- Open access
- Published: 08 April 2024

Patient satisfaction with preoperative nursing care and its associated factors in surgical procedures, 2023: a cross-sectional study
- Bizuayehu Atinafu Ataro 1 ,
- Temesgen Geta 2 ,
- Eshetu Elfios Endirias 1 ,
- Christian Kebede Gadabo 3 &
- Getachew Nigussie Bolado 1
BMC Nursing volume 23 , Article number: 235 ( 2024 ) Cite this article
359 Accesses
Metrics details
To enhance patient satisfaction, nurses engaged in preoperative care must possess a comprehensive understanding of the most up-to-date evidence. However, there is a notable dearth of relevant information regarding the current status of preoperative care satisfaction and its impact, despite a significant rise in the number of patients seeking surgical intervention with complex medical requirements.
To assess patient satisfaction with preoperative nursing care and its associated factors in surgical procedures of, 2023.
A cross-sectional study was conducted, and the data was collected from the randomly selected 468 patients who had undergone surgery during the study period. The collected data was entered into Epidata version 3.1 and analyzed using SPSS version 25 software.
The complete participation and response of 468 participants resulted in a response rate of 100%. Overall patient satisfaction with preoperative nursing care was 79.5%. Sex (Adjusted odds ratio (AOR): 1.14 (95% confidence interval (CI): 0.21–2.91)), payment status for treatment (AOR: 1.45 (95% CI: 0.66–2.97)), preoperative fear and anxiety (AOR: 1.01, 95% CI: 0.49–2.13)), patient expectations (AOR: 3.39, 95% CI: 2.17–7.11)), and preoperative education (AOR: 1.148, 95% CI: 0.54–2.86)) exhibited significant associations with patient satisfaction with preoperative nursing care.
It is important to exercise caution when interpreting the level of preoperative nursing care satisfaction in this study. The significance of preoperative nursing care satisfaction lies in its reflection of healthcare quality, as even minor deficiencies in preoperative care can potentially lead to life-threatening complications, including mortality. Therefore, prioritizing the improvement of healthcare quality is essential to enhance patient satisfaction.
Peer Review reports
Preoperative care encompasses the provisions given prior to surgery, wherein the patient’s unique requirements are considered to undertake physical and psychological preparations in anticipation of the procedure [ 1 ]. This phase commences upon the patient’s admission to the hospital or surgical facility and extends until the commencement of the actual procedure [ 1 , 2 , 3 , 4 ]. The primary emphasis in preoperative preparation should lie in the advancement of techniques aimed at mitigating the emotional distress experienced by surgical patients [ 5 ]. In this context, nurses play a crucial role in formulating, developing, expanding, and implementing interventions and modifications [ 5 , 6 ].
The primary goal of a healthcare system is to ensure the provision of medical care that is of the utmost quality and safety [ 7 ]. In this context, patient safety has emerged as a paramount concern and is currently placed at the forefront of priorities [ 8 , 9 ]. A systematic review conducted in Saudi Arabia and Turkey concluded that preoperative nursing assessment plays a vital role in mitigating preoperative complications by alleviating anxiety and enhancing patients’ understanding of the surgical procedure. This, in turn, has a substantial positive impact on patient satisfaction [ 10 , 11 ]. The review also emphasized the necessity of nurses receiving proper training and education in preoperative assessment, as the absence of adequately trained nursing staff elevates patient anxiety levels and renders them susceptible to potential complications [ 2 , 10 ].
Patient satisfaction is defined as a subjective reaction to the context, process, and result of the service experience one has received [ 12 , 13 ]. The measurement of quality is closely linked to the satisfaction levels expressed by patients regarding the care they have received [ 14 , 15 ]. Both the practice environment and the personal characteristics of nurses serve as significant indicators of the quality of patient care [ 16 ]. Enhancing working conditions and achieving improved patient outcomes, including reduced mortality rates, are facilitated by a positive relationship between the work environment attributes of nurses and their levels of proficiency and personal capabilities [ 17 ]. Additionally, various aspects of the workplace, such as the physical setting, working hours, and the level of fatigue among nursing staff, have been found to influence the safety and quality of patient care [ 18 ].
Comprehensive nursing interventions should be implemented throughout the entire perioperative phase to prevent complications and adverse events in the surgical domain [ 19 ]. Although the impact of perioperative nursing interventions on patient health outcomes may not be fully comprehended, it is substantial in its significance [ 20 ]. Through the provision of care during the postoperative period, nurses can effectively mitigate the occurrence of adverse events, even though certain studies have identified nurses’ workload and time constraints as predominant barriers to effective nurse-patient communication [ 21 , 22 , 23 , 24 ]. Preoperative nursing assessment plays a pivotal role in delineating and discerning the patient’s risk factors throughout their perioperative care, extending beyond the confines of the surgical procedure itself [ 25 , 26 ].
To optimize patient care and enhance postoperative outcomes, it is imperative for nurses engaged in patient assessment and preoperative care to possess comprehensive knowledge and understanding of the latest research in this field [ 27 ]. Throughout the preoperative phase, nurses provided comfort, guidance, and rehabilitation to the patients. However, they failed to involve the patients in their treatment [ 28 , 29 ]. An unfortunate number of patients endured minor injuries due to improper utilization of theater equipment, such as diathermy devices, along with inadequate implementation of safety precautions by the nursing staff during the surgical procedure [ 28 , 30 ]. Furthermore, patients were left feeling bewildered and unsettled due to the nurses’ deficient communication [ 28 , 31 ].
The perioperative environment possesses distinctive characteristics, encompassing intricate clinical care delivered by specialized teams, substantial costs, utilization of advanced technologies, and a vast array of challenging-to-manage resources [ 30 , 32 ]. These factors can contribute to the development of highly intricate settings prone to adverse events concerning patient safety [ 32 , 33 ]. Medication errors, omissions, patient misidentification, and surgical site misidentification are among the various types of mistakes that can occur during surgical procedures [ 34 ]. Birmingham-based research showcased that reducing waiting times, enhancing patient satisfaction, and upholding the efficacy of clinical services were the outcomes of evaluating patient load and the delivery system within the clinic [ 35 , 36 ]. To optimize patient satisfaction, nurses involved in preoperative care must possess up-to-date knowledge and understanding of the most recent research [ 27 ]. Despite the significant increase in the number of patients requiring surgery, with complex medical needs, a scarcity of pertinent data exists regarding the satisfaction levels and impacts associated with preoperative care.
Studies conducted in Ethiopia showed varying levels of patient satisfaction with preoperative nursing care in surgical procedures. The cross-sectional study carried out in Addis Ababa, Western Amhara referral hospitals, University of Gondar Comprehensive Specialized Hospital, East Amhara referral hospitals and Gamo and Gofa zone showed that the patient satisfaction with preoperative care ranges from 36.6 to 84% [ 12 , 37 , 38 , 39 , 40 ]. According to the study conducted at Sohag University, the overall satisfaction score of patients who underwent surgery was determined to be 61.9% [ 41 ].
Various factors play key roles in influencing patient satisfaction with preoperative nursing care, both related to the hospital and nursing environment (such as ward/unit dynamics, length of hospitalization, surgical specialization, waiting times, nurse responsiveness), patient and family characteristics (including financial status, prior hospitalizations, service expectations, health conditions, procedure types, complications, discharge plans, anxiety levels, illness duration, family size), and preoperative education can seriously influence satisfaction levels of patients with preoperative nursing care. Additionally, sociodemographic factors like gender, age, income, residence, marital status, religion, ethnicity, education level, and occupation may also significantly impact patient satisfaction [ 1 , 10 , 12 , 32 , 37 , 38 , 39 , 40 , 41 , 42 ].
Enhancing patient satisfaction with preoperative nursing care is vital for patient-centered healthcare. This study investigates the factors influencing patient satisfaction in surgical procedures, aiming to improve care quality. By identifying areas for enhancement, the research informs healthcare practices, potentially leading to better patient experiences and outcomes. Contributing to the existing literature, this contemporary study provides updated insights into patient preferences, guiding efforts toward optimized preoperative care delivery and improved surgical outcomes. This research can also pave the way for advancements in patient-centered care approaches and potentially lead to positive impacts on healthcare outcomes and patient experiences in surgical settings.
Most of the previous research conducted in Ethiopia has primarily focused on evaluating patient satisfaction with the overall hospital services. However, this particular study honed in on specifically examining the satisfaction levels of preoperative nursing care services. This focus was chosen due to the profound impact that such care has on surgical outcomes and subsequent postoperative recovery. Notably, this study stands as the first of its kind within our study area; as far as we know, no prior study of this nature has been conducted. It is also worth noting that while some previous studies had utilized nurses as study participants, this study appropriately selected patients, as they possess indispensable insights into the quality of nursing care and ultimately determine the level of satisfaction experienced. Additionally, this study introduced previously unstudied variables, such as patient flow per shift and nurses’ willingness to listen and respond to questions, which hold the potential for significant associations with satisfaction levels regarding preoperative nursing care services. Therefore, this study aimed to comprehensively assess patient satisfaction with preoperative nursing care and its associated factors in surgical procedures.
Methods and materials
Study area and period.
This study was carried out in the Wolaita Zone, located 329 km away from Addis Ababa, the capital of Ethiopia. Currently, Wolaita Sodo serves as the capital city of southern Ethiopia. Known for its high population density, the zone boasts 290 individuals per square kilometer, making it one of the most densely populated regions in the country. According to the 2021 population projection by the Central Statistical Agency of Ethiopia, the Wolaita Zone is home to a total population of 6,142,063 people residing within an area of 4,208.64 square kilometers (1,624.96 sq. mi). Within this zone, there are nine public hospitals, with Wolaita Sodo University Comprehensive Specialized Hospital being the sole specialized healthcare facility. The hospital provides a broad range of surgical services spanning multiple departments, including general surgery, orthopedic surgery, urologic surgery, obstetrics and gynecologic surgery, and maxillofacial surgery. The study was conducted from July 15 to July 30, 2023.
Study design:
Facility-based cross-sectional study was employed because it allows for the exploration of relationships between variables at a specific moment, providing valuable insights into the prevalence of patient satisfaction and associated factors concurrently.
Populations
Source population:.
All surgical patients who have undergone surgery.
The study sample:
All surgical patients that are available during a study period.
Eligibility
Inclusion criteria:.
All adult patients aged ≥ 18 years who have undergone surgery and have been admitted to a surgical, obstetrics/gynecology ward, ophthalmic, orthopedic, or other department were included.
Exclusion criteria:
Patients who sought treatment as outpatients, individuals who were severely ill and unconscious, as well as patients with known mental health issues, were excluded from the study.
Sample size determination and procedure
The sample size was determined using a formula for a single population proportion, taking into account the following assumptions: a prevalence of 52.75% for patient satisfaction with nursing care in Eastern Ethiopia [ 25 ], a confidence level of 95%, a margin of error of 5%, a nonresponse rate of 10% as follows:
n- The minimum sample size required.
P- Prevalence of satisfaction with preoperative nursing care.
d- Margin of error.
Z 𝛼 /2- Standard normal distribution at 95% confidence level
After accounting for a 10% contingency for potential non-response, the final sample size for this study amounted to 468 subjects.
Study variables
Dependent variable:.
Patients’ satisfaction.
Independent variables:
Sociodemographic variables (sex, age, monthly income, residence, marital status, religion, ethnicity, educational, occupational status); Hospital and nurse-related variables (ward/unit, length of hospital stay, surgical specialty, surgery waiting time, patient flow per shift, nurses’ willingness to listen and respond to questions); Patient and family factors (payment status, previous admission, patient service expectations, co-morbidity, surgery type, complications, discharge destination, preoperative fear and anxiety, duration of the illness, family size), and Preoperative education.
Data collection tools and procedures
The data was collected through a meticulously tested, structured, interview-administered questionnaire originally written in English and then translated into the local language, Wolaitigna, to ensure accessibility and accurate comprehension among the participants. The questionnaire was divided into six sections and was obtained from previous studies conducted in Ethiopia and other locations internationally [ 12 , 13 , 31 , 39 ]. The first part of the questionnaire contains the sociodemographic characteristics of the patients. The second part contains institution- or health facility-related variables affecting patients’ preoperative nursing care services. Items in the third and fourth sections assessed the nurse-related factors and patient- and family-related variables influencing patients’ preoperative nursing care services, respectively. One of the patient-related factors was preoperative fear and anxiety and it was measured by tools adapted from previous studies conducted in Ethiopia and Iraq [ 43 , 44 ]. The fifth part of the question contains items used to measure preoperative education containing 16 questions [ 12 ]. The final part contains items to measure the level of preoperative nursing care satisfaction among nurses. The instruments utilized to assess patient satisfaction with preoperative nursing care comprised a set of 22 Likert-scale questions. Each question was rated on a scale from 1, indicating “very unsatisfied,” to 5, indicating “very satisfied”. This tool was valid in Ethiopia and had internal consistency with Cronbach’s alpha of 0.96. The overall patient satisfaction with preoperative nursing care in surgical procedures was classified into two categories: satisfied and unsatisfied [ 12 , 31 , 37 ].. A team of four nursing professionals who held BSc degrees was specifically assigned to take on the role of data collectors. They were closely supervised by two BSc-qualified nurse professionals throughout the study, who were selected from Sodo Health Center.
Data processing and analysis
The collected data were cleaned, coded, and entered using Epidata software and exported into Statistical Package for the Social Sciences (SPSS) Version 26 to facilitate analysis. To explore the relationship between the dependent and independent variables, both bivariable and multivariable logistic regression techniques were utilized. In the bivariable logistic regression model, all independent variables with a p-value less than 0.25 were subsequently entered into the multivariable logistic regression model. The evaluation of significance relied on the adjusted odds ratio (AOR), accompanied by a 95% confidence interval (CI) and a p-value less than 0.05, allowing for meaningful interpretation of the obtained associations. Descriptive statistics, such as tables, graphs, frequencies, and percentages, were employed to provide an overview of the characteristics observed within the sample.
Data quality control
A preliminary assessment, commonly referred to as a pilot study, of the questionnaire, took place at Grace Primary Hospital, which lies outside the scope of the target hospitals. This pre-test was conducted on a subset of the sample size, comprising 5%, a week before the commencement of the actual data collection period. Based on the outcomes of the pre-test, necessary modifications were made to address issues such as unclear questions, typographical errors, and ambiguous wording. Furthermore, the reliability of the Likert-scale items was assessed using Cronbach’s alpha, yielding a coefficient of 0.82. To ensure proficient data collection, a comprehensive one-day training session was provided to the data collectors, encompassing instructions on both the data collection tool and the collection process itself. The principal investigator oversaw the data collection process and monitored its completeness, accuracy, and consistency daily. To enhance data integrity, a double-entry method was employed, involving two separate data clerks who independently entered the collected data into SPSS. The consistency of the entered data was cross-verified by comparing the two versions of the data to identify any discrepancies.
Socio-demographic characteristics of the participants
The response rate for this study was an impressive 100%. Out of the total of 468 respondents, the majority were female (55.1%), and the mean age of the participants was 34 years with a standard deviation of 8.9. Notably, a significant proportion (21.6%) fell within the age bracket of 25 to 34 years. Among the respondents, 210 (44.9%) resided in urban areas, while 258 (55.1%) hailed from rural regions. Regarding marital status, the majority (68.6%) were married, and adherents of the Protestant faith constituted more than 50% of the participants. Approximately 60% of the respondents were illiterate, and 138 (29.5%) identified themselves as farmers. Furthermore, 131 (28.0%) were engaged in the role of housewives, and 107 (22.9%) were students. Out of the total 468 respondents, 223 (47.6%) reported earning less than 1000 ETB per month (Table 1 ).
Patient satisfaction with preoperative nursing care
The overall satisfaction with preoperative nursing care among patients who have undergone surgical procedures at Wolaita Sodo University Comprehensive Specialized Hospital was 79.5% (75.4–83.6) (Fig. 1 ).
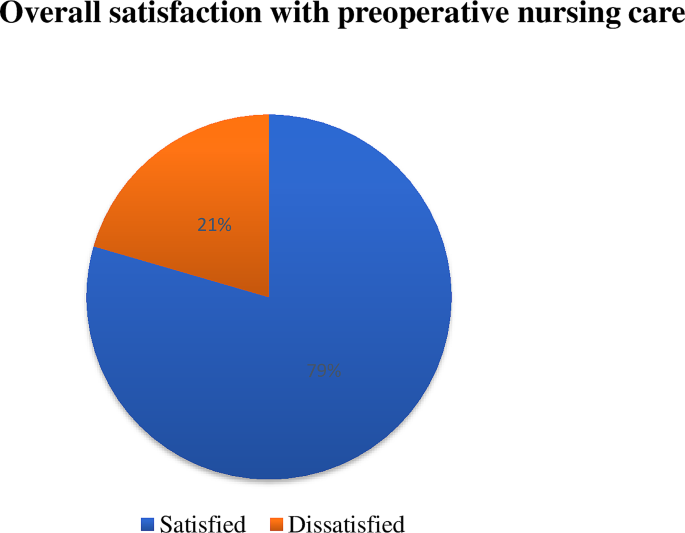
Patient satisfaction with preoperative nursing care in surgical procedures at Wolaita Sodo University Comprehensive Specialized Hospital
Variables influencing patient satisfaction with preoperative nursing care
Hospital and nurse-related variables.
Among the participants, a substantial majority (84.8%) were admitted to the surgical unit of the hospital, highlighting the prevalence of surgical cases in the study sample. In terms of the duration of hospital stay, 289 (61.8%) reported a stay of less than seven days, indicating relatively shorter periods of hospitalization. When it came to interactions with surgeons, the participants disclosed that 151 (32.2%) had contact with surgeons specializing in general surgery, while 129 (27.6%) had contact with surgeons specializing in traumatology. Regarding the waiting time for surgery, more than half of the participants (53.2%) indicated a waiting period of less than one month. Moreover, a majority of the participants (55.3%) acknowledged that there was a high number of patient or a high patient flow during their waiting period, suggesting the burden on the healthcare system. Disturbingly, 277 (59.2%) of the participants reported dissatisfaction with the nurses’ willingness to listen and respond to their concerns, indicating poor communication and responsiveness on the part of the nursing staff (Table 2 ).
Patient and family variables
Among the respondents who participated in this study, a significant proportion (61.3%) revealed that they had fewer than three family members, while 148 (31.6%) reported having four to six family members. More than half of the participants (53.4%) reported receiving free-of-charge treatment from the hospital, indicating a reliance on the hospital’s financial support. Additionally, a considerable number of respondents (63.7%) recalled previous admissions for various health issues. Similarly, 171 (63.5%) of the patients reported having co-morbidities during their initial diagnosis, further complicating their healthcare journey. A substantial proportion of the participants (83.3%) experienced complications related to their current surgery, with pain being the most prevalent complication, affecting 324 (83.1%) of those experiencing complications. The majority of the participants (40.2%) reported that their illness had persisted for several days before undergoing surgery. Abdominal surgery was the most common surgical procedure among the participants, accounting for 119 (25.4%) cases. As for the anticipated discharge destination, 301 (64.3%) participants stated that they would be returning home upon discharge, emphasizing the preference for familiar surroundings. Unsurprisingly, preoperative fear and anxiety were prevalent among the participants, with 373 (79.9%) reporting experiencing high fear and anxiety. Moreover, a significant majority (78.6%) had high service expectations from the hospital, indicating the importance of quality care and support during the preoperative period (Table 3 ).
Patient satisfaction with preoperative education
The overall patient satisfaction with preoperative education on surgical procedures was 79.5% (Fig. 2 ).
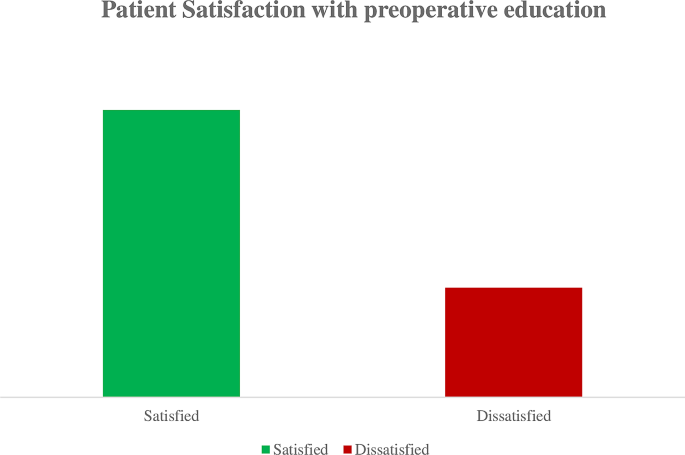
Overall patient satisfaction with preoperative education on surgical procedures at Wolaita Sodo University Comprehensive Specialized Hospital
Factors associated with satisfaction with preoperative nursing care
Sex, age, educational status, monthly income, length of hospital stays, surgery waiting time, nurses’ willingness to listen and respond, payment status for treatment, complications, duration of illness, preoperative fear and anxiety, patient expectations, and preoperative education were all evaluated as potential factors in the bivariable logistic regression analysis (p < 0.25) to determine their association with patient satisfaction with preoperative nursing care. In the multivariable logistic regression, it was found that sex, payment status for treatment, preoperative fear and anxiety, patient expectations, and preoperative education exhibited significant associations with patient satisfaction with preoperative nursing care (p < 0.05). Male patients were found to be 1.14 times more likely to report satisfaction with preoperative nursing care compared to female patients (AOR: 1.14 (95% CI: 0.21–2.91)). Patients who received free treatment were found to be 1.45 times more likely to express satisfaction with preoperative nursing care compared to those who had to pay for their treatment (AOR: 1.45 (95% CI: 0.66–2.97)). Participants who did not experience preoperative fear and anxiety were found to be 1.01 times more likely to report satisfaction with preoperative nursing care compared to those who did have preoperative fear and anxiety (AOR: 1.01, 95% CI: 0.49–2.13). Patients who had low expectations of hospital services were found to be 3.39 times more likely to express satisfaction with preoperative nursing care compared to those who had high service expectations from the hospital (AOR: 3.39, 95% CI: 2.17–7.11). Participants who received preoperative education from nurses were 1.15 times more likely to be satisfied with preoperative nursing care compared to those who did not receive such education from nurses (AOR: 1.148, 95% CI: 0.54–2.86) (Table 4 ).
The primary objective of this study was to determine the level of patient satisfaction with preoperative nursing care at Wolaita Sodo University Comprehensive Specialized Hospital. Furthermore, the study sought to identify factors significantly associated with patient satisfaction with preoperative nursing care. Consequently, the findings of this study demonstrated that the level of patient satisfaction with perioperative nursing care was 79.5%.
This finding was lower when compared with the previous studies conducted at the University of Gondar Teaching Hospital (98.1%) [ 31 ] and Public hospitals in Addis Ababa (84%) [ 12 ]. This disparity can potentially be attributed to various factors, including differences in patient variables such as sociodemographic characteristics, variations in hospital settings, potential inadequacies in the provision of preoperative education and care within the hospitals examined in this study, an increased influx of patients, heightened health-seeking behaviors among individuals, as well as elevated patient expectations regarding the quality of services rendered by the hospitals.
Nevertheless, it is noteworthy that the current finding exhibited a higher level of satisfaction when compared with previous studies conducted at Sohag University (61.9%) [ 41 ], Western Amhara referral hospitals (68.7%) [ 37 ], Gondar University Comprehensive Specialized Hospital (74%) [ 39 ], East Amhara referral hospitals (38.5%) [ 40 ], and Gamo and Gofa zones (36.6%) [ 38 ]. This discrepancy could potentially be attributed to various factors such as differences in the time gaps between the studies, variations in the study participants (for example, the study in East Amhara referral hospitals focused on nurses instead of patients), discrepancies in the services assessed (for instance, the study in the University of Gondar Comprehensive Specialized Hospital solely evaluated satisfaction related to anesthesia services), as well as variances in the perception of the services provided by the patients themselves and the methodologies employed in the studies.
The sex of the patient was significantly associated with patient satisfaction with preoperative nursing care. Male patients were found to be 1.14 times more likely to report satisfaction with preoperative nursing care compared to female patients. This was in line with the study conducted in Barcelona, Spain, [ 13 ] which, strengthens that men patients were more satisfied with preoperative nursing care than women. This finding may be attributed to the fact that women reported experiencing more challenges with hospital care when compared to men. This disparity could potentially arise from the fact that female patients place greater emphasis on their health and often assume the role of evaluators and even administrators of care practices, not just for themselves but also for other family members [ 22 ].
Similarly, payment status for treatment had a significant association with patient satisfaction with preoperative nursing care. Patients who received free treatment were found to be 1.45 times more likely to express satisfaction with preoperative nursing care compared to those who had to pay for their treatment. This could be because patients who receive treatment for free may view it as a gesture of kindness or support, which can enhance their overall experience and level of satisfaction with the preoperative care they receive. Furthermore, patients who do not have to pay for their medical needs may feel less stressed and anxious about the expense, which frees them up to concentrate more on the quality of nursing care they receive. Furthermore, patients who receive free treatment could feel appreciative of the hospital or healthcare system, which could affect how they feel about the care they receive and raise their satisfaction levels.
In this study, patients with preoperative fear and anxiety had also a significant association with satisfaction with preoperative nursing care. Patients who did not experience preoperative fear and anxiety were found to be 1.01 times more likely to report satisfaction with preoperative nursing care compared to those who did have preoperative fear and anxiety. A similar finding was reported in the study conducted in public hospitals in Addis Ababa [ 12 ]. This could be because patients who approach their surgery feeling emotionally stable and at ease may be more receptive to the nursing care they receive. Their ability to maintain composure and relaxation may have a favorable impact on how they view the nursing care they receive, increasing their level of satisfaction. Additionally, patients who do not experience worry or panic before surgery could be better able to express their needs and concerns to the nursing staff. They will be more satisfied as a consequence of this excellent communication, which can improve the standard of care and support they receive. Furthermore, people who are not experiencing preoperative worry or fear may have a more upbeat and hopeful view. This optimistic outlook may lead to a more favorable perception.
Patient expectation of the services was also significantly associated with satisfaction with preoperative nursing care. Participants who had low expectations of hospital services were found to be 3.39 times more likely to express satisfaction with preoperative nursing care compared to those who had high service expectations from the hospital. The possible explanation for this could be that patients who have modest expectations may possess a more pragmatic understanding of the limitations and complexities inherent in the healthcare system. As a consequence, they may display greater gratitude towards the care and attention delivered by the nursing staff, even if it falls short of their initial expectations. Conversely, patients with high service expectations might establish unattainable standards or possess excessively demanding criteria. Consequently, if their expectations are not met, they may experience a sense of disappointment or dissatisfaction with the preoperative nursing care, even if it is of exemplary quality. In contrast, individuals with lower expectations are more likely to find the care they receive to be satisfactory, even if it does not reach the lofty heights of their anticipations.
Likewise, preoperative education was significantly associated with satisfaction with preoperative nursing care. Participants who received preoperative education from nurses were 1.15 times more likely to be satisfied with preoperative nursing care compared to those who did not receive such education from nurses. This finding was similar to the finding of the study conducted at the University of Gondar referral hospital and public hospitals in Addis Ababa [ 12 , 31 ]. The possible reason for this might be that patients who receive preoperative education from nurses are better prepared for surgery by having knowledge and comprehension of the procedures and expectations surrounding their experience. They feel less nervous and uncertain as a result of this instruction, which may improve how they see the nursing care they get. Preoperative education also increases the likelihood that participants will feel powerful and engaged in their care. They can be more engaged in their healing process and may comprehend the significance of specific nursing interventions. A greater sense of participation and teamwork with the nursing staff may be a factor in increased satisfaction [ 12 ].
This study’s results were flavored by Kolcaba’s Comfort Theory, which centers on improving patient satisfaction through attending to their comfort requirements. The study showed that aspects aligning with the theory’s relief component can be improved by meeting particular comfort needs to alleviate pain or discomfort. Additionally, the maintenance of the ease component can be achieved through proactive measures to prevent discomfort to prevent known risk factors that would keep a patient from feeling comfortable, while fulfillment of the transcendence component involves providing patients experiencing physical or emotional discomfort with peace, significance, or opportunities for personal growth through preoperative education and creating a positive nurse-patient relationship through the lens of communication, trust, and empathy in preoperative care.
Implication of the study
In the context of nursing practice, the findings of this study can help nurses in practice by illuminating the variables influencing patients’ satisfaction with preoperative nursing care. Nurses can create tailored methods of care delivery that improve patient experiences and satisfaction by having a greater understanding of the effects of variables including patient gender, treatment costs, preoperative anxiety, and service expectations. Regarding nursing education, the study emphasizes how crucial it is to include preoperative education and communication skills in nursing curricula. It emphasizes how important it is to give nurses the skills and information they need to properly counsel and assist patients before surgery, allaying their anxieties, controlling expectations, and encouraging favorable patient outcomes. The study establishes the foundation for future research endeavors aimed at delving deeper into the topic of patient satisfaction with preoperative nursing treatment. Additional factors that might affect satisfaction, the efficacy of certain interventions or educational initiatives, and the long-term effects of preoperative nursing care on patient outcomes are all potential areas for further research. This information can support evidence-based procedures and guidelines meant to enhance patients’ overall surgical experiences.
Conclusion and recommendation
The study revealed patient satisfaction with preoperative nursing care was high, even though there is room for improvement to ensure optimal healthcare quality. Preoperative care satisfaction is a critical indicator, as even slight deficiencies in this area can have severe consequences, including fatal outcomes. Factors significantly associated with satisfaction in preoperative nursing care were sex, payment status for treatment, preoperative fear and anxiety, patient expectations, and preoperative education.
To address these findings, hospital managers and health policymakers must develop comprehensive strategies aimed at enhancing satisfaction with preoperative nursing care. Initiatives could involve the implementation of tailored training programs for nurses in collaboration with the Ethiopian Federal Ministry of Health, regional health bureaus, and non-governmental organizations. These programs should prioritize equipping nurses with the necessary skills and knowledge to deliver high-quality preoperative care. It is essential to emphasize the need for further research to fully comprehend the specific factors and their impact on patient satisfaction with preoperative nursing care. This research would contribute to a deeper understanding of how nurses can enhance satisfaction levels, ultimately informing the development of evidence-based practices and policies in this crucial healthcare domain.
Strength of the study
To enhance the representativeness and generalizability of our study findings, we employed a substantial sample size and incorporated variables that were overlooked in the previous literature. This approach contributes to a more comprehensive understanding of the factors influencing satisfaction with preoperative nursing care and ensures that our findings encompass a wider range of variables, thereby increasing the validity and applicability of the study results.
Limitations of the study
It is important to acknowledge that the cross-sectional nature of our study design only allows us to establish associations and correlations between the dependent and independent variables, rather than establishing a cause-and-effect relationship. Furthermore, as the quantitative data were collected through a self-administered questionnaire, there is a possibility of response bias from the respondents, which could introduce some limitations to the validity of the data.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
Adjusted Odds Ratio
Confidence Interval
Crude Odds Ratio
Obstetrics and Gynecology
Statistical Package for Social Sciences
Makau PM, Mbithi BW, J.J.A.J.o.H S, Odero. Factors affecting compliance to preoperative patient care guidelines among nurses working in surgical wards of a tertiary referral hospital in Nairobi, Kenya. 2023. 36(2): p. 124–30 https://doi.org/10.4314/ajhs.v36i2.4 .
Turunen E et al. An integrative review of a preoperative nursing care structure. 2017. 26(7–8): p. 915–930 https://doi.org/10.1111/jocn.13448 .
Soydaş Yeşilyurt D, Yildiz Findik Ü. Effect of preoperative video information on anxiety and satisfaction in patients undergoing abdominal surgery. 2019. 37(8): p. 430–6 https://doi.org/10.1097/cin.0000000000000505 https://journals.lww.com/cinjournal/fulltext/2019/08000/effect_of_preoperative_video_information_on.7.aspx .
Mulugeta H et al. Patient satisfaction with nursing care in Ethiopia: a systematic review and meta-analysis. 2019. 18: p. 1–12 https://doi.org/10.1186/s12912-019-0348-9 .
Dos Santos MMB, Martins JCA, L.M.N.J.R.d.E R, Oliveira. Anxiety, depression and stress in the preoperative period of surgical patients. 2014. 4(3): p. 7–15 https://doi.org/10.12707/RIII1393 .
Health F. Continuous Health Care Quality Improvement through Knowledge Management. Federal Democratic Republic of Ethiopia Ministry of Health, 2019: p. 5 https://www.healthynewbornnetwork.org/resource/continuous-health-care-quality-improvement-through-knowledge-management-in-ethiopia/ .
Van der Voorden M, Ahaus K. and A.J.B.o. Franx, explaining the negative effects of patient participation in patient safety: an exploratory qualitative study in an academic tertiary healthcare centre in the Netherlands. 2023. 13(1): p. e063175 https://doi.org/10.1136/bmjopen-2022-063175 .
Gómara AOJEc. The occurrence of adverse events potentially attributable to nursing care in hospital units. 2014. 24(6): p. 356–7 https://doi.org/10.1016/j.enfcli.2014.08.001 .
Heslop L, Lu S. and X.J.J.o.a.n. Xu, nursing-sensitive indicators: a concept analysis. 2014. 70(11): p. 2469–82 https://doi.org/10.1111/jan.12503 .
Almalki ATA et al. Effectiveness of preoperative nursing assessments in reducing Preoperative complications across Saudi Arabia; a Sysetmatic Review based study. 2023. 30(17): p. 973–83 https://doi.org/10.53555/jptcp.v30i17.2667 .
Oner B et al. Nursing-sensitive indicators for nursing care: a systematic review (1997–2017). 2021. 8(3): p. 1005–22 https://doi.org/10.1002/nop2.654 .
Deressa D et al. Satisfaction with preoperative education and surgical services among adults elective surgical patients at selected public hospitals in Addis Ababa, Ethiopia. 2022. 10: p. 20503121221143219 https://doi.org/10.1177/20503121221143219 .
Sillero Sillero A. and A.J.S.o.m. Zabalegui, satisfaction of surgical patients with perioperative nursing care in a Spanish tertiary care hospital. 2018. 6: p. 2050312118818304 https://doi.org/10.1177/2050312118818304 .
Lake ET et al. Missed nursing care is linked to patient satisfaction: a cross-sectional study of US hospitals. 2016. 25(7): p. 535–43 https://doi.org/10.1136/bmjqs-2015-003961 .
Lake ET et al. Higher quality of care and patient safety associated with better NICU work environments. 2016. 31(1): p. 24–32 https://doi.org/10.1097/NCQ.0000000000000146 .
Stimpfel AW et al. Common predictors of nurse-reported quality of care and patient safety. 2019. 44(1): p. 57–66 https://doi.org/10.1097/HMR.0000000000000155 .
Hill B. J.B.J.o.N., do nurse staffing levels affect patient mortality in acute secondary care? 2017. 26(12): p. 698–704 https://doi.org/10.12968/bjon.2017.26.12.698 .
Van Bogaert P, et al. Nurse work engagement impacts job outcome and nurse-assessed quality of care: model testing with nurse practice environment and nurse work characteristics as predictors. 5. 2014;p(1261). https://doi.org/10.3389/fpsyg.2014.01261 .
Arakelian E et al. The meaning of person-centred care in the perioperative nursing context from the patient’s perspective–an integrative review. 2017. 26(17–18): p. 2527–44 https://doi.org/10.1111/jocn.13639 .
Ball JE et al. Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. 2018. 78: p. 10–5 https://doi.org/10.1016/j.ijnurstu.2017.08.004 .
Wune G et al. Nurses to patients communication and barriers perceived by nurses at Tikur Anbessa Specilized Hospital, Addis Ababa, Ethiopia., 2018. 2020. 12: p. 100197 https://doi.org/10.1016/j.ijans.2020.100197 .
Sillero-Sillero A. and A.J.R.l.-a.d.e. Zabalegui, Safety and satisfaction of patients with nurse’s care in the perioperative. 2019. 27 https://doi.org/10.1590/1518-8345.2646.3142 .
Gonçalves MAR, Cerejo MdNR, J.C.A.J.R.d.E R, Martins. The influence of the information provided by nurses on preoperative anxiety. 2017. 4(14): p. 17–25 https://doi.org/10.12707/RIV17023 .
Alvarado LE, Bretones FD, J.A.J.F.i P, Rodríguez. The effort-reward model and its effect on burnout among nurses in Ecuador. 2021. 12: p. 760570 https://doi.org/10.3389/fpsyg.2021.760570 .
Ahmed T et al. Levels of adult patients’ satisfaction with nursing care in selected public hospitals in Ethiopia. 2014. 8(4): p. 371 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4350891/ .
Malley A et al. The role of the nurse and the preoperative assessment in patient transitions. 2015. 102(2): p. 181. e1-181. e9 https://doi.org/10.1016/j.aorn.2015.06.004 .
Liddle CJNS. An overview of the principles of preoperative care. 2018. 33(6) https://doi.org/10.7748/ns.2018.e11170 .
Adugbire BA, Aziato L, F.J.I.J.o.A NS, Dedey. Patients’ experiences of pre and intra operative nursing care in Ghana: A qualitative study. 2017. 6: p. 45–51 https://doi.org/10.1016/j.ijans.2017.04.001 .
Sadia H et al. Assessment of nurses’ knowledge and practices regarding prevention of surgical site infection. 2017. 3(6): p. 585–95 https://doi.org/10.21276/sjmps .
Fetene MB et al. Perioperative patient satisfaction and its predictors following surgery and anesthesia services in North Shewa, Ethiopia. A multicenter prospective cross-sectional study. 2022. 76: p. 103478 https://doi.org/10.1016/j.amsu.2022.103478 .
Gebremedhn EG, G.F.J.P.A.M.J., Lemma. Patient satisfaction with the perioperative surgical services and associated factors at a University Referral and Teaching Hospital, 2014: a cross-sectional study. 2017. 27(1) https://doi.org/10.11604/pamj.2017.27.176.10671 .
Kibru EA et al. Patient satisfaction with post-operative surgical services and associated factors at Addis Ababa City government tertiary hospitals’ surgical ward, cross-sectional study, 2022. 2023. 45 https://doi.org/10.11604/pamj.2023.45.189.38416 .
Trinh LN, Fortier MA, Kain ZNJPM. Primer on adult patient satisfaction in perioperative settings. 2019. 8: p. 1–13 https://doi.org/10.1186/s13741-019-0122-2 .
Astier A et al. What is the role of technology in improving patient safety? A French, German and UK healthcare professional perspective. 2020. 25(6): p. 219–24 https://doi.org/10.1177/2516043520975661 .
Tadesse F, Yohannes Z, J.R.R.J.H L. Knowledge and practice of pain assessment and management and factors associated with nurses’ working at Hawassa University Referral Hospital, Hawassa city, South Ethiopia. 2016. 6(3): p. 24–8.
Criscitelli TJAj. Improving efficiency and patient experiences: the perioperative surgical home model. 2017. 106(3): p. 249–53 https://doi.org/10.1016/j.aorn.2017.07.009 .
Alemu ME, Worku WZ, Berhie AYJH. Patient satisfaction and associated factors towards surgical service among patients undergoing surgery at referral hospitals in western Amhara Regional State, Ethiopia. 2023. 9(3) https://doi.org/10.1016/j.heliyon.2023.e14266 .
Alito GA, Madebo WE, Eromo NC, Quality of Perioperative Informations Provided and it’s Associated Factors Among Adult Patients Who Undergone Surgery in Public Hospitals of Gamo &Gofa Zones: A Mixed Design Study, Ethiopia S. 2019. 2019 https://gssrr.org/index.php/JournalOfBasicAndApplied/article/view/11761 .
Endale Simegn A et al. Patient Satisfaction Survey on Perioperative Anesthesia Service in University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, 2021. 2021. 2021 DOI: https://doi.org/10.1155/2021/3379850 .
Tadesse B et al. Preoperative Patient Education Practices and Predictors Among Nurses Working in East Amhara Comprehensive Specialized Hospitals, Ethiopia, 2022. 2023: p. 237–247 https://doi.org/10.2147/JMDH.S398663 .
Findik UY et al. Patient satisfaction with nursing care and its relationship with patient characteristics. 2019. 12(2): p. 162–9 https://doi.org/10.1111/j.1442-2018.2009.00511.x .
Teng K, Norazliah SJJEH. Surgical patients’ satisfaction of nursing care at the orthopedic wards in hospital universiti sains Malaysia (HUSM). 2012. 3(1): p. 36–43.
Dawood KSJM-LU. Preoperative anxiety and fears among adult Surgical patients in Baghdad Teaching Hospital, Iraq. 2020. 20(1) https://doi.org/10.37506/v20/i1/2020/mlu/194433 .
Dibabu AM et al. Preoperative anxiety and associated factors among women admitted for elective obstetric and gynecologic surgery in public hospitals, Southern Ethiopia: a cross-sectional study. 2023. 23(1): p. 728 https://doi.org/10.1186/s12888-023-05005-2 .
Download references
Acknowledgements
We extend our sincere appreciation and gratitude to Wolaita Sodo University and our supervisors for their invaluable advice and supportive mentorship throughout this study. We would also like to express our thanks to the management and staff of the health institution, as well as the dedicated data collectors who played a crucial role in gathering the necessary data. Moreover, we are deeply grateful to the study participants and all other groups and individuals who contributed their time and effort to make this research possible. Their valuable contributions have been instrumental in the success of this study.
No funding was received.
Author information
Authors and affiliations.
Adult Health Nursing, School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
Bizuayehu Atinafu Ataro, Eshetu Elfios Endirias & Getachew Nigussie Bolado
Maternity and Child Health Nursing, School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
Temesgen Geta
Pediatrics and Child Health Nursing, School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
Christian Kebede Gadabo
You can also search for this author in PubMed Google Scholar
Contributions
BAA wrote a manuscript, conceived data and designed a study, supervised the data collection, performed the analysis, interpreted data, drafted a manuscript, and revised and approved a manuscript for publication. TG, EEE, and GNB assisted in designing the study, were involved in data analysis and interpretation, and critically reviewed the manuscript. All authors reviewed the manuscript.
Corresponding authors
Correspondence to Bizuayehu Atinafu Ataro or Getachew Nigussie Bolado .
Ethics declarations
Ethics approval and consent to participate.
We obtained ethical clearance from the Ethical Review Committee of the Wolaita Sodo University Institutional Review Board (IRB-WSU). Written informed consent was obtained from respondents during data collection after explaining the purpose of the study. Information was also collected anonymously after obtaining written consent from each respondent, ensuring confidentiality by omitting their name and personal identification throughout the data collection period. The study identification number went from 001 to 468. This code was stored in electronic format, encrypted using the encryption software Mac OS X version 10.9.8, and password-protected on the principal investigator’s personal computer. No other identifier was collected, such as a name or the participant’s home address. Participants were also informed that they have the right to refuse, stop, or withdraw at any time during data collection. Finally, participants were informed that there was no incentive or harm to their participation in this study. This declaration was obtained according to the Helsinki form.
We, the undersigned, affirm that this paper is an original piece of work conducted by us and has not been previously presented or published in any Journal. We are fully aware of the importance of academic integrity and understand that plagiarism is strictly prohibited. Any direct quotations or material taken from other sources have been appropriately referenced and credited.
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The authors declare the absence of any other conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ataro, B.A., Geta, T., Endirias, E.E. et al. Patient satisfaction with preoperative nursing care and its associated factors in surgical procedures, 2023: a cross-sectional study. BMC Nurs 23 , 235 (2024). https://doi.org/10.1186/s12912-024-01881-5
Download citation
Received : 10 January 2024
Accepted : 18 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12912-024-01881-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preoperative nursing care
- Patient satisfaction
- Surgical procedure
- Associated factors
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Preoperative Phase
The patient who consents to have surgery , particularly surgery that requires a general anesthetic, renders himself dependent on the knowledge, skill, and integrity of the health care team. In accepting this trust, the healthcare team members have an obligation to make the patient’s welfare their first consideration during the surgical experience.
The scope of activities during the preoperative phase includes the establishment of the patient’s baseline assessment in the clinical setting or at home, carrying out preoperative interview and preparing the patient for the anesthetic to be given and the surgery.
Although the physician is responsible for explaining the surgical procedure to the patient, the patient may ask the nurse questions about the surgery. There may be specific learning needs about the surgery that the patient and support persons should know. A nursing care plan and a teaching plan should be carried out. During this phase, emphasis is placed on:
- Assessing and correcting physiological and psychological problems that may increase surgical risk.
- Giving the patient and significant others complete learning and teaching guidelines regarding the surgery.
- Instructing and demonstrating exercises that will benefit the patient postoperatively.
- Planning for discharge and any projected changes in lifestyle due to the surgery.
Physiologic Assessment
Before any treatment is initiated, a health history is obtained and a physical examination is performed during which vital signs are noted and a data base is establish for future comparisons.
The following are the physiologic assessments necessary during the preoperative phase:
- Obtain a health history and perform a physical examination to establish vital signs and a database for future comparisons.
- Assess patient’s usual level of functioning and typical daily activities to assist in patient’s care and recovery or rehabilitation plans.
- Assess mouth for dental caries, dentures, and partial plates. Decayed teeth or dental prostheses may become dislodged during intubation for anesthetic delivery and occlude the airway.
- Nutritional status and needs – determined by measuring the patient’s height and weight, triceps skinfold, upper arm circumference, serum protein levels and nitrogen balance. Obesity greatly increases the risk and severity of complications associated with surgery.
- Fluid and Electrolyte Imbalance – Dehydration , hypovolemia and electrolyte imbalances should be carefully assessed and documented.
- Drug and alcohol use – the acutely intoxicated person is susceptible to injury .
- Respiratory status – patients with pre-existing pulmonary problems are evaluated by means pulmonary function studies and blood gas analysis to note the extent of respiratory insufficiency. The goal for potential surgical patient us to have an optimum respiratory function. Surgery is usually contraindicated for a patient who has a respiratory infection.
- Cardiovascular status – cardiovascular diseases increases the risk of complications. Depending on the severity of symptoms, surgery may be deferred until medical treatment can be instituted to improve the patient’s condition.
- Hepatic and renal function – surgery is contraindicated in patients with acute nephritis, acute renal insufficiency with oliguria or anuria, or other acute renal problems. Any disorder of the liver on the other hand, can have an effect on how an anesthetic is metabolized.
- Presence of trauma
- Endocrine function – diabetes , corticosteroid intake, amount of insulin administered
- Immunologic function – existence of allergies, previous allergic reactions, sensitivities to certain medications, past adverse reactions to certain drugs, immunosuppression
- Adrenal corticosteroids – not to be discontinued abruptly before the surgery. Once discontinued suddenly, cardiovascular collapse may result for patients who are taking steroids for a long time. A bolus of steroid is then administered IV immediately before and after surgery.
- Diuretics – thiazide diuretics may cause excessive respiratory depression during the anesthesia administration.
- Phenothiazines – these medications may increase the hypotensive action of anesthetics.
- Antidepressants – MAOIs increase the hypotensive effects of anesthetics.
- Tranquilizers – medications such as barbiturates , diazepam and chlordiazepoxide may cause an increase anxiety , tension and even seizures if withdrawn suddenly.
- Insulin – when a diabetic person is undergoing surgery, interaction between anesthetics and insulin must be considered.
- Antibiotics – “Mycin” drugs such as neomycin, kanamycin, and less frequently streptomycin may present problems when combined with curariform muscle relaxant. As a result nerve transmission is interrupted and apnea due to respiratory paralysis develops.
Gerontologic Considerations
- Monitor older patients undergoing surgery for subtle clues that indicate underlying problems since elder patients have less physiologic reserve than younger patients.
- Monitor also elderly patients for dehydration , hypovolemia , and electrolyte imbalances.
Nursing Diagnosis
The following are possible nursing diagnosis during the preoperative phase:
- Anxiety related to the surgical experience (anesthesia, pain ) and the outcome of surgery
- Risk for Ineffective Therapeutic Management Regiment related to deficient knowledge of preoperative procedures and protocols and postoperative expectations
- Fear related to perceived threat of the surgical procedure and separation from support system
- Deficient Knowledge related to the surgical process
Diagnostic Tests
These diagnostic tests may be carried out during the perioperative phase:
- Blood analyses such as complete blood count , sedimentation rate, c-reactive protein, serum protein electrophoresis with immunofixation, calcium , alkaline phosphatase, and chemistry profile
- X-ray studies
- MRI and CT scans (with or without myelography)
- Electrodiagnostic studies
- Endoscopies
- Tissue biopsies
- Stool studies
- Urine studies
Significant physical findings are also noted to further describe the patient’s overall health condition. When the patient has been determined to be an appropriate candidate for surgery, and has elected to proceed with surgical intervention, the pre-operative assessment phase begins.
The purpose of pre-operative evaluation is to reduce the morbidity of surgery, increase quality of intraoperative care, reduce costs associated with surgery, and return the patient to optimal functioning as soon as possible.
Psychological Assessment
Psychological nursing assessment during the preoperative period:
- Fear of the unknown
- Fear of death
- Fear of anesthesia
- Concerns about loss of work, time, job and support from the family
- Concerns on threat of permanent incapacity
- Spiritual beliefs
- Cultural values and beliefs
- Fear of pain
Psychological Nursing Interventions
- Explore the client’s fears, worries and concerns.
- Encourage patient verbalization of feelings.
- Provide information that helps to allay fears and concerns of the patient.
- Give empathetic support.
Informed consent
- Reinforce information provided by surgeon.
- Notify physician if patient needs additional information to make his or her decision.
- Ascertain that the consent form has been signed before administering psychoactive premedication. Informed consent is required for invasive procedures, such as incisional, biopsy , cystoscopy , or paracentesis; procedures requiring sedation and/or anesthesia; nonsurgical procedures that pose more than slight risk to the patient (arteriography); and procedures involving radiation .
- Arrange for a responsible family member or legal guardian to be available to give consent when the patient is a minor or is unconscious or incompetent (an emancipated minor [married or independently earning own living] may sign his or her own surgical consent form).
- Place the signed consent form in a prominent place on the patient’s chart.
An informed consent is necessary to be signed by the patient before the surgery. The following are the purposes of an informed consent:
- Protects the patient against unsanctioned surgery.
- Protects the surgeon and hospital against legal action by a client who claims that an unauthorized procedure was performed.
- To ensure that the client understands the nature of his or her treatment including the possible complications and disfigurement.
- To indicate that the client’s decision was made without force or pressure.
Criteria for a Valid Informed Consent
- Consent voluntarily given. Valid consent must be freely given without coercion.
- For incompetent subjects, those who are NOT autonomous and cannot give or withhold consent, permission is required from a responsible family member who could either be apparent or a legal guardian. Minors (below 18 years of age), unconscious, mentally retarded, psychologically incapacitated fall under the incompetent subjects.
- Procedure explanation and the risks involved
- Description of benefits and alternatives
- An offer to answer questions about the procedure
- Statement that emphasizes that the client may withdraw the consent
- The information in the consent must be written and be delivered in language that a client can comprehend.
- Should be obtained before sedation.
Nursing Interventions
Reducing anxiety and fear.
- Provide psychosocial support.
- Be a good listener, be empathetic, and provide information that helps alleviate concerns.
- During preliminary contacts, give the patient opportunities to ask questions and to become acquainted with those who might be providing care during and after surgery.
- Acknowledge patient concerns or worries about impending surgery by listening and communicating therapeutically.
- Explore any fears with patient, and arrange for the assistance of other health professionals if required.
- Teach patient cognitive strategies that may be useful for relieving tension, overcoming anxiety, and achieving relaxation, including imagery, distraction, or optimistic affirmations.
Managing Nutrition and Fluids
- Provide nutritional support as ordered to correct any nutrient deficiency before surgery to provide enough protein for tissue repair.
- Instruct patient that oral intake of food or water should be withheld 8 to 10 hours before the operation (most common), unless physician allows clear fluids up to 3 to 4 hours before surgery.
- Inform patient that a light meal may be permitted on the preceding evening when surgery is scheduled in the morning, or provide a soft breakfast, if prescribed, when surgery is scheduled to take place after noon and does not involve any part of the GI tract.
- In dehydrated patients, and especially in older patients, encourage fluids by mouth, as ordered, before surgery, and administer fluids intravenously as ordered.
- Monitor the patient with a history of chronic alcoholism for malnutrition and other systemic problems that increase the surgical risk as well as for alcohol withdrawal ( delirium tremens up to 72 hours after alcohol withdrawal).
Promoting Optimal Respiratory and Cardiovascular Status
- Urge patient to stop smoking 2 months before surgery (or at least 24 hours before).
- Teach patient breathing exercises and how to use an incentive spirometer if indicated.
- Assess patient with underlying respiratory disease (eg, asthma , chronic obstructive pulmonary disease [COPD]) carefully for current threats to pulmonary status; assess patient’s use of medications that may affect postoperative recovery.
- In the patient with cardiovascular disease, avoid sudden changes of position, prolonged immobilization, hypotension or hypoxia, and overloading of the circulatory system with fluids or blood.
Supporting Hepatic and Renal Function
- If patient has a disorder of the liver, carefully assess various liver function tests and acid–base status.
- Frequently monitor blood glucose levels of the patient with diabetes before, during, and after surgery.
- Report the use of steroid medications for any purpose by the patient during the preceding year to the anesthesiologist and surgeon.
Monitor patient for signs of adrenal insufficiency.
- Assess patients with uncontrolled thyroid disorders for a history of thyrotoxicosis (with hyperthyroid disorders) or respiratory failure (with hypothyroid disorders).
Promoting Mobility and Active Body Movement
- Explain the rationale for frequent position changes after surgery (to improve circulation, prevent venous stasis, and promote optimal respiratory function) and show patient how to turn from side to side and assume the lateral position without causing pain or disrupting IV lines, drainage tubes, or other apparatus.
- Discuss any special position patient will need to maintain after surgery (eg, adduction or elevation of an extremity) and the importance of maintaining as much mobility as possible despite restrictions.
- Instruct patient in exercises of the extremities, including extension and flexion of the knee and hip joints (similar to bicycle riding while lying on the side); foot rotation (tracing the largest possible circle with the great toe); and range of motion of the elbow and shoulder.
- Use proper body mechanics, and instruct patient to do the same. Maintain patient’s body in proper alignment when patient is placed in any position.
Respecting Spiritual and Cultural Beliefs
- Help patient obtain spiritual help if he or she requests it; respect and support the beliefs of each patient.
- Ask if the patient’s spiritual adviser knows about the impending surgery.
- When assessing pain, remember that some cultural groups are unaccustomed to expressing feelings openly. Individuals from some cultural groups may not make direct eye contact with others; this lack of eye contact is not avoidance or a lack of interest but a sign of respect.
- Listen carefully to patient, especially when obtaining the history. Correct use of communication and interviewing skills can help the nurse acquire invaluable information and insight. Remain unhurried, understanding, and caring.
Providing Preoperative Patient Education
- Teach each patient as an individual, with consideration for any unique concerns or learning needs.
- Begin teaching as soon as possible, starting in the physician’s office and continuing during the pre admission visit, when diagnostic tests are being performed, through arrival in the operating room.
- Space instruction over a period of time to allow patient to assimilate information and ask questions.
- Combine teaching sessions with various preparation proce-dures to allow for an easy flow of information. Include descriptions of the procedures and explanations of the sensations the patient will experience.
- During the preadmission visit, arrange for the patient to meet and ask questions of the perianesthesia nurse, view audiovisuals, and review written materials. Provide a telephone number for patient to call if questions arise closer to the date of surgery.
- Reinforce information about the possible need for a ventilator and the presence of drainage tubes or other types of equipment to help the patient adjust during the postoperative period .
- Inform the patient when family and friends will be able to visit after surgery and that a spiritual advisor will be available if desired.
Teaching the Ambulatory Surgical Patient
- For the same day or ambulatory surgical patient, teach about discharge and follow-up home care. Education can be provided by a videotape, over the telephone, or during a group meeting, night classes, preadmission testing, or the preoperative interview.
- Answer questions and describe what to expect.
- Tell the patient when and where to report, what to bring (insurance card, list of medications and allergies), what to leave at home (jewelry, watch, medications, contact lenses), and what to wear (loose-fitting, comfortable clothes; flat shoes).
- During the last preoperative phone call, remind the patient not to eat or drink as directed; brushing teeth is permitted, but no fluids should be swallowed.
Teaching Deep Breathing and Coughing Exercises
- Teach the patient how to promote optimal lung expansion and consequent blood oxygenation after anesthesia by assuming a sitting position, taking deep and slow breaths (maximal sustained inspiration), and exhaling slowly.
- Demonstrate how patient can splint the incision line to minimize pressure and control pain (if there will be a thoracic or abdominal incision).
- Inform patient that medications are available to relieve pain and that they should be taken regularly for pain relief to enable effective deepbreathing and coughing exercises.
Explaining Pain Management
- Instruct patient to take medications as frequently as prescribed during the initial postoperative period for pain relief .
- Discuss the use of oral analgesic agents with patient before surgery, and assess patient’s interest and willingness to participate in pain relief methods.
- Instruct patient in the use of a pain rating scale to promote postoperative pain management.
Preparing the Bowel for Surgery
- If ordered preoperatively, administer or instruct the patient to take the antibiotic and a cleansing enema or laxative the evening before surgery and repeat it the morning of surgery.
- Have the patient use the toilet or bedside commode rather than the bedpan for evacuation of the enema, unless the patient’s condition presents some contraindication.
Preparing Patient for Surgery
- Instruct patient to use detergent–germicide for several days at home (if the surgery is not an emergency).
- If hair is to be removed, remove it immediately before the operation using electric clippers.
- Dress patient in a hospital gown that is left untied and open in the back.
- Cover patient’s hair completely with a disposable paper cap; if patient has long hair, it may be braided; hairpins are removed.
- Inspect patient’s mouth and remove dentures or plates.
Remove jewelry, including wedding rings
- If patient objects, securely fasten the ring with tape.
- Give all articles of value, including dentures and prosthetic devices, to family members , or if needed label articles clearly with patient’s name and store in a safe place according to agency policy.
- Assist patients (except those with urologic disorders) to void immediately before going to the operating room.
- Administer preanesthetic medication as ordered, and keep the patient in bed with the side rails raised. Observe patient for any untoward reaction to the medications. Keep the immediate surroundings quiet to promote relaxation.
Transporting Patient to Operating Room
- Send the completed chart with patient to operating room; attach surgical consent form and all laboratory reports and nurses’ records, noting any unusual last minute observations that may have a bearing on the anesthesia or surgery at the front of the chart in a prominent place.
- Take the patient to the preoperative holding area, and keep the area quiet, avoiding unpleasant sounds or conversation.
Attending to Special Needs of Older Patients
- Assess the older patient for dehydration , constipation , and malnutrition; report if present.
- Maintain a safe environment for the older patient with sensory limitations such as impaired vision or hearing and reduced tactile sensitivity.
- Initiate protective measures for the older patient with arthritis , which may affect mobility and comfort. Use adequate padding for tender areas. Move patient slowly and protect bony prominences from prolonged pressure. Provide gentle massage to promote circulation.
- Take added precautions when moving an elderly patient because decreased perspiration leads to dry, itchy, fragile skin that is easily abraded.
- Apply a lightweight cotton blanket as a cover when the elderly patient is moved to and from the operating room, because decreased subcutaneous fat makes older people more susceptible to temperature changes.
- Provide the elderly patient with an opportunity to express fears; this enables patient to gain some peace of mind and a sense of being understood
Attending to the Family’s Needs
- Assist the family to the surgical waiting room, where the surgeon may meet the family after surgery.
- Reassure the family they should not judge the seriousness of an operation by the length of time the patient is in the operating room.
- Inform those waiting to see the patient after surgery that the patient may have certain equipment or devices in place (ie, IV lines, indwelling urinary catheter, nasogastric tube , suction bottles, oxygen lines, monitoring equipment, and blood transfusion lines).
- When the patient returns to the room, provide explanations regarding the frequent postoperative observations.
Spiritual Considerations
- Perioperative Nursing
- Intraoperative Phase
- Postoperative Phase
7 thoughts on “Preoperative Phase”
thank you very much Matt Vera, I love that and I love you for what you did and think for student now a days……….I love you very much!!!!!!!!!!!!!
thank you po for all of these 🤗
Thank you Sir Matt for your input. This information will guide me tremendously.
The site has been helpful and has provided all that I needed for learning.
That’s music to my ears! Super happy to hear that the post about the preoperative phase met your needs. If you ever have questions or want more details on other phases or topics, just let me know. Here to support your learning journey! Thank you, Phaustine for your comment.
Amazing, this is very helpful and in depth knowledge. I find this site helpful and as a second avenue to reinstate my knowledge after my professor’s lecture in class. And it is mostly almost the same. So it helps and stick. Thank you a lot. The exams practice questions does help prepare for my actual in person exams! Started nursing school August 2023, and in my first year(second semester). May the Lord bless you for your efforts and time on these. Thank you!!
Thank you so much for your kind words and blessings! It’s incredibly rewarding to hear how Nurseslabs has been a valuable resource for you, especially as you navigate through your first year of nursing school. Exciting times right? Congratulations on starting this journey in August 2023, and it’s great to know you’re already making such positive strides in your second semester.
We’re here to support your learning every step of the way, so if there’s ever a topic you’re curious about or need more practice questions on, don’t hesitate to ask. Your success is what motivates us to keep creating and improving our content.
Best of luck with your studies and exams! May your passion for nursing continue to grow, and may you find every success in your career.
Leave a Comment Cancel reply

Quality and Safety Education for Nurses
Strategy submission, perioperative unfolding case study.
Gerry Altmiller
EdD, APRN, ACNS-BC, ANEF, FAAN
Professor of Nursing
Institution:
The College of New Jersey
Competency Categories:
Informatics, Patient-Centered Care, Quality Improvement, Safety, Teamwork and Collaboration
Learner Level(s):
Continuing Education, New Graduates/Transition to Practice, Pre-Licensure ADN/Diploma, Pre-Licensure BSN, Staff Development
Learner Setting(s):
Classroom, Skills or Simulation Laboratories
Strategy Type:
Case Studies
Learning Objectives:
Strategy Overview:
Submitted Materials:
Perioperative-unfolding-case-4.pptx - https://drive.google.com/open?id=11dYMfwXPejfb9jSTMPKaZ0NMyY3L_j-F&usp=drive_copy
267.2-Student-Worksheet-Perioperative-Unfolding-Case.docx - https://drive.google.com/open?id=1qzAel75FBGLysXeyezkK-wbN6ym5qqps&usp=drive_copy
Additional Materials:
Students can use the student worksheet to record data as the case study unfolds.
Evaluation Description:

Case Studies: Preoperative assessment
Trust/Healthboard/Hospital: University Hospitals Bristol
Thoracic pre-operative assessment
The thoracic multidisciplinary team hold a weekly ‘complex case review meeting’ to plan the most appropriate care for high risk patients. Discussion covers the type of surgery required, the patient’s pre-op review and investigations. Morbidity scoring systems are completed. Together, these guide recommendations for prehabilitation and appropriate post-operative care.
Previd incorporates video assessment where patients are videoed introducing themselves, performing the ‘sit-stand test’ and walking a fixed distance. The sit-stand test is analysed as to the quality of the exercise, the number of repetitions and the motivation the patient shows during the test. They are then timed walking down a 20 m slope and back up. The camera is kept running after completion to see how breathless they are. This video is essential as surgeons pool patients, and therefore may not have met face to face; seeing them on screen adds additional information to numbers and scans.
Skype pre-op assessments for patients referred to our tertiary centre from out of region has improved patient experience by preventing journeys to our centre. Baseline investigations are performed at the patient’s referring hospital but the pre-op consultation with a specialist nurse and anaesthetist is done over Skype.
Trust/Healthboard/Hospital: Newcastle upon Tyne NHS Foundation Trust
The Newcastle upon Tyne NHS Foundation Trust established its pre-assessment service in 2004. Over the years it has grown over 3 sites assessing an average of 30,000 patients per year (inclusive of Saturday working) and recently includes a community-based GP site. We provide a local service to all surgical specialties including: Urology, Hepatobiliary, Vascular, Colorectal, Elective Orthopaedics, Ortho-Oncology, general surgery, breast, plastics, gynaecology, intra-abdominal solid organ transplantation, ENT, Head and Neck, Endoscopy and Interventional Radiology. We also provide regional assessment to transplantation and pancreatic surgery.
We have a team of health care assistants, pre assessment nurses, specialist nurses and cardio pulmonary technicians who provide both booked and a one stop service to patients. 70% of the patients go through this nurse led service. We also offer a telephone helpline run by the senior nursing team to aid patients in stopping medications appropriately before surgery.
In addition, there are a team of dedicated Consultant Perioperative Clinicians. Together, we have developed protocol driven pathways to help investigate and optimise high risk patients. These ensure that the patients are managed in collaboration with the GP minimising referral rates to other specialities to avoid unnecessary delay to patient pathways.

Initiatives
We also run a comprehensive cardiopulmonary exercise testing service for patients undergoing major elective surgery to aid in the risk assessment process. This is run by our cardio-pulmonary technicians in conjunction with the medical team and performed over 2000 tests in 2015. This has led to some of the landmark papers in the risk assessment of patients for surgery. We are currently beneficiaries of an NIHR grant (2.5 yrs) to investigate preoperative alcohol cessation before major orthopaedic surgery and developing community based, hospital derived, habilitative exercise programmes.
We are proud to have reduced our surgical cancellation rate described as ‘unfit for surgery due to inappropriate assessment’ from 9% in 2002 to <0.5% despite a significant rise in patient co morbidity, frailty, patient numbers and the addition of multiple directorates. A recent patient satisfaction (2015) carried out on over 250 patients and compared to one in 2011 showed that 98.3% of patients were very satisfied with their overall care which we had maintained despite huge increases in patient numbers.
Trust/Healthboard/Hospital: NHS Grampian Aberdeen
In collaboration with our geriatric colleagues we have promoted the use of the 4AT for the assessment for cognitive impairment and delirium in our preassessment clinics and surgical wards. We have used the HIS -Health Improvement Scotland learning resources- Think Delirium to educate nursing staff and junior doctors as well as information leaflets to support patients’ families.
We have incorporated the rapid 4 AT in our preassessment record, to screen for cognitive impairment in all patients over 65 years of age. Cognitive impairment is a risk factor for delirium and has implications for the consent process for surgery that may necessitate Power of attorney. A score of 1-3 suggests cognitive impairment and these patients are referred back to primary care for further cognitive assessment. In the postoperative period, we follow up with the 4AT combined assessment tool to screen for delirium in these patients. A score of >4 will initiate the TIME bundle.
Trust/Healthboard/Hospital: Colchester General Hospital
Aims and objectives
We have introduced this ‘walk-round’ clinic to streamline and improve our pre-assessment service. All patients who are booked for surgery in clinic proceed directly to the IPA clinic. The two main objectives of the IPA are:
- To identify low risk patients having minor or intermediate surgery on the day they are booked for surgery (‘green’ patients) who can proceed directly to surgery without returning for further appointments pre-operatively
- To identify patients early who are high risk and may need multidisciplinary input in their preparation for surgery and/or optimisation of pre-existing medical conditions.
All patients planned for elective surgery in a surgical outpatient clinic should receive an IPA form at their clinic appointment, which they complete and present to the IPA clinic. Here the IPA nurse will be able to assess them, measure their BMI and observations, and perform MRSA swabs.The IPA nurse will also arrange investigations as appropriate for their medical comorbidities and the type of surgery they are due to have. These might include blood tests and ECGs. The IPA nurse will perform a Rockwood frailty assessment for all patients over 65 years.
On the basis of this assessment, patients will be triaged into red, amber and green groups. ‘Green’ patients can proceed directly to surgery, ‘amber’ patient require a nurse-led pre-assessment appointment and ‘red’ patients will require a nurse-led pre-assessment with notes or face-to-face review by a Consultant Anaesthetist.
Outcome/Impact
In the first 4.5 months we have built up from one to five days per weeks, with the following results:
- 739 patients through IPA
- Total of 71 clinics in 5 months
- Mean 10.4 patients, median 11 seen per day (max 20, min 2)
- Mean wait for patient 10 mins
- Mean appointment time 13 mins (full nurse pre-assessment time in clinic is 45 mins)
Improvements in quality of care
This has meant an improvement in quality of care through referral for optimisation at the earliest opportunity:
- All ‘red’ patients, 73, were identified as needing a Consultant Anaesthetist review (either notes review or face-to-face)
- 33 patients were identified to be hypertensive and were referred to the GP for management of this
- 43 patients were identified to be anaemic and commenced on the anaemia pathway
- 5 patients identified to have poorly controlled diabetes so referred for optimisation of diabetic control
- 6 patients were identified to have a BMI above our CCG’s threshold of 35 for joint replacement so referred back to their GP
- Some referrals of our most frail and elderly patients were made directly to our high risk pre-assessment clinic run jointly with a Consultant Anaesthetist and a Consultant Physician
Improvements in efficiency
For those green patients who now do not require a face-to-face preassessment clinic appointment just over 30mins clinic time is saved per patient. For many of these an additional trip into hospital for pre-assessment is also avoided.
Barriers and Enablers
Our enthusiastic staff with a new band 6 nurse to lead the IPA service have been fundamental to making this new service work.
Challenges include a lack of space in main outpatients to run such a busy clinic. The geography of our clinics is also a challenge; we currently are not providing this service for oral, ENT or ophthalmology as their clinics are in a different building across a road. Staffing and training new staff to run these clinics is an ongoing challenge as our service expands.
However we are optimistic that the excellent results will encourage support for this service going forward.
Trust/Healthboard/Hospital: Manchester University Hospitals NHS Trust
The Enhanced Surgical medicines optimisation service (ESMOS) was introduced at Manchester University Hospitals Foundation Trust, a large 1200 bedded tertiary hospital within hepatopancreato-biliary (HPB), upper gastro-intestinal (GI), lower GI and vascular specialities. ESMOS is a novel model of care which has shown to improve patient outcomes in those undergoing major surgery by active and dedicated pharmacist involvement throughout the patient’s surgical journey. All pharmacists providing the service are prescribers.
The goals of the service are aligned with the national enhanced recovery programme. The objectives are to identify high risk surgical patients once they are listed for surgery and get them in the best possible state in the pre-operative period by focusing on optimising their pre-existing co-morbidities such as hypertension and diabetes control. The ESMOS service also addresses any pre-operative anaemia. All eligible patients have their anaemia corrected pre-operatively voiding any adverse outcomes related to low haemoglobin levels.
Patients are reviewed virtually in the pre-operative period mainly over the phone. These patients may also be reviewed by face to face contact when they attend the hospital for one of their other appointments e.g. pre-op appointment in a nurse-led clinic or attendance at surgery school. Surgery school is a multidisciplinary initiative set up to provide education to patients on what to expect during their admission for surgery and the steps patients can take to optimise their general fitness prior to surgery.
Once high risk patients are identified, the relevant specialist ESMOS pharmacist contacts the patient by telephone to discuss: a) Current medication the patient is taking and any problems the patient may have such as compliance, adverse effects etc. b) Management of existing medical conditions to be able to identify areas for medicines optimisation c) Peri-operative drug management and provide advice on stopping drugs in this period.
The patient’s medication is also prescribed pre-operatively reducing the incidence of missed doses post-operatively. Following admission, patients are subsequently followed up and monitored closely after their surgery with the focus on medicines optimisation to minimise the incidence of any post-operative complications. Complications such as post-operative pain, nausea and vomiting, electrolyte disturbances etc. are addressed pro-actively at the point of need with patient-centred care with patients involved in discussions around any pharmacological management.
Any challenges experienced and how these have been overcome?
Some of the key challenges experienced include: 1. Identifying patients pre-operatively once they were listed for surgery. This required engaging the admission coordinators and consultant secretaries who had their own workload to deal with 2. Engaging other key stakeholders within the trust to include the anaesthetists, surgeons and specialist nurses. As a result, we set up an electronic referral system to receive referrals from the stakeholders which worked well.
Outcomes and evaluation
A retrospective cohort study was undertaken between September 2017 and September 2018. Adult patients undergoing elective major general surgical procedures were included and stratified into four sub‐specialties, including HPB, upper GI, lower GI and vascular surgery. Patients undergoing emergency and day case procedures or with missing outcome data were excluded from this study. Patients' demographics, baseline co‐morbidities, high‐risk medications, ASA physical status classification, surgical procedure, post‐operative complications, length of stay and nature of pharmacist interventions were collected and reported by descriptive statistics. Length of stay was compared with the corresponding expected length of stay by the national standard. A total of 246 patients were included in the four general sub‐specialties: HPB (n = 82), upper GI (n = 17), lower GI (n = 87) and vascular (n = 60). There was a significant reduction in the median length of stay in three surgical specialties, compared with the national standard: lower GI (median reduction: −2; IQR: −4, 1.8; P = .038), HPB (median reduction: −4.5; IQR: −7, −1; P = .001) and vascular (median reduction: −2; IQR: −4, 0; P = .043). The median actual length of stay was longer than the median expected length of stay in the upper GI specialty (median reduction: 5; IQR: −3, 17; P = .055), although it was not significant. This could be due to the small number of patients in this group.
Trust/Healthboard/Hospital: Sunderland City hospitals NHS Foundation Trust
Type 2 diabetes mellitus is a growing health problem associated with significant adverse impact upon outcomes in the perioperative period. The latest NHS Digital Health Survey reveals that the prevalence of type 2 diabetes has more than doubled since 1994 to approximately 8% of the adult population and expectations are for this trend to continue. Of similar concern is the issue of the increasing number patients living with undiagnosed diabetes and prediabetes who present for scheduled surgery.
There is emerging evidence to support concerns surrounding the increased risk of major perioperative complications associated with stress hyperglycaemia in the perioperative period. Furthermore, patients with untreated chronic hyperglycaemia who subsequently develop hyperglycaemia in the perioperative period are more prone to suffer from cardiac complications than those with treated diabetes. Detection and careful clinical management of patients at risk of stress hyperglycaemia in advance of surgery holds significant theoretical potential to prevent avoidable perioperative complications.
The NCEPOD Highs and Low report (Dec 2018) has highlighted that satisfactory monitoring of established diabetic patients’ blood glucose levels in the perioperative period is an ongoing challenge. The historical lack of evidence of adverse outcomes associated with perioperative hyperglycaemia combined with evidence of harm from intravenous insulin infusions designed to maintain tight blood glucose control in the hospital setting has led to a less interventional approach to perioperative diabetic control.
We wished to determine the proportion of adult patients attending our preoperative clinic who presented a potential increased risk of perioperative stress hyperglycaemia (i.e. patients with known diabetes, undiagnosed diabetes and undiagnosed pre-diabetes respectively). During 2018, 12.5% of our preoperative clinic population presented with known diabetes, which is in keeping with 2018 PQIP report finding of 13%. To identify those with undiagnosed hyperglycaemia, we employed the validated University of Leicester Diabetes Risk Score screening tool in accordance with NICE guidance PH38 (to identify patients deemed at “high risk” of having or developing type 2 diabetes).
A total of 8151 patients were screened between March and December 2018 in our pre-operative clinic. 1198 (12.4 %) were found to be at “high risk” category for diabetes. 1049 of these patients accepted an offer of HBA1c testing. 7% of patients tested had an HbA1c in the diabetic range and 24% of patients had an HbA1c in the pre-diabetic range according to UK reference range. Patients diagnosed with new diabetes (at a rate of approximately 2 per week) are now postponed and stabilised prior to elective surgery. Blood glucose monitoring during the perioperative period is now recommended for all identified pre-diabetic and diabetic patients to identify the development of perioperative stress hyperglycaemia.
In summary, HbA1c testing of the highest risk category of screened patients suggests that approximately 20% of our adult population present to our preoperative clinic with either undiagnosed pre-diabetes or diabetes. Identification of such patients in the preoperative period is warranted to help prevent avoidable perioperative complications and provides an ideal opportunity to improve patients’ long term health prospects in addition to improving short term surgical outcomes.
Trust/Healthboard/Hospital: NHS Greater Glasgow and Clyde
Local audit identified poor accuracy of drug history recording in pre-op assessment, prescribing errors on drug charts and poor communication regarding medicines to take or withhold on the day of surgery. 55% of our patients’ drug history was recorded inaccurately, 30% of drug charts contained prescribing errors. Potential perioperative optimisation issues were identified for 86% of patietns including anticholinergic and polypharmacy review, drug interactions, immunosupresive drugs and more.
It was identified that Pharmacy intervention at the pre-operative assessment phase of the patient journey could help prevent potential prescribing errors and drug interactions and the formation of a perioperative medicines plan for pre, intra and post-op periods could have a positive impact.
COVID enabled the service to explore remote means oh pharmacy review in a cohort of major surgical patients having surgery during May-August 2020. The interventions were patient centred and involved pharmacy reviews delivered remotely through telephone clinics.
47 patients were included in the pilot. 83% of patients required amendment to the medication recording history performed at pre-op assessment thus avoiding drug errors in these patients. A perioperative medicines plan was recorded for all patients in the electronic patient record which included withholding medicines pre-operatively and post-operatively if no longer required. Plans for alternative deliver of drugs in patients who were NBM post-operatively. Individualised medicines optimisation involving patient education and shared decision making was employed in 93% of cases. MDT discussions took place with plans put in place for perioperative infusions of steroids and Octreotide. Communication was improved by alerting the MDT team of potential pharmacy issues. Prescribing safety was improved as well as communication between staff groups. Patient education was improved including counselling about risk of delirium and other side effects. Two patients had their surgery delayed for optimisation following issues uncovered by the Pharmacist (acute thyrotoxicosis and drug toxicity). The Pharmacist also delivered smoking cessation advise and support.
Trust/Healthboard/Hospital: Norfolk and Norwich University NHS FT
A Consultant Anaesthetist (David Nunn) designed the electronic record fpr the preoperative assessment service with a link to the ICE system. This searches for blood results within last 3 months and identifies haemoglobin less than 130 and HBA1C greater than 69mmol/mol. When a patients records are opened in the theatre booking system( ORSOS) the user is alerted to the presence of anaemia or poorly controlled diabetes.
We have prepared standard letter templates to inform other medical staff including the patients GP, of presence of either anaemia or diabetes. These letters state whether surgery can proceed, depending on urgency of procedure and advice GP what steps need to be taken to either investigate and treat anaemia or improve diabetes control.
The alert has enabled early, consistent identification of both anaemia and poorly controlled diabetes; The letter templates enable any member of the pre op team to action the abnormal results quickly and ensure consistent management and clear communication to all involved in patient care.
Trust/Healthboard/Hospital: Barnet Hospital, Royal Free Trust
What was the problem/issue?
High risk obstetric patients requiring anaesthetic pre assessment during pandemic, with the need to offer an alternative from face to face appointments.
How did you know there was a problem?
- Speed of pandemic and need to limit patients coming into hospital unnecessarily to reduce patient risk
- Some patients who would benefit from pre assessment were not recieiving it until in active labour
The number of patients affected? 8-10% on background of 5.5-6,000 deliveries. With approx. 70% women receiving anaesthetic care during their delivery. So a small proportion of women are referred.
What solutions were identified?
- Utilising digital technology (telephone calls and video calls) during pandemic to ensure good, effective and seamless anaesthetic peri-operative assessment of obstetric patients
- Collaborative working amongst health care professionals and patients using different technology applications. Ensuring feedback was gained throughout in order to make positive tweaks and changes to the virtual clinics for a successful outcome
- We have implemented an e-learning which covers how staff should use the platform to connect with patients. As this is new territory for a lot of staff there isn’t training in place for staff on how to get the best out of a video appointment in respect to consultation technique. We have worked closely with the undergrpointments.
- Every medical school in the country is now teaching about remote consulting. It’s also important to bear in mind that we are still in an 'emergency operating mode' of teaching, having had two national lockdowns and both national and local restrictions that have caused huge and rapid changes in the way that medical school teaching is delivered - to enable students to continue to learn under these circumstances - at the same time as considerable upheaval in health service delivery.
- Telemedicine is not new, particularly for some countries, and medical schools across the UK have been collaborating to share ideas and learn from each other over the past eight to nine months.
- New subjects and domains of professional behaviour are added to the curriculum all the time and incorporated into assessments - this isn’t an unusual situation in that regard; evaluation and reflection are part of the course,aduate programme leads to ensure there is a clear process in place for students to join in on video ap
Why were these solutions chosen?
- Digital technology widely utilised amongst anaesthetists and obstetric patient cohort (patient cohort tends to be young, have smart phones and are technology savvy)
- National recommendations to perform virtual clinics and avoid unnecessary patient footfall within hospitals
- Several digital platforms to use that were NHS ‘safe.’
- Prior to pandemic, NHS plan to use technology to develop stronger relationships between care givers and service users, and to develop better-integrated, team-based services and to deliver holistic, whole-person rather than narrowly bio-medical care
- Individual services are responsible for the quality of their consultations/training in the same way they would be for a face to face clinic. There shouldn’t be a distinction between the 2 because they are just as important. In the event that a video or telephone consultation is insufficient staff always have the open to use face to face clinics to complete the consultation.
What were the barriers?
- Change behaviour always takes time to create a uniform and seamless process
- Digital technology and data warehousing in the NHS (success of digital innovation often depends on what might appear to be small details such as how long it takes for health care staff or patients to log on or how hard it is to rectify a small inputting error.)
- Non face-to-face clinics can help reduce unnecessary visits to hospitals, but are still a relatively new model of care. Guidance in the current climate is changing at a rapid pace
- Small percentage of patient cohort will find using the technology difficult
- Work space: finding appropriate rooms to undertake videocalls that met appropriate social distancing requirements
- Key challenges are around equipment and internet connection largely on the Trust side as well as having a place for patients to contact much like you would have in a physical clinic. IT are working extremely hard to upgrade the infrastructure to deal with the rapid shift to remote working. We have implemented a virtual receptionist which greets patients and checks them in . They are also a point of contact should the patient have issues joining.
What were the enablers?
- Enthusiastic and committed staff
- Digital savvy users (Clinicians and patients)
- Able to use translator service during virtual clinic
- Less admin required compared to face to face clinics
- Overall NHS trend to move from face to face clinics to virtual clinics
- Less resources required- fewer rooms required, digital applications can be downloaded on personal mobile phones, clinic can be carried out whilst working from home
- National mandate on virtual clinics to be offered
Which disciplines were involved? Anaesthetics, admin anaesthetic staff, midwives, obstetricians, managers, patients
What evidence (qualitative or quantitative) is there to demonstrate impact (either positive or negative) on:
- morbidity/mortality
- patient record outcomes
- patient experience
- process measures (e.g. reduction in referral times, hospital bed days, readmissions, cancellations etc.
Positives Positive staff feedback and informal patient feedback Reduced wait times by patients Flexibility within system to allow last minute additional appointments to be booked Less inconvenience for patients when attending virtual appointment (no need for travel, childcare, time of work) Records are electronic- minimises risk of some records being on paper and some being recorded electronically.
Negatives Patient DNAs still remain Unable to physically examine patient
Dr Yohinee Rajendran (ST7 Anaesthetic registrar North Central London Deanery) Dr Sonia Brocklesby (Consultant Anaesthetist, Deputy Regional Advisor) Dr Sanjana Singh (Consultant Anaesthetist, Lead for Obstetric Anaesthesia)
Do you have an example of great perioperative care? Please get in touch and submit a Case Study submission so we can share it with the world!
Related Content

Shared Decision Making for Clinicians

- Get Involved
Submit a case study

For Patients
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.23(8); 2018 Dec

Perioperative nursing: maintaining momentum and staying safe
Background: Perioperative practice underpins one of the key activities of many healthcare services, but the work of perioperative nurses is little known. A better understanding of their work is important to enable articulation of their contribution to clinical practice.
Aim: This study observed the practice of perioperative nurses and explored how they described their role.
Methods: Using ethnographic observation and interview, 85 hours’ observation of 11 nurses were undertaken, and 8 nurses were interviewed.
Results: Thematic analysis was undertaken enabling themes to emerge with two being identified. The first, ‘maintaining momentum’, described the need to keep people and equipment moving. The second, ‘accounting for safety’, referred to the need to keep the patient safe during this dangerous period. Tension between these two phenomena was apparent.
Conclusions: Perioperative nurses describe one of their key roles as maintaining the momentum of the patient’s journey through the operating theatre, but having to balance this with the need to ensure the patient’s safety. A core component of the perioperative nurse’s work is thus management of the tension between these two elements. This study illuminated how these nurses understand their practice.
Introduction
Surgery is a crucial component of healthcare, with the World Health Organization (WHO) estimating some 234 million procedures undertaken worldwide each year ( World Health Assembly, 2015 ; WHO, 2017 ).
In the United Kingdom 40,000 staff are employed to undertake over 10 million surgical procedures a year ( NHS Confederation, 2015 ) across more than 3100 operating theatres in England alone ( NHS England, 2016 ). Perioperative nurses form a large part of the workforce; however, their role is not well described and has been the subject of debate ( Mitchell and Flin, 2008 ; Mitchell et al., 2011 ).
Within the perioperative environment, three types of registered nurse with different responsibilities are described ( NHS Careers, 2017 ). These are generally described as anaesthetic, scrub and recovery nurses, identified by the location of their practice. In the UK, anaesthetic nurses support in the delivery of anaesthesia (often in an ante-room adjacent to the operating theatre) and scrub nurses assist in surgical procedures in theatre. Recovery nurses care for patients post surgery prior to transfer out of the theatre ( NHS Careers, 2017 ).
The role of the perioperative nurse has been explored in relatively few studies ( McGarvey et al., 2000 ; Mitchell and Flin, 2008 ) and, in common with nursing more widely, lacks clear definition. Bjorn and Lindberg Bostrom (2008) and Schreiber and MacDonald (2010) discussed nurses' own understanding of their role, while McGarvey et al (2004) suggest that the lack of a clear role definition can hamper attempts to care for patients. Care in the perioperative environment has been linked to continuity ( Lindwall et al., 2003 ) and is based on active cooperation between both the patient and nurse ( Lindwall and Von Post, 2009 ). Perioperative nurses have described the ability to ‘make people better’, often very rapidly, as a significant factor in their choice of career ( Mackintosh, 2007 ).
Other research looked at surgery ‘as theatre’. Using the dramaturgical approach of Goffman (1959) , Riley and Manias (2004) , Tanner and Timmons (2000) and Timmons and Tanner (2004) have suggested that nurses ‘perform’ theatrically by learning lines, responding to whispered cues and carrying on despite disruptions. Dramaturgical analyses also suggest the operating theatre is a ‘backstage area’ ( Tanner and Timmons, 2000 ), closed to the public, where private performances and roles are found. While those working in the setting understand these features of practice, they are not well known to other nurses, healthcare workers or the wider research community.
Allen’s (2014) analysis described perioperative nursing work as ‘invisible’, partially due to its backstage location, but this is reinforced in the literature by the absence of research from nurses’ own perspectives. This study aimed to make the work more visible, enabling nurses to gain insight from their experience and use this to articulate their role.
Methodology
This study used the ethnographic techniques of observation and interview to collect data.
Participants were registered nurses employed in the perioperative department of two NHS acute district hospitals in Southern England. One site contained nine theatres providing surgery across a traditional range of disciplines. The other comprised six main theatres. Both departments employed approximately 40 registered nurses.
Data collection took place between autumn 2011 and spring 2014 in a range of theatres undertaking surgery for diverse specialities and on different days. This enabled a broader overview of nursing activity. Three nurses who were observed were interviewed and the other interviews were undertaken with volunteers who had not been observed. Some weeks before the research was undertaken, the researcher visited the department and introduced themself to the manager and staff to explain the overall purpose of the project.
On observation days, the researcher introduced themself to the team in the area or theatre being observed and approached one theatre nurse to request consent to observe their activity. Nurses who volunteered for observation acted as the principal focus of observation for that session. Their interactions were recorded with other staff members so as to elicit what they did and said in relation to the work they undertook. Potential participants were provided with a Participant Information Sheet (PIS) and given at least 30 minutes to consider taking part. The researcher was available to answer any questions. A study consent form was signed upon agreement.
Verbal permission to observe was obtained from all team members present in the theatre and from the patient where consent could be obtained. A poster was fixed on each door of the theatre informing all entering that observation was taking place.
During observation the researcher stood or sat in the periphery of the area and recorded the participant’s activity in a notebook, timing each entry. Conversation was recorded verbatim for content and features such as emotional inflection (anger, laughter). Other observations included environmental phenomena (light, noise, odour) and movement and interactions of other staff. All participants were anonymised by the application of a code assigned to them. Immediately following the observation, the researcher reflected on the session in a diary allowing a broad contextual description of the observation. Table 1 shows the roles of the 11 nurses observed and the duration of observation.
Observation summary.
Interview participants were recruited during unit meetings prior to being approached. Those who expressed an interest were provided a PIS and given at least an hour to consider participating. A date and time to undertake the interview was arranged with volunteers. Interviews were conducted in a quiet room within the theatre suite. Informed consent was obtained prior to starting. An interview guide was used to ensure the aim of the study was addressed and included prompts to promote discussion ( Table 2 ). Brief notes were taken by the researcher during the interview to support transcription. The interviews were digitally recorded then transcribed. Interviews lasted for an hour on average.
Interview guide questions.
Ethical considerations
The study protocol was approved by a National Research Ethics Committee (reference number: 10/HO501/17) and permission to undertake the study in two acute hospitals was gained from their research offices. Patients within the study were discussed at both sites’ Local Research Ethics Committees and it was agreed that the patients would be informed of the study when they arrived in theatre. The researcher would explain the research to them, its focus on staff in the theatre and guarantee their anonymity. Patients were offered the opportunity to decline participation. Patients lacking mental capacity were excluded from the study and no patients declined participation.
Data analysis
Observations were transcribed into a Microsoft Word document within 3 days of the event. Data were analysed through a recurring process of reading and commenting, followed by sorting into clusters (or nodes) of related data, working within each field note or interview transcript initially and then looking across the data. This process was assisted by the use of computer-assisted qualitative data analysis software, in this case the NVivo 10 program, to store and retrieve coded sections of the data and map the relationships between nodes. These gradually coalesced into the two main themes of the research. Analysis was supported by reviewing the themes and ideas within supervisory meetings at which the development of ideas was tested and defended.
Altogether, 10 observation sessions totalling 85 hours were undertaken. A variety of surgical procedures were observed including elective and emergency, orthopaedic, vascular and urological procedures. Five female and three male participants with a range of experience were interviewed.
Two key themes were identified. The first, ‘managing momentum’, related to time, work directed to flow and delays, and the allocation of time, which were key factors in each of the nursing roles. The second theme, ‘maintaining safety’, primarily described the large numbers of activities undertaken ‘to prevent harm’. The contributing data clusters that underpin these themes are shown in Table 3 .

Perioperative nursing requires a balance between maintaining momentum and accounting for safety. Surgery that moves patients too rapidly will become unsafe, while surgery that focuses excessively on safety will reduce momentum. The perioperative nurses’ work must therefore balance these contrasting needs.
Factors affecting theatre momentum.
Thematic overview.
Theme 1: Managing momentum
Many activities observed or described by the participants related to ensuring that the patient journey through the department progressed quickly. Five data clusters fed into this theme. The following excerpts are a combination of observation, interview and transcribed staff dialogue.
Anticipation: Planning and predicting
The work relating to this cluster was described as anticipating the needs of personnel, equipment or situations that occurred in either the present or future. This anticipatory work comprised actions that would ensure efficient progression of patients through the day. A key example was deciding at what juncture to send for the next patient:
Staff nurses 15 and 16 and the HCA [health care assistant] are tidying things and putting rubbish into bags. Staff nurse 9 is watching, sat on a stool by the scrub room. She asks ‘Shall we send for the next patient?’ to which the HCA replies ‘I wouldn’t yet’. (Observation session 5)
This excerpt shows staff nurse 9 planning ahead with no obvious cues for this prompt and it was not apparently motivated by any observable action. Interestingly, a junior staff member offers an opinion that is accepted by the team, suggesting that this is an activity common to all staff in theatre. However, planning was an activity that in itself was stressful, as one scrub nurse observed:
You can plan so much, but you can’t assume that everything’s going to go wrong. You’d just be, it will just be a massive stress, and actually, at work I know people that are a bit like, what if that [a piece of equipment] goes, what if that goes, then, you’re like, whoa, we’ll deal with it. (Interview 2, scrub nurse)
Anticipatory work was undertaken at all levels of activity, from the management of an individual patient’s journey to managing future operating lists, in some cases as far as 10 days away:
Charge nurse 21 now phones the x-ray department to book two radiographers for a large orthopaedic list next Tuesday. While doing this he adds ‘On Thursday again, I’ve got X [surgeon’s name]. Any chance of an early start there please?’ He is now juggling lists, moving cases to avoid clashes in the need for radiographers. He is successful and very adroit at doing this and achieves the cover he needs. (Observation session 9)
Here the nurse plans ahead for the next week of surgery on two different days and lists, using his considerable knowledge to best allocate the radiographers to avoid clashes. Interestingly, charge nurse 21 was in charge of the department that day, coordinating the activities of the whole department as well as undertaking this work – maintaining the whole department’s momentum. This individual was required, in the words of one co-ordinator, to maintain a ‘high-level overview about what is going on across the theatre complex’.
Managing intrinsic and extrinsic factors
The nurses’ work was influenced by factors that were intrinsic and extrinsic to theatres (See Table 4). However, the actual work undertaken appeared to focus on the intrinsic factors, as the majority of extrinsic factors were beyond their influence.
The need to allocate time for patients requiring emergency surgery was particularly challenging as these patients ‘jumped’ others on the emergency theatre list. On one occasion, a patient with a life-threatening condition was already booked, but the co-ordinator was obliged to add the new emergency patient immediately as the next case on the list. They then had to inform other surgeons who had pending operations of this delay. This process took some significant time to organise.
Managing time/flow
The nurses had a very keen sense of time and used this to make predictions about how the day was likely to progress:
I am having a discussion with Staff Nurse 17 in which he tells me ‘They’re slow getting started today. You know what that means!’ referring to the fact that the Recovery Unit will inevitably get busy once the first cases begin finishing and entering Recovery. (Observation session 6)
An anaesthetic nurse observed that the need to maintain safety could also be used to plan effectively. In relation to a surgical safety checklist undertaken prior to operating, she noted:
There are no surprises. Any potential problems are identified and obviously, it’s allowing things to run a bit smoother, because we’ve already identified any problems, and that’s calculated into how things are going to run. (Interview 1, anaesthetic nurse)
Managing emotions
The perioperative nurses’ work also involved managing emotions. Sending for another patient was seen to put pressure on the activities being undertaken in the theatre, particularly when the current patient is still on the operating table:
Staff nurse 9 enters the theatre. She asks ‘Have we sent yet?’ Staff nurse 10 says that they haven’t yet. The consultant anaesthetist says ‘Well, we can send now and [registrar anaesthetist] can put the lines in’. Staff nurse 10 refuses this saying ‘We still need to clean the table, mop the floor and the [current] patient’s still asleep. Just give us another five minutes’. Her tone has a degree of finality to it. She is resisting pressure to speed up the list it seems: (Observation session 3)
A scrub nurse described the tension that arises, particularly first thing in the morning when a lot of the work generating momentum is undertaken:
I think first thing in the morning it’s … everyone’s running around going ‘waaah!’ Everything, got everything, got everything, got everything. Have we sent for a patient, have we seen the surgeon, have we seen the anaesthetist? And then you get, like, everyone takes a deep breath and goes [calming sigh] and ‘we’re done’. (Interview 2, scrub nurse)
In the recovery unit, a failure to discharge back to the wards led to the recovery beds being filled, prompting the nurse in charge to close the unit and delay the next operation, as the previous patient would still be in theatre. This failure would lead to a cascade backwards through the entire theatre, with existing patients unable to enter recovery and new patients unable to enter theatre.
Failing to manage momentum
If momentum failed, possible consequences included:
- surgeries being cancelled (negative for patient);
- overrunning lists finishing late (negative for staff);
- Clinical Commissioning Groups scrutinising cancellations and poor press coverage (negative for organisation).
For the nurses, the consequences of momentum failure often manifested as an empathic response:
Because if we have a, just a short delay, then, you know, it will just have a big impact on the other patients … And the worst one affected is the last patient, and they will get cancelled. … it’s my consideration. I always think that what if this is my, this is my relative or something? (Interview 8, theatre co-ordinator)
Theme 2: Maintaining safety
The second theme to emerge concerned ‘maintaining safety’; ensuring the safety of patients was described as paramount and featured in all observations of practice.
In the interviews all participants acknowledged that the patient was reliant on the theatre staff for their safety and that it was a priority in all aspects of their work, regardless of area of practice. This is illustrated by the quotes by various nurses:
ensuring that the patient is safe, and being there for the anaesthetist, and knowing all the equipment , and where I could put my hands on it quickly (Interview 1, anaesthetic nurse; emphasis added). Yeah, my main priorities are my patients’ safety at all times (Interview 5, recovery nurse; emphasis added). Being their advocate whilst they’re in theatre. So they come in and you make sure that as much as possible their dignity is kept, that they’re kept as safe as possible (Interview 2, scrub nurse; [emphasis added]).
Two main data clusters contributed to this theme (see Table 3 ).
Safe teamworking
The theatre team is composed of various people with different roles. However, there were tensions noted in the need for safety checks to be undertaken. For scrub nurses particularly, the notion of ‘the count’ was a central piece of practice, referring to the need to literally count all of the instruments, swabs and needles in and out of the surgical field to prevent items being left in the patient. This activity took a lot of time for scrub nurses and was concurrent with the WHO Surgical Safety Checklist. There was occasional difficulty with getting all of the team to comply with doing this, and the scrub nurse often had to raise the issue:
Scrub nurse calls out ‘Can we check the patient please guys – I’m sorry’. The surgeons are painting the patient (applying iodine antiseptic) at this point and the WHO checks have not yet been undertaken. Raising her voice the scrub nurse says, ‘Wait, we haven’t checked the patient, sorry!’ The team stops and verifies the patient’s details. (Observation session 1)
Here the emotional work of the scrub nurse in the context of safety is illustrated in that she is required to exert herself by raising her voice to obtain compliance with a mandatory piece of safe teamworking.
Managing the environment
The actual environment of the theatre can be unpleasant for patients, particularly the temperature, as the airflows through theatre produce a cold draught. Unconscious patients must be protected from this cooling effect, a phenomenon that all the nurses commented upon:
Of course the other is the … again, is the wellbeing of the patient and making sure the patient is comfortable, warm, protected, safe, do what we’re doing to the right person, again. (Interview 4, anaesthetic nurse)
Here, the nurse makes the link between the patient’s wellbeing and being safe, referring to comfort and warmth in terms of safety.
The nurses themselves recognised that there was a balance to be struck in the approach to their work:
And my main priority is just to make sure they’re safe … so we do have to try and look at getting patients through relatively quickly, but again still maintaining that safety margin. (Interview 3, recovery nurse)
Having examined the themes that have emerged, it is now necessary to consider their implications in practice.
A core finding of the research relates to ‘maintaining momentum’. Momentum in this context is defined as ‘The impetus and driving force gained by the development of a process or course of events’ ( Oxford English Dictionary, 2014 ). Much of the work that the nurses undertook was related to the need ‘to keep things moving’, encompassing present work and, crucially, anticipatory work. This emerged, whether for an individual patient, an operating list or indeed the wider theatre department as a whole. Anticipatory work comprises two elements, mental and physical, as well as a future (temporal) component. This correlates with Allen’s (2014) work on patient flow, suggesting that the nursing work being undertaken here is similar to that of bed managers, ensuring patient flow throughout the hospital.
The sense of urgency surrounding maintaining momentum impacts emotionally on nurses. The concept of emotional labour in theatre is not new ( Timmons and Tanner, 2005 ). When lists ran well and punctually, this produced positive talk and smooth ‘processing’ of cases. This was interesting because although there is a large body of research on theatre utilisation ( Cole and Hislop, 1998 ; Faiz et al., 2008 ; O’Donnell, 1976 ) and process analyses, the data presented here reveal the practical and emotional work required by the nurses in order to manage schedules.
Anticipatory work varied in different perioperative areas. The anaesthetic nurses were seen to prepare drugs and equipment for the anaesthetists in advance, reducing the time necessary for the induction of anaesthesia. The scrub nurses appeared to utilise the operating lists to review current and future equipment needs for the day, which enabled them to prepare appropriate equipment in advance of surgery. The recovery nurses focused on transferring the patients out of the department. For anaesthetic and scrub nurses, the drive was to process patients into and out of the theatre, then into recovery for return to the ward. The recovery nurses experienced maintaining momentum as the need to discharge patients as rapidly as possible. The anaesthetic and scrub nurses interacted in a parallel manner within the operating theatre itself with the recovery nurses acting more autonomously. This was due to the physical layout of the theatre complex and its segregation into the operating and recovery areas. The nurse in charge kept broader oversight and liaised more with the recovery area to prevent delays.
The physical work was related to surgical instrument trays, patient positioning and the use of bulky equipment like camera screens and x-ray machines. In order to undertake these activities successfully, nurses were required to have considerable insight and expertise, products of their familiarity with their work.
Factors influencing the work of the nurse in maintaining momentum were both extrinsic and intrinsic. Pope (2002) suggested ‘externally contingent’ factors (i.e. not patient- or surgeon-specific) such as equipment, assistants and other resources that may impact upon the performance of surgery. The observations particularly demonstrated the considerable amount of work that each nurse undertook in managing intrinsic factors.
The work of maintaining momentum is largely invisible as it is undertaken by nurses independently from (or occasionally because of) factors related to anaesthetic or surgical issues. The need to constantly anticipate, act and ensure that contingencies are accounted for is central to this phenomenon. During the study, nurses were seen balancing these issues both in and out of the theatre, often in response to extrinsic factors that they had little or no control over but had to respond to.
Allen (2014) describes patient flows throughout the hospital as being little understood but primarily managed by nurses. Maintaining momentum is a way of conceptualising the perioperative nursing role as it is little known and hidden. Perioperative nursing can be understood to be a continual balance between the two imperatives of maintaining momentum and safety. Becoming a skilled practitioner requires the knowledge and ability to achieve this balance and then ensure it is maintained for each individual patient and the entirety of the operating list. For various nurses in theatre, the factors affecting the balance differ but the requirement to reconcile them remains the same, with negative outcomes being very real. More positively, the satisfaction of achieving this balance is a very tangible reward for theatre nurses. Successfully balancing or managing these two imperatives constitutes ‘care’ in this strange clinical environment.
Study limitations
The main limitations of the study were its relatively small scale and it being undertaken by a lone researcher (who is also a perioperative nurse). The potential for researcher bias was managed within the supervisory relationship, with the author being required to explain and defend the analysis to impartial scrutiny. The potential for the participants to alter their behaviour as a result of being observed (the Hawthorne Effect, Landsberger, 1958) was a possibility. The fact that the author was a perioperative nurse looking at practice, and not therefore involved in any managerial assessment, hopefully led to natural behaviours being observed.
Momentum in theatre nursing work provides a way of understanding the role. It must happen alongside the imperative to maintain the patient’s safety, requiring that a balance be struck between the two. Perioperative nurses experience tension in maintaining this balance. This understanding addresses a gap in the research about what theatre nurses do, and their views about what they do. As surgery is a core activity in all healthcare systems, this knowledge about the invisible work of perioperative nurses will be useful to practitioners and researchers alike.
Key points for policy, practice and/or research
- Perioperative nurses are required to maintain momentum and simultaneously account for safety.
- Maintaining momentum requires constant efforts to ensure that patients move through the perioperative journey.
- The imperative to maintain momentum is often in conflict with the need to account for safety, and this tension has to be resolved.
- The findings will inform future research investigating the contribution of the perioperative nurse to safe and efficient perioperative practice.
Acknowledgements
The authors wish to thank all the participants involved in this study.
Jon R McGarry , RN, BSc (Hons), DClinP, is a charge nurse in a UK theatre department. His interests include nursing research and the promotion of nursing scholarship in practice. His background is in emergency department and anaesthetic nursing. This paper arose from his doctoral thesis.
Catherine Pope , BA (Hons), PhD, is Professor of Medical Sociology in the Faculty of Health Sciences at the University of Southampton in the UK, where she leads the Emergency and Urgent Care (EmU) research group. Catherine has played a leading role in developing qualitative methods and evidence synthesis in health services research and is co-author of significant books and journal papers on these methods.
Sue M Green , RN, BSc, PhD, is an Associate Professor in the Faculty of Health Sciences at the University of Southampton in the UK. Sue is a registered nurse and nutritionist with a background in acute and continuing care nursing, learning and teaching in higher education, and nutrition research. Sue’s research and teaching focuses on nutritional care by nurses.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
The study protocol was approved by a National Research Ethics Committee (reference number: 10/HO501/17) and permission to undertake the study in two acute hospitals was gained from their research offices.
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: The Wessex Deanery Clinical Academic Career group provided funding to support the research. Their generosity is gratefully acknowledged.
- Allen D. (2014) The Invisible Work of Nurses: Hospitals, Organisation and Healthcare , London: Routledge. [ Google Scholar ]
- Bjorn C, Lindberg Bostrom E. (2008) Theatre nurses’ understanding of their work: A phenomenographic study at a hospital theatre . Journal of Advanced Perioperative Care 3 ( 4 ): 149–155. [ Google Scholar ]
- Cole BO, Hislop WS. (1998) A grading system in day surgery: Effective utilization of theatre time . Journal of the Royal College of Surgeons of Edinburgh 43 ( 2 ): 87–88. [ PubMed ] [ Google Scholar ]
- Faiz O, Tekkis P, McGuire A, et al.(2008) Is theatre utilization a valid performance indicator for NHS operating theatres? BMC Health Services Research 8 ( 28 ) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Goffman E. (1959) The Presentation of Self in Everyday Life , London: The Penguin Press Ltd. [ Google Scholar ]
- Landsberger HA (1958). Hawthorne Revisited . New York, Ithaca.
- Lindwall L, von Post I. (2009) Continuity created by nurses in the perioperative dialogue: A literature review . Scandinavian Journal of Caring Science 23 ( 2 ): 395–401. [ PubMed ] [ Google Scholar ]
- Lindwall L, von Post I, Bergbom I. (2003) Patients’ and nurses’ experiences of perioperative dialogues . Journal of Advanced Nursing 43 ( 3 ): 246–253. [ PubMed ] [ Google Scholar ]
- McGarvey HE, Chambers MGA, Boore JRP. (2000) Development and definition of the role of the operating department nurse . Journal of Advanced Nursing 32 ( 5 ): 1092–1100. [ PubMed ] [ Google Scholar ]
- McGarvey HE, Chambers MGA, Boore JRP. (2004) The influence of context on role: Behaviors of perioperative nurses . AORN Journal 80 ( 6 ): 1103–1120. [ PubMed ] [ Google Scholar ]
- Mackintosh C. (2007) Making patients better: A qualitative descriptive study of registered nurses’ reasons for working in surgical areas . Journal of Clinical Nursing 16 ( 6 ): 1134–1140. [ PubMed ] [ Google Scholar ]
- Mitchell L, Flin R. (2008) Non-technical skills of the operating theatre scrub nurse . Journal of Advanced Nursing 63 ( 1 ): 15–24. [ PubMed ] [ Google Scholar ]
- Mitchell L, Flin R, Yule S, et al.(2011) Thinking ahead of the surgeon: An interview study to identify scrub nurses’ non-technical skills . International Journal of Nursing Studies 48 ( 7 ): 818–828. [ PubMed ] [ Google Scholar ]
- NHS Careers (2017) Theatre nursing. Available at: www.nhscareers.nhs.uk/explore-by-career/nursing/careers-in-nursing/theatre-nursing/ (accessed 17 October 2017).
- NHS Confederation (2015) Key statistics on the NHS. Available at: www.nhsconfed.org/resources/key-statistics-on-the-nhs (accessed July 25 2017).
- NHS England (2016) Supporting facilities data. Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/cancelled-elective-operations/supporting-facilities-data/ (accessed January 25 2017).
- O’Donnell DJ. (1976) Theatre utilization analysis . Medical Journal of Australia 2 ( 17 ): 650–651. [ PubMed ] [ Google Scholar ]
- Oxford English Dictionary (2014) http://www.oxforddictionaries.com/definition/english/momentum?q=momentum (accessed 18 June 2014).
- Pope C. (2002) Contingency in everyday surgical work . Sociology of Health & Illness 24 ( 4 ): 369–384. [ Google Scholar ]
- Riley R, Manias E. (2004) Rethinking theatre in modern operating rooms . Nursing Inquiry 12 ( 1 ): 2–9. [ PubMed ] [ Google Scholar ]
- Schreiber R, MacDonald M. (2010) Keeping vigil over the patient: A grounded theory of nurse anaesthesia . Journal of Advanced Nursing 66 ( 3 ): 552–561. [ PubMed ] [ Google Scholar ]
- Tanner J, Timmons S. (2000) Backstage in the theatre . Journal of Advanced Nursing 32 ( 4 ): 975–980. [ PubMed ] [ Google Scholar ]
- Timmons S, Tanner J. (2004) A disputed occupational boundary: Operating theatre nurses and operating department practitioners . Sociology of Health & Illness 26 ( 5 ): 645–666. [ PubMed ] [ Google Scholar ]
- Timmons S, Tanner J. (2005) Operating theatre nurses: Emotional labour and the hostess role . International Journal of Nursing Practice 11 ( 2 ): 85–91. [ PubMed ] [ Google Scholar ]
- World Health Assembly (2015) Strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage, Sixty-eighth World Health Assembly, 26 May 2015. Available at: http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R15-en.pdf?ua=1 (accessed 25 July 2017).
- World Health Organization (2017) Emergency and essential surgical care programme. Available at: http://www.who.int/surgery/emergency-essential-surgical-care-2013flyer.pdf?ua=1 (accessed 25 July 2017).
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Abbott TEF, Fowler AJ, Dobbs TD Frequency of surgical treatment and related hospital procedures in the UK: a national ecological study using hospital episode statistics. British Journal of Anaesthesia.. 2017; 119:(2)249-257 https://doi.org/10.1093/bja/aex137
American Society of Anesthesiologists. ASA physical status classification system. 2019. https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system (accessed 26 August 2020)
Anderson OA, Wearne IM. Informed consent for elective surgery--what is best practice?. J R Soc Med.. 2007; 100:(2)97-100
Association of Anaesthetists of Great Britain and Ireland. Pre-operative assessment and patient preparation: the role of the anaesthetist. AAGBI safety guideline 2. 2010. https://tinyurl.com/yxr2a3o3 (accessed 17 August 2020)
Association of Anaesthetists of Great Britain and Ireland. Checklist for anaesthetic equipment. 2012. https://tinyurl.com/yxhhef7a (accessed 17 August 2020)
Day case and short stay surgery: 2. Anaesthesia.. 2011; 66:(5)417-434 https://doi.org/10.1111/j.1365-2044.2011.06651.x
Cousley A. Documentation of phases of care. In: Cousley A, Martin D (eds). Keswick: M&K Update Ltd; 2016a
Cousley A. The Cousley model. In: Cousley A, Martin D (eds). Keswick: M&K Update Ltd; 2016b
Dejong CHC, Earnshaw JJ. Surgical innovation. Br J Surg.. 2015; 102:(2)e8-e9 https://doi.org/10.1002/bjs.9727
Dunn D. Body art and the perioperative process. AORN J.. 2016; 104:(4)326-340.e4 https://doi.org/10.1016/j.aorn.2016.07.011
Fisher M, Scott M. Patient safety and managing risk in nursing.London: SAGE; 2013
Gray CE, Baruah-Young J, Payne C. Preoperative assessment in patients presenting for elective surgery. Anaesth Intensive Care Med.. 2018; 19:(9)447-452 https://doi.org/10.1016/j.mpaic.2018.06.006
Liddle C. Postoperative care 1: principles of monitoring postoperative patients. Nurs Times. 2013a; 109:(22)22-26
Liddle C. How to reduce the risk of deterioration after surgery. Nurs Times. 2013b; 109:(23)16-17
Martin D. Peri-anaesthesia management of patient care framework. In: Cousley A, Martin D (eds). Keswick: M&K Update Ltd; 2016
National Institute for Health and Care Excellence. Pressure ulcers: prevention and management. Clinical guideline CG179. 2014. https://www.nice.org.uk/guidance/cg179 (accessed 18 August 2020)
National Institute for Health and Care Excellence. Routine preoperative tests for elective surgery. NG45. 2016a. https://www.nice.org.uk/guidance/ng45 (accessed 18 August 2020)
National Institute for Health and Care Excellence. Hypothermia: prevention and management in adults having surgery. CG65. 2016b. https://www.nice.org.uk/guidance/cg65 (accessed 18 August 2020)
National Institute for Health and Care Excellence. Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. NG89. 2019. https://www.nice.org.uk/guidance/ng89 (accessed 18 August 2020)
National Institute for Health and Care Excellence. Surgical site infections: prevention and treatment. NG125. 2020. https://www.nice.org.uk/guidance/ng125 (accessed 26 August 2020)
NHS website. Consent to treatment. 2019. https://www.nhs.uk/conditions/consent-to-treatment (accessed 18 August 2020)
Primiano M, Friend M, McClure C Pressure ulcer prevalence and risk factors during prolonged surgical procedures. AORN J.. 2011; 94:(6)555-566 https://doi.org/10.1016/j.aorn.2011.03.014
Powell R, Scott NW, Manyande A Psychological preparation and postoperative outcomes for adults undergoing surgery under general anaesthesia. Cochrane Database Syst Rev. 2016; https://doi.org/10.1002/14651858.CD008646.pub2
Royal College of Anaesthetists. Chapter 2: Guidelines for the provision of anaesthesia services for preoperative assessment and preparation 2019. (Part of the Guidelines for the provision of anaesthetic services). 2019. https://www.rcoa.ac.uk/gpas/chapter-2 (accessed 18 August 2020)
Royal College of General Practitioners. Quality patient referrals: right service, right time. 2018. https://tinyurl.com/y6b8h9vu (accessed 18 August 2020)
Royal College of Surgeons of England. Commissioning guide: groin hernia. 2013. https://tinyurl.com/y2jhq2ug
Royal College of Surgeons of England. Outpatient clinics: a guide to good practice. 2018. https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/outpatient-clinics/ (accessed 18 August 2020)
Royal College of Surgeons of England. Surgery and the NHS in numbers. 2020. https://tinyurl.com/y262ymx4 (accessed 26 August 2020)
Simpson JC, Moonesinghe SR. Introduction to the postanaesthetic care unit. Perioper Med (Lond).. 2013; 2:(1) https://doi.org/10.1186/2047-0525-2-5
Sundqvist AS, Holmefur M, Nilsson U, Anderzén-Carlsson A. Perioperative patient advocacy: an integrative review. J Perianesth Nurs.. 2016; 31:(5)422-433 https://doi.org/10.1016/j.jopan.2014.12.001
Tang R, Ranmuthugala G, Cunningham F. Surgical safety checklists: a review. ANZ J Surg.. 2014; 84:(3)148-154 https://doi.org/10.1111/ans.12168
Walker IA, Reshamwalla S, Wilson IH. Surgical safety checklists: do they improve outcomes?. Br J Anaesth.. 2012; 109:(1)47-54 https://doi.org/10.1093/bja/aes175
Wicker P. Perioperative practice at a glance, 1st edn. Chichester: Wiley Blackwell; 2015
Wicker P, O'Neill J. Caring for the perioperative patient, 2nd edn. Chichester: Wiley Blackwell; 2010
World Health Organization. WHO guidelines for safe surgery 2009: safe surgery saves lives. 2009a. https://tinyurl.com/t42lk2w (accessed 18 August 2020)
World Health Organization. Implementation manual WHO surgical safety checklist. 2009b. https://www.who.int/patientsafety/safesurgery/checklist_implementation/en/ (accessed 18 August 2020)
World Health Organization. Global guidelines on the prevention of surgical site infection. 2016. https://www.who.int/gpsc/ssi-prevention-guidelines/en/ (accessed 18 August 2020)
World Health Organization. Safe surgery: why is safe surgery important. 2020. https://www.who.int/patientsafety/safesurgery/en/ (accessed 18 August 2020)
Care of the surgical patient: part 1
Matthew Robertson
Graduate Tutor for Operating Department Practice, Northumbria University, Newcastle upon Tyne
View articles · Email Matthew
Claire Ford
Lecturer, Adult Nursing, Northumbria University, Newcastle upon Tyne, explain how to reduce the risk of contamination
View articles · Email Claire
This article provides clinical guidance on the care of a patient undergoing an elective surgical procedure. It discusses preoperative care and the preparation of the patient. It aims to provide an awareness of the complications associated with perioperative care. Through the use of a patient case study, the authors demonstrate the care required across the full perioperative journey from diagnosis to discharge.
Surgery is an inevitable and important part of health care that can offer individuals life-changing interventions for a range of medical conditions ( Wicker, 2015 ). With increased developments in surgical techniques, such as laparoscopic approaches, and innovative strategies delivering better outcomes for surgical patients, surgeries that were once deemed high risk are now considered routine across a wider range of surgical specialties ( Dejong and Earnshaw, 2015 ). As a consequence, the number of surgeries being performed rose by 27% between 2003/2004 and 2013/2014 ( Royal College of Surgeons of England (RCS), 2020 ) and it is now estimated that more than 12 million surgical procedures are carried out in the UK every year ( Abbott et al, 2017 ).
This article aims to provide the reader with clinical guidance for the care of a surgical patient from diagnosis to discharge. It will also examine some of the complications that can occur within the perioperative care continuum (see Glossary for definition of terms) and explore the management strategies that may be used. Because hernia repair has been identified as one of the most common procedures performed in the UK, with over 100 000 of these procedures carried out every year ( RCS, 2013 ), a case study ( Box 1 ) has also been included to help illustrate the care required across the patient journey.
Preoperative care
Initial investigation or contact.
Preoperative care starts at the point of diagnosis and referral and is the first opportunity for health professionals to ensure that comprehensive preparation for the surgery begins. This should be from both a physical and psychological perspective because patients should be provided with the opportunity to ask questions about the surgery and aftercare to help reduce any fears and anxieties that they may have (Wicker and O'Neill, 2013). Consequently, primary care staff, including GPs and practice nurses, have a major role to play in the preparation of individuals for surgery, which can positively impact on postoperative outcomes, such as perceived levels of pain and behavioural recovery ( Powell et al, 2016 ). GPs are also responsible for making the initial referral to a surgical specialty and ensuring that comprehensive background information (ie medical history and specific details of the condition) are communicated to the surgical team so that an outpatient consultation clinic appointment can be arranged ( Royal College of General Practitioners, 2018 ).
Outpatient consultation
Delivering a high-quality clinic requires a holistic approach and the most effective and appropriate way to deliver this is to remain focused on the quality of service and ensure that the patient is treated as an individual with particular values, concerns and wishes ( RCS, 2018 ). The surgeon may decide to go through the process of obtaining informed consent at this appointment, which incorporates discussion of the details of the surgical procedure and comprehensive exploration of the risks and benefits of having the procedure; however, the patient must have the capacity to understand the information given and competence to decide on whether to proceed ( Anderson and Wearne, 2007 ). Following the consultation, the surgeon will list the individual for the required surgery and organise a preassessment appointment. In some cases, this could be on the same day, if the service incorporates one-stop clinics, which have been initiated in some areas to help streamline the service and ensure that most of the patient's preoperative care needs are addressed in a single visit ( RCS, 2018 ).
Preoperative assessment
The process of preassessment is essential for identifying any underlying comorbidities that would increase the risk of complications when having a general anaesthetic, as well as anything that may influence the surgical procedure itself ( Gray et al, 2018 ). However, it also provides the ideal opportunity for the early identification of, and attention to, individual patient needs, for patient concerns to be addressed before admission and for patient education about surgical preparation and aftercare ( Association of Anaesthetists of Great Britain and Ireland (AAGBI) 2010 ; AAGBI and British Association of Day Surgery, 2011 ; Wicker, 2015 ; Martin, 2016 ) ( Box 2 ). The investigations conducted at the preoperative assessment would usually include a full blood count (FBC), electrocardiogram (ECG), and lung function tests, but exactly which investigations are needed mainly depends on the level of the surgery (elective surgical procedures are classified as minor, intermediate or major ( Table 1 ), and the comorbidities of the individual ( Table 2 ) ( National Institute for Health and Care Excellence (NICE), 2016a ). The American Society for Anaesthesiologists (ASA) developed a Physical Status Classification System (often referred to as the ASA Grade) ( ASA, 2019 ) which is also used to determine the level of investigations that need to be conducted at the preoperative assessment and communicate patient comorbidities to the anaesthetic and surgical team ( NICE, 2016a ).
Surgical site marking is required in an attempt to reduce errors and must be performed only by an appropriate professional, undertaken with an indelible ink pen, using an arrow at or near the intended incision, which must be unambiguous and clearly visible because the site will be checked on three more occasions (leaving the ward, entering the operating department and prior to the incision) ( World Health Organization (WHO), 2009a ). Wherever possible, written consent must also be obtained before the surgery and anaesthetic, which needs to be clearly documented (no abbreviations) and retained in the patient's notes so they can be accessed by all the health professionals ( NHS website, 2019 ).
Nursing and other healthcare staff will care for the patient in the immediate period leading up to the surgery and will ensure that venous thromboembolism prophylaxis, ie antiembolism stockings, are put into place, that preoperative medication (gastric acid suppression and pre-emptive analgesia) is administered, that the patient is showered or bathed and warmed, that protocols have been followed to minimise surgical site infections, jewellery and body piercings have been removed or taped and that the preoperative checklist has been fully completed ( Dunn, 2016 ; WHO, 2016 ; NICE, 2016b ; 2019 ; 2020 ) ( Box 4 ).
Glossary of Terms
- Day surgery: term used to define the admission of patients to hospital for a planned surgical procedure when they will be returning home on the same day (less than 24 hours)
- Inpatient: a person who stays one or more nights in the hospital and receives treatment, lodging, and food
- Perioperative: the period around surgery including before, during and after
- Preoperative: a period from the time the surgery is scheduled until the time the patient is transported from the ward to the theatre operating table
- Intraoperative: the period of care during the operation and ancillary to that operation
- Postoperative: the period of care when the patient is returned from the operating department to the ward
Intraoperative care
The safe surgery process continues within the operating theatre and begins with the perioperative team (ie surgeons, anaesthetists, nurses, operating department practitioners (ODPs) and healthcare assistants (HCAs)) discussing the surgical procedures that are listed for the day and any specific patient requirements, eg allergies and equipment requirements ( Wicker, 2015 ). Once the patient arrives at the department a member of the team will admit the patient by checking the surgical safety checklist that was commenced by the staff on the ward, because the ‘check-in’ part of the form must be completed before the induction of anaesthesia ( WHO, 2009a ; 2009b ) ( https://tinyurl.com/yybrj4tl).
This checklist, which can be tailored to the needs of the clinical area, was created to reduce the number of adverse events by improving communication between the perioperative team and, since its introduction, there has been a marked improvement in the quantity of recorded adverse events within the operating theatre ( Walker et al, 2012 ). This is supported by Tang et al (2014) , who found, from their literature review, that effectively implemented surgical safety checklists can help in avoiding complications and reduce postoperative mortality.
The intraoperative process begins with the orientation of the patient to the anaesthetic room, the application of essential monitoring (ECG, pulse oximeter) and the induction of general anaesthetic, using a range of drugs to ensure that the patient is sedated, pain free and, if necessary, paralysed ( AAGBI, 2012 ). On transfer to the operating room, the ‘time out’ element of the surgical safety checklist will be undertaken before the surgical incision in the patient's skin. All members of the team must be present and attentive at this stage because all areas of potential risks are discussed in detail and this is the last opportunity for adaptations to be made to the surgery to prevent unnecessary harm ( WHO, 2009a ). As well as the safe surgical checklist, several considerations also need to be addressed by the perioperative team ( Box 5 ): surgical positioning, skin and nerve damage, patient warming.
Because patients, in most cases, are not able to advocate for themselves, all members of the intraoperative team must ensure that these elements of care are undertaken to reduce harm and achieve high-quality perioperative care ( Cousley, 2016a ). Surgical positioning is of particular importance, not only for ease of surgical access but also to minimise any adverse physiological effects, such as pressure ulcers and nerve damage, which can extend hospitalisation, delay patient recovery and increase costs to the patient and the NHS ( Wicker, 2015 ). These can be avoided with the use of pressure-relieving equipment, use of safe moving and handling techniques and devices, frequent skin assessments and effective communication between the perioperative team ( NICE, 2014 ). The importance of being an advocate for the surgical patient cannot be overstated, especially in an environment as complex as the operating theatre ( Sundqvist et al, 2016 ). The health professional must fully consider any potential risks to the patient and develop a strategy to minimise these risks ( Box 5 ).
Following the completion of the surgical procedure, the intraoperative team undertakes the ‘sign out’, which includes confirmation of the performed surgery, surgical counts of instrumentation, swabs and other supplementary items and any key concerns for recovery or postoperative care ( WHO, 2009a ). These details will be handed over to the post-anaesthetic care unit (PACU) specialist nurse, along with a record of the patient's vital observations while in theatre ( Simpson and Moonesinghe, 2013 ). The PACU practitioner will regularly check the patient's condition, monitor their vital signs, ensure they are comfortable and, if necessary, warmed ( Box 6 ) ( Wicker, 2015 ). They will also pay particular attention to pain relief and the reduction of postoperative nausea and vomiting, which are often the elements of perioperative care that patients most fear before surgery; as a consequence, these must be minimised to increase patient satisfaction but also to promote recovery and reduce the associated postoperative complications ( Liddle, 2013a ).
Postoperative care
Before the patient is transferred back to the ward a comprehensive handover must take place between the PACU nurse and ward staff, including details of the procedure, the patient's condition, level of responsiveness, airway and breathing, oxygen therapy, circulation, wound dressings and drains, fluid output and input, pain levels, medication and any other special instructions ( Liddle, 2013a ; Wicker, 2015 ). As well as the standard nursing roles and responsibilities, nurses caring for surgical patients also need to have a deep understanding of the potential complications that can arise following surgery, such as surgical site infection, pain, hypothermia ( Box 7 ) and how they can minimise risk or recognise early signs of development ( Primiano et al, 2011 ; Liddle, 2013b ; NICE, 2014 ; 2016b ; 2019 ).
Nurses in primary and secondary care are therefore in a unique position and offer a valuable contribution to the care of the surgical patient because they have a major role to play in minimising the risk of harm and ensuring that the patient is returned to normal functioning as soon as possible, depending on the individual's condition and surgical intervention ( Liddle, 2013b ; Cousley, 2016b ).
Due to the high level of iatrogenesis in surgery, patient safety poses a significant problem and almost half of all recorded adverse hospital events are related to surgical care ( WHO, 2020 ). Consequently, because patient safety is ‘at the heart of quality care’ ( Fisher and Scott, 2013: 6 ) it is paramount that health professionals minimise the risk of adverse events occurring by undertaking appropriate risk assessments and effective teamwork ( AAGBI, 2010 ).
- For the surgical patient, preoperative care involves preoperative processes and tests and the identification of patient concerns and needs
- Intraoperative care should follow a surgical safety checklist. After surgery, particular attention should be paid to preventing postoperative nausea and vomiting, and providing adequate pain relief
- In the postoperative period, nurses should be alert to the potential complications that could arise and provide patients with the information they need for discharge
CPD reflective questions
- What aspects of surgical preparation do you think are the most important and how can you improve your own practice in relation to preparing patients for their upcoming surgery?
- Reflect upon your own practice and consider how postoperative care can be enhanced from the perspective of patient satisfaction and safety
Integrating Perioperative Content in Nursing Curricula: A Case Study Approach
- PMID: 27234794
- DOI: 10.1016/j.aorn.2016.03.013
Perioperative nursing care requires unique specialty knowledge, skills, and abilities. National initiatives in nursing education and health care support integrating perioperative nursing content into curricular offerings in nursing schools and health care institutions. We provide an overview of the initiatives affecting nursing education, followed by a case study example and a guide to assist educators with incorporating perioperative case studies into their education plans. These resources may enhance the integration of perioperative nursing concepts in undergraduate curricula, internships, and continuing education offerings. The purpose of this article is to provide resources for nurse educators to systematically create case studies and to encourage increased exposure to perioperative concepts and competencies in a myriad of educational environments.
Keywords: case studies; conceptual learning; nursing education; perioperative nursing.
Copyright © 2016 AORN, Inc. Published by Elsevier Inc. All rights reserved.
- Curriculum*
- Education, Nursing / organization & administration*
- Schools, Nursing / organization & administration*
- Introduction
- Article Information
The date filter allows for daily selection of dates from March 1, 2020, to July 1, 2022. A slider is included under the date selection box for viewing policy progression throughout the pandemic. The health care settings filter consists of 4 checkboxes, allowing for the selection of target health care settings (general health care settings, nursing homes, home health care agencies, and both). Comprehensive definitions are found in the eTable in Supplement 1. The COVID-19 burden parameter consists of 5 checkboxes, allowing for the selection of 5 distinct categories of COVID-19 burden (cases and deaths) at the community and nursing home levels. The policy type filter allows for the selection of 5 broad policy categories. The policy subtype filter contains 38 distinct subcategories related to the broader categories. On the map, the number of policies is indicated by a color gradient, ranging from the least (light gray) to the most (dark blue). COVID-19 burden is depicted as circles of varying size, with larger diameters signifying increasing severity. Circles are red if there were deaths recorded during that period, green if there were no deaths, and gray if no data were available. The central US map can be enlarged for ease of viewing, while the 5 US territories remain fixed in size.
Maps depict May 24, 2020 (during first wave and after mandatory case and death reporting in nursing homes begins), January 12, 2021 (Alpha and Delta variants), and January 16, 2022 (Omicron variant). On the maps, the number of COVID-19 policies is indicated by a color gradient, ranging from the least (light gray color) to the most (darker blue color). All targeted health care settings (general, nursing homes, home health agencies, and both) were selected for this visual. COVID-19 burden is depicted as circles of varying size, with larger circles signifying increasing severity. The 7-day average of COVID-19 community deaths per 100 000 population was selected for this visual. Circles are red if there were deaths recorded during that period and green if there were no deaths.
eMethods. Policy Dataset and Dashboard Development
eTable. Definitions of Post–Acute Care COVID-19 Policy Categories and Subcategories
eReferences
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Stone PW , Zhao S , Chastain AM, et al. State- and Territory-Level Nursing Home and Home Health Care COVID-19 Policies and Disease Burden. JAMA Netw Open. 2024;7(4):e247683. doi:10.1001/jamanetworkopen.2024.7683
Manage citations:
© 2024
- Permissions
State- and Territory-Level Nursing Home and Home Health Care COVID-19 Policies and Disease Burden
- 1 Center for Health Policy, Columbia University School of Nursing, New York, New York
- 2 Department of Anesthesiology and Perioperative Medicine, University of Rochester School of Medicine, Rochester, New York
- 3 Department of Public Health Sciences, University of Rochester School of Medicine, Rochester, New York
- 4 RAND Health, RAND Corporation, Boston, Massachusetts
The COVID-19 pandemic disproportionately affected older persons, 1 many of whom were served by home health care agencies (HHAs) and nursing homes (NHs). The extent to which state- and territory-level COVID-19 policies reinforced or expanded federal policies is unknown. Building on the work of others, 2 we created a dataset and dashboard of state- and territory-specific NH and HHA policies linked with community and NH COVID-19 burden for researchers and public health officials to evaluate policy efficacy.
In this cross-sectional study, we used the Council of State Government’s 2020-2021 State Executive Orders website 3 and comprehensive searches of state and territory government websites to identify state- and territory-specific policies enacted from March 1, 2020, to July 1, 2022. We collected start and end dates and categorized policies as general or specific to NHs, HHAs, or both. Policies were grouped into 5 categories with 38 subcategories as (1) preventing virus transmission (n = 18), (2) expanding NH and/or HHA capacity (n = 5), (3) relaxing administrative requirements (n = 5), (4) reporting COVID-19 data (n = 3), and (5) admission and discharge policies (n = 7) (eMethods in Supplement 1 ).
We linked these policy data with community-level 4 and NH-specific COVID-19 burden (case and mortality counts) 5 and entered data into Tableau Desktop, version 2023.2. 6 We used a color gradient and circle size to visualize policy counts and COVID-19 burden, respectively. The interactive dashboard displays temporality with zoom capability of setting, policy, and COVID-19 burden.
This study was approved by the Columbia University Institutional Review Board, who waived the need for informed consent because the study was not deemed human participant research. We followed the STROBE reporting guideline.
We identified 1400 policies across 50 states and 5 territories. Most included all health care settings (n = 846), followed by NH-specific (n = 486), NH- and HHA-specific (n = 43), and HHA-specific (n = 25) policies. The most common policy category was preventing virus transmission (n = 736), followed by expanding NH and HHA capacity (n = 325), relaxing administrative requirements (n = 184), reporting COVID-19 data (n = 79), and admission and discharge (n = 54). The dashboard ( Figure 1 ) illustrates variation in the number of policies per state and severity of COVID-19 burden indicated by color gradient and circle diameter, respectively. Figure 2 highlights the dynamic change in NH and HHA policies and COVID-19 burden. For example, on May 24, 2020, Montana, Hawaii, and Alaska had no COVID-19 deaths or policies, in contrast with North Carolina’s moderate burden and several policies. By January 12, 2021, New York had a severe COVID-19 burden and the greatest number of policies, while Pennsylvania, Montana, and Florida had a similar COVID-19 burden but fewer policies.
The dataset and dashboard described in this study are potentially important tools for researchers and public health officials and could provide a template for visual platforms that may inform future efforts to manage public health crises. Variations in COVID-19 burden and state and territory policy responses displayed in the dashboard highlight the complexity of pandemic management. Exploratory analyses demonstrated that higher numbers of policies at the state and territory levels were not consistently associated with reductions in community- or NH-level COVID-19 burden, suggesting policy effectiveness may depend on implementation and compliance. We also found limited attention to HHAs compared with NHs, despite both settings serving vulnerable older populations. This suggests a gap in public health planning, raising questions about resource allocation and prioritization among health care settings during pandemics.
Study limitations include the primarily descriptive data, underlying data from various sources, and limited evaluation of efficacy of public health policies on population COVID-19 outcomes. Future public health planning and pandemic responses should include adaptive and targeted policy interventions and should consider specific needs of all health care settings. Dashboards have the potential to help formulate data-driven decision-making during public health crises.
Accepted for Publication: February 17, 2024.
Published: April 22, 2024. doi:10.1001/jamanetworkopen.2024.7683
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Stone PW et al. JAMA Network Open .
Corresponding Author: Patricia W. Stone, PhD, RN, Center for Health Policy, Columbia University School of Nursing, 560 W 168th St, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Stone had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Stone, Shang, Glance, Dick.
Acquisition, analysis, or interpretation of data: Stone, Zhao, Chastain, Perera, Shang, Dick.
Drafting of the manuscript: Stone, Zhao, Chastain, Perera, Shang, Glance.
Critical review of the manuscript for important intellectual content: Stone, Shang, Glance, Dick.
Statistical analysis: Zhao, Shang, Glance, Dick.
Obtained funding: Stone, Shang, Dick.
Administrative, technical, or material support: Stone, Chastain, Perera.
Supervision: Stone, Chastain, Perera, Shang, Dick.
Conflict of Interest Disclosures: Dr Stone reported receiving grant funding from the National Institutes of Health outside the submitted work. Ms Zhao reported participating in an internship through EmblemHealth outside the submitted work. Dr Chastain reported receiving grant funding from the National Institutes of Health outside the submitted work. Dr Perera reported receiving grant funding from the National Institutes of Health outside the submitted work. Dr Shang reported receiving grant funding from the National Institutes of Health outside the submitted work. Dr Glance reported receiving grant funding from the National Institutes of Health outside the submitted work. Dr Dick reported receiving grant funding from the National Institutes of Health outside the submitted work. No other disclosures were reported.
Funding/Support: This work was funded by grant R01NR016865 from the National Institute of Nursing Research and by grant R01AG074492 from the National Institute on Aging, the National Institute of Minority Health and Health Disparities, and the National Institute of Allergy and Infectious Diseases.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: Albert Chavesta, MS, MPH, assisted in compiling and categorizing the state- and territory-level policies, as well as drafting the policy dataset development methodology. Tenzin Trinley, MPH, Jung A. Kang, MSN, RN, and Charity Ogunlusi, MD, MPH, assisted with compiling state-level policies. All those acknowledged were affiliated with the Columbia University School of Nursing during the conduct of the study and were compensated via the study funding.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 19 April 2024
Cost of care pathways before and after appropriate and inappropriate transfers to the emergency department among nursing home residents: results from the FINE study
- E. Gombault-Datzenko 1 ,
- N. Costa 1 , 2 ,
- M. Mounié 1 , 2 ,
- N. Tavassoli 3 ,
- C. Mathieu 3 , 4 ,
- H. Roussel 5 ,
- J. M. Lagarrigue 6 ,
- E. Berard 2 , 7 ,
- Y. Rolland 2 , 3 &
- L. Molinier 1 , 2
BMC Geriatrics volume 24 , Article number: 353 ( 2024 ) Cite this article
39 Accesses
Metrics details
Transfers of nursing home (NH) residents to the emergency department (ED) is frequent. Our main objective was to assess the cost of care pathways 6 months before and after the transfer to the emergency department among NH residents, according to the type of transfer (i.e. appropriate or inappropriate).
This was a part of an observational, multicenter, case-control study: the Factors associated with INappropriate transfer to the Emergency department among nursing home residents (FINE) study. Sixteen public hospitals of the former Midi-Pyrénées region participated in recruitment, in 2016. During the inclusion period, all NH residents arriving at the ED were included. A pluri-disciplinary team categorized each transfer to the ED into 2 groups: appropriate or inappropriate. Direct medical and nonmedical costs were assessed from the French Health Insurance (FHI) perspective. Healthcare resources were retrospectively gathered from the FHI database and valued using the tariffs reimbursed by the FHI. Costs were recorded over a 6-month period before and after transfer to the ED. Other variables were used for analysis: sex, age, Charlson score, season, death and presence inside the NH of a coordinating physician or a geriatric nursing assistant.
Among the 1037 patients initially included in the FINE study, 616 who were listed in the FHI database were included in this economic study. Among them, 132 (21.4%) had an inappropriate transfer to the ED. In the 6 months before ED transfer, total direct costs on average amounted to 8,145€ vs. 6,493€ in the inappropriate and appropriate transfer groups, respectively. In the 6 months after ED transfer, they amounted on average to 9,050€ vs. 12,094€.
Conclusions
Total costs on average are higher after transfer to the ED, but there is no significant increase in healthcare expenditure with inappropriate ED transfer. Support for NH staff and better pathways of care could be necessary to reduce healthcare expenditures in NH residents.
Trial registration
clinicaltrials.gov, NCT02677272.
Peer Review reports
The number of people aged 60 years and older worldwide is increasing. There were 1 billion in 2019 and this number will increase to 2.1 billion by 2050 [ 1 ]. This increase is occurring at an unprecedented pace and requires adaptations of societal structures across all sectors.
In France, there were 17 million people aged 60 years or older in 2018. This number will reach 24 million by 2060 [ 2 ]. In 2016, of the French population, 728,000 elderly people lived in nursing homes (NHs), i.e. 10% of people aged 75 years or older and one third of those aged 90 years or older [ 3 ]. NHs cater for people aged 60 and over, with varying degrees of dependency. They may be public, private or associative (private not-for-profit). The way they are organized, the staff present (coordinating physician, nurses…) and the charges vary according to the care offered to residents.
Around 50% of NH residents are hospitalized at least once per year in France, and there is an intense flow between NHs and emergency departments (EDs) [ 4 , 5 ], as is also the case in other countries (Australia, Ireland, Canada, etc.) [ 6 , 7 , 8 ]. French and international observational studies have shown that 50% of NH residents per year are transferred to an ED [ 9 ]. These transfers are often inappropriate (about 40% of cases) and costly [ 10 , 11 , 12 , 13 ]. Moreover, when the transfer to the ED is inappropriate (i.e. not a health emergency, normal vital signs), the benefit / risk balance for the patient is often unfavorable, with a high risk of confusion and functional decline [ 14 , 15 ].
For the French health insurance (FHI) in 2016, the median annual care cost per NH resident was 14,375€, with 12% for outpatient costs [ 16 ]. This cost was major and increased with the resident’s level of dependency and comorbidities. A few studies suggested that reducing inappropriate hospitalizations of NH residents could lead to lower costs [ 17 , 18 , 19 ]. We can hypothesize that inappropriate transfer is a sign of non-integrated care of elderly people before arrival in the emergency room. Then, inappropriate transfer to the ED could be associated with increased healthcare utilization and associated expenditures 6-months before and after the transfer (in- and outpatient costs).
The main objective of the current study was to assess the cost of care pathways 6 months before and after the transfer to the emergency department among NH residents, according to the type of transfer (i.e. appropriate or inappropriate). The second objective was to explore factors associated with healthcare utilization’s costs among NH residents.
Setting, design and population
This study is a part of the Factors associated with INappropriate transfer to the Emergency department among nursing home residents (FINE) study [ 20 ]. The FINE study, which is an observational, multicenter, case-control study (clinicaltrials.gov, NCT02677272), initially aimed to identify factors associated with inappropriate transfers to the ED, by comparing resident and NH characteristics, as well as the circumstances upon transfer to the ED.
Sixteen public hospitals (from among 25 in the former Midi-Pyrénées region in the southwest of France) participated in recruitment for the FINE study, from January 2016 to December 2016 (12 months). During the inclusion period, all residents arriving at the ED from an NH were included, the only inclusion criterion being arrival from an NH.
A team of experts (one geriatrician, a family doctor, an emergency doctor and a pharmacist) defined appropriate/inappropriate transfers to the ED during a face-to-face meeting using a standardized approach. Charts for each resident were reviewed by the team and three criteria characterizing inappropriate transfer were discussed: the lack of somatic or psychiatric emergency conditions, the presence of palliative care known before and advanced directives of non-hospitalization. Indeed, in these 3 clinical situations, patients should be managed differently, without being transferred to the emergency department, with no increased health risk. A patient in palliative care no longer requires emergency care, and should therefore not be transferred to an emergency department. Similarly, a patient who has formulated advance directives of non-hospitalization should not be transferred to a hospital. The method has been previously reported in detail [ 11 ].
Cost estimates
Healthcare costs were assessed from the FHI perspective. Direct medical and non-medical costs were included in this study. Direct costs corresponded to hospitalization costs, outpatient costs (i.e. visits and medical acts [imaging and other preventive exams, diagnostic exams and curative acts], paramedical acts [nurse, physical therapist and speech therapist]), medications and medical equipment costs. Non-medical costs included transportation costs. Costs were estimated by multiplying the number of units used for each resource with the corresponding unit cost.
The consumption of healthcare resources was retrospectively gathered from the FHI database. It contains fee-for-service claims for in- and outpatient medical services supplied to 80% of the residents of France (belonging to the general worker’s insurance scheme and agricultural workers insurance scheme) [ 21 ]. The remaining 20% of French residents are covered by special subdivisions of the French social healthcare system, depending on their job and their fee-for-services claims are not available in the FHI database. Administrative data corresponding to the first name, last name, birthdate, place of residence and sex were recorded for patients who live in an NH located in the Midi-Pyrénées region.
Inpatient stays were valued using per diem costs. Outpatient care, which includes visits, medical and paramedical acts, medications, medical equipment and transportation, was valued using the tariffs reimbursed by the FHI. In particular, transportation, visits and paramedical acts were valued using the French General Nomenclature of Professional Acts [ 22 ]. Medical acts were valued using the French Common Classification of Medical Acts [ 23 ], except for laboratory tests, for which valuation was based on the Nomenclature of Biological Acts [ 24 ]. Medical equipment was valued using the List of Reimbursable Products and Services [ 25 ]. Medications were valued using retail prices, and their reimbursement was present in the database only for NHs without a pharmacy for internal use (PIU) [ 26 ].
For all these fees, we applied the corresponding reimbursement rate and we subtracted, if necessary, the medical deductible, which is due by the patient and not reimbursed by the FHI. Costs were expressed in 2015–2016 euros and were recorded over a 6-month period before and after the transfer to the ED.
Other variables
Variables useful for the cost analysis collected during the FINE study were:
For the characteristics of the residents: sex, age, comorbidities using the Charlson score (score from 0 to 37), level of dependence using the Katz Activities of Daily Living (ADL) scale (score from 0 “total dependency” to 6 “autonomy”), vital status, if the resident is receiving palliative care and the presence of advanced directives for non-hospitalization,
For the characteristics of the NH: location (French department), NH with pharmacy for internal use, number of beds, distance (in kilometers) to the ED and available NH staff (presence of a coordinating physician or a geriatric nursing assistant),
For the characteristics of the transfer: season of transfer (January to March = winter, April to June = spring, etc.) and post-transfer destination (hospitalization, back at NH or death).
Statistical analysis
Patients were divided into two groups according to ED transfer: appropriate or inappropriate. Resident, NH and ED transfer characteristics were described using means and standard deviation for continuous variables and using frequencies and percentages for categorical variables. These two groups were also compared with a bivariate analysis (Mann-Whitney test for continuous variables, Chi2 test or Fisher’s exact test for categorical variables). Regarding the analysis of the main objective: for total direct costs, hospitalizations costs and outpatient costs, monthly mean costs and their 95% confidence intervals were calculated for 6 months before and after the transfer to the ED, in the two groups, and compared using the Wilcoxon test. Regarding the analysis of the secondary objective: A generalized linear mixed model (GLMM) with gamma distribution and log link was implemented to adjust monthly cost variation on confounding factors. GLMM allows the correlation within the longitudinal data to be taken into account [ 27 ]. Covariates used in the model were type of transfer (appropriate vs. inappropriate), sex, age (3 categories : < 85years old/ 85–90 years old/ > 90 years old), Charlson score (2 categories: 0–2 / ≥3), period before or after transfer, season (2 categories: winter-spring/ summer-autumn, i.e. a year divided into two semesters), death (month of death and month before, or not) and presence of a coordinating physician or a geriatric nursing assistant in the NH. We had to reduce the number of categories for some variables, in order to make the analysis possible with a sufficient sample size. A GLMM was also developed over two separate periods: before and after transfer to the ED. All statistical analyses were performed using the R software (version 3.5.3).
Characteristics of the studied population
Data were available for 616 patients in the FHI database (59.4% of patients included in the FINE study). Among these, 132 (21.4%) had an inappropriate ED transfer (see the flow chart in Supplementary Figure S 1 ).
Table 1 shows the descriptive characteristics of residents, of NHs and of ED transfer according to the appropriateness of the transfer. Residents with an inappropriate ED transfer were younger (mean age difference: -1.53 years, p = 0.024) and were more often under palliative care (+ 10%, p < 0.001) than residents with an appropriate ED transfer. The post-transfer destination are also significantly different between two groups: more hospitalizations with appropriate ED transfer (+ 27%, p < 0.001) and more returns to the NH with inappropriate ED transfer (+ 27%, p < 0.001) were observed. The characteristics of our population (616 residents) were similar to those of the FINE population not found in FHI database (421 residents) (see Supplementary Table S 2 , no significant differences, except for age in the inappropriate ED transfer group). During the 6 months after ED transfer, 208 residents died, 45 (34%) in the inappropriate ED transfer group and 163 (34%) in the appropriate ED transfer group.
Analysis of the main objective: comparison between the inappropriate and appropriate ED transfer groups
Figure 1 presents total direct costs by month for both the appropriate and inappropriate ED transfer groups, then hospitalization and outpatient costs separately (see Supplementary Table S 3 for details). In the 6 months before ED transfer, total direct costs on average amounted to 8,145€ for the inappropriate transfer group and 6,493€ for the appropriate transfer group. In the 6 months after ED transfer, they amounted on average to 9,050€ for the inappropriate transfer group and 12,094€ for the appropriate transfer group. Considering the whole period (6-month before and after ED transfer), these differences in average cost between inappropriate and appropriate transfer groups were non-significant (-1,392€, p = 0.57).
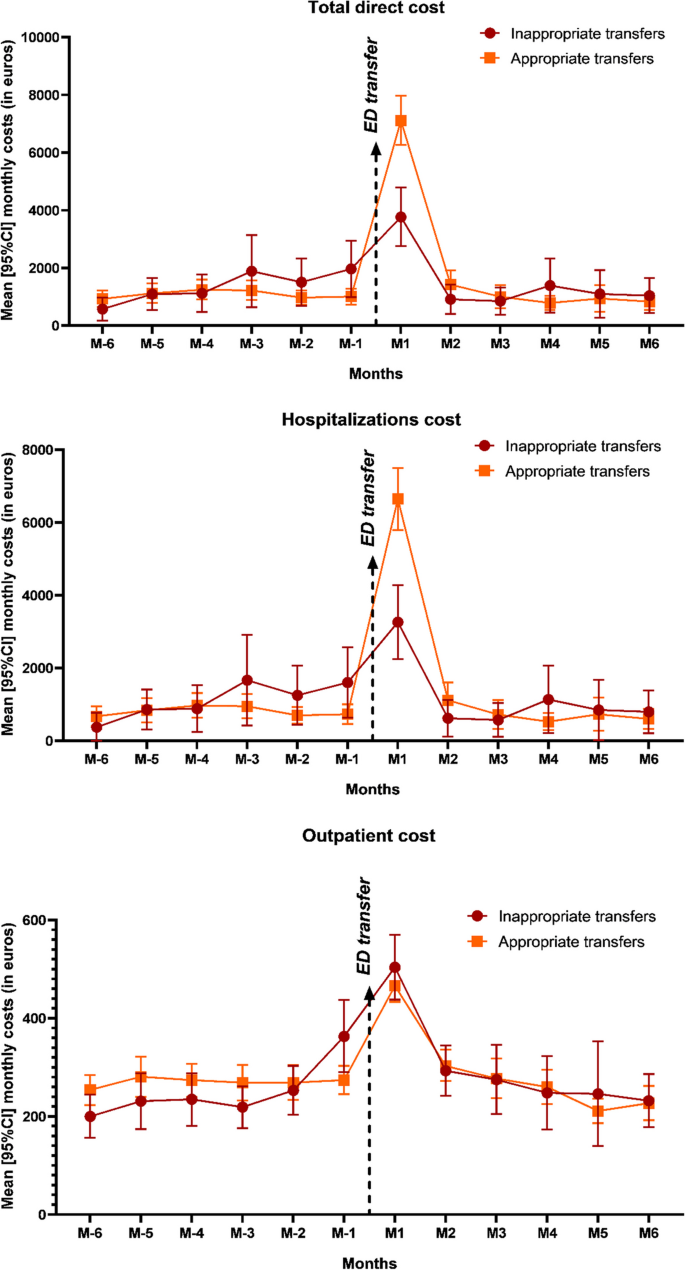
Mean [95%CI] monthly costs 6 months before and after transfer to the ED
ED emergency department; 95%CI 95% Confidence intervals
The largest part of costs after ED transfer occur during the first month (41.6% of the 6-month-post-transfer cost in the inappropriate transfer group and 58.8% in the appropriate transfer group). Regarding hospitalizations only, 6 months after ED transfer, costs amounted to 7,241€ and 10,346€ in the inappropriate and appropriate transfer groups, respectively. Most variation was due to conventional inpatient stays.
For outpatient costs, the 6 months before ED transfer amounted to 1,501€ vs. 1,621€ and the 6 months after to 1,798€ vs. 1,744€ for the inappropriate and appropriate transfer groups, respectively. Costs were already increasing one month before ED transfer. Figure 2 presents different cost categories: medical visits, medical acts, medications and medical equipment. In the inappropriate transfer group, we can observe a larger costs’ increase starting the month before ED transfer compared to the appropriate transfer group. Considering the whole period, the differential cost between the two groups was significant only for medical visits (mean annual costs: 618€ in the inappropriate ED transfer group vs. 542€ in the appropriate ED transfer group, p = 0.007).
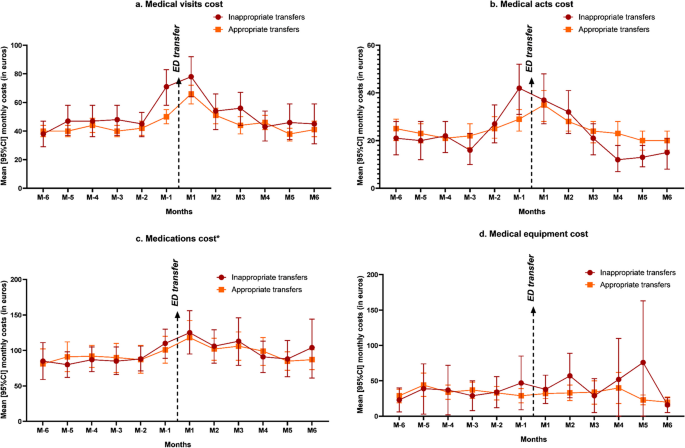
Mean [95%CI] monthly outpatient cost categories 6 months before and after transfer to the ED. a . Medical visits cost b . Medical acts cost c . Medications cost d . Medical equipment cost
* Except for residents in nursing homes with a pharmacy for internal use. ED emergency department; 95%CI 95% Confidence intervals
Analysis of the secondary objective: multivariate analysis
Figure 3 shows the results of the adjusted GLMM for total direct costs and separately for hospitalization and outpatient costs (see details in Supplementary Table S 4 ). During the follow-up year, adjusted for sex, age, Charlson score, period, season, death and NH human resources, total direct costs were 17% lower in the inappropriate group compared to the appropriate group (RR = 0.83; 95% CI 0.64–1.09, p = 0.19). On average, total direct costs were 39% lower for women compared to men (RR = 0.61; 95% CI 0.48–0.78, p < 0.001). Contrariwise, total direct costs were 33% higher when ED transfer occurred in seasons winter-spring (from January to June) than in seasons summer-autumn (RR = 1.33; 95% CI 1.07–1.66, p = 0.01), and were multiplied by 2.35 for the 6-month period after ED transfer (RR = 2.35; 95% CI 2.17–2.57, p < 0.001), and by 3.4 just the month before death (RR = 3.4; 95% CI 2.80–4.14, p < 0.001). Regarding hospitalizations cost, results were similar or even exacerbated for the 6-month period after ED transfer (RR = 6.51; 95% CI 5.32–7.97, p < 0.001) and death (RR = 31.89; 95% CI 20.27–50.19, p < 0.001). Regarding outpatient cares, on average, costs were 21% lower in NHs with coordinating physicians (RR = 0.79; 95% CI 0.62-1.00, p = 0.054).
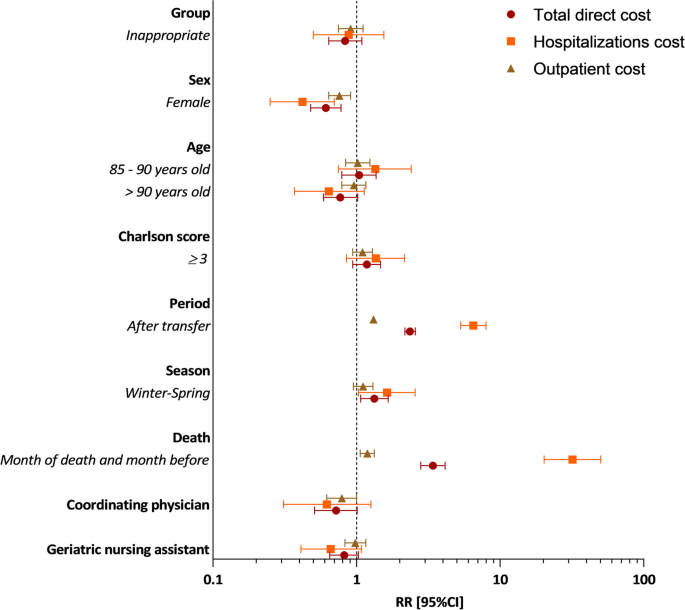
Predictors of total direct cost, hospitalizations cost and outpatient cost over a year (6 months before and after transfer to the ED). RR Relative risk; 95%CI 95% Confidence intervals; ED emergency department
Figure 4 shows the results of the adjusted GLMM, for total direct cost over two separate periods: 6 months before and 6 months after ED transfer (see details in Supplementary Table S 5 ). Six months before, total direct costs were 6% higher in the inappropriate group compared to the appropriate group, but non-significant (RR = 1.06; 95% CI 0.75–1.50, p = 0.736). On average, costs were 48% lower for women compared to men (RR = 0.52; 95% CI 0.38–0.72, p < 0.001), 25% lower in NHs with coordinating physicians compared to NHs without (RR = 0.75; 95% CI 0.49–1.16, p = 0.2021) and 28% lower in NHs with geriatric nursing assistants compared to NHs without (RR = 0.72; 95% CI 0.54–0.98, p = 0.0345). Six months after, total direct costs were lower in the inappropriate group (RR = 0.66; 95% CI 0.49–0.88, p = 0.006), for women (RR = 0.69; 95% CI 0.52–0.90, p = 0.006) and in NHs with coordinating physicians (RR = 0.68. 95% CI 0.47–0.99, p = 0.047).
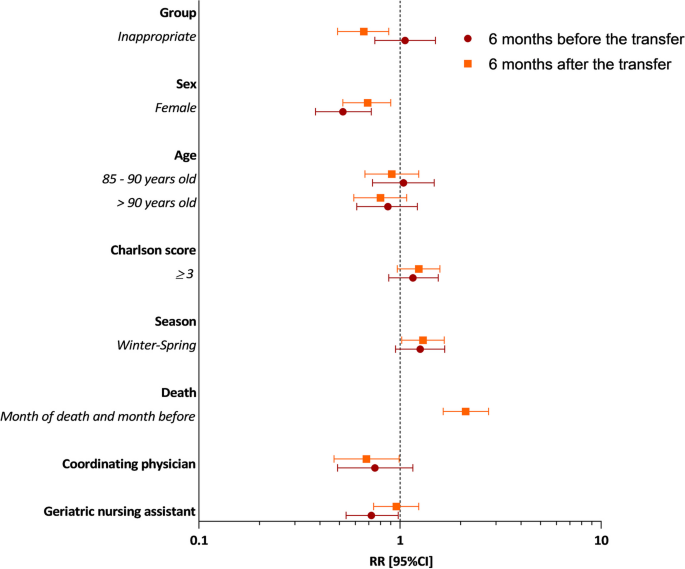
Predictors of total direct cost 6 months before and 6 months after transfer to the ED. RR Relative risk; 95%CI 95% Confidence intervals; ED emergency department
The principal findings of this study show that total costs are higher after the transfer to the ED compared to before, whatever the transfer is appropriate or inappropriate, and mainly in the first month following the transfer. Moreover, when the transfer to the ED is inappropriate, there were an increase in cost of care 6-months before ED transfer, and we observed higher outpatient costs during this period compared with the appropriate transfer group (despite a small (6%) and non-significant difference between our two groups). Our first hypothesis that inappropriate transfer to the ED could be associated with increased expenditures 6-months before and after the transfer (in- and outpatient costs) is not confirmed by our results (non-significant).
To our knowledge, there is no study aiming to estimate the extra-cost 6-months before and after the ED transfer, taking into account the overall costs (out- and inpatient) due to inappropriate ED transfer. Several studies aiming to estimate cost of inappropriate ED transfer and potentially avoidable hospitalization, but considering only inpatient costs. These studies showed an inpatient costs increase in case of inappropriate ED admissions or avoidable hospitalizations [ 17 , 18 ], but these inpatient costs are still lower than those for appropriate hospitalizations, when there is a comparison [ 13 ]. For example, in 2015, an American study explained that a significant proportion of Medicare NH patients were transferred to the ED for ambulatory care-sensitive conditions (ACSC) [ 28 ]. This was associated with higher healthcare utilization and ED costs (mean ED costs/episode of care: $401 vs. $294 for ACSC patients compared to non-ACSC patients), but lower hospitalization costs (mean hospitalization costs/episode of care: $8,356 vs. $10,226, p < 0,001).
We found a similar hospitalization cost difference in our study (but non-significant): the increase in total costs is higher in the appropriate transfer group than in the inappropriate one. However, hospitalization costs represent the largest part of total costs (between 80% and 86% after ED transfer). So, this result can be explained because patients in the appropriate transfer group are hospitalized more often and for a longer period after the ED visit than patients in the inappropriate transfer group.
During the 6-month period before ED transfer, the higher outpatient costs were unexpected in the inappropriate transfer group and require further exploration, even if non-significant results were observed. It may indicate a suboptimal care pathway. Some nonspecific symptoms, like confusion, disorientation, agitation or complaints of pain, could lead to misdiagnosis with recurrent medical exams, medical visits, ED transfers and hospitalizations. It is common in older people, especially in case of mild cognitive impairment or dementia; it has been reported that dementia increases healthcare utilization and expenditures [ 29 , 30 , 31 , 32 ]. Therefore, it is important to coordinate care and to take into account as a priority the needs and preferences of older people as proposed by the WHO guidelines on Integrated Care for Older People (ICOPE) [ 33 ].
Concerning factors associated with healthcare utilization’s costs among NH residents, total costs were significantly lower for women. We know that women have better health behavior, with better medical follow-up. They live longer in good health and they are less expensive for the healthcare system [ 34 , 35 ]. Moreover, in our study, men had more comorbidities (57% with Charlson score ≥ 3 vs. 38.6% for women), resulting in additional healthcare expenditures. Second, death was associated with a significant increase in costs, mainly due to hospital costs. The healthcare utilization is often high in the last months of life with many hospitalizations [ 36 ]. However, substantial savings are possible with a specific end-of-life program in NHs (comfort measures and limited medical intervention), thus decreasing hospitalizations and associated inpatient costs [ 37 ]. Third, costs were higher during the first half of the year (winter and spring). We can imagine that winter epidemics (influenza, bronchitis, gastroenteritis) cause an increase in healthcare utilization (medical visits, medications) and related costs. Indeed, epidemic peaks are more frequently observed at the beginning of the year. This was indeed the case for our study period, with an epidemic peak of influenza in January-February 2016 and 2017 [ 38 ].
This study also highlighted NH organization’s impact on healthcare costs. Before ED transfer, the presence of a geriatric nursing assistant in NHs significantly reduces costs and after ED transfer, this is the presence of a coordinating physician. In France, geriatric nursing assistants play a preventive and alert role with dementia patients: they identify potential decompensation and anticipate their care. Thus, we can speculate that this helps avoid the aggravation of symptoms and the costs of care it entails. Coordinating physicians are family doctors whose training in geriatrics includes 70 h of theoretical training and 70 h of practical training. They are present around 1 to 2 days per week in the NH and they are in charge of the comprehensive geriatric assessment of the resident and the coordination of the care and staff in the NH. Due to this, the coordinating physician improves interactions between the different health professionals, for optimized and less expensive patient care. NH organizational characteristics may thus affect individual healthcare consumption and costs. For example, several studies from the USA show that the use of advanced practice nurses reduces preventable hospitalizations [ 39 , 40 ]. In summary, better access to on-site evaluation could have favorable effects on healthcare utilization and expenditures [ 28 , 41 ]. This result is important for policymakers when considering resources provided to NH staff to take care of, treat and ultimately avoid the ED transfer of NH residents.
This study has several strengths. This is the first cost analysis to study healthcare expenditures before and after the inappropriate ED transfer, taking into account the overall costs (out- and inpatient costs). Moreover, this analysis used data from the FHI database, which is an accurate data source to gather healthcare consumption. It was a real-life study because all patients from NHs were included, with no other selection criteria. Therefore, our observed results reflected reality [ 42 , 43 , 44 ].
However, this study also has some limitations. First, the health economic analysis was limited to patients covered by the general worker’s regimen and farmer’s regimen with the use of the FHI database. The presence of 60% of the FINE population in the FHI database, instead of the 80% expected, could be explained by a different distribution of regimens in NHs or a healthcare utilization in another region. Furthermore, inpatient stays were not valued using the French disease-related groups of the French hospital-discharge database (PMSI), but the billing data used was close enough to real costs. Another limitation is that healthcare costs may vary between NHs for several reasons, and the total cost may therefore be underestimated. The main reason is the presence or absence of a PIU. In this study, 19% of NHs have a PIU, which means that drugs dispensed by this PIU are not specifically reimbursed individually for the patient but for the whole NH [ 45 ], and only individual reimbursements for the patient are available in the FHI database. Moreover, costs may be underestimated because of the absence of accommodation and food costs, as well as the cost of burden staff, formal and informal cares. These data are not available in the FHI database. Formal care costs in NHs increase according to the dependence level of the patient, and even if the informal care cost is not as high as in community-dwelling patients, it can be a significant part of the total healthcare cost of NH residents [ 46 ].
To conclude, we have not shown any significant increase in healthcare expenditure with inappropriate ED transfer. However, actions could be considered to prevent these inappropriate transfers from NH, with a possible financial impact on the healthcare system; how to better allocate these resources, e.g. to fund interventions aimed at improving primary care access, such as implementing ICOPE in long-term care facilities. In addition, support for NH staff and better pathways of care seem necessary to reduce healthcare expenditures in NH residents.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Ambulatory care-sensitive conditions
Emergency department
French Health Insurance
Generalized linear mixed model
- Nursing home
Pharmacy for internal use
Ageing and health. Disponible sur: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health . Consulté le: 9 Juil 2021.
Population par âge − Tableaux de l’économie française | Insee. Disponible sur: https://www.insee.fr/fr/statistiques/3303333?sommaire=3353488 . Consulté le: 9 Juil 2021.
L’enquête auprès des établissements d’hébergement pour personnes âgées (EHPA) | Direction de la recherche, des études, de l’évaluation et des statistiques. Disponible sur: https://drees.solidarites-sante.gouv.fr/sources-outils-et-enquetes/07-lenquete-aupres-des-etablissements-dhebergement-pour-personnes-agees . Consulté le: 9 Juil 2021.
Rolland Y, Abellan G, van Kan S, Hermabessiere S Gerard, Guyonnet Gillette S, Vellas B. Descriptive study of nursing home residents from the REHPA network. J Nutr Health Aging. 2009;13:679–83. https://doi.org/10.1007/s12603-009-0197-4 .
Article CAS PubMed Google Scholar
Rolland Y, Andrieu S, Crochard A, Goni S, Hein C, Vellas B. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc. 2012;13(4):4077–12. https://doi.org/10.1016/j.jamda.2011.12.056 .
Article Google Scholar
Briggs R, Coughlan T, Collins R, O’Neill D, Kennelly SP. Nursing home residents attending the emergency department: clinical characteristics and outcomes. QJM Int J Med. 2013;106(9):803–8. https://doi.org/10.1093/qjmed/hct136 .
Article CAS Google Scholar
Jensen PM, Fraser F, Shankardass K, Epstein R, Khera J. Are long-term care residents referred appropriately to hospital emergency departments? Can Fam Physician Med Fam Can. 2009;55(5):500–5.
Google Scholar
Ingarfield SL, et al. Use of emergency departments by older people from residential care: a population based study. Age Ageing. 2009;38(3):314–8. https://doi.org/10.1093/ageing/afp022 .
Article PubMed Google Scholar
Carson J, Gottheil S, Gob A, Lawson S. London transfer project: improving handover documentation from long-term care homes to hospital emergency departments. BMJ Open Qual. 2017;6(2):e000024. https://doi.org/10.1136/bmjoq-2017-000024 .
Article PubMed PubMed Central Google Scholar
Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52(10):1730–6. https://doi.org/10.1111/j.1532-5415.2004.52469.x .
Perrin A, et al. Factors predisposing nursing home resident to inappropriate transfer to emergency department. The FINE study protocol. Contemp Clin Trials Commun. 2017;7:217–23. https://doi.org/10.1016/j.conctc.2017.07.005 .
Seyit M, Yilmaz A, Seyit DA, Ozen M. Cost analysis of emergency department visits by geriatric patients living in nursing homes. J Coll Physicians Surg Pak. 2019;29(7):658–60. https://doi.org/10.29271/jcpsp.2019.07.658 .
Menand E, et al. French multicenter evaluation of the appropriateness of admission to the emergency department of the over-80s. J Nutr Health Aging. 2015;19(6):681–7. https://doi.org/10.1007/s12603-015-0489-9 .
Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing. 2014;43(6):759–66. https://doi.org/10.1093/ageing/afu117 .
Skains RM, et al. Hospital-associated disability due to avoidable hospitalizations among older adults. J Am Geriatr Soc. 2023. https://doi.org/10.1111/jgs.18238 .
La situation des établissements d’hébergement pour personnes âgées dépendantes (EHPAD) en 2016, CNSA. Disponible sur: https://www.cnsa.fr/actualites-agenda/actualites/la-situation-des-etablissements-dhebergement-pour-personnes-agees-dependantes-ehpad-en-2016 . Consulté le: 9 Juil 2021.
Muench U, et al. Preventable hospitalizations from ambulatory care sensitive conditions in nursing homes: evidence from Switzerland. Int J Public Health. 2019;64(9):1273–81. https://doi.org/10.1007/s00038-019-01294-1 .
Ouslander JG, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs: [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp 760–761]. J Am Geriatr Soc. 2010;58(4):627–35. https://doi.org/10.1111/j.1532-5415.2010.02768.x .
Grabowski DC, O’Malley AJ, Barhydt NR. The costs and potential savings associated with nursing home hospitalizations. Health Aff (Millwood). 2007;26(6):1753–61. https://doi.org/10.1377/hlthaff.26.6.1753 .
Rolland Y, et al. Factors associated with potentially inappropriate transfer to the emergency department among nursing home residents. J Am Med Dir Assoc. 2021. https://doi.org/10.1016/j.jamda.2021.04.002 .
Tuppin P, et al. Value of a national administrative database to guide public decisions: From the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017;65(Suppl 4):S149–67. https://doi.org/10.1016/j.respe.2017.05.004 .
NGAP 01.04.2022_defBIS.pdf. Disponible sur: https://www.ameli.fr/sites/default/files/Documents/NGAP%2001.04.2022_defBIS.pdf . Consulté le: 13 Avr 2022.
CCAM_V69_-_01042022.pdf. Disponible sur: https://www.ameli.fr/fileadmin/user_upload/documents/CCAM_V69_-_01042022.pdf . Consulté le: 13 Avr 2022.
Codage des actes biologiques - NABM. Disponible sur: https://www.ameli.fr/haute-garonne/medecin/exercice-liberal/remuneration/nomenclatures-codage/codage-actes-biologiques-nabm . Consulté le: 13 Avr 2022.
Liste des produits et prestations - LPP. Disponible sur: https://www.ameli.fr/haute-garonne/medecin/exercice-liberal/remuneration/consultations-actes/nomenclatures-codage/liste-produits-prestations-lpp . Consulté le: 13 Avril 2022.
Médicaments. Disponible sur: https://www.ameli.fr/haute-garonne/medecin/exercice-liberal/remuneration/nomenclatures-codage/medicaments . Consulté le: 13 Avr 2022.
Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38(4):963–74.
Axon RN, Gebregziabher M, Craig J, Zhang J, Mauldin P, Moran WP. Frequency and costs of hospital transfers for ambulatory care-sensitive conditions. Am J Manag Care. 2015;21(1):51–9.
PubMed PubMed Central Google Scholar
Goldfeld KS, Stevenson DG, Hamel MB, Mitchell SL. Medicare expenditures among nursing home residents with advanced dementia. Arch Intern Med. 2011;171(9):824–30. https://doi.org/10.1001/archinternmed.2010.478 .
Daras LC, Feng Z, Wiener JM, Kaganova Y. Medicare expenditures associated with hospital and emergency department use among beneficiaries with dementia. Inq J Med Care Organ Provis Financ. 2017;54:46958017696757. https://doi.org/10.1177/0046958017696757 .
Panca M, et al. Healthcare resource utilisation and costs of agitation in people with dementia living in care homes in England - The Managing Agitation and Raising QUality of LifE in Dementia (MARQUE) study. PLoS One. 2019;14(2):e0211953. https://doi.org/10.1371/journal.pone.0211953 .
Article CAS PubMed PubMed Central Google Scholar
Zhu CW, et al. Longitudinal study of effects of patient characteristics on direct costs in Alzheimer disease. Neurology. 2006;67(6):998–1005. https://doi.org/10.1212/01.wnl.0000230160.13272.1b .
Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity. Disponible sur: https://www.who.int/publications-detail-redirect/9789241550109 . Consulté le: 9 Juil 2021.
Forbes DA, et al. Gender differences in use and availability of home and community-based services for people with dementia. Can J Nurs Res. 2008;40(1):39–59.
PubMed Google Scholar
Hankivsky O. Women’s health, men’s health, and gender and health: implications of intersectionality. Soc Sci Med 1982. 2012;74(11):1712–20. https://doi.org/10.1016/j.socscimed.2011.11.029 .
Bähler C, Signorell A, Reich O. Health care utilisation and transitions between health care settings in the last 6 months of life in Switzerland. PloS One. 2016;11(9):e0160932. https://doi.org/10.1371/journal.pone.0160932 .
Teo WSK, Raj AG, Tan WS, Ng CWL, Heng BH, Leong IYO. Economic impact analysis of an end-of-life programme for nursing home residents. Palliat Med. 2014;28(5):430–7. https://doi.org/10.1177/0269216314526270 .
SPF, Surveillance de la grippe en Occitanie. Bilan de l’épidémie hivernale 2016–2017. Disponible sur: https://www.santepubliquefrance.fr/occitanie2/surveillance-de-la-grippe-en-occitanie.-bilan-de-l-epidemie-hivernale-2016-2017 . Consulté le: 27 Mars 2024.
Ouslander JG, Bonner A, Herndon L, Shutes J. The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc. 2014;15(3):162–70. https://doi.org/10.1016/j.jamda.2013.12.005 .
Rantz MJ, et al. Better care, better quality: reducing avoidable hospitalizations of nursing home residents. J Nurs Care Qual. 2015;30(4):290–7. https://doi.org/10.1097/NCQ.0000000000000145 .
Manckoundia P, et al. Inappropriate admissions of Ehpad residents to emergency departments. Soins Gerontol. 2023;28(159):42–5. https://doi.org/10.1016/j.sger.2022.12.013 .
Drummond MF. Experimental versus observational data in the economic evaluation of pharmaceuticals. Med Decis Making. 1998;18(2_suppl):S12–8. https://doi.org/10.1177/0272989X98018002S03 .
Drummond MF, Davies L. Economic analysis alongside clinical trials. Revisiting the methodological issues. Int J Technol Assess Health Care. 1991;7(4):561–73. https://doi.org/10.1017/s0266462300007121 .
Del Mar C, Hoffmann TC. A guide to performing a peer review of randomised controlled trials. BMC Med. 2015;13(1):248. https://doi.org/10.1186/s12916-015-0471-8 .
DICOM_Anne.G et DICOM_Anne.G, La politique du médicament en EHPAD, Ministère des Solidarités et de la Santé. Disponible sur: https://solidarites-sante.gouv.fr/ministere/documentation-et-publications-officielles/rapports/personnes-agees/article/la-politique-du-medicament-en-ehpad . Consulté le: 9 Juil 2021.
Costa N, et al. Comparison of informal care time and costs in different age-related dementias: a review. BioMed Res Int. 2013;2013:852368. https://doi.org/10.1155/2013/852368 .
Download references
Acknowledgements
This study is a part of a doctoral thesis published in university repositories:
- GOMBAULT DATZENKO E., Evaluation de l’impact économique des transferts aux urgences des résidents en EHPAD, 02 Octobre 2020 -> http://thesesante.ups-tlse.fr/3080/1/2020TOU31610.pdf
The authors thank the Midi-Pyrenees Regional Direction of Medical Service, the Midi-Pyrenees Regional Health Agency and the Research and Innovation Direction of the Toulouse University Hospital. They also thank all the geriatrician investigators, emergency physicians, and clinical research associates who participated to this research: Albi Hospital Center (W. Bouzid PhD, S. Laborie MD, J. Meunier MD); Auch Hospital Center (M. Camallières MD, V. Sarda MD); Ariège Couserans Hospital Center (F. Castéra MD, F. Del Mazo MD, S.Vidou); Bigorre Hospital Center (A. Batas, S. Benech MD, F. Huchet MD, Y. Gasnier MD, C. Périssé); Cahors Hospital Center (V. Kostek MD, C. Quénec’hdu, M. Oberlin MD); Castelsarrasin Moissac Hospital Center (M. Bersou MD, L. Brignol MD); Castres-Mazamet Hospital Center (N. Boulogne, MN. Cufi MD, N. Lagoutte MD); Jean Coulon Hospital Center (A. Hustache MD, J. Mac MD); Lannemezan Hospital Center (S. Bordes MD, L. Dugas MD); Lavaur Hospital Center (C. Blatge MD, C. Lapasse, A. Sebbane MD); Lourdes Hospital Center (S. Cottin MD, M. Péré-Saun MD); Montauban Hospital Center (C. Iché MD, N. Lafarge, V. Régniez, A. Roustan MD); Rodez Hospital Center (D. Kaya-Vaur MD, A. Pereira MD); Saint Gaudens Hospital Center (E. Deweerdt MD, P. Montastier MD); Toulouse University Hospital Center (S. Fernandez MD, A. Lendrieux, E. Paez, D. Pennetier PhD); Val d’Ariège Hospital Center (L. Bories MD, ES. Friederich MD, Y. Herades). They also thank all the nursing home professionals who contributed to this study.
This study was supported by a grant from the French Ministry of Health (Programme de recherche sur la performance du système de soins; PREPS 2014, 14–0185).
Author information
Authors and affiliations.
Present address: Department of Medical Information (DIM), Toulouse University Hospital, 2 rue Viguerie, Toulouse Cedex 9, 31059, France
E. Gombault-Datzenko, N. Costa, M. Mounié & L. Molinier
INSERM, UMR 1295, Toulouse, France
N. Costa, M. Mounié, E. Berard, Y. Rolland & L. Molinier
Gérontopôle, Toulouse University Hospital, Toulouse, France
N. Tavassoli, C. Mathieu & Y. Rolland
CREAI-ORS Occitanie, Toulouse, France
CNAM, DRSM Occitanie, 2 rue Georges Vivent, Toulouse, 31082, France
MSA Midi-Pyrénées Nord, 180 Avenue Marcel Unal, Montauban, 82000, France
J. M. Lagarrigue
Department of Epidemiology, University Hospital of Toulouse, 37 Allées Jules Guesde, Toulouse, 31000, France
You can also search for this author in PubMed Google Scholar
Contributions
EGD analyzed and interpreted data, and wrote the manuscript. NC was the major contributor for interpretation of data and have revised this work. NT, CM and EB participated to the conception and design of the work. MM analyzed data. HR and JML participated to the acquisition of data. YR and LM have substantively revised this work. All authors read and approved the final manuscript.
Corresponding author
Correspondence to E. Gombault-Datzenko .
Ethics declarations
Ethics approval and consent to participate.
This study has obtained approval from the ethics committee, the “Committee for the Protection of Persons and Competent Authority” (CPP) of Bordeaux (SOOM III, 29 may 2015) and it conforms to the provisions of the Declaration of Helsinki (as revised in Tokyo 2004). All patient’s informed consent have been obtained and their anonymity was preserved.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gombault-Datzenko, E., Costa, N., Mounié, M. et al. Cost of care pathways before and after appropriate and inappropriate transfers to the emergency department among nursing home residents: results from the FINE study. BMC Geriatr 24 , 353 (2024). https://doi.org/10.1186/s12877-024-04946-x
Download citation
Received : 04 July 2023
Accepted : 03 April 2024
Published : 19 April 2024
DOI : https://doi.org/10.1186/s12877-024-04946-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Long-term care unit
- Transfer to emergency department
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]

COMMENTS
PREOPERATIVE ASSESSMENT Case Study _____ GOALS: The goals of this learning activity seek to establish the need for preoperative nursing assessment, evaluation of chart review and considerations for plan of care and information sharing with surgical team members to ensure safe, quality surgical care and outcomes. LEARNING OBJECTIVES: 1.
This study suggests that the nursing preoperative assessment can be useful in identifying and defining patients' risk factors not just for surgery, but for the entire perioperative care trajectory. ... than later." "It allows nursing to see the red flags early and reach out to establish resources like nutrition and case management ...
Variables influencing patient satisfaction with preoperative nursing care Hospital and nurse-related variables. Among the participants, a substantial majority (84.8%) were admitted to the surgical unit of the hospital, highlighting the prevalence of surgical cases in the study sample.
Background. Preoperative care encompasses the provisions given prior to surgery, wherein the patient's unique requirements are considered to undertake physical and psychological preparations in anticipation of the procedure [].This phase commences upon the patient's admission to the hospital or surgical facility and extends until the commencement of the actual procedure [1-4].
org/perioperative-unfolding-case-study/. 6. Cronenwett L, Sherwood G, Barnsteiner J, et al. Quality and Safety Education for Nurses. Nurs Outlook. 2007;55(3):122-131. 7. International Nursing Association f or Clinical Simulation and Learning. INACSL standards of best practice: simulationSM Simulation design. Clin Sim Nurs. 2016;12:S5-S12. 8.
Presurgical evaluations are an important component of perioperative services but also pose challenges for nurse practitioners (NPs) in primary care regarding disease optimization, interdisciplinary communication, knowledge of surgical risk, and potential for surgical delays. The complexities of comorbid conditions, advancements in surgical procedures, and nuances of pharmacologic therapy ...
Abstract. The study describes basic nursing care during the perioperative. Introduces the origins of perioperative nursing, general care that must be practiced with patient in this context. During the preoperative, care related with risk assessment and preparation of patient from the emotional and physical point of view are important.
The data provided seven main tasks of a preoperative nurse, tools to support preoperative nursing and outcomes of structured preoperative nursing care. Conclusion. A preoperative nurse is a specialised coordinator of patient care, and the main purposes of this role are to meet the patient's and the family's needs individually and to prepare ...
Perioperative nursing unfolding case study is an article published in Nurse Educator, a journal that provides practical information and research on innovative teaching and learning strategies. The article presents a realistic scenario of a patient undergoing surgery and the role of the perioperative nurse in providing quality care. The article also includes learning objectives, discussion ...
The purpose of pre-operative evaluation is to reduce the morbidity of surgery, increase quality of intraoperative care, reduce costs associated with surgery, and return the patient to optimal functioning as soon as possible. Psychological Assessment. Psychological nursing assessment during the preoperative period: Fear of the unknown; Fear of death
picture. With the use of current tools for preoperative risk stratification it is possible to make a less subjective assessment. In the case study mentioned above the risks were fully elucidated to the patient; this also helped the care team's decision to cancel surgery as the patient was, at this point, unlikely to proceed with surgery.
Unfolding case studies present the opportunity for learners to develop and improve their critical thinking and problem-solving skills to deliver safe patient care. The structure of an unfolding case study actively engages learners to determine and customize nursing care based on the patient's changing situation. In addition, this type of case ...
The Perioperative Unfolding Case Study can be used for classroom or lab experiences. It follows a patient through the preoperative, intraoperative, and postoperative setting, allowing learners to gather information and react to changing situations. Theory bursts throughout the unfolding case, provide perioperative content that learners need to ...
Thoracic pre-operative assessment. The thoracic multidisciplinary team hold a weekly 'complex case review meeting' to plan the most appropriate care for high risk patients. Discussion covers the type of surgery required, the patient's pre-op review and investigations. Morbidity scoring systems are completed.
Study with Quizlet and memorize flashcards containing terms like The nurse begins the preoperative assessment by taking Ms. Jackson's vital signs. 1. Which vital sign requires follow-up by the nurse? A) BP of 160/88. B) Pulse of 68. C) Respirations of 14. D) Temperature of 97.2° F., The nurse reviews the medications taken by Ms. Jackson. Ms. Jackson states she has been taking two medications ...
Recovery nurses care for patients post surgery prior to transfer out of the theatre (NHS Careers, 2017). The role of the perioperative nurse has been explored in relatively few studies (McGarvey et al., 2000; Mitchell and Flin, 2008) and, in common with nursing more widely, lacks clear definition. Bjorn and Lindberg Bostrom (2008) and Schreiber ...
This article provides clinical guidance on the care of a patient undergoing an elective surgical procedure. It discusses preoperative care and the preparation of the patient. It aims to provide an awareness of the complications associated with perioperative care. Through the use of a patient case study, the authors demonstrate the care required ...
Perioperative nursing care requires unique specialty knowledge, skills, and abilities. ... We provide an overview of the initiatives affecting nursing education, followed by a case study example and a guide to assist educators with incorporating perioperative case studies into their education plans. These resources may enhance the integration ...
Effect of screen-based computer simulation on knowledge and skill in nursing students' learning of preoperative and postoperative care management: A randomized controlled study Computers, Informatics, Nursing , 30 ( 4 ) ( 2012 ) , pp. 196 - 203 , 10.1097/NCN.0b013e3182419134
The wide-awake local anesthesia technique in hand surgery is widely used, but there are currently no guidelines or protocols for the number of operating room personnel required to optimize patient safety intraoperatively. This study aimed to evaluate perioperative complication rates of wide-awake local anesthesia hand surgeries performed at surgery centers that used different numbers of ...
Pre-Operative Nursing Assessment. Nurse Casey uses Level 0 of the Clinical Judgment Measurement Model, or CJMM, to define the context of Jose's clinical situation as a pre-op patient. She also ...
In this case study, a substitute decision-maker was available and willing to take on the responsibility for the decision regarding Elsie's medical care - without the informed consent obtained from Wally, Elsie's surgical procedure could not have proceeded. All members of the health care team have valuable information about the patient to ...
Study with Quizlet and memorize flashcards containing terms like Meet the Client: Helen JacksonHelen Jackson, a 63-year-old Caucasian female, arrives at the surgery center for her preoperative appointment. She is scheduled to undergo left hip replacement surgery in 1 week. The nurse begins the preoperative assessment by taking Ms. Jackson's vital signs. The nurse reviews the medications taken ...
Maps depict May 24, 2020 (during first wave and after mandatory case and death reporting in nursing homes begins), January 12, 2021 (Alpha and Delta variants), and January 16, 2022 (Omicron variant). On the maps, the number of COVID-19 policies is indicated by a color gradient, ranging from the least (light gray color) to the most (darker blue ...
Transfers of nursing home (NH) residents to the emergency department (ED) is frequent. Our main objective was to assess the cost of care pathways 6 months before and after the transfer to the emergency department among NH residents, according to the type of transfer (i.e. appropriate or inappropriate). This was a part of an observational, multicenter, case-control study: the Factors associated ...