
- Vishal's account
- Prenatal Care

Shoulder Presentation – All You Should Be Aware Of
When Does the Fetus Move in Birthing Position?
What is shoulder presentation, what is transverse lie, what is the frequency of shoulder presentation, what causes shoulder presentation, how is shoulder presentation diagnosed, complications of shoulder presentation, how is shoulder presentation managed.
Most doctors and midwives will recommend that you have a natural vaginal birth if you have a choice. However, there are certain complications that can sometimes present themselves and stop this from happening. Shoulder presentation is one such complication.
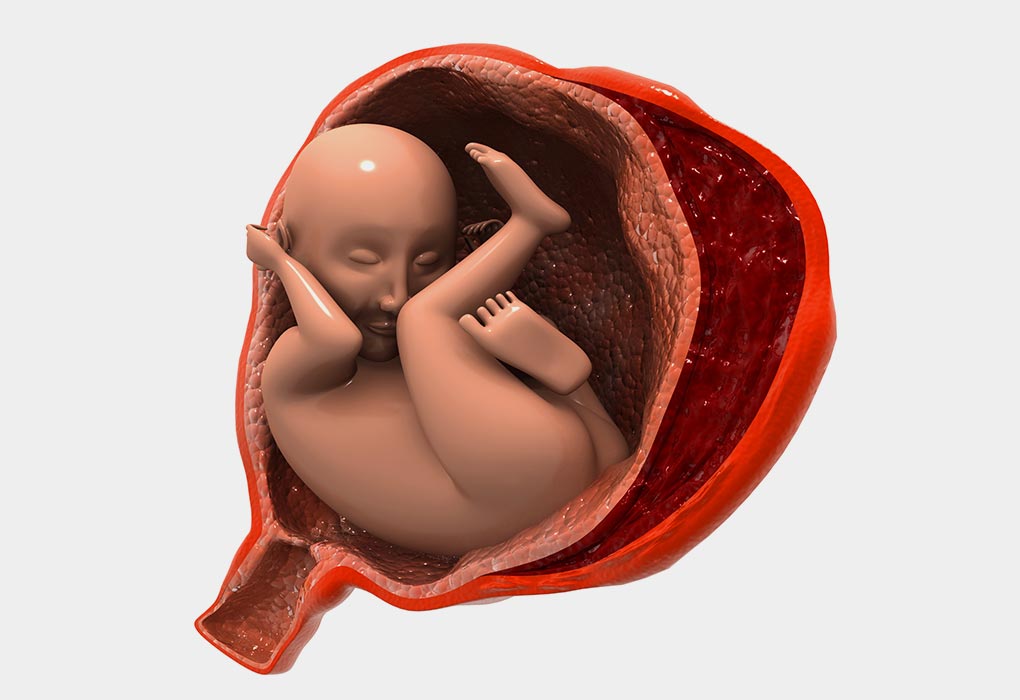
A baby will most likely begin to move into the birthing position latest by week 30 . She will have her head down and facing your spine, her body and face more inclined to one side and arms will be folded across the chest. Any other position is not normal.
This is an abnormal fetus position where the baby is in a transverse lie , causing the baby’s shoulder to be positioned to come out first if vaginal delivery is attempted. However, since this is very easy to diagnose, doctors will always recommend a C-Section and never even suggest attempting to deliver the child through normal vaginal delivery.
A transverse lie is a position where your baby is lying sideways with her head to one of your sides and her bottom at your other side. This position is considered normal before 26 gestational weeks.
Shoulder presentation takes place in 1 out of every 300 births and is commonly seen in premature and macerated babies. It is five times more likely to happen in a woman who has had children before than it is to occur in a first-time mother. Mothers carrying twins are also 40% more likely to have at least one baby in shoulder position.
Here are some reasons why a shoulder presentation can take place:
1. Contracted Pelvis
A very narrow pelvis in the mother can cause a shoulder presentation to occur.
2. Placenta Previa
A condition where the placenta covers the uterus opening, either completely or partially. This makes it difficult for your baby’s head to enter the pelvic brim.
3. Intra-Uterine Fetal Death
There are times when the fetus dies inside the womb, and when this happens, the muscle tone starts to degenerate, which results in the fetus falling lower into the uterus.
4. Lax Abnormal Musculature
Women who have had multiple pregnancies may have more relaxed uterine and abdominal muscles. This will make their ability to keep the baby in a normal position very difficult.
5. Uterine Over Distension
There are many reasons why a uterus can become enlarged. Some of these include a large baby, polyhydramnios , multiple pregnancies and others. A uterus that is too large very often leads to shoulder presentation.
6. Polyhydramnios
A very large amount of amniotic fluid that is present in the uterus is known as polyhydramnios. This causes the fetus to be able to move very freely in the uterus and will lead to shoulder presentation.
7. Uterine Abnormalities
There are different abnormalities in the uterus that can cause your baby to move into shoulder presentation. Some of these are the bicornuate uterus, a sub-septate uterus and even a large fibroid uterus .
Here is how Shoulder presentation diagnosed:
- The top of the mother’s uterus to the top of the pelvic bone is called a fundus. The height of the fundus is an indicator of whether or not the baby is in the shoulder presentation.
- The uterus becomes broader.
- The mother can feel the baby’s head on one abdominal side.
- If shoulder presentation takes place, arms prolapse will cause the baby’s arm to be seen outside the vagina.
- During a vaginal examination, the doctor will be able to feel the babies ribs.
If your doctor identifies that you have shoulder presentation before you go into labour, he will opt for a C-Section instead. If there is a case of neglected shoulder presentation and it is only identified after you go into labour, it becomes very dangerous, and you face many complications. Here are some of the complications that can occur:
1. Cord Prolapse
When the umbilical cord comes out before the fetus does, it is called a cord prolapse and is very dangerous as it can cause the baby’s heart rate to drop, cause changes in blood pressure and even result in brain damage or death of the baby.
2. Ruptured Uterus
The myometrial wall is the middle layer of the wall of the uterine. The breach of this layer during childbirth is a rupture in the uterus, and it is very dangerous for both mother and child.
3. Fetal Hypoxia
When your baby doesn’t get enough oxygen, it will lead to suffocation, and if the necessary measures are not taken, it will result in death.
4. Obstructed Labour
Though contractions are taking place, the baby is not able to come through the birth canal as there is something blocking the way. Failure to diagnose and remedy this condition is a major reason why both mother and child die during childbirth.
5. Trauma to Prolapsed Arm
If there is a prolapsed arm, there is a higher chance that it will be injured or damaged. This injury may be severe and could last for a lifetime.
Here is how Shoulder presentation is managed:
1. C-Section
The first choice for doctors who have a case of shoulder presentation is a C-Section. This is the safest method that ensures the safety of both mother and child.
2. External Cephalic Version
In this procedure, your baby’s heartbeat will be monitored, and you will be given medication through an IV to ensure a relaxed uterus. Your doctor will then place her hands on the outside of your stomach and attempt to turn your baby into the correct position. This is done only before labour starts.
3. Internal Podalic Version
This is only used in the case of twins, where the second twin will need to be moved into a breech position and then extracted.
Though it sounds scary, if you keep a careful track of your baby’s position in the weeks before delivery, you will be able to identify and rectify the problem before it becomes serious. Exercising throughout your pregnancy will be very helpful in ensuring that your baby gets into the correct position for labour.
Also Read: When Does a Baby Turn Head Down During Pregnancy?
- RELATED ARTICLES
- MORE FROM AUTHOR

Taking Care of Your Mental Health in Pregnancy

Vaginal (Internal) Examination During Pregnancy

Benefits of Prenatal and Postnatal Exercises

Salicylic Acid in Pregnancy - Safety, Benefits & Side Effects

Decreased Foetal Movement - Causes, Diagnosis, and Measures

Eating Junk Food During Pregnancy - Is It Safe for You & Baby?
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.
Cookie Monster Coloring Pages - Free Printable Pages For Kids
Robot Coloring Pages - Free Printable Pages For Kids

Cheerleading Coloring Pages - Free Printable Pages For Kids

Essay On Holi - 10 lines, Short and Long Essay for Students and Children
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
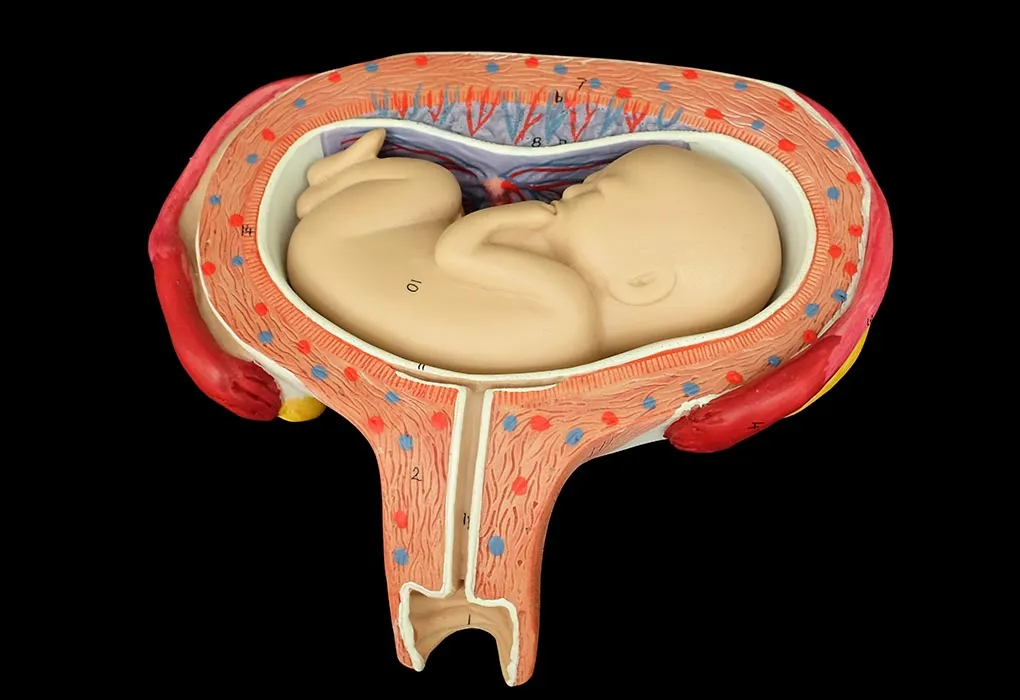
● The curvature of the fetal spine is oriented downward (also called "back down" or dorsoinferior), and the fetal shoulder presents at the cervix ( figure 1 ).
● The curvature of the fetal spine is oriented upward (also called "back up" or dorsosuperior), and the fetal small parts and umbilical cord present at the cervix.
(Note: Lie refers to the long axis of the fetus relative to the longitudinal axis of the uterus; the long axis of the fetus can be transverse to, oblique to, or parallel to [longitudinal lie] the longitudinal axis of the uterus. Presentation refers to the fetal part that directly overlies the pelvic inlet; it is usually cephalic [head] or breech [buttocks] but can be a shoulder, compound [eg, head and hand], or funic [umbilical cord]. Position is the relationship of a nominated site of the presenting part to a denominating location on the maternal pelvis [eg, right occiput anterior].)
GFMER Geneva Foundation for Medical Education and Research
- Annual reports
- GFMER members
- Country coordinators
- Obstetric fistula
- Cervical cancer
- Emergency and surgical care
- Picture of the week
- Social media
- Free medical journals
Obstetrics Simplified - Diaa M. EI-Mowafi
Shoulder Presentation (Transverse or Oblique lie)
- The longitudinal axis of the foetus does not coincide with that of the mother.
- These are the most hazardous malpresentations due to mechanical difficulties that occur during labour .
- The oblique lie which is deviation of the head or the breech to one iliac fossa, is less hazardous as correction to a longitudinal lie is more feasible.
3-4% during the last quarter of pregnancy but 0.5% by the time labour commences.
Factors that
- change the shape of pelvis, uterus or foetus,
- allow free mobility of the foetus or
- Contracted pelvis.
- Lax abdominal wall.
- Uterine causes as bicornuate, subseptate and fibroid uterus.
- Pelvic masses as ovarian tumours.
- Multiple pregnancy.
- Polyhydramnios.
- Placenta praevia.
- Prematurity.
- Intrauterine foetal death.
The scapula is the denominator
- Left scapulo-anterior.
- Right scapulo-anterior.
- Right scapulo-posterior.
- Left scapulo-posterior.
Scapulo-anterior are more common than scapulo-posterior as the concavity of the front of the foetus tends to fit with the convexity of the maternal spines.
During pregnancy
- The abdomen is broader from side to side.
- Fundal level: lower than that corresponds to the period of amenorrhoea.
- Fundal grip: The fundus feels empty.
- Umbilical grip: The head is felt on one side while the breech one the other. In transverse lie, they are at the same level, while in oblique lie one pole, usually the head as it is heavier, is in a lower level i.e. in the iliac fossa.
- First pelvic grip: Empty lower uterine segment.
- FHS are best heard on one side of the umbilicus towards the foetal head.
- Confirms the diagnosis and may identify the cause as multiple pregnancy or placenta praevia.
During labour
In addition to the previous findings, vaginal examination reveals:
- The presenting part is high.
- Membranes are bulging.
- Premature rupture of membranes with prolapsed arm or cord is common. The dorsum of the supinated hand points to the foetal back and the thumb towards the head. The right hand of the foetus can be shacked, correctly by the right hand of the obstetrician and the left hand by the left one.
- When the cervix is sufficiently dilated particularly after rupture of the membranes, the scapula, acromion, clavicle, ribs and axilla can be felt.
Mechanism of Labour
As a rule no mechanism of labour should be anticipated in transverse lie and labour is obstructed.
If a patient is allowed to progress in labour with a neglected or unrecognized transverse lie, one of the following may occur:
- This is the usual and most common outcome.
- The lower uterine segment thins and ultimately ruptures.
- The foetus becomes hyperflexed, placental circulation is impaired, cord is prolapsed and compressed leading to foetal asphyxia and death.
- Rarely the foetal lie may be corrected by the splinting effect of the contracted uterine muscles so that the head presents.
- Rarely, by similar process the breech may come to present.
- Very rarely, if the foetus is very small or dead and macerated, the shoulder may be forced through the pelvis followed by the head and trunk.
- Very rarely, the head is retained above the pelvic brim, the neck greatly elongates, the breech descends followed by the trunk and the after -coming head, i.e. spontaneous version occurs in the pelvic cavity.
External cephalic version
Can be done in late pregnancy or even early in labour if the membranes are intact and vaginal delivery is feasible. In early labour, if version succeeded apply abdominal binder and rupture the membranes as if there are uterine contractions.
Internal podalic version
It is mainly indicated in 2nd twin of transverse lie and followed by breech extraction.
Prerequisites:
- General or epidural anaesthesia.
- Fully dilated cervix.
- Intact membranes or just ruptured.
Caesarean section
- It is the best and safest method of management in nearly all cases of persistent transverse or oblique lie even if the baby is dead.
- As rupture of membranes carries the risk of cord prolapse, an elective caesarean section should be planned before labour commences.
Neglected (Impacted) shoulder
Clinical picture (impending rupture uterus)
- Exhaustion and distress of the mother.
- Shoulder is impacted may be with prolapsed arm and / or cord.
- Membranes are ruptured since a time.
- Liquor is drained.
- The uterus is tonically contracted.
- The foetus is severely distressed or dead.
- Caesarean section is the safest procedure even if the baby is dead. A classical or low vertical incision in the uterus facilitates extraction of the foetus as a breech in such a condition.
- Any other manipulations will lead eventually to rupture uterus so they are contraindicated.
UNSTABLE LIE
A foetus which changes its lie frequently from transverse to oblique to longitudinal.
- Polyhydramnios.
- Prematurity and IUFD.
- Contracted pelvis.
- Placenta praevia.
- Pelvic tumours.
- Multiparae with a lax uterus and abdominal wall.
- Can be done whenever the woman is examined but in majority of cases it will recur so it is better to defer it until full term (37-40 weeks).
- After correcting the foetal lie to longitudinal, apply an abdominal binder, start oxytocin infusion and do amniotomy when the uterine contractions started and the presenting part is well settled into the pelvic brim.
- Failure of external version .
- Some do it selectively in cases discovered after 40 weeks’ gestation.
- Shoulder dystocia : Guidelines, reviews
Transverse Lie
- First Online: 02 August 2023
Cite this chapter

- Jayashree V. Kanavi 2 &
- Rajshree Katke 3
412 Accesses
When the long axis of the fetus is perpendicular to that of the mother, then the baby is said to be in transverse lie. This position is also called as shoulder presentation, as the shoulder is positioned over the pelvic inlet. However, other fetal parts may also be present like arm, chest, abdomen, or even back. This is a serious malposition whose management must not be left to nature. We can wait for spontaneous version till 38 weeks of pregnancy.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Gary CF. Williams obstetrics. 25th ed. New York, NY: McGraw Hill Education; 2018.
Google Scholar
Black AY, Posner GD, editors. Oxorn-Foote human labor and birth. 6th ed. Sykesville: McGraw Hill Medical; 2013.
Dutta DC. In: Konar H, editor. Text book of obstetrics. 9th ed. New Delhi: Jaypee Brothers Medical Publishers; 2018.
Virkud A. Practical Obstetrics & Gynecology. 6th ed. New Delhi: APC Publisher; 2018.
External Cephalic Version (ECV) guidelines—Green-top guideline No 20a-RCOG Guidelines. 2017.
Balakrishnan S. Text book of obstetrics. 3rd ed. Hyderabad: Paras Medical Publishers; 2020.
All figures: picture courtesy Jaypee digital library—eBook reader. jaypeedigital.com .
Ali R. Professional Med J. 2011;18(2):208–11.
Article Google Scholar
Download references
Author information
Authors and affiliations.
St John’s Medical College and Hospital, Bangalore, India
Jayashree V. Kanavi
Deparment of Obstetrics and Gynaecology, Grant Govt Medical College, Mumbai, India
Rajshree Katke
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Department of Obstetrics and Gynecology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India
Ruchika Garg
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Kanavi, J.V., Katke, R. (2023). Transverse Lie. In: Garg, R. (eds) Labour and Delivery. Springer, Singapore. https://doi.org/10.1007/978-981-19-6145-8_7

Download citation
DOI : https://doi.org/10.1007/978-981-19-6145-8_7
Published : 02 August 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-6144-1
Online ISBN : 978-981-19-6145-8
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Management of neglected shoulder presentation
Affiliation.
- 1 Department of Obstetrics and Gynaecology, College of Medical Sciences, University of Benin, Benin City, Nigeria. [email protected]
- PMID: 19906016
- DOI: 10.1111/j.1471-0528.2009.02376.x
Publication types
- Cesarean Section
- Developing Countries
- Extraction, Obstetrical / methods
- Fetal Death
- Labor Presentation*
- Obstetric Labor Complications / therapy*
9.7 Embryotomy
Destructive operation to reduce the volume of a dead foetus to facilitate vaginal delivery when obstruction prevents this from occurring naturally.
There are several types of embryotomy:
- Craniotomy: a procedure in which a perforation is made in the foetal skull to reduce the volume of the foetal head which prevents delivery. It can be done on either an obstructed cephalic presentation or an entrapped aftercoming head in a breech.
- Cranioclasis: a procedure to crush the bones of the foetal skull. It is done if necessary after craniotomy in order to allow extraction of the foetal head.
- Decapitation: a procedure in which the foetus is decapitated to relieve impaction due to a transverse lie.
- Evisceration: a procedure in which an incision is made in the abdomen or thorax in the case of a mass or fluid collection (ascites) which is preventing delivery of the foetus.
- Cleidotomy: a procedure in which one or both clavicles are cut to reduce the biacromial diameter in case of a shoulder dystocia not resolved by other manoeuvres.
Embryotomy, especially as often performed on a fragile and infected uterus, carries the risk of trauma (e.g., uterine rupture, cervical or vaginal injury, and damage to maternal soft tissue with fistula). This risk is especially high in the event of decapitation.
Few people have experience with these procedures. The operators must have the knowledge of obstetrics, must feel comfortable performing obstetric manoeuvres and must have skills to manage potential complications.
Some practitioners would rather perform a caesarean section on a dead foetus than have to mutilate a foetus. However, independently of the mode of delivery (by caesarean section or vaginally), obstructed labour carries a significant risk of puerperal infection, fistula and postpartum haemorrhage. In addition, caesarean section can place the mother at significant risk in terms of both survival and function. The objective of embryotomy is to reduce such risks.
Embryotomy should be performed in a CEmONC facility (refer if necessary, even if the referral takes time).
9.7.1 General conditions and precautions
There is no urgency in extracting the foetus. The priority is maternal intensive care (intravenous line, IV hydration, antibiotic therapy for prolonged rupture of membranes or infection, and urinary catheterisation).
The embryotomy can be performed once the mother is stable, under the following conditions:
- Confirm foetal death: no heart tones on foetal Doppler or ultrasound.
- Confirm the obstacle to vaginal delivery due to size and/or presentation.
- Make sure there is adequate access to the foetus: full or nearly full dilation and ruptured membranes.
- Insert a Foley catheter.
- Perform the procedure in the operating room under strict aseptic conditions and anaesthesia; always prepare for laparotomy in case of uterine rupture.
- Take time to explain to the mother and family the expected benefits (avoiding caesarean section) and potential complications (possible laparotomy if the event of embryotomy failure or uterine rupture). Obtain the patient’s consent.
- the uterine cavity (uterine exploration with antibiotic prophylaxis, Section 9.3 );
- the vaginal walls (use the vaginal retractors in the curettage set, for example, to get adequate exposure).
- After the procedure, routinely administer oxytocin IM or slow IV: 5 IU or 10 IU.
- In the event of obstructed labour, leave the Foley catheter in place for 14 days to reduce the risk of fistula formation.
- Care for the body of the infant: suture the skin wounds; clean and wrap up the infant to show/give him to the parents or family, depending on their choice.
9.7.2 Contra-indications
- Doubt about whether the foetus is dead or alive
- Uterine rupture
- Incomplete dilation
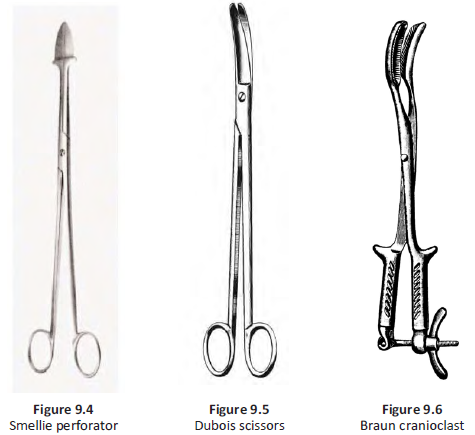
9.7.3 Equipment
- Smellie perforator (Figure 9.4)
- Dubois scissors or large, curved scissors (Figure 9.5)
- Braun cranioclast (Figure 9.6)
- 4 Faure forceps
9.7.4 Craniotomy for obstructed cephalic presentation
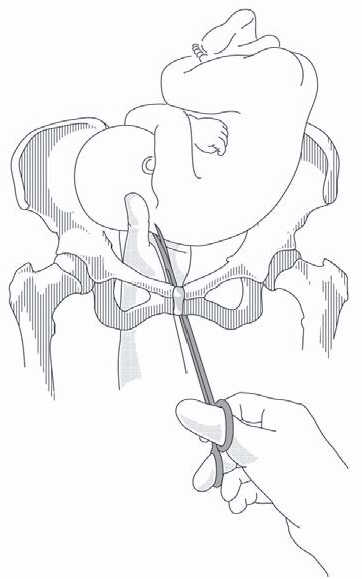
Figure 9.7 - Embryotomy with the Smellie perforator
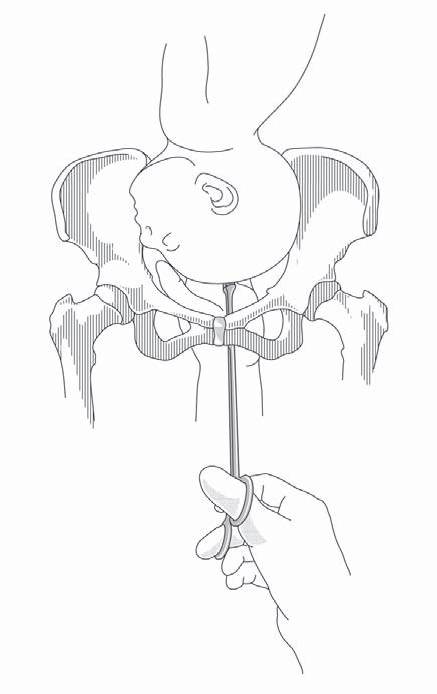
- Have an assistant place both palms on the mother's abdomen to apply downward pressure on the foetal head toward the pelvis.
- Insert one hand, shaped like a channel, into the vagina, in contact with the foetal head.
- Using the other hand, slide the perforator along the channel formed by the first hand (to protect the vagina) until it makes contact with the foetal head. This can be done under direct vision after retraction with vaginal retractors.
- The perforation should be made in the centre of the skull to protect the mother's soft tissues. It is easier to do it in a fontanelle. Rotate the instrument to make the perforation, and then remove it so that the cerebrospinal fluid and/or brain matter can drain through the hole.
- Once the cerebrospinal fluid spills out, the head should collapse and delivery should be easy; if not, apply traction to the skull with 3 or 4 forceps, gripping the scalp around the perforation. If necessary, perform cranioclasis.
Note : if the foetus is hydrocephalic, perforation can be replaced by needle aspiration.
9.7.5 Cranioclasis
- Insert the cranioclast’s solid jaw into the opening made by the perforator. The hollow jaw is placed beside the skull similar to the placement of obstetric forceps.
- Adjust the two jaws with the screw and extract the head in the most favourable orientation.
9.7.6 Craniotomy for entrapped aftercoming head in a breech
- Have an assistant place both palms n the mother's abdomen to apply downward pressure on the foetal head toward the pelvis.
- Pull the body of the foetus out and down to gain access to the occiput. If necessary, retract the anterior vaginal wall using a vaginal wall retractor.
- Insert the perforator (or scissors, if there is no perforator) under the occiput. Rotate the instrument to make the perforation. Open and close to cut up the contents.
- Remove the perforator and apply traction to the trunk. If the head remains trapped, traction can be applied directly to the skull with forceps attached around the perforation.
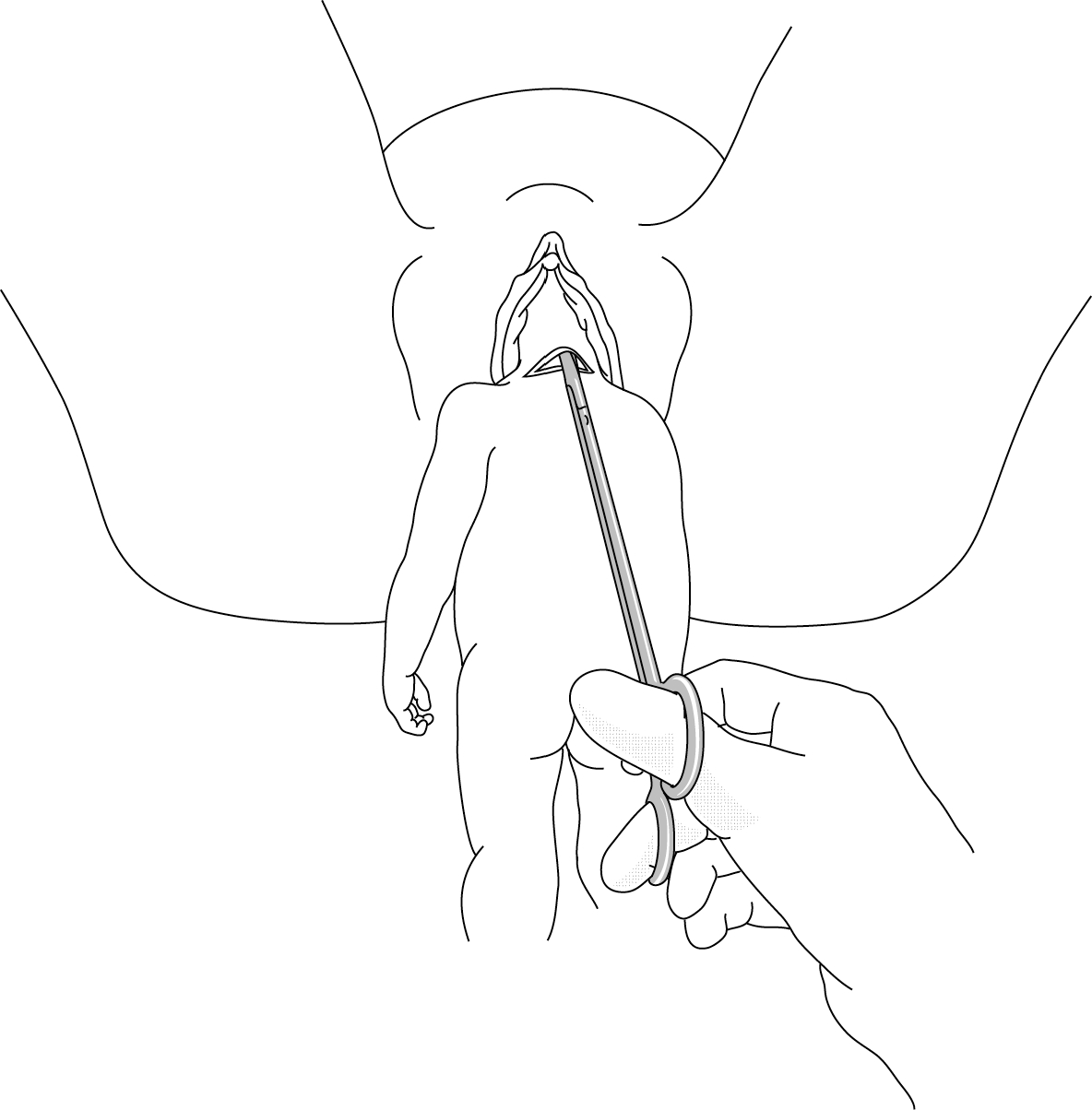
9.7.7 Decapitation for transverse lie
This is the most difficult type of embryotomy to perform, and the one carrying the greatest risk of maternal trauma.
If the foetus is big and/or hard to access, embryotomy cannot be done and caesarean section is the first and only option. Be aware that the caesarean section will be complicated, with potentially difficult foetal extraction and the risk of enlargement of the hysterotomy.
Embryotomy can be attempted if the foetus is small and easy to access. First try internal version (Chapter 7, Section 7.8 ) in the operating room under anaesthesia and total breech extraction (Chapter 6, Section 6.3 ), with or without craniotomy.
- Determine the exact position of the foetus (position of the head and neck and which arm is prolapsed.
- In case of neglected shoulder presentation (Chapter 7, Section 7.6.1 ), have an assistant apply traction to the prolapsed arm (do not try to section the arm first, as it can be used to pull the body downward).
- Slide one hand behind the foetus and surround the neck with thumb and index finger, like a necklace.
- With the other hand, slide the closed scissors into the channel formed by the first hand, keeping them flat against the hand. It is imperative to approach the neck at a right angle.
- Using fingers to control and guide, section the neck bit by bit, in the hollow of the hand, opening the scissor blades only slightly each time.
- After decapitation, bring the arms down one after the other and deliver the body.
- To deliver the head, grasp the neck stump and pull downward, performing the delivery as for retention of the aftercoming head, fingers in the foetus’ mouth.
9.7.8 Evisceration
- Initially, attempt to puncture the abdomen with a needle. This might be sufficient to reduce the foetal ascites to allow delivery.
- In case of failure (either insufficient fluid reduction or a solid mass), use scissors to incise, under vision, the abdominal wall and remove the organs.
9.7.9 Cleidotomy
It is difficult to cut one or both clavicles with Dubois scissors and there is a high risk of cutting maternal tissue. It should not be attempted unless all of the obstetrical manoeuvres described in Chapter 7, Section 7.5.1 . have failed after several attempts.
For more information on destructive delivery, see: Primary Surgery: Non-Trauma v.1. 1990. https://storage.googleapis.com/global-help-publications/books/help_primarysurgery.pdf [Accessed 12 December 2018]
- Open access
- Published: 31 January 2023
Treatment and outcomes of chronic locked posterior shoulder dislocations: a retrospective case series
- Emil George Haritinian 1 , 2 ,
- Ioan Cristian Stoica 1 , 2 ,
- Roman Popescu 1 ,
- Gavril Lucian Gheorghievici 1 , 2 &
- Laurent Nové-Josserand 3
BMC Musculoskeletal Disorders volume 24 , Article number: 82 ( 2023 ) Cite this article
2417 Accesses
2 Citations
Metrics details
Posterior shoulder dislocations are rare injuries that are often missed on initial presentation. Cases left untreated for more than three weeks are considered chronic, cannot be reduced closely (they become locked) and are usually associated with a significant reverse Hill-Sachs defect. The aim of this study was to evaluate the outcomes of chronic locked posterior shoulder dislocations treated with the McLaughlin procedure (classic or modified).
This retrospective study included 12 patients with chronic locked posterior shoulder dislocation operated on between 2000 and 2021 by two surgeons in two institutions. Patients received a thorough clinical examination and radiological assessment before and after surgery. Shoulders were repaired with the McLaughlin or modified McLaughlin procedure. Outcomes were assessed by comparing pre- and postoperative values of clinical variables.
Most of the dislocations were of traumatic origin. The average delay between dislocation and surgical reduction was 13.5 ± 9.7 weeks. Postoperative clinical outcomes were favourable, with an average subjective shoulder value of 86.4 ± 11.1 and a normalized Constant –Murley score of 90 ± 8.3. None of the patients had a recurrence of shoulder dislocation, but one patient developed avascular necrosis of the humeral head and two patients developed glenohumeral osteoarthritis.
Conclusions
In this group of patients with chronic locked posterior shoulder dislocation, the clinical outcomes of McLaughlin and modified McLaughlin procedures were satisfactory, even when surgery was significantly delayed.
Peer Review reports
Posterior shoulder dislocation is a rare injury, accounting for just 2 to 5% of all shoulder dislocations [ 1 , 2 , 3 ]. The most common causes are convulsions (epileptic, hypoglycaemic or drug withdrawal), trauma and electric shocks [ 3 , 4 ]. A significant percentage (50–79%) of posterior shoulder dislocations are missed on initial presentation [ 5 ]. Thorough clinical examination is crucial and usually shows flattening of the anterior shoulder, a prominent coracoid process, severely limited external rotation and reduced abduction [ 6 ]. True anteroposterior and axillary or scapular Y radiographic views of the affected shoulder are also required. Several diagnostic signs (light bulb, vacant glenoid, double trough, rim) have been described on anteroposterior radiographs [ 5 , 7 ].
Posterior shoulder dislocations are associated in 30 to 90% of cases [ 8 ] with an osteochondral impression fracture of the anteromedial part of the humeral head called a reverse Hill-Sachs lesion (RHSL) [ 9 ]; however, the term posterior shoulder fracture- dislocation is usually only used in cases (about one third [ 10 ]) with fractures of the humeral neck or the tuberosities [ 11 ]. Alternatively, Robinson et al. [ 12 ] have suggested referring to the latter as "complex" fracture-dislocations, as opposed to "simple" fracture-dislocations involving only an impression fracture (RHSL).
Computed tomography (CT) is required to evaluate the RHSL and other associated fractures and for preoperative planning. Irreducible dislocations with an RHSL are called "locked" or "fixed" [ 5 ], and cases neglected for more than three weeks are considered "chronic" [ 4 ]. Reverse Hill-Sachs lesions continue to grow while the shoulder remains dislocated [ 13 ].
The choice of procedure and prognosis depend on the time to surgery, the size of the RHSL and the possible presence of glenohumeral osteoarthritis. Conservative treatment can be effective in promptly diagnosed cases with stable shoulders and minor bone defects (less than 25% of the articular surface) after closed reduction [ 6 ]. Locked posterior shoulder dislocations with an RHSL involving 25–40% of the articular surface can be repaired by transposition of the subscapularis muscle (McLaughlin procedure) [ 14 , 15 ], lesser tuberosity transposition (Hawkins et al.’s modified McLaughlin procedure) [ 15 , 16 , 17 ], a modified McLaughlin procedure augmented with an autograft from the iliac crest [ 18 ], reconstruction of the humeral head defect using an allograft [ 19 , 20 ], rotational osteotomy of the humerus [ 21 , 22 ] or posterior bone block [ 23 ]. Cases in which the RHSL involves more than 40% of the articular surface are usually treated by shoulder replacement surgery, either hemiarthroplasty [ 24 ], anatomic total shoulder arthroplasty [ 24 , 25 ], or reverse total shoulder arthroplasty [ 26 ].
The purpose of this study was to evaluate the outcomes of open reduction and stabilisation of chronic locked posterior shoulder dislocations using the McLaughlin or modified McLaughlin procedure.
Study design
This was a retrospective investigation of twelve patients with chronic locked posterior shoulder dislocations operated on between 2000 and 2021 by two surgeons (LNJ and EGH) in two institutions (Hôpital Privé Jean Mermoz, Lyon, France and Foișor Orthopaedic Hospital, Bucharest, Romania).
Pre- and postoperative data
The data considered included the mechanism of injury, the active range of motion of the shoulder before and after surgery (anterior elevation, abduction, external rotation elbow at side, and internal rotation (Figs. 1 and 2 )) pre- and postoperative Constant–Murley scores [ 27 , 28 ], and subjective results at last follow-up (satisfaction on a 5-point Likert scale and subjective shoulder value (SSV) scores [ 29 ]). Internal rotation was evaluated using the Constant–Murley scale [ 27 , 28 ] based on the highest position reached by the patient’s thumb on their back. Strength in external rotation was measured using the Medical Research Council Manual Muscle Testing scale [ 30 ]. Shoulder X-rays (anteroposterior and scapular Y images , Figs. 3 and 4 ) and CT scans (Figs. 5 and 6 ) were also evaluated. We measured the size of the defect on CT-scans in the axial plane (alpha axial angle) using the method described by Moroder et al. [ 31 ]. We estimated the percentage of the involved articular surface, in the axial plane, considering the angular defect on the humeral joint surface in relation with the entire humeral articular surface [ 31 ]. Post-operatively, all patients were followed-up radiologically (x-rays and in two cases CT-scans), however we did not evaluate the healing of the subscapularis using ultrasonography or MRI.

Locked posterior shoulder dislocation (right shoulder), preoperative physical examination. Photographs of the right arm of a patient in ( a ) active anterior elevation and ( b ) active external rotation elbow at side
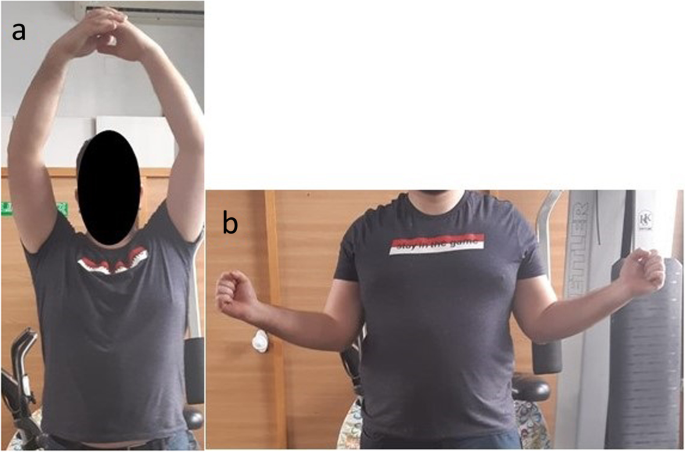
Locked posterior shoulder dislocation (right shoulder), postoperative physical examination. Photographs of the right arm of a patient with locked posterior shoulder dislocation treated with the modified McLaughlin procedure in ( a ) active anterior elevation and ( b ) active external rotation elbow at side

Locked posterior shoulder dislocation (right shoulder), preoperative imaging. a Anteroposterior and ( b ) scapular Y view X-ray images of the right shoulder of a patient with locked posterior shoulder dislocation
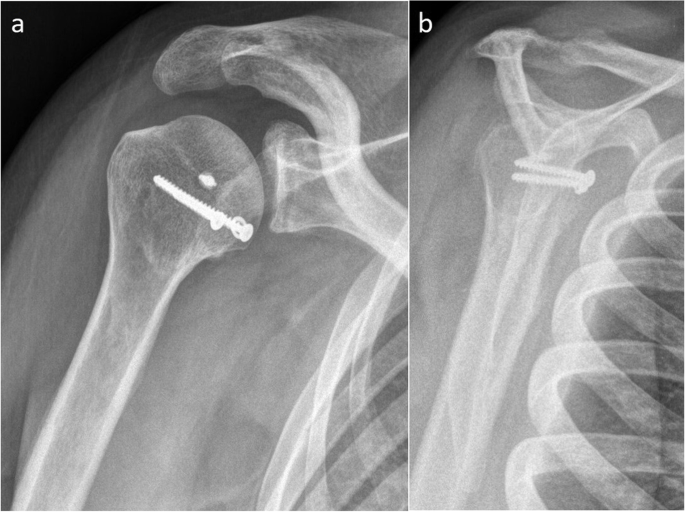
Locked posterior shoulder dislocation (right shoulder), postoperative imaging. a Anteroposterior and ( b ) scapular Y view X-ray images of the right shoulder of a patient with locked posterior shoulder dislocation treated with the modified McLaughlin procedure
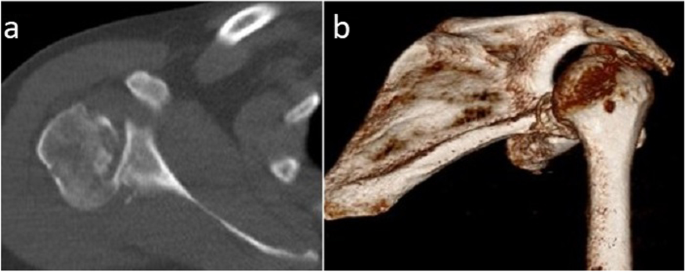
Locked posterior shoulder dislocation (right shoulder), preoperative imaging. a Axial and ( b ) three-dimensional reconstructed computed tomography images of the right shoulder of a patient with locked posterior shoulder dislocation
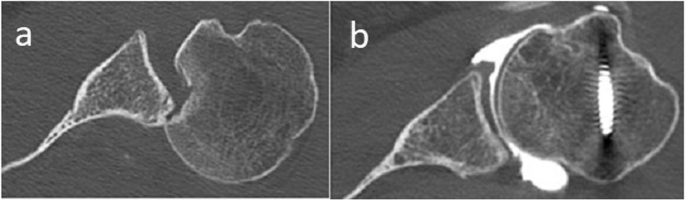
Locked posterior shoulder dislocation (left shoulder), pre- versus postoperative imaging. a Preoperative and ( b ) postoperative axial computed tomography images of a the left shoulder of a patient with locked posterior shoulder dislocation treated with the modified McLaughlin procedure
All operations were performed using a deltopectoral approach, with the patient under general anaesthesia in the beach chair position.
In patients treated with the McLaughlin procedure ( n = 2), the cranial two-thirds of the subscapularis tendon was released from its insertion on the lesser tuberosity. The tendon was marked with strong non-absorbable suture and was retracted medially. The RHSL and the glenoid were inspected after removing all fibrous tissue present. A blunt Hohmann retractor was placed between the humeral head and the glenoid. The joint was reduced using lateral distraction and gradual external rotation and the remaining humeral head cartilage and RHSL were evaluated. The base of the RHSL was rasped to obtain a bleeding surface. The subscapularis tendon was then transferred inside the RHSL, as close as possible to the medial edge, using either transosseous sutures (one case) or suture anchors (one case).
In patients treated with the modified McLaughlin procedure ( n = 10), the lesser tuberosity was osteotomised laterally from the bicipital groove up to the level of the RHSL. The subscapularis tendon was tagged with strong non-absorbable suture and the lesser tuberosity was retracted medially. After inspecting the joint and RHSL and preparing the RHSL as described above, the lesser tuberosity was transferred inside the RHSL, close to its medial edge and fixed with cancellous screws and washers. An additional anchor was inserted in the RHSL in four cases (metallic in two cases, resorbable in two cases) along with sutures passed through the subscapularis tendon. No graft was used.
The stability of the joint was evaluated at the end of the procedure.
Postoperative management
Patients wore a shoulder brace maintaining the shoulder in neutral or external rotation (mainly depending on the available brace type) for 4 to 6 weeks. Hand and elbow mobilisation began from the first day after surgery. Shoulder rehabilitation was started after removal of the brace, beginning with self-rehabilitation and passive mobilisation. Active shoulder mobilization was started at about 6 weeks for patients immobilized for 4 weeks and at about 8 weeks for patients immobilized for 6 weeks.
Statistical analysis
Categorical variables were summarised as frequencies. Continuous variables were expressed as mean ± standard deviation and compared before and after surgery using paired t tests. Independent samples t tests were run to compare the postoperative results. Differences were considered statistically significant at p < 0.05. All analyses were performed using IBM SPSS Statistics, version 24.
The average age at surgery was 48.2 ± 13.3 years (range, 30–67 years). Ten of the twelve patients were men. The average delay between injury and surgery was 13.5 ± 9.7 weeks (range, 3–32 weeks).
The cause of the dislocation was in one case, electrocution, in one case reflex epilepsy, in one case, unclear (apparently, the dislocation occurred when the patient rolled over in bed), and in the nine remaining cases, trauma (three motorcycle accidents, and six falls).
The initial dislocation was associated with a humeral fracture (other than the RHSL) in 8 of the 12 patients (66.7%), an isolated lesser tuberosity fracture in three cases, an oblique fracture of the proximal third of the humerus in two cases, and in one case each a spiral humeral shaft fracture, a fracture of the surgical neck and lesser tuberosity, and a multifragmentary fracture of the proximal humerus including the surgical neck, and the lesser and greater tuberosity. In all these cases of complex posterior shoulder fracture-dislocations, the associated fractures were initially treated conservatively. The posterior dislocation was missed on initial presentation in all but one case, in which, after closed reduction, the dislocation recurred. The associated fractures had healed at the time of surgery in six of eight cases because the patients presented late. In the two remaining cases, the unhealed lesser tuberosity fragment was fixed at the level of the RHSL.
The average alpha angle was 46.9° ± 7.9° (32.1°—59.5°). The RHSL represented on average 25.6% ± 5% (17.1%-36%) of the articular surface.
The McLaughlin procedure was used in two cases (16.7%) and the modified McLaughlin procedure in ten cases (83.3%).
The postoperative immobilisation period was four weeks in three patients (25%) and six weeks in nine patients (75%). The shoulder was immobilised in external rotation in six patients (50%) and in neutral rotation in six patients (50%).
One of the patients, a 44-year-old male, treated with the modified Mclaughlin procedure in 2014, had the last follow-up at 43 days postoperatively. The patient was satisfied with the result, had no pain, no early complications, and the reduction was maintained. Because of the very short follow-up, we decided to exclude this patient from our clinical results. The following analysis was performed on the remaining eleven patients.
The average delay between injury and surgery was 14.2 ± 9.9 weeks (range, 3–32 weeks).
The average postoperative follow-up, when the SSV, Constant score and shoulder range-of motion were recorded, was 37 ± 58 months (range, 6–206 months).
Pre- and postoperative clinical variables are compared in Table 1 .
Six patients (54.5%) were satisfied and five patients (45.5%) were very satisfied with postoperative outcomes.
The average postoperative SSV was 86.4 ± 11.1 (range 70–100). The strength in external rotation elbow at side was grade 5 in all seven cases in which it was evaluated.
All clinical variables increased significantly between pre- and postoperative assessments (Table 1 ). None of the patients had a recurrence of the dislocation on the operated shoulder. There were no implant-related, infectious or neurological complications. At last follow-up (12 months), one patient had avascular necrosis of the humeral head (Cruess stage IV [ 32 ]) and two patients had glenohumeral osteoarthritis (Samilson-Prieto Allain stages 2 and 3 [ 33 , 34 ], respectively).
There were no significant differences between the outcomes of patients treated with McLaughlin and modified McLaughlin procedures (independent samples t test, p > 0.05 for all the followed clinical variables). Also, the results of cases operated by LNJ or EGH were similar for all the observed clinical variables (independent samples t test, p > 0.05), with the exception of the normalized Constant score, which was better in the group of patients operated by LNJ (independent samples t test, p = 0.04).
The clinical results obtained with the original or modified McLaughlin procedures in patients with locked posterior shoulder dislocation were favourable and comparable with those of other published studies [ 7 , 17 , 18 , 35 ].
McLaughlin called posterior shoulder dislocation a "diagnostic trap" [ 36 ] because of the high percentage of cases missed on initial presentation. This was also the case in our study, with a significant delay between dislocation and reduction (14 weeks on average). However, even with this treatment delay in a traumatic intra-articular pathology, the clinical outcomes were still favourable, with significant improvements in all clinical variables. Also, all operated shoulders remained stable. It has to be noted that in our study the RHSL was moderate on average and this might explain our good results. A larger average RHSL would have been associated with a poorer result and, in some cases, the necessity of shoulder replacement.
These outcomes contrast with the results of the wide range of open reduction and stabilisation techniques used in chronic anterior shoulder dislocations, where a high incidence of re-subluxation and early osteoarthritis have been reported [ 37 ]. The Latarjet procedure, otherwise very successful, is considered by Walch et al. [ 38 ] to be contraindicated for locked anterior shoulder dislocations. Li et al. [ 39 ] evaluated the effectiveness of the Latarjet procedure in patients with chronic anterior dislocation and found an overall rate of postoperative redislocation or subluxation of 48%. The authors noted that in cases where the reduction was possible through a subscapularis-splitting approach, no postoperative instability was encountered [ 39 ]. However, in these chronic cases it can be very difficult to obtain reduction without a subscapularis tenotomy [ 37 , 39 ].
Nevertheless, missed diagnoses of posterior shoulder dislocations – and thereby in most cases, the need for surgery – could easily be avoided by increasing orthopaedic surgeons’ and emergency doctors’ awareness of this pathology.
The proportion of cases with an associated fracture (complex posterior fracture-dislocations, 73%) was comparable to the value reported in a literature review of locked posterior shoulder dislocations (75.8%) [ 4 ]. The incidence of glenohumeral osteoarthritis was higher than reported in the same review (18.2% vs. 6.7% [ 4 ]). However, one of the two patients had pre-existing osteoarthritis (Samilson-Prieto Allain stage 1 before surgery, which progressed to stage 2 at 19 months’ follow-up) and the other developed osteoarthritis (Samilson-Prieto Allain stage 3) a very long time (more than 17 years) after surgery. The latter patient was very satisfied with the result of surgery at last follow-up, and had 110° of active anterior elevation, 25° of active external rotation, elbow at the side, and could reach L3 with his thumb on internal rotation. His normalised Constant score was 98.5%. The other patient with shoulder osteoarthritis (Samilson-Prieto 2) was satisfied with the result of surgery, had 160° of active anterior elevation, 40° of active external rotation, elbow at side, could reach L5 with his thumb, and had a normalised Constant score of 81.1%. None of the patients required shoulder arthroplasty.
There was one case of avascular necrosis (9%), in keeping with the reported incidence in the literature (3.5%) [ 4 ] given the number of patients in the study. This case (Cruess stage IV) developed soon after surgery, after a long delay between dislocation and surgical reduction (23 weeks). The patient had a good clinical outcome (no pain and acceptable function) and did not require shoulder arthroplasty.
There were no postoperative subluxations or re-dislocations. The patient with epilepsy had posterior dislocation of the contralateral shoulder caused by another seizure, but the operated shoulder remained stable.
The modified McLaughlin procedure addresses the problem of poor healing of the transferred subscapularis at the level of the RHSL in the classic McLaughlin procedure. The transfer of the lesser tuberosity together with the subscapularis should lead to faster and more predictable bone-to-bone healing.
Hawkins et al. [ 15 ] achieved equally good results with McLaughlin and modified McLaughlin procedures. These authors also reported the results of five revisions of failed McLaughlin procedures performed by other surgeons and ascribed these failures either to the RHSL being too large for this technique or to the cartilage being too severely damaged at the time of the initial surgery.
The most commonly described treatments for chronic locked posterior shoulder dislocation are the McLaughlin procedure (classic or modified) and segmental reconstruction of the humeral head with a bone graft. Both are valid alternatives and have been shown to have consistently good long term outcomes and low complication rates [ 19 , 20 , 37 , 40 ].
In our study, the classic McLaughlin procedure was used in only two cases, with a RHSL of 17.1% and 17.9%, respectively. The reduction delay was in one case 3 weeks. However, in the other case the reduction delay was 25 weeks. The clinical results in both cases were good, with a normalized Constant score of 85% and 95%, respectively. The clinical result was better in the case of the patient with a much longer reduction delay.
Proximal humerus derotational osteotomy [ 21 , 22 , 41 ] can also lead to good outcomes in patients without severe articular cartilage damage. However, because of the technical complexity of the procedure and the risk of humeral head necrosis and osteoarthritis progression, some surgeons only consider derotational osteotomy as a salvage procedure when there are no other treatment options [ 7 ].
Posterior bone block has also been used to treat chronic locked posterior dislocations, with satisfactory mid-term clinical results but a high rate of postoperative osteoarthritis [ 23 ].
Results could still potentially be improved by using less invasive techniques. Arthroscopic McLaughlin procedures have recently been described [ 42 , 43 ]. A recent comparison [ 44 ] of the outcomes of open modified McLaughlin and arthroscopic McLaughlin procedures found that while there were no significant differences in terms of clinical results or subscapularis strength recovery, the arthroscopic McLaughlin procedure was associated with a better sense of stability and well-being.
The limitations of this study include its retrospective nature, small number of patients (which reflects the rarity of this pathology), the fact that it was conducted in only two centers and, in some cases, relatively short follow-up. As a result, this study suffers from inadequate case representation and case selective bias. However, this is a very rare pathology so most of the series in the literature have the same weaknesses.
This group of patients with chronic locked posterior shoulder dislocation treated using the McLaughlin or the modified McLaughlin procedure had good clinical outcomes, even when surgical reduction was significantly delayed.
Availability of data and materials
The datasets used and/or analysed in this study are available from the corresponding author on reasonable request.
Abbreviations
Reverse Hill–Sachs Lesion
Kowalsky MS, Levine WN. Traumatic posterior glenohumeral dislocation: classification, pathoanatomy, diagnosis, and treatment. Orthop Clin North Am. 2008;39(4):519–33.
Article Google Scholar
Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108(5):288–90.
Robinson CM, Aderinto J. Posterior shoulder dislocations and fracture-dislocations. J Bone Joint Surg Am. 2005;87(3):639–50.
Basal O, Dincer R, Turk B. Locked posterior dislocation of the shoulder : A systematic review. EFORT Open Rev. 2018;3(1):15–23.
Kelly MJ, Holton AE, Cassar-Gheiti AJ, Hanna SA, Quinlan JF, Molony DC. The aetiology of posterior glenohumeral dislocations and occurrence of associated injuries: a systematic review. Bone Joint J. 2019;101B(1):15–21.
Guehring M, Lambert S, Stoeckle U, Ziegler P. Posterior shoulder dislocation with associated reverse Hill-Sachs lesion: Treatment options and functional outcome after a 5-year follow up. BMC Musculoskelet Disord. 2017;18(1):1–7.
Babhulkar A, Unnithan V, Patil P. A treatment algorithm for locked posterior dislocation of shoulder. J Arthrosc Joint Surg. 2018;5(2):90–8.
Moroder P, Tauber M, Scheibel M, Habermeyer P, Imhoff AB, Liem D, et al. Defect characteristics of reverse hill-sachs lesions. Am J Sports Med. 2016;44(3):708–14.
Abdel-Hameed SK, Abdel-Aal MA. New technique in reconstructing humeral head defect in locked posterior dislocation of the shoulder: a case series of nine patients. Eur Orthop Traumatol. 2015;6(3):157–62.
Rouleau DM, Hebert-Davies J. Incidence of associated injury in posterior shoulder dislocation: Systematic review of the literature. J Orthop Trauma. 2012;26(4):246–51.
Kokkalis ZT, Iliopoulos ID, Antoniou G, Antoniadou T, Mavrogenis AF, Panagiotopoulos E. Posterior shoulder fracture–dislocation: an update with treatment algorithm. Eur J Orthop Surg Traumatol. 2017;27(3):285–94.
Robinson CM, Akhtar A, Mitchell M, Beavis C. Complex posterior fracture-dislocation of the shoulder: Epidemiology, injury patterns, and results of operative treatment. J Bone Joint Surg Am. 2007;89(7):1454–66.
Cohen M, Fonseca R, Amaral MVG, Monteiro MT, Filho GRM. Treatment of chronic locked posterior dislocation of the shoulder with the modified McLaughlin procedure. J Shoulder Elbow Surg. 2022;31(1):100–6.
McLaughlin HL. Locked posterior subluxation of the shoulder: diagnosis and treatment. Surg Clin North Am. 1963;43(6):1621–2.
Article CAS Google Scholar
Hawkins MD, Neer CS, Pianta RM, Mendoza FX. Locked Posterior Dislocation of the Shoulder. J Bone Joint Surg Am. 1987;69(1):9–18.
Castagna A, Delle Rose G, Borroni M, Markopoulos N, Conti M, Maradei L, et al. Modified MacLaughlin procedure in the treatment of neglected posterior dislocation of the shoulder. Chir Organi Mov. 2009;93(Suppl 1):1–5.
Google Scholar
Shams A, El-Sayed M, Gamal O, ElSawy M, Azzam W. Modified technique for reconstructing reverse Hill-Sachs lesion in locked chronic posterior shoulder dislocation. Eur J Orthop Surg Traumatol. 2016;26(8):843–9.
Khira YM, Salama AM. Treatment of locked posterior shoulder dislocation with bone defect. Orthopedics. 2017;40(3):e501–5.
Gerber C, Catanzaro S, Jundt-Ecker M, Farshad M. Long-term outcome of segmental reconstruction of the humeral head for the treatment of locked posterior dislocation of the shoulder. J Shoulder Elbow Surg. 2014;23(11):1682–90.
Martinez AA, Navarro E, Iglesias D, Domingo J, Calvo A, Carbonel I. Long-term follow-up of allograft reconstruction of segmental defects of the humeral head associated with posterior dislocation of the shoulder. Injury. 2013;44(4):488–91.
Keppler P, Holz U, Thielemann FW, Meinig R. Locked posterior dislocation of the shoulder: Treatment using rotational osteotomy of the humerus. J Orthop Trauma. 1994;8(4):286–92.
Ziran B, Nourbakhsh A. Proximal humerus derotational osteotomy for internal rotation instability after locked posterior shoulder dislocation: Early experience in four patients. Patient Saf Surg. 2015;9(1):1–5.
Aksekili MAE, Mahmut U, Çetin I, Yüksel K, Beçici V, Bozkurt M. Posterior bone block of chronic locked posterior shoulder dislocations with glenoid augmentation : a retrospective evaluation of ten shoulders. Int Orthop. 2015;40(4):813–20.
Wooten C, Klika B, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Anatomic shoulder arthroplasty as treatment for locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 2014;96(3):1–6.
Cheng SL, Mackay FCMB, Richards RR, Toronto FC. Treatment of locked posterior dislocation of the shoulder by total shoulder arthroplasty. J Shoulder Elbow Surg. 1997;6:11–7.
Raiss P, Edwards TB, Bruckner T, Loew M, Zeifang F, Walch G. Reverse arthroplasty for patients with chronic locked dislocation of the shoulder (type 2 fracture sequela). J Shoulder Elbow Surg. 2017;26(2):279–87.
Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4.
Constant CR, Gerber C, Emery RJH, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17(2):355–61.
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599–605.
Dyck PJ, Boes CJ, Mulder D, Millikan C, Windebank AJ, Dyck PJ, et al. History of standard scoring notation and summation of neuromuscular signs A current survey and recommendation. J Peripher Nerv Syst. 2005;10(2):158–73.
Moroder P, Tauber M, Hoffelner T, Auffarth A, Korn G, Bogner R, et al. Reliability of a New Standardized Measurement Technique for Reverse Hill-Sachs Lesions in Posterior Shoulder Dislocations. Arthroscopy. 2013;29(3):478–84.
Cruess R. The current status of avascular necrosis of the femoral head. Clin Orthop Relat Res. 1978;131:309–11.
Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65(4):456–60.
Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80(6):841–52.
Kokkalis ZT, Mavrogenis AF, Ballas EG, Papagelopoulos PJ, Zoubos AB. Bilateral neglected posterior fracture-dislocation of the shoulders. Orthop. 2012;35(10):e1537–41.
McLaughlin HL. Posterior dislocation of the shoulder. J Bone Joint Surg Am. 1952;24(A3):584–90.
Sahu D, Rathod V, Phadnis A, Shyam A. Results and complications of head preserving techniques in chronic neglected shoulder dislocation: a systematic review. J Shoulder Elbow Surg. 2021;30(3):685–94.
Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10(1):15–24.
Li Y, Jiang C. The effectiveness of the latarjet procedure in patients with chronic locked anterior shoulder dislocation: a retrospective study. J Bone Joint Surg Am. 2016;98(10):813–23.
Diklic ID, Ganic ZD, Blagojevic ZD, Nho SJ, Romeo AA. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Joint Surg Br. 2010;92(1):71–6.
Porteous MJ. Humeral Rotation Osteotomy for Chronic Posterior Dislocation of the Shoulder. J Bone Joint Surg Br. 1990;72(3):468–9.
Besnard M, Audebert S, Godenèche A. Arthroscopic McLaughlin Procedure for Treatment of Posterior Instability of the Shoulder With an Engaging Reverse Hill-Sachs Lesion. Arthrosc Tech. 2019;8(12):e1491–4.
Bernholt DL, Lacheta L, Goldenberg BT, Millett PJ. Arthroscopic Knotless Modified McLaughlin Procedure for Reverse Hill-Sachs Lesions. Arthrosc Tech. 2020;9(1):e65-70.
Ippolito G, Zitiello M, De Marinis G, D’Angelo F, Surace MF, Ronga M, et al. Posterior shoulder dislocation with engaging reverse hill-sachs lesion: a retrospective study of ten patients treated with arthroscopy or open reduction and stabilisation. J Clin Med. 2021;10(7):1410.
Download references
Acknowledgements
Not applicable
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Carol Davila University of Medicine and Pharmacy, 37 Dionisie Lupu, 020021, Bucharest, Romania
Emil George Haritinian, Ioan Cristian Stoica, Roman Popescu & Gavril Lucian Gheorghievici
Foișor Orthopaedic Hospital, 35-37 Ferdinand I, 021382, Bucharest, Romania
Emil George Haritinian, Ioan Cristian Stoica & Gavril Lucian Gheorghievici
Ramsay Santé, Hôpital Privé Jean Mermoz, Centre Orthopédique Santy, 24 Avenue Paul Santy, 69008, Lyon, France
Laurent Nové-Josserand
You can also search for this author in PubMed Google Scholar
Contributions
Emil George Haritinian: study design, data collection and analysis and article writing.Ioan Cristian Stoica: study design, supervision. Roman Popescu: data collection and analysis. Gavril Lucian Gheorghievici: data collection and analysis. Laurent Nové-Josserand: study design, supervision, data analysis and article writing. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Emil George Haritinian .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by Ramsay Santé Ethical Committee (COS-RGDS-2022–04-001-NOVEJOSSERAND-L /12/04/2022) and Foișor Orthopaedic Hospital Ethical Committee (3421/04.04.2022).
All methods were performed in accordance with the relevant guidelines and regulations.
All patients included in this study provided informed consent for their participation.
Consent for publication
This article contains no identifying images or details. However, it includes clinical images of one patient. Written informed consent for the clinical details and clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Haritinian, E.G., Stoica, I.C., Popescu, R. et al. Treatment and outcomes of chronic locked posterior shoulder dislocations: a retrospective case series. BMC Musculoskelet Disord 24 , 82 (2023). https://doi.org/10.1186/s12891-023-06200-8
Download citation
Received : 11 October 2022
Accepted : 25 January 2023
Published : 31 January 2023
DOI : https://doi.org/10.1186/s12891-023-06200-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Posterior shoulder dislocation
- Locked shoulder dislocation
- Chronic shoulder dislocation
- Modified Mclaughlin
BMC Musculoskeletal Disorders
ISSN: 1471-2474
- Submission enquiries: [email protected]
- General enquiries: [email protected]
NEGLECTED SHOULDER PRESENTATION (A Study of 61 Cases)
BIMAN CHAKRAVARTY, M.B.B.S., D.G.O. (Cal.), M.R.C.O.G. (Eng.)
Neglected shoulder presentation is very rapid or slow, showing signs of a rare condition in more developed foetal distress. The maternal condi parts of the world. That it is not un tion of almost all was one of exhaus common in the less developed coun tion, partly from persistent uterine tries is indicated by the fact that 61 contractions; in many of them the ute cases were collected in a period of rus was tonically contracted with no only two years. All the cases were relaxation in beween the contractions. delivered in a district hospital. The A number of them had rise of tem hospital serves a wide area and is the perature from superimposed infec only hospital with specialist service tion. in about forty square miles. The po pulation is a mixed one with various Incidence types of religious dogma and with a Garner et al. reported 65 cases in big percentage of illiterate people. 15 years in 27,249 deliveries-one in Many of them have yet to learn the 419 deliveries, Hall et al. gave an in importance of antenatal care. They cidence of 1 in 217. The present shun the hospital unless they are series was collected from 8000 deli forced to attend it. veries-an incidence of 7.5 per thou This paper does not deal with all sand. the cases of transverse lie that attend ed the hospital, but only those that Age came in very late in labour. As the Average age of the patients was 26 name suggests the cases were in such years, though there were patients in a condition on admission that they all age groups, the youngest being 15 required immediate interference; in years and the oldest 40. all of them the membranes had rup TABLE I tured for over four hours and in most cases one hand was prolapsed Up to 20 years 14 cases with or without prolapsed cord. Foe 21 years to 25 years 19 cases tal heart was not heard in more than 26 years to 30 years 19 cases 31 years to 35 years 5 cases 75 per cent cases on admission; in the 36 years to 40 years 4 cases rest foetal heart was feeble, either Department of Obstetrics and Gynaeco As shown in the above table the logy, Rao J. N. Roy Hospital, Berhampore, cases are mostly in the 20 to 35 years West Bengal, India. group.
t NEGLECTED SHOULDER PRESENTATION 753
Parity pitation was particularly difficult. The other case where hysterectomy The average parity of the patients was done, was an eighth gravida, 40 was 4.9. More than 75 % of the cases years old, for whom caesarean sec were grande multiparae i.e. they had tion was decided, but on laparatomy 5 or more pregnancies ; there were uterine rupture through the lower two cases who were eleventh parae, segment was detected. Subtotal hys ,. Seven of the cases were primigravi terectomy was performed along the dae, giving an incidence of 11% . Hall rupture and the patient made an un et al. report 8% primigravidae in eventful recovery. In one case of their series. twin pregnancy , whe;re the first baby TABLE II had shoulder presentation with hand 1st 2nd/4th 5th/7th 8th/11th prolapsed, caesarean section was per formed. Both the babies were born 8 23 19 11 alive; the second baby was present ing as vertex. Of the six destructive operations five had decapitation and I . Terminations one had evisceration. In 1963 in two To help analysis, the cases have cases of classical section rupture of been grouped in two different years. uterus was detected on laparotomy, ·The number of cases during the and so the section was followed by year 1962 was 23, in 1963 the num hysterectomy. One of them was a ber was 38. The author had the op ninth gravida, 38 years old, the other portunity to look after the cases who was 23 years old and had two child were admitted from the period of ren. In one case twin pregnancy re October 1962 to December, 1963. mained undiagnosed until the first During the period qf 1962 the 23 baby, who had a prolapsed hand, was cases terminated in the way as shown delivered by internal version. Intra in the following table (table III). venous ergometrine was injected with
Caesarean section Spontaneous Destructive Version Hysterectomy delivery operations Classical Lower
1962 1 1 6 10 5 2 1963 9 12 7 9 1 2
In 1962, in 4 cases of classical delivery of the baby. The presence caesarean section ligation of fallopian of the second baby was diagnosed tubes was done. In one case of des only after the first was delivered. The tructive operation rupture of the ute second baby was presenting by ver rus was detected following decapita tex, with the head above the pelvic tion, for which hysterectomy was brim. As soon as this misadventure performed. In this particular case was detected the second baby was de both hands were prolapsed and deca- livered as breech by internal version. 754 JOURNAL OF OBSTETRICS AND GYNAECOLOGY OF INDIA
The baby was alive and had no in Of the 38 cases in 1963, there were tracranial injury. The first baby was 39 babies including a pair of twins. found macerated on delivery. In an- . Of these only five living babies could other case of internal version in a be delivered. Three of the live-born fifth gravida, aged 35, the foetal heart babies were delivered by internal was heard on admission and cervix podalic version and two by caesarean was fully dilated. The membranes section. It was only in six cases that were ruptured about 6 hours before foetal heart was present on ,adrn'is she came in. It was decided to do an sion. Only one of the six babies was ·. internal version in the operation lost, the one which after-verson could theatre, with the patient prepared not be delivered easily due to con for caesarean section, if version fail- traction ring. . ed. The version was performed with Thirteen live-born babies out of 63 out much difficulty, but a contraction gives a percentage of 20 living-babies ring developed at the region of inter and 80 % foetal mortality, Garber et nal os and obstructed the delivery of al report foetal mortality of more the aftercoming head. Anaesthesia than 94 % when labour has be2n pro was deepened with increased con longed for more than 24 hours. centration of ether but the contrac tion ring persisted. It was only after Hospital Stay injecting adrenalin, one in thousand This district hospital is so much solution 1 c.c., intravenously tliat overcrowded that the normal deli the ring relaxed and the baby could very cases are· discharged 48 hours ... be delivered, but this long delay in after delivery. delivery of the aftercoming head led to foetal death. The baby weighed 7 TABLE IV lbs. and had irreversible asphyxia. In Hospital Stay another case during internal version Spontaneous delivery 3 days type II placenta praevia was detected. Intunal podalic version 4.3 The foetus was already dead and ver Destructive operations 5.5 sion was completed without causing Caesarean section 21.5 any vaginal bleeding. Of the 7 cases of destructive operations performed The cases of transverse lie that in 1963, 4 had decapitation and in delivered spontaneously had a hos three evisceration was performed. pital stay of only 3 days. Those with internal version required hos Foetal Salvage pitalization on the average for 4.3 days. The cases who had destructive Of the 23 cases in 1962 there were operations had an average stay of 5.5 24 babies including one pair of twins. days. The patients who had a caesa Of these 24, eight were live-born. rean section, on the other hand, re One of the twins died in the neonatal quired an average stay of 21.5 days. period from infection. All the eight One case had to stay as long as 57 living babies were delivered by cae days before being discharged cured. sarean section. Four cases had to stay more than a NEGLECTED SHOULDER PRESENTATION 755
month after caesarean section. The on admission was significant. The main postoperative complication was softening of the foetal bones perhaps infection. It is interesting to note helped in the process of expulsion in that patients who required hysterec stead of causing rupture of uterus, tomy had a smooth postoperative thougli most of the babies were not period, and they were discharged macerated. within a fortnight after operation. The author would not like to con clude that spontaneous delivery in Discussion neglected shoulder presentation is to In the Chapter on "Results of neg be expected in all cases but this series lected shoulder presentation" in the just shows that this type of termina British Obstetric and Gynaecological tion is not as rare as it is thought. Practice, MacLenan, Wrigley and Per Internal Version cival write that spontaneous deli very is possible, though extremely It is interesting to note that in the rare, when the lie is uncorn'!cted. In year 1962 there was only one case of this series of 61 cases, there have internal version, whereas in 1963, been 10 cases who delivered them there were 12 cases which were ter selves, the spontaneous delivery rate minated by internal podalic version. is, therefore, more than 16(; . In these 12 cases there was not a sin In all these 10 cases the baby was gle case of ruptured ut2rus. The dead. In all but one case the baby author feels that if internal version was over six pounds in weight. Only is carefully done, the risk of rupture four babies were macerated. One can be minimised. The decision can case was premature, of 32 weeks' only be made after the patient is pregnancy. Most of the cases of spon anaesthetised. If the uterus relaxes t:meous delivery ended by spontane and there is no contraction ring, in ous expulsion i.e. the entire foetus ternal version can be attempted. doubled up and was expelled, back Gentle manoeuvre is the secret. In foremost, the head and feet appearing some cases it was possible to pull last. Two patients were delivered by down the legs, the lie being corrected, spontaneous evolution, in which the the foetus was left to be delivered breech was driven down first and the spontaneously. This increased num baby was finally delivered as breech. ber of versions has minimised the It seems that if sufficient time is al number of caesarean sections. When lowed in labour these cases will either the foetal heart is present the author expel the foetus themselves or have would advise caesarean section even rupture of the uterus. Due to trans if the cervix is fully dilated. In cases port difficulties many of the patients of neglected shoulder presentation arrived in the hospital late in labour, the babies are moribund, if not al and perhaps that explains the high ready dead, and so it is advisable to rate of spontaneous delivery in this deliver them with minimum foetal series. The parity of the mother did manipulation which is possible only not influence this method of deli by caesarean section. Failure to fol very. That the babies were all dead low this rule cost the life of a 7 lb .
• 756 JOURNAL OF OBSTETRICS AND GYNAECOLOGY OF INDIA baby whose aftercoming head . was capitation thimble and wire saw. In obstructed by a contraction ring, as all cases after decapitation, explora has been described before. · · But the tion of the uterus was performed to '"' cases where the foetus was already exclude rupture of uterus. Some dead, internal version gave a much times the uterus that has ruptured better postoperative period than in before coming into the hospital is the caesarean section cases. These only diagnosed by exploration after cases usually are infected and give a removing the baby. In one of the stormy postoperative period. after a cases of this series, rupture was de major operation like caesarean sec tected after decapitation. In this case tion; they are mostly anaemic and decapitation was specially difficult stand blood loss adversely. In many because both the hands were prolaps the uterus is so much retracted that ed, and it is possible that manipula only a classical section can deliver the tions caused the rupture. The patient - baby. Classical section in a dehydrat required hysterectomy after decapita ed, anaemic, infected patient, is never tion and had an uneventful postopera very safe. Fortunately, in this group tave period. In no case of this series we did not lose any patient, but one was there any vesico-vaginal or case of caesarean section had to stay recto-vaginal fistula, but in cases in hospital as long as 57 days. The where there is risk of operative in lack of free availability of blood adds jury, bladder should be continuous- to the danger of section. ly drained for at least a week. All these cases had prophylactic antibio- " Destructive Operations tics. The cases of destructive opera Both eviscerations and decapita tion required hospitalization on the · tions are difficult operative proce average for only 5.5 days as against dures and the cases should be care 21.5 days after caesarean section. In fully chosen. This should always be a busy district hospital like this it undertaken by people who have suffi makes a difference in the burd2n on cient experience in these types of ope hospital beds. The author makes a rations. The type of destructive ope plea that in cases of neglected shoul ration will depend upon the most der presentation where the baby is approachable presenting part. As a dead, destructive operation gives . rule decapitation is a cleaner op2ra equally good results as caesarean sec- .,. ~ tion than evisceration and should be tion, if not better, in relation to ma preferred if the neck of the foetus is ternal morbidity and mortality. easy to approach. Both these opera In cases where the uterus is toni tions are meant for babies who are cally contracted, any uterine mani already dead. If carefully performed pulation, including decapitation, is there is very little risk of maternal in liable to fail and prove practically jury and a smooth postoperative dangerous, and in these cases caesa period is expected. In the present rean section is preferred. In Hall's series decapitation knife was used in series of 85 cases there were three the usual way. The author had no maternal deaths. All the deaths were ... opportunity to use Blond-Heidler de- in the first ten years of 1924 to 1958 .
. ' NEGLECTED SHOULDER PRESENTATION 757
There were no deaths in the later condition was also found in seven years. In the present series, of 61 primigravidae. In none of these pri cases there were no maternal deaths migravidae was any gross pelvic con though in 60 % cases vaginal delivery traction detected. Hall and O'Brien was undertaken. Antibiotics and ex found no cause in 79 7o of their series. pert anaesthesia have ~a~e vagi:r:al delivery safer. In India, m the dis Conclusion tricts blood is not yet freely available Neglected shoulder presentation is for tr'ansfusion and cannot be readily an avoidable condition. It can only organised in case of emergen~y. ~n be found in countries where antenatal view of this, caesarean sectwn m care is far from satisfactory. It is al neglected shoulder presentation ways associated with a very high foe should be carefully considered and tal mortality and maternal morbidity under the present conditions in this and mortality. The author has col country should be avoided if possible. lected 61 cases during a period of two Ceval Babumea of Istanbul seems to years in a district hospital and has have worked in similar circumstances analysed the results of the various as in India, and he has also ad methods of treatment. Where the vocated destructive operations when baby is alive caesarean section is the the baby is dead. He reports 26 case~ method of choice, but if the baby is without a maternal death . He had already dead internal podalic version two cases of ruptured uterus, one was or decapitation should be carefully _ treated conservatively and the other considered as possible alternative~. had hysterectomy. He quotes support Spontaneous expulsion may occur in from Eastman, Kurtz, Etal, and Ried. some cases but should not be awaited Discussing on Garber et al's paper for. Holmes commented that internal ver I am grateful to Dr. (Miss) Bose, sion was an ideal operation in its ap the lady medical officer of the Unit, propriate field and it would be wise for her help in collecting the cases. I to realize that· caesarean section was would like to thank Dr. Bhattacharya not a panacea for all obstetric compli for allowing me to collect the cases cation, and other obstetric operations that were under his care. My thanks still had a definite place as a means are due to Dr. Roy Choudhury, the of delivery. The author's experience Chief Medical Officer, and Dr. in this series is in complete agree Chakravarty, the Superintendent of ment with Holmes's view. the hospital, for allowing me to pub lish th2 hospital cases. I am grateful Aetiology to Mr. Mukherjee for kindly typing In this present series no cause for the manuscript for me. transverse presentation could be de tected in 58 cases. In one there was References pJacenta praevia and there were two cases of twins. No uterine abnorma- 1. Babuna, Ceval: Am. J. Obst. & , lity was detected in any case; 28 cas~s Gynec. 87, 1963. were grand multiparae, but this 2. Eastman, N. J.: Obstetrics, ed. 10, 29 758 JOURNAL OF OBSTE'l'lUCS AND OYNAECOLOGY OF. IN:OIA
New York, 1950, Applaton Century Obstetrics and Gynaecological Crofts, Inc. -Practice, ed., London, 1955, Heine 3. Garber, E. C. (Jr.), Fayetteville, mana, p. 631. N. C., Hudnall Wave, H. (Jr.)" ~. Kurtz, G. R., Stall, W. A., and Sat Richmond, V. A.: Am . .J. Obst. & tenspiel, E. and Bull E.: Margaret Gynec. 61: 62, 1951. Hagne Maternity Hospital 3: 18, 4. Hall Stanley C., O'Brien, Francis, 1950. B.: Am. J. Obst. & Gynec. 82: 1180, 7. Reid, D. E.: A Text-book of Obs 1961. tetrics, Philadelphia, 1962, W. B. 5 . Holland E. and Bourne, A.: British Saunders Company.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Orthop Case Reports
- v.5(4); Oct-Dec 2015
Neglected Anterior Dislocation of Shoulder: is surgery necessary? A Rare Case with review of literature
1 Department of Orthopaedics, R.n.cooper Municipal General Hospital, Bhaktivedanta Swami Marg, Juhu, Mumbai 400056
Tushar Ubale
Harish ugrappa, samir pilankar, atul bhaskar, satishchandra kale, introduction:.
Shoulder joint is the most frequently dislocated joint. However, it is rarely neglected and treatment is sought immediately. Delayed or neglected shoulder dislocations are difficult to manage and require extensive procedures to obtain good functional outcome. Very few cases are described in literature showing neglected shoulder dislocation with good functional range of movement. We report a case with 3 years of neglected anterior shoulder dislocation with preserved joint function.
Case Report:
A 40 years old gentleman presented withfracture distal end of the radius (left). On clinical examination we observed that he had anterior dislocation of his left shoulder which was confirmed on radiographic evaluation. He had history of seizures 3 years back, which may be the cause of dislocation which went unnoticed. On examination he had good range of motion without any pain. Patient could perform all routine activities with no major functional limitation. At three years after dislocation CT Scan showed neocavity formation.
Conclusion:
Neglected shoulder dislocation with preserved joint function without major functional limitation is a rare presentation. This condition should be kept in mind in patients with history of seizures. Proper evaluation and counseling of patients avoids extensive procedures and avoids complications of surgery. Observation can be a treatment option in patients with preserved range of movement especially involving non dominant handand having low functional demand. This report presents rare presentation of neglected shoulder dislocation highlighting its natural history and its outcome following conservative treatment.
Introduction
Shoulder joint is the most frequently dislocated joint. Anterior shoulder dislocation constitutes 95% of all shoulder dislocations, mainly caused by trauma and posterior dislocation is caused by indirect trauma like violent muscular contractions seen in epileptic attack and electrocution. Unilateral shoulder dislocation is most common constituting 85% of all dislocations [ 1 , 2 ]. Because of its typical presentation, it is rarely missed. Neglected shoulder dislocation presents with gross limitation of shoulder function and requires extensive procedures to obtain desired outcome. Also, there are many pathological changes in bony and soft tissue architecture in shoulder joint in case of neglected dislocations [ 3 , 4 ]. We present a rare case of anterior dislocation of shoulder following a seizure attack with preserved joint functions and no major functional limitation of joint function. In this report we bring this rare presentation of neglected shoulder dislocation highlighting its natural history and its outcome following conservative treatment.
Case presentation
A 31 years old right hand dominant gentleman presented to our orthopedic specialty clinic with fracture distal end radius on left side. On further evaluation, there was deformity in ipsilateral shoulder joint and asymmetry was present as compared to opposite side. There was an anterior globular bony swelling palpable with well defined margins. Transmitted movements from humerus were present confirming it to be bony humeral mass. There was wasting of deltoid muscle as compared to opposite side. Range of motion were flexion upto 170 degrees ( Fig 1A ), extension up to 10 degree ( Fig 1B ), internal rotation up to L3 ( Fig 1C ), and external rotation up to 30 degree ( Fig 1D ) and abduction up to 120 ( Fig 1E ) in both active and passive movements, further movements were restricted and mildly painful. Patient did not have any history of significant trauma to shoulder in past. However he gave a history of seizure attacks three years back following which he had shoulder pathology. He had taken antiepileptic treatment; however no treatment was taken for the shoulder. There were no further epileptic episodes and he was taking antiepileptic treatment. Radiographs of shoulder joint were taken which confirmed anteriorly dislocated humeral head ( Figure 2 ). Further views of shoulder joint were taken to check for any bony changes. They didn’t show any significant abnormality. CT scan showed anteroinferior dislocation with neocavity with pseudojoint formation ( Fig.3A , ,3B 3B , ,3C). 3C ). Chronic hillsachs lesion was also seen. MRI Scan showed anteroinferior shoulder dislocation with intact rotator cuff muscles ( Fig.4A , ,4B) 4B ) Since the patient had good functional range of movement we explained him the treatment options. He opted for non surgical line of management. Hence was given shoulder mobilization exercises. Presently patient is being followed up with no fresh complaints and maintained join movements.

(a,b,c,d & e): Clinical photographs showing functional range of movement of shoulder joint

Radiograph of joint showng anteroinferior dislocation of shoulder joint

(a,b,c & e): CT Scan showing anteroinferior dislocation with neocavity formation.

(a & b): MRI scan showing anteroinferior dislocation with intact rotator cuff muscles
Anterior dislocation of shoulder unlike posterior dislocation is most commonly traumatic in nature. The mechanism of anterior dislocation following trauma is that greater tuberosity abuts against acromion when arm is abducted and extended, causing leverage forces leading head to come out of glenoidcavity [ 5 ]. Posterior dislocation secondary to seizure attack is caused due to imbalance between strong internal rotators and weak external rotators and deltoid. The cause of anterior dislocation following seizure is postulated to be direct trauma due to collapse of patient hitting the floor [ 6 ]. Anterior dislocation of shoulder is commonly missed after seizure because of its unusual occurrence, post seizure drowsiness and subsequent medical management[ 5 ].
The term chronic dislocation of shoulder is applied to condition where there is loss of recognition of injury for at least 3 weeks [ 7 ] or 4weeks [ 8 ]. Many authors have described chronic dislocation with varying amount of duration at presentation. Rowe and Zarin presented eight patients with anterior dislocation with seven patients presenting at 3 week to 2 year interval and one patient at 10 year duration [ 7 ]. Goga presented 31 patients with chronic anterior dislocation with longest duration of failed recognition at 2 years [ 9 ]. Postacchini and Facchini presented five patients with 6 weeks as longest duration of failure of diagnosis[ 10 ].
Mansat et al showed five patients with 6 weeks to 3 years as the duration of missed diagnosis[ 11 ]. Mancini et al presented a case with 24 years of missed anterior shoulder dislocation [ 12 ]. Our case presented 10 years after the dislocation.
Treatment options for neglected shoulder dislocation include observation, manipulation, open reduction with or without allograft reconstruction, bankarts repair, capsulolabial repair and arthroplasty [ 7 , 13 ]. Surgical treatment for chronic dislocations is usually advocated for better functional outcome, however the results can be poor and unsatisfactory[ 12 ].
Very few cases describe chronic dislocation of shoulder with good functional range of motion which were treated nonsurgically. Table shows epidemiological details of patients reported with asymptomatic neglected anterior shoulder dislocation. Essi et al showed a case with 15 years old neglected anterior shoulder dislocation in a 35 year old lady with good functional range of movement and neocavity formation leading to preserved movements [ 14 ]. Similar neocavity formation seen in a case described by Mancinni et al with 24 years of neglected dislocation ion a 74 year old lady with low functional demand [ 12 ]. Jerosch et al [ 3 ] presented a case of a young male with preserved movements 4 years after missed diagnosis. This case didn’t show neocavity formation, but had a large Hill Sachs lesion which locked the head in dislocated position. In our case we found neocavity formation with large hill Sachs lesion.
Thus, we conclude that neglected shoulder dislocation after many years eventually leads to neocavity formation. Observation can be an option if patient presents late and surgical treatment is likely to have unsatisfactory results. Low demand patient with involvement of non dominant hand can be observed with good functional outcome.
Clinical Message
Neglected shoulder dislocation can present with neocavity formation and preserved joint function. In such cases, observation can be a treatment option especially when surgical option gives unsatisfactory result. This is particularly important in a patient with low demand occupation and nondominant hand.
Conflict of Interest: Nil
Source of Support: None

IMAGES
VIDEO
COMMENTS
1. Contracted Pelvis. A very narrow pelvis in the mother can cause a shoulder presentation to occur. 2. Placenta Previa. A condition where the placenta covers the uterus opening, either completely or partially. This makes it difficult for your baby's head to enter the pelvic brim. 3. Intra-Uterine Fetal Death.
7.6.1 Diagnosis. The uterus is very wide: the transverse axis is virtually equivalent to the longitudinal axis; fundal height is less than 30 cm near term. On examination: head in one side, breech in the other (Figures 7.1a and 7.1b). Vaginal examination reveals a nearly empty true pelvis or a shoulder with—sometimes—an arm prolapsing from ...
A neglected shoulder presentation is an extremely rare obstetric complication in developed countries; however, it is a reality in low-income parts of the world. Our tertiary care center is located in the rural and remote part of eastern Turkey. In this low-income region, many pregnant women deliver at home and go to the hospital only in case of ...
INTRODUCTION. Transverse lie refers to a fetal presentation in which the fetal longitudinal axis lies perpendicular to the long axis of the uterus. It can occur in either of two configurations: The curvature of the fetal spine is oriented downward (also called "back down" or dorsoinferior), and the fetal shoulder presents at the cervix ( figure ...
Shoulder Presentation (Transverse or Oblique lie) The longitudinal axis of the foetus does not coincide with that of the mother. These are the most hazardous malpresentations due to mechanical difficulties that occur during labour . The oblique lie which is deviation of the head or the breech to one iliac fossa, is less hazardous as correction ...
A shoulder presentation is a malpresentation at childbirth where the baby is in a transverse lie (its vertebral column is perpendicular to that of the mother), thus the leading part (the part that first enters the birth canal) is an arm, a shoulder, or the trunk.While a baby can be delivered vaginally when either the head or the feet/buttocks are the leading part, it usually cannot be expected ...
Prenatal Diagnosis; International Journal of Gynecology & Obstetrics; ... All cases where IPV was performed for neglected shoulder presentation with intrauterine fetal demise (IUFD) at Padhar Hospital over a 19-month period from March 2006 to September 2007 were identified. Permission to both conduct IPVs in these women (Padhar Hospital/MSO/68 ...
1.5 Diagnosis. The diagnosis is commonly made during a vaginal examination; the examiner feels a soft, usually pulsatile structure through the membranes or with membranes ruptured. ... With time, the retraction ring rises high, and the uterus will rupture especially in a multi with neglected shoulder presentation. In primi, obstructed labor and ...
4.1.3 Auscultation. The fetal heart is heard best below the umbilicus and does not have diagnostic significance. Vaginal examination in early labor reveals a nearly empty lower of the uterus or a shoulder can be felt. "Grid iron" feel of the rib is felt, if fetal thorax is over the internal os.Because of the ill-fitting fetal part at the lower pole, membranes will be bulging and herniating ...
Management of neglected shoulder presentation. Management of neglected shoulder presentation. Management of neglected shoulder presentation BJOG. 2009 Dec;116(13):1695-6. doi: 10.1111/j.1471-0528.2009.02376.x. Author F E Okonofua 1 Affiliation 1 Department of Obstetrics and ...
In case of neglected shoulder presentation (Chapter 7, Section 7.6.1), have an assistant apply traction to the prolapsed arm (do not try to section the arm first, as it can be used to pull the body downward). Slide one hand behind the foetus and surround the neck with thumb and index finger, like a necklace.
In the era of modern obstetric care, the neglected shoulder presentation is usually limited in developing countries which increase the risk of the morbidity and mortality of both mother and fetus.
Neglected shoulder presentation with fetal demise was diagnosed and was taken up to operating room. Halothane inhalation was given to relax ... A neglected shoulder presentation is an extremely
Presentation of case. We presented a 27-year-old male patient with deformity on his left shoulder. The patient has suffered a ten-month-neglected anterior shoulder dislocation with a Hill-Sachs lesion. The treatment was open reduction combined with Latarjet procedure. Evaluation of treatment was performed three months after surgery.
Introduction. Posterior dislocation of the shoulder is a rare injury (< 4% of all shoulder dislocations). The diagnosis of this injury is often missed (60-79%) on initial examination , , , .The special clinical and radiographic characteristics made McLaughlin consider it as a "diagnostic trap".. Although the imaging technique is advancing and it is well known now that it is important to ...
Posterior shoulder dislocations are rare injuries that are often missed on initial presentation. Cases left untreated for more than three weeks are considered chronic, cannot be reduced closely (they become locked) and are usually associated with a significant reverse Hill-Sachs defect. The aim of this study was to evaluate the outcomes of chronic locked posterior shoulder dislocations treated ...
Table I Clinical features at baseline of patients who presented with a diagnosis of neglected dislocation shoulder. Serial no. Age Sex Affected side Duration of neglect (mo) Glenoid bone loss Associated pathologies Range of motion CS ... late presentation of locked anterior shoulder dislocation: a case report. JSES Rev Rep Tech. 2022; 2: 380 ...
NEGLECTED SHOULDER PRESENTATION (A Study of 61 Cases) by BIMAN CHAKRAVARTY, M.B.B.S., D.G.O. (Cal.), M.R.C.O.G. (Eng.) Neglected shoulder ... The presence caesarean section ligation of fallopian of the second baby was diagnosed tubes was done. In one case of des only after the first was delivered. The tructive operation rupture of the ute ...
Introduction. Posterior dislocation of the shoulder is a rare injury (< 4% of all shoulder dislocations). The diagnosis of this injury is often missed (60-79%) on initial examination [1], [2], [3], [4].The special clinical and radiographic characteristics made McLaughlin [4] consider it as a "diagnostic trap".. Although the imaging technique is advancing and it is well known now that it ...
Introduction. Neglected shoulder dislocation is a rare condition [].Neglected dislocation of the shoulder when reported in literature is usually of the anterior type with very few posterior types reported [2, 3].A pertinent fact that usually causes neglect is the fact that the patient is usually injured in high velocity accidents and presents with more obvious accompanying injuries [4, 5].
Patients with neglected/missed anterior shoulder dislocation and an associated rotator cuff tear present a dilemma for the correct surgical approach that will facilitate a reduction of the dislocation and repair of the rotator cuff tear. This report describes an arthroscopic technique using standard arthroscopic portals to reduce neglected (3-6 weeks) anterior shoulder dislocation and repair ...
Clinical features at final follow-up of patients who presented with a diagnosis of neglected dislocation shoulder. Serial no. Follow-up (mo) ... Martineau P. Difficult access to medical care in times of COVID-19: late presentation of locked anterior shoulder dislocation: a case report. JSES Rev Rep Tech. 2022; 2:380-383. doi: 10.1016/j.xrrt ...
In this report we bring this rare presentation of neglected shoulder dislocation highlighting its natural history and its outcome following conservative treatment. ... Postacchini and Facchini presented five patients with 6 weeks as longest duration of failure of diagnosis. Mansat et al showed five patients with 6 weeks to 3 years as the ...