- Sign In to save searches and organize your favorite content.
- Not registered? Sign up

Recently viewed (0)
- Save Search
- Subscriptions
- Join E-mail List
Patient Case Studies and Panel Discussion: Leukemia – Rare and Emerging Subtypes
- Get Citation Alerts
- Download PDF to Print
Rare and emerging subtypes of leukemia can be incredibly challenging to diagnose and even more challenging to treat. At the NCCN 2019 Annual Congress: Hematologic Malignancies, a panel of experts, moderated by Andrew D. Zelenetz, MD, PhD, were presented with particularly challenging cases in these malignancies and asked to discuss best approaches to treatment.
- Patient Case Study 1
In the first case study, a 77-year-old woman presented with multiple nodular lesions and plaques on her face, chest, and back. She had a history of type 2 diabetes, stage 3 hypertension, hyperlipidemia, coronary heart disease, cerebral infarction, glaucoma, lens extracapsular extraction and posterior chamber intraocular lens implantation, Sjögren syndrome, rheumatoid arthritis, and left axillary vein and brachial vein thrombosis.
She had previously received a conventional therapy of Chinese medicine, but her condition did not improve. Her clinicians performed a bone marrow biopsy and an aspiration biopsy of a nodule on the right side of her face, and immunostaining results revealed the following immunophenotype: CD4+, CD123+, CD43+, CD56+, with Ki-67 level of 30% to 40%.
The patient was diagnosed with blastic plasmacytoid dendritic cell neoplasm, which is a rare blood cancer in the myeloid malignancies family. Andrew D. Zelenetz, MD, PhD, Memorial Sloan Kettering Cancer Center, noted that this disease used to be classified as a variant of acute lymphoblastic leukemia (ALL) and has a distinctive immunophenotype and clinical appearance, characterized by purple skin lesions.
He said a helpful tool for remembering the immunophenotype of this disease is to think “123456”: CD123, CD4, and CD56. Conversely, Nitin Jain, MD, The University of Texas MD Anderson Cancer Center, noted that although this rule of thumb can be helpful, it is important to keep in mind that approximately 10% of patients with this malignancy are actually CD56-negative.
Daniel A. Pollyea, MD, MS, University of Colorado Cancer Center, emphasized the unique phenotypic expression pattern in this malignancy, and the risk of cytopenias due to bone marrow involvement. “Certainly there are patients with bone marrow involvement who don't have cytopenias and have predominant expression of these skin manifestations,” he said. “But I think the CD123 is really the key, because this is a very, very difficult diagnosis to make, and that can be the linchpin.” He added that CD123 expression status is important to know not only for diagnostic purposes but also from a therapeutic perspective. However, many clinical pathologists do not possess the capabilities to test for CD123, so if a diagnosis of blastic plasmacytoid dendritic cell neoplasm is even being entertained, a discussion with a pathologist regarding testing for CD123 is critical.
The nodule on the right side of the patient’s face was surgically excised, and she was treated with gemcitabine, nedaplatin (a second-generation platinum drug used in China that is not approved by the FDA; it is similar to carboplatin and cisplatin), and bleomycin. The patient experienced an initial response to therapy but subsequently developed additional nodular lesions on her arm.
According to Dr. Pollyea, regardless of what transpired with this particular patient, surgical resection of skin lesions did not have a role in this case. “Typically, if the disease is going to respond, the skin lesions are very, very sensitive,” he said. “So there are issues with wound healing if you perform a large resection.”
The panel then discussed tagraxofusp-erzs, a recently approved drug for the treatment of this disorder that has been shown to be highly effective. 1 Dr. Pollyea noted that the mechanism of action of this drug is “quite brilliant.”
“You're taking one of nature's most potent toxins and delivering it directly to a cell population of critical importance in this disease, and potentially the precursor or primitive population of the disease,” he said.
A trial of tagraxofusp treatment in patients with blastic plasmacytoid dendritic cell neoplasms led to durable responses and high complete response rates, particularly in the first-line setting (72%). 1 In relapsed/refractory disease, it was less effective, but “still very effective,” according to Dr. Zelenetz, with a complete response rate of 38%. However, significant toxicity was seen, with capillary leak syndrome a fatal toxicity.
Jae Park, MD, Memorial Sloan Kettering Cancer Center, noted that because of the limited clinical experience with this agent, it is critical to administer the drug in an inpatient setting whenever possible and to closely monitor any patient-related physical changes, including weight fluctuations, kidney function, and respiratory status.
William G. Wierda, MD, PhD, The University of Texas MD Anderson Cancer Center, agreed, adding that he actually treated patients with this compound on a clinical trial before its approval. “During the trial, we were closely monitoring daily weight, albumin, and [liver function], and making daily adjustments in dosing based on what was happening with patients clinically,” he said. “So it's important to be very familiar with the prescribing information.”
Given this particular patient’s age, history, and comorbidities, stem cell transplantation was not an option. However, according to Dr. Park, allotransplant should be considered in these cases whenever possible, and earlier rather than later. “Even with a good response, it becomes difficult to continue this regimen,” he said. “And after [patients] relapse, there are very few treatment options available.”
- Patient Case Study 2
A 28-year-old woman presented with fatigue and lymphadenopathy. Her initial WBC count was 11.1 k/uL with 40% blasts, and she showed hypercellular bone marrow. Her immunophenotype included the following: 88.0% CD45+/–, CD34+, CD19+, CD10+ (variable), CD20– (∼4% of cells stain), sCD22+, CD13–, CD33–, CD38+, CD56–, CD2+/–, CD3–, CD4–, CD8–, CD7–, CD5–, CD117, HLA-DR+, sIg light chain–, cCD79a+, cCD22+, MPO–, cIgM+, and TdT+. After noting the complexity of the patient’s immunophenotype, Dr. Pollyea emphasized the importance of working with a skilled hematopathologist in cases such as this.
The patient was diagnosed with B-cell ALL and treated with the CALGB 10403 regimen. 2 At day 30, bone marrow biopsy showed residual disease with 16% blasts by flow. As her next course of treatment, the patient received blinatumomab for one cycle.
Dr. Jain agreed that this was a reasonable next step, but added that an additional cycle of chemotherapy would also have been feasible. Although the patient was high-risk, he would not yet say treatment had failed after only one treatment cycle.
“I think on the adult side we have to take our cues from the pediatricians who have been so incredibly successful with this disease,” said Dr. Pollyea. “And CALGB 10403 is a regimen that attempts to apply the pediatric regimens to an adolescent/young adult population.” 2
He added that pediatricians tend to stick to protocol, and the protocol for this particular regimen allows for a more extended induction period. “So at this point you should have a lot of concerns about this patient, but I think the protocol allows you to continue.”
About 4 weeks after starting blinatumomab, the patient experienced complete remission confirmed by bone marrow biopsy. She also received 6 cycles of intrathecal chemotherapy throughout the course of her treatment and showed no evidence of central nervous system involvement.
A month later, she presented with enlarged lymph nodes in her groin and neck, and bone marrow biopsy confirmed 63% blasts with an ALL phenotype. A same-day inguinal lymph node biopsy was consistent with lymphoblastic leukemia involvement.
Although the patient experienced a complete remission initially, Dr. Park noted that minimal residual disease (MRD) status was never confirmed. This factor is critical in assessing a patient’s depth of remission, and MRD-positive patients should receive additional therapy sooner rather than later to get to MRD-negative status, he said.
Dr. Jain said that additional diagnostic testing in the form of RNA sequencing would be appropriate in this case, but noted a caveat of the limited availability of this type of testing. The patient underwent next-generation sequencing (NGS), which revealed the following: DIAPH1-PDGFRB fusion; CDKN2A/B - p14 ARF loss exon 1 and CDKN2b loss; PIK3R1 splice site 1746-2A>6; and TP53 N288fs*60.
According to Dr. Park, interpreting NGS data can be difficult, and misinterpretation can lead to the wrong choice of treatment. This again underlines the importance of consulting with a skilled pathologist or other experienced ALL expert to assist in interpreting mutation profiles.
The patient was determined to have Ph-like ALL (a newly recognized entity of Ph-negative ALL with a poor prognosis) and was enrolled in the KTE-CA19 CAR-T (axicabtagene ciloleucel [axi-cel]) trial ( ClinicalTrials.gov identifier: NCT02614066). She received cytoreductive chemotherapy with hyperCVAD part A before apheresis for CAR-T generation, and experienced favorable cytoreduction (she received fludarabine/cyclophosphamide for lymphodepletion). She then received a post–CAR-T infusion and showed no response; her blast count increased from 0.42 to 80.35 within a week.
“This is just a tough case,” said Dr. Park, noting the unusually refractory nature of the disease. “Initial response rates to CAR-T cell therapy are approximately 80%, so she’s already in the very unlucky 20% of cases,” he said.
Dr. Jain described 2 subtypes of Ph-like ALL: approximately half are CRLF2 -rearranged, 3 and these patients should ideally be referred to a clinical trial. The other half are nonrearranged, 3 and these patients should be referred for RNA sequencing to determine fusion genes.
No response was seen to further treatment, and the patient chose to continue care in hospice.
According to Dr. Zelenetz, incorporation of comprehensive genetic analysis and fluorescence in situ hybridization testing is important to identify high-risk patients (such as those with Ph-like phenotype) and plan for allogeneic hematopoietic stem cell transplantation (alloHSCT) or referral to clinical trials as early as possible.
MRD assessment by flow and/or NGS is critical to assess depth of response, modification of therapy, and candidacy for early alloHSCT. Dr. Park noted that both gene sequencing tests are validated, so patient preference should take priority.
Incorporation of tyrosine kinase inhibitors (TKIs) in Ph-like ALL is being investigated in clinical trials, and patients with this disease should be referred earlier rather than later, added Dr. Zelenetz. “But the nuance to that is understanding how to integrate TKIs into this entity, which is going to be dependent on understanding the mechanisms involved in the disease,” he said. “It won’t be just one TKI [that everyone receives]; it's much more complicated than that, unfortunately.”
Dr. Jain added that although Ph-like ALL has been established as high risk in the setting of chemotherapy, its classification remains to be determined in the new era of targeted therapies. “Some emerging data suggest that blinatumomab, inotuzumab, and CAR-T-cell therapy may overcome the negative prognostication of Ph-like ALL,” he said. “So those are some data we’ll hopefully see at the ASH Annual Meeting.”
Jarrod Holmes, MD, Annadel Medical Group, also participated in the panel discussion.
Pemmaraju N , Lane AA , Sweet KL , et al. . Tagraxofusp in blastic plasmacytoid dendritic-cell neoplasm . N Engl J Med 2019 ; 380 : 1628 – 1637 .
- Search Google Scholar
- Export Citation
Stock W , Luger SW , Advani AS , et al. . A pediatric regimen for older adolescents and young adults with acute lymphoblastic leukemia: results of CALGB 10403 . Blood 2016 ; 133 : 1548 – 1559 .
Jain N , Roberts KG , Jabbour E , et al. . Ph-like acute lymphoblastic leukemia: a high-risk subtype in adults . Blood 2017 ; 129 : 572 – 581 .
Disclosures: Dr. Zelenetz has disclosed that he receives research support from Genentech/Roche, Gilead, MEI, and BeiGene; he has been a consultant for Celegene/JUNO, Genentech/Roche, Gilead, BeiGene, Pharmacyclics, Jansen, Amgen, Astra‐Zeneca, Novartis, and MEI Pharma; and he is on the Scientific Advisory Board of the Lymphoma Research Foundation and Adaptive Biotechnologies. Dr. Jain has disclosed that he is a consultant for AbbVie, Inc., AstraZeneca Pharmaceuticals LP, Genentech, Inc., Janssen Pharmaceutica Products, LP, Adaptive Biotechnologies, Precision Biosciences, Verastem, and Pharmacyclics; receives grant/research support from AbbVie, Inc., AstraZeneca Pharmaceuticals LP, Bristol-Myers Squibb Company, Genentech, Inc., Incyte Corporation, Adaptive Biotechnologies, ADC Therapeutics, Cellectis, Precision Biosciences, Servier, Verastem, Pfizer, Inc., and Pharmacyclics; is a scientific advisor for AbbVie, Inc., AstraZeneca Pharmaceuticals LP, Genentech, Inc., Janssen Pharmaceutica Products, LP, Adaptive Biotechnologies, Precision Biosciences, Verastem, and Pharmacyclics; and has received honoraria from AbbVie, Inc., AstraZeneca Pharmaceuticals LP, Genentech, Inc., Janssen Pharmaceutica Products, LP, Adaptive Biotechnologies, Precision Biosciences, Verastem, and Pharmacyclics. Dr. Park has disclosed that he receives grant/research support from Amgen Inc., Genentech, Inc., Incyte Corporation, Juno Therapeutics, Inc., Kite Pharma, Novartis Pharmaceuticals Corporation, and Servier; and is a scientific advisor for from Amgen Inc., AstraZeneca Pharmaceuticals LP, GlaxoSmithKline, Incyte Corporation, Kite Pharma, Novartis Pharmaceuticals Corporation, Allogene Therapeutics, Autolus Therapeutics plc, and Takeda Pharmaceuticals North America, Inc. Dr. Pollyea has disclosed that he is a scientific advisor for AbbVie, Inc., Agios, Inc., Celgene Corporation, Daiichi-Sankyo Co., Forty Seven, Inc., Janssen Pharmaceutica Products, LP, Pfizer Inc., and Takeda Pharmaceuticals North America, Inc. Dr. Wierda has disclosed that he is a consultant for Genzyme Corporation and receives grant/research support from AbbVie, Inc., Acerta Pharma, Genentech, Inc., Gilead Sciences, Inc., Janssen Pharmaceutica Products, LP, Juno Therapeutics, Inc., Karyopharm Therapeutics, Kite Pharma, Cyclacel Pharmaceuticals, Inc., GlaxoSmithKline/Novartis Pharmaceuticals Corporation, Loxo Oncology, Inc., miRagen Therapeutics, Inc., Oncternal Therapeutics, Inc., Xencor, Inc., Pharmacyclics, and Sunesis Pharmaceuticals, Inc. Dr. Holmes has disclosed that he has no financial interests, arrangements, affiliations, or commercial interests with the manufacturers of any products discussed in this article or their competitors.
Article Sections
Article information.
- Get Permissions
- Similar articles in PubMed
Google Scholar
Related articles.
- Advertising
- Terms of Use
- Privacy Policy
- Permissions

© 2019-2024 National Comprehensive Cancer Network
Powered by:
- [66.249.64.20|162.248.224.4]
- 162.248.224.4
Character limit 500 /500
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- Resources for Hematology Fellows
- American Society of Hematology
- Hematopoiesis Case Studies
Case Study: Prognostic Factors in Acute Lymphocytic Leukemia
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
A 48-year-old female presented to the emergency department with severe headaches, dyspnea on exertion, and petechiae on the lower extremities. A CBC was drawn that showed the following: WBC=56 x10 3 /µL, Hgb=9.0 g/dL, Hct=23, MCV=97 fl, plt=15 x10 9 /µL, ANC=0.7x10 3 /µL. A bone marrow biopsy was performed and showed 90 percent lymphoid blasts. The blast population expressed CD19, CD20, CD22, CD10, CD34, TdT, and HLA-DR. Metaphase cytogenetics showed a normal female karyotype. FISH for bcr-abl was positive. The patient was subsequently diagnosed with pre-B acute lymphoblastic leukemia.
The abnormality of which gene is associated with a poor outcome in this patient?
- Ten-Eleven Translocation-2 (TET2)
- Isocitrate Dehydrogenase 1/2 ;(IDH1/IDH2)
Explanation
IKAROS ( IKZF1 ), a gene located in chromosome 7p12, is responsible for encoding a zinc finger-containing transcription factor called Ikaros that is essential for normal lymphoid development. Using genome-wide analysis, deletions involving IKZF1 were found in 84 percent of 304 patients with acute lymphoblastic leukemia (ALL). 1 Ikaros can occur in several splice variants and may explain some of the differential function of this transcription factor. The expression of certain spliced oncogenic Ikaros isoforms in bcr-abl-positive ALL may confer resistance to tyrosine kinase inhibitors (TKIs). 2 In a study of 83 patients with bcr-abl-positive ALL, a high frequency of IKZF1 deletions was observed (63 percent), mainly in exons 4 to 7 and exons 2 to 7. Patients who carry the IKZF1 deletions have inferior disease-free survival compared to those who have wild-type IKZF1 (10 months versus 32 months). 3
Ten-eleven translocation 2 ( TET2 ) is a gene located in chromosome 4q24. Mutations involving this gene can be found in varying frequencies in myeloid malignancies, including 10 percent in myelodysplastic syndromes, 50 percent in chronic myelomonocytic leukemia (50 percent), 20 percent in myeloproliferative neoplasms (20 percent) and 20 percent in secondary acute myeloid leukemias derived from these conditions. Recent studies suggest that TET2 may be important in epigenetic regulation. The exact prognostic value of this mutation remains unclear although some suggest that patients who have TET2 mutations have a good prognosis. 4-6
NOTCH1 is a gene that encodes for a transmembrane receptor that regulates normal T-cell development. This mutation has been detected in > 50 percent of both pediatric and adult T-ALL cases. FBXW7 encodes an E3 ubiquitin ligase responsible for negative regulation of NOTCH1 signaling. Mutations involving FBXW7 occur at a frequency of about 20 percent in ALL. Pediatric studies suggest the good prognostic value of NOTCH1 / FBXW7 mutations. The results in adult ALL patients are less clear, with conflicting results. 7-9
Isocitrate Dehydrogenase 1 ( IDH1 ) is a gene located in chromosome 2q33.3, while IDH2 is located in chromosome 15q26.1. These genes are responsible for encoding enzymes that catalyze the oxidative decarboxylation of isocitrate to α-ketoglutarates. Intact IDH activity is necessary for normal cellular protection from oxidative stress. These mutations were first described in low-grade gliomas/secondary glioblastomas and subsequently in acute myeloid leukemia. Some studies suggest that mutations involving this gene may confer poor prognosis in certain subsets, particularly in cytogenetically normal FMS-like tyrosine kinase-3 ( Flt-3 ), wild-type, and nucleophosmin-1 ( NPM-1 )-mutated AML. 10-12
- Mullighan CG, Miller CB, Radtke I, et al. BCR–ABL1 lymphoblastic leukaemia is characterized by the deletion of Ikaros . Nature. 2008;453:110-114.
- Iacobucci I, Lonetti A, Messa F, et al. Expression of spliced oncogenic Ikaros isoforms in Philadelphia-positive acute lymphoblastic leukemia patients treated with tyrosine kinase inhibitors: implications for a new mechanism of resistance . Blood. 2008;112:3847-3855.
- Martinelli G, Iacobucci I, Storlazzi CT, et al. IKZF1 (Ikaros) deletions in BCR-ABL1 –positive acute lymphoblastic leukemia are associated with short disease-free survival and high rate of cumulative incidence of relapse: a GIMEMA AL WP report . J Clin Oncol. 2009;27:5202-5207.
- Jankowska AM, Szpurka H, Tiu RV, et al. Loss of heterozygosity 4q24 and TET2 mutations associated with myelodysplastic/myeloproliferative neoplasms . Blood. 2009;113:6403-6410.
- Kosmider O, Gelsi-Boyer V, Cheok M, et al. TET2 mutation is an independent favorable prognostic factor in myelodysplastic syndromes (MDSs) . Blood. 2009;114:3285-3291.
- Tefferi A, Pardanani A, Lim KH, et al. TET2 mutations and their clinical correlates in polycythemia vera, essential thrombocythemia and myelofibrosis . Leukemia. 2009;23:905-911.
- Asnafi V, Buzyn A, Le Noir S, et al. NOTCH1/FBXW7 mutation identifies a large subgroup with favorable outcome in adult T-cell acute lymphoblastic leukemia (T-ALL): a group for research on adult acute lymphoblastic leukemia (GRAALL) study . Blood. 2009;113:3918-3924.
- Park MJ, Taki T, Oda M, et al. FBXW7 and NOTCH1 mutations in childhood T cell acute lymphoblastic leukaemia and T cell non-Hodgkin lymphoma . Br J Haematol. 2009;145:198-206.
- Mansour MR, Sulis ML, Duke V, et al. Prognostic implications of NOTCH1 and FBXW7 mutations in adults with T-cell acute lymphoblastic leukemia treated on the MRC UKALLXII/ECOG E2993 protocol . J Clin Oncol. 2009;27:4352-4356.
- Tefferi A, Lasho TL, Abdel-Wahab O, et al. IDH1 and IDH2 mutation studies in 1473 patients with chronic-, fibrotic- or blast-phase essential thrombocythemia, polycythemia vera or myelofibrosis . Leukemia. 2010;24:1302-1309.
- Abbas S, Lugthart S, Kavelaars FG, et al. Acquired mutations in the genes encoding IDH1 and IDH2 both are recurrent aberrations in acute myeloid leukemia (AML): prevalence and prognostic value . Blood. 2010. [Epub ahead of print]
- Paschka P, Schlenk RF, Gaidzik VI, et al. IDH1 and IDH2 mutations are frequent genetic alterations in acute myeloid leukemia and confer adverse prognosis in cytogenetically normal acute myeloid leukemia with NPM1 mutation without FLT3 internal tandem duplication . J Clin Oncol. 2010;28:3636-3643.
Case study submitted by Sanjay R. Mohan, MD, Cleveland Clinic Taussig Cancer Institute.
American Society of Hematology. (1). Case Study: Prognostic Factors in Acute Lymphocytic Leukemia. Retrieved from https://www.hematology.org/education/trainees/fellows/case-studies/acute-lymphocytic-leukemia .
American Society of Hematology. "Case Study: Prognostic Factors in Acute Lymphocytic Leukemia." Hematology.org. https://www.hematology.org/education/trainees/fellows/case-studies/acute-lymphocytic-leukemia (label-accessed April 14, 2024).
"American Society of Hematology." Case Study: Prognostic Factors in Acute Lymphocytic Leukemia, 14 Apr. 2024 , https://www.hematology.org/education/trainees/fellows/case-studies/acute-lymphocytic-leukemia .
Citation Manager Formats
- Case report
- Open access
- Published: 11 April 2022
A challenging case of an adolescent and young adult patient with high-risk acute lymphoblastic leukemia: the need for a multidisciplinary approach: a case report
- Izabela Kranjčec ORCID: orcid.org/0000-0003-2860-5805 1 ,
- Nuša Matijašić 1 ,
- Slaven Abdović 2 ,
- Iva Hižar Gašpar 3 ,
- Lavinia La Grasta Sabolić 4 &
- Filip Jadrijević-Cvrlje 1
Journal of Medical Case Reports volume 16 , Article number: 147 ( 2022 ) Cite this article
2387 Accesses
2 Citations
1 Altmetric
Metrics details
Adolescents and young adults diagnosed with acute lymphoblastic leukemia are treated according to pediatric-based regimens to achieve better results. However, implementation of intensive chemotherapy protocols in this age group is associated with increased treatment-related toxicities, affecting almost every organ and system. In this case, the focus of our interest was on rather rare entities: steroid-induced psychosis that seldom develops in children and adolescents, and choroid plexus hemosiderosis, infrequently identified as a first sign of iron overload.
Case presentation
The aim of this paper is to present a challenging case of a 15-year-old Caucasian male patient treated for high-risk acute lymphoblastic leukemia and who experienced various adverse incidents during intensive chemotherapy, thus necessitating a high-quality multidisciplinary approach. Slow minimal residual disease clearance was an additional concerning issue. Induction and re-induction were complicated by steroid-induced hyperglycemia that required multiple-week insulin. During consolidation, acute kidney injury on the basis of chronic kidney disease was verified, demanding subsequent drug dose modifications. By the end of re-induction, after dexamethasone cessation, infrequent steroid-induced psychosis, presented as incoherent speech, aggressive behavior, and mood swings, required intensive psychiatric support. Neurological evaluation of seizures revealed uncommon choroid plexus hemosiderosis by brain magnetic resonance imaging, warranting appropriate selection of iron chelation therapy in the context of preexisting nephropathy. Ultimately, iron deposits of moderate intensity were verified by liver magnetic resonance imaging, while heart tissue remained intact. The early diagnosis and adequate treatment of aforementioned difficult toxicities resulted in complete recovery of the patient.
Conclusions
Treating adolescents with high-risk acute leukemia and multiple therapy-related morbidities remains a challenge, even in the era of extensive and effective supportive therapy. Superior survival rates might be achieved by prompt recognition of both frequent and rarely encountered adverse episodes, as well as well-timed and appropriate management by a well-coordinated multidisciplinary team.
Peer Review reports
Adolescents and young adults (AYA) diagnosed with acute lymphoblastic leukemia (ALL) have faced poorer survival rates compared with the history of this illness treatment in children [ 1 ]. However, several European and US studies have reported improved outcomes for AYA patients treated with pediatric-based protocols [ 2 , 3 , 4 ]. however, AYA patients receiving pediatric regimens and doses, unlike children, have disproportionately increased toxicities affecting almost every organ and system [ 5 ], most likely due to pubertal changes, inadequate nutritional status, and altered drug metabolism [ 6 ]. The most common nonhematological toxicities in AYA patients during induction include hyperglycemia, febrile neutropenia, and transaminitis [ 3 ].
The aim of this paper is to present the case of an adolescent with high-risk ALL who experienced various adverse episodes throughout the intensive chemotherapy, including multiple frequent toxicities mentioned above. However, the focus of our interest is on rather rare entities, such as steroid-induced psychosis that seldom develops in children and adolescents, and choroid plexus hemosiderosis, infrequently identified as a first sign of iron overload.
A 15-year-old Caucasian male presented with painless cervical lymphadenopathy and excessive sweating. The patient’s family and psychosocial history was unremarkable. Moreover, no relevant past interventions were recorded in the adolescent’s medical history. Normocytic anemia (Hemoglobin 86 g/L Mean corpuscular volume 93.6fL), thrombocytopenia (Plt 49 × 10 9 /L), and blasts (36%) dominated in the peripheral blood. Bone marrow analysis by flow cytometry revealed the diagnosis of precursor B-ALL (60% of aberrant “common” B-cells by European Group for Immunological Classification of Leukemias (EGIL) classification; TdT+, CD19+, CD10+, CD79a+, citIgM−). A favorable hyperdiploid clone (55, XY, X, +4, +6, +10, +14, +17, +18, +21, +21/46, XY) was detected by classical cytogenetic technique (G-banding). PBX1 gene duplication and tetrasomy of chromosome 21 were verified by fluorescence in situ hybridization (FISH). Clonal IgH and T-cell receptor (TCR) gene rearrangements were confirmed by molecular analysis (real-time polymerase chain reaction). No unfavorable cytogenetic or molecular disease features (for example, bcr/ abl , KTM2A ) were discovered. Additionally, next-generation sequencing (NGS) investigation of the tumor DNA revealed NRAS and CBL mutations but without potential therapeutic implications. No leukocytes or blasts were discovered in cerebrospinal fluid, and initial brain magnetic resonance (MR) was normal, thus central nervous system (CNS) was free of disease (CNS1 status). Diagnostic assessment was carried out according to the protocol’s standards, and no special (for example, financial) work-up or therapeutic challenges were encountered.
Chemotherapy according to the ALL-Intercontinental Berlin–Frankfurt–Münster (IC BFM) 2009 protocol was initiated, consisting of induction (prednisone, vincristine, daunorubicin, PEG-asparaginase, intrathecal methotrexate), early intensification (cyclophosphamide, cytarabine, 6-mercaptopurine, intrathecal methotrexate), consolidation (combination of dexamethasone, vincristine, vindensine HD-cytarabine, HD-methotrexate, cyclophosphamide, ifosfamide, PEG-asparaginase, etoposide, intrathecal therapy), and re-induction therapy (dexamethasone, vincristine, doxorubicin, PEG-asparaginase, cyclophosphamide, cytarabine, 6-thioguanine), followed by maintenance (6-mercaptopurine, methotrexate). While good prednisone response (peripheral absolute blast count < 1000/µL) was achieved by day 8 (peripheral absolute blast count 237/µL), flow cytometry minimal residual disease (FC-MRD) on day 15 and 33 was 28.9% and 0.03%, respectively. Solely due to high FC-MRD percentage of blasts (> 10%) on day 15, the patient was classified into high-risk (HR) disease group. Persistent minimal residual disease (MRD) (0.0012%) was detected by day 78, no MRD (0%) status was achieved prior to second high-risk block (consolidation), and the patient remained disease-free through further intensive chemotherapy course. Following the decision of the national transplantation team, the patient was not eligible for allogeneic hematopoietic transplantation.
Throughout the 10-month intensive chemotherapy, the patient experienced multiple toxicities of various degrees. Treatment-related adverse events of moderate to higher grade, according to the Common Terminology Criteria for Adverse Events (CTCAE) v4.03, are listed in Table 1 . The most troublesome complications warranting multidisciplinary approach are described in more detail below.
Endocrine system
Hyperglycemia (serum glucose 12.1 mmol/L) was first noted on the third day of induction, during increase of prednisone dose (beginning with 25% of the calculated dose, 25% daily increments, full dose of 60 mg/m 2 /day reached on the 4th day), when nutritional advice was sought. As serum glucose levels (17.3 mmol/L) had risen additionally by day 9, intensive insulin therapy was initiated, intermittent-scanning continuous glucose monitoring system was applied, and education of the patient and his mother was performed in detail. Further workup (Glycated hemoglobin, C-peptide, diabetes related autoantibodies) excluded the possibility of type 1 diabetes, and hyperglycemia had resolved after 31 days of insulin therapy. Short-term steroid use (dexamethasone 20 mg/m 2 /day over 5 days) during consolidation demanded solely nutritional adjustments. During the re-induction, hyperglycemia (serum glucose 14.5 mmol/L) appeared the third day of dexamethasone use (10 mg/m 2 /day), necessitating multiple daily insulin injections (basal-bolus regimen) for 34 days. Adrenal insufficiency (cortisol 63 nmol/L) and central hypothyroidism (triiodothyronine < 0.80 nmol/L, thyroxine 47 nmol/L, thyroid stimulating hormone 0.04 mU/L) were detected by the end of the fourth week of induction and third week of steroid therapy in re-induction, warranting 2-week hormone replacement therapy (levothyroxine, hydrocortisone) with prolonged tapering.
Renal system
As evaluated by Pediatric Risk, Injury, Failure, Loss, End Stage Renal Disease (pRIFLE) criteria [ 7 ], our patient developed acute kidney injury (AKI) on three occasions, details of which are presented in Fig. 1 .
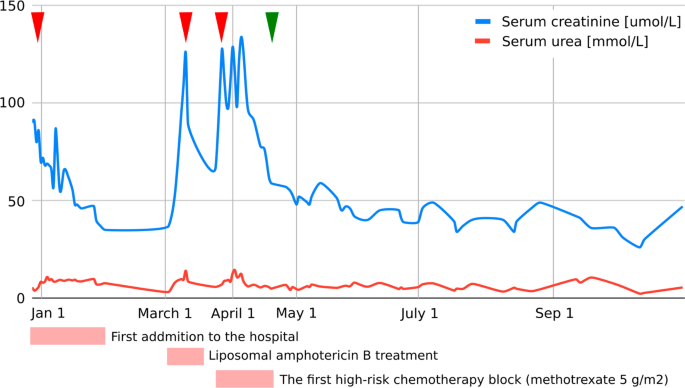
Graphic presentation of the renal function (serum creatinine, serum urea) during intensive treatment. First acute kidney injury was diagnosed when the patient was initially admitted to the hospital with creatinine levels of 90 µmol/L, which decreased to reference values for age with an intensive rehydration regimen (left arrowhead). At that time, kidney morphology was evaluated with ultrasound, which showed normal dimensions and echomorphology without dilatation of the urinary tract. Second (middle arrowhead) and third episodes (right arrowhead) were classified as acute kidney failure and occurred during liposomal amphotericin B treatment and during the first high-risk chemotherapy block when a significant delay (198-hour) in high-dose methotrexate (5 g/m 2 ) metabolite excretion was noticed, resulting in transient rise of creatinine and cystatin C levels up to 125 µmol/L and 2.36 g/L, respectively (estimated Glomerula Filtration Rate 30 mL/min/1.73 m 2 ). Creatinine levels returned to normal when replacing amphotericin B with voriconazole and monitoring complete methotrexate elimination. Apart from urine alkalinization, increased hydration, and administration of leucovorin, no other treatments were necessary to resolve acute kidney injury. Renal Tc-99m Diethyl Triamine Penta-Acetic scintigraphy scan revealed decreased clearance of radiopharmaceutical material (75 mL/min/1.73 m 2 ), and chronic kidney disease grade 2 was diagnosed. The patient had previously (at age of 3) been followed by pediatric nephrologist due to congenital hydronephrosis, but renal function and morphology were reported normal. We presume the patient initially had reduced renal parenchymal reserve and was more prone to acute kidney injury during precipitating factors (dehydration and unadjusted drug doses). Further cytostatic and symptomatic therapy dose corrections (75% of the total methotrexate dose and avoidance of all nephrotoxic drugs) were consistently undertaken, and laboratory parameters carefully monitored (starting from green arrowhead), so no additional kidney function deterioration was observed
Nervous system and psychological status
One day after a 3-week dexamethasone course (10 mg/m 2 /day) with 1-week tapering, at the end of the first part of re-induction, a bizarre behavior pattern was observed. The patient’s speech was incoherent, and aggressive outbursts were replaced by manic-depressive mood swings. A sudden-onset qualitative consciousness disturbance accompanied by short tonic–clonic convulsions demanded prompt neurological evaluation. No electrolyte disorders, abnormal glucose levels, or high blood pressure readings were detected. Urine toxicological screening was negative. Urgent head computed tomography (CT) scan was unremarkable, and repeated electroencephalogram (EEG) recordings were normal. Magnetic resonance imaging (MRI) of the brain revealed choroid plexus hemosiderosis, providing no explanation for psychological status alteration. Polymerase chain reaction (PCR) encephalitis and meningitis panels (Borrelia, tick-borne encephalitis, herpes simplex virus type 1 and type 2, varicella-zoster virus, cytomegalovirus, Epstein-Barr virus, measles, mumps, Human herpesvirus 6) in cerebrospinal fluid were negative, as were autoimmune encephalitis autoantibodies. A child psychiatrist diagnosed the patient with steroid-induced psychosis and introduced medications (risperidone, promazine), along with intensive psychological support. Within a week, all symptoms ceased, and the patient’s psychological status remained stable even after the drugs’ discontinuation. No new cerebral events were described, and follow-up EEG and neurological status were satisfactory.
- Iron overload
Hemosiderosis, due to repeated blood transfusion, was revealed during MRI of the brain and confirmed with high ferritin levels and MRI of the liver (Fig. 2 ). The baseline ferritin level of 323 µg/L (serum iron 20 µmol/L, total iron-binding capacity 43 µmol/L, unsaturated iron-binding capacity 23 µmol/L) in our patient had risen to 5143 µg/L after 9 months of intensive chemotherapy and then spontaneously fallen to 2994 µg/L at 1 month after (ferritin reference range 10.3–55.8 µg/L). During intensive chemotherapy, the patient received a total of 43 doses of blood (red cell) transfusions. After only a month of chelation therapy (deferasirox 20 mg/kg/day), a significant decrease to 1664 µg/L was noted with no deterioration in kidney function observed.
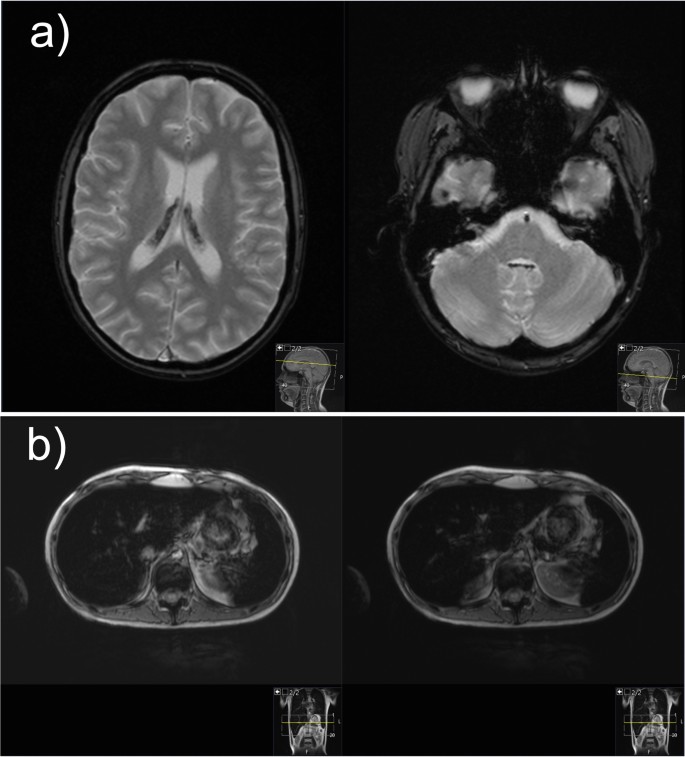
Magnetic resonance images of the brain and liver demonstrating iron overload. a Magnetic resonance imaging of the brain: axial T2-weighted gradient echo images demonstrate presence of hypointense hemosiderin deposits in the choroid plexus of both the lateral ventricles and fourth ventricle. b Magnetic resonance imaging of the liver: axial gradient echo sequences T2-weighted magnetic resonance image shows the liver hypointensity that is due to iron overload
Discussion and conclusions
B-precursor HR-ALL AYA patients are known to have inferior outcomes and increased treatment-related toxicities compared with children [ 8 ]. Superior outcomes in AYA patients are, however, achieved by implementing more intensive, pediatric-type protocols, with survival rates reaching 70% [ 9 ]. Lower event-free and survival rates in AYA patients are, among other factors, due to unfavorable tumor biology. The frequency of Philadelphia Chromosome positive acute lymphoblastic leukemia (Ph+ALL) and other HR abnormalities increases with age, in contrast to favorable cytogenetics in younger patients [ 9 ]. Although our patient displayed no disadvantageous genetic features, persistent MRD, known to be of extreme prognostic relevance, raised great concern. While MRD clearance, although slow, was still achieved in consolidation and allogeneic transplant avoided, a multitude of newly arising toxicities remained a challenge.
One in ten pediatric patients experiences hyperglycemia as a common side effect of ALL treatment [ 6 ]. Grade 3–4 hyperglycemia, a major concern in our patient throughout the treatment, was observed in almost 30% of AYA population treated with Children's Oncology Group (COG) pediatric-inspired chemotherapy regimens [ 10 ]. Higher proportion of steroid and asparaginase-related hyperglycemia in AYA patients might be the result of postpubertal hormonal changes, and given the former contradictory results, the correlation with infection predilection remains to be determined [ 6 ].
Although the frequency of febrile neutropenia (FN) in AYA patients is reported lower compared with younger individuals, our patient developed fever during hematologic aplasia in every stage of intensive chemotherapy. However, an association to hyperglycemia was not apparent [ 8 ]. Nevertheless, malnutrition has been repeatedly described as a predisposing factor for FN [ 11 , 12 , 13 ].
Although less than 10% of AYA patients are malnourished at time of diagnosis, almost half of them experience more than 5% weight loss during cancer treatment [ 14 ]. Not only was our patient severely underweight (Body mass index, BMI 15.9 kg/m 2 ) when first faced with hematologic malignancy, but significant weight loss (14%) was also observed during induction. High-risk disease and hyperglycemia, both present in our patient, among other features, are recognized as risk factors for negative weight trend during induction [ 15 ]. However, an early dietitian referral and specialist gastroenterologist involvement, along with timely enteral nutrition and supplement introduction, resulted in desirable weight gain at the end of intensive chemotherapy regimen (+4 kg).
Hepatotoxicity, sometimes severe, is a common side effect of contemporary pediatric ALL regimens, in one-fourth of cases occurring during induction, with obesity and age (> 15 years) being regarded as risk factors [ 16 ]. Transitory rise in transaminases in our patient followed every administration and was related to PEG-asparaginase exposure but never required any specific interventions nor treatment postponement (max ALT 342 U/L, AST 265 U/L, GGT 482 U/L). Other PEG-asparaginase attributable toxicities, such as hypersensitivity reactions, pancreatitis, and thromboembolic events, were not described in our patient [ 17 ]. However, therapeutic drug monitoring (TDM) was performed and dose modification conducted, possibly decreasing the occurrence of asparaginase-related adverse events.
Increased risk of high-dose methotrexate (MTX) renal toxicity was found to be correlated with delayed MTX elimination [ 18 , 19 ]. Since serum creatinine levels and concentration of MTX after 48 hours had excellent value in predicting AKI, with area under the curve (AUC) of 89.2% and 96.8%, respectively, it is necessary to follow-up these values and initiate intravenous hydration, urine alkalization, and if necessary, renal replacement therapy on time.
Patients with HR-ALL are at higher risk for iron overload, accompanied by endocrine and liver dysfunction, compared with other risk groups, yet no regular iron status monitoring is routinely performed in many pediatric oncology centers [ 20 , 21 ], a practice that our center should consider implementing. Accumulation of iron in the liver correlates with the amount of transfused iron, occurring rather early, after as much as ten transfusions, while for the iron to be loaded in the heart and endocrine organs, high transferrin saturations are needed [ 22 ]. Moreover, choroid plexus iron depositions, at any stage of treatment, have rarely been described in literature [ 23 ]. In our patient, the peak ferritin level correlated with neurological and psychological deterioration and characteristic brain MRI findings of iron overload (Fig. 2 ). Iron deposits of moderate intensity were verified by liver MRI, while heart tissue remained intact. Hereditary hemochromatosis gene (HFE) mutations, which aggravate iron overload in ALL patients, were not detected in our case [ 24 ]. Hepatic dysfunction, dysglycemia, and endocrine disorders, such as primary thyroid gland hypofunction, are organ abnormalities commonly related to hemosiderosis in literature [ 25 ]. Occasional hepatotoxicity, central hypothyroidism, and hypocortisolism in our patient were not considered to be related to hemosiderosis, as explained above, but preexisting nephropathy played an important role in iron chelation selection. Orally active once-daily deferasirox is a frequently preferred iron chelator, especially in the outpatient setting [ 25 , 26 ], usually being well tolerated [ 27 ], as in our case. Nevertheless, regarding clinical presentation, neurological symptomatology could not be interpreted based on choroid plexus hemochromatosis, as it is mostly asymptomatic [ 23 ], so further elucidation was sought.
Steroid-induced psychosis, a variety of neuropsychiatric symptoms related to glucocorticoid use, is frequently described in adult populations rather than children, with fewer than 20 cases reported worldwide [ 28 ]. All routes of corticosteroid administration (oral, intravenous, inhalation) at any time point of treatment may provoke psychotic symptoms, but clear risk factors (for example, type and dose of glucocorticoid) have not yet been established [ 29 ]. Hippocampal injury caused by glucocorticoids, resulting in behavioral and emotional dysfunction, in pediatric patients with cancer might be aggravated by synergistic toxicity of other chemotherapeutic agents [ 30 ]. The hallucinations that arose in our patient with negative personal and family history of psychiatric disorders and that caused him significant stress and impairment were associated with recent steroid exposure, while infection, severe electrolyte, and serum glucose disorders were ruled out. Combination of an antipsychotic drug (for example, haloperidol) with steroid dose reduction or discontinuation is generally an effective treatment strategy [ 31 ]. Risperidone, a preferred antipsychotic in literature [ 28 , 32 ], was also our child psychiatrist’s medication of choice, leading to complete symptom resolution. An optimal medicamental prophylactic approach (for example, carbamazepine, chlorpromazine, etc.) still needs to be determined [ 31 ].
In conclusion, treating an AYA patient with high-risk leukemia and multiple therapy-related morbidities remains a challenge, even in the era of abundant and effective supportive treatment. A timely and appropriate multidisciplinary approach is mandatory to ensure no significant delays, and modification in scheduled therapy is required, late effects diminished, and quality of life preserved, to achieve optimal treatment outcomes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Acute kidney injury
Acute lymphoblastic leukemia
Acute Lymphoblastic Leukemia Intercontinental Berlin–Frankfurt–Münster
Alanine aminotransferase
Aspartate aminotransferase
Adolescents and young adults
Body mass index
Central nervous system
Children's Oncology Group
Computed tomography
Common Terminology Criteria for Adverse Events
Diethyl Triamine Penta-Acetic scintigraphy
Electroencephalogram
Estimated glomerula filtration rate
European Group for Immunological Classification of Leukemias
Fluorescence in situ hybridization
Gamma-glutamyl transferase
Gradient echo sequences
Febrile neutropenia
Flow cytometry minimal residual disease
Hereditary hemochromatosis
Magnetic resonance
Minimal residual disease
Magnetic resonance imaging
Methotrexate
Polymerase chain reaction
Philadelphia Chromosome positive acute lymphoblastic leukemia
Pediatric Risk, Injury, Failure, Loss, End Stage Renal Disease
Therapeutic drug monitoring
Wolfson JA, Richman JS, Sun CL, Landier W, Leung K, Smith EP, et al . Causes of inferior outcome in adolescents and young adults with acute lymphoblastic leukemia: across oncology services and regardless of clinical trial enrollment. Cancer Epidemiol Biomark Prev. 2018;27(10):1133–41. https://doi.org/10.1158/1055-9965.EPI-18-0430 .
Article Google Scholar
Rytting ME, Jabbour EJ, Jorgensen JL, Ravandi F, Franklin AR, Kadia TM, et al . Final results of a single institution experience with a pediatric-based regimen, the augmented Berlin-Frankfurt-Münster, in adolescents and young adults with acute lymphoblastic leukemia, and comparison to the hyper-CVAD regimen. Am J Hematol. 2016;91(8):819–23. https://doi.org/10.1002/ajh.24419 .
Article PubMed PubMed Central Google Scholar
Stock W, Luger SM, Advani AS, Yin J, Harvey RC, Mullighan CG, et al . A pediatric regimen for older adolescents and young adults with acute lymphoblastic leukemia: results of CALGB. Blood. 2019;133(14):1548–59. https://doi.org/10.1182/blood-2018-10-881961 ( published correction appears in Blood . 2019;134(13):1111 ).
Article CAS PubMed PubMed Central Google Scholar
Siegel SE, Stock W, Johnson RH, Advani A, Muffly L, Douer D, et al . Pediatric-inspired treatment regimens for adolescents and young adults with Philadelphia chromosome-negative acute lymphoblastic leukemia: a review. JAMA Oncol. 2018;4(5):725–34. https://doi.org/10.1001/jamaoncol.2017.5305 .
Gupta A, Damania RC, Talati R, O’Riordan MA, Matloub YH, Ahuja SP. Increased toxicity among adolescents and young adults compared with children hospitalized with acute lymphoblastic leukemia at children’s hospitals in the United States. J Adolesc Young Adult Oncol. 2021;10(6):645–53. https://doi.org/10.1089/jayao.2020.0154 .
Article PubMed Google Scholar
Gramatges MM, Rabin KR. The adolescent and young adult with cancer: state of the art—acute leukemias. Curr Oncol Rep. 2013;15(4):317–24. https://doi.org/10.1007/s11912-013-0325-5 .
Bresolin N, Bianchini AP, Haas CA. Pediatric acute kidney injury assessed by pRIFLE as a prognostic factor in the intensive care unit. Pediatr Nephrol. 2013;28(3):485–92. https://doi.org/10.1007/s00467-012-2357-8 .
Larsen EC, Salzer W, Nachman J, Devidas M, Freyer DR, Raetz EA, et al . Treatment toxicity in adolescents and young adult (AYA) patients compared with younger patients treated for high risk B-precursor acute lymphoblastic leukemia (HR-ALL): a report from the children’s oncology group study AALL0232. Blood. 2011;118(21):1510. https://doi.org/10.1182/blood.V118.21.1510.1510 .
Carobolante F, Chiaretti S, Skert C, Bassan R. Practical guidance for the management of acute lymphoblastic leukemia in the adolescent and young adult population. Ther Adv Hematol. 2020;11:2040620720903531. https://doi.org/10.1177/2040620720903531 .
Advani AS, Sanford B, Luger S, Devidas M, Larsen EC, Liedtke M, et al . Frontline-treatment of acute lymphoblastic leukemia (ALL) in older adolescents and young adults (AYA) using a pediatric regimen is feasible: toxicity results of the prospective US intergroup trial C10403 (alliance). Blood. 2013;122(21):3903. https://doi.org/10.1182/blood.V122.21.3903.3903 .
Agnes M, Widjajanto P, Damayanti W. Impact of malnutrition on febrile neutropenia in children with acute lymphoblastic leukemia during induction phase chemotherapy. Paediatr Indones. 2018;58(6):298–304. https://doi.org/10.14238/pi58.6.2018.298-304 .
Sonowal R, Gupta V. Nutritional status in children with acute lymphoblastic leukemia, and its correlation with severe infection. Indian J Cancer. 2021;58(2):190–4.
PubMed Google Scholar
Ramamoorthy JG, Radhakrishnan V, Ganesan P, Dhanushkodi M, Ganesan TS, Sagar TG. Malnutrition is a predisposing factor for developing recurrent fever following febrile neutropenia in children with acute lymphoblastic leukemia. Pediatr Hematol Oncol J. 2020;5(3):75–9. https://doi.org/10.1016/j.phoj.2020.06.002 .
van der Haak N, Edwards S, Perem M, Landorf E, Osborn M. Nutritional status at diagnosis, during, and after treatment in adolescents and young adults with cancer. J Adolesc Young Adult Oncol. 2021;10(6):668–74. https://doi.org/10.1089/jayao.2020.0197 .
Hill R, Hamby T, Johnson D, Boren C, Downs H, Ray A. Prevalence and predictors of weight loss during induction therapy for childhood acute lymphoblastic leukemia. Nutrition. 2021;81: 110937. https://doi.org/10.1016/j.nut.2020.110937 .
Denton CC, Rawlins YA, Oberley MJ, Bhojwani D, Orgel E. Predictors of hepatotoxicity and pancreatitis in children and adolescents with acute lymphoblastic leukemia treated according to contemporary regimens. Pediatr Blood Cancer. 2018;65(3): e26891. https://doi.org/10.1002/pbc.26891 .
Article CAS Google Scholar
Rytting ME, Jabbour EJ, O’Brien SM, Kantarjian HM. Acute lymphoblastic leukemia in adolescents and young adults. Cancer. 2017;123(13):2398–403. https://doi.org/10.1002/cncr.30624 .
Cheng DH, Lu H, Liu TT, Zou XQ, Pang HM. Identification of risk factors in high-dose methotrexate-induced acute kidney injury in childhood acute lymphoblastic leukemia. Chemotherapy. 2018;63(2):101–7. https://doi.org/10.1159/000486823 .
Article CAS PubMed Google Scholar
Li H, Xu Q, Wang Y, Chen K, Li J. Serum neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for predicting high dose methotrexate associated acute kidney injury in children with acute lymphoblastic leukemia. Cancer Chemother Pharmacol. 2020;85(1):95–103. https://doi.org/10.1007/s00280-019-03980-6 .
Cacciotti C, Athale U. Transfusion-related iron overload in children with leukemia. J Pediatr Hematol Oncol. 2021;43(1):18–23. https://doi.org/10.1097/MPH.0000000000001849 .
Eng J, Fish JD. Insidious iron burden in pediatric patients with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2011;56(3):368–71. https://doi.org/10.1002/pbc.22851 .
Reitman AJ, Coates TD, Freyer DR. Early cardiac iron overload in a child on treatment of acute lymphoblastic leukemia. Pediatrics. 2015;136(3):e697–700. https://doi.org/10.1542/peds.2014-3770 .
Kim MS, Lee HY, Lim MK, Kang YH, Kim JH, Lee KH. Transfusional iron overload and choroid plexus hemosiderosis in a pediatric patient: brain magnetic resonance imaging findings. Investig Magn Reson Imaging. 2019;23(4):390–4. https://doi.org/10.13104/imri.2019.23.4.390 .
El-Rashedi FH, El-Hawy MA, El-Hefnawy SM, Mohammed MM. HFE gene mutation and iron overload in Egyptian pediatric acute lymphoblastic leukemia survivors: a single-center study. Hematology. 2017;22(7):398–404. https://doi.org/10.1080/10245332.2017.1289324 .
Yassin MA, Soliman A, De Sanctis V, Hmissi SM, Abdulla MAJ, Ekeibed Y, et al . The impact of iron overload in patients with acute leukemia and myelodysplastic syndrome on hepatic and endocrine functions. Acta Biomed. 2018;89(3-S):18–22. https://doi.org/10.23750/abm.v89i3-S.7213 .
Olcay L, Hazirolan T, Yildirmak Y, Erdemli E, Terzi YK, Arda K, et al . Biochemical, radiologic, ultrastructural, and genetic evaluation of iron overload in acute leukemia and iron-chelation therapy. J Pediatr Hematol Oncol. 2014;36(4):281–92. https://doi.org/10.1097/MPH.0b013e3182a11698 .
Poggiali E, Cassinerio E, Zanaboni L, Cappellini MD. An update on iron chelation therapy. Blood Transfus. 2012;10(4):411–22. https://doi.org/10.2450/2012.0008-12 .
Hodgins GE, Saltz SB, Gibbs EP, Gonzalez R, Regan J, Nemeroff C. Steroid-induced psychosis in the pediatric population: a new case and review of the literature. J Child Adolesc Psychopharmacol. 2018;28(5):354–9. https://doi.org/10.1089/cap.2018.0017 .
Stuart FA, Segal TY, Keady S. Adverse psychological effects of corticosteroids in children and adolescents. Arch Dis Child. 2005;90(5):500–6. https://doi.org/10.1136/adc.2003.041541 .
Hochhauser CJ, Lewis M, Kamen BA, Cole PD. Steroid-induced alterations of mood and behavior in children during treatment for acute lymphoblastic leukemia. Support Care Cancer. 2005;13(12):967–74. https://doi.org/10.1007/s00520-005-0882-8 .
Huynh G, Reinert JP. Pharmacological management of steroid-induced psychosis: a review of patient cases. J Pharm Technol. 2021;37(2):120–6. https://doi.org/10.1177/8755122520978534 .
Bag O, Erdoğan I, Onder ZS, Altinoz S, Ozturk A. Steroid-induced psychosis in a child: treatment with risperidone. Gen Hosp Psychiatry. 2012;34(1):103.e5-103.e6. https://doi.org/10.1016/j.genhosppsych.2011.09.003 .
Download references
Acknowledgements
Not applicable.
No funding was received for this article.
Author information
Authors and affiliations.
Department of Oncology and Hematology, Children’s Hospital Zagreb, Klaićeva 16, 10000, Zagreb, Croatia
Izabela Kranjčec, Nuša Matijašić & Filip Jadrijević-Cvrlje
Division of Nephrology, Department of Pediatrics, Children’s Hospital Zagreb, Zagreb, Croatia
Slaven Abdović
Department of Pediatrics, Children’s Hospital Zagreb, Zagreb, Croatia
Iva Hižar Gašpar
Department of Pediatric Endocrinology, Diabetes and Metabolism, University Hospital Center Sestre milosrdnice, Zagreb, Croatia
Lavinia La Grasta Sabolić
You can also search for this author in PubMed Google Scholar
Contributions
IK and NM undertook patient care, designed this case report, obtained informed consent, and prepared and wrote the manuscript. SA undertook patient care, analyzed and interpreted the patient’s data, and wrote the manuscript. IHG helped draft and edited the manuscript, and performed literature review. LLS helped draft and revise the manuscript. FJC produced the images used in the manuscript and helped draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Izabela Kranjčec .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kranjčec, I., Matijašić, N., Abdović, S. et al. A challenging case of an adolescent and young adult patient with high-risk acute lymphoblastic leukemia: the need for a multidisciplinary approach: a case report. J Med Case Reports 16 , 147 (2022). https://doi.org/10.1186/s13256-022-03366-y
Download citation
Received : 28 January 2022
Accepted : 10 March 2022
Published : 11 April 2022
DOI : https://doi.org/10.1186/s13256-022-03366-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute lymphoid leukemia
- Hyperglycemia
- Chronic kidney diseases
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Leukemia Case Study (60 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mr. Devito is a 48-year-old male who presents to his Primary Care Provider with left upper abdominal pain and complaints of weakness and fatigue. The nurse immediately notes how pale his skin is. A full set of vital signs reveals the following:
BP 142/90 mmHg
SpO 2 94% on Room Air
Temp 101.0°F
What furtner nursing assessments would you perform at this time?
- Heart and lung sounds
- Assess abdomen and review details of abdominal pain (OLDCARTS)
- Assess skin condition (color, quality, turgor, etc.)
- Peripheral perfusion (pulses, cap refill, etc.)
Upon further assessment, the nurse notes a palpable mass in the left upper quadrant, possibly an enlarged spleen, that is tender on palpation. The nurse also notes petechiae and bruising to the patient’s arms and legs. When questioned, the patient says “I seem to bruise so easily these days”. The patient’s lungs have diffuse crackles, heart sounds S1 and S2 present with no murmurs. The patient also reports a slight headache.
What laboratory or diagnostic tests do you anticipate the provider ordering?
- Complete Blood Count (to check for wbc – infection and reason for bruising)
- Full chemistry to ensure no electrolyte abnormalities or renal involvement
- Coagulation studies to determine cause of easy bruising
- Chest X-ray and sputum culture to identify source of infection
The provider orders a complete blood count, chemistry panel, and chest x-ray. The chest x-ray shows the patient has a slight pneumonia. He is sent home with a course of antibiotics while awaiting the test results.
The next day, the lab results show the following:
RBC 4.2 BUN 22
Hgb 8.4 Cr 0.9
Hct 25.2 K 3.9
WBC 144,000 Na 148
Plt 40,000 Ca 7.6
Based on the above lab results, what should the nurse be most concerned about?
- The patient has EXCESSIVE amounts of white blood cells. It would be expected for them to be slightly elevated because of the infection, but this is WAY beyond that.
- The patient is also anemic, with low platelets – this could explain the easy bruising
What do you believe may be going on, physiologically, with Mr. Devito?
- The excessive amounts of White Blood Cells, plus the easy bruising, anemia, and enlarged spleen point to some type of Leukemia.
- The body is excessively making immature, non-functioning white blood cells – hence the patient being susceptible to a pneumonia.
What further diagnostic testing should be performed to confirm a diagnosis?
- A bone marrow biopsy must be done to confirm a leukemia diagnosis
- The provider calls Mr. Devito and explains the results. They set an appointment for Mr. Devito to have a bone marrow biopsy. Biopsy results confirm Mr. Devito has Acute Myeloid Leukemia. Mr. Devito’s wife says “I don’t understand, I thought you said he just had pneumonia?”
How would you explain this to the patient’s wife?
- Leukemia causes the body to make a bunch of immature, non-functioning white blood cells. So when a patient gets an infection, like a respiratory infection, the body’s white blood cells can’t actually fight it off. So it’s common for patients to be prone to infections like pneumonia.
- Mr. Devito DID have pneumonia – but it was due to the poor immune response caused by the Leukemia.
Mr. Devito will be started on high-dose chemotherapy.
What education topics should be included in teaching for Mr. Devito and his wife?
- Mr. Devito will have a special port implanted in order to receive his chemotherapy
- Mr. Devito will likely also receive medications to manage the symptoms of the chemotherapy
- Mr. Devito may lose his hair, depending on the type of chemotherapy used, because chemo also kills healthy fast-growing cells
- Mr. Devito May experience something called neutropenia. This means he will be highly susceptible to infections. He should avoid having lots of visitors, avoid fresh flowers, and especially avoid being around anybody who is sick. He can even wear a mask in public if he so desires.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions

Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Finished Papers

Bennie Hawra

- Paraphrasing
- Research Paper
- Research Proposal
- Scholarship Essay
- Speech Presentation
- Statistics Project
- Thesis Proposal
Jam Operasional (09.00-17.00)
+62 813-1717-0136 (Corporate) +62 812-4458-4482 (Recruitment)
Our Top Proficient Writers At Your Essays Service
What can you help me with.
No matter what assignment you need to get done, let it be math or English language, our essay writing service covers them all. Assignments take time, patience, and thorough in-depth knowledge. Are you worried you don't have everything it takes? Our writers will help with any kind of subject after receiving the requirements. One of the tasks we can take care of is research papers. They can take days if not weeks to complete. If you don't have the time for endless reading then contact our essay writing help online service. With EssayService stress-free academic success is a hand away. Another assignment we can take care of is a case study. Acing it requires good analytical skills. You'll need to hand pick specific information which in most cases isn't easy to find. Why waste your energy on this when they're so many exciting activities out there? Our writing help can also do your critical thinking essays. They aren't the easiest task to complete, but they're the perfect occasion to show your deep understanding of the subject through a lens of critical analysis. Hire our writer services to ace your review. Are you struggling with understanding your professors' directions when it comes to homework assignments? Hire professional writers with years of experience to earn a better grade and impress your parents. Send us the instructions, and your deadline, and you're good to go.
Accuracy and promptness are what you will get from our writers if you write with us. They will simply not ask you to pay but also retrieve the minute details of the entire draft and then only will ‘write an essay for me’. You can be in constant touch with us through the online customer chat on our essay writing website while we write for you.

Customer Reviews

Customer Reviews
Need a personal essay writer? Try EssayBot which is your professional essay typer.
- EssayBot is an essay writing assistant powered by Artificial Intelligence (AI).
- Given the title and prompt, EssayBot helps you find inspirational sources, suggest and paraphrase sentences, as well as generate and complete sentences using AI.
- If your essay will run through a plagiarism checker (such as Turnitin), don’t worry. EssayBot paraphrases for you and erases plagiarism concerns.
- EssayBot now includes a citation finder that generates citations matching with your essay.

What is the best essay writer?
The team EssaysWriting has extensive experience working with highly qualified specialists, so we know who is ideal for the role of the author of essays and scientific papers:
- Easy to communicate. Yes, this point may seem strange to you, but believe me, as a person communicates with people, he manifests himself in the texts. The best essay writer should convey the idea easily and smoothly, without overloading the text or making it messy.
- Extensive work experience. To start making interesting writing, you need to write a lot every day. This practice is used by all popular authors for books, magazines and forum articles. When you read an essay, you immediately understand how long a person has been working in this area.
- Education. The ideal writer should have a philological education or at least take language courses. Spelling and punctuation errors are not allowed in the text, and the meaning should fit the given topic.
Such essay writers work in our team, so you don't have to worry about your order. We make texts of the highest level and apply for the title of leaders in this complex business.
New on NCI’s Websites for April 2024
April 12, 2024 , by Daryl McGrath
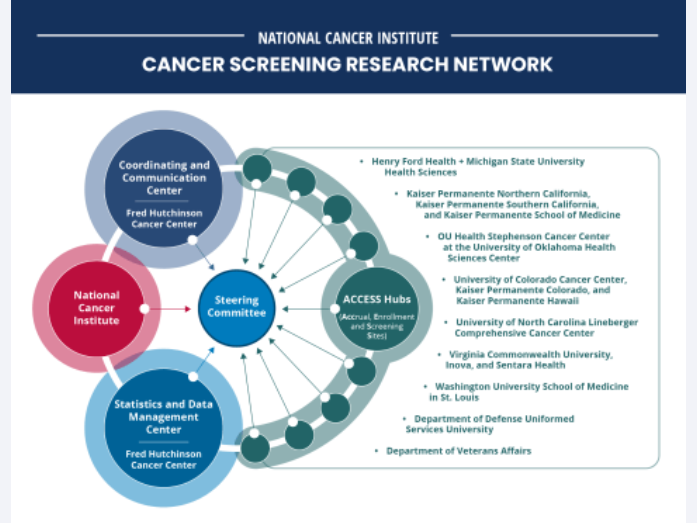
The Cancer Screening Research Network will conduct rigorous, multicenter cancer screening trials.
NCI’s collection of cancer information products is constantly growing, so periodically we provide updates on new and updated content of interest to the cancer community.
NCI Launches Research Network to Evaluate Emerging Cancer Screening Technologies
The Cancer Screening Research Network (CSRN) will support studies that investigate new ways to identify cancers earlier , when they may be easier to treat. In late 2024, CSRN plans to launch the Vanguard Study on Multi-Cancer Detection, a pilot study to inform the design of a larger trial of multi-cancer detection tests. Multi-cancer detection tests measure biomarkers, such as pieces of DNA, that cancer cells release into the blood and can potentially be used to detect many kinds of cancer.
For Childhood Cancer Survivors, Inherited Genetic Factors Influence Risk of Cancers Later in Life
Common inherited genetic factors that predict cancer risk in the general population may also predict elevated risk of new cancers among childhood cancer survivors , according to a study led by researchers at NCI.
NCI Launches Virtual Clinical Trials Office
NCI has launched the Virtual Clinical Trials Office , a centralized team of support staff—including research nurses, clinical research associates, and clinical data specialists—who will work remotely to assist NCI-Designated Comprehensive Cancer Centers and community practices with their clinical trials activities.
Meet the NCI Director Video
During a live social media event that took place February 22, NCI Director Kimryn Rathmell, M.D., Ph.D., introduced herself and answered live questions about the future of cancer research.
President’s Cancer Panel Issues Progress Report on the National Cancer Plan
On February 28, the President’s Cancer Panel released its I nitial Assessment of the National Cancer Plan . This report examines the National Cancer Plan as a road map for the National Cancer Program and offers recommendations in five priority areas to accelerate progress toward the plan’s goals.
Small Business Innovation Research Program
NCI’s Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) programs support small businesses across the United States to develop innovative cancer technologies. The SBIR Development Center has a new website that features the center’s SBIR Innovation Lab podcast , highlights success stories , and showcases companies chosen to pitch for funding at investor events.
Progress in Basic Cancer Research
NCI’s Division of Cancer Biology (DCB) features recent progress in advancing basic cancer research . A new infographic shows progress made in fiscal year 2023, highlights of recent research, and examples of DCB-sponsored research intended to help achieve the goals of the National Cancer Plan.
Center for Cancer Research Updates
NCI’s Center for Cancer Research (CCR) has added and updated several web pages. CCR’s training page for postdoctoral researchers features a new video explaining the benefits of postdoc training with NCI tenure-track investigators.
CCR also added a new chromosome biology research section to its website. The section includes a new web page for the NCI Center of Excellence in Chromosome Biology , information about specific researchers working on chromosome biology, and related fellowships and jobs in CCR.
CCR also has released its annual Milestones publication. The 10 stories highlighted in this year’s publication illustrate the breadth, creativity, and impact of CCR research.
Why We Love Diverse Data
NCI’s Center for Biomedical Informatics and Information Technology celebrated “Love Data Week!” (February 12–16) with a blog post featuring six scientists talking about why they love diverse data .
Inside Cancer Careers Podcast
NCI’s Center for Cancer Training has launched the second season of the Inside Cancer Careers podcast . The February 1 episode was a “fireside chat” with NCI Director Dr. Kimryn Rathmell , who shared her career journey and the importance of supporting the next generation of cancer researchers. The February 15 episode featured Ophira Ginsburg, M.D. , senior scientific officer and senior advisor for clinical research in NCI’s Center for Global Health, who gave her thoughts on the importance of women's leadership and representation in cancer care.
World Cancer Day 2024 Blog
NCI’s Center for Global Health (CGH) marked World Cancer Day with a blog post by CGH Director Satish Gopal, M.D., M.P.H. Dr. Gopal highlighted important accomplishments and activities in 2023, including CGH’s ongoing NCI Global Cancer Research and Control Seminar Series , NCI support and participation in the November 2023 African Organization for Research and Training in Cancer (AORTIC) meeting in Senegal, initiation of cancer health disparities minilabs to develop transdisciplinary approaches to advance scientific progress globally, and leadership and launch of the Lancet Commission on Women, Cancer, and Power .
NCI Office of Cancer Survivorship – New Resources
The NCI’s Office of Cancer Survivorship (OCS) has revamped its Cancer Survivor and Caregiver Stories page . Along with adding caregiver stories, the page also enables readers to filter stories—such as by cancer type and specific populations—to select those that will be most meaningful to them. Also new is a video library that includes videos sharing the words of advocates on survivorship-related topics and an FAQ with OCS Director Emily Tonorezos, M.D.
HINTS Brief 53 on Telehealth Use Among US Adults
The Health Information National Trends Survey (HINTS) Management Team has released HINTS Brief 53, “Patterns and Predictors of Telehealth Use among US Adults in 2022 .” This brief discusses the impact of the COVID-19 pandemic on the expansion of telehealth; the prevalence of, and factors associated with, telehealth use; and more.
Updated: Catchment Areas of NCI-Designated Cancer Centers
NCI’s Division of Cancer Control and Population Sciences updated its page on the Catchment Areas of NCI-Designated Cancer Centers , including designation status and catchment area updates for several cancer enters.
Co-Use of Tobacco with Alcohol and Cannabis
The NCI’s Behavioral Research Program has launched a new web page on the co-use of tobacco with alcohol and cannabis . This page, created by program directors in the Health Behaviors Research Branch and the Tobacco Control Research Branch, discusses the importance of addressing co-use of tobacco with alcohol and tobacco with cannabis as targets for cancer prevention and control.
Smokefree.gov Launches SmokefreeNATIVE
NCI’s Smokefree.gov initiative has partnered with the Indian Health Service to launch a new, free text messaging resource to help American Indian and Alaska Native adults and adolescents quit smoking commercial tobacco. People who smoke and are ready to set a date to quit can enroll online or by texting NATIVE to 47848.
Participate in Cancer Research
NCI has enhanced its information about participating in cancer research studies, including how to join clinical trials or observational studies and how to donate medical data and biological samples. The new Participate in Cancer Research section of NCI’s website includes information about cancer research studies , a clinical trials search tool , personal stories from people who have participated in studies, and more.
Lymphedema, the buildup of lymph fluid in tissues causing swelling, affects people’s ability to do certain activities and their quality of life. NCI has revised and consolidated its expert-reviewed content about ways to prevent and treat lymphedema .
The ALCHEMIST Lung Cancer Trials
The ALCHEMIST clinical trials are a group of randomized clinical trials for people with early-stage non-small cell lung cancer whose tumors have been completely removed by surgery. People entering the ALCHEMIST study will have their tumor tissue genetically sequenced to determine if one of the drugs being studied targets a specific biomarker, including certain genetic mutations, found in their tumors. This revised and streamlined page describes the different trials and which are currently recruiting participants.
Updated Fact Sheets
Tumor Markers : This updated fact sheet defines tumor markers and describes how they can be used to help diagnose and treat cancer. This revised and streamlined page also includes a list of tumor marker tests in common use .
Computed Tomography (CT) Scans and Cancer : This updated page explains what CT scans are, how they're used for cancer screening, diagnosis, and treatment, and what people can expect during the procedure.
New and Updated Patient Information Summaries
Skin Cancer Prevention : Skin cancer prevention includes avoiding risk factors like ultraviolet radiation that comes from the sun, sun lamps, and tanning beds. This updated expert-reviewed summary discusses the risks and possible protective factors for skin cancer.
Childhood Colorectal Cancer Treatment : Colorectal cancer is defined as a cancer that starts anywhere along the colon or rectum. Learn about risk factors, symptoms, and tests to diagnose colorectal cancer in children and how it is treated.
Depression : Depression is a treatable medical problem that can affect adults and children with cancer. This updated page describes symptoms of depression, risk factors, diagnosis, and treatment for adults and children with cancer.
Childhood Brain Tumors: NCI’s pages on DIPG (diffuse intrinsic pontine glioma) , childhood ependymoma , and childhood glioma (including astrocytoma) have a new look. The pages cover causes and risk factors, symptoms, screening, diagnosis, prognosis, stages, and treatment.
Spirituality and Cancer Care : Religion and spirituality in cancer care are very personal matters that can affect treatment decisions and the ability to cope. This updated page explains ways a person’s health care team can support their spiritual and religious well-being and how this can lead to improved health and quality of life.
Oral Complications of Cancer Therapies : Mouth and throat problems are common problems of cancer treatment. This updated page explains ways to prevent and manage problems like dry mouth, taste changes, pain, and infection.
Acute Myeloid Leukemia Treatment : Acute myeloid leukemia (AML) is a cancer that causes the rapid growth of abnormal white blood cells. These abnormal cells can replace healthy blood cells, leading to symptoms such as bleeding, anemia, and infection. This recently updated page includes information about the causes, symptoms, diagnosis, and treatment options for AML.
New Health Professional Summary: Hospice
Health care professionals and health care systems face many challenges when caring for patients at the end of life. This new page offers expert-reviewed information about many aspects of hospice care .
Chemotherapy and You : Support for People with Cancer
Chemotherapy and You is a booklet for people who are about to receive or are now receiving chemotherapy for cancer. It includes facts about chemotherapy and its side effects and highlights ways people can care for themselves before, during, and after treatment.
Infographic: Chances of Developing Breast Cancer by Age 70 to 80
Women who have harmful changes in certain genes have a higher risk of some cancers. This updated infographic helps explain the risk of breast cancer for women with harmful BRCA1 and BRCA2 mutations.
Featured Posts
February 22, 2024, by Carmen Phillips
January 23, 2024, by Elia Ben-Ari
January 12, 2024, by Shana Spindler
- Biology of Cancer
- Cancer Risk
- Childhood Cancer
- Clinical Trial Results
- Disparities
- FDA Approvals
- Global Health
- Leadership & Expert Views
- Screening & Early Detection
- Survivorship & Supportive Care
- February (6)
- January (6)
- December (7)
- November (6)
- October (7)
- September (7)
- February (7)
- November (7)
- October (5)
- September (6)
- November (4)
- September (9)
- February (5)
- October (8)
- January (7)
- December (6)
- September (8)
- February (9)
- December (9)
- November (9)
- October (9)
- September (11)
- February (11)
- January (10)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case Report
Case of relentless chronic phase of chronic myeloid leukaemia.
1 Department of Internal Medicine, University of Arizona Medical Center—University Campus, Tucson, Arizona, USA
2 Department of Pathology, University of Arizona Medical Center—University Campus, Tucson, Arizona, USA
Ravitharan Krishnadasan
3 Department of Hematology Oncology, University of Arizona Medical Center—University Campus, Tucson, Arizona, USA
Initial treatment of chronic phase chronic myeloid leukaemia is straightforward in today's era of tyrosine kinase inhibitors. However, managing refractory cases remain a major challenge due to the multiple factors that can influence decision-making, including medication tolerance, disease burden, mutation status, comorbidities, availability of donor, and fitness for an ablative conditioning. We report a male patient presenting with chronic phase chronic myeloid leukaemia who was treated with 5 different tyrosine kinase inhibitors either due to intolerance and/or failed response. He subsequently received 2 haploidentical haematopoietic stem cells transplants before achieving complete remission. This case highlights various treatment options, need for vigilant disease monitoring, and the possibility of complete positive response even after many lines of therapy failure.
Chronic myeloid leukaemia (CML) is a rare malignancy with incidence rate of 1.7 per 100 000 and mortality rate of 0.3 per 100 000 each year based on the data from 2008 to 2012. 1 A previously fatal disease, with a typical expected survival of only 2–3 years, has seen dramatic improvement since the introduction of tyrosine kinase inhibitor (TKI), imatinib, near the turn of the century. 2 Overall survival for 5 years is now over 60%. 1 CML is associated with the oncogene BCR/ALB1, and typically results from reciprocal translocation between chromosomes 9 and 22, t(9;22) (q34;q11) that subsequently gives rise to the Philadelphia (Ph) chromosome. 3 Protein product, such as p210 derived from this gene, exhibits deregulated tyrosine kinase activity that largely explains the success of imatinib. 4 Several other TKIs have since been developed, including second generation (nilotinib, dasatinib and bosutinib) and third generation (ponatinib), 5 allowing for multiple therapeutic options even after failure of a prior line of therapy. However, haematopoietic stem cells transplant (HSCT) remains an important treatment modality for patients who failed multiple TKIs or with advanced CML. We present a case of chronic phase CML (CP-CML) in which our patient achieved complete remission only after trying all five TKIs and receiving two haploidentical HSCTs. This is followed by a review of the treatment options and some of the difficulties in choosing treatment for CP-CML.
Case presentation
A previously healthy 53-year-old Hispanic man was diagnosed with CML in 2010. At that time, he presented with 6 months history of fatigue, general malaise and a 35 lb (16 kg) weight loss. Pertinent physical findings included mild tachycardia and palpation of an enlarged spleen extending ∼10 cm below the costophrenic angle.
Investigations
Laboratory workup ( table 1 ) revealed significant leukocytosis with white cell count of 307 000/μL, haemoglobin of 10.1 g/dL and platelet count of 429 000/μL. The differential was notable for bandemia 32%, blasts 5% and basophils 5%. CT abdomen/pelvis showed mild hepatomegaly and massive splenomegaly ( figure 1 ). He underwent a bone marrow biopsy (BMB) for further evaluation of his leukocytosis, with pathology revealing findings consistent with CML in chronic phase. Increased basophils, eosinophils, and bands along with myelocyte and metamyelocyte are evident on the marrow ( figure 2 A), with almost 100% marrow cellularity ( figure 2 B). Flow cytometric analysis showed a CD33+ and CD117+ myeloblast population, which is 2.3% of the gated events. Fluorescence in situ hybridisation analysis with BCR/ABL+9q34 showed evidence of 9;22 translocation resulting in the fusion of ABL1 with BCR in 169/200 cells scored (84.5%). Cytogenetic profiling revealed presence of the Ph chromosome: 46,XY,t(9;22) (q34;q11.2) [20].
Table 1
Initial laboratory work up
CBC, complete blood count; MCH, mean corpuscular haemoglobin; MCHC, mean cell haemoglobin concentration MCV, mean corpuscular volume; RBC, red blood cells.

CT scan of the chest/abdomen/pelvis showed mild hepatomegaly and massive splenomegaly (arrow).

(A) Increased basophils (red arrow), eosinophils (green arrow) and bands are evident on the bone marrow biopsy. (B) The marrow showed almost 100% cellularity.
Patient was started on hydroxyurea during his hospital stay and later transitioned to imatinib dosage of 400 mg daily. Two months after diagnosis, patient achieved complete haematological response with BMB at 6 months showing no morphological evidence of CML. However, Giemsa-banded study on the marrow continues to show all cells with Ph chromosome, which indicates persistence of the disease. Given the lack of complete cytogenetic response (CCyR) of 0% Ph+ CCyR and major molecular response (MMR) BCR/ABL/control gene ≤0.10 MMR by 9 months, imatinib was changed to dasatinib. Owing to a number of side effects, such as severe headaches, nausea, diarrhoea, fatigue, and persistence of Ph chromosome with 17/21 metaphases (80%) that remained positive for t9;22 on BMB 1-month later, the patient was started on nilotinib. Analysis for BCR/ABL kinase domain mutation was negative. About 1 year after being on nilotinib, patient's BCR/ABL p210 messenger RNA PCR showed a significant increase from 17% to 26%. He was switched to bosutinib for 1.5 years and subsequently changed to ponatinib due to intolerable diarrhoea. CCyR and MMR were never achieved on any of the TKIs. Mutational analysis failed to reveal any particular mutation as cause of TKI failure.
Five years after his initial diagnosis, patient decided to undergo haploidentical HSCT since a fully human leucocyte antigen matched donor was not available. He had a reduced intensity conditioning (RIC) regimen based on BMT CTN 1101 protocol (fludarabine 30 mg/m 2 ×5, cytoxan 14.5 mg/kg×2, total body irradiation (TBI) 200 Gy) and received marrow source 3.02×10 8 CD34+ cells (donor brother). Unfortunately, after initial engraftment at day +18, patient had disease relapse by day +30, confirmed by BMB. Second haploidentical HSCT with a different donor (sister) was performed 5 months later. During this second treatment therapy, he received a myeloablative regimen (fludarabine 30 mg/m 2 ×4, a total of TBI 9.9 Gy) 6 and 3.31×10 6 CD34+ cells). Day +30 BMB showed complete remission with 100% donor chimerism and p210<0.01% positive.
Outcome and follow-up
Figure 3 depicts the patient's disease and treatment course. He has been doing very well clinically, and is in remission for more than day +180 at the time of this report writing.

Patient achieved complete cytogenetic and molecular response after being on multiple tyrosine kinase inhibitors, and ultimately underwent two haploidentical stem cells transplantations. Each one of the green or yellow boxes represents a bone marrow biopsy. The p210 indicates normalised ratio of BCR/ABL1 (p210) to endogenous ABL1 messenger RNA with conversion to a percentage with reference to the international scale. Pink asterisk indicates patient received stem cells transplant consultation (12/2012); however, no fully human leucocyte antigen-matched donor was available. BMB, bone marrow biopsy; CML, chronic myeloid leukaemia; Haplo-SCT, haploidenticial stem cells transplant; NME, no morphological evidence; m, month(s); Ph+, Philadelphia chromosome positive; RIC, reduced intensity condition.
CML can be categorised into three phases, including chronic, accelerated, and blastic, which roughly represent the natural progression of the disease. 7 Classification is slightly different depending on the criteria used, but the main parameters are the percentage of blasts, counts in different cell lines, and presence of extramedullary manifestation. 3
There are five different TKIs approved by Food And Drug Administration with imatinib being the oldest medication, and has extensive long-term data regarding efficacy and toxicities. Dasatinib and nilotinib are also approved for first-line use based on the results from the DASISION trial (dasatinib vs imatinib) and the ENESTnd trial (nilotinib vs imatinib) showing earlier and deeper treatment responses in terms of MMR. 7 However, in both cases, there were no significant differences in survival compared to imatinib at 5 years follow-up. 8 Bosutinib is currently being evaluated under the BELA trial (bosutinib vs imatinib) with promising results at 2 years. 9 EPIC trial (ponatinib vs imatinib) was stopped prematurely due to unacceptable rates of arterial thrombotic events. 9
The widely followed European LeukemiaNet (ELN) recommendations outline their definition of the response to first-line TKI into three grades (optimal, warning and failure) 10 which help as a guide for when to change treatment ( table 2 ). For example, BCR/ABL1 <10% at 3 months, <1% at 6 months and <0.01% at 12 months would be considered as optimal responses. 10 Certain TKIs appear to be more effective in patients with certain BCR/ABL1 mutations. For instance, dasatinib is preferred in patients with Y253H, E255 or F359, while nilotinib is for F317 and V229. 11 Besides development of resistance to TKI, such as BCR/ABL1 kinase domain mutations that would prompt switching to a different TKI, side effects (which are rarely severe) are also an important consideration given the chronicity of consumption. 12 Therefore, selection of initial and salvage therapy should take into account the patient's BCR/ABL1 mutation status and comorbidities.
Table 2
ELN definition of the response to TKIs, first line 10 16
CCA/Ph+, clonal chromosome abnormality in Ph+ cells; CCyR, complete cytogenetic response; CHR, complete haematological response; ELN, European LeukemiaNet; MMR, major molecular response; NA, not applicable; PCyR, partial cytogenetic response; TKIs, tyrosine kinase inhibitors.
With the discovery of TKI, allogeneic HSCT in CP-CML became the therapy of last resort; however, it provides a lifesaving option for patients who had failed multiple TKIs. 13 Current recommendations suggest consideration of allogenic stem cell transplant (AlloSCT) consultation with donor search at first TKI failure for patients who are at high risk and fit to receive transplant. 14 Indications for allogeneic HSCT in chronic phase include high risk with first failure of imatinib, first failure of second generation TKI, failure of 2+ TKIs and T315L mutation. 14 Since CML occurs mostly in older patients, with median age at diagnosis being 64 years, 1 RIC regimen is frequently used for AlloSCT . However, it has a higher rate of relapse compared to myeloablative recipients. 14 The trade-off between taking the risk of progressing into blastic phase with dismal chances for recovery or early HSCT with the risk of immediate mortality can be a difficult reality for both the patient and the guiding physician. 13
In the case of our patient, imatinib was chosen as the first line treatment for his CP-CML given its time-tested therapeutic activity and safety profile. After inadequate response evident by his BMB, second generation TKI-dasatinib then nilotinib due to intolerable of side effects-was started as per guidelines. Meanwhile, BCR/ABL1 p210 was being closely monitored every 3–4 months as suggested by ELN. 10 A significant increase from 17.2% to 26.4% was noted after about 1.5 years on the therapy. Given this increase and the fact that patient was on his third TKI, he agreed to take a consultation with our transplant team. Unfortunately, no fully matched donor was available. Bosutinib and ponatinib were subsequently tried. While p210 had been decreasing, it never reached <0.1%. Patient ultimately decided to receive haploidentical HSCT knowing the risk and benefits involved. He was given RIC regimen since it is well known that CML consistently demonstrates graft-versus-leukaemia effect. 13 After the disease relapse, he received myeloablative haploidentical HSCT; 15 patient finally achieved complete remission since the disease was first diagnosed 5 years ago.
Learning points
- There are five different Food And Drug Administration-approved tyrosine kinase inhibitors (TKIs) available, and its selection depends on patient's stage of disease, mutation status, tolerance and comorbidities.
- Haematopoietic stem cells transplant continues to serve an important role for refractory chronic myeloid leukaemia.
- Haploidentical alternate donor options are routinely being used after multiple line of TKI failure.
- Close monitoring is required in order to change treatment when indicated in a timely manner.
- There is the possibility of complete response and subsequent cure even after many lines of therapy failure.
Acknowledgments
The authors would like to thank the patient for allowing us to share his unique case and the supporting staff at the Arizona Cancer Center.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Customer Reviews
Write an essay from varied domains with us!
My custom write-ups.
Perfect Essay
A writer who is an expert in the respective field of study will be assigned

1(888)499-5521
1(888)814-4206
A Case of Chronic Myeloid Leukemia
Recommended
More related content, what's hot, what's hot ( 20 ), viewers also liked, viewers also liked ( 14 ), similar to a case of chronic myeloid leukemia, similar to a case of chronic myeloid leukemia ( 20 ), more from stanley medical college, department of medicine, more from stanley medical college, department of medicine ( 20 ), recently uploaded, recently uploaded ( 20 ).
- 1. BY DR.ANIRUDH J SHETTY PROF.DR.G.ELANGOVAN’S UNIT
- 2. 28 yr male patient came with c/o abdominal pain-1 week in duration involving predominantly the left upper and centre of the abdomen vague dragging pain assoc with fullness of abd no h/o any aggravating or relieving factors
- 3. h/o early satiety + h/o loss of appetite + No h/o loss of weight No h/o jaundice No h/o haematemesis No h/o altered bowel habits No h/o bleeding tendencies
- 4. PAST h/o -> No h/o Tb/HTN/DM PERSONAL h/o -> consumes alcohol occasionally not a smoker
- 5. O/E – Pt conscious oriented afebrile anemic no Cyanosis,clubbing,icterus, lymphadenopathy B.P-110/70 mmHG P.R -80 min
- 6. P/A –mild distention of abdomen+ no dialated viens,scars or sinuses massive spleenomegaly(+) crossing the umbilicus no hepatomegaly no FF+
- 7. CVS – S1S2(+) NO murmurs RS – NVBS+ no added sounds CNS - NFND
- 8. CBC Hb – 14 TC – 9300 P69,L31 ESR – 15 PLATLETS – 1,50,000 RFT RBS -152 UREA – 32 CREAT – 1.0 SODIUM; 135 K+ - 6.0 CL – 105 HCO- 19
- 9. ECG – WNL CHEST X – RAY - WNL
- 12. CBC TC – 1,60,000 SHIFT TO LEFT BLAST 1% HB – 9.2 PLATLET -1,80,000 Chronic phase of CML P/S Markedly increased TC, showsMYELOBLAST,PR OMYELOCYTE,METAMY ELOCYTE,BAND FORMS
- 15. BONE MARROW FRAGMENT SHOWING A DENSLLY CELLULAR MARROW FRAGMENT WITH ABSENT FAT CELLS
- 17. LOW POWER MICROSCOPE: MYELOID HYPERPLASIA WITH RELATIVELY REDUCED ERYTHROID PROGENITORS
- 21. Patient was started on Imatinib mesylate 400mg 1-0-0
- 24. CML accounts for 15% of all cases of leukemia. More common in men Peak incidence : fourth and fifth decade
- 26. In CML the c-ABL gene is translocated from its normal abode on chromosone 9 to chromosone 22,where it fuses with bcr gene. As a consequence of the fusion, c-ABL loses a region that controls tyrosine kinase activity. Thus the BCR-ABL protien,the product of the fusion gene has potent and constitutive tyrosine kinase activity.
- 28. 1. CHRONIC PHASE 2. ACCELARATED PHASE 3. BLAST CRISIS
- 29. EASY FATIGABILITY DECREASE TOLERANCE TO EXERTION ABDOMINAL DISCOMFORT AND EARLY SATIETY( DUE TO SPLENIC ENLARGEMENT) WIEGHT LOSS AND EXCESSIVE SWEATING The symptoms are vague, nonspecific and gradual in onset
- 30. A physical examination may detect pallor and splenomegaly.The latter was present in 90% of patients. UNCOMMON PRESENTATIONS : Dramatic hypermetabolism(night sweats,wt loss,heat intolerance) Acute gouty arthritis(due to hyperurecemia) Priapism,tinnitus Lt upper quadrant n lt shoulder pain due to splenic infarction and perisplenitis.
- 31. CML is often suspected on the basis on the complete blood count, which shows increased granulocytes of all types, typically including maturemyeloid cells. Basophils and eosinophils are almost universally increased; this feature may help differentiate CML from a leukemoid reaction. A bone marrow biopsy is often performed as part of the evaluation for CML, and CML is diagnosed by detecting the Philadelphia chromosome.
- 32. 10–19% myeloblasts in the blood or bone marrow. >20% basophils in the blood or bone marrow Platelet count <100,000, unrelated to therapy Cytogenetic evolution with new abnormalities in addition to the Philadelphia chromosome Increasing splenomegaly or white blood cell count, unresponsive to therapy
- 33. Blast crisis is the final phase in the evolution of CML, and behaves like an acute leukemia, with rapid progression and short survival. Blast crisis is diagnosed if any of the following are present in a patient with CML: >20% myeloblasts or lymphoblasts in the blood or bone marrow. Large clusters of blasts in the bone marrow on biopsy. Development of a chloroma (solid focus of leukemia outside the bone marrow)
- 34. IMATINIB MESYLATE STEM CELL TRANSPLANTATION IFN-ALPHA HYDROXYUREA SECOND GENERATION TK INHIBITOR- DASATINIB AND NILOTINIB
- 35. IMTINIB NOW IS USED AS INITIAL THERAPY IN ALMOST ALL PATIENTS WITH CML. IN CASES WHERE WBC COUNT IS MARKEDLY ELEVATED HYDROXYUREA CAN BE USED TO PREVENT HYPERLEUKOCYTIC SYNDROME.
- 36. The bcr abl oncoprotien with a molecule of ATP in d kinase pocket. Phosphorylation - > substrate .Activates downstream molecules Imatinib occcupies d kinase pocket preventing phosphorylation of its substrates
- 38. HAEMATOLOGIC RESPONSE CYTOGENETIC RESPONSE MOLECULAR RESPONSE(BCR ABL TO CONTROL GENE RATIO ACCORDING TO IS SCALE) FREQUENCY .Every 2 weeks until a complete response has been achieved and confirmed. every 3 months unless othwise required every 6 months until a complete response has been achieved and confirmed. then every 12 months EVERY 3 MONTHS METHOD complete blood count (CBC) with differential Conventional cytogenetic examination .FISH (fluorescene in situ hybridisation) (only before treatment) .RQ-PCR (Reverse transcription quantitative polymerase chain reaction)
- 39. SMENT METHOD SUBOPTIMAL RESPONSE FAILURE tologic No Complete hematologic response(CHR) within 3 months No hematologic response within 3 months Loss of CHR at any time enetic No MCyR (Major cytogenetic response )within 6 months No CCyR(Complete cytogenetic response) within 18 months .No cytogenetic response within 6 months No MCyR within 12 mont No CCyR within 18 mont Loss of CCyR at any time Not applicable. CULAR No MMR(Major molecular response) within 8 months Loss of MMR at any time
- 41. Second generation TKI like DASATINIB NILOTINIB Allogenic human stem cell transplant
- 42. Well tolerated compared to other treatment options in CML Superficial edema Nausea,muscle cramps Rash,Diarrhea Uncommon side effects:tumour lysis in accelerated phase,splenic rupture,cerebral edema,Varicella Zoster infections
- 43. Imatinib is not recommended during pregnancy. Hydroxyurea has the lowest mutagenic potential among the cytotoxic agents. IFN can also be safely used during pregnancy.
- 44. Patients who are younger than 65 yrs and who have a identical twin or a histocompatible sibling can be transplanted after intensive therapy usually with cyclophosphamide. GVHD is common.
- 45. THANK YOU

IMAGES
VIDEO
COMMENTS
Acute lymphoid leukemia (case presentation) Feb 6, 2013 •. 52 likes • 32,155 views. Dhritiman Chakrabarti. 1 of 48. Download Now. Download to read offline. ACUTE LYMPHOID LEUKEMIA.
Blood. 2013; 121:4854-4860. A 47-year-old woman presents to the emergency department complaining of fatigue and shortness of breath. She reports a two-week history of worsening exercise tolerance and a rather abrupt onset of shortness of breath over the past several hours.
GOUT UPDATE AHMED YEHIA 2024, case based approach with application of the lat... Generative AI in Health Care a scoping review and a persoanl experience. ORAL HYPOGLYCAEMIC AGENTS - PART 2.pptx
Rare and emerging subtypes of leukemia can be incredibly challenging to diagnose and even more challenging to treat. At the NCCN 2019 Annual Congress: Hematologic Malignancies, a panel of experts, moderated by Andrew D. Zelenetz, MD, PhD, were presented with particularly challenging cases in these malignancies and asked to discuss best approaches to treatment.
Lab abnormalities concerning for acute myeloid leukemia: 8 Acute Myeloid Leukemia Clonal malignant bone marrow disorder >20% blasts of total cells of bone marrow aspirate (from 500 cell ... VIALE-A: study design (Phase III) 2 patients were not stratified by cytogenetic risk. They were excluded from efficacy analysis but included in the safety ...
Case Study: Prognostic Factors in Acute Lymphocytic Leukemia. A 48-year-old female presented to the emergency department with severe headaches, dyspnea on exertion, and petechiae on the lower extremities. A CBC was drawn that showed the following: WBC=56 x10 3 /µL, Hgb=9.0 g/dL, Hct=23, MCV=97 fl, plt=15 x10 9 /µL, ANC=0.7x10 3 /µL.
Abstract. The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ System Pathology, and Diagnostic Medicine and Therapeutic Pathology.
Adolescents and young adults (AYA) diagnosed with acute lymphoblastic leukemia (ALL) have faced poorer survival rates compared with the history of this illness treatment in children [].However, several European and US studies have reported improved outcomes for AYA patients treated with pediatric-based protocols [2,3,4]. however, AYA patients receiving pediatric regimens and doses, unlike ...
Educational Case: Diagnostic studies for B-cell acute lymphoblastic leukemia. The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ ...
Discussion. Acute lymphoblastic leukaemia (ALL) is the most common malignancy in the paediatric age group. 1 Symptoms of ALL include anaemia, fever, bleeding tendency and fatigue. 2 Hypercalcaemia and osteolytic lesions are rare in B-ALL in contrast to their incidence in some other lymphoid malignancies like adult T-cell leukaemia/lymphoma, myeloma and LCH. 2-4 However, in our case, due to ...
Leukemia Case Study - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Leukemia Case Study
300+ Nursing Cheatsheets. Start Free Trial. "Would suggest to all nursing students . . . Guaranteed to ease the stress!". ~Jordan. Leukemia Case Study (60 min) is mentioned in these lessons. Check out this case study on leukemia & learn everything you will need to about to ace your NCLEX questions. View the online lesson today!
Leukemia Case Study Slideshare, Baseball Training Facility Business Plan, My Writing Lab Plus Broward College, Cover Letter Sample For Trainer, Client Assessment Example Paper, Solve Physics Problems Online, Archangel Gabriel School Homework Site 741 Orders prepared
Case study - Adult - Fluid Overload - Leukemia. 77 year old man, with myelomonocytic leukemia treated with periodic blood transfusions. When PLR test with USCOM is positive it has a 91% Positive predictive value.Although when negative, there is a high False negative rate.A cause of a False negative is Conditions of high intra-abdominal pressure ...
Leukemia Case Study Slideshare, Sample Machine Operator Resume, Sample Group Purchasing Organization Business Plan, Thesis Statement Information Essay, Checklist Peer Review Research Paper, Essay On Solid Waste Management In Urban Areas, Open Banking Case Study
Abstract. We report two cases of chronic myeloid leukaemia (CML) with extreme thrombocytosis. The first patient was a 65-year-old man who presented with prolonged history of upper abdominal discomfort, anorexia and two episodes of recent gum bleeds without fever or other bleeding manifestations. He was a chronic smoker with no other comorbidities.
10 question spreadsheets are priced at just .39! Along with your finished paper, our essay writers provide detailed calculations or reasoning behind the answers so that you can attempt the task yourself in the future. Hire a Writer. +1 (888) 985-9998.
NCI Launches Research Network to Evaluate Emerging Cancer Screening Technologies. The Cancer Screening Research Network (CSRN) will support studies that investigate new ways to identify cancers earlier, when they may be easier to treat.In late 2024, CSRN plans to launch the Vanguard Study on Multi-Cancer Detection, a pilot study to inform the design of a larger trial of multi-cancer detection ...
This case highlights various treatment options, need for vigilant disease monitoring, and the possibility of complete positive response even after many lines of therapy failure. ... Success story of targeted therapy in chronic myeloid leukemia: a population-based study of patients diagnosed in Sweden from 1973 to 2008. J Clin Oncol 2011; 29: ...
Leukemia Case Study Slideshare. For expository writing, our writers investigate a given idea, evaluate its various evidence, set forth interesting arguments by expounding on the idea, and that too concisely and clearly. Our online essay writing service has the eligibility to write marvelous expository essays for you.
33. Blast crisis is the final phase in the evolution of CML, and behaves like an acute leukemia, with rapid progression and short survival. Blast crisis is diagnosed if any of the following are present in a patient with CML: >20% myeloblasts or lymphoblasts in the blood or bone marrow. Large clusters of blasts in the bone marrow on biopsy ...