- Open access
- Published: 27 June 2011

The case study approach
- Sarah Crowe 1 ,
- Kathrin Cresswell 2 ,
- Ann Robertson 2 ,
- Guro Huby 3 ,
- Anthony Avery 1 &
- Aziz Sheikh 2
BMC Medical Research Methodology volume 11 , Article number: 100 ( 2011 ) Cite this article
766k Accesses
1031 Citations
37 Altmetric
Metrics details
The case study approach allows in-depth, multi-faceted explorations of complex issues in their real-life settings. The value of the case study approach is well recognised in the fields of business, law and policy, but somewhat less so in health services research. Based on our experiences of conducting several health-related case studies, we reflect on the different types of case study design, the specific research questions this approach can help answer, the data sources that tend to be used, and the particular advantages and disadvantages of employing this methodological approach. The paper concludes with key pointers to aid those designing and appraising proposals for conducting case study research, and a checklist to help readers assess the quality of case study reports.
Peer Review reports
Introduction
The case study approach is particularly useful to employ when there is a need to obtain an in-depth appreciation of an issue, event or phenomenon of interest, in its natural real-life context. Our aim in writing this piece is to provide insights into when to consider employing this approach and an overview of key methodological considerations in relation to the design, planning, analysis, interpretation and reporting of case studies.
The illustrative 'grand round', 'case report' and 'case series' have a long tradition in clinical practice and research. Presenting detailed critiques, typically of one or more patients, aims to provide insights into aspects of the clinical case and, in doing so, illustrate broader lessons that may be learnt. In research, the conceptually-related case study approach can be used, for example, to describe in detail a patient's episode of care, explore professional attitudes to and experiences of a new policy initiative or service development or more generally to 'investigate contemporary phenomena within its real-life context' [ 1 ]. Based on our experiences of conducting a range of case studies, we reflect on when to consider using this approach, discuss the key steps involved and illustrate, with examples, some of the practical challenges of attaining an in-depth understanding of a 'case' as an integrated whole. In keeping with previously published work, we acknowledge the importance of theory to underpin the design, selection, conduct and interpretation of case studies[ 2 ]. In so doing, we make passing reference to the different epistemological approaches used in case study research by key theoreticians and methodologists in this field of enquiry.
This paper is structured around the following main questions: What is a case study? What are case studies used for? How are case studies conducted? What are the potential pitfalls and how can these be avoided? We draw in particular on four of our own recently published examples of case studies (see Tables 1 , 2 , 3 and 4 ) and those of others to illustrate our discussion[ 3 – 7 ].
What is a case study?
A case study is a research approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context. It is an established research design that is used extensively in a wide variety of disciplines, particularly in the social sciences. A case study can be defined in a variety of ways (Table 5 ), the central tenet being the need to explore an event or phenomenon in depth and in its natural context. It is for this reason sometimes referred to as a "naturalistic" design; this is in contrast to an "experimental" design (such as a randomised controlled trial) in which the investigator seeks to exert control over and manipulate the variable(s) of interest.
Stake's work has been particularly influential in defining the case study approach to scientific enquiry. He has helpfully characterised three main types of case study: intrinsic , instrumental and collective [ 8 ]. An intrinsic case study is typically undertaken to learn about a unique phenomenon. The researcher should define the uniqueness of the phenomenon, which distinguishes it from all others. In contrast, the instrumental case study uses a particular case (some of which may be better than others) to gain a broader appreciation of an issue or phenomenon. The collective case study involves studying multiple cases simultaneously or sequentially in an attempt to generate a still broader appreciation of a particular issue.
These are however not necessarily mutually exclusive categories. In the first of our examples (Table 1 ), we undertook an intrinsic case study to investigate the issue of recruitment of minority ethnic people into the specific context of asthma research studies, but it developed into a instrumental case study through seeking to understand the issue of recruitment of these marginalised populations more generally, generating a number of the findings that are potentially transferable to other disease contexts[ 3 ]. In contrast, the other three examples (see Tables 2 , 3 and 4 ) employed collective case study designs to study the introduction of workforce reconfiguration in primary care, the implementation of electronic health records into hospitals, and to understand the ways in which healthcare students learn about patient safety considerations[ 4 – 6 ]. Although our study focusing on the introduction of General Practitioners with Specialist Interests (Table 2 ) was explicitly collective in design (four contrasting primary care organisations were studied), is was also instrumental in that this particular professional group was studied as an exemplar of the more general phenomenon of workforce redesign[ 4 ].
What are case studies used for?
According to Yin, case studies can be used to explain, describe or explore events or phenomena in the everyday contexts in which they occur[ 1 ]. These can, for example, help to understand and explain causal links and pathways resulting from a new policy initiative or service development (see Tables 2 and 3 , for example)[ 1 ]. In contrast to experimental designs, which seek to test a specific hypothesis through deliberately manipulating the environment (like, for example, in a randomised controlled trial giving a new drug to randomly selected individuals and then comparing outcomes with controls),[ 9 ] the case study approach lends itself well to capturing information on more explanatory ' how ', 'what' and ' why ' questions, such as ' how is the intervention being implemented and received on the ground?'. The case study approach can offer additional insights into what gaps exist in its delivery or why one implementation strategy might be chosen over another. This in turn can help develop or refine theory, as shown in our study of the teaching of patient safety in undergraduate curricula (Table 4 )[ 6 , 10 ]. Key questions to consider when selecting the most appropriate study design are whether it is desirable or indeed possible to undertake a formal experimental investigation in which individuals and/or organisations are allocated to an intervention or control arm? Or whether the wish is to obtain a more naturalistic understanding of an issue? The former is ideally studied using a controlled experimental design, whereas the latter is more appropriately studied using a case study design.
Case studies may be approached in different ways depending on the epistemological standpoint of the researcher, that is, whether they take a critical (questioning one's own and others' assumptions), interpretivist (trying to understand individual and shared social meanings) or positivist approach (orientating towards the criteria of natural sciences, such as focusing on generalisability considerations) (Table 6 ). Whilst such a schema can be conceptually helpful, it may be appropriate to draw on more than one approach in any case study, particularly in the context of conducting health services research. Doolin has, for example, noted that in the context of undertaking interpretative case studies, researchers can usefully draw on a critical, reflective perspective which seeks to take into account the wider social and political environment that has shaped the case[ 11 ].
How are case studies conducted?
Here, we focus on the main stages of research activity when planning and undertaking a case study; the crucial stages are: defining the case; selecting the case(s); collecting and analysing the data; interpreting data; and reporting the findings.
Defining the case
Carefully formulated research question(s), informed by the existing literature and a prior appreciation of the theoretical issues and setting(s), are all important in appropriately and succinctly defining the case[ 8 , 12 ]. Crucially, each case should have a pre-defined boundary which clarifies the nature and time period covered by the case study (i.e. its scope, beginning and end), the relevant social group, organisation or geographical area of interest to the investigator, the types of evidence to be collected, and the priorities for data collection and analysis (see Table 7 )[ 1 ]. A theory driven approach to defining the case may help generate knowledge that is potentially transferable to a range of clinical contexts and behaviours; using theory is also likely to result in a more informed appreciation of, for example, how and why interventions have succeeded or failed[ 13 ].
For example, in our evaluation of the introduction of electronic health records in English hospitals (Table 3 ), we defined our cases as the NHS Trusts that were receiving the new technology[ 5 ]. Our focus was on how the technology was being implemented. However, if the primary research interest had been on the social and organisational dimensions of implementation, we might have defined our case differently as a grouping of healthcare professionals (e.g. doctors and/or nurses). The precise beginning and end of the case may however prove difficult to define. Pursuing this same example, when does the process of implementation and adoption of an electronic health record system really begin or end? Such judgements will inevitably be influenced by a range of factors, including the research question, theory of interest, the scope and richness of the gathered data and the resources available to the research team.
Selecting the case(s)
The decision on how to select the case(s) to study is a very important one that merits some reflection. In an intrinsic case study, the case is selected on its own merits[ 8 ]. The case is selected not because it is representative of other cases, but because of its uniqueness, which is of genuine interest to the researchers. This was, for example, the case in our study of the recruitment of minority ethnic participants into asthma research (Table 1 ) as our earlier work had demonstrated the marginalisation of minority ethnic people with asthma, despite evidence of disproportionate asthma morbidity[ 14 , 15 ]. In another example of an intrinsic case study, Hellstrom et al.[ 16 ] studied an elderly married couple living with dementia to explore how dementia had impacted on their understanding of home, their everyday life and their relationships.
For an instrumental case study, selecting a "typical" case can work well[ 8 ]. In contrast to the intrinsic case study, the particular case which is chosen is of less importance than selecting a case that allows the researcher to investigate an issue or phenomenon. For example, in order to gain an understanding of doctors' responses to health policy initiatives, Som undertook an instrumental case study interviewing clinicians who had a range of responsibilities for clinical governance in one NHS acute hospital trust[ 17 ]. Sampling a "deviant" or "atypical" case may however prove even more informative, potentially enabling the researcher to identify causal processes, generate hypotheses and develop theory.
In collective or multiple case studies, a number of cases are carefully selected. This offers the advantage of allowing comparisons to be made across several cases and/or replication. Choosing a "typical" case may enable the findings to be generalised to theory (i.e. analytical generalisation) or to test theory by replicating the findings in a second or even a third case (i.e. replication logic)[ 1 ]. Yin suggests two or three literal replications (i.e. predicting similar results) if the theory is straightforward and five or more if the theory is more subtle. However, critics might argue that selecting 'cases' in this way is insufficiently reflexive and ill-suited to the complexities of contemporary healthcare organisations.
The selected case study site(s) should allow the research team access to the group of individuals, the organisation, the processes or whatever else constitutes the chosen unit of analysis for the study. Access is therefore a central consideration; the researcher needs to come to know the case study site(s) well and to work cooperatively with them. Selected cases need to be not only interesting but also hospitable to the inquiry [ 8 ] if they are to be informative and answer the research question(s). Case study sites may also be pre-selected for the researcher, with decisions being influenced by key stakeholders. For example, our selection of case study sites in the evaluation of the implementation and adoption of electronic health record systems (see Table 3 ) was heavily influenced by NHS Connecting for Health, the government agency that was responsible for overseeing the National Programme for Information Technology (NPfIT)[ 5 ]. This prominent stakeholder had already selected the NHS sites (through a competitive bidding process) to be early adopters of the electronic health record systems and had negotiated contracts that detailed the deployment timelines.
It is also important to consider in advance the likely burden and risks associated with participation for those who (or the site(s) which) comprise the case study. Of particular importance is the obligation for the researcher to think through the ethical implications of the study (e.g. the risk of inadvertently breaching anonymity or confidentiality) and to ensure that potential participants/participating sites are provided with sufficient information to make an informed choice about joining the study. The outcome of providing this information might be that the emotive burden associated with participation, or the organisational disruption associated with supporting the fieldwork, is considered so high that the individuals or sites decide against participation.
In our example of evaluating implementations of electronic health record systems, given the restricted number of early adopter sites available to us, we sought purposively to select a diverse range of implementation cases among those that were available[ 5 ]. We chose a mixture of teaching, non-teaching and Foundation Trust hospitals, and examples of each of the three electronic health record systems procured centrally by the NPfIT. At one recruited site, it quickly became apparent that access was problematic because of competing demands on that organisation. Recognising the importance of full access and co-operative working for generating rich data, the research team decided not to pursue work at that site and instead to focus on other recruited sites.
Collecting the data
In order to develop a thorough understanding of the case, the case study approach usually involves the collection of multiple sources of evidence, using a range of quantitative (e.g. questionnaires, audits and analysis of routinely collected healthcare data) and more commonly qualitative techniques (e.g. interviews, focus groups and observations). The use of multiple sources of data (data triangulation) has been advocated as a way of increasing the internal validity of a study (i.e. the extent to which the method is appropriate to answer the research question)[ 8 , 18 – 21 ]. An underlying assumption is that data collected in different ways should lead to similar conclusions, and approaching the same issue from different angles can help develop a holistic picture of the phenomenon (Table 2 )[ 4 ].
Brazier and colleagues used a mixed-methods case study approach to investigate the impact of a cancer care programme[ 22 ]. Here, quantitative measures were collected with questionnaires before, and five months after, the start of the intervention which did not yield any statistically significant results. Qualitative interviews with patients however helped provide an insight into potentially beneficial process-related aspects of the programme, such as greater, perceived patient involvement in care. The authors reported how this case study approach provided a number of contextual factors likely to influence the effectiveness of the intervention and which were not likely to have been obtained from quantitative methods alone.
In collective or multiple case studies, data collection needs to be flexible enough to allow a detailed description of each individual case to be developed (e.g. the nature of different cancer care programmes), before considering the emerging similarities and differences in cross-case comparisons (e.g. to explore why one programme is more effective than another). It is important that data sources from different cases are, where possible, broadly comparable for this purpose even though they may vary in nature and depth.
Analysing, interpreting and reporting case studies
Making sense and offering a coherent interpretation of the typically disparate sources of data (whether qualitative alone or together with quantitative) is far from straightforward. Repeated reviewing and sorting of the voluminous and detail-rich data are integral to the process of analysis. In collective case studies, it is helpful to analyse data relating to the individual component cases first, before making comparisons across cases. Attention needs to be paid to variations within each case and, where relevant, the relationship between different causes, effects and outcomes[ 23 ]. Data will need to be organised and coded to allow the key issues, both derived from the literature and emerging from the dataset, to be easily retrieved at a later stage. An initial coding frame can help capture these issues and can be applied systematically to the whole dataset with the aid of a qualitative data analysis software package.
The Framework approach is a practical approach, comprising of five stages (familiarisation; identifying a thematic framework; indexing; charting; mapping and interpretation) , to managing and analysing large datasets particularly if time is limited, as was the case in our study of recruitment of South Asians into asthma research (Table 1 )[ 3 , 24 ]. Theoretical frameworks may also play an important role in integrating different sources of data and examining emerging themes. For example, we drew on a socio-technical framework to help explain the connections between different elements - technology; people; and the organisational settings within which they worked - in our study of the introduction of electronic health record systems (Table 3 )[ 5 ]. Our study of patient safety in undergraduate curricula drew on an evaluation-based approach to design and analysis, which emphasised the importance of the academic, organisational and practice contexts through which students learn (Table 4 )[ 6 ].
Case study findings can have implications both for theory development and theory testing. They may establish, strengthen or weaken historical explanations of a case and, in certain circumstances, allow theoretical (as opposed to statistical) generalisation beyond the particular cases studied[ 12 ]. These theoretical lenses should not, however, constitute a strait-jacket and the cases should not be "forced to fit" the particular theoretical framework that is being employed.
When reporting findings, it is important to provide the reader with enough contextual information to understand the processes that were followed and how the conclusions were reached. In a collective case study, researchers may choose to present the findings from individual cases separately before amalgamating across cases. Care must be taken to ensure the anonymity of both case sites and individual participants (if agreed in advance) by allocating appropriate codes or withholding descriptors. In the example given in Table 3 , we decided against providing detailed information on the NHS sites and individual participants in order to avoid the risk of inadvertent disclosure of identities[ 5 , 25 ].
What are the potential pitfalls and how can these be avoided?
The case study approach is, as with all research, not without its limitations. When investigating the formal and informal ways undergraduate students learn about patient safety (Table 4 ), for example, we rapidly accumulated a large quantity of data. The volume of data, together with the time restrictions in place, impacted on the depth of analysis that was possible within the available resources. This highlights a more general point of the importance of avoiding the temptation to collect as much data as possible; adequate time also needs to be set aside for data analysis and interpretation of what are often highly complex datasets.
Case study research has sometimes been criticised for lacking scientific rigour and providing little basis for generalisation (i.e. producing findings that may be transferable to other settings)[ 1 ]. There are several ways to address these concerns, including: the use of theoretical sampling (i.e. drawing on a particular conceptual framework); respondent validation (i.e. participants checking emerging findings and the researcher's interpretation, and providing an opinion as to whether they feel these are accurate); and transparency throughout the research process (see Table 8 )[ 8 , 18 – 21 , 23 , 26 ]. Transparency can be achieved by describing in detail the steps involved in case selection, data collection, the reasons for the particular methods chosen, and the researcher's background and level of involvement (i.e. being explicit about how the researcher has influenced data collection and interpretation). Seeking potential, alternative explanations, and being explicit about how interpretations and conclusions were reached, help readers to judge the trustworthiness of the case study report. Stake provides a critique checklist for a case study report (Table 9 )[ 8 ].
Conclusions
The case study approach allows, amongst other things, critical events, interventions, policy developments and programme-based service reforms to be studied in detail in a real-life context. It should therefore be considered when an experimental design is either inappropriate to answer the research questions posed or impossible to undertake. Considering the frequency with which implementations of innovations are now taking place in healthcare settings and how well the case study approach lends itself to in-depth, complex health service research, we believe this approach should be more widely considered by researchers. Though inherently challenging, the research case study can, if carefully conceptualised and thoughtfully undertaken and reported, yield powerful insights into many important aspects of health and healthcare delivery.
Yin RK: Case study research, design and method. 2009, London: Sage Publications Ltd., 4
Google Scholar
Keen J, Packwood T: Qualitative research; case study evaluation. BMJ. 1995, 311: 444-446.
Article CAS PubMed PubMed Central Google Scholar
Sheikh A, Halani L, Bhopal R, Netuveli G, Partridge M, Car J, et al: Facilitating the Recruitment of Minority Ethnic People into Research: Qualitative Case Study of South Asians and Asthma. PLoS Med. 2009, 6 (10): 1-11.
Article Google Scholar
Pinnock H, Huby G, Powell A, Kielmann T, Price D, Williams S, et al: The process of planning, development and implementation of a General Practitioner with a Special Interest service in Primary Care Organisations in England and Wales: a comparative prospective case study. Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO). 2008, [ http://www.sdo.nihr.ac.uk/files/project/99-final-report.pdf ]
Robertson A, Cresswell K, Takian A, Petrakaki D, Crowe S, Cornford T, et al: Prospective evaluation of the implementation and adoption of NHS Connecting for Health's national electronic health record in secondary care in England: interim findings. BMJ. 2010, 41: c4564-
Pearson P, Steven A, Howe A, Sheikh A, Ashcroft D, Smith P, the Patient Safety Education Study Group: Learning about patient safety: organisational context and culture in the education of healthcare professionals. J Health Serv Res Policy. 2010, 15: 4-10. 10.1258/jhsrp.2009.009052.
Article PubMed Google Scholar
van Harten WH, Casparie TF, Fisscher OA: The evaluation of the introduction of a quality management system: a process-oriented case study in a large rehabilitation hospital. Health Policy. 2002, 60 (1): 17-37. 10.1016/S0168-8510(01)00187-7.
Stake RE: The art of case study research. 1995, London: Sage Publications Ltd.
Sheikh A, Smeeth L, Ashcroft R: Randomised controlled trials in primary care: scope and application. Br J Gen Pract. 2002, 52 (482): 746-51.
PubMed PubMed Central Google Scholar
King G, Keohane R, Verba S: Designing Social Inquiry. 1996, Princeton: Princeton University Press
Doolin B: Information technology as disciplinary technology: being critical in interpretative research on information systems. Journal of Information Technology. 1998, 13: 301-311. 10.1057/jit.1998.8.
George AL, Bennett A: Case studies and theory development in the social sciences. 2005, Cambridge, MA: MIT Press
Eccles M, the Improved Clinical Effectiveness through Behavioural Research Group (ICEBeRG): Designing theoretically-informed implementation interventions. Implementation Science. 2006, 1: 1-8. 10.1186/1748-5908-1-1.
Article PubMed Central Google Scholar
Netuveli G, Hurwitz B, Levy M, Fletcher M, Barnes G, Durham SR, Sheikh A: Ethnic variations in UK asthma frequency, morbidity, and health-service use: a systematic review and meta-analysis. Lancet. 2005, 365 (9456): 312-7.
Sheikh A, Panesar SS, Lasserson T, Netuveli G: Recruitment of ethnic minorities to asthma studies. Thorax. 2004, 59 (7): 634-
CAS PubMed PubMed Central Google Scholar
Hellström I, Nolan M, Lundh U: 'We do things together': A case study of 'couplehood' in dementia. Dementia. 2005, 4: 7-22. 10.1177/1471301205049188.
Som CV: Nothing seems to have changed, nothing seems to be changing and perhaps nothing will change in the NHS: doctors' response to clinical governance. International Journal of Public Sector Management. 2005, 18: 463-477. 10.1108/09513550510608903.
Lincoln Y, Guba E: Naturalistic inquiry. 1985, Newbury Park: Sage Publications
Barbour RS: Checklists for improving rigour in qualitative research: a case of the tail wagging the dog?. BMJ. 2001, 322: 1115-1117. 10.1136/bmj.322.7294.1115.
Mays N, Pope C: Qualitative research in health care: Assessing quality in qualitative research. BMJ. 2000, 320: 50-52. 10.1136/bmj.320.7226.50.
Mason J: Qualitative researching. 2002, London: Sage
Brazier A, Cooke K, Moravan V: Using Mixed Methods for Evaluating an Integrative Approach to Cancer Care: A Case Study. Integr Cancer Ther. 2008, 7: 5-17. 10.1177/1534735407313395.
Miles MB, Huberman M: Qualitative data analysis: an expanded sourcebook. 1994, CA: Sage Publications Inc., 2
Pope C, Ziebland S, Mays N: Analysing qualitative data. Qualitative research in health care. BMJ. 2000, 320: 114-116. 10.1136/bmj.320.7227.114.
Cresswell KM, Worth A, Sheikh A: Actor-Network Theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inform Decis Mak. 2010, 10 (1): 67-10.1186/1472-6947-10-67.
Article PubMed PubMed Central Google Scholar
Malterud K: Qualitative research: standards, challenges, and guidelines. Lancet. 2001, 358: 483-488. 10.1016/S0140-6736(01)05627-6.
Article CAS PubMed Google Scholar
Yin R: Case study research: design and methods. 1994, Thousand Oaks, CA: Sage Publishing, 2
Yin R: Enhancing the quality of case studies in health services research. Health Serv Res. 1999, 34: 1209-1224.
Green J, Thorogood N: Qualitative methods for health research. 2009, Los Angeles: Sage, 2
Howcroft D, Trauth E: Handbook of Critical Information Systems Research, Theory and Application. 2005, Cheltenham, UK: Northampton, MA, USA: Edward Elgar
Book Google Scholar
Blakie N: Approaches to Social Enquiry. 1993, Cambridge: Polity Press
Doolin B: Power and resistance in the implementation of a medical management information system. Info Systems J. 2004, 14: 343-362. 10.1111/j.1365-2575.2004.00176.x.
Bloomfield BP, Best A: Management consultants: systems development, power and the translation of problems. Sociological Review. 1992, 40: 533-560.
Shanks G, Parr A: Positivist, single case study research in information systems: A critical analysis. Proceedings of the European Conference on Information Systems. 2003, Naples
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2288/11/100/prepub
Download references
Acknowledgements
We are grateful to the participants and colleagues who contributed to the individual case studies that we have drawn on. This work received no direct funding, but it has been informed by projects funded by Asthma UK, the NHS Service Delivery Organisation, NHS Connecting for Health Evaluation Programme, and Patient Safety Research Portfolio. We would also like to thank the expert reviewers for their insightful and constructive feedback. Our thanks are also due to Dr. Allison Worth who commented on an earlier draft of this manuscript.
Author information
Authors and affiliations.
Division of Primary Care, The University of Nottingham, Nottingham, UK
Sarah Crowe & Anthony Avery
Centre for Population Health Sciences, The University of Edinburgh, Edinburgh, UK
Kathrin Cresswell, Ann Robertson & Aziz Sheikh
School of Health in Social Science, The University of Edinburgh, Edinburgh, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sarah Crowe .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
AS conceived this article. SC, KC and AR wrote this paper with GH, AA and AS all commenting on various drafts. SC and AS are guarantors.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Crowe, S., Cresswell, K., Robertson, A. et al. The case study approach. BMC Med Res Methodol 11 , 100 (2011). https://doi.org/10.1186/1471-2288-11-100
Download citation
Received : 29 November 2010
Accepted : 27 June 2011
Published : 27 June 2011
DOI : https://doi.org/10.1186/1471-2288-11-100
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Case Study Approach
- Electronic Health Record System
- Case Study Design
- Case Study Site
- Case Study Report
BMC Medical Research Methodology
ISSN: 1471-2288
- General enquiries: [email protected]

Patients’ Lived Experiences During the Transplant and Cellular Therapy Journey pp 9–17 Cite as
Creating a Patient-Centered Case Study
- Jennifer Holl 5 ,
- Lisa Wesinger 6 ,
- Judi Gentes 7 ,
- Carissa Morton 8 &
- Jean Coffey 9
- First Online: 25 August 2023
65 Accesses
Case studies provide an invaluable record of professional clinical practice and have been used in medicine since the late 1800s to describe both traditional and unusual presentations of specific disease pathologies. In medicine, case studies traditionally take a detached, objective approach to outlining the clinical course of a disease and its treatment. In keeping with the holistic approach to patient care found in nursing and using the theoretical foundations established in Jean Watson’s Theory of Human Caring as well as the Relationship-Based Care Model, this research team sought to revolutionize the case study paradigm and deconstruct the traditional case study approach, placing the patient, instead of the provider, at the center of the narrative. This new case study method intercalates the clinicians’ analysis of the case with the patient’s commentary. This chapter outlines the methods and theoretical underpinnings used to create a patient-centered case study and seeks to provide nurses with a creative alternative to the traditional, objective case study approach. Implications for future research include whether using patient-centered case studies, instead of traditional case studies, provide a valuable learning tool to educate nurses.
- Qualitative research
- Phenomenology
- Relationship-based care
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Bergen A, While A. A case for case studies: exploring the use of case study design in community nursing research. J Adv Nurs. 2000;31(4):926–34.
Article CAS PubMed Google Scholar
Benner P. Interpretive phenomenology. Thousand Oaks: Sage Publications; 1994.
Google Scholar
Gary JC, Hudson CE. Reverse engineering: strategy to teach evidence-based practice to online RN-to-BSN students. Nurse Educ. 2016;41(2):83–5.
Article PubMed Google Scholar
Koloroutis M, editor. Relationship-based care: a model for transforming practice. Minneapolis: Creative Health Care Management; 2004.
Luck L, Jackson D, Usher K. Case study: a bridge across the paradigms. Nurs Inq. 2006;13(2):103–9.
Meyer CB. A case in case study methodology. Field Methods. 2001;13:329–52.
Article Google Scholar
Noble H, Smith J. Issues of validity and reliability in qualitative research. Evid Based Nurs. 2015;18(2):34–5. https://doi.org/10.1136/eb-2015-102054 .
Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2014.
Smith J, Flowers P, Larkin M. Interpretative phenomenological analysis: theory, method and research. London: Sage; 2013.
Taylor R, Thomas-Gregory A. Case study research. Nurs Stand. 2015;29(41):36–40.
Watson J. Nursing: the philosophy and science of caring. Rev. ed. Boulder: University Press of Colorado; 2008.
Yin RK. Case study research: design and methods. 5th ed. Thousand Oaks: Sage Publications; 2014.
Download references
Author information
Authors and affiliations.
Hematology/Oncology, Dartmouth Health, Lebanon, NH, USA
Jennifer Holl
Transplant and Cellular Therapy, Dartmouth Health, Lebanon, NH, USA
Lisa Wesinger
Oncology/Hematology, Dartmouth Health, Lebanon, NH, USA
Judi Gentes
Dartmouth Health, Dartmouth Cancer Center, St. Johnsbury, VT, USA
Carissa Morton
School of Nursing, University of Connecticut, Storrs, CT, USA
Jean Coffey
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jean Coffey .
Editor information
Editors and affiliations.
Dartmouth Health, Dartmouth–Hitchcock Medical Center, Lebanon, NH, USA
John M. Hill Jr.
School Nursing, University of Connecticut, Storrs, CT, USA
Thomas Long
Elizabeth B. McGrath
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Holl, J., Wesinger, L., Gentes, J., Morton, C., Coffey, J. (2023). Creating a Patient-Centered Case Study. In: Coffey, J., Hill Jr., J.M., Long, T., McGrath, E.B. (eds) Patients’ Lived Experiences During the Transplant and Cellular Therapy Journey. Springer, Cham. https://doi.org/10.1007/978-3-031-25602-8_2
Download citation
DOI : https://doi.org/10.1007/978-3-031-25602-8_2
Published : 25 August 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-25601-1
Online ISBN : 978-3-031-25602-8
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Call for Papers
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 7, Issue 2
- Fundamentals of case study research in family medicine and community health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1141-7613 Sergi Fàbregues 1 and
- Michael D Fetters 2
- 1 Department of Psychology and Education , Universitat Oberta de Catalunya , Barcelona , Spain
- 2 Department of Family Medicine , University of Michigan , Ann Arbor , Michigan , USA
- Correspondence to Dr Sergi Fàbregues, Department of Psychology and Education, Universitat Oberta de Catalunya, Rambla del Poblenou, 156, 08018, Barcelona, Spain; sfabreguesf{at}uoc.edu
The aim of this article is to introduce family medicine researchers to case study research, a rigorous research methodology commonly used in the social and health sciences and only distantly related to clinical case reports. The article begins with an overview of case study in the social and health sciences, including its definition, potential applications, historical background and core features. This is followed by a 10-step description of the process of conducting a case study project illustrated using a case study conducted about a teaching programme executed to teach international family medicine resident learners sensitive examination skills. Steps for conducting a case study include (1) conducting a literature review; (2) formulating the research questions; (3) ensuring that a case study is appropriate; (4) determining the type of case study design; (5) defining boundaries of the case(s) and selecting the case(s); (6) preparing for data collection; (7) collecting and organising the data; (8) analysing the data; (9) writing the case study report; and (10) appraising the quality. Case study research is a highly flexible and powerful research tool available to family medicine researchers for a variety of applications.
- Case study research
- research design
- mixed methods
- family practice
- primary care
- general practice
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0
https://doi.org/10.1136/fmch-2018-000074
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Significance statement
Given their potential for answering ‘how’ and ‘why’ questions about complex issues in their natural setting, case study designs are being increasingly used in the health sciences. Conducting a case study can, however, be a complex task because of the possibility of combining multiple methods and the need to choose between different types of case study designs. In order to introduce family medicine and community health researchers to the fundamentals of case study research, this article reviews its definition, potential applications, historical background and main characteristics. It follows on with a practical, step-by-step description of the case study process that will be useful to researchers interested in implementing this research design in their own practice.
Introduction
This article provides family medicine and community health researchers a concise resource to conduct case study research. The article opens with an overview of case study in the social and health sciences, including its definition, potential applications, historical background and core features. This is followed by a 10-step description of the process of conducting a case study project, as described in the literature. These steps are illustrated using a case study about a teaching programme executed to teach international medical learners sensitive examination skills. The article ends with recommendations of useful articles and textbooks on case study research.
Origins of case study research
Case study is a research design that involves an intensive and holistic examination of a contemporary phenomenon in a real-life setting. 1–3 It uses a variety of methods and multiple data sources to explore, describe or explain a single case bounded in time and place (ie, an event, individual, group, organisation or programme). A distinctive feature of case study is its focus on the particular characteristics of the case being studied and the contextual aspects, relationships and processes influencing it. 4 Here we do not include clinical case reports as these are beyond the scope of this article. While distantly related to clinical case reports commonly used to report unusual clinical case presentations or findings, case study is a research approach that is frequently used in the social sciences and health sciences. In contrast to other research designs, such as surveys or experiments, a key strength of case study is that it allows the researcher to adopt a holistic approach—rather than an isolated approach—to the study of social phenomena. As argued by Yin, 3 case studies are particularly suitable for answering ‘how’ research questions (ie, how a treatment was received) as well as ‘why’ research questions (ie, why the treatment produced the observed outcomes).
Given its potential for understanding complex processes as they occur in their natural setting, case study increasingly is used in a wide range of health-related disciplines and fields, including medicine, 5 nursing, 6 health services research 1 and health communication. 7 With regard to clinical practice and research, a number of authors 1 5 8 have highlighted how insights gained from case study designs can be used to describe patients’ experiences regarding care, explore health professionals’ perceptions regarding a policy change, and understand why medical treatments and complex interventions succeed or fail.
In anthropology and sociology, case study as a research design was introduced as a response to the prevailing view of quantitative research as the primary way of undertaking research. 9 From its beginnings, social scientists saw case study as a method to obtain comprehensive accounts of social phenomena from participants. In addition, it could complement the findings of survey research. Between the 1920s and 1960s, case study became the predominant research approach among the members of the Department of Sociology of the University of Chicago, widely known as ‘The Chicago School’. 10 11 During this period, prominent sociologists, such as Florian Znaniecki, William Thomas, Everett C Hughes and Howard S Becker, undertook a series of innovative case studies (including classical works such as The Polish peasant in Europe and America or Boys in White ), which laid the foundations of case study designs as implemented today.
In the 1970s, case study increasingly was adopted in the USA and UK in applied disciplines and fields, such as education, programme evaluation and public policy research. 12 As a response to the limitations of quasi-experimental designs for undertaking comprehensive programme evaluations, researchers in these disciplines saw in case studies—either alone or in combination with experimental designs—an opportunity to gain additional insights into the outcomes of programme implementation. In the mid-1980s and early 1990s, the case study approach became recognised as having its own ‘logic of design’ (p46). 13 This period coincides with the publication of a considerable number of influential articles 14–16 and textbooks 4 17 18 on case study research.
These publications were instrumental in shaping contemporary case study practice, yet they reflected divergent views about the nature of case study, including how it should be defined, designed and implemented (see Yazan 19 for a comparison of the perspectives of Yin, Merriam and Stake, three leading case study methodologists). What these publications have in common is that case study revolves around four key features.
First, case study examines a specific phenomenon in detail by performing an indepth and intensive analysis of the selected case. The rationale for case study designs, rather than more expansive designs such as surveys, is that the researcher is interested in investigating the particularity of a case, that is, the unique attributes that define an event, individual, group, organisation or programme. 2 Second, case study is conducted in natural settings where people meet, interact and change their perceptions over time. The use of the case study design is a choice in favour of ‘maintaining the naturalness of the research situation and the natural course of events’ (p177). 20
Third, case study assumes that a case under investigation is entangled with the context in which it is embedded. This context entails a number of interconnected processes that cannot be disassociated from the case, but rather are part of the study. The case study researcher is interested in understanding how and why such processes take place and, consequently, uncovering the interactions between a case and its context. Research questions concerning how and why phenomena occur are particularly appropriate in case study research. 3
Fourth, case study encourages the researcher to use a variety of methods and data types in a single study. 20 21 These can be solely qualitative, solely quantitative or a mixture of both. The latter option allows the researcher to gain a more comprehensive understanding of the case and improve the accuracy of the findings. The four above-mentioned key features of case study are shown in table 1 , using the example of a mixed methods case study evaluation. 22
- View inline
Key features of case study as presented by Shultz et al 22
There are many potential applications for case study research. While often misconstrued as having only an exploratory role, case study research can be used for descriptive and explanatory research (p7–9). 3 Family medicine and community health researchers can use case study research for evaluating a variety of educational programmes, clinical programmes or community programmes.
Case study illustration from family medicine
In the featured study, Japanese family medicine residents received standardised patient instructor-based training in female breast, pelvic, male genital and prostate examinations as part of an international training collaboration to launch a new family medicine residency programme. 22 From family medicine residents, trainers and staff, the authors collected and analysed data from post-training feedback, semistructured interviews and a web-based questionnaire. While the programme was perceived favourably, they noted barriers to reinforcement in their home training programme, and taboos regarding gender-specific healthcare appear as barriers to implementing a similar programme in the home institution.
A step-by-step description of the process of carrying out a case study
As shown in table 2 and illustrated using the article by Shultz et al , 22 case study research generally includes 10 steps. While commonly conducted in this order, the steps do not always occur linearly as data collection and analysis may occur over several iterations or implemented with a slightly different order.
Ten steps for conducting a case study
Examples of published studies using the four types of case study designs suggested by Yin 3
Step 1. Conduct a literature review
During the literature review, researchers systematically search for publications, select those most relevant to the study’s purpose, critically appraise them and summarise the major themes. The literature review helps researchers ascertain what is and is not known about the phenomenon under study, delineate the scope and research questions of the study, and develop an academic or practical justification for the study. 23
Step 2. Formulate the research questions
Research questions critically define in operational terms what will be researched and how. They focus the study and play a key role in guiding design decisions. Key decisions include the case selection and choice of a case study design most suitable for the study. According to Fraenkel et al , 24 the key attributes of good research questions are (1) feasibility, (2) clarity, (3) significance, (4) connection to previous research identified in the literature and (5) compliance with ethical research standards.
Step 3. Ensure that a case study is appropriate
Before commencing the study, researchers should ensure that case study design embodies the most appropriate strategy for answering the study questions. The above-noted four key features—in depth examination of phenomena, naturalness, a focus on context and the use of a combination of methods—should be reflected in the research questions as well as subsequent design decisions.
Step 4. Determine the type of case study design
Researchers need to choose a specific case study design. Sometimes, researchers may define the case first (step 5), for example, in a programme evaluation, and the case may need to be defined before determining the type. Yin’s 3 typology is based on two dimensions, whether the study will examine a single case or multiple cases, and whether the study will focus on a single or multiple units of analysis. Figure 1 illustrates these four types of design using a hypothetical example of a programme evaluation. Table 3 shows an example of each type from the literature.
- Download figure
- Open in new tab
- Download powerpoint
Types of case study designs. 3 21
In type 1 holistic single case design , researchers examine a single programme as the sole unit of analysis. In type 2 embedded single case design , the interest is not exclusively in the programme, but also in its different subunits, including sites, staff and participants. These subunits constitute the range of units of analysis. In type 3 holistic multiple case design , researchers conduct a within and cross-case comparison of two or more programmes, each of which constitutes a single unit of analysis. A major strength of multiple case designs is that they enable researchers to develop an in depth description of each case and to identify patterns of variation and similarity between the cases. Multiple case designs are likely to have stronger internal validity and generate more insightful findings than single case designs. They do this by allowing ‘examination of processes and outcomes across many cases, identification of how individual cases might be affected by different environments, and the specific conditions under which a finding may occur’ (p583). 25 In type 4 embedded multiple case design , a variant of the holistic multiple case design, researchers perform a detailed examination of the subunits of each programme, rather than just examining each case as a whole.
Step 5. Define the boundaries of the case(s) and select the case(s)
Miles et al 26 define a case as ‘a phenomenon of some sort occurring in a bounded context’ (p28). What is and is not the case and how the case fits within its broader context should be explicitly defined. As noted in step 4, this step may occur before choice of the case study type, and the process may actually occur in a back-and-forth fashion. A case can entail an individual, a group, an organisation, an institution or a programme. In this step, researchers delineate the spatial and temporal boundaries of the case, that is, ‘when and where it occurred, and when and what was of interest’ (p390). 9 Aside from ensuring the coherence and consistency of the study, bounding the case ensures that the planned research project is feasible in terms of time and resources. Having access to the case and ensuring ethical research practice are two central considerations in case selection. 1
Step 6. Prepare to collect data
Before beginning the data collection, researchers need a study protocol that describes in detail the methods of data collection. The protocol should emphasise the coherence between the data collection methods and the research questions. According to Yin, 3 a case study protocol should include (1) an overview of the case study, (2) data collection procedures, (3) data collection questions and (4) a guide for the case study report. The protocol should be sufficiently flexible to allow researchers to make changes depending on the context and specific circumstances surrounding each data collection method.
Step 7. Collect and organise the data
While case study is often portrayed as a qualitative approach to research (eg, interviews, focus groups or observations), case study designs frequently rely on multiple data sources, including quantitative data (eg, surveys or statistical databases). A growing number of authors highlight the ways in which the use of mixed methods within case study designs might contribute to developing ‘a more complete understanding of the case’ (p902), 21 shedding light on ‘the complexity of a case’ (p118) 27 or increasing ‘the internal validity of a study’ (p6). 1 Guetterman and Fetters 21 explain how a qualitative case study can also be nested within a mixed methods design (ie, be considered the qualitative component of the design). An interesting strategy for organising multiple data sources is suggested by Yin. 3 He recommends using a case study database in which different data sources (eg, audio files, notes, documents or photographs) are stored for later retrieval or inspection. See guidance from Creswell and Hirose 28 for conducting a survey and qualitative data collection in mixed methods and DeJonckheere 29 on semistructured interviewing.
Step 8. Analyse the data
Bernard and Ryan 30 define data analysis as ‘the search for patterns in data and for ideas that help explain why these patterns are there in the first place’ (p109). Depending on the case study design, analysis of the qualitative and quantitative data can be done concurrently or sequentially. For the qualitative data, the first step of the analysis involves segmenting the data into coding units, ascribing codes to data segments and organising the codes in a coding scheme. 31 Depending on the role of theory in the study, an inductive, data-driven approach can be used where meaning is found in the data, or a deductive, concept-driven approach can be adopted where predefined concepts derived from the literature, or previous research, are used to code the data. 32 The second step involves searching for patterns across codes and subsets of respondents, so major themes are identified to describe, explain or predict the phenomenon under study. Babchuk 33 provides a step-by-step guidance for qualitative analysis in this issue. When conducting a single case study, the within-case analysis yields an in depth, thick description of the case. When the study involves multiple cases, the cross-comparison analysis elicits a description of similarities and divergence between cases and may generate explanations and theoretical predictions regarding other cases. 26
For the quantitative part of the case study, data are entered in statistical software packages for conducting descriptive or inferential analysis. Guetterman 34 provides a step-by-step guidance on basic statistics. In case study designs where both data strands are analysed simultaneously, analytical techniques include pattern matching, explanation building, time-series analysis and creating logic models (p142–167). 3
Step 9. Write the case study report
The case study report should have the following three characteristics. First, the description of the case and its context should be sufficiently comprehensive to allow the reader to understand the complexity of the phenomena under study. 35 Second, the data should be presented in a concise and transparent manner to enable the reader to question, or to re-examine, the findings. 36 Third, the report should be adapted to the interests and needs of its primary audience or audiences (eg, academics, practitioners, policy-makers or funders of research). Yin 3 suggests six formats for organising case study reports, namely linear-analytic, comparative, chronological, theory building, suspense and unsequenced structures. To facilitate case transferability and applicability to other similar contexts, the case study report must include a detailed description of the case.
Step 10. Appraise quality
Although presented as the final step of the case study process, quality appraisal should be considered throughout the study. Multiple criteria and frameworks for appraising the quality of case study research have been suggested in the literature. Yin 3 suggests the following four criteria: construct validity (ie, the extent to which a study accurately measures the concepts that it claims to investigate), internal validity (ie, the strength of the relationship between variables and findings), external validity (ie, the extent to which the findings can be generalised) and reliability (ie, the extent to which the findings can be replicated by other researchers conducting the same study). Yin 37 also suggests using two separate sets of guidelines for conducting case study research and for appraising the quality of case study proposals. Stake 4 presents a 20-item checklist for critiquing case study reports, and Creswell and Poth 38 and Denscombe 39 outline a number of questions to consider. Since these quality frameworks have evolved from different disciplinary and philosophical backgrounds, the researcher’s approach should be coherent with the epistemology of the study. Figure 2 provides a quality appraisal checklist adapted from Creswell and Poth 38 and Denscombe. 39
Checklist for evaluating the quality of a case study. 38 39
The challenges to conducting case study research include rationalising the literature based on literature review, writing the research questions, determining how to bound the case, and choosing among various case study purposes and designs. Factors held in common with other methods include analysing and presenting the findings, particularly with multiple data sources.
Other resources
Resources with more in depth guidance on case study research include Merriam, 17 Stake 4 and Yin. 3 While each reflects a different perspective on case study research, they all provide useful guidance for designing and conducting case studies. Other resources include Creswell and Poth, 38 Swanborn 2 and Tight. 40 For mixed methods case study designs, Creswell and Clark, 27 Guetterman and Fetters, 21 Luck et al , 6 and Plano Clark et al 41 provide guidance. Byrne and Ragin’s 42 The SAGE Handbook of Case-Based Methods and Mills et al ’s 43 Encyclopedia of case study research provide guidance for experienced case study researchers.
Conclusions
Family medicine and community health researchers engage in a wide variety of clinical, educational, research and administrative programmes. Case study research provides a highly flexible and powerful research tool to evaluate rigorously many of these endeavours and disseminate this information.
Acknowledgments
The authors would like to acknowledge the help of Dick Edelstein and Marie-Hélène Paré in editing the final manuscript.
- Cresswell K ,
- Robertson A , et al
- Walshe CE ,
- Caress AL ,
- Chew-Graham C , et al
- Jackson D ,
- Adelman C ,
- Eurepos G ,
- Eurepos G , et al
- Lincoln YS ,
- Eisenhardt KM
- Hijmans E ,
- Guetterman TC ,
- Shultz CG ,
- Yajima A , et al
- Fraenkel J ,
- Huberman A ,
- Creswell J ,
- DeJonckheere M
- Bernard H ,
- Guetterman T
- Denscombe M
- Plano Clark VL ,
- Walton JB , et al
- Little SH ,
- Motohara S ,
- Miyazaki K , et al
- Peterson JC ,
- Rogers EM ,
- Cunningham-Sabo L , et al
- Halladay JR ,
- Reed D , et al
Contributors SF and MDF conceived and drafted the manuscript, and approved the final version of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:
Health Case Studies
(29 reviews)
Glynda Rees, British Columbia Institute of Technology
Rob Kruger, British Columbia Institute of Technology
Janet Morrison, British Columbia Institute of Technology
Copyright Year: 2017
Publisher: BCcampus
Language: English
Formats Available
Conditions of use.
Learn more about reviews.
Reviewed by Jessica Sellars, Medical assistant office instructor, Blue Mountain Community College on 10/11/23
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and... read more
Comprehensiveness rating: 5 see less
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and plan. There is an appendix to refer to as well if you are needing to find something specific quickly. I have been looking for something like this to help my students have a base to do their project on. This is the most comprehensive version I have found on the subject.
Content Accuracy rating: 5
This is a book compiled of medical case studies. It is very accurate and can be used to learn from great care and mistakes.
Relevance/Longevity rating: 5
This material is very relevant in this context. It also has plenty of individual case studies to utilize in many ways in all sorts of medical courses. This is a very useful textbook and it will continue to be useful for a very long time as you can still learn from each study even if medicine changes through out the years.
Clarity rating: 5
The author put a lot of thought into the ease of accessibility and reading level of the target audience. There is even a "how to use this resource" section which could be extremely useful to students.
Consistency rating: 5
The text follows a very consistent format throughout the book.
Modularity rating: 5
Each case study is individual broken up and in a group of similar case studies. This makes it extremely easy to utilize.
Organization/Structure/Flow rating: 5
The book is very organized and the appendix is through. It flows seamlessly through each case study.
Interface rating: 5
I had no issues navigating this book, It was clearly labeled and very easy to move around in.
Grammatical Errors rating: 5
I did not catch any grammar errors as I was going through the book
Cultural Relevance rating: 5
This is a challenging question for any medical textbook. It is very culturally relevant to those in medical or medical office degrees.
I have been looking for something like this for years. I am so happy to have finally found it.
Reviewed by Cindy Sun, Assistant Professor, Marshall University on 1/7/23
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and... read more
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and students. For faculty, the introduction section titled ‘How to use this resource’ and individual notes to educators before each case study contain application tips. An appendix overview lists key elements as issues / concepts, scenario context, and healthcare roles for each case study. For students, learning objectives are presented at the beginning of each case study to provide a framework of expectations.
The content is presented accurately and realistic.
The case studies read similar to ‘A Day In the Life of…’ with detailed intraprofessional communications similar to what would be overheard in patient care areas. The authors present not only the view of the patient care nurse, but also weave interprofessional vantage points through each case study by including patient interaction with individual professionals such as radiology, physician, etc.
In addition to objective assessment findings, the authors integrate standard orders for each diagnosis including medications, treatments, and tests allowing the student to incorporate pathophysiology components to their assessments.
Each case study is arranged in the same framework for consistency and ease of use.
This compilation of eight healthcare case studies focusing on new onset and exacerbation of prevalent diagnoses, such as heart failure, deep vein thrombosis, cancer, and chronic obstructive pulmonary disease advancing to pneumonia.
Each case study has a photo of the ‘patient’. Simple as this may seem, it gives an immediate mental image for the student to focus.
Interface rating: 4
As noted by previous reviewers, most of the links do not connect active web pages. This may be due to the multiple options for accessing this resource (pdf download, pdf electronic, web view, etc.).
Grammatical Errors rating: 4
A minor weakness that faculty will probably need to address prior to use is regarding specific term usages differences between Commonwealth countries and United States, such as lung sound descriptors as ‘quiet’ in place of ‘diminished’ and ‘puffers’ in place of ‘inhalers’.
The authors have provided a multicultural, multigenerational approach in selection of patient characteristics representing a snapshot of today’s patient population. Additionally, one case study focusing on heart failure is about a middle-aged adult, contrasting to the average aged patient the students would normally see during clinical rotations. This option provides opportunities for students to expand their knowledge on risk factors extending beyond age.
This resource is applicable to nursing students learning to care for patients with the specific disease processes presented in each case study or for the leadership students focusing on intraprofessional communication. Educators can assign as a supplement to clinical experiences or as an in-class application of knowledge.
Reviewed by Stephanie Sideras, Assistant Professor, University of Portland on 8/15/22
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five... read more
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five overarching learning objectives pulled from the Institute of Medicine core competencies will clearly resonate with any faculty familiar with Quality and Safety Education for Nurses curriculum.
The presentation of symptoms, treatments and management of the health alterations was accurate. Dialogue between the the interprofessional team was realistic. At times the formatting of lab results was confusing as they reflected reference ranges specific to the Canadian healthcare system but these occurrences were minimal and could be easily adapted.
The focus for learning from these case studies was communication - patient centered communication and interprofessional team communication. Specific details, such as drug dosing, was minimized, which increases longevity and allows for easy individualization of the case data.
While some vocabulary was specific to the Canadian healthcare system, overall the narrative was extremely engaging and easy to follow. Subjective case data from patient or provider were formatted in italics and identified as 'thoughts'. Objective and behavioral case data were smoothly integrated into the narrative.
The consistency of formatting across the eight cases was remarkable. Specific learning objectives are identified for each case and these remain consistent across the range of cases, varying only in the focus for the goals for each different health alterations. Each case begins with presentation of essential patient background and the progress across the trajectory of illness as the patient moves from location to location encountering different healthcare professionals. Many of the characters (the triage nurse in the Emergency Department, the phlebotomist) are consistent across the case situations. These consistencies facilitate both application of a variety of teaching methods and student engagement with the situated learning approach.
Case data is presented by location and begins with the patient's first encounter with the healthcare system. This allows for an examination of how specific trajectories of illness are manifested and how care management needs to be prioritized at different stages. This approach supports discussions of care transitions and the complexity of the associated interprofessional communication.
The text is well organized. The case that has two levels of complexity is clearly identified
The internal links between the table of contents and case specific locations work consistently. In the EPUB and the Digital PDF the external hyperlinks are inconsistently valid.
The grammatical errors were minimal and did not detract from readability
Cultural diversity is present across the cases in factors including race, ethnicity, socioeconomic status, family dynamics and sexual orientation.
The level of detail included in these cases supports a teaching approach to address all three spectrums of learning - knowledge, skills and attitudes - necessary for the development of competent practice. I also appreciate the inclusion of specific assessment instruments that would facilitate a discussion of evidence based practice. I will enjoy using these case to promote clinical reasoning discussions of data that is noticed and interpreted with the resulting prioritizes that are set followed by reflections that result from learner choices.
Reviewed by Chris Roman, Associate Professor, Butler University on 5/19/22
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various... read more
Comprehensiveness rating: 4 see less
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various learning strategies to be employed to leverage the cases for deeper student learning and application.
The narrative form of the cases is less subject to issues of accuracy than a more content-based book would be. That said, the cases are realistic and reasonable, avoiding being too mundane or too extreme.
These cases are narrative and do not include many specific mentions of drugs, dosages, or other aspects of clinical care that may grow/evolve as guidelines change. For this reason, the cases should be “evergreen” and can be modified to suit different types of learners.
Clarity rating: 4
The text is written in very accessible language and avoids heavy use of technical language. Depending on the level of learner, this might even be too simplistic and omit some details that would be needed for physicians, pharmacists, and others to make nuanced care decisions.
The format is very consistent with clear labeling at transition points.
The authors point out in the introductory materials that this text is designed to be used in a modular fashion. Further, they have built in opportunities to customize each cases, such as giving dates of birth at “19xx” to allow for adjustments based on instructional objectives, etc.
The organization is very easy to follow.
I did not identify any issues in navigating the text.
The text contains no grammatical errors, though the language is a little stiff/unrealistic in some cases.
Cases involve patients and members of the care team that are of varying ages, genders, and racial/ethnic backgrounds
Reviewed by Trina Larery, Assistant Professor, Pittsburg State University on 4/5/22
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand... read more
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand and apply to the classroom. The E-reader format included hyperlinks that bring the students to subsequent clinical studies.
Content Accuracy rating: 4
The treatments were explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse. The case studies were accurate in explanation. The DVT case study incorrectly identifies the location of the clot in the popliteal artery instead of in the vein.
The content is relevant to a variety of different types of health care providers and due to the general nature of the cases, will remain relevant over time. Updates should be made annually to the hyperlinks and to assure current standard of practice is still being met.
Clear, simple and easy to read.
Consistent with healthcare terminology and framework throughout all eight case studies.
The text is modular. Cases can be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point providing great flexibility. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
The book is well organized, presenting in a logical clear fashion. The appendix allows the student to move about the case study without difficulty.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change based on current guidelines. A few hyperlinks had "page not found".
Few grammatical errors were noted in text.
The case studies include people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. There are roughly 25 broken online links or "pages not found", care needs to be taken to update at least annually and assure links are valid and utilizing the most up to date information.
Reviewed by Benjamin Silverberg, Associate Professor/Clinician, West Virginia University on 3/24/22
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what... read more
Comprehensiveness rating: 3 see less
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what is going on where, especially since each case is largely conversation-based. Since this presents 8 cases (really 7 with one being expanded upon), there are many medical topics (and venues) that are not included. It's impossible to include every kind of situation, but I'd love to see inclusion of sexual health, renal pathology, substance abuse, etc.
Though there are differences in how care can be delivered based on personal style, changing guidelines, available supplies, etc, the medical accuracy seems to be high. I did not detect bias or industry influence.
Relevance/Longevity rating: 4
Medications are generally listed as generics, with at least current dosing recommendations. The text gives a picture of what care looks like currently, but will be a little challenging to update based on new guidelines (ie, it can be hard to find the exact page in which a medication is dosed/prescribed). Even if the text were to be a little out of date, an instructor can use that to point out what has changed (and why).
Clear text, usually with definitions of medical slang or higher-tier vocabulary. Minimal jargon and there are instances where the "characters" are sorting out the meaning as well, making it accessible for new learners, too.
Overall, the style is consistent between cases - largely broken up into scenes and driven by conversation rather than descriptions of what is happening.
There are 8 (well, again, 7) cases which can be reviewed in any order. Case #2 builds upon #1, which is intentional and a good idea, though personally I would have preferred one case to have different possible outcomes or even a recurrence of illness. Each scene within a case is reasonably short.
Organization/Structure/Flow rating: 4
These cases are modular and don't really build on concepts throughout. As previously stated, case #2 builds upon #1, but beyond that, there is no progression. (To be sure, the authors suggest using case #1 for newer learners and #2 for more advanced ones.) The text would benefit from thematic grouping, a longer introduction and debriefing for each case (there are learning objectives but no real context in medical education nor questions to reflect on what was just read), and progressively-increasing difficulty in medical complexity, ethics, etc.
I used the PDF version and had no interface issues. There are minimal photographs and charts. Some words are marked in blue but those did not seem to be hyperlinked anywhere.
No noticeable errors in grammar, spelling, or formatting were noted.
I appreciate that some diversity of age and ethnicity were offered, but this could be improved. There were Canadian Indian and First Nations patients, for example, as well as other characters with implied diversity, but there didn't seem to be any mention of gender diverse or non-heterosexual people, or disabilities. The cases tried to paint family scenes (the first patient's dog was fairly prominently mentioned) to humanize them. Including more cases would allow for more opportunities to include sex/gender minorities, (hidden) disabilities, etc.
The text (originally from 2017) could use an update. It could be used in conjunction with other Open Texts, as a compliment to other coursework, or purely by itself. The focus is meant to be on improving communication, but there are only 3 short pages at the beginning of the text considering those issues (which are really just learning objectives). In addition to adding more cases and further diversity, I personally would love to see more discussion before and after the case to guide readers (and/or instructors). I also wonder if some of the ambiguity could be improved by suggesting possible health outcomes - this kind of counterfactual comparison isn't possible in real life and could be really interesting in a text. Addition of comprehension/discussion questions would also be worthwhile.
Reviewed by Danielle Peterson, Assistant Professor, University of Saint Francis on 12/31/21
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare... read more
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare workers in acute hospital settings. The cases are primarily set in the inpatient hospital setting, so the bulk of the clinical information is basic emergency care and inpatient protocol: vitals, breathing, medication management, etc. The text provides a table of contents at opening of the text and a handy appendix at the conclusion of the text that outlines each case’s issue(s), scenario, and healthcare roles. No index or glossary present.
Although easy to update, it should be noted that the cases are taking place in a Canadian healthcare system. Terms may be unfamiliar to some students including “province,” “operating theatre,” “physio/physiotherapy,” and “porter.” Units of measurement used include Celsius and meters. Also, the issue of managed care, health insurance coverage, and length of stay is missing for American students. These are primary issues that dictate much of the healthcare system in the US and a primary job function of social workers, nurse case managers, and medical professionals in general. However, instructors that wish to add this to the case studies could do so easily.
The focus of this text is on healthcare communication which makes it less likely to become obsolete. Much of the clinical information is stable healthcare practice that has been standard of care for quite some time. Nevertheless, given the nature of text, updates would be easy to make. Hyperlinks should be updated to the most relevant and trustworthy sources and checked frequently for effectiveness.
The spacing that was used to note change of speaker made for ease of reading. Although unembellished and plain, I expect students to find this format easy to digest and interesting, especially since the script is appropriately balanced with ‘human’ qualities like the current TV shows and songs, the use of humor, and nonverbal cues.
A welcome characteristic of this text is its consistency. Each case is presented in a similar fashion and the roles of the healthcare team are ‘played’ by the same character in each of the scenarios. This allows students to see how healthcare providers prioritize cases and juggle the needs of multiple patients at once. Across scenarios, there was inconsistency in when clinical terms were hyperlinked.
The text is easily divisible into smaller reading sections. However, since the nature of the text is script-narrative format, if significant reorganization occurs, one will need to make sure that the communication of the script still makes sense.
The text is straightforward and presented in a consistent fashion: learning objectives, case history, a script of what happened before the patient enters the healthcare setting, and a script of what happens once the patient arrives at the healthcare setting. The authors use the term, “ideal interactions,” and I would agree that these cases are in large part, ‘best case scenarios.’ Due to this, the case studies are well organized, clear, logical, and predictable. However, depending on the level of student, instructors may want to introduce complications that are typical in the hospital setting.
The interface is pleasing and straightforward. With exception to the case summary and learning objectives, the cases are in narrative, script format. Each case study supplies a photo of the ‘patient’ and one of the case studies includes a link to a 3-minute video that introduces the reader to the patient/case. One of the highlights of this text is the use of hyperlinks to various clinical practices (ABG, vital signs, transfer of patient). Unfortunately, a majority of the links are broken. However, since this is an open text, instructors can update the links to their preference.
Although not free from grammatical errors, those that were noticed were minimal and did not detract from reading.
Cultural Relevance rating: 4
Cultural diversity is visible throughout the patients used in the case studies and includes factors such as age, race, socioeconomic status, family dynamics, and sexual orientation. A moderate level of diversity is noted in the healthcare team with some stereotypes: social workers being female, doctors primarily male.
As a social work instructor, I was grateful to find a text that incorporates this important healthcare role. I would have liked to have seen more content related to advance directives, mediating decision making between the patient and care team, emotional and practical support related to initial diagnosis and discharge planning, and provision of support to colleagues, all typical roles of a medical social worker. I also found it interesting that even though social work was included in multiple scenarios, the role was only introduced on the learning objectives page for the oncology case.
Reviewed by Crystal Wynn, Associate Professor, Virginia State University on 7/21/21
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied... read more
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied health care team members are represented within the case study. Key terms appear throughout the case study textbook and readers are able to click on a hyperlink which directs them to the definition and an explanation of the key term.
Content is accurate, error-free and unbiased.
The content is up-to-date, but not in a way that will quickly make the text obsolete within a short period of time. The text is written and/or arranged in such a way that necessary updates will be relatively easy and straightforward to implement.
The text is written in lucid, accessible prose, and provides adequate context for any jargon/technical terminology used
The text is internally consistent in terms of terminology and framework.
The text is easily and readily divisible into smaller reading sections that can be assigned at different points within the course. Each case can be divided into a chronic disease state unit, which will allow the reader to focus on one section at a time.
Organization/Structure/Flow rating: 3
The topics in the text are presented in a logical manner. Each case provides an excessive amount of language that provides a description of the case. The cases in this text reads more like a novel versus a clinical textbook. The learning objectives listed within each case should be in the form of questions or activities that could be provided as resources for instructors and teachers.
Interface rating: 3
There are several hyperlinks embedded within the textbook that are not functional.
The text contains no grammatical errors.
Cultural Relevance rating: 3
The text is not culturally insensitive or offensive in any way. More examples of cultural inclusiveness is needed throughout the textbook. The cases should be indicative of individuals from a variety of races and ethnicities.
Reviewed by Rebecca Hillary, Biology Instructor, Portland Community College on 6/15/21
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health... read more
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health care program. I read the textbook in E-reader format and this includes hyperlinks that bring the students to subsequent clinical study if the book is being used in a clinical classroom. This book is significantly more comprehensive in its approach from other case studies I have read because it provides a bird’s eye view of the many clinicians, technicians, and hospital staff working with one patient. The book also provides real time measurements for patients that change as they travel throughout the hospital until time of discharge.
Each case gave an accurate sense of the chaos that would be present in an emergency situation and show how the conditions affect the practitioners as well as the patients. The reader gets an accurate big picture--a feel for each practitioner’s point of view as well as the point of view of the patient and the patient’s family as the clock ticks down and the patients are subjected to a number of procedures. The clinical information contained in this textbook is all in hyperlinks containing references to clinical skills open text sources or medical websites. I did find one broken link on an external medical resource.
The diseases presented are relevant and will remain so. Some of the links are directly related to the Canadian Medical system so they may not be applicable to those living in other regions. Clinical links may change over time but the text itself will remain relevant.
Each case study clearly presents clinical data as is it recorded in real time.
Each case study provides the point of view of several practitioners and the patient over several days. While each of the case studies covers different pathology they all follow this same format, several points of view and data points, over a number of days.
The case studies are divided by days and this was easy to navigate as a reader. It would be easy to assign one case study per body system in an Anatomy and Physiology course, or to divide them up into small segments for small in class teaching moments.
The topics are presented in an organized way showing clinical data over time and each case presents a large number of view points. For example, in the first case study, the patient is experiencing difficulty breathing. We follow her through several days from her entrance to the emergency room. We meet her X Ray Technicians, Doctor, Nurses, Medical Assistant, Porter, Physiotherapist, Respiratory therapist, and the Lab Technicians running her tests during her stay. Each practitioner paints the overall clinical picture to the reader.
I found the text easy to navigate. There were not any figures included in the text, only clinical data organized in charts. The figures were all accessible via hyperlink. Some figures within the textbook illustrating patient scans could have been helpful but I did not have trouble navigating the links to visualize the scans.
I did not see any grammatical errors in the text.
The patients in the text are a variety of ages and have a variety of family arrangements but there is not much diversity among the patients. Our seven patients in the eight case studies are mostly white and all cis gendered.
Some of the case studies, for example the heart failure study, show clinical data before and after drug treatments so the students can get a feel for mechanism in physiological action. I also liked that the case studies included diet and lifestyle advice for the patients rather than solely emphasizing these pharmacological interventions. Overall, I enjoyed reading through these case studies and I plan to utilize them in my Anatomy and Physiology courses.
Reviewed by Richard Tarpey, Assistant Professor, Middle Tennessee State University on 5/11/21
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate... read more
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate for entry-level health care students. The book includes important health problems, but I would like to see coverage of at least one more chronic/lifestyle issue such as diabetes. The book covers adult issues only.
Content is accurate without bias
The content of the book is relevant and up-to-date. It addresses conditions that are prevalent in today's population among adults. There are no pediatric cases, but this does not significantly detract from the usefulness of the text. The format of the book lends to easy updating of data or information.
The book is written with clarity and is easy to read. The writing style is accessible and technical terminology is explained with links to more information.
Consistency is present. Lack of consistency is typically a problem with case study texts, but this book is consistent with presentation, format, and terminology throughout each of the eight cases.
The book has high modularity. Each of the case studies can be used independently from the others providing flexibility. Additionally, each case study can be partitioned for specific learning objectives based on the learning objectives of the course or module.
The book is well organized, presenting students conceptually with differing patient flow patterns through a hospital. The patient information provided at the beginning of each case is a wonderful mechanism for providing personal context for the students as they consider the issues. Many case studies focus on the problem and the organization without students getting a patient's perspective. The patient perspective is well represented in these cases.
The navigation through the cases is good. There are some terminology and procedure hyperlinks within the cases that do not work when accessed. This is troubling if you intend to use the text for entry-level health care students since many of these links are critical for a full understanding of the case.
There are some non-US variants of spelling and a few grammatical errors, but these do not detract from the content of the messages of each case.
The book is inclusive of differing backgrounds and perspectives. No insensitive or offensive references were found.
I like this text for its application flexibility. The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology. The content is also helpful for the identification of healthcare administration managerial issues for students to consider. The book has many applications.
Reviewed by Paula Baldwin, Associate Professor/Communication Studies, Western Oregon University on 5/10/21
The different case studies fall on a range, from crisis care to chronic illness care. read more
The different case studies fall on a range, from crisis care to chronic illness care.
The contents seems to be written as they occurred to represent the most complete picture of each medical event's occurence.
These case studies are from the Canadian medical system, but that does not interfere with it's applicability.
It is written for a medical audience, so the terminology is mostly formal and technical.
Some cases are shorter than others and some go in more depth, but it is not problematic.
The eight separate case studies is the perfect size for a class in the quarter system. You could combine this with other texts, videos or learning modalities, or use it alone.
As this is a case studies book, there is not a need for a logical progression in presentation of topics.
No problems in terms of interface.
I have not seen any grammatical errors.
I did not see anything that was culturally insensitive.
I used this in a Health Communication class and it has been extraordinarily successful. My studies are analyzing the messaging for the good, the bad, and the questionable. The case studies are widely varied and it gives the class insights into hospital experiences, both front and back stage, that they would not normally be able to examine. I believe that because it is based real-life medical incidents, my students are finding the material highly engaging.
Reviewed by Marlena Isaac, Instructor, Aiken Technical College on 4/23/21
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with... read more
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with a situation in clinical they are not surprised and now how to move through it effectively.
The case studies provided accurate information that relates to the named disease.
It is relevant to health care studies and the development of critical thinking.
Cases are straightforward with great clinical information.
Clinical information is provided concisely.
Appropriate for clinical case study.
Presented to facilitate information gathering.
Takes a while to navigate in the browser.
Cultural Relevance rating: 1
Text lacks adequate representation of minorities.
Reviewed by Kim Garcia, Lecturer III, University of Texas Rio Grande Valley on 11/16/20
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at... read more
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at different levels of clinical knowledge. The human element of both patient and health care provider is well captured. The cases are presented with a focus on interprofessional interaction and collaboration, more so than teaching medical content.
Content is accurate and un-biased. No errors noted. Most diagnostic and treatment information is general so it will remain relevant over time. The content of these cases is more appropriate for teaching interprofessional collaboration and less so for teaching the medical care for each diagnosis.
The content is relevant to a variety of different types of health care providers (nurses, radiologic technicians, medical laboratory personnel, etc) and due to the general nature of the cases, will remain relevant over time.
Easy to read. Clear headings are provided for sections of each case study and these section headings clearly tell when time has passed or setting has changed. Enough description is provided to help set the scene for each part of the case. Much of the text is written in the form of dialogue involving patient, family and health care providers, making it easy to adapt for role play. Medical jargon is limited and links for medical terms are provided to other resources that expound on medical terms used.
The text is consistent in structure of each case. Learning objectives are provided. Cases generally start with the patient at home and move with the patient through admission, testing and treatment, using a variety of healthcare services and encountering a variety of personnel.
The text is modular. Cases could be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
Each case follows a patient in a logical, chronologic fashion. A clear table of contents and appendix are provided which allows the user to quickly locate desired content. It would be helpful if the items in the table of contents and appendix were linked to the corresponding section of the text.
The hyperlinks to content outside this book work, however using the back arrow on your browser returns you to the front page of the book instead of to the point at which you left the text. I would prefer it if the hyperlinks opened in a new window or tab so closing that window or tab would leave you back where you left the text.
No grammatical errors were noted.
The text is culturally inclusive and appropriate. Characters, both patients and care givers are of a variety of races, ethnicities, ages and backgrounds.
I enjoyed reading the cases and reviewing this text. I can think of several ways in which I will use this content.
Reviewed by Raihan Khan, Instructor/Assistant Professor, James Madison University on 11/3/20
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients. read more
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients.
The health information contained in the textbook is mostly accurate.
I think the book is written focusing on the current culture and health issues faced by the patients. To keep the book relevant in the future, the contexts especially the culture/lifestyle/health care modalities, etc. would need to be updated regularly.
The language is pretty simple, clear, and easy to read.
There is no complaint about consistency. One of the main issues of writing a book, consistency was well managed by the authors.
The book is easy to explore based on how easy the setup is. Students can browse to the specific section that they want to read without much hassle of finding the correct information.
The organization is simple but effective. The authors organized the book based on what can happen in a patient's life and what possible scenarios students should learn about the disease. From that perspective, the book does a good job.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change that is beyond the author's control. It's frustrating for the reader when the external link shows no information.
The book is free of any major language and grammatical errors.
The book might do a little better in cultural competency. e.g. Last name Singh is mainly for Sikh people. In the text Harj and Priya Singh are Muslim. the authors can consult colleagues who are more familiar with those cultures and revise some cultural aspects of the cases mentioned in the book.
The book is a nice addition to the open textbook world. Hope to see more health issues covered by the book.
Reviewed by Ryan Sheryl, Assistant Professor, California State University, Dominguez Hills on 7/16/20
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality... read more
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality improvement, and informatics. While the case studies do not cover all medical conditions or bodily systems, the book is thorough in conveying details of various patients and medical team members in a hospital environment. Rather than an index or glossary at the end of the text, it contains links to outside websites for more information on medical tests and terms referenced in the cases.
The content provided is reflective of best practices in patient care, interdisciplinary collaboration, and communication at the time of publication. It is specifically accurate for the context of hospitals in Canada. The links provided throughout the text have the potential to supplement with up-to-date descriptions and definitions, however, many of them are broken (see notes in Interface section).
The content of the case studies reflects the increasingly complex landscape of healthcare, including a variety of conditions, ages, and personal situations of the clients and care providers. The text will require frequent updating due to the rapidly changing landscape of society and best practices in client care. For example, a future version may include inclusive practices with transgender clients, or address ways medical racism implicitly impacts client care (see notes in Cultural Relevance section).
The text is written clearly and presents thorough, realistic details about working and being treated in an acute hospital context.
The text is very straightforward. It is consistent in its structure and flow. It uses consistent terminology and follows a structured framework throughout.
Being a series of 8 separate case studies, this text is easily and readily divisible into smaller sections. The text was designed to be taken apart and used piece by piece in order to serve various learning contexts. The parts of each case study can also be used independently of each other to facilitate problem solving.
The topics in the case studies are presented clearly. The structure of each of the case studies proceeds in a similar fashion. All of the cases are set within the same hospital so the hospital personnel and service providers reappear across the cases, giving a textured portrayal of the experiences of the various service providers. The cases can be used individually, or one service provider can be studied across the various studies.
The text is very straightforward, without complex charts or images that could become distorted. Many of the embedded links are broken and require updating. The links that do work are a very useful way to define and expand upon medical terms used in the case studies.
Grammatical errors are minimal and do not distract from the flow of the text. In one instance the last name Singh is spelled Sing, and one patient named Fred in the text is referred to as Frank in the appendix.
The cases all show examples of health care personnel providing compassionate, client-centered care, and there is no overt discrimination portrayed. Two of the clients are in same-sex marriages and these are shown positively. It is notable, however, that the two cases presenting people of color contain more negative characteristics than the other six cases portraying Caucasian people. The people of color are the only two examples of clients who smoke regularly. In addition, the Indian client drinks and is overweight, while the First Nations client is the only one in the text to have a terminal diagnosis. The Indian client is identified as being Punjabi and attending a mosque, although there are only 2% Muslims in the Punjab province of India. Also, the last name Singh generally indicates a person who is a Hindu or Sikh, not Muslim.
Reviewed by Monica LeJeune, RN Instructor, LSUE on 4/24/20
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process. read more
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process.
Accurately presents health scenarios with real life assessment techniques and patient outcomes.
Relevant to nursing practice.
Clearly written and easily understood.
Consistent with healthcare terminology and framework
Has a good reading flow.
Topics presented in logical fashion
Easy to read.
No grammatical errors noted.
Text is not culturally insensitive or offensive.
Good book to have to teach nursing students.
Reviewed by april jarrell, associate professor, J. Sargeant Reynolds Community College on 1/7/20
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process. read more
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process.
The content is accurate and evidence based. There is no bias noted
The content in the text is relevant, up to date for nursing students. It will be easy to update content as needed because the framework allows for addition to the content.
The text is clear and easy to understand.
Framework and terminology is consistent throughout the text; the case study is a continual and takes the student on a journey with the patient. Great for learning!
The case studies can be easily divided into smaller sections to allow for discussions, and weekly studies.
The text and content progress in a logical, clear fashion allowing for progression of learning.
No interface issues noted with this text.
No grammatical errors noted in the text.
No racial or culture insensitivity were noted in the text.
I would recommend this text be used in nursing schools. The use of case studies are helpful for students to learn and practice the nursing process.
Reviewed by Lisa Underwood, Practical Nursing Instructor, NTCC on 12/3/19
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own... read more
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own set of learning objectives that can be tweaked to fit several allied health courses. Although the case studies are designed around the Canadian Healthcare System, they are quite easily adaptable to fit most any modern, developed healthcare system.
Content Accuracy rating: 3
Overall, the text is quite accurate. There is one significant error that needs to be addressed. It is located in the DVT case study. In the study, a popliteal artery clot is mislabeled as a DVT. DVTs are located in veins, not in arteries. That said, the case study on the whole is quite good. This case study could be used as a learning tool in the classroom for discussion purposes or as a way to test student understanding of DVTs, on example might be, "Can they spot the error?"
At this time, all of the case studies within the text are current. Healthcare is an ever evolving field that rests on the best evidence based practice. Keeping that in mind, educators can easily adapt the studies as the newest evidence emerges and changes practice in healthcare.
All of the case studies are well written and easy to understand. The text includes several hyperlinks and it also highlights certain medical terminology to prompt readers as a way to enhance their learning experience.
Across the text, the language, style, and format of the case studies are completely consistent.
The text is divided into eight separate case studies. Each case study may be used independently of the others. All case studies are further broken down as the focus patient passes through each aspect of their healthcare system. The text's modularity makes it possible to use a case study as individual work, group projects, class discussions, homework or in a simulation lab.
The case studies and the diagnoses that they cover are presented in such a way that educators and allied health students can easily follow and comprehend.
The book in itself is free of any image distortion and it prints nicely. The text is offered in a variety of digital formats. As noted in the above reviews, some of the hyperlinks have navigational issues. When the reader attempts to access them, a "page not found" message is received.
There were minimal grammatical errors. Some of which may be traced back to the differences in our spelling.
The text is culturally relevant in that it includes patients from many different backgrounds and ethnicities. This allows educators and students to explore cultural relevance and sensitivity needs across all areas in healthcare. I do not believe that the text was in any way insensitive or offensive to the reader.
By using the case studies, it may be possible to have an open dialogue about the differences noted in healthcare systems. Students will have the ability to compare and contrast the Canadian healthcare system with their own. I also firmly believe that by using these case studies, students can improve their critical thinking skills. These case studies help them to "put it all together".
Reviewed by Melanie McGrath, Associate Professor, TRAILS on 11/29/19
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case. read more
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case.
I saw no areas of inaccuracy
As in all healthcare texts, treatments and/or tests will change frequently. However, everything is currently up-to-date thus it should be a good reference for several years.
Each case is written so that any level of healthcare student would understand. Hyperlinks in the text is also very helpful.
All of the cases are written in a similar fashion.
Although not structured as a typical text, each case is easily assigned as a stand-alone.
Each case is organized clearly in an appropriate manner.
I did not see any issues.
I did not see any grammatical errors
The text seemed appropriately inclusive. There are no pediatric cases and no cases of intellectually-impaired patients, but those types of cases introduce more advanced problem-solving which perhaps exceed the scope of the text. May be a good addition to the text.
I found this text to be an excellent resource for healthcare students in a variety of fields. It would be best utilized in inter professional courses to help guide discussion.
Reviewed by Lynne Umbarger, Clinical Assistant Professor, Occupational Therapy, Emory and Henry College on 11/26/19
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational... read more
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational purposes. The material was easily understood by the students but challenging enough for classroom discussion. There are no mentions in the book about occupational therapy, but it is easy enough to add a couple words and make inclusion simple.
Very nice lab values are provided in the case study, making it more realistic for students.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
The material is easily understood by allied health students. The cases have links to additional learning materials for concepts that may be less familiar or should be explored further in a particular health field.
The language used in the book is consistent between cases. The framework is the same with each case which makes it easier to locate areas that would be of interest to a particular allied health profession.
The case studies are comprehensive but well-organized. They are short enough to be useful for class discussion or a full-blown assignment. The students seem to understand the material and have not expressed that any concepts or details were missing.
Each case is set up like the other cases. There are learning objectives at the beginning of each case to facilitate using the case, and it is easy enough to pull out material to develop useful activities and assignments.
There is a quick chart in the Appendix to allow the reader to determine the professions involved in each case as well as the pertinent settings and diagnoses for each case study. The contents are easy to access even while reading the book.
As a person who attends carefully to grammar, I found no errors in all of the material I read in this book.
There are a greater number of people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book. With each case, I could easily picture the person in the case. This book appears to be Canadian and more inclusive than most American books.
I was able to use this book the first time I accessed it to develop a classroom activity for first-year occupational therapy students and a more comprehensive activity for second-year students. I really appreciate the links to a multitude of terminology and medical lab values/issues for each case. I will keep using this book.
Reviewed by Cindy Krentz, Assistant Professor, Metropolitan State University of Denver on 6/15/19
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some... read more
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some understanding of the patient's background. I think it could benefit from having a glossary. I liked how the authors included the vital signs in an easily readable bar. I would have liked to see the labs also highlighted like this. I also felt that it would have been good written in a 'what would you do next?' type of case study.
The book is very accurate in language, what tests would be prudent to run and in the day in the life of the hospital in all cases. One inaccuracy is that the authors called a popliteal artery clot a DVT. The rest of the DVT case study was great, though, but the one mistake should be changed.
The book is up to date for now, but as tests become obsolete and new equipment is routinely used, the book ( like any other health textbook) will need to be updated. It would be easy to change, however. All that would have to happen is that the authors go in and change out the test to whatever newer, evidence-based test is being utilized.
The text is written clearly and easy to understand from a student's perspective. There is not too much technical jargon, and it is pretty universal when used- for example DVT for Deep Vein Thrombosis.
The book is consistent in language and how it is broken down into case studies. The same format is used for highlighting vital signs throughout the different case studies. It's great that the reader does not have to read the book in a linear fashion. Each case study can be read without needing to read the others.
The text is broken down into eight case studies, and within the case studies is broken down into days. It is consistent and shows how the patient can pass through the different hospital departments (from the ER to the unit, to surgery, to home) in a realistic manner. The instructor could use one or more of the case studies as (s)he sees fit.
The topics are eight different case studies- and are presented very clearly and organized well. Each one is broken down into how the patient goes through the system. The text is easy to follow and logical.
The interface has some problems with the highlighted blue links. Some of them did not work and I got a 'page not found' message. That can be frustrating for the reader. I'm wondering if a glossary could be utilized (instead of the links) to explain what some of these links are supposed to explain.
I found two or three typos, I don't think they were grammatical errors. In one case I think the Canadian spelling and the United States spelling of the word are just different.
This is a very culturally competent book. In today's world, however, one more type of background that would merit delving into is the trans-gender, GLBTQI person. I was glad that there were no stereotypes.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. Since we are becoming more interprofessional, I liked that we saw what the phlebotomist and other ancillary personnel (mostly different technicians) did. I think that it could become even more interdisciplinary so colleges and universities could have more interprofessional education- courses or simulations- with the addition of the nurse using social work, nutrition, or other professional health care majors.
Reviewed by Catherine J. Grott, Interim Director, Health Administration Program, TRAILS on 5/5/19
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this. read more
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this.
The book is accurate, however it has numerous broken online links.
Relevance/Longevity rating: 3
The content is very relevant, but some links are out-dated. For example, WHO Guidelines for Safe Surgery 2009 (p. 186) should be updated.
The book is written in clear and concise language. The side stories about the healthcare workers make the text interesting.
The book is consistent in terms of terminology and framework. Some terms that are emphasized in one case study are not emphasized (with online links) in the other case studies. All of the case studies should have the same words linked to online definitions.
Modularity rating: 3
The book can easily be parsed out if necessary. However, the way the case studies have been written, it's evident that different authors contributed singularly to each case study.
The organization and flow are good.
Interface rating: 1
There are numerous broken online links and "pages not found."
The grammar and punctuation are correct. There are two errors detected: p. 120 a space between the word "heart" and the comma; also a period is needed after Dr (p. 113).
I'm not quite sure that the social worker (p. 119) should comment that the patient and partner are "very normal people."
There are roughly 25 broken online links or "pages not found." The BC & Canadian Guidelines (p. 198) could also include a link to US guidelines to make the text more universal . The basilar crackles (p. 166) is very good. Text could be used compare US and Canadian healthcare. Text could be enhanced to teach "soft skills" and interdepartmental communication skills in healthcare.
Reviewed by Lindsey Henry, Practical Nursing Instructor, Fletcher on 5/1/19
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning... read more
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning objectives, which were effectively met in the readings.
As a seasoned nurse, I believe that the content regarding pathophysiology and treatments used in the case studies were accurate. I really appreciated how many of the treatments were also explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse.
The case studies are up to date and correlate with the current time period. They are easily understood.
I really loved how several important medical terms, including specific treatments were highlighted to alert the reader. Many interventions performed were also explained further, which is great to enhance learning for the nursing student or novice nurse. Also, with each scenario, a background and history of the patient is depicted, as well as the perspectives of the patient, patients family member, and the primary nurse. This really helps to give the reader a full picture of the day in the life of a nurse or a patient, and also better facilitates the learning process of the reader.
These case studies are consistent. They begin with report, the patient background or updates on subsequent days, and follow the patients all the way through discharge. Once again, I really appreciate how this book describes most if not all aspects of patient care on a day to day basis.
Each case study is separated into days. While they can be divided to be assigned at different points within the course, they also build on each other. They show trends in vital signs, what happens when a patient deteriorates, what happens when they get better and go home. Showing the entire process from ER admit to discharge is really helpful to enhance the students learning experience.
The topics are all presented very similarly and very clearly. The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough.
The book is very easy to navigate, prints well on paper, and is not distorted or confusing.
I did not see any grammatical errors.
Each case study involves a different type of patient. These differences include race, gender, sexual orientation and medical backgrounds. I do not feel the text was offensive to the reader.
I teach practical nursing students and after reading this book, I am looking forward to implementing it in my classroom. Great read for nursing students!
Reviewed by Leah Jolly, Instructor, Clinical Coordinator, Oregon Institute of Technology on 4/10/19
Good variety of cases and pathologies covered. read more
Good variety of cases and pathologies covered.
Content Accuracy rating: 2
Some examples and scenarios are not completely accurate. For example in the DVT case, the sonographer found thrombus in the "popliteal artery", which according to the book indicated presence of DVT. However in DVT, thrombus is located in the vein, not the artery. The patient would also have much different symptoms if located in the artery. Perhaps some of these inaccuracies are just typos, but in real-life situations this simple mistake can make a world of difference in the patient's course of treatment and outcomes.
Good examples of interprofessional collaboration. If only it worked this way on an every day basis!
Clear and easy to read for those with knowledge of medical terminology.
Good consistency overall.
Broken up well.
Topics are clear and logical.
Would be nice to simply click through to the next page, rather than going through the table of contents each time.
Minor typos/grammatical errors.
No offensive or insensitive materials observed.
Reviewed by Alex Sargsyan, Doctor of Nursing Practice/Assistant Professor , East Tennessee State University on 10/8/18
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study. read more
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study.
Overall the book is accurately depicting the clinical environment. There are numerous references to external sites. While most of them are correct, some of them are not working. For example Homan’s test link is not working "404 error"
Book is relevant in its current version and can be used in undergraduate and graduate classes. That said, the longevity of the book may be limited because of the character of the clinical education. Clinical guidelines change constantly and it may require a major update of the content.
Cases are written very clearly and have realistic description of an inpatient setting.
The book is easy to read and consistent in the language in all eight cases.
The cases are very well written. Each case is subdivided into logical segments. The segments reflect different setting where the patient is being seen. There is a flow and transition between the settings.
Book has eight distinct cases. This is a great format for a book that presents distinct clinical issues. This will allow the students to have immersive experiences and gain better understanding of the healthcare environment.
Book is offered in many different formats. Besides the issues with the links mentioned above, overall navigation of the book content is very smooth.
Book is very well written and has no grammatical errors.
Book is culturally relevant. Patients in the case studies come different cultures and represent diverse ethnicities.
Reviewed by Justin Berry, Physical Therapist Assistant Program Director, Northland Community and Technical College, East Grand Forks, MN on 8/2/18
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles,... read more
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles, interprofessional roles, when to initiate communication with other healthcare practitioners due to a change in patient status, and treatment ideas. Some additional patient information, such as lab values, would have been beneficial to include.
Case study information is accurate and unbiased.
Content is up to date. The case studies are written in a way so that they will not be obsolete soon, even with changes in healthcare.
The case studies are well written, and can be utilized for a variety of classroom assignments, discussions, and projects. Some additional lab value information for each patient would have been a nice addition.
The case studies are consistently organized to make it easy for the reader to determine the framework.
The text is broken up into eight different case studies for various patient diagnoses. This design makes it highly modular, and would be easy to assign at different points of a course.
The flow of the topics are presented consistently in a logical manner. Each case study follows a patient chronologically, making it easy to determine changes in patient status and treatment options.
The text is free of interface issues, with no distortion of images or charts.
The text is not culturally insensitive or offensive in any way. Patients are represented from a variety of races, ethnicities, and backgrounds
This book would be a good addition for many different health programs.
Reviewed by Ann Bell-Pfeifer, Instructor/Program Director, Minnesota State Community and Technical College on 5/21/18
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical... read more
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical laboratory technologists, medical radiology technologists, and respiratory therapists and their roles in caring for patients. Most of the overview is accurate. One suggestion is to provide an embedded radiologist interpretation of the exams which are performed which lead to the patients diagnosis.
Overall the book is accurate. Would like to see updates related to the addition of direct radiography technology which is commonly used in the hospital setting.
Many aspects of medicine will remain constant. The case studies seem fairly accurate and may be relevant for up to 3 years. Since technology changes so quickly in medicine, the CT and x-ray components may need minor updates within a few years.
The book clarity is excellent.
The case stories are consistent with each scenario. It is easy to follow the structure and learn from the content.
The book is quite modular. It is easy to break it up into cases and utilize them individually and sequentially.
The cases are listed by disease process and follow a logical flow through each condition. They are easy to follow as they have the same format from the beginning to the end of each case.
The interface seems seamless. Hyperlinks are inserted which provide descriptions and references to medical procedures and in depth definitions.
The book is free of most grammatical errors. There is a place where a few words do not fit the sentence structure and could be a typo.
The book included all types of relationships and ethnic backgrounds. One type which could be added is a transgender patient.
I think the book was quite useful for a variety of health care professionals. The authors did an excellent job of integrating patient cases which could be applied to the health care setting. The stories seemed real and relevant. This book could be used to teach health care professionals about integrated care within the emergency department.
Reviewed by Shelley Wolfe, Assistant Professor, Winona State University on 5/21/18
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should... read more
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should be noted that the authors include a statement that conveys that this text is not like traditional textbooks and is not meant to be read in a linear fashion. This allows the educator more flexibility to use the text as a supplement to enhance learning opportunities.
The content of the text appears accurate and unbiased. The “five overarching learning objectives” provide a clear aim of the text and the educator is able to glean how these objectives are captured into each of the case studies. While written for the Canadian healthcare system, this text is easily adaptable to the American healthcare system.
Overall, the content is up-to-date and the case studies provide a variety of uses that promote longevity of the text. However, not all of the blue font links (if using the digital PDF version) were still in working order. I encountered links that led to error pages or outdated “page not found” websites. While the links can be helpful, continued maintenance of these links could prove time-consuming.
I found the text easy to read and understand. I enjoyed that the viewpoints of all the different roles (patient, nurse, lab personnel, etc.) were articulated well and allowed the reader to connect and gain appreciation of the entire healthcare team. Medical jargon was noted to be appropriate for the intended audience of this text.
The terminology and organization of this text is consistent.
The text is divided into 8 case studies that follow a similar organizational structure. The case studies can further be divided to focus on individual learning objectives. For example, the case studies could be looked at as a whole for discussing communication or could be broken down into segments to focus on disease risk factors.
The case studies in this text follow a similar organizational structure and are consistent in their presentation. The flow of individual case studies is excellent and sets the reader on a clear path. As noted previously, this text is not meant to be read in a linear fashion.
This text is available in many different forms. I chose to review the text in the digital PDF version in order to use the embedded links. I did not encounter significant interface issues and did not find any images or features that would distract or confuse a reader.
No significant grammatical errors were noted.
The case studies in this text included patients and healthcare workers from a variety of backgrounds. Educators and students will benefit from expanding the case studies to include discussions and other learning opportunities to help develop culturally-sensitive healthcare providers.
I found the case studies to be very detailed, yet written in a way in which they could be used in various manners. The authors note a variety of ways in which the case studies could be employed with students; however, I feel the authors could also include that the case studies could be used as a basis for simulated clinical experiences. The case studies in this text would be an excellent tool for developing interprofessional communication and collaboration skills in a variety healthcare students.
Reviewed by Darline Foltz, Assistant Professor, University of Cincinnati - Clermont College on 3/27/18
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks... read more
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks Clinical Procedures for Safer Patient Care and Anatomy and Physiology: OpenStax" as noted by the authors.
The book appears to be accurate. Although one of the learning outcomes is as follows: "Demonstrate an understanding of the Canadian healthcare delivery system.", I did not find anything that is ONLY specific to the Canadian healthcare delivery system other than some of the terminology, i.e. "porter" instead of "transporter" and a few french words. I found this to make the book more interesting for students rather than deter from it. These are patient case studies that are relevant in any country.
The content is up-to-date. Changes in medical science may occur, i.e. a different test, to treat a diagnosis that is included in one or more of the case studies, however, it would be easy and straightforward to implement these changes.
This book is written in lucid, accessible prose. The technical/medical terminology that is used is appropriate for medical and allied health professionals. Something that would improve this text would to provide a glossary of terms for the terms in blue font.
This book is consistent with current medical terminology
This text is easily divided into each of the 6 case studies. The case studies can be used singly according to the body system being addressed or studied.
Because this text is a collection of case studies, flow doesn't pertain, however the organization and structure of the case studies are excellent as they are clear and easy to read.
There are no distractions in this text that would distract or confuse the reader.
I did not identify any grammatical errors.
This text is not culturally insensitive or offensive in any way and uses patients and healthcare workers that are of a variety of races, ethnicities and backgrounds.
I believe that this text would not only be useful to students enrolled in healthcare professions involved in direct patient care but would also be useful to students in supporting healthcare disciplines such as health information technology and management, medical billing and coding, etc.
Table of Contents
- Introduction
Case Study #1: Chronic Obstructive Pulmonary Disease (COPD)
- Learning Objectives
- Patient: Erin Johns
- Emergency Room
Case Study #2: Pneumonia
- Day 0: Emergency Room
- Day 1: Emergency Room
- Day 1: Medical Ward
- Day 2: Medical Ward
- Day 3: Medical Ward
- Day 4: Medical Ward
Case Study #3: Unstable Angina (UA)
- Patient: Harj Singh
Case Study #4: Heart Failure (HF)
- Patient: Meryl Smith
- In the Supermarket
- Day 0: Medical Ward
Case Study #5: Motor Vehicle Collision (MVC)
- Patient: Aaron Knoll
- Crash Scene
- Operating Room
- Post Anaesthesia Care Unit (PACU)
- Surgical Ward
Case Study #6: Sepsis
- Patient: George Thomas
- Sleepy Hollow Care Facility
Case Study #7: Colon Cancer
- Patient: Fred Johnson
- Two Months Ago
- Pre-Surgery Admission
Case Study #8: Deep Vein Thrombosis (DVT)
- Patient: Jamie Douglas
Appendix: Overview About the Authors
Ancillary Material
About the book.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
The case studies can be used online in a learning management system, in a classroom discussion, in a printed course pack or as part of a textbook created by the instructor. This flexibility is intentional and allows the educator to choose how best to convey the concepts presented in each case to the learner.
Because these case studies were primarily developed for an electronic healthcare system, they are based predominantly in an acute healthcare setting. Educators can augment each case study to include primary healthcare settings, outpatient clinics, assisted living environments, and other contexts as relevant.
About the Contributors
Glynda Rees teaches at the British Columbia Institute of Technology (BCIT) in Vancouver, British Columbia. She completed her MSN at the University of British Columbia with a focus on education and health informatics, and her BSN at the University of Cape Town in South Africa. Glynda has many years of national and international clinical experience in critical care units in South Africa, the UK, and the USA. Her teaching background has focused on clinical education, problem-based learning, clinical techniques, and pharmacology.
Glynda‘s interests include the integration of health informatics in undergraduate education, open accessible education, and the impact of educational technologies on nursing students’ clinical judgment and decision making at the point of care to improve patient safety and quality of care.
Faculty member in the critical care nursing program at the British Columbia Institute of Technology (BCIT) since 2003, Rob has been a critical care nurse for over 25 years with 17 years practicing in a quaternary care intensive care unit. Rob is an experienced educator and supports student learning in the classroom, online, and in clinical areas. Rob’s Master of Education from Simon Fraser University is in educational technology and learning design. He is passionate about using technology to support learning for both faculty and students.
Part of Rob’s faculty position is dedicated to providing high fidelity simulation support for BCIT’s nursing specialties program along with championing innovative teaching and best practices for educational technology. He has championed the use of digital publishing and was the tech lead for Critical Care Nursing’s iPad Project which resulted in over 40 multi-touch interactive textbooks being created using Apple and other technologies.
Rob has successfully completed a number of specialist certifications in computer and network technologies. In 2015, he was awarded Apple Distinguished Educator for his innovation and passionate use of technology to support learning. In the past five years, he has presented and published abstracts on virtual simulation, high fidelity simulation, creating engaging classroom environments, and what the future holds for healthcare and education.
Janet Morrison is the Program Head of Occupational Health Nursing at the British Columbia Institute of Technology (BCIT) in Burnaby, British Columbia. She completed a PhD at Simon Fraser University, Faculty of Communication, Art and Technology, with a focus on health information technology. Her dissertation examined the effects of telehealth implementation in an occupational health nursing service. She has an MA in Adult Education from St. Francis Xavier University and an MA in Library and Information Studies from the University of British Columbia.
Janet’s research interests concern the intended and unintended impacts of health information technologies on healthcare students, faculty, and the healthcare workforce.
She is currently working with BCIT colleagues to study how an educational clinical information system can foster healthcare students’ perceptions of interprofessional roles.
Contribute to this Page
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 1
- What is a case study?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Roberta Heale 1 ,
- Alison Twycross 2
- 1 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr Roberta Heale, School of Nursing, Laurentian University, Sudbury, ON P3E2C6, Canada; rheale{at}laurentian.ca
https://doi.org/10.1136/eb-2017-102845
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is it?
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research. 1 However, very simply… ‘a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units’. 1 A case study has also been described as an intensive, systematic investigation of a single individual, group, community or some other unit in which the researcher examines in-depth data relating to several variables. 2
Often there are several similar cases to consider such as educational or social service programmes that are delivered from a number of locations. Although similar, they are complex and have unique features. In these circumstances, the evaluation of several, similar cases will provide a better answer to a research question than if only one case is examined, hence the multiple-case study. Stake asserts that the cases are grouped and viewed as one entity, called the quintain . 6 ‘We study what is similar and different about the cases to understand the quintain better’. 6
The steps when using case study methodology are the same as for other types of research. 6 The first step is defining the single case or identifying a group of similar cases that can then be incorporated into a multiple-case study. A search to determine what is known about the case(s) is typically conducted. This may include a review of the literature, grey literature, media, reports and more, which serves to establish a basic understanding of the cases and informs the development of research questions. Data in case studies are often, but not exclusively, qualitative in nature. In multiple-case studies, analysis within cases and across cases is conducted. Themes arise from the analyses and assertions about the cases as a whole, or the quintain, emerge. 6
Benefits and limitations of case studies
If a researcher wants to study a specific phenomenon arising from a particular entity, then a single-case study is warranted and will allow for a in-depth understanding of the single phenomenon and, as discussed above, would involve collecting several different types of data. This is illustrated in example 1 below.
Using a multiple-case research study allows for a more in-depth understanding of the cases as a unit, through comparison of similarities and differences of the individual cases embedded within the quintain. Evidence arising from multiple-case studies is often stronger and more reliable than from single-case research. Multiple-case studies allow for more comprehensive exploration of research questions and theory development. 6
Despite the advantages of case studies, there are limitations. The sheer volume of data is difficult to organise and data analysis and integration strategies need to be carefully thought through. There is also sometimes a temptation to veer away from the research focus. 2 Reporting of findings from multiple-case research studies is also challenging at times, 1 particularly in relation to the word limits for some journal papers.
Examples of case studies
Example 1: nurses’ paediatric pain management practices.
One of the authors of this paper (AT) has used a case study approach to explore nurses’ paediatric pain management practices. This involved collecting several datasets:
Observational data to gain a picture about actual pain management practices.
Questionnaire data about nurses’ knowledge about paediatric pain management practices and how well they felt they managed pain in children.
Questionnaire data about how critical nurses perceived pain management tasks to be.
These datasets were analysed separately and then compared 7–9 and demonstrated that nurses’ level of theoretical did not impact on the quality of their pain management practices. 7 Nor did individual nurse’s perceptions of how critical a task was effect the likelihood of them carrying out this task in practice. 8 There was also a difference in self-reported and observed practices 9 ; actual (observed) practices did not confirm to best practice guidelines, whereas self-reported practices tended to.
Example 2: quality of care for complex patients at Nurse Practitioner-Led Clinics (NPLCs)
The other author of this paper (RH) has conducted a multiple-case study to determine the quality of care for patients with complex clinical presentations in NPLCs in Ontario, Canada. 10 Five NPLCs served as individual cases that, together, represented the quatrain. Three types of data were collected including:
Review of documentation related to the NPLC model (media, annual reports, research articles, grey literature and regulatory legislation).
Interviews with nurse practitioners (NPs) practising at the five NPLCs to determine their perceptions of the impact of the NPLC model on the quality of care provided to patients with multimorbidity.
Chart audits conducted at the five NPLCs to determine the extent to which evidence-based guidelines were followed for patients with diabetes and at least one other chronic condition.
The three sources of data collected from the five NPLCs were analysed and themes arose related to the quality of care for complex patients at NPLCs. The multiple-case study confirmed that nurse practitioners are the primary care providers at the NPLCs, and this positively impacts the quality of care for patients with multimorbidity. Healthcare policy, such as lack of an increase in salary for NPs for 10 years, has resulted in issues in recruitment and retention of NPs at NPLCs. This, along with insufficient resources in the communities where NPLCs are located and high patient vulnerability at NPLCs, have a negative impact on the quality of care. 10
These examples illustrate how collecting data about a single case or multiple cases helps us to better understand the phenomenon in question. Case study methodology serves to provide a framework for evaluation and analysis of complex issues. It shines a light on the holistic nature of nursing practice and offers a perspective that informs improved patient care.
- Gustafsson J
- Calanzaro M
- Sandelowski M
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Educ Curric Dev
- v.3; Jan-Dec 2016
Case-Based Learning and its Application in Medical and Health-Care Fields: A Review of Worldwide Literature
Susan f. mclean.
Department of Surgery, Texas Tech University Health Sciences Center El Paso, El Paso, TX, USA.
Introduction
Case-based learning (CBL) is a newer modality of teaching healthcare. In order to evaluate how CBL is currently used, a literature search and review was completed.
A literature search was completed using an OVID© database using PubMed as the data source, 1946-8/1/2015. Key words used were “Case-based learning” and “medical education”, and 360 articles were retrieved. Of these, 70 articles were selected to review for location, human health care related fields of study, number of students, topics, delivery methods, and student level.
All major continents had studies on CBL. Education levels were 64% undergraduate and 34% graduate. Medicine was the most frequently represented field, with articles on nursing, occupational therapy, allied health, child development and dentistry. Mean number of students per study was 214 (7–3105). The top 3 most common methods of delivery were live presentation in 49%, followed by computer or web-based in 20% followed by mixed modalities in 19%. The top 3 outcome evaluations were: survey of participants, knowledge test, and test plus survey, with practice outcomes less frequent. Selected studies were reviewed in greater detail, highlighting advantages and disadvantages of CBL, comparisons to Problem-based learning, variety of fields in healthcare, variety in student experience, curriculum implementation, and finally impact on patient care.
Conclusions
CBL is a teaching tool used in a variety of medical fields using human cases to impart relevance and aid in connecting theory to practice. The impact of CBL can reach from simple knowledge gains to changing patient care outcomes.
Medical and health care-related education is currently changing. Since the advent of adult education, educators have realized that learners need to see the relevance and be actively engaged in the topic under study. 1 Traditionally, students in health care went to lectures and then transitioned into patient care as a type of on-the-job training. Medical schools have realized the importance of including clinical work early and have termed the mixing of basic and clinical sciences as vertical integration. 2 Other human health-related fields have also recognized the value of illustrating teaching points with actual cases or simulated cases. Using clinical cases to aid teaching has been termed as case-based learning (CBL).
There is not a set definition for CBL. An excellent definition has been proposed by Thistlewaite et al in a review article. In their 2012 paper, a CBL definition is “The goal of CBL is to prepare students for clinical practice, through the use of authentic clinical cases. It links theory to practice, through the application of knowledge to the cases, using inquiry-based learning methods”. 3
Others have defined CBL by comparing CBL to a similar yet distinct clinical integration teaching method, problem-based learning (PBL). PBL sessions typically used one patient and had very little direction to the discussion of the case. The learning occurred as the case unfolded, with students having little advance preparation and often researching during the case. Srinivasan et al compared CBL with PBL 4 and noted that in PBL the student had little advance preparation and very little guidance during the case discussion. However, in CBL, both the student and faculty prepare in advance, and there is guidance to the discussion so that important learning points are covered. In a survey of students and faculty after a United States medical school switched from PBL to CBL, students reported that they enjoyed CBL better because there were fewer unfocused tangents. 4
CBL is currently used in multiple health-care settings around the world. In order to evaluate what is now considered CBL, current uses of CBL, and evaluation strategies of CBL-based curricular elements, a literature review was completed.
This review will focus on human health-related applications of CBL-type learning. A summary of articles reviewed is presented with respect to fields of study, delivery options for CBL, locations of study, outcomes measurement if any, number of learners, and level of learner's education. These findings will be discussed. The rest of this review will focus on expanding on the article summary by describing in more detail the publications that reported on CBL. The review is organized into definitions of CBL, comparison of CBL with PBL, and the advantages of using CBL. The review will also examine the utility and usage of CBL with respect to various fields and levels of learner, as well as the methods of implementation of CBL in curricula. Finally, the impact of CBL training on patient and health-care outcomes will be reviewed. One wonders with the proliferation of articles that have CBL in the title, whether or not there has been literature defining exactly what CBL is, how it is used, and whether or not there are any advantages to using CBL over other teaching strategies. The rationale for completing this review is to assess CBL as a discrete mode of transmitting medical and related fields of knowledge. A systematic review of how CBL is accomplished, including successes and failures in reports of CBL in real curricula, would aid other teachers of medical knowledge in the future. Examining the current use of CBL would improve the current methodology of CBL. Therefore, the aims of this review are to discover how widespread the use of CBL is globally, identify current definitions of CBL, compare CBL with PBL, review educational levels of learners, compare methods of implementation of CBL in curricula, and review CBL reports on outcomes of learning.
A literature search was completed using an OVID© database search with PubMed as the database, 1946 to August 1, 2015. The search key words were “Case Based Learning, Medical Education”. Investigational Review Board declined to review this project as there were no human subjects involved and this was an article review. A total of 360 articles were retrieved. Articles were excluded for the following reasons: unable to find complete article on the search engine OVID, unable to find English language translation, article did not really describe CBL, article was not medically or health related, or article did not describe human beings. Articles that originated in another language but had English language translation were included.
After excluding the articles as described, 70 of these articles were selected to review for location of study, description of CBL used, human health care-related fields of study, number of students if available, topics of study, method of delivery, and level of student (eg, graduate or undergraduate). Students were considered undergraduate if they were considered undergraduate in their field. For example, medical students were considered undergraduate, because they would still have to undergo more training to become fully able to practice. If the student was in the terminal degree, then that was considered a study of graduate students. For example, nutrition students were listed as graduate students. CBL encounters for both residents and independent practitioners who were in their final training prior to practice were listed as graduates. Residents were listed under graduate medical education. If a group had already graduated, they were listed as graduates. For example, MDs who participated in a continuing medical education (CME)-type CBL were listed as graduate type of student. Articles that did not list the total number of students were included, as one of the purposes of this review was to discover how widespread the use of CBL was globally, and what types of students and types of delivery were used. By including descriptive articles that were not specific, the global use of CBL could attempt to be assessed. Including locations of studies would then help decide whether CBL was isolated from the Western countries or has it truly spread around the world.
In order to review how CBL was used, in addition to where it was used, the method of delivery was assessed. Method of delivery refers to how the total educational content was delivered. Articles were reviewed for description of exactly how material was imparted to learners. Since many authors described their learning methods in detail, an attempt was undertaken to classify these methods. Method of delivery was classified as follows: live was considered a live presentation of the case, this could be a description, a patient, or a simulated patient. Computer or web based meant that the case and content were web based. Mixed modalities meant that more than two modalities were used during presentation. For example, if an article described assigned reading, lectures, small group discussions, a live case-based session, and patient interactions, then that article would be described as mixed modalities.
Method of evaluation of the educational intervention was also reviewed. The multiple ways in which the interventions were evaluated varied. A survey of how the learners viewed the intervention was frequent. Tests of knowledge gained were frequent, and these ranged from written, to oral, to Observed Skills Clinical Examination (OSCE). Another way by which CBL intervention knowledge was evaluated was review of practice behavior in clinicians. These multiple ways to evaluate the introduction of CBL into a curriculum are summarized in a table.
Results are presented in simple frequencies and percentages. SPSS (Statistical Program for the Social Sciences, IBM) version 22 was used for analysis.
All continuously inhabited continents had studies on CBL ( Fig. 1 ). North America is represented with the most with 54.9% of articles, followed by Europe (25.4%) and Asia, including India, Australia, and New Zealand (15.5%). South America had 2.8% and Africa had 1%. 5 – , 75

CBL use worldwide.
Level of education was undergraduation in 45 (64%) articles and graduation in 24 (34%) articles, with one article having both levels. One study with both faculty and residents was considered as a type of graduate education. The types of fields of study varied ( Fig. 2 ). The most represented field was medicine including traditional Chinese medicine, with articles also on nursing, occupational therapy, allied health, child development, and dentistry. The number of students ranged from 7 to 3105 and the mean number of students was 214. One study reported on the use of teams of critical care personnel, in which it was mentioned that there were three persons per team usually. Thus, the number of students was multiplied: 40 teams x 3 = 120 in total. The total number of students were 9884 from the 46 papers that explicitly stated the number of students.

Fields of study.
Methods of delivery also varied ( Fig. 3 ). The most common method of delivery was live presentation (49%), followed by computer or web based (20%) and then mixed modalities (19%). Method of evaluation or outcomes was studied ( Fig. 4 ). Survey (36%), test (17%), and test plus survey (16%) were the top three methods of evaluation of a CBL learning session. Lesser in frequency was review of practice behavior (9%), test plus OSCE (9%), and others. Review of practice behavior could include reviewing prescription writing, or in one case reviewing the number of adverse drug events reported spontaneously in Portugal. 65

Mode of delivery of CBL.

Method of evaluation.
Discussion and Review
CBL is used worldwide. There was a large variety of fields of medicine. The numbers reported included a wide range of number of learners. Some studies were descriptive, and it was hard to know exactly how many students were involved. This problem was noted in another recent review. 3 CBL was used in various educational levels, from undergraduate to graduate. The number of students ranged from very small studies of 7 students to over 3000 students. The media used to deliver a CBL session varied, from several live forms to paper and pencil or internet-based media. The outcomes measurement to review if CBL sessions were successful ranged from surveys of participants to knowledge tests to measures of patient outcomes. In order to further analyze the worldwide use of CBL, the articles are reviewed below in more detail.
Definition of CBL
CBL has been used in medical fields since at least 1912, when it was used by Dr. James Lorrain Smith while teaching pathology in 1912 at the University of Edinburgh. 63 , 68 Thistlewaite et al 3 pointed out in a recent review of CBL that “There is no international consensus as to the definition of case-based learning (CBL) though it is contrasted to problem based learning (PBL) in terms of structure. We conclude that CBL is a form of inquiry based learning and fits on the continuum between structured and guided learning.” They offer a definition of CBL: “The goal of CBL is to prepare students for clinical practice, through the use of authentic clinical cases. It links theory to practice, through the application of knowledge to the cases, using inquiry-based learning methods.” 3
Another pathology article from Africa, describing a course in laboratory medicine for mixed graduate medical education (residents) and CME for clinicians, defines CBL: “Case-based learning is structured so that trainees explore clinically relevant topics using open-ended questions with well-defined goals.” 7 The exploring that students or trainees do factors into other definitions. In a dental education article originating in Turkey, the authors remark: “The advantages of the case-based method are promotion of self-directed learning, clinical reasoning, clinical problem solving, and decision making by providing repeated experiences in class and by enabling students to focus on the complexity of clinical care.” 8 Another definition of CBL was offered in a physiology education paper regarding teaching undergraduate medical students in India: “What is CBL? By discussing a clinical case related to the topic taught, students evaluated their own understanding of the concept using a high order of cognition. This process encourages active learning and produces a more productive outcome.” 13 In an article published in 2008, regarding teaching graduate pharmacology students, CBL was defined as “Case-based learning (CBL) is an active-learning strategy, much like problem-based learning, involving small groups in which the group focuses on solving a presented problem.” 45 Another study, which was from China regarding teaching undergraduate medical student's pharmacology, describes CBL as “CBL is a long-established pedagogical method that focuses on case study teaching and inquiry-based learning: thus, CBL is on the continuum between structured and guided learning.” 63 It is apparent that the definition requires at least: (1) a clinical case, (2) some kind of inquiry on the part of the learner, which is all of the information to be learned, is not presented at first, (3) enough information presented so that there is not too much time spent learning basics, and (4) a faculty teaching and guiding the discussion, ensuring that learning objectives are met. In most studies, CBL is not presented as free inquiry. The inquiry may be a problem or question. Based on the fact that a problem is expected to be solved or question answered, the information covered cannot be completely new, or the new information must be presented alongside the case.
A modern definition of CBL is that CBL is a form of learning, which involves a clinical case, a problem or question to be solved, and a stated set of learning objectives with a measured outcome. Included in this definition is that some, but not all, of the information is presented prior to or during the learning intervention, and some of the information is discovered during the problem solving or question answering. The learner acquires some of the learning objectives during the CBL session, whether it is live, web based, or on paper. In contrast, if all of the information were given prior or during the session, without the need for inquiry, then the session would just be a lecture or reading.
Comparison of CBL and PBL
CBL is not the first and only method of inquiry-based education. PBL is similar, with distinct differences ( Fig. 5 ). In many papers, CBL is compared and contrasted with PBL in order to define CBL better. PBL is also centered around a clinical case. Often the objectives are less clearly defined at the outset of the learning session, and learning occurs in the course of solving the problem. There is a teacher, but the teacher is less intrusive with the guidance than in CBL. One comparison of CBL to PBL was described in an article on Turkish dental school education: “… CBL is effective for students who have already acquired foundational knowledge, whereas PBL invites the student to learn foundational knowledge as part of researching the clinical case.” Study, of postgraduate education in an American Obstetrics and Gynecology residency, describes CBL as “CBL is a variant of PBL and involves a case vignette that is designed to reflect the educational objectives of a particular topic.” 54 In an overview of CBL and PBL in a dental education article from the United States, the authors note that the main focus of PBL is on the cases and CBL is more flexible in its use of clinical material. 16 The authors quote Donner and Bickley, 70 stating that PBL is “… a form of education in which information is mastered in the same context in which it will be used … PBL is seen as a student-driven process in which the student sets the pace, and the role of the teacher becomes one of guide, facilitator, and resource … (p294).” The authors note that where PBL has the student as the driver , in CBL the teachers are the drivers of education, guiding and directing the learning much more than in PBL. 16 The authors also note that there has not been conclusive evidence that PBL is better than traditional lecture-based learning (LBL) and has been noted to cover less material, some say 80% of a curriculum. 71 It is apparent that PBL has been used to aid case-related teaching in medical fields.

Differences in CBL and PBL.
Two studies highlight the advantages and disadvantages of CBL compared with PBL. Both studies report on major curriculum shifts at three major medical schools. The first study, published in 2005, reported on the performance outcomes during the third-year clerkship rotations at Southern Illinois University (SIU). 19 At SIU, during the 1994–2002 school years, there was both a standard (STND) and PBL learning tract offered for the preclinical years, years 1–2. During the PBL tract, basics of medicine were taught in small group tutoring sessions using PBL modules and standardized patients. In addition, there was a weekly live clinical session. The two tracts were compared over all those years with respect to United States Medical Licensing Exam© (USMLE) test performance on Steps 1 and 2, and also overall grades and subcategories on the six third-year clerkships. So the two tracks had differing years 1–2 and the same year 3. Results noted that the PBL track had more women and older students, so these variables were set out as covariates analyzing other scores. Comparing the PBL versus STND tracks, USMLE scores were statistically equal over the years 1994–2002. PBL was 204.90 ± 21.05 and STND was 205.09 ± 23.07 ( P , 0.92); Step 2 scores were PBL 210.17 ± 21.83, STND 201.32 ± 23.25 ( P , 0.15). Clerkship overall scores were overall statistically significantly higher for PBL tract students in Obstetrics and Gynecology and Psychiatry ( P = 0.02, P < 0.001, respectively) and statistically not different for other clerkships. Clerkship subcategory analysis demonstrated statistically significantly higher scores for PBL tract students in clinical performance, knowledge and clinical reasoning, noncognitive behaviors, and percent honors grades, with no difference in the percentage of remediations. The school decided to switch to a single-tract curriculum after 2002. The problems noted with the PBL curriculum involved recruiting PBL faculty and faculty acceptance of student interactions, and also assessment issues. Faculty had to be trained to teach in PBL, which was time consuming and interfered with the process of learning by students. In addition, some faculty felt that the teachers should determine the learner's needs and not vice versa. The PBL assessment tools were novel and not immediately accepted by the faculty. 19 Other schools noted similar problems with PBL: it is different than LBL, and difficult to teach, as it is extremely learner centered. Learning objectives are essentially generated by the student, making faculty control over learning difficult. At this school, the difficulties in using PBL contributed to its abandonment as a stand-alone curriculum tract.
The difficulties in using PBL were associated with changes in other medical schools. Two medical schools in the United States, namely, University of California, Los Angeles, and University of California, Davis, changed from a PBL method to a CBL method for teaching a course entitled Doctoring , which was a small group faculty led course given over years 1–3 in both schools. 4 Both schools had a typical PBL approach, with little student advance preparation, little faculty direction during the session, and a topic that was initially unknown to the student. After the shift in curriculum to CBL, there were still small group sessions, but the students were expected to do some advance reading, and the faculty members were instructed to guide or direct the problem solving. Since in both schools the students and faculty had some experience with PBL before the shift, a survey was used to assess student and faculty experiences and perceptions of the two methods. Both students and faculty preferred CBL (89% of students and 84% of faculty favored CBL). Reasons for preference of CBL over PBL were as follows: fewer unfocused tangents (59% favoring CBL, odds ratio [OR] 4.10, P = 0.01), less busywork (80% favoring CBL, OR 3.97 and P = 0.01), and more opportunities for clinical skills application (52%, OR 25.6, P = 0.002). 4 In summary, these two reports indicate that while a case-oriented learning session can prepare students for both tests of knowledge and also clinical reasoning, PBL has the problems of difficult to initiate faculty or teachers in teaching this way, difficult to cover a large amount of clinical ground, and difficulty in assessment. CBL, on the other hand, has advantages of flexibility in using the case and offers the same reality base that offers relevance for the adult health-care learner. In addition, CBL appears to be accepted by the faculty that may be practicing clinicians and offers a way to teach specific learning objectives. These advantages of CBL led to it being the preferred method of case-related learning at these two large medical schools.
Advantages of CBL and deeper learning
Another touted advantage of CBL is deeper learning. That is, learning that goes beyond simple identification of correct answers and is more aligned with either evidence of critical thinking or changes in behavior and generalizability of learning to new cases. Several articles described this aspect of CBL. One article was set at a tertiary care hospital, the Mayo Clinic, and was a teaching model for quality improvement to prevent patient adverse events. 33 The students were clinicians, and the course was a continuing education or postgraduate course. The authors in the Quality Improvement, Information Technology, and Medical Education departments created an online CBL module with three cases representing the most common type of patient adverse events in internal medicine. The authors use Kirkpatrick's outcomes hierarchy to assess the level of critical thinking after the CBL intervention. Kirkpatrick's outcomes hierarchy is based on four levels: the first, reaction of learner to educational intervention, the second, actual learning: acquiring knowledge or skills, the third, behavior or generalizing lessons learned to actual practice, and the fourth, results that would be patient outcomes. 72 The authors note that as one moves up this hierarchy, learning is more difficult to measure. A survey can measure hierarchy level 1, a written test, and level 2. Behavior is more difficult but still able to be measured. The authors measured critical thinking in physicians, taking their Quality Improvement course by measuring critical reflection by a survey. The authors constructed a reflection survey, which asked course participants about items constructed to assess their level of reflection on the cases. Least reflective levels consisted of habitual action, and most critically, reflective items asked physicians if they would change the way they do things based on the cases. The results of their intervention showed that physicians had the lowest scores in reaching the higher levels of reflective thinking. However, the reflection scores were shown to be associated with physicians’ perceptions of case relevance ( P = 0.01) and event generalizability ( P = 0.001). This study was the first to evaluate physician's reflections after a CBL module on adverse events. The assumption is that deeper learning will be more likely to lead to behavioral changes.
Another attempt to measure deeper learning was reported from a dental school in Turkey. 8 The authors compared a CBL course with an older LBL course from the previous year by using “SOLO” taxonomy, developed by Biggs and Collis. 73 SOLO taxonomy rates the learning outcomes from prestructural through extended abstract. For example, in unistructural, the second item of SOLO, items could be “define”, “identify”, or “do a simple procedure”, whereas in the “extended abstract” level, the items are “evaluate”, “predict”, “generalize”, “create”, “reflect”, or “hypothesize” in higher mental order tasks. 8 A post-test was used to measure the responses on the test. The test questions were assigned to SOLO categories. In the first three categories of SOLO taxonomy questions, there was no statistical difference in scores between LBL and CBL groups. In the last two or higher categories of questions based on SOLO taxonomy, there was a statistically significant increase in the scores for relational and extended types of questions for the CBL group ( P = 0.014 and 0.026, respectively). This review shows a benefit in higher level learning using a CBL program. Again, the assumption is that by inducing higher order mental tasks, deeper learning will occur and behavioral change will follow.
Two other studies discussed the levels of thinking and preparation for practice. One study compared students in interdisciplinary (ID) versus single-discipline students (SD; clinical anatomy) in a Graduate School for Health Sciences in Missouri, U.S. The two groups had slightly different cases. The ID group had complex ID cases and answered multiple choice questions about the cases. The SD group had cases in their discipline and answered multiple choice cases around the case. The assessment tool was the Watson-Glaser Critical Thinking Appraisal. The mean scores of both groups were not statistically different. However, ID students who scored below the median on the pretest scored significantly higher on the posttest. While this study set out to compare the differences in SD vs ID teaching using CBL, it also compared the effects of an ID course on critical thinking and it appears to be synergistic with improving scores for students who started below the median on testing. This is important in education programs, because while mean scores may not rise, if less students are scoring lower, then less students will fail the course and have to repeat.
The second paper that attempted to measure higher learning outcomes queried dental school graduates who had completed a CBL course during their dental school training. 22 The survey was designed to assess the CBL curriculum with respect to actual job requirements of practicing dentists. The graduates spanned 16 years, from 1990 to 2006, and the survey was conducted in 2007–2008. The response rate was 41%. The findings were that the CBL course was associated with positive correlations in “research competence”, “interdisciplinary thinking”, “practical dental skills”, “team work”, and “independent learning/working”. Other items including “problem-solving skills”, “psycho-social competence”, and “business competence” were not scored as highly with respondents. This article measured self-reported competencies and not the competencies as assessed by independent observers. However, it does attempt to link CBL with the actual practice with which it was attempting to teach, which is one of the generally accepted benefits of CBL.
In summary, CBL is defined as an inquiry structured learning experience utilizing live or simulated patient cases to solve, or examine a clinical problem, with the guidance of a teacher and stated learning objectives. Advantages of using CBL include more focusing on learning objectives compared with PBL, flexibility on the use of the case, and ability to induce a deeper level of learning by inducing more critical thinking skills.
Uses of CBL with respect to various fields and various levels in health-care training
CBL is used to impart knowledge in various fields in health care and various fields of medicine. The findings in this review showed that articles demonstrated the use of CBL in medicine, 2 , 4 – , 7 , 9 , 10 , 12 – , 14 , 18 – , 21 , 24 – , 26 , 30 , 33 , 34 , 36 , 37 , 39 – , 44 , 46 , 48 – , 62 , 64 – , 67 dentistry, 8 , 15 , 16 , 22 , 23 , 28 pharmacology, 11 , 27 , 29 , 35 , 45 , 63 occupational and physical therapy, 31 nursing, 5 , 21 , 38 , 47 , 51 allied health fields, 32 and child development. 17
Eighteen fields of medicine were seen in this review, from internal medicine and surgery to palliative medicine and critical care ( Fig. 2 , “fields of study”). Several articles highlight ID care or interprofessional care. A 2011 article in critical care medicine demonstrated the utility of both simulators and CBL on behaviors in critical situations of critical care teams of physicians and nurses. 5 Palliative care 21 and primary care 51 , 59 articles also reported on using a CBL course for learning with physicians and nurses. An article from the United Arab Emirates discussed how CBL better prepared participants for critical situations as well as basic primary care. 59
CBL is also used in various levels, including undergraduate education in the professions, graduate education, and postgraduate education. One field that uses CBL for all levels is surgery. Several articles describe surgical undergraduate medical education. One article describes using a paper and pencil plus live review sessions on improving student knowledge as tested by a standardized test in surgery. 6 Another paper from Germany describes initiation of a CBL curriculum for medical students and lists the pitfalls in establishing this curriculum. 26 A third undergraduate paper in a medical school course in surgery describes utilizing CBL and a more structured curriculum to aid in knowledge gains. A study utilizing both surgical simulators for laparoscopic procedural skills and CBL for clinical knowledge and reasoning demonstrates learning enhancement using CBL in surgical residents, or graduate surgical training. 20 In this study, scores in both procedural ratings during surgery for residents and also knowledge scores when presented with complications from surgery both rated higher in the CBL-enhanced course. Graduate use of CBL in surgery is frequent. CME courses are taught in trauma, which features lectures, skill stations, and simulation-based CBL. 74 Advanced Trauma Life Support (ATLS) certification is required for all surgeons who practice in a designated trauma center in the United States. 74 In addition, the American College of Surgeons publishes a self-assessment course entitled “SESAP” or Surgical Education and Self-Assessment Program, which is a web or CD-ROM course that is largely case based, with commentaries. 75 These two courses are widely available and are constantly revised to reflect new advances in patient care research. The use of CBL programs was employed in undergraduate and graduate including postgraduate fields in this review.
Use of CBL in rural and underserved areas
One practical use of CBL is to use CBL to enhance knowledge in rural or underserved areas. An excellent example of CBL is the Project Extension for Community Healthcare Outcomes (ECHO) program in Arizona and Utah states, United States. 10 , 12 This program was based on the Project ECHO program initially devised at the University of New Mexico Health Sciences Center in 2003. 10 In Arizona and Utah, the CDC helped fund a program to teach primary care providers and also provide access to specialist to treat hepatitis C virus (HCV)-infected patients. The primary aim was to increase treatment, as new drugs have become available, which are highly effective in treating HCV. The program works by recruiting primary care physician to participate. An initial teaching session is held on site at the health-care clinic in the rural or underserved area. Then, the provider teams are asked to participate in “tele ECHO” clinics in which participants present cases and have experts in HCV treatment comment. There are also educational sessions. Ninety providers participated, with 66% or 73% being primary care providers in rural or community health centers and not at universities. Over one and a half years, 280 patients were enrolled with 46.1% starting treatment. Other patients were likely not able to be treated, as their laboratory values indicated advanced liver disease. The percentage starting treatment was more than twice as many as expected to receive treatment prior to the project, based on historical controls. In addition to showing how CBL can impact rural medical care, this study is an example of learning assessment measured in patient outcomes.
A second CBL project was used in the United Arab Emirates to train rural practitioner's vital aspects of primary and emergency care using a CBL project. 60 The learners were able to provide feedback to the teachers as to the topics needed. This demonstrates the potential for interaction between teachers and learners using CBL, as it is a practical way to teach active practitioners. A third demonstration of using CBL in rural areas is in a report on teaching laboratory medicine in Africa. 7 In Sub-Saharan Africa, there is low trust in laboratory medicine services due in part to lower the quality of laboratories. This problem directly impacts patient care. Multiple international agencies are assisting the clinical laboratories in Sub-Saharan Africa in order to improve the quality of service. According to this report, the quality problem has led to decreased trust in laboratory medicine in the region. The course, given at Addis Ababa University in Ethiopia, was initiated to provide knowledge and also increase trust in laboratory medicine. The participants were 21 residents (graduate medical education), 3 faculty members, and 4 laboratory workers. The course was structured with both lectures and cases. Students were given homework for the differing cases. The assessments were both knowledge gains and also surveys of satisfaction for the course. Ratings on the survey were by ratings on a Likert scale of 1 (least valuable) to 5 (most valuable). Regarding the methods of delivery, the CBL sessions were rated highest with 85% of learners rating them as most valuable. In all, 81% rated case discussions as most valuable. Lectures received the most valuable rating by 65%. On the 12 question pre-/posttest, the mean score rose and also the number of questions answered correctly by the majority of learners. 7 These reports from three continents demonstrate that CBL is a practical way to impart knowledge in a diverse range of topics to clinicians who may be remote from a medical university.
Delivery of CBL: implementation and media
As illustrated in the above examples of use of CBL in rural settings, CBL use is varied as to the delivery method and implementation. Several articles demonstrate the importance of preparation for use in CBL. As many practitioners and students in all fields likely have more experience with LBL, participating in a course with CBL requires a different strategy and mindset in order to reach learning objectives. Preparation of both students and teachers in a CBL format is also very important for success. Two studies highlight the preparation and implementation of CBL: one not as successful as the other. In a qualitative study of introducing a new CBL format series to undergraduate medical students based in Sweden, the authors found that preparation of both students and faculty was likely inadequate for complete success. This study, held at the Karolinska Institutet, described the implementation of a CBL format for learning surgery during a semester course. All LBL classes were replaced with CBL sessions. The authors noted that at this time, there were organizational obstacles to starting a CBL course: lack of time and funds for faculty training. As such, faculty training was delayed and decreased. The study was a survey of five students and five faculty, who were picked from larger pools. There was a lot of criticism by students that the CBL needed more structure, or that the faculty often turned the CBL session more into a lecture session. The faculty described problems with getting the students to engage, and also with the lack of preparation for teaching in that format. Still, the overall impression was that CBL could increase interactive learning for this level of student. 26 This study demonstrates how lack of adequate preparation can impact a CBL experience for both faculty and students.
Another article demonstrated the differences in student motivation for autonomous learning, which was different, depending on how CBL was introduced. In a study of child development students in Sweden, there were four group methods to compare how students learned, depending on how CBL was introduced. The four groups were as follows: (1) LLL or all lecture, (2) CCCC or all CBL, (3) LCLC in which lecture and CBL were alternated in each session after the introduction, and (4) LLCC, in which there were three sessions with all lectures, two mixed lecture plus CBL, and two CBL only lectures to finish. There was a knowledge pretest and post-test to assess what the authors call prior knowledge (pretest) and achievement (posttest). Student motivation for learning was assessed by means of a modified Academic Self-Regulation Scale. 76 The results were that achievement scores and also autonomous motivation were both the highest in the LLCC group, or the group in which CBL was introduced after LBL. The authors conclude that students are more prepared for CBL after some foundational knowledge is imparted. These two articles demonstrate that both teacher and student preparation is necessary for a successful CBL learning encounter.
Use of CBL to impact patients and measurement of results
As described earlier, the Kirkland model of learning and assessment of outcomes includes assessment of the results of the training as its final method of assessing an intervention. In other words, how did the training impact patient care or its surrogate marker? Four recent studies illustrated how CBL can impact patient care. 10 , 12 , 40 , 54 , 69 The first, already described, is the Project ECHO for HCV treatment, which resulted in 46.1% of patients in the areas affected being started on treatment, and a large proportion of those treated being started on the newer antivirals. The second study was a study on practices by primary care physicians on treating diabetic patients. In this study, 122 primary care physicians (Family and Internal Medicine) at 18 sites were divided into three groups to enhance diabetes care. Group A received surveys and no intervention and served as a control group; group B received Internet-based software with three cases in a virtual patient encounter. The cases had simulated time and could include laboratory and medication orders and follow-up visits. After the cases, the physicians received feedback in the form of what an expert would do. Group C received the same CBL as group B with the addition of 60 minutes of verbal feedback and instruction from a physician opinion leader. The authors were able to obtain clinical data for the results. The results were that group B had a significant decline in hemoglobin A1C measures, the most common means of assessing glucose control over time in diabetics, while groups A and C did not. Groups B and C had a significant decline in prescribing metformin in patients with contraindications also. This demonstrates favorable clinical results using a CBL intervention. 40 The third was a study to institute chlamydia screening in offices. While the intervention did not globally increase chlamydia screening, the impact was that there was less of a decay on chlamydia screening in the intervention groups. 54 The last study demonstrated a CBL study in Portugal, which demonstrated an increase in reporting of adverse drug events after a CBL intervention in a study population of over 4000 physicians. 69 These four articles describe the use of CBL to impart medical knowledge and the use of patient outcomes to assess that learned knowledge. This is the ultimate test of learning for health-care practitioners: knowledge that improves patient care.
Limitations of this Review
This review was an attempt to classify a term, case-based learning , which is used frequently. In reviewing articles, this term was used as a search term. It is possible that articles written which would fit the definition of CBL but were termed differently by the individuals writing that article might have been missed. In addition, foreign language articles were not retrieved if there was not an English translation. There may be additional articles that would be instructional in other languages. The higher number of articles retrieved from North America may be biased by using a United States database. In an attempt to describe the various articles, which were termed case-based learning , the methods of delivery and evaluation were described in terms familiar to medical personnel. In the learning situation, these terms might be describing slightly different experiences. For example, several articles described the use of an observed skills examination to evaluate the learner; this examination was classified as “observed skills clinical examination or OSCE”. These OSCEs might have been more, or less, stringent. In defense of the search strategy, since the objective of the article was to write about what is currently considered case-based learning , this item was used as the search term. In order to classify and further define what exactly is CBL and how it is used, putting into discrete categories the described methods of delivery and evaluation was necessary, or else the review would reduce to a listing of separate articles without being able to provide a meaningful commentary.
CBL is a tool that involves matching clinical cases in health care-related fields to a body of knowledge in that field, in order to improve clinical performance, attitudes, or teamwork. This type of learning has been shown to enhance clinical knowledge, improve teamwork, improve clinical skills, improve practice behavior, and improve patient outcomes. CBL advantages include providing relevance to the adult learner, allowing the teacher more input into the direction of learning, and inducing learning on a deeper level. Learners or students in health care-related fields will one day need to interact with patients, and so education that relates to patient is particularly relevant. Relevance is an important concept in adult education. CBL was found to be used in all continents. Even limiting the search to English and English translations, articles were found on all continuously inhabited continents. This finding demonstrates that the use of CBL is not isolated to Western countries, but is used worldwide. In addition, based on the number and variety of fields of medicine and health care reported, CBL is used across multiple fields.
In reviewing the worldwide use of CBL, several constants became apparent. One is that this involves a case as a stimulant for learning. The second is that advance preparation of the learner is necessary. The third is that a set of learning objectives must be adhered to. A comparison with PBL across several articles revealed that most teachers who use CBL, in contrast to PBL, need to get through a list of learning objectives, and in so doing, must provide enhanced guidance to the learning session. That adherence to learning objectives was evident in most articles. There were varied methods of delivery, depending on the learning situation. That is one of the practical aspects of learning sessions termed case-based learning or CBL. The teachers used cases within their realm of teaching and adapted a CBL approach to their situation; for example, live CBL might be used with medical students, video cases might be used with practitioners. CBL differs from PBL in that it can cover a larger amount of topics because of the stated learning objectives, and guidance from the teacher or facilitator who does not allow unguided tangents, which may delay covering the stated objectives. Contrasting CBL with CBL, in PBL, the focus is on the process of learning as much as the topic, whereas in CBL, the learning objectives are stated at the outset, and both learners and teachers try to adhere to these. Because there are stated objectives at the outset of the learning experience in CBL, these objectives can be tested to see if they are met. These tests of knowledge were explored as methods of evaluation, which varied.
The methods of evaluation ran the range of Kirkpatrick's hierarchy of learning. One of the important aspects of CBL which was explored was that perhaps CBL could induce learning on a deeper level. And so going up the hierarchy of learning, some evaluations were simple surveys of the learners/and or the teachers on how they liked the CBL intervention. Some were tests of knowledge or skills learned. A few studies evaluated practice behavior; that is, going beyond knowledge learned into what behaviors that knowledge induced. The last hierarchy was how the knowledge learned from CBL affected actual patients: a few studies revealed that patient outcomes were affected positively from CBL. Thus, published studies of CBL spanned the hierarchy of learning, from opinions of the activity to actual patients affected by the learning of practitioners.
In summary, CBL was found to be practiced worldwide, by various practitioners, in various fields. CBL delivery was found to be varied to the situation. Methods of evaluation for CBL included all the steps on Kirkpatrick's hierarchy of learning and demonstrated that CBL could be shown conclusively to produce deeper learning.
To repeat the definition included earlier in this review, CBL is a form of learning that involves a clinical case, a problem or question requiring student thought, a set of learning objectives, information given prior and during the learning intervention, and a measured outcome.
CBL imparts relevance to medical and related curricula, is shown to tie theory to practice, and induce deeper learning. CBL is practical and efficient as a mode of teaching for adult learners. CBL is certain to become part of every medical and health profession's curriculum.
Author Contributions
Conceived the concepts: SFM. Analyzed the data: SFM. Wrote the first draft of the manuscript: SFM. Made critical revisions: SFM. The author reviewed and approved of the final manuscript.
Peer Review: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 779 words, excluding any confidential comments to the Academic Editor.
Competing Interests: Author discloses no external Funding sources.
Funding: SFM has been selected as a local site primary investigator for a study of a new tissue insert for use in surgical repair of ventral hernia. The study is sponsored by BARD-Davol Inc.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent Academic Editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of Competing Interests and Funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 21 September 2021
Patient apprehensions about the use of artificial intelligence in healthcare
- Jordan P. Richardson 1 ,
- Cambray Smith ORCID: orcid.org/0000-0001-9723-891X 1 ,
- Susan Curtis ORCID: orcid.org/0000-0001-6317-1577 1 ,
- Sara Watson ORCID: orcid.org/0000-0001-9116-5940 1 ,
- Xuan Zhu 2 ,
- Barbara Barry ORCID: orcid.org/0000-0002-0755-6939 2 &
- Richard R. Sharp ORCID: orcid.org/0000-0001-5441-2084 1
npj Digital Medicine volume 4 , Article number: 140 ( 2021 ) Cite this article
23k Accesses
107 Citations
133 Altmetric
Metrics details
- Health policy
- Medical ethics
- Translational research
While there is significant enthusiasm in the medical community about the use of artificial intelligence (AI) technologies in healthcare, few research studies have sought to assess patient perspectives on these technologies. We conducted 15 focus groups examining patient views of diverse applications of AI in healthcare. Our results indicate that patients have multiple concerns, including concerns related to the safety of AI, threats to patient choice, potential increases in healthcare costs, data-source bias, and data security. We also found that patient acceptance of AI is contingent on mitigating these possible harms. Our results highlight an array of patient concerns that may limit enthusiasm for applications of AI in healthcare. Proactively addressing these concerns is critical for the flourishing of ethical innovation and ensuring the long-term success of AI applications in healthcare.
Similar content being viewed by others

Shaping the future of AI in healthcare through ethics and governance
Rabaï Bouderhem

An integrative review on the acceptance of artificial intelligence among healthcare professionals in hospitals
Sophie Isabelle Lambert, Murielle Madi, … Astrid Stephan

The value of standards for health datasets in artificial intelligence-based applications
Anmol Arora, Joseph E. Alderman, … Xiaoxuan Liu
Introduction
Artificial Intelligence (AI), the ability of computers to perform tasks typically associated with human intelligence 1 , has the capacity to impact millions of patients by changing the way medicine is practiced. Enthusiasm for applications of AI in healthcare has continued to grow, with early successes involving ChatBots, diagnostic tools, and radiological image analysis 2 , 3 , 4 , 5 . While there is considerable excitement about these emerging technologies, prospective analyses of how AI technologies might be implemented responsibly into clinical practice has been limited. Importantly, to date there has been very little engagement with patients who will be impacted by applications of AI in healthcare. This is troubling since patient concerns about AI could be a significant barrier to the dissemination and use of these tools. Studies of nonmedical applications of AI have shown that the public tends to view nonmedical AI in highly variable ways 6 , with factors such as media coverage and early experiences playing key roles in shaping public opinion. These considerations highlight the importance of patient engagement to ensure that these technologies are integrated into healthcare in a manner that fosters public trust 7 , 8 and mitigates widespread patient concerns that might result in another “AI Winter” 9 .
Moreover, since patients are the intended beneficiaries of many of these AI innovations, more carefully characterizing their needs, values, and priorities is important for ensuring that these advances are not just well-received but are developed and implemented in an ethical way that improves patient care. Even in situations where patients do not interface directly with AI technologies, patients still bear the largest risk should implementation be done incorrectly or unethically 10 . To the extent that patients will be asked to accept the potential risks associated with novel applications of AI in healthcare, there is an ethical obligation to ensure that patient values and needs are incorporated into implementation plans. As in other areas of medical innovation, proactive patient engagement is an essential component of implementing healthcare AI in an ethical manner 11 .
Applications of AI in medicine take advantage of unprecedented volumes of clinical data and computing power to inform evidence-based decision making 3 . This raises new ethical questions related to the transparency of data use, accountability for data stewardship, and potential inequities in the deployment of AI 12 . Currently, very little research has been done characterizing patient and other stakeholder perspectives on applications of AI in healthcare. Additionally, the few studies that have assessed patient perspectives have focused on a narrow array of AI tools, which limits their utility as a guide in anticipating patient engagement with other AI applications in healthcare 13 , 14 . While engaging patients around specific applications of AI is a crucial step in the research and development process, engagement at this level of specificity does not facilitate analysis of broader public perspectives on AI and its application in healthcare, which is much needed for health policy development, innovation priority setting, and implementation design.
The aim of the research study we report was to understand how patients view the use of AI in their healthcare. To clarify sources of patient excitement and concern about healthcare AI, we used focus groups and case-study discussions to characterize the range of patient opinions about emerging AI applications in healthcare. This approach allowed us to make AI technologies more accessible to patients, while also engaging across diverse cases to promote broader reflection on the potential technological, societal, and medical impacts of AI. The results we report highlight a range of patient concerns about applications of AI in healthcare. We hope AI developers and healthcare institutions seeking to deploy new AI technologies find these results useful as they consider how best to integrate AI technologies into healthcare and create governance structures that promote patient safety and foster the trust of the patients they serve.
We conducted 15 focus groups with 87 participants between November 2019 and February 2020. Each focus group had between three and seven participants and lasted 90 min. Approximately half of our participants were female (49.4%) and the average age of participants was 53.5 years old. A majority of participants were white (93.1%) and non-Hispanic/Latino (94.3%). Most participants had an education level higher than a high school degree (87.3%). Approximately one in five participants had experience working in technology or computer science (19.5%) for an average of 17.6 years. Nearly half of our participants had experience working in healthcare or health science (44.8%) for an average of 17.1 years. No participants reported any prior experience with AI impacting their healthcare. A detailed description of these and other participant characteristics is presented in Table 1 .
In what follows, we describe several major themes that emerged during focus-group discussions of healthcare AI. These themes reflect multiple sources of patient concern and excitement about applications of AI in medicine. We found that, while patients are generally enthusiastic about the possibility of AI improving their care, they are also concerned about the safety and oversight of healthcare AI. We describe these concerns about AI safety, the importance of patient choice, concerns about rising healthcare costs, questions about data quality, and view of the security of AI systems below.
Participants were excited about healthcare AI but wanted assurances about safety
In general, participants reported enthusiasm about the ability of AI to be a positive force in medicine. They felt healthcare AI was compatible with the goals of medicine: to heal as many patients as possible. Participants were supportive of developing AI tools for a variety of different healthcare applications.
I feel good about it. I think it has the ability to be better. I mean, it’s not a human. It’s got more data, so probably. … [I]t probably has more intelligence; it just has more information to work with to try to come up with a proper diagnosis. … I don’t think you will cure a lot of diseases without that advanced intellect. Obviously, we’ve come a long way with the human brain, but we could probably go a lot farther and speed the process with AI. (FG14) .
Our participants also reported being aware that healthcare AI was still an emerging technology. As such, participants felt that it still had potential to be used in many different creative and positive ways.
This was often expressed as a sentiment of hopefulness, coupled with an acknowledgment that these benefits could only be realized through thoughtful implementation.
I feel like the future of AI just depends on how we choose to use it. The impact will be what we choose it to be. … Because it’s moldable, it’s not going to do anything that we don’t allow it to do. (FG7).
Participants urged caution in developing and implementing AI tools. They reported a need for a careful transition period to ensure that any AI tool used in their care is well-tested and accurate.
So when this intelligence is built we have to test it, right? We have to test it to make sure that it’s helping correctly, and that to me represents a big challenge and one we don’t wanna jump into and see what happens. We’ve gotta be very careful there. (FG4).
Participants also called for oversight and regulatory protections against potential harms. While participants often could not articulate what these regulations should include or who should enact them, they felt additional protections were necessary for AI tools.
It’s gonna do what it’s gonna do. I think that I look forward with excitement… but I agree that there’s definitely some flaws, and there definitely needs to be some markers in there, at least right now, that can also protect people. But it’s going to be positive if we can get those safe markers in. (FG11).
Patients expect their clinicians to ensure AI safety
Participants reported that they felt their clinicians should act as a safeguard to buffer patients from the potential harms that might result from mistakes made by healthcare AI. One way this was commonly expressed was in terms of their healthcare providers retaining final discretion over treatment plans and maintaining responsibility for patient care.
I believe the doctor always has the responsibility to be checking for you, and you’re his responsibility, you know? The AI is not responsible; that’s just a tool. (FG13).
Other participants were comfortable extending more authority to AI tools, but still calling for their providers to provide “checks and balances” or “second opinions” on recommendations generated by healthcare AI. Most participants felt strongly that an AI algorithm should not have the ability to act autonomously in a clinical setting, stressing that both treatment decisions and the monitoring of ongoing care should be done by a human provider.
I’d be okay with them telling a doctor what to do, but I don’t know that I’d want a machine doing the treatment, especially depending on what it is. Aiding, sure, they already do that with robotics and CT scans and all that, but I want a human there making sure that it’s doing what it’s supposed to. (FG13).
Participants also noted the uniqueness of each patient, and commented on the resultant individuality required in approaching medical decision making. They viewed the providers’ role in using AI as one of adapting AI recommendations to the patient’s unique personal situation, ensuring that they are not harmed and that patients follow through with clinical recommendations.
[I]t’s important to take into account that people, depending on what the AI comes out with, people might not be willing to go with what that is, they might need alternates. And also just the question of creativity, like what if the solution were actually something where you would have to think outside the box? … What if it’s something they haven’t encountered before? (FG13).
Preservation of patient choice and autonomy
Participants reported that the preservation of choice was an important factor in their overall comfort with applications of AI in healthcare. They felt that patients should have the right to choose to have an AI tool used in their care and be able to opt-out of AI involvement if they felt strongly.
I think it all comes back to choice, though, I think everybody’s getting the mentality that, and maybe I’m wrong, but that an AI is being pushed, but at the end of the day, our choice is still our choice, and it’s not being taken away. (FG 15).
In addition to the ability to choose whether an AI tool is used or not, participants wanted to have the ability to dispute the recommendations of an AI algorithm, or correct those recommendations if they believed they were in error. Participants were uncomfortable relying solely on recommendations made by an AI without being able to evaluate the rationale for those recommendations directly themselves.
So I’d rather know what they’re observing and, if it’s [AI] wrong, I would [want to] be able to correct it rather than have them just collect data and make assumptions. (FG 13).
Concerns about healthcare costs and insurance coverage
Participants also voiced concerns that AI tools might increase healthcare costs and that those costs might be passed on to patients. While participants acknowledged that AI might make the delivery of some healthcare services more efficient, they anticipated high development and deployment costs. They felt that adding another advanced technology would likely increase the cost of their healthcare.
So it sounds expensive, and health care is already fairly expensive. To go on his note, a lot of times you can get something that works just as well for a lot less or you could get something super fancy, that makes you think, hey I got this big fancy thing, but it really doesn’t do any better than the original cheaper version. (FG 9).
Additionally, participants worried about the impact that AI recommendations could have on what types of treatment their insurance providers would cover. For example, some participants were concerned that an AI algorithm might recommend a treatment that they could not afford. Similarly, others worried that insurance companies might chose to cover only those treatments that are supported by AI recommendations, thereby taking away some of the discretion traditionally reserved for physicians.
Is insurance only gonna cover what the machine says it is and not look for anything else? There is no reason for further diagnostics because the machine already did it? I mean we already have a situation in our healthcare system where money comes into play for diagnosing things. (FG 9).
Participants recognized how the ability of AI to draw connections and make highly accurate predictions from images or complex symptoms could be very helpful. However, they were concerned that new types of predictions could result in new forms of discrimination. Participants were especially worried that insurance companies would use AI to discover otherwise unknown medical information that could be used to deny coverage or increase premiums.
I mean, … that information is wonderful, but who’s gonna get it after the doctors look at it is my big thing. Is the insurance company gonna take it, and now all of a sudden … my premium doubles for health insurance? (FG1).
Ensuring data integrity
Participants considered the impact of data quality on AI tools and their recommendations, and had several concerns related to the way healthcare AI might be developed using flawed datasets, potentially resulting in harm to patients. They felt data from the electronic health record was not accurate enough to be reliable in teaching healthcare AI, citing personal experiences with errors they had found in their own health records.
There’s a lot of discrepancies in the medical record I must say, especially now that you can see your portal. I know I’ve seen things saying that certain things were done or about myself and procedures that were totally not true. So I’ve had a lot of different things in my medical chart that are inaccurate, very inaccurate, so if they’re training an artificial intelligence that this is facts, it’s like, well no. (FG 4).
Participants were also concerned about the possibility that AI tools might reinforce existing biases in healthcare datasets. They explained that this could happen as a result of an inherently biased learning dataset or from developers unintentionally incorporating their own bias into an AI algorithm.
Prejudices that people can have, like it could absorb those or it could be taught to work against them, like a lot of people who are overweight have said that their providers assume that that’s the cause and ignore doing other tests or pursuing other avenues, and if an AI wasn’t going to make the assumption that that was what was the problem, then that would be good, but if it was learning from people around it that it should make that assumption, then it would perpetuate the problem. (FG 13).
Risks of technology-dependent systems
Participants also expressed concerns about technological systems that might be highly dependent on new AI technologies and worried that some risks might be exacerbated if AI were to be widely deployed in medicine. One such concern was a worry about a systems-level crash or mass technological failure, and the impact this might have on a clinical system that is heavily reliant on AI tools.
I have some background in electronics, and one thing you can guarantee with electronics is they will fail. Might not be now, might never happen in 10, 20 years. The way things are made, ‘cause I’ve actually worked in the industry of making medical equipment, it’s all about using the cheapest method to get the end result. Well, electronics fail. They just do. (FG9).
Additionally, participants brought up examples of bad actors hacking into AI systems and manipulating these tools for nefarious purposes.
I was just gonna say another concern that I think I would have, just because of the way our world is evolving and revolving, is can that artificial intelligence be hacked? Who can control that? …I don’t know. Because any time you have a computerized program, I don’t care what anybody says, it can and it will get hacked because there’s always somebody that’s out there just to do evil rather than good. (FG15).
These concerns were compounded by the perception that healthcare providers could easily become overly dependent on AI tools, and over time might not be able to provide high-quality care if access to those healthcare AI tools was unavailable.
If they were to get hacked or a system goes down … like what’s the contingency plan, but what is the contingency plan? If you have all these doctors who are so used to having this artificial intelligence read all these, and they don’t have the skill of reading it, then what happens? (FG6).
The patients we consulted shared a variety of concerns that will shape their perceptions of future AI applications in healthcare. While they envisioned AI having a generally positive impact on healthcare, this view was contingent on proactive oversight that mitigates potential harms resulting from AI. While participants were able to appreciate the widereaching impact of AI on healthcare, their concerns centered on specific ways in which AI might result in harm to them personally, or to those they care about. This finding contrasts with much of the existing literature examining the potential implications of AI for healthcare, which tends to take a more abstract approach that is not connected to the practical concerns that patients and families may have, such as the potential for AI to limit access to a preferred medication or increase healthcare costs 12 , 15 . Participants expected to be protected from these harms and felt that physician oversight would be critical. Translational researchers and clinical implementation teams deploying new AI tools must be aware of these expectations if they hope to ensure the successful integration of AI into healthcare systems.
A subset of the concerns voiced by our participants are reminiscent of concerns raised about prior medical advances, including worries about higher costs, discriminatory uses, and fewer choices available to patients and providers. Both personal and national healthcare expenditures have been rising steadily for decades 16 , and many interventions that promise to increase efficiency have not delivered on their promise to decrease healthcare costs 17 , 18 . Similarly, respect for patient autonomy is one of the core principles of medical ethics 19 , and participants were clear that they wanted to be able to choose whether or not to have AI tools as a component of their care. To the extent that AI tools could operate surreptitiously in the background, patients who do not want AI used in their care may not know it is being used, which could result in significant breaches of public trust should this approach to AI deployment be discovered by those patients. Similarly, while concerns about discrimination based on predictive analytics are reminiscent of concerns about genetic information 20 , it is unclear if legislators will recognize these similarities and develop special protections that apply to AI-enabled medical predictions. Here too, these considerations highlight the value of proactive engagement with patients, both to understand their concerns but also to consider what effective policy responses might entail.
Other patient apprehensions about AI applications in healthcare did not have obvious parallels to concerns about prior healthcare technologies. These concerns mirror some of the most contentious debates about the impact that AI may have on medicine. For example, participants stressed the role of physicians as safety monitors. A similar conversation is reflected in contemporary literature advocating for the necessity of the physician in AI-driven healthcare systems 21 , 22 , 23 , 24 , 25 . Academics and patients alike seem to feel that the physician must be at the center of medical decision-making to preserve patient safety 22 , 26 . Participants were also concerned about the future of healthcare systems, as they become increasingly dependent on digital tools. The multiple challenges of ensuring source-data quality, algorithmic reliability, and unbiased AI outcomes have been recognized as a substantial ethical and technological barrier to successful clinical implementation by bioethicists and AI developers alike 15 .
Addressing patient apprehensions about healthcare AI will require creative solutions that incorporate systems-level trust building, proactive technological innovation, and a recognition of the complex social forces at work. Those advocating for clinical uses of AI tools should support the development of transparent oversight mechanisms that promote stakeholder engagement at each step of AI development and implementation—from the curation of healthcare datasets to widespread clinical usage 27 . Importantly, our results show that patients recognize and are beginning to grapple with the many nuanced issues raised by applications of AI in healthcare. Despite the abstractness of machine learning, and lack of personal experience with AI, participants were quickly able to appreciate how they and their families could be impacted (and potentially harmed) by healthcare AI without appropriate oversight. Those concerns could easily evolve into a deep skepticism about the promise of AI without consistent and deliberate patient engagement.
A limitation of this study is the racial and ethnic diversity of our sample, which was limited by our recruitment methods, which involved contacting primary care patients at a large health system in the upper Midwest. Additionally, many participants had personal or familial connections to healthcare occupations, which likely influenced their perceptions of medical innovation. The education level of participants and their insurance coverage was higher than typical, which also may have impacted their engagement with topics related to healthcare. These limitations suggest caution in generalizing the findings we report to other clinical settings and patient populations.
While use of focus-group methods was a strength of the study, allowing us to explore a wide range of patient perspectives on healthcare AI, use of specific case studies to structure focus-group discussions may have influenced our results by encouraging participants to focus on more familiar applications of AI in healthcare. Additionally, the technical complexity of the AI tools we examined may have resulted in inaccurate participant understandings of those technologies and their potential impact.
While this research study provides important insights into patient apprehensions about applications of AI in healthcare, the limitations above highlight a clear need for additional research. Of note, patient-centered research involving underrepresented or historically disadvantaged populations is crucial for ensuring equitable and just applications of AI in healthcare. Additionally, future research studies should seek to characterize the frequency and potential impact of various patient concerns, using survey methods and behavioral models of technology acceptance. Patient engagement around real-world AI tools at various stages of implementation are also critical for ensuring that AI innovation is responsive to patient concerns. Finally, patient perspectives on healthcare AI are only one important factor in the ecosystem of responsible AI development and implementation. Future research should also examine systems-level readiness for healthcare AI and engage other stakeholders, including healthcare providers, payers, and administrators.
Addressing patient concerns relating to AI applications in healthcare is essential for effective clinical implementation. While participants in our study may not have had a complete understanding of AI algorithms or their capabilities, they were able to engage with core concepts relating to healthcare AI and could readily express their expectations and apprehensions. Our results clarify several potential sources of patient concern about applications of AI in healthcare and highlight patients’ desire for physician-led oversight of these technologies. If this expectation is not met, it is possible that we could see a third “AI Winter” in which fears of patient harm lead to widespread rejection of healthcare AI by patients and their providers 9 . To avoid that possibility, it is critical that AI developers engage the public in dialogue about both the potential benefits and harms of applications of AI in healthcare 28 .
Participant recruitment
We contacted 946 patients who visited a Mayo Clinic primary care facility in Minnesota or Wisconsin between November 19, 2019 and February 25, 2020. Potential research participants were recruited by phone. Study inclusion criteria included being conversant in English and being 18 years or older. Participants received $50 for their participation. This study was approved by the Mayo Clinic Institutional Review Board (protocol #19-010128). We did not solicit personal health information from participants, and oral consent was obtained for all participants at the beginning of each focus group before data collection began in accordance with the IRB recommendations.
Data collection
We selected a focus group design for this study because we anticipated participants having limited prior knowledge of the subject area. Focus groups encourage participants to react to each other’s comments and questions, revealing more nuanced views. Focus groups also allow for a more accessible and open discussion for individuals with varying levels of familiarity with the topics discussed. This approach allowed us to capture diverse opinions generated through the discussion and reflection process 29 .
Focus groups were co-facilitated by three research team members, with one person serving as the primary moderator, and the other two taking field notes and asking follow-up questions to clarify critical points 30 , 31 . Participants were first asked a series of general questions about AI to gauge their knowledge and familiarity such as “What does AI mean to you” or “What comes to mind when you think about AI and medicine?”. The moderators then offered a brief definition of AI, along with examples of nonmedical applications of AI. The explanation of AI given during the focus group was specific to machine learning, a method of providing data to algorithms without explicit programming, allowing the algorithms to optimize mapping connections between input and output data points 32 . Case studies of specific uses of AI in medicine were then presented to participants for discussion and reflection, followed by questions about participants’ comfort with and concerns about each case study 33 such as “What are your initial thoughts or reactions to this AI tool?” or “How would you feel about this technology being used for you or your loved one?” Some cases also had specific probes about data use, preferred situations, or relationships with providers. The focus group concluded with a broad discussion of AI applications in healthcare, including general concerns, sources of enthusiasm, and comparisons of perspectives across the different case studies including questions such as “What tradeoffs do you see with AI in healthcare and how do you balance them?”.
The case studies were selected to be representative of emerging applications of AI in healthcare, as determined by a review of the literature on AI technologies 2 , 3 , 4 . Each case was based on a specific type of tool, which allowed participants to engage with the tools in a way that was both generalizable but grounded in reality. Focus groups 1–6 used three case studies: an image analysis tool, a ChatBot for asking questions about a medical procedure, and a risk prediction tool that analyzed and flagged patients at risk of developing a preventable condition. (These case studies are available from the authors upon request.) Focus groups 7–15 used three different cases: a complex diagnostic tool, a well-person visit involving a ChatBot, and a tool for monitoring patients in an intensive care unit (ICU). After each focus group, the research team met to debrief about the session. Each team member generated a field note summarizing the discussion and describing general themes. A fourth team member then combined the memos from the three team members who were present at the focus group to generate a consensus memo for that focus group 34 , 35 . The moderator guide was also refined throughout data collection to improve its clarity and effectiveness.
Participants were asked to complete a short questionnaire at the beginning of the focus group to collect demographic data, which included: age, gender, race, ethnicity, and educational attainment. The questionnaire also included two questions related to participant’s work experiences; one question examined work experience in a technology or computer-science field, and a second question examined experience working in healthcare or the health sciences. These questions were included to assess the extent to which our sample included persons whose work might be impacted more directly by applications of AI in healthcare, which we hypothesized would impact participants’ familiarity and engagement with the topics discussed.
Data analysis
After the first six focus groups, a synthesized memo was generated for each of the cases, summarizing preliminary findings and emerging themes 34 , 35 . A second set of case studies was designed using this preliminary analysis, resulting in three completely new cases. The same memoing process was done for the second set of case studies after the remaining focus groups were completed. Data collection, memoing, and preliminary data analysis continued until the study team agreed that thematic saturation had been reached 36 . Each focus group was audio recorded, with recordings sent to a transcription service and transcribed verbatim. All recordings were deidentified and reviewed for accuracy by the study team.
Transcripts were analyzed using a modified inductive approach which employed constant comparison analysis 37 , 38 , 39 . The qualitative analysis team consisted of one primary coder (J.P.R.) and two secondary coders (C.S., S.C.). A preliminary codebook was generated using the memos that were written and synthesized during data collection 34 . All three analysis team members then applied the codebook to three transcripts from different points in data collection, revised the codebook based on those experiences, and generated a final codebook that was used to examine the entire dataset 40 . Each transcript was coded independently by two coders. The two coders then met to discuss code any discrepancies until consensus was reached. All coding was done using NVivo 11 Software. Data available upon request.

Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Additional supporting data available upon request to authors
Goodfellow, I., Bengio, Y., Courville, A. & Bengio, Y. Deep learning . 1 (MIT press Cambridge, 2016).
Matheny, M., Israni, S. T., Ahmed, M. & Whicher, D. Artificial intelligence in health care: The hope, the hype, the promise, the peril. Natl Acad Med , 94–97 (2020).
Topol, E. J. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 25 , 44–56 (2019).
Article CAS Google Scholar
He, J. X. et al. The practical implementation of artificial intelligence technologies in medicine. Nat. Med. 25 , 30–36 (2019).
Gómez González, E. & Gómez Gutiérrez, E. Artificial Intelligence in Medicine and Healthcare: applications, availability and societal impact. (2020).
Fast, E. & Horvitz, E. In Proceedings of the Thirty-First AAAI Conference on Artificial Intelligence 963–969 (AAAI Press, 2017).
Concannon, T. W. et al. A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research. J. Gen. Intern. Med. 29 , 1692–1701, https://doi.org/10.1007/s11606-014-2878-x (2014).
Article PubMed PubMed Central Google Scholar
Holzer, J. K., Ellis, L. & Merritt, M. W. Why we need community engagement in medical research. J. Investig. Med. 62 , 851–855 (2014).
Article Google Scholar
Muthukrishnan, N. et al. Brief history of artificial intelligence. Neuroimaging Clin. N. Am. 30 , 393 (2020). +.
Yarborough, M. et al. Relationships hold the key to trustworthy and productive translational science: recommendations for expanding community engagement in biomedical research. Clin. Transl. Sci. 6 , 310–313 (2013).
Borry, P., Schotsmans, P. & Dierickx, K. What is the role of empirical research in bioethical reflection and decision-making? An ethical analysis. Med Health Care Philos. 7 , 41–53 (2004).
Morley, J. et al. The ethics of AI in health care: a mapping review. Soc. Sci. Med 260 , 113172 (2020).
Stai, B. et al. Public Perceptions of Artificial Intelligence and Robotics in Medicine. J. Endourol . https://doi.org/10.1089/end.2020.0137 (2020).
Juravle, G., Boudouraki, A., Terziyska, M. & Rezlescu, C. Trust in artificial intelligence for medical diagnoses. Prog. Brain Res 253 , 263–282 (2020).
Matheny, M. E., Whicher, D. & Thadaney Israni, S. Artificial intelligence in health care: a report from the national academy of medicine. JAMA 323 , 509–510 (2020).
National Health Expenditure Data: Historical. (Centers for Medicare & Medicaid Services, 2019).
Callahan, D. What Kind of Life?: The Limits of Medical Progress . (Georgetown University Press, 1995).
Moraros, J., Lemstra, M. & Nwankwo, C. Lean interventions in healthcare: do they actually work? A systematic literature review. Int. J. Qual. Health Care 28 , 150–165 (2016).
Childress, J. F. & Beauchamp, T. L. Principles of biomedical ethics . (Oxford University Press, 2001).
Holtzman, N. A. & Shapiro, D. Genetic testing and public policy. BMJ 316 , 852–856 (1998).
Liu, X., Keane, P. A. & Denniston, A. K. Time to regenerate: the doctor in the age of artificial intelligence. J. R. Soc. Med. 111 , 113–116 (2018).
Verghese, A., Shah, N. H. & Harrington, R. A. What This Computer Needs Is a Physician: Humanism and Artificial Intelligence. JAMA 319 , 19–20 (2018).
Obermeyer, Z. & Lee, T. H. Lost in Thought—The Limits of the Human Mind and the Future of Medicine. N. Engl. J. Med. 377 , 1209–1211 (2017).
Wartman, S. A. & Combs, C. D. Reimagining Medical Education in the Age of AI. AMA J. ethics 21 , E146–E152 (2019).
Johnston, S. C. Anticipating and Training the Physician of the Future: The Importance of Caring in an Age of Artificial Intelligence. Academic Med. 93 , 1105–1106 (2018).
Johnston, S. C. Anticipating and Training the Physician of the Future: The Importance of Caring in an Age of Artificial Intelligence. Acad. Med 93 , 1105–1106 (2018).
Flinterman, F., Broerse, J., & Bunders, J. The experiential knowledge of patients: a new resource for biomedical research? Soc. Sci. Med. 60 , 2575–2584 (2005).
Ahmed, S. M. & Palermo, A. G. S. Community engagement in research: frameworks for education and peer review. Am. J. Public Health 100 , 1380–1387 (2010).
McLafferty, I. Focus group interviews as a data collecting strategy. J. Adv. Nurs. 48 , 187–194 (2004).
Wilkinson, S. Focus group methodology: a review. Int. J. Soc. Res. Methodol. 1 , 181–203 (1998).
Morrison-Beedy, D., Côté-Arsenault, D. & Feinstein, N. F. Maximizing results with focus groups: moderator and analysis issues. Appl Nurs. Res 14 , 48–53 (2001).
Deo, R. C. Machine learning in medicine. Circulation 132 , 1920–1930 (2015).
Hughes, R. Using vignettes in qualitative research. Socio. Health Illn. 20 , 381–400 (1998).
Lempert, L. B. Asking questions of the data: Memo writing in the grounded. The Sage handbook of grounded theory, 245–264 (2007).
Birks, M., Chapman, Y. & Francis, K. Memoing in qualitative research: Probing data and processes. J. Res. Nurs. 13 , 68–75 (2008).
Guest, G., Namey, E. & McKenna, K. How Many Focus Groups Are Enough? Building an Evidence Base for Nonprobability Sample Sizes. Field Methods 29 , 3–22 (2017).
Corbin, J. & Strauss, A. Basics of qualitative research: Techniques and procedures for developing grounded theory (Sage publications, 2014).
Donovan, J. The process of analysis during a grounded theory study of men during their partners’ pregnancies. J. Adv. Nurs. 21 , 708–715 (1995).
Onwuegbuzie, A. J., Dickinson, W. B., Leech, N. L. & Zoran, A. G. A qualitative framework for collecting and analyzing data in focus group research. Int. J. Qualitative Methods 8 , 1–21 (2009).
MacQueen, K. M., McLellan, E., Kay, K. & Milstein, B. Codebook development for team-based qualitative analysis. CAM J. 10 , 31–36 (1998).
Download references
Acknowledgements
This study was funded by the Mayo Clinic Biomedical Ethics Research Program. No external funding was associated with the work described. The authors thank Joel Pacyna for his help with study recruitment.
Author information
Authors and affiliations.
Biomedical Ethics Research Program, Mayo Clinic Rochester, Rocheste, MN, 55905-0002, USA
Jordan P. Richardson, Cambray Smith, Susan Curtis, Sara Watson & Richard R. Sharp
Kern Center for the Science of Healthcare Delivery, Mayo Clinic Rochester, Rocheste, MN, 55905-0002, USA
Xuan Zhu & Barbara Barry
You can also search for this author in PubMed Google Scholar
Contributions
J.P.R. contributed to study design, data collection, analysis, and writing. C.S. contributed to data collection, analysis, and writing. S.C. contributed to data collection, analysis, and writing. S.W. contributed to data collection and writing. X.Z. contributed to analysis and writing. B.B. contributed to analysis and writing. R.R.S. contributed to study design, analysis, and writing.
Corresponding author
Correspondence to Richard R. Sharp .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Richardson, J.P., Smith, C., Curtis, S. et al. Patient apprehensions about the use of artificial intelligence in healthcare. npj Digit. Med. 4 , 140 (2021). https://doi.org/10.1038/s41746-021-00509-1
Download citation
Received : 18 February 2021
Accepted : 23 August 2021
Published : 21 September 2021
DOI : https://doi.org/10.1038/s41746-021-00509-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- MEMBER DIRECTORY
- Member Login
- Publications
- Clinician Well-Being
- Culture of Health and Health Equity
- Fellowships and Leadership Programs
- Future of Nursing
- U.S. Health Policy and System Improvement
- Healthy Longevity
- Human Gene Editing
- U.S. Opioid Epidemic
- Staff Directory
- Opportunities
- Action Collaborative on Decarbonizing the U.S. Health Sector
- Climate Communities Network
- Communicating About Climate Change & Health
- Research and Innovation
- Culture of Health
- Fellowships
- Emerging Leaders in Health & Medicine
- Culture & Inclusiveness
- Digital Health
- Evidence Mobilization
- Value Incentives & Systems
- Substance Use & Opioid Crises
- Reproductive Health, Equity, & Society
- Credible Sources of Health Information
- Emerging Science, Technology, & Innovation
- Pandemic & Seasonal Influenza Vaccine Preparedness and Response
- Preventing Firearm-Related Injuries and Deaths
- Vital Directions for Health & Health Care
- NAM Perspectives
- All Publications
- Upcoming Events
- Past Events
- MEMBER HOME

Telehealth and Mobile Health: Case Study for Understanding and Anticipating Emerging Science and Technology

Introduction
This case study was developed as one of a set of three studies, focusing on somewhat mature but rapidly evolving technologies. These case studies are intended to draw out lessons for the development of a cross-sectoral governance framework for emerging technologies in health and medicine. The focus of the case studies is the governance ecosystem in the United States, though where appropriate, the international landscape is included to provide context. Each of these case studies:
- describes how governance of the technology has developed within and across sectors and how it has succeeded, created challenges, or fallen down;
- outlines ethical, legal, and social issues that arise within and across sectors;
- considers a multitude of factors (market incentives, intellectual property, etc.) that shape the evolution of emerging technologies; and
- identifies key stakeholders.
Each case study begins with two short vignettes designed to highlight and make concrete a subset of the ethical issues raised by the case (see Box 1 and Box 2 ). These vignettes are not intended to be comprehensive but rather to provide a sense of the kinds of ethical issues being raised today by the technology in question.

The cases are structured by a set of guiding questions, outlined subsequently. These questions are followed by the historical context for the case to allow for clearer understanding of the trajectory and impact of the technology over time, and the current status (status quo) of the technology. The bulk of the case consists of a cross-sectoral analysis organized according to the following sectors: academia, health care/nonprofit, government, private sector, and volunteer/consumer. Of note, no system of dividing up the world will be perfect—there will inevitably be overlap and imperfect fits. For example, “government” could be broken into many categories, including international, national, tribal, sovereign, regional, state, city, civilian, or military. The sectoral analysis is further organized into the following domains: science and technology, governance and enforcement, affordability and reimbursement, private companies, and social and ethical considerations. Following the cross-sectoral analysis is a broad, nonsectoral list of additional questions regarding the ethical and societal implications raised by the technology.
The next section of the case is designed to broaden the lens beyond the history and current status of the technology at the center of the case. The “Beyond” section highlights additional technologies in the broad area the focal technology occupies (e.g., neurotechnology), as well as facilitating technologies that can expand the capacity or reach of the focal technology. The “Visioning” section is designed to stretch the imagination to envision the future development of the technology (and society), highlighting potential hopes and fears for one possible evolutionary trajectory that a governance framework should take into account.
Finally, lessons learned from the case are identified—including both the core case and the visioning exercise. These lessons will be used, along with the cases themselves, to help inform the development of a cross-sectoral governance framework, intended to be shaped and guided by a set of overarching principles. This governance framework will be created by a committee of the National Academies of Sciences, Engineering, and Medicine (https://www.nationalacademies.org/our-work/creating-a-framework-for-emerging-science-technology-and-innovation-in-health-and-medicine).
Case Study: Telehealth
As far back as the Civil War, the United States has used electronic means (in this early example, telegraphs) to communicate patient health information. After a long, slow ramp-up, there has been steady evolution and growth in electronic health data and communication since 1990, pulled by advances in technology and pushed by changes in regulation.
Prior to the COVID-19 pandemic, which began in March 2020, three broad trends were under way in the evolution of telehealth: first, a shift in application from efforts to expand health care access that motivated early use to the use of telehealth to control costs; second, the expansion of telehealth use from the context of acute care to the management of chronic conditions; and third, a transition of the site of care from health care institutions to patients’ homes and mobile devices (Dorsey and Topol, 2016). The recent exponential increase in mobile health applications and physical distancing requirements that accompanied the pandemic have dramatically accelerated the evolution and adoption of telehealth (Olla and Shimskey, 2014).
It is important to note that “telehealth” and “mobile health (mHealth)” do not have consensus definitions, nor do many other terms used in this space, such as “electronic health (eHealth),” “telemedicine,” and “digital health” (HealthIT.gov, 2019; Doarn et al., 2014; WHO, 2010). From a regulatory perspective, definitions are important because countries and states must describe what they do and do not regulate and how (Hashiguchi, 2020). In the United States, telehealth is generally the umbrella term covering telemedicine (defined as provider-based medical care at a distance); telemedicine within medical specialties such as telepsychiatry, telestroke, and teledermatology; and mHealth (initially used to describe care provision through text messaging, but now includes the use of wearable and ambient sensors, mobile apps, social media, and location-tracking technology in service of health and wellness) (APAa, 2020; Sim, 2019; CMS, 2011).
One widely used definition of telemedicine—the component of telehealth with the longest history—is from the World Health Organization (WHO), which defines it as, “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interest of advancing the health of individuals and their communities” (WHO, 2010).
In Norway, an early adopter and regulator of telemedicine, “telemedicine” is defined by law as “the use of videoconferencing to perform an outpatient consultation, examination, or treatment at a distance” (Zanaboni et al., 2014). In South Africa, by contrast, telemedicine is defined not by statute but by the Health Professions Council of South Africa as “using electronic communications, information technology or other electronic means between a health care practitioner in one location and a health care practitioner in another location for the purpose of facilitating, improving and enhancing clinical, educational and scientific health care and research” (HPCSA, 2020).
Telehealth can include everything from medical websites (e.g., the Mayo Clinic, WebMD) to remotely controlled surgical robots. Telehealth can also be categorized into groups of technologies, including interactive telemedicine (including video visits and electronic consults between providers), telemonitoring, store-and-forward technology (the collection and use of non-urgent medical information), and mHealth.
Early applications of telehealth were designed to expand access, and in fact, telehealth has been critical (if not entirely successful) in this regard. There are, of course, long-standing and persistent concerns about the number and geographic distribution of health care providers, and telehealth has improved access to those in remote and historically underserved populations in states such as Alaska and Texas, as well as for those in the military (e.g., those at sea or in a combat zone), prisons, and astronauts (NRHA, n.d.). Telehealth has also expanded access to language interpreters and specialists for patients with rare disease.
Telehealth, as it is traditionally construed, offers significant benefits, but it also raises a number of concerns. These concerns pertain to the use of telehealth in and of itself and the ways in which availability has been exponentially and almost instantaneously expanded in response to the COVID-19 pandemic and in recent years by mHealth. One broad issue, at least in the United States prior to the COVID-19 pandemic, is the shift mentioned previously from a focus on the use of telehealth to expand access to health care to the use of this technology to cut health care costs (Dorsey and Topol, 2016). In addition, and despite the dramatic expansion in telehealth, many of those most in need remain without access to high-quality health care (Park et al., 2018). On the individual level, telehealth raises concerns not only about privacy, both due to the site of care and the transmission, storage, and sharing of data, but also about both concrete and intangible losses related to physical distancing from the care relationship and ‘the healing touch’ (Bauer, 2001).
Guiding Questions
(derived from global neuroethics summit delegates, 2018; mathews, 2017).
The following guiding questions were used to frame and develop this case study.
- Historical context: What are the key scientific antecedents and ethics touchstones?
- Status quo: What are the key questions, research areas, and products/applications today?
- Cross-sectoral footprint: Which individuals, groups, and institutions have an interest or role in emerging biomedical technology?
- Ethical and societal implications: What is morally at stake? What are the sources of ethical controversy? Does this technology or application raise different and unique equity concerns?
Additional guiding questions to consider include the following:
- Key assumptions around technology: What are the key assumptions of both the scientists around the technology and the other stakeholders that may impede communication and understanding or illuminate attitudes?
- International context and relevant international comparisons: How are the technology and associated ethics and governance landscape evolving internationally?
- Legal and regulatory landscape: What are the laws and policies that currently apply, and what are the holes or challenges in current oversight?
- Social goals of the research: What are the goals that are oriented toward improving the human condition? Are there other goals?
Historical Context
What are the key scientific antecedents and ethics touchstones.
Despite its association for most people with the last decade or even just with the COVID-19 pandemic, telehealth was first employed in the United States more than 100 years ago—one of the first health-related telephone calls was described in 1874 (Nesbitt and Katz-Bell, 2018). In 1905, the first “telecardiogram” was recorded and sent by telephone wire from a laboratory to a hospital (IOM, 2012). By the 1920s, Norwegian providers began giving medical advice to clinics on ships over radio, a use that quickly spread to other parts of the world (Ryu, 2010).
Over time, technology and applications expanded to include transmission of images and video. Teleradiology has been used for more than 60 years in the United States, with some of the first radiologic images transmitted by telephone between West Chester, Pennsylvania and Philadelphia, Pennsylvania, in 1948 (Gershon-Cohen and Cooley, 1950). Similar use in Canada soon followed.
The first use of interactive video in health care communications in the United States likely occurred at the University of Nebraska in 1959, through the transmission of neurological exams (Wittson and Benschoter, 1972). In an early and famous use of telemedicine, Norfolk State Hospital employees provided psychiatric consultations for the Nebraska Psychiatric Institute in the 1950s and 1960s (IOM, 1996). Wireless transfers of electrocardiogram and X-rays became prominent around this time as well (IOM, 1996).
In collaboration with the state of Arizona, the National Aeronautics and Space Administration (NASA) advanced satellite-based telemedicine in order to provide future care to astronauts, while also benefiting the Papago Indians in Arizona through a demonstration project called the STARPAHC (Space Technology Applied to Rural Papago Advanced Health Care) project (Freiburger et al., 2007). During the 1970s, the use of this technology spread to other parts of the United States, serving remote and historically underserved communities, such as those in Alaska (Nesbitt and Katz-Bell, 2018). However, without private-sector investment, such projects were not sustainable, leaving the populations they were designed help without the capacity to maintain the expanded access (Greene, 2020).
Following slow growth in the 1980s, the 1990s saw a great expansion of telehealth use and services through the development of statewide telemedicine projects, passage of state and federal legislation making telemedicine services reimbursable, and increasing affordability of telemedicine (Nesbitt and Katz-Bell, 2018). The hub-and-spoke model emerged in which multiple distant care sites were connected to a larger specialty health center. These programs were often funded through legislative appropriations or grants and focused on increasing outpatient access to specialty care (particularly for patients in remote or historically underserved areas) and provision of continuing provider education. Many health systems, which have traditionally operated as competitors, formed telehealth alliances, such as the New Mexico American Telemedicine Association, in order to decrease barriers to health care (Nesbitt and Katz-Bell, 2018).
Research on the efficacy of telehealth also dramatically increased in the 1990s. Publications from the Veterans Health Administration (VHA) and Kaiser Permanente added to the telehealth evidence base and suggested that home telehealth may benefit some patients (Darkins, 2014; Johnston et al., 2000). Telehealth also became more common in correctional facilities due to the costs and significant risks in transporting patients to physically see health care providers (Nesbitt and Katz-Bell, 2018).
Throughout the early 2000s, telemedicine platforms multiplied across states (every state had a platform by 2010) and around the world (Nesbitt and Katz-Bell, 2018). The Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act, enacted in 2001, lowered barriers to telehealth in a number of ways, including requiring payment parity (equivalent payment for in-person and telemedicine visits) by Medicare, requiring Medicare to pay a $24 facility fee payment to the originating site for each telehealth visit, and expanding the range of telehealth services covered under Medicare (Gilman and Stensland, 2013; 106th Congress, 1999). In addition, Teladoc Health, now the world’s largest telemedicine company, was launched in 2002 (Teladoc Health, 2022).
Inpatient and emergency care telehealth services then started to become more common. teleICU care increased and began to incorporate interactive video conferencing and smart alarms in intensive care units (ICUs) (Lilly et al., 2011). The Department of Veterans Affairs (VA) led the way in adapting telehealth to care for patients with chronic health conditions (Nesbitt and Katz-Bell, 2018).
In 2008, the Medicare Improvements for Patients and Providers Act further expanded both covered services and eligible providers, including community mental health centers (Gilman and Stensland, 2013). As internet speed and affordability improved, the Federal Communications Commission (FCC) provided grants to expand broadband to rural areas, further increasing the number of Americans who could access telehealth. In addition, the American Recovery and Reinvestment Act of 2009 helped expand telehealth services, with a focus on disaster preparedness (Nesbitt and Katz-Bell, 2018). The Office for the Advancement of Telehealth, within Health Resources and Services Administration (HRSA), part of the Department of Health and Human Services (HHS), helped start state clinical telehealth networks and funded telehealth research (Nesbitt and Katz-Bell, 2018).
By 2010, 11 states (California, Colorado, Georgia, Hawaii, Kentucky, Louisiana, Maine, New Hampshire, Oklahoma, Oregon, and Texas) had mandated that insurance payers cover telemedicine services (although each state’s rules varied) (Nesbitt and Katz-Bell, 2018). In addition, 36 states covered telehealth services under Medicaid (CCHP, 2018). In 2011, CMS approved proxy credentialing of providers for telehealth services, greatly decreasing barriers to access. Although some state Medicaid programs began to reimburse for more telehealth services, there was tremendous variation across states (Nesbitt and Katz-Bell, 2018). In 2016, 48 states and Washington, DC, reimbursed for live video telemedicine services, and 19 reimbursed for remote patient monitoring (CCHP, 2021). However, despite significant improvements in access for many, telehealth has increasingly received more attention from venture capital than from the sort of government and nonprofit actors that might deliver on the original promise of telehealth for the expansion of health care access to low-income and rural populations (Greene, 2020).
By 2016, 46 percent of health care providers reported using multiple forms of telehealth technology in practice (HIMSS Analytics, 2016). At this time, the top seven diagnoses for Medicare beneficiaries receiving telehealth services were related to mental health (CMS, 2018). In 2020, 85.8 percent of Americans had access to the internet, suggesting that a greater proportion of people in the United States might be able to access telehealth services (Johnson, 2022). However, access to the internet is far from the only barrier to accessing telehealth, while it is a major barrier—others include language barriers between patients and providers, digital literacy, and access to equipment (more on this subsequently) (Park et al., 2018).
What are the key questions, research areas, and products or applications today?
Telehealth and telemedicine occupy a rapidly evolving evidence development and regulatory space. While the literature on telehealth effectiveness is limited, it is expanding rapidly. A 2019 Agency for Healthcare Research and Quality (AHRQ) evidence review included 106 studies of telehealth effectiveness (Seehusen and Azrak, 2019). While evidence was insufficient or low for many specialties, moderate strength of evidence was found for telehealth effectiveness in wound care, psychiatric care, and chronic disease management. Furthermore, patient satisfaction with telehealth services has been consistently found to be high (Orlando et al., 2019; Kruse et al., 2017).
International regulation of telemedicine varies widely. In contrast to other areas of complex regulation, there have been to date no generally applicable treaties governing telemedicine or attempts at legally harmonizing the practice across jurisdictions. This even includes an absence of general laws across countries that are otherwise bound together by supranational organizations like the European Union (EU) (Callens, 2010). Where specific regulations do exist governing telemedicine apart from traditional medicine, almost all countries broadly regulate telemedicine on a national or supranational level in contrast the United States’ federalist (i.e., subnational) approach. Exceptions to this general observation include countries with similarly robust federalist structures like Spain, Australia, Canada, and, to a lesser extent, Germany, which, like the United States, allows subnational jurisdictions to implement their own regulations governing telemedicine (Hashiguchi, 2020). Countries that have specific broad, national legislation implementing a permissive approach to telemedicine include the Netherlands, Finland, Iceland, and Norway (Hashiguchi, 2020). Hungary stands, to date, as a major exception among countries with explicit telemedicine policy, with national legislation restricting (rather than permitting) the practice of telemedicine beyond what would be afforded absent the law (Hashiguchi, 2020).
In the United States, telehealth options for Medicare Advantage patients expanded in January 2020 with the enactment of the 2018 Bipartisan Budget Act, which removed requirements with respect to the originating (patient) and distant (physician) sites, allowing patients to access telehealth services from home (Contreras et al., 2020). In response to the COVID-19 pandemic, the U.S. federal government has relaxed many telehealth regulations and increased telehealth funding. The number of telemedicine visits dramatically increased across the country during the pandemic (Mehrotra et al., 2020). The CMS 1135 waiver and the Coronavirus Preparedness and Response Supplemental Appropriations Act, enacted in March 2020, expanded telehealth benefits for Medicare Advantage patients to patients with standard Medicare by removing requirements that patients be physically located within a health care facility in order to participate in telemedicine (116th Congress, 2020; CMS, 2020). CMS also established equivalent reimbursement (parity) for video telemedicine visits and traditional in-person visits (CMS, 2020). Furthermore, the HHS Office for Civil Rights relaxed the enforcement of software-based violations of the Health Insurance Portability and Accountability Act (HIPAA), enabling flexibility in platforms through which telemedicine is delivered, as huge amounts of health care shifted to telemedicine in a matter of days following the onset of the COVID-19 pandemic (HHS, 2020).
Medicaid has always allowed states the flexibility to reimburse telemedicine visits in whatever way they deemed best, and although many states already required private health insurance and Medicaid plans to cover telehealth, many more expanded these policies in response to the COVID-19 pandemic (APAb, 2022). Some states also relaxed state-specific licensure requirements, allowing providers to conduct telehealth (and teletherapy) services more easily across state lines, although as the pandemic wanes in the United States, states have begun rolling back such measures (PSYPACT, n.d.; Richardson et al., 2022).
Relaxed requirements and reduced barriers to access do not necessarily mean uniform increased utilization, however. A 2018 study found that from 2013 to 2016, though overall telehealth use increased dramatically, this increased use was largely driven by higher-income populations and younger Medicare beneficiaries (Park et al., 2018). Telehealth was less likely to be used by Medicaid beneficiaries and low-income and rural populations, even in states with less restrictive state telehealth policies (Park et al., 2018).
mHealth is much newer than telehealth, and its evidence base is smaller, but it is rapidly growing, seeing $8.1 billion in investments in 2018, aided tremendously by the high-powered computers the vast majority of us carry on our persons, the smartphone, which is designed to track our motion and position in three-dimensional space (Day and Zweig, 2019). mHealth app and device developers have taken advantage of this capacity to turn smartphones into fall detectors, spirometers, heart-rate sensors, and much more, not only expanding diagnostic and treatment options but also generating new kinds of health data and evidence (Sim, 2019). The Apple Health app can combine data collected from the iPhone or Apple watch with a consumer/patient’s electronic health record. The lucrative segment of mHealth focused on concierge care for those with means does expand access to care, but not in the way originally envisioned in the 1970s (Greene, 2020).
Apps specific to COVID-19 have also proliferated in the mHealth space. A survey of iOS and Android apps available between April 27 and May 2, 2020, identified 114 COVID-related apps, 84 (74%) of which were categorized as either health and well-being/fitness or medicine apps. About half of all apps were developed by regional or national governments, and all but one was free (Collado-Borrell et al., 2020).
As alluded to previously, access to the full range of telehealth services is dependent on access to high-speed internet (“broadband”), although it is important to note that a great deal of telehealth still happens by phone. According to the 2018 American Communities Survey (ACS), 18 million U.S. households lacked access to broadband, 60 percent of which had household incomes below $35,000/year (Siefer and Callahan, 2020). Additionally, the substantial racial disparities present in access to broadband can exacerbate racial disparities in use of telehealth (Singh et al., 2020). Internationally, it has been suggested that a 10 percent increase in internet access yields 1–2 percent increase in GDP (DeLaTorre, 2022). Policies aiming to address the “digital divide” are often targeted at building internet infrastructure in rural areas, but many Americans who lack access to broadband actually live in urban regions and are simply unable to afford all but the slowest internet speeds—a fact that has been made clear by stories of children and parents doing their schooling and jobs from the parking lots of public libraries and fast food restaurants during the COVID-19 pandemic (Greene, 2020; Kang, 2020). More inclusive efforts to close the digital divide have emerged, particularly in response to the growing need for broadband in the era of COVID-19. The HEROES Act, a COVID-19 relief bill passed by the U.S. House of Representatives in May 2020, included significant funding to help low-income households pay for broadband and acquire internet-capable devices, as well as funding to expand broadband access to urban health care providers left out of previous efforts to reach rural providers, though it did not receive a vote in the Senate (116th Congress, 2020; Cochrane, 2020). Versions of many of these provisions were maintained in the $900 billion stimulus bill that was signed into law in December 2020 (Montague, 2020).
Currently, the regulation of telehealth in the United States is at a major inflection point. The COVID-19 pandemic has dramatically altered the way that health care is sought and provided, and it is unlikely that the practice of medicine will return to the pre-COVID-19 status quo after the pandemic recedes. The rapid expansion in use of, and reimbursement for, telehealth services in the face of a global pandemic has accelerated the shift from traditional in-person medicine to a normalization of telemedicine. Similarly, the use of (largely non-evidence-based) health and wellness apps, as well as apps that enable digital contact tracing, has expanded over the course of the pandemic. How these products will be used and regulated in a post-COVID-19 world remains to be seen (Figueroa and Aguilera, 2020; JHU, 2020; Lagasse, 2020).
Cross-Sectoral Footprint
The cross-sectoral analysis is structured according to sectors (academia, health care, private sector, government, and volunteer/consumer—see Figure 1 ) and domains (science and technology, governance and enforcement, end-user affordability and insurance reimbursement [affordability and reimbursement], private companies, and social and ethical considerations). The sectors described subsequently are intended to be sufficiently broad to encompass a number of individuals, groups, and institutions that have an interest or role in telehealth. Health care is the primary nonprofit actor of interest, and so in this structure, ‘health care’ has replaced ‘nonprofit’, though other nonprofit actors may have a role in this and other emerging technologies, and, of course, not all health care institutions are nonprofits.

Today, many telehealth technologies are researched, developed, and promoted by a scientific-industrial complex largely driven by market-oriented goals. The development of various components of telehealth may be altered by differing IP regimes. This larger ecosystem is also embedded in a broad geopolitical context, in which the political and the economic are deeply intertwined, shaping national and regional investment and regulation. The political economy of emerging technologies involves and affects not only global markets and regulatory systems across different levels of government but also non-state actors and international governance bodies. Individuals and societies subsequently adopt emerging technologies, adjusting their own values, attitudes, and norms as necessary, even as these technologies begin to shape the environments where they are deployed or adopted. Furthermore, individual and collective interests may change as the “hype cycle” of an emerging technology evolves (Gartner, n.d.). Stakeholders in this process may include researchers, technologists, business firms and industry associations, government officials, civil society groups, worker safety groups, privacy advocates, and environmental protection groups, as well as economic and social justice-focused stakeholders (Marchant et al., 2014).
This intricate ecosystem of stakeholders and interests may be further complicated by the simultaneous introduction of other technologies and platforms with different constellations of ethical issues, modes of governance, and political economy contexts. In contrast to the development of therapeutics or, to a lesser extent, medical devices, the development of telehealth technologies and platforms has not appeared to be controlled by the availability of intellectual property (McGowan et al., 2012). Subsequently, this ecosystem is disaggregated and organized for ease of presentation. This section will address both telehealth and mHealth but will endeavor to address telehealth first and then mHealth in the subsections. It is important to keep in mind that there are entanglements and feedback loops between and among the different sectors, such that pulling on a single thread in one sector often affects multiple areas and actors across the broader ecosystem.
Cross-Sectoral Analysis
For the purposes of this case study, the primary actors within the academic sector interested are those engaging in cost-effectiveness, comparative effectiveness, health services, basic and translational device, and mHealth research; and scholars working in bioethics.
Science and technology: Research on telemedicine has been conducted for decades, primarily focusing on effectiveness and cost relative to traditional in-person care (Torre-Diez et al., 2015). While the literature on telehealth effectiveness is limited, it is expanding rapidly. A 2019 AHRQ evidence review included 106 studies of telehealth effectiveness (Seehusen and Azrak, 2019). While evidence was insufficient or low for many specialties, moderate strength of evidence was found for telehealth effectiveness in wound care, psychiatric care, and chronic disease management. Furthermore, patient satisfaction with telehealth services has been consistently found to be high (Orlando et al., 2019). The evidence base for the use of telehealth and wellness apps (mHealth) is small, and more research is needed, particularly on the effects these technologies may have on reducing or exacerbating existing health disparities.
Governance and enforcement: Within the research context, governance is primarily through institutional human subject research review boards and research ethics boards, research funding bodies, academic publication standards, and scientific and professional societies (i.e., self-regulation).
Affordability and reimbursement: N/A
Private companies: N/A
Social and ethical considerations: There has been some academic research on social factors related to telehealth adoption and use, as well as ethical issues associated with telehealth adoption. There are related, growing literatures on the privacy and other implications of persistent data collection, big data, digital phenotyping, and so forth, with direct relevance to mHealth.
Health Care
Given the focus of CESTI on health and medicine, for the purpose of this case study, the primary actors within the nonprofit sector are those involved in health care.
Science and technology: As noted previously, research on efficacy across specialties is ongoing but limited.
Governance and enforcement: Health care systems are the main hubs for telemedicine. Their use of these technologies is subject to HIPAA regulation, as well as the licensing requirements of the state in which they operate. Proposals related to licensing for practicing across state lines could potentially change the reach of health systems (e.g., a proposal that licensing requirements only apply for the location of the telemedicine provider would enable a provider in a health system located in only one state to reach patients across the country) (Lee et al., 2020).
Physicians are governed by their respective state licensing boards. In general—and with the exception of psychiatry—state licensing boards do not grant their physicians blanket permissions or prohibitions to practice telemedicine, requiring only (again, in general) that physicians provide their patients “competent care” (APAb, 2022).
Professional bodies have also developed position papers regarding telehealth, including in the context of the pandemic (AHA, 2020). In Europe, there are cross-sectoral committees that include academics, industry/technology representatives, and regulators; similarly cross-sectoral committees were established in the United States to address the COVID-19 pandemic (NIH, 2020). These committees could potentially serve as a model for coordination of cross-sectoral governance of emerging technologies.
Affordability and reimbursement: The United States’ multimodal payer system makes reimbursement and payment for medical services in the United States difficult to summarize. Federally organized public payers (e.g., Medicare, Medicaid, the VHA) are largely governed by federal law, while strictures on state-level public and private payers are governed by state law. Each payer—including administrative agencies—sets different rates and schedules for each service, including those pertaining to telemedicine. Beyond this, states may have additional laws in place governing which services must be covered by private insurers.
Parity in reimbursement between in-person and telemedicine-based services remains an issue, and laws in some states require insurers to reimburse telemedicine visits at the same rate as in-person visits. From a health system perspective, this might make telemedicine an attractive option, as it is often less expensive to provide relative to traditional face-to-face care, though state medical boards have often required an in-person consultation before allowing for telehealth services (Lee et al., 2020). Furthermore, the traditional reimbursement model does not incentivize physicians to use telemedicine because they get paid more for in-person services and procedures (Goldberg et al., 2022). There are also basic questions related to implementation of telemedicine more broadly: What are the clinical workflows for telehealth care? How can physicians/health systems leverage and utilize remote monitoring effectively? How does data flow into the health system? Should these data be integrated with the medical record, and if so, how? Who is responsible for understanding and analyzing a potentially near-real-time stream of patient data? What are the shared expectations and liability concerns around these new platforms?
Private companies: Health care institutions partner with private companies that provide many enabling technologies for telehealth, including telemedicine care delivery platforms, monitoring and management technologies, mHealth apps, and more. While some of these technologies may be protected by trade secrets (e.g., confidential algorithms), few are robustly protected by patents given the difficulties in patenting software applications (Price, 2015). Furthermore, there have been calls for more rigorous testing of many of these technologies for clinical effectiveness (Sim, 2019).
Social and ethical considerations: While health data in the United States is regulated by HIPAA, there is no blanket data privacy law (104th Congress, 1996). Data privacy, like medical consent, is largely an issue of contract and tort. Data privacy is arguably the principal international issue concerning telemedicine regulation. Most significantly, the European Union’s General Data Protection Regulation (GDPR) provides a robust set of rights to individuals’ “personal data,” that is, “any information relating to an identified or identifiable natural person” (European Parliament, 2016). This includes the right to forbid its collection; to demand a third party destroy it; and, if electronic, to download it where it resides. Health data, specifically, receives further protections under the GDPR (although there are public health exceptions). The GDPR’s reach is not only cabined within the European Union but extends to anywhere in the world where the processing of European citizens’ data occurs. Penalties for noncompliance can be stiff (European Parliament, 2016). While other countries invested in telemedicine—including Colombia, Costa Rica, and Peru—have data privacy laws, the GDPR seems unique in its global reach and effect on data transmission practices.
In most countries, patient consent for telemedicine tracks with each respective country’s model for other forms of health care delivery. For example, where delivery operates at the physician level, patients’ consent typically is obtained through their physicians. Notable exceptions include Japan and Greece, which require explicit consent from patients before physicians can conduct treatment through telemedicine (Hashiguchi, 2020).
Physicians, particularly in subspecialties conducive to telemedicine (e.g., dermatology and psychiatry) may have workforce concerns as restrictions on cross-jurisdictional medical practice are relaxed. Providers may resist lowering licensing barriers as this could allow for competition from other states’ telehealth services (IOM, 2012).
As mentioned previously, the digital divide has significant equity implications for telehealth access, in addition to other challenges, including language barriers between patients and providers, digital literacy, and access to necessary equipment (Park et al., 2018). There are special issues related to safety, efficacy, and privacy/data security when mHealth devices/toys are used in the treatment of children (Comscore, 2014).
Private Sector
For the purposes of this case study, the primary actors within the private sector are digital health platform providers, startups, and app developers.
Science and technology: Telehealth startups are currently targeting large, self-insured employers with strong incentives to keep costs low (Dorsey and Topol, 2016). mHealth apps have been developed for a wide array of purposes, including tracking fertility and exercise; diabetes management; medication adherence; treating depression, anxiety, and traumatic brain injury; and preventing suicide.
Governance and enforcement: Many companies in the telemedicine space offer services designed to help physicians do their jobs and so fall under the umbrella of “physician practice,” which is not regulated by the U.S. Food and Drug Administration (FDA). Telemedicine platforms used by health systems are subject to stronger scrutiny, but in the interest of expanding access to telemedicine during the COVID-19 pandemic, the HHS Office for Civil Rights has “waived penalties for HIPAA violations against health care providers that serve patients through everyday communications technologies” during the public health emergency (HHS, 2020). There are thousands of health- and wellness-focused apps available for smartphones, some of which make dubious or unproven claims about their effectiveness. In addition to a shallow evidence base about the effectiveness of many health and wellness apps, they also raise significant privacy concerns because they are not all governed by the same privacy laws (like HIPAA) that protect sensitive patient information in traditional care settings (Singer, 2019). While some companies may be required or choose to engage third-party compliance services to monitor their data security, this is not a legal requirement for all.
The FDA’s Digital Health Software Precertification (Pre-Cert) Program has piloted new ways of regulating software-based medical devices, but this regulatory innovation has faced pushback from the U.S. Congress, suggesting that such innovation will be challenging (FDA, 2021; Warren et al., 2018).
Affordability and reimbursement: As described in more detail subsequently, states can and have mandated that commercial insurance plans offer parity for telemedicine visits (Yang, 2016). Historically, concern about medical liability has been a persistent barrier to the broader adoption of telemedicine (WHO, 2010). The United States, which has a robust medical practice tort system, appears to assign liability in much the same way for errors in telemedicine as it does for traditional practice. There is frequently lack of clarity about who should pay for mHealth technology, in particular when prescribed by a physician. Many mHealth apps are free or low-cost to download, though the safety and efficacy of many of these apps are unclear, and there are significant associated data privacy concerns.
As noted previously, an explicit goal of telehealth has long been expanded access in rural and remote areas. There are a number of companies that seek to address barriers to health and health care beyond geographic barriers and are focused squarely on improving equity in health care, such as ConsejoSano (SameSky Health), Hazel Health, and CareMessage (CareMessage, n.d., Hazel, n.d.; SameSky Health, n.d.).
At the same time, another major driver of telehealth is lowering the cost of health care. Insurers are motivated by the low cost of telehealth compared to the high cost of in-person care and self-insured employers also highly motivated to reduce costs and maintain a healthy workforce.
Private companies: One assessment of digital health startups highlighted 150 companies that had collectively raised more than $20 billion, and which had among them established partnerships with the American Heart Association, Sanofi, Cigna, Mount Sinai Health System, Mercy Health, and Arizona Care Network, demonstrating tremendous interest and growth in this space (CBInsights, 2021). Apple has partnered with both Aetna and the government of Singapore to incentivize individuals to engage in health-promoting behaviors. Fitbit has a similar partnership with United Health (Aetna, n.d.; Elegant, 2020; Gurdus, 2017).
Social and ethical considerations: Significant concerns about privacy, transparency, and accountability with regard to the algorithms and data generation by commercial devices and apps. As noted previously, there have been calls for more rigorous testing of many of these technologies for clinical effectiveness (Sim, 2019). The is often a wide range of third parties involved in telehealth delivery, some of which will be outside the “covered entity” and be governed by different (or few) rules (Gerke et al., 2020). Equity concerns are raised by algorithms trained on the healthy, well-off, and White.
For the purposes of this case study, the primary actors within the government sector are both the federal government and the states, which play critical gatekeeping (or facilitating) roles in the development and evolution of telehealth.
Science and technology: As noted previously, NASA and the VA have been leaders in telehealth research and development. The federal government also partners with tribal governments to administer the Indian Health Service (IHS), which provides care to American Indian/Alaska Native (AI/AN) people across the country. Telemedicine is particularly important to the work of the IHS due to the rurality of many AI/AN communities, which has led to innovation in telehealth systems (Hays et al., 2014). The IHS also has a Telebehavioral Health Center of Excellence, which offers behavioral health care and mental health care through multiple telehealth modalities (IHS, n.d.).
Governance and enforcement: U.S. federal and state governments have significant interests in the governance of telehealth. Prime among these is their interest in requiring public and private insurers to provide reimbursement for telemedicine services. As a result of the COVID-19 pandemic, CMS has waived reimbursement requirements that patients be physically located within a health center when receiving telemedicine services, making it possible for millions to access care safely from their homes. Every state has different reimbursement requirements for their state Medicaid plan, and states also have the power to control reimbursement parity for commercial insurance, which has led to the development of essentially 50 different reimbursement policies across the country.
As noted, the VA has been a leader in telehealth adoption and implementation, as they retain significant control over telemedicine and telehealth offered within the VHA, including control over licensure requirements and copay amounts (CRS, 2019). Since 2012, the VA secretary has had the ability to waive copays for telemedicine provided to veterans in their homes, and VA-employed providers can practice telemedicine across state lines with any patients within the VHA (CRS, 2019).
Another key role for the government is the protection of protected health information (PHI)—personally identifiable information that relates to a medical condition, the provision of care, or payment—which is regulated via HIPAA (104th Congress, 1996). HIPAA establishes restrictions on the dissemination of PHI by “covered entities”—providers, plans, clearinghouses, or business—without the express consent of the patient.
HIPAA is of particular concern in telemedicine because PHI is necessarily generated in telemonitoring and store-and-forward technologies. In addition, the nature of telemedicine is such that users of telemonitoring and store-and-forward technologies are almost certainly “covered entities” under the statute, that is, providers, businesses, or health care plans. In addition, HIPAA demands extra precautions from covered entities for most telemedicine applications under the HIPAA Security Rule, a regulation promulgated by HHS that concerns electronic PHI (CFR, 2011). Prior to the COVID-19 pandemic, the HIPAA Security Rule limited the types of platforms that could be used for the transmission of electronic PHI. In March 2020, the HHS Office for Civil Rights issued a Notification of Enforcement Discretion indicating that providers who engage in telemedicine using non-public-facing communication technologies in good faith will not be subject to penalties for noncompliance with HIPAA rules (HHS, 2021).
With respect to medical devices used in telemedicine, these are typically regulated at the federal level by the FDA (94th Congress, 1976). For example, the Da Vinci Xi Surgical System, a robotic surgical assistant and a form of interactive telemedicine, is regulated by the FDA as a Class II device (Stevenson, 2017).
Telemedicine encompasses devices in all three risk classes, from a WiFi-enabled digital pulse oximeter (Class I) to remotely controlled continuous glucose monitoring systems (Class III). In some instances, FDA considers software to constitute a medical device (FDA, 2017).
Affordability and reimbursement: See the previous discussion of reimbursement. Various national efforts to expand internet access have been key to the expansion of telehealth access, and will continue to be critical moving forward, as advanced technologies demand higher bandwidth.
Social and ethical considerations: Ethical issues raised by telehealth in the government sector include disparities in telehealth (and broadband) access, fiduciary duties of health care providers, privacy, equity, and workforce concerns.
Volunteer/Consumer
For the purposes of this case study, the primary actors within the volunteer/consumer sector are patients and consumers accessing telehealth, including mHealth. It is important to keep in mind that many members of “the public” nationally and internationally never have the opportunity to be patients or consumers of emerging technologies, and so do not show up in the following analysis. These members of the public may nonetheless be affected by the development, deployment, and use of such technologies, and those impacts should be taken into account.
Science and technology: Prior to the COVID-19 pandemic, mHealth apps may have been most people’s primary experience with telehealth, as many of these apps are free or low-cost to download for iOS and Android phones (Friedman et al., 2022). There is little data available on the safety and efficacy of many of these apps.
Governance and enforcement: Currently, there is little regulatory enforcement of many mHealth apps, though a number of mHealth devices have received FDA clearance.
Affordability and reimbursement: As noted previously, insurance coverage for telehealth has expanded dramatically in recent years, and particularly since the start of the COVID-19 pandemic. mHealth apps are free or low-cost to download, though they require that the consumer have a smartphone and internet access.
Private companies: These include mHealth app developers and companies like Apple and FitBit, offering direct-to-consumer health and wellness applications outside health care institutions and employee-sponsored wellness programs.
Social and ethical considerations: Potential drivers include adult children caring for aging parents at a distance, seeking the capacity to both monitor their parents’ health and safety and communicate with their parents’ health care providers; concerns about equity regarding access if Apple continues to expand in the mHealth space and Android continues to lag (more than half of U.S. smartphone owners have Androids, and Android users have a lower average income than iPhone users); and concerns about the use of mHealth devices/toys with children in regard to safety, efficacy, and privacy/data security (Comscore, 2014).
Ethical and Societal Implications
What is morally at stake what are the sources of ethical controversy does this technology/application raise different and unique equity concerns.
In outlining the concerns of the authors in terms of the use of this technology, we considered the following ethical dimensions, as outlined in the recent National Academies of Sciences, Engineering, and Medicine report A Framework for Addressing Ethical Dimensions of Emerging and Innovative Biomedical Technologies: A Synthesis of Relevant National Academies Reports (NASEM, 2019).
- Promote societal value
- Minimize negative societal impact
- Protect the interests of research participants
- Advance the interests of patients
- Maximize scientific rigor and data quality
- Engage relevant communities
- Ensure oversight and accountability
- Recognize appropriate government and policy roles
It is important to keep in mind that different uses of this technology in different populations and contexts will raise different constellations of issues. For example, telephone-based telehealth can be very different than video- or app-based telehealth, with different implications when used to serve urban, high-income adults versus rural, low-income children. Some of the specific concerns might include the following (Nittari et al., 2020):
- Is the quality of care delivered via any given telehealth platform of comparable quality to in-person care? What is gained? What is lost?
- How does a focus on efficiency or cost savings affect compassion/patient welfare? (Jacobs, 2019)
- How is continuity of care affected by communication gaps or barriers between providers at a distance, the patient, a physically present clinical care team, mHealth applications, and documentation in the medical record?
- Are there risks to safety associated with virtual physical exams and treatment?
- What is the effect on the physician–patient relationship and the establishment of trust in the absence of any physical interaction?
- What are the risks to patient privacy and confidentiality, particularly in mHealth, and how can they be mitigated?
- What kind of access to and control over data produced by mHealth devices do patients/consumers have?
- What are the proprietary interests over domains of fragmented patient data and how do they affect care?
- How can governance address the blurring boundary between personal medical data, public health data, and monetized consumer data?
- What ought the requirements be for content and documentation of informed consent for telehealth as a mode of care, and within telehealth, for example, for the transmission and processing of health data?
- How should countries regulate telemedicine when telemedicine services and patients are split across jurisdictions? When the operation of devices is split across jurisdictions?
- How will the changing global political climate likely affect the regulation of telemedicine?
- What are the issues raised by telemedicine across state and national borders, including both ethical (e.g., lack of cultural awareness or familiarity) and legal (e.g., cross-jurisdictional credentialing, regulation, liability)?
- What is the level of reliability and fidelity of data transmitted from mHealth devices?
- Who, how, and with what permissions can various actors access, store, and use the vast amounts of data generated by various telehealth interactions?
- How transparent and accountable are the algorithms used by commercial telehealth devices/apps, as well as the data collection, storage, and use by telehealth companies?
- Which entities involved in telehealth are outside the “covered entity” for the purposes of HIPAA, and how do they collect, store, and use patient data?
- Will a shift to telehealth increase or decrease the isolation and quality of life of historically underserved and marginalized populations, including the elderly, and others with visual, hearing, or cognitive impairments? What about caregivers managing a dependent’s telehealth participation?
Beyond Telehealth
mHealth “is at the swirling confluence of remote sensing, consumer-facing personal technologies, and artificial intelligence (AI)” (Sim, 2019). Currently, AI, wearable and ambient sensors, and other emerging technologies are being used in research and are able to suggest future possibilities, but these have not yet been realized in the market. AI, of course, brings with it a whole host of additional concerns related not only to the technical challenges, including reliability and explainability of autonomous systems but also significant ethical concerns, including those related to bias in training data leading to structural racism being replicated at scale with AI, trust, trustworthiness of systems, and so on. Smart homes, also in ascendance, hold potential in the telehealth space, but the potential health benefits (and risks) remain largely in the future.
As alluded to previously, it is possible to foresee numerous future scenarios regarding the evolution of telehealth. In an effort to probe the kinds of worries the authors have about the trajectories of emerging technologies, to expand the range of lessons learned from each case, and ultimately to “pressure test” the governance framework, the authors have developed a brief “visioning” narrative that pushes the technology presented in the core case 10–15 years into the future, playing out one plausible (but imagined) trajectory. The narrative was developed iteratively in collaboration with a case-specific working group, with additional feedback from members of CESTI. All reviewers are acknowledged in the back matter of this paper. Each narrative is told from a particular perspective and is designed to highlight a small set of social shifts that shape and are shaped by the evolving technology.
Telehealth Case Visioning Narrative
Perspective: A remote caregiver and digital health navigator dyad
It is 2035, and the home has become the preferred site for the receipt of most acute and non-acute medical services (labs, imaging, nursing visits, retail pharmacy) in the United States. Termed hospital-at-home (HaH), it is also the dominant model for non-ICU-level in-person care in much of the world. Although this care paradigm has been around for decades, the COVID-19 pandemic catalyzed this shift due to physical distancing requirements and fears among patients about contracting the virus within the hospital setting. Massive investments from the private sector into telemedicine platforms, coupled with technology advancements in AI-enabled remote monitoring, voice-activated medical devices, augmented reality, and sensors were also pivotal in this care transformation. Results from randomized controlled trials showed that the HaH was just as effective as the traditional hospital setting for a wide range of medical conditions, and with lower cost. However, the data on patient safety has been mixed thus far, with certain kinds of care episodes demonstrating clear reductions in adverse events while others result in poorer outcomes, often due to poor recognition of the need for escalation to emergency care (e.g., malignant bowel obstruction being mistaken for constipation). Hospital visits are increasingly limited to serious conditions that mandate an in-person work-up (e.g., biopsy for a cancer diagnosis) or procedural intervention (e.g., surgical procedure or cardiac catheterization).
Chronic Disease Management
Beyond increasing access to specialty providers (physicians, nurses, pharmacists, physical therapists), this new care paradigm revolutionized chronic disease management. Through “digital touchpoints,” providers were able to durably increase patients’ engagement with their own self-care and remotely manage the trajectory of chronic diseases at increasingly earlier time points. By leveraging ambient clinical intelligence tools (i.e., Internet of Medical Things [IoMT]), all data became re-imagined as health care data, including music preferences, voice pitch, communication logs, gait, step counts, and sleep patterns—a process known as digital phenotyping. In this new personalized care paradigm, conditions such as hypertension, diabetes, heart failure, and renal insufficiency were now managed prospectively and continuously as opposed to in a reactive and episodic fashion. Patients could now be managed within the context of their lives, and for many, this meant the ability to safely “age in place.” However, over time questions arose as to how the governance of emerging technologies intersects with the provision of care in the home. Specifically, issues regarding data standards, quality assurance, interoperability, oversight, bias, and transparency were yet to be definitively addressed in the context of care delivery. Whom should be held legally responsible in instances of harm due to erroneous automated diagnosis? How can the authenticity, accuracy, and integrity of such a wide variety of devices be reliably established?
Impact on Equity
Unfortunately, HaH in some cases led to a widening of existing equity gaps. This is because many of the infrastructural technologies were not developed through the lens of equity or cultural competency (e.g., to account for language barriers, vision/hearing/physical impairments, digital and health literacy, or other impacts of the social determinants of health). Non-English-speaking patients who were more than 80 years of age had tremendous difficulty engaging with this care model, as their communication preferences were more consistent with an in-person encounter. Although HaH uptake was relatively low in areas of high economic deprivation due to poor infrastructure and add-on device costs (smartphones and sensing equipment), great strides were made in improving access to rural communities, in step with investments in broadband and satellite internet service. For the first time, specialty care became available in many areas previously described as “medical deserts.” There was also growing recognition that HaH models implicitly exclude individuals experiencing unstable housing or homelessness.
Impact on the Health Care Workforce
The often ad hoc implementation of these virtual workflows sent prevailing levels of physician burnout soaring even higher due to the lack of clear practice guidelines, time to engage with the data and patient communication that these systems generate, and concerns for liability exposure. Lengthy wait times were reported in many urban areas, as physicians now had to manage two distinct clinic schedules (in-person and virtual). There was also considerable displacement of many health care provider roles due to automation and the transition to HaH. Custodial staff, nursing assistants, clerical workers, and some administrative staff roles were transitioned out of the traditional medical infrastructure and into caretaker or home health worker roles. For those “essential health care workers” such as nurses and physicians, retraining was set in motion by credentialing bodies to ensure that fluency in statistics, data science, and information systems became core competencies, allowing these workers to remain relevant and effective in the new digital age. Rote memorization of medical facts was no longer the norm in medical schools. A stronger emphasis was also placed on the human skills that cannot be displaced with automation such as empathy, physical examination, and implicit bias awareness. New health care roles also emerged in this data-rich delivery paradigm, such as digital health navigators, telenurses, and health data specialists. However, many of these new positions and several traditional ones (e.g., physicians, nurses, care coordinators) were increasingly outsourced to global vendors in an attempt to reduce the administrative costs of health care. In this distributed staffing model, international hubs of excellence also began to emerge for certain conditions or treatments (e.g., Sweden for the best interpretation of radiology images). With this in mind, the broader question of how to appropriately regulate remote second opinions across international borders arose. What licensure requirements should be enforced for the practice of international telemedicine? In an increasingly networked world, do state-based licensures still make sense? Calls for the nationalization of medical licensure, or at a minimum the harmonization of requirements across states, were proposed by a variety of stakeholders.
Data Privacy, Trust, and the Wisdom of Crowds
Mr. Jeff Jackson is a 63-year-old Black male with hard-to-control type 2 diabetes, early-onset Alzheimer’s disease, and stable chronic heart failure (CHF). He has chosen to live alone in Youngstown, Ohio, since his wife died 5 years ago. An implanted microchip is able to sample, interpret, and transmit biometric (heart rate, temperature, oxygen saturation) and biochemical data (blood glucose, sodium levels, creatinine levels) about Mr. Jackson at high frequency. AI algorithms embedded within wall-mounted camera-based sensors are also able to detect the progression of his Alzheimer’s or warning signs of acute exacerbations of his CHF. All of this information is relayed 24/7 to a “digital health navigator” assigned by his health plan who serves as a health coach and care coordinator. As outlined in the consent agreement, monthly summaries of routine care are sent to his 23-year-old daughter, Jean, who resides in Miami, Florida. Potentially concerning events sensed in Ohio automatically trigger real-time “red alerts” to both the digital navigator and Jean. Arrangements like this raised many questions during their rollout, including but not limited to the potential vulnerability of these technologies to data breaches and cyberattacks, particularly since the identifiable medical record of every U.S. patient was transitioned to the cloud to facilitate interoperability and timely access. Should HIPAA include the home digital infrastructure in its scope? Under what circumstance should employers or insurance companies have access to personal data? What should be the recourse for care episodes involving harm due to egregious digital navigator negligence? Lastly, instances wherein elder or child abuse or domestic violence were detected using camera-based sensors (“bycatching”) raised ethical concerns as to whether the gravity of these offenses justified circumventing the confidentiality, privacy, and anonymity of involved patients and family members. These events also give rise to the broader question of who owns or is able to repossess these data. Will commercial entities be able to contract and monetize passively captured (audio or video) personal information (e.g., targeted advertising on social media based on fridge contents)?
About 6 months ago, based on his personality traits, risk preferences, and at the strong suggestion of his daughter, Jeff joined a health platform called “All2Gether” that linked individuals across the globe based on more than 200 phenotypes. The goal was to provide phenotype-specific social support to reduce loneliness. The platform offered crowd-sourced medical advice based on lived experiences, behavioral change interventions, and in some instances, mental health therapies based on biofeedback techniques. The much-heralded age of “democratizing medical knowledge” had finally arrived, with these platforms now able to serve millions of people worldwide and drive robust engagement. Over time, Jean had grown much more comfortable entrusting her father’s health data to these cloud-based platforms, rather than a primary care physician or the digital health navigation company. For Jean, this mistrust in her father’s primary care physician and the digital health navigation company was undergirded by the fact that neither she nor Jeff had direct access to the raw data or proprietary algorithms that informed his care. Conspiracy theories and science denial began to rapidly proliferate on these platforms, casting doubt on the value of long-established medical treatments and entrenching health care mistrust. This accelerated in some quarters, a rejection of digital therapeutics and data-driven medicine all together, in favor of more relationship-based approaches to health care.
The international reach of these companies also made regulatory oversight difficult because the practice of medicine is usually controlled through state-specific licensure. Legal experts pointed out that these international platform companies are often predatory and in violation of the existing corporate practice of medicine. Proponents argue that these companies are not “health services establishments” and their business model does not constitute a “provider–patient relationship,” in fact, they claim it is no different from a patient-initiated search engine query. Furthermore, for many patients in rural areas and parts of the developing world, these platforms are the only portal to timely and affordable medical advice. All of these issues are illustrative of the fact that many of the normative behaviors and standards around the practice of medicine evolved well before the information boom associated with the internet and digital care transformation catalyzed by the COVID-19 pandemic.
Telehealth Case Study: Lessons Learned
Some lessons drawn from the above core case and visioning exercise that can inform the development of a cross-sectoral governance framework for emerging technologies focused on societal benefit are given below.
- The coexistence of health and non-health (e.g., wellness) applications can complicate governance.
- It is important to keep in mind the dual roles of state and federal regulation, as well, potentially, of regional (e.g., European Union) regulation.
- There are opportunities for shared or distributed governance in the gaps between regulatory authorities.
- There is a potential role for cross-sectoral governance groups at multiple levels and stages of governance.
- It is important to keep in mind the role of key enabling technologies (e.g., internet access and speed) in the development of the primary technology of interest.
- Key stakeholders to a technology will need to be adequately prepared for large shifts (e.g., dramatic ramping up of telehealth).
- Opportunities for regulatory nimbleness have been revealed by the federal response to the COVID-19 pandemic (e.g., steps skipped).
- Attention must be paid to the equity implications of access (or lack thereof) to enabling technologies.
- Attention should be paid to identifying and assessing the impact of intangible losses (e.g., healing touch, patient–provider relationships).
- Despite an explicit focus and justification for telehealth based on concerns about equity and access, success has been mixed—improving access in some cases and recapitulating existing inequities in others.
- Special attention must be paid to technologies requiring collection, storage, and use of human data.
- As the degree to which our lives are lived online versus in-person, we can become increasingly alienated from our normal markers of trust.
- We lack appropriate governance tools for a health care delivery landscape that is becoming increasingly digital and international.
- We may need to reconsider the traditional risk/benefit analysis of health care treatments when the opportunity for “immediate rescue” in situations of acute decompensation, no longer exists due to physical distance.
- One person’s valued benefit is another person’s harm (and vice versa) (e.g., home monitoring for safety versus surveillance).
- In order to adequately assess the risk/benefit balance, we need to make the trade-offs explicit (e.g., gains in convenience versus loss of privacy).
- We need both ethics and governance frameworks for addressing instances of “bycatching” (e.g., elder abuse captured via camera-based sensors).
- Technology (beyond traditional social media) can drive or erode trust in medical expertise (e.g., dissemination of false information about available treatment options on online platforms).
- There is flexibility/lack of oversight in the grey area that exists following the development of promising data regarding a new technology, but before proven efficacy and regulated products; this lack of oversight can drive innovation and investment in emerging technologies or delivery models, but also comes with risks.
- In the digital home, there are no silos around work/personal or public/private. What happens when the same living environment has to pivot from a place of rest to a place of work (remote work) to a place to get care (hospital-at-home)?
Join the conversation!
Download the graphics below and share on social media!

- 94th Congress. 1976. Public Law 94-295. Available at: https://www.govinfo.gov/content/pkg/STATUTE-90/pdf/STATUTE-90-Pg539.pdf (accessed July 7, 2022).
- 104th Congress. 1996. H.R. 3103—Health Insurance Portability and Accountability Act of 1996. Available at: https://www.govinfo.gov/content/pkg/PLAW-104publ191/pdf/PLAW-104publ191.pdf (accessed July 7, 2022).
- 106th Congress. 1999. H.R. 5661—Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000. Available at: https://www.congress.gov/bill/106th-congress/house-bill/5661 (accessed July 6, 2022).
- 116th Congress. 2020. H.R. 6074—Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. Available at: https://www.congress.gov/bill/116th-congress/house-bill/6074 (accessed July 6, 2022).
- 116th Congress. 2020. H.R. 6800—The Heroes Act. Available at: https://www.congress.gov/bill/116th-congress/house-bill/6800/text#toc-HB620586BD56748DB89E836562C948801 (accessed July 7, 2022).
- Aetna. n.d. Attain. Available at: https://www.attainbyaetna.com (accessed July 7, 2022).
- American Heart Association (AHA). 2020. Expanding access to care through telehealth. Available at: https://www.heart.org/-/media/files/about-us/policy-research/policy-positions/access-to-healthcare/telehealth-policy-guidance-document-2020.pdf?la=en (accessed July 7, 2022).
- American Psychiatry Association (APAa). 2020. What is telepsychiatry? Available at: https://www.psychiatry.org/patients-families/what-is-telepsychiatry (accessed July 1, 2020).
- American Psychological Association (APAb). 2022. Telehealth guidance by state during COVID-19. Available at: https://www.apaservices.org/practice/clinic/covid-19-telehealth-state-summary (accessed July 6, 2022).
- Andrews, E. L. 1996. Communications reshaped: The overhaul; Congress votes to reshape communications industry, ending a 4-year struggle. The New York Times, February 2. Available at: https://www.nytimes.com/1996/02/02/business/communications-reshaped-overhaul-congress-votes-reshape-communications-industry.html (accessed July 6, 2022).
- Bauer, K. A. 2001. Home-based telemedicine: A survey of ethical issues. Cambridge Quarterly of Healthcare Ethics 10(2):137–146. https://doi.org/10.1017/s0963180101002043.
- Callens, S. 2010. The EU legal framework on e-health. In Health Systems Governance in Europe , edited by E. Mossialos, G. Permanand, R. Baeten, and T. Hervey. Available at: https://www.euro.who.int/__data/assets/pdf_file/0006/138147/E94886_prelims.pdf (accessed July 6, 2022).
- CareMessage. n.d. Our mission. Available at: https://www.caremessage.org (accessed July 7, 2022).
- CBInsights. 2021. The digital health 150: The top digital health companies of 2021. Available at: https://www.cbinsights.com/research/report/digital-health-startups-redefining-healthcare/#method (accessed July 7, 2022).
- Center for Connected Health Policy (CCHP). 2021. State telehealth laws and Medicaid program policies. Available at: https://www.cchpca.org/2021/10/Fall2021_ExecutiveSummary_FINAL.pdf (accessed July 6, 2022).
- Center for Connected Health Policy (CCHP). 2018. Staying connected; a progress report: Reimbursement under the Telemedicine Development Act of 1996: Summary report. Available at: https://www.cchpca.org/resources/staying-connected-a-progress-report-reimbursement-under-the-telemedicine-development-act-of-1996-summary-report (accessed July 6, 2022).
- Centers for Medicare & Medicaid Services (CMS). 2020. President Trump expands telehealth benefits for Medicare beneficiaries during COVID-19 outbreak. Available at: https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak (accessed July 6, 2022).
- CMS. 2018. Information on Medicare telehealth. Available at: https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Information-on-Medicare-Telehealth-Report.pdf (accessed July 6, 2022).
- CMS. 2011. Telemedicine services in hospitals and critical access hospitals (CAHs). Available at: https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertificationgeninfo/downloads/scletter11_32.pdf (accessed July 1, 2022).
- Cochrane, E. 2020. House passes $3 trillion aid bill over Republican opposition. The New York Times, May 15. Available at: https://www.nytimes.com/2020/05/15/us/politics/house-simulus-vote.html (accessed July 7, 2022).
- Code of Federal Regulations (CFR). 2011. 45 CFR 160.101—Statutory basis and purpose. Available at: https://www.govinfo.gov/app/details/CFR-2011-title45-vol1/CFR-2011-title45-vol1-sec160-101 (accessed July 7, 2022).
- Collado-Borrell, R., V. Escudero-Vilaplana, C. Villaneuva-Bueno, A. Herranz-Alonso, and M. Sanjurjo-Saez. 2020. Features and functionalities of smartphone apps related to COVID-19: Systematic search in app stores and content analysis. Journal of Medical Internet Research 22(8):e20334. https://doi.org/10.2196/20334.
- Comscore. 2014. iPhone users earn higher income, engage more on apps than Android users. Available at: https://www.comscore.com/ita/Public-Relations/Infographics/iPhone-Users-Earn-Higher-Income-Engage-More-on-Apps-than-Android-Users (accessed July 7, 2022).
- Congressional Research Service (CRS). 2019. Department of Veterans Affairs (VA): A primer on telehealth. Available at: https://sgp.fas.org/crs/misc/R45834.pdf (accessed July 7, 2022).
- Contreras, C. M., G. A. Metzger, J. D. Beane, P. H. Dedhia, A. Ejaz, and T. M. Pawlik. 2020. Telemedicine: Patient-provider clinical engagement during the COVID-19 pandemic and beyond. Journal of Gastrointestinal Surgery 24(7):1692–1697. https://doi.org/10.1007/s11605-020-04623-5.
- Darkins, A. 2014. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: A study in the diffusion of innovation. Telemedicine and e-Health 20(9). https://doi.org/10.1089/tmj.2014.0143.
- Day, S., and M. Zweig. 2019. 2018 year end funding report: Is digital health in a bubble? Rock Health, January 7. Available at: https://rockhealth.com/reports/2018-year-end-funding-report-is-digital-health-in-a-bubble (accessed July 6, 2022).
- DeLaTorre, M. 2022. Personal communication.
- Doarn, C. R., S. Pruitt, J. Jacobs, Y. Harris, D. M. Bott, W. Riley, C. Lamer, and A. L. Oliver. 2014. Federal efforts to define and advance telehealth—a work in progress. Telemedicine Journal and e-Health 20(5):409–418. https://doi.org/ 10.1089/tmj.2013.0336.
- Dorsey, E. R., and E. J. Topol. 2016. State of telehealth. New England Journal of Medicine 375(2):154–161. https://doi.org/10.1056/NEJMra1601705.
- Elegant, N. X. 2020. One country is now paying citizens to exercise with their Apple Watch. Fortune, September 16. Available at: https://fortune.com/2020/09/16/apple-watch-exercise-work-out-singapore-pay-government (accessed July 7, 2022).
- European Parliament. 2016. Regulation (EU) 2016/679 of the European Parliament and the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation). Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32016R0679 (accessed July 7, 2022).
- Figueroa, C. A., and A. Aguilera. 2020. The need for a mental health technology revolution in the COVID-19 pandemic. Frontiers , June 3. https://doi.org/10.3389/fpsyt.2020.00523.
- U.S. Food and Drug Administration (FDA). 2021. Digital health software precertification (pre-cert) program. Available at: https://www.fda.gov/medical-devices/digital-health-center-excellence/digital-health-software-precertification-pre-cert-program (accessed July 7, 2022).
- FDA. 2017. Software as a medical device (SAMD): Clinical evaluation. Available at: https://www.fda.gov/media/100714/download (accessed July 7, 2022).
- Freiburger, G., M. Holcomb, and D. Piper. 2007. The STARPAHC collection: Part of an archive of the history of telemedicine. Journal of Telemedicine and Telecare 13(5):221–223. https://doi.org/10.1258/135763307781458949.
- Friedman, A. B., S. Gervasi, H. Song, A. M. Bond, A. T. Chen, A. Bergman, G. David, J. M. Bailey, R. Brooks, and A. Smith-McLallen. 2022. Telemedicine catches on: Changes in the utilization of telemedicine services during the COVID-19 pandemic. The American Journal of Managed Care 28(1). Available at: https://www.ajmc.com/view/telemedicine-catches-on-changes-in-the-utilization-of-telemedicine-services-during-the-covid-19-pandemic (accessed July 7, 2022).
- Gartner. n.d. Gartner hype cycle. Available at: https://www.gartner.com/en/research/methodologies/gartner-hype-cycle (accessed July 7, 2022).
- Gerke, S., C. Shachar, P. R. Chai, and I. G. Cohen. 2020. Regulatory, safety, and privacy concerns of home monitoring technologies during COVID-19. Nature Medicine 26:1176–1182. https://doi.org/10.1038/s41591-020-0994-1.
- Gershon-Cohen, J., and A. G. Cooley. 1950. Telognosis. Radiology 55(4):582–587. https://doi.org/10.1148/55.4.582.
- Gilman, M., and J. Stensland. 2013. Telehealth and Medicare: Payment policy, current use, and prospects for growth. Medicare & Medicaid Research Review 3(4):mmrr.003.04.a04. https://doi.org/10.5600/mmrr.003.04.a04.
- Global Neuroethics Summit Delegates, K. S. Rommelfanger, S.-J. Jeong, A. Ema, T. Fuushi, K. Kasai, K. M. Ramos, A. Salles, and I. Singh. 2018. Neuroethics questions to guide ethical research in the international brain initiatives. Neuron 100(1):19–36. https://doi.org/10.1016/j.neuron.2018.09.021.
- Goldberg, E. M., M. P. Lin, L. G. Burke, F. N. Jimenez, N. M. Davoodi, and R. C. Merchant. 2022. Perspectives on telehealth for older adults during the COVID-19 pandemic using the quadruple aim: Interviews with 48 physicians. BMC Geriatrics 22(188). https://doi.org/10.1186/s12877-022-02860-8.
- Greene, J. A. 2020. As telemedicine surges, will community health suffer? Boston Review, April 13. Available at: https://bostonreview.net/articles/jeremy-greene-telemedicine-and-new-infrastructure-care (accessed July 6, 2022).
- Gurdus, L. 2017. UnitedHealthcare and Fitbit to pay users up to $1,500 to use devices, Fitbit co-founder says. CNBC, January 5. Available at: https://www.cnbc.com/2017/01/05/unitedhealthcare-and-fitbit-to-pay-users-up-to-1500-to-use-devices.html (accessed July 7, 2022).
- Hashiguchi, T. C. O. 2020. Bringing health care to the patient: An overview of the use of telemedicine in OECD countries. OECD Health Working Papers no. 116. Available at: https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=DELSA/HEA/WD/HWP(2020)1&docLanguage=En (accessed July 1, 2022).
- Hays, H., M. Carroll, S. Ferguson, C. Fore, and M. Horton. 2014. The success of telehealth care in the Indian Health Service. Virtual Mentor 16(12):986–996. https://doi.org/10.1001/virtualmentor.2014.16.12.stas1-1412.
- Hazel. n.d. Hazel provides all children whole child health care. Available at: https://www.hazel.co (accessed July 7, 2022).
- HealthIT.gov. 2019. What is telehealth? How is telehealth different from telemedicine? Available at: https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine (accessed July 1, 2022).
- U.S. Department of Health and Human Services (HHS). 2021. Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. Available at: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (accessed July 7, 2022).
- HHS. 2020. OCR announces notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. Available at: https://www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html (accessed July 6, 2022).
- Health Professions Council of South Africa (HPCSA). 2020. Guidelines on telemedicine in South Africa. Available at: https://www.hpcsa.co.za/Uploads/Press%20Realeses/2020/Guidelines_to_telemedicine_in_South_Africa.pdf (accessed July 1, 2020).
- HIMSS Analytics. 2016. 2016 telemedicine study. Available at: http://www.himssanalytics.org/research/himss-analytics-essentials-brief-2016-telemedicine-study (accessed December 30, 2020).
- Indian Health Service (IHS). n.d. About telehealth and telebehavioral health. Available at: https://www.ihs.gov/telebehavioral/abouttelehealth (accessed July 7, 2022).
- Institute of Medicine (IOM). 2012. The role of telehealth in an evolving health care environment: Workshop summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/13466.
- IOM. 1996. Telemedicine: A guide to assessing telecommunications for health care. Washington, DC: National Academy Press. https://doi.org/10.17226/5296.
- Jacobs, J. 2019. Doctor on video screen told a man he was near death, leaving relatives aghast. The New York Times, March 9. Available at: https://www.nytimes.com/2019/03/09/science/telemedicine-ethical-issues.html (accessed July 7, 2022).
- Johns Hopkins University (JHU). 2020. Digital contact tracing for pandemic response: Ethics and governance guidance. Edited by Jeffrey P. Kahn and the Johns Hopkins Project on Ethics and Governance of Digital Contact Tracing Technologies. Available at: https://www.press.jhu.edu/books/title/12716/digital-contact-tracing-pandemic-response (accessed July 7, 2022).
- Johnson, J. 2022. Internet user penetration in the United States from 2018 to 2027. Available at: https://www.statista.com/statistics/590800/internet-usage-reach-usa (accessed July 6, 2022).
- Johnston, B., L. Wheeler, J. Deuser, and K. H. Sousa. 2000. Outcomes of the Kaiser Permanente Tele-Home Health Research Project. Archives of Family Medicine 9(1):40–45. https://doi.org/10.1001/archfami.9.1.40.
- Kang, C. 2020. Parking lots have become a digital lifeline. The New York Times, May 5. Available at: https://www.nytimes.com/2020/05/05/technology/parking-lots-wifi-coronavirus.html (accessed July 7, 2022).
- Kruse, C. S., N. Krowski, B. Rodriguez, L. Tran, J. Vela, and M. Brooks. 2017. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 7:e016242. https://doi.org/10.1136/bmjopen-2017-016242.
- Lagasse, J. 2020. COVID-19 telehealth waivers won’t last forever, but permanent regulatory changes are afoot. Healthcare Finance, May 14. Available at: https://www.healthcarefinancenews.com/news/covid-19-telehealth-waivers-wont-last-forever-permanent-regulatory-changes-are-afoot (accessed July 7, 2022).
- Lee, N. T., J. Karsten, and J. Roberts. 2020. Removing regulatory barriers to telehealth before and after COVID-19. The Brookings Institution, May 6. Available at: https://www.brookings.edu/research/removing-regulatory-barriers-to-telehealth-before-and-after-covid-19 (accessed July 7, 2022).
- Lilly, C. M., S. Cody, H. Zhao, K. Landry, S. P. Baker, J. McIlwaine, M. W. Chandler, R. S. Irwin, and the University of Massachusetts Memorial Critical Care Operations Group. 2011. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 305(21):2175–2183. https://doi.org/10.1001/jama.2011.697.
- Marchant, G. E., K. W. Abbott, and B. Allenby. 2014. Innovative governance models for emerging technologies. Edward Elgar Publishing. Available at: https://www.e-elgar.com/shop/usd/innovative-governance-models-for-emerging-technologies-9781782545637.html (accessed July 7, 2022).
- Mathews, D. J. H. 2017. When emerging biomedical technologies converge or collide. In Neuroethics: Anticipating the future. Oxford Scholarship. Available at: https://doi.org/10.1093/oso/9780198786832.003.0001.
- McGowan, J. J., C. M. Cusack, and M. Bloomrosen. 2012. The future of health IT innovation and informatics: A report from AMIA’s 2010 policy meeting. Journal of the American Medical Informatics Association 19(3):460–467. https://doi.org/10.1136/amiajnl-2011-000522.
- Mehrotra, A., K. Ray, D. M. Brockmeyer, M. L. Barnett, and J. A. Bender. 2020. Rapidly converting to “virtual practices”: Outpatient care in the era of COVID-19. NEJM Catalyst . https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0091.
- Montague, Z. 2020. A look at what’s in the stimulus package Trump signed. The New York Times, December 28. Available at: https://www.nytimes.com/2020/12/28/business/economy/second-stimulus-package.html (accessed July 7, 2022).
- National Academies of Sciences, Engineering, and Medicine (NASEM). 2019. Framework for addressing ethical dimensions of emerging and innovative biomedical technologies: A synthesis of relevant National Academies reports. Washington, DC: The National Academies Press. https://doi.org/10.17226/25491.
- National Institutes of Health (NIH). 2020. Accelerating COVID-19 therapeutic interventions and vaccines (ACTIV). Available at: https://www.nih.gov/research-training/medical-research-initiatives/activ (accessed July 7, 2022).
- National Rural Health Association (NRHA). n.d. About rural health care. Available at: https://www.ruralhealthweb.org/about-nrha/about-rural-health-care (accessed July 1, 2020).
- Nesbitt, T. S., and J. Katz-Bell. 2018. History of telehealth. In Understanding telehealth, edited by K. S. Rheuban and E. A. Krupinski. New York: McGraw-Hill Education. Available at: https://accessmedicine.mhmedical.com/content.aspx?bookid=2217§ionid=187794434.
- Nittari, G., R. Khuman, S. Baldoni, G. Pallotta, G. Battineni, A. Sirignano, F. Amenta, and G. Ricci. 2020. Telemedicine practice: Review of the current ethical and legal challenges. Telemedicine Journal and e-Health 26(12):1427-1437. https://doi.org/10.1089/tmj.2019.0158.
- Olla, P., and C. Shimskey. 2014. mHealth taxonomy: A literature survey of mobile health applications. Health Technology 4(4):299–308. https://doi.org/10.1007/s12553-014-0093-8.
- Orlando, J. F., M. Beard, and S. Kumar. 2019. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One 14(8):e0221848. https://doi.org/10.1371/journal.pone.0221848.
- Park, J., C. Erikson, X. Han, and P. Iyer. 2018. Are state telehealth policies associated with the use of telehealth services among underserved populations? Health Affairs 37(12):2060–2068. https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.05101.
- Psychology Interjurisdictional Compact (PSYPACT). n.d. About us. Available at: https://psypact.site-ym.com/general/custom.asp?page=About (accessed July 6, 2022).
- Price, W. N. 2015. Black-box medicine. Harvard Journal of Law and Technology 28(2). Available at: https://jolt.law.harvard.edu/articles/pdf/v28/28HarvJLTech419.pdf (accessed July 7, 2022).
- Puskin, D. S. 2001. Telemedicine: Follow the money modalities. Online Journal of Issues in Nursing 6(3):2. Available at: https://pubmed.ncbi.nlm.nih.gov/11936941 (accessed July 6, 2022).
- Richardson, L. D’A., G. L. Bertolini, and E. C. Naughton. 2022. COVID-19: State law telehealth update: State licensure requirements persist, permissible telehealth modalities generally expand, and insurance parity laws ensure reimbursement. K&L Gates. Available at: https://www.klgates.com/State-Law-Telehealth-Update-State-Licensure-Requirements-Persist-Permissible-Telehealth-Modalities-Generally-Expand-and-Insurance-Parity-Laws-Ensure-Reimbursement-2-21-2022 (accessed July 6, 2022).
- Ryu, S. 2010. History of telemedicine: Evolution, context, and transformation. Healthcare Informatics Research 16(1):65–66. https://doi.org/10.4258/hir.2010.16.1.65.
- SameSky Health. n.d. Who we are as people matters, especially when it comes to healthcare. Available at: https://www.sameskyhealth.com (accessed July 7, 2022).
- Seehusen, D. A., and A. Azrak. 2019. The effectiveness of outpatient telehealth consultations. American Family Physician 100(9):575–577. Available at: https://pubmed.ncbi.nlm.nih.gov/31674747 (accessed July 6, 2022).
- Siefer, A., and B. Callahan. 2020. Limiting broadband investment to “rural only” discriminates against Black Americans and other communities of color. Available at: https://www.digitalinclusion.org/digital-divide-and-systemic-racism (accessed July 6, 2022).
- Sim, I. 2019. Mobile devices and health. New England Journal of Medicine 381(10):956–968. https://doi.org/10.1056/NEJMra1806949.
- Singer, N. 2019. When apps get your medical data, your privacy may go with it. The New York Times, September 3. Available at: https://www.nytimes.com/2019/09/03/technology/smartphone-medical-records.html (accessed July 7, 2022).
- Singh, G. K., M. Girmay, M. Allender, and R. T. Christine. 2020. Digital divide: Marked disparities in computer and broadband internet use and associated health inequalities in the United States. International Journal of Translational Medical Research and Public Health 4(1):64–79. https://doi.org/10.21106/ijtmrph.148.
- Stevenson, J. R. 2017. Letter to Intuitive Surgical, Inc. January 19. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf16/K161178.pdf (accessed July 7, 2022).
- Teladoc Health. 2022. About us. Available at: https://teladochealth.com/about (accessed July 6, 2022).
- Torre-Diez, I., M. Lopez-Coronado, C. Vaca, J. S. Aguado, and C. de Castro. 2015. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: A systematic review. Telemedicine Journal and e-Health 21(2):81–85. https://doi.org/10.1089/tmj.2014.0053.
- Warren, E., P. Murray, and T. Smith. 2018. Letter to Scott Gottlieb and Jeffrey Shuren. U.S. Senate, October 10. Available at: https://www.warren.senate.gov/imo/media/doc/2018.10.10%20Letter%20to%20FDA%20on%20regulation%20of%20sofware%20as%20medical%20device.pdf (accessed July 7, 2022).
- Wittson, C. L., and R. A. Benschoter. 1972. Two-way television: Helping the medical center reach out. American Journal of Psychiatry 129(5):136–139. https://doi.org/10.1176/ajp.129.5.624.
- World Health Organization (WHO). 2010. Telemedicine: Opportunities and developments in member states: report on the second global survey on eHealth. Geneva, Switzerland: World Health Organization. Available at: https://apps.who.int/iris/handle/10665/44497.
- Yang, Y. T. 2016. Telehealth parity laws. Health Affairs. https://doi.org/10.1377/hpb20160815.244795.
- Zanaboni, P., U. Knarvik, and R. Wootton. 2014. Adoption of routine telemedicine in Norway: The current picture. Global Health Action 7:22801. https://doi.org/10.3402/gha.v7.22801.
https://doi.org/10.31478/202311e
Suggested Citation
Mathews, D., A. Abernethy, A. J. Butte, P. Ginsburg, B. Kocher, C. Novelli, L. Sandy, J. Smee, R. Fabi, A. C. Offodile II, J. S. Sherkow, R. D. Sullenger, E. Freiling, and C. Balatbat. 2023. Telehealth and Mobile Health: Case Study for Understanding and Anticipating Emerging Science and Technology. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/202311e .
Author Information
Debra Mathews, PhD, MA, is Associate Director for Research and Programs at the Johns Hopkins Berman Institute of Bioethics and Professor, Department of Genetic Medicine at the Johns Hopkins University School of Medicine. Amy Abernethy, MD, PhD, is President of Product Development and Chief Medical Officer at Verily. Atul J. Butte, MD, PhD, is Priscilla Chan and Mark Zuckerberg Distinguished Professor at the University of California, San Francisco. Paul Ginsburg, PhD, is Professor of the Practice of Health Policy and Management at the University of Southern California and Senior Fellow at the USC Schaeffer Center. Bob Kocher, MD, is Partner at Venrock. Catherine Novelli, JD, LLM, is President of Listening for America. Lewis Sandy, MD, is Principal and Co-founder, Sulu Coaching. John Smee, PhD, is Senior VP Engineering at Qualcomm Technologies, Inc. Rachel Fabi, PhD, is Associate Professor, Center for Bioethics and Humanities at SUNY Upstate Medical University. Anaeze C. Offodile II, MD, MPH, is Chief Strategy Officer at Memorial Sloan Kettering Cancer Center. Jacob S. Sherkow, JD, MA, is Professor of Law at the Illinois College of Law, Professor of Medicine at the Carle Illinois College of Medicine, Professor at the European Union Center, and Affiliate of the Carl R. Woese Institute for Genomic Biology at the University of Illinois. Rebecca D. Sullenger, BSPH, is a medical student at the Duke University School of Medicine. Emma Freiling, BA, is a Research Associate at the National Academy of Medicine. Celynne Balatbat, BA, was the Special Assistant to the NAM President at the National Academy of Medicine while this paper was authored.
Acknowledgments
This paper benefitted from the thoughtful input of Bernard Lo , University of California San Francisco; and George Demiris , University of Pennsylvania.
Conflict-of-Interest Disclosures
Amy Abernethy reports personal fees from Verily/Alphabet, relationships with Georgiamune and EQRx, and personal investments in Iterative Health and One Health, outside the submitted work. Atul J. Butte reports support for the present manuscript from National Institutes of Health; grants or contracts from Merck, Genentech, Peraton (as a prime for an NIH contract), Priscilla Chan and Mark Zuckerberg, the Bakar Family Foundation; royalties or licenses from NuMedii, Personalis, and Progenity; consulting fees from Samsung, Gerson Lehman Group, Dartmouth, Gladstone Institute, Boston Children’s Hospital, and the Mango Tree Corporation; payment of honoraria from Boston Children’s Hospital, Johns Hopkins University, Endocrine Society, Alliance for Academic Internal Medicine, Roche, Children’s Hospital of Philadelphia, University of Pittsburgh Medical Center, Cleveland Clinic, University of Utah, Society of Toxicology, Mayo Clinic, Pfizer, Cerner, Johnson and Johnson, and the Transplantation Society; payment for expert testimony from Foresight, support for attending meetings and/or travel from Alliance for Academic Internal Medicine, Cleveland Clinic, University of Utah, Society of Toxicology, Mayo Clinic, Children’s Hospital of Philadelphia, American Association of Clinical Chemistry, Analytical, and Life Science & Diagnostics Association; patents planned, issued, or pending from Personalis, NuMedii, Carmenta, Progenity, Stanford, and University of California, San Francisco; participation on a Data Safety Monitoring Board or Advisory Board from Washington University in Saint Louis, Regenstrief Institute, Geisinger, and University of Michigan; leadership or fiduciary role in other board, society, committee or advocacy group, from National Institutes of Health, National Academy of Medicine, and JAMA; and stock or stock options from Sophia Genetics, Allbirds, Coursera, Digital Ocean, Rivian, Invitae, Editas Medicine, Pacific Biosciences, Snowflake, Meta, Alphabet, 10x Genomics, Snap, Regeneron, Doximity, Netflix, Illumina, Royalty Pharma, Starbucks, Sutro Biopharma, Pfizer, Biontech, Advanced Micro Devices, Amazon, Microsoft, Moderna, Tesla, Apple, Personalis, and Lilly. Paul Ginsburg reports personal fees from the American Academy of Ophthalmology outside the submitted work. Bob Kocher reports being a Partner at the venture capital firm Venrock which invests in technology and healthcare businesses. Dr. Kocher is on the Boards of several healthcare services businesses that utilize telehealth technology including Lyra Health, Aledade, Devoted Health, Virta Health, Accompany Health, Sitka, Need, and Candid. Jacob S. Sherkow reports employment with the University of Illinois, grants from National Institutes of Health, personal fees from Expert Consulting services, outside the submitted work.
Correspondence
Questions or comments should be directed to Debra Mathews at [email protected].
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies. Copyright by the National Academy of Sciences. All rights reserved.
Join Our Community
Sign up for nam email updates.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
- Open access
- Published: 07 October 2022
Advances in e-learning in undergraduate clinical medicine: a systematic review
- T. Delungahawatta 1 ,
- S. S. Dunne 1 ,
- S. Hyde 1 ,
- L. Halpenny 1 ,
- D. McGrath 1 , 2 ,
- A. O’Regan 1 &
- C. P. Dunne 1 , 2
BMC Medical Education volume 22 , Article number: 711 ( 2022 ) Cite this article
4735 Accesses
10 Citations
3 Altmetric
Metrics details
E-learning is recognised as a useful educational tool and is becoming more common in undergraduate medical education. This review aims to examine the scope and impact of e-learning interventions on medical student learning in clinical medicine, in order to aid medical educators when implementing e-learning strategies in programme curricula.
A systematic review compliant with PRISMA guidelines that appraises study design, setting and population, context and type of evaluations. Specific search terms were used to locate articles across nine databases: MEDLINE/PubMed, ScienceDirect, EMBASE, Cochrane Library, ERIC, Academic Search Complete, CINAHL, Scopus and Google Scholar. Only studies evaluating e-learning interventions in undergraduate clinical medical education between January 1990 and August 2021 were selected. Of the 4,829 papers identified by the search, 42 studies met the inclusion criteria.
The 42 studies included varied in scope, cognitive domain, subject matter, design, quality and evaluation. The most popular approaches involved multimedia platforms (33%) and case-based approaches (26%), were interactive (83%), asynchronous (71%) and accessible from home (83%). Twelve studies (29%) evaluated usability, all of which reported positive feedback. Competence in use of technology, high motivation and an open attitude were key characteristics of successful students and preceptors.
Conclusions
Medical education is evolving consistently to accommodate rapid changes in therapies and procedures. In today’s technologically adept world, e-learning is an effective and convenient pedagogical approach for the teaching of undergraduate clinical medicine.
Peer Review reports
E-learning, a pedagogical approach supported by the principles of connectivism learning theory, involves the use of technology and electronic media in knowledge transfer [ 1 , 2 ]. Connectivism views knowledge as a fluid entity circulated through technology enabled networks that foster interactions between individuals, organizations, and societies at large [ 2 ]. Based on this conceptual framework, medical curricula can potentially benefit from enhanced communication and knowledge exchange using technology.
Common e-learning instructional designs in clinical medicine include “online and offline computer-based programmes, massive open online courses, virtual reality environments, virtual patients, mobile learning, digital game-based learning and psychomotor skills trainers”[ 1 ]. To maximize the potential for e-learning, it seems rational that the roles and needs of the e-learner, e-teacher and host institution should be defined and appreciated. According to the Association for Medical Education in Europe (AMEE), an e-learner is any individual taught in an online learning environment [ 1 ]. As the role of the e-learner is central to the learning process, effective e-learning strategies should consider potential learning challenges encountered by the e-learner. Employing skilled e-teachers and providing them with sufficient supports are also important considerations. Furthermore, institutional management of the content versus process elements of educational technology use should best align with the objectives of the program [ 1 ]. For example, if the intent is to provide student access to digital content, then managing sound or video files, podcasts, and online access to research papers, clinical protocols, or reference materials, should be prioritized. On the other hand, if the focus is on student participation in digital activities, then managing processes such as discussion boards and test-taking should take precedence. Accounting for the role of the e-learner, e-teacher, and host institution in this manner, can result in successful implementation of an e-learning system. In fact, e-learning has been shown to be at least as effective as, and can serve as an adjunct to, face-to-face teaching and learning methods [ 3 , 4 , 5 ].
An institution may choose to employ educational technologies for the entirety of the course or provide a combination of online and in-class interactions, with the latter approach referred to as ‘blended learning’ [ 1 ]. Incorporation of e-learning into the curriculum allows for new avenues of interactive knowledge and skill transfer between teachers and students and amongst students. Interactions are not limited to face-to-face conversations but can involve text, audio, images, or video, thereby enriching the learning experience. Giving access to a greater breadth of learning resources further develops lifelong learning skills in students as they are required to independently evaluate and extract the pertinent information [ 1 ]. E-learning interventions can also be accessed at any time from almost any location, which facilitates a student-centred approach through self-directed and flexible learning [ 6 ]. As such, e-learning is an attractive instructional undergraduate health education approach [ 7 ].
To date, e-learning interventions in the sciences, particularly anatomy [ 8 ] and physiology [ 9 ], and postgraduate medical training [ 3 , 4 ] have been described. However, their use has not been reviewed systematically in the specific context of augmenting, enhancing or supporting student learning in undergraduate clinical medicine [ 10 ], or replacing face-to-face learning with online learning in the case of COVID-19 emergency remote teaching. In 2014, survey responses from senior medical students in Illinois, reported use of online collaborative authoring, multimedia, social-networking, and communication tools as point of opportunity study resources during clinical rotations [ 11 ]. Additionally, the COVID-19 pandemic has necessitated stepping away from traditional classroom and bedside teaching, and development of more flexible course delivery. A recent survey by Barton et al. collected 1,626 responses from medical students across 41 medical schools in the United Kingdom during the COVID lockdown. Results of study resources accessed daily showed that 41.6% of students used information provided by university (PowerPoint lecture slides, personal notes), 29.6% accessed free websites and question banks, and 18.4% accessed paid websites and question banks [ 12 ]. The work therefore suggests a strong tendency for students to supplement university materials with online resources [ 12 , 13 ]. The popularity of online learning platforms seems to stem from an association with achieving higher exam scores [ 14 , 15 ], ability to self-monitor knowledge gaps [ 16 ], improved knowledge retention from repeat exposure [ 17 , 18 ], and to practice exam technique [ 16 ].
Medical school educators are, therefore, called to evaluate e-learning approaches and to consider incorporation of suitable strategies into current curricula to ensure equitable access and student success. Thus, we aimed to systematically review the scope and impact of e-learning interventions published regarding undergraduate clinical medicine, and to inform medical educators of the effectiveness and character of various online learning environments.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines are used for the reporting of this systematic review [ 19 ]. The PRISMA checklist is included as Additional File 1 .
Search methods
The early 1990s marked the commercial availability of computer-based learning multimedia [ 20 ] as well as the emergence of online education programs [ 21 ]. Thus, medical subject headings (MeSH), key words and specific database headings were used to locate articles published between January 1990 and August 2021: ‘e-learning’ or ‘digital resources’ or ‘internet learning resources’ AND ‘medical education’ AND ‘undergraduate’ AND ‘techniques’ or ‘programmes’ or ‘interventions’. The search was piloted on PubMed and adapted subsequently for the databases. A total of nine databases were searched: MEDLINE/PubMed, ScienceDirect, EMBASE, Cochrane Library, ERIC, Academic Search Complete, CINAHL, Scopus, Google Scholar and grey literature. The bibliographies of each selected paper were searched manually for further studies. Websites of medical education organisations were searched for position statements and guidelines, including the Association for the Study of Medical Education, AMEE and the British Medical Journal.
Inclusion and exclusion criteria
Only studies in the English language that evaluated an e-learning intervention in subjects related to clinical medicine were selected. These included: family medicine, surgery, internal medicine, radiology, psychiatry, dermatology, paediatrics and obstetrics. Studies that did not involve undergraduate medical students, were based on pre-clinical sciences or were not focussed on an e-learning intervention were excluded. Studies that focussed on the use of internet for assessment and course administration only were not included. Additionally, studies that described interventions but not their evaluation were excluded. Of the 4,829 papers identified by the search, 42 studies were deemed eligible for inclusion in this review.
Data extraction and analysis
AMEE guidelines on e-learning interventions [ 1 ] were used to modify a previous data extraction tool that had been used in a systematic evaluation of effectiveness of medical education interventions [ 22 ]. This was subsequently piloted and refined by three of the authors until consensus was achieved to form the data extraction tool (see Additional File 2 ). With application of connectivism, individual elements of e-learning were identified to infer and appreciate their collective effects on the learning process. More specifically, data was extracted by examining two central questions: how and when to use e-learning in undergraduate clinical medical education. The primary outcomes relating to how to use e-learning were: instructional features that made the e-learning intervention effective; usability features; assessment of effectiveness and quality of the intervention. Primary outcomes relating to when were: the context, and the learner and preceptor characteristics. In addition to the outcomes measured, descriptive data was also extracted to summarise the studies including: the study design, setting and population; context and discipline; type of evaluations. All selected papers were filed in an Endnote library and the data extraction tool for each was stored in an Excel file, a summary of which is provided as Additional File 2 and Additional File 3 .
Guidelines for evaluating papers on medical education interventions from the Education Group for Guidelines on Evaluation were used as a framework to assign a global score for the strength of each paper [ 23 ]. Among these guidelines, significant value is placed on development of strong intervention rationale and intervention evaluation methods [ 23 ]. The impact of the evaluation was also measured using Kirkpatrick’s levels, a recognised system of understanding the effect of interventions [ 24 ]. The first level, reaction, is a measure of learner satisfaction with the intervention [ 24 ]. The second Kirkpatrick level, learning, is a measure of change in knowledge, skills, or experience. The third Kirkpatrick level of behaviour is a measure of behavioural change. The final level, results, is a measure of overall impact on the organization (i.e., improved quality of work, reduction in time wasted, better patient care).
Search results
A total of 4,829 papers were retrieved from database and manual searches, and this number was reduced to 42 after removal of duplicates and application of inclusion/exclusion criteria at set stages (see Fig. 1 for the PRISMA flow diagram). Two papers were retrieved from manual searches of bibliographies [ 25 , 26 ]. The main reasons for excluding studies were a lack of focus on undergraduate medical students (112 studies) or absence of an e-learning intervention (34 studies).
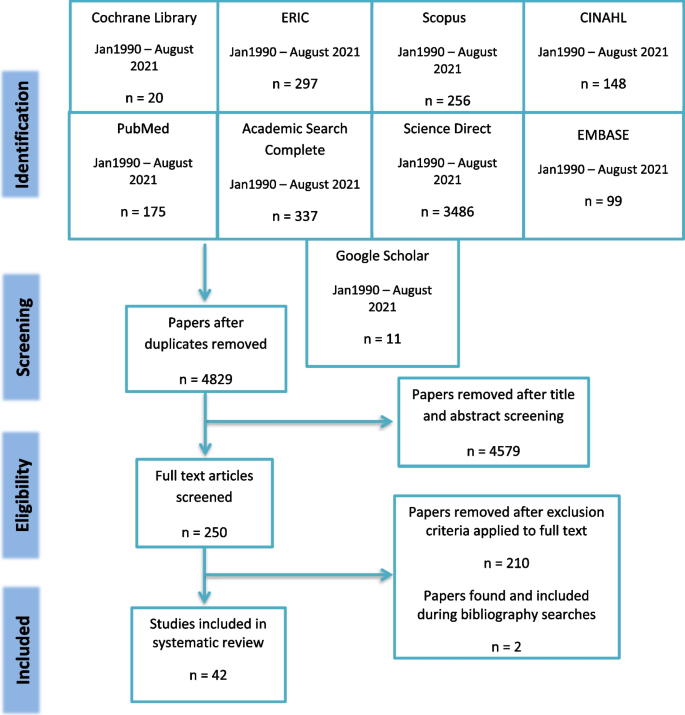
PRISMA flow diagram
Design of included studies
The year of publication ranged from 2003 to 2021, with most conducted within the past ten years (31 studies). Interventions were conducted in nine different countries, mainly the United States (13 studies) and Germany (9 studies). More than half of the studies were conducted in the European Union (21 studies). Several research designs were described, including 17 observational studies [ 25 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], 13 randomised control trials [ 26 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ], three non-randomised control trials [ 55 , 56 , 57 ], eight qualitative studies [ 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 ], and one mixed methods study [ 66 ]. Thirteen of the total studies included data collection both pre- and post- intervention [ 25 , 27 , 31 , 34 , 36 , 38 , 39 , 45 , 48 , 52 , 53 , 54 , 61 ]. Six studies had follow-up data (collected weeks to months after intervention) [ 34 , 45 , 49 , 52 , 54 , 56 ] and twelve papers reported ethical approval [ 28 , 29 , 30 , 31 , 33 , 34 , 39 , 40 , 42 , 46 , 49 , 54 ]. Furthermore, eight studies described learning theories in the development or evaluation of medical curricula [ 29 , 30 , 33 , 49 , 51 , 52 , 56 , 58 ]. Of these studies, five referenced constructivism [ 29 , 49 , 51 , 52 , 58 ] three studies highlighted cognitivism [ 30 , 56 , 59 ], and one study evaluated behaviourist learning theory [ 33 ].
Study population
Students in the third year of medical school experiencing clinical exposure were the most commonly studied (sixteen studies), with fourteen studies involving multiple cohorts of students (see Additional File 3 ). Sample sizes ranged from 10 to 42,190 individuals. The most common disciplines investigated were interdisciplinary (13 studies), surgery (8 studies), radiology (7 studies), and dermatology (4 studies) (see Fig. 2 Intervention Discipline).
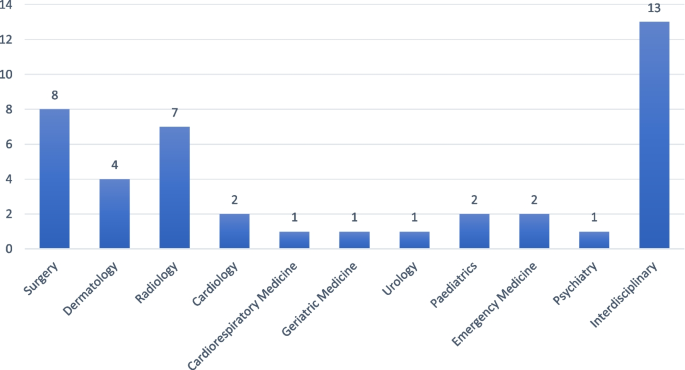
Intervention discipline
Intervention characteristics
Twelve types of intervention were described and the most commonly used were multimedia platforms (fourteen studies) and case-based learning (eleven studies), as per Additional File 2 and Fig. 3 . In terms of cognitive domain, 27 interventions were in the domain of knowledge [ 25 , 26 , 27 , 29 , 30 , 32 , 33 , 34 , 35 , 39 , 40 , 42 , 43 , 47 , 48 , 50 , 52 , 53 , 54 , 57 , 60 , 61 , 62 , 63 , 64 , 66 , 67 ]; eight were in the domain of skills [ 9 , 30 , 31 , 36 , 37 , 46 , 49 , 51 ] and seven in combined knowledge and skills [ 38 , 41 , 44 , 45 , 56 , 59 , 65 ]. The interventions ranged in duration from a single session to a complete academic year. Thirteen of the interventions were synchronous, where users log on at a given time [ 8 , 26 , 27 , 31 , 33 , 34 , 37 , 43 , 47 , 51 , 52 , 58 , 66 ], and the remaining 29 used an asynchronous platform (users logging on independently in their own time). Seven were accessible in a classroom setting only [ 26 , 27 , 36 , 47 , 52 , 58 , 66 ] while the others could be accessed from home (Fig. 4 ).
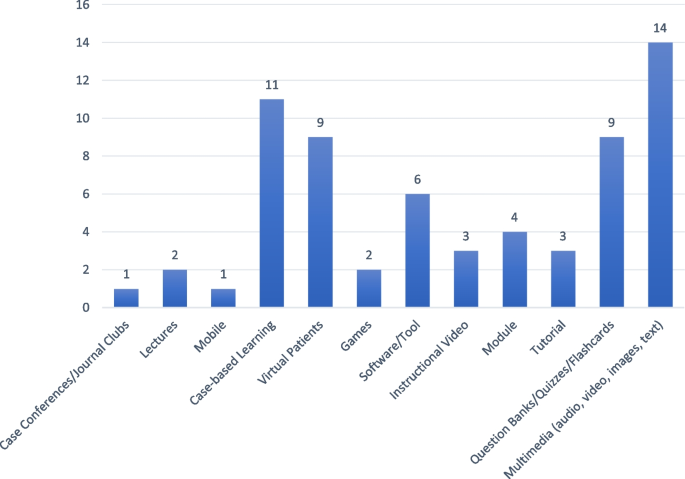
Intervention type
Reported roles for e-learning within the curriculum included a revision aid for examinations [ 58 ]; the flipped classroom concept [ 44 , 57 ], whereby lectures held after an e-lecture become an interactive session; to facilitate an online community where knowledge could be discussed/ shared [ 25 ]; and, enabling just-in-time learning through timely access to facts [ 30 , 31 , 37 ]. Seven (17%) of the 42 interventions were didactic in approach [ 27 , 30 , 37 , 55 , 57 , 63 , 65 ], while the others were interactive. Twelve studies described a collaborative approach, whereby students discussed cases and problems with one another and engaged in role-plays [ 25 , 26 , 36 , 38 , 40 , 41 , 42 , 46 , 52 , 59 , 61 , 66 ]. The context of e-learning in relation to the curriculum was not stated in ten of the studies but another thirteen studies used the terms “adjunct”, “complement”, “supplement”,”hybrid” and “blended” to illustrate the common theme of integrating e-learning with traditional learning [ 25 , 29 , 30 , 32 , 44 , 45 , 46 , 47 , 50 , 56 , 57 , 58 , 62 , 63 ]. Seven studies describe temporary replacement of traditional curricula with e-learning platforms in response to COVID-19 [ 33 , 40 , 41 , 42 , 61 , 62 , 64 ]. Eight studies described a pilot phase or the inclusion of students in the development of the intervention [ 33 , 37 , 44 , 45 , 48 , 49 , 53 , 66 ]. Nineteen of the interventions had a built-in assessment, with multiple choice questions being used in most cases, to evaluate whether an improvement in learning had taken place [ 25 , 27 , 31 , 34 , 37 , 39 , 43 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 55 , 59 , 66 ]. Justification for the chosen assessment strategy or a statement on its suitability was included in two studies [ 50 , 66 ]. Kourdioukova et al. reported an improvement in knowledge and skills with computer supported collaborative case-based approach as judged by in-built multiple-choice questions (MCQ), suggesting the importance of content-specific scripting [ 66 ]. Schneider et al. used a combination of MCQ and survey, and justified their use by demonstrating that learning improved with the intervention compared to the control [ 50 ]. Five of the interventions used end of module assessments as the marker of quality [ 26 , 29 , 53 , 56 , 57 ], with one stating that this was not a suitable mechanism due to its inability to assess the students’ ability to take a patient history or perform a clinical examination [ 53 ].
Intervention evaluation
Each study was given a global rating from 1–5 based on guideline criteria from the Education Group for Guidelines on Evaluation, including whether learning outcomes and curricular context were outlined and the power and rigor of the studies [ 23 ] (Additional File 2 ). Accordingly, eleven studies scored 4/5; two scored 3.5/5; twelve studies scored 3/5; twelve studies scored 2.5/5; and five scored 2/5 (σ = 0.138).
Intervention effectiveness and acceptability
Nine studies described an impact matching a Kirkpatrick level 1, where the student reaction to e-learning intervention was evaluated using student surveys or questionnaires [ 32 , 35 , 44 , 58 , 60 , 61 , 62 , 64 , 65 ]. All these studies report that most students were satisfied with the addition of an e-learning intervention. For instance, Orton et al. note that over 91% of survey responses either ‘strongly agreed’ or ‘agreed’ that use of computer-based virtual patients enabled learning [ 35 ].
Twenty-one (50%) of the 42 studies evaluated acceptability [ 26 , 30 , 32 , 33 , 36 , 37 , 40 , 41 , 42 , 44 , 48 , 53 , 54 , 55 , 56 , 57 , 58 , 63 , 65 , 66 , 68 ]. Of these, 17 reported that the intervention was acceptable. A neutral attitude was reported to a radiology e-learning intervention that involved peer collaboration and was found to be time consuming[ 66 ]. Attitude in another study was much more favourable in junior years than in senior years, with the authors commenting on the conflict between completing assignments and preparing for high stakes examinations [ 55 ]. Another study that focussed on acceptability, with positive outcomes, found that perceived utility and ease of use were the key factors [ 30 ]. Twelve (57%) of the 21 studies further evaluated usability [ 30 , 36 , 37 , 40 , 41 , 42 , 44 , 53 , 56 , 57 , 58 , 65 ], all with positive outcomes, but only one used a formal usability assessment tool [ 58 ]. In that study, Farrimond et al. found that a usable intervention should be: simple and intuitive to use and, from a learner perspective, interactive and enjoyable [ 58 ]. In the development of virtual lectures, ease of navigation, audio-visual quality and accessibility were the key usability features [ 57 ]. Wahlgren et al. concluded that as well as navigation, interactivity is a priority for e-learning development [ 53 ]. Regarding mobile learning, the display should be adaptable to varying screen sizes, termed ‘chunking’, and it should be suitable for a number of platforms [ 30 ].
Twenty-nine (69%) of the 42 studies described an impact matching a Kirkpatrick level 2, where evaluation of whether learning took place was assessed through post intervention scores [ 25 , 27 , 31 , 36 , 38 , 39 , 47 , 48 , 50 , 52 , 53 , 54 , 56 , 57 , 61 ], final exam results [ 26 , 29 , 45 , 66 ], direct observation [ 28 , 31 , 33 , 43 , 46 , 51 , 55 ] and student survey [ 25 , 26 , 30 , 37 , 38 , 39 , 40 , 41 , 42 , 45 , 48 , 49 , 53 , 54 , 56 , 65 , 66 ]. Among these studies, two studies had included both pre- and post- intervention evaluations but neither had a control group nor longer term follow-up [ 25 , 27 ]. One randomised control trial showed a statistically significant improvement in factual knowledge acquisition after participation in an online module as judged based on performance in end of year assessments, compared to a traditional teaching control group (84.8% ± 1.3 vs. 79.5% ± 1.4, p = 0.006, effect size 0.67) [ 26 ]. Likewise, Davis et al., found that the use of a procedural animation video on mobile device resulted in higher medical student scores on skills checklist (9.33 ± 2.65 vs. 4.52 ± 3.64, p < 0.001, effect size 1.5) [ 30 ]. Similarly, in Sijstermans et al., mean students’ self-evaluation of their skills using five-point Likert scale questionnaire, before and after two patient stimulations showed improvement (3.91 ± 0.28 vs 3.56 ± 0.34, P < 0.0001, effect size 1.12). Furthermore, in one study employing a problem-based e-learning approach, the number of first-class honours awarded were found to be significantly improved when compared to control group [ 29 ]. However, in another study using a problem-based e-learning intervention, no significant difference was found between control and intervention groups in subsequent examinations ( p = 0.11) [ 53 ]. In contrast, Al Zahrani et al. found that delivery of new e-learning platforms (Blackboard Collaborate, ZOOM) in response to COVID-19 was poorly accepted by students, whereby 59.2% did not feel adequately educated on learning outcomes, 30% felt no educational difference between e-learning and traditional curriculums, and 56.1% felt e-learning is insufficient as an educational tool for the health sciences [ 40 ].
Four studies demonstrated a change in student behaviour in line with Kirkpatrick level 3 [ 50 , 52 , 59 , 63 ]. In de Villiers et al., it was found that students were using podcasts to learn course content and the classroom teaching setting to strengthen their understanding, inadvertently accepting the flipped classroom approach [ 63 ]. In Sward et al., students who were assigned to a gaming intervention were more willing to engage in answer creating and answer generating as well as independent study of subject materials prior to session time [ 52 ]. Similarly, in Schneider et al., students in the computer case-based intervention group were found to invest more time into studying course subjects (38.5 min vs 15.9 min) which resulted in significantly higher test scores [ 50 ]. Finally, in Moriates et al., following the integration of value-based modules, students have reported increased awareness of patient needs and discussions with peers regarding value-based decision-making during clerkship [ 59 ].
Learner and preceptor characteristics
Learner characteristics identified to enable successful e-learning include: good digital skills, less resistance to change [ 32 ] and a willingness to collaborate with peers [ 66 ]. Preceptor characteristics were not described in most of the studies, but the role involved guiding students through their learning [ 33 , 46 , 61 , 66 ], selection of topics of broad interest to students [ 60 ], technical support [ 54 ], student evaluation[ 28 , 31 , 37 , 40 , 42 , 45 , 46 , 49 , 51 ], content development and management [ 32 , 41 , 42 , 46 , 54 , 62 ] and providing feedback and clear instruction on what is expected of the learners [ 28 , 37 , 40 , 42 , 51 , 54 , 60 ].
The COVID-19 pandemic resulted in global university closures during periods of lockdown, necessitating educators to quickly adopt alternate pedagogical approaches. As a result, there has been a substantial increase in the use of e-learning, by which teaching and learning activities occur at a distance on online platforms [ 69 ].
In enabling a shift in the control of knowledge acquisition and distribution from the teacher to the student, e-learning facilitates the learning process. Learners filter the available information, develop new perspectives, log into networks to share their understanding, and repeat the cycle [ 2 ]. This view of learning as a fluid and dynamic process is the basis of the learning theory of connectivism and highlights the benefit of this instructional design in medical education – a field amenable to rapid changes in therapies and procedures. In fact, educational theorists have significantly influenced the development of medical curricula throughout history. Amongst the 25 higher impact studies (achieving a global score greater or equal to 3), only 7 studies (28%) were found to have described theoretical underpinnings [ 30 , 33 , 49 , 51 , 52 , 58 , 59 ]. Initially, the behaviourist perspective supported pedological practices [ 70 ]. Behaviourism described learning as largely deriving from responses to external stimuli and led to curricula aimed to influence behaviour through reward and positive and negative reinforcement. In one study reviewed, the lack of direct observation of non-verbal communication by instructors was seen as a significant learning challenge in the virtual environment [ 33 ]. A shift from behaviourism to cognitivism later ensued with the belief that the brain is much more than a ‘black box’ and learning rather involved mental processing and organization of knowledge, and memory functions [ 70 ]. With the recognition of individual differences in the learning process, online systems attempted to introduce interventions that suited multiple learning strategies. For example, learning from auditory narration with animation was found to be more effective than use of text with animation [ 71 ]. This review further highlighted the impact of repetition [ 30 ] and clinical reasoning [ 56 , 59 ] on the learning process. More recently, constructivist learning theory and the perception that learners incorporate new information into pre-existing knowledge schemas has greatly contributed to reformation of medical education [ 70 ]. Incorporating real world connections [ 29 , 49 , 58 ], building on motivations [ 52 ], application of feedback [ 51 ] and continuous reflection [ 49 ] has been noted in this review as important factors in knowledge handling and retention. Presently, e-learning interventions often utilize aspects of more than one theoretical perspective. For instance, problem-based learning interventions have emphasised the critical thinking processes of cognitivism and the self-direction of constructivism [ 29 ]. While primary studies have increased the reporting of underlying theory over time, there is still a significant lack of discussion – future work should reference theoretical principles to objectively frame and assess online education.
In addition to recognizing the needs of the e-learner, identifying required skills of e-teachers and developing content that appropriately supplement the curriculum are vital to ensuring successful implementation of an e-learning system [ 1 ]. Therefore, this study involved review of studies published between 1990 and 2021, assessing the effectiveness and character of various online learning environments in undergraduate clinical medical education. Specifically, these studies involved medical students pursuing medicine as a primary degree and those enrolled with prior degrees.
Intervention design
Critical appraisal of the collected studies using EGGE criteria, identified seventeen studies (40%) meeting a global rating of less than 3. The EGGE criteria encompass a standardized framework by which quality indicators can be recognized. Lower ratings of included studies suggests that conducting and reporting of e-learning interventions is largely lacking in methodological rigour and therefore limits transferability of study results. This finding is consistent with conclusions from a review by Kim et al., describing how most of the existing literature on e-learning interventions have little quantitative data, evaluate a limited range of outcomes and have significant gaps in study designs [ 72 ]. Additionally, only 13 (31%) randomized control trials (RCTs) were included in the review [ 26 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ]. Amongst these studies, five reported pre and post test scores [ 45 , 48 , 52 , 53 , 54 ], three of which report long term follow up [ 45 , 52 , 54 ]. Interestingly, all the RCTs report no significant differences in knowledge mastery between control and intervention groups. However, in the immediate short term, e-learning interventions were associated with greater learner satisfaction. For example, in Lee et al., mobile learning with interactive multimedia had higher satisfaction scores compared with conventional Microsoft PowerPoint Show content, despite non-significant differences in knowledge gain [ 48 ]. Similarly, in the study by Wahlgren et al., the majority of students in the intervention group reported that the interactive computerised cases enabled better understanding of disease diagnosis and management, particularly referencing the user-friendliness and feedback [ 53 ]. Yet, knowledge gain as assessed by post-intervention examination scores did not show statistically significant differences between the two groups. Systematic reviews examining the effect of e-learning on nursing education have also demonstrated no differences between e-learning and traditional teaching modalities but report high satisfaction rates with the former [ 73 , 74 ]. While these studies suggest that e-learning is as effective as traditional educational methods, higher student satisfaction levels are indicative of more effective learning programs [ 75 ]. Therefore, the lack of longitudinal data may limit our ability to accurately evaluate the impact of e-learning technologies.
Many of the studies in this review used virtual patient and case-based pedagogical methods reflecting an educational trend towards more critical thinking [ 76 ]. Thirty-five of the interventions under review used an interactive approach, encouraging a style in which students collaborated and discussed ideas with their peers and tutors, the importance of which has been recognised [ 77 ]. Two studies of mobile learning identified wasted time for students as a concern that could be addressed by allowing immediate access to information that would soon be required [ 30 , 55 ]. This ‘just in time learning’, defined as a “brief educational experience targeting a specific need or clinical question” [ 78 ], can be facilitated through e-learning. Ten of the included studies concluded that an integrated approach works best, whereby educators do not seek to replace traditional methods but rather supplement them. This has previously been described as a ‘blended-learning’ style [ 77 ]. A recent study suggests that students thrive in blended- versus self-directed virtual reality environments due to face-to-face teacher support [ 79 ].
Despite variability in methodological design, several studies of e-learning across domains of education, politics, business, and military training have shown knowledge gains assessed by pre- versus post-intervention tests [ 80 ]. Similarly, subjects within the studies we have reviewed have reported e-learning interventions to be conducive to learning [ 32 , 35 , 36 , 44 , 58 , 60 , 61 , 62 , 64 , 65 ], have demonstrated improvements in learning [ 25 , 26 , 27 , 29 , 30 , 31 , 34 , 36 , 37 , 38 , 39 , 43 , 46 , 48 , 49 , 54 , 55 , 56 , 57 , 66 ] and modified learning strategies [ 50 , 52 , 63 ]. The specific features of e-learning strategies most likely to enhance the learning experience may include: peer-to-peer learning [ 52 ], making use of wasted time [ 30 , 40 , 41 , 42 , 81 ], feedback from clinicians and ongoing technical support [ 32 , 82 ], consolidation of information and skill through repetition [ 52 , 82 , 83 ], and convenience of online content access [ 25 , 30 , 40 , 41 , 42 ]. Usability of the intervention has specifically featured strongly in this review. Vital features of e-learning interventions facilitating its use may include: interactive software, active learning promotion (built-in quizzes following cases), asynchronous use, multimedia platforms (i.e., slideshows, videos, images), ease of use and adaptability [ 76 , 81 , 84 ]. Unsurprisingly, students are more engaged with educational material after the typical 9-to-5 work hours [ 25 , 35 ]. Whereas traditional learning opportunities may be restricted to these hours, the flexibility of being able to access online resources outside of this timeframe, may better facilitate achievement of learning objectives [ 25 , 35 ]. Additionally, the use of discussion boards [ 78 ] and games [ 77 ] may facilitate active learning and feedback to be sought and received in a timely manner. Furthermore, quality assurance is recognized as a critical factor, and if considered at the planning stage of an intervention and built into e-learning interventions, may lead to more favourable outcomes [ 23 ]. Engagement with students in this manner is in keeping with the AMEE recommended goals of e-learning [ 1 ]. Several studies also highlight how online learning might provide an encouraging environment for the development of knowledge and skills, relatively easily tailored to individual learning preferences and prior knowledge, and with the possibility of compensating for a lack of accessibility of patients or teachers [ 35 , 36 , 38 , 63 , 85 ]. Furthermore, the ability to access an extensive network of additional resources may allow students to take control of their learning and regulate the volume of information studied [ 36 ].
While our review found improved learning outcomes, other systematic reviews assessing the effectiveness of technology and electronic media in health education, report equivocal findings [ 77 , 86 ]. Proposed factors that may limit learning capacity include: hesitancy to adopt changes by students and teachers, poor technical or financial support, limited technological skills, and the lack of direct and personalized teacher communication [ 25 , 32 , 82 , 87 ]. For example, Davies et al. suggests that an open outlook on mobile device usage was required by students and clinicians, to limit non-use and acquire potential benefits [ 30 ]. In another study conducted by Alsoufi et al., online medical education programs implemented in Libya in response to COVID-19 were found to be negatively received by respondents [ 87 ]. Financial and technical barriers and the lack of hands-on bedside teaching were stated by respondents as limitations to acceptance of e-learning. The shift to online medical learning in the Philippines during the COVID-19 pandemic also identified lack of access to computers and the internet as a significant barrier [ 82 ]. Of course, with these later interventions, the rapid onset of the pandemic required development of e-learning platforms with relatively little training and preparation. As such, the logistics of e-learning curricula as it pertains to specific communities may not have been foreseen. Another reason for such discrepancies may be the underlying discipline in which the intervention is being evaluated [ 47 ]. For instance, the use of only e-learning materials when teaching new skills may not be sufficient, as the direct observation and guidance of an expert is valuable [ 88 ]. A blended-learning environment may be more appropriate in these circumstances [ 47 ]. Indeed, viewing e-learning as a complement rather than replacement of traditional approaches is already well accepted amongst students [ 80 ].
Learner, preceptor and institution characteristics
The twenty-first century learners are known to be avid consumers of various digital platforms. However, studies have shown an incongruence between their ability to use technology for entertainment and ability to use it for educational purposes [ 89 ]. Most students require guidance to synthesize information and create new understanding. In fact, students in middle school through undergraduate level studies have consistently demonstrated poor digital research skills [ 90 , 91 ]. Furthermore, students may require adjustment of learning practices to best engage with the presented e-learning platform. For example, use of PowerPoint presentations or handouts in replacement of in-class teaching can cause visual and auditory learners to require more time to comprehend the information [ 82 ]. Therefore, in addition to carrying an acceptant attitude and a willingness to collaborate with peers, the ability to engage with and extract relevant content from online resources, is a characteristic linked to success in e-learning [ 32 , 66 ].
Nevertheless, recognition of the need for continued mentoring and support in the online learning environment, requires appreciation of the role of the e-teacher. Preceptors’ roles involve development and delivery of the intervention and acting as a resource person for the duration of the module [ 68 ]. In our previous discussion of e-learning strategy effectiveness, two further roles of the e-teacher can be recognized. Firstly, the e-teacher is instrumental in providing timely feedback, one of the main features associated with improved e-learning outcomes [ 32 ]. E-teachers should actively monitor student activity and provide feedback or support where needed [ 92 ]. Secondly, success of e-learning is also strongly related to the motivation of the students and indirectly the motivation demonstrated by the e-teacher [ 30 , 92 ]. The ARCS motivational model highlights four components needed to create a highly motivational e-learning system: maintain student attention, content relevance, student confidence, student satisfaction [ 93 ]. If e-teachers can convey subject material through strategies which encompass use of interactive multimedia, humour, and inquiry for instance, they can satisfy the first component of attention [ 92 ]. Generating activities that best illustrate main ideas, tailoring to the learner knowledge level and providing positive feedback are examples of methods to instil content relevance, student confidence and student satisfaction, accordingly. In Gradl-Dietsch et al., combination of video-based learning, team-based learning and peer-teaching, along with practical skills teaching in point of care ultrasound, feedback from peer teachers, and positive instructor-learner interactions, collectively fulfil the components of the ARCS model [ 54 ]. In Sox et al., the use of a web-based module to teach oral case presentation skills satisfied student attention and content relevance [ 51 ]. However, poor adherence to module largely due to time constraints, can be suggestive of poor student satisfaction. As a result, student confidence and the quality of oral case presentations did not differ from controls (faculty-led feedback sessions). As suggested by the authors, a combination of web module with direct faculty feedback may better instil student confidence and satisfaction with module content, and thereby improve student performance [ 51 ]. Recent studies have shown that the digital literacy skills of most instructors are inadequate [ 90 , 91 ]. Therefore, institutions need to invest into the provision of training programs and supports to allow e-teachers to develop and strengthen competencies needed to sufficiently handle educational technologies [ 92 , 94 , 95 ]. For example, the use of offline tablet-based materials was shown to improve medical education in Zambia, but reported usage amongst healthcare workers was low [ 95 ]. Authors suggest that a lack of training in tablet use was the underlying reason. Taken together, while the role of the teacher has changed compared to traditional pedological approaches, their actions can still heavily influence student learning outcomes.
Limitations and future directions
In a field where technology is changing faster than studies can be completed and interventions are evolving rapidly, medical education research has become a challenging topic of debate. Research can “provide the evidence to prove—and improve—the quality and effectiveness of teaching” and therefore advise the restructuring of curricula to respond to advances in science and technology [ 96 ]. In this review, 29 studies received a global score of 3 or less out of 5, highlighting a lack of transparency and rigour in most of the studies. This justifies a need for a standardised approach for reporting medical education interventions. Pre- and post-intervention testing is informative, but follow-up months later would be an important measure of knowledge retention and therefore intervention effectiveness. Moreover, most of the studies in this review examined knowledge or skill development but few examined higher Kirkpatrick levels. The inclination towards focus on the lower levels of the Kirkpatrick model may stem from difficulty following students in the field to evaluate long-term results of the educational intervention on student behaviours (level three) and the organization at large (level four) [ 97 ]. Future work on the evaluation of associated changes in behaviour, professional practice or patient outcomes would be valuable. Other e-learning characteristics that can be evaluated in future work (Fig. 4 ) may include the capacity for adaptivity (to accommodate changing student needs and performance) and collaboration [ 98 ]. Including descriptions of curricula context can also facilitate the exploration of which e-learning strategies are best suited for specific medicine disciplines and socioeconomic settings. The use of internet resources by both students and patients alike, and the exponential growth in social media influence may also provide a platform for future e-learning interventions [ 99 ].
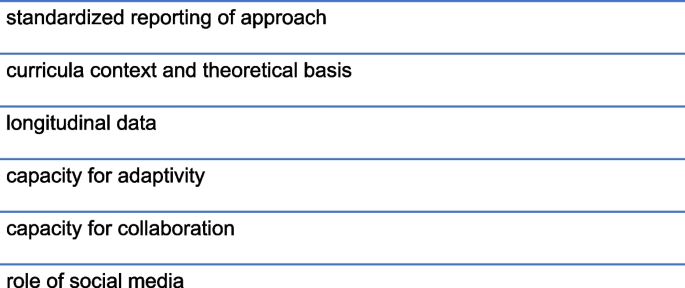
Future intervention design recommendations
Over the past twenty years and with the recent advent of the COVID-19 pandemic, there has been a substantial increase in the use of e-learning. This review found that e-learning interventions are positively perceived by students and associated with improvements in learning. Improved learning outcomes are closely correlated with interactive, asynchronous, easily accessible and usable interventions, and those involving students and preceptors with digital skills, high motivation and receptive attitudes. While further exploration of the strengths and weaknesses of e-learning technologies is warranted, use of online platforms is a creditable educational tool for undergraduate clinical medicine.
Abbreviations
Association for Medical Education in Europe
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Ellaway R, Masters K. AMEE Guide 32: e-Learning In Medical Education - Part 1: Learning. Teaching And Assessment Med Teach. 2008;30(5):455–73.
Google Scholar
Goldie JG. Connectivism: A Knowledge Learning Theory For The Digital Age? Med Teach. 2016;38(10):1064–9.
Article Google Scholar
Maertens H, Madani A, Landry T, Vermassen F, Van Herzeele I, Aggarwal R. Systematic Review Of E-Learning For Surgical Training. Br J Surg. 2016;103(11):1428–37.
Tarpada SP, Morris MT, Burton DA. E-Learning In Orthopedic Surgery Training: A Systematic Review. J Orthop. 2016;13(4):425–30.
Feng J-Y, Chang Y-T, Chang H-Y, Erdley WS, Lin C-H, Chang Y-J. Systematic Review of Effectiveness of Situated E-Learning on Medical and Nursing Education. Worldviews Evid Based Nurs. 2013;10(3):174–83.
Price Kerfoot B, Masser BA, Hafler JP. Influence Of New Educational Technology On Problem-Based Learning At Harvard Medical School. Med Educ. 2005;39(4):380–7.
Guarino S, Leopardi E, Sorrenti S, De Antoni E, Catania A, Alagaratnam S. Internet-Based Versus Traditional Teaching And Learning Methods. Clin Teach. 2014;11(6):449–53.
Trelease RB. From Chalkboard, Slides, And Paper To E-Learning: How Computing Technologies Have Transformed Anatomical Sciences Education. Anat Sci Educ. 2016;9(6):583–602.
Felder E, Fauler M, Geiler S. Introducing E-Learning/Teaching In A Physiology Course For Medical Students: Acceptance By Students And Subjective Effect On Learning. Adv Physiol Educ. 2013;37(4):337–42.
Martin EA. Concise medical dictionary. 9th ed. Oxford: Oxford University Press; 2015.
Book Google Scholar
Han H, Nelson E, Wetter N. Medical students’ online learning technology needs. Clin Teach. 2014;11(1):15–9.
Barton J, Rallis KS, Corrigan AE, Hubbard E, Round A, Portone G, et al. Medical students’ pattern of self-directed learning prior to and during the coronavirus disease 2019 pandemic period and its implications for Free Open Access Meducation within the United Kingdom. J Educ Eval Health Prof. 2021;18:5.
O’Hanlon R, Laynor G. Responding to a new generation of proprietary study resources in medical education. J Med Libr Assoc. 2019;107(2):251–7.
Zhang J, Peterson RF, Ozolins IZ. Student approaches for learning in medicine: What does it tell us about the informal curriculum? BMC Med Educ. 2011;11(1):87.
Cooper AL, Elnicki DM. Resource utilisation patterns of third-year medical students. Clin Teach. 2011;8(1):43–7.
Wynter L, Burgess A, Kalman E, Heron JE, Bleasel J. Medical students: what educational resources are they using? BMC Med Educ. 2019;19(1):36.
Larsen DP, Butler AC, Roediger HL 3rd. Test-enhanced learning in medical education. Med Educ. 2008;42(10):959–66.
Augustin M. How to learn effectively in medical school: test yourself, learn actively, and repeat in intervals. Yale J Biol Med. 2014;87(2):207–12.
Moher D, Liberati A, Tetzlaff J, Altman DG. Reprint—Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Phys Ther. 2009;89(9):873–80.
Hammond M, editor Learning From Experience: Approaching The Research Of CD-ROM In Schools. WCCE; 1995.
Kentnor HE. Distance Education and the Evolution of Online Learning in the United States. Curric Teach. 2015;17:21–34.
Barry Issenberg S, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features And Uses Of High-Fidelity Medical Simulations That Lead To Effective Learning: A BEME Systematic Review. Med Teach. 2005;27(1):10–28.
Evaluation. EGfGo. Guidelines for Evaluating Papers on Educational Interventions. Education Group for Guidelines on Evaluation ed: BMJ; 1999. p. 1265–7.
Kirkpatrick D, Kirkpatrick J. Transferring Learning to Behavior : Using the Four Levels to Improve Performance. Oakland, United States: Berrett-Koehler Publishers, Incorporated; 2005.
Bernardo V, Ramos MP, Plapler H, De Figueiredo LF, Nader HB, Ancao MS, et al. Web-Based Learning In Undergraduate Medical Education: Development And Assessment Of An Online Course On Experimental Surgery. Int J Med Inform. 2004;73(9–10):731–42.
Raupach T, Munscher C, Pukrop T, Anders S, Harendza S. Significant Increase In Factual Knowledge With Web-Assisted Problem-Based Learning As Part Of An Undergraduate Cardio-Respiratory Curriculum. Adv Health Sci Educ Theory Pract. 2010;15(3):349–56.
Casillas JM, Gremeaux V. Evaluation Of Medical Students’ Expectations For Multimedia Teaching Materials: Illustration By An Original Method Using The Evaluation Of A Web Site On Cardiovascular Rehabilitation. Ann Phys Rehabil Med. 2012;55(1):25–37.
Cevik AA, Shaban S, El Zubeir M, Abu-Zidan FM. The Role Of Emergency Medicine Clerkship E-Portfolio To Monitor The Learning Experience Of Students In Different Settings: A Prospective Cohort Study. Int J Emerg Med. 2018;11(1):24.
Corrigan M, Reardon M, Shields C, Redmond H. “SURGENT” – Student E-Learning For Reality: The Application Of Interactive Visual Images To Problem-Based Learning In Undergraduate Surgery. J Surg Educ. 2008;65(2):120–5.
Davies BS, Rafique J, Vincent TR, Fairclough J, Packer MH, Vincent R, et al. Mobile Medical Education (Momed) - How Mobile Information Resources Contribute To Learning For Undergraduate Clinical Students - A Mixed Methods Study. BMC Med Educ. 2012;12:1.
de Sena DP, Fabricio DD, Lopes MH, da Silva VD. Computer-Assisted Teaching Of Skin Flap Surgery: Validation Of A Mobile Platform Software For Medical Students. PLoS ONE. 2013;8(7):e65833.
Howlett D, Vincent T, Gainsborough N, Fairclough J, Taylor N, Cohen J, et al. Integration Of A Case-Based Online Module Into An Undergraduate Curriculum: What Is Involved And Is It Effective? E-Learn. 2009;6(4):372–84.
Khalil R, Mansour AE, Fadda WA, Almisnid K, Aldamegh M, Al-Nafeesah A, et al. The Sudden Transition To Synchronized Online Learning During The COVID-19 Pandemic In Saudi Arabia: A Qualitative Study Exploring Medical Students’ Perspectives. BMC Med Educ. 2020;20(1):285.
Ogura A, Hayashi N, Negishi T, Watanabe H. Effectiveness of an e-Learning Platform for Image Interpretation Education of Medical Staff and Students. J Digit Imaging. 2018;31(5):622–7.
Orton E, Mulhausen P. E-Learning Virtual Patients For Geriatric Education. Gerontol Geriatr Educ. 2008;28(3):73–88.
Sijstermans R, Jaspers MW, Bloemendaal PM, Schoonderwaldt EM. Training Inter-Physician Communication Using The Dynamic Patient Simulator. Int J Med Inform. 2007;76(5–6):336–43.
Tews M, Brennan K, Begaz T, Treat R. Medical Student Case Presentation Performance And Perception When Using Mobile Learning Technology In The Emergency Department. Med Educ Online. 2011;16. https://doi.org/10.3402/meo.v16i0.7327 .
Wunschel M, Leichtle U, Wulker N, Kluba T. Using A Web-Based Orthopaedic Clinic In The Curricular Teaching Of A German University Hospital: Analysis Of Learning Effect, Student Usage And Reception. Int J Med Inform. 2010;79(10):716–21.
Zayed MA, Lilo EA, Lee JT. Impact of an Interactive Vascular Surgery Web-Based Educational Curriculum on Surgical Trainee Knowledge and Interest. J Surg Educ. 2017;74(2):251–7.
Al Zahrani EM, Al Naam YA, AlRabeeah SM, Aldossary DN, Al-Jamea LH, Woodman A, et al. E- Learning experience of the medical profession’s college students during COVID-19 pandemic in Saudi Arabia. BMC Med Educ. 2021;21(1):443.
Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11): e042378.
Coffey CS, MacDonald BV, Shahrvini B, Baxter SL, Lander L. Student Perspectives on Remote Medical Education in Clinical Core Clerkships During the COVID-19 Pandemic. Medical Science Educator. 2020;30(4):1577–84.
Diekhoff T, Kainberger F, Oleaga L, Dewey M, Zimmermann E. Effectiveness Of The Clinical Decision Support Tool ESR Eguide For Teaching Medical Students The Appropriate Selection Of Imaging Tests: Randomized Cross-Over Evaluation. Eur Radiol. 2020;30(10):5684–9.
Dombrowski T, Wrobel C, Dazert S, Volkenstein S. Flipped Classroom Frameworks Improve Efficacy In Undergraduate Practical Courses – A Quasi-Randomized Pilot Study In Otorhinolaryngology. BMC Med Educ. 2018;18(1):294.
Hari R, Kälin K, Harris M, Walter R, Serra A. Comparing Blended Learning With Faculty-Led Ultrasound Training: Protocol For A Randomised Controlled Trial (The SIGNATURE Trial). Praxis (Bern 1994). 2020;109(8):636–40.
Herrmann-Werner A, Weber H, Loda T, Keifenheim KE, Erschens R, Mölbert SC, et al. “But Dr Google Said…” - Training Medical Students How To Communicate With E-Patients. Med Teach. 2019;41(12):1434–40.
Jenkins S, Goel R, Morrell DS. Computer-Assisted Instruction Versus Traditional Lecture For Medical Student Teaching Of Dermatology Morphology: A Randomized Control Trial. J Am Acad Dermatol. 2008;59(2):255–9.
Lee LA, Chao YP, Huang CG, Fang JT, Wang SL, Chuang CK, et al. Cognitive Style and Mobile E-Learning in Emergent Otorhinolaryngology-Head and Neck Surgery Disorders for Millennial Undergraduate Medical Students: Randomized Controlled Trial. J Med Internet Res. 2018;20(2): e56.
Plackett R, Kassianos AP, Kambouri M, Kay N, Mylan S, Hopwood J, et al. Online Patient Simulation Training To Improve Clinical Reasoning: A Feasibility Randomised Controlled Trial. BMC Med Educ. 2020;20(1):245.
Schneider AT, Albers P, Muller-Mattheis V. E-Learning in Urology: Implementation of the Learning and Teaching Platform CASUS(R) - Do Virtual Patients Lead to Improved Learning Outcomes? A Randomized Study among Students. Urol Int. 2015;94(4):412–8.
Sox CM, Tenney-Soeiro R, Lewin LO, Ronan J, Brown M, King M, et al. Efficacy of a Web-Based Oral Case Presentation Instruction Module: Multicenter Randomized Controlled Trial. Acad Pediatr. 2018;18(5):535–41.
Sward KARNP, Richardson SRNP, Kendrick JMD, Maloney CMDP. Use of a Web-Based Game to Teach Pediatric Content to Medical Students. Acad Pediatr. 2008;8(6):354–9.
Wahlgren CF, Edelbring S, Fors U, Hindbeck H, Stahle M. Evaluation Of An Interactive Case Simulation System In Dermatology And Venereology For Medical Students. BMC Med Educ. 2006;6:40.
Gradl-Dietsch G, Menon AK, Gürsel A, Götzenich A, Hatam N, Aljalloud A, et al. Basic Echocardiography For Undergraduate Students: A Comparison Of Different Peer-Teaching Approaches. Eur J Trauma Emerg Surg. 2018;44(1):143–52.
Davis JS, Garcia GD, Wyckoff MM, Alsafran S, Graygo JM, Withum KF, et al. Use Of Mobile Learning Module Improves Skills In Chest Tube Insertion. J Surg Res. 2012;177(1):21–6.
Roesch A, Gruber H, Hawelka B, Hamm H, Arnold N, Popal H, et al. Computer Assisted Learning In Medicine: A Long-Term Evaluation Of The “Practical Training Programme Dermatology 2000.” Med Inform Internet Med. 2003;28(3):147–59.
Sendra-Portero F, Torales-Chaparro OE, Ruiz-Gomez MJ, Martinez-Morillo M. A Pilot Study To Evaluate The Use Of Virtual Lectures For Undergraduate Radiology Teaching. Eur J Radiol. 2013;82(5):888–93.
Farrimond H, Dornan TL, Cockcroft A, Rhodes LE. Development And Evaluation Of An E-Learning Package For Teaching Skin Examination. Action Research Br J Dermatol. 2006;155(3):592–9.
Moriates C, Valencia V, Stamets S, Joo J, MacClements J, Wilkerson L, et al. Using Interactive Learning Modules to Teach Value-Based Health Care to Health Professions Trainees Across the United States. Acad Med. 2019;94(9):1332–6.
Naeger DM, Straus CM, Phelps A, Courtier J, Webb EM. Student-Created Independent Learning Modules: An Easy High-Value Addition To Radiology Clerkships. Acad Radiol. 2014;21(7):879–87.
Smith E, Boscak A. A Virtual Emergency: Learning Lessons From Remote Medical Student Education During The COVID-19 Pandemic. Emerg Radiol. 2021;28(3):445–52.
Taurines R, Radtke F, Romanos M, König S. Using Real Patients In E-Learning: Case-Based Online Training In Child And Adolescent Psychiatry. GMS J Med Educ. 2020;37(7):Doc96-Doc.
De Villiers M, Walsh S. How Podcasts Influence Medical Students’ Learning – A Descriptive Qualitative Study. Afr J Health Prof Educ. 2015;7(1):130–3.
Wagner-Menghin M, Szenes V, Scharitzer M, Pokieser P. Designing Virtual Patient Based Self-Study Quizzes Covering Learning Goals In Clinical Diagnostic Sciences For Undergraduate Medical Students - The Radiology Example. GMS J Med. 2020;37(7):Doc91.
Nelson TM. Preparing for Practice: Strengthening Third-Year Medical Students’ Awareness of Point-of-Care Resources. Med Ref Serv Q. 2018;37(3):312–8.
Kourdioukova EV, Verstraete KL, Valcke M. The Quality And Impact Of Computer Supported Collaborative Learning (CSCL) In Radiology Case-Based Learning. Eur J Radiol. 2011;78(3):353–62.
Clark RC, Mayer RE. E-Learning and the Science of Instruction: Proven Guidelines for Consumers and Designers of Multimedia Learning. Hoboken: Center for Creative Leadership; 2016.
Gruner D, Pottie K, Archibald D, Allison J, Sabourin V, Belcaid I, et al. Introducing global health into the undergraduate medical school curriculum using an e-learning program: a mixed method pilot study. BMC Med Educ. 2015;15(1):142.
UNESCO. National education responses to COVID-19: summary report of UNESCO's online survey. United Nations Educational, Scientific and Cultural Organization.
Mann KV. Theoretical Perspectives In Medical Education: Past Experience And Future Possibilities. Med Ed. 2011;45(1):60–8.
Moreno R, Mayer RE. Cognitive Principles Of Multimedia Learning: The Role Of Modality And Contiguity. J Educ Psychol. 1999;91(2):358–68.
Kim S. The Future of e-Learning in Medical Education: Current Trend and Future Opportunity. J Educ Eval Health Prof. 2006;3:3.
Du S, Liu Z, Liu S, Yin H, Xu G, Zhang H, et al. Web-based distance learning for nurse education: a systematic review. Int Nurs Rev. 2013;60(2):167–77.
Lahti M, Hätönen H, Välimäki M. Impact of e-learning on nurses’ and student nurses knowledge, skills, and satisfaction: A systematic review and meta-analysis. Int J Nurs Stud. 2014;51(1):136–49.
Kirkpatrick DL. The Four Levels of Evaluation. In: Brown SM, Seidner CJ, editors. Evaluating Corporate Training: Models and Issues. Dordrecht: Springer, Netherlands; 1998. p. 95–112.
Chapter Google Scholar
Fuks A, Boudreau JD, Cassell EJ. Teaching Clinical Thinking To First-Year Medical Students. Med Teach. 2009;31(2):105–11.
Chumley-Jones HS, Dobbie A, Alford CL. Web-Based Learning: Sound Educational Method Or Hype? A Review Of The Evaluation Literature. Acad Med. 2002;77(10 Suppl):S86-93.
Kahn CE Jr, Ehlers KC, Wood BP. Radiologists’ Preferences for Just-in-Time Learning. J Digit Imaging. 2006;19(3):202–6.
Fairén M, Moyés J, Insa E. VR4Health: Personalized teaching and learning anatomy using VR. J Med Syst. 2020;44(5):94.
Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–12.
Klímová B. Mobile Learning in Medical Education. J Med Syst. 2018;42(10):194.
Baticulon RE, Sy JJ, Alberto NRI, Baron MBC, Mabulay REC, Rizada LGT, et al. Barriers to Online Learning in the Time of COVID-19: A National Survey of Medical Students in the Philippines. Medical Science Educator. 2021;31(2):615–26.
Mehrpour SR, Aghamirsalim M, Motamedi SM, Ardeshir Larijani F, Sorbi R. A supplemental video teaching tool enhances splinting skills. Clin Orthop Relat Res. 2013;471(2):649–54.
Larvin M. E-Learning In Surgical Education And Training. ANZ J Surg. 2009;79(3):133–7.
Lane J, Slavin S. Simulation in Medical Education: A Review. Simulation & Gaming - Simulat Gaming. 2001;32.
Bell DS, Fonarow GC, Hays RD, Mangione CM. elf-study from web-based and printed guideline materials. A randomized, controlled trial among resident physicians. Annals of internal medicine. 2000;132(12):938–46.
Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE. 2020;15(11):e0242905.
Rogers DA, Regehr G, Yeh KA, Howdieshell TR. Computer-assisted Learning versus a Lecture and Feedback Seminar for Teaching a Basic Surgical Technical Skill. The American journal of surgery. 1998;175(6):508–10.
Guri RS. E-Teaching In Higher Education: An Essential Prerequisite For E-Learning. J New Approaches Educ Res. 2018;7(2):93–7.
Alexander B, Adams-Becker S, Cummins M, Hall-Giesinger C. Digital Literacy in Higher Education, Part II: An NMC Horizon Project Strategic Brief. . Austin, Texas; 2017.
Wineburg S, McGrew S, Breakstone J, Ortega T. Evaluating Information: The Cornerstone of Civic Online Reasoning. Stanford Digital Repository; 2016.
Yengin İ, Karahoca D, Karahoca A, Yücel A. Roles Of Teachers In E-Learning: How To Engage Students & How To Get Free E-Learning And The Future. Procedia Soc. 2010;2(2):5775–87.
Keller J, Suzuki K. Learner Motivation and E-learning Design: A Multinationally Validated Process. Learn Media Technol. 2004;29:229–39.
Howe DL, Heitner KL, Dozier A, Silas S. Health Professions Faculty Experiences Teaching Online During the COVID-19 Pandemic. ABNF J. 2021;32(1):6–11.
Barteit S, Neuhann F, Bärnighausen T, Bowa A, Lüders S, Malunga G, et al. Perspectives of Nonphysician Clinical Students and Medical Lecturers on Tablet-Based Health Care Practice Support for Medical Education in Zambia, Africa: Qualitative Study. JMIR Mhealth Uhealth. 2019;7(1):e12637.
Easton G. Primary care education research-time to raise our game? Educ Prim Care. 2014;25(6):304–7.
Cahapay M. Kirkpatrick Model: Its Limitations As Used in Higher Education Evaluation. IJATE. 2021;8:135–44.
Byrnes KG, Kiely PA, Dunne CP, McDermott KW, Coffey JC. Communication, collaboration and contagion: “Virtualisation” of anatomy during COVID-19. Clin Anat. 2021;34(1):82–9.
Dunne S, Cummins NM, Hannigan A, Shannon, Dunne C, Cullen W. A method for the design and development of medical or health care information websites to optimize search engine results page rankings on Google. Journal of Medical Internet Research. 2013;15(8):e2632.
Download references
Acknowledgements
Not applicable
No funding received.
Author information
Authors and affiliations.
School of Medicine, University of Limerick, Limerick, Ireland
T. Delungahawatta, S. S. Dunne, S. Hyde, L. Halpenny, D. McGrath, A. O’Regan & C. P. Dunne
Centre for Interventions in Infection, Inflammation & Immunity (4I), University of Limerick, Limerick, Ireland
D. McGrath & C. P. Dunne
You can also search for this author in PubMed Google Scholar
Contributions
CPD, AOR, SH and DM conceived the study and its design. LH and AOR performed initial analysis. TD and SSD drafted and revised the manuscript. All authors co-wrote and approved the final manuscript.
A uthors’ information
Not applicable.
Corresponding author
Correspondence to C. P. Dunne .
Ethics declarations
Ethics approval and consent to participate, availability of data and material.
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
PRISMA Checklist.
Additional file 2:
Summary of Review Results.
Additional file 3:
Intervention Characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Delungahawatta, T., Dunne, S.S., Hyde, S. et al. Advances in e-learning in undergraduate clinical medicine: a systematic review. BMC Med Educ 22 , 711 (2022). https://doi.org/10.1186/s12909-022-03773-1
Download citation
Received : 26 February 2022
Accepted : 26 September 2022
Published : 07 October 2022
DOI : https://doi.org/10.1186/s12909-022-03773-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Online learning
- Distance learning
- Medical education
- Medical students
- Clinical medicine
- Systematic review
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
No Increased Risk Of Autism Or ADHD From Acetaminophen Use During Pregnancy, Study Suggests
- Share to Facebook
- Share to Twitter
- Share to Linkedin
A new study which compared siblings who were and weren’t exposed to acetaminophen during pregnancy found the drug doesn’t increase the risk of autism and ADHD, adding new evidence to a long-debated topic.
A pregnant mother holding her belly.
The researchers followed millions of children for 26 years after they were born, and they did see a small increase in ADHD, autism and intellectual disability in the overall population compared to when they were younger; around 7.5% were exposed to acetaminophen (the active ingredient in Tylenol) during pregnancy.
The risk of developing these neurodevelopmental disorders in kids who weren’t exposed to acetaminophen before birth versus those who were was 1.33% vs 1.53% for autism, 2.46% vs 2.87% for ADHD, and 0.70% vs 0.82% for intellectual disability, according to the study published Tuesday in JAMA Network Open.
However, the researchers decided to also use a sibling model to examine the risks, because prenatal acetaminophen exposure was more common in kids with parents who smoked during pregnancy, had lower socioeconomic status and previous diagnoses of neurodevelopmental disorders , all potential risk factors for ADHD and autism.
They didn’t find any increased risk when comparing siblings who were exposed to acetaminophen before birth and those who weren't exposed, meaning the increased risk of developing neurodevelopmental disorders may be due to other factors like genetics.
Some previous research has concluded prenatal acetaminophen use may increase the risk of neurobehavioral issues, but the current study found no evidence to support a cause-and-effect link when using a sibling model.
The study researchers noted that because siblings share a large portion of the same genetic background and may be exposed to similar environmental factors during pregnancy, comparing siblings—which most previous studies didn’t do—helps to control for these outside factors.
Acetaminophen is the only pain reliever generally considered safe for use during pregnancy, but many pregnant people may not take acetaminophen due to fears of potentially harmful side effects, so the researchers are hopeful this study provides “reassurance” to expectant parents.
Crucial Quote
“This study’s findings may be welcome news for birthing people who use acetaminophen as a pain or fever management option, since there are few safe alternatives for relief available,” Renee Gardner, a study author and principal researcher at Sweden’s Karolinska Institutet, said in a statement.
2.4 million. That’s how many children—who were all born in Sweden—were used as a part of this cohort, making this the largest study to date to examine the connection between Tylenol and ADHD, autism and intellectual disability, according to the study.
Acetaminophen’s link to neurodevelopmental disorders has been a controversial topic within the health community, as several studies have previously found the drug does cause an increase in neurobehavioral issues. Children whose umbilical cord blood samples had the highest doses of acetaminophen were around three times more likely to develop ADHD and autism, according to a separate JAMA study published in 2019. An international group of researchers recommended in 2021 that pregnant individuals limit their exposure by using the lowest effective dose for the shortest amount of time, and called for more warnings around taking acetaminophen during pregnancy, according to research published in Nature Reviews Endocrinology. However, they noted other factors like maternal alcohol use and stress may also play a role. Long term acetaminophen use during pregnancy resulted in a 20% higher risk of autism and a 30% higher risk of ADHD, a 2018 meta analysis published in the American Journal of Endocrinology found.
Key Background
A separate 2021 study also used a sibling model to examine this link, and it found both the exposed and unexposed children of mothers who took acetaminophen during pregnancy had an increased risk of developing ADHD. The researchers concluded these results may be partly due to “unobserved familial factors.” The Food and Drug Administration said in 2015 evidence was too “limited” to make any recommendations against using over-the-counter medications like acetaminophen during pregnancy. A class action lawsuit was brought against the makers of Tylenol and similar generic versions of the drug partially due to the recommendations from the 2021 Nature paper. However, a federal judge ruled in December 2023 the research cited in the lawsuit cannot be used as evidence since at least one of experts the plaintiffs used "cherry-picked and misrepresented study results and refused to acknowledge the role of genetics in the etiology of either [autism spectrum disorder] or ADHD." In September 2023, the FDA declined to comment on the lawsuit, though it conducted a new review of more recent studies earlier that year and said they were “limited” and “inconsistent.” Other medical bodies like the American College of Obstetricians and Gynecologists (ACOG) maintain that acetaminophen use during pregnancy is safe in moderation.
Further Reading
Federal judge says research can't be used to link acetaminophen to autism, ADHD (ABC News)

- Editorial Standards
- Reprints & Permissions
Ozempic, Wegovy Won't Boost Thyroid Cancer Risk: Study
Ozempic, Wegovy Won't Boost Thyroid Cancer Risk: Study
By Ernie Mundell HealthDay Reporter

WEDNESDAY, April 10, 2024 (HealthDay News) -- Wegovy, Ozempic and other drugs known as GLP-1 analogues have become wildly popular for controlling diabetes and helping folks lose weight.
There were concerns that longer term use of the drugs might raise users' odds for thyroid cancer, but a Swedish study of more than 435,000 people finds no evidence to support that notion.
“Many people take these medicines, so it is important to study potential risks associated with them,” said study lead author Björn Pasternak . He's principal researcher at the department of medicine at the Karolinska Institute in Stockholm.
“Our study covers a broad group of patients and provides strong support that GLP-1 analogues are not associated with an increased risk of thyroid cancer," he said in an institute news release .
U.S. Cities With the Most Homelessness

The findings were published April 9 in the BMJ .
In the analysis, Pasternak's team used data from a major Scandinavian database involving 145,000 people who were taking GLP-1 analogues such as liraglutide (Victoza) or semaglutide ( Ozempic ), and 290,000 people who were taking one of another class of diabetes drugs called DPP4 inhibitors.
The study found no higher odds for thyroid cancer among folks taking GLP-1 analogues compared to those on DPP4 inhibitors.
That finding was repeated when GLP-1 analogue users were compared to patients taking a third class of diabetes meds, called SGLT2 inhibitors.
Study co-author Peter Ueda , an assistant professor of medicine at the Karolinska Institute, stressed that the final verdict on GLP-1 analogues' effect on the thyroid is still to come.
“We cannot rule out that the risk of certain subtypes of thyroid cancer is increased in smaller patient groups that we could not study here, for example in people with a high congenital risk of medullary thyroid cancer who are advised against using these drugs,” Ueda said.
More information
Find out more about thyroid cancer at the American Cancer Society .
SOURCE: Karolinska Institute, news release, April 9, 2024
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Embattled Johnson Bruised Again
Aneeta Mathur-Ashton April 10, 2024

What to Know About Biden's State Dinner
Laura Mannweiler April 10, 2024

Fed: Inflation Path ‘Somewhat Uneven’
Tim Smart April 10, 2024

No Letup From Inflation in March

Arizona Court Upholds 1864 Abortion Ban
Lauren Camera April 9, 2024

EXPLAINER: Rare Human Case of Bird Flu
Cecelia Smith-Schoenwalder April 9, 2024


IMAGES
VIDEO
COMMENTS
The aim of this article is to introduce family medicine researchers to case study research, a rigorous research methodology commonly used in the social and health sciences and only distantly related to clinical case reports. The article begins with an overview of case study in the social and health sciences, including its definition, potential ...
Editorial. Introduction. Case reports and case series or case study research are descriptive studies to present patients in their natural clinical setting. Case reports, which generally consist of three or fewer patients, are prepared to illustrate features in the practice of medicine and potentially create new research questions that may contribute to the acquisition of additional knowledge ...
A case study is a research approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context. It is an established research design that is used extensively in a wide variety of disciplines, particularly in the social sciences. A case study can be defined in a variety of ways (Table 5 ), the ...
A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine. Some reports contain an extensive review of the relevant ...
Case studies have been used in the medical profession for over 100 years to convey the clinical course of a disease and its treatment. This form of inquiry is important to many disciplines because it allows researchers to explore a phenomenon of interest in rich detail. This chapter describes an innovative case study method whereby the patient ...
The aim of this article is to introduce family medicine researchers to case study research, a rigorous research methodology commonly used in the social and health sciences and only distantly related to clinical case reports. The article begins with an overview of case study in the social and health sciences, including its definition, potential applications, historical background and core features.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
S.M. Holmes and Others. The Case Studies in Social Medicine demonstrate that when physicians use only biologic or individual behavioral interventions to treat diseases that stem from or are ...
This red paper for faculty and librarians in medical schools, APN programs, and PA programs reviews the research on case-based learning in medical environments and covers: ⊲ Key elements that define case-based instruction ⊲ Advantages of this pedagogical approach ⊲ Evidence of improvement in clinical decision-making
Case-Based Learning (CBL) in medical education is a teaching approach that engages students as learners through active learning in small, collaborative groups to solve cases from clinical patients. Due to the challenges afforded by the COVID-19 pandemic, small group learning such as CBL, transitioned quickly to include technology-enhanced learning to enable distance delivery, with little ...
2.3. DIFFERENT STUDY TYPES USED IN MEDICAL AND EPIDEMIOLOGICAL RESEARCH Case Report. The Case Report describes the occurrence of a health condition in one or two patients usually in terms of patient symptoms, clinical manifestations, diagnosis, treatment, and outcome. E.g. Description of a case of trachoma with unusual manifestations and evolution.
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
Case Studies in Academic Medicine. Kanter, Steven L. MD. Academic Medicine: April 2010 - Volume 85 - Issue 4 - p 567. doi: 10.1097/ACM.0b013e3181d953f3. Free. Metrics. Everyone who works in a medical school or teaching hospital has heard someone say, "Don't make too much of that article. It's not a real study, just a case study.".
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
Case-based learning has drawn a lot of attention in medical education because it is a student-centered teaching. model that exposes students to real -world situations that they must answer using ...
case study method is considered to be the link between theory and practice in. medical education (Turk et al., 2019). The case study dates back to Harvard Law School in the 1870s (Servant-Miklos ...
Key words used were "Case-based learning" and "medical education", and 360 articles were retrieved. Of these, 70 articles were selected to review for location, human health care related fields of study, number of students, topics, delivery methods, and student level.
Focus groups 1-6 used three case studies: an image analysis tool, a ChatBot for asking questions about a medical procedure, and a risk prediction tool that analyzed and flagged patients at risk ...
These case studies are intended to draw out lessons for the development of a cross-sectoral governance framework for emerging technologies in health and medicine. The focus of the case studies is the governance ecosystem in the United States, though where appropriate, the international landscape is included to provide context.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
Svenningsson P, Wirdefeldt K, Yin L, et al. Reduced incidence of Parkinson's disease after dipeptidyl peptidase-4 inhibitors — a nationwide case-control study. Mov Disord 2016;31:1422-1423 ...
E-learning is recognised as a useful educational tool and is becoming more common in undergraduate medical education. This review aims to examine the scope and impact of e-learning interventions on medical student learning in clinical medicine, in order to aid medical educators when implementing e-learning strategies in programme curricula. A systematic review compliant with PRISMA guidelines ...
BIDMC physician-scientists report on a study concerning an AI, ChatGBT-4, outperforming internal medicine residents and physicians at processing medical data. ... these things are capable of showing the equivalent or better reasoning than people throughout the evolution of clinical case." Rodman and colleagues used a previously validated tool ...
Case Study - Pearl Family Medicine. Focus on High Leverage Change: Risk Assessment. PRACTICE SNAPSHOT: Pearl Family Medicine. A new, physician-owned practice in Denver, Colorado Clinicians: 1 MD, 1 PA. 1. Number of patients: 1,200 Quality Improvement team: The (MD) practice owner was the QI Lead for this project and has
Screening rates for alcohol use disorder (AUD) are low, warranting the re-evaluation of the accuracy of screening tests to fit with the DSM-5 criteria. New case definitions have an impact on the ...
The risk of developing these neurodevelopmental disorders in kids who weren't exposed to acetaminophen before birth versus those who were was 1.33% vs 1.53% for autism, 2.46% vs 2.87% for ADHD ...
From September 2017 through May 2023, a total of 5020 patients were enrolled (95.4% of whom were from Sweden). The median follow-up was 3.5 years (interquartile range, 2.2 to 4.7).
There were concerns that longer term use of the drugs might raise users' odds for thyroid cancer, but a Swedish study of more than 435,000 people finds no evidence to support that notion.
The Federation Credentials Verification Service (FCVS) provides a centralized process for state medical boards to obtain a verified record of a physician's core medical credentials. Call FCVS at 888-275-3287 for more information. It might take 60 days.