An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature
Olivia remes.
1 Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK
João Francisco Mendes
2 NOVA Medical School, Universidade NOVA de Lisboa, 1099-085 Lisbon, Portugal; ku.ca.mac@94cfj
Peter Templeton
3 IfM Engage Limited, Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK; ku.ca.mac@32twp
4 The William Templeton Foundation for Young People’s Mental Health (YPMH), Cambridge CB2 0AH, UK
Associated Data
Depression is one of the leading causes of disability, and, if left unmanaged, it can increase the risk for suicide. The evidence base on the determinants of depression is fragmented, which makes the interpretation of the results across studies difficult. The objective of this study is to conduct a thorough synthesis of the literature assessing the biological, psychological, and social determinants of depression in order to piece together the puzzle of the key factors that are related to this condition. Titles and abstracts published between 2017 and 2020 were identified in PubMed, as well as Medline, Scopus, and PsycInfo. Key words relating to biological, social, and psychological determinants as well as depression were applied to the databases, and the screening and data charting of the documents took place. We included 470 documents in this literature review. The findings showed that there are a plethora of risk and protective factors (relating to biological, psychological, and social determinants) that are related to depression; these determinants are interlinked and influence depression outcomes through a web of causation. In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression.
1. Introduction
Depression is one of the most common mental health issues, with an estimated prevalence of 5% among adults [ 1 , 2 ]. Symptoms may include anhedonia, feelings of worthlessness, concentration and sleep difficulties, and suicidal ideation. According to the World Health Organization, depression is a leading cause of disability; research shows that it is a burdensome condition with a negative impact on educational trajectories, work performance, and other areas of life [ 1 , 3 ]. Depression can start early in the lifecourse and, if it remains unmanaged, may increase the risk for substance abuse, chronic conditions, such as cardiovascular disease, and premature mortality [ 4 , 5 , 6 , 7 , 8 ].
Treatment for depression exists, such as pharmacotherapy, cognitive behavioural therapy, and other modalities. A meta-analysis of randomized, placebo-controlled trials of patients shows that 56–60% of people respond well to active treatment with antidepressants (selective serotonin reuptake inhibitors, tricyclic antidepressants) [ 9 ]. However, pharmacotherapy may be associated with problems, such as side-effects, relapse issues, a potential duration of weeks until the medication starts working, and possible limited efficacy in mild cases [ 10 , 11 , 12 , 13 , 14 ]. Psychotherapy is also available, but access barriers can make it difficult for a number of people to get the necessary help.
Studies on depression have increased significantly over the past few decades. However, the literature remains fragmented and the interpretation of heterogeneous findings across studies and between fields is difficult. The cross-pollination of ideas between disciplines, such as genetics, neurology, immunology, and psychology, is limited. Reviews on the determinants of depression have been conducted, but they either focus exclusively on a particular set of determinants (ex. genetic risk factors [ 15 ]) or population sub-group (ex. children and adolescents [ 16 ]) or focus on characteristics measured predominantly at the individual level (ex. focus on social support, history of depression [ 17 ]) without taking the wider context (ex. area-level variables) into account. An integrated approach paying attention to key determinants from the biological, psychological, and social spheres, as well as key themes, such as the lifecourse perspective, enables clinicians and public health authorities to develop tailored, person-centred approaches.
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social determinants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
The subsidiary aim: we have paid special attention to important themes, including the lifecourse perspective and interactions between determinants, to guide further efforts by public health and medical professionals.
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions.
2. Materials and Methods
We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years. We decided to focus on these determinants after discussions with academics (from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas), charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020. In several aspects, we attempted to conduct this review according to PRISMA guidelines [ 18 ].
The inclusion and exclusion criteria are the following:
- - We included documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries on the determinants of depression. The determinants refer to variables that appear to be linked to the development of depression, such as physiological factors (e.g., the nervous system, genetics), but also factors that are further away or more distal to the condition. Determinants may be risk or protective factors, and individual- or wider-area-level variables.
- - We focused on major depressive disorder, treatment-resistant depression, dysthymia, depressive symptoms, poststroke depression, perinatal depression, as well as depressive-like behaviour (common in animal studies), among others.
- - We included papers regardless of the measurement methods of depression.
- - We included papers that focused on human and/or rodent research.
- - This review focused on articles written in the English language.
- - Documents published between 2017–2020 were captured to provide an understanding of the latest research on this topic.
- - Studies that assessed depression as a comorbidity or secondary to another disorder.
- - Studies that did not focus on rodent and/or human research.
- - Studies that focused on the treatment of depression. We made this decision, because this is an in-depth topic that would warrant a separate stand-alone review.
- Next, we searched PubMed (2017–2020) using keywords related to depression and determinants. Appendix A contains the search strategy used. We also conducted focused searches in Medline, Scopus, and PsycInfo (2017–2020).
- Once the documents were identified through the databases, the inclusion and exclusion criteria were applied to the titles and abstracts. Screening of documents was conducted by O.R., and a subsample was screened by J.M.; any discrepancies were resolved through a communication process.
- The full texts of documents were retrieved, and the inclusion and exclusion criteria were again applied. A subsample of documents underwent double screening by two authors (O.R., J.M.); again, any discrepancies were resolved through communication.
- a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour).
- b. The data charting form was piloted on a subset of documents, and refinements to it were made. The data charting form was created with the data elements described above and tested in 20 studies to determine whether refinements in the wording or language were needed.
- c. Data charting was conducted on the documents.
- d. Narrative analysis was conducted on the data charting table to identify key themes. When a particular finding was noted more than once, it was logged as a potential theme, with a review of these notes yielding key themes that appeared on multiple occasions. When key themes were identified, one researcher (O.R.) reviewed each document pertaining to that theme and derived concepts (key determinants and related outcomes). This process (a subsample) was verified by a second author (J.M.), and the two authors resolved any discrepancies through communication. Key themes were also checked as to whether they were of major significance to public mental health and at the forefront of public health discourse according to consultations we held with stakeholders from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas, charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020.
We condensed the extensive information gleaned through our review into short summaries (with key points boxes for ease of understanding and interpretation of the data).
Through the searches, 6335 documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries, were identified. After applying the inclusion and exclusion criteria, 470 papers were included in this review ( Supplementary Table S1 ). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections.
3.1. Biological Factors
The following aspects will be discussed in this section: physical health conditions; then specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway. Finally, aspects related to cognition will also be discussed in the context of depression.
3.1.1. Physical Health Conditions
Studies on physical health conditions—key points:
- The presence of a physical health condition can increase the risk for depression
- Psychological evaluation in physically sick populations is needed
- There is large heterogeneity in study design and measurement; this makes the comparison of findings between and across studies difficult
A number of studies examined the links between the outcome of depression and physical health-related factors, such as bladder outlet obstruction, cerebral atrophy, cataract, stroke, epilepsy, body mass index and obesity, diabetes, urinary tract infection, forms of cancer, inflammatory bowel disorder, glaucoma, acne, urea accumulation, cerebral small vessel disease, traumatic brain injury, and disability in multiple sclerosis [ 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 ]. For example, bladder outlet obstruction has been linked to inflammation and depressive behaviour in rodent research [ 24 ]. The presence of head and neck cancer also seemed to be related to an increased risk for depressive disorder [ 45 ]. Gestational diabetes mellitus has been linked to depressive symptoms in the postpartum period (but no association has been found with depression in the third pregnancy trimester) [ 50 ], and a plethora of other such examples of relationships between depression and physical conditions exist. As such, the assessment of psychopathology and the provision of support are necessary in individuals of ill health [ 45 ]. Despite the large evidence base on physical health-related factors, differences in study methodology and design, the lack of standardization when it comes to the measurement of various physical health conditions and depression, and heterogeneity in the study populations makes it difficult to compare studies [ 50 ].
The next subsections discuss specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway; and aspects related to cognition.
3.1.2. Genetics
Studies on genetics—key points:
There were associations between genetic factors and depression; for example:
- The brain-derived neurotrophic factor (BDNF) plays an important role in depression
- Links exist between major histocompatibility complex region genes, as well as various gene polymorphisms and depression
- Single nucleotide polymorphisms (SNPs) of genes involved in the tryptophan catabolites pathway are of interest in relation to depression
A number of genetic-related factors, genomic regions, polymorphisms, and other related aspects have been examined with respect to depression [ 61 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ]. The influence of BDNF in relation to depression has been amply studied [ 117 , 118 , 141 , 142 , 143 ]. Research has shown associations between depression and BDNF (as well as candidate SNPs of the BDNF gene, polymorphisms of the BDNF gene, and the interaction of these polymorphisms with other determinants, such as stress) [ 129 , 144 , 145 ]. Specific findings have been reported: for example, a study reported a link between the BDNF rs6265 allele (A) and major depressive disorder [ 117 ].
Other research focused on major histocompatibility complex region genes, endocannabinoid receptor gene polymorphisms, as well as tissue-specific genes and gene co-expression networks and their links to depression [ 99 , 110 , 112 ]. The SNPs of genes involved in the tryptophan catabolites pathway have also been of interest when studying the pathogenesis of depression.
The results from genetics studies are compelling; however, the findings remain mixed. One study indicated no support for depression candidate gene findings [ 122 ]. Another study found no association between specific polymorphisms and major depressive disorder [ 132 ]. As such, further research using larger samples is needed to corroborate the statistically significant associations reported in the literature.
3.1.3. Microbiome
Studies on the microbiome—key points:
- The gut bacteria and the brain communicate via both direct and indirect pathways called the gut-microbiota-brain axis (the bidirectional communication networks between the central nervous system and the gastrointestinal tract; this axis plays an important role in maintaining homeostasis).
- A disordered microbiome can lead to inflammation, which can then lead to depression
- There are possible links between the gut microbiome, host liver metabolism, brain inflammation, and depression
The common themes of this review have focused on the microbiome/microbiota or gut metabolome [ 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ], the microbiota-gut-brain axis, and related factors [ 152 , 162 , 163 , 164 , 165 , 166 , 167 ]. When there is an imbalance in the intestinal bacteria, this can interfere with emotional regulation and contribute to harmful inflammatory processes and mood disorders [ 148 , 151 , 153 , 155 , 157 ]. Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome [ 158 ].
Research has also attempted to disentangle the links between the gut microbiome, host liver metabolism, brain inflammation, and depression, as well as the role of the ratio of lactobacillus to clostridium [ 152 ]. The literature has also examined the links between medication, such as antibiotics, and mood and behaviour, with the findings showing that antibiotics may be related to depression [ 159 , 168 ]. The links between the microbiome and depression are complex, and further studies are needed to determine the underpinning causal mechanisms.
3.1.4. Inflammation
Studies on inflammation—key points:
- Pro-inflammatory cytokines are linked to depression
- Pro-inflammatory cytokines, such as the tumour necrosis factor (TNF)-alpha, may play an important role
- Different methods of measurement are used, making the comparison of findings across studies difficult
Inflammation has been a theme in this literature review [ 60 , 161 , 164 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 ]. The findings show that raised levels of inflammation (because of factors such as pro-inflammatory cytokines) have been associated with depression [ 60 , 161 , 174 , 175 , 178 ]. For example, pro-inflammatory cytokines, such as tumour necrosis factor (TNF)-alpha, have been linked to depression [ 185 ]. Various determinants, such as early life stress, have also been linked to systemic inflammation, and this can increase the risk for depression [ 186 ].
Nevertheless, not everyone with elevated inflammation develops depression; therefore, this is just one route out of many linked to pathogenesis. Despite the compelling evidence reported with respect to inflammation, it is difficult to compare the findings across studies because of different methods used to assess depression and its risk factors.
3.1.5. Stress and HPA Axis Dysfunction
Studies on stress and HPA axis dysfunction—key points:
- Stress is linked to the release of proinflammatory factors
- The dysregulation of the HPA axis is linked to depression
- Determinants are interlinked in a complex web of causation
Stress was studied in various forms in rodent populations and humans [ 144 , 145 , 155 , 174 , 176 , 180 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 ].
Although this section has some overlap with others (as is to be expected because all of these determinants and body systems are interlinked), a number of studies have focused on the impact of stress on mental health. Stress has been mentioned in the literature as a risk factor of poor mental health and has emerged as an important determinant of depression. The effects of this variable are wide-ranging, and a short discussion is warranted.
Stress has been linked to the release of inflammatory factors, as well as the development of depression [ 204 ]. When the stress is high or lasts for a long period of time, this may negatively impact the brain. Chronic stress can impact the dendrites and synapses of various neurons, and may be implicated in the pathway leading to major depressive disorder [ 114 ]. As a review by Uchida et al. indicates, stress may be associated with the “dysregulation of neuronal and synaptic plasticity” [ 114 ]. Even in rodent studies, stress has a negative impact: chronic and unpredictable stress (and other forms of tension or stress) have been linked to unusual behaviour and depression symptoms [ 114 ].
The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [ 127 , 130 , 131 , 182 , 212 ]. One review indicates that a potential underpinning mechanism of depression relates to “HPA axis abnormalities involved in chronic stress” [ 213 ]. There is a complex relationship between the HPA axis, glucocorticoid receptors, epigenetic mechanisms, and psychiatric sequelae [ 130 , 212 ].
In terms of the relationship between the HPA axis and stress and their influence on depression, the diathesis–stress model offers an explanation: it could be that early stress plays a role in the hyperactivation of the HPA axis, thus creating a predisposition “towards a maladaptive reaction to stress”. When this predisposition then meets an acute stressor, depression may ensue; thus, in line with the diathesis–stress model, a pre-existing vulnerability and stressor can create fertile ground for a mood disorder [ 213 ]. An integrated review by Dean and Keshavan [ 213 ] suggests that HPA axis hyperactivity is, in turn, related to other determinants, such as early deprivation and insecure early attachment; this again shows the complex web of causation between the different determinants.
3.1.6. Kynurenine Pathway
Studies on the kynurenine pathway—key points:
- The kynurenine pathway is linked to depression
- Indolamine 2,3-dioxegenase (IDO) polymorphisms are linked to postpartum depression
The kynurenine pathway was another theme that emerged in this review [ 120 , 178 , 181 , 184 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 ]. The kynurenine pathway has been implicated not only in general depressed mood (inflammation-induced depression) [ 184 , 214 , 219 ] but also postpartum depression [ 120 ]. When the kynurenine metabolism pathway is activated, this results in metabolites, which are neurotoxic.
A review by Jeon et al. notes a link between the impairment of the kynurenine pathway and inflammation-induced depression (triggered by treatment for various physical diseases, such as malignancy). The authors note that this could represent an important opportunity for immunopharmacology [ 214 ]. Another review by Danzer et al. suggests links between the inflammation-induced activation of indolamine 2,3-dioxegenase (the enzyme that converts tryptophan to kynurenine), the kynurenine metabolism pathway, and depression, and also remarks about the “opportunities for treatment of inflammation-induced depression” [ 184 ].
3.1.7. Cognition
Studies on cognition and the brain—key points:
- Cognitive decline and cognitive deficits are linked to increased depression risk
- Cognitive reserve is important in the disability/depression relationship
- Family history of cognitive impairment is linked to depression
A number of studies have focused on the theme of cognition and the brain. The results show that factors, such as low cognitive ability/function, cognitive vulnerability, cognitive impairment or deficits, subjective cognitive decline, regression of dendritic branching and hippocampal atrophy/death of hippocampal cells, impaired neuroplasticity, and neurogenesis-related aspects, have been linked to depression [ 131 , 212 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 ]. The cognitive reserve appears to act as a moderator and can magnify the impact of certain determinants on poor mental health. For example, in a study in which participants with multiple sclerosis also had low cognitive reserve, disability was shown to increase the risk for depression [ 63 ]. Cognitive deficits can be both causal and resultant in depression. A study on individuals attending outpatient stroke clinics showed that lower scores in cognition were related to depression; thus, cognitive impairment appears to be associated with depressive symptomatology [ 226 ]. Further, Halahakoon et al. [ 222 ] note a meta-analysis [ 240 ] that shows that a family history of cognitive impairment (in first degree relatives) is also linked to depression.
In addition to cognitive deficits, low-level cognitive ability [ 231 ] and cognitive vulnerability [ 232 ] have also been linked to depression. While cognitive impairment may be implicated in the pathogenesis of depressive symptoms [ 222 ], negative information processing biases are also important; according to the ‘cognitive neuropsychological’ model of depression, negative affective biases play a central part in the development of depression [ 222 , 241 ]. Nevertheless, the evidence on this topic is mixed and further work is needed to determine the underpinning mechanisms between these states.
3.2. Psychological Factors
Studies on psychological factors—key points:
- There are many affective risk factors linked to depression
- Determinants of depression include negative self-concept, sensitivity to rejection, neuroticism, rumination, negative emotionality, and others
A number of studies have been undertaken on the psychological factors linked to depression (including mastery, self-esteem, optimism, negative self-image, current or past mental health conditions, and various other aspects, including neuroticism, brooding, conflict, negative thinking, insight, cognitive fusion, emotional clarity, rumination, dysfunctional attitudes, interpretation bias, and attachment style) [ 66 , 128 , 140 , 205 , 210 , 228 , 235 , 242 , 243 , 244 , 245 , 246 , 247 , 248 , 249 , 250 , 251 , 252 , 253 , 254 , 255 , 256 , 257 , 258 , 259 , 260 , 261 , 262 , 263 , 264 , 265 , 266 , 267 , 268 , 269 , 270 , 271 , 272 , 273 , 274 , 275 , 276 , 277 , 278 , 279 , 280 , 281 , 282 , 283 , 284 , 285 , 286 , 287 , 288 , 289 , 290 ]. Determinants related to this condition include low self-esteem and shame, among other factors [ 269 , 270 , 275 , 278 ]. Several emotional states and traits, such as neuroticism [ 235 , 260 , 271 , 278 ], negative self-concept (with self-perceptions of worthlessness and uselessness), and negative interpretation or attention biases have been linked to depression [ 261 , 271 , 282 , 283 , 286 ]. Moreover, low emotional clarity has been associated with depression [ 267 ]. When it comes to the severity of the disorder, it appears that meta-emotions (“emotions that occur in response to other emotions (e.g., guilt about anger)” [ 268 ]) have a role to play in depression [ 268 ].
A determinant that has received much attention in mental health research concerns rumination. Rumination has been presented as a mediator but also as a risk factor for depression [ 57 , 210 , 259 ]. When studied as a risk factor, it appears that the relationship of rumination with depression is mediated by variables that include limited problem-solving ability and insufficient social support [ 259 ]. However, rumination also appears to act as a mediator: for example, this variable (particularly brooding rumination) lies on the causal pathway between poor attention control and depression [ 265 ]. This shows that determinants may present in several forms: as moderators or mediators, risk factors or outcomes, and this is why disentangling the relationships between the various factors linked to depression is a complex task.
The psychological determinants are commonly researched variables in the mental health literature. A wide range of factors have been linked to depression, such as the aforementioned determinants, but also: (low) optimism levels, maladaptive coping (such as avoidance), body image issues, and maladaptive perfectionism, among others [ 269 , 270 , 272 , 273 , 275 , 276 , 279 , 285 , 286 ]. Various mechanisms have been proposed to explain the way these determinants increase the risk for depression. One of the underpinning mechanisms linking the determinants and depression concerns coping. For example, positive fantasy engagement, cognitive biases, or personality dispositions may lead to emotion-focused coping, such as brooding, and subsequently increase the risk for depression [ 272 , 284 , 287 ]. Knowing the causal mechanisms linking the determinants to outcomes provides insight for the development of targeted interventions.
3.3. Social Determinants
Studies on social determinants—key points:
- Social determinants are the conditions in the environments where people are born, live, learn, work, play, etc.; these influence (mental) health [ 291 ]
- There are many social determinants linked to depression, such as sociodemographics, social support, adverse childhood experiences
- Determinants can be at the individual, social network, community, and societal levels
Studies also focused on the social determinants of (mental) health; these are the conditions in which people are born, live, learn, work, play, and age, and have a significant influence on wellbeing [ 291 ]. Factors such as age, social or socioeconomic status, social support, financial strain and deprivation, food insecurity, education, employment status, living arrangements, marital status, race, childhood conflict and bullying, violent crime exposure, abuse, discrimination, (self)-stigma, ethnicity and migrant status, working conditions, adverse or significant life events, illiteracy or health literacy, environmental events, job strain, and the built environment have been linked to depression, among others [ 52 , 133 , 235 , 236 , 239 , 252 , 269 , 280 , 292 , 293 , 294 , 295 , 296 , 297 , 298 , 299 , 300 , 301 , 302 , 303 , 304 , 305 , 306 , 307 , 308 , 309 , 310 , 311 , 312 , 313 , 314 , 315 , 316 , 317 , 318 , 319 , 320 , 321 , 322 , 323 , 324 , 325 , 326 , 327 , 328 , 329 , 330 , 331 , 332 , 333 , 334 , 335 , 336 , 337 , 338 , 339 , 340 , 341 , 342 , 343 , 344 , 345 , 346 , 347 , 348 , 349 , 350 , 351 , 352 , 353 , 354 , 355 , 356 , 357 , 358 , 359 , 360 , 361 , 362 , 363 , 364 , 365 , 366 , 367 , 368 , 369 , 370 , 371 ]. Social support and cohesion, as well as structural social capital, have also been identified as determinants [ 140 , 228 , 239 , 269 , 293 , 372 , 373 , 374 , 375 , 376 , 377 , 378 , 379 ]. In a study, part of the findings showed that low levels of education have been shown to be linked to post-stroke depression (but not severe or clinical depression outcomes) [ 299 ]. A study within a systematic review indicated that having only primary education was associated with a higher risk of depression compared to having secondary or higher education (although another study contrasted this finding) [ 296 ]. Various studies on socioeconomic status-related factors have been undertaken [ 239 , 297 ]; the research has shown that a low level of education is linked to depression [ 297 ]. Low income is also related to depressive disorders [ 312 ]. By contrast, high levels of education and income are protective [ 335 ].
A group of determinants touched upon by several studies included adverse childhood or early life experiences: ex. conflict with parents, early exposure to traumatic life events, bullying and childhood trauma were found to increase the risk of depression (ex. through pathways, such as inflammation, interaction effects, or cognitive biases) [ 161 , 182 , 258 , 358 , 362 , 380 ].
Gender-related factors were also found to play an important role with respect to mental health [ 235 , 381 , 382 , 383 , 384 , 385 ]. Gender inequalities can start early on in the lifecourse, and women were found to be twice as likely to have depression as men. Gender-related factors were linked to cognitive biases, resilience and vulnerabilities [ 362 , 384 ].
Determinants can impact mental health outcomes through underpinning mechanisms. For example, harmful determinants can influence the uptake of risk behaviours. Risk behaviours, such as sedentary behaviour, substance abuse and smoking/nicotine exposure, have been linked to depression [ 226 , 335 , 355 , 385 , 386 , 387 , 388 , 389 , 390 , 391 , 392 , 393 , 394 , 395 , 396 , 397 , 398 , 399 , 400 , 401 ]. Harmful determinants can also have an impact on diet. Indeed, dietary aspects and diet components (ex. vitamin D, folate, selenium intake, iron, vitamin B12, vitamin K, fiber intake, zinc) as well as diet-related inflammatory potential have been linked to depression outcomes [ 161 , 208 , 236 , 312 , 396 , 402 , 403 , 404 , 405 , 406 , 407 , 408 , 409 , 410 , 411 , 412 , 413 , 414 , 415 , 416 , 417 , 418 , 419 , 420 , 421 , 422 , 423 , 424 , 425 , 426 , 427 , 428 ]. A poor diet has been linked to depression through mechanisms such as inflammation [ 428 ].
Again, it is difficult to constrict diet to the ‘social determinants of health’ category as it also relates to inflammation (biological determinants) and could even stand alone as its own category. Nevertheless, all of these factors are interlinked and influence one another in a complex web of causation, as mentioned elsewhere in the paper.
Supplementary Figure S1 contains a representation of key determinants acting at various levels: the individual, social network, community, and societal levels. The determinants have an influence on risk behaviours, and this, in turn, can affect the mood (i.e., depression), body processes (ex. can increase inflammation), and may negatively influence brain structure and function.
3.4. Others
Studies on ‘other’ determinants—key points:
- A number of factors are related to depression
- These may not be as easily categorized as the other determinants in this paper
A number of factors arose in this review that were related to depression; it was difficult to place these under a specific heading above, so this ‘other’ category was created. A number of these could be sorted under the ‘social determinants of depression’ category. For example, being exposed to deprivation, hardship, or adversity may increase the risk for air pollution exposure and nighttime shift work, among others, and the latter determinants have been found to increase the risk for depression. Air pollution could also be regarded as an ecologic-level (environmental) determinant of mental health.
Nevertheless, we have decided to leave these factors in a separate category (because their categorization may not be as immediately clear-cut as others), and these factors include: low-level light [ 429 ], weight cycling [ 430 ], water contaminants [ 431 ], trade [ 432 ], air pollution [ 433 , 434 ], program-level variables (ex. feedback and learning experience) [ 435 ], TV viewing [ 436 ], falls [ 437 ], various other biological factors [ 116 , 136 , 141 , 151 , 164 , 182 , 363 , 364 , 438 , 439 , 440 , 441 , 442 , 443 , 444 , 445 , 446 , 447 , 448 , 449 , 450 , 451 , 452 , 453 , 454 , 455 , 456 , 457 , 458 , 459 , 460 , 461 , 462 , 463 , 464 , 465 , 466 , 467 , 468 , 469 ], mobile phone use [ 470 ], ultrasound chronic exposure [ 471 ], nighttime shift work [ 472 ], work accidents [ 473 ], therapy enrollment [ 226 ], and exposure to light at night [ 474 ].
4. Cross-Cutting Themes
4.1. lifecourse perspective.
Studies on the lifecourse perspective—key points:
- Early life has an importance on mental health
- Stress has been linked to depression
- In old age, the decline in social capital is important
Trajectories and life events are important when it comes to the lifecourse perspective. Research has touched on the influence of prenatal or early life stress on an individual’s mental health trajectory [ 164 , 199 , 475 ]. Severe stress that occurs in the form of early-life trauma has also been associated with depressive symptoms [ 362 , 380 ]. It may be that some individuals exposed to trauma develop thoughts of personal failure, which then serve as a catalyst of depression [ 380 ].
At the other end of the life trajectory—old age—specific determinants have been linked to an increased risk for depression. Older people are at a heightened risk of losing their social networks, and structural social capital has been identified as important in relation to depression in old age [ 293 ].
4.2. Gene–Environment Interactions
Studies on gene–environment interactions—key points:
- The environment and genetics interact to increase the risk of depression
- The etiology of depression is multifactorial
- Adolescence is a time of vulnerability
A number of studies have touched on gene–environment interactions [ 72 , 77 , 82 , 119 , 381 , 476 , 477 , 478 , 479 , 480 , 481 ]. The interactions between genetic factors and determinants, such as negative life events (ex. relationship and social difficulties, serious illness, unemployment and financial crises) and stressors (ex. death of spouse, minor violations of law, neighbourhood socioeconomic status) have been studied in relation to depression [ 82 , 135 , 298 , 449 , 481 ]. A study reported an interaction of significant life events with functional variation in the serotonin-transporter-linked polymorphic region (5-HTTLPR) allele type (in the context of multiple sclerosis) and linked this to depression [ 361 ], while another reported an interaction between stress and 5-HTTLPR in relation to depression [ 480 ]. Other research reported that the genetic variation of HPA-axis genes has moderating effects on the relationship between stressors and depression [ 198 ]. Another study showed that early-life stress interacts with gene variants to increase the risk for depression [ 77 ].
Adolescence is a time of vulnerability [ 111 , 480 ]. Perceived parental support has been found to interact with genes (GABRR1, GABRR2), and this appears to be associated with depressive symptoms in adolescence [ 480 ]. It is important to pay special attention to critical periods in the lifecourse so that adequate support is provided to those who are most vulnerable.
The etiology of depression is multifactorial, and it is worthwhile to examine the interaction between multiple factors, such as epigenetic, genetic, and environmental factors, in order to truly understand this mental health condition. Finally, taking into account critical periods of life when assessing gene–environment interactions is important for developing targeted interventions.
5. Discussion
Depression is one of the most common mental health conditions, and, if left untreated, it can increase the risk for substance abuse, anxiety disorders, and suicide. In the past 20 years, a large number of studies on the risk and protective factors of depression have been undertaken in various fields, such as genetics, neurology, immunology, and epidemiology. However, there are limitations associated with the extant evidence base. The previous syntheses on depression are limited in scope and focus exclusively on social or biological factors, population sub-groups, or examine depression as a comorbidity (rather than an independent disorder). The research on the determinants and causal pathways of depression is fragmentated and heterogeneous, and this has not helped to stimulate progress when it comes to the prevention and intervention of this condition—specifically unravelling the complexity of the determinants related to this condition and thus refining the prevention and intervention methods.
The scope of this paper was to bring together the heterogeneous, vast, and fragmented literature on depression and paint a picture of the key factors that contribute to this condition. The findings from this review show that there are important themes when it comes to the determinants of depression, such as: the microbiome, dysregulation of the HPA axis, inflammatory reactions, the kynurenine pathway, as well as psychological and social factors. It may be that physical factors are proximal determinants of depression, which, in turn, are acted on by more distal social factors, such as deprivation, environmental events, and social capital.
The Marmot Report [ 291 ], the World Health Organization [ 482 ], and Compton et al. [ 483 ] highlight that the most disadvantaged segments of society are suffering (the socioeconomic context is important), and this inequality in resources has translated to inequality in mental health outcomes [ 483 ]. To tackle the issue of egalitarianism and restore equality in the health between the groups, the social determinants need to be addressed [ 483 ]. A wide range of determinants of mental health have been identified in the literature: age, gender, ethnicity, family upbringing and early attachment patterns, social support, access to food, water and proper nutrition, and community factors. People spiral downwards because of individual- and societal-level circumstances; therefore, these circumstances along with the interactions between the determinants need to be considered.
Another important theme in the mental health literature is the lifecourse perspective. This shows that the timing of events has significance when it comes to mental health. Early life is a critical period during the lifespan at which cognitive processes develop. Exposure to harmful determinants, such as stress, during this period can place an individual on a trajectory of depression in adulthood or later life. When an individual is exposed to harmful determinants during critical periods and is also genetically predisposed to depression, the risk for the disorder can be compounded. This is why aspects such as the lifecourse perspective and gene–environment interactions need to be taken into account. Insight into this can also help to refine targeted interventions.
A number of interventions for depression have been developed or recommended, addressing, for example, the physical factors described here and lifestyle modifications. Interventions targeting various factors, such as education and socioeconomic status, are needed to help prevent and reduce the burden of depression. Further research on the efficacy of various interventions is needed. Additional studies are also needed on each of the themes described in this paper, for example: the biological factors related to postpartum depression [ 134 ], and further work is needed on depression outcomes, such as chronic, recurrent depression [ 452 ]. Previous literature has shown that chronic stress (associated with depression) is also linked to glucocorticoid receptor resistance, as well as problems with the regulation of the inflammatory response [ 484 ]. Further work is needed on this and the underpinning mechanisms between the determinants and outcomes. This review highlighted the myriad ways of measuring depression and its determinants [ 66 , 85 , 281 , 298 , 451 , 485 ]. Thus, the standardization of the measurements of the outcomes (ex. a gold standard for measuring depression) and determinants is essential; this can facilitate comparisons of findings across studies.
5.1. Strengths
This paper has important strengths. It brings together the wide literature on depression and helps to bridge disciplines in relation to one of the most common mental health problems. We identified, selected, and extracted data from studies, and provided concise summaries.
5.2. Limitations
The limitations of the review include missing potentially important studies; however, this is a weakness that cannot be avoided by literature reviews. Nevertheless, the aim of the review was not to identify each study that has been conducted on the risk and protective factors of depression (which a single review is unable to capture) but rather to gain insight into the breadth of literature on this topic, highlight key biological, psychological, and social determinants, and shed light on important themes, such as the lifecourse perspective and gene–environment interactions.
6. Conclusions
We have reviewed the determinants of depression and recognize that there are a multitude of risk and protective factors at the individual and wider ecologic levels. These determinants are interlinked and influence one another. We have attempted to describe the wide literature on this topic, and we have brought to light major factors that are of public mental health significance. This review may be used as an evidence base by those in public health, clinical practice, and research.
This paper discusses key areas in depression research; however, an exhaustive discussion of all the risk factors and determinants linked to depression and their mechanisms is not possible in one journal article—which, by its very nature, a single paper cannot do. We have brought to light overarching factors linked to depression and a workable conceptual framework that may guide clinical and public health practice; however, we encourage other researchers to continue to expand on this timely and relevant work—particularly as depression is a top priority on the policy agenda now.
Acknowledgments
Thank you to Isla Kuhn for the help with the Medline, Scopus, and PsycInfo database searches.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/brainsci11121633/s1 , Figure S1: Conceptual framework: Determinants of depression, Table S1: Data charting—A selection of determinants from the literature.
Appendix A.1. Search Strategy
Search: ((((((((((((((((“Gene-Environment Interaction”[Majr]) OR (“Genetics”[Mesh])) OR (“Genome-Wide Association Study”[Majr])) OR (“Microbiota”[Mesh] OR “Gastrointestinal Microbiome”[Mesh])) OR (“Neurogenic Inflammation”[Mesh])) OR (“genetic determinant”)) OR (“gut-brain-axis”)) OR (“Kynurenine”[Majr])) OR (“Cognition”[Mesh])) OR (“Neuronal Plasticity”[Majr])) OR (“Neurogenesis”[Mesh])) OR (“Genes”[Mesh])) OR (“Neurology”[Majr])) OR (“Social Determinants of Health”[Majr])) OR (“Glucocorticoids”[Mesh])) OR (“Tryptophan”[Mesh])) AND (“Depression”[Mesh] OR “Depressive Disorder”[Mesh]) Filters: from 2017—2020.
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R)
- exp *Depression/
- exp *Depressive Disorder/
- exp *”Social Determinants of Health”/
- exp *Tryptophan/
- exp *Glucocorticoids/
- exp *Neurology/
- exp *Genes/
- exp *Neurogenesis/
- exp *Neuronal Plasticity/
- exp *Kynurenine/
- exp *Genetics/
- exp *Neurogenic Inflammation/
- exp *Gastrointestinal Microbiome/
- exp *Genome-Wide Association Study/
- exp *Gene-Environment Interaction/
- exp *Depression/et [Etiology]
- exp *Depressive Disorder/et
- or/4-16 637368
- limit 22 to yr = “2017–Current”
- “cause* of depression”.mp.
- “cause* of depression”.ti.
- (cause adj3 (depression or depressive)).ti.
- (caus* adj3 (depression or depressive)).ti.
Appendix A.2. PsycInfo
(TITLE ( depression OR “ Depressive Disorder ”) AND TITLE (“ Social Determinants of Health ” OR tryptophan OR glucocorticoids OR neurology OR genes OR neurogenesis OR “ Neuronal Plasticity ” OR kynurenine OR genetics OR “ Neurogenic Inflammation ” OR “ Gastrointestinal Microbiome ” OR “ Genome-Wide Association Study ” OR “ Gene-Environment Interaction ” OR aetiology OR etiology )) OR TITLE ( cause* W/3 ( depression OR depressive )).
Author Contributions
O.R. was responsible for the design of the study and methodology undertaken. Despite P.T.’s involvement in YPMH, he had no role in the design of the study; P.T. was responsible for the conceptualization of the study. Validation was conducted by O.R. and J.F.M. Formal analysis (data charting) was undertaken by O.R. O.R. and P.T. were involved in the investigation, resource acquisition, and data presentation. The original draft preparation was undertaken by O.R. The writing was conducted by O.R., with review and editing by P.T. and J.F.M. Funding acquisition was undertaken by O.R. and P.T. All authors have read and agreed to the published version of the manuscript.
This research was funded by The William Templeton Foundation for Young People’s Mental Health, Cambridge Philosophical Society, and the Aviva Foundation.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
- Download PDF
- Order a free hardcopy
What is depression?
Everyone feels sad or low sometimes, but these feelings usually pass. Depression (also called major depression, major depressive disorder, or clinical depression) is different. It can cause severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working.
Depression can affect anyone regardless of age, gender, race or ethnicity, income, culture, or education. Research suggests that genetic, biological, environmental, and psychological factors play a role in the disorder.
Women are diagnosed with depression more often than men, but men can also be depressed. Because men may be less likely to recognize, talk about, and seek help for their negative feelings, they are at greater risk of their depression symptoms being undiagnosed and undertreated. Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community.
In addition, depression can co-occur with other mental disorders or chronic illnesses, such as diabetes, cancer, heart disease, and chronic pain. Depression can make these conditions worse and vice versa. Sometimes, medications taken for an illness cause side effects that contribute to depression symptoms as well.
What are the different types of depression?
There are two common types of depression.
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe depression symptoms that last much longer, usually for at least 2 years.
Other types of depression include the following.
- Seasonal affective disorder comes and goes with the seasons, with symptoms typically starting in the late fall and early winter and going away during the spring and summer.
- Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions or hallucinations.
- Bipolar disorder involves depressive episodes, as well as manic episodes (or less severe hypomanic episodes) with unusually elevated mood, greater irritability, or increased activity level.
Additional types of depression can occur at specific points in a woman’s life. Pregnancy, the postpartum period, the menstrual cycle, and menopause are associated with physical and hormonal changes that can bring on a depressive episode in some people.
- Premenstrual dysphoric disorder is a more severe form of premenstrual syndrome, or PMS, that occurs in the weeks before menstruation.
- Perinatal depression occurs during pregnancy or after childbirth. It is more than the “baby blues” many new moms experience after giving birth.
- Perimenopausal depression affects some women during the transition to menopause. Women may experience feelings of intense irritability, anxiety, sadness, or loss of enjoyment.
What are the signs and symptoms of depression?
Common signs and symptoms of depression include:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration‚ or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet responsibilities or ignoring other important roles
- Problems with sexual desire and performance
Not everyone who is depressed shows all these symptoms. Some people experience only a few symptoms, while others experience many. Depression symptoms interfere with day-to-day functioning and cause significant distress for the person experiencing them.
If you show signs or symptoms of depression and they persist or do not go away, talk to a health care provider. If you see signs of depression in someone you know, encourage them to seek help from a mental health professional.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
How is depression diagnosed?
To be diagnosed with depression, a person must have symptoms most of the day, nearly every day, for at least 2 weeks. One of the symptoms must be a depressed mood or a loss of interest or pleasure in most activities. Children and adolescents may be irritable rather than sad.
Although several persistent symptoms, in addition to low mood, are required for a depression diagnosis, people with only a few symptoms may benefit from treatment. The severity and frequency of symptoms and how long they last vary depending on the person.
If you think you may have depression, talk to a health care provider, such as a primary care doctor, psychologist, or psychiatrist. During the visit, the provider may ask when your symptoms began, how long they have lasted, how often they occur, and if they keep you from going out or doing your usual activities. It may help to take some notes about your symptoms before the visit.
Certain medications and medical conditions, such as viruses or thyroid disorders, can cause the same symptoms as depression. A provider can rule out these possibilities by doing a physical exam, interview, and lab tests.
Does depression look the same in everyone?
Depression can affect people differently depending on their age.
- Children may be anxious or cranky, pretend to be sick, refuse to go to school, cling to a parent, or worry that a parent may die.
- Older children and teens may get into trouble at school, sulk, be easily frustrated‚ feel restless, or have low self-esteem. They may have other disorders, such as anxiety, an eating disorder, attention-deficit/hyperactivity disorder, or substance use disorder. Older children and teens are also more likely to experience excessive sleepiness (called hypersomnia) and increased appetite (called hyperphagia).
- Young adults are more likely to be irritable, complain of weight gain and hypersomnia, and have a negative view of life and the future. They often have other disorders, such as generalized anxiety disorder, social phobia, panic disorder, or substance use disorder.
- Middle-aged adults may have more depressive episodes, decreased libido, middle-of-the-night insomnia, or early morning waking. They often report stomach problems, such as diarrhea or constipation.
- Older adults often feel sadness, grief, or other less obvious symptoms. They may report a lack of emotions rather than a depressed mood. Older adults are also more likely to have other medical conditions or pain that can cause or contribute to depression. Memory and thinking problems (called pseudodementia) may be prominent in severe cases.
Depression can also look different in men versus women, such as the symptoms they show and the behaviors they use to cope with them. For instance, men (as well as women) may show symptoms other than sadness, instead seeming angry or irritable.
For some people, symptoms manifest as physical problems (for example, a racing heart, tightened chest, chronic headaches, or digestive issues). Many men are more likely to see a health care provider about these physical symptoms than their emotional ones. While increased use of alcohol or drugs can be a sign of depression in any person, men are also more likely to use these substances as a coping strategy.
How is depression treated?
Depression treatment typically involves psychotherapy (in person or virtual), medication, or both. If these treatments do not reduce symptoms sufficiently, brain stimulation therapy may be another option.
Choosing the right treatment plan is based on a person’s needs, preferences, and medical situation and in consultation with a mental health professional or a health care provider. Finding the best treatment may take trial and error.
For milder forms of depression, psychotherapy is often tried first, with medication added later if the therapy alone does not produce a good response. People with moderate or severe depression usually are prescribed medication as part of the initial treatment plan.
Psychotherapy
Psychotherapy (also called talk therapy or counseling) can help people with depression by teaching them new ways of thinking and behaving and helping them change habits that contribute to depression. Psychotherapy occurs under the care of a licensed, trained mental health professional in one-on-one sessions or with others in a group setting.
Psychotherapy can be effective when delivered in person or virtually via telehealth. A provider may support or supplement therapy using digital or mobile technology, like apps or other tools.
Evidence-based therapies to treat depression include cognitive behavioral therapy and interpersonal therapy. Using other forms of psychotherapy, such as psychodynamic therapy, for a limited time also may help some people with depression.
- Cognitive behavioral therapy (CBT) : With CBT, people learn to challenge and change unhelpful thoughts and behaviors to improve their depressive and anxious feelings. Recent advances in CBT include adding mindfulness principles and specializing the therapy to target specific symptoms like insomnia.
- Interpersonal therapy (IPT) : IPT focuses on interpersonal and life events that impact mood and vice versa. IPT aims to help people improve their communication skills within relationships, form social support networks, and develop realistic expectations to better deal with crises or other issues that may be contributing to or worsening their depression.
Learn more about psychotherapy .
Antidepressants are medications commonly used to treat depression. They work by changing how the brain produces or uses certain chemicals involved in mood or stress.
Antidepressants take time—usually 4−8 weeks—to work, and problems with sleep, appetite, and concentration often improve before mood lifts. Giving a medication a chance to work is important before deciding whether it is right for you.
Treatment-resistant depression occurs when a person doesn’t get better after trying at least two antidepressants. Esketamine is a medication approved by the U.S. Food and Drug Administration (FDA) for treatment-resistant depression. Delivered as a nasal spray in a doctor’s office, clinic, or hospital, the medication acts rapidly, typically within a couple of hours, to relieve depression symptoms. People will usually continue to take an antidepressant pill to maintain the improvement in their symptoms.
Another option for treatment-resistant depression is to combine an antidepressant with a different type of medication that may make it more effective, such as an antipsychotic or anticonvulsant medication.
All medications can have side effects. Talk to a health care provider before starting or stopping any medication. Learn more about antidepressants .
Note : In some cases, children, teenagers, and young adults under 25 years may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. The FDA advises that patients of all ages taking antidepressants be watched closely, especially during the first few weeks of treatment.
Information about medication changes frequently. Learn more about specific medications like esketamine, including the latest approvals, side effects, warnings, and patient information, on the FDA website .
Brain stimulation therapy
Brain stimulation therapy is an option when other depression treatments have not worked. The therapy involves activating or inhibiting the brain with electricity or magnetic waves.
Although brain stimulation therapy is less frequently used than psychotherapy and medication, it can play an important role in treating depression in people who have not responded to other treatments. The therapy generally is used only after a person has tried psychotherapy and medication, and those treatments usually continue. Brain stimulation therapy is sometimes used as an earlier treatment option when severe depression has become life-threatening, such as when a person has stopped eating or drinking or is at a high risk of suicide.
The FDA has approved several types of brain stimulation therapy. The most used are electroconvulsive therapy (ECT) and repetitive transcranial magnetic stimulation (rTMS). Other brain stimulation therapies are newer and, in some cases, still considered experimental. Learn more about brain stimulation therapies .
Natural products
The FDA has not approved any natural products for treating depression. Although research is ongoing and findings are inconsistent, some people report that natural products, including vitamin D and the herbal dietary supplement St. John’s wort, helped their depression symptoms. However, these products can come with risks, including, in some cases, interactions with prescription medications.
Do not use vitamin D, St. John’s wort, or other dietary supplements or natural products without first talking to a health care provider. Rigorous studies must test whether these and other natural products are safe and effective.
How can I take care of myself?
Most people with depression benefit from mental health treatment. Once you begin treatment, you should gradually start to feel better. Go easy on yourself during this time. Try to do things you used to enjoy. Even if you don’t feel like doing them, they can improve your mood.
Other things that may help:
- Try to get physical activity. Just 30 minutes a day of walking can boost your mood.
- Try to maintain a regular bedtime and wake-up time.
- Eat regular, healthy meals.
- Do what you can as you can. Decide what must get done and what can wait.
- Connect with people. Talk to people you trust about how you are feeling.
- Delay making important life decisions until you feel better. Discuss decisions with people who know you well.
- Avoid using alcohol, nicotine, or drugs, including medications not prescribed for you.
How can I find help for depression?
You can learn about ways to get help and find tips for talking with a health care provider on the NIMH website.
The Substance Abuse and Mental Health Services Administration (SAMHSA) also has an online tool to help you find mental health services in your area.
How can I help a loved one who is depressed?
If someone you know is depressed, help them see a health care provider or mental health professional. You also can:
- Offer support, understanding, patience, and encouragement.
- Invite them out for walks, outings, and other activities.
- Help them stick to their treatment plan, such as setting reminders to take prescribed medications.
- Make sure they have transportation or access to therapy appointments.
- Remind them that, with time and treatment, their depression can lift.
What are clinical trials and why are they important?
Clinical trials are research studies that look at ways to prevent, detect, or treat diseases and conditions. These studies help show whether a treatment is safe and effective in people. Some people join clinical trials to help doctors and researchers learn more about a disease and improve health care. Other people, such as those with health conditions, join to try treatments that aren’t widely available.
NIMH supports clinical trials across the United States. Talk to a health care provider about clinical trials and whether one is right for you. Learn more about participating in clinical trials .
For more information
Learn more about mental health disorders and topics . For information about various health topics, visit the National Library of Medicine’s MedlinePlus .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 24-MH-8079 Revised 2024
Clinical Trials
Depression (major depressive disorder).
Displaying 61 studies
The purpose of this study is to evaluate the effectiveness of adjunctive lithium in the acute (2 weeks) and continuation phase (4 weeks) for maintenance of ketamine-associated remission.
The purpose of this study is to learn if measures of brain activity are different in children and adolescents with depression who are in different stages of treatment. This is important because it may identify a biological marker for depression that could one day be used to identify depressed children who would benefit from certain treatments (medications for example), or to monitor how well treatments are working. Brain activity measures(known as cortical excitability and inhibition) will be collected by Transcranial Magnetic Stimulation (TMS). TMS is a noninvasive (no surgery or implants) brain stimulation technology which can make parts of the ...
The purpose of this study is to ascertain the effects of the Authentic Connections intervention among nurse leaders who are mothers at Mayo Clinic Rochester in comparison to a control group. Outcomes that will be measured include: psychological distress, depression, self-compassion, parenting stress, burnout, and feasibility measures.
This is a double-blind, sham controlled, multi-center study to confirm the safety and efficacy of synchronized transcranial magnetic stimulation (sTMS) for the treatment of patients currently experiencing an episode of depression who have failed to respond to at least one (1) antidepressant medication. Patients will be randomly assigned to either active or sham therapy and will undergo daily treatments for a period of time. Following completion of blinded treatments, patients may be eligible for a course of open label treatments.
The purpose of this study is to evaluate the feasibility of developing a microbiome probe of depression and to evaluate the microbiome change in a preliminary analysis of treatment response (n=20) vs. non response (n=20) to the antidepressant citalopram. This study is a 12 week open trial that will enroll approximately 80 participants (anticipated 40 study completers with paired biomarker data) with an episode of major depression, Bipolar I or Bipolar II and 40 age- and sex-matched healthy controls.
Depression is common in patients with cancer. Current medications for depression, while effective, take several weeks to take effect. Ketamine has emerged as a drug with promise for cancer patients. In two reported cases, a single dose of ketamine induced rapid and moderately sustained symptom reduction in depression and anxiety with no adverse side effects. Benefit was seen in as little as 1 hour and sustained up to 30 days. This study is a randomized, double-blind, placebo-controlled investigation testing whether a single dose of ketamine improves depression and anxiety relative to placebo in patients with cancer.
This study is to learn how effective a night of no sleep, with or without light therapy, is for patients in an inpatient setting who are experiencing Major depression.
To evaluate the safety and efficacy of daily, active Neurostar® TMS (when compared with sham treatment) in adolescents meeting criteria for Major Depressive Disorder (MDD).
The purpose of this study is to evaluate and analyze the clinical data that is already being collected for clinical purposes to determine the long-term effects of the repeated use of subanaesthetic ketamine/esketamine for patients with depression. We hypothesize that patients who have a greater number of infusions/treatments will be more likely to have increased side effects to the drug. We would like to be able to also analyze data related to any other assessments that are implemented as part of the clinical practice in the future.
The primary purpose of this study is to compare outcomes of depressive symptoms (PHQ-9 and HAM-D) over 6 months following an eight-week program of SMART-D therapy + treatment as usual versus treatment as usual for patients with major depression in partial-to full-remission.
The purpose of this study is to systematically investigate the use of repetitive transcranial magnetic stimulation (rTMS) as an added treatment for patients who have depression that is not decreasing with standard care.
The purpose of this study is to measure, rank, and categorize the subject sample of depression, stress, resilience, and happiness scores using quantitive surgeys. This research aims to learn how a Three Good Things (3GT) journaling activity affects a subject's symptoms of stress, depression, reslieince, and happiness. The data will allow the project team to gain an in-depth understanding of the impact of the use of resilience strategies from a patient's perspective. This project aims to review if there is a correlation between stress, depression, resiliency, and happiness scores to the use of Positive Psychology.
The purpose of this study is to explore the role of Cognitive Behavioral Therapy (CBT), a treatment for depression, on self-effectiveness (feeling empowered to accomplish a given task) and depression in persons with chronic pain and depression. Past research has shown that persons with chronic pain show improvement in self-efficacy and depression scores when they are using CBT. The Pain rehabilitation Center (PRC) at Mayo Clinic is adding CBT focused groups to better understand the role of CBT on self-efficacy and depression in persons with chronic pain and depression.
The primary purpose of this study is to evaluate the degree of statistical agreement between observed clinical outcomes (non-response/remission) after 8 weeks of treatment and the outcomes predicted by an Augmented Human Intelligence (AHI)-based clinical decision support tool after 2 weeks of follow up.
In this project the investigators will develop and pilot test a supervised, vigorous intensity exercise intervention for depressed female smokers. If the pilot intervention is successful, the investigators will have a blueprint for a large randomized controlled trial. The long term objective is to develop interventions for depressed women that will ultimately reduce their risk of tobacco-caused disease and mortality.
The purpose of this study is to assess the feasibility and acceptability of passive data collection with a smartphone in depressed patients and investigate how passive data gathered via technology platforms can generate transdiagnostic digital phenotypes that potentially inform the assessment and/or treatment outcome of major mood disorders. This study aims to assess self-reported, behavioral, cognitive, and physiological data gathered from smartphones and smart watches as compared to gold standard clinical measured in treatment seeking depressed patients.
The purpose of this study is to gather information regarding the use of rTMS as a treatment for depression in adolescents with Major Depressive Disorder. The investigators also hope to learn if measures of brain activity (cortical excitability and inhibition) collected with transcranial magnetic stimulation (TMS) can be used to identify which patients will benefit from certain types of rTMS treatment.
This research proposal aims to better understand the neurobiology of depression in adolescents and how repetitive transcranial magnetic stimulation (rTMS) may therapeutically impact brain function and mood. This investigation also proposes the first study to examine the efficacy of rTMS maintenance therapy in adolescents who have met clinical criteria following acute rTMS treatment. The magnetic resonance (MR) spectroscopy pattern of rTMS response will be analyzed according to previously established protocols.
The overall goal of this investigator-initiated trial is to evaluate the impact of platform algorithm products designed to rapidly identify pharmacokinetic (PK) and/or pharmacodynamic (PD) genomic variation on treatment outcome of depression in adolescents. This new technology may have the potential to optimize treatment selection by improving response, minimizing unfavorable adverse events / side effects and increasing treatment adherence
The purpose of this research study is to find out if the medication known as ketamine can help the symptoms of depression. This drug is approved by the Food and Drug Administration (FDA) but the investigators will use it for a non-FDA approved reason (depression).
The purpose of this study is to explore whether Medibio’s system can provide objective measures of response to standard medication treatment for unipolar depression and bipolar depression, and to see if the system can tell these two conditions apart.
Medibio’s system uses software to analyse a person’s heart rate, activity, and posture to provide objective measures of a person’s autonomic nervous system, sleep, and other daily patterns.
This research study aims to test the safety and effectiveness of repetitive transcranial magnetic stimulation (rTMS) on teens with depression. The study also seeks to understand how rTMS treatment affects the neurobiology of teens with depression.
The purpose of this study is to learn if measures of brain chemicals from a brain scan called Magnetic Resonance Imaging and Spectroscopy (MRI/MRS) and brain activity (known as cortical excitability and inhibition) collected by Transcranial Magnetic Stimulation (TMS) are different in adolescents with depression who are in different stages of treatment. Researchers are conducting this study to learn more about how the brain works in adolescents with depression and without depression (healthy controls). This is important because it may identify a biological marker (a measure of how bad an illness is) for depression that could one day be used ...
The proposed study seeks to obtain preliminary signal of the tolerability and efficacy of transcranial direct current stimulation (tDCS) for depressive symptoms in a sample of adolescents with depression and epilepsy. Additionally, effects of tDCS will be assessed via electroencephalographic, cognitive, and psychosocial measures.
The purpose of this study is to contribute to our understanding of the relationships between social media use in adolescents and psychological development, psychiatric comorbidity, and physiological markers of stress.
Quetiapine, a second generation antipsychotic, is only available as oral tablets. However, topical and rectal formulations have been produced in compounding pharmacies. There is no data available suggesting that topical or rectal formulations provide serum levels similar to oral medication. In the clinical setting, when oral administration of quetiapine is not possible (for example, when a patient is extremely ill physically or mentally or both), clinicians and pharmacists have collaborated in such cases and have at times had to administer quetiapine compounded in other dosage formulations such as rectal or topical formulations. Despite clinical effectiveness of these "other" formulations, there ...
The purposes of this study are to summarize clinician evaluations of the NNDC battery in the single clinic where the adult battery is currently being administered to adolescents, to determine patient and clinician level of interest in using the NNDC battery in clinics where the adult battery is not currently being administered to adolescent patients (n=14), to measure change in evaluation 3 months post-implementation for any sites that begin administering the NNDC battery to adolescents, and to generate potential new Child and Adolescent Mood Disorders Interest Group (CAMDIG) research protocols for future consideration.
The overall goal of this investigator-initiated trial is to evaluate the treatment outcome of depression utilizing platform algorithm products that can allow rapid identification of pharmacokinetic (PK) and/or pharmacodynamic (PD) genomic variation. This new technology may have the potential to optimize treatment selection by improving response, minimizing unfavorable adverse events / side effects and increasing treatment adherence.
Transcranial Magnetic Stimulation (TMS) is an increasingly accepted neurostimulation- based treatment for major depressive disorder. While there is a growing anecdotal database supporting its use in bipolar depression the investigators propose to collect open label efficacy and safety data in a small population of patients with clinically verified bipolar disorder.
The purpose of this study is to assess the effectiveness and safety of MYDAYIS® as an augmentation agent for bipolar depression.
The purpose of this study is to determine the baseline chronotype patterns (with Morningness-Eveningness Questionnaire (MEQ) ) among inpatients with Major depressive disorder and then compare the chronotype distribution with the control group.
The purpose of this study is to validate measures of depression, anxiety, traumatic stress, and factors related to these outcomes in medical patients, to develop a model for identifying persons with myocarditis who are at risk for depressive and anxiety disorders (clinically significant depressive and anxious symptoms), and for examining the effects of anxiety and depression on quality of life and health outcomes in respondents with myocarditis and caregivers.
This feasibility study aims to better understand the neurobiology of major depression and how ketamine may therapeutically impact brain function. This research may provide important insights into the mechanism of ketamine response, thus, potentially increasing the likelihood of successful treatment interventions and decrease the number of ineffective treatments and/or risk for serious side effects.
The purpose of this study is to analyze the prevalence of mood disorders in newly-diagnosed breast cancer patients with use of specific questionnaires, aimed to diagnose clinically significant depression and anxiety, at a rural community hospital.
The FLAME Study is a 16-week clinical trial to study treatment with lamotrigine or fluoxetine in bipolar I, II and bipolar schizoaffective depressed adults. The purpose of the trial is to have a better understanding of whether individuals with a particular gene type and other inherited biological markers will have a good response to fluoxetine or lamotrigine, or alternatively, would be more likely to have side effects to this medication.
This study aims to assess the level of anxiety and depression in children with epilepsy and compare to the level of anxiety and depression perceived by family by using validated, standardized measures as both comorbid conditions can significantly impact both quality of life and disease course.
People with COPD have a greater risk for symptoms of depression, anxiety, and fear of breathlessness. Those emotions are independently associated with lower physical activity, poorer quality of life, and higher hospitalization and exacerbations; all independent predictors of survival and costs. There is a lack of treatment options to be routinely used in primary clinics for patients with COPD. Systematic reviews suggest that interventions that promote an accepting mode of response, such as mindfulness, might be more appropriate and effective for managing psychological distress in COPD patients, especially breathing-related anxiety. Hypothesis: A home-based 8-week Mindfulness-Based Stress Reduction (MBSR) for COPD ...
The purpose of this study is to examine the effects of a health coaching intervention on the stress and burden of caregivers of patients awaiting heart or lung transplant.
Hypotheses: Caregivers will have traits and behaviors pre-transplant that will predict caregiver readiness, quality of life, and transplant recipient outcomes. Specifically, thoracic pre-transplant caregivers report stress, symptoms of anxiety or depression, and perceive high caregiver burden. These factors may be amenable to pre-transplant intervention to improve overall patient and caregiver outcomes.
Aims, purpose, or objectives: We will conduct a pilot trial to test whether caregivers of heart and lung transplant candidates ...
In an effort to understand the effects of evidence-based interventions on children and adolescents, the aims of this study are to 1) evaluate the feasibility of utilizing wearable devices to track health information (i.e., sleep, physical activity); 2) evaluate the effectiveness of evidence-based intervention components on emotional and interpersonal functioning, family engagement, and sleep and physical activity level outcomes.
The purpose of this study is to implement a facilitated peer support group for women that have experienced an unexpected birth process in the last 12 months.
Data collected from the MEVOKED Study #1 (IRB#14-009159) showed wide variability in how participants engaged with and used the MEVOKED program. This study will obtain additional information on participants – in particular PHQ9 depression scores and medication use during their enrollment in the MEVOKED program will provide additional data to support the analysis of the MEVOKED Study #1 (IRB#14-009159).
The goal of this proposed study is to examine the genetic signature of the validated proteomic signature (model) based on a panel of serum proteomic markers that discriminates different mood disorders.
The purpose of this research study is to compare the antidepressant effect of lithium versus placebo in adults receiving ketamine. Lithium is available commercially for depression; ketamine is available commercially and can help the symptoms of depression; however, it has not been approved by the U.S. Food and Drug Administration (FDA) for this use. The FDA has allowed the use of this drug in this research study.
The proposed study will examine sequential bilateral accelerated theta burst stimulation (aTBS). Three sessions are administered daily for 10 days (5 days per week). During each session continuous theta burst stimulation (cTBS) in which 1800 pulses are delivered continuously over 120 seconds to the right dorsolateral prefrontal cortex (RDPFC) is administered first, followed by iTBS in which 1800 pulses are delivered in 2 second bursts, repeated every 10 seconds for 570 seconds (1800 pulses) to the left dorsolateral prefrontal cortex (LDPFC). The theta burst stimulation (TBS) parameters were adopted from prior work, with 3-pulse 50 Hz bursts given ...
The purpose of this study is to study brain chemistry in depressed patients compared to healthy patients who are not depressed.
The purpose of this study is to:
- Increase screening of adolescents for symptoms of depression in primary care La Crosse, WI clinics using the PHQ9M screening tool.Screening to occur at all well child visits and all subsequent visits for adolescents with Depression on their problem list.Clinics to include Pediatrics, Family Medicine, Family Health, Center for Womens Health.
- Develop a clear care pathway for adolescents identified with clinically meaningful symptoms of depression through increased screening, referral and treatment options. Pathway may include psychoeducational materials (multimedia options), intake paperwork and process for Department of Behavioral Health locally, and ...
This study will compare glutamate and other neurometabolites measured by proton magnetic resonance spectroscopy (1H-MRS) in bipolar I and II patients currently depressed with age-matched healthy controls. The study will also compare 1H-MRS of bipolar I and II patients before and after taking a 12-week course of lamotrigine. This study requires 8 visits over a 12 week period. These visits need to occur at Mayo Clinic in Rochester, MN.
The overall goal is to better understand the underlying pathophysiology of mood disorders and bipolar disorders in particular. We aim to investigate whether the subclinical atherosclerotic and inflammatory markers differ between patients with bipolar disorder, major depressive disorder, and psychiatric non-mood disorders and healthy subjects.
The purpose of this study is to identify pre-operative emotional factors that may affect surgical outcomes and how a multidisciplinary approach may improve success after urologic surgery for voiding dysfunction.
The purpose of this study is to promote patient-centered care by efficiently determining the presence of quality of life issues and their relation to depression and psoriatic arthritis in psoriasis patients. Screening for quality of life, depression, and psoriatic arthritis is a standard of care for psoriasis patients.
The purpose of this study is to evaluate the impact of interventions on important CV biomarkers to provide valuable information on the mechanism linking depression and anxiety to cardiac prognosis resulting in improved quality of life and diagnosis.
Study hypothesis: Do serial low-dose ketamine infusions, followed by weekly maintenance infusions, increase the length of time depressive symptoms stay in remission and the length of time associated suicide risk is improved? Brief Summary: This open label clinical trial is intended to further clarify initial response to low-dose ketamine infusion with repeated dosing and maintenance treatment model. Primary outcomes will be reduction in depression severity and reduction of suicide risk along with duration of response.
The purpose of this research is to gather information from the child and parent with regards to the use of electronic treatment tools to treat those with a mental health illness.
The purpose of this study is to remotely use the Ellipsis Health (EH) voice analysis technology to record the speech patterns and content of individuals with a recent diagnosis of Coronavirus-19 (COVID-19) presenting to the post-COVID-19 clinic at Mayo Clinic, to validate its use as a tool to screen for major depressive disorder (MDD) and generalized anxiety disorder (GAD) against gold-standard questionnaires used in clinical practice namely the PHQ-9 and GAD-7
Primary Aim
We aim to evaluate: 1) the correlation between patient-reported rectal bleeding and stool frequency and health-related quality of life focused on fatigue, depression and anxiety, and work productivity; and 2) the correlation between the severity of endoscopic inflammation and health-related quality of life focused on fatigue, depression and anxiety, and work productivity.
Secondary Aims
We also aim to evaluate the correlation between the combination of clinical/PRO and the severity of endoscopic inflammation and health-related quality of life focused on fatigue, depression and anxiety, and work productivity.
The purpose of this study is to evaluate the long-term impact of treatment with sertraline on aspects of cognitive, emotional and physical development and maturation at puberty, in pediatric subjects ages 6 to 16 years (inclusive) with a diagnosis of anxiety disorder, depressive disorder or obsessive compulsive disorder.
The purpose of this study is to see if there is a connection between bad experiences in the patient's childhood, either by the patient or the parent, and poor blood sugar control, obesity, poor blood lipid levels, and depression in patients with type 1 diabetes.
Physical activity plays an important role in reducing the adverse effects of cancer treatment. There are few studies using prehabilitation to improve peri-operative outcomes in patients undergoing cancer surgery. This study will pilot a program of structured activity for women undergoing neoadjuvant chemotherapy with the intent to improve their physical state prior to surgical intervention and thus improve outcomes.
It has been shown that patients with advanced ovarian cancer may suffer from high levels of cancer –specific distress, depression and anxiety. It has also been proposed that psychological resilience can favorably affect psychological and treatment-related outcomes in cancer ...
The purpose of this study is to measure the frequency and severity of posttraumatic stress symptoms, depressive symptoms, anxiety symptoms, and cognitive impairment following dismissal from the ICU and three months later. This study also seeks to identify which of the multiple ICUs at Mayo Clinic yields the highest incidence of post-intensive care syndrome so that a future study designed to provide a therapeutic intervention can be implemented in those areas with the greatest potential.
The purpose of this study is to compare the effectiveness of combination therapy with antidepressants (AD), fear avoidance rehabilitation (EFAR) AD+EFAR vs. each treatment alone to improve pain, self-reported function, depression, and anxiety in patients with chronic low back pain and high negative affect.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
- Katelyn M. Cooper
- Logan E. Gin
- M. Elizabeth Barnes
- Sara E. Brownell
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Department of Biology, University of Central Florida, Orlando, FL, 32816
Search for more papers by this author
Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates’ symptoms of depression affect their research experiences and how research affects undergraduates’ feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students’ depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students’ social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students’ depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
INTRODUCTION
Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed ( American Psychiatric Association [APA], 2013 ). Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings of worthlessness or excessive guilt, and suicidality ( APA, 2013 ). While depression results from a complex interaction of psychological, social, and biological factors ( World Health Organization, 2018 ), studies have shown that increased stress caused by college can be a significant contributor to student depression ( Dyson and Renk, 2006 ).
Depression is one of the top undergraduate mental health concerns, and the rate of depression among undergraduates continues to rise ( Center for Collegiate Mental Health, 2017 ). While we cannot discern whether these increasing rates of depression are due to increased awareness or increased incidence, it is clear that is a serious problem on college campuses. The percent of U.S. college students who self-reported a diagnosis with depression was recently estimated to be about 25% ( American College Health Association, 2019 ). However, higher rates have been reported, with one study estimating that up to 84% of undergraduates experience some level of depression ( Garlow et al. , 2008 ). Depression rates are typically higher among university students compared with the general population, despite being a more socially privileged group ( Ibrahim et al. , 2013 ). Prior studies have found that depression is negatively correlated with overall undergraduate academic performance ( Hysenbegasi et al. , 2005 ; Deroma et al. , 2009 ; American College Health Association, 2019 ). Specifically, diagnosed depression is associated with half a letter grade decrease in students’ grade point average ( Hysenbegasi et al. , 2005 ), and 21.6% of undergraduates reported that depression negatively affected their academic performance within the last year ( American College Health Association, 2019 ). Provided with a list of academic factors that may be affected by depression, students reported that depression contributed to lower exam grades, lower course grades, and not completing or dropping a course.
Students in the natural sciences may be particularly at risk for depression, given that such majors are noted to be particularly stressful due to their competitive nature and course work that is often perceived to “weed students out”( Everson et al. , 1993 ; Strenta et al. , 1994 ; American College Health Association, 2019 ; Seymour and Hunter, 2019 ). Science course instruction has also been described to be boring, repetitive, difficult, and math-intensive; these factors can create an environment that can trigger depression ( Seymour and Hewitt, 1997 ; Osborne and Collins, 2001 ; Armbruster et al ., 2009 ; Ceci and Williams, 2010 ). What also distinguishes science degree programs from other degree programs is that, increasingly, undergraduate research experiences are being proposed as an essential element of a science degree ( American Association for the Advancement of Science, 2011 ; President’s Council of Advisors on Science and Technology, 2012 ; National Academies of Sciences, Engineering, and Medicine [NASEM], 2017 ). However, there is some evidence that undergraduate research experiences can add to the stress of college for some students ( Cooper et al. , 2019c ). Students can garner multiple benefits from undergraduate research, including enhanced abilities to think critically ( Ishiyama, 2002 ; Bauer and Bennett, 2003 ; Brownell et al. , 2015 ), improved student learning ( Rauckhorst et al. , 2001 ; Brownell et al. , 2015 ), and increased student persistence in undergraduate science degree programs ( Jones et al. , 2010 ; Hernandez et al. , 2018 ). Notably, undergraduate research experiences are increasingly becoming a prerequisite for entry into medical and graduate programs in science, particularly elite programs ( Cooper et al. , 2019d ). Although some research experiences are embedded into formal lab courses as course-based undergraduate research experiences (CUREs; Auchincloss et al. , 2014 ; Brownell and Kloser, 2015 ), the majority likely entail working with faculty in their research labs. These undergraduate research experiences in faculty labs are often added on top of a student’s normal course work, so they essentially become an extracurricular activity that they have to juggle with course work, working, and/or personal obligations ( Cooper et al. , 2019c ). While the majority of the literature surrounding undergraduate research highlights undergraduate research as a positive experience ( NASEM, 2017 ), studies have demonstrated that undergraduate research experiences can be academically and emotionally challenging for students ( Mabrouk and Peters, 2000 ; Seymour et al. , 2004 ; Cooper et al. , 2019c ; Limeri et al. , 2019 ). In fact, 50% of students sampled nationally from public R1 institutions consider leaving their undergraduate research experience prematurely, and about half of those students, or 25% of all students, ultimately leave their undergraduate research experience ( Cooper et al. , 2019c ). Notably, 33.8% of these individuals cited a negative lab environment and 33.3% cited negative relationships with their mentors as factors that influenced their decision about whether to leave ( Cooper et al. , 2019c ). Therefore, students’ depression may be exacerbated in challenging undergraduate research experiences, because studies have shown that depression is positively correlated with student stress ( Hish et al. , 2019 ).
While depression has not been explored in the context of undergraduate research experiences, depression has become a prominent concern surrounding graduate students conducting scientific research. A recent study that examined the “graduate student mental health crisis” ( Flaherty, 2018 ) found that work–life balance and graduate students’ relationships with their research advisors may be contributing to their depression ( Evans et al. , 2018 ). Specifically, this survey of 2279 PhD and master’s students from diverse fields of study, including the biological/physical sciences, showed that 39% of graduate students have experienced moderate to severe depression. Fifty-five percent of the graduate students with depression who were surveyed disagreed with the statement “I have good work life balance,” compared to only 21% of students with depression who agreed. Additionally, the study highlighted that more students with depression disagreed than agreed with the following statements: their advisors provided “real” mentorship, their advisors provided ample support, their advisors positively impacted their emotional or mental well-being, their advisors were assets to their careers, and they felt valued by their mentors. Another recent study identified that depression severity in biomedical doctoral students was significantly associated with graduate program climate, a perceived lack of employment opportunities, and the quality of students’ research training environment ( Nagy et al. , 2019 ). Environmental stress, academic stress, and family and monetary stress have also been shown to be predictive of depression severity in biomedical doctoral students ( Hish et al. , 2019 ). Further, one study found that self-esteem is negatively correlated and stress is positively correlated with graduate student depression; presumably research environments that challenge students’ self-esteem and induce stress are likely contributing to depressive symptoms among graduate students ( Kreger, 1995 ). While these studies have focused on graduate students, and there are certainly notable distinctions between graduate and undergraduate research, the research-related factors that affect graduate student depression, including work–life balance, relationships with mentors, research environment, stress, and self-esteem, may also be relevant to depression among undergraduates conducting research. Importantly, undergraduates in the United States have reported identical levels of depression as graduate students but are often less likely to seek mental health care services ( Wyatt and Oswalt, 2013 ), which is concerning if undergraduate research experiences exacerbate depression.
Based on the literature on the stressors of undergraduate research experiences and the literature identifying some potential causes of graduate student depression, we identified three aspects of undergraduate research that may exacerbate undergraduates’ depression. Mentoring: Mentors can be an integral part of a students’ research experience, bolstering their connections with others in the science community, scholarly productivity, and science identity, as well as providing many other benefits ( Thiry and Laursen, 2011 ; Prunuske et al. , 2013 ; Byars-Winston et al. , 2015 ; Aikens et al. , 2016 , 2017 ; Thompson et al. , 2016 ; Estrada et al. , 2018 ). However, recent literature has highlighted that poor mentoring can negatively affect undergraduate researchers ( Cooper et al. , 2019c ; Limeri et al. , 2019 ). Specifically, one study of 33 undergraduate researchers who had conducted research at 10 institutions identified seven major ways that they experienced negative mentoring, which included absenteeism, abuse of power, interpersonal mismatch, lack of career support, lack of psychosocial support, misaligned expectations, and unequal treatment ( Limeri et al. , 2019 ). We hypothesize negative mentoring experiences may be particularly harmful for students with depression, because support, particularly social support, has been shown to be important for helping individuals with depression cope with difficult circumstances ( Aneshensel and Stone, 1982 ; Grav et al. , 2012 ). Failure: Experiencing failure has been hypothesized to be an important aspect of undergraduate research experiences that may help students develop some the most distinguishing abilities of outstanding scientists, such as coping with failure, navigating challenges, and persevering ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, experiencing failure and the stress and fatigue that often accompany it may be particularly tough for students with depression ( Aldwin and Greenberger, 1987 ; Mongrain and Blackburn, 2005 ). Lab environment: Fairness, inclusion/exclusion, and social support within one’s organizational environment have been shown to be key factors that cause people to either want to remain in the work place and be productive or to want to leave ( Barak et al. , 2006 ; Cooper et al. , 2019c ). We hypothesize that dealing with exclusion or a lack of social support may exacerbate depression for some students; patients with clinical depression react to social exclusion with more pronounced negative emotions than do individuals without clinical depression ( Jobst et al. , 2015 ). While there are likely other aspects of undergraduate research that affect student depression, we hypothesize that these factors have the potential to exacerbate negative research experiences for students with depression.
Depression has been shown to disproportionately affect many populations that are underrepresented or underserved within the scientific community, including females ( American College Health Association, 2018 ; Evans et al. , 2018 ), first-generation college students ( Jenkins et al. , 2013 ), individuals from low socioeconomic backgrounds ( Eisenberg et al. , 2007 ), members of the LGBTQ+ community ( Eisenberg et al. , 2007 ; Evans et al. , 2018 ), and people with disabilities ( Turner and Noh, 1988 ). Therefore, as the science community strives to be more diverse and inclusive ( Intemann, 2009 ), it is important that we understand more about the relationship between depression and scientific research, because negative experiences with depression in scientific research may be contributing to the underrepresentation of these groups. Specifically, more information is needed about how the research process and environment of research experiences may affect depression.
Given the high rate of depression among undergraduates, the links between depression and graduate research, the potentially challenging environment of undergraduate research, and how depression could disproportionately impact students from underserved communities, it is imperative to begin to explore the relationship between scientific research and depression among undergraduates to create research experiences that could maximize student success. In this exploratory interview study, we aimed to 1) describe how undergraduates’ symptoms of depression affect their research experiences, 2) understand how undergraduate research affects students’ feelings of depression, and 3) identify recommendations based on the literature and undergraduates’ reported experiences to promote a positive research experience for students with depression.
This study was done with an approved Arizona State University Institutional Review Board protocol #7247.
In Fall 2018, we surveyed undergraduate researchers majoring in the life sciences across 25 research-intensive (R1) public institutions across the United States (specific details about the recruitment of the students who completed the survey can be found in Cooper et al. (2019c) ). The survey asked students for their opinions about their undergraduate research experiences and their demographic information and whether they would be interested in participating in a follow-up interview related to their research experiences. For the purpose of this study, we exclusively interviewed students about their undergraduate research experiences in faculty member labs; we did not consider students’ experiences in CUREs. Of the 768 undergraduate researchers who completed the survey, 65% ( n = 496) indicated that they would be interested in participating in a follow-up interview. In Spring 2019, we emailed the 496 students, explaining that we were interested in interviewing students with depression about their experiences in undergraduate research. Our specific prompt was: “If you identify as having depression, we would be interested in hearing about your experience in undergraduate research in a 30–60 minute online interview.” We did not define depression in our email recruitment because we conducted think-aloud interviews with four undergraduates who all correctly interpreted what we meant by depression ( APA, 2013 ). We had 35 students agree to participate in the interview study. The interview participants represented 12 of the 25 R1 public institutions that were represented in the initial survey.
Student Interviews
We developed an interview script to explore our research questions. Specifically, we were interested in how students’ symptoms of depression affect their research experiences, how undergraduate research negatively affects student depression, and how undergraduate research positively affects student depression.
We recognized that mental health, and specifically depression, can be a sensitive topic to discuss with undergraduates, and therefore we tried to minimize any discomfort that the interviewees might experience during the interview. Specifically, we conducted think-aloud interviews with three graduate students who self-identified with having depression at the time of the interview. We asked them to note whether any interview questions made them uncomfortable. We also sought their feedback on questions given their experiences as persons with depression who had once engaged in undergraduate research. We revised the interview protocol after each think-aloud interview. Next, we conducted four additional think-aloud interviews with undergraduates conducting basic science or biology education research who identified with having depression to establish cognitive validity of the questions and to elicit additional feedback about any questions that might make someone uncomfortable. The questions were revised after each think-aloud interview until no question was unclear or misinterpreted by the students and we were confident that the questions minimized students’ potential discomfort ( Trenor et al. , 2011 ). A copy of the final interview script can be found in the Supplemental Material.
All interviews were individually conducted by one of two researchers (K.M.C. and L.E.G.) who conducted the think-aloud interviews together to ensure that their interviewing practices were as similar as possible. The interviews were approximately an hour long, and students received a $15 gift card for their participation.
Personal, Research, and Depression Demographics
All student demographics and information about students’ research experiences were collected using the survey distributed to students in Fall 2018. We collected personal demographics, including the participants’ gender, race/ethnicity, college generation status, transfer status, financial stability, year in college, major, and age. We also collected information about the students’ research experiences, including the length of their first research experiences, the average number of hours they spend in research per week, how they were compensated for research, who their primary mentors were, and the focus areas of their research.
In the United States, mental healthcare is disproportionately unavailable to Black and Latinx individuals, as well as those who come from low socioeconomic backgrounds ( Kataoka et al. , 2002 ; Howell and McFeeters, 2008 ; Santiago et al. , 2013 ). Therefore, to minimize a biased sample, we invited anyone who identified with having depression to participate in our study; we did not require students to be diagnosed with depression or to be treated for depression in order to participate. However, we did collect information about whether students had been formally diagnosed with depression and whether they had been treated for depression. After the interview, all participants were sent a link to a short survey that asked them if they had ever been diagnosed with depression and how, if at all, they had ever been treated for depression. A copy of these survey questions can be found in the Supplemental Material. The combined demographic information of the participants is in Table 1 . The demographics for each individual student can be found in the Supplemental Material.
a Students reported the time they had spent in research 6 months before being interviewed and only reported on the length of time of their first research experiences.
b Students were invited to report multiple ways in which they were treated for their depression; other treatments included lifestyle changes and meditation.
c Students were invited to report multiple means of compensation for their research if they had been compensated for their time in different ways.
d Students were asked whether they felt financially stable, particularly during the undergraduate research experience.
e Students reported who they work/worked with most closely during their research experiences.
f Staff members included lab coordinators or lab managers.
g Other focus areas of research included sociology, linguistics, psychology, and public health.
Interview Analysis
The initial interview analysis aimed to explore each idea that a participant expressed ( Charmaz, 2006 ) and to identify reoccurring ideas throughout the interviews. First, three authors (K.M.C., L.E.G., and S.E.B.) individually reviewed a different set of 10 interviews and took detailed analytic notes ( Birks and Mills, 2015 ). Afterward, the authors compared their notes and identified reoccurring themes throughout the interviews using open coding methods ( Saldaña, 2015 ).
Once an initial set of themes was established, two researchers (K.M.C. and L.E.G.) individually reviewed the same set of 15 randomly selected interviews to validate the themes identified in the initial analysis and to screen for any additional themes that the initial analysis may have missed. Each researcher took detailed analytic notes throughout the review of an interview, which they discussed after reviewing each interview. The researchers compared what quotes from each interview they categorized into each theme. Using constant comparison methods, they assigned quotes to each theme and constantly compared the quotes to ensure that each quote fit within the description of the theme ( Glesne and Peshkin, 1992 ). In cases in which quotes were too different from other quotes, a new theme was created. This approach allowed for multiple revisions of the themes and allowed the authors to define a final set of codes; the researchers created a final codebook with refined definitions of emergent themes (the final coding rubric can be found in the Supplemental Material). Once the final codebook was established, the researchers (K.M.C. and L.E.G.) individually coded seven additional interviews (20% of all interviews) using the coding rubric. The researchers compared their codes, and their Cohen’s κ interrater score for these seven interviews was at an acceptable level (κ = 0.88; Landis and Koch, 1977 ). One researcher (L.E.G.) coded the remaining 28 out of 35 interviews. The researchers determined that data saturation had been reached with the current sample and no further recruitment was needed ( Guest et al. , 2006 ). We report on themes that were mentioned by at least 20% of students in the interview study. In the Supplemental Material, we provide the final coding rubric with the number of participants whose interview reflected each theme ( Hannah and Lautsch, 2011 ). Reporting the number of individuals who reported themes within qualitative data can lead to inaccurate conclusions about the generalizability of the results to a broader population. These qualitative data are meant to characterize a landscape of experiences that students with depression have in undergraduate research rather than to make claims about the prevalence of these experiences ( Glesne and Peshkin, 1992 ). Because inferences about the importance of these themes cannot be drawn from these counts, they are not included in the results of the paper ( Maxwell, 2010 ). Further, the limited number of interviewees made it not possible to examine whether there were trends based on students’ demographics or characteristics of their research experiences (e.g., their specific area of study). Quotes were lightly edited for clarity by inserting clarification brackets and using ellipses to indicate excluded text. Pseudonyms were given to all students to protect their privacy.
The Effect of Depressive Symptoms on Undergraduate Research
We asked students to describe the symptoms associated with their depression. Students described experiencing anxiety that is associated with their depression; this could be anxiety that precedes their depression or anxiety that results from a depressive episode or a period of time when an individual has depression symptoms. Further, students described difficulty getting out of bed or leaving the house, feeling tired, a lack of motivation, being overly self-critical, feeling apathetic, and having difficulty concentrating. We were particularly interested in how students’ symptoms of depression affected their experiences in undergraduate research. During the think-aloud interviews that were conducted before the interview study, graduate and undergraduate students consistently described that their depression affected their motivation in research, their creativity in research, and their productivity in research. Therefore, we explicitly asked undergraduate researchers how, if at all, their depression affected these three factors. We also asked students to describe any additional ways in which their depression affected their research experiences. Undergraduate researchers commonly described five additional ways in which their depression affected their research; for a detailed description of each way students’ research was affected and for example quotes, see Table 2 . Students described that their depression negatively affected their productivity in the lab. Commonly, students described that their productivity was directly affected by a lack of motivation or because they felt less creative, which hindered the research process. Additionally, students highlighted that they were sometimes less productive because their depression sometimes caused them to struggle to engage intellectually with their research or caused them to have difficulty remembering or concentrating; students described that they could do mundane or routine tasks when they felt depressed, but that they had difficulty with more complex and intellectually demanding tasks. However, students sometimes described that even mundane tasks could be difficult when they were required to remember specific steps; for example, some students struggled recalling a protocol from memory when their depression was particularly severe. Additionally, students noted that their depression made them more self-conscious, which sometimes held them back from sharing research ideas with their mentors or from taking risks such as applying to competitive programs. In addition to being self-conscious, students highlighted that their depression caused them to be overly self-critical, and some described experiencing imposter phenomenon ( Clance and Imes, 1978 ) or feeling like they were not talented enough to be in research and were accepted into a lab by a fluke or through luck. Finally, students described that depression often made them feel less social, and they struggled to socially engage with other members of the lab when they were feeling down.
The Effect of Undergraduate Research Experiences on Student Depression
We also wanted to explore how research impacted students’ feelings of depression. Undergraduates described how research both positively and negatively affected their depression. In the following sections, we present aspects of undergraduate research and examine how each positively and/or negatively affected students’ depression using embedded student quotes to highlight the relationships between related ideas.
Lab Environment: Relationships with Others in the Lab.
Some aspects of the lab environment, which we define as students’ physical, social, or psychological research space, could be particularly beneficial for students with depression.
Specifically, undergraduate researchers perceived that comfortable and positive social interactions with others in the lab helped their depression. Students acknowledged how beneficial their relationships with graduate students and postdocs could be.
Marta: “I think always checking in on undergrads is important. It’s really easy [for us] to go a whole day without talking to anybody in the lab. But our grad students are like ‘Hey, what’s up? How’s school? What’s going on?’ (…) What helps me the most is having that strong support system. Sometimes just talking makes you feel better, but also having people that believe in you can really help you get out of that negative spiral. I think that can really help with depression.”
Kelley: “I know that anytime I need to talk to [my postdoc mentors] about something they’re always there for me. Over time we’ve developed a relationship where I know that outside of work and outside of the lab if I did want to talk to them about something I could talk to them. Even just talking to someone about hobbies and having that relationship alone is really helpful [for depression].”
In addition to highlighting the importance of developing relationships with graduate students or postdocs in the lab, students described that forming relationships with other undergraduates in the lab also helped their depression. Particularly, students described that other undergraduate researchers often validated their feelings about research, which in turn helped them realize that what they are thinking or feeling is normal, which tended to alleviate their negative thoughts. Interestingly, other undergraduates experiencing the same issues could sometimes help buffer them from perceiving that a mentor did not like them or that they were uniquely bad at research. In this article, we use the term “mentor” to refer to anyone who students referred to in the interviews as being their mentors or managing their research experiences; this includes graduate students, postdoctoral scholars, lab managers, and primary investigators (PIs).
Abby: “One of my best friends is in the lab with me. A lot of that friendship just comes from complaining about our stress with the lab and our annoyance with people in the lab. Like when we both agree like, ‘Yeah, the grad students were really off today, it wasn’t us,’ that helps. ‘It wasn’t me, it wasn’t my fault that we were having a rough day in lab; it was the grad students.’ Just being able to realize, ‘Hey, this isn’t all caused by us,’ you know? (…) We understand the stresses in the lab. We understand the details of what each other are doing in the lab, so when something doesn’t work out, we understand that it took them like eight hours to do that and it didn’t work. We provide empathy on a different level.”
Meleana: “It’s great to have solidarity in being confused about something, and it’s just that is a form of validation for me too. When we leave a lab meeting and I look at [another undergrad] I’m like, ‘Did you understand anything that they were just saying?’ And they’re like, ‘Oh, no.’ (…) It’s just really validating to hear from the other undergrads that we all seem to be struggling with the same things.”
Developing positive relationships with faculty mentors or PIs also helped alleviate some students’ depressive feelings, particularly when PIs shared their own struggles with students. This also seemed to normalize students’ concerns about their own experiences.
Alexandra: “[Talking with my PI] is helpful because he would talk about his struggles, and what he faced. A lot of it was very similar to my struggles. For example, he would say, ‘Oh, yeah, I failed this exam that I studied so hard for. I failed the GRE and I paid so much money to prepare for it.’ It just makes [my depression] better, like okay, this is normal for students to go through this. It’s not an out of this world thing where if you fail, you’re a failure and you can’t move on from it.”
Students’ relationships with others in the lab did not always positively impact their depression. Students described instances when the negative moods of the graduate students and PIs would often set the tone of the lab, which in turn worsened the mood of the undergraduate researchers.
Abby: “Sometimes [the grad students] are not in a good mood. The entire vibe of the lab is just off, and if you make a joke and it hits somebody wrong, they get all mad. It really depends on the grad students and the leadership and the mood that they’re in.”
Interviewer: “How does it affect your depression when the grad students are in a bad mood?”
Abby: “It definitely makes me feel worse. It feels like, again, that I really shouldn’t go ask them for help because they’re just not in the mood to help out. It makes me have more pressure on myself, and I have deadlines I need to meet, but I have a question for them, but they’re in a bad mood so I can’t ask. That’s another day wasted for me and it just puts more stress, which just adds to the depression.”
Additionally, some students described even more concerning behavior from research mentors, which negatively affected their depression.
Julie: “I had a primary investigator who is notorious in the department for screaming at people, being emotionally abusive, unreasonable, et cetera. (…) [He was] kind of harassing people, demeaning them, lying to them, et cetera, et cetera. (…) Being yelled at and constantly demeaned and harassed at all hours of the day and night, that was probably pretty bad for me.”
While the relationships between undergraduates and graduate, postdoc, and faculty mentors seemed to either alleviate or worsen students’ depressive symptoms, depending on the quality of the relationship, students in this study exclusively described their relationships with other undergraduates as positive for their depression. However, students did note that undergraduate research puts some of the best and brightest undergraduates in the same environment, which can result in students comparing themselves with their peers. Students described that this comparison would often lead them to feel badly about themselves, even though they would describe their personal relationship with a person to be good.
Meleana: “In just the research field in general, just feeling like I don’t really measure up to the people around me [can affect my depression]. A lot of the times it’s the beginning of a little spiral, mental spiral. There are some past undergrads that are talked about as they’re on this pedestal of being the ideal undergrads and that they were just so smart and contributed so much to the lab. I can never stop myself from wondering like, ‘Oh, I wonder if I’m having a contribution to the lab that’s similar or if I’m just another one of the undergrads that does the bare minimum and passes through and is just there.’”
Natasha: “But, on the other hand, [having another undergrad in the lab] also reminded me constantly that some people are invested in this and meant to do this and it’s not me. And that some people know a lot more than I do and will go further in this than I will.”
While students primarily expressed that their relationships with others in the lab affected their depression, some students explained that they struggled most with depression when the lab was empty; they described that they did not like being alone in the lab, because a lack of stimulation allowed their minds to be filled with negative thoughts.
Mia: “Those late nights definitely didn’t help [my depression]. I am alone, in the entire building. I’m left alone to think about my thoughts more, so not distracted by talking to people or interacting with people. I think more about how I’m feeling and the lack of progress I’m making, and the hopelessness I’m feeling. That kind of dragged things on, and I guess deepened my depression.”
Freddy: “Often times when I go to my office in the evening, that is when I would [ sic ] be prone to be more depressed. It’s being alone. I think about myself or mistakes or trying to correct mistakes or whatever’s going on in my life at the time. I become very introspective. I think I’m way too self-evaluating, way too self-deprecating and it’s when I’m alone when those things are really, really triggered. When I’m talking with somebody else, I forget about those things.”
In sum, students with depression highlighted that a lab environment full of positive and encouraging individuals was helpful for their depression, whereas isolating or competitive environments and negative interactions with others often resulted in more depressive feelings.
Doing Science: Experiencing Failure in Research, Getting Help, Receiving Feedback, Time Demands, and Important Contributions.
In addition to the lab environment, students also described that the process of doing science could affect their depression. Specifically, students explained that a large contributor to their depression was experiencing failure in research.
Interviewer: “Considering your experience in undergraduate research, what tends to trigger your feelings of depression?”
Heather: “Probably just not getting things right. Having to do an experiment over and over again. You don’t get the results you want. (…) The work is pretty meticulous and it’s frustrating when I do all this work, I do a whole experiment, and then I don’t get any results that I can use. That can be really frustrating. It adds to the stress. (…) It’s hard because you did all this other stuff before so you can plan for the research, and then something happens and all the stuff you did was worthless basically.”
Julie: “I felt very negatively about myself [when a project failed] and pretty panicked whenever something didn’t work because I felt like it was a direct reflection on my effort and/or intelligence, and then it was a big glaring personal failure.”
Students explained that their depression related to failing in research was exacerbated if they felt as though they could not seek help from their research mentors. Perceived insufficient mentor guidance has been shown to be a factor influencing student intention to leave undergraduate research ( Cooper et al. , 2019c ). Sometimes students talked about their research mentors being unavailable or unapproachable.
Michelle: “It just feels like [the graduate students] are not approachable. I feel like I can’t approach them to ask for their understanding in a certain situation. It makes [my depression] worse because I feel like I’m stuck, and that I’m being limited, and like there’s nothing I can do. So then I kind of feel like it’s my fault that I can’t do anything.”
Other times, students described that they did not seek help in fear that they would be negatively evaluated in research, which is a fear of being judged by others ( Watson and Friend, 1969 ; Weeks et al. , 2005 ; Cooper et al. , 2018 ). That is, students fear that their mentor would think negatively about them or judge them if they were to ask questions that their mentor thought they should know the answer to.
Meleana: “I would say [my depression] tends to come out more in being more reserved in asking questions because I think that comes more like a fear-based thing where I’m like, ‘Oh, I don’t feel like I’m good enough and so I don’t want to ask these questions because then my mentors will, I don’t know, think that I’m dumb or something.’”
Conversely, students described that mentors who were willing to help them alleviated their depressive feelings.
Crystal: “Yeah [my grad student] is always like, ‘Hey, I can check in on things in the lab because you’re allowed to ask me for that, you’re not totally alone in this,’ because he knows that I tend to take on all this responsibility and I don’t always know how to ask for help. He’s like, ‘You know, this is my lab too and I am here to help you as well,’ and just reminds me that I’m not shouldering this burden by myself.”
Ashlyn: “The graduate student who I work with is very kind and has a lot of patience and he really understands a lot of things and provides simple explanations. He does remind me about things and he will keep on me about certain tasks that I need to do in an understanding way, and it’s just because he’s patient and he listens.”
In addition to experiencing failure in science, students described that making mistakes when doing science also negatively affected their depression.
Abby: “I guess not making mistakes on experiments [is important in avoiding my depression]. Not necessarily that your experiment didn’t turn out to produce the data that you wanted, but just adding the wrong enzyme or messing something up like that. It’s like, ‘Oh, man,’ you know? You can get really down on yourself about that because it can be embarrassing.”
Commonly, students described that the potential for making mistakes increased their stress and anxiety regarding research; however, they explained that how other people responded to a potential mistake was what ultimately affected their depression.
Briana: “Sometimes if I made a mistake in correctly identifying an eye color [of a fly], [my PI] would just ridicule me in front of the other students. He corrected me but his method of correcting was very discouraging because it was a ridicule. It made the others laugh and I didn’t like that.”
Julie: “[My PI] explicitly [asked] if I had the dedication for science. A lot of times he said I had terrible judgment. A lot of times he said I couldn’t be trusted. Once I went to a conference with him, and, unfortunately, in front of another professor, he called me a klutz several times and there was another comment about how I never learn from my mistakes.”
When students did do things correctly, they described how important it could be for them to receive praise from their mentors. They explained that hearing praise and validation can be particularly helpful for students with depression, because their thoughts are often very negative and/or because they have low self-esteem.
Crystal: “[Something that helps my depression is] I have text messages from [my graduate student mentor] thanking me [and another undergraduate researcher] for all of the work that we’ve put in, that he would not be able to be as on track to finish as he is if he didn’t have our help.”
Interviewer: “Why is hearing praise from your mentor helpful?”
Crystal: “Because a lot of my depression focuses on everybody secretly hates you, nobody likes you, you’re going to die alone. So having that validation [from my graduate mentor] is important, because it flies in the face of what my depression tells me.”
Brian: “It reminds you that you exist outside of this negative world that you’ve created for yourself, and people don’t see you how you see yourself sometimes.”
Students also highlighted how research could be overwhelming, which negatively affected their depression. Particularly, students described that research demanded a lot of their time and that their mentors did not always seem to be aware that they were juggling school and other commitments in addition to their research. This stress exacerbated their depression.
Rose: “I feel like sometimes [my grad mentors] are not very understanding because grad students don’t take as many classes as [undergrads] do. I think sometimes they don’t understand when I say I can’t come in at all this week because I have finals and they’re like, ‘Why though?’”
Abby: “I just think being more understanding of student life would be great. We have classes as well as the lab, and classes are the priority. They forget what it’s like to be a student. You feel like they don’t understand and they could never understand when you say like, ‘I have three exams this week,’ and they’re like, ‘I don’t care. You need to finish this.’”
Conversely, some students reported that their research labs were very understanding of students’ schedules. Interestingly, these students talked most about how helpful it was to be able to take a mental health day and not do research on days when they felt down or depressed.
Marta: “My lab tech is very open, so she’ll tell us, ‘I can’t come in today. I have to take a mental health day.’ So she’s a really big advocate for that. And I think I won’t personally tell her that I’m taking a mental health day, but I’ll say, ‘I can’t come in today, but I’ll come in Friday and do those extra hours.’ And she’s like, ‘OK great, I’ll see you then.’ And it makes me feel good, because it helps me take care of myself first and then I can take care of everything else I need to do, which is amazing.”
Meleana: “Knowing that [my mentors] would be flexible if I told them that I’m crazy busy and can’t come into work nearly as much this week [helps my depression]. There is flexibility in allowing me to then care for myself.”
Interviewer: “Why is the flexibility helpful given the depression?”
Meleana: “Because sometimes for me things just take a little bit longer when I’m feeling down. I’m just less efficient to be honest, and so it’s helpful if I feel like I can only go into work for 10 hours in a week. It declutters my brain a little bit to not have to worry about all the things I have to do in work in addition the things that I need to do for school or clubs, or family or whatever.”
Despite the demanding nature of research, a subset of students highlighted that their research and research lab provided a sense of stability or familiarity that distracted them from their depression.
Freddy: “I’ll [do research] to run away from those [depressive] feelings or whatever. (…) I find sadly, I hate to admit it, but I do kind of run to [my lab]. I throw myself into work to distract myself from the feelings of depression and sadness.”
Rose: “When you’re sad or when you’re stressed you want to go to things you’re familiar with. So because lab has always been in my life, it’s this thing where it’s going to be there for me I guess. It’s like a good book that you always go back to and it’s familiar and it makes you feel good. So that’s how lab is. It’s not like the greatest thing in the world but it’s something that I’m used to, which is what I feel like a lot of people need when they’re sad and life is not going well.”
Many students also explained that research positively affects their depression because they perceive their research contribution to be important.
Ashlyn: “I feel like I’m dedicating myself to something that’s worthy and something that I believe in. It’s really important because it contextualizes those times when I am feeling depressed. It’s like, no, I do have these better things that I’m working on. Even when I don’t like myself and I don’t like who I am, which is again, depression brain, I can at least say, ‘Well, I have all these other people relying on me in research and in this area and that’s super important.’”
Jessica: “I mean, it just felt like the work that I was doing had meaning and when I feel like what I’m doing is actually going to contribute to the world, that usually really helps with [depression] because it’s like not every day you can feel like you’re doing something impactful.”
In sum, students highlighted that experiencing failure in research and making mistakes negatively contributed to depression, especially when help was unavailable or research mentors had a negative reaction. Additionally, students acknowledged that the research could be time-consuming, but that research mentors who were flexible helped assuage depressive feelings that were associated with feeling overwhelmed. Finally, research helped some students’ depression, because it felt familiar, provided a distraction from depression, and reminded students that they were contributing to a greater cause.
We believe that creating more inclusive research environments for students with depression is an important step toward broadening participation in science, not only to ensure that we are not discouraging students with depression from persisting in science, but also because depression has been shown to disproportionately affect underserved and underrepresented groups in science ( Turner and Noh, 1988 ; Eisenberg et al. , 2007 ; Jenkins et al. , 2013 ; American College Health Association, 2018 ). We initially hypothesized that three features of undergraduate research—research mentors, the lab environment, and failure—may have the potential to exacerbate student depression. We found this to be true; students highlighted that their relationships with their mentors as well as the overall lab environment could negatively affect their depression, but could also positively affect their research experiences. Students also noted that they struggled with failure, which is likely true of most students, but is known to be particularly difficult for students with depression ( Elliott et al. , 1997 ). We expand upon our findings by integrating literature on depression with the information that students provided in the interviews about how research mentors can best support students. We provide a set of evidence-based recommendations focused on mentoring, the lab environment, and failure for research mentors wanting to create more inclusive research environments for students with depression. Notably, only the first recommendation is specific to students with depression; the others reflect recommendations that have previously been described as “best practices” for research mentors ( NASEM, 2017 , 2019 ; Sorkness et al. , 2017 ) and likely would benefit most students. However, we examine how these recommendations may be particularly important for students with depression. As we hypothesized, these recommendations directly address three aspects of research: mentors, lab environment, and failure. A caveat of these recommendations is that more research needs to be done to explore the experiences of students with depression and how these practices actually impact students with depression, but our national sample of undergraduate researchers with depression can provide an initial starting point for a discussion about how to improve research experiences for these students.
Recommendations to Make Undergraduate Research Experiences More Inclusive for Students with Depression
Recognize student depression as a valid illness..
Allow students with depression to take time off of research by simply saying that they are sick and provide appropriate time for students to recover from depressive episodes. Also, make an effort to destigmatize mental health issues.
Undergraduate researchers described both psychological and physical symptoms that manifested as a result of their depression and highlighted how such symptoms prevented them from performing to their full potential in undergraduate research. For example, students described how their depression would cause them to feel unmotivated, which would often negatively affect their research productivity. In cases in which students were motivated enough to come in and do their research, they described having difficulty concentrating or engaging in the work. Further, when doing research, students felt less creative and less willing to take risks, which may alter the quality of their work. Students also sometimes struggled to socialize in the lab. They described feeling less social and feeling overly self-critical. In sum, students described that, when they experienced a depressive episode, they were not able to perform to the best of their ability, and it sometimes took a toll on them to try to act like nothing was wrong, when they were internally struggling with depression. We recommend that research mentors treat depression like any other physical illness; allowing students the chance to recover when they are experiencing a depressive episode can be extremely important to students and can allow them to maximize their productivity upon returning to research ( Judd et al. , 2000 ). Students explained that if they are not able to take the time to focus on recovering during a depressive episode, then they typically continue to struggle with depression, which negatively affects their research. This sentiment is echoed by researchers in psychiatry who have found that patients who do not fully recover from a depressive episode are more likely to relapse and to experience chronic depression ( Judd et al. , 2000 ). Students described not doing tasks or not showing up to research because of their depression but struggling with how to share that information with their research mentors. Often, students would not say anything, which caused them anxiety because they were worried about what others in the lab would say to them when they returned. Admittedly, many students understood why this behavior would cause their research mentors to be angry or frustrated, but they weighed the consequences of their research mentors’ displeasure against the consequences of revealing their depression and decided it was not worth admitting to being depressed. This aligns with literature that suggests that when individuals have concealable stigmatized identities, or identities that can be hidden and that carry negative stereotypes, such as depression, they will often keep them concealed to avoid negative judgment or criticism ( Link and Phelan, 2001 ; Quinn and Earnshaw, 2011 ; Jones and King, 2014 ; Cooper and Brownell, 2016 ; Cooper et al. , 2019b ; Cooper et al ., unpublished data ). Therefore, it is important for research mentors to be explicit with students that 1) they recognize mental illness as a valid sickness and 2) that students with mental illness can simply explain that they are sick if they need to take time off. This may be useful to overtly state on a research website or in a research syllabus, contract, or agreement if mentors use such documents when mentoring undergraduates in their lab. Further, research mentors can purposefully work to destigmatize mental health issues by explicitly stating that struggling with mental health issues, such as depression and anxiety, is common. While we do not recommend that mentors ask students directly about depression, because this can force students to share when they are not comfortable sharing, we do recommend providing opportunities for students to reveal their depression ( Chaudoir and Fisher, 2010 ). Mentors can regularly check in with students about how they’re doing, and talk openly about the importance of mental health, which may increase the chance that students may feel comfortable revealing their depression ( Chaudoir and Quinn, 2010 ; Cooper et al ., unpublished data ).
Foster a Positive Lab Environment.
Encourage positivity in the research lab, promote working in shared spaces to enhance social support among lab members, and alleviate competition among undergraduates.
Students in this study highlighted that the “leadership” of the lab, meaning graduate students, postdocs, lab managers, and PIs, were often responsible for establishing the tone of the lab; that is, if they were in a bad mood it would trickle down and negatively affect the moods of the undergraduates. Explicitly reminding lab leadership that their moods can both positively and negatively affect undergraduates may be important in establishing a positive lab environment. Further, students highlighted how they were most likely to experience negative thoughts when they were alone in the lab. Therefore, it may be helpful to encourage all lab members to work in a shared space to enhance social interactions among students and to maximize the likelihood that undergraduates have access to help when needed. A review of 51 studies in psychiatry supported our undergraduate researchers’ perceptions that social relationships positively impacted their depression; the study found that perceived emotional support (e.g., someone available to listen or give advice), perceived instrumental support (e.g., someone available to help with tasks), and large diverse social networks (e.g., being socially connected to a large number of people) were significantly protective against depression ( Santini et al. , 2015 ). Additionally, despite forming positive relationships with other undergraduates in the lab, many undergraduate researchers admitted to constantly comparing themselves with other undergraduates, which led them to feel inferior, negatively affecting their depression. Some students talked about mentors favoring current undergraduates or talking positively about past undergraduates, which further exacerbated their feelings of inferiority. A recent study of students in undergraduate research experiences highlighted that inequitable distribution of praise to undergraduates can create negative perceptions of lab environments for students (Cooper et al. , 2019). Further, the psychology literature has demonstrated that when people feel insecure in their social environments, it can cause them to focus on a hierarchical view of themselves and others, which can foster feelings of inferiority and increase their vulnerability to depression ( Gilbert et al. , 2009 ). Thus, we recommend that mentors be conscious of their behaviors so that they do not unintentionally promote competition among undergraduates or express favoritism toward current or past undergraduates. Praise is likely best used without comparison with others and not done in a public way, although more research on the impact of praise on undergraduate researchers needs to be done. While significant research has been done on mentoring and mentoring relationships in the context of undergraduate research ( Byars-Winston et al. , 2015 ; Aikens et al. , 2017 ; Estrada et al. , 2018 ; Limeri et al. , 2019 ; NASEM, 2019 ), much less has been done on the influence of the lab environment broadly and how people in nonmentoring roles can influence one another. Yet, this study indicates the potential influence of many different members of the lab, not only their mentors, on students with depression.
Develop More Personal Relationships with Undergraduate Researchers and Provide Sufficient Guidance.
Make an effort to establish more personal relationships with undergraduates and ensure that they perceive that they have access to sufficient help and guidance with regard to their research.
When we asked students explicitly how research mentors could help create more inclusive environments for undergraduate researchers with depression, students overwhelmingly said that building mentor–student relationships would be extremely helpful. Students suggested that mentors could get to know students on a more personal level by asking about their career interests or interests outside of academia. Students also remarked that establishing a more personal relationship could help build the trust needed in order for undergraduates to confide in their research mentors about their depression, which they perceived would strengthen their relationships further because they could be honest about when they were not feeling well or their mentors might even “check in” with them in times where they were acting differently than normal. This aligns with studies showing that undergraduates are most likely to reveal a stigmatized identity, such as depression, when they form a close relationship with someone ( Chaudoir and Quinn, 2010 ). Many were intimidated to ask for research-related help from their mentors and expressed that they wished they had established a better relationship so that they would feel more comfortable. Therefore, we recommend that research mentors try to establish relationships with their undergraduates and explicitly invite them to ask questions or seek help when needed. These recommendations are supported by national recommendations for mentoring ( NASEM, 2019 ) and by literature that demonstrates that both social support (listening and talking with students) and instrumental support (providing students with help) have been shown to be protective against depression ( Santini et al. , 2015 ).
Treat Undergraduates with Respect and Remember to Praise Them.
Avoid providing harsh criticism and remember to praise undergraduates. Students with depression often have low self-esteem and are especially self-critical. Therefore, praise can help calibrate their overly negative self-perceptions.
Students in this study described that receiving criticism from others, especially harsh criticism, was particularly difficult for them given their depression. Multiple studies have demonstrated that people with depression can have an abnormal or maladaptive response to negative feedback; scientists hypothesize that perceived failure on a particular task can trigger failure-related thoughts that interfere with subsequent performance ( Eshel and Roiser, 2010 ). Thus, it is important for research mentors to remember to make sure to avoid unnecessarily harsh criticisms that make students feel like they have failed (more about failure is described in the next recommendation). Further, students with depression often have low self-esteem or low “personal judgment of the worthiness that is expressed in the attitudes the individual holds towards oneself” ( Heatherton et al. , 2003 , p. 220; Sowislo and Orth, 2013 ). Specifically, a meta-analysis of longitudinal studies found that low self-esteem is predictive of depression ( Sowislo and Orth, 2013 ), and depression has also been shown to be highly related to self-criticism ( Luyten et al. , 2007 ). Indeed, nearly all of the students in our study described thinking that they are “not good enough,” “worthless,” or “inadequate,” which is consistent with literature showing that people with depression are self-critical ( Blatt et al. , 1982 ; Gilbert et al. , 2006 ) and can be less optimistic of their performance on future tasks and rate their overall performance on tasks less favorably than their peers without depression ( Cane and Gotlib, 1985 ). When we asked students what aspects of undergraduate research helped their depression, students described that praise from their mentors was especially impactful, because they thought so poorly of themselves and they needed to hear something positive from someone else in order to believe it could be true. Praise has been highlighted as an important aspect of mentoring in research for many years ( Ashford, 1996 ; Gelso and Lent, 2000 ; Brown et al. , 2009 ) and may be particularly important for students with depression. In fact, praise has been shown to enhance individuals’ motivation and subsequent productivity ( Hancock, 2002 ; Henderlong and Lepper, 2002 ), factors highlighted by students as negatively affecting their depression. However, something to keep in mind is that a student with depression and a student without depression may process praise differently. For a student with depression, a small comment that praises the student’s work may not be sufficient for the student to process that comment as praise. People with depression are hyposensitive to reward or have reward-processing deficits ( Eshel and Roiser, 2010 ); therefore, praise may affect students without depression more positively than it would affect students with depression. Research mentors should be mindful that students with depression often have a negative view of themselves, and while students report that praise is extremely important, they may have trouble processing such positive feedback.
Normalize Failure and Be Explicit about the Importance of Research Contributions.
Explicitly remind students that experiencing failure is expected in research. Also explain to students how their individual work relates to the overall project so that they can understand how their contributions are important. It can also be helpful to explain to students why the research project as a whole is important in the context of the greater scientific community.
Experiencing failure has been thought to be a potentially important aspect of undergraduate research, because it may provide students with the potential to develop integral scientific skills such as the ability to navigate challenges and persevere ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, in the interviews, students described that when their science experiments failed, it was particularly tough for their depression. Students’ negative reaction to experiencing failure in research is unsurprising, given recent literature that has predicted that students may be inadequately prepared to approach failure in science ( Henry et al. , 2019 ). However, the literature suggests that students with depression may find experiencing failure in research to be especially difficult ( Elliott et al. , 1997 ; Mongrain and Blackburn, 2005 ; Jones et al. , 2009 ). One potential hypothesis is that students with depression may be more likely to have fixed mindsets or more likely to believe that their intelligence and capacity for specific abilities are unchangeable traits ( Schleider and Weisz, 2018 ); students with a fixed mindset have been hypothesized to have particularly negative responses to experiencing failure in research, because they are prone to quitting easily in the face of challenges and becoming defensive when criticized ( Forsythe and Johnson, 2017 ; Dweck, 2008 ). A study of life sciences undergraduates enrolled in CUREs identified three strategies of students who adopted adaptive coping mechanisms, or mechanisms that help an individual maintain well-being and/or move beyond the stressor when faced with failure in undergraduate research: 1) problem solving or engaging in strategic planning and decision making, 2) support seeking or finding comfort and help with research, and 3) cognitive restructuring or reframing a problem from negative to positive and engaging in self encouragement ( Gin et al. , 2018 ). We recommend that, when undergraduates experience failure in science, their mentors be proactive in helping them problem solve, providing help and support, and encouraging them. Students also explained that mentors sharing their own struggles as undergraduate and graduate students was helpful, because it normalized failure. Sharing personal failures in research has been recommended as an important way to provide students with psychosocial support during research ( NASEM, 2019 ). We also suggest that research mentors take time to explain to students why their tasks in the lab, no matter how small, contribute to the greater research project ( Cooper et al. , 2019a ). Additionally, it is important to make sure that students can explain how the research project as a whole is contributing to the scientific community ( Gin et al. , 2018 ). Students highlighted that contributing to something important was really helpful for their depression, which is unsurprising, given that studies have shown that meaning in life or people’s comprehension of their life experiences along with a sense of overarching purpose one is working toward has been shown to be inversely related to depression ( Steger, 2013 ).
Limitations and Future Directions
This work was a qualitative interview study intended to document a previously unstudied phenomenon: depression in the context of undergraduate research experiences. We chose to conduct semistructured interviews rather than a survey because of the need for initial exploration of this area, given the paucity of prior research. A strength of this study is the sampling approach. We recruited a national sample of 35 undergraduates engaged in undergraduate research at 12 different public R1 institutions. Despite our representative sample from R1 institutions, these findings may not be generalizable to students at other types of institutions; lab environments, mentoring structures, and interactions between faculty and undergraduate researchers may be different at other institution types (e.g., private R1 institutions, R2 institutions, master’s-granting institutions, primarily undergraduate institutions, and community colleges), so we caution against making generalizations about this work to all undergraduate research experiences. Future work could assess whether students with depression at other types of institutions have similar experiences to students at research-intensive institutions. Additionally, we intentionally did not explore the experiences of students with specific identities owing to our sample size and the small number of students in any particular group (e.g., students of a particular race, students with a graduate mentor as the primary mentor). We intend to conduct future quantitative studies to further explore how students’ identities and aspects of their research affect their experiences with depression in undergraduate research.
The students who participated in the study volunteered to be interviewed about their depression; therefore, it is possible that depression is a more salient part of these students’ identities and/or that they are more comfortable talking about their depression than the average population of students with depression. It is also important to acknowledge the personal nature of the topic and that some students may not have fully shared their experiences ( Krumpal, 2013 ), particularly those experiences that may be emotional or traumatizing ( Kahn and Garrison, 2009 ). Additionally, our sample was skewed toward females (77%). While females do make up approximately 60% of students in biology programs on average ( Eddy et al. , 2014 ), they are also more likely to report experiencing depression ( American College Health Association, 2018 ; Evans et al. , 2018 ). However, this could be because women have higher rates of depression or because males are less likely to report having depression; clinical bias, or practitioners’ subconscious tendencies to overlook male distress, may underestimate depression rates in men ( Smith et al. , 2018 ). Further, females are also more likely to volunteer to participate in studies ( Porter and Whitcomb, 2005 ); therefore, many interview studies have disproportionately more females in the data set (e.g., Cooper et al. , 2017 ). If we had been able to interview more male students, we might have identified different findings. Additionally, we limited our sample to life sciences students engaged in undergraduate research at public R1 institutions. It is possible that students in other majors may have different challenges and opportunities for students with depression, as well as different disciplinary stigmas associated with mental health.
In this exploratory interview study, we identified a variety of ways in which depression in undergraduates negatively affected their undergraduate research experiences. Specifically, we found that depression interfered with students’ motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing. We also identified that research can negatively affect depression in undergraduates. Experiencing failure in research can exacerbate student depression, especially when students do not have access to adequate guidance. Additionally, being alone or having negative interactions with others in the lab worsened students’ depression. However, we also found that undergraduate research can positively affect students’ depression. Research can provide a familiar space where students can feel as though they are contributing to something meaningful. Additionally, students reported that having access to adequate guidance and a social support network within the research lab also positively affected their depression. We hope that this work can spark conversations about how to make undergraduate research experiences more inclusive of students with depression and that it can stimulate additional research that more broadly explores the experiences of undergraduate researchers with depression.
Important note
If you or a student experience symptoms of depression and want help, there are resources available to you. Many campuses provide counseling centers equipped to provide students, staff, and faculty with treatment for depression, as well as university-dedicated crisis hotlines. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (Text “CONNECT” to 741741; Text Depression Hotline , 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can also learn more about depression and where to find help near you through the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Biopolar Support Alliance: http://dbsalliance.org ( Depression and Biopolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are extremely grateful to the undergraduate researchers who shared their thoughts and experiences about depression with us. We acknowledge the ASU LEAP Scholars for helping us create the original survey and Rachel Scott for her helpful feedback on earlier drafts of this article. L.E.G. was supported by a National Science Foundation (NSF) Graduate Fellowship (DGE-1311230) and K.M.C. was partially supported by a Howard Hughes Medical Institute (HHMI) Inclusive Excellence grant (no. 11046) and an NSF grant (no. 1644236). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or HHMI.
- Aikens, M. L., Robertson, M. M., Sadselia, S., Watkins, K., Evans, M., Runyon, C. R. , … & Dolan, E. L. ( 2017 ). Race and gender differences in undergraduate research mentoring structures and research outcomes . CBE—Life Sciences Education , 16 (2), ar34. Link , Google Scholar
- Aikens, M. L., Sadselia, S., Watkins, K., Evans, M., Eby, L. T., & Dolan, E. L. ( 2016 ). A social capital perspective on the mentoring of undergraduate life science researchers: An empirical study of undergraduate–postgraduate–faculty triads . CBE—Life Sciences Education , 15 (2), ar16. Link , Google Scholar
- Aldwin, C., & Greenberger, E. ( 1987 ). Cultural differences in the predictors of depression . American Journal of Community Psychology , 15 (6), 789–813. Medline , Google Scholar
- American Association for the Advancement of Science . ( 2011 ). Vision and change in undergraduate biology education: A call to action . Retrieved November 29, 2019, from http://visionandchange.org/files/2013/11/aaas-VISchange-web1113.pdf Google Scholar
- American College Health Association . ( 2018 ). Undergraduate reference group executive summary, Fall 2018 . Retrieved November 29, 2019, from www.acha.org/documents/ncha/NCHA-II_Fall_2018_Reference_Group_Executive_Summary.pdf Google Scholar
- American College Health Association . ( 2019 ). Retrieved November 29, 2019, from NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- Aneshensel, C. S., & Stone, J. D. ( 1982 ). Stress and depression: A test of the buffering model of social support . Archives of General Psychiatry , 39 (12), 1392–1396. Medline , Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Home page . Retrieved November 29, 2019, from https://adaa.org Google Scholar
- Armbruster, P., Patel, M., Johnson, E., & Weiss, M. ( 2009 ). Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology . CBE—Life Sciences Education , 8 (3), 203–213. Link , Google Scholar
- Ashford, S. J. ( 1996 ). Working with doctoral students: Rhythms of Academic Life: Personal Accounts of Careers in Academia . In Front, P. J.Taylor, M. S. (Eds.), Rhythms of Academic Life: Personal Accounts of Careers in Academia (pp. 153–158). Thousand Oaks, CA: Sage. Google Scholar
- Auchincloss, L. C., Laursen, S. L., Branchaw, J. L., Eagan, K., Graham, M., Hanauer, D. I. , … & Rowland, S. ( 2014 ). Assessment of course-based undergraduate research experiences: A meeting report . CBE—Life Sciences Education , 13 (1), 29–40. Link , Google Scholar
- Barak, M. E. M., Levin, A., Nissly, J. A., & Lane, C. J. ( 2006 ). Why do they leave? Modeling child welfare workers’ turnover intentions . Children and Youth Services Review , 28 (5), 548–577. Google Scholar
- Bauer, K. W., & Bennett, J. S. ( 2003 ). Alumni perceptions used to assess undergraduate research experience . Journal of Higher Education , 74 (2), 210–230. Google Scholar
- Birks, M., & Mills, J. ( 2015 ). Grounded theory: A practical guide . Thousand Oaks, CA: Sage. Google Scholar
- Blatt, S. J., Quinlan, D. M., Chevron, E. S., McDonald, C., & Zuroff, D. ( 1982 ). Dependency and self-criticism: Psychological dimensions of depression . Journal of Consulting and Clinical Psychology , 50 (1), 113. Medline , Google Scholar
- Brown, R. T., Daly, B. P., & Leong, F. T. ( 2009 ). Mentoring in research: A developmental approach . Professional Psychology: Research and Practice , 40 (3), 306. Google Scholar
- Brownell, S. E., Hekmat-Scafe, D. S., Singla, V., Seawell, P. C., Imam, J. F. C., Eddy, S. L. , … & Cyert, M. S. ( 2015 ). A high-enrollment course-based undergraduate research experience improves student conceptions of scientific thinking and ability to interpret data . CBE—Life Sciences Education , 14 (2), ar21. Link , Google Scholar
- Brownell, S. E., & Kloser, M. J. ( 2015 ). Toward a conceptual framework for measuring the effectiveness of course-based undergraduate research experiences in undergraduate biology . Studies in Higher Education , 40 (3), 525–544. Google Scholar
- Byars-Winston, A. M., Branchaw, J., Pfund, C., Leverett, P., & Newton, J. ( 2015 ). Culturally diverse undergraduate researchers’ academic outcomes and perceptions of their research mentoring relationships . International Journal of Science Education , 37 (15), 2533–2554. Medline , Google Scholar
- Cane, D. B., & Gotlib, I. H. ( 1985 ). Depression and the effects of positive and negative feedback on expectations, evaluations, and performance . Cognitive Therapy and Research , 9 (2), 145–160. Google Scholar
- Ceci, S. J., & Williams, W. M. ( 2010 ). Sex differences in math-intensive fields . Current Directions in Psychological Science , 19 (5), 275–279. Medline , Google Scholar
- Center for Collegiate Mental Health . ( 2017 ). Center for Collegiate Mental Health 2017 Annual Report . State College, PA: Penn State Universit. Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chaudoir, S. R., & Fisher, J. D. ( 2010 ). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity . Psychological Bulletin , 136 (2), 236. Medline , Google Scholar
- Chaudoir, S. R., & Quinn, D. M. ( 2010 ). Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being . Journal of Social Issues , 66 (3), 570–584. Medline , Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cooper, K. M., Ashley, M., & Brownell, S. E. ( 2017 ). A bridge to active learning: A summer bridge program helps students maximize their active-learning experiences and the active-learning experiences of others . CBE—Life Sciences Education , 16 (1), ar17. Link , Google Scholar
- Cooper, K. M., Blattman, J. N., Hendrix, T., & Brownell, S. E. ( 2019a ). The impact of broadly relevant novel discoveries on student project ownership in a traditional lab course turned CURE . CBE—Life Sciences Education , 18 (4), ar57. Link , Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. https://doi.org/10.1187/cbe.16-01-0074 Link , Google Scholar
- Cooper, K. M., Brownell, S. E., & Gormally, C. C. ( 2019b ). Coming out to the class: Identifying factors that influence college biology instructor decisions about whether to reveal their LGBQ identity in class . Journal of Women and Minorities in Science and Engineering , 25 (3). Google Scholar
- Cooper, K. M., Downing, V. R., & Brownell, S. E. ( 2018 ). The influence of active learning practices on student anxiety in large-enrollment college science classrooms . International Journal of STEM Education , 5 (1), 23. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B. , … & Brownell, S. E. ( 2019c ). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 (8). https://doi.org/10.1371/journal.pone.0220186 Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2019d ). Diagnosing differences in what introductory biology students in a fully online and an in-person biology degree program know and do regarding medical school admission . Advances in Physiology Education , 43 (2), 221–232. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( In press ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , ( in press ). Google Scholar
- Depression and Biopolar Support Alliance . ( 2019 ). Home page . Retrieved November 28, 2019, from www.dbsalliance.org Google Scholar
- Deroma, V. M., Leach, J. B., & Leverett, J. P. ( 2009 ). The relationship between depression and college academic performance . College Student Journal , 43 (2), 325–335. Google Scholar
- Dweck, C. S. ( 2008 ). Mindset: The new psychology of success . New York, NY: Random House Digital. Google Scholar
- Dyson, R., & Renk, K. ( 2006 ). Freshmen adaptation to university life: Depressive symptoms, stress, and coping . Journal of Clinical Psychology , 62 (10), 1231–1244. Medline , Google Scholar
- Eddy, S. L., Brownell, S. E., & Wenderoth, M. P. ( 2014 ). Gender gaps in achievement and participation in multiple introductory biology classrooms . CBE—Life Sciences Education , 13 (3), 478–492. https://doi.org/10.1187/cbe.13-10-0204 Link , Google Scholar
- Eisenberg, D., Gollust, S. E., Golberstein, E., & Hefner, J. L. ( 2007 ). Prevalence and correlates of depression, anxiety, and suicidality among university students . American Journal of Orthopsychiatry , 77 (4), 534–542. Medline , Google Scholar
- Elliott, R., Sahakian, B. J., Herrod, J. J., Robbins, T. W., & Paykel, E. S. ( 1997 ). Abnormal response to negative feedback in unipolar depression: Evidence for a diagnosis specific impairment . Journal of Neurology, Neurosurgery & Psychiatry , 63 (1), 74–82. Medline , Google Scholar
- Eshel, N., & Roiser, J. P. ( 2010 ). Reward and punishment processing in depression . Biological Psychiatry , 68 (2), 118–124. Medline , Google Scholar
- Estrada, M., Hernandez, P. R., & Schultz, P. W. ( 2018 ). A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers . CBE—Life Sciences Education , 17 (1), ar9. Link , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Everson, H. T., Tobias, S., Hartman, H., & Gourgey, A. ( 1993 ). Test anxiety and the curriculum: The subject matters . Anxiety, Stress, and Coping , 6 (1), 1–8. Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Retrieved November 29, 2019, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Forsythe, A., & Johnson, S. ( 2017 ). Thanks, but no-thanks for the feedback . Assessment & Evaluation in Higher Education , 42 (6), 850–859. Google Scholar
- Garlow, S. J., Rosenberg, J., Moore, J. D., Haas, A. P., Koestner, B., Hendin, H., & Nemeroff, C. B. ( 2008 ). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University . Depression and Anxiety , 25 (6), 482–488. Medline , Google Scholar
- Gelso, C. J., & Lent, R. W. ( 2000 ). Scientific training and scholarly productivity: The person, the training environment, and their interaction . In Brown, S. D.Lent, R. W. (Eds.), Handbook of counseling psychology (pp. 109–139). Hoboken, NJ: John Wiley & Sons Inc. Google Scholar
- Gilbert, P., Baldwin, M. W., Irons, C., Baccus, J. R., & Palmer, M. ( 2006 ). Self-criticism and self-warmth: An imagery study exploring their relation to depression . Journal of Cognitive Psychotherapy , 20 (2), 183. Google Scholar
- Gilbert, P., McEwan, K., Bellew, R., Mills, A., & Gale, C. ( 2009 ). The dark side of competition: How competitive behaviour and striving to avoid inferiority are linked to depression, anxiety, stress and self-harm . Psychology and Psychotherapy: Theory, Research and Practice , 82 (2), 123–136. Medline , Google Scholar
- Gin, L. E., Rowland, A. A., Steinwand, B., Bruno, J., & Corwin, L. A. ( 2018 ). Students who fail to achieve predefined research goals may still experience many positive outcomes as a result of CURE participation . CBE—Life Sciences Education , 17 (4), ar57. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, England, UK: Longman. Google Scholar
- Grav, S., Hellzèn, O., Romild, U., & Stordal, E. ( 2012 ). Association between social support and depression in the general population: The HUNT study, a cross-sectional survey . Journal of Clinical Nursing , 21 (1–2), 111–120. Medline , Google Scholar
- Guest, G., Bunce, A., & Johnson, L. ( 2006 ). How many interviews are enough? An experiment with data saturation and variability . Field Methods , 18 (1), 59–82. Google Scholar
- Hancock, D. R. ( 2002 ). Influencing graduate students’ classroom achievement, homework habits and motivation to learn with verbal praise . Educational Research , 44 (1), 83–95. Google Scholar
- Hannah, D. R., & Lautsch, B. A. ( 2011 ). Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it . Journal of Management Inquiry , 20 (1), 14–22. Google Scholar
- Heatherton, T. F., & Wyland, C. L. ( 2003 ). Assessing self-esteem . In Lopez, S. J.Snyder, C. R. (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 219–233). Washington, DC: American Psychological Association. https://doi.org/10.1037/10612-014 . Google Scholar
- Henderlong, J., & Lepper, M. R. ( 2002 ). The effects of praise on children’s intrinsic motivation: A review and synthesis . Psychological Bulletin , 128 (5), 774. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hernandez, P. R., Woodcock, A., Estrada, M., & Schultz, P. W. ( 2018 ). Undergraduate research experiences broaden diversity in the scientific workforce . BioScience , 68 (3), 204–211. Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Hysenbegasi, A., Hass, S. L., & Rowland, C. R. ( 2005 ). The impact of depression on the academic productivity of university students . Journal of Mental Health Policy and Economics , 8 (3), 145. Medline , Google Scholar
- Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. ( 2013 ). A systematic review of studies of depression prevalence in university students . Journal of Psychiatric Research , 47 (3), 391–400. Medline , Google Scholar
- Intemann, K. ( 2009 ). Why diversity matters: Understanding and applying the diversity component of the National Science Foundation’s broader impacts criterion . Social Epistemology , 23 (3–4), 249–266. Google Scholar
- Ishiyama, J. ( 2002 ). Does early participation in undergraduate research benefit social science and humanities students? College Student Journal , 36 (3), 381–387. Google Scholar
- Jenkins, S. R., Belanger, A., Connally, M. L., Boals, A., & Durón, K. M. ( 2013 ). First-generation undergraduate students’ social support, depression, and life satisfaction . Journal of College Counseling , 16 (2), 129–142. Google Scholar
- Jobst, A., Sabass, L., Palagyi, A., Bauriedl-Schmidt, C., Mauer, M. C., Sarubin, N. , … & Zill, P. ( 2015 ). Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression . Journal of Psychiatric Research , 60 , 170–177. Medline , Google Scholar
- Jones, K. P., & King, E. B. ( 2014 ). Managing concealable stigmas at work: A review and multilevel model . Journal of Management , 40 (5), 1466–1494. Google Scholar
- Jones, M. T., Barlow, A. E., & Villarejo, M. ( 2010 ). Importance of undergraduate research for minority persistence and achievement in biology . Journal of Higher Education , 81 (1), 82–115. Google Scholar
- Jones, N. P., Papadakis, A. A., Hogan, C. M., & Strauman, T. J. ( 2009 ). Over and over again: Rumination, reflection, and promotion goal failure and their interactive effects on depressive symptoms . Behaviour Research and Therapy , 47 (3), 254–259. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , … & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kahn, J. H., & Garrison, A. M. ( 2009 ). Emotional self-disclosure and emotional avoidance: Relations with symptoms of depression and anxiety . Journal of Counseling Psychology , 56 (4), 573. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kreger, D. W. ( 1995 ). Self-esteem, stress, and depression among graduate students . Psychological Reports , 76 (1), 345–346. Medline , Google Scholar
- Krumpal, I. ( 2013 ). Determinants of social desirability bias in sensitive surveys: A literature review . Quality & Quantity , 47 (4), 2025–2047. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 33 (2), 363–374. Medline , Google Scholar
- Laursen, S., Hunter, A.-B., Seymour, E., Thiry, H., & Melton, G. ( 2010 ). Undergraduate research in the sciences: Engaging students in real science . Hoboken, NJ: Wiley. Google Scholar
- Limeri, L. B., Asif, M. Z., Bridges, B. H., Esparza, D., Tuma, T. T., Sanders, D. , … & Maltese, A. V. ( 2019 ). “Where’s my mentor?” Characterizing negative mentoring experiences in undergraduate life science research . CBE—Life Sciences Education , 18 (4), ar61. Link , Google Scholar
- Link, B. G., & Phelan, J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 27 (1), 363–385. Google Scholar
- Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C. , … & Corveleyn, J. ( 2007 ). Dependency and self-criticism: Relationship with major depressive disorder, severity of depression, and clinical presentation . Depression and Anxiety , 24 (8), 586–596. Medline , Google Scholar
- Mabrouk, P. A., & Peters, K. ( 2000 ). Student perspectives on undergraduate research (UR) experiences in chemistry and biology . CUR Quarterly , 21 (1), 25–33. Google Scholar
- Maxwell, J. A. ( 2010 ). Using numbers in qualitative research . Qualitative Inquiry , 16 (6), 475–482. Google Scholar
- Mongrain, M., & Blackburn, S. ( 2005 ). Cognitive vulnerability, lifetime risk, and the recurrence of major depression in graduate students . Cognitive Therapy and Research , 29 (6), 747–768. Google Scholar
- Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Burnout and mental health problems in biomedical doctoral students . CBE—Life Sciences Education , 18 (2), ar27. Link , Google Scholar
- National Academies of Sciences, Engineering, and Medicine (NASEM) . ( 2017 ). Undergraduate research experiences for STEM students: Successes, challenges, and opportunities . Washington, DC: National Academies Press. https://doi.org/10.17226/24622 Google Scholar
- NASEM . ( 2019 ). The science of effective mentorship in STEMM . Washington, DC: National Academies Press. Retrieved November 29, 2019, from www.nap.edu/download/25568 Google Scholar
- Osborne, J., & Collins, S. ( 2001 ). Pupils’ views of the role and value of the science curriculum: A focus-group study . International Journal of Science Education , 23 (5), 441–467. https://doi.org/10.1080/09500690010006518 Google Scholar
- Porter, S. R., & Whitcomb, M. E. ( 2005 ). Non-response in student surveys: The role of demographics, engagement and personality . Research in Higher Education , 46 (2), 127–152. Google Scholar
- President’s Council of Advisors on Science and Technology . ( 2012 ). Engage to excel: Producing one million additional college graduates with degrees in science, Technology, Engineering, and mathematics . Washington, DC: U.S. Government Office of Science and Technology. Google Scholar
- Prunuske, A. J., Wilson, J., Walls, M., & Clarke, B. ( 2013 ). Experiences of mentors training underrepresented undergraduates in the research laboratory . CBE—Life Sciences Education , 12 (3), 403–409. Link , Google Scholar
- Quinn, D. M., & Earnshaw, V. A. ( 2011 ). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes . Social Issues and Policy Review , 5 (1), 160–190. Google Scholar
- Rauckhorst, W. H., Czaja, J. A., & Baxter Magolda, M. ( 2001 ). Measuring the impact of the undergraduate research experience on student intellectual development . Snowbird, UT: Project Kaleidoscope Summer Institute. Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schleider, J., & Weisz, J. ( 2018 ). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial . Journal of Child Psychology and Psychiatry , 59 (2), 160–170. Medline , Google Scholar
- Seymour, E., & Hewitt, N. M. ( 1997 ). Talking about leaving: Why undergraduates leave the sciences . Westview Press. Google Scholar
- Seymour, E., & Hunter, A.-B. ( 2019 ). Talking about leaving revisited . New York, NY: Springer. Google Scholar
- Seymour, E., Hunter, A.-B., Laursen, S. L., & DeAntoni, T. ( 2004 ). Establishing the benefits of research experiences for undergraduates in the sciences: First findings from a three-year study . Science Education , 88 (4), 493–534. Google Scholar
- Smith, D. T., Mouzon, D. M., & Elliott, M. ( 2018 ). Reviewing the assumptions about men’s mental health: An exploration of the gender binary . American Journal of Men’s Health , 12 (1), 78–89. Medline , Google Scholar
- Sorkness, C. A., Pfund, C., Ofili, E. O., Okuyemi, K. S., Vishwanatha, J. K., Zavala, M. E. , … & Deveci, A. ( 2017 ). A new approach to mentoring for research careers: The National Research Mentoring Network . BMC Proceedings , 11 , 22. Medline , Google Scholar
- Sowislo, J. F., & Orth, U. ( 2013 ). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies . Psychological Bulletin , 139 (1), 213. Medline , Google Scholar
- Steger, M. F. ( 2013 ). Experiencing meaning in life: Optimal functioning at the nexus of well-being, psychopathology, and spirituality . In Wong, P. T. P. (Ed.), The human quest for meaning (pp. 211–230). England, UK: Routledge. Google Scholar
- Strenta, A. C., Elliott, R., Adair, R., Matier, M., & Scott, J. ( 1994 ). Choosing and leaving science in highly selective institutions . Research in Higher Education , 35 (5), 513–547. Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved November 29, 2019, from www.crisistextline.org/depression Google Scholar
- Thiry, H., & Laursen, S. L. ( 2011 ). The role of student–advisor interactions in apprenticing undergraduate researchers into a scientific community of practice . Journal of Science Education and Technology , 20 (6), 771–784. Google Scholar
- Thompson, J. J., Conaway, E., & Dolan, E. L. ( 2016 ). Undergraduate students’ development of social, cultural, and human capital in a networked research experience . Cultural Studies of Science Education , 11 (4), 959–990. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . 118th American Society for Engineering Education Annual Conference and Exposition, Vancouver, BC, Canada . Google Scholar
- Turner, R. J., & Noh, S. ( 1988 ). Physical disability and depression: A longitudinal analysis . Journal of Health and Social Behavior , 29 (1), 23–37. Medline , Google Scholar
- Watson, D., & Friend, R. ( 1969 ). Measurement of social-evaluative anxiety . Journal of Consulting and Clinical Psychology , 33 (4), 448. Medline , Google Scholar
- Weeks, J. W., Heimberg, R. G., Fresco, D. M., Hart, T. A., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. ( 2005 ). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder . Psychological Assessment , 17 (2), 179. Medline , Google Scholar
- World Health Organization . ( 2018 ). Depression . Retrieved November 29, 2019, from www.who.int/news-room/fact-sheets/detail/depression Google Scholar
- Wyatt, T., & Oswalt, S. B. ( 2013 ). Comparing mental health issues among undergraduate and graduate students . American Journal of Health Education , 44 (2), 96–107. Google Scholar
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Colin Harrison, Monitoring Editor
- Emma C. Goodwin ,
- Danielle Pais ,
- Logan E. Gin , and
- Derek Braun, Monitoring Editor
- Baylee A. Edwards ,
- Chloe Bowen ,
- M. Elizabeth Barnes , and
- Tati Russo-Tait, Monitoring Editor
- Sara E. Grineski ,
- Danielle X. Morales , and
- Timothy W. Collins
- Carly A. Busch , and
- Tasneem F. Mohammed ,
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Coping behavior versus coping style: characterizing a measure of coping in undergraduate STEM contexts 14 February 2022 | International Journal of STEM Education, Vol. 9, No. 1
- Lisa A. Corwin ,
- Michael E. Ramsey ,
- Eric A. Vance ,
- Elizabeth Woolner ,
- Stevie Maiden ,
- Nina Gustafson and
- Joseph A. Harsh
- Erin Shortlidge, Monitoring Editor
- K. Supriya ,
- Brian Sato, Monitoring Editor
- Logan E. Gin ,
- Clark Coffman, Monitoring Editor
- Nicholas J. Wiesenthal , and
- Maryrose Weatherton and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Eight Recommendations to Promote Effective Study Habits for Biology Students Enrolled in Online Courses Journal of Microbiology & Biology Education, Vol. 23, No. 1
- Fostering professional development through undergraduate research: supporting faculty mentors and student researchers 30 March 2022 | Mentoring & Tutoring: Partnership in Learning, Vol. 30, No. 2
- Jeffrey Maloy ,
- Monika B. Kwapisz , and
- Bryce E. Hughes
- Terrell Morton, Monitoring Editor
- Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic 14 December 2021 | Journal of American College Health, Vol. 9
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor
- Dominant Learning Styles of Interior Design Students in Generation Z 26 July 2021 | Journal of Interior Design, Vol. 46, No. 4
- Linking Emotional Intelligence, Physical Activity and Aggression among Undergraduates 26 November 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 23
- Advancing undergraduate synthetic biology education: insights from a Canadian iGEM student perspective Canadian Journal of Microbiology, Vol. 67, No. 10
- Frank A. Guerrero ,
- Sara E. Brownell , and
- Jennifer Momsen, Monitoring Editor
- Nicholas J. Wiesenthal ,
- Isabella Ferreira , and
- Grant Ean Gardner, Monitoring Editor
- Carolyn E. Clark ,
- Deanna B. Elliott ,
- Travis B. Roderick ,
- Rachel A. Scott ,
- Denisse Arellano ,
- Diana Ramirez ,
- Kimberly Velarde ,
- Allyson Aeschliman ,
- Sarah T. Avalle ,
- Jessica Berkheimer ,
- Rachel Campos ,
- Michael Gerbasi ,
- Sophia Hughes ,
- Julie A. Roberts ,
- Quinn M. White ,
- Ehren Wittekind ,
- Rachelle Spell, Monitoring Editor
- Christine Pfund ,
- Janet L. Branchaw ,
- Melissa McDaniels ,
- Angela Byars-Winston ,
- Steven P. Lee ,, and
- Bruce Birren
- Vladimir Anokhin ,
- MacKenzie J. Gray ,
- Daniel E. Zajic ,
- Jason E. Podrabsky , and
- Erin E. Shortlidge
- Depression as a concealable stigmatized identity: what influences whether students conceal or reveal their depression in undergraduate research experiences? 4 June 2020 | International Journal of STEM Education, Vol. 7, No. 1
Submitted: 4 November 2019 Revised: 24 February 2020 Accepted: 6 March 2020
© 2020 K. M. Cooper, L. E. Gin, et al. CBE—Life Sciences Education © 2020 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).

- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story

Analysis: Depression is probably not caused by a chemical imbalance in the brain – new study
20 July 2022
Writing in The Conversation, Professor Joanna Moncrieff and Dr Mark Horowitz (both UCL Psychiatry) report on their new research showing no clear evidence that serotonin levels or serotonin activity are responsible for depression.

For three decades, people have been deluged with information suggesting that depression is caused by a “chemical imbalance” in the brain – namely an imbalance of a brain chemical called serotonin. However, our latest research review shows that the evidence does not support it.
Although first proposed in the 1960s, the serotonin theory of depression started to be widely promoted by the pharmaceutical industry in the 1990s in association with its efforts to market a new range of antidepressants, known as selective serotonin-reuptake inhibitors or SSRIs. The idea was also endorsed by official institutions such as the American Psychiatric Association, which still tells the public that “differences in certain chemicals in the brain may contribute to symptoms of depression”.
Countless doctors have repeated the message all over the world, in their private surgeries and in the media. People accepted what they were told. And many started taking antidepressants because they believed they had something wrong with their brain that required an antidepressant to put right. In the period of this marketing push, antidepressant use climbed dramatically, and they are now prescribed to one in six of the adult population in England, for example.
For a long time, certain academics, including some leading psychiatrists, have suggested that there is no satisfactory evidence to support the idea that depression is a result of abnormally low or inactive serotonin. Others continue to endorse the theory. Until now, however, there has been no comprehensive review of the research on serotonin and depression that could enable firm conclusions either way.
At first sight, the fact that SSRI-type antidepressants act on the serotonin system appears to support the serotonin theory of depression. SSRIs temporarily increase the availability of serotonin in the brain, but this does not necessarily imply that depression is caused by the opposite of this effect.
There are other explanations for antidepressants’ effects. In fact, drug trials show that antidepressants are barely distinguishable from a placebo (dummy pill) when it comes to treating depression. Also, antidepressants appear to have a generalised emotion-numbing effect which may influence people’s moods, although we do not know how this effect is produced or much about it.
There has been extensive research on the serotonin system since the 1990s, but it has not been collected systematically before. We conducted an “umbrella” review that involved systematically identifying and collating existing overviews of the evidence from each of the main areas of research into serotonin and depression. Although there have been systematic reviews of individual areas in the past, none have combined the evidence from all the different areas taking this approach.
One area of research we included was research comparing levels of serotonin and its breakdown products in the blood or brain fluid. Overall, this research did not show a difference between people with depression and those without depression.
Another area of research has focused on serotonin receptors, which are proteins on the ends of the nerves that serotonin links up with and which can transmit or inhibit serotonin’s effects. Research on the most commonly investigated serotonin receptor suggested either no difference between people with depression and people without depression, or that serotonin activity was actually increased in people with depression – the opposite of the serotonin theory’s prediction.
Research on the serotonin “transporter”, that is the protein which helps to terminate the effect of serotonin (this is the protein that SSRIs act on), also suggested that, if anything, there was increased serotonin activity in people with depression. However, these findings may be explained by the fact that many participants in these studies had used or were currently using antidepressants.
We also looked at research that explored whether depression can be induced in volunteers by artificially lowering levels of serotonin. Two systematic reviews from 2006 and 2007 and a sample of the ten most recent studies (at the time the current research was conducted) found that lowering serotonin did not produce depression in hundreds of healthy volunteers. One of the reviews showed very weak evidence of an effect in a small subgroup of people with a family history of depression, but this only involved 75 participants.
Very large studies involving tens of thousands of patients looked at gene variation, including the gene that has the instructions for making the serotonin transporter. They found no difference in the frequency of varieties of this gene between people with depression and healthy controls.
Although a famous early study found a relationship between the serotonin transporter gene and stressful life events, larger, more comprehensive studies suggest no such relationship exists. Stressful life events in themselves, however, exerted a strong effect on people’s subsequent risk of developing depression.
Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin.
The serotonin theory of depression has been one of the most influential and extensively researched biological theories of the origins of depression. Our study shows that this view is not supported by scientific evidence. It also calls into question the basis for the use of antidepressants.
Most antidepressants now in use are presumed to act via their effects on serotonin. Some also affect the brain chemical noradrenaline. But experts agree that the evidence for the involvement of noradrenaline in depression is weaker than that for serotonin.
There is no other accepted pharmacological mechanism for how antidepressants might affect depression. If antidepressants exert their effects as placebos, or by numbing emotions, then it is not clear that they do more good than harm.
Although viewing depression as a biological disorder may seem like it would reduce stigma, in fact, research has shown the opposite, and also that people who believe their own depression is due to a chemical imbalance are more pessimistic about their chances of recovery.
It is important that people know that the idea that depression results from a “chemical imbalance” is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe. People need all this information to make informed decisions about whether or not to take antidepressants.
This article originally appeared in The Conversation on 20 July 2022.
- Article in The Conversation
- Article in The Conversation (Spanish)
- Professor Joanna Moncrieff's academic profile
- Dr Mark Horowitz's academic profile
- UCL Division of Psychiatry
- UCL Faculty of Brain Sciences
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Mental health and the pandemic: What U.S. surveys have found
The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world . In the U.S, the COVID-19 outbreak in early 2020 caused widespread lockdowns and disruptions in daily life while triggering a short but severe economic recession that resulted in widespread unemployment. Three years later, Americans have largely returned to normal activities, but challenges with mental health remain.
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic. These findings reflect a snapshot in time, and it’s possible that attitudes and experiences may have changed since these surveys were fielded. It’s also important to note that concerns about mental health were common in the U.S. long before the arrival of COVID-19 .
Three years into the COVID-19 outbreak in the United States , Pew Research Center published this collection of survey findings about Americans’ challenges with mental health during the pandemic. All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
The research behind the first item in this analysis, examining Americans’ experiences with psychological distress, benefited from the advice and counsel of the COVID-19 and mental health measurement group at Johns Hopkins Bloomberg School of Public Health.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022.
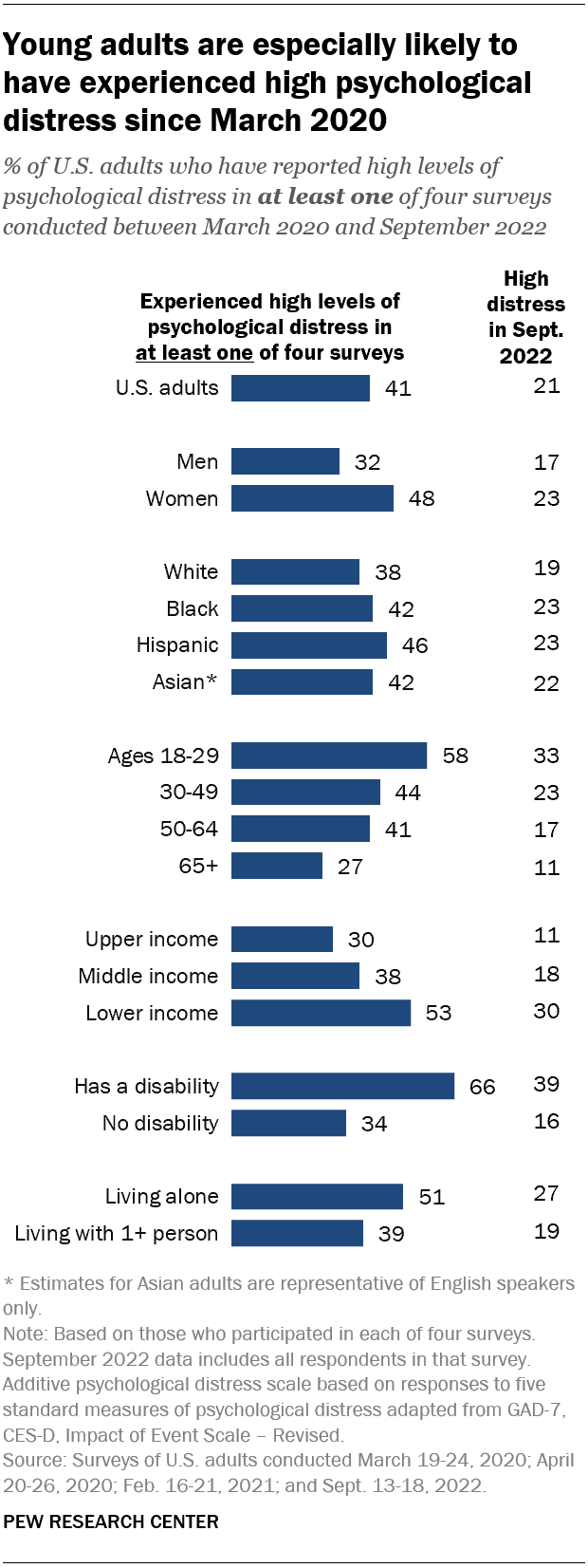
Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this category, based on their answers in at least one of these four surveys.
Women are much more likely than men to have experienced high psychological distress (48% vs. 32%), as are people in lower-income households (53%) when compared with those in middle-income (38%) or upper-income (30%) households.
In addition, roughly two-thirds (66%) of adults who have a disability or health condition that prevents them from participating fully in work, school, housework or other activities have experienced a high level of distress during the pandemic.
The Center measured Americans’ psychological distress by asking them a series of five questions on subjects including loneliness, anxiety and trouble sleeping in the past week. The questions are not a clinical measure, nor a diagnostic tool. Instead, they describe people’s emotional experiences during the week before being surveyed.
While these questions did not ask specifically about the pandemic, a sixth question did, inquiring whether respondents had “had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart” when thinking about their experience with the coronavirus outbreak. In September 2022, the most recent time this question was asked, 14% of Americans said they’d experienced this at least some or a little of the time in the past seven days.
More than a third of high school students have reported mental health challenges during the pandemic. In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%).
In the same survey, an even larger share of high school students (44%) said that at some point during the previous 12 months, they had felt sad or hopeless almost every day for two or more weeks in a row – to the point where they had stopped doing some usual activities. Roughly six-in-ten high school girls (57%) said this, as did 31% of boys.
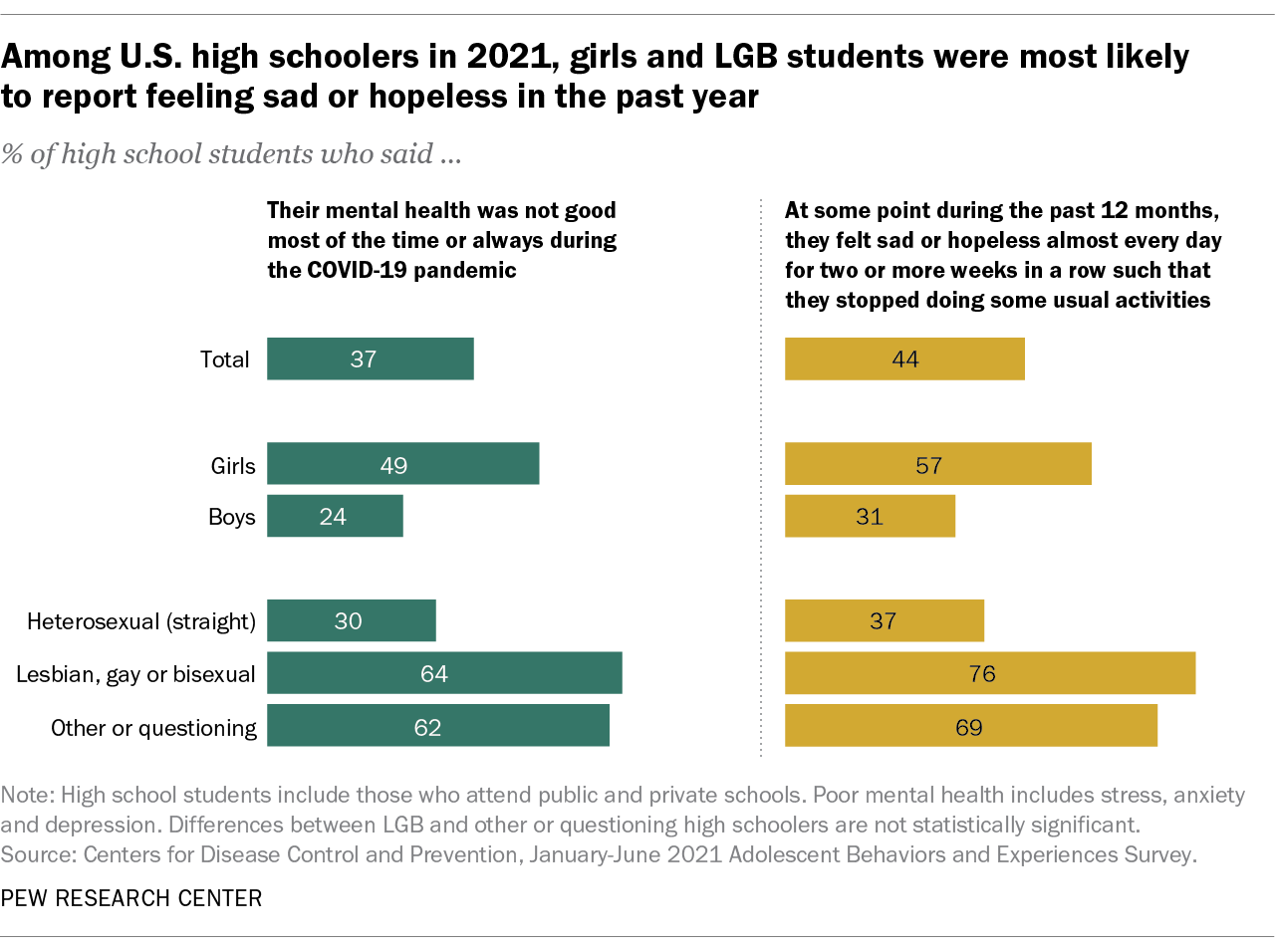
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health.
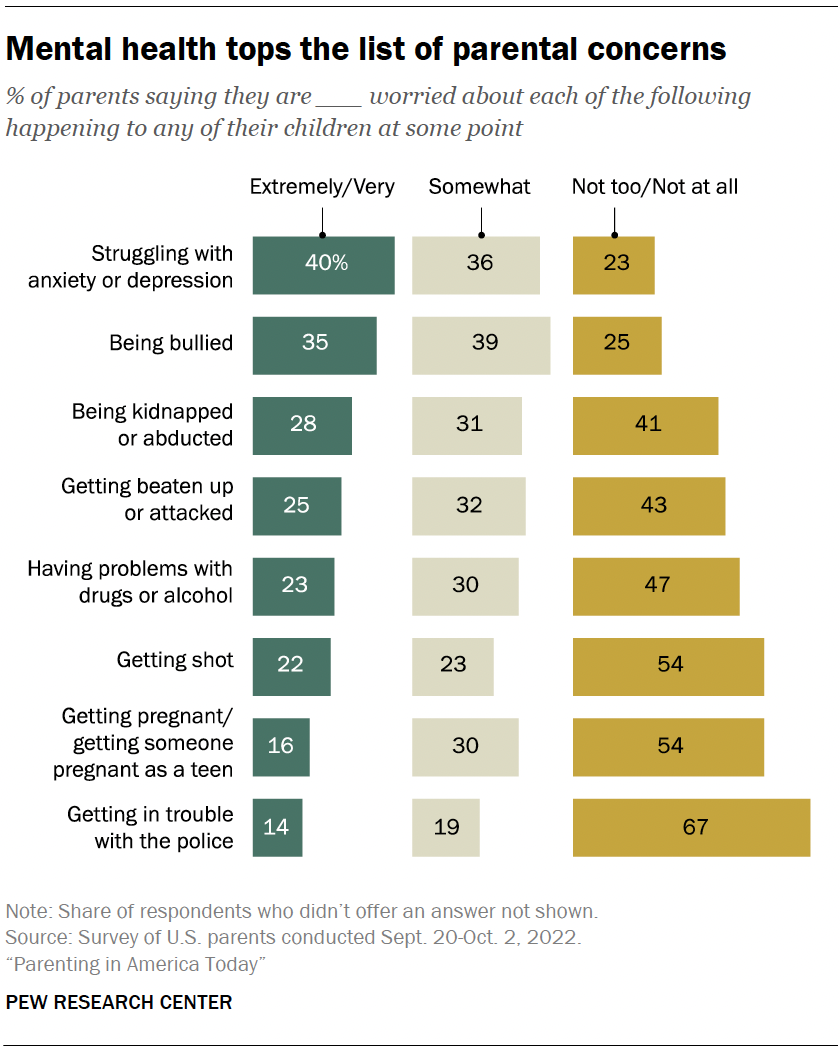
Mental health tops the list of worries that U.S. parents express about their kids’ well-being, according to a fall 2022 Pew Research Center survey of parents with children younger than 18. In that survey, four-in-ten U.S. parents said they’re extremely or very worried about their children struggling with anxiety or depression. That was greater than the share of parents who expressed high levels of concern over seven other dangers asked about.
While the fall 2022 survey was fielded amid the coronavirus outbreak, it did not ask about parental worries in the specific context of the pandemic. It’s also important to note that parental concerns about their kids struggling with anxiety and depression were common long before the pandemic, too . (Due to changes in question wording, the results from the fall 2022 survey of parents are not directly comparable with those from an earlier Center survey of parents, conducted in 2015.)
Among parents of teenagers, roughly three-in-ten (28%) are extremely or very worried that their teen’s use of social media could lead to problems with anxiety or depression, according to a spring 2022 survey of parents with children ages 13 to 17 . Parents of teen girls were more likely than parents of teen boys to be extremely or very worried on this front (32% vs. 24%). And Hispanic parents (37%) were more likely than those who are Black or White (26% each) to express a great deal of concern about this. (There were not enough Asian American parents in the sample to analyze separately. This survey also did not ask about parental concerns specifically in the context of the pandemic.)
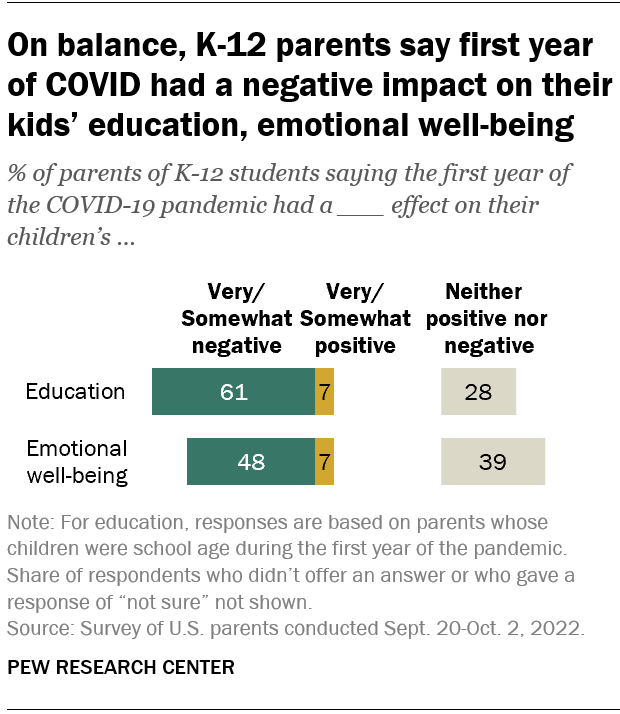
Looking back, many K-12 parents say the first year of the coronavirus pandemic had a negative effect on their children’s emotional health. In a fall 2022 survey of parents with K-12 children , 48% said the first year of the pandemic had a very or somewhat negative impact on their children’s emotional well-being, while 39% said it had neither a positive nor negative effect. A small share of parents (7%) said the first year of the pandemic had a very or somewhat positive effect in this regard.
White parents and those from upper-income households were especially likely to say the first year of the pandemic had a negative emotional impact on their K-12 children.
While around half of K-12 parents said the first year of the pandemic had a negative emotional impact on their kids, a larger share (61%) said it had a negative effect on their children’s education.
- Coronavirus (COVID-19)
- Happiness & Life Satisfaction
- Medicine & Health
- Teens & Youth

How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, economy remains the public’s top policy priority; covid-19 concerns decline again, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
Clinical Research Studies
SPECIALIZING IN NOVEL AND INNOVATIVE RESEARCH APPROACHES FOR ALL TYPES OF CLINICAL DEPRESSION
Currently Enrolling Studies


Efficacy, Safety, and Tolerability of COMP360 in Participants With Treatment Resistant Depression
Exploring potential new routes away from treatment-resistant depression, introducing the comp 005 clinical study.
Many people who receive antidepressant treatment for their depression do not get an adequate response to the medicines they are taking. If someone is taking two or more antidepressants and they are failing, this is sometimes referred to as treatment-resistant depression or TRD.
The COMP 005 study is looking into a new treatment approach for people with TRD using an investigational medicine given with psychological support. The study is suitable for people who have been diagnosed with major depression and are currently experiencing a recurrent or single episode of depression but that have not responded to antidepressant treatment.
You may be eligible to participate in a Compass Pathfinder study if you:
- Are 18 years of age or older
- Have been diagnosed with major depression (single or recurrent episodes)
- Are experiencing treatment-resistant depression, defined as failing 2, 3 or 4 pharmacological treatments for your current episode of depression
- Meet additional study criteria.
About the study
The study, which will last up to 16 weeks, will compare the effectiveness of the active investigational medicine with a placebo, a substance that has no therapeutic effect, given with psychological support. Two-thirds of the people in the study will receive the active investigational medicine and one third will receive placebo. If you join the study, neither you nor your study doctors will know which study treatment you are going to receive because the decision is made randomly by a computer and not revealed to anyone.
Participants will receive support from study clinicians to help them taper off any prohibited medications, including current antidepressants. Participants will be asked to remain off prohibited medications for the duration of the study.
Reimbursement for reasonable, out-of-pocket expenses for travel and other expenses may be available to qualified individuals
To find out if this study is a good fit for you, please fill out our online survey , call (650) 723-8330, or email [email protected] .
For further details, please see the following link: https://clinicaltrials.gov/study/NCT05624268
RELIANCE-II: A Study to Assess the Efficacy and Safety of REL-1017 as Adjunctive Treatment for Major Depressive Disorder (MDD)
This is an outpatient, 2-arm, Phase 3, multicenter, randomized, double-blind, placebo-controlled study to assess the efficacy and safety of REL-1017 once daily (QD) as an adjunctive treatment of Major Depressive Disorder.
Eligible participants will either receive the study drug, REL-1017, or placebo. Esmethadone (also known as dextromethadone) is the active ingredient in REL-1017 tablets. This study drug selectively works on nerve cells that seem to play a role in depression. A placebo is an inactive tablet that looks identical to the study drug (tablet) but does not contain the active study drug. Researchers use a placebo to see if the study drug works better or is safer than taking nothing. The main goals of this study are to learn how safe the study drug is and how well the study drug works when taken with the antidepressants you are currently taking for MDD.
For further details, please see the following link: https://clinicaltrials.gov/ct2/show/NCT04855747
Opiate Suicide Study in Patients with Major Depression
We are doing this study to determine if suicidal thoughts are lessened after an infusion of ketamine followed by 4 weeks of a medication called buprenorphine. Participants for this research will be currently experiencing depression and will have not responded to treatment with antidepressants or have an intolerance to these types of medicines. Recent studies have shown a single infusion of ketamine to reduce suicidal ideation within 24 hours and to last for at least one week. We would like to determine if a single infusion of ketamine followed by 4 weeks of low dose burprenorphine produces longer lasting anti-suicidal effects than does ketamine followed by placebo.
This research study is expected to take approximately 2 years to complete with at least 6 weeks of active participation by each participant. During this time, participants will make 10 study visits to Stanford University, including an 8-hour infusion visit.
Under the close supervision and monitoring by the study clinicians, eligible subjects will receive a single infusion of ketamine 0.5mg/kg followed by oral buprenorphine or placebo for 4 weeks.
This research study will use either Buprenorphine or a placebo, containing no drug, to study if the benefits experienced from Ketamine can be improved or last longer when buprenorphine is taken for 4 weeks.
To find out if this study is a good fit for you, please fill out our online survey , call (650) 723-8330, or email [email protected] .
For further details, please see the following link: https://clinicaltrials.gov/ct2/show/NCT04116528
Tianeptine for Treatment Resistant Depression
Although not available in the United States, Tianeptine is an atypical antidepressant that has been used clinically in Europe, Asia, and South America since the late 1980s in millions of patients. Until recently tianeptine's molecular mechanism of action had remained unknown. Tianeptine is a different type of antidepressant than those currently approved in the United States in that it has a different mechanism of action than other antidepressants. Eligible participants will receive 8-weeks of treatment with Tianeptine. The major goals of this project are (1) to determine if tianeptine is an effective antidepressant in patients who have failed two previous trials, (2) to define the relationship between opioid signaling deficits and response to tianeptine treatment, and (3) to develop a comprehensive assessment battery capable of identifying endogenous opioid signaling deficits to explore biological heterogeneity in the TRD population. For further details, please see the following link: https://clinicaltrials.gov/ct2/show/NCT04249596
THERAPEUTIC GROUP FOR WOMEN TRAUMA SURVIVORS
We are conducting a research study on the Building Empowerment and Resilience (BEAR) Therapeutic Group for adult women who have experienced interpersonal trauma. We are recruiting women who would like to participate in the therapeutic group, as well as women who prefer not to participate in the group but are willing to complete a series of questionnaires.
The BEAR Therapeutic group includes psychoeducation, psychological skills, and physical empowerment (self-defense) training. The group will run for 12-weeks, for 1.5 hours once per week. The psychological skills portion of the class will cover topics such as assertiveness, communication skills, and boundary setting. In addition, we will cover basic self-defense techniques one can use to protect themselves if the need arises. This project is focusing on women who have been victims of interpersonal violence (e.g., physical, emotional, or sexual abuse/assault). To be eligible:
- Women ages 18-70 years old
- History of physical, sexual, or emotional violence with subsequent interpersonal or emotional difficulties related to this history
- participate in the BEAR therapy group OR
- to completed a series of questionnaires and not participate in the therapy group
The study is at Stanford University Medical Center during the day. The 12- week program will be provided at no charge or payment to the participants. The study consists of 14 visits: one screening visit, twelve classes, and one debriefing visit. In addition, on-line questionnaires will be completed periodically throughout the study.
For more information, contact us at (650) 724-7184 or email [email protected] .
To fill out a screening for this study, visit https://redcap.link/BEARscreening
All calls/contacts are confidential.
Enrolling Soon
Other clinical trial opportunities for depression at stanford medicine.
Current studies in the Brain Stimulation Lab (BSL) Dr. Williams, Assistant Professor of Psychiatry and Behavioral Sciences (General Psychiatry and Psychology) at the Stanford University Medical Center and Director of the Stanford Brain Stimulation Lab

The Brain Stimulation Lab (BSL) utilizes novel brain stimulation techniques to probe and modulate the neural networks underlying neuropsychiatric diseases/disorders in an effort to develop new models and novel treatments.
Learn more here
Current studies in the Heifets Lab Dr. Boris Heifets, Assistant Professor of Anesthesiology, Perioperative and Pain Medicine (Adult MSD) at the Stanford University Medical Center

Our research group is dedicated to understanding and improving on powerful, rapid-acting therapies for psychiatric disease, such as ketamine, MDMA and psilocybin. We bridge basic science and clinical trials, connecting neuroscience, psychiatry and anesthesiology in pursuit of highly effective, safe treatment strategies scalable to the millions of patients who need them.
This paper is in the following e-collection/theme issue:
Published on 22.4.2024 in Vol 10 (2024)
Digital Dietary Behaviors in Individuals With Depression: Real-World Behavioral Observation
Authors of this article:

Original Paper
- Yue Zhu 1, 2 , PhD ;
- Ran Zhang 1, 2 , PhD ;
- Shuluo Yin 3 , MS ;
- Yihui Sun 3, 4 , MS ;
- Fay Womer 5 , MD ;
- Rongxun Liu 6 , MS ;
- Sheng Zeng 3, 4 , MS ;
- Xizhe Zhang 1, 3 * , PhD ;
- Fei Wang 1, 2 * , MD
1 Early Intervention Unit, Department of Psychiatry, The Affiliated Brain Hospital of Nanjing Medical University, Nanjing, China
2 Functional Brain Imaging Institute of Nanjing Medical University, Nanjing, China
3 School of Biomedical Engineering and Informatics, Nanjing Medical University, Nanjing, China
4 School of Computer Science and Engineering, Northeastern University, Shenyang, China
5 Department of Psychiatry and Behavioral Sciences, Vanderbilt University Medical Center, Nashville, TN, United States
6 Henan Key Laboratory of Immunology and Targeted Drug, Henan Collaborative Innovation Center of Molecular Diagnosis and Laboratory Medicine, School of Laboratory Medicine, Xinxiang Medical University, Xinxiang, China
*these authors contributed equally
Corresponding Author:
Xizhe Zhang, PhD
Early Intervention Unit
Department of Psychiatry
The Affiliated Brain Hospital of Nanjing Medical University
264 Guangzhou Road, Gulou District, Nanjing City, China
Nanjing, 210000
Phone: 1 86 02583295953
Fax:1 86 02583295953
Email: [email protected]
Background: Depression is often accompanied by changes in behavior, including dietary behaviors. The relationship between dietary behaviors and depression has been widely studied, yet previous research has relied on self-reported data which is subject to recall bias. Electronic device–based behavioral monitoring offers the potential for objective, real-time data collection of a large amount of continuous, long-term behavior data in naturalistic settings.
Objective: The study aims to characterize digital dietary behaviors in depression, and to determine whether these behaviors could be used to detect depression.
Methods: A total of 3310 students (2222 healthy controls [HCs], 916 with mild depression, and 172 with moderate-severe depression) were recruited for the study of their dietary behaviors via electronic records over a 1-month period, and depression severity was assessed in the middle of the month. The differences in dietary behaviors across the HCs, mild depression, and moderate-severe depression were determined by ANCOVA (analyses of covariance) with age, gender, BMI, and educational level as covariates. Multivariate logistic regression analyses were used to examine the association between dietary behaviors and depression severity. Support vector machine analysis was used to determine whether changes in dietary behaviors could detect mild and moderate-severe depression.
Results: The study found that individuals with moderate-severe depression had more irregular eating patterns, more fluctuated feeding times, spent more money on dinner, less diverse food choices, as well as eating breakfast less frequently, and preferred to eat only lunch and dinner, compared with HCs. Moderate-severe depression was found to be negatively associated with the daily 3 regular meals pattern (breakfast-lunch-dinner pattern; OR 0.467, 95% CI 0.239-0.912), and mild depression was positively associated with daily lunch and dinner pattern (OR 1.460, 95% CI 1.016-2.100). These changes in digital dietary behaviors were able to detect mild and moderate-severe depression (accuracy=0.53, precision=0.60), with better accuracy for detecting moderate-severe depression (accuracy=0.67, precision=0.64).
Conclusions: This is the first study to develop a profile of changes in digital dietary behaviors in individuals with depression using real-world behavioral monitoring. The results suggest that digital markers may be a promising approach for detecting depression.
Introduction
The mental health of students has become the forefront of concerns, particularly since the onset of the COVID-19 pandemic. Approximately 45% of college students in China reported experiencing mental health issues during the outbreak [ 1 ]. Depression screening typically involves self-reported data, but there is a lack of objective markers to promptly identify individuals experiencing depression. Early identification and intervention are crucial for mitigating the impact of depression during critical periods for the academic and occupational functioning of students [ 2 ].
Appetite disturbance or changes in dietary behaviors are common symptoms of depression and may serve as objective indicators of the condition in a large population [ 3 ]. Dietary behavior can exert an influence on mental health through a variety of pathways, including circadian rhythms, oxidative stress, and the gut microbiota [ 4 ]. Based on the time of meals, intervals between meals, daily eating window, and food intake of the day, dietary behavior patterns can be categorized into morningness, intermediate, and eveningness chronotypes [ 5 ]. Eveningness chronotype commonly exhibits a higher tendency to skip breakfast, eat dinner later, and allocate a greater proportion of their daily food intake to later hours of the day [ 6 ]. Prior research has additionally demonstrated that the eveningness chronotype, coupled with social jetlag, constitutes a risk factor for depression [ 7 , 8 ]. Besides, individuals with more pronounced fluctuations in their eating windows often display heightened emotional vulnerability [ 9 ]. However, previous studies of diet relied on retrospective questionnaires or interviews, which may fail to accurately reflect real-world behavior [ 10 ]. Additionally, these methods typically assess only 1 aspect of dietary behavior, such as diet quality or eating habits [ 8 , 11 , 12 ]. To fully understand dietary behaviors, it is necessary to use multiple scales to assess multiple dimensions, such as diet quality, emotional eating, and chronotype of eating habits. However, using multiple scales can lead to participants taking too long to complete the questionnaire, reducing its validity. Furthermore, understanding daily behavior features requires repeated behavioral monitoring over an extended period, while retrospective reports from a single point in time may not accurately reflect true behavior [ 13 ].
The use of electronic platforms for behavioral monitoring allows for real-time assessment of human behavior and can trigger an alert if measured behavior deviates from healthy norms [ 14 , 15 ]. Additionally, these platforms enable the collection of large amounts of high-frequency, high-dimensional continuous data, which can be used to identify typical multidimensional behavior features over an extended period based on naturalistic situations [ 16 , 17 ]. The growing body of literature leveraging behavioral monitoring for depression prediction has gained traction, spurred by the profound shifts in lifestyle behavior patterns, especially during the COVID-19 pandemic [ 18 - 20 ]. Nonetheless, predominant inquiries have predominantly concentrated on probing the correlation between physical activity, social network engagement, and mental well-being facilitated through mobile devices [ 21 - 23 ]. However, an evident void persists in comprehensively exploring the nexus between the surveillance of dietary behavior patterns and depression. On university campuses, meals are often paid for using electronic transactions linked to a student account, providing the opportunity to collect digital dietary behavior data. In this study, real-world monitoring was used to track dietary behavior for a month, and data on time, expenditure, and location patterns were collected.
To the best of our knowledge, this is the first study to use electronic device–based behavioral monitoring instead of retrospective self-reported data to examine the digital dietary behaviors of individuals with depression compared with controls, and to investigate the relationship between these behaviors and depression. It is common for depression to occur alongside other symptoms, but the relationship between digital dietary behaviors and these comorbid symptoms of depression remains underexplored. Therefore, we also aim to determine whether these comorbid symptoms are associated with dietary behaviors and to clarify the role these symptoms play in the relationship between changes in dietary behavior and depression. The final data analysis will involve using digital dietary behavior features to detect depression.
Recruitment of Participants
A total of 3678 medical students from Xinxiang Medical University willingly engaged in this study, responding to the institution’s mental health survey notification. As part of this engagement, they underwent a cross-sectional mental status survey from October 6 to 12, 2020. Concurrently, during the survey, these participants also consented to furnish records of their eating behaviors for the period spanning from October 1 to 31, 2020. These records were sourced from electronic transactions linked to their respective student accounts. All participants completed questionnaires via WeChat (Tencent Corp) and signed web-based informed consent.
Web-Based Measurements
Basic sociodemographic characteristics, such as gender, age, BMI, and educational level, were collected using the WeChat official account platform. All participants also completed the following psychological assessments: the Patient Health Questionnaire-9 (PHQ-9), the Generalized Anxiety Disorder Questionnaire-7 (GAD-7), the Perceived Stress Scale-14 (PSS-14), and the Insomnia Severity Index (ISI). All the details of these psychological assessments can be found in Multimedia Appendix 1 .
Study Participants and Inclusion Criteria
Based on the outcomes of the psychological survey, the inclusion criteria for the mild depression group, the moderate-severe depression group, and the healthy control (HC) group, as well as the exclusion criteria, were defined as follows.
Inclusion criteria were established as follows: individuals in the mild depression group had PHQ-9 scores between 5 and 9, while those in the moderate-severe depression group had PHQ-9 scores of 10 or higher. The HC group had PHQ-9 scores below 5, GAD-7 scores below 5, PSS-14 scores below 29, and ISI scores below 8. Exclusion criteria for all participants included PHQ-9 scores below 5 and any of the following conditions: GAD-7 scores of 5 or higher, PSS-14 scores of 29 or higher, or ISI scores of 8 or higher. The participant inclusion process for this study is depicted in Figure 1 (Step 1).

Ethical Considerations
Prior to their involvement in the study, all participants provided their informed consent through a formally endorsed consent form. The study was approved by the Biomedical Ethics Committee of Xinxiang Medical University (XYLL-2020235).
Dietary Data Collection
During the COVID-19 pandemic in China, students were required to stay on campus, resulting in most students eating at the campus cafeterias on a daily basis. These meals are often paid for using electronic transactions linked to a student’s account, and there are 3 cafeterias at the school. The dietary data preprocess can be found in Multimedia Appendix 1 . Previous studies have shown that diet time, or chronotype, is related to circadian rhythms and mood [ 5 ], and location and periodicity of meals are related to depression symptoms [ 24 ]. Therefore, we evaluated 6 dietary behavior features, including time, location, expenditure, daily dietary items and frequency of meals, and all-day dietary behavior patterns, to objectively assess dietary behaviors in relation to depression in this study ( Figure 1 , Step 2).
Calculation of Dietary Features
Time patterns.
To determine the number of daily meals, we counted the number of records starting from the first recorded meal. Dietary behaviors within 2 hours of this initial record were part of a single meal, which could be further divided into up to 1, 2, or 3 meals per day: breakfast, lunch, and dinner. In addition, based on the cafeteria’s hours of operation, the 3 meals are divided into time slots as follows: breakfast from 6:30 AM to 8:30 AM, lunch from 11 AM to 1 PM, and dinner from 5:30 PM to 7:30 PM. If there were multiple electronic transactions within a single meal, we used the timestamp of the first transaction as the time of the meal for analysis.
Time Intervals Between Meals
We used the times of breakfast, lunch, and dinner calculated from the time patterns to determine the time intervals between each pair of meals: breakfast and lunch, lunch and dinner, and breakfast and dinner.
Expenditure on Meals
After dividing meals into breakfast, lunch, and dinner based on the time patterns, we calculated the total cost for each meal by summing up multiple electronic transactions for a single meal. Expenditure on a single meal may indicate an individual’s appetite as it reflects the amount of food purchased.
Location Patterns
To determine location patterns of dietary behavior, we calculated the frequency of visits to each cafeteria by counting total number of cafeterias visited in October and calculated the frequency of the student’s visits to the cafeteria for breakfast, lunch, and dinner using the following formula:

Daily Dietary Diversity and Frequency of Meals
The average number of different foods consumed per day in October was calculated as a measure of food diversity. The frequency of breakfast, lunch, and dinner in the month was also calculated as a measure of dietary habits. These measures were used to understand the dietary behaviors of participants in the study.
All-Day Dietary Behavior Patterns
People may have regular or irregular dietary behavior patterns, such as consistently or selectively eating breakfast, lunch, and dinner. There are 7 possible dietary behavior patterns: eating only breakfast, only lunch, only dinner, breakfast-lunch, lunch-dinner, and all 3 meals (breakfast-lunch-dinner pattern). All-day dietary behavior patterns are defined as the meals eaten by a participant on a given day. The frequency of a participant’s daily dietary behavior patterns can be calculated based on their dietary records for the entire month of October. To do this, the daily records are taken as a unit and the frequency of each dietary behavior pattern is calculated using the following formula:

Statistical Indices of Dietary Features
Statistical indices were calculated for dietary features such as time patterns, intervals between meals, and expenditure on meals, including mean, median, median absolute deviation (MAD), and maximum and minimum values for the entire month of October. The study also separated weekday and weekend behavior by calculating dietary features separately for the 2 time periods. More information can be found in Table S1 in Multimedia Appendix 1 .
Statistical Analysis
ANOVA and chi-square tests were used to analyze demographic and psychological characteristics. ANCOVA (analyses of covariance) was used to compare dietary behavior features among groups, with age, gender, BMI, and educational level as covariates. All variables in the 6 dietary features were transformed into Z-scores to give equal weight and minimize the impact of outliers in the study. Logistic regression analyses were used to examine associations between all-day dietary behavior patterns and depression severity (mild depression, and moderate-severe depression), as well as associations between other psychological symptoms in depression groups or all participants and all-day dietary behavior patterns, with age, gender, BMI, and educational level as covariates. The all-day dietary behavior patterns were categorized into tertiles: Rare (less than 1 SD), Normal (within 1 SD), and Always (more than 1 SD) in logistic regression analyses. Mediation analysis was performed using Model 4 with 1 independent variable (all-day dietary behavior patterns), 1 dependent variable (groups), and 1 moderator (other psychological symptoms) in the PROCESS. A bootstrapping procedure with 95% CIs was used to measure the moderating effect, with 5000 bootstrap samples. Age, gender, BMI, and educational level were included as covariates in the model. All analyses were conducted using SPSS (version 25.0; IBM Corp).
Classification Model
We analyzed changes in dietary behaviors between individuals with HC and depression to detect depression. These dietary behaviors were divided into tertile levels (HC, mild depression, and moderate-severe depression) and binary levels (HC and moderate-severe depression). We used a support vector machine with a radial basis function kernel as the classifier and selected the optimal parameters (0.1 for C and 0.001 for gamma) through grid search. These same parameters were used in all subsequent experiments. To avoid overfitting the model and ensure the accuracy of our results, we used 5-fold cross-validation and divided the training and validation sets in a 4:1 ratio.
Demographic and Clinical Characteristics of Participators
A total of 3310 students, consisting of 2222 HC, 916 mild depression, and 172 moderate-severe depression, met the inclusion criteria and were ultimately included in the study. And 368 students exhibited psychological symptoms, notably anxiety, insomnia, or abnormal stress, while concurrently not manifesting depressive symptoms. As a result, they were excluded from the study cohort. In the students with mild depression, the following rates were observed: 37.7% (n=345) with anxiety, 17.8% (n=163) with perceived abnormal stress, and 23.8% (n=218) with insomnia. In moderate-severe depressive students, the corresponding percentages were: 75% (n=129) with anxiety, 70.3% (n=121) with perceived abnormal stress, and 53.5% (n=92) with insomnia. The demographic and clinical characteristics of the participants can be found in Table 1 .
a HC: healthy control.
b N/A: not applicable.
c Information that was missing for some participants.
d PHQ-9: Patient Health Questionnaire-9.
e GAD-7: Generalized Anxiety Disorder Questionnaire-7.
f PSS-14: Perceived Stress Scale-14.
g ISI: Insomnia Severity Index.
Dietary Features Among HC, Mild Depression, and Moderate-Severe Depression
The ANCOVA analyses showed that there were significant differences between the groups in terms of time patterns, the intervals between meals, expenditure on meals, daily dietary diversity and frequency of meals, and all-day dietary behavior patterns (details in Table S2 in Multimedia Appendix 1 ). There was no significant difference in location patterns among the 3 groups.
In terms of time patterns, post hoc analyses showed that compared with mild depression and HC, moderate-severe depression had significantly increased MAD of lunchtime ( P =.04 and P =.004, separately), latest lunchtime ( P =.02 and P =.007, separately) and MAD of dinner time ( P =.02 and P =.01, separately) on weekdays, and there was no significant difference between mild depression and HC ( Figure 2 A). In terms of time intervals between meals, post hoc analyses that compared mild depression and HC, moderate-severe depression had increased MAD ( P =.001 and P <.001, separately) and maximum ( P =.02 and P =.005, separately) time intervals between lunch and dinner on weekdays, respectively, but mild depression and HC had no significant difference with each other ( Figure 2 B). On weekends, post hoc analyses that compared with HC, mild depression had a significant decrease in the mean time interval between breakfast and lunch ( P =.01), while mild depression and moderate-severe depression had significant decreases in the maximum time interval between breakfast and lunch ( P =.02 and P =.03 separately; Figure 2 B). The MAD of lunchtime on weekdays was higher in moderate-severe depression (18 minutes 58 seconds) than mild depression (17 minutes 38 seconds) and HC (17 minutes 5 seconds). Similarly, the MAD of dinner time on a weekday was higher in moderate-severe depression (26 minutes 11 seconds) than in mild depression (23 minutes 39 seconds) and HC (23 minutes 26 seconds). Additionally, the MAD time interval between lunch and dinner on weekdays was larger in moderate-severe depression (34 minutes 20 seconds) than in mild depression (29 minutes 25 seconds) and HC (29 minutes 23 seconds; Table S2 in Multimedia Appendix 1 ). These findings indicate a temporally erratic lunch and dinner dietary pattern in moderate-severe depression.

In terms of expenditure on meals, compared with HC, both students with mild and moderate-severe depression had significant increases in the mean ( P =.02 and P =.02, separately) and median ( P =.002 and P =.006, separately) of dinner expenditure on weekdays ( Figure 2 C). However, there was no significant difference between mild depression and moderate-severe depression. On weekends, the mild depressive students had a significant increase in the minimum lunch expenditure compared with HC ( P =.03) and moderate-severe depression ( P =.01), but HC and moderate-severe depression had no significant difference from each other ( Figure 2 C).
In terms of daily dietary diversity, post hoc analyses that moderate-severe depression had significant decreases compared with mild depression and HC both on weekdays ( P =.02 and P =.01, separately) and weekends ( P =.03 and P =.01, separately). However, there was no significant difference between mild depression and HC. We also found that compared with HC, moderate-severe depression had a significant reduction in breakfast frequency on weekdays ( P =.02) and weekends ( P =.005). Additionally, compared with mild depression, moderate-severe depression had a significant reduction in breakfast frequency on weekends ( P =.05). However, there was no significant difference between mild depression and HC in breakfast frequency on weekdays and weekends ( Figure 2 D).
Finally, in terms of all-day dietary behavior patterns, compared with HC and mild depression, moderate-severe depression had a reduction in the breakfast-lunch-dinner pattern on weekdays ( P =.001 and P =.002, separately) and enrichment in the lunch-dinner pattern on weekdays ( P =.005 and P =.03 separately; Figure 2 E). However, there was no significant difference between HC and mild depression. On weekends, we observed that moderate-severe depression had an enrichment in the lunch-dinner pattern compared with HC ( P =.008; Figure 2 E).
Associations Between All-Day Dietary Behavior Patterns and Depression
To gain a deeper understanding of the relationship between comprehensive indicators of all-day dietary behavior patterns and depression severity. Using multiple logistic regression, we analyzed the associations between alterations in all-day dietary behavior patterns and depression severity in Figures 3 A and 3B. After adjusting for age, gender, BMI, and educational level, we found that the Normal and Always lunch-dinner patterns on weekdays were positively associated with mild depression (Exp(B), 95% CI 1.360, 1.050-1.761; 1.460, 1.016-2.100; respectively), and the Always breakfast-lunch-dinner pattern on weekdays was negatively associated with moderate-severe depression (Exp(B), 95% CI 0.467, 0.239-0.912). The comparison of tertile levels of these all-day dietary behavior patterns among 3 groups can be found in Table S3 in Multimedia Appendix 1 , and the percent of tertile levels of these all-day dietary behavior patterns can be found in Multimedia Appendix Figure S1.

Associations Between All-Day Dietary Behavior Patterns and Other Clinical Symptoms
Our findings revealed a positive correlation between anxiety and adherence to the consistent always breakfast-lunch-dinner pattern on weekdays among individuals with depression as well as all participants ( Figures 3 C and 3D). However, no significant associations were discovered between other all-day dietary patterns and other clinical symptoms (Table S4 in Multimedia Appendix 1 ). In the mediation model, anxiety served as a mediator ( R 2 =0.570, P <.001). A bootstrapped 95% CI confirmed that the indirect effect of groups (HC, mild depression, and moderate-severe depression) had an impact of 0.042 that was produced by anxiety as a mediator on breakfast-lunch-dinner pattern ( Figure 3 E).
The Detection of Dietary Patterns for Depression
Our results showed that alterations in dietary behaviors of depression had an accuracy of 0.53, F 1 -score of 0.52, precision of 0.60, recall of 0.62, and an area under curve of 0.59 for detecting mild depression and moderate-severe depression. For detecting moderate-severe depression specifically, the accuracy was 0.67, F 1 -score was 0.60, precision was 0.64, recall was 0.65, and area under curve was 0.69 ( Table 2 ).
a AUC: area under the curve.
b HC: healthy control.
Principal Results
This study is the first to investigate digital dietary patterns of individuals with mild and moderate-severe depression using electronic device–based monitoring. The results indicate that individuals with moderate-severe depression exhibit more irregular eating time patterns, greater fluctuations in their feeding window, higher expenditure on dinner, lower food diversity, and a decreased frequency of consuming breakfast, as well as more irregular lunch-dinner patterns and less regular breakfast-lunch-dinner patterns compared with HC. The study also found that maintaining a regular breakfast-lunch-dinner pattern is negatively associated with moderate-severe depression, and maintaining an irregular lunch-dinner pattern is positively associated with mild depression. Additionally, the presence of anxiety is positively associated with the breakfast-lunch-dinner pattern, and the severity of anxiety has an indirect effect on the relationship between depression and the breakfast-lunch-dinner pattern. Importantly, the study suggests that digital dietary features can be used to detect depression, particularly moderate-severe depression, indicating that quantified digital behavior could be a promising approach to the detection of depression.
Comparison With Prior Work in Dietary Behavior of Depression
We found that individuals with moderate-severe depression exhibited a reduction in dietary diversity, a decreased frequency of consuming breakfast, and irregular timing for lunch and dinner. The loss of interest in pleasurable activities, including eating, is a core symptom of depression, which may explain the decreased dietary diversity in individuals with moderate-severe depression. The findings of decreased breakfast frequency in moderate-severe depression align with previous research, which has identified a significant association between skipped or infrequent breakfast and an increased risk for depression [ 25 , 26 ]. The frequency of lunch and dinner did not significantly contribute to depression [ 26 , 27 ]. This discrepancy may be attributed to the fact that individuals with depression tend to have worse moods in the morning, which may negatively impact their appetite for breakfast. Considering these findings, it is important to consider the specific meal that is skipped when implementing dietary interventions to prevent depression. The study found that individuals with mild and moderate-severe depression exhibited significant fluctuations in the timing of lunch and dinner, as well as an irregular time interval between these meals. These findings align with previous research that has identified the importance of the feeding window on mental health [ 28 , 29 ], with irregular eating time patterns being associated with an increased risk of mental health distress [ 30 ]. Additionally, this study is the first to investigate the expenditure on 3 meals in individuals with depression, which provides insight into their food intake and appetite for each meal. The results indicate that individuals with mild and moderate-severe depression spent more money on dinner, which is consistent with the observation that individuals with major depressive disorder tend to have higher food intake during dinner compared with breakfast and lunch [ 31 ]. Notably, this study is the first to report that depression is associated with a preference for higher expenditure on dinner, while also being accompanied by a low frequency of breakfast.
This study is the first to objectively quantify all-day dietary behavior patterns by integrating time patterns, frequency of meals, and other parameters, and it revealed that moderate-severe depression is associated with an increase in lunch-dinner patterns and a decrease in breakfast-lunch-dinner patterns. Previous research has demonstrated that consuming breakfast, lunch, and dinner every day can reduce the prevalence of first-onset depression in a 5-year follow-up [ 32 ]. The lunch-dinner pattern is associated with eating later in the day and a meta-analysis has indicated that depressed patients are more inclined to spend on food later in the day, a phenomenon known as eveningness chronotype [ 33 ]. The relationship between eveningness chronotype and depressive symptoms aligns with pre-existing theories of chronobiology, which suggest that circadian dysfunction can have adverse effects on psychological well-being [ 34 , 35 ]. Eveningness chronotype is associated with a higher likelihood of regularly skipping or postponing breakfast [ 36 ] and it is well recognized that eating breakfast plays an important role in lowering blood cortisol levels and disturbances in glucose metabolism, which may affect serotonin levels [ 37 ].
Prior research in the dietary patterns field, whether dietary nutrition, dietary frequency, or dietary chronotype studies, predominantly relied on questionnaires [ 38 , 39 ]. The use of electronic behavioral monitoring for evaluating dietary behavioral patterns is still in its nascent technological phase. The self-monitoring is a prevalent method for assessing electronic dietary behaviors in the study of mental health [ 40 , 41 ]. This approach predominantly entails participants proactively documenting their daily dietary intake using an electronic device, often an app. However, it is important to acknowledge that excessive self-recording of behaviors could potentially lead to fatigue and monotony. While a frequency ranging from 2 to 3 times per week proved to be acceptable and reasonable [ 42 ], it once again harbors the inherent issue of recall bias that was previously encountered. Moreover, the field of wearable device-based monitoring for tracking dietary behavior has witnessed notable advancements [ 43 , 44 ]. However, its application in the field of psychiatry remains unexplored to date. The study marks the pioneering use of objective electronic device–based monitoring, unveiling anomalous eating patterns among individuals with depression.
The Associations Between Dietary Behavioral Patterns and Depression
The study found that maintaining a lunch-dinner pattern was positively associated with mild depression. Furthermore, maintaining a breakfast-lunch-dinner pattern was negatively associated with moderate-severe depression. These findings align with previous research that has identified eating breakfast as a health-promoting behavior [ 45 ] and a positive association between skipping breakfast and depressive symptoms [ 46 ]. Additionally, it highlights the importance of meal substitution for regular eating patterns as a positive association with emotional disorders [ 47 ]. Overall, these findings suggest that maintaining a regular dietary pattern can be considered a dietary strategy for depression prevention.
Furthermore, the study found that anxiety is positively associated with the breakfast-lunch-dinner pattern. We can infer from the result that individuals with anxiety tend to choose to regularly eat 3 meals in their daily life and that depression with increasing anxiety may lead to an increase in the breakfast-lunch-dinner eating behavior. Literature has also indicated that individuals with anxiety tend to engage in more overeating situations [ 48 ] and have a positive association between anxiety symptoms and emotional and external eating [ 49 ]. However, the study also indicates that those with depression tend to intake more in dinner and then postpone or skip breakfast the next day. The study also found that anxiety could mediate the relationship between depression and breakfast-lunch-dinner pattern, which indicates that students with anxiety tend to maintain a regular breakfast-lunch-dinner pattern rather than postponing or skipping breakfast. This highlights the need for careful consideration when implementing dietary interventions for the comorbidity of depression and anxiety.
The Potential Value of Digital Dietary Behaviors in Depression
This study is the first to use digital dietary behaviors based on real-world behavioral monitoring to detect mild depression and moderate-severe depression. The results indicate that digital dietary behaviors could distinguish between moderate-severe depression and HC. Depression is a disorder characterized by brain-based dysfunction that is expressed through behavioral changes. The diagnosis of depression traditionally relies on structured interviews or questionnaires, which are based on retrospective self-reports and the threshold scores of questionnaires. These methods can be prone to bias and subjectivity. The use of digital markers of continuous daily behavioral monitoring as an objective indicator to detect depression represents a promising supplementary approach [ 13 ].
In this study, students’ dietary behaviors were analyzed over a period of 1 month to draw a profile of dietary patterns in depression. This is the first exploration of the relationship between digital dietary behaviors and depression, and the use of digital dietary behaviors to detect depression. Another thing to watch out for is that the results indicate that a deep learning model of dietary behaviors from digital devices holds more accurate detection of moderate-severe depression than mild depression. This is likely due to the observation that moderate-severe depression presents more erratic dietary behaviors than mild depression and HCs. Overall, this study highlights the potential of digital dietary features as a promising manner in the detection of depression, particularly moderate-severe depression.
Limitations
There are several limitations in this study that should be acknowledged. First, the measurement of depression severity in this study was based on self-reported data, future studies should consider clinician-based rating scales to reduce bias. Additionally, this study used a cross-sectional survey of depression, which does not capture changes in symptomology over time. A longitudinal psychological survey combined with continuous daily behavioral monitoring could provide further insight into dietary progression markers related to the severity of depressive symptoms over time. Finally, the study did not assess daily dietary structure and nutrient intake.
Conclusions
This study represents a pioneering endeavor in objectively characterizing the digital dietary behaviors of individuals experiencing depression, using real-world monitoring as opposed to self-reported retrospective data. Our findings indicate that students with depression experience disruptions in various aspects, including time patterns, the intervals between meals, expenditure on meals, daily dietary diversity and frequency of meals, and all-day dietary behavior patterns. Notably, individuals with moderate-severe depression showcase greater irregularities in eating time patterns, fluctuated feeding windows, decreased food diversity, higher expenditure on dinner, and a preference for consuming only lunch and dinner. Furthermore, maintaining a regular breakfast-lunch-dinner eating pattern exhibits a negative correlation with moderate-severe depression. Keeping a lunch-dinner pattern is positively associated with mild depression. This research not only fills a critical gap in the existing academic literature but also sheds light on the promising potential of digital dietary behaviors as objective makers to the detection of depression, particularly moderate-severe depression.
Acknowledgments
This study was supported by grants from National Science Fund for Distinguished Young Scholars (81725005 to FW), NSFC-Guangdong Joint Fund (U20A6005 to FW), Jiangsu Provincial Key Research and Development Program (BE2021617 to FW), National Natural Science Foundation of China (62176129 to XZ), National Key Research and Development Program (2022YFC2405603 to XZ), and Henan Provincial Research and Practice Project for Higher Education Teaching Reform (2021SJGLX189Y to RL). The authors would like to thank all participants who took part in this study. The authors would also like to thank the support to recruitment by personnel at Xinxiang Medical University.
Data Availability
The data sets generated and analyzed during this study are available from the co-corresponding authors (FW: [email protected]; XZZ: [email protected]) on reasonable request.
Authors' Contributions
FW and XZZ are co-corresponding authors. XZZ and FW designed the study. RXL and YZ enrolled participants. YHS, YZ, SLY, and SZ analyzed data. YZ, RZ, and FYW wrote the paper.
Conflicts of Interest
None declared.
Supplemental materials.
- Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. 2020;29:e181. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228-229. [ FREE Full text ] [ CrossRef ] [ Medline ]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Arlington, VA. American Psychiatric Publishing; 2013.
- Marx W, Lane M, Hockey M, Aslam H, Berk M, Walder K, et al. Diet and depression: exploring the biological mechanisms of action. Mol Psychiatry. 2021;26(1):134-150. [ CrossRef ] [ Medline ]
- Phoi YY, Rogers M, Bonham MP, Dorrian J, Coates AM. A scoping review of chronotype and temporal patterns of eating of adults: tools used, findings, and future directions. Nutr Res Rev. 2022;35(1):112-135. [ CrossRef ] [ Medline ]
- Teixeira GP, Guimarães KC, Soares AGNS, Marqueze EC, Moreno CRC, Mota MC, et al. Role of chronotype in dietary intake, meal timing, and obesity: a systematic review. Nutr Rev. 2022;81(1):75-90. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Qu Y, Li T, Xie Y, Tao S, Yang Y, Zou L, et al. Association of chronotype, social jetlag, sleep duration and depressive symptoms in Chinese college students. J Affect Disord. 2023;320:735-741. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Antypa N, Verkuil B, Molendijk M, Schoevers R, Penninx BWJH, Van Der Does W. Associations between chronotypes and psychological vulnerability factors of depression. Chronobiol Int. 2017;34(8):1125-1135. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Qian J, Vujovic N, Nguyen H, Rahman N, Heng SW, Amira S, et al. Daytime eating prevents mood vulnerability in night work. Proc Natl Acad Sci U S A. 2022;119(38):e2206348119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nicolaou M, Colpo M, Vermeulen E, Elstgeest LEM, Cabout M, Gibson-Smith D, et al. Association of a priori dietary patterns with depressive symptoms: a harmonised meta-analysis of observational studies. Psychol Med. 2020;50(11):1872-1883. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kennedy ET, Ohls J, Carlson S, Fleming K. The healthy eating index: design and applications. J Am Diet Assoc. 1995;95(10):1103-1108. [ CrossRef ] [ Medline ]
- Romo-Nava F, Blom TJ, Guerdjikova A, Winham SJ, Cuellar-Barboza AB, Nunez NA, et al. Evening chronotype, disordered eating behavior, and poor dietary habits in bipolar disorder. Acta Psychiatr Scand. 2020;142(1):58-65. [ CrossRef ] [ Medline ]
- Taliaz D, Souery D. A new characterization of mental health disorders using digital behavioral data: evidence from major depressive disorder. J Clin Med. 2021;10(14):3109. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sun S, Folarin AA, Ranjan Y, Rashid Z, Conde P, Stewart C, et al. Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J Med Internet Res. 2020;22(9):e19992. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Oladeji O, Zhang C, Moradi T, Tarapore D, Stokes AC, Marivate V, et al. Monitoring information-seeking patterns and obesity prevalence in Africa with internet search data: observational study. JMIR Public Health Surveill. 2021;7(4):e24348. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morita PP, Hussain IZ, Kaur J, Lotto M, Butt ZA. Tweeting for health using real-time mining and artificial intelligence-based analytics: design and development of a big data ecosystem for detecting and analyzing misinformation on Twitter. J Med Internet Res. 2023;25:e44356. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mavragani A, Ochoa G. Google trends in infodemiology and infoveillance: methodology framework. JMIR Public Health Surveill. 2019;5(2):e13439. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Felez-Nobrega M, Werneck AO, El Fatouhi D, de Luca K, Islam SMS, Franzese F. Device-based physical activity and late-life depressive symptoms: an analysis of influential factors using share data. J Affect Disord. 2023;322:267-272. [ CrossRef ] [ Medline ]
- Biernesser C, Montano G, Miller E, Radovic A. Social media use and monitoring for adolescents with depression and implications for the COVID-19 pandemic: qualitative study of parent and child perspectives. JMIR Pediatr Parent. 2020;3(2):e21644. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lekkas D, Gyorda JA, Price GD, Jacobson NC. Depression deconstructed: wearables and passive digital phenotyping for analyzing individual symptoms. Behav Res Ther. 2023;168:104382. [ CrossRef ] [ Medline ]
- Masud MT, Mamun MA, Thapa K, Lee DH, Griffiths MD, Yang SH. Unobtrusive monitoring of behavior and movement patterns to detect clinical depression severity level via smartphone. J Biomed Inform. 2020;103:103371. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sequeira L, Battaglia M, Perrotta S, Merikangas K, Strauss J. Digital phenotyping with mobile and wearable devices: advanced symptom measurement in child and adolescent depression. J Am Acad Child Adolesc Psychiatry. 2019;58(9):841-845. [ CrossRef ] [ Medline ]
- Daryabeygi-Khotbehsara R, Islam SMS, Dunstan D, McVicar J, Abdelrazek M, Maddison R. Smartphone-based interventions to reduce sedentary behavior and promote physical activity using integrated dynamic models: systematic review. J Med Internet Res. 2021;23(9):e26315. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saeb S, Lattie EG, Schueller SM, Kording KP, Mohr DC. The relationship between mobile phone location sensor data and depressive symptom severity. PeerJ. 2016;4:e2537. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pengpid S, Peltzer K. Skipping breakfast and its association with health risk behaviour and mental health among university students in 28 countries. Diabetes Metab Syndr Obes. 2020;13:2889-2897. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kwak Y, Kim Y. Association between mental health and meal patterns among elderly Koreans. Geriatr Gerontol Int. 2018;18(1):161-168. [ CrossRef ] [ Medline ]
- Yun H, Kim DW, Lee EJ, Jung J, Yoo S. Analysis of the effects of nutrient intake and dietary habits on depression in Korean adults. Nutrients. 2021;13(4):1360. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Almeneessier AS, BaHammam AS. How does diurnal intermittent fasting impact sleep, daytime sleepiness, and markers of the biological clock? current insights. Nat Sci Sleep. 2018;10:439-452. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Currenti W, Godos J, Castellano S, Mogavero MP, Ferri R, Caraci F, et al. Time restricted feeding and mental health: a review of possible mechanisms on affective and cognitive disorders. Int J Food Sci Nutr. 2021;72(6):723-733. [ CrossRef ] [ Medline ]
- Tahara Y, Makino S, Suiko T, Nagamori Y, Iwai T, Aono M, et al. Association between irregular meal timing and the mental health of Japanese workers. Nutrients. 2021;13(8):2775. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BWJH. Chronotype associations with depression and anxiety disorders in a large cohort study. Depress Anxiety. 2016;33(1):75-83. [ CrossRef ] [ Medline ]
- Wilson JE, Blizzard L, Gall SL, Magnussen CG, Oddy WH, Dwyer T, et al. An eating pattern characterised by skipped or delayed breakfast is associated with mood disorders among an Australian adult cohort. Psychol Med. 2020;50(16):2711-2721. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Au J, Reece J. The relationship between chronotype and depressive symptoms: a meta-analysis. J Affect Disord. 2017;218:93-104. [ CrossRef ] [ Medline ]
- Leng Y, Musiek ES, Hu K, Cappuccio FP, Yaffe K. Association between circadian rhythms and neurodegenerative diseases. Lancet Neurol. 2019;18(3):307-318. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci. 2010;11(8):589-599. [ CrossRef ] [ Medline ]
- Roßbach S, Diederichs T, Nöthlings U, Buyken AE, Alexy U. Relevance of chronotype for eating patterns in adolescents. Chronobiol Int. 2018;35(3):336-347. [ CrossRef ] [ Medline ]
- Wehrens SMT, Christou S, Isherwood C, Middleton B, Gibbs MA, Archer SN, et al. Meal timing regulates the human circadian system. Curr Biol. 2017;27(12):1768-1775.e3. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Taeymans J, Luijckx E, Rogan S, Haas K, Baur H. Physical activity, nutritional habits, and sleeping behavior in students and employees of a Swiss university during the COVID-19 lockdown period: questionnaire survey study. JMIR Public Health Surveill. 2021;7(4):e26330. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pei Z, Zhang J, Qin W, Hu F, Zhao Y, Zhang X, et al. Association between dietary patterns and depression in Chinese older adults: a longitudinal study based on CLHLS. Nutrients. 2022;14(24):5230. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hahn SL, Kaciroti N, Eisenberg D, Weeks HM, Bauer KW, Sonneville KR. Introducing dietary self-monitoring to undergraduate women via a calorie counting app has no effect on mental health or health behaviors: results from a randomized controlled trial. J Acad Nutr Diet. 2021;121(12):2377-2388. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zuppinger C, Taffé P, Burger G, Badran-Amstutz W, Niemi T, Cornuz C, et al. Performance of the digital dietary assessment tool MyFoodRepo. Nutrients. 2022;14(3):635. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pagoto S, Tulu B, Agu E, Waring ME, Oleski JL, Jake-Schoffman DE. Using the habit app for weight loss problem solving: development and feasibility study. JMIR Mhealth Uhealth. 2018;6(6):e145. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alshurafa N, Lin AW, Zhu F, Ghaffari R, Hester J, Delp E, et al. Counting bites with bits: expert workshop addressing calorie and macronutrient intake monitoring. J Med Internet Res. 2019;21(12):e14904. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dimitratos SM, German JB, Schaefer SE. Wearable technology to quantify the nutritional intake of adults: validation study. JMIR Mhealth Uhealth. 2020;8(7):e16405. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pearson N, Biddle SJH, Gorely T. Family correlates of breakfast consumption among children and adolescents. a systematic review. Appetite. 2009;52(1):1-7. [ CrossRef ] [ Medline ]
- Lee SA, Park EC, Ju YJ, Lee TH, Han E, Kim TH. Breakfast consumption and depressive mood: a focus on socioeconomic status. Appetite. 2017;114:313-319. [ CrossRef ] [ Medline ]
- Farhangi MA, Dehghan P, Jahangiry L. Mental health problems in relation to eating behavior patterns, nutrient intakes and health related quality of life among Iranian female adolescents. PLoS One. 2018;13(4):e0195669. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Klatzkin RR, Gaffney S, Cyrus K, Bigus E, Brownley KA. Stress-induced eating in women with binge-eating disorder and obesity. Biol Psychol. 2018;131:96-106. [ CrossRef ] [ Medline ]
- Song YM, Lee K, Sung J. Genetic and environmental relationships between eating behavior and symptoms of anxiety and depression. Eat Weight Disord. 2019;24(5):887-895. [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani, T Sanchez; submitted 27.03.23; peer-reviewed by A Lamer, A Ghosh; comments to author 17.08.23; revised version received 02.09.23; accepted 01.03.24; published 22.04.24.
©Yue Zhu, Ran Zhang, Shuluo Yin, Yihui Sun, Fay Womer, Rongxun Liu, Sheng Zeng, Xizhe Zhang, Fei Wang. Originally published in JMIR Public Health and Surveillance (https://publichealth.jmir.org), 22.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Public Health and Surveillance, is properly cited. The complete bibliographic information, a link to the original publication on https://publichealth.jmir.org, as well as this copyright and license information must be included.

Initiatives
Our community.
- Education & Admissions
New research in psychedelic therapy shows clinician-patient bond may matter most
Author: Kelli Trinoskey
- College Updates

“What persisted the most was the connection between the therapeutic alliance and long-term outcomes, which indicates the importance of a strong relationship,” said lead author Adam Levin , a psychiatry and behavioral health resident in The Ohio State University College of Medicine .
Read more .
More from Ohio State

Alumni Spotlight: Ava Willoughby

Genetic Counseling Graduate Program welcomes new assistant professor

Student Spotlight: Nicole Moulas
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

In psychedelic therapy, clinician-patient bond may matter most
Study links relationship strength to reduced depression for up to 1 year.
Drug effects have dominated the national conversation about psychedelics for medical treatment, but a new study suggests that when it comes to reducing depression with psychedelic-assisted therapy, what matters most is a strong relationship between the therapist and study participant.
Researchers analyzed data from a 2021 clinical trial that found psilocybin (magic mushrooms) combined with psychotherapy in adults was effective at treating major depressive disorder.
Data included depression outcomes and participant reports about their experiences with the drugs and their connection with therapists. Results showed that the stronger the relationship between a participant and clinician – called a therapeutic alliance – the lower the depression scores were one year later.

“What persisted the most was the connection between the therapeutic alliance and long-term outcomes, which indicates the importance of a strong relationship,” said lead author Adam Levin , a psychiatry and behavioral health resident in The Ohio State University College of Medicine .
Past research has consistently found that as mental health treatments changed, a trusting relationship between clients and clinicians has remained key to better outcomes, said senior author Alan Davis , associate professor and director of the Center for Psychedelic Drug Research and Education in The Ohio State University College of Social Work .
“This concept is not novel. What is novel is that very few people have explored this concept as part of psychedelic-assisted therapy,” Davis said. “This data suggests that psychedelic-assisted therapy relies heavily on the therapeutic alliance, just like any other treatment.”
The study was published recently in the journal PLOS ONE .
Twenty-four adults who participated in the trial received two doses of psilocybin and 11 hours of psychotherapy. Participants completed the therapeutic alliance questionnaire, assessing the strength of the therapist-participant relationship, three times: after eight hours of preparation therapy and one week after each psilocybin treatment.

Participants also completed questionnaires about any mystical and psychologically insightful experiences they had during the drug treatment sessions. Their depression symptoms were assessed one week, four weeks, and up to one year after the trial’s end.
The analysis showed that the overall alliance score increased over time and revealed a correlation between a higher alliance score and more acute mystical and/or psychologically insightful experiences from the drug treatment. Acute effects were linked to lower depression at the four-week point after treatment, but were not associated with better depression outcomes a year after the trial.
“The mystical experience, which is something that is most often reported as related to outcome, was not related to the depression scores at 12 months,” Davis said. “We’re not saying this means acute effects aren’t important – psychological insight was still predictive of improvement in the long term. But this does start to situate the importance and meaning of the therapeutic alliance alongside these more well-established effects that people talk about.”
That said, the analysis showed that a stronger relationship during the final therapy preparation session predicted a more mystical and psychologically insightful experience – which in turn was linked to further strengthening the therapeutic alliance.
“That’s why I think the relationship has been shown to be impactful in this analysis – because, really, the whole intervention is designed for us to establish the trust and rapport that’s needed for someone to go into an alternative consciousness safely,” Davis said.
Considering that psychedelics carry a stigma as Schedule I drugs under the Controlled Substances Act , efforts to minimize negative experiences in future studies of their therapeutic potential should be paramount – and therapy is critical to creating a supportive environment for patients, the authors said.
This study ideally will help clearly position psychedelics treatment as a psychotherapeutic intervention moving forward – rather than its primary purpose being administration of a drug, Levin said.
“This isn’t a case where we should try to fit psychedelics into the existing psychiatric paradigm – I think the paradigm should expand to include what we’re learning from psychedelics,” Levin said. “Our concern is that any effort to minimize therapeutic support could lead to safety concerns or adverse events. And what we showed in this study is evidence for the importance of the alliance in not just preventing those types of events, but also in optimizing therapeutic outcomes.”
This work was supported by the Center for Psychedelic and Consciousness Research, funded by the Steven & Alexandra Cohen Foundation, the RiverStyx Foundation and private donors. It was also supported by the Center for Psychedelic Drug Research and Education (CPDRE), funded by anonymous donors.
Additional co-authors are Rafaelle Lancelotta, Nathan Sepeda and Theodore Wagener of Ohio State, and Natalie Gukasyan, Sandeep Nayak, Frederick Barrett and Roland Griffiths of the Center for Psychedelic and Consciousness Research at Johns Hopkins University, where Davis is an affiliate.
More Ohio State News
A message from president carter.
As the semester draws to a close, I want to thank you for your dedication to teaching, learning, research, patient care – and to Ohio State. As we look forward to spring commencement and the events surrounding this momentous occasion for the class of 2024, I am reminded of the resilience of this class as they navigated starting their collegiate careers during a pandemic.
University of Tennessee chancellor calls on land-grant universities to lead
Plowman, chancellor of the University of Tennessee, Knoxville, has led the state’s flagship land-grant research university since 2019. She was the guest speaker Thursday for the 2024 James F. Patterson Land-Grant University Lecture at The Ohio State University
Older adults in Ohio are among the most vulnerable to extreme weather
Nearly 1 in 5 older adults in central Ohio report not being prepared for emergencies, such as extreme weather events, or not knowing if they are ready. That is concerning because research shows older adults are at greater risk of harm during disasters such as extreme weather events.

Contact: Admissions | Webmaster | Page maintained by University Communications
Request an alternate format of this page | Web Services Status | Nondiscrimination notice
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 22 April 2024
Measuring algorithmic bias to analyze the reliability of AI tools that predict depression risk using smartphone sensed-behavioral data
- Daniel A. Adler 1 ,
- Caitlin A. Stamatis 2 ,
- Jonah Meyerhoff 2 ,
- David C. Mohr 2 ,
- Fei Wang 3 ,
- Gabriel J. Aranovich 1 ,
- Srijan Sen 4 &
- Tanzeem Choudhury 1
npj Mental Health Research volume 3 , Article number: 17 ( 2024 ) Cite this article
8 Altmetric
Metrics details
- Machine learning
- Predictive markers
AI tools intend to transform mental healthcare by providing remote estimates of depression risk using behavioral data collected by sensors embedded in smartphones. While these tools accurately predict elevated depression symptoms in small, homogenous populations, recent studies show that these tools are less accurate in larger, more diverse populations. In this work, we show that accuracy is reduced because sensed-behaviors are unreliable predictors of depression across individuals: sensed-behaviors that predict depression risk are inconsistent across demographic and socioeconomic subgroups. We first identified subgroups where a developed AI tool underperformed by measuring algorithmic bias, where subgroups with depression were incorrectly predicted to be at lower risk than healthier subgroups. We then found inconsistencies between sensed-behaviors predictive of depression across these subgroups. Our findings suggest that researchers developing AI tools predicting mental health from sensed-behaviors should think critically about the generalizability of these tools, and consider tailored solutions for targeted populations.
Similar content being viewed by others

Real-world behavioral dataset from two fully remote smartphone-based randomized clinical trials for depression
Abhishek Pratap, Ava Homiar, … Pat Areán
Differential temporal utility of passively sensed smartphone features for depression and anxiety symptom prediction: a longitudinal cohort study
Caitlin A. Stamatis, Jonah Meyerhoff, … David C. Mohr

Digital health tools for the passive monitoring of depression: a systematic review of methods
Valeria De Angel, Serena Lewis, … Matthew Hotopf
Introduction
Mental healthcare systems are simultaneously facing a shortage of mental health specialty care providers and a large number of patients whose treatment needs remain unmet 1 , 2 . This service gap is driving research into AI-driven mental health monitoring tools, where sensed-behavioral data, defined as inferred behavioral data gathered by sensors and software embedded in everyday devices (e.g. smartphones, wearables), are repurposed to remotely monitor depression symptoms 3 , 4 , 5 , 6 , 7 . Sensed-behavioral data has also been referred to as personal, behavioral, or passive sensing data in other work 7 . AI tools that leverage sensed-behavioral data intend to near-continuously identify individuals experiencing elevated depression symptoms in-between clinical encounters and consequently deliver preventive care 8 . These tools can also be integrated into digital therapeutics to automate precision interventions 9 . Initial work showed that depression risk could be predicted from sensed-behavioral data at a similar accuracy to general practitioners 10 in small populations 5 , 11 . More recent work shows that these AI tools predict depression risk at an accuracy only slightly better than a coin flip in larger, more diverse samples 4 , 6 , 12 , 13 . This prior work has not specifically explored why accuracy is reduced in larger samples, and it is unclear how to improve AI tools for clinical use.
In this work, we hypothesized that accuracy is reduced in larger, more diverse populations because sensed-behaviors are unreliable predictors of depression risk: sensed-behaviors that predict depression are inconsistent across demographic and socioeconomic (SES) subgroups 14 . We intentionally use the term reliability due to its importance in both a psychometric and AI context. In a psychometric context, reliability refers to the consistency of a tool, typically a symptom assessment, across different contexts (e.g. raters, time) 14 , 15 . In AI, reliability is related to generalizability, if an AI tool is consistently accurate in different contexts (e.g. different populations, over time, etc.) 12 . Given these definitions, researchers in AI fairness have argued that aspects of psychometric reliability are important in an AI context: similar inputs (e.g. sensed-behaviors) to an AI model should yield similar outputs (e.g. estimated depression risk) 16 .
In this paper, we adapt these ideas to study a specific aspect of reliability important for mental health AI tools deployed in large populations, i.e. if similar sensed-behaviors are consistently related to depression risk across different subgroups of individuals. We hypothesize that if the sensed-behaviors predictive of depression risk are inconsistent across subgroups, AI models that use sensed-behaviors to predict depression risk will be inaccurate because similar sensed-behavioral patterns will indicate different levels of depression risk for different subgroups. For example, imagine that mobility positively correlates with depression risk in subgroup A, and negatively correlates with depression risk in subgroup B. An AI model trained across subgroups using exclusively mobility data, blind to subgroup information as is typically the case in this literature 3 , 4 , 5 , 17 , will receive unreliable information – high mobility can simultaneously indicate both low and high depression risk – and will make incorrect predictions for one of the subgroups. We note upfront that in this manuscript we do not consider temporal aspects of reliability, though we acknowledge that this is important in discussions of psychometric reliability, specifically if the AI tool is consistently accurate for the same individual, with predictions made under similar conditions 18 .
We tested our hypothesis by identifying population subgroups where a depression risk prediction tool underperformed, and then analyzed sensed-behavioral differences across these subgroups. We identified subgroups where the tool underperformed by measuring algorithmic ranking bias (hereafter referred to as “bias”), which measures the degree to which individuals experiencing depression from one subgroup (e.g. older individuals) are incorrectly ranked by the tool to be at lower risk than healthier individuals from other subgroups (e.g. younger individuals) 19 , 20 , 21 , 22 . Reliability was analyzed by measuring ranking bias because if individuals in large populations have inconsistent relationships between sensed-behaviors and mental health, behaviors that represent high depression risk for one subgroup may represent lower risk for another subgroup. For example, imagine an AI tool predicting that higher phone use increases depression risk. Studies 23 , 24 show that younger individuals have higher phone use than older individuals. Thus, the AI tool may incorrectly rank older individuals with depression to be at lower risk than healthier younger individuals, decreasing model accuracy (Fig. 1a ).
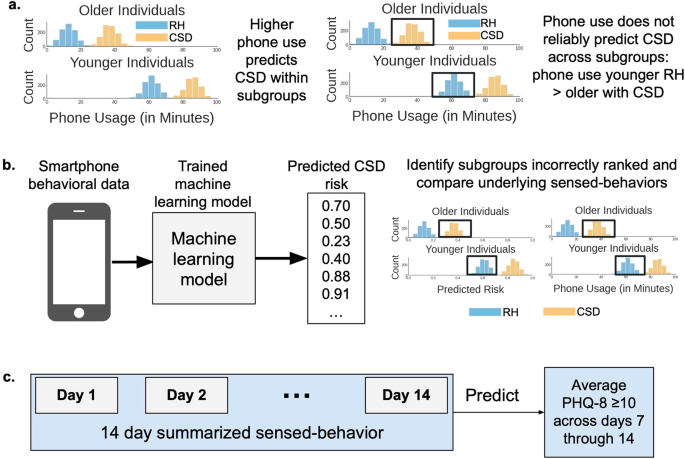
a We hypothesized that sensed-behaviors, like phone use, unreliably predict depression in larger populations because behaviors representing high depression risk for some subgroups (e.g. older individuals) may represent lower risk for other subgroups (e.g. younger individuals). RH is relatively healthy and CSD is clinically-significant depression. Histograms show simulated data describing the count of individuals ( y -axis) with specific daytime phone usage ( x -axis). Colors indicate individuals experiencing CSD (orange) versus RH (light-blue). Plots are split by age subgroups. Black boxes show that increased phone usage is not a reliable predictor of depression because RH younger individuals have higher phone use than CSD older individuals. b The analysis pipeline. Behavioral data from smartphones and mental health outcomes collected during a U.S.-based NIMH-funded study 3 , 25 , 26 , 27 , 28 , 29 were used to train and validate AI models that predicted depression symptom risk from the behavioral data. We then measured algorithmic ranking bias in the developed tool to identify subgroups where the predicted CSD risk was incorrectly ranked lower than RH subgroups, and compared sensed-behaviors across subgroups where algorithms underperformed. c Similar to prior work 3 , 25 , 14 days of sensed-behavioral data were used to predict whether the PHQ-8 value across each weekly reported period indicated clinically-significant depression symptoms (PHQ-8 ≥ 10 33 ).
Against this backdrop, we developed an AI tool that estimated depression symptom risk using behavioral data collected from individuals’ smartphones, using similar sensed-behaviors and outcome measures from recent work 3 , 4 , 5 , 13 , 25 (Fig. 1b ). The data used to develop and analyze the AI tool was collected during a U.S.-based National Institute of Mental Health (NIMH)-funded study 3 , 25 , 26 , 27 , 28 , 29 , one of the largest, most geographically diverse studies of its kind. We then measured bias across attributes including age, sex at birth, race, family income, health insurance, and employment to identify subgroups where the tool underperformed. We studied these specific attributes because of known behavioral differences across demographic and SES subgroups 23 , 24 , 30 , 31 , 32 that could impact the reliability of the developed AI tool. Finally, we interpreted why the tool underperformed by identifying inconsistencies between the AI tool and sensed-behaviors predicting depression across subgroups. A summary of this analysis can be found in Fig. 1 .
Data collection
We analyzed data from a U.S.-based, NIMH-funded study conducted from 2019–2021 to identify associations between behavioral data collected from smartphones and depression symptoms 3 , 25 , 26 , 27 , 28 , 29 . Smartphone sensed-behavioral data on GPS location, phone usage (timestamp of screen unlock), and sleep were near-continuously collected from participants across the United States for 16 weeks and the PHQ-8, a self-reported measure of two week depression symptoms 33 , 34 frequently used in mental health research 3 , 5 , 25 , 27 , was administered multiple times a week every three weeks (on weeks 1, 4, 7, …, known as weekly reporting periods ). Sensed-behaviors were summarized over two weeks to align with collected PHQ-8 depression symptoms for prediction (see Table 1 ). For example, sensed-behaviors collected during weeks 3 and 4 were summarized to predict PHQ-8 responses collected during week 4.
Table 2 summarizes the data used for analysis. 3900 samples were analyzed from 650 individuals, a large cohort and sample size compared to most studies to date analyzing associations between sensed-behaviors and mental health 4 , 5 , 25 , 35 , 36 . A sample was a set of sensed-behaviors, summarized over 2 weeks, corresponding to the average PHQ-8 response collected during a single weekly reporting period. 46% of the average self-reported PHQ-8 values were ≥10, indicating clinically-significant depression (CSD) 33 . The majority of participants were relatively young to middle aged (75% 25 to 54 years old), female (74%), white (82%), middle to high income (61% annual family income ≥$ 40,000), insured (93%) and employed (62%). We focused our results on subgroups with at least 15 participants 37 . The sensed-behavior distributions across the population for each subgroup can be found in the supplementary materials.
Identifying subgroups where AI models underperform
The PHQ-8 asked participants to self-report depression symptoms experienced over 14 days, and PHQ-8’s were delivered multiple times throughout each weekly reporting period. We trained AI models using 14 days of smartphone sensed-behavioral data to predict if the average PHQ-8 value across each weekly reporting period (days 7 through 14, see Fig. 1c ) indicated clinically-significant depression (CSD, PHQ-8 score ≥10 33 ) symptoms. While the PHQ-8 asks participants to self-report 2 week depression symptoms, studies suggest that individual assessments may suffer from recency bias 38 or indicate “briefly” elevated depression symptoms 39 . For this reason, PHQ-8 values were averaged over each weekly reporting period to predict a more stable estimate of self-reported symptoms.
Model performance was assessed by performing 5-fold cross-validation, partitioning on subjects, and predictions across folds were concatenated to calculate model performance. Similar to prior work 4 , 6 , within each cross-validation split, models were trained using data collected from 80% of the participants (520 participants), and the trained model was applied to predict CSD in the remaining 20% (130 participants). To analyze performance variability due to specific cross-validation splits, we performed 100 cross-validation trials, shuffling participants into different folds during each trial.
AI models output a predicted risk score from 0–1 of experiencing CSD. We used the predicted risk to calculate common ranking bias metrics 20 , 21 , 22 (Fig. 2 ) across the subgroups in Table 2 . These metrics were based upon the area under the receiver operating curve (AUC), which measured the probability models correctly predicted that CSD samples were ranked higher (in the predicted risk) than relatively healthy (RH, PHQ-8 < 10) samples. We first calculated the AUC within each subgroup (the “Subgroup AUC”). Note that equal Subgroup AUCs do not guarantee high AUC across an entire sample. For example, Fig. 2a shows simulated data where an algorithm correctly predicted CSD risk within subgroups, but younger individuals, compared to older individuals, have a higher overall predicted risk. Thus, across subgroups, healthy younger individuals may be incorrectly predicted to be at higher risk than older individuals experiencing CSD. Two additional performance metrics assessed such errors. Specifically, the background-negative-subgroup-positive, or BNSP AUC (Fig. 2b ) measured the probability that individuals experiencing CSD (the “positive” label) from a subgroup were correctly predicted to have higher risk than RH (the “negative label”) individuals from other subgroups (“the background”), and the background-positive-subgroup-negative, or BPSN AUC (Fig. 2c ), measured the probability RH individuals from a subgroup were correctly predicted to have lower risk than background individuals experiencing CSD.
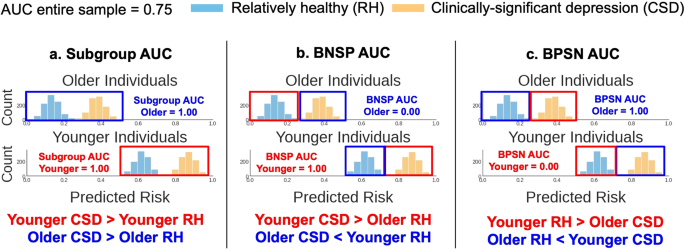
We considered three metrics from prior work to assess algorithmic ranking bias 20 , 21 , 22 . The predicted risk is the probability, output by the AI tool, that individuals were experiencing clinically-significant depression (CSD). Histograms show simulated example predictions from an AI tool, describing the count of individuals ( y -axis) who fell into a predicted risk bin ( x -axis). Colors indicate individuals experiencing CSD (orange) versus RH (light-blue). Plots are split by age subgroups (younger/older). The AUC is the area under the receiver operating curve. The red and dark-blue boxes, and corresponding text color below each plot, highlight the subgroups compared for each metric. a The high Subgroup AUCs show that the predicted risk for individuals experiencing CSD was greater than the predicted risk for relatively healthy (RH) individuals within both age subgroups. But, this AI tool was biased to predict higher risk for younger individuals, overall, than older individuals. This bias is quantified using the ( b ) Background-Negative-Subgroup-Positive (BNSP) AUC and ( c ) Background-Positive-Subgroup-Negative (BPSN) AUC, which respectively show that younger individuals with CSD (“positive samples”) were correctly ranked higher (high BNSP) than RH (“negative samples”) samples from all other subgroups (older individuals, the “background”), but RH younger individuals were incorrectly ranked higher (low BPSN) than background samples with CSD. Older individuals show the complementary result (low BNSP, high BPSN). This bias reduces the model AUC when measured across the entire sample (assuming equal number of older and younger individuals, AUC = 0.75), compared to the AUC in each subgroup (1.00).
The highest performing AI model (a random forest, 100 trees, max depth of 10, balanced class weights, see methods) achieved a median (95% confidence interval, CI) AUC of 0.55 (0.54 to 0.57) across trials. Note that this low AUC was expected: it is comparable to the cross-validation performance of similar depression symptom prediction tools developed in larger, more diverse populations 4 , 6 , 13 , and motivates the objective of this work to study the reliability of these tools in larger populations.
Figure 3 shows the model results by each metric across subgroups. The Subgroup AUC was lower for males (median, 95% CI 0.52, 0.49 to 0.55), Black/African Americans (0.50, 0.46 to 0.54), individuals from low income families (<$ 20,000, 0.46, 0.43 to 0.50), uninsured (0.45, 0.41 to 0.51), and unemployed (0.46, 0.42 to 0.50) individuals, compared to the median subgroup AUC for each attribute (e.g. “Sex at Birth”) across trials. The BNSP AUC increased with age (from 0.50, 0.46 to 0.52 for 18 to 25 year olds, to 0.67, 0.62 to 0.73 for 65 to 74 year olds), but decreased with family income (from 0.60, 0.58 to 0.63 for individuals from <$ 20,000 income families, to 0.45, 0.42 to 0.48 for individuals from $ 100,000+ income families). Individuals who were White (0.49, 0.46 to 0.52), male (0.52, 0.49 to 0.55), insured (0.47, 0.43 to 0.50), employed (0.43, 0.41 to 0.45), or identified with an “Other” type of employment (0.55, 0.52 to 0.59) also had lower BNSP AUC, compared to the median BNSP AUC for each attribute.
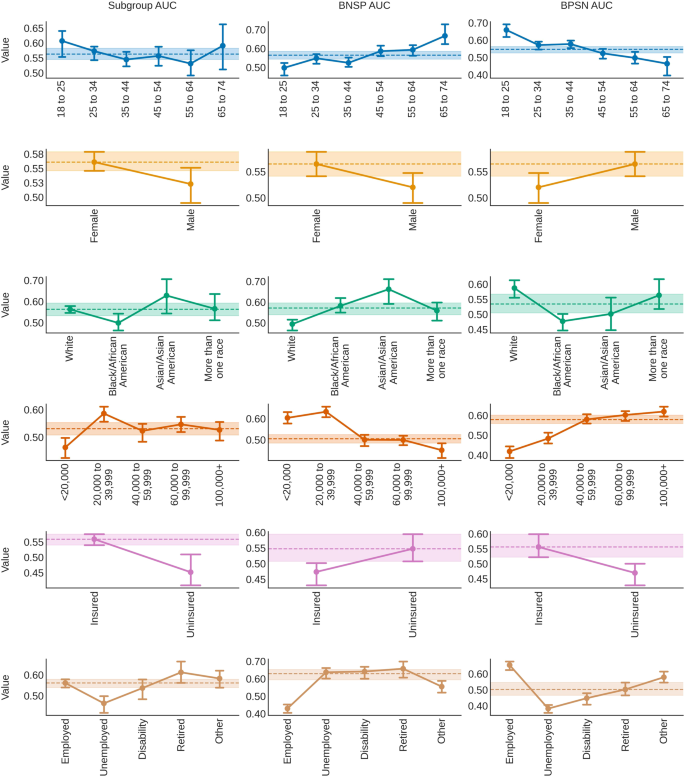
Bias was assessed by measuring the area under the receiver operating curve comparing positive (clinically-significant depression, CSD) and negative (relatively healthy, RH) samples within subgroups (Subgroup AUC, left column), subgroup positive samples to negative samples from all other subgroups, called “the background” (background-negative-subgroup-positive, or BNSP AUC, middle column), and subgroup negative samples to background positive samples (background-positive-subgroup-negative, or BPSN AUC, right column) 20 , 22 . Point values indicate the median value across trials. Error bars show 95% confidence intervals (2.5 and 97.5 percentiles). Dotted lines and shaded areas show the distribution (median and 95% confidence intervals) of either the median (if >2 subgroups) or highest performing subgroups across trials.
The BPSN AUC findings showed complementary trends: RH older individuals (e.g. 65 to 74, 0.46, 0.40 to 0.50), unemployed (0.38, 0.36 to 0.41), uninsured (0.47, 0.43 to 0.50), Black/African American (0.48, 0.45 to 0.50), females (0.52, 0.49 to 0.55), and individuals coming from lower income families (e.g. <$ 20,000 0.42, 0.39 to 0.44) had a lower BPSN AUC. Results were reasonably consistent across different types of models, within subgroup base rates (% samples with PHQ-8 ≥ 10) were sometimes, but not always, associated with the BNSP/BPSN AUC, and subgroup sample size did not appear to be associated with the Subgroup AUC (see supplementary materials).
Isolating the effects of subgroup membership
We wished to account for intersectional identities (e.g. female and employed) and isolate the effect of subgroup membership on model underperformance. For an ideal classifier, the predicted risk would be low for RH subgroups, and high for CSD subgroups. In addition, we would expect subgroups with higher base rates (% of samples with PHQ-8 ≥ 10) to have a higher average predicted risk. We thus modeled expected differences from subgroups with either the lowest (for RH) or highest (for CSD) average risk across trials. Generalized estimating equations (GEE, exchangeable correlation structure) 40 , a type of linear regression, was used to estimate the average effect of subgroup membership on the predicted risk after controlling across all other attributes. GEE was used instead of linear regression to correct for the non-independence of repeated samples across trials 40 .
The regression results can be found in Fig. 4 . The RH individuals with the lowest average predicted risk were 18 to 25 years old, male, White, had a family income of $ 100,000 + , were insured, and employed. The predicted risk was expected to be higher than these subgroups (95% CI lower-bound >0) for RH individuals who were older than 34 (e.g. for 65 to 74 year olds, mean, 95% confidence interval 0.02, 0.01 to 0.04), identified as Asian/Asian American (0.02, 0.01 to 0.03), Black/African American (0.01, 0.00 to 0.01), came from <$ 60,000 income families (e.g. for <$ 20,000, 0.02, 0.01 to 0.03), were unemployed (0.03, 0.03 to 0.04), and/or on disability (0.01, 0.00 to 0.02).
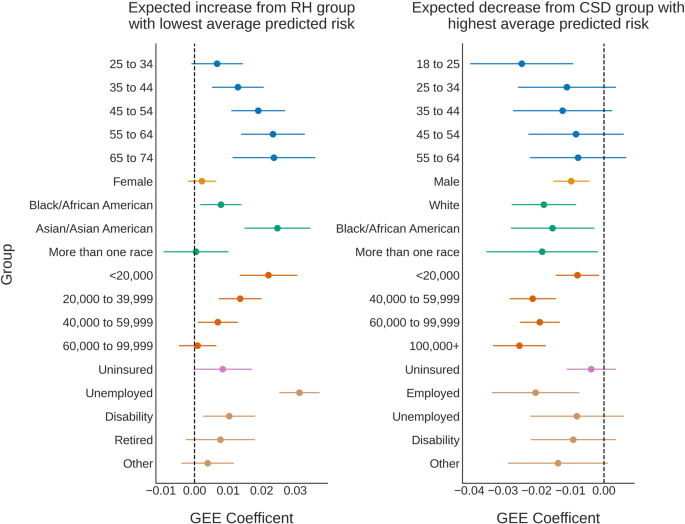
For an ideal classifier, the predicted risk would be low for relatively healthy (RH) individuals, and high for individuals with clinically-significant depression (CSD). We thus modeled expected differences from the subgroups with either the lowest (for RH, left) or highest (for CSD, right) average predicted risk across trials. Subgroup effects were calculated using generalized estimating equations (GEE) 40 , a type of linear model, to analyze the average effect of subgroup membership on the predicted risk, controlling across all attributes. GEE accounted for the non-independence of repeated samples across trials 40 . Separate regression models were created for each outcome (RH, CSD) to remove the effects of the subgroup base rate. Points represent the GEE coefficient (expected effect), and error bars are 95% confidence intervals around the estimated effect. Dotted vertical lines highlight an expected subgroup effect of 0.
For individuals who were experiencing CSD, models predicted the highest average risk for 65 to 74 year olds, Females, Asian/Asian Americans, individuals who came from families with incomes of $ 20,000 to $ 39,999, were insured, and/or retired. The predicted risk for individuals experiencing CSD was expected to be lower (95% CI upper-bound <0) if individuals were 18 to 25 (–0.02, –0.04 to –0.01), male (–0.01, –0.02 to –0.00), Black/African American (–0.02, –0.03 to –0.00), more than one race (–0.02, –0.03 to –0.00), White (–0.02, –0.03 to –0.01), came from any family with an annual income <$ 20,000 or ≥$ 40,000 (e.g. $100,000+ –0.03, –0.03 to –0.02), and/or were employed (–0.02, –0.03 to –0.01). Predicted risk distributions often overlapped across subgroups with higher or lower risk, though there were general trends across subgroups (e.g. the predicted risk increased with age and unemployment in RH individuals, and risk decreased with income level for both CSD and RH individuals, see Fig. 4 for more details).
Interpreting sensed-behaviors
We hypothesized that models underperformed because sensed-behaviors predictive of CSD were inconsistent across subgroups. We thus conducted an analysis to understand differences between how AI tools predicted CSD risk and the different relationships between sensed-behaviors and CSD across subgroups. First, we retrained the AI model on the entire data, and used Shapley additive explanations (SHAP) 41 to interpret how the AI tool predicted CSD risk from sensed-behaviors. We then compared SHAP values with coefficients from explanatory logistic regression models estimating how subgroup membership affected the relationship between each sensed-behavior and depression.
We found different relationships between the SHAP values (Fig. 5a ) and sensed-behaviors associated with CSD across subgroups (Fig. 5b , comparisons across each attribute and feature can be found in the supplementary materials). For example, the AI tool predicted that higher morning phone usage (6–12PM) was generally associated with lower predicted depression risk. Higher morning phone usage decreased depression risk for 18 to 25 year olds (mean, 95% CI effect on depression, standardized units: –0.77, –1.07 to –0.47), but increased risk for 65 to 74 year olds (0.60, 0.07 to 1.12). Younger individuals, overall, also had higher morning phone use (standardized median, 95% CI 18 to 25 year olds: 0.32, –2.27 to 1.60) compared to older individuals (65 to 74 year olds: –0.62, –1.96 to 0.76).
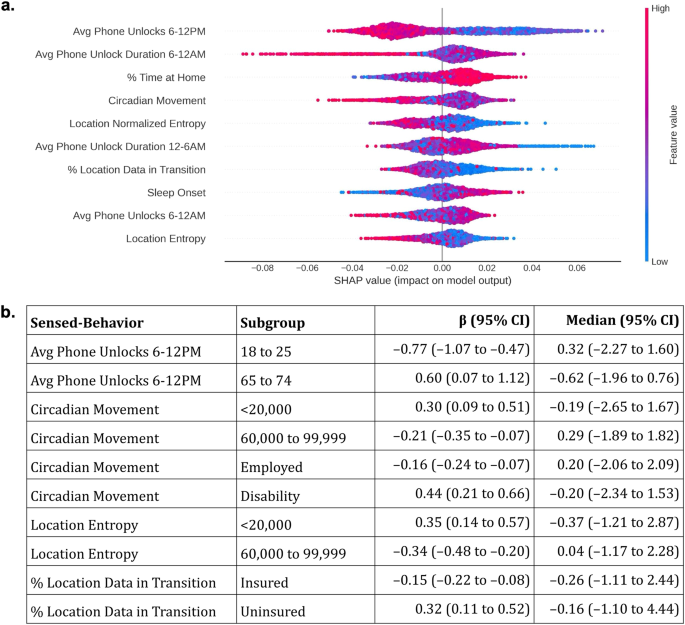
a Shapley additive explanations (SHAP) 41 were used to interpret how the AI tool predicted depression risk using sensed-behaviors. Sensed-behaviors are ordered, descending, on the y -axis by their average impact on the predicted risk (the “SHAP value”, x -axis). Only the top 10 sensed-behaviors with the highest average impact are listed, for space. Colors dictate whether a higher sensed-behavior “feature” value (red) is associated with higher or lower predicted risk. For example, higher average (“Avg”) phone unlocks from 6–12 PM were generally associated with lower predicted risk. Averages and deviations summarize sensed-behaviors over 14 days (see Fig. 1c ). b Example coefficients (β, 95% CI, standardized units) from explanatory logistic regression models estimating the associations between sensed-behaviors and depression across subgroups, as well as the median and 95% CI of the sensed-behavior distribution. Full coefficients and statistics can be found in the supplementary materials.
Figure 5a also shows that specific mobility features, including the circadian movement (regularity in 24 hour movement), location entropy (regularity in travel to unique locations), and the percentage of collected GPS samples in transition (approximated speed >1 km/h) were often associated with lower predicted CSD risk. Circadian movement decreased CSD risk for employed individuals (–0.16, –0.24 to –0.07), but increased CSD risk for individuals who were on disability (0.44, 0.21 to 0.66). Circadian movement and location entropy also decreased depression risk for individuals from middle income ($ 60,000 to $ 99,999) families (circadian movement: –0.21, –0.35 to –0.07; location entropy: –0.34, –0.48 to –0.20), but increased risk for individuals from low income (<$ 20,000) families (circadian movement: 0.30, 0.09 to 0.51; location entropy: 0.35, 0.14 to 0.57). Finally, a higher percentage of GPS samples in transition decreased depression risk for insured individuals (–0.15, –0.22 to –0.08), but increased risk for uninsured individuals (0.32, 0.11 to 0.52).
In this study, we hypothesized that sensed-behaviors are unreliable measures of depression in larger populations, reducing the accuracy of AI tools that use sensed-behaviors to predict depression risk. To test this hypothesis, we developed an AI tool that predicted clinically-significant depression (CSD) from sensed-behaviors and measured algorithmic bias to identify specific age, race, sex at birth, and socioeconomic subgroups where the tool underperformed. We then found differences between SHAP values estimating how the AI tool predicted CSD from sensed-behaviors, and explanatory logistic regression models estimating the associations between sensed-behaviors and CSD across subgroups. In this discussion, we show how differences in sensed-behaviors across subgroups may explain the identified bias and AI underperformance in larger, more diverse populations.
Measuring bias showed that models predicted older, female, Black/African American, low income, unemployed, and individuals on disability were at higher risk of experiencing CSD (high BNSP, low BPSN AUC), and younger, male, White, high income, insured, and employed individuals were at lower risk of experiencing CSD (high BPSN, low BNSP AUC), independent of outcomes. Comparing SHAP values to explanatory logistic regression coefficients suggests why AI models incorrectly predicted depression risk. For example, our findings show that younger individuals had higher daytime phone usage than older individuals. Models predicted that higher daytime phone usage was associated with lower CSD risk (Fig. 5a ), potentially explaining why younger individuals, overall, had lower predicted risk, and older adults had higher predicted risk (Fig. 3 ). Differences could be attributed to younger individuals using phones for entertainment and social activities that support well-being, while older individuals may prefer to use their phones for necessary communication or information gathering 23 .
In another example, the model predicted that mobility, measured through circadian movement, location entropy, and GPS samples in transition, was associated with lower CSD risk (see Fig. 5 ). Prior work has identified a negative association between these same mobility features and CSD 5 , 25 , suggesting that mobility decreases depression risk. While we found the expected negative associations across majority, higher SES ($ 60,000 to $ 99,999 family income, insured, and employed) subgroups, we found the opposite, positive association across less-represented lower SES (<$ 20,000 family income, on disability, uninsured) subgroups, potentially explaining the reduced model performance (lower Subgroup AUC) in these subgroups. There are many possible explanations for the identified differences in behavior. First, underlying reasons to be mobile (e.g. navigating bureaucracy to receive government payments) may increase stress for individuals who are lower income and/or on disability 31 , increasing depression risk. Second, the analyzed data was collected during the early-to-mid stages of the COVID-19 pandemic, when mobility for low SES essential workers may indicate work travel and increased COVID-19 risk, contributing to stress 32 and depression. These findings suggest that sensed-behaviors approximating phone use and mobility used to predict depression in prior work 3 , 4 , 5 , 6 , 25 do not reliably predict depression in larger populations because of subgroup differences.
While existing work developing similar AI tools has strived to achieve generalizability 4 , 42 , our findings question this goal. Instead, it may be more practical to improve reliability by developing models for specific, targeted populations 43 , 44 . In addition, it may be helpful to train AI models using both sensed-behaviors and demographic information. In prior work and this study, AI models were trained using exclusively sensed-behavioral data 3 , 4 , 5 , 17 . However, prior work suggests that models may not be more predictive even with added demographic information 45 . This shows that additional methods are needed to clearly define subgroups, beyond demographics, with more homogenous relationships between sensed-behaviors and depression symptoms.
Another method to improve reliability is to develop personalized models, trained on participants’ data over time 6 , 46 . While personalization seems appealing, researchers should ensure that personalized predictions are meaningful. For example, we experimented with personalized models using a procedure suggested from prior work 46 . The model AUC improved (0.68) compared to the presented results (0.55), but we achieved a higher AUC (>0.80) by developing a naive model re-predicting participants’ first self-reported PHQ-8 value for all future outcomes. Given at least one participant self-report is often needed for personalization, models should show greater accuracy than these naive benchmarks.
Even if accuracy improves, models can still be biased 19 , 37 , and it is important to consider the clinical and public health implications of using biased risk scores for depression screening. For example, more frequent exposure to stress 47 contributes to higher rates of depression in lower SES populations 48 , but overestimating depression risk for healthy low SES individuals allocates mental health resources away from other individuals who need care. Similar issues persist for underestimating depression risk. For example, models predicted lower risk for males experiencing depression compared to healthier females (see Fig. 3 ). Males are less likely to seek treatment for their mental health than females 49 , and AI tools underestimating male depression risk may further reduce the likelihood that males seek care. Uncovering these biases are important before algorithmic tools are used in clinical settings.
To reduce these harms, researchers can use methods described in this and other work 37 to identify subgroups where AI tools underperform by measuring bias. Resources could then be directed to develop new or retrain existing models for these subgroups. Simultaneously, clinical personnel using these tools can be trained to identify algorithmic bias and mitigate its effects 50 . In addition, depositing de-identified sensed-behavior and mental health outcomes data in research repositories could increase available data to analyze the reliability of AI tools 12 . Finally, our findings show the importance of developing AI tools using data from populations that have similar behavioral patterns to the populations where these tools will be deployed. More thorough reporting of model training data 51 , and monitoring AI tools in “silent mode”, in which predictions are made but not used for decision making 52 , could prevent AI tools developed in dissimilar populations from causing harm.
Finally, it is important to consider how the choice to classify depression symptom severity influenced our results, specifically choosing to predict binarized PHQ-8 values instead of raw PHQ-8 scores. Predicting binarized symptom scores is a fairly common practice in both the depression prediction literature 3 , 4 , 5 , 17 , as well as in the clinical AI literature, broadly 53 , 54 . This practice is motivated by an interest to use AI tools for near-continuous symptom monitoring, in which an action (e.g. follow-up by a care provider) is triggered at a specific elevated symptom threshold. This motivation may be difficult to realize if the field continues to use depression symptom scales as outcomes. As recent work shows, symptom scales do not produce categorical response distributions, with a clear decision boundary distinguishing individuals experiencing versus not experiencing symptoms 14 . Instead, responses tend to exist along a continuum 14 . It is also important to consider if subgroup differences affect the interpretation and self-reporting of depression symptom scales. Despite this consideration, prior work provides evidence that the PHQ-8 exhibits measurement invariance across demographic and socioeconomic subgroups 55 , 56 . Thus, it may be unlikely that the bias identified in this work was due to subgroup differences in self-reporting symptoms, but our findings could be partially attributed to the mistreatment of depression symptom scales as categorical in nature.
This work had limitations. First, we analyzed data from a single study, though the studied cohort was larger in size, geographic representation, and timespan compared to prior work. In addition, the study cohort was majority White, employed, and female, though we did not find that sample size was associated with classification accuracy. Only inter-individual variability was considered, not intra-individual variability, and thus these findings do not extend to longitudinal monitoring contexts, where changes in sensed-behaviors may indicate changes in depression risk. In addition, data was only analyzed from participants who provided complete outcomes data (participants who reported at least one PHQ-8 value during each of the 6 weekly reporting periods). Data was exclusively collected from individuals who owned Android devices, and only specific data types (GPS and phone usage) were analyzed. Only smartphone sensed-behaviors were analyzed, and data collected from other devices (e.g. wearables) and platforms (e.g. social media) were not analyzed. Finally, data collection took place from 2019–2021, when COVID-19 restrictions varied across the United States, which may influence our findings. Future work can examine if these results replicate over larger, more diverse cohorts, in both demographic and socioeconomic attributes, as well as the data collection devices and platforms. In addition, future work can explore if sensed-behaviors are reliable predictors of depression in longitudinal monitoring contexts, though recent work suggests that sensed-behaviors have low predictive power, even when used for longitudinal monitoring 25 .
In conclusion, we present one method to assess the reliability of AI tools that use sensed-behaviors to predict depression risk. Specifically we measured ranking bias in a developed AI tool to identify subgroups where the tool underperformed, and then we interpreted why models underperformed by comparing the AI tool to sensed-behaviors predictive of depression across subgroups. Researchers and practitioners developing AI-driven mental health monitoring tools using behavioral data should think critically about whether these tools are likely to generalize, and consider developing tailored solutions that are well-validated in specific, targeted populations.
In this work, we performed a secondary analysis of data collected during a U.S.-based National Institute of Mental Health (NIMH) funded study. The motivation for this study was to identify smartphone sensed-behavioral patterns predictive of depression symptoms 3 , 25 , 26 , 27 , 28 , 29 . Participants were recruited from across the United States using social media, online advertisements, and an internally maintained registry of individuals interested in participating in digital mental health research. Participants were also recruited through Focus Pointe Global, a national research panel. Focus Pointe Global merged with the Schlesinger Group during data collection.
Eligible participants lived in the United States, could read/write English, and owned an Android smartphone and data plan. In addition, eligible participants with at least moderate depression symptom severity based upon the Patient Health Questionnaire-8 (PHQ-8) ≥ 10 were intentionally oversampled to create a sample with elevated depression symptoms. Individuals were excluded from the study if they self-reported a diagnosis of bipolar disorder, any psychotic disorder, shared a smartphone with another individual, or were unwilling to share data. Eligible participants were asked to provide electronic informed consent after receiving a complete description of the study. Eligible participants had the option to not provide consent, and could withdraw from the study at any point.
Consented participants downloaded a study smartphone application 57 and completed a baseline assessment to self-report demographic and lifestyle information. The study application passively collected GPS location, sampled every 5 min, and smartphone interactions (screen unlock and time of unlock) for 16 weeks. Individuals completed depression symptom assessments every 3 weeks within the smartphone application (the PHQ-8 33 , 34 ). Data collection took place from 2019–2021, and all study procedures were approved by the Northwestern University Institutional Review Board (study #STU00205316).
Sensed-behavioral features
We calculated sensed-behavioral features from the collected smartphone data to predict depression risk. Following established methods from prior work 3 , 5 , 25 , we calculated GPS mobility features including the location variance (variability in GPS), number of unique locations, location entropy (variability in unique locations), normalized location entropy (entropy normalized by number of unique locations), duration of time spent at home, percentage of collected samples in-transition (participant moving at >1 km/h), and circadian movement (24 hour regularity in movement) 5 . We also calculated phone usage features from the screen unlock data 42 , including the duration of phone use and the number of screen unlocks each day and within four 6 hour periods (12–6 AM, 6–12 PM, 12–6 PM, 6–12 AM). Finally, we used a standard algorithm 42 , 58 to approximate daily sleep onset and duration from screen unlock data.
Depression symptom classification
The PHQ-8 asks participants to self-report depression symptoms that occurred during the past 2 weeks. Symptoms are reported from 0 (not experiencing the symptom) to 3 (frequently experiencing the symptom). Scores are summed and thresholded to classify severity, where summed scores of 10 or greater indicate a higher likelihood of experiencing a clinically-significant depression 33 . We thus followed prior work 5 , 25 to calculate sensed-behavioral features in the 2 week period up to and including each weekly PHQ-8 reporting period. Behavioral features were input into machine learning models to predict clinically-significant symptoms (PHQ-8 ≥ 10).
Data preprocessing
Screen unlock and sleep features were summarized to align with the PHQ-8 42 . The average and standard deviation of each daily and 6 hour epoch feature were calculated across the 2 week prediction period, and the number of days with daily phone use and within each 6 hour epoch were summed. GPS features were directly calculated over the 2 weeks. As recommended by Saeb et al. 5 , skewed features were log-transformed. Missing data was filled using multivariate imputation 59 and then standardized (mean = 0, standard deviation = 1) based upon each training dataset prior to being input into predictive models.
AI model training and validation
We trained machine learning models commonly used to predict mental health status from smartphone behavioral data including regularized (L2-norm) logistic regression (LR) 3 , 5 , support vector machines (SVM) 4 , 60 , and tree-based ensemble models including random forest (RF) and gradient boosting trees (GBT) 3 , 42 . We varied the strength of the LR and SVM regularization parameter (0.01, 0.1, 1.0), used a radial basis function SVM kernel, varied class balancing weights in the RF and SVM (unbalanced/balanced), varied the number of ensemble tree estimators (10, 100), depth (3, 10, or until pure), and the GBT learning rate (0.01, 0.1, 1.0) and loss (deviance and exponential). Non-logistic prediction models were calibrated using Platt scaling to approximately match the predicted risk to the proportion of individuals experiencing clinically-significant symptoms at each risk level 61 . Logistic regression models, as shown in prior work 61 , output calibrated probabilities. Models were implemented using the scikit-learn Python library 62 .
Multiple PHQ-8 surveys were administered each weekly reporting period (e.g. week 1, 4, 7, etc.). Survey scores in each reporting week were averaged to remove overlap between sensor and outcomes data. Data was analyzed from study participants who self-reported at least one PHQ-8 during each reporting week, resulting in 6 predictions per participant. Data from all other participants were removed (288 participants removed, 31% of 938 total, leaving 650 participants for analysis) to focus this analysis towards algorithmic bias due to subgroup differences rather than bias due to missing outcomes data.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Sensed-behavioral data cannot be made publicly available due to potentially identifying information (e.g. GPS location) that may compromise participant privacy. De-identified self-reported data (the PHQ-8) will be made available through the NIMH Data Archive.
Code availability
A repository for all code used for analysis can be found at the following link: https://github.com/dadler6/reliability_depression_ml .
Cai, A. et al. Trends In mental health care delivery by psychiatrists and nurse practitioners in medicare, 2011–19. Health Aff. (Millwood) 41 , 1222–1230 (2022).
Article PubMed Google Scholar
Mohr, D. C. et al. Banbury forum consensus statement on the path forward for digital mental health treatment. Psychiatr. Serv . 6 , 677–683 (2021).
Liu, T. et al. The relationship between text message sentiment and self-reported depression. J. Affect. Disord. 302 , 7–14 (2022).
Xu, X. et al. GLOBEM: Cross-dataset generalization of longitudinal human behavior modeling. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 6 , 190:1–190:34 (2023).
Google Scholar
Saeb, S. et al. Mobile phone sensor correlates of depressive symptom severity in daily-life behavior: an exploratory study. J. Med. Internet Res. 17 , e175 (2015).
Article PubMed PubMed Central Google Scholar
Meegahapola, L. et al. Generalization and personalization of mobile sensing-based mood inference models: an analysis of college students in eight countries. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 6 , 176:1–176:32 (2023).
Mohr, D. C., Shilton, K. & Hotopf, M. Digital phenotyping, behavioral sensing, or personal sensing: names and transparency in the digital age. Npj Digit. Med. 3 , 1–2 (2020).
Article Google Scholar
Lee, E. E. et al. Artificial intelligence for mental health care: clinical applications, barriers, facilitators and artificial isdom. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 6 , 856–864(2021).
Frank, E. et al. Personalized digital intervention for depression based on social rhythm principles adds significantly to outpatient treatment. Front. Digit. Health 4 , 870522 (2022).
Mitchell, A. J., Vaze, A. & Rao, S. Clinical diagnosis of depression in primary care: a meta-analysis. The Lancet. 374 , 609–619 (2009).
Wang, R. et al. Tracking depression dynamics in college students using mobile phone and wearable sensing. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2 , 43:1–43:26 (2018).
Adler, D. A. et al. A call for open data to develop mental health digital biomarkers. BJPsych. Open 8 , e58 (2022).
Müller, S. R. et al. Depression predictions from GPS-based mobility do not generalize well to large demographically heterogeneous samples. Sci. Rep. 11 , 14007 (2021).
Fried, E. I., Flake, J. K. & Robinaugh, D. J. Revisiting the theoretical and methodological foundations of depression measurement. Nat. Rev. Psychol . 1 , 358–368 (2022).
Beck, A. T. Reliability of psychiatric diagnoses: 1 a critique of systematic studies. Am. J. Psychiatry 119 , 210–216 (1962).
Jacobs, A. Z. & Wallach, H. Measurement and fairness. In Proc. 2021 ACM Conference on Fairness, Accountability, and Transparency 375–385 (ACM, 2021).
Jacobson, N. C., Weingarden, H. & Wilhelm, S. Digital biomarkers of mood disorders and symptom change. Npj Digit. Med. 2 , 1–3 (2019).
Boateng, G. O., Neilands, T. B., Frongillo, E. A., Melgar-Quiñonez, H. R. & Young, S. L. Best practices for developing and validating scales for health, social and behavioral research: a primer. Front. Public Health 6 , 149 (2018).
Obermeyer, Z., Powers, B., Vogeli, C. & Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 366 , 447–453 (2019).
Article CAS PubMed Google Scholar
Borkan, D., Dixon, L., Sorensen, J., Thain, N. & Vasserman, L. Nuanced Metrics for Measuring Unintended Bias with Real Data for Text Classification. In Companion Proceedings of The 2019 World Wide Web Conference 491–500 (ACM, 2019).
Kallus, N. & Zhou, A. The Fairness of Risk Scores Beyond Classification: Bipartite Ranking and the XAUC Metric. In Advances in Neural Information Processing Systems vol. 32 (Curran Associates, Inc., 2019).
Vogel, R., Bellet, A. & Clémençon, S. Learning fair scoring functions: bipartite ranking under ROC-based fairness constraints. In Proc. The 24th International Conference on Artificial Intelligence and Statistics 784–792 (PMLR, 2021).
Andone, I. et al. How age and gender affect smartphone usage. In Proc. 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct 9–12 (ACM, 2016).
Horwood, S., Anglim, J. & Mallawaarachchi, S. R. Problematic smartphone use in a large nationally representative sample: Age, reporting biases, and technology concerns. Comput. Hum. Behav. 122 , 106848 (2021).
Meyerhoff, J. et al. Evaluation of changes in depression, anxiety, and social anxiety using smartphone sensor features: longitudinal cohort study. J. Med. Internet Res. 23 , e22844 (2021).
Mohr, D. C. LifeSense: Transforming Behavioral Assessment of Depression Using Personal Sensing Technology . https://reporter.nih.gov/search/N6YCr94ZvkOVUNu1i5HNaQ/project-details/9982127 (2017).
Stamatis, C. A. et al. Prospective associations of text-message-based sentiment with symptoms of depression, generalized anxiety, and social anxiety. Depress. Anxiety 39 , 794–804 (2022).
Meyerhoff, J. et al. Analyzing text message linguistic features: do people with depression communicate differently with their close and non-close contacts. Behav. Res. Ther. 166 , 104342 (2023).
Stamatis, C. A. et al. The association of language style matching in text messages with mood and anxiety symptoms. Procedia Comput. Sci. 206 , 151–161 (2022).
Greissl, S. et al. Is unemployment associated with inefficient sleep habits a cohort study using objective sleep measurements. J. Sleep Res. 31 , e13516 (2022).
Iezzoni, L. I., McCarthy, E. P., Davis, R. B. & Siebens, H. Mobility difficulties are not only a problem of old age. J. Gen. Intern. Med. 16 , 235–243 (2001).
Article CAS PubMed PubMed Central Google Scholar
Levy, B. L., Vachuska, K., Subramanian, S. V. & Sampson, R. J. Neighborhood socioeconomic inequality based on everyday mobility predicts COVID-19 infection in San Francisco, Seattle and Wisconsin. Sci. Adv. 8 , eabl3825 (2022).
Kroenke, K. et al. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 114 , 163–173 (2009).
Wu, Y. et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: a systematic review and individual participant data meta-analysis. Psychol. Med. 50 , 1368–1380 (2020).
Opoku Asare, K. et al. Predicting depression from smartphone behavioral markers using machine learning methods, hyperparameter optimization and feature importance analysis: exploratory study. JMIR. MHealth UHealth. 9 , e26540 (2021).
Corponi, F. et al. Automated mood disorder symptoms monitoring from multivariate time-series sensory data: getting the full picture beyond a single number. medRXiv https://doi.org/10.1101/2023.03.25.23287744 (2023).
Seyyed-Kalantari, L., Zhang, H., McDermott, M. B. A., Chen, I. Y. & Ghassemi, M. Underdiagnosis bias of artificial intelligence algorithms applied to chest radiographs in under-served patient populations. Nat. Med. 27 , 2176–2182 (2021).
Aguilera, A., Schueller, S. & Leykin, Y. Daily mood ratings via text message as a proxy for clinic based depression assessment. J. Affect. Disord. 175 , 471–474 (2015).
Horwitz, A. G., Zhao, Z. & Sen, S. Peak-end bias in retrospective recall of depressive symptoms on the PHQ-9. Psychol. Assess. 35 , 378–381 (2023).
Ballinger, G. A. Using generalized estimating equations for longitudinal data analysis. Organ. Res. Methods 7 , 127–150 (2004).
Lundberg, S. M. & Lee, S.-I. A unified approach to interpreting model predictions. arXiv https://doi.org/10.48550/arXiv.1705.07874 (2017).
Adler, D. A., Wang, F., Mohr, D. C. & Choudhury, T. Machine learning for passive mental health symptom prediction: Generalization across different longitudinal mobile sensing studies. PLoS One 17 , e0266516 (2022).
Sperrin, M., Riley, R. D., Collins, G. S. & Martin, G. P. Targeted validation: validating clinical prediction models in their intended population and setting. Diagn. Progn. Res. 6 , 24 (2022).
Mitchell, M. et al. Model cards for model reporting. arXiv https://doi.org/10.48550/arXiv.1810.03993 (2019).
Pratap, A. et al. The accuracy of passive phone sensors in predicting daily mood. Depress. Anxiety 36 , 72–81 (2019).
Wang, R. et al. CrossCheck: toward passive sensing and detection of mental health changes in people with schizophrenia. In Proc. 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing 886–897 (ACM, 2016).
Williams, D. R., Mohammed, S. A., Leavell, J. & Collins, C. Race, socioeconomic status and health: complexities, ongoing challenges and research opportunities. Ann. N. Y. Acad. Sci. 1186 , 69–101 (2010).
Everson, S. A., Maty, S. C., Lynch, J. W. & Kaplan, G. A. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity and diabetes. J. Psychosom. Res. 53 , 891–895 (2002).
Chatmon, B. N. Males and mental health stigma. Am. J. Mens Health 14 , 1557988320949322 (2020).
Rajkomar, A., Hardt, M., Howell, M. D., Corrado, G. & Chin, M. H. Ensuring fairness in machine learning to advance health equity. Ann. Intern. Med. 169 , 866–872 (2018).
Gebru, T. et al. Datasheets for datasets. arXiv https://doi.org/10.48550/arXiv.1803.09010 (2020).
Wiens, J. et al. Do no harm: a roadmap for responsible machine learning for health care. Nat. Med. 25 , 1337–1340 (2019).
Wong, A. et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern. Med. https://doi.org/10.1001/jamainternmed.2021.2626 (2021).
Adams, R. et al. Prospective, multi-site study of patient outcomes after implementation of the TREWS machine learning-based early warning system for sepsis. Nat. Med . 7 ,1455–1460 (2022).
Galenkamp, H., Stronks, K., Snijder, M. B. & Derks, E. M. Measurement invariance testing of the PHQ-9 in a multi-ethnic population in Europe: the HELIUS study. BMC Psychiatry. 17 , 349 (2017).
Villarreal-Zegarra, D., Copez-Lonzoy, A., Bernabé-Ortiz, A., Melendez-Torres, G. J. & Bazo-Alvarez, J. C. Valid group comparisons can be made with the patient health questionnaire (PHQ-9): a measurement invariance study across groups by demographic characteristics. PLoS One 14 , e0221717 (2019).
Audacious Software. Passive Data Kit . https://passivedatakit.org/ (2018).
Abdullah, S., Matthews, M., Murnane, E. L., Gay, G. & Choudhury, T. Towards circadian computing: ‘early to bed and early to rise’ makes some of us unhealthy and sleep deprived. In Proc. 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing 673–684 (ACM, 2014).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 45 , 1–67 (2011).
Tseng, V. W.-S. et al. Using behavioral rhythms and multi-task learning to predict fine-grained symptoms of schizophrenia. Sci. Rep. 10 , 15100 (2020).
Niculescu-Mizil, A. & Caruana, R. Predicting Good Probabilities With Supervised Learning. https://www.cs.cornell.edu/~alexn/papers/calibration.icml05.crc.rev3.pdf (2005).
Pedregosa, F. et al. Scikit-learn: Machine Learning in Python . https://www.jmlr.org/papers/v12/pedregosa11a.html (2018).
Download references
Acknowledgements
D.A. is supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-2139899, and a Digital Life Initiative Doctoral Fellowship. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. Data collection was supported by NIMH Grant No. R01MH111610 to D.C.M. J.M. is supported by K08MH128640. C.A.S. is supported by T32MH115882. Computing costs were funded by a Microsoft Azure Cloud Computing Grant through the Cornell Center for Data Science for Enterprise and Society, awarded to T.C. T.C. and F.W. were also supported by a multi-investigator seed grant awarded from the Cornell Academic Integration program.
Author information
Authors and affiliations.
Cornell Tech, Information Science, 2 W Loop Rd, New York, NY, 10044, USA
Daniel A. Adler, Gabriel J. Aranovich & Tanzeem Choudhury
Northwestern University Feinberg School of Medicine, Center for Behavioral Intervention Technologies, Chicago, IL, 60611, USA
Caitlin A. Stamatis, Jonah Meyerhoff & David C. Mohr
Weill Cornell Medicine, Population Health Sciences, New York, NY, 10065, USA
Michigan Medicine, Department of Psychiatry, Ann Arbor, MI, 48109, USA
You can also search for this author in PubMed Google Scholar
Contributions
D.A. conducted the analysis and wrote the draft manuscript. T.C., F.W., J.M., C.A.S. and D.C.M. provided supervisory support throughout the analysis. D.C.M. and J.M. were involved in data collection. All authors participated in drafting and revising the manuscript.
Corresponding author
Correspondence to Daniel A. Adler .
Ethics declarations
Competing interests.
D.A. and T.C. have submitted patent applications related to this work. T.C. is a co-founder and equity holder of HealthRhythms, Inc. and has received grants from Click Therapeutics related to digital therapeutics. D.C.M has accepted honoraria and consulting fees from Boehringer-Ingelheim, Otsuka Pharmaceuticals, Optum Behavioral Health, Centerstone Research Institute, and the One Mind Foundation, royalties from Oxford Press, and has an ownership interest in Adaptive Health, Inc. J.M. has accepted consulting fees from Boehringer Ingelheim. G.J.A. holds equity in HealthRhythms, Inc. and Lyra Health, Inc., and has accepted consulting fees and honoraria from BetterUp and Quantum Health.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Adler, D.A., Stamatis, C.A., Meyerhoff, J. et al. Measuring algorithmic bias to analyze the reliability of AI tools that predict depression risk using smartphone sensed-behavioral data. npj Mental Health Res 3 , 17 (2024). https://doi.org/10.1038/s44184-024-00057-y
Download citation
Received : 09 June 2023
Accepted : 07 February 2024
Published : 22 April 2024
DOI : https://doi.org/10.1038/s44184-024-00057-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
A study reported an interaction of significant life events with functional variation in the serotonin-transporter-linked polymorphic region (5-HTTLPR) allele type (in the context of multiple sclerosis) and linked this to depression , while another reported an interaction between stress and 5-HTTLPR in relation to depression . Other research ...
Studies of depression associated with physical conditions and specific subtypes of depression (e.g. bipolar depression) were excluded. ... with most research on depression focusing on the 5-HT 1A ...
Our lack of knowledge cannot be put down to a scarcity of research in existing treatments. In the past decades, more than 500 randomised trials have examined the effects of antidepressant medications, and more than 600 trials have examined the effects of psychotherapies for depression (although comparatively few are conducted for early-onset depression).
The current speed of progress in depression research is simply remarkable. We have therefore been able to create a second special issue of Molecular Psychiatry, 2020, focused on depression, with ...
The Effects of an Internet-based Cognitive Behavioral Therapy Program on Depression in Thai High School Students: A Quasiexperimental Study, Pacific Rim International Journal of Nursing Research ...
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2; range, 10-47%).Of these, the most widely used depression scales were the PHQ-9 (9 studies ...
Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community. In addition, depression can co-occur with other mental disorders or chronic illnesses, such as diabetes, cancer, heart disease, and chronic pain. ... Clinical trials are research studies that look at ways to prevent ...
To improve our understanding, some research has been undertaken in which YP themselves are asked about their experience of depression. In a questionnaire study involving adolescents with depression in New Zealand, the researchers identified the aforementioned irritability as the most common characteristic alongside interpersonal problems and ...
Depression is one of them, according to the latest research. In the largest-ever study of depression and inflammation, published in 2021 in the American Journal of Psychiatry, scientists confirmed ...
The BIO-K Study: A Single-Arm, Open-Label, Biomarker Development Clinical Trial of Ketamine for Non-Psychotic Unipolar Major Depression and Bipolar I or II Depression. Rochester, MN. The purpose of this research study is to find out if the medication known as ketamine can help the symptoms of depression.
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect ...
These research efforts have yielded important insights on multiple levels of description, linking depression with abnormalities in genes, neurotransmitter systems, neuroendocrine systems, functional and structural brain anatomy, and cognition. ... Functional imaging studies of patients with depression have examined task-related and resting ...
We also looked at research that explored whether depression can be induced in volunteers by artificially lowering levels of serotonin. Two systematic reviews from 2006 and 2007 and a sample of the ten most recent studies (at the time the current research was conducted) found that lowering serotonin did not produce depression in hundreds of ...
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this ...
Its severe form, major depression is classified as a mood disorder. Latest Research and Reviews Measuring algorithmic bias to analyze the reliability of AI tools that predict depression risk using ...
The main goals of this study are to learn how safe the study drug is and how well the study drug works when taken with the antidepressants you are currently taking for MDD. To find out if this study is a good fit for you, please fill out our online survey, call (650) 723-8330, or email [email protected].
Depressive disorder (also known as depression) is a common mental disorder. It involves a depressed mood or loss of pleasure or interest in activities for long periods of time. Depression is different from regular mood changes and feelings about everyday life. It can affect all aspects of life, including relationships with family, friends and ...
Background: Depression is often accompanied by changes in behavior, including dietary behaviors. The relationship between dietary behaviors and depression has been widely studied, yet previous research has relied on self-reported data which is subject to recall bias. Electronic device-based behavioral monitoring offers the potential for objective, real-time data collection of a large amount ...
A recent study published in the journal PLOS ONE links the relationship between the therapist and the study participant participating in psychedelic-assisted therapy with reducing depression for up to one year. Researchers analyzed data from a 2021 clinical trial that found psilocybin (magic mushrooms) combined with psychotherapy in adults was effective at treating major depressive disorder.
Funding for this research was provided by National Institutes of Health grants MH-092443, MH-094268, K99MH-094408, MH-105660, MH-107730, DA-040127, and MH-116869; the Brain and Behavior Research Foundation (formerly the National Alliance for Research on Schizophrenia and Depression); and other sources. The study authors do not have financial or ...
Drug effects have dominated the national conversation about psychedelics for medical treatment, but a new study suggests that when it comes to reducing depression with psychedelic-assisted therapy, what matters most is a strong relationship between the therapist and study participant. Researchers analyzed data from a 2021 clinical trial that fou...
Data collection. We analyzed data from a U.S.-based, NIMH-funded study conducted from 2019-2021 to identify associations between behavioral data collected from smartphones and depression ...
Research has long shown that exercise reduces heart disease risk, but a new study finds the connection between the two may be a decrease in the brain's stress signals. CNN values your feedback 1.