Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Factors that influence uptake of routine postnatal care: Findings on women’s perspectives from a qualitative evidence synthesis
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of International Health, Johns Hopkins School of Public Health, Baltimore, Maryland, United States of America
Roles Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing
Affiliation School of Community Health and Midwifery, University of Central Lancashire, Preston, United Kingdom
Roles Data curation, Formal analysis, Methodology, Validation, Writing – review & editing
Affiliation Department of Reproductive Health and Research, World Health Organization, Genève, Switzerland
Roles Data curation, Methodology, Writing – review & editing
Affiliation Centre Hospitalier de l’Universite de Montreal, Montreal, Canada
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Validation, Writing – review & editing
Affiliation Partnership for Maternal, Newborn, and Child Health, World Health Organization, Genève, Switzerland
Affiliation Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, United States of America
Roles Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing
- Emma Sacks,
- Kenneth Finlayson,
- Vanessa Brizuela,
- Nicola Crossland,
- Daniela Ziegler,
- Caroline Sauvé,
- Étienne V. Langlois,
- Dena Javadi,
- Soo Downe,
- Mercedes Bonet

- Published: August 12, 2022
- https://doi.org/10.1371/journal.pone.0270264
- Reader Comments
Effective postnatal care is important for optimal care of women and newborns–to promote health and wellbeing, identify and treat clinical and psychosocial concerns, and to provide support for families. Yet uptake of formal postnatal care services is low and inequitable in many countries. As part of a larger study examining the views of women, partners, and families requiring both routine and specialised care, we analysed a subset of data on the views and experiences of women related to routine postnatal care.
We undertook a qualitative evidence synthesis, using a framework analysis approach. We included studies published up to December 2019 with extractable qualitative data, with no language restriction. We focused on women in the general population and their accounts of routine postnatal care utilization. We searched MEDLINE, PUBMED, CINAHL, EMBASE, EBM-Reviews, and grey literature. Two reviewers screened each study independently; inclusion was agreed by consensus. Data abstraction and scientific quality assessment were carried out using a study-specific extraction form and established quality assessment tools. The analysis framework was developed a priori based on previous knowledge and research on the topic and adapted. Due to the number of included texts, the final synthesis was developed inductively from the initial framework by iterative sampling of the included studies, until data saturation was achieved. Findings are presented by high versus low/middle income country, and by confidence in the finding, applying the GRADE-CERQual approach.
Of 12,678 papers, 512 met the inclusion criteria; 59 articles were sampled for analysis. Five themes were identified: access and availability; physical and human resources; external influences; social norms; and experience of care. High confidence study findings included the perceived low value of postnatal care for healthy women and infants; concerns around access and quality of care; and women’s desire for more emotional and psychosocial support during the postnatal period. These findings highlight multiple missed opportunities for postnatal care promotion and ensuring continuity of care.
Conclusions
Factors that influence women’s utilization of postnatal care are interlinked, and include access, quality, and social norms. Many women recognised the specific challenges of the postnatal period and emphasised the need for emotional and psychosocial support in this time, in addition to clinical care. While this is likely a universal need, studies on mental health needs have predominantly been conducted in high-income settings. Postnatal care programmes and related research should consider these multiple drivers and multi-faceted needs, and the holistic postpartum needs of women and their families should be studied in a wider range of settings.
Registration
This protocol is registered in the PROSPERO database for systematic reviews: CRD42019139183.
Citation: Sacks E, Finlayson K, Brizuela V, Crossland N, Ziegler D, Sauvé C, et al. (2022) Factors that influence uptake of routine postnatal care: Findings on women’s perspectives from a qualitative evidence synthesis. PLoS ONE 17(8): e0270264. https://doi.org/10.1371/journal.pone.0270264
Editor: Hannah Tappis, Jhpiego, UNITED STATES
Received: September 20, 2021; Accepted: June 7, 2022; Published: August 12, 2022
Copyright: © 2022 Sacks et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting information files.
Funding: Funding was provided by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research, World Health Organization, Geneva, Switzerland.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: LMIC, Low- or Middle-Income Countries; MeSH, Medical Subject Headings; PNC, Postnatal Care; PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analyses; WHO, World Health Organisation
Postnatal care (PNC) is a fundamental component of the maternal, newborn and child care continuum, and contributes to reducing maternal and neonatal morbidity and mortality and improving overall health and wellbeing [ 1 – 3 ]. It is generally defined as the care provided during the postnatal period, beginning immediately after childbirth and up to six weeks (42 days) after birth [ 1 ] or beyond [ 4 ]. PNC represents a set of healthcare services designed to promote the health of women and newborns; it includes risk identification, preventive measures, health education and promotion, and management or referral for complications. Postnatal care not only improves mortality and clinical care, but also affects the satisfaction and experience of health care users; understanding the experiences and needs of women and their families with regard to postnatal care can improve utilization and positive experiences. The World Health Organisation (WHO) recommends that all women and newborns receive postnatal care in the first 24 hours following childbirth, regardless of where the birth occurs, and subsequent postnatal check-ups in the first six weeks [ 5 ].
Nevertheless, postnatal care ranks among the lowest coverage of maternal and child health services interventions; after facility discharge, only 31% of women and 13% of newborns receive a postnatal check [ 6 , 7 ]. Previous studies have also identified important socioeconomic and geographic inequities in access to and utilisation of postnatal care services [ 8 ].
Over the last two decades, there have been multiple contributions to a large and growing canon of literature on facilitators and barriers to maternity care, including recent systematic reviews [ 9 – 11 ]. However, most of these studies have focused on care-seeking for intrapartum care and immediate PNC (within 24 hours), and not later (e.g. post discharge) postnatal care [ 12 – 14 ]. Much of the literature on maternity care focuses on facilitators and barriers to utilization [ 15 – 18 ] but, as low quality care has recently been associated with a potentially higher attributable risk of mortality than lack of access [ 19 ], studies have begun to examine perceived and actual quality of care, including disrespect and abuse at facilities, as contributing factors to low utilisation of maternal health services [ 15 – 18 ]. Very few studies have examined the impact of mistreatment or disrespect of newborns as discouraging factors for uptake of postnatal care, but recent studies have demonstrated the importance of satisfaction with maternal and neonatal care on subsequent care utilization [ 20 , 21 ].
This paper presents the results of a sub-set of the data from a qualitative evidence synthesis designed to explore the views and experiences of women, their partners, families and communities in the postnatal period, and factors that influence uptake of routine postnatal care. For this analysis, our aim was to assess the views and experiences of women in the general population in accessing routine postnatal care for themselves and their infants.
We included qualitative or mixed-methods studies where the focus was the views of women in the general population (i.e. excluding sub-populations such as adolescents or migrants) on factors that influence uptake of routine postnatal care (i.e. those without additional postnatal needs due to comorbidities or identified medical risk), irrespective of parity, mode of delivery, or place of delivery. Qualitative studies and mixed methods studies were those that included a qualitative component, either for design (i.e. ethnography, phenomenology), data collection (i.e. focus groups, interviews, observations, diaries, oral histories), or analysis (i.e. thematic analysis, framework approach, grounded theory).
A framework approach was used to inductively develop initial themes [ 22 ] and thematic synthesis [ 23 ] and was then used iteratively based on the initial thematic framework. Study assessment included the use of a validated quality appraisal tool [ 24 ]. Confidence in the findings was assessed using the GRADE-CERQual tool [ 25 ].
Definitions
We define the postnatal period as the time between birth, including the immediate postpartum period (first 24 hours after birth), and up to six weeks (42 days) after birth [ 1 ]. This period varies cross-culturally, but usually coincides with confinement periods and other cultural practices in the 30–45 days following birth.
We define ‘routine postnatal care’ as formal service provision that is specifically designed to support, advise, inform, educate, identify those at risk and, where necessary, manage or refer women or newborns, to ensure optimal transition from childbirth to motherhood and childhood. Postnatal care can include a wide range of activities, including risk identification (assessments, screening), prevention of complications, health education and promotion (infant feeding and care, life-skills education, postpartum family planning, nutrition, vaccines, mental health support, and prevention and management of harmful practices—including smoking and alcohol—and violence) and support for families. Routine postnatal care does not typically include specialist services for comorbidities, address social needs, or the management of conditions not related to pregnancy or postpartum care, though referrals can be made for such services as a result of routine postnatal care.
Reflexive statement
Our study team included a medical doctor, a midwife, epidemiologists, public health researchers, and librarians, all with extensive experience in the provision and study of maternal and neonatal healthcare. We began this study with anecdotal and experiential knowledge that postnatal care is very often unavailable or inadequate, with minimal emphasis on the psychosocial needs. We believed PNC to be poorly and inequitably accessible, even in high-income settings, and especially in low- and middle-income countries (LMICs), and that due to perceived or actual poor quality care, including potential fears of mistreatment, and services not being user-friendly, families may be discouraged from seeking care. Multiple members of our study team have been involved in the direct provision of postnatal care, and in developing national and international guidelines for postnatal care.
Search strategy
The search strategy was developed with senior librarians based on the following concepts: barriers and limitations, postnatal care, and health services needs and demands. The search was limited to qualitative and mixed-methods studies (see S1 Appendix ). Databases searched included MEDLINE (OVID), PubMed, CINAHL (EBSCO), EMBASE (OVID), and EBM-Reviews (OVID), as well as a search for grey literature. The search strategy covered papers published from inception through December 2019. There were no language restrictions. Hand searching was used to identify grey literature documents on the following websites: BASE (Bielefeld University Library), OpenGrey, and on the World Health Organization. Duplicates were excluded through the EndNote X9 software using a method developed by Bramer et al. [ 26 ] Inclusion and exclusion criteria are presented in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0270264.t001
Study selection
- Either “general population” or sub-populations such as adolescents, migrants
- “Women’s view’s only”, “partners and family views only”, or “women’s, and partner/family views”.
- Either high-income (HIC) or low or middle-income (LMIC) country setting, using the 2019 World Bank Classification Scheme.
In accord with the global nature of the review, and to ensure sufficient representation of country levels especially lower income settings, we divided the studies into either HIC or LMIC for sampling. Due to the very large number of eligible papers, 40 papers (~15%) from each geographic group (HIC or LMIC) were randomly sampled at a time, and screening and extraction was conducted until it was agreed by consensus that thematic saturation was reached for each geographic group, at which point 10 additional papers were selected from each group for confirmatory analysis (if saturation was not, 20 more papers were selected for that group, until it was agreed that saturation was reached, at which point a confirmatory set was then selected). Prior to undertaking this process, it was agreed that, if no further themes were identified after confirmatory analysis, the group was considered saturated.
Extraction of data and assessment of quality was conducted for each eligible paper by study team members. Disagreements were settled by consensus among reviewers. Themes from HIC and LMIC groups were analysed together, which notations made where the specifics or manifestation of each theme different between country groups.
Study team members did not assess papers in which they were a co-author. Two of the included studies were published in a language other than English: a Brazilian study [ 27 ] was analysed by one of the study team members fluent in Portuguese and a Japanese study [ 28 ] was translated by a Japanese-speaker into English prior to analysis. All quotes included in this manuscript were translated into English by the study authors, the respective study team members, or colleagues who assisted with translation.
Papers which did not meet either the general or specific inclusion criteria upon full review were either excluded or put aside to be evaluated separately for future analysis. Studies which did not include first-hand reports of women’s experiences were excluded; studies which focused exclusively on a sub-population (e.g. young adolescent mothers) were put aside for separate subsequent analysis.
Data extraction and analysis
Data extraction, analysis and quality appraisal proceeded concurrently and broadly followed the ‘best fit’ framework approach described by Carroll [ 22 ]. Based on previous related reviews of antenatal care [ 29 ] and intrapartum care [ 30 ] as well as a recent thematic synthesis of ‘what matters to women’ during the postnatal period [ 31 ] we used a deductive approach to develop a thematic framework comprising four broad concepts (Resources and access; Behaviours and attitudes; External influences; What women want and need) as well as a number of sub-themes (see S2 Appendix ). We then used thematic synthesis techniques [ 23 ] to confirm our a priori framework, or to develop new themes where emerging data failed to fit. We began by using an Excel spreadsheet to record pertinent details from each study (e.g. author, country, publication date, study design, setting and location of birth, setting and location of postnatal care, sample size, data collection methods, participant demographics, contexts, study objectives). The four concepts from our a priori framework were added to the Excel sheet and the author-identified findings from each study were extracted (along with supporting quotes) and mapped to the framework as appropriate. Any codes which did not map to the framework were placed in a section marked ‘other’ to allow for the emergence of new sub-themes or concepts. This process included looking for what was similar between papers and for what contradicted (‘disconfirms’) the emerging themes. For the disconfirming process we consciously looked for data that would contradict our emerging themes, or our prior beliefs, and views related to the topic of the review.
Quality assessment
Included studies were appraised using an instrument developed by Walsh and Downe [ 32 ] and modified by Downe et al. [ 33 ]. Studies were rated against 11 pre-defined criteria [ 33 ], and then allocated a score from A–D (including + and -), where A+ was the highest and D- the lowest (see Table 2 ). Studies rated with a D were excluded from further data analysis.
https://doi.org/10.1371/journal.pone.0270264.t002
Studies were appraised by each reviewer independently and a 10% sample was cross-checked by a different study team member to ensure consistency. Each reviewer was asked to extract and assess both LMIC and HIC papers in order to increase intra-rater reliability between the two geographic groups. Any studies where there were scoring discrepancies of more than a grade were referred to another study team member for moderation.
Once the framework of descriptive themes (or review findings) was agreed by the study team, the level of confidence in each review finding was assessed using the GRADE-CERQual tool [ 34 ] and agreed by consensus between two study team members. GRADE-CERQual assesses the methodological limitations and relevance to the review of the studies contributing to a review finding, the coherence of the review finding, and the adequacy of data supporting a review finding. Based on these criteria, review findings were graded for confidence using a classification system ranging from ‘high’ to ‘moderate’ to ‘low’ to ‘very low’. Following CERQual assessment the review findings were grouped into higher order analytical themes and the final framework was agreed by consensus amongst the study team.
Papers included in overall study and analytic sample
Our systematic searches yielded 12,678 records, of which 17 were duplicates. An additional 12,149 were excluded by title and by abstract, leaving 602 for full text review (See Fig 1 ).
https://doi.org/10.1371/journal.pone.0270264.g001
Our final list of articles for the analytic sample included 59 studies with views from women in the general population on routine postnatal care, with 32 coming from HICs and 27 from LMICs. Specifically, of the LMIC studies, 6 were from low income countries, 12 from lower-middle income countries, and 9 from upper-middle income countries. The global representation of studies was reasonably wide with 17 coming from Europe, 13 from Africa, 10 from North America, 9 from Asia, 4 from the Middle East, 4 from Australasia, and 2 from South America. The two South American studies were both from Brazil and, although we actively searched our entire database for studies from other Latin American countries, no others fulfilled our inclusion criteria. The studies were generally of good quality with an average quality rating of B and were mainly qualitative and descriptive in design. A full list of the included studies with relevant characteristics is shown in Table 3 .
https://doi.org/10.1371/journal.pone.0270264.t003
This process generated 20 review findings. Following discussions amongst the study team, these descriptive themes were then mapped against our a priori framework themes to generate our final analytical themes. Resources and Access was split into two separate themes: Access and Availability and Physical and Human Resources . We changed Behaviours and Attitudes to Social Norms to better reflect the larger group of stakeholders influencing maternal choice or behaviour, and we changed the title of What Women Want and Need to Experience of Care to better reflect the experiential nature of the findings.
Our analysis reinforced some aspects of the themes in our a priori framework and modified or expanded others. This final framework includes twenty-one themes and five overarching study findings: Access and Availability; Physical and Human Resources; External Influences; Social Norms; and Experience of Care . Our final framework displaying the analytical themes and descriptive themes, with their associated CERQual gradings, is shown in Table 4 .
https://doi.org/10.1371/journal.pone.0270264.t004
Themes identified from included studies
Access and availability..
Whilst proximity to a health facility appeared to encourage engagement with maternity providers, our evidence suggests that, for some women living in remote or rural areas, a lack of transport or the poor quality of transport networks limited attendance at postnatal clinics. This was compounded in situations where women did not have the personal resources to pay for relatively expensive journeys to health facilities and/or could not afford to take time away from their work or family. Even in high income settings where access to postnatal services is ostensibly free at point of care, the additional costs associated with attendance including insurance levies, childcare costs, and transport costs limited engagement for women living in poverty.
For accessing postnatal care post-discharge from a health facility after birth, women wanted a wide range of possible options and flexible schedules for reaching healthcare workers. Women generally valued the ability to contact providers at convenient times even more so than having a large number of contacts. Women wanted to be able to get support during moments of high stress, or on their schedules, rather than on a pre-defined health systems schedule, and many referenced the value of their time. Women expressed frustration about not being able to reach healthcare workers when needed. Service providers that were able to offer more flexible opportunities for engagement like drop-in clinics, telephone contacts, out of hours services and, in particular, home visits, were viewed more positively.
Physical and human resources.
For women in a variety of different settings, the ability to engage with formal postnatal services was influenced by resource and infrastructure constraints, especially in settings where community-based services were limited or non-existent. The evidence also suggests that the poor availability of resources in some health facilities may act as a deterrent to women who might otherwise benefit from postnatal care. A lack of basic medicine and equipment and inadequate or inconsistent water or electricity supplies limited attendance in some low-income settings. Whilst the availability of essential equipment and utilities was not reported to be an issue in most high-income countries, women were sometimes aware of staff shortages on postnatal wards and this affected their experience of care. Women’s perception that some health facilities were understaffed, especially from studies in LMICs, was also reflected in the length of time they had to wait to be seen by a healthcare provider. In some instances, this was compounded by cursory and impersonal exchanges with care providers, leaving women feeling frustrated, annoyed and undervalued.
External influences.
Women identified several external influences as having a bearing on their engagement with postnatal services. These ranged from environmental influences such as the physical condition of the health facility itself to the availability and affordability of private providers to a willingness (or otherwise) to engage with traditional postnatal practices, either in accordance with or against the advice of family and community members.
For women in a variety of different settings and contexts, the condition of postnatal wards and health facilities was important. Women used words such as ‘clean’ and ‘modern’ to frame positive perceptions or ‘dirty’ and ‘unhygienic’ to highlight negative experiences. These negative accounts were more commonly associated with facilities in low-income settings but even in high income countries women used words like ‘dilapidated’ and ‘unwelcoming’ to describe postnatal wards. In addition to the condition of the buildings, women also commented on the lack of physical space in some facilities and how this impacted on their sense of personal space and perception of privacy. Some women felt the opportunity to engage in confidential conversations with family members or healthcare providers was compromised whilst others felt the shared facilities and tight surroundings in some postnatal wards generated a noisy and disruptive atmosphere. For mothers who already felt exhausted and fatigued from childbirth, the impact of this environment coupled with their inability to control system-oriented, organizational routines, led to feelings of frustration and exasperation.
By contrast, for women who gave birth at home, the nurturing nature of familiar surroundings as well as their ability to establish personal routines and control access to their home created a more relaxing environment. In settings where private facilities were available, they were generally considered to be of better quality and were utilised by some women with the financial means to do so. However, in some contexts, the integration between private and public providers was inadequate and impacted on women’s engagement with postnatal services once they were discharged from the health facility.
Women’s capacity to engage with postnatal services was influenced by other family members and individuals in their social circles. In some contexts, women’s autonomy was inhibited by patriarchal social structures and decisions relating to engagement with maternity services, including postnatal care, were largely deferred to husbands. Sometimes, these kinds of decisions were agreed jointly between the woman’s husband and her mother-in-law and sometimes the decision was solely the responsibility of the mother-in-law.
Women expressed that elderly relatives and the broader beliefs and expectations of local communities influenced their observance of traditional postnatal practices rather than ‘westernised’ approaches to postnatal care, which some may have preferred. In some rural communities, especially in Africa, the reliance on TBAs to administer specific herbs and medicines in the postnatal period was integral to a communal belief system, whilst in other settings it was simply more convenient or financially viable. For other women, especially in Asia, the cultural practice of ‘doing the month’ involved extended periods of isolation and seclusion and limited interaction with formal postnatal services. Our findings also indicate that, in these contexts, some women (and their families) found it difficult to steer a course between the increasing influence of “Western” approaches to postnatal care and adhering to the traditional practices advocated by previous generations.
Social norms.
Women highlighted a variety of behaviours and understandings about the health system that affected their willingness to engage with postnatal care providers. For some women, especially from studies in LMICs, these understandings were based on a perception that attendance at health facilities offering postnatal care was only necessary if they felt unwell or if there was a problem with their infant. In many cases, this notion was reinforced by healthcare providers who did not encourage attendance or devalued the services they offered. When health workers devalued PNC, families also tended to devalue PNC and not see the need to seek care.
Some women also believed that postnatal services were solely focused on infant wellbeing and development and, although they valued the services on offer for newborns (clinical assessments and immunizations), they were not aware of, or did not acknowledge, any sources of care and support for themselves.
For some women, a reluctance to engage with postnatal services was rooted in a lack of trust in the system. In certain contexts, this was based on a perception that some providers were corrupt and expected informal payments, gifts, or bribes in return for care. In other settings, women’s trust in the system was undermined by perceived inadequacies in the clinical or personal skills of the healthcare providers. More infrequently, women complained that confidential information shared with health providers might be compromised or abused and, in more extreme cases, women believed that disclosure of mental health issues (like postnatal depression) might lead to their infant being taken away from them. In a few specific contexts, women expressed a preference to be seen by female health providers and highlighted safety concerns when postnatal visits at home were conducted by male health workers.
Experience of care.
Based on their experiences of postnatal care, women identified a range of issues that were of particular importance during their postnatal journey, including the need for information and support and the desire to be treated with care and respect by familiar and trusted healthcare providers.
Women from a variety of different settings and contexts highlighted the need for information during all phases of postnatal care. Although some of these informational needs were met by friends, peers, family members and online sources, women looked to healthcare providers for information about infant nutrition and development as well as tips and advice on infant crying cues, sleeping patterns, breastfeeding, and safety concerns. Although women tended to prioritise the needs of their newborns over their own, they also sought personal information for example on wound care, contraception, and when to resume sexual activity. The timing and delivery of information was also discussed by many women indicating that information should be supplied both antenatally and postnatally and given in a clear and consistent format. For some women, intense emotions of joy and elation coupled with feelings of extreme fatigue affected their ability to absorb information in the immediate postnatal period, whilst for others, the sheer volume of information was difficult to process.
In addition to a need for information, women also identified needs for both practical support and, especially in high-income countries, for psychosocial support. In a practical sense, women appreciated the support they received from family members but also valued support from healthcare providers, particularly in the immediate postpartum period, prior to hospital discharge, when they were trying to bond with their newborn and/or establish breastfeeding. Help with specific newborn-oriented tasks like nappy changing and bathing as well as tending to the newborn whilst the mothers recuperated, showered, or carried out chores, were highlighted and, in some instances, women felt disappointed when these needs were not recognised.
In many settings, women also highlighted the need for ongoing practical support once they returned home and, although this was often facilitated by family members, women also appreciated assistance from healthcare providers during the transition to motherhood. Usually this was a continuation of the advice received in hospital relating to infant feeding and development but, in uncommon circumstances, women received visits from associated agency workers to helped with domestic activities (shopping, cleaning, cooking) and these services were highly valued.
Many women experienced intense emotional peaks and troughs during the postpartum period ranging from elation to despair to overwhelming exhaustion. Women, particularly first-time mothers, discussed their fears, anxieties, and insecurities about becoming a mother and, for some, the pressure and responsibility of living up to some idealised version of a mother. Women wanted support from healthcare providers to help them to process and manage these difficult emotions and often expressed this in terms of a need for reassurance. In some contexts, particularly in high-income settings, where much of the published evidence comes from, women wanted to discuss the birth experience with a midwife who was present or have access to healthcare providers support if they felt their birth was challenging or traumatic.
In a broader sense, many women felt that their own care needs were overlooked or undervalued during the postpartum period. Whilst new mothers completely accepted and understood that the focus of postnatal care was on their infant, they nevertheless felt disappointed when unvoiced pleas for attention or recognition were ignored by healthcare providers.
Our findings also indicate that women placed great importance on their ability to build a relationship with care providers and this was particularly apparent in high-income settings. For some women this involved seeing the same healthcare provider at each postnatal contact, for others it meant being able to see the same midwife during the postnatal period as they saw antenatally, and for women who gave birth at home, the prospect of having the same midwife throughout their maternity journey played a significant role in their decision to opt for a homebirth. Where women were able to build these relationships, they were more likely to report ‘a sense of companionship’, ‘trust’ and ‘authenticity’, but in settings where continuity of healthcare models were not in place, women reported feeling ‘dissatisfied’, ‘like a number’ or even, ‘like an animal’.
For women in several contexts, interactions with healthcare providers sometimes became disrespectful and abusive. In high income settings, women indicated that healthcare providers could be rude or undermining and occasionally discriminatory during postnatal encounters, whilst in lower-income contexts women reported acts of rudeness, humiliation and, in rare cases, punishment by health providers.
Factors that influence women’s utilization of postnatal care are interlinked, and include access, quality, and social norms. Five review findings were identified: access and availability; physical and human resources; external influences; social norms; and experience of care. Many women recognised the specific challenges of the postnatal period and emphasised the need for emotional and psychosocial support in this time, in addition to clinical care.
Staffing and resources were important to women, although in low-resource settings, more emphasis was placed on poor physical infrastructure. In low- and middle-income countries, women further expressed that healthcare providers themselves often devalued postnatal care, contributing to their lack of utilization and sense of unpreparedness. Many studies from high-income countries highlighted women’s desire for more psychosocial and emotional support; yet, women in low income settings may not have been asked as directly about this challenge. Women also may not believe this is a role of the health system, or may not feel comfortable stating this as a vulnerability. These findings point to the need to strengthen comprehensive health care services, which can more fully address the holistic and ongoing needs of women and their families.
Many of the findings related to experience of care derived from high-income countries. Because of the number of included studies related to this topic were biased toward high income countries, this review finding should not be interpreted necessarily as women in low- and middle-income countries having positive experiences of care; evidence indicates that disrespectful practices are common globally [ 93 ]. This area is understudied in low- and middle-income countries and therefore it is difficult to draw robust conclusions. However, it is likely that women in settings with insufficient resources will more often refer to unhygienic conditions or lack of equipment as a more immediate priority than their experiences, and/or that they perceive less ability to change the situation than women in settings with more resources. A recent qualitative evidence review of studies in sub-Saharan Africa affirmed that aspects of respectful and disrespectful maternity care and women’s previous experiences of health care influenced their “decisions to access postnatal care services” [ 94 ]. The fact that many of the studies related to experience of care are from high-income settings may reflect the study authors’ biases and points to the need to study women and families’ experiences more holistically in low- and middle-income settings.
When situating this review within the context of other research [ 29 ], many similarities emerge in review findings across various phases of maternity care. From antenatal and intrapartum through postnatal care, women emphasised the need for information, continuity of care, adequate resources, and comprehensive and holistic support. Access and cost continue to be issues for many women, especially in low- and middle-income countries and in rural areas, but compared with intrapartum care, the incentive to overcome these challenges is further diminished with the devaluing of postnatal care and perception of low need for healthy women and their healthy infants. In the postnatal period, women’s access needs include when and how they can contact healthcare providers and for what purposes. Women greatly value continuity of care and flexible schedules for obtaining information and assistance. Infrastructure and health system resources play into both decisions about if and when to seek care, as well as the experience of care itself. This pattern and commonality across maternity care periods reflects the fact women may seek care from the same places and thus experience some of the same facilitators and challenges, but also emphasises women’s perception that maternity and the postnatal period are a continuum. The factors influencing postnatal care utilization may be different than other maternal and child health services for a number of reasons: postnatal may not be seen as important (especially if the woman and newborn are apparently healthy); during the postnatal care period, maternal and newborn needs may arise at the same time, adding to complexity of recognition and care seeking; and health care visits may take place in the home, unlike visits which must take place in a health facility. However, many of the same factors may be at play, including the recognition of need, the perception of quality, and the physical barriers such as cost and distance.
The review findings on postnatal care utilization largely conform with previous studies around what women want during this time period, as well as challenges related to access, health system quality, and experience of care. Our review builds on previous work in postnatal care utilization by explicitly including both women and newborns. The strengths of this review include a rigorous methodology, comprehensive search, very large database, wide search terms and concepts, and a diverse study team. Our review encompassed a geographically and linguistically diverse search, with a balance of papers from high, middle, and low-income countries, although the number of available studies from certain regions (e.g. Latin America and the Eastern Mediterranean) were limited. Despite the design of the search to be global, including a lack of language restrictions, we identified few papers from Australasia, Middle East, and South America.
Some potential limitations of the study include the limitations of the included papers themselves, especially the different prioritised topics studied in different regions of the world. Although the objectives of the included papers represented a range of topics, it is possible that certain areas, as well as certain topics in each region, are understudied. While we acknowledge that there may be context specific issues, we are bound by the content of the included studies and recognise that different questions may have been posed to participants in different contexts, depending on the nature of the research inquiry and the pre-existing beliefs of the research team members of those particular studies. Further, the World Bank Country Classifications are broad and group countries with very different profiles together. Country-specific terminology (such as the specific words used in a particular setting around health insurance or a certain cadre of support worker) may not have been captured.
As with other systematic reviews, there is a trade-off between speed and comprehensiveness and, while our use of sampling could limit our interpretation, our iterative process until reaching saturation increases confidence in our findings [ 95 , 96 ]. New studies have been published since the end of the search that were not included, however, the comprehensiveness and rigor of our search and analysis provides confidence in the findings.
Many papers identified in our search included the term “postnatal care” but in fact referred only to intrapartum care. It was difficult to disentangle experiences of postnatal care by time period as this was rarely disaggregated in studies. The differentiation was included in our extraction form, but some papers reported on when data were collected and others on the period the respondents were referring to with the latter often encompassing multiple time points post birth. More research is needed in distinguishing the needs during the immediate (e.g. pre-discharge from a health facility) and later postnatal periods.
The findings from this study have implications at the individual, family, health system, and policy levels, and interventions may be needed to address factors at each. Individual empowerment of women may be insufficient if her partner, family, or community have significant influence in healthcare decisions. The desire of women to have increased emotional and psychosocial support may or may not be best served by existing cadres of medical providers. Future research should explore who the optimal providers might be and what the scope (and burden) might be for each type of provider, including traditional birth attendants [ 97 ] and non-medical carers. The intervening time from the end of our search to completion of analysis included the emergence of a global pandemic, which has already had significant impact on postnatal experiences and care utilization [ 98 , 99 ]. Further areas of research include the impact of the pandemic on care utilization, increased anxiety and psychosocial support needs [ 100 ], and the role of digital and virtual care technologies [ 101 ].
There are clear steps which can be taken to improve the quality, experience, and uptake of care for women and newborns in the postnatal period. The value of PNC should be promoted as part of quality improvement, health worker training, and community mobilization. As much as possible, care should be provided in a continuous and coordinated manner, between health facilities, clinics, medical offices, communities, and households. At each level there must be sufficient staffing, resources, and infrastructure to provide high quality of care. Efforts should be taken to eliminate barriers to cost and transport, including illegal or unethical barriers such as bribes and other out-of-pocket or unanticipated costs for care, and all types of abuse and denial of care.
Postnatal care must be positioned as a high priority for both the woman and the newborn, much like antenatal and intrapartum care, and not seen as an optional service, or one only accessed in cases of emergencies. As a pre-requisite for increased utilization of postnatal care, quality must be improved [ 102 ]. The benefit of postnatal care for the mother and entire family may increase utilization, especially if services are available to improve emotional and psychosocial support. The implementation of standards for quality of care and respectful care must move beyond childbirth to ensure a positive experience of postnatal care for all women and their newborns.
Supporting information
S1 appendix. full search strategy..
https://doi.org/10.1371/journal.pone.0270264.s001
S2 Appendix. A priori framework.
https://doi.org/10.1371/journal.pone.0270264.s002
S1 Checklist. PRISMA 2020 checklist.
https://doi.org/10.1371/journal.pone.0270264.s003
Acknowledgments
The authors owe a debt of gratitude to Annie Portela at WHO for feedback on the analysis and manuscript. The authors also acknowledge the methodological inputs from the Cochrane EPOC group, specifically Simon Lewin, Claire Glenton, and Susan Munabi-Babigamura. Thank you to the many research assistants who worked on various stages of this review: Uktarsh Ojha, Clara Tam, Sakshi Jain, Sushama Sreedhara, Younghee Jung, Kate Cho, Lex Londino, Leonie Sawoh, and Prince Gyebi. Thanks to Kiriko Sasayama for assistance in translation of an included study.
- 1. WHO. WHO technical consultation on postpartum and postnatal care. Geneva: World Health Organization; 2010.
- 2. WHO. Maternal, Newborn, Child and Adolescent Health. In. Geneva: World Health Organization; 2013.
- 3. National Institute for Care and Health Excellence. Postnatal care quality standard [QS37]. London, UK; Published: 16 July 2013 Last updated: 20 April 2021.
- 4. American College of Obstetrics and Gynecology. Optimizing Postpartum Care. Committee Opinion. Number 736. May 2018.
- 5. WHO. WHO recommendations on maternal and newborn care for a positive postnatal experience. Geneva: World Health Organization; 2022.
- View Article
- PubMed/NCBI
- Google Scholar
- 28. 野口真貴子,; 高橋紀子,; 藤田和佳子,; 安積陽子,; 髙室典子,札幌市産後ケア事業を利用した女性の認識, Journal of Japan Academy of Midwifery 2018;32(2):178–189
- 52. Hindley J. Having a baby in Balsall Heath: women’s experiences and views of continuity and discontinuity of midwifery care in the mother-midwife relationship: a review of the findings from a report of a research project commissioned by ’Including Women’. Birmingham Community Empowerment Network, Birmingham. 2005.
- 99. Unicef. Coronavirus could reverse decades of progress toward eliminating preventable child deaths, agencies warn. Press release 9 September 2020, New York, NY. https://www.unicef.org.uk/press-releases/coronavirus-could-reverse-decades-of-progress-toward-eliminating-preventable-child-deaths-agencies-warn/
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier Sponsored Documents

A qualitative study of first time mothers’ experiences of postnatal social support from health professionals in England
Jenny mcleish.
a NIHR Policy Research Unit in Maternal and Neonatal Health and Care, National Perinatal Epidemiology Unit, University of Oxford, Old Road Campus, Headington, Oxford OX3 7LF, UK
Merryl Harvey
b School of Nursing and Midwifery, City South Campus, Birmingham City University, Westbourne Road, Birmingham B15 3TN, UK
Maggie Redshaw
Fiona alderdice.
Many women experience the transition to motherhood as stressful and find it challenging to cope, contributing to poor emotional wellbeing.
Postnatal social support from health professionals can support new mothers in coping with this transition, but their social support role during the postnatal period is poorly defined.
To explore how first time mothers in England experienced social support from health professionals involved in their postnatal care.
A qualitative descriptive study, theoretically informed by phenomenological social psychology, based on semi-structured, in-depth interviews with 32 mothers from diverse backgrounds. These were analysed using inductive thematic analysis, with themes subsequently mapped on to the four dimensional model of social support (emotional, appraisal, informational, practical).
There were nine themes connected to social support, with the strongest mapping to appraisal and informational support: for appraisal support, ‘Praise and validation’, ‘Criticism and undermining’, and ‘Made to feel powerless’; for informational support, ‘Is this normal?’, ‘Need for proactive information’, and ‘Confusion about postnatal care’; for emotional support, ‘Treated as an individual and heard’ and ‘Impersonal care and being ignored’; for practical support, ‘Enabling partners to provide practical support’.
Conclusions
Health professionals can play an important role postnatally in helping first time mothers to cope, develop confidence and to thrive, by taking every opportunity to give appropriate and personalised appraisal, informational and emotional social support alongside clinical care. Training and professional leadership may help to ensure that all health professionals are able and expected to offer the positive social support already offered by some.
Statement of significance
Becoming a mother for the first time can be stressful and some mothers struggle to cope.
What is already known
Social support from health professionals can help new mothers to cope with this transition, but their social support role is unclear.
What this paper adds
Appraisal and informational support from health professionals were very important for confidence and coping in first time mothers from varied socio-demographic backgrounds, whether or not they also had social support from a partner, family or friends. Emotional support was valued but had a more limited role. There was minimal practical support from health professionals.
1. Introduction
National guidance in England conceptualises the role of postnatal care to be primarily about support for the transition to parenthood [ 1 ]. Some women experience becoming a mother for the first time as a time of stress and poor emotional wellbeing, leading to psychological distress (including depression and anxiety) if they feel unable to cope effectively [ [2] , [3] , [4] ]. Social support – a person’s perception of the availability of others to provide emotional, psychological and material resources [ 5 ] – is an important factor in enabling a successful transition to motherhood [ 3 ]. Empirical research demonstrates that effective social support from health professionals can assist new mothers in coping with the stress of new parenthood by increasing their parenting confidence [ [6] , [7] , [8] ].
Social support is a multi-dimensional concept, commonly analysed as having four functional aspects — emotional, appraisal (affirmational), informational and practical [ 9 ]. Emotional support consists of words or actions that show love, liking, empathy, respect and trust, leading the recipient to believe that they are cared for, esteemed and valued [ 9 ]. Appraisal or affirmational support is the communication of information to enable positive self-evaluation, specifically affirmation of the rightness of what the recipient has done or said [ 9 ], and thus a key ingredient of constructive feedback [ 10 ]. Informational support is information provided to another at a time of stress [ 9 ], including information about a baby’s health and development [ 10 ]. Practical or instrumental support is the provision of tangible goods, services or aid [ 9 ], in this context specifically help with caring for the baby [ 10 ].
There are contrasting findings from different countries about the principal aspect of social support mothers report receiving from health professionals postnatally, for example practical or informational support on postnatal wards in Finland [ 11 ], and informational support in Ireland [ 8 ] and in the community in Finland [ 6 ]. This is complicated by different definitions, for example Salonen et al. [ 11 ] categorise ‘infant-care instructions’ as part of appraisal support and ‘directions for infant feeding’ as part of practical support, while Tarkka et al. [ 6 ] categorise information and advice on child development as part of affirmation support.
New mothers may receive social support from a variety of sources apart from health professionals, including their partner, parents, other family members, friends, neighbours, and community volunteers [ [6] , [7] , [8] , 12 ]. They may want and receive different aspects of support from informal and formal sources, so one does not replace the other [ 7 , 8 ]. Where the aspect of support received does not match the aspect of support desired, it may be ineffective or may increase rather than diminish stress [ 5 ]. In particular, where health professionals do not provide the emotional and affirmational support that new mothers want in the immediate postnatal period, interactions with health professionals may themselves become an additional source of stress instead of buffering the stress of new motherhood [ 7 ].
Mothers who give birth in England usually have access to free National Health Service postnatal care. This includes support from midwives and maternity support workers on a hospital postnatal ward or birth centre and in the community, a health visitor who takes over from the midwifery team as the lead practitioner approximately 10–14 days after birth, and a general practitioner who assesses the baby and mother at 6–8 weeks [ 1 ]. The social support role expected of health professionals in the postnatal period is poorly defined, but every interaction with a health professional in the postnatal period has a potential social support meaning for the mother, and being aware of these meanings these will enable health professionals to avoid harm and maximise their positive impact on maternal wellbeing [ 10 ]. In order to deepen understanding of their social support role and how it can contribute to maternal wellbeing in the transition to motherhood, this article explores how first time mothers in England experienced different aspects of social support from health professionals involved in their immediate postnatal care in the hospital or birth centre and in the community. It reports research that is part of a programme of work on first time mothers’ expectations and experiences of postnatal care that includes an online survey, antenatal interviews and a qualitative longitudinal study, which have been reported separately [ [13] , [14] , [15] ].
2. Participants, ethics and methods
2.1. study design.
This was a qualitative descriptive study [ 16 ], based on semi-structured, in-depth interviews, theoretically informed by phenomenological social psychology which focuses on participants’ lived experiences and subjective meanings of social interactions [ 17 ]. This ‘low-inference’ [ 16 ] design was chosen because the purpose was to explore participants’ own perceptions and thus to stay close to their accounts [ 17 ], while acknowledging the role of both participants’ understandings and the researchers’ interpretations in the production of knowledge [ 18 ]. Throughout the research process, the researchers worked with a reflexive awareness of their own perspectives on the transition to motherhood and postnatal care, based on professional knowledge and diverse personal experiences.
The University of Oxford Medical Sciences Inter-Divisional Research Ethics Committee (reference {"type":"entrez-nucleotide","attrs":{"text":"R52703","term_id":"814605"}} R52703 /RE001) approved the study.
2.2. Participants
The interviews reported in this paper were second (postnatal) interviews within a qualitative longitudinal study. Participants were women who had given birth to a live baby or babies in England in the past four months, and had previously taken part in a first (pregnancy) interview. The original recruitment criteria for the pregnancy interviews were: currently in the third trimester of pregnancy; aged 16 or over; planning to give birth in England; and had not given birth previously. Purposive maximum variation sampling [ 19 ] was used to recruit women with a range of socio-demographic characteristics, with a particular emphasis on seeking diversity in age, ethnicity, and socio- economic status using postcode quintiles [ 20 ]. Multiple recruitment strategies were used to include women who are less likely to participate in research [ 21 ] and in particular younger women and women living in more deprived areas, who are less likely to respond to maternity surveys [ 22 ]. These were: (1) an invitation at the end of an online survey about expectations of postnatal care, promoted on social media by parenting organisations; (2) an in-person invitation from a researcher to women attending three sessions of a young mothers’ antenatal group and two sessions of a free antenatal exercise class, each run by a community group in a different area of high deprivation; (3) an advertisement circulated on social media by a multiple birth charity. There was intentional over-recruitment at the stage of pregnancy interviews, to allow for the likelihood that some participants would drop out before the postnatal interviews and to ensure demographic variation. The only prior relationship between the researchers and the participants was the research relationship established during the pregnancy interviews.
Thirty two women took part in the postnatal interviews reported here, when their babies were 7–15 weeks old (median 11 weeks). A further eight women who had taken part in pregnancy interviews could not be contacted after birth. Background information about participants in postnatal interviews is shown in Table 1 .
Background informationabout participants.
2.3. Data collection
Data were collected through semi-structured qualitative interviews between January and July 2018. Topics included the help received from health professionals and others postnatally in hospital or birth centre and in the community, whether this matched what the mother felt she needed, and the impact the mother felt the postnatal care had on her. At the end of the first (pregnancy) interview, participants were asked for permission for the researcher to contact them approximately six weeks after their baby’s due date to arrange a second (postnatal) interview, either face-to-face at a time and place of their choice, or by telephone. Twenty nine postnatal interviews were by telephone and three were face-to-face, ranging in length from 21 to 56 min (mean 37.5 min). Informed consent to participate had been obtained before the pregnancy interview through a signed consent form if face-to-face, or given orally and recorded in writing when interviews were carried out by telephone; participants were reminded of this at the start of the postnatal interview and asked to confirm verbally whether they continued to consent. Participants were offered a shopping voucher worth £15 at the end of the interview, to thank them for their time. All interviews were carried out in English, although interpreting support was available if required. No one else (apart from babies) was present at the face-to-face interviews. Interviews were audio-recorded and fully professionally transcribed, with each participant being given an anonymous identifier beginning with PNC for ‘postnatal care’.
Data collection continued past the point where saturation was reached in these postnatal interviews (that is, participants were repeating what had been expressed by previous participants and there were no new codes or themes). Instead, all women who took part in pregnancy interviews were invited to take part in postnatal interviews. This was done to preserve the demographic variation of the initial sample, and to honour the commitment made to participants in the original participant information that they would be contributing to a qualitative longitudinal study through interviews before and after birth.
2.4. Data analysis
Inductive thematic analysis was carried out in parallel with ongoing data collection. Interview transcripts (which were the units of analysis) were checked against the audio-recordings, and read and reread for familiarity. Data were coded using NVIVO software. Codes were refined and combined as data collection continued, and themes describing manifest content were developed, using constant comparison to reconsider early analysis in the light of subsequent interviews. In order to explore the specific functional aspects of social support in postnatal interactions, themes were then mapped deductively onto the four dimensional model of social support [ 9 ], as widely used in social support research including Leahy-Warren’s concept analysis of social support for new mothers [ 10 ]. To increase the validity of the analysis, one researcher analysed all the transcripts and another analysed a subset; codes and themes were discussed and agreed. De-identified excerpts of interviews were selected to illustrate the findings.
3. Findings
There were 9 themes identified relevant to social support. Fig. 1 shows how these themes mapped on to the four functional aspects of social support. The strongest mapping was to appraisal and informational support. There were no differences identified according to socio-demographic background of mothers.

Themes and functional aspects of support interactions from professionals.
3.1. Appraisal support
There were three themes related to appraisal support: ‘Praise and reassurance’, ‘Criticism and undermining’, and ‘Made to feel powerless’.
3.1.1. Praise and validation
Many mothers described how, as first time mothers, they had no way to evaluate themselves: “I didn’t quite know what I was doing and what was right and what wasn’t right” (PNC110). They highlighted the importance of being reassured by midwives or health visitors that they were doing things ‘correctly’: “Praise, but not in a patronising way … ‘You’re talking to him, you’re engaging with him, he’s growing really well.’ … She just made me feel really good about what I was doing” (PNC060). Positive appraisal was felt to be much more meaningful when it came from a professional who was seen as objective, compared to friends and family who might be positive out of kindness: “And it’s different, when one professional says it, than when it’s like your mum or your friend says [insincere tone], ‘Oh you’re doing great!’” (PNC055). They were worried about being seen as “ a really over-exaggerating mother” (PNC105), so it was affirming to hear from professionals that having lots of questions was completely normal: “I expected for myself that I should know how to do all of this, and that was helpful at that stage to be told, ‘Nobody expects you to know what you’re doing, you haven’t done this before’” (PNC603). One mother commented that receiving only basic postnatal support had in itself felt like an affirmation of her parenting competence: “The fact that they haven’t felt that I’ve needed any extra help has given me confidence that I’m doing it right” (PNC224).
There were differences in the extent to which mothers believed that there was a ‘right’ way to carry out parenting tasks which they could master, and that health professionals were the experts in what this was. For example, one mother had asked midwives to watch her breastfeeding: “Just correct anything I’m doing wrong or [the baby] ’s doing wrong” (PNC055). Some others strongly preferred to be given non- directive advice and to make their own choices. Health professionals’ praise was often linked to how well the baby was growing and many mothers also accepted this as a reflection of their own performance as parents:
“Measurements and weight and things like that have all been spot on and I’ve always had nice compliments from midwives and the health visitor …You did get a lot of, ‘Well done, mum,’ pat on the back kind of thing. It was quite a confidence boost” (PNC158).
This carried the risk that if babies did not feed and gain weight as expected, mothers could feel that they were personally failing: “I was very tearful and upset about it, and I think that was because I had such strong ideas about what it was going to be like and the experience wasn’t matching up with that ” (PNC603).
3.1.2. Criticism and undermining
Many mothers reported encounters with professionals that disaffirmed their competence and undermined their confidence. They were given negative feedback in ways that left them feeling “like a little kid that had been told off” (PNC131), either through direct comments or body language such as eye rolling: “There’s quite a lot of pressure put on you in the hospital to be this perfect mum… They don’t quite say you’re being a terrible mother, but that’s how it felt … It makes you doubt everything that you’re doing a lot of the time ” (PNC250). This was particularly demoralising to mothers who were criticised when they were following a different health professional’s advice:
“She said, ‘What are you doing? You shouldn’t be doing that.’ We’d been told two days ago that that’s what we should be doing, it was then really confusing to be told something else, and she was quite abrupt in her manner and it was a bit of a knock to the confidence … It doesn’t make you feel very good” (PNC129).
Far from being reassured that their questions were welcomed and normal, some mothers described being made to foolish or incapable when they tried to get answers: “ It felt like I was being put back in my place with the sort of questions I was asking my health visitor” (PNC158). One mother had felt criticised and reprimanded in several encounters with professionals, and she reflected on the irony that they asked questions about maternal mental health but were lacking in self-awareness about the negative impact of their ordinary interactions with mothers:
“Why was she so angry at me about asking? … They concentrate so much on looking for signs of postnatal depression but don’t understand how they can just add to that, because then you’re left feeling like an idiot for asking a simple question” (PNC131).
Where a mother was struggling, it was very upsetting to feel she was being judged by someone who did not know the individual facts but was just giving generic advice, as in this example of a mother who was told by a health visitor at the six week check that combination feeding was not the best choice:
“She didn’t know the back story, she didn’t know us … On day 5 when we had the midwife it was like 90% formula, hardly any boob at all, and now it was about 75% breastfeeding and 25% formula, and it was something that we’d worked really hard at and it had taken a long time, and at a point I was really proud of, and then I just met her and she very quickly made it feel like it just wasn’t good enough.” (PNC194).
Another mother’s experience illustrates the sensitivity of new mothers to the possibility of implied criticism, when the health professional’s remark was intended to be affirming but sounded insincere because it was not related to the mother’s actual needs. This mother had just had an assisted birth:
“[The midwife] said, ‘Well, don’t feel disappointed with yourself’ … She was saying it more as like a platitude than a genuine, ‘You’ve done amazing.’ But I think because I wasn’t feeling disappointed or feeling like things had gone badly, her saying that then made me think, ‘Oh, maybe she’s thinking it didn’t go that well… actually maybe I should be disappointed’…I’m still upset about it” (PNC012).
3.1.3. Made to feel powerless
A few mothers reported that some health professionals had acted as though they had power over the mother’s and baby’s bodies that the mother had no right to challenge. Although this did not involve explicit criticism of the mothers (as in the previous subtheme), they had understood an implication that the mother was not seen as competent to make her own choices: “They think, ‘Oh yes, we’re God and you just trust us … We know, you don’t know anything’” (PNC702). Most of these situations related to professionals either administering medication or carrying out procedures without the mother’s informed consent: “Nobody told me that [my baby] had a chest X-ray or asked if that was okay” (PNC046). Others related to mothers being required to stay in hospital for extended periods without a clear explanation of why this was necessary, and feeling scared to disobey: “We weren’t allowed to leave the ward … I was getting to the point where I was just going to be like, ‘I’m just going to discharge myself,’ then I thought they might think I’m an unfit mother” (PNC250).
One mother had experienced multiple forms of disempowerment while in hospital, which had a dramatic impact on her emotional wellbeing, and affected her interpretation of routine aspects of postnatal care like electronic tagging:
“They had an electronic tag on [the baby]’s leg, which at first I thought was so they don’t steal your baby, and then I realised we can’t leave. So, I felt really trapped, like we were in prison … No one explained anything … They came and did a lumbar puncture at some point and didn’t tell me why. I thought [the baby] was going to be paralyzed … And people kept coming with more and more drugs for us... I didn’t want to be on antibiotics, and they didn’t give me an option. I wish I had known that I had that power [to give consent]… I ended up feeling like I’d failed [the baby], and at the beginning of his life story. I was so sad.” (PNC702).
3.2. Informational support
There were three themes related to informational support: ‘Is this normal? ’, ‘Need for proactive information’, and ‘Confusion about postnatal care’.
3.2.1. Is this normal?
Most mothers had checked with a professional about an aspect of their own health or their baby’s health or development that they were worried about, asking the question “Is this normal…?” Generally they had received the reassuring information that they needed, which also boosted positive self-appraisal. They strongly valued having ready access to professionals who could answer their questions:
“ I could always ring the postnatal ward in the hospital if there were any problems … Nearly every day that first week we had a midwife come, and that was really helpful and we were able to write down all our questions … I don’t think we would have coped nearly half as well without them.” (PNC110).
Most had received advice about feeding their babies, and a few commented that they had also received helpful information about practical aspects of baby care from an individual midwife or health visitor in response to specific challenges: “The best thing [the midwife] did for us was to give us advice that wasn’t ‘midwife advice’, that wasn’t necessarily about the weight of baby, the jaundice. It was more about, ‘Here’s something you can do so that you can get more sleep’” (PNC091).
Confidence in professional advice was seriously eroded for the many mothers who reported receiving conflicting information from health professionals, concerning issues such as how to breastfeed, expressing milk, swaddling, keeping babies warm, safe sleeping, self-care after a caesarean, oil for the baby’s skin, jaundice, tongue tie and vitamins. This made their advice appear to be anecdotal and unreliable:
“You would have a different midwife every eight hours and they had very different opinions of the clothes he should have on, how I should be feeding him, what I should be doing … if people are telling you different things, you don’t know who to listen to.” (PNC701).
A couple of mothers said they did not mind this inconsistency: “The plus side of that is you get two different opinions ” (PNC105). Diverse opinions opened space for a more confident mother to make her own choice, but she would also check the information against independent sources: “It seemed they had a favourite personal preference for doing things certain ways … it did mean that I could take what I wanted from whichever midwife… I definitely have continued to look stuff up myself as well” (PNC224).
Despite multiple experiences with advice that they found questionable, in principle most of the mothers wanted to get their information from health professionals or NHS- approved resources, believing that this was likely to be more reliable, up to date and evidence- based than information from other sources. Nonetheless all the mothers described how they sought out different kinds of postnatal information from different people. Even if they saw health professionals as approachable and accessible, they were selective in what they asked them, because they did not want to bother them with what might turn out to be unimportant questions: “I’ve relied more on my friends to ask them, because as much as [the health visitor] said you could call her any time, you kind of feel as though you can’t” (PNC192). Sometimes this was a strategic choice to prioritise professional information on specific topics: “ The health visitor it’s pretty much all about health, and then the other mums it’s about life” (PNC240). Other reasons for mothers’ reluctance to ask questions are explored in the next subtheme.
Very few mothers had turned to their own mothers as reliable sources of information: “Quite a lot of the advice has changed from when she had me” (PNC272). Generally they asked other recent mothers instead, in person, online or using group messaging. Some commented on the risks of relying on peers instead of professionals for information about ‘normality’, when those mothers might be trying to meet their own needs for affirmation either through boasting: “There’s a lot of competition, ‘My baby’s done this, my baby’s done that’” (PNC158), or competitive negativity: “I don’t tell them my baby sleeps so well, because I want to make friends. Everyone [at the baby group] really likes to complain and it’s like one- upmanship on how bad things are: ‘My baby only sleeps for two hours at a time!’ ‘Well my baby only sleeps for half an hour!’” (PNC105).
3.2.2. Need for proactive information
Although they valued the reassurance and advice they received, mothers identified a need for new mothers to be given important information in advance. Some had been given comprehensive written information: “ I got about 6000 leaflets from the health visitor when she first came, on every possible thing” ( PNC501). They questioned whether this format was useful to an overwhelmed new mother who would never have time to read it all to find what she needed, or was merely intended to tick the box that information had been given. What they wanted instead was proactive and concise information about key postnatal problems and typical scenarios for mother and baby, including crying, sleep and feeding:
“ I think they just try to cover themselves with lots of paper giving. At the time after you’ve given birth, you’re not going to be prepared to read all those leaflets, you’re struggling to keep your eyes open … A classic ‘this is normal’ guide would probably be helpful, and a solution page. So, ‘Is this normal to have this?’ and, ‘This is what you can do’” (PNC102).
There were several overlapping reasons for wanting health professionals to take responsibility for giving mothers relevant information, rather than waiting for mothers to ask. Some were inhibited from asking questions when they did not know the health professional, because of the risk of encountering someone judgmental: “It’s quite hard to ask someone questions without feeling bad or stupid in yourself when you’ve literally just met them” (PNC152). Some pointed out that first time mothers might find it hard to articulate a problem, because everything was unfamiliar: “I didn’t know what the question was. Because if I had just said that the baby is crying, that wouldn’t have been helpful ” (PNC704). This also applied to making the best use of routine contacts with health professionals: “She was asking if there was anything that I wanted to ask, and sometimes I find it a little bit difficult to know what I want to know” (PNC272). Another key reason for wanting to be given information before a problem arose was to prevent the considerable stress of worrying about the situation:
“We didn’t really sleep that first night because we were just watching to make sure [the baby] didn’t choke herself … the midwife on the triage [helpline] said, ‘Oh it just sounds like the mucus, it’s very normal,’ So that was good, but we were both left thinking, ‘If it’s so normal, why didn’t anyone tell you to expect it?’” (PNC055).
The biggest category of difficulties that mothers said they had not been warned about were related to feeding, particularly that latching on might be painful in the early days of breastfeeding, and the frequency with which a newborn might feed. Advance information about the reality of breastfeeding – “a bit more honesty” (PNC060) – would have prevented the loss of parenting confidence when mothers assumed they were to blame:
“Nobody had really explained cluster feeding and growth spurts, so I just felt like she wasn’t getting enough milk and I was failing her. If I’d have been better prepared for that, then I don’t think I’d have panicked as much or had crying sessions.” (PNC113).
Some commented that it would have been useful if antenatal classes gave much more time to postnatal life: “Talk about what to expect when you actually have a baby” (PNC152). By contrast a few noted that in the antenatal period it might be difficult to fully process information about postnatal life: “People did say to me, ‘Breastfeeding’s really hard.’ I wish someone had smacked me in the face and said, ‘BREASTFEEDING’S REALLY HARD!’ because they did tell me that, but I didn’t understand” (PNC091).
3.2.3. Confusion about postnatal care
Most of the mothers gave birth in hospital, and a repeated problem was the lack of effective orientation when they went to the postnatal ward afterwards: “You’re still in this wheelchair with your baby you’ve just given birth to and they wheel you into the room and they start to walk out the door. Both me and my husband were like, ‘Where are you going? You can’t just leave us! What do we do now?’” (PNC055). Lack of information about what to do in this unfamiliar situation had led to additional stress about the risk of unwittingly breaking hospital rules: “It was silly things, like I needed to go and get breakfast … and I was like, ‘Am I going to get in trouble for leaving [the baby] on his own?’” (PNC060). It had also caused confusion about how much support they could ask for from staff, leading some not to get the help they needed: “I didn’t really realise until after I’d left hospital … how much more help I could have asked for” (PNC046).
In the community, some mothers reported being given clear information about the postnatal care they could expect. Others had not: “No one’s contacted me. I don’t even know who to contact in the health visitor clinic. I don’t know if there is a health visitor clinic” (PNC131). They suggested that it would have been helpful to be given a list of standard postnatal care appointments, with their likely timing, location and purpose.
3.3. Emotional support
There were two themes related to emotional support: ‘Being treated as an individual and heard’ and ‘Being processed impersonally or not listened to.’
3.3.1. Being treated as an individual and heard
Some mothers had received personalised and responsive postnatal care which made them feel liked, valued and cared about:
“[Midwives] gave me 100% of their care. It wasn’t just their job that they’d done every day for the last however many years: I was really an individual with my own needs … Like you were the only person that mattered at that point … If I texted [the health visitor] to say that [the baby]’d put on weight she’d respond with a positive feedback … genuinely pleased with the milestones I had met.” (PNC270).
Where the mother had received care from the same midwife on more than one occasion (which applied to only a few), emotional support could be expressed in the context of a relationship: “[The midwife] was obviously pleased to see me and pleased to see [the baby] and see how well he was getting on … I remember that being particularly special” (PNC240). Emotional support could also be experienced during one-off interactions where the health professional demonstrated concern and regard by their demeanour: “I definitely felt [the midwife] was championing my needs and she genuinely cared” (PNC184). Mothers who believed that professionals had gone beyond their strict responsibility felt cared for and safe: “ The midwives were supposed to finish at the time that the baby went to hospital, but they made sure they called again just to make sure everything was okay” (PNC078).
Both in hospital and in the community, mothers felt emotionally supported when health professionals listened to them. Some mothers praised individual health professionals who had conveyed sincere interest in their wellbeing by giving them full attention, despite being very busy:
“She was rushing a bit, but when she asked how my mood was and I said, 'Actually I have been feeling a bit low,'... she really took time, and actually sitting down on the end of my bed… That made it feel really open and okay to talk.” (PNC603).
3.3.2. Being processed impersonally or not listened to
Many mothers had received inattentive, functional care, particularly on busy postnatal wards, which undermined feelings of safety:
“It just felt like you were being handed around like a rugby ball, chucked from player to player …They had so many things to do that something could easily be missed. That put you on tenterhooks for the entirety of your stay.” (PNC184).
This could also be very disappointing for women who had just gone through the life-changing experience of becoming a mother for the first time: “The after bit in hospital, I thought it would feel a bit more special… we were just shoved off to one side… I wouldn’t say that they really knew who we were” (PNC189).
These mothers mostly attributed emotionally unsupportive care to staff workloads: “They were just so exhausted and stretched that they didn’t get a chance to care as much as they could” (PNC189). It was nonetheless demoralising to be processed impersonally, for example through a confusing hospital discharge less than 6 h after birth:
“ When I literally was verging on 48 hours without any sleep … that lady then came in, she spoke really fast, and just basically went through this sheet of paper… I didn’t know what was going on … then it was like, ‘If you can pee, you can go home.’ So, I peed and I went home” (PNC152).
Mothers’ emotional wellbeing was also undermined when health professionals did not listen to them, for example when their concerns about their baby or their body were dismissed: “I told about 10 different people about my blood pressure, I told about 10 different people about him not feeding but … they weren’t having any of it … I felt awful” (PNC250). These new mothers needed their feelings to be acknowledged and accepted as they learned to cope with motherhood. A mother who was experiencing mental health difficulties, including flashbacks to a traumatic birth and hallucinations, described how professionals did not pay attention to her subjective experience of exhaustion and worry. Instead their attempts to normalise her experience felt to her like they were minimising its significance:
“These women who have been working in this industry for 20-plus years and think that you’re being a bit pathetic for being in tears …A lot of my mental health has been linked to my lack of sleep …They’ve just completely dismissed it… It’s almost like, ‘Every woman’s exhausted after they give birth, deal with it’” (PNC131).
3.4. Practical support
There was one theme: ‘Enabling partners to provide practical support’.
3.4.1. Enabling partners to provide practical support
Mothers had received very little direct practical support from health professionals. A couple said that staff had helped to calm their crying baby or bottlefeed a twin, but the great majority had not received any practical support at all. This had been particularly challenging and disappointing for mothers who were recovering from a caesarean: “On the one hand they’re like, ‘Try and rest,’ but then on the other hand they’re like, ‘You still need to do everything that you need to do for your baby’” (PNC194). Instead, mothers in this study had relied on their partners, family, friends, neighbours and communities for all their practical postnatal support in hospital and at home, particularly while they were recovering from birth interventions: “In those first couple of days when I couldn’t get up [my partner] did pretty much everything ” (PNC501).
Many mothers commented on the ways in which health professionals and the rules they operated could obstruct the practical support role of partners and family members on postnatal wards. Where they were not allowed to stay with the mother overnight, the absence of their practical support could motivate the mother to leave hospital sooner than she might want: “I didn’t want to spend another night in the hospital on my own without my husband … just having the help at night time” (PNC105). Where partners were allowed to stay with the mother all the time, the postnatal ward was not a hospitable environment for them, as most had to sleep on a chair or on the floor, and were not allowed to eat the food or use the shower. This seemed to mothers to undervalue their role and create a barrier to their ability to provide this essential practical support: “ At the birth centre, the person attending, they also are given are a comfortable place to take rest, because that person has to take care of the new mother, right? At the hospital this was completely missing . This was very strange” (PNC704). As a result some partners felt they had to go home overnight to sleep, even though they were allowed to stay. One mother described how her partner was actively made to feel unwelcome by the way staff enforced the rules:
“He had been awake with me for over 24 hours … then on the ward the partners weren’t allowed to lay down anywhere. Even if I was up with the baby and happy to be up with the baby, and he was on the bed to have a 10 minute nap or something, they’d come and wake him up and shoo him off again and tell him not to do that.” (PNC250).
4. Discussion
Previous research has identified that the majority of mothers are satisfied with their postnatal care in England, but a substantial minority report problems with hospital postnatal care such as insufficient and inconsistent information, poor quality interactions with staff including derogatory comments, and lack of respect for choices [ 23 , 24 ]. Similar problems have been reported internationally and about postnatal care in the community [ [25] , [26] , [27] , [28] , [29] , [30] , [31] ]. Walker et al. [ 32 ] argue from the results of their qualitative systematic review that the key to supporting a successful transition to motherhood is the ability of women and midwives to connect, and that this can best be achieved through postnatal midwifery home care. This study deepens understanding of the ways in which the social support aspects of postnatal care in any setting can be an opportunity to enhance first time mothers’ confidence and skills, or alternatively can undermine mothers’ ability to cope and thrive in the transition to parenthood. It highlights the value that first time mothers from a range of demographics attach to effective postnatal social support from health professionals, even if they also have social support from family and friends; and emphasises the need for health professionals to use every postnatal contact and conversation as an opportunity to offer care in ways that are not only kind and respectful [ 1 ], but are also socially supportive.
The strongest themes in this study related to appraisal and informational support from health professionals, and these are the aspects of social support identified by Leahy-Warren [ 8 ] as having the greatest salience for maternal confidence. Building up mothers’ parenting confidence through timely information and positive feedback assists them to cope with the stress of having a new baby, by both helping them to deal with stressors effectively and reassuring them that they can rise to this challenge successfully [ 5 ]. The varied experiences of mothers in this study, with some receiving significant social support within postnatal interactions and others very little, reflect the uneven provision of postnatal care within overstretched services in England [ 33 ].
Almost all mothers, from a range of socio-demographic backgrounds, described the beneficial impact on their parenting confidence of having their actions affirmed and validated by health professionals, even if they also had this affirmation from other sources. They also described the negative impact of feeling judged, criticised, or actively disempowered, and some were acutely sensitive to perceived as well as actual criticism, including where an attempt at affirmation was not related to the mother’s own needs. The importance of affirmation in the context of breastfeeding has previously been highlighted by Schmied et al. [ 26 ]. However, the fact that health professionals often linked their praise to successful breastfeeding or a baby growing well could undermine the confidence of mothers where this was not successful, reinforcing their feelings of grief and failure [ 34 , 35 ]. The powerful subjective significance to mothers of interactions being affirming or disaffirming echoes the findings of Razurel et al. [ 7 ], who found that unhelpful interactions with caregivers were the single greatest source of stress in the immediate postnatal period, and Aston et al. [ 36 ] and Wilkins [ 37 ], who described the sensitivity needed to overcome power differentials between ‘expert’ health professionals and new mothers afraid of being judged by experts as not ‘doing it right’.
New mothers are frequently reported to be overwhelmed by the sheer amount of advice available to them from online and offline sources, and to find it challenging to navigate its reliability [ [38] , [39] , [40] ]. The fact that very few mothers in this study relied on their own mothers for postnatal information represents a significant social shift from the patterns identified by Leahy-Warren [ 8 ]. They felt they had to ration the questions that they asked professionals and turned primarily to other mothers to fill the information gaps, while recognising that informal sources of information might be unreliable or embody unhelpful ideas about ‘normality’ [ 38 ]. Nevertheless, despite the perennial problem of inconsistent professional advice [ 23 ], mothers in this study generally wanted to get their information from health professionals or resources recommended by health professionals.
In theory, all new mothers in England should have access to information and advice about self-care and baby care [ 1 ], and many mothers described positive experiences of seeking answers to their repeated question “Is this normal? ” However they also questioned the way in which they had been either given so much written information that they could not find what they needed, or given very little and invited to ask for more. Like the mothers interviewed by Wilkins [ 37 ], they suggested that new mothers should proactively be given concise important information about common problems, solutions and reassurances, and clear information about postnatal care itself. This would alleviate unnecessary anxiety, support mothers who felt too vulnerable to expose their lack of knowledge to potentially judgemental health professionals, and protect mothers from the fear of being reprimanded for failing to navigate the unfamiliar system correctly. Although the need for more realistic antenatal preparation for the practical realities of parenthood has been identified many times [ 41 ], this research suggests that effective antenatal preparation should sit alongside information available postnatally in a form that new mothers find useful.
Schmied et al. [ 26 ], in their metasynthesis of breastfeeding support, distinguish between a ‘facilitative style’ where professionals give realistic, accurate, and proactive information that can both pre-empt and respond to worries, and a ‘reductionist approach’ where professionals give standard information didactically and disregarding the mother’s own views or needs. Other researchers have emphasised how the way in which information is given to new mothers is as important as its content [ 38 , 42 ]. This study reinforces the importance of a facilitative and individualised style across all aspects of postnatal information, even where the mother herself believes that there is a ‘right’ way to look after her baby and that she needs guidance from experts on how to do this.
The current policy aim in England is for most women to have continuity of midwifery carer through the antenatal, intrapartum and postnatal periods, but fewer than one in ten women currently have postnatal care from at least one midwife who was involved in both their antenatal and intrapartum care [ 24 ]. Mothers in this study described how emotional support could occur in the context of an ongoing relationship in the few cases where that existed, but it could also occur when one-off interactions were managed skilfully by a health professional. Kind, respectful, empathetic interactions had made them feel safe, valued and cared for, while superficial, rushed interactions had made them feel insignificant and demoralised at a life-changing time. For mothers who were experiencing difficulties, there could be a fine line between having their problems normalised by professionals and feeling that they had been minimised, as also reported by Razurel et al. [ 7 ]. This underscores the importance of listening carefully to mothers’ concerns and responding sensitively.
Although three quarters of mothers surveyed by the Care Quality Commission in 2019 reported that their partner or another companion was able to stay with them all the time [ 24 ], this study illustrates how the policy intention could be undermined if there were no facilities to accommodate partners and companions, or if they were made to feel unwelcome, leading some mothers to leave the postnatal ward sooner than they wanted in order to have the practical support which was not available from professionals.
4.1. Strengths and limitations
It was a strength of this research that it included 32 women from across England and from a variety of socio-demographic backgrounds, enabling a thematic analysis of experiences that were not linked to a single institution or area or any individual demographic group. It was a limitation that some of the initial socio-demographic diversity was lost between recruitment in pregnancy and the postnatal interviews reported here, so these participants were older, less ethnically diverse and less likely to live in disadvantaged areas than the original sample.
5. Conclusions
First time mothers felt uncertain and sometimes overwhelmed by the intensity of the unfamiliar challenges of becoming a mother. They described how they wanted professionals to affirm their competence as mothers by giving positive feedback, to proactively give them necessary and reliable information in a useable format, to reassure them that their baby was behaving normally, to treat them with compassion while acknowledging the magnitude of the life transition, and to enable their partner or family member to provide effective practical support. Health professionals working in postnatal care can play an important role in helping first time mothers to cope with stress of becoming a parent and to thrive, by taking every opportunity to give appropriate and personalised appraisal, informational and emotional social support alongside clinical or functional care. Training and professional leadership may help to ensure that all health professionals are able and expected to offer the positive social support already offered by some. Further research could investigate the formats of information that postnatal mothers find most useful.
Authors’ agreement
We confirm that:
- • The article is our original work.
- • The article has not received prior publication and is not under consideration for publication elsewhere.
- • All authors have seen and approved the manuscript being submitted.
- • The authors abide by the copyright terms and conditions of Elsevier and the Australian College of Midwives.
This research is funded by the National Institute for Health Research (NIHR) Policy Research Programme, conducted through the Policy Research Unit in Maternal and Neonatal Health and Care, PR-PRU-1217-21202. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. The funders did not have any role in the study.

Ethical statement
The University of Oxford Medical Sciences Inter-Divisional Research Ethics Committee (reference {"type":"entrez-nucleotide","attrs":{"text":"R52703","term_id":"814605"}} R52703 /RE001) approved the study on 8th September 2017. Participants consented to data collection and for their experiences to be used in reports or publications with no details or other information being published that could identify them. Following the consent process the individual qualitative interview transcripts will not be made publicly available.
Conflict of interest
None declared.
CRediT authorship contribution statement
Jenny McLeish: Methodology, Investigation, Formal analysis, Writing - original draft. Merryl Harvey: Methodology, Investigation, Writing - review & editing. Maggie Redshaw: Conceptualization, Methodology, Writing - review & editing. Fiona Alderdice: Conceptualization, Methodology, Formal analysis, Writing - review & editing.
Acknowledgements
Thank you to all the women who participated in this study and the organisations and individuals who facilitated the research: NCT, Babycentre, TAMBA, Island House Community Parents, Lucy November.
Postnatal care - current issues and future challenges
Affiliations.
- 1 School of Nursing and Midwifery, University of Western Sydney, Building EBLG Room 33, Parramatta South Campus, Sydney, Australia. Electronic address: [email protected].
- 2 Kings College London Florence Nightingale School of Nursing and Midwifery, Division of Women׳s Health, Room 4.32, James Clerk Maxwell Building, 57 Waterloo Road, London SE1 8WA, UK.
- PMID: 24856096
- DOI: 10.1016/j.midw.2014.05.001
- Maternal-Child Health Services / trends*
- Midwifery / trends*
- Postnatal Care / trends*
- United Kingdom
A Postnatal Depression Case Study – What is it Really Like?

By: Joshua/Yoon Hernandez
by Natalie Trice
It’s not uncommon to experience ‘baby blues’ after giving birth. For some women this goes away as quickly as it arrived. For others, it develops into full-blown postnatal depression (PND) , a condition that is often hidden but can have a significant impact on you and your family.
NHS figures show postnatal depression affecting one in ten mothers, but this figure only includes those who seek help. Stigma still exists around not fitting the mould of the happy new mum, leaving many to suffer in silence, blaming themselves and worrying that if someone finds out they feel are depressed their child might be taken away.
What it is really like to be a sufferer of postnatal depression? This is Natalie’s story.
My Struggle with Postnatal depression
Having suffered from anxiety in the past due too a high-pressured career , being a candidate for PND shouldn’t have really been a surprise.
But I was so focused on getting things right with the birth of my first son I just didn’t entertain the idea that I wouldn’t be able to cope.
And perhaps I desperately wanted to believe in the image I presented to the outside world of the woman who had it all. The sort who had an amazing wedding, moved out of London to a gorgeous house, had no troubles getting pregnant, and as a freelancer with a supportive husband could start maternity leave when she wanted with no pressure to go back until she was ready.
My son was nearly two weeks overdue. It ended up a quick labour to produce a big baby, and was traumatic for both he and I. But he was a beautiful little boy and there was certainly no issue with bonding, so I told myself everything was perfect.

But if I am honest, from day one I knew something wasn’t quite right.

By: Frédérique Voisin-Demery
Once my husband was back at work I felt completely overwhelmed by the responsibility for another life , and became very anxious that I’d do something wrong. I sterilised everything obsessively, I even made visitors use hand gel!
Then there were my endless worries about whether I was getting feeds right , and when the correct time would be to help him make his first new friends. Which would send me into a panic that he might pick up a bug, which would, I told myself, be all my fault.
And the exhaustion! I had never know such tiredness.
I put on my bravest face, or, as a good friend calls it, my “I’m fine” mask.
But I’d see the other women on the high street with their bugaboos and smiles, and I just felt like I was in another world altogether. More and more I’d just sit at home and cry, if I’m honest, wishing for my old life back. I’d leave home less and less, becoming more and more reclusive, some days not even opening the curtains.
I was told more than once to pull myself together, to remember that children are a gift. I knew that. But being reminded of it did nothing. The reality is that being a new mum can be hard; having depression is miserable and when the two collide life becomes a frightening haze.
And oh, the guilt and shame I felt for not being able to snap out of it! I’d beat myself up constantly. I was a senior global PR manager, who had juggled staff and budgets, but when it came to being a mum I couldn’t hack it? I told myself my son deserved better than me.
As the weeks went past I found it harder and harder to keep it all together. One morning, after a night with very little sleep due to my son having colic, I broke down and told my husband he couldn’t go to work that day as I couldn’t cope.
I was lucky; my husband was amazing. An emergency appointment to see our GP was quickly arranged. And while I admit in the back of my mind I thought she would take my child away and lock me up in a mad house, opening up was the best decision I made. The doctor was kind and supportive, her door was open 24/7, and plans were put into place.
I was put on anti-depressants, which I felt a bit nervous about. But I knew in my heart it was the right move for me at the time.

By: zoetnet
The best thing was just to suddenly feel so supported. A local health visitor popped by three times a week and my husband would come home for lunch.
And there was a local postnatal depression support group and I would attend once a week, which was both helpful and inspiring. I would sit in a room of people who were experiencing what I was experiencing, just listening and talking. We were all in the same boat and no one made me feel like I was being self indulgent or selfish.
The realisation that I wasn’t a bad, mad mother, just ill, definitely took some of the pressure away.
Bit by bit, day by day, I started to relax and feel the anxiety lifting. Instead of just sitting by my baby’s cot while he slept making sure he was breathing, I was having a power nap myself. Out came my pre-pregnancy clothes, even some make-up. I would open the curtains and get out of the house each day, just to the corner shop to start with. A big step for me was starting to pop to the local Costa without panicking he’d pick up germs from other customers.
After about six weeks I felt as if I was back on track and enjoying my new life as a mummy.
Of course it’s not cut and dried. I still sometimes have panicky thoughts. Even writing this postnatal depression case study I feel a bit pathetic that I couldn’t cope with a tiny baby and that I failed him. But now I know those are just thoughts, not the truth. I can see nowadays that I was far too hard on myself back then. I wanted to the perfect mum and wife with a well-behaved baby who slept throw the night.
Eight years on and I have two very happy little boys who I adore and life is good.
If I could go back I would be easier on myself. I would tell myself to relax and trust my own instincts.
And my advice if you are a partner, relative or friend of a mum who you think may have postnatal depression? Reassure her that it’s normal to feel this way. Getting her to relax and open up is really important. And often it is the simple things that can really help such as:
- Help her to organise her time, and work out what needs doing now, and what can wait – this is key as many women feel like they have to do it all now and be perfect
- Cook dinner for her or make some meals for the freezer
- Encourage her to rest as much as possible
- Tell her what a great mum she is and how well she is doing
- Offer to look after the baby so she can have a bath, go out for a manicure or simply get some rest
- In the early days help her to set boundaries over too many visitors, asking well-meaning people to call or text rather than turning up on the doorstep
- Listen to her and let her cry if she needs to
- Let her know you are there for her, no matter what
- Give her space so she can take care of herself and process how she is feeling and what help she needs
- Get her to talk to her health visitor or GP and seek professional help if it is all too much

Natalie Trice is a freelance writer and blogger who lives in Buckinghamshire with her husband, two sons, cat and dog. She writes a regular feature column for Families Magazine.
Would you like to share you experience of postnatal depression? Or have a question you are burning to ask about PND? Do so below, we love hearing from you.

Your email address will not be published. Required fields are marked *
Currently you have JavaScript disabled. In order to post comments, please make sure JavaScript and Cookies are enabled, and reload the page. Click here for instructions on how to enable JavaScript in your browser.
Open Popup Form
ASK US A QUESTION

ARE YOU A JOURNALIST WRITING ABOUT THIS TOPIC?
If you are a journalist writing about this subject, do get in touch - we may be able to comment or provide a pull quote from a professional therapist.
Yes, I am a journalist Click here to confirm you are a journalist
Related Posts
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

- Front Matter
- Contributors
- Acknowledgments
- Introduction
- How to Approach Clinical Problems

Case Files: High-Risk Obstetrics
Author(s): Eugene C. Toy; Edward R. Yeomans; Linda Fonseca; Joseph M. Ernest
- 1 Physiologic Adaptation to Pregnancy
- 2 First-Trimester Screening
- 3 Second-Trimester Serum Screening
- 4 Vaginal Breech Delivery
- 5 VBAC—The "Approach to Counseling and Management"
- 6 Cesarean Section Leading to Cesarean Hysterectomy
- 7 Abruption/Dead Fetus
- 8 Placenta Accreta
- 9 Puerperal Vulvovaginal Hematoma
- 10 Postpartum Hemorrhage
- 11 HIV Exposure During Pregnancy
- 12 Congenital Infection of the Neonate
- 13 Hepatitis A During Pregnancy
- 14 Acute Fatty Liver of Pregnancy
- 15 Eclampsia
- 16 HELLP Syndrome
- 17 Severe Preeclampsia
- 18 Epilepsy in Pregnancy
- 19 Pregestational Diabetes
- 20 Gestational Diabetes
- 21 Hyperthyroidism due to Graves Disease
- 22 Acute Kidney Injury
- 23 Thrombophilia
- 24 Intrauterine Growth Restriction (IUGR)
- 25 Kell Alloimmunization
- 26 Shoulder Dystocia
- 27 Stillbirth
- 28 Breast Cancer in Pregnancy
- 29 Depression in Pregnancy
- 30 Operative Vaginal (Forceps) Delivery for Fetal Indication
- 31 Sickle Cell Disease
- 32 Idiopathic Thrombocytopenic Purpura
- 33 Ventilator Management
- 34 Septic Shock
- 35 Anaphylactic Reaction to Penicillin
- 36 Asthma in Pregnancy
- 37 Preeclampsia in a Patient with SLE
- 38 Peripartum Cardiomyopathy
- 39 Twin-Twin Transfusion
- 40 Idiopathic Preterm Labor
- 41 Preterm Premature Rupture of Membranes (PPROM)
- 42 Adnexal Masses in Pregnancy
- 43 Polyhydramnios
- 44 Nonimmune Hydrops
- Abruption/Dead Fetus
- Acute Fatty Liver of Pregnancy
- Acute Kidney Injury
- Adnexal Masses in Pregnancy
- Anaphylactic Reaction to Penicillin
- Asthma in Pregnancy
- Breast Cancer in Pregnancy
- Cesarean Section Leading to Cesarean Hysterectomy
- Congenital Infection of the Neonate
- Depression in Pregnancy
- Epilepsy in Pregnancy
- First-Trimester Screening
- Gestational Diabetes
- HELLP Syndrome
- Hepatitis A During Pregnancy
- HIV Exposure During Pregnancy
- Hyperthyroidism due to Graves Disease
- Idiopathic Preterm Labor
- Idiopathic Thrombocytopenic Purpura
- Intrauterine Growth Restriction (IUGR)
- Kell Alloimmunization
- Nonimmune Hydrops
- Operative Vaginal (Forceps) Delivery for Fetal Indication
- Peripartum Cardiomyopathy
- Physiologic Adaptation to Pregnancy
- Placenta Accreta
- Polyhydramnios
- Postpartum Hemorrhage
- Preeclampsia in a Patient with SLE
- Pregestational Diabetes
- Preterm Premature Rupture of Membranes (PPROM)
- Puerperal Vulvovaginal Hematoma
- Second-Trimester Serum Screening
- Septic Shock
- Severe Preeclampsia
- Shoulder Dystocia
- Sickle Cell Disease
- Thrombophilia
- Twin-Twin Transfusion
- Vaginal Breech Delivery
- VBAC—The "Approach to Counseling and Management"
- Ventilator Management
- Research article
- Open access
- Published: 27 December 2018
Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community- based cross-sectional study
- Kihinetu Gelaye Wudineh 1 ,
- Azezu Asres Nigusie 1 ,
- Shumiye Shiferaw Gesese 1 ,
- Azimeraw Arega Tesu 1 &
- Fentahun Yenealem Beyene 1
BMC Pregnancy and Childbirth volume 18 , Article number: 508 ( 2018 ) Cite this article
54k Accesses
42 Citations
Metrics details
A Correction to this article was published on 19 May 2020
This article has been updated
World health organization stated that postnatal care is defined as a care given to the mother and her newborn baby immediately after the birth of the placenta and for the first six weeks of life. Majority of maternal and neonatal deaths occur during childbirth and the postpartum period. Scaling up of maternal and newborn health through proper postnatal care services is the best way of reducing maternal and neonatal mortality.
A community based cross sectional study was conducted among 588 mothers who gave birth in the last one year from March 1–21; 2017. Systematic random sampling technique was used to select study participants. A pre-tested and structured questionnaire was used to collect the data. Data was entered in EPI info version 7 and analyzed using SPSS version 21. Logistic regression was applied to identify association between explanatory variables and the outcome variable. An adjusted odds ratio with 95% confidence interval and p -value less than 0.05 was computed to determine the level of significance.
A total of 588 participants were included in the analysis which was the response rate of 100%.
The prevalence of postnatal care service utilization in this study was 57.5%.
Maternal educational status of secondary school and above (AOR = 3.29, 95%CI: 1.94–5.57), family monthly income of above 1500 ETB (AOR = 2.85, 95%CI: 1.21–6.68), alive birth outcome of last pregnancy (AOR = 5.70, 95%CI: 1.53–21.216), planned and supported last pregnancy (AOR = 3.94, 95%CI: 1.72–9.01) and institutional delivery of last pregnancy (AOR = 3.08, 95%CI: 1.24–7.68) were positively associated with PNC service utilization.
This study showed that the overall utilization of PNC service in Debretabour town is low. Mothers’ education, monthly income, last pregnancy birth outcome, wantedness of the pregnancy and place of delivery were significantly associated with postnatal care service utilization. To enhance PNC service utilization and reduce maternal and neonatal mortality women should obtain appropriate education. Furthermore all pregnant women should give birth in the health facilities.
Peer Review reports
The world Health Organization (WHO) stated that postnatal care (PNC) is defined as a care given to the mother and her newborn baby immediately after the birth of the placenta and for the first 42 days of life [ 1 ].
Majority of maternal and neonatal deaths occur during childbirth and postnatal period [ 2 , 3 ].
The estimated maternal mortality ratio (MMR) declined across all MDG regions between 19,990 and 2015, although the magnitude of reduction varies substantially between regions [ 4 ].
According to 2015, the two regions with highest MMR are sub-Saharan Africa and Oceania. The MMR in developing regions was 19 times higher than in developed regions. Sub-Saharan Africa has the highest regional MMR (546) per 100,000 live births [ 4 ].
The 2016 Ethiopian Demographic and Health Survey (EDHS) showed that the MMR was 412 deaths per 100,000 live births. In other words for every 1000 live births about four women (4.12) died during pregnancy, childbirth or within six weeks of childbirth.
According to EDHS 2016, only 17% of women receive at least one postnatal care service from a health institution in the first 48 h after birth and Amhara region is the 3rd least region in postnatal care service utilization [ 5 ].
Utilization of maternal health care services decreases maternal and child mortality.
Postnatal care particularly prevents most maternal and child morbidity and mortality. Care given in the postpartum period assists health care providers to detect post- delivery problems and to give treatments timely [ 3 , 6 ]. Shortage of care during this period could result in ill health, disabilities and deaths [ 3 ]. Around 65% of maternal deaths and 75% of newborn deaths occur in the first seven days after birth, and around half of these deaths occur in the first one day. A newborn is about 500 times more likely to die in the first day of life than at one month of age [ 7 ].
Appropriate postnatal care could save up to 60,000 newborn lives a year. In Ethiopia, if all new born receives appropriate postnatal care in the recommended time, neonatal mortality could be reduced by 10–27% [ 7 ].
Globally, there were an estimated 303,000 maternal deaths from complications related to pregnancy and childbirth in 2015 which is a decline of 43% from 1990. Majority of the maternal deaths occur in developing regions. It accounts for approximately 99% of the global maternal deaths in 2015, with Sub- Saharan Africa alone accounting for roughly 66% followed by southern Asia 22% [ 4 ].
Less attention was given for postnatal period in developing countries; women and their newborns don’t receive postnatal care services from a skilled birth attendant during the first days after childbirth [ 2 ].
Great majority of maternal and neonatal deaths occur during the first 2 days after childbirth. Hence, postnatal care for the women and the child is important in detecting and treating complications occur during the delivery as well as providing information for the mother on her and her newborn health [ 5 ].
To assess the extent of postnatal care utilization, EDHS 2016 asked respondents for their last birth in the 2 years preceding the survey, whether they had received a check up after delivery and the timing of the first checkup and it was found that the level of postnatal care coverage was low in Ethiopia. Only 17% of women reported having received a PNC checkup in the first 2 days after birth. In the case of the Amhara region percentage of women with a postnatal checkup in the first two days after birth was18.4% [ 5 ].
Study area and period
This study was conducted from March 1st to 21th, 2017, at Debretabour town. Debretabour, the city of South Gondar zone is found in the northern part of Amhara regional state 98 Kilometers from Bahirdar, the main city of Amhara regional state and 666 Kilometers away from Addis Ababa, the capital city of Ethiopia. According to the 2015 population projection estimate, there were 55,596 residents and around half of them were females. There are 3 health centers, 4 health posts, and 1 general hospital providing postnatal care services in the town.
Study design and population
A quantitative research involving community based cross-sectional study was conducted among randomly selected reproductive age group of mothers who gave birth in the past one year preceding the data collection period.
Mothers who lived less than six months in the study area at the time of interview and who had communication problem were excluded from the study.
Sample size calculation and sampling procedure
The single population proportion formula was used to calculate the sample size considering the following assumptions: proportion of women using postnatal care services 33.5% [ 8 ], 95% confidence level, 4% margin of error (absolute level of precision).
Adding 10% non-response rate, a total sample size of 588 women were included.
Debretabour town intentionally was selected as a study site by considering the health status of women in the town and lack of previous researches related to maternal health care services. Systematic sampling technique was used to select the study units. From the four kebeles all kebeles were selected. The calculated sample size was distributed across the four kebeles proportionally to the size of the households in each kebele. Then the proportion of eligible mothers those who gave birth in the last one year prior to this study were identified. Based on this assumption the available data from registry of the local health extension workers they recently conducted the survey for immunization program was used. The sampling interval of households in each kebele was determined by dividing the total number of households to the allocated sample size. The initial household to be interviewed was selected randomly from the kebele house number registry using a number between 1 and the sample interval. The subsequent household to be included in the study was identified systematically through house-to-house visit. For households with more than one eligible woman, interview was done for one of the mothers using simple random sampling technique. Revisits of two to three times were made in case where eligible respondents were not available at the time of the survey by asking the neighbors whether an eligible women in that house was present or not, after all they were considered as non-respondents.
Data collection tools and procedures
Data was collected by face to face interview using a structured and pre-tested questionnaire. The questionnaire first prepared in English and translated to Amharic, and then back to English. Four 3rd year diploma midwife students were used to collect data. Two BSC midwives were assigned to supervise the data collection process. Both the data collectors and supervisors were given one day training before the actual work about the aim of study, procedures and collection techniques going through the questionnaires question by question, art of interviewing and ways of collecting the data.
Data quality control
The quality of data was assured by proper designing and pre-testing of the questionnaires in one of the Kebeles other than Debretabour, in Woreta town on 30 participants. Every day after data collection, questionnaires were reviewed and checked for completeness by the supervisor and principal investigator and the necessary feedback was offered to data collectors in the next morning and before ending all session incomplete questions were completed using precoded for controlling errors during data analysis.
Data processing and analysis
The entire questionnaire were checked, coded and entered into EPI Info version 7 and exported to SPSS version 21 software. For analysis descriptive statistical procedures were utilized. Descriptive statistics like percentage, mean and standard deviation were used for the presentation of demographic data and magnitude of post natal care service utilization. Tables and graphs were also used for data presentation.
Binary logistic regression was used to identify factors associated with PNC service utilization on mothers. Variables with P -value less than or equal to 0.2 were selected in to multiple logistic regression models for controlling the possible effect of confounders and finally variables which had independent association with PNC service utilization were identified on the basis of AOR, with 95%CI and p -value less than 0.05.
Ethical consideration
Ethical clearance was obtained from institutional Ethical Committee of Bahirdar University. Formal letter of cooperation was written for Regional Health Bureau, Debretabour health office and respective kebeles and permission was obtained. Written informed consent was obtained from each study subjects, each respondent was informed about the objective of the study that it contribute to improve maternal health. Any mother who was not willing to participate in the study has not been forced to participate. They were also informed that all data obtained from them would be kept confidential by using codes instead of any personal identifiers and is meant only for the purpose of the study. Health education on postnatal care service and related complication and other information was given for the participants during interview.
Socio demographic characteristics of the participants
The total of 588 women participated in the study making the overall response rate 100%. More than half 330(56.1%) of the respondents were in the age group 20–29 with the mean ± SD 27.35 ± 5.48 years. Five hundred twenty one (88.6%) of them were married and 564(95.9%) of them were Orthodox Christian followers. Nearly one-six, 102(17.3%) of the respondents were unable to read and write and 260(44.2%) of them attend secondary school and above. Concerning their husbands’ educational status, 337(57.3%) of them were attended secondary school and above, and 269(45.7%) of respondents’ husband were government employed by occupation. The total monthly household’s income was ranging from 100 to 16,000 ETB while 74% of the participants had earned above 1500 ETB per month. Majority, 530 (90%) of the respondents had either TV and/or Radio in their houses (Table 1 ).
Obstetric characteristics of respondents
Among the total respondents, 347 (59.0%) mothers were categorized as Para two to Para four. Of these, 18(3.1%) of mothers faced stillbirth while they gave the last birth.
Three hundred ninety- six (67.3%) of the current pregnancy were planned and supported. Almost all, 567(96.4%) of the mothers had antenatal care follow-up during the last pregnancy while 559(95.1%) of mothers gave their last birth at health institution.
Regarding to the mode of delivery, most respondents 432(77.28%) delivered by spontaneous vaginal delivery (Table 2 ).
Proportion of postnatal care utilization
From total respondents, 338(57.5%) mothers were utilized postnatal care services with confidence interval of (53.4–61.6). Regarding to the frequency of postnatal care visit, 228(67.5%) of participants had visited once, 63(18.6%) women had two times, and the remaining 47(13.9%) were having three or more. The proportion of postnatal care visit within 24 h, at 3–7 days and at six weeks of postpartum were 103(30.5%),104(30.8%) and 162(47.9%) respectively.
Concerning types of service utilization during the postnatal visit, one-hundred sixty seven (28.4%) of the respondents utilized family planning, nearly half (44.9%) of them received immunization, 22.6% of them were tested and counseled for HIV and 106(18%) of them was counseled on breast feeding.
Reasons for nonutilization of PNC services
Different reasons were given by the participants for not attending postnatal care services. The most common reason mentioned by the participants for none utilization of postnatal care service was being apparently healthy (Fig. 1 ).
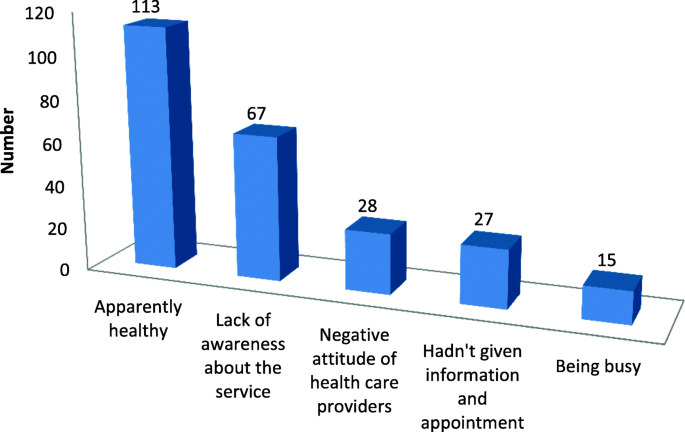
Reasons for not attending postnatal care services given by the study participants at Debretabour town, North West Ethiopia, March 2017( n = 250)
Associated factors of postnatal care utilization
During bivariable logistic regression analysis, those variables that had significant association were marital status, respondents educational level, monthly income, decision making style of the women on her health, decision making style of the women on her child health, parity, birth outcome of the last baby, nature of the last pregnancy and place of delivery.
In multiple logistic regression analysis all variables with p values less than 0.2 were entered. Only educational status of the respondents, monthly income, birth outcome of the last pregnancy, nature of the last pregnancy and place of delivery were had significant association with postnatal care service utilization.
Accordingly, those women whose educational status secondary school and above were 3 times (AOR = 3.29, 95% CI: 1.94–5.57) more likely to utilize PNC service than those women who couldn’t read and write. Those mothers who had monthly household income greater than 1500 ETB were 2.8 times more likely to utilize PNC services than those women who earned less than 500 ETB (AOR = 2.85, 95%CI:1.21–6.68).Mothers who gave birth alive neonate were 5.7 times more likely to get postnatal care services than mothers who gave still birth(AOR = 5.70,95%CI:1.53–21.21).
The odds of having postnatal care visit for those women whose pregnancy were planned and supported were 3.9 times more likely to have PNC visit than those women whose pregnancy were unplanned and unsupported(AOR = 3.96,95%CI:1.72–9.01).
Those mothers who gave birth to their latest child at the health institution were 3 times (AOR = 3.08, 95%CI: 1.24–7.68) more likely to get postnatal care service utilization when compared with those mothers who gave birth to their latest child at home (Table 3 ).
This study indicated that more than half, 338(57.5%) of the participants had received PNC services with confidence interval of (53.4–61.6).
The utilization of postnatal care service in this study is lower than a study done in Bahi District, Tanzania 70.8% [ 9 ]. The possible explanation for this difference may be due to social context variation.
This result is also lower than the previous Ethiopian studies: Addis Ababa, 65.6% [ 10 ], Gondar Zuria District, 66.83% [ 11 ] and Adwa town 78.3% [ 12 ]. The possible explanation for this difference might be due to those communities with a low concentration of educated and poor women lead to the lower attention of the need for postnatal care service utilization. The other suggestion might be due to sample size determination differences. Lastly it might be due to lack of information about postnatal care, low maternal knowledge about danger signs of postnatal care and low attention of health professionals in counseling the women to came back for postnatal care.
According to this study the utilization of postnatal care service is higher than a study conducted in rural area of Western Rajasthan, India 35.86% [ 13 ], Nepal 43.2% [ 14 ], Palestine 36.6% [ 15 ], Soroti district Eastern Uganda 15.4% [ 16 ], Africa 36% [ 17 ] developing countries 36% [ 18 ], a study done in four Sub-Saharan African countries: Burkina Faso 25%, Kenya 33%, Malawi 41% and Mozambique 40% [ 19 ].The possible reason to the discrepancies might be due to cultural differences, time differences of study socioeconomic status, geographical factors, heterogeneity of study population and political concern of governments. The other possible explanation for the difference might be due to the unique nature of Ethiopia utilizing health extension workers.
This finding is also higher than the 2016 EDHS national and Amhara regional report [ 5 ].The possible reason for this difference may be the study area where EDHS included both women who lives in urban and rural areas of the country while our study includes only urban residents. Hence, women who live in urban areas are at a greater advantage of getting education opportunity and maternal health care services. Additionally, women in the urban areas may get easy access to health facility and health professionals as compared to their counterparts.
Postnatal care utilization of this study is higher than the research carried out in Sidama zone (Southern Ethiopia) 37.2% [ 20 ], Debre Markos town 33.5% [ 8 ], Abuna Gindeberet District, Oromiya 31.7% [ 21 ],Hadiya zone, South Ethiopia 22.7% [ 22 ], Dembecha District 34.8% [ 23 ], baseline and end line postnatal care surveys in Amhara and Oromia region [ 24 ], Jabitena district, Amhara regional state, 20.2% [ 25 ] and Lemo Woreda 51.4% [ 26 ].This difference may be due to time difference between these studies, socioeconomic status, and cultural factor. The Other possible explanation for these differences may be increased governmental focuses from year to year in order to improve maternal and neonatal healths.
According to this study, the odds of PNC service utilization among women with secondary school and above by education were 3 times than those who couldn’t read and write. This finding is consistent with the study done in Nepal [ 14 ], Cambodia [ 27 ], rural area of Western Rajasthan, India [ 13 ], developing countries [ 18 ], Africa [ 17 ], Nigeria [ 28 ], Bahi District, Tanzania [ 9 ] , rural India [ 29 ], Entoto Fana health center, Addis Ababa [ 30 ], rural Haramaya District, Eastern Ethiopia [ 31 ], southern Ethiopia [ 20 ], Abi-Adi Town, Tigray [ 32 ], Jabitena district, Amhara region [ 25 ] and Dembecha District, North West Ethiopia [ 23 ].The possible reasons for this similarity might be due to the fact that once a women is educated, her autonomy and decision making skill on her health and maternal health care services utilization is high [ 32 ].Similarly, uneducated mothers have no chance to participate in different social and economic positions, decision making and women’s empowerment. Additionally, education helps to increase mothers’ level of awareness and their acceptance of new idea and provides better education to other women regarding postnatal care services utilization.
In the present study, the odds of PNC service utilization among women with monthly income greater than 1500 ETB were 2.8 times than those who earn less than 500 ETB. This finding is consistent with a study done in developing countries [ 18 ], Rwanda [ 33 ], Nigeria [ 28 ], Tanzania [ 34 ], India [ 29 ], Nepal [ 14 ] and Addis Ababa, Ethiopia [ 30 ].
The possible suggestion for this might be women having better monthly income can afford for all expenses like for transportation.
The analysis also showed that, the odds of PNC service utilization among women with alive birth outcome were 5.7 times than those who gave still birth. This is in line with a study done in Debre Markos town [ 8 ]. The possible reason for this similarity may be good birth outcome might have better insight in postnatal care service utilization.
This study also showed that, the odds of PNC service utilization among women with desire of pregnancy were 4 times than those whose pregnancy was unplanned and unsupported. This finding is supported by a study done in three rural districts of Tanzania [ 35 ] and California [ 36 ].
This study also revealed that the odds of PNC service utilization among women who gave birth at health facility were 3 times than those who delivered at home. This finding is consistent with a study done in three rural districts of Tanzania [ 35 ], Rwanda [ 33 ], Nigeria [ 28 ], Tanzania [ 34 ], Nepal [ 14 ] , Addis Ababa, Ethiopia [ 30 ], Hadiya zone, South Ethiopia [ 22 ], Debre Markos town [ 8 ], Lemo Woreda, Ethiopia [ 26 ] and another study done in Jabitena district, Amhara region [ 25 ].The possible explanation for the similarity between place of delivery and postnatal care services utilization can be evidenced by women who gave birth in health institutions have better opportunity to receive health education related to postnatal care services, get access on benefits and availabilities of PNC services during their stay in health facilities.
Limitation of the study
There could be recall bias since the women were asked for events within the last one year prior to the study. On the other hand the study did not include the rural population which is restricting the scope and relevance. Lastly, since the the design is quantitative it doesn’t address cultural issues of the respondents.
This study demonstrated that utilization of postnatal care service is still low.
Educational status of the women, monthly household income, birth outcome of the latest pregnancy, wantedness of the last pregnancy and place of delivery were found to be statistically significant for the current PNC service Utilization.
Change history
19 may 2020.
An amendment to this paper has been published and can be accessed via the original article.
Abbreviations
Ethiopian demographic health survey
Millennium development goal
Maternal mortality ratio
- Postnatal care
World health organization
WHO. Technical Consultation on Postpartum and Postnatal Care: Department of making pregnancy safer; Switzerland; World Health Organization. 2008.
WHO, UNFPA, the World Bank. Trends in maternal mortality: 1990 to 2010. World health organization, UNICEF, UNFPA, and the World Bank 2012.
Addis Ababa, Maryland, USA: Central Statistical Agency and ICF International; 2012. Central Statistical Agency [Ethiopia] and ICF International: Ethiopia Demographic and Health Survey 2011.
Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. 2016;387(10017):462–74.
Article Google Scholar
Central Statistical Agency [Ethiopia] and ICF International. Ethiopia demographic and health survey 2016 report Addis Ababa, Maryland, USA: central statistical agency and ICF international. Ethiopia demographic and health survey 2016 report Addis Ababa. Rockville, Maryland. In: USA: central statistical agency and ICF international; 2016.
FDRE MOH. National reproductive health strategy: 2006–2015. Ministry of health: Department of FH Addis Ababa; 2006.
Google Scholar
FDRE, MOH. Postnatal Care Blended Learning Module for Health Extension program Ethiopia.
Limenih MA, Endale ZM, Dachew BA. Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, northwestern Ethiopia: a community-based cross-sectional study. International Journal of Reproductive Medicine. 2016;2016.
James L, John S, Angelina S. Utilization of maternal postnatal care services among women in selected villages of Bahi District, Tanzania. Curr Res J Soc Sci. 2015;7(4):106–11.
Senait B. Assessment of prevalence of postnatal care utilization and associated factors among women who gave birth and attending immunization clinic in selected government health centers in Addis Ababa, Ethiopia, 2015: AAU; 2015.
Tesfahun F, Worku W, Mazengiya F, Kifle M. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria District, Ethiopia: a cross-sectional study. Matern Child Health J. 2014;18(10):2341–51.
Berhe H, Tilahun W, Aregay A, Bruh G, Gebremedhin HGH. Utilization and associated factors of postnatal care in Adwa town, tigray, Ethiopia-a cross sectional study a Peer Reviewed. International Journal for Pharmaceutical and Allied Research. 2012;3(1).
Sandeep Kumar Uppadhaya SB, Sivodia SK, et al. Utilization of postnatal care services in rural area of Western Rajasthan, India. National Journal of Community Medicine, July. 2016:7(7).
Khanal V, Adhikari M, Karkee R, Gavidia T. Factors associated with the utilization of postnatal care services among the mothers of Nepal: analysis of Nepal demographic and health survey 2011. BMC Womens Health. 2014;14(1):19.
Dhaher E, Mikolajczyk R, Maxwell A, Krämer A. Factors associated with lack of postnatal care among Palestinian women: a cross-sectional study of three clinics in the West Bank. BMC pregnancy and childbirth. 2008;8(1):26.
J.Izudi D. Use of early postnatal care among postpartum women in eastern Uganda. Int J Gynecol Obstet. 2015;129:161–4.
Yugbare DKS, Goujon A, et al. A review of factors associated with the utilization of health care services and strategies for improving postpartum care in Africa. Afrika Focus. 2015;28(2):83–105.
Adhikari C, Yadav RK, Timilshina P, Ojha R, Gaire D, Ghimire A. Proportion and factors affecting for post-natal care utilization in developing countries: a systematic review. Journal of Manmohan Memorial Institute of Health Sciences. 2016;2:14–9.
Al. De. Opportunities to improve postpartum care for mothers and infants: design of context -specific packages of postpartum interventions in rural districts in four sub-Saharan African countries. BMC Pregnancy and Childbirth. 2015;15(131):1–11.
Regassa N. Antenatal and postnatal care service utilization in southern Ethiopia: a population-based study. African health sciences. 2011;11(3).
Birhanu Darega ND, Fikru Tafese and Shimeles Ololo. Institutional delivery and postnatal care services utilizations in Abuna Gindeberet District, west Shewa, Oromiya region, Central Ethiopia: a community-based cross sectional study BMC Pregnancy and Childbirth 2016;16(149).
Al ZAe. Magnitude and predictors of postnatal care utilization in Hadiya zone, South Ethiopia. International Journal of Current Research. 2015;7(11):23176–82.
Hordofa M, Almaw S, Berhanu M, Lemiso H. Postnatal Care Service Utilization and Associated Factors Among Women in Dembecha District. Northwest Ethiopia. 2015;3(5):686–92.
Tesfaye S, Barry D, Gobezayehu AG, Frew AH, Stover KE, Tessema H, et al. Improving coverage of postnatal care in rural Ethiopia using a community-based, collaborative quality improvement approach. Journal of Midwifery & Women’s Health. 2014;59(s1):S55–64.
Workineh YG, Hailu DA. Factors affecting utilization of postnatal care service in Jabitena district, Amhara region Ethiopia. Sci J Public Health. 2014;23:169–76.
Tefera B, Ayanos T,Tamiru B. Postnatal care service utilization and associated factors among mothers in Lemo Woreda, Ethiopia Women’s Health Care 2016; 5(3).
Ith P, Dawson A, Homer C, Whelan A. Practices of skilled birth attendants during labour, birth and the immediate postpartum period in Cambodia. Midwifery. 2013;29(4):300–7.
Ibisomi Sa. Determinants of postnatal care non-utilization among women in Nigeria. BMC Res Notes 2016; 9(21).
Singh PK, Alagarajan M, Singh L. Determinants of maternity care services utilization among married adolescents in rural India. PLoS One. 2012;7(2).
Admassu EA. Factors associated with postnatal care utilization at Entoto Fana health center, Gullele sub-city. Addis Ababa: International Journal of Medical Science and Public Health August; 2015.
Dereje Kifle TA, Yalemzewod Assefa Gelaw and Yayehirad Alemu Melsew. Maternal health care service seeking behaviors and associated factors among women in rural Haramaya District, eastern Ethiopia: a triangulated community-based cross-sectional study Reprod Health 2017; 14(6).
Alemayeh H, Assefa H, Adama Y. Prevalence and factors associated with post Natal Care utilization in Abi-Adi town, Tigray, Ethiopia: A Cross Sectional Study.
Al. Re. Factors associated with postnatal care utilisation in Rwanda: a secondary analysis of 2010 demographic and health survey data BMC Pregnancy and Childbirth 2016; 16(122).
James Lwelamira JSaAS. Utilization of maternal postnatal care services among women in selected villages of Bahi District. Tanzania Current Research Journal of Social Sciences. 2015;7(4):106–11.
Al. Ke. Factors associated with compliance with the recommended frequency of postnatal care services in three rural districts of Tanzania BMC Pregnancy and Childbirth 2015; 15(341).
DiBari JN, Yu SM, Chao SM, Lu MC. Use of postpartum care: predictors and barriers. J Pregnancy. 2014.
Download references
Acknowledgments
The authors would like to pass their gratitude to Bahirdar University for the approval of ethical clearance. We would like to extend our thanks to Amhara Regional health Bureau, Debretabour health office and respected kebeles for permitting to conduct the study and providing the necessary preliminary information. The authors are also very grateful for data collectors and mothers who participated in this study.
Bahir Dar University. This study was done by the fund obtained from Bahir Dar University for the design and collection, analysis and interpretation of data. However, the funder has no specific role in the preparation of the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the.
current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Midwifery, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Kihinetu Gelaye Wudineh, Azezu Asres Nigusie, Shumiye Shiferaw Gesese, Azimeraw Arega Tesu & Fentahun Yenealem Beyene
You can also search for this author in PubMed Google Scholar
Contributions
KGW, AAN and SSG conceived and designed the protocol, performed the data collection, contributed for data analysis, wrote the paper and revised the manuscript. AAT and FYB participate on the editorial and data entry and analysis. All authors read and approved the final paper.
Corresponding author
Correspondence to Kihinetu Gelaye Wudineh .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from the institutional review board of Bahir Dar University.
Formal letter of cooperation was written for Regional Health Bureau, Debretabour health office and respective kebeles and permission was obtained. Written consent was obtained from each study participants. Confidentiality of information and privacy was maintained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Wudineh, K.G., Nigusie, A.A., Gesese, S.S. et al. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community- based cross-sectional study. BMC Pregnancy Childbirth 18 , 508 (2018). https://doi.org/10.1186/s12884-018-2138-x
Download citation
Received : 03 November 2017
Accepted : 05 December 2018
Published : 27 December 2018
DOI : https://doi.org/10.1186/s12884-018-2138-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Utilization
- Maternal death
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- International edition
- Australia edition
- Europe edition

Postnatal depression: ‘I went downhill very fast’
Joanna Friend, from Woodbury, near Exeter, Devon, first experienced depression and anxiety five days after the birth of her first son: “I started feeling an intense anxiety, and I went downhill very fast – I was lying on the floor crying and asking for people to help me. It got so bad a friend said I needed to call the mental health crisis team.”
With no specialist care available Friend, now 36, was given tranquillisers and antidepressants, which required her to stop breastfeeding. After six months she was able to go off medication, only to relapse 18 months later, when she became pregnant with her younger son.
“I woke up feeling really sick and I felt all the anxiety coming back, and this time it was even worse. I was almost catatonic, lying on the floor in the kitchen. No one could make me speak or move.”
With no mother and baby units in her area – the closest is in Poole, Dorset – Friend spent a week on a standard psychiatric unit, which she remembers being far from suitable: “Because I was still being sick all the time I was needing to eat little and often,” she recalls. “I went to the kitchen to ask for some toast and the chef said: ‘No, nothing between mealtimes.’ I told him I was pregnant. He said: “I’ve heard that before.’ ”
Staff from a new specialist team intervened to send Friend home, prescribing antidepressants. Again, the recovery was mixed: “I never got fully well when I was pregnant, but about 10 weeks after the birth I was completely back to normal again. I stayed on the drugs for two and a half years and started to wean off, but when I got to a low level I had a massive relapse.
“I went back on the drugs and they didn’t work, and had to go through all sort of different drugs till I found one that did. It’s only really in the last month I’ve recovered from that relapse.”
Friend in part blames the long wait for psychotherapy: “I only had my assessment a month ago – my sons are seven and four – and I’m now on a two-year waiting list. If, after I’d had the eldest, I could have had talking therapy, when I came off my drugs I would have had some strategies to fall back on when I started to relapse.”
The experience has affected her. “I’m thinking that I won’t have any more children. I always wanted loads of children, but my episodes are so severe we just think the threat to the family is too great.”
- Postnatal depression
- Mental health
- Health & wellbeing
- Parents and parenting

Better care urged for pregnant women with mental health problems – study

I had postpartum psychosis. More must be done to help mothers like me

The terrible effects of postnatal depression

Gaps in mental health care for new mothers cost UK £8bn a year – study

Sad state of support for new families

Our health system is failing new mothers
Most viewed.

IMAGES
VIDEO
COMMENTS
The days and weeks following childbirth—the postnatal period—are a critical phase in the lives of mothers and newborn babies. Most maternal and infant deaths occur in the first month after birth: almost half of postnatal maternal deaths occur within the first 24 hours,1 and 66% occur during the first week.2 In 2013, 2.8 million newborns ...
Background. Postnatal Care (PNC) is one of the care packages that make up the continuum of care for mothers and babies globally [1, 2].A significant number of maternal deaths still occur during the postnatal period and an estimated 2.8 million babies die in the first month of life (neonatal death) [3, 4].Neonatal deaths account for up to 52% of all deaths in children under-5 years of age [].
In this session we review the key information to be communicated to women who have just given birth and their partners and/or families. This covers general care of both the mother and the baby as well as danger signs in the postnatal period. Special mention is made for supporting women with depression.This topic is used to practise the skills of facilitating family and group support and ...
Introduction. The days and weeks following childbirth - the postnatal period - is a critical time for women and newborns [].Major physical, social and emotional changes occur during this period, yet this is often the most neglected period on the continuum of maternal and newborn care, challenged by the fragmentation of services [].Quality postnatal care (PNC) services can have a lifelong ...
Results. We included 36 studies from 15 countries, representing the views of more than 800 women. Confidence in most results was moderate to high. What mattered to women was a positive postnatal experience where they were able to adapt to their new self-identity and develop a sense of confidence and competence as a mother; adjust to changes in ...
Background Effective postnatal care is important for optimal care of women and newborns-to promote health and wellbeing, identify and treat clinical and psychosocial concerns, and to provide support for families. Yet uptake of formal postnatal care services is low and inequitable in many countries. As part of a larger study examining the views of women, partners, and families requiring both ...
The WHO postnatal care model places the woman- newborn dyad at the centre of care (Fig. 1). The foundation of this postnatal care model is a minimum of four postnatal care contacts. In particular, the GDG considered the first two weeks after birth to be a key time to promote health, identify health problems, and
This scoping review aims to document the measures used to assess the quality of postnatal care and their validity. The review was conducted according to the Preferred Reporting Items for ...
Contents by subject matter Antenatal care 56-63 Antepartum haemorrhage 157-161, 182-186 Breech presentation 190-197 Cancer of cervix 10 1-[ 04 of endometrium 217-221 of ovary 81-85 of vulva 46-50 Cervical cytology 11-19,24-28 Contraception 11-19,95-100,105-109,147-151
Optimal care during the antenatal and postnatal phases of the life cycle is a potentially positive determinant of health elsewhere in the continuum. A successful transition from the antenatal to the postnatal period requires early detection, optimal management, and prevention of disease; health promotion; birth preparedness; and complication readiness. Women, their babies, and families need ...
The early postnatal period is a dangerous time for both mother and baby where morbidity and mortality are highly prevalent if proper care is not done. Post natal care (PNC) knowledge has significant role in reducing such complications. In this study, the knowledge of postpartum mothers on PNC and its determinants were determined. A cross-sectional quantitative study was conducted in postpartum ...
The sample size calculation for this nested case-control study was performed using Open EPI version 3.1. minimum sample size of 100 cases and 498 controls was required in order to achieve 80% power, with an anticipated prevalence of risk factors among the controls ranging from 4 to 59%, an anticipated odds ratio of 2 and a level of significance ...
Sometimes this was a strategic choice to prioritise professional information on specific topics: ... and that this can best be achieved through postnatal midwifery home care. This study deepens understanding of the ways in which the social support aspects of postnatal care in any setting can be an opportunity to enhance first time mothers ...
Study design Prospective Cohort Study. Methodology Study was carried out in the Sheth L.G. Hospital, a tertiary health care centre, enrolling subjects, who had attended outpatient department of obstetrics department with gestational age between 11 to 13 weeks (±6 days), over a period of 1.5 years, from June 2019 to Jan 2020. One hundred and ...
Postnatal care - current issues and future challenges Midwifery. 2014 Jun;30(6):571-4. doi: 10.1016/j.midw.2014.05.001. Authors Virginia Schmied 1 , Debra Bick 2 Affiliations 1 School of Nursing and Midwifery, University of Western Sydney, Building EBLG Room 33, Parramatta South Campus, Sydney, Australia. Electronic address: [email protected] ...
by Natalie Trice. It's not uncommon to experience 'baby blues' after giving birth. For some women this goes away as quickly as it arrived. For others, it develops into full-blown postnatal depression (PND), a condition that is often hidden but can have a significant impact on you and your family. NHS figures show postnatal depression ...
Katrynni Oliveira Rodrigues & Marcio Fronza (2019): Postpartum depression: a case-control study, The Journal of Maternal-Fetal & Neonatal Medicine, DOI: 10.1080/14767058.2019.1671335
Postnatal Care (PNC) is one of the care packages that make up the continuum of care for mothers and babies globally [1, 2].A significant number of maternal deaths still occur during the postnatal period and an estimated 2.8 million babies die in the first month of life (neonatal death) [3, 4].Neonatal deaths account for up to 52% of all deaths in children under-5 years of age [].
Case Files: High-Risk Obstetrics. Author (s): Eugene C. Toy; Edward R. Yeomans; Linda Fonseca; Joseph M. Ernest. View by: Case Topic A-Z Unlabeled Number View. Abruption/Dead Fetus. Acute Fatty Liver of Pregnancy.
In the case of the Amhara region percentage of women with a postnatal checkup in the first two days after birth was18.4% . Methods. Study area and period. ... The utilization of postnatal care service in this study is lower than a study done in Bahi District, Tanzania 70.8% . The possible explanation for this difference may be due to social ...
Sun 19 Oct 2014 19.05 EDT. Last modified on Thu 30 Nov 2017 01.58 EST. Joanna Friend, from Woodbury, near Exeter, Devon, first experienced depression and anxiety five days after the birth of her ...
Postnatl Case Study - Free download as Word Doc (.doc), PDF File (.pdf), Text File (.txt) or read online for free. postnatal case study of a woman
The perception of danger in different cultures. The origins of bipolar disorder through the prism of domestic violence. Covid-19 and related anxiety cases among college students. The dangers of advertisements on children's TV networks. The negative influence of Instagram and distorted body image.