Roblox The Presentation Experience Codes (July 2024)

Your changes have been saved
Email Is sent
Please verify your email address.
You’ve reached your account maximum for followed topics.

Roblox: Da Hood Codes (July 2024)
Roblox: driving empire codes (july 2024), 8 survival games with no combat.
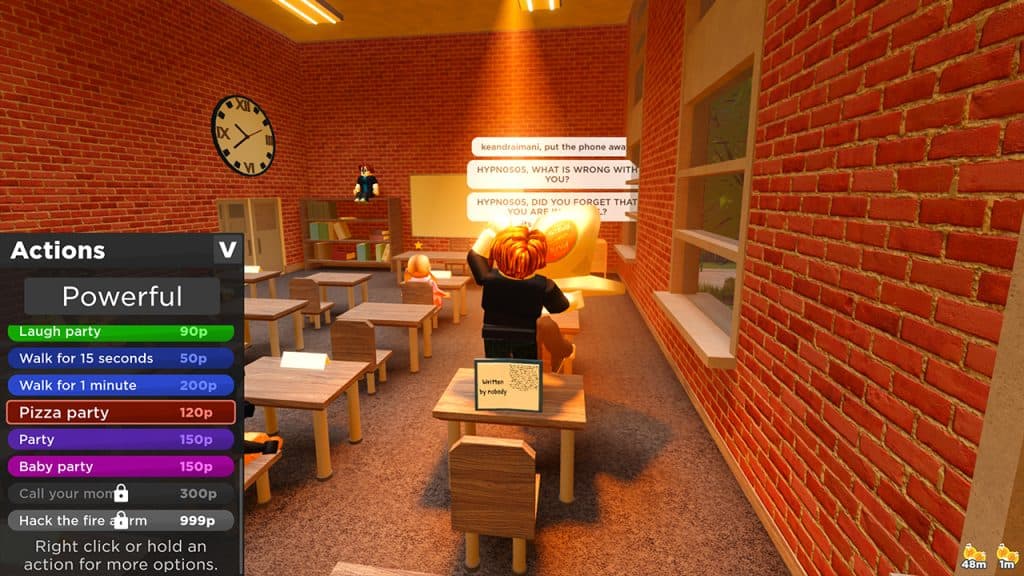
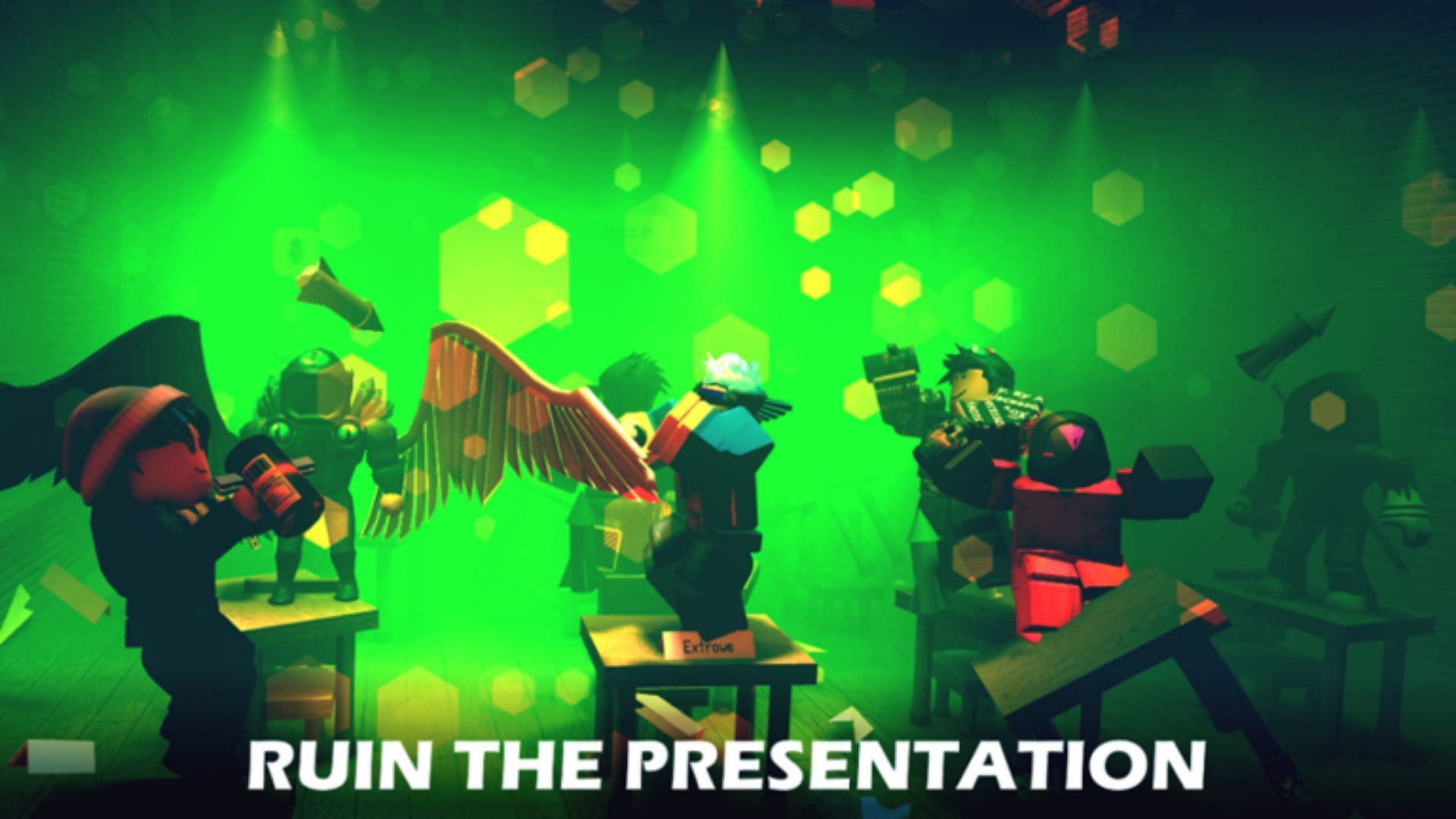
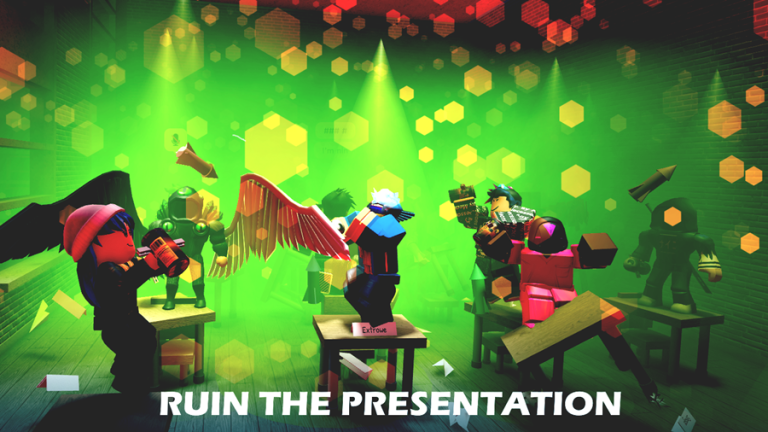
In The Presentation Experience , Roblox players will find themselves in a school and must spend time in class. However, this school offers much more freedom than any real one because players can do whatever they want and no one can punish them for breaking the rules. In this school, students can shout out phrases from popular memes , but they need to pay Points for this. Fortunately, these points can be obtained by entering the codes in this article.
Updated July 17, 2024, by Artur Novichenko: We've thoroughly searched for The Presentation Experience codes, but it seems the developers haven't released any new yet. Keep checking back for future updates.

Roblox players who are looking to earn some free in-game cash and wrap rewards can use these Da Hood codes to get them.
All The Presentation Experience Codes
Working The Presentation Experience Codes
- COFFEE - Enter this code to get 60 Points.
- MAXWELLGOOD - Enter this code to get 20 Gems.
- MANFACEPOOPER - Enter this code to get 5x Points Boost for 10 minutes
- HALLWAY - Enter this code to get 10 Gems.
- UWU - Enter this code to get 20 Gems.
- THEREARENOOTHERTEACHERSINTHESCHOOLBECAUSENOBODYWANTSTOSEETHEBADTEACHER - Enter this code to get 10 Gems.
- MINIMALGAMESPRO - Enter this code to get 25 Points.
- HELICOPTER - Enter this code to get 50 Points.
- MEGABOOST - Enter this code to get 5x Points Boost for 1 minute.
- 5GEMS - Enter this code to get 5 Gems.
- CODE - Enter this code to get 15 Points.
- RAT - Enter this code to get 25 Points.
- BOOKWORM - Enter this code to get 80 Points.
- 10POINTS - Enter this code to get 10 Points.
- TEACHERMADCUZBAD - Enter this code to get 150 Points.
- AZUREOPTIX - Enter this code to get 25 Points.
- TOILET - Enter this code to get 50 Points.
- POOP - Enter this code to get 100 Points.
- EMOTIONALDAMAGE - Enter this code to get 80 Points.
All Expired The Presentation Experience Codes
- FARTYREWARD
- FUNNYBACKROOMS
- dodgingcode
- scaryhalloween2023
- spookpoints
- OMG350KLIKES
- ITSABOUTDRIVEITSABOUTPOWER
- 200MVISITS !
- summerboost
- bababooeypoints
- CHRISTMASGIFT
- MILLIONMEMBERS !
- 700kmembers
- 600kmembers

In this guide, Roblox players can find all of the latest Driving Empire codes, which can be redeemed for in-game rewards like cash and wraps.
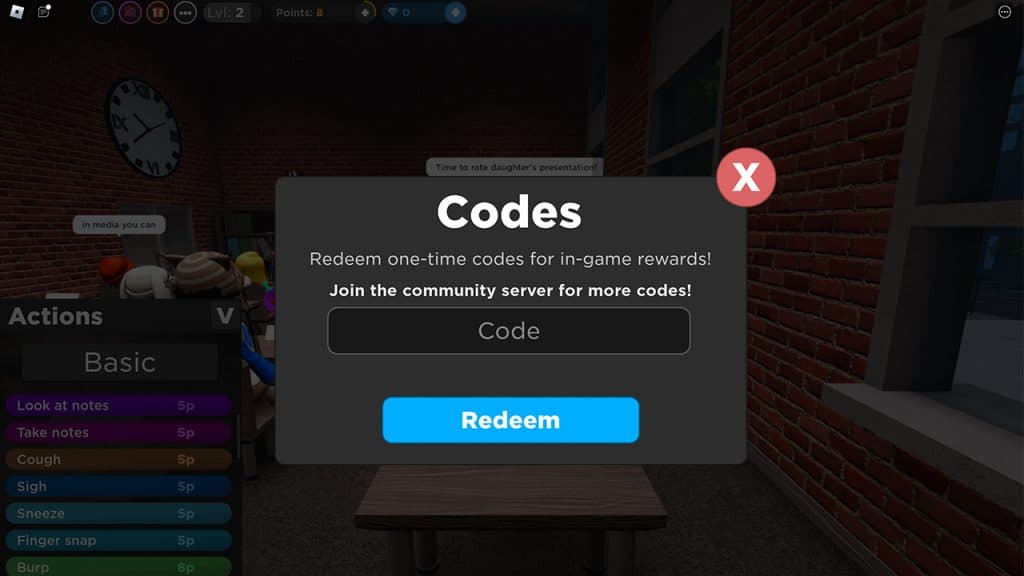
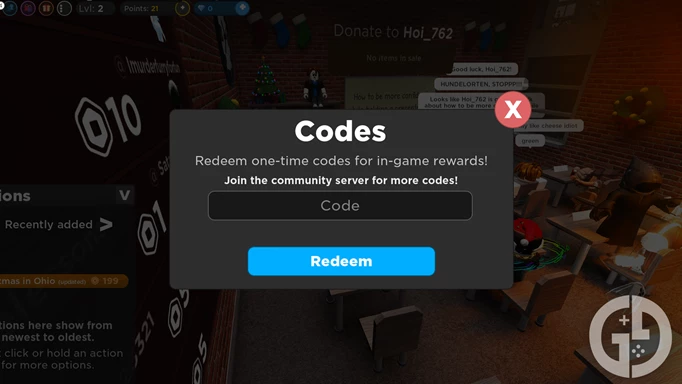
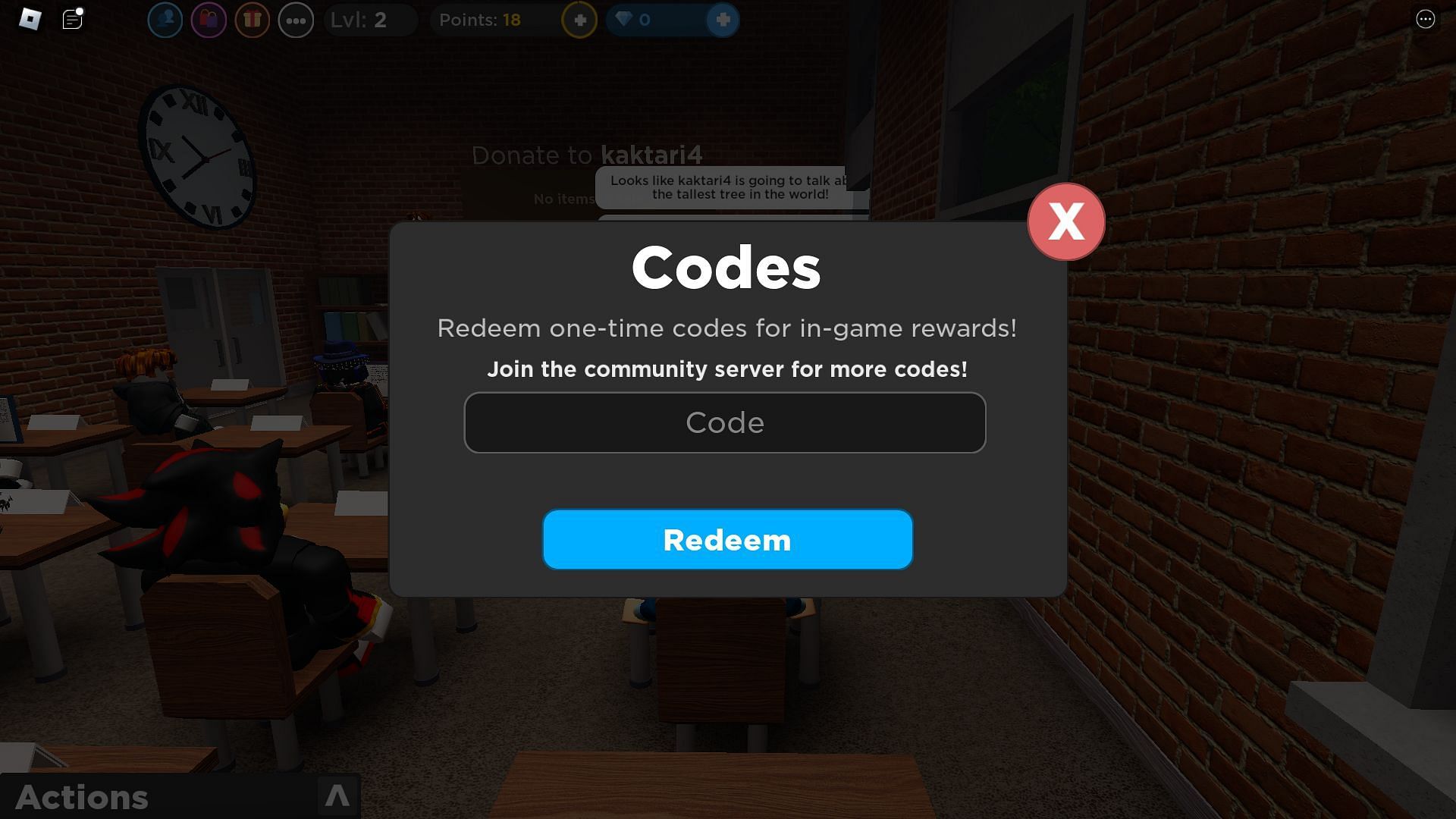
How to Redeem Codes in The Presentation Experience
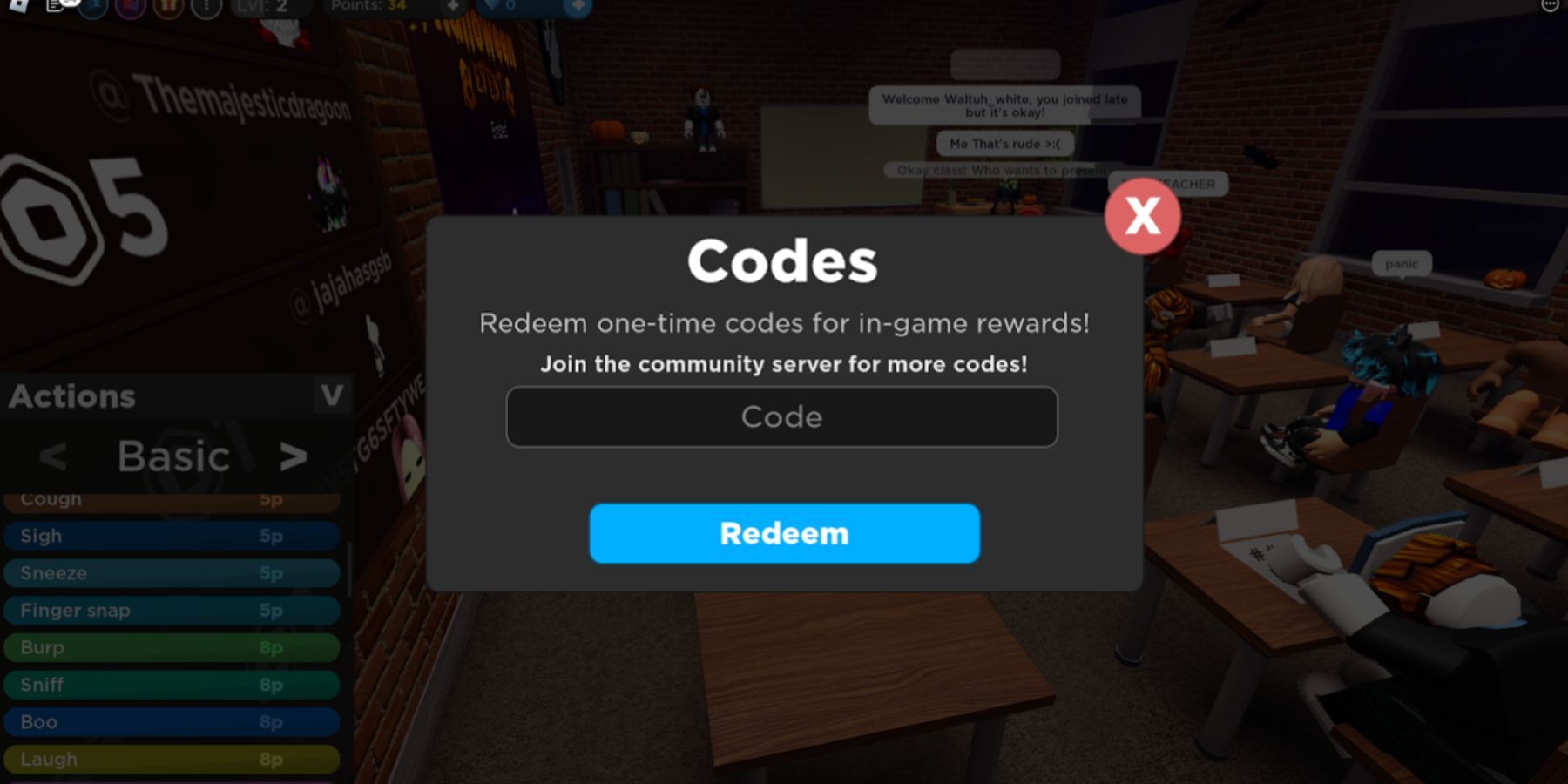
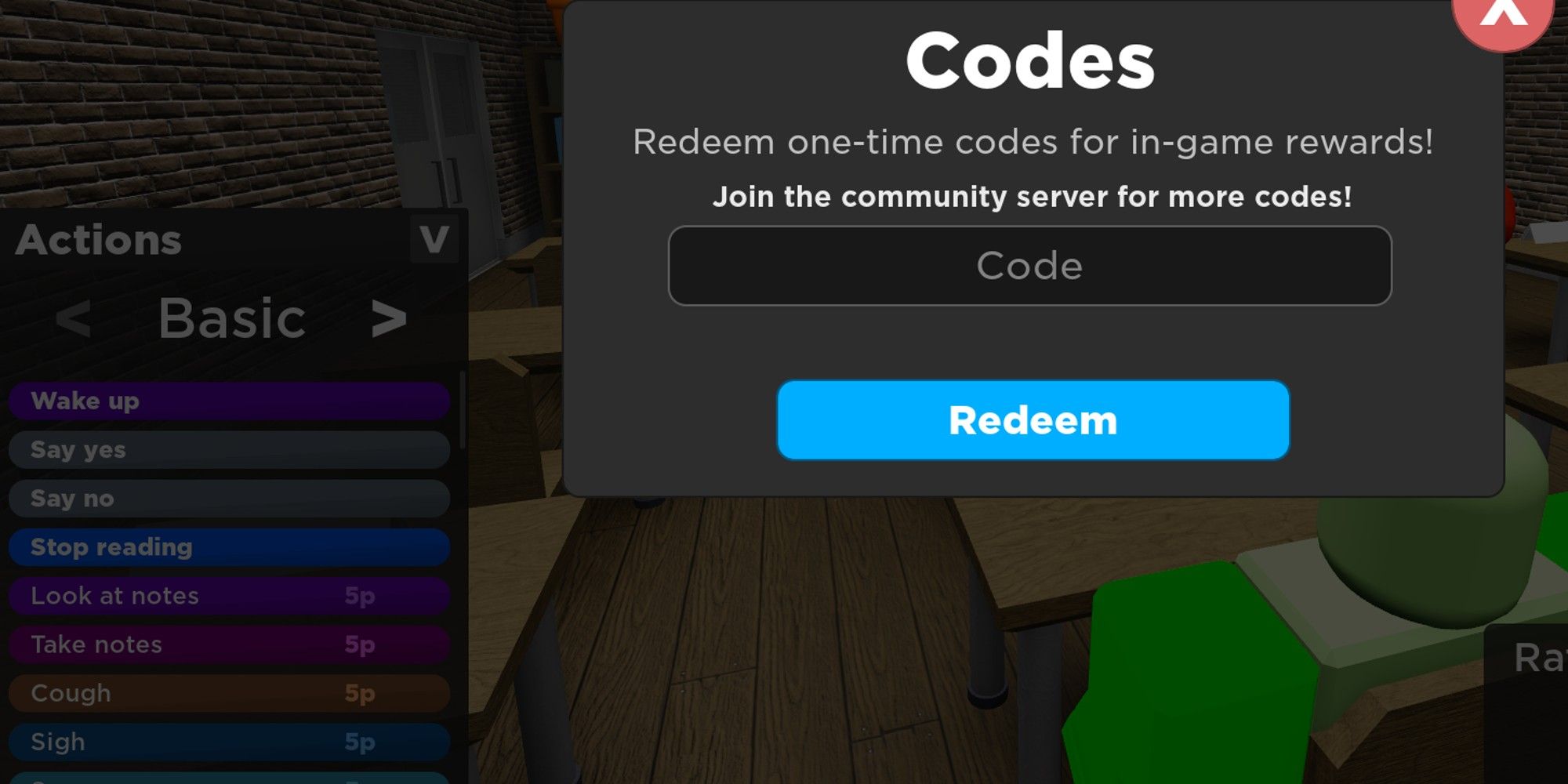
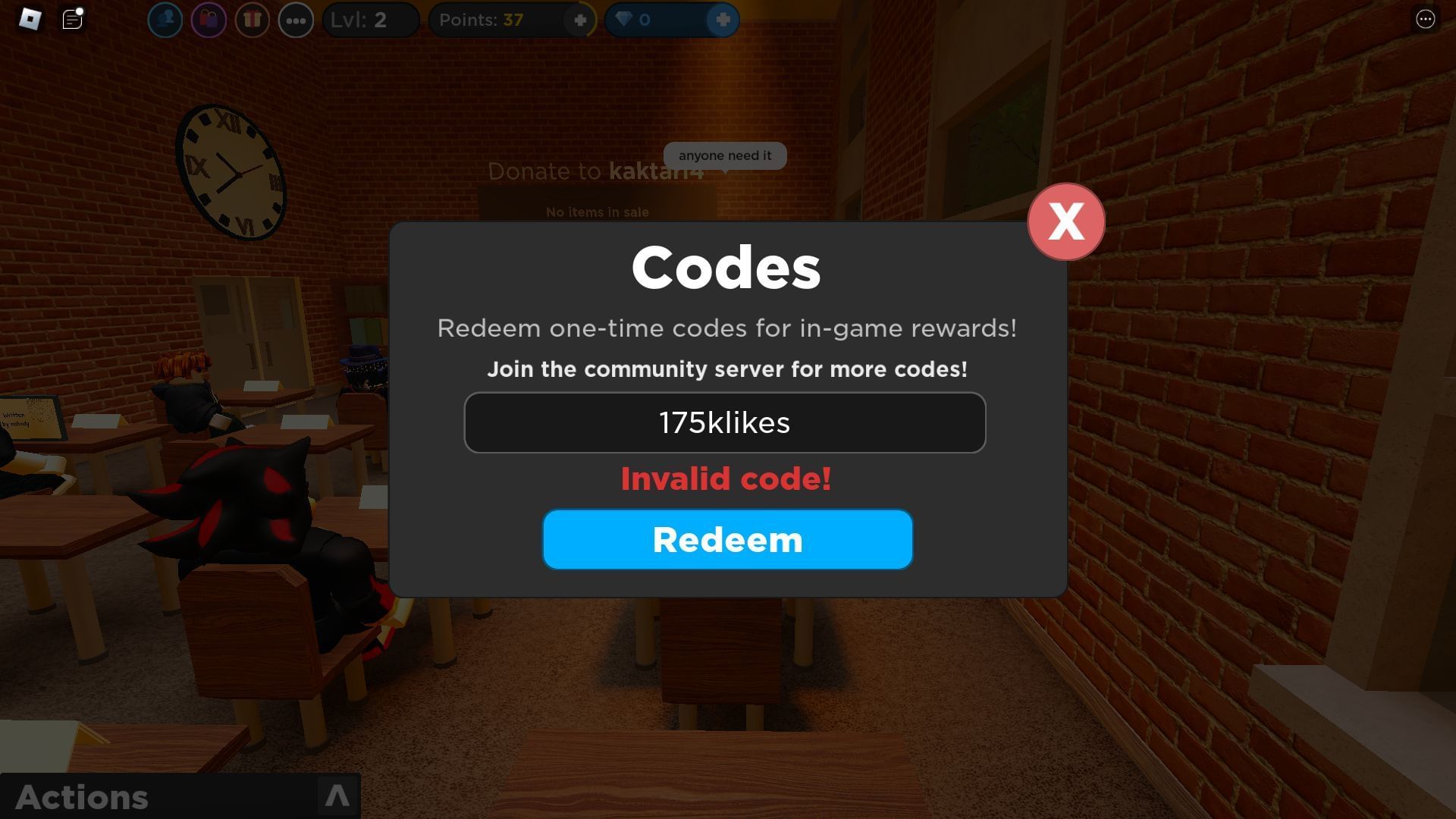
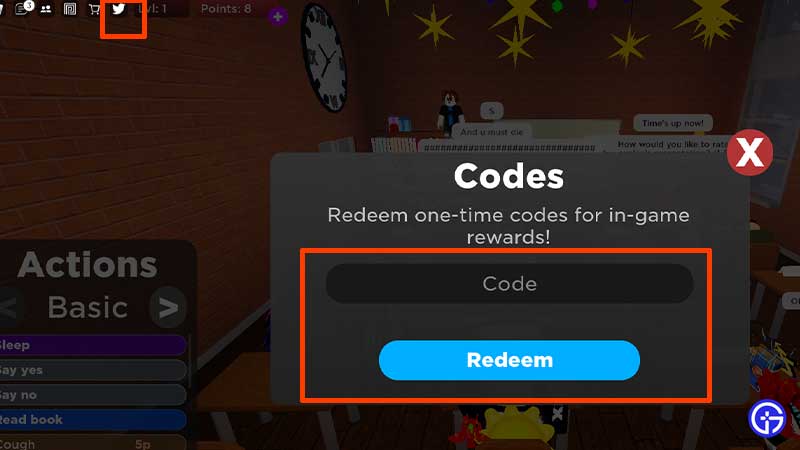
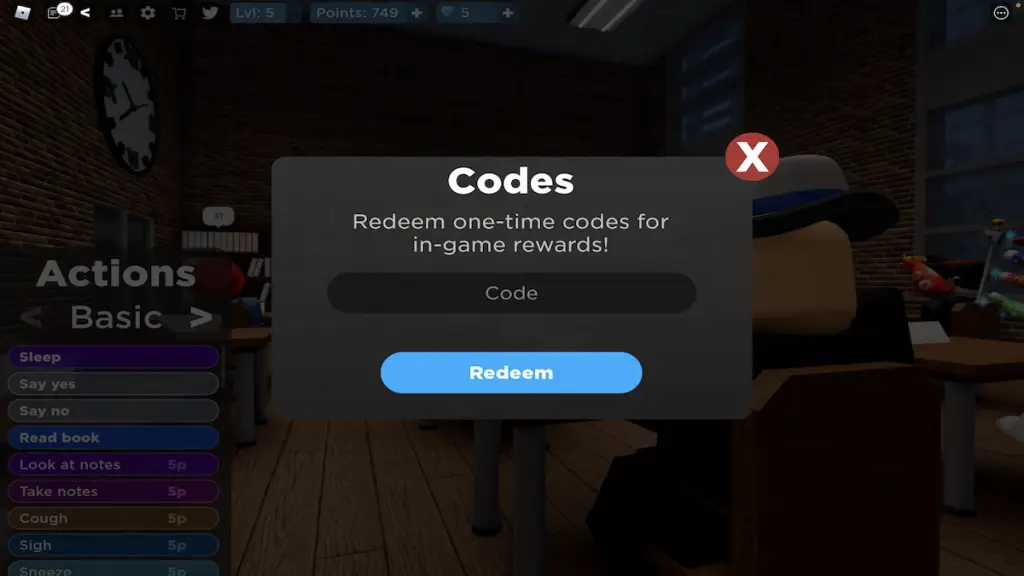
The buttons in The Presentation Experience interface are quite small, so it is not easy to find the one needed for entering the codes. If players are confused about redeeming the codes, they can use the instructions below:
- Go to Roblox and launch The Presentation Experience .
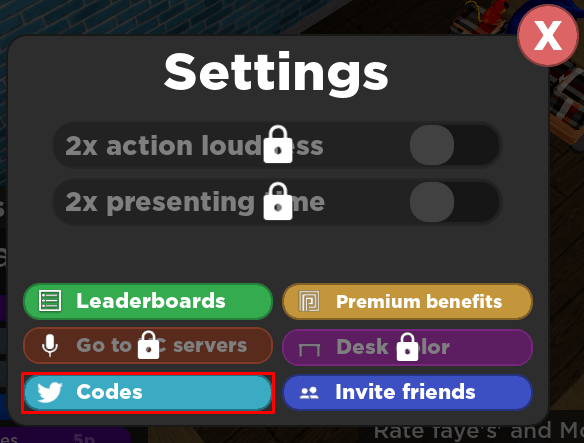
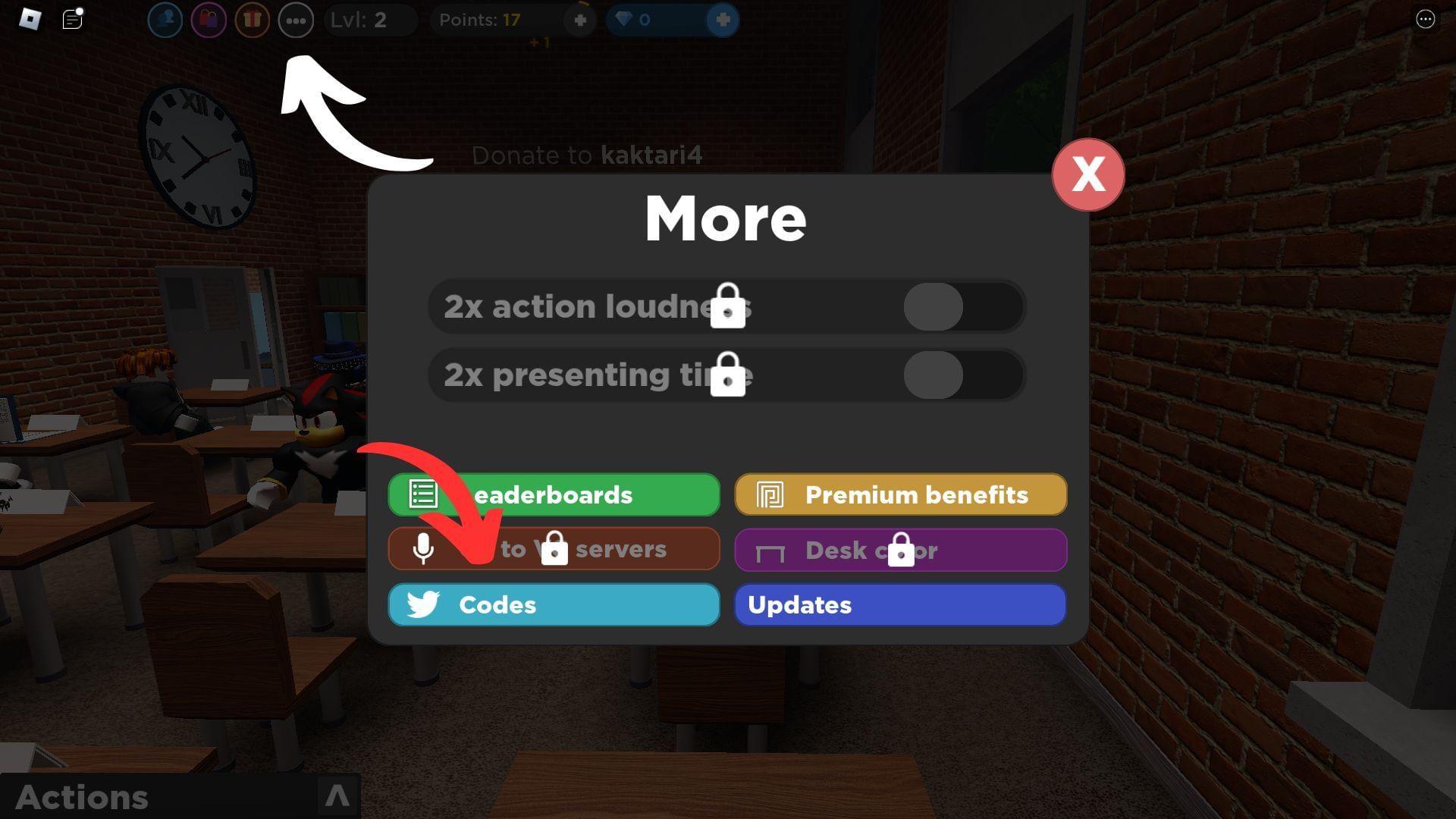
- In the upper-left corner, there are several small round buttons. Click the button with 3 dots to the left of the player's level.
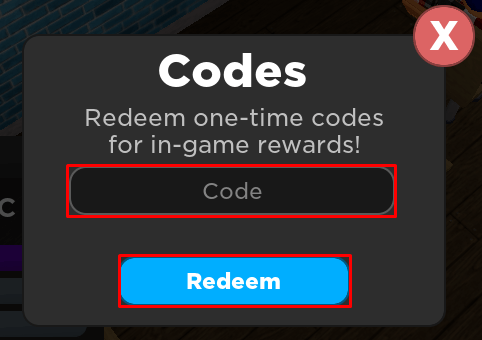
- After pressing this button, a menu will pop up in which gamers have to press the Codes button. It is blue and has a bird on it, the symbol of Twitter.
- In the Code field, enter or paste the code and click Redeem.

Roblox - Game
The Presentation Experience codes (April 2024) – Free Points & Gems

Score free points, gems, boosts, and more with our list of all the latest Roblox The Presentation Experience codes. Here are all the active and expired codes for April 2024.
Did you ever enjoy giving presentations in school? If not then The Presentation Experience on Roblox is going to change that. In this unique game, you get to give presentations or interrupt the presentations in hilarious ways.
From beatboxing to shooting a firework, you get to do it all. However, you need a bunch of points to execute these actions. Luckily, our list of codes will give you all the points required to perform popular memes and other fun actions right away.
While you’re here, check out more goodies in other fun Roblox games at Dragon Soul codes , Restaurant Tycoon 2 codes , Titan Warfare codes , and Ro Ghoul codes .
- The Presentation Experience codes
- How to use codes
- All expired codes
- What are codes
All The Presentation Experience codes (April 2024)
Here are all the latest The Presentation Experience codes:
- dodgingcode – Free 50 Gems
- 400KLIKES – Free 10 Gems, Points Boost
- scaryhalloween2023 – Free 60 Points, 15 Gems
- spookpoints – Free 100 Points
- OMG350KLIKES – Free 100 Points, 12 Gems
- UGC – Free 30 Gems
- CODE – Free 15 Points
- RAT – Free 25 Points
- BOOKWORM – Free 80 Points
- 10POINTS – Free 10 Points
- TEACHERMADCUZBAD – Free 150 Points
- AZUREOPTIX – Free 25 Points
- TOILET – Free 50 Points
- POOP – Free 100 Points
- EMOTIONALDAMAGE – Free 80 Points
- COFFEE – Free 60 Points
- MAXWELLGOOD – Free 20 Gems
- FARTYREWARD – Free 100 Points
- MANFACEPOOPER – Free 5x Points Boost for 10 Minutes
- HALLWAY – Free 10 Gems
- UWU – Free 20 Gems
- THEREARENOOTHERTEACHERSINTHESCHOOLBECAUSENOBODYWANTSTOSEETHEBADTEACHER – Free 10 Gems
- FUNNYBACKROOMS – Free 5 Gems
- MINIMALGAMESPRO – Free 25 Points
- HELICOPTER – Free 50 Points
- MEGABOOST – Free 5x Points Boost for 1 Minute
- 5GEMS – Free 5 Gems
How to redeem The Presentation Experience codes?
Redeeming codes in The Presentation Experience is quite easy, here are some simple steps:
- Go to the official The Presentation Experience page and click on the green button to launch the game .
- Tap on the three dots button on the top-left corner of the screen.
- Click on the Twitter icon and paste the code in the box.
- Hit Redeem to get your free rewards.
Can’t use codes? Note that they are case-sensitive so enter them exactly as they are mentioned. Moreover, the codes expire after a certain period so use them as soon as possible.
List of expired codes
- ITSABOUTDRIVEITSABOUTPOWER – Free Rewards
- nootnoot – Free Rewards
- 200MVISITS! – Free Rewards
- summerboost – Free Rewards
- beatbox – Free Rewards
- bababooeypoints – Free Rewards
- unexpected – Free Rewards
- CHRISTMASGIFT – Free Rewards
- sus – Free Rewards
- MILLIONMEMBERS! – Free Rewards
- 100MVISITS – Free Rewards
- 175klikes – Free Rewards
- 700kmembers – Free Rewards
- 150KLIKES – Free Rewards
- pencil – Free Rewards
- 600kmembers – Free Rewards
- 180klikes – Free Rewards
- Easter – Free Rewards
What are The Presentation Experience codes?
Codes in The Presentation Experience offer free in-game resources like points, gems, and more. The developers release new codes to help players unlock the funniest class interruptions. You will find all the new codes right here since we regularly update the page.
So there you have it – everything you need to know about The Presentation Experience codes for April 2024.
Doodle World codes | Race Clicker codes | Simon Says codes | A One Piece Game codes | All Star Tower Defense codes
Subscribe to our newsletter for the latest updates on Esports, Gaming and more.
Roblox: The Presentation Experience Codes

Your changes have been saved
Email Is sent
Please verify your email address.
You’ve reached your account maximum for followed topics.

Roblox - Game
Roblox is enjoyed by millions. A sandbox game where you can play, create, and come together with people all over the world. Jump into any of the community experiences, or take advantage of promo codes for cool content.
We added a new code on March 10th, 2024.
If you are looking for a few easy points, the new code is just what the doctor ordered!
Finally, we have a game that allows us to do what we always wanted to do during a classroom presentation—create utter chaos! This Roblox game is designed to relieve the stress of presenting in front of class, as the player gets to choose the topic, and they get to indulge in their darkest impulses! Ultimately, all of this makes The Presentation Experience a funny roleplaying game where the players make it what they want it to be.
Roblox: 18 Best Roblox Horror Games
What are the scariest Roblox horror games out there? We've picked the very spookiest that can be played alone with the lights off, or with friends!
We check for new Presentation Experience codes daily, and new codes are usually added for updates and milestones. Come back soon to see if there are any more free rewards up for grabs.
The Presentation Experience Codes
Code | Reward |
|---|---|
| 50 Points |
| 20 Points |
| 10 Points and 2x Point Boost |
| 25 Points |
| 50 Points |
| 10 Gems |
| 80 Points |
| 200 Points |
| 60 Points |
| 100 Points |
| 100 Points |
| 100 Points & 12 Gems |
| Free 20 Gems |
| Free Boost |
| 20 gems |
| 25 points |
| 10 free gems |
| 5 free gems |
| 5x points boost for one minute |
Roblox codes are case-sensitive which means you need to input the code as it appears in the table above - copy and paste exactly, with matching numbers, capital letters, and punctuation.
Expired The Presentation Experience Codes
unexpected | 15 Gems |
200MVISITS! | 100 points |
CHRISTMASGIFT | 39 free gems |
pencil | 100 free points |
nootnoot | 75 free points |
MILLIONMEMBERS! | |
100MVISITS | |
700kmembers |
How To Redeem Codes In The Presentation Experience
- Load up the game and enter your first presentation
- On the top left, there's a tiny Settings button that looks like a cog/gear
- Click on that button, then enter the Codes into the box
- Redeem, and enjoy! You will receive a message underneath that tells you what the code has given you
Codes not working? We always check that our codes are active and not expired, but we might have missed one going inactive. Also double-check that you have entered the code correctly.

15 Best Roblox Anime Games
There are hundreds of Roblox games inspired by anime and manga. Here are our favorite anime Roblox games that we recommend.
What Are The Presentation Experience Codes?

The Presentation Experience codes are free rewards given out by the developer that can be redeemed for points and gems. These are the currencies that you let do fun stuff during the class, like shaking the whole place with an earthquake or turning into a helicopter. New codes are released alongside updates, events, and like milestones.
How To Get More Codes

New codes are usually posted on the community Discord server, but if you want an easy way to access all the old and new codes alike you can just check our list. We've got them all here.

Roblox: 18 Best Games To Play With Your Friends
Sometimes, there's nothing better than playing with friends. These Roblox games let you do just that.
- Triple-A Games
The Presentation Experience codes (July 2024)

The Presentation Experience in Roblox transports you back to school, where you roleplay as a student in a classroom to disrupt the teacher and your classmates.
As there are a bunch of rewards available for you right away through codes , here’s a list of The Presentation Experience codes that can be redeemed for free in July 2024.
Active codes for The Presentation Experience
- bookworm – 80 Points
- OMG350KLIKES – 100 Points, 12 Gems
- UGC – 30 Gems
- COFFEE – 60 Points
- MAXWELLGOOD – 20 Gems
- FARTYREWARD – 100 Points
- MANFACEPOOPER – 5x Points Boost (10 minutes)
- uwu – 20 Gems
- THEREARENOOTHERTEACHERSINTHESCHOOLBECAUSENOBODYWANTSTOSEETHEBADTEACHER – 10 Gems
- FUNNYBACKROOMS – 5 Gems
- MINIMALGAMESPRO – 25 Points
- HELICOPTER – 50 Points
- MEGABOOST – 5x Points Boost (1 minute)
- 5GEMS – 5 Gems
- CODE – 15 Points
- RAT – 25 Points
- 10POINTS – 10 Points
- TEACHERMADCUZBAD – 200 Points
- AZUREOPTIX – 25 Points
- TOILET – 50 Points
- POOP – 100 Points
- EMOTIONALDAMAGE – 80 Points
Expired codes
- 600kmembers
- scaryhalloween2023
- dodgingcode
- spookpoints
- bababooeypoints
- ITSABOUTDRIVEITSABOUTPOWER
- 200MVISITS!
- 700kmembers
- CHRISTMASGIFT
How to redeem codes in The Presentation Experience
- Launch The Presentation Experience through the official Roblox website.
- Tap on the X icon at the top of the screen. A redemption box should appear.
- Carefully type or copy-paste the desired code and hit Redeem .
- If the code is correct and valid, the corresponding rewards should appear on the screen.

What are The Presentation Experience codes used for?
The Presentation Experience codes can be used to get resources like Points and Gems . This content is useful for buying all the actions to annoy the teacher and increase your score, which will give you a chance of getting more rewards.
Why aren’t my codes working?
If your codes are not working, this may be because they’ve expired or have a typo or capitalization error . Do note that Roblox codes are usually case-sensitive, so it is better to copy-paste them directly from the list above and avoid any errors. Also, be sure to redeem them as fast as possible and prevent them from expiring.
If you are into Roblox, make sure to check out our code lists for other Roblox games such as Money Race .
- The Presentation Experience Game Codes
Please let us know about any new or missing codes through the below form. Thank you for helping to keep the content on Roblox Den up-to-date and accurate!
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Please let us know about any expired codes, or other codes that have problems, via the below form. Thank you for helping to keep the content on Roblox Den up-to-date and accurate!
If you've encountered a problem on this page, please report it via the below form. Thank you for helping to keep the content on Roblox Den up-to-date and error free!
The Presentation Experience Codes
All current and previous game codes for The Presentation Experience on Roblox.

This code credits your account with 60 Points and 15 Gems .
This code credits your account with 100 Points and 12 Gems .
This code credits your account with 30 Gems .
This code credits your account with 100 Points .
This code credits your account with 20 Gems .
This code credits your account with a 10 Minute 5x Points Boost .
This code credits your account with 10 Gems .
This code credits your account with 5 Gems .
This code credits your account with 25 Points .
This code credits your account with 50 Points .
This code credits your account with a 1 Minute 5x Points Boost .
This code credits your account with 15 Points .
This code credits your account with 80 Points .
This code credits your account with 10 Points .
This code credits your account with 150 Points .
This code credits your account with 10 Gems and 2x Points Boost (1 hour) .
This code credits your account with 15 Gems .
This code credits your account with 75 Gems .
This code credits your account with 39 Gems .
This code credits your account with 10 Points and a 10 Minute 5x Points Boost .
This code credits your account with a 2 Minute 2x Points Boost .
This code credits your account with 30 Points .
| Code | Description | Status | Works |
|---|---|---|---|
| This code credits your account with and . | Active | ||
| This code credits your account with and . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with a . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with a . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Active | ||
| This code credits your account with . | Check | ||
| This code credits your account with and . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with and a . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with a . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired | ||
| This code credits your account with . | Expired |
How to Use Codes in The Presentation Experience
To use codes in The Presentation Experience, first click on the settings button at the top left corner of the screen:

Next, click on the Codes button:
Next, type your code into the Code box, and then click Redeem :
About The Presentation Experience
Put your presentation skills to the test in The Presentation Experience, a roleplaying presentation game. Starting out as a student in a school classroom, you'll have to sit tight until a random player is chosen to give a presentation about a randomly selected topic. As a student, it is your job to interrupt the presentation as much as possible, whether that be through crying, farting, or even vomiting. If chosen to give a presentation, you'll need to wow the audience in order to receive a good score. Higher scores will earn you more points, which can be spent in the shop on cool new emotes and interruption methods!
Enter your email below and we'll send you an alert when new codes are released!
The Presentation Experience codes
How to redeem Presentation Experience codes in Roblox.
The Presentation Experience is a Roblox school roleplay game where you’ll complete tests, answer questions, and give presentations to earn Points. With Points, you can earn actions, where you’ll be able to disrupt the class by doing everything from going to the bathroom to throwing a pizza party.
You’ll earn Points as you sit in class and complete homework or present, but if you want to disrupt class even more, you can use Roblox codes to get free Points, Gems, and various boosts. These codes are normally announced by developers on socials and on the game’s Roblox page (and hidden within the game’s classroom and bathroom), but we’ve done all the work right here and compiled this list of all the latest The Presentation Experience codes to help let you be the most annoying student possible.
All working The Presentation Experience codes
All expired the presentation experience codes, how do i redeem codes in the presentation experience.
- dodgingcode : 50 Points
- 400KLIKES : 10 Gems, 2x Points Boost (60 minutes)
- bookworm : 80 Points
- scaryhalloween2023 : 60 Points, 15 Gems
- spookpoints : 100 Points
- OMG350KLIKES : 100 Points, 12 Gems
- UGC : 30 Gems
- COFFEE : 60 Points
- MAXWELLGOOD : 20 Gems
- FARTYREWARD : 100 Points
- MANFACEPOOPER : 5x Points Boost (10 minutes)
- uwu : 20 Gems
- THEREARENOOTHERTEACHERSINTHESCHOOLBECAUSENOBODYWANTSTOSEETHEBADTEACHER : 10 Gems
- FUNNYBACKROOMS : 5 Gems
- MINIMALGAMESPRO : 25 Points
- HELICOPTER : 50 Points
- MEGABOOST : 5x Points Boost (1 minute)
- 5GEMS : 5 Gems
- CODE : 15 Points
- RAT : 25 Points
- 10POINTS : 10 Points
- TEACHERMADCUZBAD : 200 Points
- AZUREOPTIX : 25 Points
- ITSABOUTDRIVEITSABOUTPOWER : 100 Points
- TOILET : 50 Points
- POOP : 100 Points
- EMOTIONALDAMAGE : 80 Points
- 200MVISITS!
- summerboost
- bababooeypoints
- CHRISTMASGIFT
- MILLIONMEMBERS!
- 700KMEMBERS
- 600KMEMBERS
- jennahacker
Not sure how to redeem codes in The Presentation Experience? Here’s what you’ll need to do:
- Launch The Presentation Experience in Roblox.
- Click the button with the three dots near the top left corner of your screen.

- Click the “Codes” button near the bottom left corner of the menu that pops up.

- Enter your code in the field and press redeem.
If you’re done disrupting class in The Presentation Experience but want another popular Roblox game that’s easy to get started in, we’ve got you covered with our codes lists for Cabin Crew Simulator , Collect All Pets , Pet Simulator X , and Adopt Me .
Read this next
- Hooray, Roblox's virtual IKEA opens today, and the jobs it offered spawned "over 178,000" applications
- Good news, Roblox job-seekers - a virtual IKEA is now hiring meatball servers
- Roblox teams with Netflix on virtual "theme park" Nextworld to bring Stranger Things, One Piece, and more to millions of players
- Monopoly Go passes Go 15 million times, collects $3 billion
- New Elden Ring boss just dropped in the real world
- Publishers of GTA 6, Call of Duty, and more to be impacted as video game voice actors strike over AI implementation
- Blizzard will talk Diablo 4 Season 5, and how the recent PTR will affect the upcoming season next week
- It might not be Elden Ring Numbers, but Armored Core 6 sailing past a sales milestone proves the people still yearn for mecha action
- Stalker 2's been delayed again but the new release date trailer shows that, despite everything, the devs are in good spirits
- Zenless Zone Zero player takes immersion to another level, playing the game on a CRT
- Honkai Star Rail Yunli kit, materials, and Traces priority
- How to fix Fallout: London crashes
- Zenless Zone Zero Zhu Yuan build and teams
- How to set Turn Ons and Turn Offs in The Sims 4 Lovestruck
- How to make Sims polyamorous in The Sims 4 Lovestruck
- Once Human A Family Legacy Walkthrough
- How to get Pyro Dino in Once Human: Securement Silo Phi
- No Rest for the Wicked's combat gets more brutal, the Crucible gets a revamp and stray animals arrive in latest update 1
The Presentation Experience Wiki
Welcome to The Presentation Experience Wiki! You need to sign in to edit.

The "Codes" screen, as well as a 5X Points boost redeemed via Codes at the bottom-right corner.
Codes are a feature in The Presentation Experience. It's not really crucial since it's not a core feature in the game, however they can help you if you want a special bonus or want free Points or Gems . Codes have existed since the game existed (probably), and they still exist in the experience to this day.
List of codes [ ]
Here are many codes in The Presentation Experience that you can redeem! These are not all the codes.
Redeemable Codes [ ]
Limited and Expired Codes [ ]
These are expired codes that you can no longer redeem.
- 600kmembers
- 660kfavorites
- 700kmembers
- bababooeypoints
- CHRISTMAS2022
- OHIOFIRETRUCK
- summerboost
All The Presentation Experience codes to redeem free gems & points

Written by
Kiera Mills
Last updated
4th Dec 2023 16:15
The Presentation Experience has plenty of codes for players to use, that can make their lives a lot easier. The Presentation Experience is as it sounds, a Roblox game that reenacts the experience of being in the classroom, with all the stress that entails.
To ease that burden somewhat, the codes below provide useful gems and points in the game , so continue reading to find the full list of up-to-date codes and instructions on how to redeem them.
December 04 2023: We checked for any new active or expired The Presentation Experience codes. Check out the full list below.
All active The Presentation Experience codes
Below are all the currently active codes for The Presentation Experience, we have tested them all to ensure they are working at the time of writing. While several of these codes are older and have been active for some time, some are new and may expire sooner, so be sure to use them up.
Most of the codes give you gems and points, but some grant you extra points for a certain amount of time, so make sure to only use those codes when you plan on earning some points soon after.
| 30 Gems | |
| 60 Points | |
| 20 Gems | |
| 100 Points | |
| 5x Points for 10 minutes | |
| 25 Points | |
| 20 Gems | |
| 10 Gems | |
| 5 Gems | |
| 5x Points for 1 minute |
How to redeem TPE codes
Now that you have them all, here is how to redeem codes for The Presentation Experience.
- Click the button with three dots in the top left
- Hit the Codes button with the Twitter icon
- Enter any of the codes from this guide in the Code box
- Press Redeem and enjoy your free rewards
That is all we have for The Presentation Experience codes. For more, head to our Roblox homepage where you can find codes for games like Haze Piece , Peroxide , and Project Slayers .

Established in 2019, we don’t just cover games - we live them. Our expert team is full of dedicated gamers, qualified journalists, and industry insiders who collectively boast decades of experience covering gaming and esports. This deep-rooted expertise allows us to provide authoritative and nuanced perspectives first-hand from a team who are playing, and researching every game covered on our website.
Our foundation is built on a profound commitment to editorial independence, ensuring our content remains free from external influence and advertising pressures and is held to the highest level of editorial conduct, integrity, and quality.
Every article on GGRecon comes from rigorous research, informed analysis, and a passion for gaming that resonates with our readers. We uphold these standards through a transparent editorial policy, accessible here , which governs our processes and maintains our accountability.
- Roblox Game Codes
- Blox Fruits codes
- Roblox Guide
- Spin 4 Free UGC Codes
- Murder Mystery 2 Codes
- Best Roblox Horror Games
- Roblox The Hunt: First Edition
- Roblox Music Codes
- Adopt Me Codes
- Blade Ball Codes
- Evade Codes
- Type Soul Codes
The Presentation Experience Codes (July 2024)
Using The Presentation Experience codes is the best way to accumulate a large number of points and gems in the title. Additionally, the Roblox game offers boosts to help you increase the rate of these currencies' acquisition. They don't require you to jump through extra hoops either, allowing you to redeem them the moment you load into the game.
This article lists all the codes for The Presentation Experience while giving you a tutorial on using them.
Bookmark this article to access the latest Roblox game codes in The Presentation Experience. We'll keep updating the page whenever new codes for The Presentation Experience are issued.
All The Presentation Experience codes (Active)
Listed below are codes for The Presentation Experience that are confirmed to be working as of now. They can expire at any moment, so we recommend using them quickly. Once they become inactive, the freebies associated with them are rendered inaccessible.
List of Active Presentation Experience Codes | |
Code | Rewards |
dodgingcode | 50 gems |
400KLIKES | 10 Gems and Boost |
scaryhalloween2023 | 60 Points and 15 Gems |
spookpoints | 100 Points |
summerboost | 5x Point boost for 10 minutes |
OMG350KLIKES | 50 Points |
unexpected | 15 Gems |
UGC | 30 Gems |
coffee | 60 Points |
maxwellgood | 20 Gems |
manfacepooper | 5x Point boost for 10 minutes |
fartyreward | 100 Points |
minimalgamespro | 25 Points |
UwU | 20 Gems |
Hallway | 10 Gems |
pencil | 100 Points |
100MVISITS | 15 Gems |
MILLIONMEMBERS! | 10 Gems, 5x XP for 10 minutes |
nootnoot | 75 Points |
Megaboost | 5x points boost for one minute |
5gems | Five gems |
toilet | 50 Points |
itsaboutdriveitsaboutpower | 150 Points |
poop | 100 Points |
NikkoCoder | 50 Points |
bookworm | 80 Points |
code | 15 Points |
RAT | 25 Points |
Teachermadcuzbad | 200 Points |
Inactive The Presentation Experience codes
The codes listed below can no longer be used in The Presentation Experience because of a built-in expiration date. This date is often unspecified, which is what causes codes to expire unexpectedly.
If you’re worried about losing rewards to this expiration date, rest assured that the developers have taken note of this. They have already replaced inactive codes with new ones that offer similar or outright better freebies, something they will likely continue to do in the future.
The Presentation Experience codes | |
Code | Rewards |
200MVISITS! | 100 Points |
CHRISTMASGIFT | 39 Gems |
anfisanova | 25 Points |
bababooeypoints | 50 Points |
180klikes | 10 gems |
Easter | Eight gems |
700kmembers | 10 Gems, 5x Points boost for one minute |
600kmembers | 2x Boost for five minutes |
175klikes | 10 Gems, 5x Point boost |
150KLIKES | Freebies |
beatbox | 30 Points |
sus | 30 Points |
How to redeem active The Presentation Experience codes
Here’s how you can redeem active codes for The Presentation Experience:
- Launch The Presentation Experience on the Roblox Game Client.
- Tap the three dots at the top of the screen.
- Open the code box by clicking the Twitter bird icon.
- Enter a working code in the text box and press Confirm to receive your freebies.
- Do the same for all active codes.
The Presentation Experience codes are case-sensitive. Neglecting this fact will result in errors during code redemption. Since these codes incorporate both uppercase and lowercase types, it may be better to paste them directly from this list instead.
Using the copy-paste method is quicker and far more accurate, resulting in fewer errors while redeeming tens of codes at once.
The Presentation Experience codes and their importance
Codes for The Presentation Experience offer points, gems, boosts, and more, helping players progress through the game at a faster pace. Points can be used to perform various actions in class, while gems can be exchanged for useful resources.
This makes their impact quite significant, allowing players to perform more actions for free without spending Robux or other real-world resources.
Also read: Unique Roblox usernames for new players
The Presentation Experience code troubleshooting [How to fix]
The Presentation Experience can identify incorrect or expired codes and displays an error message when they are entered.
As of yet, players have yet to discover any server-related issues that affect the code system negatively. If you run into such an error, restarting the Roblox Game Client may help.

Where to find new The Presentation Experience codes
More codes for The Presentation Experience can be found on the Minimal Games Roblox group and Discord server. You can also rely on this page for its active codes table, which will be updated the moment new ones are released.
FAQs on The Presentation Experience codes
What are the different rewards offered by the presentation experience codes.
You can receive points, gems, and boosts for redeeming codes in The Presentation Experience.
What is the highest amount of points obtainable through a single code in The Presentation Experience?
You can receive 200 points for redeeming the code Teachermadcuzbad , which is the highest out of any other codes in The Presentation Experience.
How many gems are available through codes for The Presentation Experience?
You can receive up to 190 gems by redeeming every code for The Presentation Experience.
- Clickbait / Misleading
- Factually Incorrect
- Hateful or Abusive
- Baseless Opinion
- Too Many Ads
Check out this A-Z list of all of our Roblox Codes 2024
Quick Links
Your perspective matters! Start the conversation
- Brainbuster🆕
- Money in the bank
- NXT Heatwave
- SK Shorts⏱️
- WWE WrestleMania XL
- Seth Rollins
- Roman Reigns
- Cody Rhodes
- PPV Schedule
- Dynasty Trade Analyzer
- Playoff Predictor ⚡
- Playoff Chances
- Mock Draft Simulator
- 2024 Draft Big Board
- Depth Charts
- Stat Leaders
- Start/ Sit Optimizer
- Patrick Mahomes
- NFL Mock Draft 2024
- Tony Pauline
- 2024 Scouting Reports
- Basketball Home
- NBA Draft Simulator
- Trade Rumors
- Players and Roster 2023
- Injury Updates
- World Baseball Classic
- Top MLB Picks
- Predictions
- New York Yankees
- Shohei Ohtani
- Alex Rodriguez
- Derek Jeter
- Free Agency
- NHL Predictions
- NHL Power Rankings
- Stanley Cup Final
- Tennis Home
- Wimbledon 2024
- Halle Open 2024
- Queen's Club Championships 2024
- Novak Djokovic
- Rafael Nadal
- Roger Federer
- Jannik Sinner
- Carlos Alcaraz
- Serena Williams
- Iga Swiatek
- Aryna Sabalenka
- ATP Rankings
- WTA Rankings
- ONE Championship
- UFC Fight Night
- UFC Fights Tonight
- ONE Championship Results
- ONE Championship Schedule
- ONE Championship Rankings
- Football Home
- Newsletters
- Copa America
- Champions League
- Nations League
- Charles Schwab Challenge
- Tiger Woods
- Phil Mickelson
- Paige Spiranac
- The Masters 2024
- The US Open
- Travelers Championship
- Canadian Grand Prix
- Max Verstappen
- Lewis Hamilton
- Red Bull Racing F1
- Mercedes F1 AMG
- F1 World Champions
- College Football Home
- Standings ⚡
- 2024 Recruitment Ranking
- College Basketball Home
- Cricket Home
- Womens Asia Cup T20
- ENG-W vs NZ-W
- Vitality Blast
- KL T20 Bash
- Global T20 Canada
- Esports Home
- Call Of Duty
- Wuthering Waves
- Gaming Tech
- Helldivers 2
- Word Game Solvers
- Wiki Guides
- Fortnite Home
- Fortnite Item Shop
- Fortnite Shop Predicted
- Fortnite Chapter 5 Season 3
- Fortnite Updates
- Creative Codes
- Deathrun Codes
- Skins & Characters
- Zone Wars Codes
- Prop Hunt Codes
- Horror Map Codes
- GTA 6 Leaks
- GTA 5 Cheats
- GTA 5 Cheats Xbox One
- GTA San Andreas
- GTA Vice City
- GTA San Andreas Cheats
- GTA 5 Songs
- GTA V Cheats PS4
- GTA 5 Cheats PS3
- GTA 6 Price
- Minecraft Home
- Minecraft 1.21 Update
- Best Seed Minecraft 1.20
- Minecraft 1.21 Seeds
- Minecraft 1.20 Update
- Minecraft Snapshots
- Minecraft Dungeons
- Minecraft Farms
- Minecraft Guide
- Minecraft Championship (MCC)
- Minecraft Villager Jobs
- Best Y Level for Diamonds 1.20
- Netherite in Minecraft
- AEW Dynamite
- AEWxNJPW: Forbidden Door III
- AEW Rampage
- Dragon Ball
- Jujutsu Kaisen
- Demon Slayer
- Tokyo Revengers
- Jujutsu Kaisen Chapter 262 Spoilers
- One Piece chapter 1117 Spoilers
- My Hero Academia chapter 426 spoilers
- Jujutsu Kaisen Chapter 263 spoilers
- Olympics 2024 Home
- Connections Hints
- Today's Wordle Answer
- Wordle Solver
- Word Unscrambler
- Spelling Bee Solver
- Minecraft Wiki
- Naruto Wiki
- TikTok Wiki
- Youtube Wiki
- Terraria Wiki
- One Piece Wiki
- Community Hub
- Motorsports
- Battlegrounds Mobile India
- College Baseball
- High School Sports
- Sports Fashion
- Daily Soaps
- Fantasy Cricket
- Indian Football
Hardcore Gamer
Roblox | the presentation experience codes (updated august 2023).

Your changes have been saved
Email Is sent
Please verify your email address.
You’ve reached your account maximum for followed topics.
Whirlight: No Time to Trip Demo Goes Live on Steam
Tokyo xanadu ex+ finally makes the jump to switch, maingear announces new 17" gaming laptop, quick links, active codes for the presentation experience, how to redeem codes in the presentation experience, expired codes for the presentation experience, what are roblox codes.
The Roblox game The Presentation Experience is a life simulator game created by Minimal Games. If you are looking for the latest 'The Presentation Experience' codes, then you have come to the right place.
Check out our other code guides for more Roblox fun here .
Listed below are all the currently known and working codes for The Presentation Experience. Roblox codes are released and expire at random intervals so be sure to check back frequently to get the latest free items.
'Codes were checked 8/8 and no new codes were added.'
- OMG350KLIKES – 100 Points & 12 Gems
- unexpected – 15 Gems
- 200MVISITS! – 100 Points
- maxwellgood – 20 Gems
- manfacepooper – 5x Points Boost for 10 Minutes
- fartyreward – 100 Points
- CHRISTMASGIFT – Free in-game Reward
- minimalgamespro – Free Gems or Points
- UwU – Free Gems or Points
- Hallway – Free Gems or Points
- pencil – Free Gems or Points
- 100MVISITS – Free Gems or Points
- MILLIONMEMBERS! – Free Gems or Points
- 800KFAVORITES – Free Gems or Points
- 900KMEMBERS – Free Gems or Points
- therearenootherteachersintheschoolbecausenobodywantstoseethebadteacher – Free Gems or Points
- nootnoot – Redeem code for free rewards
- 200KLIKES – Redeem code for 200 Points and 20 Gems
- funnybackrooms – Redeem code for 5 Gems
- bababooeypoints – Redeem code for free rewards
- egg – Redeem code for 50 Points
- 700kmembers – Redeem code for free rewards
- 180klikes – Redeem code for 10 Gems
- 660kfavorites – Redeem code for free rewards
- 175klikes – Redeem code for 10 Gems & 5x Points Boost for 5 Minutes
- Megaboost – Redeem code for a 5x Points Boost for 1 Minute
- anfisanova – Redeem code for 25 Points
- Minimalgamespro – Redeem code for 25 Points
- 5gems – Redeem code for 5 Gems
- update – Redeem code for 20 Gems
- 600kmembers – Redeem code for Free Points
- takenotes – Redeem code for Free Points
- emotionaldamage – Redeem code for 80 Points
- Poop – Redeem code for 100 Points
- toilet – Redeem code for 50 Points
- itsaboutdriveitsaboutpower – Redeem code for 150 Points
- helicopter – Redeem code for 50 Points
- RAT – Redeem code for 25 Points
- code – Redeem code for 15 Points
- 10points – Redeem code for 10 Points
- teachermadcuzbad – Redeem code for 200 Points
- NikkoCoder – Redeem code for 50 Points
- bookworm – Redeem code for 80 Points
- azureoptix – Redeem code for 25 Points
Redeeming Roblox codes varies from game to game. Follow our easy instructions listed below to redeem your free items. All codes are Case Sensitive so be sure to enter them exactly as shown above in our active list. If a code does not work after entering it correctly then it may have recently expired.
- Launch Roblox The Presentation Experience on the platform of your choice.
- Click on the triple dot icon on the top left of the screen.
- Click on the Codes icon in the new window.
- Copy a code from our active list into the box (Note: Codes are Case Sensitive)
- Click Redeem.
- Enjoy your new rewards!
Listed below are all the known expired codes for The Presentation Experience that are no longer redeemable.
- push-ups – Redeem code for 100 Points
- easter – Redeem code for free rewards
- minibonus – Redeem code for free rewards
- aprilfools – Redeem code for 150 Points
- jennahacker – Redeem code for 100 Points
- lava – Redeem code for 50 Points
- chugjug – Redeem code for 100 Points
- 500Kmembers – Redeem code for 500 Points
- 150KLIKES – Redeem code for Free Points
- Cringe – Redeem code for 25 Points
- Sheesh – Redeem code for 30 Points
- 220kmembers – Redeem code for 80 Points
- 210kmembers – Redeem code for Free Points
- 100klikes – Redeem code for 10x Points for 10 Minutes
- santaclaus – Redeem code for 50 Points
- Christmas – Redeem code for 250 Points
- beatbox – Redeem code for 30 Points
Roblox codes are redeemable phrases a game creator puts out to give their players free bonuses. Codes may come in the form of free spins, money, characters, potions, and some even unlock new content. They are mainly used to help players when they are starting out to get a jump start to their gaming experience.
- Mobile Games

The Presentation Experience Codes (July 2024) – Roblox Presentation Experience Codes List
The Presentation Experience is an experience developed by Minimal Games for the Roblox platform. The Presentation Experience is a roleplaying game in a school setting. A player is chosen to perform a presentation and all the other students in the classroom have to disrupt them. You can fart, cough, scream walk around, and more! To help you stir up trouble we have collected all of the latest The Presentation Experience codes .
The Presentation Experience codes are an easy way to earn in-game points. Points are used to perform disrupting actions. The more points the crazier the action. Use codes as soon as they release to accumulate your points since codes can expire at any moment. Bookmark this page so you can check back often.
If you find this post helpful, you can check out these posts on Manic Mining 2 codes , Anime Training Simulator codes , and Pet Simulator X codes .
The Presentation Experience Codes (Working)
Latest working the presentation experience codes.
There are currently no active codes. Please check back soon for updates.
Expired Codes
There are no expired codes.
How to redeem codes for The Presentation Experience
To redeem codes for The Presentation Experience , follow these steps:
- Launch The Presentation Experience in Roblox.
- Find and tap on the twitter codes icon on the top left.
- Enter a working code into the code redemption box.
- Tap on the Redeem button to redeem the code.
- Enjoy your free in-game rewards.

How to get more codes for The Presentation Experience
We will update this page as soon as new codes are released but you can also join the developer’s Discord community. Please be sure to follow their community guidelines. Don’t forget that you can hit CTRL+D to bookmark this page so that you can easily check back for new updates.


Roblox The Presentation Experience Codes (July 2023)
If you are playing Roblox The Presentation Experience and searching for codes to redeem for free in-game rewards, this article will help you out. Here, we’ve listed out all the available, new and latest codes that will earn you free points. It’s a funny roleplay game set in a school where you get to hold a presentation about a randomly chosen subject. The other students can interrupt the presentation by coughing, farting, screaming, beatboxing, and doing a lot of funny actions. You will need points to perform actions, so let’s find out how to claim them.
Note: These are all the codes that are working on March 31 , 2023 . There is no given expiry date for them but usually, such Roblox codes expire in 2 to 3 days.
Roblox The Presentation Experience Codes (Active)
Make sure to redeem these codes exactly as shown otherwise they may not work properly. You can also simply copy codes from the list above straight into Roblox to avoid any errors.
- maxwellgood – Redeem this code to get 20 Gems
- manfacepooper – Redeem this code to get 5x Points Boost for 10 Minutes
- fartyreward – Redeem this code to get 100 Points
- minimalgamespro – Redeem this code to get Free Gems or Points
- UwU – Redeem this code to get Free Gems or Points
- itsaboutdriveitsaboutpower – Redeem this code to get 150 Points for free
- Hallway – Redeem this code to get 10 Gems for free
- 5gems – Redeem this code to get 5 Gems for free
- emotionaldamage – Redeem this code to get 80 Points for free
- poop – Redeem this code to get 100 Points for free
- toilet – Redeem this code to get 50 Points for free
- helicopter – Redeem this code to get 50 Points for free
- code – Redeem this code to get 15 Points for free
- RAT – Redeem this code to get 25 Points for free
- NikkoCoder – Redeem this code to get 50 points for free
- 10points – Redeem this code to get 10 points for free
- teachermadcuzbad – Redeem this code to get 200 points for free
- azureoptix – Redeem this code to get 25 points for free
- Bookworm – Redeem this code to get 80 points for free
Don’t forget to join the Roblox group for 15 points every time you join the game. Plus, you will earn 2x Points in your own private server!
Expired Codes
- pencil – Redeem this code to get 100 Points
- nootnoot – Redeem this code to get 75 Points
- therearenootherteachersintheschoolbecausenobodywantstoseethebadteacher – Redeem this code to get 10 Gems for free
- Megaboost – Redeem this code to get 5X Points Boost for 1 minute for free
- anfisanova – Redeem this code to get 25 Points for free
- Minimalgamespro – Redeem this code to get 25 Points for free
- 660kfavorites – Redeem this code to get 66 Points for free
- minibonus – Redeem this code to get 50 Points and 3 Gems for free
- chugjug – Redeem this code to get 100 Points for free
- jennahacker – Redeem this code to get 100 Points for free
- 500Kmembers – Redeem this code to get 500 Points for free
- lava – Redeem this code to get 50 Points for free
- push-ups – Redeem this code to get 100 Points for free
- bababooeypoints – Redeem this code to get 50 Points for free
- 175klikes – Redeem this code to get 10 Gems and 5X Points Boost for 5 minutes for free
- beatbox – Redeem this code to get 30 Points for free
- sus – Redeem this code to get 30 Points for free
- Christmas – Redeem this code to get 250 points for free
- 75klikes – Redeem this code to get 150 points for free
- 80klikes – Redeem this code to get 50 points for free
- 20mvisits – Redeem this code to get 200 points for free
How to Redeem Codes in The Presentation Experience?
This is the easy process to redeem codes in this Roblox experience.
- First, launch the game.
- In the window that appears, type in a working code in the text field.
- Hit Redeem.
- You will know the reward that you have claimed immediately.
How to Get More New Codes?
New codes are released by the developers on social media so you can follow them on their Discord server . And you can always check back here often because we will keep this page updated with the latest codes.
That’s everything you need to know about these codes. We’ve got lots more Roblox codes posted on Gamer Tweak that you can check out for more rewards.

From making games to writing about them, she's been in the world of entertainment since a decade now. She writes features, the latest trending news and guides on games like Diablo 4, Overwatch 2, Roblox, codes and more fun stuff! Connect with her at - [email protected]
Related Posts
Dress to impress: how to get dti stars, all ranks in dress to impress (dti), how to rank up in dress to impress, once human: how to switch to ap ammo.
Type above and press Enter to search. Press Esc to cancel.
- All Game Guides
- Genshin Impact
- Call of Duty
- Final Fantasy
- Blox Fruits Codes
- Blade Ball Codes
- Fruit Battlegrounds Codes
- Haze Piece Codes
- King Legacy Codes
- Shindo Life Codes
- Peroxide Codes
- General Game Codes
- Genshin Impact Codes
- All Fortnite Guides and Cosmetics
- Fortnite Skins List
- Fortnite Item Shop
- Fortnite Leaked Skins & Cosmetics List
- Fortnite Rarest Skins
- Fortnite Rarest Emotes
Roblox The Presentation Experience Codes
Get ready to present!

Get your note cards ready, it's time to present! Hop into a virtual classroom inside of The Presentation Experience and be whatever kind of student you want! Are you the class clown? The attentive listener? The sleeper? The one who reminds the teacher that there's homework? The choice is yours! Interact with your peers by spending points to cheer them on while they present, or throw them off with various sounds and physical interruptions! So how do you get points quickly? With codes of course!
All of the codes below can be used to redeem a certain amount of points, or even a special point boost if you're lucky! If you're looking for even more freebies, be sure to check back with this article regularly—we update this list as soon as new codes come out! If you find a code in the Working Codes section that seems expired, please let us know so we can remove it as soon as possible. Keep in mind, also, that you'll need to enter each code exactly as it's written or the experience won't accept it!
If you're looking for more Roblox content to browse while you wait for new codes, check out some of our best of articles including 5 best Roblox games like Call of Duty , 5 best Roblox games like Pokémon , or Best Roblox games like The Sims !
All The Presentation Experience Codes List
The presentation experience codes (working).
- scaryhalloween2023 —Redeem for 60 Points and 15 Gems (New)
- spookpoints —Redeem for 100 Points (New)
- summerboost —Redeem for a 5x Point Boost for 10 min (New)
- OMG350KLIKES —Redeem for 50 Points
- unexpected —Redeem for 15 Gems
- UGC —Redeem for 30 Gems
- coffee —Redeem for 60 Points
- maxwellgood —Redeem for 20 Gems
- manfacepooper —Redeem for a 5x Point Boost for 10 min
- fartyreward —Redeem for 100 Points
- minimalgamespro —Redeem for 25 Points
- UwU —Redeem for 20 Gems
- Hallway —Redeem for 10 Gems
- pencil —Redeem for 100 Points
- 100MVISITS —Redeem for 15 Gems
- MILLIONMEMBERS! —Redeem for 10 Gems and 10 minutes of 5x XP
- therearenootherteachersintheschoolbecausenobodywantstoseethebadteacher —Redeem for 10 Gems
- nootnoot —Redeem for 75 Points
- Megaboost —Redeem for 5x Points for mone minute
- 5gems —Redeem for 5 Gems
- toilet —Redeem for 50 points
- itsaboutdriveitsaboutpower —Redeem for 150 Points
- poop - Redeem for 100 Points
- NikkoCoder - Redeem for 50 Points
- bookworm - Redeem for 80 Points
- code - Redeem for 15 Points
- RAT - Redeem for 25 Points
- Teachermadcuzbad - Redeem for 200 Points
The Presentation Experience Codes (Expired)
These The Presentation Experience codes no longer work.
- 200MVISITS! —Redeem for 100 Points
- CHRISTMASGIFT —Redeem for 39 Gems
- anfisanova —Redeem for 25 Points
- bababooeypoints —Redeem for 50 Points
- 180klikes —Redeem for 10 Gems
- Easter —Redeem for 8 Gems
- 700kmembers —Redeem for 10 Gems and a 1 minute 5x Points Boost
- 600kmembers —Redeem for 5 minutes of 2x Boost
- 175klikes —Redeem for 10 Gems and 5x Point Boost
- beatbox - Redeem for 30 Points
- sus - Redeem for 30 Points
How to Redeem The Presentation Experience Codes
It's easy to redeem codes for free rewards in The Presentation Experience ! To do so, simply follow the steps below.
- First, launch the experience
- Once inside, look for the Gear in the top left corner and click on it .
- Then, select the Twitter bird icon labeled Codes.
- Type or copy and paste a code into the new window that appears.
- Press confirm to receive your free reward!
How do I get more The Presentation Experience codes?
Codes for The Presentation Experience are typically released each time that the experience hits a new like milestone. To stay up to date on these codes, be sure to check back with this article often, join the Minimal Community Discord server, and join the Minimal Games Roblox group . Players who join the Roblox group will also receive a bonus 500 points and 10 Gems!
Why aren't my codes working?
Not all Roblox codes are active for the same amount of time, meaning some expire exceptionally quickly and may even become inactive after 24 hours or less! If you attempt to enter a code and it says Code Expired , that code is no longer active and, unfortunately, can no longer be redeemed. There's nothing that you can do to fix this issue, the code is simply unobtainable. If you attempt to type in a code and it says Invalid Code , however, this means that you've likely mistyped the code or neglected to use the correct capitalization. If this happens, try to retype and re-enter the code once more, being sure to copy it exactly as it's written!
What is The Presentation Experience?
The Presentation Experience is a school-based role play experience that allows players to take turns presenting randomly selected topics that are either created by the AI teacher or other players/students in the classroom. Once the teacher calls on you to present, you better be ready—you only have a few minutes to make a great impression! During presentations, other students can clap, scream, jump out of their seat, sleep, burp, and more to interrupt or cheer on their peers. The teacher will do her best to control the class, but it's only a matter of time before things get out of hand!
If you're looking for codes for other games, we have a ton of them in our Roblox Game Codes post! You can also get a bunch of free stuff via our Roblox Promo Codes page.
About the Author
More Stories by Jean-Pierre van Wyk
52 comments, cancel reply.
Comments are on moderation and will be approved in a timely manner. Please read the following rules before commenting:
- All comments must be on topic and add something of substance to the post
- No swearing or inappropriate words
- No asking or begging for anything free
- Do not attempt to start a poll in the comments
- Comments in all CAPS will be removed
- We reserve the right to remove a comment for any reason
- Do not impersonate a staff member or influencer
Save my nickname and email in this browser for the next time I comment.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Generic selectors Exact matches only Search in title Search in content Post Type Selectors Learn More
Roblox: All The Presentation Experience codes and how to use them (Updated March 2023)

In school, you’ve probably experienced trying not to laugh when your friend says something funny while someone is discussing the lesson in front.
With The Presentation Experience on Roblox , you no longer need to stop laughing. In fact, you can interrupt the presentation as much as you want by coughing, farting, screaming, raging, partying, and more!
READ MORE: Roblox: All Demon Blade Tycoon Codes and How to Use Them
While that does sound fun in-game, we do NOT recommend that in real life. Remember to respect and listen to your teachers and/or whoever speaks in front. Moreover, things could change, and you might also become the interrupted presenter. You don’t want to get interrupted, do you?
Nonetheless, we have gathered The Presentation Experience codes that you can use to redeem points and let you enjoy the game even more.

List of All The Presentation Experience Codes
Below is a list of codes that will give you a lot of points in The Presentation Experience . Make sure you enter the codes as they are because they can be case-sensitive.
Moreover, redeem these codes as fast as you can . You never know when they will expire.
Active Codes
- coffee – redeem 60 points (New!)
- maxwellgood – redeem 20 Gems
- UwU – redeem 20 Gems
- Hallway – redeem 10 Gems
- fartyreward – redeem 100 Points
- manfacepooper – redeem 5x Points for 10 minutes
- CHRISTMASGIFT – redeem 39 Gems
- minimalgamespro – redeem 25 Points
- pencil – redeem 100 Points
- 5gems – redeem 5 Gems
- nootnoot – redeem 50 Points
- Megaboost – redeem 5x Points for 60 seconds
Expired Codes
Below are the codes that are no longer valid. We will make sure to update the article once some of the current active codes expire.
- CHRISTMASGIFT – Redeem 39 Gems
- anfisanova – Redeem 25 Points
- bababooeypoints
- 700kmembers
- 600kmembers
- beatbox
READ MORE: Roblox: All Anime Warrior Simulator Codes and How to Use Them
How to Use Codes
- Launch the game.
- Press the Twitter Bird icon.
- Type in the code of your choice. Again, make sure to enter the code exactly as it appears on the list above.
- Press redeem.
Roblox is an online game platform and game creation system. Released in 2006, it allows users to create games for others to play and/or play games created by others.

All Rights Reserved. No part of this site or its content may be reproduced without the permission of the copyright holder.
Genshin Impact
Grand theft auto, click media group, battle pass, advertise with us | write for us | privacy policy | opencritic | brands | contact us, © 2024 click media group | all rights reserved | proudly developed by darkdev. design.

Generic selectors Exact matches only Search in title Search in content Post Type Selectors
The Presentation Experience Codes, Free Points and Gems (October 2023)

Video Gamer is reader-supported. When you buy through links on our site, we may earn an affiliate commission. Prices subject to change. Learn more
The Presentation Experience is a game mode in Roblox that allows you to relive your school days as you try to give your presentation to a rowdy class of players. You could also operate as a listener yourself and aim to disrupt the classroom presentations and possibly get your own experience as a troublemaker, a listener, a clown, or whatever student you wish to be.
However, if you want to have an easier time dealing with these ruffians, then make sure to avail all the redeemable codes this game mode has to offer. What are redeemable codes and where can you get them? Keep on reading to find out!
Now Read: Today’s Coin Master Free Spins and Coins Links
What Are The Presentation Experience Codes
The presentation experience codes generally offer two kinds of rewards. The first one of these is the Gems currency which is what you can use to purchase a variety of different cosmetics for this game mode. The second kind of redeem code reward are the points which are what players use to interact with the classroom during the presentations and cause all sorts of hilarious shenanigans.
NOW READ: Check Out All The Hot Deals At Green Man Gaming – 15% OFF Selected PC Games
Active Presentation Experience Codes
Below is a list of the currently active codes for this game mode that you can redeem. Make sure to redeem these on time, as we never know when the developers may decide to expire them.
| summerboost | 5x Point Boost for 10 Minutes |
| OMG350KLIKES | 50 Points |
| unexpected | 100 Points |
| 200MVISITS! | 100 Points |
| UwU | 20 Free Gems |
| minimalgamespro | 25 Points |
| pencil | 100 Points |
| Megaboost | Get 5x more points for 1 minute |
| coffee | 60 Points |
| maxwellgood | 20 Gems |
| fartyreward | 100 Points |
| manfacepooper | 5x points for ten minutes |
| CHRISTMASGIFT | 39 Gems |
| Hallway | 10 Gems |
| 5gems | 5 Gems |
| nootnoot | 50 Points |
Expired Presentation Experience Codes
These are the currently expired codes for presentation experience. This means you will not be able to redeem the rewards even if you are trying to make use of these codes.
| bababooeypoints | 50 Points |
| 180klikes | 10 Gems |
| Easter | 8 Gems |
| 700kmembers | 10 Gems and a 1 minute 5x Points Boost |
| 600kmembers | 2x Boost for 5 minutes |
| 175klikes | 10 Gems and 5x Point Boost |
| beatbox | 30 Points |
| sus | 30 Points |
How to Redeem Presentation Experience Codes
There are a lot of codes to go through for The Presentation Experience but luckily the method to redeem these is simple like most other Roblox game modes. Just follow these steps:
- Launch Roblox and open up The Presentation Experience
- On the top left of the screen, click the Settings icon (looks like a gear)
- From here, click the Codes icon (looks like the Twitter bird)
- Enter the redeemable code from our list above. Keep in mind that these are case-sensitive codes
- Finally, press the Redeem button and receive your free rewards!
Final Thoughts
The Presentation Experience is a fun game mode that lets players relive the classroom experience together. It is growing quickly and receives a lot of updates which include new redeemable codes for the players to access. With that said, make sure to check back on this page once in a while to get an update on any new redeemable codes available.
About the Author
Si Yan is an editor on Videogamer.com, researching interesting topics, working with a team for content creation and then editing onto site. Game wise Si Yan loves Pokémon and Super Mario.

- - 27 January 2016 ( Xbox One )
- Platform(s): Android, iOS, macOS, PC, PlayStation 4, PlayStation 5, Xbox One, Xbox Series S, Xbox Series X
- Genre(s): Action, Adventure, Arcade, Board Games, Card, Casual, Educational, Family, Fighting, Indie, Massively Multiplayer, Massively Multiplayer Online, Platformer, Puzzle, Racing, RPG, Shooter, Simulation, Sports, Strategy
Related Topics
Subscribe to our newsletters.
By subscribing, you agree to our Privacy Policy and may receive occasional deal communications; you can unsubscribe anytime.
- Call of Duty
- Apex Legends
- Dead By Daylight
- Attachments
- Field Upgrades
- Killstreaks
- Action and Adventure Games
- Battle Royale
- Indie Games
- Like a Dragon Gaiden: The Man Who Erased His Name
- Only Mobile Gaming
- Role Playing Games
- Shooter Games
- Sports Games
- Strategy and Simulation Games
- The Casting of Frank Stone
- The Day Before
The Presentation Experience codes (September 2023) - Free points and actions
Break the rules with our The Presentation Experience codes.

Published: Aug 08, 2022, 11:09 Updated: Sep 21, 2023, 11:25
Looking for The Presentation Experience codes ? We're here to help! This wildly popular Roblox game is all about going back to school, with lobbies of players randomly selected to present in front of the class. So they can discuss anything they wish, no matter how wacky. This is where the game's charm shines through.
Our list of codes will break down each and every redeemable currently available in the game for you to use. We'll also go over how to redeem your codes, as well as where to check for new freebies in the future.
Table of Contents
New the presentation experience codes (september 2023), how do i use codes, what are the presentation experience codes, how do i get more codes, how to get free presentation experience points.
But do you want even more Roblox codes ? Then be sure to grab some AFSX codes and IQ Wars Simulator codes for two very popular games. We've also got an Anime Fighting Simulator X tier list to use!
- OMG350KLIKES (NEW)
- unexpected - 15 Gems
- UGC - 30 Gems
- coffee - 60 points
- maxwellgood - 20 Gems
- fartyreward - 100 points
- manfacepooper - 5x points boost for 10 minutes
- minimalgamespro - 25 ponts
- UwU - 20 Gems
- Hallway - 10 Gems
- 5gems - 5 Gems
- Megaboost - 5x points boost for one minute
Expired codes:
- MILLIONMEMBERS! - Free Gems
- egg - 50 points
- 800KFAVORITES - Free Gems
- 900KMEMBERS - Free Gems
- therearenootherteachersintheschoolbecausenobodywantstoseethebadteacher - 10 Gems
- nootnoot - 75 points
- anfisanova - 25 points
- Megaboost - 5x points for 60 seconds
- 5gems - 5 gems
- toilet - 50 points
- code - 15 points
- RAT - 25 points
- Poop - 100 points
- itsaboutdriveitsabuotpower - 100 points
- NikkoCoder - 50 Points
- Bookworm - 80 points
- teachermadcuzbad - 200 points
- bababooeypoints
- intensesilence
- 500Kmembers
- 160kmembers
- Boot up The Presentation Experience, either via the Roblox game page or the mobile app.
- Once you're in a lobby, tap the Twitter bird icon at the top of the screen. This takes you to the code redemption menu.
- Choose your code from our list and paste it into this text box.
- Hit Redeem, and if the code is valid and working, you'll get a message detailing your new items!
The good news is that using codes is a really easy process. Plus, it's identical regardless of whether you're playing on PC or mobile. So once you're in-game, it's just a matter of tapping the Twitter icon at the top of the screen, entering your codes, and spending those points being a class clown.
In The Presentation Experience, codes are used to redeem free items. That's the case with most Roblox games, but for this specific title, they grant you access to a bunch of free points. This is an all-important in-game currency used to execute actions.
Usually, you're stuck at your desk, unable to walk about or interact with anything. Only a few actions, like saying yes, or no, or falling asleep, are available for zero points. Other wackier actions like shooting fireworks, vomiting, or walking around cost points.
- Further freebies: Anime Simulator X codes
As such, points are quite a valuable commodity. You can earn them passively just by sitting at your desk, but this is quite a slow process.
Using our codes gets you a healthy amount of points instantly. This means you'll be able to use any of the basic actions, with money left over. The premium actions are slightly more advanced, however. These involve you walking out of the classroom or controlling other players' actions. But these cost Robux to use, so they won't be available through codes.
Since it's such a popular game, you can guarantee that more codes will arrive for The Presentation Experience in the future. As such, we've compiled a few places you should check for new freebies, and when they might drop.
First off, it's a good idea to frequently check the Roblox game page. Brand-new codes are posted in the description, which is where the code will land for the first time. They'll subsequently be posted in the Minimal Community Discord server , so head over and join that to stay in the loop.
Of course, we also recommend bookmarking this page and coming back often. We'll update our list as and when new codes for The Presentation Experience are released. If you don't fancy trawling through social media in search of codes, we'll compile them all together here for you. Enjoy your free points!
Why are my The Presentation Experience codes not working?
It may be a simple case of trying to redeem a code that's already expired. So be sure to check back with us regularly, because we'll keep this list up to date with brand-new codes as well as expired ones!
Have you exhausted the latest Presentation Experience codes? Need more points to fart your way through school? You can get a bunch of free Presentation Experience codes by joining the game group . You'll get 500 points just for logging in each day, which is far more than any of the current codes will give you.
But there you have it, that's all you need to know about redeeming codes for this game! Of course, there's a lot more to Roblox than just this title. We recommend checking out our Shindo Life codes if ninja-based action is up your street. Additionally, Tower Defense fans will appreciate some Retro TDS codes and All Star Tower Defense codes , too. As well as that, outside of Roblox, you can't go wrong with our Cookie Run: Kingdom codes list.
Explore new topics and discover content that's right for you!
Welcome back!
Sign in or create an account to enjoy GINX perks, enter competitions and access exclusive features.
Your status: free member
Your status: friend, your status: supporter, your status: super fan, your status: producer, your status: producer (permanently whitelisted).

- Counter-Strike 2
- EA Sports College Football
- Dead by Daylight

Roblox The Presentation Experience Codes (September 2023): Free Points & Gems
The Presentation Experience in Roblox is a funny school roleplay game in which players will have to give a presentation on a subject that they can choose according to their own will, or a topic will be assigned to them randomly.
The objective is to give the presentation to earn points that you can use to create disturbance in other players' presentations by coughing, farting, screaming, raging, partying, and more.
While it's fun to play, sometimes it can be interrupted if you are short on points. In that case, you can earn some free points by redeeming The Presentation Experience codes.
1 September 2023 update - We've checked for the latest 'Roblox The Presentation Experience Codes.' All the most recent and active codes can be found just below.
Table of Contents
- Latest The Presentation News
New Roblox The Presentation Experience Codes - Working
All expired the presentation experience codes, how to redeem the presentation experience codes.

All Roblox The Presentation Experience Codes
Roblox The Presentation Experience codes are released via the game’s social media handles, Discord server, and more. Also, make sure to redeem these codes as early as possible since most of them are time-limited.
- summerboost - Redeem for a 5x Point Boost for 10 min
- OMG350KLIKES - Redeem for 50 Points
- unexpected - Redeem for 15 Gems
- UGC - Redeem for 30 Gems
- coffee - Redeem for 60 Points
- maxwellgood - Redeem for 20 Gems
- manfacepooper - Redeem for a 5x Point Boost for 10 min
- fartyreward - Redeem for 100 Points
- minimalgamespro - Redeem for 25 Points
- UwU - Redeem for 20 Gems
- Hallway - Redeem for 10 Gems
- pencil - Redeem for 100 Points
- 100MVISITS - Redeem for 15 Gems
- MILLIONMEMBERS! - Redeem for 10 Gems and 10 minutes of 5x XP
- therearenootherteachersintheschoolbecausenobodywantstoseethebadteacher - Redeem for 10 Gems
- nootnoot - Redeem for 75 Points
- Megaboost - Redeem for 5x Points for mone minute
- 5gems - Redeem for 5 Gems
- toilet - Redeem for 50 points
- itsaboutdriveitsaboutpower - Redeem for 150 Points
- poop - Redeem for 100 Points
- NikkoCoder - Redeem for 50 Points
- bookworm - Redeem for 80 Points
- code - Redeem for 15 Points
- RAT - Redeem for 25 Points
- Teachermadcuzbad - Redeem for 200 Points
We will keep on updating the list as soon as new codes arrive, so make sure to keep an eye on this page to not miss out on anything.
Below is a list of Roblox The Presentation Experience codes that have now expired. Somewhat surprisingly, some players actually Google ‘How do I use expired The Presentation Experience codes?’ but sorry, they can no longer be used once they've expired.
For the sake of prosperity, below is the list of all expired The Presentation Experience codes that are no longer available for redemption.
- 200MVISITS! - Redeem for 100 Points
- CHRISTMASGIFT - Redeem for 39 Gems
- anfisanova - Redeem for 25 Points
- bababooeypoints - Redeem for 50 Points
- 180klikes - Redeem for 10 Gems
- Easter - Redeem for 8 Gems
- 700kmembers - Redeem for 10 Gems and a 1 minute 5x Points Boost
- 600kmembers - Redeem for 5 minutes of 2x Boost
- 175klikes - Redeem for 10 Gems and 5x Point Boost
- beatbox - Redeem for 30 Points
- sus - Redeem for 30 Points
If you are new to the game and don’t know how to redeem Roblox The Presentation Experience codes, we have listed below the steps that you can follow to claim free rewards:
- Open Roblox The Presentation Experience on your device.
- Click on the Twitter icon button present at the upper side of the screen.
- Paste the code there and hit enter to claim your rewards.
So there you have it, the latest Roblox Redeem codes to use for free rewards and how to redeem them with ease.

IMAGES
VIDEO
COMMENTS
The Presentation Experience Codes (Working) scaryhalloween2023 —Redeem for 60 Points and 15 Gems (New) spookpoints —Redeem for 100 Points (New) summerboost —Redeem for a 5x Point Boost for 10 min (New) OMG350KLIKES —Redeem for 50 Points. unexpected —Redeem for 15 Gems. UGC —Redeem for 30 Gems. coffee —Redeem for 60 Points.
Working The Presentation Experience Codes. COFFEE - Enter this code to get 60 Points. MAXWELLGOOD - Enter this code to get 20 Gems. MANFACEPOOPER - Enter this code to get 5x Points Boost for 10 ...
Here are all the latest The Presentation Experience codes: dodgingcode - Free 50 Gems. 400KLIKES - Free 10 Gems, Points Boost. scaryhalloween2023 - Free 60 Points, 15 Gems. spookpoints ...
The Presentation Experience codes are free rewards given out by the developer that can be redeemed for points and gems. These are the currencies that you let do fun stuff during the class, like shaking the whole place with an earthquake or turning into a helicopter. New codes are released alongside updates, events, and like milestones.
How to redeem codes in The Presentation Experience. Launch The Presentation Experience through the official Roblox website. Tap on the X icon at the top of the screen. A redemption box should appear. Carefully type or copy-paste the desired code and hit Redeem. If the code is correct and valid, the corresponding rewards should appear on the screen.
This code credits your account with 20 Gems. This code credits your account with 10 Gems. This code credits your account with 5 Gems. This code credits your account with 25 Points. This code credits your account with 50 Points. This code credits your account with a 1 Minute 5x Points Boost.
To redeem codes in Roblox The Presentation Experience, you will just need to follow these steps: Open up Roblox The Presentation Experience on your PC or Mobile device. Tap on the Twitter button at the top of the screen. Copy a code from our list. Paste it into the "Code" textbox.
Here's what you'll need to do: Launch The Presentation Experience in Roblox. Click the button with the three dots near the top left corner of your screen. Image credit: Minimal Games/VG247 ...
Codes are a feature in The Presentation Experience. It's not really crucial since it's not a core feature in the game, however they can help you if you want a special bonus or want free Points or Gems. Codes have existed since the game existed (probably), and they still exist in the experience to this day. Here are many codes in The Presentation Experience that you can redeem! These are not ...
The Presentation Experience has plenty of codes for players to use, that can make their lives a lot easier. The Presentation Experience is as it sounds, a Roblox game that reenacts the experience of being in the classroom, with all the stress that entails.. To ease that burden somewhat, the codes below provide useful gems and points in the game, so continue reading to find the full list of up ...
Using The Presentation Experience codes is the best way to accumulate a large number of points and gems in the title. Additionally, the Roblox game offers boosts to help you increase the rate of ...
Expired Codes For The Presentation Experience. Listed below are all the known expired codes for The Presentation Experience that are no longer redeemable. push-ups - Redeem code for 100 Points ...
How to redeem codes for The Presentation Experience . To redeem codes for The Presentation Experience, follow these steps: Launch The Presentation Experience in Roblox. Find and tap on the twitter codes icon on the top left. Enter a working code into the code redemption box. Tap on the Redeem button to redeem the code. Enjoy your free in-game ...
The Presentation Experience is a fun roleplaying Roblox game where you can either hold a presentation or interrupt someone else's presentation. Spend your Points, Gems or Robux to do actions like cough, fart, scream, rage, party, earthquake, and much more. Use The Presentation Experience codes to get free rewards such as Points and Gems to make the game more enjoyable.
This is the easy process to redeem codes in this Roblox experience. First, launch the game. Click on the Twitter bird icon at the top left section of the screen. Here's how to Redeem Codes in The Presentation Experience. In the window that appears, type in a working code in the text field. Hit Redeem.
The Presentation Experience Codes (Working) scaryhalloween2023 —Redeem for 60 Points and 15 Gems (New) spookpoints —Redeem for 100 Points (New) summerboost —Redeem for a 5x Point Boost for 10 min (New) OMG350KLIKES —Redeem for 50 Points. unexpected —Redeem for 15 Gems. UGC —Redeem for 30 Gems. coffee —Redeem for 60 Points.
5gems - redeem 5 Gems. nootnoot - redeem 50 Points. Megaboost - redeem 5x Points for 60 seconds. Expired Codes. Below are the codes that are no longer valid. We will make sure to update the article once some of the current active codes expire. CHRISTMASGIFT - Redeem 39 Gems. anfisanova - Redeem 25 Points. bababooeypoints.
Just follow these steps: Launch Roblox and open up The Presentation Experience. On the top left of the screen, click the Settings icon (looks like a gear) From here, click the Codes icon (looks ...
The Presentation Experience Codes. Last checked for new codes on April 26. Active Codes. 200MVISITS! - 100 Points. coffee - 60 Points. maxwellgood - 20 Gems. manfacepooper - Point Boost ...
In The Presentation Experience, codes are used to redeem free items. That's the case with most Roblox games, but for this specific title, they grant you access to a bunch of free points. This is an all-important in-game currency used to execute actions. Usually, you're stuck at your desk, unable to walk about or interact with anything.
Here are the steps to take to redeem The Presentation Experience codes: Open Roblox and start The Presentation Experience. Hit the three dots on the top of the screen. Hit 'Codes'. Enter the codes into the box and hit enter. What To Do About A Broken Code. If you try and redeem a code and it doesn't work, this is likely due to an expired ...
Also, make sure to redeem these codes as early as possible since most of them are time-limited. New Roblox The Presentation Experience Codes - Working. summerboost - Redeem for a 5x Point Boost for 10 min. OMG350KLIKES - Redeem for 50 Points. unexpected - Redeem for 15 Gems.
Roblox fans can take a look at this article to find all the latest codes for The Presentation Experience. Roblox: Anime Last Stand: All Codes Redeeming active codes will give you a bunch of Emeralds.