental health, physical health, and wellbeing in adults at 6 months post-RCL compared to pre-RCL and 1-month post-RCL ( P = .02). 51 Mental health perceptions of cannabis use increased from being perceived as “slightly harmful” pre-RCL to perceived as “slightly beneficial” at 6 months post-RCL. 51 However, in a sample of treatment seeking individuals with an opioid use disorder, the vast majority of participants reported beliefs that RCL would not impact their cannabis use, with no difference in beliefs pre- to post-RCL (85.9% reported belief it would have no impact pre-RCL and 85.7%, post-RCL). 62 The combined results of the studies suggest potential associations of RCL with risk and benefit perceptions of cannabis use, however as 55% of studies suggest a lack of or inconsistent association with RCL, on balance the literature on RCL’s impact on cannabis attitudes is mixed.
Health-related outcomes
We identified 33 articles that examined various health-related outcomes associated with RCL (see Table 3 ). The largest number involved hospital utilization (ie, seeking emergency services for cannabis-related problems such as unintentional exposure, CUD, and other harms). Other health-care outcomes included opioid-related harms, mental health variables, and adverse birth outcomes.
Studies investigating the relationship of recreational cannabis legalization and health-related outcomes.
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; CDC, Center for Disease Prevention; WONDER, Wide-Ranging Online Data for Epidemiologic Research; RCL, Recreational Cannabis Legalization.
Emergency service utilization
Seventeen studies examined the association between RCL and use of emergency services related to cannabis (eg, hospital visits, calls to regional poison centers). Regarding emergency service rates in youth, a Colorado study found the rate of pediatric cannabis-related emergency visits increased pre- to post-RCL ( P ⩽ .0001). 67 Similarly, cannabis-related visits requiring further evaluation in youth also increased. 67 This increasing need for emergency service related to cannabis exposure in youth following RCL was supported in 4 other U.S. studies. 68 - 71 A Canadian study supported the U.S. studies, finding a 2.6 increase in children admissions for cannabis poisonings post-RCL. 72 In contrast, overall pediatric emergency department visits did not change from pre- to post-RCL in Alberta, Canada, 73 but there was a non-significant increase of the rate and proportion of children under 12 presenting to the emergency department. However, unintentional cannabis ingestion did increase post-RCL for children under 12 (95% CI: 1.05-1.47) and older adolescents (1.48, 95% CI: 1.21-1.81). 74 Taken together, these studies do suggest a risk for increasing cannabis-related emergency visits in youth following RCL, with 75% of studies finding an association between RCL and increasing emergency service rates in youth.
There is also evidence of increased hospital utilization in adults following RCL. Five studies found evidence of increased emergency service utilization or poison control calls from cannabis exposure associated with RCL in the U.S. and Canada. 24 , 69 , 74 - 76 Finally, a Colorado study saw an increase in cannabis involved pregnancy-related hospital admissions from 2011 to 2018, with notable spikes after 2012 and 2014, timeframes associated with state RCL. 77
However, some evidence points to a lack of association between RCL and emergency service utilization. A chart review in Ontario, Canada found no difference in number of overall cannabis emergency room visits pre- versus post-RCL ( P = .27). 78 When broken down by age group, visits only increased for those 18 to 29 ( P = .03). This study also found increases in patients only needing observation ( P = .002) and fewer needing bloodwork or imaging services (both P s ⩽.05). 78 Further in a California study that found overall cannabis exposure rates were increasing, when breaking these rates down by age there was no significant change in calls for those aged 13 and up, only for those 12 and under. 69 An additional Canadian study found that rates of cannabis related visits were already increasing pre-RCL. 79 Following RCL, although there was a non-significant immediate increase in in cannabis-related emergency visits post-RCL this was followed a significant drop off in the increasing monthly rates seen prior to RCL. 79 Another Canadian study that examined cannabis hyperemesis syndrome emergency visits found that rates of admissions were increasing prior to RCL and the enactment of RCL was not associated with any changes in rates of emergency admissions. 80 As this attenuation occurred in Canada prior to commercialization where strict purchasing policy was in place, it may suggest that having proper regulations in place can prevent the uptick in cannabis-related emergency visits seen in U.S. studies.
Other hospital-related outcomes examined included admissions for cannabis misuse and other substance use exposure. One study found decreasing CUD admission rates over time (95% CI: −4.84, −1.91), with an accelerated, but not significant, decrease in Washington and Colorado (following RCL) compared to the rest of the U.S. 81 In contrast, another study found increased rates of healthcare utilization related to cannabis misuse in Colorado compared to New York and Oklahoma ( P s ⩽.0005). 82 With respect to other substance use, findings revealed post-RCL increases in healthcare utilization in Colorado for alcohol use disorder and overdose injuries but a decrease in chronic pain admissions compared to both controls ( P ⩽ .05). 82 However, two Canadian studies found the rate of emergency department visits with co-ingestant exposure of alcohol, opioid, cocaine, and unclassified substances in older adolescents and adults decreased post-RCL. 73 , 77 Another Canadian study found no change in cannabis-induced psychosis admissions nor in alcohol- or amphetamine-induced admissions. 83
Finally, three studies examined miscellaneous hospital-related outcomes. A study examining hospital records in Colorado to investigate facial fractures (of significance as substance impairment can increase the risk of accidents) showed a modest but not significant influence of RCL. 84 The only significant increases of facial trauma cases were maxillary and skull base fracture cases ( P s ⩽ .001) suggesting a partial influence of RCL on select trauma fractures. The second study found increased trauma activation (need for additional clinical care in hospital) post-RCL in California ( P = .01). 57 Moreover, both adult and pediatric trauma patients had increased mortality after RCL ( P = .03; P = .02, respectively). 57 The final study examining inflammatory bowel disease (IBD) outcomes in the U.S. found more cannabis users on total parenteral nutrition post-RCL (95% CI: 0.02, 0.89) and lower total hospital costs in users post-RCL (95% CI: −15 717, −1119). 58 No other IBD outcomes differed pre- to post-RCL (eg, mortality, length of stay, need for surgery, abscess incision and drainage).
Overall, these studies point to increased cannabis-related health-care utilization following RCL for youth and pediatrics (75% finding an increase). However, the impact of legalization on adult rates of cannabis-related emergency visits is mixed (44% finding lack of an association with RCL). As findings also varied across different countries (ie, Canada vs the U.S.), it suggests the importance of continually monitoring the role of RCL across different jurisdictions which may have different cannabis regulations in place. These studies also suggest there may be other health consequences associated with RCL. Further research should be done to examine trends of other emergency service use that could be influenced by RCL.
Two studies reported a weak or non-existent effect of RCL on opioid related outcomes. 85 , 86 First, a U.S. administrative study found no association of RCL and opioid prescriptions from orthopedic surgeons. 85 The second study found that, of U.S. states that passed RCL, those that passed policies before 2015 had fewer Schedule III opioid prescriptions ( P = .003) and fewer total doses prescribed ( P = .027), 86 but when compared to states with medicinal cannabis legislation, there were no significant differences. However, 3 studies suggested a potential protective effect of RCL, with one study finding a significant decrease for monthly opioid-related deaths following RCL (95% CI: –1.34, –0.03), compared to medical cannabis legalization and prohibition. 87 A Canadian study examining opioid prescription claims also found an accelerated decline in claims for public payers post-RCL compared to declines seen pre-RCL ( P ⩽ .05). 88 Next a study examining women with pelvic pain found that post-RCL patients were less likely to report daily opioid use, including use for pain ( P = .026). 59 These studies indicate some inconsistencies in relationships between RCL, opioid prescriptions and use indicators in the current literature, while the literature on balance points to a potential relationship with RCL (60%), the overall evidence is still mixed as 40% of studies support a weak association with RCL.
Adverse birth outcomes
Changes in adverse birth outcomes including small for gestational age (SGA) births, low birth weight, and congenital anomalies were examined in two studies. The first study, which examined birth outcomes in both Colorado and Washington, found that RCL was associated with an increase in congenital anomaly births for both states ( P ⩽ .001, P = .01 respectively). 89 Preterm births also significantly increased post-RCL, but only in Colorado ( P ⩽ .001). Regarding SGA outcomes, there was no association with RCL for either state. 89 Similarly, the second study did find an increase in the prevalence of low birth weight and SGA over time, but RCL was not directly associated with these changes. 90 Although the current literature is small and limited to studies in Washington and Colorado, the evidence suggests minimal changes in adverse birth outcomes following RCL.
Mental health outcomes
Six studies examined mental health related outcomes. A Canadian study examining psychiatric patients did not see a difference in rates of psychotic disorders pre- to post-RCL. 45 Similarly, another Canadian study did not see a difference in hospital admissions with schizophrenia or related codes post-RCL. 83 However, the prevalence of personality disorders and “other” diagnoses was higher post-RCL ( P = .038). 45 In contrast, another Canadian study found that rates of pediatric cannabis-related emergency visits with co-occurring personality and mood-related co-diagnoses decreased post-RCL among older adolescents. 73 A U.S. study examining the relationship between cannabis use and anxious mood fluctuations in adolescents found RCL had no impact on the association. 91 Similarly, another Canadian study found no difference in mental health symptomology pre- to post-RCL. 61 In contrast, anxiety scores in women with pelvic pain were higher post-RCL compared to pre-RCL ( P = .036). 59 The small number and mixed findings of these studies, 66.7% finding no association or mixed findings and 33.3% finding an association but in opposite directions, identify a need for further examination of mental health outcomes post-RCL.
Miscellaneous health outcomes
Three studies examined additional health-related outcomes. First, a California study examined changes in medical cannabis status across RCL. Post-RCL, 47.5% of medical cannabis patients remained medical cannabis patients, while 73.8% of non-patients remained so. 92 The transition into medical cannabis patient status post-RCL represented the smallest group (10%). Cannabis legalization was the most reported reason for transition out of medical cannabis patient status (36.2%). 92 Next, a study examining pelvic pain in women found that post-RCL patients reported greater pain catastrophizing ( P ⩽ .001), less anti-inflammatory ( P ⩽ .001) and nerve medication use ( P = .027), but more herbal pain medication use ( P = .010). 59 Finally, a Canadian study that examined cannabinoids in post-mortem blood samples reported that post-RCL deaths had higher odds of positive cannabis post-mortem screens compared to pre-RCL (95% CI: 1.09-1.73). 93 However, the majority of growth for positive cannabinoid screens took place in the two years prior to RCL implementation. In sub-group analyses, only 25- to 44-year-olds had a significant increase in positive cannabinoid screens (95% CI: 0.05-0.19). Additional post-mortem drug screens found an increase in positive screens for amphetamines ( P ⩽ .001) and cocaine ( P = .042) post-RCL. These additional health outcomes demonstrate the wide-ranging health impacts that may be associated with RCL and indicate a continued need to examine the role of RCL on a variety of outcomes.
Driving-related outcomes
Six studies examined rates of motor vehicle accidents and fatalities (see Table 4 ). Two U.S. studies found no statistical difference in fatal motor vehicle collisions associated with RCL. 94 , 95 Further, a California-based study examining THC toxicology screens in motor vehicle accident patients, did find a significant increase in positive screens, but this increase was not associated with implementation of RCL. 96 However, three studies suggest a negative impact of RCL, as one U.S. study found both RCL states and their neighboring states had an increase in motor vehicle fatalities immediately following RCL. 97 Additionally, a Canadian study did find a significant increase in moderately injured drivers with cannabis positive blood screens post-RCL. 98 Finally, a study in Uruguay found RCL was associated with increased immediate fatal crashes for cars, but not motorcycles; further investigation suggested this effect was noticeable in urban areas, but not rural areas. 99 While the overall evidence was inconsistent, current evidence does suggest a modest increase, seen in two studies, in motor vehicle accidents associated with RCL. Further longitudinal research in more jurisdictions is needed to understand the long-term consequences of RCL on motor vehicle accidents.
Studies looking at recreational cannabis legalization and driving related outcomes.
Crime-related outcomes
Three studies explored crime-related outcomes associated with RCL (see Table 5 ). A Washington study examining cannabis-related arrest rates in adults did find significant drops in cannabis-related arrests post-RCL for both 21+ year olds (87% drop; P ⩽ .001) and 18 to 20-year-olds (46% drop; P ⩽ .001). 100 However, in another study examining Oregon youth this post-RCL decline for arrests was not seen; cannabis-related allegations in youth actually increased following RCL (28%; 95% CI = 1.14, 1.44). 101 Further, declines in youth allegations prior to RCL ceased after RCL was implemented. In contrast, a Canadian study did find significant decreases in cannabis-related offenses in youth post RCL ( P ⩽ .001), but rates of property and violent crime did not change across RCL. 102 These studies highlight the diverse effects of RCL across different age groups. However, there remains a need for a more comprehensive evaluation on the role of RCL on cannabis-related arrests.
Studies investigating recreational cannabis legalization and crime related outcomes.
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; RCL, Recreational Cannabis Legalization.
Notably, two studies also examined race disparities in cannabis-related arrests. For individuals 21+ relative arrest disparities between Black and White individuals grew post-RCL. 100 When looking at 18 to 20-year-olds, cannabis-related arrest rates for Black individuals did slightly decrease, albeit non-significantly, but there was no change in racial disparities. 100 In youth ages 10 to 17, Indigenous and Alaska Native youth were more likely than White youth to receive a cannabis allegation before RCL (95% CI: 2.31, 3.01), with no change in disparity following RCL (95% CI: 2.10, 2.81). 101 On the other hand, Black youth were more likely to receive a cannabis allegation than White youth prior to RCL (95% CI: 1.66, 2.13), but the disparity decreased following RCL (95% CI: 1.06, 1.43). 101 These studies suggest improvements in racial disparities for cannabis-related arrests following RCL, although there ware only two studies and they are limited to the U.S.
The aim of this systematic review was to examine the existing literature on the impacts of RCL on a broad range of behavioral and health-related outcomes. The focus on more rigorous study designs permits greater confidence in the conclusions that can be drawn. The literature revealed five main outcomes that have been examined: cannabis use behaviors, cannabis attitudes, health-related outcomes, driving-related outcomes, and crime-related outcomes. The overall synthesizing of the literature revealed heterogenous and complex effects associated with RCL implementation. The varied findings across behavioral and health related outcomes does not give a clear or categorical answer as to whether RCL is a negative or positive policy change overall. Rather, the review reveals that while a great deal of research is accumulating, there remains a need for more definitive findings on the causal role of RCL on a large variety of substance use, health, attitude-related, driving, and crime-related outcomes.
Overall, studies examining cannabis use behavior revealed evidence for cannabis use increases following RCL, particularly for young adults (100%), peri-natal users (66%), and certain clinical populations (66%). 47 , 54 , 59 While general adult samples had some mixed findings, the majority of studies (80%) suggested increasing rates of use associated with RCL. 51 Of note, the increasing cannabis use rates found in peri-natal and clinical populations are particularly concerning as they do suggest increasing rates in more vulnerable samples where potential adverse consequences of cannabis use are more pressing. 103 However, for both groups the overall literature revealed only a few studies and thus requires further examination. Further, a reason to caution current conclusions surround RCL impacts on substance use, is that there is research suggesting cannabis use rates were increasing prior to RCL in Canada. 104 Thus, there still remains a need to better disentangle causal consequences of RCL on cannabis use rates.
In contrast to studies of adults, studies of adolescents pointed to inconsistent evidence of RCL’s influence on cannabis use rates, 38 , 45 with 60% of studies finding no change or inconsistent evidence surrounding adolescent use following RCL. Thus, a key conclusion of the cannabis use literature is that there is not overwhelming evidence that RCL is associated with increasing rates of cannabis among adolescents, which is notable as potential increases in adolescent use is a concern often voiced by critics of RCL. 16 This might suggest that current RCL policies that limit access to minors may be effective. However, a methodological explanation for the discrepancy between findings for adolescents and adults is that adults may be more willing to report their use of cannabis following RCL as it is now legal for them to use. However, for adolescents’ cannabis use remained illicit, which may lead to biased reporting from adolescents. Thus, additional research using methods to overcome limitations of self-reports may be required.
With regard to other substance use, primarily alcohol and cigarettes, there is little evidence that RCL is associated with increased use rates and may even be associated with decreased rates of cigarette use. 42 , 61 The lack of a relationship with RCL and increasing alcohol and other substance use, seen in 60% of studies, is relevant due to concerns of RCL causing “spill-over” effects to substances other than cannabis. However, the decreasing rates on cigarette use associated with RCL seen in 33% of studies may also suggest a substitution effect of cannabis. 105 It is possible that RCL encourages a substitution effect where cannabis is used to replace use other substances such as cigarettes, but 66% of studies found no association of RCL and cigarette use so further research examining a potential substitution effect is needed. In sum, the literature points to a heterogenous impact of RCL on cannabis and other substance use rates, suggesting complex effects of RCL on use rates that may vary across age and population. However, the review also highlights that there are still limited studies examining RCL and other substance use, particularly a lack of multiple studies examining the same age group.
The current evidence for the impact of RCL on attitudes surrounding cannabis revealed mixed or limited results, with 44% studies finding some sort of relationship with attitudes and RCL and 55% studies suggest a lack of or inconsistent relationship. Studies examining cannabis use attitudes or willingness to use revealed conflicting evidence whereas some studies pointed to increased willingness to use associated with RCL, 43 and others found no change or that changes were not specific to regions that implemented RCL. 48 For attitude-related studies that did reveal consistent findings (eg, use motivation changes, perceptions of lower risk and greater benefits of use), the literature was limited in the number of studies or involved heterogenous samples, making it difficult to make conclusive statements surrounding the effect of RCL. As cannabis-related attitudes (eg, perceived risk, intentions to use) can have implications for cannabis use and consequences 106 , 107 it is interesting that current literature does not reveal clear associations of cannabis-related attitudes and RCL. Rather, this review reveals a need for more research examining changes in cannabis-attitudes over time and potential impacts of RCL.
In terms of health outcomes, the empirical literature suggests RCL is associated with increased cannabis-related emergency visits 24 , 67 , 70 , 76 and other health consequences (eg, trauma-related cases 57 ). The literature also suggests there may be other potential negative health consequences associated with RCL, such as increasing adverse birth outcomes and post-mortem cannabis screens. 45 , 89 Synthesizing of the literature points to a well-established relationship of RCL and increasing cannabis-related emergency visits. While some extant literature was mixed, on balance most studies included in the review (70.6%) found consistent evidence of increased emergency service use (eg, emergency department admissions and poison control calls) for both adolescents and adults with only 31% of studies finding mixed or no association with RCL. This points to a need for stricter RCL policies to prevent unintentional consumption or hyperemesis such as promoting safe or lower risk use of cannabis (eg, using lower THC products, avoiding deep inhales while smoking), clearer packaging for cannabis products, and safe storage procedures.
However, the literature on health outcomes outside of emergency service utilization is limited and requires more in-depth evaluations to be fully understood. Additionally, not all health-outcomes indicated negative consequences associated with RCL. There is emerging evidence of the potential of RCL to help decrease CUD and multiple substance hospital admissions 74 , 82 Furthermore, while some findings were mixed and the number of studies limited, 60% of studies found potential for RCL to have protective effects for opioid-related negative consequences. 87 , 88 However, opioid-related findings should be considered in the context of population-level changes in opioid prescriptions and shifting opioid policy influence. 108 Thus, findings may be a result of changes driven by the response to the opioid epidemic rather than RCL, and there remains a need to better disentangle RCL impacts on opioid-related consequences. It is also worth noting that some opioid and cannabis studies are underwritten by the cannabis industry, so the findings should be interpreted with caution due to potential for conflicts of interest. 88 In sum, the overall literature suggests that RCL is associated with both negative and positive health-related consequences and reveals a need to examine the role of RCL across a wide range of health outcomes.
The findings from the driving-related literature do suggest RCL is associated with increased motor vehicle accidents (50% of studies) although the literature was quite evenly split as higher accident rates were not seen across all studies (50% studies). These results point to potential negative consequence associated with RCL and may indicate a need for better measures to prevent driving while under the influence of cannabis in legalized jurisdictions. However, as the evidence was split and predominately in the U.S. additional studies spanning diverse geographical jurisdictions are still needed.
On the other hand, the findings from crime-related outcomes showed some inconsistencies. While one study did suggest minimal decreases for substance-use related arrests in adults, the findings were not consistent across the two studies examining arrest-rates in youth. 100 - 102 These potential decreases in arrest rates for adults can have important implications as cannabis-related crime rates make up a large amount of overall crime statistics and drug-specific arrests. 30 , 31 This discrepancy in youth findings between a U.S. and Canadian study are notable as Canadian RCL policies do include stipulations to allow small scale regulations in youth. Thus, it suggests RCL policies that maintain prohibition of use among underage youth do not address issues related to arrests and crime among youth. In fact, the current literature suggests that cannabis-related charges are still being enforced for youth under the legal age of consumption in the U.S. Another important outcome revealed is racial disparities in cannabis-related arrests. Previous evidence has shown there are racial disparities, particularly between Black, Indigenous, and Hispanic individuals compared to White counterparts, in cannabis-related charges and arrests. 109 , 110 Regarding racial disparities and RCL, there was very little evidence of decreases in disparities for cannabis-related arrests following RCL. 100 , 101 This racialized arresting is significant as it can be associated with additional public health concerns such as physical and mental health outcomes, harm to families involved, and to communities. 111 This finding is particularly concerning as it suggests racialized arrests for cannabis are still occurring despite the intentions of liberalization of cannabis policies to help reduce racial disparities in the criminal justice system. However, it is important to note that there were only 2 studies of racial disparities in cannabis-related arrests and both were conducted in the U.S. Thus, additional research is required before drawing any firm conclusions about the ability of RCL to address systemic issues in the justice system.
Limitations
The findings should be considered within context of the following limitations. The research was predominately from North America (U.S. and Canada). While both countries have either federal or state RCL, findings only from two countries that are geographically connected may not reflect the influence of RCL across different cultures and countries globally. The majority of studies also relied on self-report data for cannabis-related outcomes. Thus, there is a risk that any increases in use or other cannabis-related outcomes may be due to an increased comfort in disclosing cannabis use due to RCL.
Given the large number of studies on multiple outcomes, we chose to focus on implementation of RCL exclusively, rather than related policy changes such as commercialization (ie, the advent of legal sales), to allow for clearer conclusions about the specific impacts on RCL. However, a limitation is that the review does not address the impact of commercialization or changes in product availability. While outside the scope of the current review, it does limit the conclusions that can be drawn about RCL overall as some jurisdictions implemented features of commercialization separately from legalization. For example, in Ontario, Canada, storefronts and edible products became legal a year after initial RCL (when online purchase was the exclusive modality), which may have had an additional impact on behavioral and health-related outcomes. Additionally, the scope of the review was limited to recreational legalization and did not consider other forms of policy changes such as medicinal legalization or decriminalization, as these have been summarized more comprehensively in prior reviews. 112 - 114 Further, this review focused on behavioral and health outcomes; other important outcomes to examine in the future include economic aspects such as cannabis pricing and purchasing behaviors, and product features such as potency. Finally, as this review considered a broad range of outcomes, we did not conduct a meta-analysis which limits conclusions that can be drawn regarding the magnitude of the associations.
Conclusions
The topic of RCL is a contentious and timely issue. With nationwide legalization in multiple countries and liberalizing policies across the U.S., empirical research on the impacts of RCL has dramatically expanded in recent years. This systematic review comprehensively evaluated a variety of outcomes associated with RCL, focusing on longitudinal study designs and revealing a wide variety of findings in terms of substance use, health, cannabis attitudes, crime, and driving outcomes examined thus far. However, the current review highlights that the findings regarding the effects of RCL are highly heterogenous, often inconsistent, and disproportionately focused on certain jurisdictions. With polarizing views surrounding whether RCL is a positive or negative policy change, it is noteworthy that the extant literature does not point to one clear answer at the current time. In general, the collective results do not suggest dramatic changes or negative consequences, but instead suggest that meaningful tectonic shifts are happening for several outcomes that may or may not presage substantive changes in personal and public health risk. Furthermore, it is clear that a more in-depth examinations of negative (eg, frequent use, CUD prevalence, ‘gateway’ relationships with other substance use), or positive consequences (eg, therapeutic benefits for mental health and/or medical conditions, use of safer products and routes of administration), are needed using both quantitative and qualitative approaches.
Acknowledgments
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding support from the Peter Boris Chair in Addictions Research and a Canada Research Chair in Translational Addiction Research (JM). Funders had no role in the design or execution of the review.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: James MacKillop discloses he is a principal and senior scientist in Beam Diagnostics, Inc, and a consultant to ClairvoyantRx. No other authors have disclosures.
Author Contributions: The author’s contribution is as follows: study conceptualization and design: KF, JW, JT, JM; data collection and interpretation: KF, EM, MS; manuscript writing and preparation: KF, EM, MS, PN; manuscript reviewing and editing: JW, JT, JM. All authors have reviewed and approved the final manuscript.
- Research article
- Open access
- Published: 04 February 2020
Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health
- Xinguang Chen 1 ,
- Xiangfan Chen 2 &
- Hong Yan 2
BMC Public Health volume 20 , Article number: 156 ( 2020 ) Cite this article
107k Accesses
70 Citations
83 Altmetric
Metrics details
Marijuana is the most commonly used illicit drug in the United States. More and more states legalized medical and recreational marijuana use. Adolescents and emerging adults are at high risk for marijuana use. This ecological study aims to examine historical trends in marijuana use among youth along with marijuana legalization.
Data ( n = 749,152) were from the 31-wave National Survey on Drug Use and Health (NSDUH), 1979–2016. Current marijuana use, if use marijuana in the past 30 days, was used as outcome variable. Age was measured as the chronological age self-reported by the participants, period was the year when the survey was conducted, and cohort was estimated as period subtracted age. Rate of current marijuana use was decomposed into independent age, period and cohort effects using the hierarchical age-period-cohort (HAPC) model.
After controlling for age, cohort and other covariates, the estimated period effect indicated declines in marijuana use in 1979–1992 and 2001–2006, and increases in 1992–2001 and 2006–2016. The period effect was positively and significantly associated with the proportion of people covered by Medical Marijuana Laws (MML) (correlation coefficients: 0.89 for total sample, 0.81 for males and 0.93 for females, all three p values < 0.01), but was not significantly associated with the Recreational Marijuana Laws (RML). The estimated cohort effect showed a historical decline in marijuana use in those who were born in 1954–1972, a sudden increase in 1972–1984, followed by a decline in 1984–2003.
The model derived trends in marijuana use were coincident with the laws and regulations on marijuana and other drugs in the United States since the 1950s. With more states legalizing marijuana use in the United States, emphasizing responsible use would be essential to protect youth from using marijuana.
Peer Review reports
Introduction
Marijuana use and laws in the united states.
Marijuana is one of the most commonly used drugs in the United States (US) [ 1 ]. In 2015, 8.3% of the US population aged 12 years and older used marijuana in the past month; 16.4% of adolescents aged 12–17 years used in lifetime and 7.0% used in the past month [ 2 ]. The effects of marijuana on a person’s health are mixed. Despite potential benefits (e.g., relieve pain) [ 3 ], using marijuana is associated with a number of adverse effects, particularly among adolescents. Typical adverse effects include impaired short-term memory, cognitive impairment, diminished life satisfaction, and increased risk of using other substances [ 4 ].
Since 1937 when the Marijuana Tax Act was issued, a series of federal laws have been subsequently enacted to regulate marijuana use, including the Boggs Act (1952), Narcotics Control Act (1956), Controlled Substance Act (1970), and Anti-Drug Abuse Act (1986) [ 5 , 6 ]. These laws regulated the sale, possession, use, and cultivation of marijuana [ 6 ]. For example, the Boggs Act increased the punishment of marijuana possession, and the Controlled Substance Act categorized the marijuana into the Schedule I Drugs which have a high potential for abuse, no medical use, and not safe to use without medical supervision [ 5 , 6 ]. These federal laws may have contributed to changes in the historical trend of marijuana use among youth.
Movements to decriminalize and legalize marijuana use
Starting in the late 1960s, marijuana decriminalization became a movement, advocating reformation of federal laws regulating marijuana [ 7 ]. As a result, 11 US states had taken measures to decriminalize marijuana use by reducing the penalty of possession of small amount of marijuana [ 7 ].
The legalization of marijuana started in 1993 when Surgeon General Elder proposed to study marijuana legalization [ 8 ]. California was the first state that passed Medical Marijuana Laws (MML) in 1996 [ 9 ]. After California, more and more states established laws permitting marijuana use for medical and/or recreational purposes. To date, 33 states and the District of Columbia have established MML, including 11 states with recreational marijuana laws (RML) [ 9 ]. Compared with the legalization of marijuana use in the European countries which were more divided that many of them have medical marijuana registered as a treatment option with few having legalized recreational use [ 10 , 11 , 12 , 13 ], the legalization of marijuana in the US were more mixed with 11 states legalized medical and recreational use consecutively, such as California, Nevada, Washington, etc. These state laws may alter people’s attitudes and behaviors, finally may lead to the increased risk of marijuana use, particularly among young people [ 13 ]. Reported studies indicate that state marijuana laws were associated with increases in acceptance of and accessibility to marijuana, declines in perceived harm, and formation of new norms supporting marijuana use [ 14 ].
Marijuana harm to adolescents and young adults
Adolescents and young adults constitute a large proportion of the US population. Data from the US Census Bureau indicate that approximately 60 million of the US population are in the 12–25 years age range [ 15 ]. These people are vulnerable to drugs, including marijuana [ 16 ]. Marijuana is more prevalent among people in this age range than in other ages [ 17 ]. One well-known factor for explaining the marijuana use among people in this age range is the theory of imbalanced cognitive and physical development [ 4 ]. The delayed brain development of youth reduces their capability to cognitively process social, emotional and incentive events against risk behaviors, such as marijuana use [ 18 ]. Understanding the impact of marijuana laws on marijuana use among this population with a historical perspective is of great legal, social and public health significance.
Inconsistent results regarding the impact of marijuana laws on marijuana use
A number of studies have examined the impact of marijuana laws on marijuana use across the world, but reported inconsistent results [ 13 ]. Some studies reported no association between marijuana laws and marijuana use [ 14 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ], some reported a protective effect of the laws against marijuana use [ 24 , 26 ], some reported mixed effects [ 27 , 28 ], while some others reported a risk effect that marijuana laws increased marijuana use [ 29 , 30 ]. Despite much information, our review of these reported studies revealed several limitations. First of all, these studies often targeted a short time span, ignoring the long period trend before marijuana legalization. Despite the fact that marijuana laws enact in a specific year, the process of legalization often lasts for several years. Individuals may have already changed their attitudes and behaviors before the year when the law is enacted. Therefore, it may not be valid when comparing marijuana use before and after the year at a single time point when the law is enacted and ignoring the secular historical trend [ 19 , 30 , 31 ]. Second, many studies adapted the difference-in-difference analytical approach designated for analyzing randomized controlled trials. No US state is randomized to legalize the marijuana laws, and no state can be established as controls. Thus, the impact of laws cannot be efficiently detected using this approach. Third, since marijuana legalization is a public process, and the information of marijuana legalization in one state can be easily spread to states without the marijuana laws. The information diffusion cannot be ruled out, reducing the validity of the non-marijuana law states as the controls to compare the between-state differences [ 31 ].
Alternatively, evidence derived based on a historical perspective may provide new information regarding the impact of laws and regulations on marijuana use, including state marijuana laws in the past two decades. Marijuana users may stop using to comply with the laws/regulations, while non-marijuana users may start to use if marijuana is legal. Data from several studies with national data since 1996 demonstrate that attitudes, beliefs, perceptions, and use of marijuana among people in the US were associated with state marijuana laws [ 29 , 32 ].
Age-period-cohort modeling: looking into the past with recent data
To investigate historical trends over a long period, including the time period with no data, we can use the classic age-period-cohort modeling (APC) approach. The APC model can successfully discompose the rate or prevalence of marijuana use into independent age, period and cohort effects [ 33 , 34 ]. Age effect refers to the risk associated with the aging process, including the biological and social accumulation process. Period effect is risk associated with the external environmental events in specific years that exert effect on all age groups, representing the unbiased historical trend of marijuana use which controlling for the influences from age and birth cohort. Cohort effect refers to the risk associated with the specific year of birth. A typical example is that people born in 2011 in Fukushima, Japan may have greater risk of cancer due to the nuclear disaster [ 35 ], so a person aged 80 in 2091 contains the information of cancer risk in 2011 when he/she was born. Similarly, a participant aged 25 in 1979 contains information on the risk of marijuana use 25 years ago in 1954 when that person was born. With this method, we can describe historical trends of marijuana use using information stored by participants in older ages [ 33 ]. The estimated period and cohort effects can be used to present the unbiased historical trend of specific topics, including marijuana use [ 34 , 36 , 37 , 38 ]. Furthermore, the newly established hierarchical APC (HAPC) modeling is capable of analyzing individual-level data to provide more precise measures of historical trends [ 33 ]. The HAPC model has been used in various fields, including social and behavioral science, and public health [ 39 , 40 ].
Several studies have investigated marijuana use with APC modeling method [ 17 , 41 , 42 ]. However, these studies covered only a small portion of the decades with state marijuana legalization [ 17 , 42 ]. For example, the study conducted by Miech and colleagues only covered periods from 1985 to 2009 [ 17 ]. Among these studies, one focused on a longer state marijuana legalization period, but did not provide detailed information regarding the impact of marijuana laws because the survey was every 5 years and researchers used a large 5-year age group which leads to a wide 10-year birth cohort. The averaging of the cohort effects in 10 years could reduce the capability of detecting sensitive changes of marijuana use corresponding to the historical events [ 41 ].
Purpose of the study
In this study, we examined the historical trends in marijuana use among youth using HAPC modeling to obtain the period and cohort effects. These two effects provide unbiased and independent information to characterize historical trends in marijuana use after controlling for age and other covariates. We conceptually linked the model-derived time trends to both federal and state laws/regulations regarding marijuana and other drug use in 1954–2016. The ultimate goal is to provide evidence informing federal and state legislation and public health decision-making to promote responsible marijuana use and to protect young people from marijuana use-related adverse consequences.
Materials and methods
Data sources and study population.
Data were derived from 31 waves of National Survey on Drug Use and Health (NSDUH), 1979–2016. NSDUH is a multi-year cross-sectional survey program sponsored by the Substance Abuse and Mental Health Services Administration. The survey was conducted every 3 years before 1990, and annually thereafter. The aim is to provide data on the use of tobacco, alcohol, illicit drug and mental health among the US population.
Survey participants were noninstitutionalized US civilians 12 years of age and older. Participants were recruited by NSDUH using a multi-stage clustered random sampling method. Several changes were made to the NSDUH after its establishment [ 43 ]. First, the name of the survey was changed from the National Household Survey on Drug Abuse (NHSDA) to NSDUH in 2002. Second, starting in 2002, adolescent participants receive $30 as incentives to improve the response rate. Third, survey mode was changed from personal interviews with self-enumerated answer sheets (before 1999) to the computer-assisted person interviews (CAPI) and audio computer-assisted self-interviews (ACASI) (since 1999). These changes may confound the historical trends [ 43 ], thus we used two dummy variables as covariates, one for the survey mode change in 1999 and another for the survey method change in 2002 to control for potential confounding effect.
Data acquisition
Data were downloaded from the designated website ( https://nsduhweb.rti.org/respweb/homepage.cfm ). A database was used to store and merge the data by year for analysis. Among all participants, data for those aged 12–25 years ( n = 749,152) were included. We excluded participants aged 26 and older because the public data did not provide information on single or two-year age that was needed for HAPC modeling (details see statistical analysis section). We obtained approval from the Institutional Review Board at the University of Florida to conduct this study.
Variables and measurements
Current marijuana use: the dependent variable. Participants were defined as current marijuana users if they reported marijuana use within the past 30 days. We used the variable harmonization method to create a comparable measure across 31-wave NSDUH data [ 44 ]. Slightly different questions were used in NSDUH. In 1979–1993, participants were asked: “When was the most recent time that you used marijuana or hash?” Starting in 1994, the question was changed to “How long has it been since you last used marijuana or hashish?” To harmonize the marijuana use variable, participants were coded as current marijuana users if their response to the question indicated the last time to use marijuana was within past 30 days.
Chronological age, time period and birth cohort were the predictors. (1) Chronological age in years was measured with participants’ age at the survey. APC modeling requires the same age measure for all participants [ 33 ]. Since no data by single-year age were available for participants older than 21, we grouped all participants into two-year age groups. A total of 7 age groups, 12–13, ..., 24–25 were used. (2) Time period was measured with the year when the survey was conducted, including 1979, 1982, 1985, 1988, 1990, 1991... 2016. (3). Birth cohort was the year of birth, and it was measured by subtracting age from the survey year.
The proportion of people covered by MML: This variable was created by dividing the population in all states with MML over the total US population. The proportion was computed by year from 1996 when California first passed the MML to 2016 when a total of 29 states legalized medical marijuana use. The estimated proportion ranged from 12% in 1996 to 61% in 2016. The proportion of people covered by RML: This variable was derived by dividing the population in all states with RML with the total US population. The estimated proportion ranged from 4% in 2012 to 21% in 2016. These two variables were used to quantitatively assess the relationships between marijuana laws and changes in the risk of marijuana use.
Covariates: Demographic variables gender (male/female) and race/ethnicity (White, Black, Hispanic and others) were used to describe the study sample.
Statistical analysis
We estimated the prevalence of current marijuana use by year using the survey estimation method, considering the complex multi-stage cluster random sampling design and unequal probability. A prevalence rate is not a simple indicator, but consisting of the impact of chronological age, time period and birth cohort, named as age, period and cohort effects, respectively. Thus, it is biased if a prevalence rate is directly used to depict the historical trend. HAPC modeling is an epidemiological method capable of decomposing prevalence rate into mutually independent age, period and cohort effects with individual-level data, while the estimated period and cohort effects provide an unbiased measure of historical trend controlling for the effects of age and other covariates. In this study, we analyzed the data using the two-level HAPC cross-classified random-effects model (CCREM) [ 36 ]:
Where M ijk represents the rate of marijuana use for participants in age group i (12–13, 14,15...), period j (1979, 1982,...) and birth cohort k (1954–55, 1956–57...); parameter α i (age effect) was modeled as the fixed effect; and parameters β j (period effect) and γ k (cohort effect) were modeled as random effects; and β m was used to control m covariates, including the two dummy variables assessing changes made to the NSDUH in 1999 and 2002, respectively.
The HAPC modeling analysis was executed using the PROC GLIMMIX. Sample weights were included to obtain results representing the total US population aged 12–25. A ridge-stabilized Newton-Raphson algorithm was used for parameter estimation. Modeling analysis was conducted for the overall sample, stratified by gender. The estimated age effect α i , period β j and cohort γ k (i.e., the log-linear regression coefficients) were directly plotted to visualize the pattern of change.
To gain insight into the relationship between legal events and regulations at the national level, we listed these events/regulations along with the estimated time trends in the risk of marijuana from HAPC modeling. To provide a quantitative measure, we associated the estimated period effect with the proportions of US population living with MML and RML using Pearson correlation. All statistical analyses for this study were conducted using the software SAS, version 9.4 (SAS Institute Inc., Cary, NC).
Sample characteristics
Data for a total of 749,152 participants (12–25 years old) from all 31-wave NSDUH covering a 38-year period were analyzed. Among the total sample (Table 1 ), 48.96% were male and 58.78% were White, 14.84% Black, and 18.40% Hispanic.
Prevalence rate of current marijuana use
As shown in Fig. 1 , the estimated prevalence rates of current marijuana use from 1979 to 2016 show a “V” shaped pattern. The rate was 27.57% in 1979, it declined to 8.02% in 1992, followed by a gradual increase to 14.70% by 2016. The pattern was the same for both male and female with males more likely to use than females during the whole period.
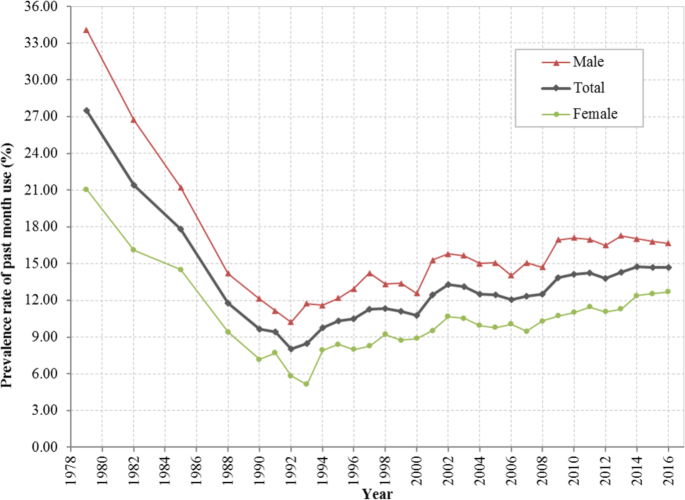
Prevalence rate (%) of current marijuana use among US residents 12 to 25 years of age during 1979–2016, overall and stratified by gender. Derived from data from the 1979–2016 National Survey on Drug Use and Health (NSDUH)
HAPC modeling and results
Estimated age effects α i from the CCREM [ 1 ] for current marijuana use are presented in Fig. 2 . The risk by age shows a 2-phase pattern –a rapid increase phase from ages 12 to 19, followed by a gradually declining phase. The pattern was persistent for the overall sample and for both male and female subsamples.
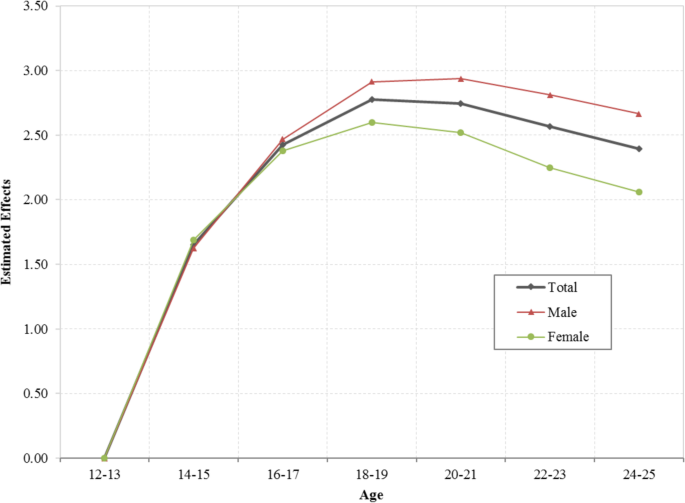
Age effect for the risk of current marijuana use, overall and stratified by male and female, estimated with hierarchical age-period-cohort modeling method with 31 waves of NSDUH data during 1979–2016. Age effect α i were log-linear regression coefficients estimated using CCREM (1), see text for more details
The estimated period effects β j from the CCREM [ 1 ] are presented in Fig. 3 . The period effect reflects the risk of current marijuana use due to significant events occurring over the period, particularly federal and state laws and regulations. After controlling for the impacts of age, cohort and other covariates, the estimated period effect indicates that the risk of current marijuana use had two declining trends (1979–1992 and 2001–2006), and two increasing trends (1992–2001 and 2006–2016). Epidemiologically, the time trends characterized by the estimated period effects in Fig. 3 are more valid than the prevalence rates presented in Fig. 1 because the former was adjusted for confounders while the later was not.
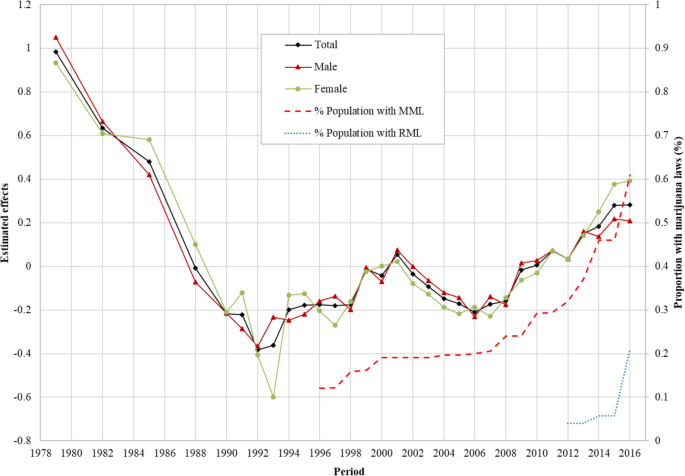
Period effect for the risk of marijuana use for US adolescents and young adults, overall and by male/female estimated with hierarchical age-period-cohort modeling method and its correlation with the proportion of US population covered by Medical Marijuana Laws and Recreational Marijuana Laws. Period effect β j were log-linear regression coefficients estimated using CCREM (1), see text for more details
Correlation of the period effect with proportions of the population covered by marijuana laws: The Pearson correlation coefficient of the period effect with the proportions of US population covered by MML during 1996–2016 was 0.89 for the total sample, 0.81 for male and 0.93 for female, respectively ( p < 0.01 for all). The correlation between period effect and proportion of US population covered by RML was 0.64 for the total sample, 0.59 for male and 0.49 for female ( p > 0.05 for all).
Likewise, the estimated cohort effects γ k from the CCREM [ 1 ] are presented in Fig. 4 . The cohort effect reflects changes in the risk of current marijuana use over the period indicated by the year of birth of the survey participants after the impacts of age, period and other covariates are adjusted. Results in the figure show three distinctive cohorts with different risk patterns of current marijuana use during 1954–2003: (1) the Historical Declining Cohort (HDC): those born in 1954–1972, and characterized by a gradual and linear declining trend with some fluctuations; (2) the Sudden Increase Cohort (SIC): those born from 1972 to 1984, characterized with a rapid almost linear increasing trend; and (3) the Contemporary Declining Cohort (CDC): those born during 1984 and 2003, and characterized with a progressive declining over time. The detailed results of HAPC modeling analysis were also shown in Additional file 1 : Table S1.

Cohort effect for the risk of marijuana use among US adolescents and young adults born during 1954–2003, overall and by male/female, estimated with hierarchical age-period-cohort modeling method. Cohort effect γ k were log-linear regression coefficients estimated using CCREM (1), see text for more details
This study provides new data regarding the risk of marijuana use in youth in the US during 1954–2016. This is a period in the US history with substantial increases and declines in drug use, including marijuana; accompanied with many ups and downs in legal actions against drug use since the 1970s and progressive marijuana legalization at the state level from the later 1990s till today (see Additional file 1 : Table S2). Findings of the study indicate four-phase period effect and three-phase cohort effect, corresponding to various historical events of marijuana laws, regulations and social movements.
Coincident relationship between the period effect and legal drug control
The period effect derived from the HAPC model provides a net effect of the impact of time on marijuana use after the impact of age and birth cohort were adjusted. Findings in this study indicate that there was a progressive decline in the period effect during 1979 and 1992. This trend was corresponding to a period with the strongest legal actions at the national level, the War on Drugs by President Nixon (1969–1974) President Reagan (1981–1989) [ 45 ], and President Bush (1989) [ 45 ],and the Anti-Drug Abuse Act (1986) [ 5 ].
The estimated period effect shows an increasing trend in 1992–2001. During this period, President Clinton advocated for the use of treatment to replace incarceration (1992) [ 45 ], Surgeon General Elders proposed to study marijuana legalization (1993–1994) [ 8 ], President Clinton’s position of the need to re-examine the entire policy against people who use drugs, and decriminalization of marijuana (2000) [ 45 ] and the passage of MML in eight US states.
The estimated period effect shows a declining trend in 2001–2006. Important laws/regulations include the Student Drug Testing Program promoted by President Bush, and the broadened the public schools’ authority to test illegal drugs among students given by the US Supreme Court (2002) [ 46 ].
The estimated period effect increases in 2006–2016. This is the period when the proportion of the population covered by MML progressively increased. This relation was further proved by a positive correlation between the estimated period effect and the proportion of the population covered by MML. In addition, several other events occurred. For example, over 500 economists wrote an open letter to President Bush, Congress and Governors of the US and called for marijuana legalization (2005) [ 47 ], and President Obama ended the federal interference with the state MML, treated marijuana as public health issues, and avoided using the term of “War on Drugs” [ 45 ]. The study also indicates that the proportion of population covered by RML was positively associated with the period effect although not significant which may be due to the limited number of data points of RML. Future studies may follow up to investigate the relationship between RML and rate of marijuana use.

Coincident relationship between the cohort effect and legal drug control
Cohort effect is the risk of marijuana use associated with the specific year of birth. People born in different years are exposed to different laws, regulations in the past, therefore, the risk of marijuana use for people may differ when they enter adolescence and adulthood. Findings in this study indicate three distinctive cohorts: HDC (1954–1972), SIC (1972–1984) and CDC (1984–2003). During HDC, the overall level of marijuana use was declining. Various laws/regulations of drug use in general and marijuana in particular may explain the declining trend. First, multiple laws passed to regulate the marijuana and other substance use before and during this period remained in effect, for example, the Marijuana Tax Act (1937), the Boggs Act (1952), the Narcotics Control Act (1956) and the Controlled Substance Act (1970). Secondly, the formation of government departments focusing on drug use prevention and control may contribute to the cohort effect, such as the Bureau of Narcotics and Dangerous Drugs (1968) [ 48 ]. People born during this period may be exposed to the macro environment with laws and regulations against marijuana, thus, they may be less likely to use marijuana.
Compared to people born before 1972, the cohort effect for participants born during 1972 and 1984 was in coincidence with the increased risk of using marijuana shown as SIC. This trend was accompanied by the state and federal movements for marijuana use, which may alter the social environment and public attitudes and beliefs from prohibitive to acceptive. For example, seven states passed laws to decriminalize the marijuana use and reduced the penalty for personal possession of small amount of marijuana in 1976 [ 7 ]. Four more states joined the movement in two subsequent years [ 7 ]. People born during this period may have experienced tolerated environment of marijuana, and they may become more acceptable of marijuana use, increasing their likelihood of using marijuana.
A declining cohort CDC appeared immediately after 1984 and extended to 2003. This declining cohort effect was corresponding to a number of laws, regulations and movements prohibiting drug use. Typical examples included the War on Drugs initiated by President Nixon (1980s), the expansion of the drug war by President Reagan (1980s), the highly-publicized anti-drug campaign “Just Say No” by First Lady Nancy Reagan (early 1980s) [ 45 ], and the Zero Tolerance Policies in mid-to-late 1980s [ 45 ], the Anti-Drug Abuse Act (1986) [ 5 ], the nationally televised speech of War on Drugs declared by President Bush in 1989 and the escalated War on Drugs by President Clinton (1993–2001) [ 45 ]. Meanwhile many activities of the federal government and social groups may also influence the social environment of using marijuana. For example, the Federal government opposed to legalize the cultivation of industrial hemp, and Federal agents shut down marijuana sales club in San Francisco in 1998 [ 48 ]. Individuals born in these years grew up in an environment against marijuana use which may decrease their likelihood of using marijuana when they enter adolescence and young adulthood.
This study applied the age-period-cohort model to investigate the independent age, period and cohort effects, and indicated that the model derived trends in marijuana use among adolescents and young adults were coincident with the laws and regulations on marijuana use in the United States since the 1950s. With more states legalizing marijuana use in the United States, emphasizing responsible use would be essential to protect youth from using marijuana.
Limitations
This study has limitations. First, study data were collected through a household survey, which is subject to underreporting. Second, no causal relationship can be warranted using cross-sectional data, and further studies are needed to verify the association between the specific laws/regulation and the risk of marijuana use. Third, data were available to measure single-year age up to age 21 and two-year age group up to 25, preventing researchers from examining the risk of marijuana use for participants in other ages. Lastly, data derived from NSDUH were nation-wide, and future studies are needed to analyze state-level data and investigate the between-state differences. Although a systematic review of all laws and regulations related to marijuana and other drugs is beyond the scope of this study, findings from our study provide new data from a historical perspective much needed for the current trend in marijuana legalization across the nation to get the benefit from marijuana while to protect vulnerable children and youth in the US. It provides an opportunity for stack-holders to make public decisions by reviewing the findings of this analysis together with the laws and regulations at the federal and state levels over a long period since the 1950s.
Availability of data and materials
The data of the study are available from the designated repository ( https://nsduhweb.rti.org/respweb/homepage.cfm ).
Abbreviations
Audio computer-assisted self-interviews
Age-period-cohort modeling
Computer-assisted person interviews
Cross-classified random-effects model
Contemporary Declining Cohort
Hierarchical age-period-cohort
Historical Declining Cohort
Medical Marijuana Laws
National Household Survey on Drug Abuse
National Survey on Drug Use and Health
Recreational Marijuana Laws
Sudden Increase Cohort
The United States
CDC. Marijuana and Public Health. 2017. Available from: https://www.cdc.gov/marijuana/index.htm . Accessed 13 June 2018.
SAMHSA. Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. 2016 [cited 2018 Jan 31]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm
Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda, Board on Population Health and Public Health Practice, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, D.C.: National Academies Press; 2017.
Collins C. Adverse health effects of marijuana use. N Engl J Med. 2014;371(9):879.
PubMed Google Scholar
Belenko SR. Drugs and drug policy in America: a documentary history. Westport: Greenwood Press; 2000.
Google Scholar
Gerber RJ. Legalizing marijuana: Drug policy reform and prohibition politics. Westport: Praeger; 2004.
Single EW. The impact of marijuana decriminalization: an update. J Public Health Policy. 1989:456–66.
Article CAS Google Scholar
SFChronicle. Ex-surgeon general backed legalizing marijuana before it was cool [Internet]. 2016 [cited 2018 Oct 7]. Available from: https://www.sfchronicle.com/business/article/Ex-surgeon-general-backed-legalizing-marijuana-6799348.php
PROCON. 31 Legal Medical Marijuana States and DC. 2018 [cited 2018 Oct 4]. Available from: https://medicalmarijuana.procon.org/view.resource.php?resourceID=000881
Bifulco M, Pisanti S. Medicinal use of cannabis in Europe: the fact that more countries legalize the medicinal use of cannabis should not become an argument for unfettered and uncontrolled use. EMBO Rep. 2015;16(2):130–2.
European Monitoring Centre for Drugs and Drug Addiction. Models for the legal supply of cannabis: recent developments (Perspectives on drugs). 2016. Available from: http://www.emcdda.europa.eu/publications/pods/legal-supply-of-cannabis . Accessed 10 Jan 2020.
European Monitoring Centre for Drugs and Drug Addiction. Cannabis policy: status and recent developments. 2017. Available from: http://www.emcdda.europa.eu/topics/cannabis-policy_en#section2 . Accessed 10 Jan 2020.
Hughes B, Matias J, Griffiths P. Inconsistencies in the assumptions linking punitive sanctions and use of cannabis and new psychoactive substances in Europe. Addiction. 2018;113(12):2155–7.
Article Google Scholar
Anderson DM, Hansen B, Rees DI. Medical marijuana laws and teen marijuana use. Am Law Econ Rev. 2015;17(2):495-28.
United States Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States, States, and Puerto Rico Commonwealth: April 1, 2010 to July 1, 2016 2016 Population Estimates. 2017 [cited 2018 Mar 14]. Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
Chen X, Yu B, Lasopa S, Cottler LB. Current patterns of marijuana use initiation by age among US adolescents and emerging adults: implications for intervention. Am J Drug Alcohol Abuse. 2017;43(3):261–70.
Miech R, Koester S. Trends in U.S., past-year marijuana use from 1985 to 2009: an age-period-cohort analysis. Drug Alcohol Depend. 2012;124(3):259–67.
Steinberg L. The influence of neuroscience on US supreme court decisions about adolescents’ criminal culpability. Nat Rev Neurosci. 2013;14(7):513–8.
Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, et al. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction. 2018;113(6):1003–16.
Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601–8.
Pacula RL, Chriqui JF, King J. Marijuana decriminalization: what does it mean in the United States? National Bureau of Economic Research; 2003.
Donnelly N, Hall W, Christie P. The effects of the Cannabis expiation notice system on the prevalence of cannabis use in South Australia: evidence from the National Drug Strategy Household Surveys 1985-95. Drug Alcohol Rev. 2000;19(3):265–9.
Gorman DM, Huber JC. Do medical cannabis laws encourage cannabis use? Int J Drug Policy. 2007;18(3):160–7.
Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013 Aug;103(8):1500–6.
Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana and alcohol use: the devil is in the details. National Bureau of Economic Research; 2013.
Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–12.
Stolzenberg L, D’Alessio SJ, Dariano D. The effect of medical cannabis laws on juvenile cannabis use. Int J Drug Policy. 2016;27:82–8.
Wang GS, Roosevelt G, Heard K. Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatr. 2013;167(7):630–3.
Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–6.
Chen X, Yu B, Stanton B, Cook RL, Chen D-GD, Okafor C. Medical marijuana laws and marijuana use among U.S. adolescents: evidence from michigan youth risk behavior surveillance data. J Drug Educ. 2018;47237918803361.
Chen X. Information diffusion in the evaluation of medical marijuana laws’ impact on risk perception and use. Am J Public Health. 2016;106(12):e8.
Chen X, Yu B, Stanton B, Cook RL, Chen DG, Okafor C. Medical marijuana laws and marijuana use among US adolescents: Evidence from Michigan youth risk behavior surveillance data. J Drug Educ. 2018;48(1-2):18-35.
Yang Y, Land K. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. Boca Raton: Chapman and Hall/CRC; 2013.
Yu B, Chen X. Age and birth cohort-adjusted rates of suicide mortality among US male and female youths aged 10 to 19 years from 1999 to 2017. JAMA Netw Open. 2019;2(9):e1911383.
Akiba S. Epidemiological studies of Fukushima residents exposed to ionising radiation from the Fukushima Daiichi nuclear power plant prefecture--a preliminary review of current plans. J Radiol Prot. 2012;32(1):1–10.
Yang Y, Land KC. Age-period-cohort analysis of repeated cross-section surveys: fixed or random effects? Sociol Methods Res. 2008;36(3):297–326.
O’Brien R. Age-period-cohort models: approaches and analyses with aggregate data. Boca Raton: Chapman and Hall/CRC; 2014.
Book Google Scholar
Chen X, Sun Y, Li Z, Yu B, Gao G, Wang P. Historical trends in suicide risk for the residents of mainland China: APC modeling of the archived national suicide mortality rates during 1987-2012. Soc Psychiatry Psychiatr Epidemiol. 2018;54(1):99–110.
Yang Y. Social inequalities in happiness in the United States, 1972 to 2004: an age-period-cohort analysis. Am Sociol Rev. 2008;73(2):204–26.
Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69(10):1439–48.
Kerr WC, Lui C, Ye Y. Trends and age, period and cohort effects for marijuana use prevalence in the 1984-2015 US National Alcohol Surveys. Addiction. 2018;113(3):473–81.
Johnson RA, Gerstein DR. Age, period, and cohort effects in marijuana and alcohol incidence: United States females and males, 1961-1990. Substance Use Misuse. 2000;35(6–8):925–48.
Substance Abuse and Mental Health Services Administration. Results from the 2013 NSDUH: Summary of National Findings, SAMHSA, CBHSQ. 2014 [cited 2018 Sep 23]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.htm
Bauer DJ, Hussong AM. Psychometric approaches for developing commensurate measures across independent studies: traditional and new models. Psychol Methods. 2009;14(2):101–25.
Drug Policy Alliance. A Brief History of the Drug War. 2018 [cited 2018 Sep 27]. Available from: http://www.drugpolicy.org/issues/brief-history-drug-war
NIDA. Drug testing in schools. 2017 [cited 2018 Sep 27]. Available from: https://www.drugabuse.gov/related-topics/drug-testing/faq-drug-testing-in-schools
Wikipedia contributors. Legal history of cannabis in the United States. 2015. Available from: https://en.wikipedia.org/w/index.php?title=Legal_history_of_cannabis_in_the_United_States&oldid=674767854 . Accessed 24 Oct 2017.
NORML. Marijuana law reform timeline. 2015. Available from: http://norml.org/shop/item/marijuana-law-reform-timeline . Accessed 24 Oct 2017.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Epidemiology, University of Florida, Gainesville, FL, 32608, USA
Bin Yu & Xinguang Chen
Department of Epidemiology and Health Statistics School of Health Sciences, Wuhan University, Wuhan, 430071, China
Xiangfan Chen & Hong Yan
You can also search for this author in PubMed Google Scholar
Contributions
BY designed the study, collected the data, conducted the data analysis, drafted and reviewed the manuscript; XGC designed the study and reviewed the manuscript. XFC and HY reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Hong Yan .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Institutional Review Board at the University of Florida. Data in the study were public available.
Consent for publication
All authors consented for the publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: table s1..
Estimated Age, Period, Cohort Effects for the Trend of Marijuana Use in Past Month among Adolescents and Emerging Adults Aged 12 to 25 Years, NSDUH, 1979-2016. Table S2. Laws at the federal and state levels related to marijuana use.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Yu, B., Chen, X., Chen, X. et al. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health. BMC Public Health 20 , 156 (2020). https://doi.org/10.1186/s12889-020-8253-4
Download citation
Received : 15 June 2019
Accepted : 21 January 2020
Published : 04 February 2020
DOI : https://doi.org/10.1186/s12889-020-8253-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents and young adults
- United States
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
The Evidence—and Lack Thereof—About Cannabis
Research is still needed on cannabis’s risks and benefits.
Lindsay Smith Rogers
Although the use and possession of cannabis is illegal under federal law, medicinal and recreational cannabis use has become increasingly widespread.
Thirty-eight states and Washington, D.C., have legalized medical cannabis, while 23 states and D.C. have legalized recreational use. Cannabis legalization has benefits, such as removing the product from the illegal market so it can be taxed and regulated, but science is still trying to catch up as social norms evolve and different products become available.
In this Q&A, adapted from the August 25 episode of Public Health On Call , Lindsay Smith Rogers talks with Johannes Thrul, PhD, MS , associate professor of Mental Health , about cannabis as medicine, potential risks involved with its use, and what research is showing about its safety and efficacy.
Do you think medicinal cannabis paved the way for legalization of recreational use?
The momentum has been clear for a few years now. California was the first to legalize it for medical reasons [in 1996]. Washington and Colorado were the first states to legalize recreational use back in 2012. You see one state after another changing their laws, and over time, you see a change in social norms. It's clear from the national surveys that people are becoming more and more in favor of cannabis legalization. That started with medical use, and has now continued into recreational use.
But there is a murky differentiation between medical and recreational cannabis. I think a lot of people are using cannabis to self-medicate. It's not like a medication you get prescribed for a very narrow symptom or a specific disease. Anyone with a medical cannabis prescription, or who meets the age limit for recreational cannabis, can purchase it. Then what they use it for is really all over the place—maybe because it makes them feel good, or because it helps them deal with certain symptoms, diseases, and disorders.
Does cannabis have viable medicinal uses?
The evidence is mixed at this point. There hasn’t been a lot of funding going into testing cannabis in a rigorous way. There is more evidence for certain indications than for others, like CBD for seizures—one of the first indications that cannabis was approved for. And THC has been used effectively for things like nausea and appetite for people with cancer.
There are other indications where the evidence is a lot more mixed. For example, pain—one of the main reasons that people report for using cannabis. When we talk to patients, they say cannabis improved their quality of life. In the big studies that have been done so far, there are some indications from animal models that cannabis might help [with pain]. When we look at human studies, it's very much a mixed bag.
And, when we say cannabis, in a way it's a misnomer because cannabis is so many things. We have different cannabinoids and different concentrations of different cannabinoids. The main cannabinoids that are being studied are THC and CBD, but there are dozens of other minor cannabinoids and terpenes in cannabis products, all of varying concentrations. And then you also have a lot of different routes of administration available. You can smoke, vape, take edibles, use tinctures and topicals. When you think about the explosion of all of the different combinations of different products and different routes of administration, it tells you how complicated it gets to study this in a rigorous way. You almost need a randomized trial for every single one of those and then for every single indication.
What do we know about the risks of marijuana use?
Cannabis use disorder is a legitimate disorder in the DSM. There are, unfortunately, a lot of people who develop a problematic use of cannabis. We know there are risks for mental health consequences. The evidence is probably the strongest that if you have a family history of psychosis or schizophrenia, using cannabis early in adolescence is not the best idea. We know cannabis can trigger psychotic symptoms and potentially longer lasting problems with psychosis and schizophrenia.
It is hard to study, because you also don't know if people are medicating early negative symptoms of schizophrenia. They wouldn't necessarily have a diagnosis yet, but maybe cannabis helps them to deal with negative symptoms, and then they develop psychosis. There is also some evidence that there could be something going on with the impact of cannabis on the developing brain that could prime you to be at greater risk of using other substances later down the road, or finding the use of other substances more reinforcing.
What benefits do you see to legalization?
When we look at the public health landscape and the effect of legislation, in this case legalization, one of the big benefits is taking cannabis out of the underground illegal market. Taking cannabis out of that particular space is a great idea. You're taking it out of the illegal market and giving it to legitimate businesses where there is going to be oversight and testing of products, so you know what you're getting. And these products undergo quality control and are labeled. Those labels so far are a bit variable, but at least we're getting there. If you're picking up cannabis at the street corner, you have no idea what's in it.
And we know that drug laws in general have been used to criminalize communities of color and minorities. Legalizing cannabis [can help] reduce the overpolicing of these populations.
What big questions about cannabis would you most like to see answered?
We know there are certain, most-often-mentioned conditions that people are already using medical cannabis for: pain, insomnia, anxiety, and PTSD. We really need to improve the evidence base for those. I think clinical trials for different cannabis products for those conditions are warranted.
Another question is, now that the states are getting more tax revenue from cannabis sales, what are they doing with that money? If you look at tobacco legislation, for example, certain states have required that those funds get used for research on those particular issues. To me, that would be a very good use of the tax revenue that is now coming in. We know, for example, that there’s a lot more tax revenue now that Maryland has legalized recreational use. Maryland could really step up here and help provide some of that evidence.
Are there studies looking into the risks you mentioned?
Large national studies are done every year or every other year to collect data, so we already have a pretty good sense of the prevalence of cannabis use disorder. Obviously, we'll keep tracking that to see if those numbers increase, for example, in states that are legalizing. But, you wouldn't necessarily expect to see an uptick in cannabis use disorder a month after legalization. The evidence from states that have legalized it has not demonstrated that we might all of a sudden see an increase in psychosis or in cannabis use disorder. This happens slowly over time with a change in social norms and availability, and potentially also with a change in marketing. And, with increasing use of an addictive substance, you will see over time a potential increase in problematic use and then also an increase in use disorder.
If you're interested in seeing if cannabis is right for you, is this something you can talk to your doctor about?
I think your mileage may vary there with how much your doctor is comfortable and knows about it. It's still relatively fringe. That will very much depend on who you talk to. But I think as providers and professionals, everybody needs to learn more about this, because patients are going to ask no matter what.
Lindsay Smith Rogers, MA, is the producer of the Public Health On Call podcast , an editor for Expert Insights , and the director of content strategy for the Johns Hopkins Bloomberg School of Public Health.
Could Medical Marijuana Help Address the Opioid Epidemic?
Policy Is Public Health
Medical Marijuana Laws Linked to Health and Labor Supply Benefits in Older Adults
Related Content

How Dangerous is Dengue?

Research Identifies Characteristics of Cities That Would Support Young People’s Mental Health

Alumni Spotlight: Junrui Di, PhD '19

Child Diarrhea Has a Cheap and Easy Fix—Why Isn’t It Reaching Patients?

How Abortion Trigger Laws Impact Mental Health
Effects of cannabis legalization on the use of cannabis and other substances
Affiliations.
- 1 Department of Epidemiology, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, 90110.
- 2 Department of Psychiatry, Faculty of Medicine, Chulalongkorn University.
- 3 Department of Psychiatry, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok.
- 4 Srithanya Psychiatric Hospital, Nonthaburi, Thailand.
- PMID: 37185310
- DOI: 10.1097/YCO.0000000000000868
Purpose of review: As more jurisdictions legalize cannabis for non-medical use, the evidence on how legalization policies affect cannabis use and the use of other substances remains inconclusive and contradictory. This review aims to summarize recent research findings on the impact of recreational cannabis legalization (RCL) on cannabis and other substance use among different population groups, such as youth and adults.
Recent findings: Recent literature reports mixed findings regarding changes in the prevalence of cannabis use after the adoption of RCL. Most studies found no significant association between RCL and changes in cannabis use among youth in European countries, Uruguay, the US, and Canada. However, some studies have reported increases in cannabis use among youth and adults in the US and Canada, although these increases seem to predate RCL. Additionally, there has been a marked increase in unintentional pediatric ingestion of cannabis edibles postlegalization, and an association between RCL and increased alcohol, vaping, and e-cigarette use among adolescents and young adults.
Summary: Overall, the effects of cannabis legalization on cannabis use appear to be mixed. Further monitoring and evaluation research is needed to provide longer-term evidence and a more comprehensive understanding of the effects of RCL.
Copyright © 2023 Wolters Kluwer Health, Inc. All rights reserved.
Publication types
- Canada / epidemiology
- Cannabis* / adverse effects
- Electronic Nicotine Delivery Systems*
- Legislation, Drug
- Marijuana Use* / adverse effects
- Marijuana Use* / epidemiology
- Young Adult
This website uses cookies.
By clicking the "Accept" button or continuing to browse our site, you agree to first-party and session-only cookies being stored on your device to enhance site navigation and analyze site performance and traffic. For more information on our use of cookies, please see our Privacy Policy .
- Journal of Economic Literature
The Public Health Effects of Legalizing Marijuana
- D. Mark Anderson
- Daniel I. Rees
- Article Information
Additional Materials
- Author Disclosure Statement(s) (158.63 KB)
JEL Classification
- R41 Transportation: Demand, Supply, and Congestion; Travel Time; Safety and Accidents; Transportation Noise
The Effects of Recreational Marijuana Legalization on Employment and Earnings
Despite nearly 70 percent of the American public supporting legalization of recreational marijuana, opponents argue that increased marijuana use may diminish motivation, impede cognitive function, and harm health, each of which could adversely affect adults’ economic wellbeing. This study is the first to explore the impacts of recreational marijuana laws (RMLs) on employment and wages. Difference-in-differences estimates show little evidence that RMLs adversely affect labor market outcomes among most working-age individuals. Rather, our estimates show that RML adoption is associated with an increase in agricultural employment, consistent with the opening of a new licit market. A causal interpretation of our findings is supported by (1) event-study analyses using dynamic difference-in-differences estimates designed to expunge bias due to heterogeneous and dynamic treatment effects, and (2) alternative policy estimates generated using a synthetic control design.
Dr. Sabia acknowledges research support from the Center for Health Economics & Policy Studies (CHEPS) at San Diego State University, which has received grant funding from the Charles Koch Foundation and the Troesh Family Foundation. We thank Evan Kim for excellent research assistance on an earlier version of this paper. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
Dr. Sabia acknowledges research support from the Center for Health Economics & Policy Studies (CHEPS) at San Diego State University, which includes grants received from the Charles Koch Foundation.
MARC RIS BibTeΧ
Download Citation Data
Mentioned in the News
More from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

Marijuana and Cannabinoids: Health, Research and Regulatory Considerations (Position Paper)
Executive summary.
Marijuana and related substance misuse are complex issues impacting family medicine, patient health, and public health. The American Academy of Family Physicians (AAFP) believes family physicians are essential in addressing all forms of inappropriate substance use. The AAFP urges its members to be involved in the diagnosis, treatment, and prevention of substance use, as well as secondary diseases impacted or caused by use. The World Health Organization (WHO) reports approximately 2.5% of the global population uses cannabis annually, making it the most commonly used drug worldwide. 1 Simultaneously, the AAFP acknowledges preliminary evidence indicates marijuana and cannabinoids may have potential therapeutic benefits, while also recognizing subsequent negative public health and health outcomes associated with cannabis use. 2
During the 20 th century, law enforcement and public policy activities have undermined opportunities for scientific exploration. Barriers to facilitating both clinical and public health research regarding marijuana is detrimental to treating patients and the health of the public. The lack of regulation poses a danger to public health and impedes meaningful, patient-centered research to exploring both therapeutic and negative impacts of marijuana and cannabinoids.
Relevant AAFP Policy
Marijuana Possession for Personal Use The American Academy of Family Physicians (AAFP) opposes the recreational use of marijuana. However, the AAFP supports decriminalization of possession of marijuana for personal use. The AAFP recognizes the benefits of intervention and treatment for the recreational use of marijuana, in lieu of incarceration, for all individuals, including youth. 3
The AAFP also recognizes that several states have passed laws approving limited recreational use and/or possession of marijuana. Therefore, the AAFP advocates for further research into the overall safety and health effects of recreational use, as well as the effects of those laws on patient and societal health. 4
It should be noted that cannabis and marijuana are not interchangeable terms. In this position paper, cannabis is an overarching term used to refer to the plant Cannabis sativa . Substances derived from the cannabis plant include marijuana, hemp, and cannabinoids.
Call to Action Family physicians have a vested interest in policies that advance and protect the health of their patients and the public. The regulatory environment surrounding cannabis, medical and recreational marijuana, and cannabidiol (CBD) is rapidly changing, along with the retail environment. This shift has not been accompanied by robust scientific research regarding the health effects of cannabis, both therapeutic or detrimental. The AAFP recognizes the need for substantial clinical, public health, and policy evidence and research regarding cannabis, marijuana, cannabinoids, and CBD to inform evidence-based practice and the impact on public health.
- The AAFP promotes a society which is free of substance misuse, including alcohol and drugs. 3
- The AAFP recognizes there is support for the medical use of marijuana and cannabinoids, but advocates that usage be based on high-quality, evidence-based public health, policy, and patient-centered research, including the impact on vulnerable populations. 3
- The AAFP advocates for further studies into the use of medical marijuana and related compounds. This process should also ensure appropriate funding allocated for this research.
- The AAFP calls for decreased regulatory barriers to facilitate clinical and public health cannabis research, including reclassifying cannabis from a Schedule I controlled substance. 3
- The AAFP advocates for further research into the overall safety and health effects of recreational use, as well as the impact of legal recreational marijuana use laws on patient and societal health. 4
- The AAFP advocates for robust regulation regarding labeling and child-proof packaging of all marijuana and cannabinoid products.
- The AAFP opposes the recreational use and legalization of marijuana, but supports decriminalization of marijuana for personal use. The AAFP recognizes the benefits associated with intervention and treatment, in lieu of incarceration. 4
- The AAFP advocates for regulation regarding marketing claims, labeling, and advertising of all marijuana and cannabinoid products.
- The AAFP supports requirements testing current marijuana and cannabinoid products for safety, dosing, and product consistency.
In the Exam Room
- The AAFP urges its members to be involved in the diagnosis, treatment, and prevention of substance use, as well as the secondary diseases impacted by use.
- The AAFP calls for family physicians to discuss the health consequences of marijuana and cannabis use, as well as prevention strategies to prevent use and unintended consequences of marijuana exposure in at-risk populations.
Cannabis use, both medically and recreationally, is prevalent throughout history. Extensive evidence indicates cannabis was used by ancient civilizations, dating back more than 5,000 years ago. 1 In the U.S. in the 19th and early 20th centuries, cannabis was frequently used for medicinal purposes, often prescribed by clinicians. 1,5 Cannabis was first listed in the United States Pharmacopoeia in 1851, indicating use as an analgesic, hypnotic, and anticonvulsant agent. 5 After the 1937 Marihuana Tax Act , in 1942, cannabis was removed from the United States Pharmacopoeia . 5
Attitudes and perceived risk of marijuana use have changed with the varying levels of legalization in the U.S. Surveying marijuana use is essential to gauge public health implications of increased access to marijuana, cannabinoid, and cannabis products. According to the 2018 National Institute on Drug Abuse (NIDA) Monitoring the Future Survey (MTF), daily, past month, past year, and lifetime marijuana use among 8 th graders has declined, and remained unchanged in 10 th and 12 th graders, when compared to the 2013 MTF survey. 6 Despite the changing landscape of marijuana regulations nationwide, past year use of marijuana reached and maintained its lowest levels in more than two decades in 2016 among 8 th and 10 th graders. 6 However, marijuana vaping did significantly increase between 2017 and 2018, mirroring trends in youth tobacco use. 6 The NIDA 2017 National Survey on Drug Use and Health indicates nearly 53% of adults between the ages of 18-25 have tried marijuana at some point in their lifetime, 35% have used marijuana within the past year, and 22% within the past month. 7 While the lifetime use remains relatively stable for this cohort, from 2015-2017, past year and past month use increased 2.7% and 2.3%, respectively. 7 Nearly half of adults 26 or older reported using marijuana at some point in their lifetime. 7 Although adults ages 26 and up report the highest percentage of lifetime use, this age group has a significantly lower past year use (12%) and past month use (8%). 7
Forms and Use of Cannabis The cannabis plant, Cannabis sativa , is comprised of both non-psychoactive and psychoactive chemicals called cannabinoids. 5 The cannabinoid commonly known for its psychoactive properties is delta-9-tetrahydrocannabinol (THC). 5 CBD is the most abundant cannabinoid in cannabis, and is considered to be largely non-psychoactive. 5 The biological system responsible for the synthesis and degradation of cannabinoids in mammals is referred to as the endocannabinoid system, which is largely comprised of two g-coupled protein receptors (GPCRs). 8 The GPCRs—CB1 and CB2—are found throughout many bodily tissues. However, CB1 is most concentrated in the neural tissues. 5,8 CB2 receptors are found in the brain, but are mostly found in immune cells, like macrophages, microglia, osteoclasts, and osteoblasts. 5,8
There are many forms of, and products derived from, the Cannabis sativa plant, including hemp, CBD, and marijuana. Cannabis sativa with less than 0.3% THC is considered industrial hemp, and can be used for industrial agriculture cultivation. 9,10 Industrial hemp can be harvested and used for many things, including fibers for textiles, food products, and building materials. 11,12 CBD, the non-psychoactive cannabinoid, is extracted from the flower of industrial hemp. 13 Marijuana and hemp, technically speaking, are the same plant. 13 However, the hemp variety of cannabis contains no more than 0.3% THC, while the marijuana variety contains 5-20% THC. 13
Marijuana and CBD are most commonly used via inhalation, ingestion, and topical absorption. 5 Inhalation can be through combustible mechanisms using dried flowers, including the use of a pipe, rolled joints, blunts, and water pipes (also called bongs). 14 Vaping marijuana and CBD concentrates are an increasingly popular inhalation method. 5,6 Concentrates, the concentrated form of marijuana and CBD, come in various forms, including oil, butter, or a dark sticky substance often referred to as shatter. 15 Concentrates can be both smoked or vaporized, and may also be used as additives or cooking agents for ingestion. 5,15 There are many different ways to ingest cannabinoids. Food products—called edibles—like brownies, gummies, cookies, and candies are common forms of cannabis ingestion, as well as liquid forms like juices, soda, and tea. 5,16 Tinctures are liquid, ultra-concentrated alcohol-based cannabis extracts commonly applied in and absorbed through the mouth. 17 Topical cannabis is applied to, and absorbed through, the skin in a cream or salve form. 18
Routes or methods of administration affect cannabis delivery. When cannabis is smoked or vaporized, onset of effect is within 5-10 minutes with a duration of 2-4 hours. 19 When ingested, effect is within 60-180 minutes with a duration of 6-8 hours. 19 The oromucosal route has an onset of 15-45 minutes and a duration of 6-8 hours. 19 Topical administration of cannabis or cannabinoids has variable onset and duration. 19 The smoked or vaporized method offers the more rapid activity for acute symptoms with the topical preparations offering less systemic effects. 19
Health Effects of Cannabis
Although there is preliminary evidence indicating cannabinoids may have some therapeutic benefit, a large portion of the evidence is very limited for many reasons. These include small sample sizes, lack of control groups, poor study design, and the use of unregulated cannabis products. There are also clear negative health and public health consequences that must be considered, as well as the need for a significant increase in evidence. More research is needed to create a robust evidence base to weigh the potential therapeutic benefits against potential negative impacts on health and public health. Currently, there are three medical formulations of cannabis approved for use in the U.S.; dronabinol, nabilone, and epidiolex. 20 Nabiximols is approved for use in the United Kingdom. 21 Dronabinol is delta-9 THC and ingested as either an oral solution or an oral capsule. 22 Nabilone is an oral capsule containing synthetic THC. 23 Epidiolex is a CBD oral solution. 24 Nabiximols is an oral mucosa spray containing the cannabinoids THC and CBD. 25
In 2015, Whiting, et al, performed a meta-analysis and systematic review of research on the medical use of cannabis. 25 This systematic review served as the basis for many recommendations in 2017 by the National Academy of Science, Engineering, and Health Report on medical marijuana. 5 Dronabinol, nabilone, and nabiximols were included in the studies. However, other cannabis formulations were found in research trials, including CBD, marijuana, and other cannabinoids. 26 Evidence is most substantial for nausea and vomiting associated with chemotherapy, chronic pain treatment, multiple sclerosis spasticity, and intractable seizures associated with Dravet syndrome and Lennox-Gastaut syndrome. 27 There is moderate evidence for the use of cannabinoids for sleep and limited evidence for use in psychiatric conditions, such as post-traumatic stress disorder, depression, anxiety, and psychosis; appetite stimulation and weight gain; and no evidence for cancer treatment. 5
Dronabinol and nabilone were both approved in 1985 for use in treating refractory chemotherapy-induced nausea and vomiting. 5,23 Dronabinol is approved by the Food and Drug Administration (FDA) for appetite stimulation and weight gain, despite limited and often inconclusive evidence that it or other cannabinoids are effective. 22 This drug has traditionally been used in human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) patients to mitigate weight loss and to treat anorexia-cachexia syndrome associated with cancer and anorexia nervosa. 5,22
Cannabinoids have been assessed for chronic pain management. Many forms of chronic pain management were studied, including cancer and chemotherapy-induced pain, fibromyalgia, neuropathic pain, rheumatoid arthritis, non-cancer pain, and musculoskeletal pain. Several studies indicate smoked THC and nabiximols were both associated with pain reduction. 5,25,26 There is limited, mixed evidence regarding the viability of cannabinoids for some forms of chronic pain management. 5 However, limitations exist with these studies, including the variable doses of THC and CBD; unregulated, non-FDA approved products; and conflicting evidence. Studies assessing cannabinoids in treating the spasticity due to multiple sclerosis or paraplegia have mixed results. The cannabinoids nabiximols, dronabinol, and TCH/CBD have all been associated with decreased spasticity. Nabilone and nabiximols were the only drugs with statically-significant decreases. 2,25
In 2018, the FDA approved a cannabidiol oral solution called epidiolex for the treatment of refractory seizures associated with Dravet syndrome and Lennox-Gastaut syndrome. 28 Epidiolex was associated with significant seizure reduction when compared to placebo. 29–31 Dravet syndrome and Lennox-Gastaut syndrome are disorders associated with severe seizures, impaired cognitive skills and development, and uncontrollable muscle contractions. 29–31
Moderate evidence exists for the use of cannabis for sleep. Nabilone and nabiximols have been associated with improvement in sleep from a baseline and sleep restfulness. 2,5,25 Improved sleep was also considered a secondary outcome when evaluating other conditions (chronic pain, multiple sclerosis) with various cannabinoids. 2,5,25
There is limited evidence for the use of cannabis or cannabinoids for the treatment of post-traumatic stress disorder (PTSD), anxiety, depression, or psychosis. Of the limited evidence, nabilone was associated with a decrease in PTSD related nightmares. 5,25 One small study indicated CBD improved public speaking anxiety. 5 There are no studies directly evaluating the effectiveness of cannabis in the treatment of depression. However, some studies measured depression as a secondary outcome, but indicated no difference in depression when compared to placebo. 25 Limited evidence (two studies) have shown no difference in treating psychosis with CBD, amisulpride, or placebo. 25 Evidence indicates individuals who use marijuana are more likely to experience temporary psychosis and chronic mental illness, including schizophrenia. 5,32
There was no evidence or insufficient evidence for the use of cannabis or cannabinoids in the treatment of cancer; neurodegenerative disorders like Huntington’s chorea, Parkinson’s disease, or amyotrophic lateral sclerosis; irritable bowel syndrome; or addiction. 5
Cannabis overdose is rare in adults and adolescents. 33 Children who experience acute intoxication from cannabis generally ingest marijuana or other cannabinoids through experimentation. 33 When compared to adults and adolescents, children are more likely to experience life-threatening symptoms of acute cannabis intoxication, which may include depressed respiration rates, hyperkinesis, or coma. 33 Management consists of supportive care dependent on the manifestation of symptoms. 33 Adults and adolescents may experience increased blood pressure and respiratory rates, red eyes, dry mouth, increased appetite, and slurred speech. 33
Negative health effects are also associated with marijuana and cannabinoid use. Frequent marijuana use has been associated with disorientation. In teens, it has been linked with depression, anxiety, and suicide. 5,32 However, this is not a proven causal relationship. Lung health can also be negatively impacted depending on the delivery mechanism. 34 Smoking marijuana can cause lung tissue scarring and damage blood vessels, further leading to an increased risk of bronchitis, cough, and phlegm production. 34 This generally decreases when users quit. 34
Secondhand smoke is a serious issue associated with marijuana use. However, there is limited evidence on how it impacts heart and lung health. 34 Detectable THC has been found in children who live in the home or have a caretaker who use marijuana, subjecting children to developmental risks of THC exposure. 35 Fetal, youth, and adolescent exposure to THC is associated with negative health effects, including impacting brain development. 34 There is inconsistent, insufficient evidence to determine the long-term effects of marijuana and cannabinoid use while breastfeeding. 36 However, THC has been detected in breast milk for up to six days post-cannabinoid use, and exposure to cannabinoids is known to impact development in children. 37 Evidence also suggests cannabis use during pregnancy may be linked with preterm birth. 38 Cardiovascular health may be impacted by smoked marijuana use. However, the negative health effects are associated with the harmful chemicals in smoke similar to tobacco smoke. 34
Approximately 9% of all individuals who use marijuana develop an addiction, which is variable by age of first use and frequency of use. 34 That number for addiction jumps to 17% for individuals who begin using marijuana as teenagers and 25-50% of those who smoke marijuana daily. 34 Marijuana use does not typically lead to harder drug use, like cocaine and heroin, in most individuals. 39 Further research is needed to evaluate any potential gateway effect. 39
Mental health outcomes associated with marijuana use include an increased risk of anxiety and depression. Marijuana has been linked to schizophrenia, psychoses, and advancing the trajectory of the disease, particularly in individuals with pre-existing genetic indicators. 5,34 Global research also suggests daily use of high-potency marijuana increases risk for psychotic episodes among individuals with no underlying mental health condition. 40 While it is widely accepted that marijuana acutely impairs cognitive function, studies suggest differential outcomes regarding short- versus long-term cognitive impairment. 34
Research Considerations
The regulatory environment surrounding cannabis, marijuana, and cannabinoid research creates barriers detrimental to facilitating meaningful medical, public health, policy, and public safety research. Approval for research expands beyond institutional review boards. Due to the Schedule I classification by the Drug Enforcement Agency (DEA), researchers seeking to investigate health effects associated with cannabis must follow a regimented application process. 41 Applicants must submit an Investigational New Drug (IND) application to the FDA, which will then be reviewed to determine scientific validity and research subjects’ rights and safety. 42 Researchers must also follow the NIDA regulatory procedures for obtaining cannabis for research purposes. 41 Researchers may only use cannabis supplied by the University of Mississippi, the single NIDA-approved source for cannabis research. 41 Requiring research to rely on one source of cannabis limits availability and the variety of products. While the University of Mississippi cultivates different strains of cannabis, it is unable to supply the vast array of strains of cannabis found in the evolving retail environment with varying levels of THC, CBD, and cannabinoid content. 5 Substantial funding and capacity is required for researchers to obtain all regulatory approval and remain in compliance while conducting cannabis-related research. The required processes and procedures present a serious burden, dissuading researchers from pursuing cannabis-related projects. This has led to a lack of empirical evidence regarding a myriad of health-related issues, including potential therapeutic benefits of cannabis, public health impact, health economics, and the short- and long-term health effects from cannabis use.
In order to address the research gaps associated with both beneficial and harmful effects of cannabinoids used in both medical and recreational capacities, the AAFP calls for a comprehensive review of processes and procedures required to obtain approval for cannabis research.
The AAFP encourages the appropriate regulatory bodies, such as the DEA, NIDA, FDA, Department of Health and Human Services (DHHS), National Institutes of Health (NIH), and the Centers for Disease Control and Prevention (CDC), to collaborate with non-governmental stakeholders to determine procedures to decrease the burden of cannabis-related research while maintaining appropriate regulatory safety guards. This should include a reclassification of marijuana from Schedule I to facilitate clinical research. The AAFP calls for increased funding from both public and private sectors to support rigorous scientific research to address gaps in evidence regarding cannabis to protect the health of the public and inform evidence-based practices. 3 Future research should address the impact of cannabis use on vulnerable and at-risk populations.
Regulatory Considerations
While cannabis was federally regulated in 1906 for consumer and safety standards and labeling requirements, the Marihuana Tax Act of 1937 was the first federal regulation to impose a fine or imprisonment for non-medical use and distribution of cannabis. 5 The tax act also regulated production, distribution, and use of cannabis, further requiring anyone dealing with cannabis to register with the federal government. 5 In 1970, the DEA classified marijuana as a Schedule I drug, which is defined as a drug with no current acceptable medical use and a high potential for abuse. 43 Other Schedule 1 drugs include heroin, lysergic acid diethylamide (LSD), 3,4-methylenedioxymethamphetamine (ecstasy), methaqualone, and peyote. 43 Since this class of substances is determined as having no medical usage, they cannot be legally prescribed and thus, there is no medical coverage for them.
Marijuana is illegal under federal law. Penalties cover possession, sale, cultivation, and paraphernalia. However, the Agriculture Improvement Act of 2018 included a U.S. Department of Agriculture (USDA) Hemp Production Program, removing hemp from the Controlled Substances Act. 10,44 As a result, CBD sourced from hemp plants containing no more than 0.3% THC is legal to produce. 10,44 The FDA has approved three medications containing cannabinoids: epidiolex (CBD), dronabinol, and nabilone (synthetic cannabinoids). 5 No other forms of cannabis are currently regulated by the FDA. The AAFP calls upon the FDA to take swift action to regulate CBD and cannabinoid products now legal in order to protect the health of the public.
States have separate marijuana, cannabinoid, and cannabis laws, some of which mirror federal laws, while others may be more harsh, or have decriminalized and even legalized marijuana and cannabis. 45 In 1996, California was the first state to legalize the medical use of marijuana. 46 States have subsequently decriminalized and/or legalized cannabinoids, medical marijuana, and recreational marijuana. 46 As of August 2019, 30 states, along with the District of Columbia, Guam, and Puerto Rico have legalized marijuana in varying forms. 46 Decriminalization laws may include reduction of fines for possession of small amounts of marijuana, reclassification of criminal to civil infractions, excluding the infraction from criminal records and expunging prior offenses and convictions related to marijuana. 47 Thirty-three states, along with the District of Columbia, Guam, Puerto Rico, and the U.S. Virgin Islands have a comprehensive, publicly-available medical marijuana/cannabis program, and 13 of these states have also removed jail time for possessing small amounts of non-medical marijuana. 47 Adult recreational marijuana use is legal in 13 states and the District of Columbia. 47 Vermont and the District of Columbia, however, do not allow the sale of marijuana for recreational purposes. This means it is not a crime to use and possess marijuana recreationally, but commercial sales are not allowed. 47 States have also authorized the sale of products that have low levels of THC, but high levels of CBD. These products are widely available in retail locations, but are highly unregulated. 47 The benefits of CBD touted by the public and retailers are largely anecdotal. The vast majority of these claims are not substantiated by valid research.
Decriminalizing and legalizing marijuana can decrease the number of individuals arrested and subsequently prosecuted for possession and/or use. 48 However, evidence suggests that these practices are not applied equitably. People of color are more likely to be arrested and prosecuted for marijuana possession despite overall decreased arrest rates. 48 Incarceration impacts health. People who are incarcerated have significantly higher rates of disease than those who are not, and are less likely to have access to adequate medical care. 49
The AAFP “opposes the recreational use of marijuana. However, the AAFP supports decriminalization of possession of marijuana for personal use. The AAFP recognizes the benefits of intervention and treatment for the recreational use of marijuana, in lieu of incarceration, for all individuals, including youth.” 4 The AAFP calls for family physicians to advocate to prevent unnecessary incarceration by diverting eligible people from the justice system to substance abuse and/or mental health treatment. 49
There are many public health considerations when regulating cannabis products. Serious public health concerns include impaired driving, youth exposure to advertisements, and accidental poisoning in children. Second to alcohol, marijuana is the most common illicit drug associated with impaired driving and accidents. 34 Marijuana slows reaction time and decision making, substantially increasing risk for traffic accidents. 50 Some states have a zero-tolerance policy, where there is no allowable detectable level of THC while driving, while other states have set five nanograms per milliliter or higher limits of THC, or minimally-detectable amounts of THC. 51
Evidence indicates adolescents who are exposed to medical marijuana advertising are more likely to have positive views of and subsequently use marijuana. 52 Those exposed to medical marijuana advertising were more likely to report past use and expectant future use. 52 These adolescents also reported agreeing with statements like, marijuana helps people relax and get away from their problems. 52 Adolescent exposure to medical marijuana advertising was also associated with self-reporting negative consequences associated with marijuana use, including missing school and concentration issues. 52 The AAFP calls for immediate regulation of advertising of all marijuana and cannabinoid products to decrease youth exposure to aid in preventing initiation and subsequent use of marijuana.
Children are most susceptible to severe effects associated with marijuana poisoning, including decreased coordination, lethargy, sedation, difficulty concentrating, and slurred speech. 53 Exposure may also include serious, potentially life-threatening symptoms like respiratory distress and coma. 33 Unintentional exposures to marijuana in children have increased each year since 2012, likely due to legalization policies across the U.S. and popularity of edibles. 53 Edibles often look exactly like their non-THC counterparts, and come in brightly colored packaging appealing to children, often mimicking candy products. 53 Effective legislation requiring childproof packaging for edible products can help mitigate and prevent unintentional exposure in children. 54 Family physicians should discuss safe storage of all cannabis products with their patients who live with children. 54 Under the Child Abuse Prevention and Treatment Act (CAPTA), physicians are mandated reporters of suspected child abuse and neglect. 55 The 2010 law requires states to enact laws for reporting substance use-exposed infants to child protective services. 55
Family physicians play a key role in addressing marijuana, cannabinoid, and cannabis product use; reducing barriers to research; and advocating for appropriate policy to protect the health of patients and the public.
Family physicians can address the inappropriate use of marijuana, cannabinoid, and cannabis products. Family physicians should discuss safe storage of all cannabis products with patients who live with or serve as primary caregivers for children to prevent unintended exposure. 56 It is important to discuss the developmental and negative impacts of marijuana and cannabis products with individuals who are or can become pregnant, children, and adolescents. Family physicians should also emphasize the serious consequences of impaired driving and marijuana intoxication.
It is essential to decrease barriers to research all forms of marijuana, cannabis, and cannabinoids, including a reclassification of cannabis as a Schedule I drug. High-quality research regarding the impact on patients, public health, society, and health policy are essential to providing patient-centered care and promoting evidence-based public health practices. Immediate regulations for marijuana and cannabinoid products, including CBD, like product safety and consistency safeguards, child-proof packaging, labeling, marketing claims and advertising, and impairment standards are vital for consumer safety and injury prevention. Regulatory measures focused on preventing youth initiation of marijuana and cannabinoid product use must be prioritized to prevent a public health epidemic.
The health benefits associated with intervention and treatment of recreational marijuana and cannabinoid use, in lieu of incarceration, is an important policy consideration.
Utilizing an interdisciplinary, evidence-based approach to addressing both medical and recreational marijuana and cannabis use is essential to promote public health, inform policy, and provide patient-centered care. Family physicians, in partnership with public health and policy professionals, can play an imperative role in addressing the changing landscape of marijuana and cannabis products.
- Bridgeman MB, Abazia DT. Medicinal cannabis: history, pharmacology, and implications for the acute care setting. P T . 2017;42(3):180-188. Accessed August 20, 2019.
- Abrams DI. The therapeutic effects of cannabis and cannabinoids: An update from the National Academies of Sciences, Engineering and Medicine report. Eur J Intern Med . 2018;49:7-11.
- American Academy of Family Physicians. Substance abuse and addiction . Accessed August 20, 2019.
- American Academy of Family Physicians. Marijuana possession for personal use . Accessed August 20, 2019.
- The National Academies of Science, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids . Washington, D.C.: National Academies Press; 2017.
- National Institute on Drug Abuse. DrugFacts: Monitoring the Future Survey: high school and youth trends. www.drugabuse.gov/publications/drugfacts/monitoring-future-survey-high-school-youth-trends. Accessed August 20, 2019.
- National Institute on Drug Abuse. National Survey of Drug Use and Health . Accessed August 20, 2019.
- Mackie K. Cannabinoid receptors: where they are and what they do. J Neuroendocrinol . 2008;20(s1):10-14.
- Hilderbrand RL. Hemp & cannabidiol: what is a medicine? Mo Med . 2018;115(4):306-309. Accessed August 20, 2019.
- U.S. Department of Agriculture. Hemp production program . Accessed August 20, 2019.
- Heidi H. Oregon State University launches largest, most comprehensive hemp research center in the nation. Oregon State University. www.today.oregonstate.edu/news/oregon-state-university-launches-largest-most-comprehensive-hemp-research-center-nation. Accessed August 20, 2019.
- Lee MJ. The legalization of hemp. Accessed August 20, 2019.
- Shipman M. Is hemp the same thing as marijuana? NC State University. Accessed August 20, 2019.
- National Institute on Drug Abuse. What is marijuana? Accessed August 20, 2019.
- Drug Policy Alliance. Marijuana concentrates. Accessed August 20, 2019.
- MacCoun RJ, Mello MM. Half-baked — the retail promotion of marijuana edibles. N Engl J Med . 2015;372(11):989-991.
- Peschel W, Peschel, Wieland. Quality control of traditional cannabis tinctures: pattern, markers, and stability. Sci Pharm . 2016;84(3):567-584.
- Rosenblatt S, Tucker J, DeAngelo S. Methods and compositions of cannabis extracts. Accessed August 20, 2019.
- MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med . 2018;49:12-19.
- U.S. Food and Drug Administration. FDA regulation of cannabis and cannabis-derived products: questions and answers . Accessed August 20, 2019.
- National Cancer Institute. NCI Drug Dictionary. Nabiximols. Accessed August 20, 2019.
- U.S. Food and Drug Administration. Syndros (dronabinol) oral solution . Accessed August 20, 2019.
- U.S. Food and Drug Administration. CESAMETTM (nabilone) capsules. Accessed August 20, 2019.
- Greenwich Biosciences. Epidiolex® (cannabidiol). www.epidiolex.com/. Accessed August 20, 2019.
- Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use. A systematic review and meta-analysis. JAMA . 2015;313(24):2456-2473.
- Abuhasira R, Shbiro L, Landschaft Y. Medical use of cannabis and cannabinoids containing products – Regulations in Europe and North America. Eur J Intern Med . 2018;49:2-6.
- Devinsky O, Cilio MR, Cross H, et al. Cannabidiol: pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia . 2014;55(6):791-802.
- U.S. Food and Drug Administration. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. Accessed August 20, 2019.
- Devinsky O, Patel AD, Cross JH, et al. Effect of cannabidiol on drop seizures in the Lennox–Gastaut syndrome. N Engl J Med . 2018;378(20):1888-1897.
- Devinsky O, Cross JH, Laux L, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med . 2017;376(21):2011-2020.
- Perucca E. Cannabinoids in the treatment of epilepsy: hard evidence at last? J Epilepsy Res . 2017;7(2):61-76.
- Volkow ND, Swanson JM, Evins AE, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry . 2016;73(3):292-297.
- Wang GS. Cannabis (marijuana): acute intoxication. UpToDate. Accessed August 20, 2019.
- Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse health effects of marijuana use. N Engl J Med . 2014;370(23):2219-2227.
- Wilson KM, Torok MR, Wei B, et al. Detecting biomarkers of secondhand marijuana smoke in young children. Pediatr Res . 2017;81(4):589-592.
- Reece-Stremtan S, Marinelli KA. ABM Clinical Protocol #21: Guidelines for Breastfeeding and Substance Use or Substance Use Disorder, Revised 2015. Breastfeed Med . 2015;10(3):135-141.
- Bertrand KA, Hanan NJ, Honerkamp-Smith G, Best BM, Chambers CD. Marijuana use by breastfeeding mothers and cannabinoid concentrations in breast milk. Pediatrics . 2018;142(3):e20181076.
- Corsi DJ, Walsh L, Weiss D, et al. Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA . 2019;322(2):145-152.
- Centers for Disease Control and Prevention. Does marijuana use lead to other drug use? Accessed August 20, 2019.
- Di Forti M, Quattrone D, Freeman TP, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. The Lancet Psychiatry . 2019;6(5):427-436.
- U.S. Food and Drug Administration. Marijuana research with human subjects . Accessed August 20, 2019.
- National Institute on Drug Abuse (NIDA). NIDA’s role in providing marijuana for research. www.drugabuse.gov/drugs-abuse/marijuana/nidas-role-in-providing-marijuana-research. Accessed August 20, 2019.
- U.S. Drug Enforcement Administration. Drug scheduling . Accessed August 20, 2019.
- U.S. Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, M.D., on signing of the Agriculture Improvement Act and the agency's regulation of products containing cannabis and cannabis-derived compounds. Accessed August 20, 2019.
- American Bar Assocation. Conflicting state and federal marijuana laws create ethical complications for lawyers. Accessed August 20, 2019.
- National Conference of State Legislatures. Marijuana laws. www.ncsl.org/bookstore/state-legislatures-magazine/marijuana-deep-dive.aspx. Accessed August 20, 2019.
- National Conference of State Legislatures. Marijuana laws. Accessed August 20, 2019.
- Drug Policy Alliance. From prohibition to progress: a status report on marijuana legalization. Accessed August 20, 2019.
- American Academy of Family Physicians. Incarceration and health: a family medicine perspective (position paper) . Accessed August 20, 2019.
- Centers for Disease Control and Prevention. What you need to know about marijuana use and driving . Accessed August 20, 2019.
- National Conference of State Legislatures. Drugged driving | Marijuana-impaired driving . Accessed August 20, 2019.
- RAND Corporation. Adolescents who view more medical marijuana advertising are more likely to use marijuana, have positive views about the drug . Accessed August 20, 2019.
- Center on Addiction. Childhood poisoning: safeguarding young children from addictive substances. Accessed August 20, 2019.
- Center on Addiction. Toddlers and THC: the number of young children exposed to marijuana is on the rise. Accessed August 20, 2019.
- Child Welfare Information Gateway. Mandatory reporters of child abuse and neglect. Accessed August 20, 2019.
- Children’s Hospital Colorado. Marijuana safety in the home . Accessed August 20, 2019.
(July 2019 BOD)
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Read our research on: Gun Policy | International Conflict | Election 2024
Regions & Countries
9 facts about americans and marijuana.

The use and possession of marijuana is illegal under U.S. federal law, but about three-quarters of states have legalized the drug for medical or recreational purposes. The changing legal landscape has coincided with a decades-long rise in public support for legalization, which a majority of Americans now favor.
Here are nine facts about Americans’ views of and experiences with marijuana, based on Pew Research Center surveys and other sources.
As more states legalize marijuana, Pew Research Center looked at Americans’ opinions on legalization and how these views have changed over time.
Data comes from surveys by the Center, Gallup , and the 2022 National Survey on Drug Use and Health from the U.S. Substance Abuse and Mental Health Services Administration. Information about the jurisdictions where marijuana is legal at the state level comes from the National Organization for the Reform of Marijuana Laws .
More information about the Center surveys cited in the analysis, including the questions asked and their methodologies, can be found at the links in the text.
Around nine-in-ten Americans say marijuana should be legal for medical or recreational use, according to a January 2024 Pew Research Center survey . An overwhelming majority of U.S. adults (88%) say either that marijuana should be legal for medical use only (32%) or that it should be legal for medical and recreational use (57%). Just 11% say the drug should not be legal in any form. These views have held relatively steady over the past five years.
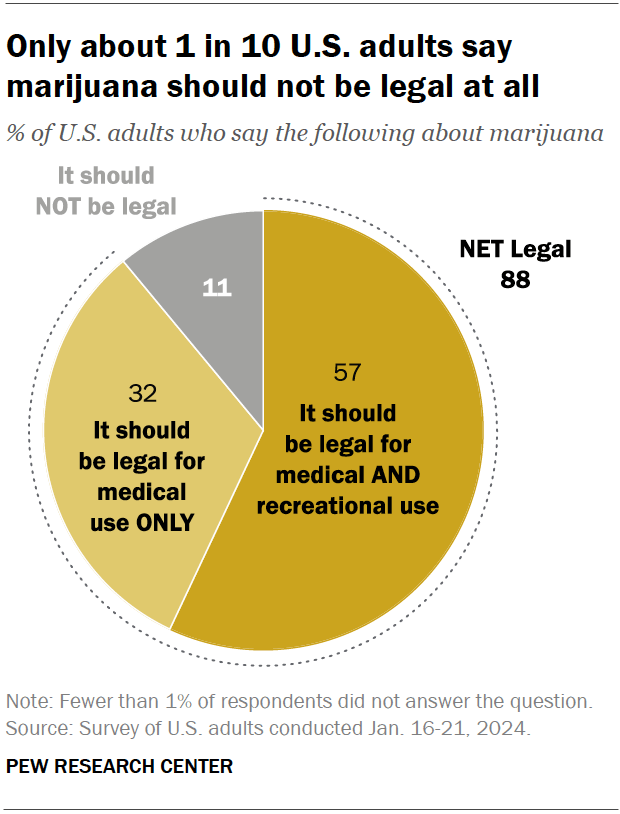
Views on marijuana legalization differ widely by age, political party, and race and ethnicity, the January survey shows.

While small shares across demographic groups say marijuana should not be legal at all, those least likely to favor it for both medical and recreational use include:
- Older adults: 31% of adults ages 75 and older support marijuana legalization for medical and recreational purposes, compared with half of those ages 65 to 74, the next youngest age category. By contrast, 71% of adults under 30 support legalization for both uses.
- Republicans and GOP-leaning independents: 42% of Republicans favor legalizing marijuana for both uses, compared with 72% of Democrats and Democratic leaners. Ideological differences exist as well: Within both parties, those who are more conservative are less likely to support legalization.
- Hispanic and Asian Americans: 45% in each group support legalizing the drug for medical and recreational use. Larger shares of Black (65%) and White (59%) adults hold this view.
Support for marijuana legalization has increased dramatically over the last two decades. In addition to asking specifically about medical and recreational use of the drug, both the Center and Gallup have asked Americans about legalizing marijuana use in a general way. Gallup asked this question most recently, in 2023. That year, 70% of adults expressed support for legalization, more than double the share who said they favored it in 2000.
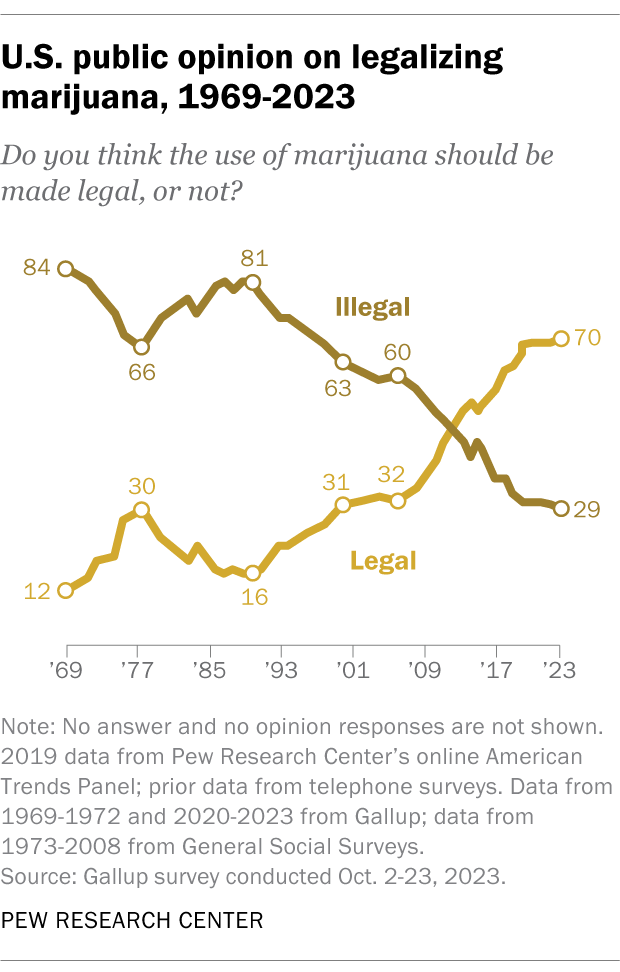
Half of U.S. adults (50.3%) say they have ever used marijuana, according to the 2022 National Survey on Drug Use and Health . That is a smaller share than the 84.1% who say they have ever consumed alcohol and the 64.8% who have ever used tobacco products or vaped nicotine.
While many Americans say they have used marijuana in their lifetime, far fewer are current users, according to the same survey. In 2022, 23.0% of adults said they had used the drug in the past year, while 15.9% said they had used it in the past month.
While many Americans say legalizing recreational marijuana has economic and criminal justice benefits, views on these and other impacts vary, the Center’s January survey shows.
- Economic benefits: About half of adults (52%) say that legalizing recreational marijuana is good for local economies, while 17% say it is bad. Another 29% say it has no impact.
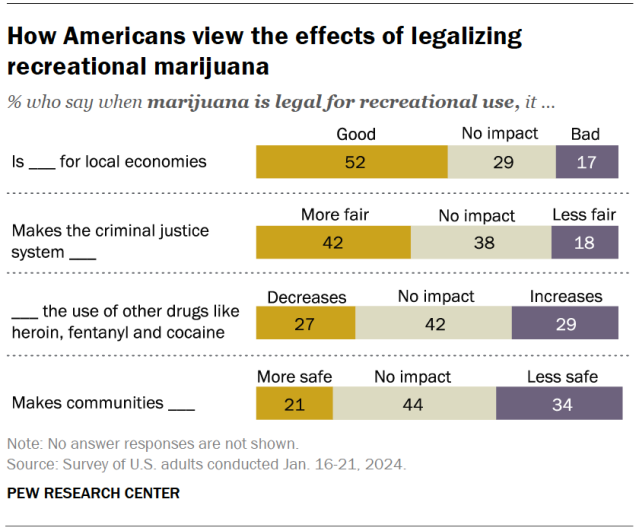
- Criminal justice system fairness: 42% of Americans say legalizing marijuana for recreational use makes the criminal justice system fairer, compared with 18% who say it makes the system less fair. About four-in-ten (38%) say it has no impact.
- Use of other drugs: 27% say this policy decreases the use of other drugs like heroin, fentanyl and cocaine, and 29% say it increases it. But the largest share (42%) say it has no effect on other drug use.
- Community safety: 21% say recreational legalization makes communities safer and 34% say it makes them less safe. Another 44% say it doesn’t impact safety.
Democrats and adults under 50 are more likely than Republicans and those in older age groups to say legalizing marijuana has positive impacts in each of these areas.
Most Americans support easing penalties for people with marijuana convictions, an October 2021 Center survey found . Two-thirds of adults say they favor releasing people from prison who are being held for marijuana-related offenses only, including 41% who strongly favor this. And 61% support removing or expunging marijuana-related offenses from people’s criminal records.
Younger adults, Democrats and Black Americans are especially likely to support these changes. For instance, 74% of Black adults favor releasing people from prison who are being held only for marijuana-related offenses, and just as many favor removing or expunging marijuana-related offenses from criminal records.
Twenty-four states and the District of Columbia have legalized small amounts of marijuana for both medical and recreational use as of March 2024, according to the National Organization for the Reform of Marijuana Laws (NORML), an advocacy group that tracks state-level legislation on the issue. Another 14 states have legalized the drug for medical use only.
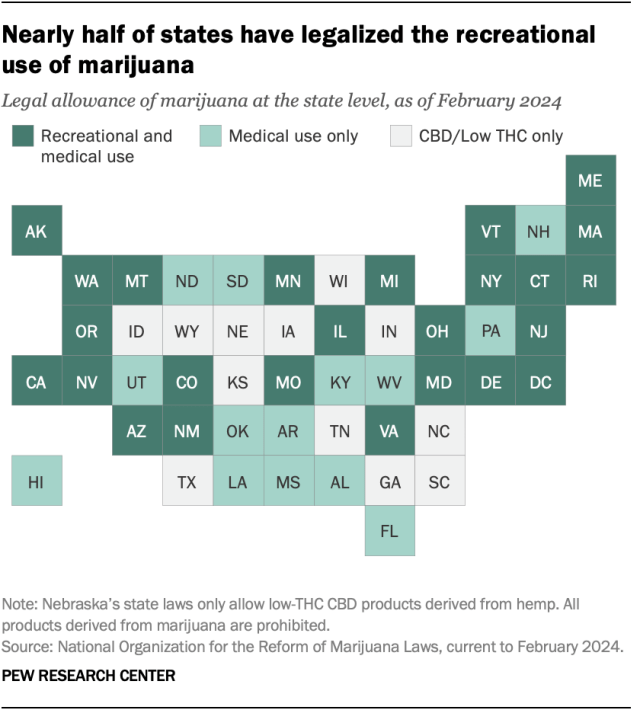
Of the remaining 12 states, all allow limited access to products such as CBD oil that contain little to no THC – the main psychoactive substance in cannabis. And 26 states overall have at least partially decriminalized recreational marijuana use , as has the District of Columbia.
In addition to 24 states and D.C., the U.S. Virgin Islands , Guam and the Northern Mariana Islands have legalized marijuana for medical and recreational use.
More than half of Americans (54%) live in a state where both recreational and medical marijuana are legal, and 74% live in a state where it’s legal either for both purposes or medical use only, according to a February Center analysis of data from the Census Bureau and other outside sources. This analysis looked at state-level legislation in all 50 states and the District of Columbia.
In 2012, Colorado and Washington became the first states to pass legislation legalizing recreational marijuana.
About eight-in-ten Americans (79%) live in a county with at least one cannabis dispensary, according to the February analysis. There are nearly 15,000 marijuana dispensaries nationwide, and 76% are in states (including D.C.) where recreational use is legal. Another 23% are in medical marijuana-only states, and 1% are in states that have made legal allowances for low-percentage THC or CBD-only products.
The states with the largest number of dispensaries include California, Oklahoma, Florida, Colorado and Michigan.
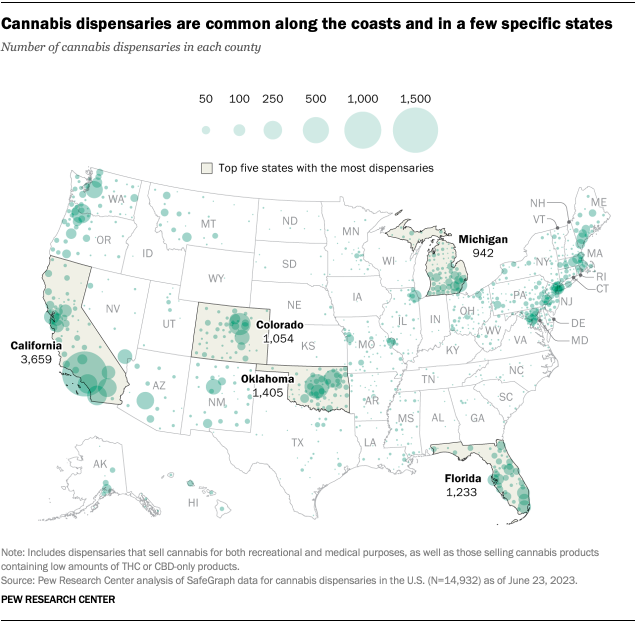
Note: This is an update of a post originally published April 26, 2021, and updated April 13, 2023.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Americans overwhelmingly say marijuana should be legal for medical or recreational use
Religious americans are less likely to endorse legal marijuana for recreational use, four-in-ten u.s. drug arrests in 2018 were for marijuana offenses – mostly possession, two-thirds of americans support marijuana legalization, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .

How Marijuana Legalization Changed Use in States
How has marijuana legalization changed the way Americans use it, and what does this mean for public health?
As of 2024, marijuana has become legalized for recreational use in 24 states, with 38 states permitting its use in medical contexts. However, as per the Drug Enforcement Administration, marijuana remains a Schedule I substance, in the same class as other drugs such as heroin, ecstasy and LSD.
This puts marijuana in a weird legal limbo: while it is available to buy and use in numerous states across America, its Schedule I classification has significantly impeded scientific research into its health effects and medical uses.
Between 2016 and 2022, the number of people enrolled in medical cannabis programs increased by more than 600 percent. However, these rises are not uniform across the country.
In a new study, published in the Annals of Internal Medicine , researchers from the University of Michigan Medical School and the Centers for Disease Control and Prevention found that although the overall number of medical marijuana users had risen, those living in states where marijuana is legal were much less likely to be enrolled in the programs.
"We had previously seen decreases in patient enrollment after non-medical adult use laws passed, but we were surprised at how dramatic some of the decreases were, especially in states like Arizona where the patient population dropped by over 50 percent from 2021 to 2022," Kevin Boehnke, an assistant professor of anesthesiology at the University of Michigan, told Newsweek .
"Practically, we see that enrolment in medical cannabis programs generally decreases after the passage of adult use cannabis laws. This warrants further study, but may be due to several factors, including licensing fees for medical use, inconvenience of appointments, and the ability to use nonmedical cannabis medically."
In other words, due to the restrictions and red tape you need to go through to acquire marijuana in a clinical context, many of those who seek to use marijuana for medical conditions choose to self-medicate because it is easier.
"Thus, much of the use and advice around medical cannabis occurs outside of the doctor's office, and may come from other sources like retailers," Boehnke said.
Boehnke added that the dramatic growth in medical cannabis licenses since 2016 shows the widespread demand for medical marijuana and highlights the need for policymakers to consider how best to regulate it to prioritize patient safety and public health.
"Medical cannabis isn't going anywhere, and it is important to figure out how best to effectively integrate cannabis into medical treatment given the widespread use," he said. "The remarkable growth in the number of people with medical cannabis licenses demonstrates the importance of conducting more and better research on the potential benefits and harms of cannabis for medical purposes."
"The continued criminalization of cannabis at the federal level through 'War on Drugs' policies is harmful and needs to change. These policies are a substantial barrier to effective research into the potential benefits and risks of cannabis."
Related Articles
- Now Is Congress' Chance To Close Its Hemp Loophole—And Save Lives | Opinion
- Psychoactive Drug Study Shows 'Concerning' Use by US 12th Graders
- Global Cannabis Outlook: Worldwide Developments in 2024
Start your unlimited Newsweek trial

- Share full article
Advertisement
Supported by
Oregon Is Recriminalizing Drugs. Here’s What Portland Learned.
Oregon’s governor has signed a measure to reimpose criminal penalties for hard drugs. Mayor Ted Wheeler of Portland talks about why the experiment “failed.”

By Mike Baker
Reporting from Portland, Ore.
When Oregon embarked on a landmark plan three years ago to decriminalize hard drugs , it wagered that a focus on treatment over punishment would create a new model for drug policy around the country.
But after a deluge of overdose deaths and frequent chaos in the streets of Portland, Gov. Tina Kotek signed into law on Monday a measure to restore criminal penalties for drug possession . It brought to an end a key portion of one of the nation’s most ambitious attempts to find alternatives other than jail for drug users, embodied in a 2020 voter initiative known as Measure 110 .
The rollback has supporters among a wide range of public officials, including Mayor Ted Wheeler of Portland, who found himself presiding over a series of crises since taking office in 2016. They included surging unsheltered homelessness, turbulent street protests, an exodus of downtown businesses, record numbers of homicides , the rapid spread of fentanyl and soaring overdose deaths .
Over the past year, Mr. Wheeler has set out to restore order. He has battled in court to ban daytime camping and tried to establish mass shelter locations (known in Portland as TASS sites) for those without housing. After initially supporting budget cuts to the police department , he has pushed to increase the law enforcement presence in the city and to crack down on crime.
And he concluded that it was time to restore criminal penalties for hard drug possession. Under the new law, people caught with small amounts of drugs like fentanyl and methamphetamine could face up to 180 days in jail, although lawmakers also built in a series of offramps that allow people in many cases to get treatment instead of confinement.
Mr. Wheeler sat down with The New York Times recently to discuss the shift on drug policy and his city’s future. Here are excerpts from the interview, edited and condensed for length and clarity.
There’s concern that bringing back criminal penalties is going back to the war on drugs. Is that what’s happening?
The war on drugs didn’t work. And so I hope the answer to that question is ‘no.’ And I hope this isn’t an excuse for people to turn their backs on the hard work of building a mental health system. We’re doing that, and we’re doing it at the very local level. At our TASS sites, we actually went out and we contracted at the municipal level with service providers who can provide basic behavioral health, substance-use disorder, domestic-violence treatment, job training. We’re creating those pathways.
So we appreciate that the legislature took the steps to return law enforcement and public safety tools to our first responders. I think that was necessary. But it’s also necessary to do the hard work to build the behavioral health infrastructure that was lacking.
When you look back to 2020, when Measure 110 passed, you have pretty wide support in Oregon. In Portland, three-quarters of voters in this area approved it. I’m curious how excited you were at the time about this new path that was emerging.
I was cautiously optimistic. I’ve been around enough to know that it’s always in the implementation.
Where do you think things most went wrong with the measure?
There’s no question that the state botched the implementation. And as I say, the timing couldn’t have been worse. In terms of the botched implementation: To decriminalize the use of drugs before you actually had the treatment services in place was obviously a huge mistake.
With the benefit of hindsight, the way that should have been structured is that it would create the mechanism for funding. The state would build up its behavioral health services, and when it reached a certain threshold, then they would decriminalize. It shouldn’t have gone the other way around.
The truth is that addiction rates and overdose rates skyrocketed. I personally do not attribute all of that to the passage of Measure 110. I think you can see national trends that would suggest that it wasn’t all ballot Measure 110, but it was very easy for the public to draw a line between the passage of Measure 110, the decriminalization of hard drugs, the increase in addiction and the increase in overdoses — and criminal activity associated with drugs.

Jordan Gale for The New York Times
You’ve said that you’ve been concerned about the future viability of this city . What does a worst-case scenario look like to you?
A worst-case scenario is a city where you don’t have laws that can be enforced. You don’t have alternative treatment for those who are ready to be treated. And you lose the public’s trust in your local institutions of democracy. That’s when things start to unwind. We’re not there. And I will tell you, from where I was sitting four years ago today, night and day difference. I’m very optimistic about the future of this city.
I hear your optimism.
I can see it. I mean, the city looks much better. Foot traffic is way up. Criminal activity is way down. With the opening of our TASS sites, with the expansion of our services at our safe-rest villages, we have a thousand new shelter beds we didn’t have even a year ago. Things have improved.
At the same time, in relatively recent polling, I think 81 percent said they feel unsafe going downtown in Portland at night . Are they wrong to feel that way?
I would never tell anybody they’re wrong to feel unsafe. If you feel unsafe, you feel unsafe. And that is your prerogative. What I would say is, objectively, crime rates are way down .
I was looking back when you first ran for office in 2015. One of your big messages was trying to deal with this nexus of homelessness and mental health issues and addiction. You had vowed at the time to eliminate unsheltered homelessness by 2018 . What went wrong?
Well, first of all, I’m not a great predictor of the future, it turns out. I don’t think anybody in 2015 could have possibly imagined where we would be today, as a city, as a state, as a nation. In 2015, P2P meth didn’t exist. Fentanyl didn’t exist. We hadn’t seen the explosion in the homeless population that we saw, particularly during the pandemic, but also leading up to the pandemic. What happened there, I think, honestly, is the long-term decisions we had made as a state to not invest in behavioral health, to not invest in treatment services, came home to roost as all of these crises hit simultaneously during Covid.
Do you look at yourself and say, “I have blame in this?”
I think we all have blame in this. Of course. We have somewhat reaped what we have sown. And I don’t just mean here in Portland, Oregon. I mean as a nation. Our nation has been very slow to accept behavioral health as an important issue. It’s starting to happen. It’s happening with particularly a younger generation being more willing to talk about it openly.
Along with this rollback of Measure 110, across the country there’s been a shift toward more conservative policies on policing and crime and drug policy. What do you think is motivating that shift?
People are exhausted from feeling like they’re under siege. They want order restored to their environment. And that makes perfect sense to me. These are very dislocating times. These are uncertain times for people economically, socially, in terms of the environment. There are so many existential threats. I mean, even despotism is seeming to grow worldwide. These are very uncertain times.
And you see it particularly amongst young people. I feel it. I think other people feel it, too. And so they have a minimum expectation that where they live is an orderly, safe, secure, prosperous place to be. And if they don’t see it, that is unsettling. They need to have that.
For other states or cities that are thinking about drug decriminalization — it might not be this year, maybe it’s down the line — what would be your guidance?
The treatment infrastructure has to be in place first.
Do you think there is a future where decriminalization could happen again? Or have we learned some other lesson about hard drugs in society?
I do believe there is a future where decriminalization in favor of treatment could happen, but it can’t happen if you don’t have the treatment, and that seems self-evident. There’s no question that what Oregon did was a bold experiment, and it failed. Let’s just be honest about that. It was botched in terms of the implementation. The timing was wrong, and frankly, the politics were wrong.
Going forward, could this experiment happen again? I don’t think anybody will completely decriminalize the use of drugs. I wouldn’t support it, personally, but the piece about providing enough behavioral health services is critically important. And again, in this country, we haven’t done that.
Mike Baker is a national reporter for The Times, based in Seattle. More about Mike Baker

IMAGES
VIDEO
COMMENTS
Introduction. Cannabis is one of the most widely used substances globally, with nearly 2.5% of the world population reporting past year cannabis use. 1 Cannabis use rates are particularly high in North America. In the U.S., 45% of individuals reported ever using cannabis and 18% reported using at least once annually in 2019. 2,3 In Canada, approximately 21% of people reported cannabis use in ...
Background Marijuana is the most commonly used illicit drug in the United States. More and more states legalized medical and recreational marijuana use. Adolescents and emerging adults are at high risk for marijuana use. This ecological study aims to examine historical trends in marijuana use among youth along with marijuana legalization. Method Data (n = 749,152) were from the 31-wave ...
effect and 12 state recreational marijuana laws (RMLs) went into effect . According to recent public-opinion polls, two out of three Americans favor the legalization of marijuana (Gurley 2019; Lopez 2019). 2 Given this level of support, it seems likely that more states will legalize marijuana in upcoming years.
It may be that marijuana legalization and other secular trends have perturbed normative adult reductions in marijuana use. Additionally, we found differences in the sources of variation underlying cannabis use over time using a gene-environment interaction model. The larger environmental variation prior to legalization in states that would go ...
ments such as the possibility of legalization leading to increased use among youth and increased cannabis-impaired driving. 16 A nationally representative survey in the U.S. found that pro-legalization arguments were perceived to be more persuasive than public health anti-legalization arguments in a U.S. nation-
Cannabis legalization has benefits, such as removing the product from the illegal market so it can be taxed and regulated, but science is still trying to catch up as social norms evolve and different products become available. In this Q&A, adapted from the August 25 episode of Public Health On Call, Lindsay Smith Rogers talks with Johannes ...
Rebecca L. Haffajee. Amanda Mauri. Evidence regarding the effects of recreational cannabis legalization on public health is inconsistent. Future research should assess heterogeneous policy design ...
Purpose of review: As more jurisdictions legalize cannabis for non-medical use, the evidence on how legalization policies affect cannabis use and the use of other substances remains inconclusive and contradictory. This review aims to summarize recent research findings on the impact of recreational cannabis legalization (RCL) on cannabis and other substance use among different population groups ...
Overall, rates of cannabis use have shown long-term increasing trends among several age groups in North America. 7-9 Moreover, research has revealed recent cannabis use increases in at risk populations, such as individuals with depression and pregnant women. 10,11 Parallel to increased cannabis use over time, rates of cannabis-related consequences have also increased across Canada and the U.S ...
15-19, 20-24, and 25 years and older indicate past year use of 21 %, 30 %, and 10%, respectively. (Statistics Canada, 2017). Among youth, nonmedical cannabis use in Canada has a rate 2.5. times ...
Thirty-six states have legalized medical marijuana and 18 states have legalized the use of marijuana for recreational purposes. In this paper, we review the literature on the public health consequences of legalizing marijuana, focusing on studies that have appeared in economics journals as well as leading public policy, public health, and ...
DOI 10.3386/w30813. Issue Date December 2022. Despite nearly 70 percent of the American public supporting legalization of recreational marijuana, opponents argue that increased marijuana use may diminish motivation, impede cognitive function, and harm health, each of which could adversely affect adults' economic wellbeing.
A 57% majority of Republicans ages 18 to 29 favor making marijuana legal for medical and recreational use, compared with 52% among those ages 30 to 49 and much smaller shares of older Republicans. Still, wide majorities of Republicans in all age groups favor legalizing marijuana at least for medical use. Among those ages 65 and older, just 20% ...
Nearly two-thirds of conservative and moderate Democrats (63%) say marijuana should be legal for medical and recreational use. An overwhelming majority of liberal Democrats (84%) say the same. There also are racial and ethnic differences in views of legalizing marijuana. Roughly two-thirds of Black adults (68%) and six-in-ten White adults say ...
As of 2018 there have been eight states in the United States legalize the recreational use. of Marijuana: Colorado, Washington, Nevada, California, Oregon, Alaska, Maine and. Massachusetts. This research paper is going to discuss the history of marijuana and why it was. originally made illegal throughout the United States.
The AAFP recognizes the need for substantial clinical, public health, and policy evidence and research regarding cannabis, marijuana, cannabinoids, and CBD to inform evidence-based practice and ...
Around nine-in-ten Americans say marijuana should be legal for medical or recreational use, according to a January 2024 Pew Research Center survey.An overwhelming majority of U.S. adults (88%) say either that marijuana should be legal for medical use only (32%) or that it should be legal for medical and recreational use (57%).Just 11% say the drug should not be legal in any form.
As of 2024, marijuana has become legalized for recreational use in 24 states, with 38 states permitting its use in medical contexts. However, as per the Drug Enforcement Administration, marijuana ...
April 1, 2024. When Oregon embarked on a landmark plan three years ago to decriminalize hard drugs, it wagered that a focus on treatment over punishment would create a new model for drug policy ...