An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- MedEdPORTAL


Maternal-Fetal Physiology, Intrapartum Care, Postpartum Care: A Team-Based Learning Module for Normal Obstetrics
Lindsey b. sward.
1 Assistant Professor, Department of Obstetrics and Gynecology, University of Arkansas for Medical Sciences College of Medicine
Sara G. Tariq
2 Professor, Department of Internal Medicine, University of Arkansas for Medical Sciences College of Medicine
3 Assistant Dean of Undergraduate Clinical Education, University of Arkansas for Medical Sciences College of Medicine
Associated Data
B. RAT Instructor Version.docx
C. Application Exercise Instructor Guide.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Introduction
Team-based learning (TBL) is an active learning strategy used at the University of Arkansas for Medical Sciences in both the preclinical and clinical years of medical school. The Department of Obstetrics and Gynecology (OB/GYN) uses TBLs during a 6-week clinical clerkship. This TBL is the first in a series of six and was designed to teach the topic of normal obstetrics to third-year medical students.
Prior to the TBL, students were provided with learning objectives and a list of advance preparation resources. These resources included a reading assignment from the student textbook, as well as optional online videos and optional online interactive quizzes. The students then came to class and completed an individual readiness assurance test (iRAT) and a group readiness assurance test (gRAT). The majority of in-class time was spent working through complex application exercises in the form of case vignettes. The TBLs were facilitated by a faculty member in the OB/GYN department.
Since its initiation in June 2018, 93 students have participated in this TBL activity. The mean score on the iRAT was 88.9%, and the mean score on the gRAT was 98.8%. Ninety-eight percent of students reported that they were satisfied with this learning activity.
This TBL was well received by students and unique in that it utilized a variety of types of advance preparation resources. With few other published OB/GYN TBLs available, we believe that this module could be a valuable resource for OB/GYN clerkships.
Educational Objectives
By the end of this activity, learners will be able to:
- 1. Identify signs and symptoms associated with maternal physiologic changes of pregnancy, focusing on those related to the cardiovascular, respiratory, and hematologic systems.
- 2. Apply knowledge of the four stages of labor to clinical decision-making.
- 3. Interpret electronic fetal heart rate monitoring by describing fetal heart rate baseline, variability, and presence of decelerations.
- 4. Discuss normal anatomic and physiologic changes in the postpartum period (uterine involution, lochia, return of ovarian function, cardiovascular changes, breast changes).
- 5. Differentiate between postpartum blues, postpartum depression, and postpartum psychosis.
Obstetrics and gynecology (OB/GYN) is a diverse discipline that integrates preventive medicine, complex problem solving, and surgical intervention. Despite the complexity of the field, it is often relegated to a shorter clerkship length in medical school curricula. 1 This makes planning of didactic sessions for students on the OB/GYN clerkship especially difficult, as these sessions must cover a significant amount of varied material over a short amount of time.
This team-based learning (TBL) activity was developed as the first in a series of six TBLs for a 6-week OB/GYN clerkship. It was designed to teach normal obstetrics—encompassing maternal and fetal physiology, intrapartum care, and postpartum care—to third-year medical students at the University of Arkansas for Medical Sciences (UAMS).
TBL is an active learning strategy that has been used in medical schools throughout the United States since 2001. 2 TBL is characterized by three components—preparation in advance by the students, individual readiness assurance tests (iRATs) and group readiness assurance tests (gRATs), and the majority of in-class time spent focusing on application assignments. 2 , 3 TBL has been shown to have a positive impact on the learning of medical students. 4 Despite the noted benefits of TBL, there is a paucity of data on the use of TBL in OB/GYN clinical clerkships. 5 A search of MedEdPORTAL revealed only six TBL activities specifically related to the field of OB/GYN. 6 – 11
In comparing this TBL activity to the other six published in MedEdPORTAL , only one of them, “Post-Partum Depression: Diagnosis, Screening, and Treatment,” by Freerksen, Brooks, and Siddiqui, 8 contains overlapping content. There are no published TBLs covering the topics of maternal and fetal physiology, basic intrapartum care, or comprehensive postpartum care. In contrast to the other published TBLs, this TBL activity utilizes a variety of different modes of advance preparation resources, whereas the other OB/GYN TBLs use textbook reading only. 6 – 11 Finally, this TBL activity uniquely incorporates a significant amount of basic science into a clinical clerkship curriculum, with a focus on maternal and fetal physiology and maternal physiologic changes during the puerperium.
Curricular Context
Although the OB/GYN clerkship at UAMS has used TBL since 2007, 6 , 7 a new TBL series was developed and instituted in June 2018. This TBL was the first in the new six-part series of TBLs given over a 6-week OB/GYN clerkship. Medical students at our institution were familiar with the TBL model of active learning as they had completed several TBLs during their preclinical years. The class size at UAMS at the time of the initiation of this TBL was 174 students. Third-year medical students rotated through their OB/GYN clerkship in groups ranging on average from 18 to 24 students.
In our OB/GYN clerkship, TBL in its entirety accounted for 20% of the student's grade. This module, as one of six TBLs, corresponded to approximately 3.3% of the final clerkship grade.
Team Formation
At the beginning of each new clerkship, we randomly divided students into four different teams of five to seven students. These teams remained unchanged throughout the 6 weeks of the OB/GYN clerkship but were not consistent with teams in which students may previously have been placed in other courses.
Description of Advance Preparation Resources
We sent the students their TBL learning objectives and a list of advance preparation resources 1 week prior to the TBL activity. The preparatory assignment for this TBL included a review of chapters in their textbook, Obstetrics and Gynecology, seventh edition. 12 Students were asked to read chapter 5 (“Maternal-Fetal Physiology”), chapter 8 (“Intrapartum Care”), and chapter 11 (“Postpartum Care”) in their entireties. They were also asked to read only the portion of chapter 9 (“Abnormal Labor and Intrapartum Fetal Surveillance”) regarding intrapartum fetal surveillance. All items tested on the readiness assurance tests could be answered using the textbook reading alone.
We also encouraged the students to watch optional online videos produced by the Association of Professors of Gynecology and Obstetrics (APGO) 13 that corresponded to the aforementioned chapters. The videos, 5- to 10-minute educational videos on various OB/GYN topics, were entitled Medical Student Educational Objectives and could be accessed on YouTube. For this TBL, the videos that corresponded to the reading material were topics 8 (Maternal-Fetal Physiology), 11 (Intrapartum Care), 13 (Postpartum Care), 14 (Lactation), 26 (Intrapartum Fetal Surveillance), and 29 (Anxiety and Depression).
We also recommend that the students complete the optional corresponding APGO online quizzes, called uWISE objectives. 14 These quizzes were part of an online question bank to which our department had purchased a subscription. The question bank could be accessed, free of charge, by any student on our clerkship. The recommended uWISE objectives for this TBL were 8 (Maternal-Fetal Physiology), 11 (Intrapartum Care), 13 (Postpartum Care), 14 (Lactation), 26 (Intrapartum Fetal Surveillance), and 29 (Anxiety and Depression). Although completion of the uWISE objectives was not required for the TBL, we did award students a small completion grade at the end of the OB/GYN clerkship for completing all recommended uWISE objectives.
Description of the Readiness Assurance Process
Students began the TBL by taking an iRAT ( Appendix A ). The iRAT was a 10-item multiple-choice quiz, given as a closed-book, closed-note quiz. We did not grade the iRAT prior to the students’ taking the gRAT. The students next broke into their teams to take the gRAT, which was the same 10-item multiple-choice quiz that they had been given for the iRAT ( Appendix A ). The TBL facilitator, who was a faculty member in the OB/GYN department and also a content expert, graded each gRAT upon its completion using a key ( Appendix B ). The facilitator gave immediate verbal feedback to the team about which items had been missed. Although we used a paper examination and key at our facility for financial reasons, we recognize that Immediate Feedback Assessment Technique cards 15 could easily be adopted into this TBL activity.
Teams were allowed to use their textbooks or other materials to appeal questions. Questions were able to be appealed on the basis of poor or ambiguous wording or if the team believed that the answer was incongruent with information provided in the advance preparation materials. The teams were required to give appeals in writing for the faculty facilitator to review. Appeals could be written only by teams, not by individual students, and had to be turned into the faculty facilitator for review within 5 minutes of the grading of the gRAT.
After the gRAT was completed and any appeals reviewed, the TBL facilitator clarified difficult or poorly understood concepts with the students.
Description of Team Application Activities
There were four application exercises in this TBL module ( Appendix C ), each designed according to the 4S principles of significant problem, same problem, specific choice, and simultaneous reporting. 2 These exercises were structured as clinical vignettes with corresponding multiple-choice questions. Students worked in their groups to answer these complex clinical vignettes and were allowed to use a variety of resources, including textbooks and online components. Teams were asked to commit to an answer via simultaneous reporting. 3 We conducted simultaneous reporting by having each team hold up a laminated card labeled A, B, C, D, or E corresponding to its answer. The facilitator then discussed the questions and answers with the groups.
Facilitation Schema
This TBL was designed as a single, 90-minute educational session. The following is a suggested facilitation time line:
- • Welcome and learning objectives (2-3 minutes).
- • iRAT (15 minutes).
- • gRAT (10 minutes).
- • Appeals, clarification of difficult concepts (15 minutes).
- • Application exercises (45 minutes).
Third-year medical students beginning in June 2018 participated in this TBL activity, with a total of 93 participants. The mean iRAT score on this TBL activity was 88.9%, with a minimum score of 50% and a maximum score of 100%. The median IRAT was 90%. The mean gRAT score was 98.8%, with all groups scoring either 90% or 100%.
Application exercises were not scored but were for discussion only. Although application exercise number 4 was almost universally agreed upon by all groups, there was more discussion regarding application exercise numbers 1-3, with groups typically being divided between two answer choices.
After participating in the TBL, students were sent an optional anonymous survey by email. The survey polled students on resources used and amount of time spent studying. The survey's response rate was 66% (61 out of 93 students). When students were asked which resources—reading, APGO videos, and uWISE objectives—they used to prepare for the TBL, 97% said they used the APGO videos, 74% said they used the uWISE objectives, and 67% said they used some or all of the reading. When asked which resources they found helpful for the TBL (with the ability to choose more than one resource type on the survey), 47% said they found the reading helpful, 75% said they found the APGO videos helpful, and 33% said they found the uWISE objectives helpful. The students polled spent 4 hours on average preparing for the TBL.
Students formally evaluated this TBL activity using a standard evaluation form utilized for all lectures and educational activities in the UAMS College of Medicine curriculum. The evaluation was voluntary and was scored on a 5-point Likert scale (1 = strongly disagree , 2 = disagree , 3 = neither agree nor disagree , 4 = agree , 5 = strongly agree ). On an evaluation item stating, “Instructor provided learning material that was appropriate and well-organized, defined the learning objectives well, emphasized the stated objectives, presented lectures in an organized fashion, summarized major points, and illustrated relationships among topics,” 98% (50 out of 51 students) completing evaluations rated this TBL either a 4 or a 5. Of those, 94% (48 out of 51 students) rated it a 5. There were a total of 19 open-ended student responses from the evaluations, all of which were positive in nature. Select student comments regarding the TBL activity included: “So organized, energizing, and helpful”; “The topics were covered very well, and I left feeling much more confident in being able to know the topics when seen in clinicals”; and “The TBL format encourages student involvement. I think most didactic sessions for the M3 year could improve by taking tips from [this instructor].”
The UAMS OB/GYN clerkship has used TBL as a teaching method for more than a decade, 6 , 7 but previously, little attention had been paid to the organization or quality of the TBL content. In the past, each TBL faculty facilitator wrote his or her own readiness assurance tests and application exercises, and TBLs were often not structured around a framework of learning objectives. This resulted in TBL activities that covered a wide variety of often-unrelated topics and did not consistently meet the strict definition of TBL. With lessons learned from past experience in mind, we desired to create a series of structured TBL activities that covered naturally interrelated content using truly active methods. A large amount of material must be taught in the OB/GYN clerkship in a span of time that is often shorter than that allotted to other clerkships 1 —because of this, we found it imperative to prioritize content we felt to be foundational and then to organize it in a logical manner.
Besides the challenge of covering large amounts of material, we also faced the challenge of incorporating new faculty members into TBL sessions. The majority of these faculty members had not been trained in TBL techniques. As a part of overcoming this barrier, we worked to create robust multiple-choice questions and application exercises that met the criteria of a true TBL session as outlined in the literature. 2 , 3 This eased faculty burden in that these materials facilitated active learning, requiring that faculty learn only how to best proctor a TBL session.
This TBL activity utilized active learning strategies to teach basic knowledge of normal obstetrics to third-year medical students. We feel that this TBL could easily be adapted for use by other OB/GYN educators as an introductory didactic session for obstetrics in both traditional and longitudinal clerkship settings. The TBL was well liked by medical students, with 98% of them either agreeing or strongly agreeing that the TBL was an effective learning event. Faculty facilitators also voiced their satisfaction with this TBL as a learning activity. As there are few published OB/GYN TBL activities, 6 – 11 our TBL could be a noteworthy contribution to an active learning–centered curriculum for OB/GYN clerkships.
We believe that this TBL is unique in that it uses a variety of different types of advance preparation resources. Traditional textbook reading has been combined with optional online educational videos and optional online quizzes. The videos and online quizzes allow students with different learning styles access to materials in their preferred learning style. 16 The uWISE online quizzes are also interactive, and interactive learning tools such as online question banks have been associated with better medical student performance. 17 We curated a list of several different types of advance preparation resources, all designed to teach the student the same material but in different ways. Based on the students who responded to a poll sent after the TBL's completion, a large majority of them utilized the APGO videos and the uWISE objectives in preparing for the TBL. In terms of which resources students found helpful in preparing for the TBL, 75% responded that the APGO videos were helpful, which was a higher percentage than those reporting the textbook reading to be helpful. Although the uWISE quizzes were not as highly regarded in terms of helpfulness as the APGO videos, one-third of students still found them helpful.
A current limitation of this resource is that we do not know if it will lead to improved student performance on OB/GYN standardized examinations. As this particular TBL series was implemented only this academic year, there are no current trends in grades on the National Board of Medical Examiners OB/GYN shelf examination that would lead us to believe the material is being mastered more effectively. We will continue to look for these trends, however. We will also begin to look for possible improvements in OB/GYN content on the United States Medical Licensing Examination Step 2 CK (Clinical Knowledge) exam.
Overall, this TBL activity was well organized, was well liked by students and faculty facilitators, and incorporated several different learning activities to teach a complex topic. As published TBL modules in OB/GYN are few, with no published resources on the majority of the material covered here, this TBL could serve as a valuable resource for other OB/GYN clerkships looking to adopt TBL as an active learning strategy.
A. RAT Student Version.docx
Disclosures
None to report.
Funding/Support
Ethical approval.
Reported as not applicable.

Maternal Health Task Force
Pregnancy debate revisited: To induce labor, or not?
Associations between improved care during the second stage of labour and maternal and neonatal health outcomes in a rural hospital in bangladesh, new drug shows promise in preventing one of the most common causes of maternal death.
By: Kayla McGowan , Project Coordinator, Women and Health Initiative , Harvard T.H. Chan School of Public Health
A large randomized trial conducted by the World Health Organization has found that heat-stable carbetocin is as safe and effective as oxytocin in preventing postpartum hemorrhage—excessive bleeding after childbirth and one of the leading causes of global maternal deaths… read more

Asking different questions: A call to action for research to improve the quality of care for every woman, every child
Intergrowth-21st gestational dating and fetal and newborn growth standards in peri-urban nairobi, kenya: quasi-experimental implementation study protocol, maternal intra and postpartum near‐miss following assisted reproductive technology: a retrospective study, can india’s primary care facilities deliver a cross-sectional assessment of the indian public health system’s capacity for basic delivery and newborn services, do provider birth attitudes influence cesarean delivery rate: a cross-sectional study, pregnancy complications might ‘turn on’ schizophrenia genes, study says.
Basic Obstetrics & Gynecology for Physician Assistants
11. intrapartum care.
Duration = 8:28
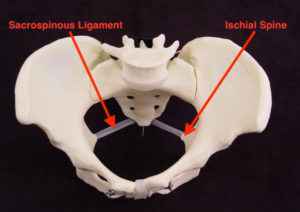
00:00 APGO educational topic number eleven 00:02 intrapartum care meet la florida live 00:05 which she is a gravida one pair zero at 00:07 39 weeks estimated gestational age and 00:10 we are going to follow her through the 00:11 process of a normal labor and delivery 00:13 the learning objectives are to 00:15 differentiate between the signs and 00:17 symptoms of true and false labor perform 00:19 the initial assessment of a laboring 00:21 patient describe the four stages of 00:23 labor and recognize common abnormalities 00:25 explain pain management approaches 00:27 during labor describe methods for 00:29 monitoring the mother and fetus describe 00:32 the steps of a vaginal delivery list 00:34 indications for operative delivery and 00:36 finally identify maternal risks specific 00:39 to delivery in developing countries 00:41 labora is at home feeling contractions 00:44 and she’s not sure if she’s in true or 00:45 false labor what is the definition of 00:47 labor let’s check our smart device the 00:50 definition of labor requires that two 00:52 things need to occur number one painful 00:55 uterine contractions and number two 00:56 cervical dilation at term many women 01:00 will feel spontaneous contractions which 01:01 they describe as tightening of the 01:03 uterus if they are not causing cervical 01:05 dilation then they are referred to as 01:06 Braxton Hicks contractions labora is on 01:09 the phone with her OB provider and she’s 01:11 trying to decide whether she should come 01:12 in to be evaluated on labor and delivery 01:14 what does the OB provider recommend come 01:17 in if you have leakage of fluid bleeding 01:19 painful contractions every five minutes 01:22 for one hour or decrease in fetal 01:24 movements laborious contractions are 01:27 every five minutes and they happen for 01:29 one hour so she and her partner head to 01:31 labor and delivery 01:31 in triage laborious prenatal records 01:34 will be reviewed and a focused history 01:36 will be performed let’s review the 01:39 assessments unique to pregnancy and 01:41 labor and delivery we need to assess 01:43 both maternal and fetal status fetal 01:46 heart tones are usually assessed with a 01:47 fetal heart monitor we also need to know 01:50 fetal presentation whether the fetuses 01:52 vertex or breech assess with either an 01:54 abdominal ultrasound or by exam since we 01:56 need to assess whether labora is in 01:58 labor we need to perform a sterile 01:59 vaginal examination we described three 02:01 components from this exam we assess the 02:03 cervical dilation the effacement and the 02:05 fetal station will first discuss 02:08 cervical dilation and effacement here is 02:11 the uterus and the cervix with the 02:13 internal 02:13 and the external loss the cervix will 02:15 dilate and this refers to the opening of 02:17 the internal loss complete dilation is 02:19 10 centimeters the cervix will also 02:22 undergo a Faceman which means that it 02:23 will thin out or the distance between 02:25 the internal and the external 02:27 awesome marked by the screen error will 02:29 become zero a non effaced cervix is 02:31 about four centimeters this green dotted 02:34 line shows a cervix that is about 50% 02:36 thinned out or will be about two 02:38 centimeters and this pink dotted line 02:41 shows a completely effaced cervix that 02:43 is zero centimeters thick moving on to 02:45 fetal station station describes the 02:48 fetal presenting part usually the vertex 02:50 in relation to the issue of spines which 02:51 are palpable vaginally when the 02:53 presenting parts at the level of the 02:54 ischial spines it is zero station as the 02:57 vertex descends down the pelvis the 02:59 station passes plus one plus two all the 03:01 way to plus five these divisions 03:02 represent centimeters below the ischial 03:04 spines on the other hand a minus one 03:07 station would meet the vertex was still 03:08 one centimeter above the ischial spine 03:10 minus 2 station would be 2 centimeters 03:12 above etc labora is found to be 5 03:15 centimeters dilated 80% effaced and 0 03:18 station so she is now admitted to labor 03:20 and delivery we described four stages of 03:22 labor the first stage of labor is from 03:25 the onset of labor to full cervical 03:27 dilation stage one is further divided 03:29 into the latent phase and the active 03:31 phase labora is already passed the 03:33 latent phase which includes from 03:34 cervical dilation to about 4 centimeters 03:37 and can be variable in length the active 03:39 phase starts at about 4 centimeters 03:41 dilated and there should be more rapid 03:43 and predictable cervical dilation the 03:45 latent phase can last for days whereas 03:47 the cervix should dilate at 03:49 approximately 1.2 to 1.5 centimeters per 03:52 hour in the active phase stage 2 is from 03:54 complete dilation to delivery of the 03:56 infant stage 3 is from delivery of the 03:59 infant to delivery of the placenta stage 04:02 4 is the immediate postpartum period of 04:04 approximately two hours after delivery 04:05 of the placenta labora is in the active 04:08 phase of stage 1 of labor walking is 04:10 generally more comfortable than laying 04:12 supplying there is decreased GI 04:14 peristalsis so patients should limit 04:15 their solid food intake for this can 04:17 lead to nausea and vomiting fetal 04:20 well-being is monitored during labor by 04:22 measurement of the fetal heart tones 04:23 which can be done by either electronic 04:25 fetal monitoring or intermittent oskol 04:27 an external toka motor is used to assess 04:29 uterine activity labor would like for us 04:32 to start discussing pain management 04:33 options during labor labor results 04:35 severe pain for most women during stage 04:38 1 of labor pain results from the 04:40 contractions of the uterus and dilation 04:42 of the cervix resulting in visceral pain 04:44 at the levels of T 10 to l1 as labor 04:47 progresses the fetal head distance the 04:49 lower birth canal and perineum resulting 04:51 in somatic pain transmitted through s2 04:53 to s4 some patients tolerate the pain of 04:56 labor and delivery without any need for 04:58 medications for women who opt for pain 05:00 relief during labor we have many safe 05:02 effective methods the epidural block is 05:04 the most effective form of intrapartum 05:06 pain relief in the United States local 05:08 anesthetic or narcotics are infused 05:10 through a catheter into the epidural 05:12 space this lasts during labor and 05:14 delivery and can be individually 05:15 titrated IV opioids and opioid agonist 05:19 and antagonist can also be used however 05:21 since they are systemically administered 05:23 the primary mechanism of pain relief is 05:25 via a sedation labora is now completely 05:28 dilated at 10 centimeters and is now in 05:30 stage 2 of Labor 05:31 how long do women push once they are 05:34 completely dilated for women who have 05:36 not had a vaginal delivery pushing 05:38 usually takes about two to three hours 05:39 the length is shorter if the woman has 05:41 not received an epidural if a woman has 05:44 already had one vaginal delivery the 05:46 second stage may be very short and she 05:48 may not need to push for very long since 05:51 this is laborious first delivery she 05:52 will likely need to push for 2 to 3 05:54 hours as a student you may stay in the 05:56 room to help with this pushing part of 05:58 stage 2 delivery of the fetus is 06:00 imminent when a half dollar size amount 06:02 of the fetal vertex is visible in 06:04 between pushes as the fetus crowns it is 06:07 helpful to support the perineum and 06:09 facilitate extension of the head after 06:11 delivery of the head there is 06:13 restitution then there is delivery of 06:16 the anterior shoulder then the delivery 06:19 of the posterior shoulder the optimum 06:21 place for baby after delivery is skin to 06:23 skin on the maternal chest next we’ll 06:25 move on to stage 3 active management of 06:28 the third stage of labor it decreases 06:30 the risk of postpartum hemorrhage this 06:32 involves bundle massage gentle core 06:34 traction and administration of IV or I 06:36 am oxytocin the placenta can take up to 06:39 30 minutes to do 06:41 there are two classic signs that the 06:42 placenta is separating from the uterus 06:44 one a gush of blood and two lengthening 06:47 of the umbilical cord after the placenta 06:50 delivers the uterus should be palpated 06:51 to ensure that it is firm and has 06:53 contracted and the placenta should be 06:55 visually examined to make sure it has 06:57 been completely removed moving now to 06:59 operative deliveries operative 07:01 deliveries are accomplished by applying 07:03 direct traction to the fetal skull with 07:05 forceps or by applying traction to the 07:07 fetal scalp with a vacuum extractor the 07:10 incidence of operative vaginal delivery 07:12 in the United States is estimated to be 07:13 approximately 3.5% the general 07:16 indications are one prolonged or 07:18 arrested second stage number two 07:20 suspicion of immediate or potential 07:22 fetal compromise and number three 07:24 shortening of the second stage for 07:26 maternal benefit our journey on to labor 07:28 and delivery with our patient labora has 07:30 assumed that we are in a high resource 07:32 setting in low resource settings there 07:34 are a multitude of risks of labor and 07:36 delivery and 99% of maternal deaths 07:38 occur in developing countries every day 07:41 800 women die from preventable causes 07:43 related to pregnancy and childbirth this 07:45 is the equivalent of two jumbo jets 07:47 daily more than half of these deaths 07:49 occur in sub-saharan Africa and another 07:51 one-third occur in Southeast Asia the 07:54 highest risk is for adolescent girls the 07:56 major complications that account for 75% 07:58 of maternal deaths are bleeding 08:00 infection high blood pressure 08:02 complications from delivery and unsafe 08:04 abortion this concludes the aapko video 08:06 on intrapartum care we reviewed normal 08:08 labor and delivery operative deliveries 08:10 and maternal risks specific to 08:12 developing countries 08:19 [Music]
I believe the video is a little unclear about the exact location of the ischial spines. Here are a couple of images that I hope will clarify their location and clinical use.
– Dr. Hughey
Definitions of the latent and active phases of the first stage of labor have changed over time.
This came about after a workshop was convened with ACOG, Society of Maternal Fetal Medicine (SMFM) and the NIH to address the high Cesarean delivery rates in the U.S. resulting in the publication of “Safe Prevention of the Primary Cesarean Delivery.”
Data suggest that the active phase of labor more likely begins at approximately 6 cm dilation (previously 4 cm). Data also suggest that the active phase of labor and the 2nd stage of labor (pushing) can take longer than previously believed. Generally, we wait 4-6 hrs in the active phase of labor before diagnosing arrest of dilation and can wait up to 4 hr in the second stage of labor before diagnosing arrest of descent. Each of these changes should give patients more time to deliver vaginally without compromising safety.
– Dr. Smith
Introductory Women's HealthCare
- NICE Guidance
- Conditions and diseases
- Fertility, pregnancy and childbirth
Intrapartum care
NICE guideline [NG235] Published: 29 September 2023
- Tools and resources
- Information for the public
Recommendations
- Recommendations for research
- Rationale and impact
- Appendix A: Adverse outcomes for different places of birth
- Appendix B: Outcomes for different places of birth – by BMI at booking
- Appendix C: Outcomes for intravenous remifentanil patient-controlled analgesia (PCA) compared with intramuscular pethidine
- Finding more information and committee details
- Update information
- Quality standard - Intrapartum care
This guideline covers the care of women and their babies during labour and immediately after birth. It focuses on women who give birth between 37 and 42 weeks of pregnancy (‘term’). The guideline helps women to make informed choices about where to have their baby and about their care in labour. It also aims to reduce variation in aspects of care.
Using inclusive language in healthcare is important for safety, and to promote equity, respect and effective communication with everyone. This guideline does not use inclusive language because it was developed before NICE’s style change to use gender-inclusive language.
Healthcare professionals should use their clinical judgement when implementing recommendations, taking into account the individual's circumstances, needs and preferences, and ensuring all people are treated with dignity and respect throughout their care.
NICE has also produced guidelines on intrapartum care for women with existing medical conditions or obstetric complications and their babies , fetal monitoring in labour and caesarean birth . For information on other related topics, see our women's and reproductive health summary page .
This guideline includes recommendations on:
- antenatal education about labour
- planning place of birth
- care throughout labour in all birth settings
- transfer of care and changing place of birth
- pain relief during labour
- prelabour rupture of membranes at term
- first , second and third stages of labour
- care of the newborn baby and care of the woman after birth
- service organisation
Who is it for?
- Healthcare professionals
- Commissioners and providers
- Healthy women who have had a straightforward pregnancy and give birth between 37 and 42 weeks of pregnancy
Is this guideline up to date?
Monitoring decision: Water birth: we will reconsider the evidence when the POOL study has published (expected 2024). For more information, see the May 2023 surveillance decision .
Portfolio review in May 2023: We have reviewed our guidelines portfolio to identify topics that we think will add the most value to the health and care system and have agreed that the updates on angle of episiotomy and rectal examination recommended in the 2022 surveillance report will not proceed as planned.
Guideline development process
How we develop NICE guidelines
This guideline updates and replaces NICE guideline CG190 (December 2014).
This guideline was previously called intrapartum care for healthy women and babies.
Your responsibility
The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service. It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
All problems (adverse events) related to a medicine or medical device used for treatment or in a procedure should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card Scheme .
Local commissioners and providers of healthcare have a responsibility to enable the guideline to be applied when individual professionals and people using services wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with complying with those duties.
Commissioners and providers have a responsibility to promote an environmentally sustainable health and care system and should assess and reduce the environmental impact of implementing NICE recommendations wherever possible.
- Find a hospital Results See all results Balashikha 1 hospitals Barnaul 2 hospitals Ivanovo 2 hospitals Kaliningrad 2 hospitals Kazan 2 hospitals Kislovodsk 1 hospitals Korolev 1 hospitals Kovrov 1 hospitals Krasnodar 3 hospitals Krasnogorsk 1 hospitals Moscow 41 hospitals Nizhny Novgorod 3 hospitals Novokuibyshevsk 1 hospitals Novokuznetsk 1 hospitals Novosibirsk 4 hospitals Obninsk 1 hospitals Orenburg 1 hospitals Penza 1 hospitals Saint Petersburg 8 hospitals Samara 3 hospitals Surgut 1 hospitals Tomsk 1 hospitals Tyumen 1 hospitals Ulan-Ude 1 hospitals Ulyanovsk 2 hospitals Vladivostok 1 hospitals Volgograd 1 hospitals Vologda 1 hospitals Yalta 1 hospitals Yekaterinburg 2 hospitals All hospitals
- Find a sanatorium Results See all results Altai region 4 sanatoriums Buryatia 1 sanatoriums Crimea 4 sanatoriums Ingushetia 1 sanatoriums Karelia 1 sanatoriums Kislovodsk 1 sanatoriums Krasnodar region 2 sanatoriums Moscow region 5 sanatoriums Nizhny Novgorod Region 1 sanatoriums Saint Petersburg region 1 sanatoriums All sanatoriums
- Check the prices Allergology 29 hospitals Andrology 35 hospitals Bariatric surgery 15 hospitals Cardiology 42 hospitals Cosmetology 21 hospitals Dentistry 25 hospitals Dermatology 37 hospitals Dietetics 15 hospitals Endocrinology 42 hospitals Gastroenterology 38 hospitals Genetics 4 hospitals Gynecology 54 hospitals Hematology 17 hospitals IVF (In Vitro Fertilization) 14 hospitals Mammalogy 33 hospitals Maxillofacial Surgery 9 hospitals Narcology 3 hospitals Neurology 51 hospitals Neurosurgery 16 hospitals Obstetrics 14 hospitals Oncology 42 hospitals Ophthalmology 36 hospitals Orthopedics and traumatology 32 hospitals Otolaryngology (ENT) 39 hospitals Pediatrics 29 hospitals Phlebology 29 hospitals Plastic surgery 22 hospitals Proctology 27 hospitals Psychiatry 13 hospitals Pulmonology 24 hospitals Rehabilitation 17 hospitals Rheumatology 26 hospitals Speech therapy 6 hospitals Surgery 37 hospitals Urology 47 hospitals Venereology 21 hospitals
- List of diseases Aesthetic problems 24 hospitals Allergic diseases 31 hospitals Blood diseases 17 hospitals Cardiovascular diseases 44 hospitals Childhood diseases 27 hospitals Colon diseases 27 hospitals Diseases of the digestive system 42 hospitals Diseases of the mammary glands 34 hospitals Diseases of the musculoskeletal system and injuries 37 hospitals Diseases of veins and lymph nodes 32 hospitals Endocrine diseases 46 hospitals ENT (eye, nose, throat) diseases 40 hospitals Eye diseases 39 hospitals Female diseases 56 hospitals Genetic diseases 6 hospitals Infectious diseases 25 hospitals Male diseases 39 hospitals Mental disorders and phenomena 13 hospitals Narcological problems 6 hospitals Nervous diseases 50 hospitals Oncological diseases 43 hospitals Respiratory diseases 25 hospitals Rheumatic diseases 27 hospitals Skin diseases 37 hospitals Speech disorders 7 hospitals Teeth Diseases 26 hospitals Urological diseases 50 hospitals Venereal diseases 24 hospitals
- Our contacts
Morozovskaya Children's City Clinical Hospital
Tap to book

About clinic
The largest children's hospital in Russia and Europe. More than a third of the total number of hospitalized children in Moscow falls on the Morozovskaya hospital. Located on nine hectares in the historical center of the capital, it resembles a small town in its spirit.
The bed capacity is 1205 beds. Morozovskaya Children's Hospital is a multidisciplinary (31 profiles) clinical hospital and has 48 departments, including 34 clinical ones.
The Morozov hospital employs:
- 10 out of 24 children's Chief freelance specialists of the Moscow City Health Department are a neonatologist, geneticist, rheumatologist, endocrinologist, ophthalmologist, pulmonologist, gastroenterologist, oncologist, hematologist, cardiovascular surgeon.
- more than 700 doctors,
- more than 900 nursing staff.
13 unique Centers
On the basis of the Morozov hospital, 13 unique Centers of city specialized medical care for children and adolescents have been formed and are constantly operating:
- Center for the treatment of cerebrovascular pathology in children and adolescents (the only one in Russia)
- Center for Pediatric Rheumatology (the only one in the city health care system)
- Center for Pediatric Oncology and Hematology
- Center for Orphan and Other Rare Diseases
- Center for the treatment of children with von Willebrand disease
- Reference center for congenital hereditary diseases, genetic abnormalities, orphan and other rare diseases
- Center for Reproductive Health of Children and Adolescents
- Center for Pediatric Endocrinology
- Center for Pediatric Gastroenterology
- Neonatal Screening Center
- Center for the Prevention of Chronic Noncommunicable Diseases
- Respiratory Medicine Center
- Consultative and Diagnostic Center of Neurology and Family Psychotherapy
Medical equipment
More than 3 thousand units of unique and advanced medical equipment have been installed in the Morozov hospital, including integrated equipment in operating rooms for microsurgical, endovascular and endoscopic operations, pain stress monitors, equipment for artificial lung ventilation of newborns and incubators for nursing children with extremely low body weight, computer and magnetic resonance tomographs (including 3.0 TL), digital X-ray diagnostic and X-ray surgical devices, ultrasound diagnostic systems, high-tech equipment for laboratory, including genetic research, etc.
The figures for the effectiveness of treatment are comparable, and in some cases even exceed the indicators of the world's leading children's clinics.
A team of specialist doctors works seven days a week at the hospital, which allows to provide emergency multidisciplinary medical care (pediatricians, pediatric surgeons, orthopedic traumatologists, maxillofacial surgeons, anesthesiologists-resuscitators, neonatologists, otorhinolaryngologists, hematologist, neurologists, doctors of radiation, ultrasound and clinical laboratory diagnostics, etc.). There is no similar one-step round-the-clock work of a multidisciplinary team of medical specialists in any children's hospital in Russia and Europe.
Today, the medical care that patients receive at the Morozov hospital is no different from that which they could receive in any other country in the world.
Since 2015, the Morozovskaya Children's Hospital has received a license for the implementation of educational detail and became the Center for Postgraduate Pediatric Education. The Morozovskaya hospital is a clinical base for 15 departments of three medical universities in Moscow.
Since 1903, the Morozovskaya hospital has not interrupted its work for a single day, remaining faithful to the motto "Mercy and professionalism", laid down when the hospital was founded.
Specialization
What diseases are treated, additional services and facilities, patients also choose.

[ORGANIZATION OF MEDICAL CARE FOR CHILDREN WITH A NEW CORONAVIRUS INFECTION IN PATIENT CONDITIONS ON THE EXAMPLE OF THE CHILDREN'S CITY CLINICAL HOSPITAL NAMED AFTER Z. A. BASHLYAEVA]
Affiliations.
- 1 Children's City Clinical Hospital named after Z. A. Bashlyaeva of the Moscow City Health Department, 125373, Moscow, Russian Federation.
- 2 Pirogov Russian National Research Medical University, 117997, Moscow, Russian Federation.
- 3 Russian Medical Academy of Continuous Professional Education of the Ministry of Healthcare of the Russian Federation, 125993, Moscow, Russian Federation.
- 4 Pirogov Russian National Research Medical University, 117997, Moscow, Russian Federation, [email protected].
- 5 Research Institute for Healthcare Organization and Medical Management of Moscow Healthcare Department, 115088, Moscow, Russian Federation.
- PMID: 34792888
- DOI: 10.32687/0869-866X-2021-29-s2-1343-1349
The article presents an analysis of the work of the largest children's COVID-19 center in Moscow, organized on the basis of the Children's City Clinical Hospital named after Z. A. Bashlyaeva of the Moscow City Health Department. From March to November 2020 at the COVID-19 Center were hospitalized 2,837 patients with suspected/confirmed diagnosis of COVID-19, in total in 2020 1,876 children with a confirmed diagnosis of COVID-19 were treated, 58 (3%) children were in serious condition in the intensive care unit, of which children 11-18 years old were 25%. At the 2020 neonatal COVID-19 center, 215 newborns were observed with suspected COVID-19 diagnosis. The diagnosis of COVID-19 was confirmed in 18 children, while 8 newborns came from the home of COVID-19. In the Center for rehabilitation, where children aged 0 to 3 years old who were born with very low and extremely low body weight are observed, dispensary observation for children who have undergone COVID-19 is organized. 45 children who were observed fell ill with the new coronavirus infection. There were no deaths among children with COVID-19.
Keywords: COVID-19; COVID-center; children; new coronavirus infection; newborns; treatment.
- COVID-19 Testing*
- Child, Preschool
- Hospitals, Pediatric
- Infant, Newborn
- Retrospective Studies

IMAGES
VIDEO
COMMENTS
TEACHING CASE. CASE: A 23-year old G1P0 woman at 38 weeks gestation comes to Labor and Delivery complaining of a 5-hour history of painful contractions occurring every 5 minutes and lasting 45-60 seconds in duration. She denies leaking of fluid per vagina, but has noted bloody show. She reports normal fetal movement.
Educational Topic 11: Intrapartum Care. Rationale: Students should understand the normal course of labor and childbirth. Intrapartum care includes ongoing risk assessment of the labor course and the timely recognition of abnormal events to achieve a safe, healthy birth for the mother and infant. Interprofessional teamwork and effective ...
Educational Topic 11: Intrapartum Care Students should understand the normal course of labor and childbirth. Intrapartum care includes ongoing risk assessment of the labor course and the timely recognition of abnormal events to . achieve a safe, healthy birth for the mother and infant. Interprofessional teamwork and effective
"*Since the publication of this video, 6 cm has been re-defined as the start of the active stage of labor.*"The Association of Professors of Gynecology and O...
Educational Topic 11: Intrapartum Care. Rationale: Understanding the process of normal labor and delivery allows optimal care and reassurance for the woman and timely recognition of abnormal events. Intended Learning Outcomes: A student should be able to: • Differentiate between the signs and symptoms of true and false labor.
Study with Quizlet and memorize flashcards containing terms like Tocometer shows irregular contractions every 2-8 minutes. Urine dipstick is notable for 1+ glucose wit negative ketones. All else is normal. Most likely diagnosis, Management options regarding Group B streptococcus in pregnancy?, Initial evaulation of patients presenting to hospital for labor and more.
APGO educational topic number eleven 00:02 intrapartum care meet la florida live 00:05 which she is a gravida one pair zero at 00:07 39 weeks estimated gestational age and 00:10 we are going to follow her through the 00:11 process of a normal labor and delivery 00:13 the learning objectives are to 00:15 differentiate between the signs and 00:17
9 Preconception Care. MSO Video Teaching Case - Student-Fillable. 10 Antepartum Care. MSO Video Teaching Case - Student-Fillable. 11 Intrapartum Care. MSO Video Teaching Case - Student-Fillable. 12 Immediate Care of the Newborn. MSO Teaching Case - Student-Fillable. 13 Postpartum Care. MSO Video Teaching Case - Student-Fillable. 14 ...
The guideline highlights the importance of woman-centred care to optimize the experience of labour and childbirth for women and their babies through a holistic, human rights-based approach. It introduces a global model of intrapartum care, which takes into account the complexity and diverse nature of prevailing models of care and contemporary ...
11th. Edition. APGO MEDICAL STUDENT . EDUCATIONAL OBJECTIVES. Outlining the core women's health knowledge, skills and attitudes . fundamental to today's medical student.
This guideline includes 56 evidence-based recommendations on intrapartum care - 26 new recommendations adopted by the Guideline Development Group (GDG) at the 2017 meetings, and 30 existing recommendations relevant to intrapartum care that were integrated from previously published WHO guidelines. Sections 3.1-3.6 outline the narrative summaries and the corresponding recommendations ...
Body mass index (BMI) at booking (kg/m 2) Average rate of intrapartum caesarean birth (category 1, 2 or 3) Average rate of stillbirth, neonatal death or the baby needing neonatal care. Average rate of birth with forceps or ventouse. Less than 18.5. No difference compared with women with a BMI 18.5 to 24.9 kg/m 2.
The committee began with the 64 Educational Topic Areas and the underlying educational objectives published in the Objectives 7th edition. Three of these Educational Topic Areas were considered ... 11 Intrapartum Care 12 Immediate Care of the Newborn 13 Postpartum Care 14 Lactation Section B: Abnormal Obstetrics 15 Ectopic Pregnancy
The videos, 5- to 10-minute educational videos on various OB/GYN topics, were entitled Medical Student Educational Objectives and could be accessed on YouTube. For this TBL, the videos that corresponded to the reading material were topics 8 (Maternal-Fetal Physiology), 11 (Intrapartum Care), 13 (Postpartum Care), 14 (Lactation), 26 (Intrapartum ...
Posted on July 12, 2018. By: Kayla McGowan, Project Coordinator, Women and Health Initiative, Harvard T.H. Chan School of Public Health. A large randomized trial conducted by the World Health Organization has found that heat-stable carbetocin is as safe and effective as oxytocin in preventing postpartum hemorrhage—excessive bleeding after ...
APGO educational topic number eleven 00:02 intrapartum care meet la florida live 00:05 which she is a gravida one pair zero at 00:07 39 weeks estimated gestational age and 00:10 we are going to follow her through the 00:11 process of a normal labor and delivery 00:13 the learning objectives are to 00:15 differentiate between the signs and 00:17
Guidance. This guideline covers the care of women and their babies during labour and immediately after birth. It focuses on women who give birth between 37 and 42 weeks of pregnancy ('term'). The guideline helps women to make informed choices about where to have their baby and about their care in labour. It also aims to reduce variation in ...
Educational Topic 11: Intrapartum Care Students should understand the normal course of labor and childbirth. Intrapartum care includes ongoing risk assessment of the labor course and the timely recognition of abnormal events to achieve a safe, healthy birth for the mother and infant. Interprofessional teamwork and effective
The largest children's hospital in Russia and Europe. More than a third of the total number of hospitalized children in Moscow falls on the Morozovskaya hospital. Located on nine hectares in the historical center of the capital, it resembles a small town in its spirit. It is a multidisciplinary (31 profiles) clinical hospital and has 48 departments, including 34 clinical ones.
Requests the Director-General to convene the World Conference on Early Childhood Care and Education from 22 to 24 September 2010 in Moscow, Russian Federation, in order to reaffirm the importance of EFA goal 1 in the EFA and other development agendas, to identify policy gaps in early childhood care and education (ECCE) and develop concrete ...
APGO MEDICAL STUDENT EDUCATIONAL OBJECTIVES, 11TH EDITION ... UNIT 2: OBSTETRICS Educational Topic 26: Intrapartum Fetal Surveillance Intrapartum fetal surveillance is used to evaluate fetal well-being and manage labor with the goal . of a safe, healthy birth for the mother and infant. ... value-based care and the impact on patient safety KH ...
3 Russian Medical Academy of Continuous Professional Education of the Ministry of Healthcare of the Russian Federation, 125993, Moscow, Russian Federation. ... (3%) children were in serious condition in the intensive care unit, of which children 11-18 years old were 25%. At the 2020 neonatal COVID-19 center, 215 newborns were observed with ...
Perhaps the most prominent of the city's hospitals is the Botkinskaya, founded in 1911. As in the rest of Russia, public health care facilities in Moscow are free. Education. Moscow has an exceptionally large concentration of educational establishments, and the number of universities increased in the 1990s.