Enter search terms to find related medical topics, multimedia and more.

Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Fetal Presentation, Position, and Lie (Including Breech Presentation)
, MD, Children's Hospital of Philadelphia
- 3D Models (0)
- Calculators (0)

Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery Operative Vaginal Delivery Operative vaginal delivery involves application of forceps or a vacuum extractor to the fetal head to assist during the second stage of labor and facilitate delivery. Indications for forceps... read more , or cesarean delivery Cesarean Delivery Cesarean delivery is surgical delivery by incision into the uterus. The rate of cesarean delivery was 32% in the United States in 2021 (see March of Dimes: Delivery Method). The rate has fluctuated... read more .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
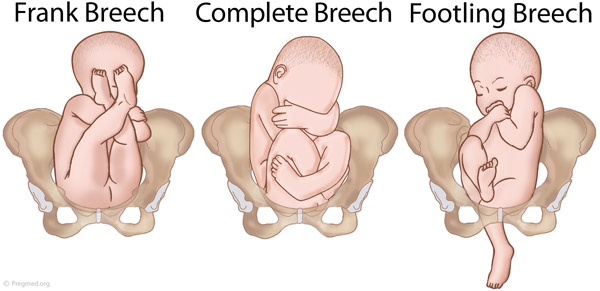
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor Preterm Labor Labor (regular uterine contractions resulting in cervical change) that begins before 37 weeks gestation is considered preterm. Risk factors include prelabor rupture of membranes, uterine abnormalities... read more
Multiple gestation Multifetal Pregnancy Multifetal pregnancy is presence of > 1 fetus in the uterus. Multifetal (multiple) pregnancy occurs in up to 1 of 30 deliveries. Risk factors for multiple pregnancy include Ovarian stimulation... read more
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse

Perinatal death
It is best to detect abnormal fetal lie or presentation before delivery. During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks. This technique involves gently pressing on the maternal abdomen to reposition the fetus. A dose of a short-acting tocolytic ( terbutaline 0.25 mg subcutaneously) may help. The success rate is about 50 to 75%. For persistent abnormal lie or presentation, cesarean delivery is usually done at 39 weeks or when the woman presents in labor.

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery Operative Vaginal Delivery Operative vaginal delivery involves application of forceps or a vacuum extractor to the fetal head to assist during the second stage of labor and facilitate delivery. Indications for forceps... read more or cesarean delivery Cesarean Delivery Cesarean delivery is surgical delivery by incision into the uterus. The rate of cesarean delivery was 32% in the United States in 2021 (see March of Dimes: Delivery Method). The rate has fluctuated... read more is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.
Drugs Mentioned In This Article

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada) — dedicated to using leading-edge science to save and improve lives around the world. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge.
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Manual

- IN THIS TOPIC
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Christine Zink, MD, is a board-certified emergency medicine with expertise in the wilderness and global medicine. She completed her medical training at Weill Cornell Medical College and residency in emergency medicine at New York-Presbyterian Hospital. She utilizes 15-years of clinical experience in her medical writing.
Breech presentation: diagnosis and management
Key messages.
- All women with a breech presentation should be offered an external cephalic version (ECV) from 37 weeks, if there are no contraindications.
- Elective caesarean section (ELCS) for a singleton breech at term has been shown to reduce perinatal and neonatal mortality rates.
- Planning for vaginal breech birth requires careful assessment of suitability criteria, contraindications and the ability of the service to provide experienced personnel.
In June 2023, we commenced a project to review and update the Maternity and Neonatal eHandbook guidelines, with a view to targeting completion in 2024. Please be aware that pending this review, some of the current guidelines may be out of date. In the meantime, we recommend that you also refer to more contemporaneous evidence.
Breech and external cephalic version
Breech presentation is when the fetus is lying longitudinally and its buttocks, foot or feet are presenting instead of its head.
Figure 1. Breech presentations
- Breech presentation occurs in three to four per cent of term deliveries and is more common in nulliparous women.
- External cephalic version (ECV) from 37 weeks has been shown to decrease the incidence of breech presentation at term and the subsequent elective caesarean section (ELCS) rate.
- Vaginal breech birth increases the risk of low Apgar scores and more serious short-term complications, but evidence has not shown an increase in long-term morbidity.
- Emergency caesarean section (EMCS) is needed in approximately 40 per cent of women planning a vaginal breech birth.
- 0.5/1000 with ELCS for breech >39 weeks gestation
- 2.0/1000 planned vaginal breech birth >39/40
- 1.0/1000 with planned cephalic birth.
- A reduction in planned vaginal breech birth followed publication of the Term Breech Trial (TBT) in 2001.
- Acquisition of skills necessary to manage breech presentation (for example, ECV) is important to optimise outcomes.
Clinical suspicion of breech presentation
- Abdominal palpation: if the presenting part is irregular and not ballotable or if the fetal head is ballotable at the fundus
- Pelvic examination: head not felt in the pelvis
- Cord prolapse
- Very thick meconium after rupture of membranes
- Fetal heart heard higher in the abdomen
In cases of extended breech, the breech may not be ballotable and the fetal heart may be heard in the same location as expected for a cephalic presentation.
If breech presentation is suspected, an ultrasound examination will confirm diagnosis.
Cord prolapse is an obstetric emergency. Urgent delivery is indicated after confirming gestation and fetal viability.
Diagnosis: preterm ≤36+6 weeks
- Breech presentation is a normal finding in preterm pregnancy.
- If diagnosed at the 35-36 week antenatal visit, refer the woman for ultrasound scan to enable assessment prior to ECV.
- Mode of birth in a breech preterm delivery depends on the clinical circumstances.
Diagnosis: ≥37+0 weeks
- determine type of breech presentation
- determine extension/flexion of fetal head
- locate position of placenta and exclude placenta praevia
- exclude fetal congenital abnormality
- calculate amniotic fluid index
- estimate fetal weight.
Practice points
- Offer ECV if there are no contraindications.
- If ECV is declined or unsuccessful, provide counselling on risks and benefits of a planned vaginal birth versus an ELCS.
- Inform the woman that there are fewer maternal complications with a successful vaginal birth, however the risk to the woman increases significantly if there is a need for an EMCS.
- Inform the woman that caesarean section increases the risk of complication in future pregnancies, including the risk of a repeat caesarean section and the risk of invasive placentation.
- If the woman chooses an ELCS, document consent and organise booking for 39 weeks gestation.
Information and decision making
Women with a breech presentation should have the opportunity to make informed decisions about their care and treatment, in partnership with the clinicians providing care.
Planning for birth requires careful assessment for risk of poor outcomes relating to planned vaginal breech birth. If any risk factors are identified, inform the woman that an ELCS is recommended due to increased perinatal risk.
Good communication between clinicians and women is essential. Treatment, care and information provided should:
- take into account women's individual needs and preferences
- be supported by evidence-based, written information tailored to the needs of the individual woman
- be culturally appropriate
- be accessible to women, their partners, support people and families
- take into account any specific needs, such as physical or cognitive disabilities or limitations to their ability to understand spoken or written English.
Documentation
The following should be documented in the woman's hospital medical record and (where applicable) in her hand-held medical record:
- discussion of risks and benefits of vaginal breech birth and ELCS
- discussion of the woman's questions about planned vaginal breech birth and ELCS
- discussion of ECV, if applicable
- consultation, referral and escalation
External cephalic version (ECV)
- ECV can be offered from 37 weeks gestation
- The woman must provide written consent prior to the procedure
- The success rate of ECV is 40-60 per cent
- Approximately one in 200 ECV attempts will lead to EMCS
- ECV should only be performed by a suitably trained, experienced clinician
- continuous electronic fetal monitoring (EFM)
- capability to perform an EMCS.
Contraindications
Table 1. Contraindications to ECV
Precautions
- Hypertension
- Oligohydramnios
- Nuchal cord
Escalate care to a consultant obstetrician if considering ECV in these circumstances.
- Perform a CTG prior to the procedure - continue until RANZCOG criteria for a normal antenatal CTG are met.
- 250 microg s/c, 30 minutes prior to the procedure.
- Administer Anti-D immunoglobulin if the woman is rhesus negative.
- Do not make more than four attempts at ECV, for a suggested maximum time of ten minutes in total.
- Undertake CTG monitoring post-procedure until RANZCOG criteria for a normal antenatal CTG are met.
Emergency management
Urgent delivery is indicated in the event of the following complications:
- abnormal CTG
- vaginal bleeding
- unexplained pain.
Initiate emergency response as per local guidelines.
Alternatives to ECV
There is a lack of evidence to support the use of moxibustion, acupuncture or postural techniques to achieve a vertex presentation after 35 weeks gestation.
Criteria for a planned vaginal breech birth
- Documented evidence of counselling regarding mode of birth
- Documentation of informed consent, including written consent from the woman
- Estimated fetal weight of 2500-4000g
- Flexed fetal head
- Emergency theatre facilities available on site
- Availability of suitably skilled healthcare professional
- Frank or complete breech presentation
- No previous caesarean section.
- Cord presentation
- Fetal growth restriction or macrosomia
- Any presentation other than a frank or complete breech
- Extension of the fetal head
- Fetal anomaly incompatible with vaginal delivery
- Clinically inadequate maternal pelvis
- Previous caesarean section
- Inability of the service to provide experienced personnel.
If an ELCS is booked
- Confirm presentation by ultrasound scan when a woman presents for ELCS.
- If fetal presentation is cephalic on admission for ELCS, plan ongoing management with the woman.
Intrapartum management
Fetal monitoring.
- Advise the woman that continuous EFM may lead to improved neonatal outcomes.
- Where continuous EFM is declined, perform intermittent EFM or intermittent auscultation, with conversion to EFM if an abnormality is detected.
- A fetal scalp electrode can be applied to the breech.
Position of the woman
- The optimal maternal position for birth is upright.
- Lithotomy may be appropriate, depending on the accoucheur's training and experience.
Pain relief
- Epidural analgesia may increase the risk of intervention with a vaginal breech birth.
- Epidural analgesia may impact on the woman's ability to push spontaneously in the second stage of labour.
Induction of labour (IOL)
See the IOL eHandbook page for more detail.
- IOL may be offered if clinical circumstances are favourable and the woman wishes to have a vaginal birth.
- Augmentation (in the absence of an epidural) should be avoided as adequate progress in the absence of augmentation may be the best indicator of feto-pelvic proportions.
The capacity to offer IOL will depend on clinician experience and availability and service capability.
First stage
- Manage with the same principles as a cephalic presentation.
- Labour should be expected to progress as for a cephalic presentation.
- If progress in the first stage is slow, consider a caesarean section.
- If an epidural is in situ and contractions are less than 4:10, consult with a senior obstetrician.
- Avoid routine amniotomy to avoid the risk of cord prolapse or cord compression.
Second stage
- Allow passive descent of the breech to the perineum prior to active pushing.
- If breech is not visible within one hour of passive descent, a caesarean section is normally recommended.
- Active second stage should be ½ hour for a multigravida and one hour for a primipara.
- All midwives and obstetricians should be familiar with the techniques and manoeuvres required to assist a vaginal breech birth.
- Ensure a consultant obstetrician is present for birth.
- Ensure a senior paediatric clinician is present for birth.
VIDEO: Maternity Training International - Vaginal Breech Birth
- Encouragement of maternal pushing (if at all) should not begin until the presenting part is visible.
- A hands-off approach is recommended.
- Significant cord compression is common once buttocks have passed the perineum.
- Timely intervention is recommended if there is slow progress once the umbilicus has delivered.
- Allow spontaneous birth of the trunk and limbs by maternal effort as breech extraction can cause extension of the arms and head.
- Grasp the fetus around the bony pelvic girdle, not soft tissue, to avoid trauma.
- Assist birth if there is a delay of more than five minutes from delivery of the buttocks to the head, or of more than three minutes from the umbilicus to the head.
- Signs that delivery should be expedited also include lack of tone or colour or sign of poor fetal condition.
- Ensure fetal back remains in the anterior position.
- Routine episiotomy not recommended.
- Lovset's manoeuvre for extended arms.
- Reverse Lovset's manoeuvre may be used to reduce nuchal arms.
- Supra-pubic pressure may aide flexion of the fetal head.
- Maricueau-Smellie-Veit manoeuvre or forceps may be used to deliver the after coming head.
Undiagnosed breech in labour
- This occurs in approximately 25 per cent of breech presentations.
- Management depends on the stage of labour when presenting.
- Assessment is required around increased complications, informed consent and suitability of skilled expertise.
- Do not routinely offer caesarean section to women in active second stage.
- If there is no senior obstetrician skilled in breech delivery, an EMCS is the preferred option.
- If time permits, a detailed ultrasound scan to estimate position of fetal neck and legs and estimated fetal weight should be made and the woman counselled.
Entrapment of the fetal head
This is an extreme emergency
This complication is often due to poor selection for vaginal breech birth.
- A vaginal examination (VE) should be performed to ensure that the cervix is fully dilated.
- If a lip of cervix is still evident try to push the cervix over the fetal head.
- If the fetal head has entered the pelvis, perform the Mauriceau-Smellie-Veit manoeuvre combined with suprapubic pressure from a second attendant in a direction that maintains flexion and descent of the fetal head.
- Rotate fetal body to a lateral position and apply suprapubic pressure to flex the fetal head; if unsuccessful consider alternative manoeuvres.
- Reassess cervical dilatation; if not fully dilated consider Duhrssen incision at 2, 10 and 6 o'clock.
- A caesarean section may be performed if the baby is still alive.
Neonatal management
- Paediatric review.
- Routine observations as per your local guidelines, recorded on a track and trigger chart.
- Observe for signs of jaundice.
- Observe for signs of tissue or nerve damage.
- Hip ultrasound scan to be performed at 6-12 weeks post birth to monitor for developmental dysplasia of the hip (DDH). See Neonatal eHandbook - Developmental dysplasia of the hip .
More information
Audit and performance improvement.
All maternity services should have processes in place for:
- auditing clinical practice and outcomes
- providing feedback to clinicians on audit results
- addressing risks, if identified
- implementing change, if indicated.
Potential auditable standards are:
- number of women with a breech presentation offered ECV
- success rate of ECV
- ECV complications
- rate of planned vaginal breech birth
- breech birth outcomes for vaginal and caesarean birth.
For more information or assistance with auditing, please contact us via [email protected]
- Bue and Lauszus 2016, Moxibustion did not have an effect in a randomised clinical trial for version of breech position. Danish Medical Journal 63(2), A599
- Coulon et.al. 2014, Version of breech fetuses by moxibustion with acupuncture. Obstetrics and Gynecology 124(1), 32-39. DOI: 10.1097/AOG.0000000000000303
- Coyle ME, Smith CA, Peat B 2012, Cephalic version by moxibustion for breech presentation. Cochrane Database of Systematic Reviews 2012, Issue 5. Art. No.: CD003928. DOI: 10.1002/14651858.CD003928.pub3
- Evans J 2012, Essentially MIDIRS Understanding Physiological Breech Birth Volume 3. Number 2. February 2012
- Hoffmann J, Thomassen K, Stumpp P, Grothoff M, Engel C, Kahn T, et al. 2016, New MRI Criteria for Successful Vaginal Breech Delivery in Primiparae. PLoS ONE 11(8): e0161028. doi:10.1371/journal.pone.0161028
- Hofmeyr GJ, Kulier R 2012, Cephalic version by postural management for breech presentation. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No.: CD000051. DOI: 10.1002/14651858.CD000051.pub2
- New South Wales Department of Health 2013, Maternity: Management of Breech Presentation HNELHD CG 13_01, NSW Government; 2013
- Royal College of Obstetricians and Gynaecologists 2017, External Cephalic Version and Reducing the Incidence of Term Breech Presentation. Green-top Guideline No. 20a . London: RCOG; 2017
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) 2016, Management of breech presentation at term , July 2016 C-Obs-11:
- The Royal Women's Hospital 2015, Management of Breech - Clinical Guideline
- Women's and Newborn Health Service, King Edward Memorial Hospital 2015, Complications of Pregnancy Breech Presentation
Abbreviations
Get in touch, version history.
First published: November 2018 Due for review: November 2021
Uncontrolled when downloaded
Related links.
- Search Please fill out this field.
- Newsletters
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles
Loading metrics
Open Access
Peer-reviewed
Research Article
Screening for breech presentation using universal late-pregnancy ultrasonography: A prospective cohort study and cost effectiveness analysis
Roles Formal analysis, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Cambridge Centre for Health Services Research, Cambridge Institute of Public Health, Cambridge, United Kingdom, The Primary Care Unit, Department of Public Health and Primary Care, University of Cambridge, Cambridge, United Kingdom
Roles Formal analysis, Writing – review & editing
Affiliation Department of Obstetrics and Gynaecology, University of Cambridge, NIHR Cambridge Comprehensive Biomedical Research Centre, Cambridge, United Kingdom
Roles Conceptualization, Investigation, Writing – original draft
Roles Formal analysis, Methodology, Writing – review & editing
Affiliations Cambridge Centre for Health Services Research, Cambridge Institute of Public Health, Cambridge, United Kingdom, Health Economics Group, Norwich Medical School, University of East Anglia, Norwich, United Kingdom
Roles Conceptualization, Methodology, Writing – review & editing
- David Wastlund,
- Alexandros A. Moraitis,
- Alison Dacey,
- Ulla Sovio,
- Edward C. F. Wilson,
- Gordon C. S. Smith

- Published: April 16, 2019
- https://doi.org/10.1371/journal.pmed.1002778
- Reader Comments
Despite the relative ease with which breech presentation can be identified through ultrasound screening, the assessment of foetal presentation at term is often based on clinical examination only. Due to limitations in this approach, many women present in labour with an undiagnosed breech presentation, with increased risk of foetal morbidity and mortality. This study sought to determine the cost effectiveness of universal ultrasound scanning for breech presentation near term (36 weeks of gestational age [wkGA]) in nulliparous women.
Methods and findings
The Pregnancy Outcome Prediction (POP) study was a prospective cohort study between January 14, 2008 and July 31, 2012, including 3,879 nulliparous women who attended for a research screening ultrasound examination at 36 wkGA. Foetal presentation was assessed and compared for the groups with and without a clinically indicated ultrasound. Where breech presentation was detected, an external cephalic version (ECV) was routinely offered. If the ECV was unsuccessful or not performed, the women were offered either planned cesarean section at 39 weeks or attempted vaginal breech delivery. To compare the likelihood of different mode of deliveries and associated long-term health outcomes for universal ultrasound to current practice, a probabilistic economic simulation model was constructed. Parameter values were obtained from the POP study, and costs were mainly obtained from the English National Health Service (NHS). One hundred seventy-nine out of 3,879 women (4.6%) were diagnosed with breech presentation at 36 weeks. For most women (96), there had been no prior suspicion of noncephalic presentation. ECV was attempted for 84 (46.9%) women and was successful in 12 (success rate: 14.3%). Overall, 19 of the 179 women delivered vaginally (10.6%), 110 delivered by elective cesarean section (ELCS) (61.5%) and 50 delivered by emergency cesarean section (EMCS) (27.9%). There were no women with undiagnosed breech presentation in labour in the entire cohort. On average, 40 scans were needed per detection of a previously undiagnosed breech presentation. The economic analysis indicated that, compared to current practice, universal late-pregnancy ultrasound would identify around 14,826 otherwise undiagnosed breech presentations across England annually. It would also reduce EMCS and vaginal breech deliveries by 0.7 and 1.0 percentage points, respectively: around 4,196 and 6,061 deliveries across England annually. Universal ultrasound would also prevent 7.89 neonatal mortalities annually. The strategy would be cost effective if foetal presentation could be assessed for £19.80 or less per woman. Limitations to this study included that foetal presentation was revealed to all women and that the health economic analysis may be altered by parity.
Conclusions
According to our estimates, universal late pregnancy ultrasound in nulliparous women (1) would virtually eliminate undiagnosed breech presentation, (2) would be expected to reduce foetal mortality in breech presentation, and (3) would be cost effective if foetal presentation could be assessed for less than £19.80 per woman.
Author summary
Why was this study done.
- Risks of complications at delivery are higher for babies that are in a breech position, but sometimes breech presentation is not discovered until the time of birth.
- Ultrasound screening could be used to detect breech presentation before birth and lower the risk of complications but would be associated with additional costs.
- It is uncertain if offering ultrasound screening to every pregnancy is cost effective.
What did the researchers do and find?
- This study recorded the birth outcomes of pregnancies that were all screened using ultrasound.
- Economic modelling and simulation was used to compare these outcomes with those if ultrasound screening had not been used.
- Modelling demonstrated that ultrasound screening would lower the risk of breech delivery and, as a result, reduce emergency cesarean sections and the baby’s risk of death.
What do these findings mean?
- Offering ultrasound screening to every pregnancy would improve the health of mothers and babies nationwide.
- Whether the health improvements are enough to justify the increased cost of ultrasound screening is still uncertain, mainly because the cost of ultrasound screening for presentation alone is unknown.
- If ultrasound screening could be provided sufficiently inexpensively, for example, by being used during standard midwife appointments, routinely offering ultrasound screening would be worthwhile.
Citation: Wastlund D, Moraitis AA, Dacey A, Sovio U, Wilson ECF, Smith GCS (2019) Screening for breech presentation using universal late-pregnancy ultrasonography: A prospective cohort study and cost effectiveness analysis. PLoS Med 16(4): e1002778. https://doi.org/10.1371/journal.pmed.1002778
Academic Editor: Jenny E. Myers, University of Manchester, UNITED KINGDOM
Received: August 30, 2018; Accepted: March 11, 2019; Published: April 16, 2019
Copyright: © 2019 Wastlund et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The terms of the ethical permission for the POP study do not allow publication of individual patient level data. Requests for access to patient level data will usually require a Data Transfer Agreement, and should be made to Mrs Sheree Green-Molloy at the Department of Obstetrics and Gynaecology, Cambridge University, UK ( [email protected] ).
Funding: This study was funded by the National Institute for Health Research (NIHR) Health Technology Assessment programme, grant number 15/105/01. EW is part funded by the NIHR Cambridge Biomedical Research Centre. US is funded by the NIHR Cambridge Comprehensive Biomedical Research Centre. The views expressed here are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health ( https://www.nihr.ac.uk/ ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: I have read the journal's policy and the authors of this manuscript have the following competing interests: GS reports grants from the National Institute for Health Research (NIHR), Stillbirth and Neonatal Death Society, and MRC and reports other from GE and NIHR Cambridge Clinical Research Facility, during the study; reports personal fees and other from GlaxoSmithKline and Roche, and reports other from Chiesi, outside of the study. GS is an Academic Editor on PLOS Medicine's editorial board. DW, AM, AD, US, and EW declare no competing interests.
Abbreviations: AFI, amniotic fluid index; AGA, appropriate for gestational age; CrI, credibility interval; ECV, external cephalic version; ELCS, elective cesarean section; EMCS, emergency cesarean section; FTE, full-time education; HCHS, Hospital and Community Health Services; ICER, incremental cost effectiveness ratio; IMD, Index of Multiple Deprivation; LGA, large for gestational age; MOD, mode of delivery; NHS, National Health Service; NICE, National Institute for Health and Care Excellence; POP, Pregnancy Outcome Prediction; PSA, probabilistic sensitivity analysis; QALY, quality-adjusted life-year; SGA, small for gestational age; wkGA, weeks of gestational age; RCOG, Royal College of Obstetricians and Gynaecologists; SRC, spontaneous reversion to cephalic; STROBE, Strengthening the Reporting of Observational Studies in Epidemiology
Introduction
Undiagnosed breech presentation in labour increases the risk of perinatal morbidity and mortality and represents a challenge for obstetric management. The incidence of breech presentation at term is around 3%–4% [ 1 – 3 ], and fewer than 10% of foetuses who are breech at term revert spontaneously to a vertex presentation [ 4 ]. Although breech presentation is easy to detect through ultrasound screening, many women go into labour with an undetected breech presentation [ 5 ]. The majority of these women will deliver through emergency cesarean section (EMCS), which has high costs and increased risk of morbidity and mortality for both mother and child.
In current practice, foetal presentation is routinely assessed by palpation of the maternal abdomen by a midwife, obstetrician, or general practitioner. The sensitivity of abdominal palpation varies between studies (range: 57%–70%) and depends on the skill and experience of the practitioner [ 6 , 7 ]. There is currently no guidance on what is considered an acceptable false negative rate when screening for breech presentation using abdominal palpation. In contrast, ultrasound examination provides a quick and safe method of accurately identifying foetal presentation.
Effective interventions exist for the care of women who have breech presentation diagnosed near term. The Royal College of Obstetricians and Gynaecologists recommends ‘that all women with an uncomplicated breech presentation at term should be offered external cephalic version (ECV)’ [ 2 ]. The rationale for this is to reduce the incidence of breech presentation at term and avoid the risks of vaginal breech birth or cesarean section. The success rate of ECV is considered to be approximately 50% [ 2 , 8 , 9 ], but it differs greatly between nulliparous and parous women (34% and 66%, respectively) [ 9 ]. ECV is overall safe, with less than 1% risk to the foetus and even smaller risk to the mother [ 10 ]; despite this, a significant number of women decline ECV for various reasons [ 11 ]. Should ECV be declined or fail, generally women are offered delivery by planned (elective) cesarean section, as there is level 1 evidence of reduced risk of perinatal death and severe morbidity compared with attempting vaginal breech birth, and it is also associated with lower costs [ 3 , 12 , 13 ]. However, some women may still opt for an attempt at vaginal breech birth if they prioritise nonintervention over managing the relatively small absolute risks of a severe adverse event [ 1 , 14 ].
We sought to assess the cost effectiveness of universal late-pregnancy ultrasound presentation scans for nulliparous women. We used data from the Pregnancy Outcome Prediction (POP) study, a prospective cohort study of >4,000 nulliparous women, which included an ultrasound scan at 36 weeks of gestational age (wkGA) [ 15 ]. Here, we report the outcomes for pregnant nulliparous women with breech presentation in the study and use these data to perform a cost effectiveness analysis of universal ultrasound as a screening test for breech presentation.
Study design
The POP study was a prospective cohort study of nulliparous women conducted at the Rosie Hospital, Cambridge (United Kingdom) between January 14, 2008 and July 31, 2012, and the study has been described in detail elsewhere [ 15 – 17 ]. Ethical approval for the study was obtained from the Cambridgeshire 2 Research Ethics Committee (reference 07/H0308/163), and all participants provided informed consent in writing. Participation in the POP study involved serial phlebotomy and ultrasound at approximately 12 wkGA, 20 wkGA, 28 wkGA, and 36 wkGA [ 16 ]. The outcome of pregnancy was obtained by individual review of all case records by research midwives and by linkage to the hospital’s electronic databases of ultrasonography, biochemical testing, delivery data, and neonatal care data. The research ultrasound at 36 wkGA was performed by sonographers and included presentation, biometry, uteroplacental Doppler, and placental location. The ultrasound findings were blinded except in cases of breech presentation, low lying placenta, or foetal concerns such as newly diagnosed foetal anomaly and an amniotic fluid index (AFI) < 5 cm. This study was not prospectively defined in the POP study protocol paper [ 16 ] but required no further data collection.
If the foetus was in a breech presentation at 36 wkGA, women were counselled by a member of the medical team. In line with guidelines from the National Institute for Health and Care Excellence (NICE), ECV was routinely offered unless there was a clinical indication that contraindicated the procedure, e.g., reduced AFI (<5 cm) [ 18 ]. ECV was performed by 1 of 5 obstetric consultants in the unit between 36–38 wkGA, patients were scanned before the procedure to confirm presentation, and it was performed with ultrasound assessment; 0.25 mg terbutaline SC was given prior to the procedure at the discretion of the clinician. If women refused ECV or the procedure failed, the options of vaginal breech delivery and elective cesarean section (ELCS) were discussed and documented. The local guideline for management of breech presentation, including selection criteria for vaginal breech delivery, was based upon recommendations from the Royal College of Obstetricians and Gynaecologists (RCOG) [ 1 ]. We extracted information about ECV from case records that were individually reviewed by research midwives. Finally, we obtained delivery-related information from our hospital electronic database (Protos; iSoft, Banbury, UK).
Foetal outcomes included mode of delivery (MOD), birth weight, and gestational age at delivery. We used the UK population reference for birthweight, with the 10th and 90th percentile cut-offs for small and large for gestational age, respectively; the centiles were adjusted for sex and gestational age [ 19 ]. Maternal age was defined as age at recruitment. Smoking status, racial ancestry, alcohol consumption, and BMI were taken from data recorded at the booking assessment by the community midwife. Socioeconomic status was quantified using the Index of Multiple Deprivation (IMD) 2007, which is based on census data from the area in the mother’s postcode [ 20 ]. Ethical approval for the study was obtained from the Cambridgeshire 2 Research Ethics Committee (reference 07/H0308/163), and all participants provided informed consent in writing.
This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline.
Statistical analysis
Data are presented as median (interquartile range) or n (%), as appropriate. P values are reported for the difference between groups calculated using the two-sample Wilcox rank-sum (Mann–Whitney) test for continuous variables and the Pearson Chi-square test for categorical variables, with trend tests when appropriate. Comparisons were performed using Stata (version 15.1). Missing values were included in the presentation of patient characteristics and outcomes but were excluded from the economic analysis and estimation of parameters.
Economic model and analysis
To evaluate the cost effectiveness of routinely offering late-pregnancy presentation scans, a decision-tree simulation model was constructed using R (version 3.4.1) [ 21 – 24 ]. The time horizon of the economic analysis was from the ultrasound scan (36 wkGA) to infant lifetime, and costs were from the perspective of the English National Health Service (NHS). Costs for modes of delivery were obtained from NHS reference costs [ 25 ]; since these do not list a separate cost for vaginal breech delivery, we assumed that the cost ratio between vaginal breech and ELCS deliveries was the same as in another study (see Supporting information , S1 Text ) [ 12 ].
The population of interest is unselected nulliparous women. The model compares the outcomes at birth for two strategies: ‘universal ultrasound’ and ‘selective ultrasound’ ( Fig 1 ). For universal ultrasound, we assumed that all breech presentations at the time of scanning would be detected (i.e., assumed 100% sensitivity and specificity for the test). For selective ultrasound, the breech presentation was diagnosed either clinically (by abdominal palpation followed by ultrasound for confirmation) or as an incidental finding during a scan for a different indication. These assumptions were based upon current practice and derived from the POP study.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Structure of economic simulation model. ‘Universal ultrasound’ strategy starts in Model A, and patients with breech presentation enter Model C. ‘Selective ultrasound’, i.e., no routine ultrasound, starts in Model B, and only those with a detected breech presentation enter Model C. The letter–number codes for each node are equivalent to the codes in Table 1 . ELCS, elective cesarean section; EMCS, emergency cesarean section.
https://doi.org/10.1371/journal.pmed.1002778.g001
Compared to a standard antenatal ultrasound for which, typically, multiple measurements are made, an ultrasound scan for foetal presentation alone is technically simple. We theorised that such a scan could be provided by an attending midwife in conjunction with a standard antenatal visit in primary care, using basic ultrasound equipment. Since a specific unit cost for a scan for foetal presentation alone is not included in the national schedule of reference costs [ 25 ], we estimated the cost of ultrasound to include the midwife’s time, the cost of equipment, and room. More details are presented in the Supporting information, S1 Text . The cost of ECV was obtained from James and colleagues [ 26 ] and converted to the 2017 price level using the Hospital and Community Health Services (HCHS) index [ 27 ]. The probability of ECV uptake and success rate as well as MOD were obtained from the POP study. All model inputs are presented in Table 1 and S1 Table , and the calculation of cost inputs is shown in Supporting information, S1 Text .
https://doi.org/10.1371/journal.pmed.1002778.t001
The end state of the decision tree was the MOD, which was either vaginal, ELCS, or EMCS. Delivery could be either cephalic or breech. EMCS could be either due to previously undiagnosed breech presentation or for other reasons. All cases of breech could spontaneously revert to cephalic presentation. However, we assumed the probability of this to be lower if ECV had been attempted and failed [ 28 ]. If ECV was successful, a reversion back to breech presentation was possible. It is currently unclear whether the probability of MOD varies depending on whether cephalic presentation is the result of successful ECV or spontaneous reversion [ 2 , 10 , 29 – 31 ], but we assumed that the probabilities differed.
Long-term health outcomes were modelled based upon the mortality risk associated with each MOD. The risk of neonatal mortality was taken from the RCOG guidelines. For breech presentation, these risks were 0.05% for delivery through ELCS and 0.20% for vaginal delivery. The risk of neonatal mortality for cephalic presentation with vaginal delivery was 0.10% [ 1 ]. There were no randomised clinical trials that allowed us to compare the outcomes of ELCS versus vaginal delivery for uncomplicated pregnancies with cephalic presentation; however, most observational studies found no significant difference in neonatal mortality and serious morbidity between the two modes [ 32 – 34 ]. For this reason, we assumed the mortality risk for cephalic vaginal and ELCS deliveries to be identical. We also assumed that EMCS would have the same mortality rate as ELCS, both for cephalic and breech deliveries. Studies have found that the MOD for breech presentation affects the risk of serious neonatal morbidity in the short term but not in the long term [ 1 , 3 , 35 ]. For this reason, we focused the economic analysis on the effect from mortality only. The average lifetime quality-adjusted life-years (QALYs) per member of the UK population was estimated using data on quality of life from Euroqol, weighted by longevity indexes from the Office for National Statistics (ONS) [ 36 , 37 ]. Using the annual discount rate of 3.5%, as recommended by NICE, the net present value for the average lifetime QALYs at birth was 24.3 [ 38 ].
The model was probabilistic, capturing how uncertainty in the input parameters affected the outputs by allowing each parameter to vary according to its distribution. Binary and multivariable outcomes were modelled using the beta and the Dirichlet distributions, respectively [ 39 ]. Probabilities of events were calculated from the POP study and presented in Table 1 . On top of the probabilistic sensitivity analysis (PSA), the sensitivity of individual parameters was also explored through one-way sensitivity analyses modifying probabilities by +/− 1 percentage point and costs by +/− £10 to see which parameters had the greatest impact on cost effectiveness estimates.
Total costs depended on the distribution of MOD, the number of expected mortalities, and the cost of ultrasound scanning and ECV. Nationwide costs for each screening strategy were calculated for 585,489 deliveries, i.e., the number of births in England from 2016–2017, assuming 92% occur after 36 wkGA [ 15 , 40 ]. Model parameters were sampled from their respective distributions in a PSA of 100,000 simulations for each strategy. To determine cost effectiveness, we used two different willingness-to-pay thresholds: £20,000 and £30,000 [ 38 ]. A copy of the model code is available from the corresponding author (EW) upon request.
Recruitment to the POP study cohort is shown in Fig 2 and has been previously described [ 17 ]. Information about presentation at the 36-week scan was available for 3,879 women who delivered at the Rosie Hospital, Cambridge, UK; 179 of these had a breech presentation.
Schedule of patient recruitment in the POP study shown by foetal presentation. POP, Pregnancy Outcome Prediction.
https://doi.org/10.1371/journal.pmed.1002778.g002
We compared maternal and foetal characteristics of the 179 women with breech presentation at 36 weeks to the women with a cephalic presentation ( Table 2 ). Women diagnosed with breech presentation were, on average, a year older than women with a cephalic presentation, but other maternal characteristics did not differ. The babies of women diagnosed breech were smaller and born earlier, but their birth weight centile and the proportions of small for gestational age (SGA) or large for gestational age (LGA) were not markedly different. There were no differences in maternal BMI between the groups. As expected, women with breech presentation were more likely to deliver by ELCS or EMCS.
https://doi.org/10.1371/journal.pmed.1002778.t002
Breech presentation was suspected before the 36-wkGA scan for 79 (44.1%) of the women with breech presentation through abdominal palpation by the midwife or doctor; out of these, 27 had a clinically indicated scan between 32–36 weeks in which the presentation was reported. For 96 women, the breech presentation was unsuspected before the 36-week scan. Information on suspected breech position was missing for 4 women. There were no differences in BMI between the 79 women with suspected breech and the 96 women misdiagnosed as cephalic prior to the scan (median BMI was 24 in both groups, Wilcoxon rank-sum test P = 0.31).
MOD by ECV status is shown in Table 3 . ECV was performed for 84 women, declined by 45 women, and unsuitable for 23; contraindications included low AFI at screening (18 women), uterine abnormalities (2), and other reasons (3). For 25 women, an ECV was never performed despite consent; 17 babies turned spontaneously, 6 had reduced AFI on the day of the ECV, and 2 went into labour before ECV. When performed, ECV was successful for 12 women; in one case, the baby later reverted to breech presentation before delivery. Information on ECV uptake was missing for 2 women. Foetal presentation and ECV status in the structure of the economic model is shown in Supporting information, S1 Fig .
https://doi.org/10.1371/journal.pmed.1002778.t003
The results from the economic analysis are presented in Table 4 . On average, universal ultrasound resulted in an absolute decrease in breech deliveries by 0.39%. It also led to fewer vaginal breech deliveries (absolute decrease by 1.04%) and overall EMCS deliveries (0.72%) than selective ultrasound but increased overall deliveries through ELCS (1.51%). Resulting from the more favourable distribution of MOD, the average risk of mortality fell by 0.0013%. On average, 40 women had to be scanned to identify one previously unsuspected breech presentation (95% Credibility Interval [CrI]: 33 to 49); across England, this would mean that 14,826 (95% CrI: 12,048–17,883) unidentified breech presentations could be avoided annually.
https://doi.org/10.1371/journal.pmed.1002778.t004
The expected per person cost of universal ultrasound was £2,957 (95% CrI: £2,922–£2,991), compared to £2,949 (95% CrI: £2,915–£2,984) from selective ultrasound, a cost increase of £7.29 (95% CrI: 2.41–11.61). Across England, this means that universal ultrasound would cost £4.27 million more annually than current practice. The increase stems from higher costs of ultrasound scan (£20.3 per person) and ECV (£3.6 per person) but is partly offset by the lower delivery costs (−£16.5 per person). The distribution of differences in costs between the two strategies is shown as Supporting information, S2 Fig . The simulation shows that universal ultrasound would, on average, increase the number of total ELCS deliveries by 8,858 (95% CrI: 7,662–10,068) but decrease the number of EMCS and vaginal breech deliveries by 4,196 (95% CrI: 2,779–5,603) and 6,061 (95% CrI: 6,617–8,670) per year, respectively.
The long-term health outcomes are presented in Table 4 . Nationwide, universal ultrasound would be expected to lower mortality by 7.89 cases annually (95% CrI: 3.71, 12.7). After discounting, this means that universal ultrasound would be expected to yield 192 QALYs annually (95% CrI: 90,308). The cost effectiveness of universal ultrasound depends on the value assigned to these QALYs. The incremental cost effectiveness ratio (ICER) was £23,611 (95% CrI: 8,184, 44,851), which is of borderline cost effectiveness (given NICE’s willingness to pay of £20,000 to £30,000) [ 38 ]. The number needed to scan per prevented mortality was 74,204 (95% CrI: 46,124–157,642).
One-way sensitivity analysis showed that the probability parameter with the greatest impact upon the cost effectiveness of universal ultrasound was the prevalence of breech: increasing this parameter by 1 percentage point was associated with a relative reduction of costs for universal ultrasound by £3.07. The results were less sensitive to the ECV success rate; an increase by 1 percentage point led to a relative reduction in the cost of universal ultrasound by £0.12. The most important cost parameter was the unit cost of ultrasound scan; an increase in this parameter by £10 led to a relative increase for universal ultrasound by £9.79 (see Supporting information , S3 Fig ). Keeping all other parameters equal, universal ultrasound would be cost effective if ultrasound scanning could be provided for less than £19.80 or £23.10 per mother, for a willingness-to-pay threshold of £20,000 or £30,000, respectively. For universal ultrasound to be cost saving, scans would need to cost less than £12.90 per mother.
In a prospective cohort study of >3,800 women having first pregnancies, a presentation scan at approximately 36 wkGA identified the 4.6% of women who had a foetus presenting by the breech, and for more than half of these, breech presentation had not previously been clinically suspected. The majority of these women were ultimately delivered by planned cesarean section, some experienced labour before their scheduled date and were delivered by EMCS, and a small proportion had a cephalic vaginal delivery following either spontaneous cephalic version or ECV. No woman in the cohort had a vaginal breech delivery or experienced an intrapartum cesarean for undiagnosed breech. The low uptake of vaginal breech birth is likely to reflect the fact that this is a nulliparous population, and it is generally accepted that the risks associated with vaginal breech delivery are lower in women who have had a previous normal birth.
Our economic analysis suggests that a universal late-pregnancy presentation scan would decrease the number of foetal mortalities associated with breech presentation and that this is of borderline cost effectiveness, costing an estimated £23,611 per QALY gained. The key driver of cost effectiveness is the cost of the scan itself. In the absence of a specific national unit cost, we have identified the maximum cost at which it would be cost effective. This is £19.80 per scan to yield an ICER of £20,000 per QALY and £23.10 at £30,000. These unit costs may be possible if assessment of presentation could be performed as part of a routine antenatal visit. Portable ultrasound systems adequate for presentation scans are available at low cost, and a presentation scan is technically quite simple, so the required level of skill could be acquired by a large cadre of midwives. This would result in a small fraction of the costs associated with a trained ultrasonographer performing a scan in a dedicated space using a high-specification machine. If universal ultrasound could be provided for less than £12.90 per scan, the policy would also be cost saving.
Our sensitivity analysis shows that the unit cost of ultrasound scans and the prevalence of breech presentation were by far the biggest determinants of the cost and cost effectiveness of universal ultrasound. The detection rate with abdominal palpation (i.e., for selective ultrasound) is the most important parameter aside from these. By contrast, the costs, attempt, and success rates for ECV have modest impact upon the choice of scanning strategy. It appears that the main short-term cost benefit from late-pregnancy screening lies in the possibility of scheduling ELCSs when breech presentation is detected, rather than turning the baby into a cephalic position.
This analysis may have underestimated the health benefits of universal late-pregnancy ultrasound. In the absence of suitable data on long-term outcomes by MOD and foetal presentation, we made the simplifying assumption that mortality rates were equal for ELCSs and EMCSs. Relaxing this assumption would likely favour universal ultrasound, as this strategy would reduce EMCSs, and these are associated with higher risks of adverse outcomes than ELCSs [ 41 – 44 ]; on top of health benefits, this may also reduce long-term NHS costs. It is also possible that an EMCS for a known breech presentation is less expensive and has better health outcomes than one for which breech is detected intrapartum, although lack of separate data for these two scenarios prevented us from pursuing this analysis further.
Our analysis shows that universal late-pregnancy ultrasound screening would increase total number of cesarean sections. Evidence suggests that cesarean delivery may have long-term consequences on the health of the child (increased risk of asthma and obesity), the mother (reduced risk of pelvic organ prolapse and increased risk of subfertility), and future pregnancies (increased risk of placenta previa and stillbirth) [ 45 , 46 ]. There is no evidence that these are related to the type of the cesarean section (elective versus emergency) [ 45 , 46 ]. Our economic modelling has not been able to capture these complex effects due to the model’s endpoints and the focus on the current pregnancy only. However, accounting for these effects, it seems plausible that universal late-pregnancy ultrasound would be more favourable for mothers than children or future pregnancies.
Our results are also driven by vaginal delivery yielding worse long-term health outcomes than ELCS for breech presentation [ 1 ]. However, even though the rate of vaginal breech birth declined after the Term Breech Study, in many cases, the outcomes are not inferior to that of ELCS, and the RCOG guidelines state that vaginal breech delivery may be attempted following careful selection and counselling [ 1 , 3 , 47 ]. It is hard to assess how an increase in vaginal breech delivery would affect the cost effectiveness of universal ultrasound; while decreased mortality risk from vaginal breech delivery would decrease the importance of knowing the foetal presentation, universal screening would facilitate selection for attempted vaginal breech delivery.
One limitation of this study is that foetal presentation was revealed to all women in the POP study. Consequently, this study cannot say what would have happened without routine screening. However, we felt that it was appropriate to reveal the presentation at the time of the 36-wkGA scan, as there is level 1 evidence that planned cesarean delivery reduces the risk of perinatal morbidity and mortality in the context of breech presentation at term [ 44 ]. Another weakness was that the study was being undertaken in a single centre only and that the sample size was too small to avoid substantial parameter uncertainty for rare events. Moreover, less than half of all breech presentations in the POP study were detected by abdominal palpation. It is unclear whether the detection rates were affected by midwives knowing that the women were part of the POP study and, hence, would receive an ultrasound scan at 36 wkGA.
The prevalence of breech presentation in this study (4.6%) appears higher than the 3%–4% that is often reported in literature [ 1 ]. However, this study is unique in that it reports the prevalence at the time of ultrasound scanning, approximately 36 wkGA. Taking into account the number of spontaneous reversions to cephalic and that some cases of successful ECV may have turned spontaneously without intervention, our finding is consistent with the literature. The ECV success rate in the POP study was considerably lower than reported elsewhere in the literature; it was even lower than the 32% success rate that has been reported as the threshold level for when ECV is preferred over no intervention at all [ 48 ]. This might partly reflect the participants in the POP study; they were older and more likely to be obese than in many previous studies, and the cohort consisted of nulliparous women, who have higher rates of ECV failure than parous women [ 9 , 49 , 50 ]. It is also possible that the real-world ECV success rate is lower than in the literature due to publication bias. However, sensitivity analysis indicates that the impact from an increased ECV success rate would be modest (an increase in ECV success rate by 10 percentage points lowers the incremental cost of universal ultrasound by £0.91 per patient).
The findings from this study cannot easily be transferred to another health system due to the differences in healthcare costs and antenatal screening routines. Some countries, e.g., France and Germany, already offer a third-trimester routine ultrasound scan. However, these scans are offered prior to 36 wkGA, and as many preterm breech presentations revert spontaneously, it would have limited predictive value for breech at term [ 51 ]. Whether screening for breech presentation in lower-income settings is likely to be cost effective largely depends on the coverage of the healthcare system; while screening may be relatively more costly, the benefits from avoiding undiagnosed breech presentation may also be relatively larger.
Whether the findings of this study could be extrapolated beyond nulliparous women is hard to assess. The absence of comparable data on screening sensitivity without universal ultrasound for parous women is an important limitation. The risks associated with breech birth also differ between nulliparous and parous women [ 52 , 53 ]. Compared to nulliparous women, parous women have higher success rates for ECV but also higher risk of spontaneous reversion to breech after 36 wkGA [ 9 , 28 ]. Also, the risks associated with vaginal breech delivery are lower in women who have had a previous vaginal birth [ 30 ].
Breech presentation is not the only complication that could be detected through late-pregnancy ultrasound screening. The same ultrasound session could also be used to screen for other indicators of foetal health, such as biometry and signs of growth restriction. Whether also scanning for other complications could increase the benefits from universal ultrasound has been and currently is subject to research [ 54 , 55 ]. Exploring the consequences from such joint screening strategies goes beyond the scope of this paper but has important implications for policy-makers and should therefore be subject to further research.
This study shows that implementation of universal late-pregnancy ultrasound to assess foetal presentation would virtually eliminate undiagnosed intrapartum breech presentation in nulliparous women. If this procedure could be implemented into routine care, for example, by midwives conducting a routine 36-wkGA appointment and using a portable ultrasound system, it is likely to be cost effective. Such a programme would be expected to reduce the consequences to the child of undiagnosed breech presentation, including morbidity and mortality.
Supporting information
S1 strobe checklist. strobe, strengthening the reporting of observational studies in epidemiology..
https://doi.org/10.1371/journal.pmed.1002778.s001
S1 Text. Cost input estimation.
https://doi.org/10.1371/journal.pmed.1002778.s002
S1 Table. Input costs and probabilities for the economic model, detailed.
https://doi.org/10.1371/journal.pmed.1002778.s003
S1 Fig. Foetal presentation and ECV status in the POP breech study.
ECV, external cephalic version; POPs, Pregnancy Outcome Prediction.
https://doi.org/10.1371/journal.pmed.1002778.s004
S2 Fig. PSA of cost differences between universal ultrasound and selective ultrasound.
PSA, Probabilistic Sensitivity Analysis.
https://doi.org/10.1371/journal.pmed.1002778.s005
S3 Fig. One-way sensitivity analysis of the difference in costs between universal ultrasound and selective ultrasound.
https://doi.org/10.1371/journal.pmed.1002778.s006
- View Article
- Google Scholar
- PubMed/NCBI
- 18. National Institute for Health and Care Excellence. Quality standard: Antenatal care. In: National Institute for Health and Care Excellence, ed., 2012.
- 21. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing, 2017.
- 25. Department of Health. NHS Reference Costs 2015–16, 2016.
- 36. Szende A, Janssen B, Cabasés J. Self-Reported Population Health: An International Perspective based on EQ-5D: Springer Dordrecht Heidelberg New York London, 2014.
- 38. National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal 2013, 2013.
- 39. Briggs A, Claxton K, Sculpher M. Decision modelling for health economic evaluation. Oxford: Oxford University Press 2006.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.

Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
It may just be a matter of chance that your baby has not turned into the head-first position. However, there are certain factors that make it more difficult for your baby to turn during pregnancy and therefore more likely to stay in the breech position. These include:
- if this is your first pregnancy
- if your placenta is in a low-lying position (also known as placenta praevia); see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- if you have too much or too little fluid ( amniotic fluid ) around your baby
- if you are having more than one baby.
Very rarely, breech may be a sign of a problem with the baby. If this is the case, such problems may be picked up during the scan you are offered at around 20 weeks of pregnancy.
If your baby is breech at 36 weeks of pregnancy, your healthcare professional will discuss the following options with you:
- trying to turn your baby in the uterus into the head-first position by external cephalic version (ECV)
- planned caesarean section
- planned vaginal breech birth.
What does ECV involve?
ECV involves applying gentle but firm pressure on your abdomen to help your baby turn in the uterus to lie head-first.
Relaxing the muscle of your uterus with medication has been shown to improve the chances of turning your baby. This medication is given by injection before the ECV and is safe for both you and your baby. It may make you feel flushed and you may become aware of your heart beating faster than usual but this will only be for a short time.
Before the ECV you will have an ultrasound scan to confirm your baby is breech, and your pulse and blood pressure will be checked. After the ECV, the ultrasound scan will be repeated to see whether your baby has turned. Your baby’s heart rate will also be monitored before and after the procedure. You will be advised to contact the hospital if you have any bleeding, abdominal pain, contractions or reduced fetal movements after ECV.
ECV is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labour. You do not need to make any preparations for your ECV.
ECV can be uncomfortable and occasionally painful but your healthcare professional will stop if you are experiencing pain and the procedure will only last for a few minutes. If your healthcare professional is unsuccessful at their first attempt in turning your baby then, with your consent, they may try again on another day.
If your blood type is rhesus D negative, you will be advised to have an anti-D injection after the ECV and to have a blood test. See the NICE patient information Routine antenatal anti-D prophylaxis for women who are rhesus D negative , which is available at: www.nice.org.uk/guidance/ta156/informationforpublic .
Why turn my baby head-first?
If your ECV is successful and your baby is turned into the head-first position you are more likely to have a vaginal birth. Successful ECV lowers your chances of requiring a caesarean section and its associated risks.
Is ECV safe for me and my baby?
ECV is generally safe with a very low complication rate. Overall, there does not appear to be an increased risk to your baby from having ECV. After ECV has been performed, you will normally be able to go home on the same day.
When you do go into labour, your chances of needing an emergency caesarean section, forceps or vacuum (suction cup) birth is slightly higher than if your baby had always been in a head-down position.
Immediately after ECV, there is a 1 in 200 chance of you needing an emergency caesarean section because of bleeding from the placenta and/or changes in your baby’s heartbeat.
ECV should be carried out by a doctor or a midwife trained in ECV. It should be carried out in a hospital where you can have an emergency caesarean section if needed.
ECV can be carried out on most women, even if they have had one caesarean section before.
ECV should not be carried out if:
- you need a caesarean section for other reasons, such as placenta praevia; see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- you have had recent vaginal bleeding
- your baby’s heart rate tracing (also known as CTG) is abnormal
- your waters have broken
- you are pregnant with more than one baby; see the RCOG patient information Multiple pregnancy: having more than one baby .
Is ECV always successful?
ECV is successful for about 50% of women. It is more likely to work if you have had a vaginal birth before. Your healthcare team should give you information about the chances of your baby turning based on their assessment of your pregnancy.
If your baby does not turn then your healthcare professional will discuss your options for birth (see below). It is possible to have another attempt at ECV on a different day.
If ECV is successful, there is still a small chance that your baby will turn back to the breech position. However, this happens to less than 5 in 100 (5%) women who have had a successful ECV.
There is no scientific evidence that lying down or sitting in a particular position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called mugwort) at 33–35 weeks of pregnancy may help your baby to turn into the head-first position, possibly by encouraging your baby’s movements. This should be performed under the direction of a registered healthcare practitioner.
Depending on your situation, your choices are:
There are benefits and risks associated with both caesarean section and vaginal breech birth, and these should be discussed with you so that you can choose what is best for you and your baby.
Caesarean section
If your baby remains breech towards the end of pregnancy, you should be given the option of a caesarean section. Research has shown that planned caesarean section is safer for your baby than a vaginal breech birth. Caesarean section carries slightly more risk for you than a vaginal birth.
Caesarean section can increase your chances of problems in future pregnancies. These may include placental problems, difficulty with repeat caesarean section surgery and a small increase in stillbirth in subsequent pregnancies. See the RCOG patient information Choosing to have a caesarean section .
If you choose to have a caesarean section but then go into labour before your planned operation, your healthcare professional will examine you to assess whether it is safe to go ahead. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
Vaginal breech birth
After discussion with your healthcare professional about you and your baby’s suitability for a breech delivery, you may choose to have a vaginal breech birth. If you choose this option, you will need to be cared for by a team trained in helping women to have breech babies vaginally. You should plan a hospital birth where you can have an emergency caesarean section if needed, as 4 in 10 (40%) women planning a vaginal breech birth do need a caesarean section. Induction of labour is not usually recommended.
While a successful vaginal birth carries the least risks for you, it carries a small increased risk of your baby dying around the time of delivery. A vaginal breech birth may also cause serious short-term complications for your baby. However, these complications do not seem to have any long-term effects on your baby. Your individual risks should be discussed with you by your healthcare team.
Before choosing a vaginal breech birth, it is advised that you and your baby are assessed by your healthcare professional. They may advise against a vaginal birth if:
- your baby is a footling breech (one or both of the baby’s feet are below its bottom)
- your baby is larger or smaller than average (your healthcare team will discuss this with you)
- your baby is in a certain position, for example, if its neck is very tilted back (hyper extended)
- you have a low-lying placenta (placenta praevia); see the RCOG patient information Placenta Praevia, placenta accreta and vasa praevia
- you have pre-eclampsia or any other pregnancy problems; see the RCOG patient information Pre-eclampsia .
With a breech baby you have the same choices for pain relief as with a baby who is in the head-first position. If you choose to have an epidural, there is an increased chance of a caesarean section. However, whatever you choose, a calm atmosphere with continuous support should be provided.
If you have a vaginal breech birth, your baby’s heart rate will usually be monitored continuously as this has been shown to improve your baby’s chance of a good outcome.
In some circumstances, for example, if there are concerns about your baby’s heart rate or if your labour is not progressing, you may need an emergency caesarean section during labour. A paediatrician (a doctor who specialises in the care of babies, children and teenagers) will attend the birth to check your baby is doing well.
If you go into labour before 37 weeks of pregnancy, the balance of the benefits and risks of having a caesarean section or vaginal birth changes and will be discussed with you.
If you are having twins and the first baby is breech, your healthcare professional will usually recommend a planned caesarean section.
If, however, the first baby is head-first, the position of the second baby is less important. This is because, after the birth of the first baby, the second baby has lots more room to move. It may turn naturally into a head-first position or a doctor may be able to help the baby to turn. See the RCOG patient information Multiple pregnancy: having more than one baby .
If you would like further information on breech babies and breech birth, you should speak with your healthcare professional.
Further information
- NHS information on breech babies
- NCT information on breech babies
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions , if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
- https://aqua.nhs.uk/resources/shared-decision-making-case-studies/
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Clinical Guidelines No. 20a External Cephalic Version and Reducing Incidence of Term Breech Presentation and No. 20b Management of Breech Presentation . The guidelines contain a full list of the sources of evidence we have used.
This information was reviewed before publication by women attending clinics in Nottingham, Essex, Inverness, Manchester, London, Sussex, Bristol, Basildon and Oxford, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
Please give us feedback by completing our feedback survey:
- Members of the public – patient information feedback
- Healthcare professionals – patient information feedback
External Cephalic Version and Reducing the Incidence of Term Breech Presentation Green-top Guideline
Management of Breech Presentation Green-top Guideline
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Original Article
- Published: 24 October 2013
Breech presentation at delivery: a marker for congenital anomaly?
- D Mostello 1 ,
- J J Chang 2 ,
- C Guild 4 ,
- K Stamps 2 &
- T L Leet 2 na1
Journal of Perinatology volume 34 , pages 11–15 ( 2014 ) Cite this article
19k Accesses
21 Citations
17 Altmetric
Metrics details
- Paediatrics
- Pregnancy outcome
To determine whether congenital anomalies are associated with breech presentation at the time of birth.
Study Design:
A population-based, retrospective cohort study was conducted among 460 147 women with singleton live births using the Missouri Birth Defects Registry, which includes all defects diagnosed during the first year of life. Maternal and obstetric characteristics and outcomes between breech and cephalic presentation groups were compared using χ 2 -square statistic and Student’s t -test. Multivariable binary logistic regression analysis was used to estimate adjusted odds ratios (aORs) and 95% confidence intervals (CIs).
At least one congenital anomaly was more likely present among infants breech at birth (11.7%) than in those with cephalic presentation (5.1%), whether full-term (9.4 vs 4.6%) or preterm (20.1 vs 11.6%). The relationship between breech presentation and congenital anomaly was stronger among full-term births (aOR 2.09, CI 1.96, 2.23, term vs 1.40, CI 1.26, 1.55, preterm), but not in all categories of anomalies.
Conclusion:
Breech presentation at delivery is a marker for the presence of congenital anomaly. Infants delivered breech deserve special scrutiny for the presence of malformation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
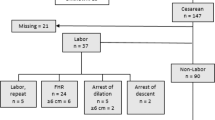
Maternal and neonatal factors associated with cesarean delivery in a cohort of pregnancies complicated by prenatally diagnosed congenital heart disease
Heather Masters, Elisa Marcuccio, … Allison Divanovic

Congenital anomalies among newborn babies in Felege-Hiwot Comprehensive Specialized Referral Hospital, Bahir Dar, Ethiopia
Daniel Mekonnen, MollaTaye & Walelegn Worku
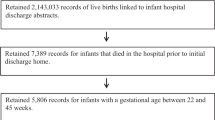
Understanding the relative contributions of prematurity and congenital anomalies to neonatal mortality
Ciaran S. Phibbs, Molly Passarella, … Scott A. Lorch
Cruikshank DP . Breech presentation. Clin Obstet Gynecol 1986; 29 : 255–263.
Article CAS Google Scholar
Braun FHT, Jones KL, Smith DW . Breech presentation as an indicator of fetal abnormality. J Pediatr 1975; 86 : 419–421.
Axelrod FB, Leistner HL, Porges RF . Breech presentation among infants with familial dysautonomia. J Pediatr 1974; 84 : 107–109.
Fianu S, Vaclavinkova V . The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand 1978; 57 : 371–372.
Brenner WE, Bruce RD, Hendricks CH . The characteristics and perils of breech presentation. Am J Obstet Gynecol 1974; 118 : 700–712.
Luterkort M, Persson P, Weldner B . Maternal and fetal factors in breech presentation. Obstet Gynecol 1984; 64 : 55–59.
Rayl J, Gibson PJ, Hickok DE . A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol 1996; 174 : 28–32.
Axelrod FB, Porges RF, Sein ME . Neonatal recognition of familial dysautonomia. J Pediatr 1987; 110 : 946–948.
Gimovsky ML, Paul RH . Singleton breech presentation in labor: experience in 1980. Am J Obstet Gynecol 1982; 143 : 733–739.
Berendes HW, Weiss W, Deutschberger J, Jackson E . Factors associated with breech delivery. Am J Public Health Health 1965; 55 : 708–719.
Mazor M, Hagay ZJ, Leiberman JR, Biale Y, Insler V . Fetal malformations associated with breech delivery. Implications for obstetric management. J Reprod Med 1985; 30 : 884–886.
CAS PubMed Google Scholar
Alexander GR, Kogan MD, Himes JH . 1994–1996 US singleton birth weight percentiles for gestational age by race, Hispanic origin, and gender. Matern Child Health J 1999; 3 : 225–231.
Sorensen T, Hasch E, Lange AP . Fetal presentation during pregnancy [Letter]. Lancet 1979; 2 : 477.
Mickey RM, Greenland S . The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989; 129 : 125–137.
Hall JE, Kohl SG, O’Brien F, Ginsberg M . Breech presentation and perinatal mortality. Am J Obstet Gynecol 1965; 91 : 665–683.
Kauppila O . The perinatal mortality in breech deliveries and observations on affecting factors: a retrospective study of 2227 cases. Acta Obstet Gynecol Scand (Suppl) 1975; 39 : 1–79.
CAS Google Scholar
Goldberg JD . Routine screening for fetal anomalies: expectations. Obstet Gynecol Clin N Am 2004; 31 : 35–50.
Article Google Scholar
Grandjean H, Larroque D, Levi S . Sensitivity of routine ultrasound screening of pregnancies in the Eurofetus database. The Eurofetus Team. Ann N Y Acad Sci 1998; 847 : 118–124.
Wren C, Reinhardt Z, Khawaja K . Twenty-year trends in diagnosis of life-threatening neonatal cardiovascular malformations. Arch Dis Child Fetal Neonatal Ed 2008; 93 : F33–F35.
Bower C, Rudy E, Callaghan A, Quick J, Nassar N . Age at diagnosis of birth defects. Birth Defects Res A Clin Mol Teratol 2010; 88 : 251–255.
Tanner JP, Salemi JL, Hauser KW, Correia JA, Watkins SM, Kirby RS . Birth defects surveillance in Florida: infant death certificates as a case ascertainment source. Birth Defects Res A Clin Mol Teratol 2010; 88 : 1017–1022.
Wang Y, Sharpe-Stimac M, Cross PK, Druschel CM, Hwang S . Improving case ascertainment of a population-based birth defects registry in New York state using hospital discharge data. Birth Defects Res A Clin Mol Teratol 2005; 73 : 663–668.
Salemi JL, Tanner JP, Kennedy S, Block S, Bailey M, Correia JA et al . A comparison of two surveillance strategies for selected birth defects in Florida. Public Health Rep 2012; 127 : 391–400.
Frost F, Starzyk P, George S, McLaughlin JF . Birth complication reporting: the effect of birth certificate design. Am J Public Health 1984; 74 : 505–506.
Zollinger TW, Przybylski MJ, Gamache RE . Reliability of Indiana birth certificate data compared to medical records. Ann Epidemiol 2006; 16 : 1–10.
Download references
Acknowledgements
Many thanks go to Gilad Gross, MD for his helpful advice on improving this manuscript. The authors also acknowledge the Missouri Department of Health and Senior Services, Section of Epidemiology for Public Health Practice as the original source of the data. The analysis, interpretations and conclusions in the present study are those of the authors and not the Missouri Department of Health and Senior Services, Section of Epidemiology for Public Health Practice.
Author information
T L Leet: Dr Leet is deceased.
Authors and Affiliations
Division of Maternal-Fetal Medicine, Department of Obstetrics, Gynecology and Women’s Health, School of Medicine, Saint Louis University, St Louis, MO, USA
Department of Epidemiology, School of Public Health, Saint Louis University, St Louis, MO, USA
J J Chang, F Bai, K Stamps & T L Leet
Department of Biostatistics, School of Public Health, Saint Louis University, St Louis, MO, USA
Department of Pediatrics and the Center for Outcomes Research, School of Medicine, Saint Louis University, St Louis, MO, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to D Mostello .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Additional information
Presented at the 32nd Annual Meeting of the Society for Maternal-Fetal Medicine, February 6–11, 2012, Dallas, TX, USA.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mostello, D., Chang, J., Bai, F. et al. Breech presentation at delivery: a marker for congenital anomaly?. J Perinatol 34 , 11–15 (2014). https://doi.org/10.1038/jp.2013.132
Download citation
Received : 01 May 2013
Revised : 01 September 2013
Accepted : 13 September 2013
Published : 24 October 2013
Issue Date : January 2014
DOI : https://doi.org/10.1038/jp.2013.132
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- congenital abnormalities
- labor presentation
- pregnancy outcome
This article is cited by
A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case–control study.
- Anna E. Toijonen
- Seppo T. Heinonen
- Georg Macharey
Archives of Gynecology and Obstetrics (2020)
Outcome of small for gestational age-fetuses in breech presentation at term according to mode of delivery: a nationwide, population-based record linkage study
- Pia Hinnenberg
- Anna Toijonen
Archives of Gynecology and Obstetrics (2019)
Cesarean deliveries and maternal weight retention
- Kandice A. Kapinos
- Olga Yakusheva
- Marianne Weiss
BMC Pregnancy and Childbirth (2017)
Breech presentation at term and associated obstetric risks factors—a nationwide population based cohort study
- Mika Gissler
- Seppo Heinonen
Archives of Gynecology and Obstetrics (2017)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.20(4); 2023 Apr
- PMC10079042

Impact of point-of-care ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: An observational multicentre cohort study
Samantha knights.
1 Department of Obstetrics and Gynaecology, Norfolk and Norwich University Hospitals NHS Foundation Trust, Norwich, United Kingdom
Smriti Prasad
2 Fetal Medicine Unit, St George’s University Hospitals NHS Foundation Trust, London, United Kingdom
Erkan Kalafat
3 Department of Statistics, Middle East Technical University, Faculty of Arts and Sciences, Ankara, Turkey
4 Department of Obstetrics and Gynaecology, Koc University, School of Medicine, Istanbul, Turkey
Anahita Dadali
Francoise harlow, asma khalil.
5 Vascular Biology Research Centre, Molecular and Clinical Sciences Research Institute, St George’s University of London, London, United Kingdom
6 Fetal Medicine Unit, Liverpool Women’s Hospital, Liverpool, United Kingdom
Associated Data
Data cannot be shared publicly because consent was not obtained from women; permission for sharing data was not sought as part of ethical approval. Data is only available following approval from Research Ethics Committee and Confidentiality Advisory Group. Enquiries and requests should be made to the the Research Governance and Delivery team at St George's University of London ( ku.ca.lugs@CERlugs ).
Accurate knowledge of fetal presentation at term is vital for optimal antenatal and intrapartum care. The primary objective was to compare the impact of routine third trimester ultrasound or point-of-care ultrasound (POCUS) with standard antenatal care, on the incidence of overall and proportion of all term breech presentations that were undiagnosed at term, and on the related adverse perinatal outcomes.
Methods and findings
This was a retrospective multicentre cohort study where we included data from St. George’s (SGH) and Norfolk and Norwich University Hospitals (NNUH). Pregnancies were grouped according to whether they received routine third trimester scan (SGH) or POCUS (NNUH). Women with multiple pregnancy, preterm birth prior to 37 weeks, congenital abnormality, and those undergoing planned cesarean section for breech presentation were excluded. Undiagnosed breech presentation was defined as follows: (a) women presenting in labour or with ruptured membranes at term subsequently discovered to have a breech presentation; and (b) women attending for induction of labour at term found to have a breech presentation before induction. The primary outcome was the proportion of all term breech presentations that were undiagnosed. The secondary outcomes included mode of birth, gestational age at birth, birth weight, incidence of emergency cesarean section, and the following neonatal adverse outcomes: Apgar score <7 at 5 minutes, unexpected neonatal unit (NNU) admission, hypoxic ischemic encephalopathy (HIE), and perinatal mortality (including stillbirths and early neonatal deaths). We employed a Bayesian approach using informative priors from a previous similar study; updating their estimates (prior) with our own data (likelihood). The association of undiagnosed breech presentation at birth with adverse perinatal outcomes was analyzed with Bayesian log-binomial regression models. All analyses were conducted using R for Statistical Software (v.4.2.0).
Before and after the implementation of routine third trimester scan or POCUS, there were 16,777 and 7,351 births in SGH and 5,119 and 4,575 in NNUH, respectively. The rate of breech presentation in labour was consistent across all groups (3% to 4%). In the SGH cohort, the percentage of all term breech presentations that were undiagnosed was 14.2% (82/578) before (years 2016 to 2020) and 2.8% (7/251) after (year 2020 to 2021) the implementation of universal screening ( p < 0.001). Similarly, in the NNUH cohort, the percentage of all term breech presentations that were undiagnosed was 16.2% (27/167) before (year 2015) and 3.5% (5/142) after (year 2020 to 2021) the implementation of universal POCUS screening ( p < 0.001). Bayesian regression analysis with informative priors showed that the rate of undiagnosed breech was 71% lower after the implementation of universal ultrasound (RR, 0.29; 95% CrI 0.20, 0.38) with a posterior probability greater than 99.9%. Among the pregnancies with breech presentation, there was also a very high probability (>99.9%) of reduced rate of low Apgar score (<7) at 5 minutes by 77% (RR, 0.23; 95% CrI 0.14, 0.38). There was moderate to high probability (posterior probability: 89.5% and 85.1%, respectively) of a reduction of HIE (RR, 0.32; 95% CrI 0.0.05, 1.77) and extended perinatal mortality rates (RR, 0.21; 95% CrI 0.01, 3.00). Using informative priors, the proportion of all term breech presentations that were undiagnosed was 69% lower after the initiation of universal POCUS (RR, 0.31; 95% CrI 0.21, 0.45) with a posterior probability greater of 99.9%. There was also a very high probability (99.5%) of a reduced rate of low Apgar score (<7) at 5 minutes by 40% (RR, 0.60; 95% CrI 0.39, 0.88). We do not have reliable data on number of facility-based ultrasound scans via the standard antenatal referral pathway or external cephalic versions (ECVs) performed during the study period.
Conclusions
In our study, we observed that both a policy of routine facility-based third trimester ultrasound or POCUS are associated with a reduction in the proportion of term breech presentations that were undiagnosed, with an improvement in neonatal outcomes. The findings from our study support the policy of third trimester ultrasound scan for fetal presentation. Future studies should focus on exploring the cost-effectiveness of POCUS for fetal presentation.
Author summary
Why was this study done.
- Accurate knowledge of fetal presentation is essential for optimal care during pregnancy and birth. Vaginal breech delivery is associated with adverse maternal and perinatal outcomes.
- Abdominal palpation has poor sensitivity (50% to 70%) for determination of fetal presentation.
- The role of a routine third ultrasound assessment of fetal presentation has been reported but the impact on neonatal outcomes is yet to be determined.
- There are limited reports on antenatal use of handheld point-of-care ultrasound (POCUS) for the determination of fetal presentation, but the impact of their systematic use for this purpose is largely unknown.
What did the researchers do and find?
- We analysed 2 cohorts of pregnant women from 2 large teaching hospitals in the United Kingdom where a policy of routine third trimester ultrasound or POCUS has been implemented.
- We studied the impact of routine third trimester ultrasound or POCUS on the percentage of all term breech presentations that were undiagnosed and adverse neonatal outcomes, in pre- and post-screening epochs.
- Due to the rarity of adverse outcomes, we employed Bayesian regression analysis with informative priors. This statistical tool permits updating previous findings with new data to generate new evidence.
- We found that the incidence of all term breech presentations that were undiagnosed reduced drastically in the post-screening epoch following the implementation of either a third trimester ultrasound (decreased from 14.2% to 2.8%) or POCUS (decreased from 16.2% to 3.5%). There was an associated improvement in neonatal outcomes.
What do these findings mean?
- Our findings imply that a policy of either a third trimester ultrasound by sonographers or POCUS by trained midwives was effective in reducing the proportion of all term breech presentations at the time of birth that were undiagnosed and associated neonatal complications.
- Cost-effectiveness of POCUS needs to be explored further for feasibility of implementation on a wider scale for assessment of fetal presentation at term.
Introduction
The incidence of breech presentation at term is 3% to 4% [ 1 ]. Breech vaginal birth is associated with an increase in both perinatal mortality and morbidity as well as maternal morbidity [ 2 – 7 ]. Correct knowledge of fetal presentation at term is essential for providing optimum antepartum and intrapartum care. Women with breech presentation at term can be effectively counselled about their options—external cephalic version (ECV), planned vaginal birth, or elective cesarean birth—with their inherent risks and perceived benefits [ 1 ]. There is substantial evidence that clinical examination is not accurate enough for determination of fetal presentation, with unacceptably high rates of missed breech/noncephalic presentations at term [ 8 , 9 ].
There are 2 modalities to screen for fetal presentation at term, each with its advantages and disadvantages: routine third trimester ultrasound or point-of-care/portable ultrasound (POCUS). Currently, routine third trimester ultrasound is not recommended by the United Kingdom National Institute for Health and Care Excellence (NICE) in low-risk pregnancies due to insufficient clinical and cost-effectiveness evidence [ 10 , 11 ]. In the UK, the current practice is to perform an early pregnancy risk assessment followed by referral pathways for low-risk and high-risk women. These risks relate to maternal, fetal, and placental pathology but are unrelated to the risk of breech presentation at term. Women deemed to be at high risk are referred for an ultrasound scan at 28 weeks’ gestation for fetal biometry with or without additional follow-up ultrasound scans. Low-risk women are followed up with clinical assessment (serial measurement of symphysio-fundal height) and referred for third trimester ultrasound if fetal growth restriction is suspected or if it is difficult to perform clinical examination, as in women with high body mass index (BMI), multiple pregnancy, or multiple uterine fibroids, or there is clinical suspicion of noncephalic fetal presentation at term [ 12 – 14 ]. Emerging data from observational studies and a systematic review indicate that it is feasible to accurately diagnose fetal presentation at term by third trimester ultrasound, thereby reducing the proportion of all term breech presentations that were undiagnosed at the time of labour and birth [ 15 – 18 ]. The clinical end point of any study of the diagnosis of breech presentation at term would be an improvement in neonatal outcomes, associated with reduction in incidence of undiagnosed breech. Hitherto published literature, however, could not demonstrate a translation of increased antenatal diagnosis of breech presentation into a statistically significant improvement in neonatal outcomes, most likely owing to the rarity of adverse outcomes.
Most of the data on the use of POCUS in antenatal settings are from low-resource settings where there is inadequate access to ultrasound owing to both material and physical constraints; hence, the focus is on task-shifting of obstetric ultrasound from sonographers to primary care providers [ 19 , 20 ]. A recently published review reported improved diagnostic accuracy with POCUS compared to clinical examination only, for high-risk obstetric conditions including fetal malpresentation, albeit studies were heterogeneous and referred to varying standards [ 21 ]. The Society of Obstetricians and Gynaecologists of Canada identifies POCUS as a useful modality for timely determination of fetal presentation [ 22 ]. A retrospective criterion-based audit performed in one of our study hospitals demonstrated that the use of POCUS by midwives in the antenatal ward/labour ward was associated with identification of previously unrecognized breech presentation, thereby preventing inappropriate induction of labour [ 23 ]. A recent validation study of POCUS in obstetric care showed near perfect agreement for assessment of fetal presentation [95.6% agreement, Kappa −0.887, 95% CI (0.78 to 0.99)] when compared to routine ultrasound [ 24 ]. There is, however, scanty literature on the diagnostic accuracy of POCUS in antenatal care settings for assessment of fetal presentation, compared to standard antenatal care, i.e., routine abdominal palpation, with referral for ultrasound when there is clinical suspicion of breech presentation.
In our study, we aimed to compare the impact of routine third trimester ultrasound or POCUS with standard antenatal care, on the incidence of overall and proportion of all term breech presentations that were undiagnosed at term, and on the related adverse perinatal outcomes.
The study included data from St. George’s University Hospital NHS Foundation Trust (SGH) and Norfolk and Norwich University Hospital NHS Foundation Trust (NNUH). For both centres, pregnancies were grouped according to whether they received routine third trimester scan (SGH) or POCUS (NNUH).
Routine third trimester scan cohort
We included a cohort of pregnant women who gave birth between 4 April 2016 and 30 September 2021, at SGH, a large teaching hospital in South West London. The chosen starting point was the date when birth records were first systematically entered into the current electronic database. At SGH, a policy of routine third trimester (at 36 weeks) ultrasound scan by sonographers for all pregnant women has been implemented since January 2020; this includes assessment of fetal biometry, umbilical and middle cerebral artery Doppler, placental localization, amniotic fluid volume, and fetal presentation. Following a diagnosis of breech presentation during the ultrasound scan, women are counselled about their options: ECV, planned cesarean birth, or planned vaginal birth. If women declined ECV or if it was unsuccessful, they were offered elective cesarean delivery from 39 weeks of gestation. The population was divided into 2 study groups: Group 1 (women who were offered and accepted a routine third trimester scan) and Group 2 (women who received standard antenatal care in line with national guidance, without a routine third trimester scan).
POCUS cohort
The POCUS cohort included pregnant women from NNUH where a policy of routine POCUS at the 36-week antenatal visit was fully adopted from November 2020 following stage-wise implementation in 2016. The POCUS is performed by a midwife using Vscan Air (GE Healthcare). NNUH is a large teaching hospital with approximately 6,000 births per year, and approximately 250 midwives working across the hospital and community. We included 2 groups: a historical cohort of women who received routine care—abdominal palpation and referral for selective ultrasound on clinical suspicion of breech presentation (2015) and those who had POCUS at the 36- to 37-week visit (November 2020 to 2021). Through 2016 to November 2020, POCUS was variably used, either on the labour ward or via referral from community midwives, on clinical suspicion of noncephalic presentation, and these women were not included in this study.
Training of midwives for POCUS cohort
The midwives in NNUH underwent a structured 3-month training programme. The workshops consisted of daily handheld scanning sessions with an hour of dedicated lectures. The theoretical lectures were followed by practice on consenting women in the antenatal ward. All the trainee midwives maintained a competency logbook, detailing both successful and unsuccessful cases. Following the initial workshops, “midwife champions” were identified who were deemed competent or held other ultrasound qualifications and were suitable for cascade training. POCUS training was a part of preceptor ship training of newly qualified midwives, while midwives working in nonpermanent roles were supported and advised to work with one of the champions.
The primary outcome was the proportion of all term breech presentations that were undiagnosed. Undiagnosed breech presentation was defined as follows: (a) breech presentation after the onset of labour or rupture of membranes at term; and (b) breech presentation diagnosed immediately before commencing induction of labour. The secondary outcomes included mode of birth, gestational age at birth, birth weight, incidence of emergency cesarean section, and the following neonatal adverse outcomes: Apgar score <7 at 5 minutes, unexpected neonatal unit (NNU) admission, hypoxic ischemic encephalopathy (HIE) 1 to 3, and perinatal mortality (includes stillbirths and early neonatal deaths).
Women with multiple pregnancies, preterm birth <37 weeks, and congenital abnormalities were excluded. Pregnancies undergoing planned cesarean section for breech presentation were excluded from the analysis of the study outcomes, except for the neonatal outcomes. Maternal demographic characteristics, antenatal, intrapartum, and perinatal data were extracted from Euroking E3 maternity information system and Viewpoint database (ViewPoint 5.6.8.428, ViewPoint Bildverarbeitung GmbH, Weßling, Germany). Routinely collected clinical data were collated from electronic health records and were deemed not to require ethics approval or signed patient consent as per the Health Research Authority (HRA) decision tool.
Statistical analysis
Descriptive variables were compared with Wilcoxon-signed rank test, t test, or chi-squared test, where appropriate. An adequately powered analysis is not practically feasible due to rarity of adverse outcomes following breech delivery. Therefore, we employed a Bayesian approach using informative priors from a previous similar study; updating their estimates (prior) with our own data (likelihood) [ 18 ]. The association of undiagnosed breech presentation at birth with adverse perinatal outcomes was analyzed with Bayesian log-binomial regression models and reported as RR (risk ratios) with credible intervals (CrI). Informative priors ( N ~ μ, σ ) for population mean were derived from Salim and colleagues and a weakly informative prior (Student t , df = 3) for model intercept. Prior parameters were estimated by using the log-risk ratios and log-confidence intervals from Salim and colleagues, and in case an effect could not be estimated in the original study due to a no-event situation, we added a single event to the corresponding group and reestimated the risk ratios. Two Markov chains were run for 1,500 iterations after an initial 500 burn-in period. Posterior probabilities were calculated using the probability density function of normal distribution. A sensitivity analysis using flat priors (noninformative) was also undertaken to investigate the weight of informative prior on the posterior density. Number needed to treat for important outcomes was calculated using current population numbers without incorporating external data. Convergence was checked with trace plots. All analyses were conducted using R for Statistical Software (v.4.2.0) using “brms” and “its.analysis” packages [ 25 , 26 ]. This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline ( S1 STROBE Checklist).
Study cohorts
In the SGH cohort, there were 24,128 singleton pregnancies during the eligibility period, of which 16,777 births were before the introduction of universal third trimester ultrasound scan and 7,351 after. Baseline characteristics of included pregnancies are presented in Table 1 . Women who gave birth before universal ultrasound scan were significantly younger (33.2 versus 35.7 years, p < 0.001), had similar BMI (25.6 versus 25.7 kg/m 2 , p = 0.194) and multiparity rate (49.6% [8,316/16,777] versus 49.2% [3,617/7,351], p = 0.612) compared to those who gave birth after. There was a slight drop in the proportion of births that were in women from black, Asian, and minority ethnic (BAME) background (39.3% [6,588/16,777] versus 37.9% [2,785/7,351], p = 0.044). The index of multiple deprivation (IMD) quintiles were similar between the 2 epochs ( p > 0.05 for all quintiles; Table 1 ), as was the total number of breech presentations at the time of birth (3.4% [578/16,777] versus 3.4% [251/7,351], p = 0.953), including all diagnosed and undiagnosed cases. A comparison of the baseline characteristics, as well as the gestational age at delivery in weeks and mode of birth of pregnancies with breech presentation at birth in the study epochs before and after the introduction of universal 36-week ultrasound scan is shown in Table 2 . Pregnancies with breech presentation at term were significantly more likely to be delivered by elective cesarean section (76.9% [193/251] versus 60.7% [351/278], p < 0.001) after compared to before the implementation of the universal 36-week ultrasound scan. Emergency cesarean section was lower (17.1% [43/251] versus 30.8% [178/578], p < 0.001) after compared to before the implementation of the universal 36-week ultrasound scan. A similar trend was noted for vaginal breech delivery ( Table 2 ). The gestational age at birth was 39.1 weeks in both groups with a mean difference of 1 day. Although the difference was statistically significant, it would be deemed clinically inconsequential.
Comparison between the 2 groups was performed using Wilcoxon-signed rank test, t test (for continuous variables), or chi-squared test (for binary or categorical variables), where appropriate.
BAME, black, Asian, and minority ethnic; BMI, body mass index; IMD, index of multiple deprivation.
Comparison between the 2 groups was performed using Wilcoxon-signed rank test, t test, (for continuous variables), or chi-squared test (for binary or categorical variables), where appropriate.
# These categories are mutually exclusive.
BMI, body mass index; IMD, index of multiple deprivation.
The percentage of all term breech presentations that were undiagnosed was 14.2% (82/578) before and 2.8% (7/251) after the implementation of universal screening ( p < 0.001) ( Table 3 ). The rate of elective cesarean delivery was higher during the universal scan epoch (13.0% [959/7,351] versus 12.0% [2,019/16,777], p = 0.029), while the emergency cesarean rate was lower (12.9% [2,169/16,777] versus 11.5% [845/7,351], p = 0.029) compared to the previous epoch. The total number of vaginal breech births reduced from 29 per 10,000 births to 20 per 10,000 births, but this difference did not reach statistical significance ( p = 0.276). A regression discontinuity (interrupted time series) analysis showed significant variation in the number of undiagnosed breech presentations between 2 epochs (before and after universal ultrasound, p < 0.001) ( Fig 1 ).

Dotted line represents the fitted regression curve with splines.
*Weakly informative priors (N~μ,σ) for population mean and (Student t, df = 3) model intercept.
†Informative priors (N~μ,σ) for population mean was derived from Salim and colleagues and a weakly informative prior (Student t, df = 3) for model intercept.
CrI, credible interval; HIE, hypoxic ischemic encephalopathy; NE, not estimable; NNU, neonatal unit; RR, relative risk.
In the NNUH cohort, there were 9,694 singleton births during the eligibility period, of which 5,119 births were before the initiation of POCUS screening and 4,575 births after the complete implementation of POCUS. Women who gave birth before POCUS were significantly older (34.6 versus 31.6 years, p < 0.001) and had a lower BMI (25.6 versus 26.5 kg/m 2 , p < 0.001) than those who gave birth after. The percentage of all term breech presentations that were undiagnosed was 16.2% (27/167) before and 3.5% (5/142) after the implementation of universal POCUS screening ( p < 0.001) ( Table 4 ).
*Weakly informative priors ( N ~ μ, σ ) for population mean and (Student t , df = 3) model intercept.
†Informative priors ( N ~ μ, σ ) for population mean was derived from Salim and colleagues and a weakly informative prior (Student t , df = 3) for model intercept.
CrI, credible interval; HIE, hypoxic ischemic encephalopathy; NE, not estimable; NNU, neonatal unit; POCUS, point-of-care ultrasound; RR, relative risk.
Perinatal outcomes
We analysed the SGH cohort using Bayesian regression analysis with both flat (noninformative) and informative priors (Using data from Salim and colleagues) [ 18 ]. Regression with informative priors showed the percentage of all term breech presentations that were undiagnosed was 71% lower after the implementation of universal ultrasound (RR, 0.29; 95% CrI 0.20, 0.38) with a posterior probability greater than 99.9% ( Table 3 ). Among the pregnancies with breech presentation, there was also a very high probability (>99.9%) of reduced rate of low Apgar score (<7) at 5 minutes by 77% (RR, 0.23; 95% CrI 0.14, 0.38). There was moderate to high probability (posterior probability: 89.5% and 85.1%, respectively) of a reduction of HIE (RR, 0.32; 95% CrI 0.05, 1.77) and extended perinatal mortality rates (RR, 0.21; 95% CrI 0.01, 3.00). Analysis using flat priors (noninformative) also showed that the percentage of all term breech presentations that were undiagnosed was 74% lower (RR, 0.26; 95% CrI 0.10, 0.59) with very high posterior probability of 99.8%. The reduction in low Apgar scores was also observed in flat prior analysis that corresponded to a 65% reduction (RR, 0.35; 95% CrI 0.06, 1.42) with a moderate to high probability (89.8%). The number needed to scan to prevent one case of undiagnosed breech presentation was 255 (95% CI: 192 to 376).
We analysed the NNUH cohort using the same methods. Using informative priors, the proportion of all term breech presentations that were undiagnosed was 69% lower after the initiation of universal POCUS (RR, 0.31; 95% CrI 0.21, 0.45) with a posterior probability greater of 99.9% ( Table 4 ). There was also a very high probability (99.5%) of a reduced rate of low Apgar score (<7) at 5 minutes by 40% (RR, 0.60; 95% CrI 0.39, 0.88). Flat prior analysis also showed that undiagnosed breech presentation was lower by 80% (RR, 0.20; 95% CrI: 0.07, 0.51) with very high posterior probability of 99.9%. No inference could be made for HIE or extended perinatal mortality as there were no events in either period.
In our study, use of a policy of either routine third trimester scan or routine third trimester POCUS was associated with a significant reduction in the proportion of all breech presentations that were undiagnosed at term, when compared to standard antenatal care. Short-term adverse perinatal outcomes, including NNU admission and low Apgar scores, were significantly lower for the pregnancies with diagnosed breech presentation at term following a policy for screening by either routine third trimester scan or POCUS. Previous studies were unable to study perinatal outcomes due to their small numbers.
Our cohorts are derived from real-world data from 2 large teaching hospitals in the UK. Much of the previously reported literature on use of third trimester ultrasound for diagnosis of breech presentation is from research settings with a dedicated breech clinic and available expertise and skills for manoeuvres like ECV and vaginal breech births. Conclusions from research settings may not be generalizable to clinical settings and may be prone to bias. Furthermore, our study is the first to compare the impact of POCUS with routine antenatal care for diagnosis of fetal presentation. Routine ultrasound scan is effective at reducing the proportion of all term breech presentations that were undiagnosed, but the clinical impact of this change is hard to assess owing to the rarity of adverse outcomes [ 18 ]. We employed a Bayesian approach using both informative priors from similar studies and flat priors as a sensitivity analysis that allowed us to estimate the effect of universal ultrasound in probabilistic terms without depending on P values.
There are some limitations to our study. Firstly, we did not have reliable data on ECV for both our cohorts. The universal scan might have implications, not just for babies that were breech at birth (e.g., ECV could be performed, which could lead to not being breech and therefore not being included in the outcomes, or some other benefit, or indeed, theoretically, harm). Salim and colleagues included all babies diagnosed as breech. The method employed by Salim and colleagues also has drawbacks as it did not include those undiagnosed before the universal scan. Nevertheless, it is unlikely to have had a substantial impact on our results given the low acceptance and variable success rates. This is reflected in the almost identical incidence of overall (undiagnosed and diagnosed) breech presentation before and after screening. Salim and colleagues also reported no difference in the rates of overall breech presentations despite systematic use of ECV with acceptance rates of as high as 80% [ 18 ]. Secondly, the number of adverse neonatal outcomes such as extended perinatal mortality and HIE were not sufficient to estimate an effect in the NNUH cohort. Finally, the maternity records at NNUH were uploaded on electronic database only from April 2015. Therefore, reliable data on demographic parameters like BMI, ethnicity, and IMD were not available for the first quarter of 2015. These factors, however, are unlikely to influence the results.
Our findings of a reduction in the proportion of all term breech presentations that were undiagnosed at term after implementation of routine third trimester scan resonates with those of Salim and colleagues, who reported a reduction from 22.3% to 4.7% following the introduction of universal third trimester scan, compared to standard antenatal care [ 18 ]. Yet there are no published data from the UK on the impact of routine POCUS on the reduction of the percentage of all term breech presentations that were undiagnosed at term. Observational studies from Kenya [ 19 ], Uganda [ 27 ], and Guatemala [ 28 ] have reported that midwives who underwent focused basic obstetric ultrasound training for 3 to 8 weeks were able to identify fetal presentation with high sensitivity and specificity. The proportion of all term breech presentations that were undiagnosed at term, however, could not be eliminated in both cohorts, with 7 and 5 such cases in the routine third trimester scan and POCUS cohorts, respectively. Most of these cases were a consequence of spontaneous version to breech from cephalic presentation in multiparous women. Salim and colleagues also described spontaneous version to breech in multiparous women (76% of cases of undiagnosed breech) in their cohort. Wastlund and colleagues reported in their prospective cohort of 3,879 women that a policy of universal third trimester scan virtually eliminated undiagnosed breech presentations in labour [ 16 ]. It should, however, be noted that their cohort comprised of nulliparous women only in a strict research setting.
We also noted a significant improvement in short-term neonatal outcomes including low Apgar scores at 5 minutes and NNU admission. Salim and colleague demonstrated a nonsignificant improvement in short-term neonatal outcomes [ 18 ]. Although we were unable to demonstrate an effect on outcomes such as HIE and neonatal mortality, observational data from low-resource settings report a reduction in neonatal mortality when women were referred in a timely manner for fetal malpresentation [ 29 ].
Accurate knowledge of fetal presentation at term is crucial for optimal antenatal and intrapartum care. Both routine third trimester scan by a sonographer/clinician or use of POCUS by trained midwives can achieve this objective. Although evidence suggests that a planned breech vaginal birth may be offered after careful case selection and counselling, a large proportion of maternity units in the UK and worldwide lack skilled providers for vaginal breech births. Antenatal identification of breech presentation would allow healthcare providers to offer unbiased information such that pregnant women feel empowered to make an informed decision and have a positive birth experience. A meeting of the UK National Screening Committee (NSC) in March 2021 acknowledged that ultrasound for fetal presentation appears promising; however, the committee recommended that further work on screening for fetal presentation could not be commissioned at that time. The NSC agreed to add screening for fetal presentation to the recommendations list for reconsideration in 3 years’ time if significant evidence evolves in the interim [ 30 ]. Our findings add to that evidence base. A cost-effectiveness analysis study conducted in the UK showed that universal third trimester ultrasound would “virtually eliminate” the proportion of all term breech presentations that were undiagnosed and would be cost-effective if fetal presentation could be assessed at £19.80 pounds per woman or less [ 16 ]. A National Institute for Health Research (NIHR) Health Technology Assessment (HTA) review has suggested that handheld portable ultrasound can readily close this gap as a low-cost device that antenatal care providers like midwives could use for fetal presentation with minimal training [ 31 ]. The major obstacles to routine third trimester scan policy include the costs incurred, whereas a policy of using POCUS in community clinics and the labour ward by healthcare providers, after a short period of training, appears to be as effective as a policy of routine third trimester formal departmental ultrasound. Implementation of POCUS in the community for fetal presentation would also curtail indirect costs by reduction in referrals for facility-based ultrasound based on clinical suspicion, apart from also instilling a sense of empowerment among the care providers and satisfaction among pregnant women. The policy of POCUS was acceptable to pregnant women in our cohort who wanted to avoid nonessential hospital visits during the COVID-19 pandemic. A potential pitfall of the portable ultrasound cited when used in low-resource settings was dependence on internet coverage, which is unlikely to be a deterrent in the UK. Nonetheless, regular audits, ongoing training, and quality improvement measures should be in place to support community healthcare providers to ensure safe practice.
Our data suggest that a policy of either third trimester ultrasound or POCUS by healthcare providers could be effective in reducing the proportion of all term breech presentations that were undiagnosed at birth with an associated improvement in neonatal outcomes.
Supporting information
S1 strobe checklist, abbreviations, funding statement.
The author(s) received no specific funding for this work.
Data Availability
- PLoS Med. 2023 Apr; 20(4): e1004192.
Decision Letter 0
25 Aug 2022
Dear Dr Khalil,
Thank you for submitting your manuscript entitled "Impact of Point of Care Ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes" for consideration by PLOS Medicine.
Your manuscript has now been evaluated by the PLOS Medicine editorial staff and I am writing to let you know that we would like to send your submission out for external peer review.
However, before we can send your manuscript to reviewers, we need you to complete your submission by providing the metadata that is required for full assessment. To this end, please login to Editorial Manager where you will find the paper in the 'Submissions Needing Revisions' folder on your homepage. Please click 'Revise Submission' from the Action Links and complete all additional questions in the submission questionnaire.
Please re-submit your manuscript within two working days, i.e. by Aug 29 2022 11:59PM.
Login to Editorial Manager here: https://www.editorialmanager.com/pmedicine
Once your full submission is complete, your paper will undergo a series of checks in preparation for peer review. Once your manuscript has passed all checks it will be sent out for review.
Feel free to email us at gro.solp@enicidemsolp if you have any queries relating to your submission.
Kind regards,
Beryne Odeny
PLOS Medicine
Decision Letter 1
16 Nov 2022
Dear Dr. Khalil,
Thank you very much for submitting your manuscript "Impact of Point of Care Ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes" (PMEDICINE-D-22-02818R1) for consideration at PLOS Medicine.
Your paper was evaluated by a senior editor and discussed among all the editors here. It was also sent to independent reviewers, including a statistical reviewer. The reviews are appended at the bottom of this email and any accompanying reviewer attachments can be seen via the link below:
In light of these reviews, I am afraid that we will not be able to accept the manuscript for publication in the journal in its current form, but we would like to consider a revised version that addresses the reviewers' and editors' comments. Obviously we cannot make any decision about publication until we have seen the revised manuscript and your response, and we plan to seek re-review by one or more of the reviewers.
In revising the manuscript for further consideration, your revisions should address the specific points made by each reviewer and the editors. Please also check the guidelines for revised papers at http://journals.plos.org/plosmedicine/s/revising-your-manuscript for any that apply to your paper. In your rebuttal letter you should indicate your response to the reviewers' and editors' comments, the changes you have made in the manuscript, and include either an excerpt of the revised text or the location (eg: page and line number) where each change can be found. Please submit a clean version of the paper as the main article file; a version with changes marked should be uploaded as a marked up manuscript.
In addition, we request that you upload any figures associated with your paper as individual TIF or EPS files with 300dpi resolution at resubmission; please read our figure guidelines for more information on our requirements: http://journals.plos.org/plosmedicine/s/figures . While revising your submission, please upload your figure files to the PACE digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email us at gro.solp@enicideMSOLP .
We expect to receive your revised manuscript by Dec 07 2022 11:59PM. Please email us ( gro.solp@enicidemsolp ) if you have any questions or concerns.
***Please note while forming your response, if your article is accepted, you may have the opportunity to make the peer review history publicly available. The record will include editor decision letters (with reviews) and your responses to reviewer comments. If eligible, we will contact you to opt in or out.***
We ask every co-author listed on the manuscript to fill in a contributing author statement, making sure to declare all competing interests. If any of the co-authors have not filled in the statement, we will remind them to do so when the paper is revised. If all statements are not completed in a timely fashion this could hold up the re-review process. If new competing interests are declared later in the revision process, this may also hold up the submission. Should there be a problem getting one of your co-authors to fill in a statement we will be in contact. YOU MUST NOT ADD OR REMOVE AUTHORS UNLESS YOU HAVE ALERTED THE EDITOR HANDLING THE MANUSCRIPT TO THE CHANGE AND THEY SPECIFICALLY HAVE AGREED TO IT. You can see our competing interests policy here: http://journals.plos.org/plosmedicine/s/competing-interests .
Please use the following link to submit the revised manuscript:
https://www.editorialmanager.com/pmedicine/
Your article can be found in the "Submissions Needing Revision" folder.
To enhance the reproducibility of your results, we recommend that you deposit your laboratory protocols in protocols.io, where a protocol can be assigned its own identifier (DOI) such that it can be cited independently in the future. Additionally, PLOS ONE offers an option to publish peer-reviewed clinical study protocols. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols
Please ensure that the paper adheres to the PLOS Data Availability Policy (see http://journals.plos.org/plosmedicine/s/data-availability ), which requires that all data underlying the study's findings be provided in a repository or as Supporting Information. For data residing with a third party, authors are required to provide instructions with contact information for obtaining the data. PLOS journals do not allow statements supported by "data not shown" or "unpublished results." For such statements, authors must provide supporting data or cite public sources that include it.
We look forward to receiving your revised manuscript.
Philippa Dodd MBBS MRCP PhD
plosmedicine.org
-----------------------------------------------------------
Requests from the editors:
Please respond to all editor and reviewer comments detailed below, in full.
Please ensure that the study is reported according to the STROBE guideline, and include the completed STROBE checklist as Supporting Information. Please add the following statement, or similar, to the Methods: "This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline (S1 Checklist)." The STROBE guideline can be found here: http://www.equator-network.org/reporting-guidelines/strobe/ When completing the checklist, please use section and paragraph numbers, rather than page (or line) numbers.
Throughout, please ensure that all abbreviation are defined at first use
DATA AVAILABILITY STATEMENT
PLOS Medicine requires that the de-identified data underlying the specific results in a published article be made available, without restrictions on access, in a public repository or as Supporting Information at the time of article publication, provided it is legal and ethical to do so. Please see the policy at http://journals.plos.org/plosmedicine/s/data-availability and FAQs at http://journals.plos.org/plosmedicine/s/data-availability #loc-faqs-for-data-policy
The Data Availability Statement (DAS) requires revision. For each data source used in your study:
a) If the data are freely or publicly available, note this and state the location of the data: within the paper, in Supporting Information files, or in a public repository (include the DOI or accession number).
b) If the data are owned by a third party but freely available upon request, please note this and state the owner of the data set and contact information for data requests (web or email address). Note that a study author cannot be the contact person for the data.
c) If the data are not freely available, please describe briefly the ethical, legal, or contractual restriction that prevents you from sharing it. Please also include an appropriate contact (web or email address) for inquiries (again, this cannot be a study author).
Please revise your title according to PLOS Medicine's style. Your title must be nondeclarative and not a question. It should begin with main concept if possible. "Effect of" should be used only if causality can be inferred, i.e., for an RCT. Please place the study design ("A randomized controlled trial," "A retrospective study," "A modelling study," etc.) in the subtitle (ie, after a colon).
Please structure your abstract using the PLOS Medicine headings (Background, Methods and Findings, Conclusions). Please combine the Methods and Findings sections into one section, “Methods and findings”.
* Abstract Background:
Pleas provide the context of why the study is important. The final sentence should clearly state the study question.
* Abstract Methods and Findings:
Please ensure that all numbers presented in the abstract are present and identical to numbers presented in the main manuscript text.
Please include the study design, population and setting, number of participants, years during which the study took place, length of follow up, and main outcome measures.
Please quantify the main results with 95% CIs and p values.
Please include the important dependent variables that are adjusted for in the analyses.
Please include the actual amounts and/or absolute risk(s) of relevant outcomes (including NNT or NNH where appropriate), not just relative risks or correlation coefficients. (example for absolute risks: PMID: 28399126).
Please ensure you clearly report numerators and denominators used to derive percentages
Please revise your statistical reporting such that all numerical values are clearly defined for the reader. Please define CI, RR etc at first use
Please include a summary of adverse events if these were assessed in the study.
In the last sentence of the Abstract Methods and Findings section, please describe the main limitation(s) of the study's methodology.
* Abstract Conclusions:
Please expand the conclusion, in -keeping with the below comments:
Please address the study implications without overreaching what can be concluded from the data; the phrase "In this study, we observed ..." may be useful.
Please interpret the study based on the results presented in the abstract, emphasizing what is new without overstating your conclusions.
Please avoid vague statements such as "these results have major implications for policy/clinical care". Mention only specific implications substantiated by the results.
Please avoid assertions of primacy ("We report for the first time....")
AUTHOR SUMMARY
At this stage, we ask that you include a short, non-technical Author Summary of your research to make findings accessible to a wide audience that includes both scientists and non-scientists. The Author Summary should immediately follow the Abstract in your revised manuscript. This text is subject to editorial change and should be distinct from the scientific abstract. Please see our author guidelines for more information: https://journals.plos.org/plosmedicine/s/revising-your-manuscript#loc-author-summary
Please place this author summary, appropriately structured with bulleted point, under sub-headings (as detailed in our guidance)
METHODS and RESULTS
Please ensure you have clearly reported the number of participants dates of recruitment, and account for all methods used in your study.
Please define "lost to follow-up" as used in this study. Other reasons for exclusion should be defined.
Please define the length of follow up (eg, in mean, SD, and range).
Please indicate which, if any, factors have been adjusted for in your analyses
Did your study have a prospective protocol or analysis plan? Please state this (either way) early in the Methods section.
a) If a prospective analysis plan (from your funding proposal, IRB or other ethics committee submission, study protocol, or other planning document written before analyzing the data) was used in designing the study, please include the relevant prospectively written document with your revised manuscript as a Supporting Information file to be published alongside your study, and cite it in the Methods section. A legend for this file should be included at the end of your manuscript.
b) If no such document exists, please make sure that the Methods section transparently describes when analyses were planned, and when/why any data-driven changes to analyses took place.
c) In either case, changes in the analysis-- including those made in response to peer review comments-- should be identified as such in the Methods section of the paper, with rationale.
For all observational studies, we ask that in the manuscript text you clearly indicate:
(1) the specific hypotheses you intended to test,
(2) the analytical methods by which you planned to test them,
(3) the analyses you actually performed, and
(4) when reported analyses differ from those that were planned, transparent explanations for differences that affect the reliability of the study's results. If a reported analysis was performed based on an interesting but unanticipated pattern in the data, please be clear that the analysis was data-driven If analyses were performed in response to the peer review process, please clearly indicate this.
Throughout, we politely request that you be more nuanced in respect to statistical reporting.
Please provide the actual numbers of events for the outcomes, not just summary statistics or ORs.
Where you report percentages, please clearly report numerators and denominators used to derive them.
Please quantify main results with 95% CIs as well as p-values.
Where p-values are reported please detail the statistical tests used to determine them.
Please include appropriate captions which clearly detail the content of the tables, and which define numerical values contained within. Please ensure all abbreviations are also clearly defined for each table e.g., RR, CI, SGHG, NNUH, NE
Are any factors adjusted for in the analyses presented here? Please detail such factors in the appropriate caption and where adjusted analyses are presented, please also include the unadjusted analyses to help facilitate transparency of observational data reporting.
Please quantify main results reported in the tables with 95% CIs and p-values.
Please indicate in the captions the statistical tests used to determine p-values
Table 2 – suggest removing the second header row between the cohorts – I appreciate that this is to detail the difference in n numbers across the different cohorts but a lot of information is repeated, perhaps unnecessarily, to satisfy that specific requirement. Please revise the presentation of this table to improve accessibility to the reader
Please indicate where in the manuscript the tables should be placed
Please consider using a color palate that is accessible to those with color blindness (i.e., avoids the uses of red and/or green)
Please indicate where in the manuscript the figures should be placed
Please remove all subheadings from the discussion such that it reads as one continuous piece of prose ending in a one paragraph conclusion.
Please remove COI statement, funding statement and ethics statement from the end of the main manuscript and include only in the manuscript submission form.
Please remove the patient consent statement and incorporate with your ethics statement.
For in-text reference callouts, citations should be in square brackets, and preceding punctuation as follows: “…[1,2,3,4].” Please not the absence of spaces where more than one citation is reported.
In the reference list, where more than 6 authors contribute to a study please list the first 6 only followed by et al.
Please see our website for other reference guidelines https://journals.plos.org/plosmedicine/s/submission-guidelines#loc-references
Journal name abbreviations should be those found in the National Center for Biotechnology Information (NCBI) databases.
Comments from the reviewers:
Reviewer #1:
This study assesses the 'impact' of a universal third trimester ultrasound on breech presentation. It concludes, using 2 'before and after' cohorts from 2 different units introducing 2 different types of 3rd trimester scans, that undiagnosed breech presentation is significantly reduced, that the incidence of breech presentation stays the same, and that the incidence of low Apgar scores is significantly reduced.
The first two findings subsequent to a universal scan have been shown before in a single unit cohort previously published in Plos Medicine (salim et al) to which this papers refers, and from which the analysis takes 'informative priors'. The reduction in undiagnosed breech has been shown too, albeit in nulliparous women in research setting, also published in this journal (Wastlund et al) (also cited in this paper). The reduction in Apgar scores was not 'significant' in the Salim study, but with this, it is. That this is so when more data is used should not be considered a surprise: antenatal diagnosis allows more caesarean sections (I note overall numbers not changed but no analysis is specifically presented on cs rates for breech babies- see point below) for breech babies: caesarean sections for breech improve short term outcomes and, according to the term breech trial and huge cohorts from the Netherlands, death.
The methodology requires scrutiny by a statistical reviewer and I am not one. This means that I do not fully understand- and apologise for this- how, for instance, despite my point above, the paper concludes that 5 min Apgar scores <7 are reduced, when using a simple chi-squared test amalgamating numbers from Salim et al and from this paper I calculate a chi-square statistic of 2.2251; p= 0.14: i.e. still 'not significant' in lay terms.
Although I have outlined that antenatal diagnosis will have benefits, the abstract suggests to the uninitiated reader like me that the paper actually demonstrates a reduction in HIE: 'There was moderate to high probability (posterior probability: 89.5% and 85.1%, respectively) of a reduction of hypoxic ischemic encephalopathy (HIE) (RR: 0.23, 95% CI: 0.14-0.38)… '. Yet this is not the case, the numbers simply being inadequate for this: table 2 shows just 2 before and 1 after the scan was introduced. Without fully understanding the methodology this seems disingenuous.
Another issue with this paper is the loss of the 'real world' (what happens in a unit when…) benefits to an impact/ 'changes subsequent to' paper. This is because of there being 2 different units, the intervention was slightly different (proper scan and presentation scan) and ECV was not documented/ discussed. This means it potentially has less relevance for a 'unit' and is more of a 'poor man's' (person's) RCT.
I remain surprised at all the research into a universal 'presentation only' scan. I think we know the answer- most breeches become diagnosed. This affects only about 5% of the population. Given the (accepted) benefits of elective caesarean for breech babies have probably been exaggerated (RCOG Greentop Guideline 2017) the overall effect on pregnancy safety is going to be small. And of course performing caesarean sections on all breech babies leads to a loss of skills and therefore probably increased risk for the small (in this study and that of Salim et al) but persistent breeches that still slip through. I make this comment because this pertains to the relevance of this- and other studies such as Salim et al- for overall pregnancy safety; in contrast, a 'proper' scan that could affect the other 95% as well is the one that needs the research attention.
I would like to see data on how many third trimester scans were actually performed- before and after.
No table data on gestation at birth or mode of birth is presented for the babies who were actually breech.
The lack of ECV data is acknowledged as a limitation but inadequately so. The Salim study they quote was not a 'research setting' and its data and discussion of ECV was comprehensive. This lack also causes the problem below:
By looking at outcomes in breech babies only at birth (this is not 100% clear at least in the table) an assumption is being made that the universal scan could not alter outcomes for other babies. It could- not just for babies that were breech at birth (eg ECV could be performed which could lead to not being breech and therefore not being included in the outcomes, or some other benefit, or indeed, theoretically, harm). Salim et al 'get around' this by including all babies diagnosed as breech. The method employed by Salim et al has drawbacks too (it did not include those undiagnosed before the universal scan), but the method used here should at least be justified and discussed as a limitation.
The pretty Figs 1 and 2 add little useful information bar perhaps demonstrating causality better re undiagnosed breech presentation- but this should be obvious by now.
In spite of my largely minor reservations, if this stands up to statistical review, this paper cleverly demonstrates one of the benefits to spreading the use of ultrasound in pregnancy.
Reviewer #2: This was a clinically meaningful study, well-written and generally easy to follow. The conclusions are clear and compelling. The role of midwives in delivering POCUS is especially unique and helpful given the potential for this model to be introduced more widely in clinical settings globally. The use of probabilities in the results is confusing to follow, the risk reduction is much easier to understand clinically, however these results are presented in the context of the analysis conducted.
The only suggested changes relate to the interpretation of findings. In the Discussion, I think it is important to clearly mention a) the role of mode of birth in the risk of neonatal adverse outcomes (ie what proportion of women with breech babies proceeded to CS and thus what was the impact of MOB on outcomes, if any, assuming that CS eliminates most of the breech-related risks of vaginal breech birth) and b) the role of parity or the proportion of multiparous women in each group.
Reviewer #3: 1. Line 120-122. "For both centers, pregnancies were grouped according to whether they received routine third-trimester scan (SGH) or POCUS (MNUH)." For the analysis, did the author include all the pregnancies or just include those received routine third-trimester scan at SGH or PROCUS at MNUH?
2. What's the reason for only including SGH cohort was in Table 1/Figure 1 ? How about the NNUH cohort?
3. As the log-binomial regression is used to analyze the association between undiagnosed breach presentation at birth and adverse perinatal outcomes, should the outcome be OR (odds ratio) rather than RR (relative risk?)
Reviewer #4: Thanks for allowing me to review your very interesting manuscript. I agree that the data presented show an impressive reduction in the chance of an undiagnosed breech presentation at term after both routine ultrasound screening and POCUS, carried out in two different hospitals. It would, of course, be a more rigorous study design to compare routine antenatal care with both routine ultrasound and POCUS in the same setting, or to have randomised rather than use a before and after design, but based on your data both methods appear to reduce the percentage of breech presentations that are undiagnosed at the start of labour or membrane rupture. I have a few minor points to make which could lead to some minor revisions:
1. I found the phrase 'the rate of undiagnosed breech' a bit confusing as it suggested to me that, for example, 14.2% of babies were presenting in labour as undiagnosed breeches. It might be better to say the 'percentage of all term breech presentations that were undiagnosed was 14.2%.....'
2. The statement that there was no significant change in the rate of vaginal breech birth (and the figures are given of 10 per 10,000, which was reducing to 5 per 10,000 after the scanning interventions) is somewhat surprising given the very significant change (reduction) in the percentage of undiagnosed breech presentations. Are you able to explain that?
3. These data would suggest to me that prior to the intervention most breech babies were born by c/section, so it is then a little hard to understand how such an improvement in perinatal outcome has been achieved. I realise that the outcome data were secondary outcomes but the paper seems to argue that there is a high rate of morbidity/mortality associated with vaginal breech birth, yet the improvement in perinatal outcomes has occurred without much change in the rate. Indeed, given the numbers quoted the numbers of term vaginal births at SGH during the study period would have reduced from about 17 in the pre-ultrasound period to 4 after. To have seen a measurable reduction in the rate of low Apgar scores and rates of HIE would be remarkable, and would imply that outcomes for vaginal breeches were very poor in the pre-ultrasound period. Can you comment further on this?
3. A minor point is that data is a plural noun and is sometimes used as a singular one (e.g. page 172)
4. Finally, I was left uncertain as to whether or not you would advocate a policy of routine ultrasound or POCUS or a hybrid of the two depending on risk? Or do you have plans to compare the two approaches in the same setting?
Any attachments provided with reviews can be seen via the following link:
Author response to Decision Letter 1
Submitted filename: PLOS medicine reviewers Asma 27.12.2022.docx
Decision Letter 2
19 Jan 2023
Thank you very much for re-submitting your manuscript "Impact of Point of Care Ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: a retrospective study" (PMEDICINE-D-22-02818R2) for review by PLOS Medicine.
I have discussed the paper with my colleagues and the academic editor and it was also seen again by 4 reviewers. I am pleased to say that provided the remaining editorial and production issues are dealt with we are planning to accept the paper for publication in the journal.
The remaining issues that need to be addressed are listed at the end of this email. Any accompanying reviewer attachments can be seen via the link below. Please take these into account before resubmitting your manuscript:
In revising the manuscript for further consideration here, please ensure you address the specific points made by each reviewer and the editors. In your rebuttal letter you should indicate your response to the reviewers' and editors' comments and the changes you have made in the manuscript. Please submit a clean version of the paper as the main article file. A version with changes marked must also be uploaded as a marked up manuscript file.
Please also check the guidelines for revised papers at http://journals.plos.org/plosmedicine/s/revising-your-manuscript for any that apply to your paper. If you haven't already, we ask that you provide a short, non-technical Author Summary of your research to make findings accessible to a wide audience that includes both scientists and non-scientists. The Author Summary should immediately follow the Abstract in your revised manuscript. This text is subject to editorial change and should be distinct from the scientific abstract.
We expect to receive your revised manuscript within 1 week. Please email us ( gro.solp@enicidemsolp ) if you have any questions or concerns.
We ask every co-author listed on the manuscript to fill in a contributing author statement. If any of the co-authors have not filled in the statement, we will remind them to do so when the paper is revised. If all statements are not completed in a timely fashion this could hold up the re-review process. Should there be a problem getting one of your co-authors to fill in a statement we will be in contact. YOU MUST NOT ADD OR REMOVE AUTHORS UNLESS YOU HAVE ALERTED THE EDITOR HANDLING THE MANUSCRIPT TO THE CHANGE AND THEY SPECIFICALLY HAVE AGREED TO IT.
Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript.
Please note, when your manuscript is accepted, an uncorrected proof of your manuscript will be published online ahead of the final version, unless you've already opted out via the online submission form. If, for any reason, you do not want an earlier version of your manuscript published online or are unsure if you have already indicated as such, please let the journal staff know immediately at gro.solp@enicidemsolp .
If you have any questions in the meantime, please contact me or the journal staff on gro.solp@enicidemsolp .
We look forward to receiving the revised manuscript by Jan 26 2023 11:59PM.
Philippa Dodd, MBBS MRCP PhD
------------------------------------------------------------
Requests from Editors:
Thank you for your detailed and considerate responses to previous editor and reviewer comments. Please see below for further comments that we require you respond to in full.
Thank you for revising your title suggest “Impact of Point of Care Ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: an observational multi-centre cohort study” or something similar
Thank you for revising your abstract and for including p-values as well as 95% CIs. For each outcome measure reported we request that both p-values and 95% CIs are reported. If not please clearly state the reasons why not, for purposes of transparent data reporting (please remember that when reporting p-values to report as p<0.001 or where higher the exact p-value as p= 0.002, for example).
Suggest reporting as follows – for example, line 59 - (RR: 59 0.29, 95% CI [0.20–0.38], p<0.001) for optimal reader accessibility.
Please note the use of parentheses around the CIs and the absence of the semi-colon. You may wish to consider separating upper and lower limits with commas rather than hyphens (as these can be confused with negative values) but we leave it to your discretion.
Please check and revise throughout, including in the main manuscript text and tables where relevant – please see below also
Thank you for including an author summary which reads very nicely.
Line 100: we appreciate the explanation of your chosen methodological approach, suggest revising to ensure that the statement is interpretable to the more general reader – some may be unfamiliar with the concept of informative priors, for example
Line 103: “incidence of percentage…” suggest removing of percentage perhaps?
Line 104: suggest quantifying “drastically (a percentage will be adequate here)
Line 113: It would be helpful to elaborate on the reasons why assessing cost-effectiveness is necessary – i.e. for feasibility of implementation on a wider scale
Please revise statistical reporting as suggested above
please quantify all reported percentages with numerators and denominators, for example line 271, “(12.9 vs 11.5%, p=0.029)” - please check and amend throughout
Please also report CIs where p-values are reported, if not please clearly state why not, for purposes of transparent data reporting
Currently journal requirements stipulate that where 95% CIs are presented, including in tables, that p-values are also reported. Please include p-values but if not in your rebuttal letter, please clearly state the reasons why not, for transparency of data reporting
Table 3.a – suggest removing the SGH cohort row – perhaps a remnant of the previous version
Please remove the sub-heading conclusion.
Line 404: given the observational nature of the study suggest tempering the language here slightly, “Our data suggest that a policy….could be effective in…” or something similar, for example
SOCIAL MEDIA
To help us extend the reach of your research, please provide any Twitter handle(s) that would be appropriate to tag, including your own, your co-authors’, your institution, funder, or lab. Please include these in the manuscript submission form when you re-submit your manuscript
Comments from Reviewers:
Reviewer #1: the authors have addressed all points satisfactorily
Reviewer #2: Thank you for your thorough attempts to rectify requested changes. The manuscript has been satisfactorily updated and improved.
Reviewer #3: I appreciate authors' effors in addressing the questions and revising the paper. I have no further comments.
Reviewer #4: Thanks for responding to my previous comments and to those of other reviewers. I have three relatively minor additional points to make about your revised manuscript;
1. Line 50 (Abstract). Can you confirm that the statement 'the rate of breech presentation in labour was consistent across all groups (3-4%)' is correct and does this refer to all births? It seems very high if the usual exclusions of preterm, multiples, congenital anomalies are applied.
2. Line 116 (Introduction). Similarly, is this figure of 3-4% used in the Introduction inclusive of all births, and does it exclude multiple pregnancies?
3. Line 175. I would think that 'Southwest London' is usually written as 'South West London' but as I am not a resident of London I am happy to be corrected.
Author response to Decision Letter 2
29 Jan 2023
Submitted filename: PLoS reviewers comments 21.01.2023 Asma.docx
Decision Letter 3
Dear Dr Khalil,
On behalf of my colleagues and the Academic Editor, Dr. Anthea C Lindquist, I am pleased to inform you that we have agreed to publish your manuscript "Impact of Point of Care Ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: an observational multi-centre cohort study" (PMEDICINE-D-22-02818R3) in PLOS Medicine.
Prior to publication, on advice of the Academic Editor, whose comments are also included below, we require that you make the following final revisions:
This is an important study with direct clinical impact and will be of great interest to maternity clinicians globally.
The suggested revisions have generally been very appropriately addressed or appropriately rebutted. There are a few remaining issues to address:
Line 103 - wording doesn't make sense, needs to be clarified
Line 222 - 'excluding' should be 'excluded'
Line 226 - 'was' should be 'were' in keeping with the plural nature of data
Line 270-271 - reads as though the GA was the same (39.1 weeks) between groups but still significantly different - needs to be clarified, how can this differ?
Table 2 - mode of birth - needs to include in legend if all 3 breech vaginal birth categories (breech extraction, breech with forceps and spontaneous breech) were mutually exclusive or not? The same babies could all feasibly be included in all groups.
Line 317-318 - 'term' is used twice, only one is necessary
Line 328 - should read 'the first'
Line 331 - should read 'the rarity'
Line 349 - 'was not' should read 'were not' owing to plural data
Line 359-360 - 'term' is used twice, only needed once
Line 371 - remove 'the' from 'the neonatal'
Before your manuscript can be formally accepted you will need to complete some formatting changes, which you will receive in a follow up email. Please be aware that it may take several days for you to receive this email; during this time no action is required by you. Once you have received these formatting requests, please note that your manuscript will not be scheduled for publication until you have made the required changes.
In the meantime, please log into Editorial Manager at http://www.editorialmanager.com/pmedicine/ , click the "Update My Information" link at the top of the page, and update your user information to ensure an efficient production process.
We frequently collaborate with press offices. If your institution or institutions have a press office, please notify them about your upcoming paper at this point, to enable them to help maximise its impact. If the press office is planning to promote your findings, we would be grateful if they could coordinate with gro.solp@sserpenicidem . If you have not yet opted out of the early version process, we ask that you notify us immediately of any press plans so that we may do so on your behalf.
We also ask that you take this opportunity to read our Embargo Policy regarding the discussion, promotion and media coverage of work that is yet to be published by PLOS. As your manuscript is not yet published, it is bound by the conditions of our Embargo Policy. Please be aware that this policy is in place both to ensure that any press coverage of your article is fully substantiated and to provide a direct link between such coverage and the published work. For full details of our Embargo Policy, please visit http://www.plos.org/about/media-inquiries/embargo-policy/ .
Thank you again for submitting to PLOS Medicine, it has been a pleasure handling your manuscript. We look forward to publishing your paper.
Best wishes,
Philippa Dodd, MBBS MRCP PhD

IMAGES
VIDEO
COMMENTS
During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks.
Women in the selective ultrasound scan arm only received an ultrasound scan after detection of a breech presentation by abdominal palpation. Where a breech was detected, a woman was offered external cephalic version (ECV). The structure of the model undertook a decision tree, with end states being the mode of birth; either vaginal, elective or ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
However, we felt that it was appropriate to reveal the presentation at the time of the 36-wkGA scan, as there is level 1 evidence that planned cesarean delivery reduces the risk of perinatal morbidity and mortality in the context of breech presentation at term . Another weakness was that the study was being undertaken in a single centre only ...
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
"Breech in the third trimester" was a surrogate definition created to allow neonatal outcome data to take account of the risks of ECV as well as being breech presentation at birth. It was defined as breech presentation at birth, or at any scan from 35+0 weeks or where a successful ECV had been performed.
Investigations. An ultrasound scan is diagnostic for breech presentation. Growth, amniotic fluid volume and anatomy should be assessed to check for abnormalities. Management. There are three management options for breech presentation at term, with consideration of maternal choice: external cephalic version, vaginal delivery and Caesarean section. External cephalic version
Breech presentation: clinical practice guideline from the French College of Gynaecologists and Obstetricians [2020] ... The model of care allows the team to increase their level of skill over a relatively short time, improving the safety of the breech births they attend while receiving specialist support [Spillane E.
Diagnosis: preterm ≤36+6 weeks. Breech presentation is a normal finding in preterm pregnancy. If diagnosed at the 35-36 week antenatal visit, refer the woman for ultrasound scan to enable assessment prior to ECV. Mode of birth in a breech preterm delivery depends on the clinical circumstances.
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of births at term.
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or ...
For universal ultrasound, we assumed that all breech presentations at the time of scanning would be detected (i.e., assumed 100% sensitivity and specificity for the test). For selective ultrasound, the breech presentation was diagnosed either clinically (by abdominal palpation followed by ultrasound for confirmation) or as an incidental finding ...
Breech presentation was diagnosed in 179 (4.6%) of these women at the 36-week scan. In most ( n = 96) of those women, there was no prior suspicion that the presentation was not cephalic. External cephalic version was offered to all women for whom this was appropriate and was attempted in 84 (46.9%).
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed ... All pregnant women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36 +0; weeks ; Intervention ; Cephalic version by the following listed interventions will be considered:
Introduction. Breech presentation has an incidence at term of 3% to 4% and is more common among preterm births [].Vaginal breech birth has been associated with higher neonatal morbidity and mortality than cesarean (CS) [] or cephalic birth.In an attempt to reduce birth-related complications, most breech babies are delivered by CS and thus breech babies make a substantial contribution to CS ...
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position. Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech ...
To determine whether congenital anomalies are associated with breech presentation at the time of birth. A population-based, retrospective cohort study was conducted among 460 147 women with ...
The main aim of the Presentation Scan (or Pre Delivery Scan) is to diagnose breech position or other abnormalities in the baby's position. We also perform thorough checkup of fetal growth and estimate fetal weight. We assess fetal wellbeing by umbilical artery and middle cerebral artery Dopplers. Normally, a few weeks prior to birth, the baby ...
Breech presentation at birth is an established risk factor for DDH and is hypothesized to be secondary to mechanical forces on the hips during the third trimester (22,27). The correlation between length of time spent in the breech position in utero and DDH is less understood. In this study, breech referred to position at the time of delivery.
A breech presentation occurs when the fetus is lying longitudinally, and its buttocks or feet will be positioned to be delivered first. It happens in approximately 1 out of 25 full-term births. The probability of breech presentation decreases with the increase in gestational age (a measure of the age of a pregnancy taken from the beginning of a ...
Background. Accurate knowledge of fetal presentation at term is vital for optimal antenatal and intrapartum care. The primary objective was to compare the impact of routine third trimester ultrasound or point-of-care ultrasound (POCUS) with standard antenatal care, on the incidence of overall and proportion of all term breech presentations that were undiagnosed at term, and on the related ...