
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Basic Fitness
What is my Body Mass Index (BMI)? How will it change over this semester?
There are ways to measure body fat percentage, such as skin fold tests or using BIA (Bioelectrical Impedance Analysis) device. Examples of a BIA device include a Tanita Scale or handheld device. Below is a tool to help you calculate your BMI and longer-term weight/health goals. BMI is calculated using only your height and weight. Keep in mind …
Since many of you are not growing anymore, BMI can be tricky. If you develop muscle and lose fat, you could still weigh more because muscle weighs more than fat. An increased weight, even if due to muscle, will increase your BMI. Thus, percent body fat becomes more important.
A Personal Challenge…
>Have your body index percentage measured at the start of the semester and see if it improves over a period of time. Ask your instructor about access to a handheld device.
Basic Physical Education Copyright © by user is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.

Share This Book
What Is BMI In Physical Education? Learn How To Calculate It And Why It Matters!
Physical Education is an essential subject that focuses on developing a student’s physical well-being and overall health through various activities. One of the important metrics used in Physical Education to assess a person’s health status is Body Mass Index (BMI). BMI measures the relationship between a person’s weight and height, which helps determine whether they are underweight, normal weight, overweight or obese.
BMI calculation is a simple process that requires only your weight and height measurement. Once you have calculated your BMI, it can provide insights into potential health problems, such as high blood pressure, type 2 diabetes and heart disease, amongst others. This information can be especially relevant in a Physical Education context where active living habits are encouraged to prevent these chronic diseases.
In general, a healthy BMI falls within a specific range for individuals based on age, gender and other factors. However, there are limitations to this metric, and it should be seen as one tool in conjunction with other indicators when evaluating an individual’s overall health. It is also important to consider personal circumstances in combination with BMI results; for example, some athletes may have a higher BMI due to increased muscle mass while still being extremely fit and healthy.
The purpose of this article is to give readers an overview of what BMI is, how to calculate it, why it matters in Physical Education and exercise science, and its limitations. Further exploration about the topic could lead students to understand better their health and approach training and nutritional goals more effectively.
What Is BMI?
Definition of bmi.
BMI is an acronym for Body Mass Index, which is a measurement used to determine if a person’s weight is appropriate for their height.
The National Institutes of Health defines BMI as “a measure of body fat based on height and weight that applies to adult men and women.” BMI is calculated by dividing your weight in kilograms by the square of your height in meters.
BMI gives an estimate of the amount of body fat, but does not directly measure it. So, BMI measurements can help you monitor changes over time or compare how you stack up against other people in terms of body size.
Importance of BMI
BMI is important because it helps health care professionals assess whether or not someone is underweight, overweight, obese, or within a healthy weight range for their height.
Being underweight or overweight can have negative impacts on physical health, such as increased risk of heart disease, diabetes, and certain types of cancer. Therefore, maintaining a healthy weight through proper diet and exercise is essential for overall wellness.
History of BMI
BMI was invented more than 150 years ago by Adolphe Quetelet, a Belgian mathematician and statistician who developed the concept of “social physics” – the idea that social phenomena could be studied using mathematical principles.
In Quetelet’s formulation BMI corresponded minimally with actual levels of adiposity; BMI was disproportionately shifted toward muscularity among those highly muscled (e.g., athletes) and toward adiposity among those poorly muscled (e.g., elderly individuals).
In the WWI era scientists began to believe that being undernourished predisposed recruits to greater infectious disease risk and higher mortality observed in soldiers. In the WWII era, an obesity epidemic of sorts emerged due to rationing and then post-war affluence.
It wasn’t until around 1985 that BMI began to become popular as a surrogate measure for body composition in the U.S. The National Institutes of Health brought it into public consciousness at that point when they published guidelines on “acceptable” weight-for-height based on studies of Caucasian adults across varied populations decades before.
“BMI is not perfect but offers insight into how much overweight and obese individuals weigh.” -Dr. Scheer
How Is BMI Calculated?
BMI stands for Body Mass Index, which is a numerical value of a person’s weight in relation to their height. Essentially, it calculates the amount of body fat that someone has based on their weight and height. It was first introduced by a Belgian mathematician named Adolphe Quetelet in the early 19th century as an alternative to simply measuring weight. Today, it is widely used in the field of physical education, health, and nutrition.
Formula for BMI Calculation
The formula for calculating BMI involves dividing a person’s weight (in kilograms) by the square of their height (in meters). The resulting number is then classified into one of four categories: underweight, normal weight, overweight, or obese. A BMI between 18.5 and 24.9 is considered normal weight, while anything below or above those values falls within the other three categories.
“The formula for calculating BMI has been around for over 200 years, but it really gained popularity in the 1970s when researchers discovered its usefulness in predicting obesity-related diseases.” -Dr. David Katz
Units of Measurement for BMI
BMI can be calculated using either the metric system (kilograms and meters) or the imperial system (pounds and inches). However, the results will differ slightly depending on which unit of measurement is used. For this reason, it is important to be consistent with the units that you use when taking measurements and calculating BMI.
“BMI calculations are highly dependent on the units of measurement that are used. Be sure to double-check your units before doing any calculations.” -Dr. Sally Norton
Factors That Affect BMI Calculation
While BMI is generally accurate for most people, there are certain factors that can affect the accuracy of BMI calculations. For example, athletes and bodybuilders who have a lot of muscle mass may have a higher BMI than someone with the same weight and height who has more body fat. Additionally, age, gender, and ethnicity may also play a role in determining an accurate BMI measurement.
“BMI is just one tool that we use to measure overall health. It’s important to take into account other factors like muscle mass and lifestyle habits when analyzing someone’s risk for obesity-related diseases.” -Dr. David Katz
Interpretation of BMI Results
As mentioned earlier, BMI results are typically classified into one of four categories: underweight, normal weight, overweight, or obese. While these classifications can be helpful in identifying potential health risks, they should not be used as a definitive diagnosis. Other factors such as age, gender, family history, and personal health history should also be taken into account before making any significant dietary or lifestyle changes based on BMI results alone.
“BMI is a useful starting point for assessing health status, but it’s important to remember that it only tells us part of the story. We need to look at the whole person to fully understand their nutritional needs.” -Dr. Sally Norton
What Are The Different BMI Categories?
Underweight.
In physical education, Body Mass Index (BMI) is a measure of body fat based on height and weight. An individual with a BMI below 18.5 is considered underweight. Being underweight can result in health issues such as malnutrition, anemia, and weakened immune system. It can also lead to complications during surgery and longer hospital stays after procedures.
“Being underweight reduces your immune function and ability to fight off infections, making it more likely for you to get sick.” -Dr. Sherry Ross
Factors contributing to being underweight include genetics, high metabolism, eating disorders, chronic illnesses, stress, and hyperactivity.
Normal Weight
An individual with a BMI between 18.5 and 24.9 falls into the normal weight category. Normal weight individuals have lower risks of developing health issues such as heart disease, diabetes, and some types of cancer. They tend to have higher energy levels, good concentration, and better sleep patterns which can improve performance in physical activities.
“A healthy weight range is generally defined as a BMI of 18.5-24.9, so try to aim for that. Within this range, there are still differences in how much fat versus muscle people hold, so keep working out and eating well!” -Julia Belluz
Maintaining a normal weight requires consuming a balanced diet, engaging in regular physical activity or exercise, managing stress, avoiding tobacco and excessive alcohol intake, adequate sleep, and getting routine medical check-ups.
Why Is BMI Important in Physical Education?
BMI, also known as Body Mass Index, is a useful tool to determine if an individual has a healthy weight-to-height ratio. In physical education, BMI plays a crucial role in assessing the overall fitness and health of students.
BMI as a Tool for Fitness Assessment
BMI can be used by physical education teachers to assess the weight status of their students and identify those who are overweight or obese. By measuring height and weight and calculating BMI, teachers can have a better understanding of the student’s body composition and make recommendations based on their findings.
According to The National Institute of Diabetes and Digestive and Kidney Diseases, a BMI between 18.5-24.9 indicates a healthy weight, while a BMI of 25 or higher suggests that someone may be overweight or obese.
Physical educators should encourage their students to maintain a healthy BMI by engaging in regular exercise and adopting healthy eating habits. This includes aiming for at least 150 minutes of moderate-intensity aerobic activity each week, such as brisk walking or jogging. Additionally, strength exercises should be incorporated to help build muscle mass and increase metabolism.
BMI and Health Education
BMI is also an essential component of health education. Students must understand how to calculate their BMI and interpret its value so they can make informed decisions about their nutritional choices and lifestyle changes. It is vital to educate young adults on how obesity and being overweight can lead to various chronic diseases like diabetes, hypertension, and heart diseases.
The Centers for Disease Control and Prevention emphasizes the importance of educating children and adolescents about healthy eating habits and physical activity. They recommend creating supportive environments that positively influence healthy behaviors than using shame-based tactics alone to motivate change.
BMI and Goal Setting
BMI can be an effective tool for setting specific fitness and health goals. An individual’s BMI score provides a baseline measurement that helps them track their progress as they work to achieve a healthy weight.
“Specific, measurable, achievable, relevant, time-bound (SMART) goals are necessary when encouraging students to make lifestyle changes,” says Dr. Charles Platkin of Hunter College in New York City.
The SMART approach to goal-setting is highly recommended by experts in physical education because it provides clear objectives designed to improve the student’s overall health outcomes. Goals such as decreasing BMI by one point over a designated period or increasing 10 minutes of daily activity each week are considered realistic, achievable targets.
BMI plays a vital role in physical education classes since it is a helpful tool in determining a student’s body composition, weight status, and potential risk factors. It can also motivate young adults to adopt healthier lifestyles by providing essential information to set achievable goals through proper nutrition and consistent exercise regimens.
How Can BMI Be Used To Assess Health Risks?
Correlation between bmi and health risks.
BMI stands for body mass index, which is a measure of body fat based on a person’s weight and height. BMI can be used as an indicator of health risks associated with carrying excess body fat. There is a direct correlation between BMI and various health risks such as heart disease, stroke, diabetes, high blood pressure, and some types of cancer.
The higher the BMI score, the greater the risk of developing these chronic diseases. According to the World Health Organization (WHO), a BMI score of 25 or above indicates overweight, while a score of 30 or above indicates obesity. Individuals who fall within these ranges should consult their physician and implement lifestyle changes to reduce their health risks.
“BMI is not without its limitations, but it remains one of the most widely used methods for assessing weight-related health risks.” – Harvard Health Publishing
BMI and Chronic Diseases
Excess body fat can have a negative impact on overall health and increase your risk of developing chronic diseases. Studies have found that obesity is associated with an increased risk of cardiovascular diseases, type II diabetes, hypertension, sleep apnea, osteoarthritis, and certain cancers such as breast, colon, and prostate cancer.
A study conducted by the National Institutes of Health(CDC) found that individuals with a BMI over 40 had a significantly greater risk of mortality from all causes than those with normal BMI scores. Obesity can add many more health issues including depression and joint pain making day-to-day activities difficult.
“There is no doubt in my mind that reducing obesity would lower healthcare costs.”- Lamar Alexander
Moreover, individuals with a BMI between 25 and 29.9 are classified as overweight, and they too are at a higher risk of developing chronic diseases. In addition to the health risks associated with carrying excess body fat, there is also a substantial economic burden associated with obesity-related healthcare costs.
It is critical to recognize that BMI serves as an indicator of overall health risks, but it should not be considered a diagnosis for any specific disease. A healthy lifestyle incorporating physical activity, good nutrition, and proper sleep hygiene is essential for maintaining optimal weight and reducing the risk of developing chronic diseases.
What Are Some Limitations Of BMI?
Does not distinguish between muscle and fat.
The Body Mass Index (BMI) is a commonly used method to measure the body fat through calorimetry. It measures the total weight of an individual in relation to their height, making it possible to classify them according to their degree of thinness or obesity.
One of the main limitations of BMI is that it does not distinguish between muscle mass and fat mass. This means that individuals who have a high amount of muscle mass can be classified as overweight or obese even if they are healthy and have a low percentage of body fat.
“BMI doesn’t account for your bone density, how much water you’re retaining, or other factors that influence your weight” – Christopher Wharton, PhD, MS
Does Not Account for Body Shape and Distribution of Fat
BMI also has a limitation in accounting for different body shapes and distribution of fat. For instance, someone with a pear-shaped figure may have more fat around their hips and thighs but less abdominal fat compared to an apple-shaped person, who tends to carry more fat around their midsection.
This distinction is important because research indicates that having excess visceral fat (fat around the organs) is associated with a higher risk of chronic diseases such as diabetes, heart disease, and stroke.
“While BMI is a useful tool when taken in context with many other indicators of health, single measurements of height and weight aren’t enough to diagnose someone as healthy or unhealthy” – Whitney English, R.D., CPT
Does Not Account for Age and Gender
BMI also lacks specificity for age and gender categories making its use limiting at best when analyzing body composition. As individuals age, the amount of lean mass in their body decreases while the amount of fat increases. This can result in a higher BMI score even if body fat has not increased.
In addition, men and women have different body compositions, with men typically having more muscle mass and bone density than women. This can lead to inaccuracies in BMI results when applied to both genders without specific adjustment factors.
“BMI is an important basic tool for assessing someone’s weight status, but it’s not as accurate or helpful on its own as many people think” – Christine Rosenbloom, PhD, RDN
Does Not Account for Ethnicity and Genetics
BMI may also present limitations with respect to ethnicity and genetics. Individuals from certain ethnic groups tend to have a higher incidence of obesity-related health concerns such as heart diseases and diabetes despite numbers that indicate smaller BMIs than individuals of other ethnicities.
This highlights the need for consideration beyond just the standardized BMI score, taking into account factors such as genetics and environment exposure during upbringing phases of life which greatly influence how good of a representation bmI will be for these individuals.
“It’s important to realize that although BMI provides some information about your health, other factors — including quality and quantity of calories consumed, lifestyle levels (caloric expenditure), blood pressure, and cholesterol levels — should always be considered in conjunction with BMI.” – Isabel Smith, MS, RD, CDN
Frequently Asked Questions
What does bmi stand for in physical education.
BMI stands for Body Mass Index, which is a measure of body fat based on height and weight. It is commonly used in physical education to assess a person’s health status and determine if they are underweight, normal weight, overweight, or obese.
How is BMI calculated?
BMI is calculated by dividing a person’s weight in kilograms by their height in meters squared. The formula is BMI = weight (kg) / height (m)². Alternatively, BMI can also be calculated using pounds and inches with the formula BMI = (weight (lbs) / height (in)²) x 703.
What is a healthy BMI range?
A healthy BMI range is typically considered to be between 18.5 and 24.9. A BMI below 18.5 is considered underweight, while a BMI between 25 and 29.9 is considered overweight. A BMI of 30 or higher is considered obese and can increase the risk of health problems such as heart disease, diabetes, and certain cancers.
Why is BMI important in physical education?
BMI is important in physical education because it can help identify potential health risks associated with being underweight, overweight, or obese. It can also be used to track changes in body composition over time and provide guidance for setting weight loss or weight gain goals. Additionally, BMI can be a useful tool for evaluating the effectiveness of physical education programs and interventions.
How can BMI affect an individual’s physical fitness and health?
BMI can affect an individual’s physical fitness and health in many ways. Being overweight or obese can increase the risk of chronic health conditions such as heart disease, diabetes, and certain cancers. It can also negatively impact physical fitness by reducing mobility, endurance, and strength. On the other hand, being underweight can also lead to health problems such as malnutrition and weakened immune function. Maintaining a healthy BMI range is important for overall health and well-being.
Privacy Overview
The Body Mass Index – BMI
The body mass index is also called the Quetelet index. It is a statistical measurement which compares an individual in weight and height. It is a handy tool to estimate a healthy body weight based on how tall an individual is accurate, and it is most widely used tool to identify the weight problem. 2 BMI is straightforward to measure and evaluate with the help of BMI. Its value is measured in kg/m2.
What is Body Mass Index – BMI?
- How do we find BMI?
- BMI in Hindi Medium
- Class 11 Physical Education
- Class 12 Physical Education
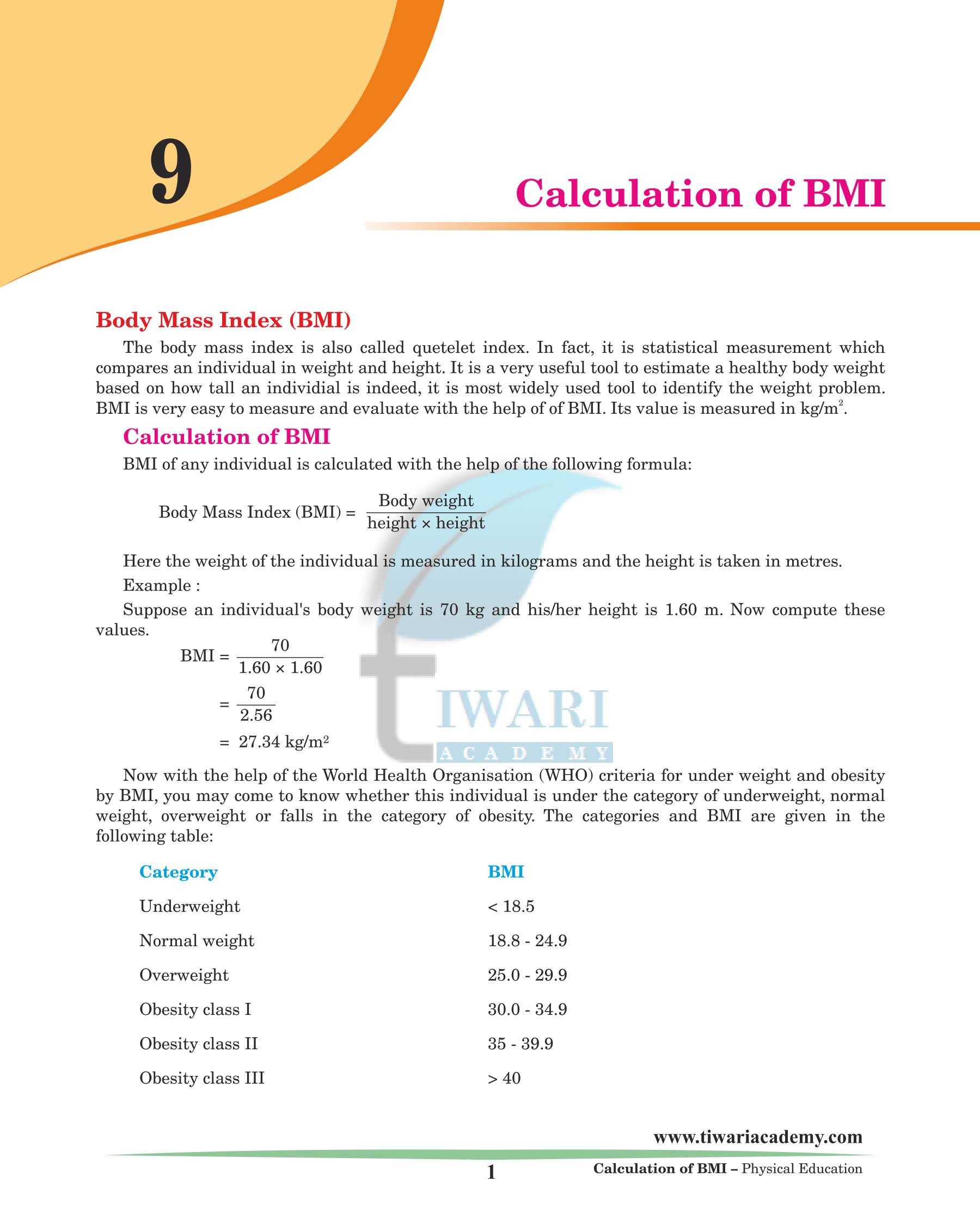
Now with the help of the World Health Organisation (WHO) criteria for underweight and obesity by BMI, you may come to know whether this individual is under the category of underweight, average weight, overweight or falls in the category of obesity.
BMI of any individual is calculated with the help of the following formula: Body Mass Index (BMI) = Body weight / (height × height) Here the weight of the individual is measured in kilograms and the height is taken in metres. Example: Suppose an individual’s body weight is 70 kg and his/her height is 1.60 m. Now compute these values. BMI = 70 / (1.60 x 1.60) = 70 / 2.56 = 27.34 kg/m2 Now with the help of the World Health Organisation (WHO) criteria for underweight and obesity by BMI, you may come to know whether this individual is under the category of underweight, normal weight, overweight or falls in the category of obesity.
The categories and BMI are given in the following table:
The following precautions must be taken while taking the measurements for BMI.
- The body weight must be taken on a reliable and perfect weighing machine.
- The student, whose body weight is to be taken, must wear minimum required clothes specially without shoes.
- During the measurement of height the student should be bare-footed and his/her complete body must be straight.
AAPHERD i.e. American Alliance for Health, Physical Education, Recreation and Dance is a test to judge and evaluate the fitness levels of youth. The first version of this test was published in 1958 and then revised in 1966 and after that in 1976. Many changes in the test battery were made in 1976 in AAPHER youth fitness test. This test is designed to test the fitness levels of the youth. The tests measure body composition, flexibility, agility, coordination, upper body strength, and aerobic endurance. The tests are designed so that they could be administered by professionals in the field.
Following are the test components of the AAPHERD physical fitness test:
- Pull ups (boys)
- Flexed-arm hang (girls)
- Flexed leg sit ups
- Shuttle run
- Standing broad jump
- 50-yard dash, 9 minute run for ages 10 to 12 years and 1.5 mile or 12 minute run for children age 13 & above.
In 1980 AAPHERD introduced the ‘Physical Best’ test which included the following items: 1. 1½ mile walk run or 12-minute run 2. Skin fold measurement body fat 3. Sit ups 4. Pull ups 5. Sit and reach test
The physical fitness test recognizes students for their level of physical fitness in the above events.
This event measures speed, quickness and agility of the students. Mark two parallel lines 30 feet apart and place two blocks of wood, behind one of the lines. Students start at the parallel line. On the signal ‘Go’ the student runs to the blocks picks one up, runs back to the starting line, places block behind the line, runs back and picks up the second block and runs back across starting line. Blocks should be placed within the lines.
Student hangs from a horizontal bar at a height the student can hang from, with arms fully extended and feet free from floor using either an overhand grip or under hand grip. Students with short height may be lifted to starting position. They raise body until chin clears the bar and then lower body to full hang starting position. Student performs as many correct pull ups as he can.
With an overhand grasp or underhand grip, student assumes flexed arm hang position with chin clearing the bar. Students may be lifted to this position. Student holds this position as long as he can.
Student’s chest should be held close to bar with legs hanging straight. Measurement of time is stopped when student’s chin touches or falls below the bar.
The standing long jump is a very common and easy test to administer test of explosive leg power. The student stands behind a line marked on the ground. With feet slightly apart. A two-foot take-off and landing is used with swinging of the arms and bending of the knees to provide forward drive. The student attempts to jump as far as possible, landing on both feet without falling backwards. Three attempts are allowed. The measurement is taken from take-off line to the nearest point of contact on landing the longest distance jumped in best of three attempts is recorded.
It is a test to measure the speed of the student. The student stands behind the starting line and starts running on the signal ‘Go’. As soon as the distance is covered the time taken to complete 50 yards is noted.
The new test of AAPHERD attempts to measure fitness of health:
Students are asked to run 1.5 mile. Their timings are taken by stop watch. If this method is not suitable then students are asked to run for 12 minutes. In this method their distance is noted down. The first method is considered to be the best method to know the cardiovascular fitness.
In this test calipers skin is used to measure the thickness of fat in various parts of the body After measuring the thickness of different parts of body, the measurements are put in an equation (different equation for girls and boys) to calculate the body density. After calculating body density, it is put in equation to calculate the body fat percentage. All the measurements must be done on the right side of the body. The following three parts are measured: (a) Abdominal skinfold (b) Chest skinfold (c) Arm skinfold
Equation for body density = 1.1017 – (0.000282) × (A) – (0.000736) × (B) – (0.000883) × (C) where A = Abdominal skinfold B = Chest skinfold C = Arm skinfold Equation for fat percentage Fat percentage = [4.570/Body Density – 4.142] x 100
The following two body parts are measured for women or girls A = Arm skinfold B = Skinfold
Body density = 1.0764 – (0.00081) × (A) – (0.000888) × (B), Where A = Arm skinfold, B = Skinfold
Fat percentage = [4.570/Body Density – 4.142] x 100
The sit-up test measures the maximum number of repetition that can be performed in one minute. The total number of repetitions are noted.
Copyright 2024 by Tiwari Academy | A step towards Free Education

Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Study Protocol
School health programs of physical education and/or diet among pupils of primary and secondary school levels I and II linked to body mass index: A systematic review protocol within the project From Science 2 School
Roles Methodology, Writing – original draft
* E-mail: [email protected]
Affiliations Department of Sport Science, Leopold-Franzens University of Innsbruck, Innsbruck, Austria, Department of Research and Development in Teacher Education, University College of Teacher Education Tyrol, Innsbruck, Austria
Roles Supervision, Writing – review & editing
Affiliation Department of Sport Science, Leopold-Franzens University of Innsbruck, Innsbruck, Austria
Affiliation Division of Physical Education, University of Education Upper Austria, Linz, Austria
Roles Writing – review & editing
Affiliation Sydney School of Education and Social Work, The University of Sydney, Sydney, Australia
Roles Resources, Writing – review & editing
Affiliation Institute of Primary Care, University of Zurich, Zurich, Switzerland
Roles Conceptualization, Methodology, Supervision, Writing – review & editing
Affiliations Department of Sport Science, Leopold-Franzens University of Innsbruck, Innsbruck, Austria, Department of Research and Development in Teacher Education, University College of Teacher Education Tyrol, Innsbruck, Austria, Health and Lifestyle Science Cluster Tirol, Subcluster Health/Medicine/Psychology, Tyrolean University Conference, Verbund West, Innsbruck, Austria, Research Center Medical Humanities, Leopold-Franzens University of Innsbruck, Innsbruck, Austria
- Derrick R. Tanous,
- Gerhard Ruedl,
- Werner Kirschner,
- Clemens Drenowatz,
- Joel Craddock,
- Thomas Rosemann,
- Katharina Wirnitzer

- Published: October 6, 2022
- https://doi.org/10.1371/journal.pone.0275012
- Peer Review
- Reader Comments
The most common causes of death in Western countries today are preventable diseases mainly attributed to daily behavior. It has been well documented that genetics are influential but not the deciding factor for developing non-communicable diseases. Ideally, the public should be educated to perform methods of optimal health and wellbeing independently, meaning that individuals should be in control of their health without relying on others. As behavior is known to be consistent over time, good or poor health behavior will track from childhood into adulthood. Physical activity and diet are permanently linked to the individual’s state of health, and when properly balanced, the effects on personal health summate, resulting in greater benefits from this dual-approach for public health. The objective is to highlight the different approaches (physical intervention, nutritional intervention, and dual-approach of diet and exercise) and identify effective interventions for sustainable body weight and healthy body mass index in school children. A systematic review will be conducted following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines. The review will assess school-based diet and exercise interventions on children in primary and secondary school levels I and II. Overweight and obesity develop as a result of a prolonged imbalance in the energy balance model, with both physical activity and diet being influential in the fluctuation of body weight. A dual-approach including physical activity and diet could therefore be a very promising method to promote sustainable healthy body weight in school children.
Citation: Tanous DR, Ruedl G, Kirschner W, Drenowatz C, Craddock J, Rosemann T, et al. (2022) School health programs of physical education and/or diet among pupils of primary and secondary school levels I and II linked to body mass index: A systematic review protocol within the project From Science 2 School . PLoS ONE 17(10): e0275012. https://doi.org/10.1371/journal.pone.0275012
Editor: Hans-Peter Kubis, Bangor University, UNITED KINGDOM
Received: August 9, 2021; Accepted: September 8, 2022; Published: October 6, 2022
Copyright: © 2022 Tanous et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: No datasets were generated or analysed during the current study. All relevant data from this study will be made available upon study completion.
Funding: This work was supported by the doctoral scholarship University of Innsbruck Vice Rector for Research for promoting young scientists (Author DT): No. 2020/2/PSY/SPORT-21. URL: https://www.uibk.ac.at/rektorenteam/forschung/index.html.en The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared no competing interests exist.
Introduction
The most common causes of death in Western countries are non-communicable diseases (NCDs), which can be mainly attributed to daily lifestyle behaviors [ 1 – 11 ]. Up to 71% of the world’s deaths per year (41 million) are caused by NCDs [ 12 ]. Developing the symptoms of NCDs is a slow process that occurs over decades and results in pain and suffering in the long-term for affected individuals and their families, with nine out of the ten leading causes for years lived with disability attributed to NCDs [ 13 ]. NCDs are widely known to be preventable, even at a low economic cost [ 1 – 3 , 6 , 7 , 9 , 12 , 14 ]. It has been well documented that genetics are influential but not the deciding factor for developing chronic (non-communicable) diseases [ 2 , 4 , 5 , 8 , 15 – 18 , 20 ].
Given the importance of behavior in preventing NCDs, health promotion through proper education on developing and maintaining personal health and wellbeing may be a feasible option to improve the burden of NCDs on nations [ 14 , 19 , 21 , 22 ]. Nevertheless, personal health behavior is just one of the determinants of health in addition to genetics, social circumstances, health care, and environmental factors [ 23 , 24 ].
To maximize personal health care, the public could be educated through competence-orientated health literacy to learn how to control one’s health independently before relying on others, such as commercial suppliers [ 25 ]. Two key environments where children grow up and develop their health behaviors are: (1) at home and (2) at school [ 26 ]. Schools provide a viable intervention setting, as they allow a large number and variety of children and adolescents to be reached independently of their socio-economic background [ 4 , 8 , 10 , 21 , 27 – 32 ]. School settings differ from clinical settings and are well controlled in terms of age groups (school levels), state educational mandate of national curricula, and standardized teacher education at tertiary level (such as University level, specialized University College of Teacher Education). Due to their educational efforts, schools influence lifestyle choices and contribute to developing lifelong health promotion and disease prevention [ 4 , 8 , 10 , 21 , 27 – 34 ].
Children and adolescents who are overweight or obese have an increased risk for developing chronic diseases over the lifespan [ 7 , 9 , 14 , 23 , 35 – 39 ]. Ruedl et al. 2018 concluded that “evidence-based preventative measures to decelerate the rise in body mass index (BMI) of primary school children should be implemented at the earliest” [ 40 ]. Overweight/obesity BMI classification is an indicator for excess body fat suggested by the World Health Organization and Centers for Disease Control and Prevention to classify children and adolescents (underweight, normal, overweight, obese 1–3) [ 39 , 41 – 43 ]. In addition to biological and genetic aspects, the BMI category is likely related to the individual’s physical activity (PA) level and diet [ 39 , 41 , 42 , 44 ]. According to the energy balance model, excess body fat results from consuming more calories per day than calories burned [ 45 ]. Therefore, increasing daily PA levels or making adjustments to diet composition can result in slowing, stopping, or reversing the accumulation of excess body fat [ 45 ].
There is strong scientific evidence of the beneficial effects of PA regarding the prevention of chronic disease [ 1 , 3 , 4 , 6 – 10 , 18 , 20 , 46 – 62 ]. Regular PA or physical exercise is not only the key to achieving optimal health but is considered as “medicine,” which no pill or supplement can replace [ 1 , 3 , 4 , 6 – 10 , 18 , 20 , 46 – 61 ]. Diet is another fundamental pillar in the development of optimal health and wellness [ 2 , 5 , 63 – 97 ], which can also function as a “medicine” for health but only if the diet is well-planned and balanced, containing mostly plant-based, whole foods [ 2 , 5 , 63 – 68 , 70 – 85 , 87 – 93 , 98 – 101 ]. The Academy of Nutrition and Dietetics stated in their position paper that appropriately planned vegetarian, including vegan, diets are healthful, nutritionally adequate, and may provide health benefits for the prevention and treatment of certain diseases and that these diets are appropriate for all stages of the life cycle (pregnancy, infancy, childhood, adulthood, and old age as well as for athletes) [ 85 ]. Moreover, studies have consistently shown that people eating plant-based (vegetarian, vegan) diets have healthier BMI on average compared to people eating a mixed (omnivorous) diet [ 65 – 67 , 70 , 102 , 103 ].
PA interventions, dietary interventions, and the dual-approach (permanent linkage or combination of PA and diet) have been implemented in the school setting to improve BMI and body weight (BW), as children and adolescents spend a great deal of time at school [ 4 , 10 , 18 , 27 , 40 , 46 , 47 , 104 – 111 ]. Although PA is known as an effective tool for improving personal fitness and shaping good health, PA interventions in schools have been shown to be insufficient to reverse overweight/obesity in the majority of pupils with the condition [ 47 , 104 , 106 , 108 , 112 ]. Participation in the compulsory subject of physical education (PE) at school is a well-studied and well-functioning opportunity to begin developing the behaviors that lead to a lifetime of PA [ 4 , 46 , 47 , 113 ]. However, PA is just one pillar of health, while diet displays another important pillar of health [ 1 , 3 , 6 , 7 , 9 , 10 , 25 , 80 , 114 – 120 ]. Moreover, school-based dietary interventions have also been shown to be inconsistent in reversing overweight/obesity in most pupils with the condition [ 10 , 28 – 31 , 112 ].
Considering overweight and obesity develops from an imbalance between energy intake and expenditure, it would be unlikely to stop, prevent, or reverse the condition by solely focusing on PA or diet [ 45 ]. The most promising approach appears to be an interaction of PA and diet as an effective solution for sustaining ideal BW [ 10 , 14 , 28 – 31 , 108 , 116 , 121 – 123 ]. PA permanently combined with diet is consistently linked to the individuals’ state of health, and when properly balanced, the effects on personal health summate, resulting in superior benefits from a “dual-approach” [ 2 , 10 , 14 , 28 – 31 , 47 , 63 – 65 , 67 , 108 , 121 , 123 , 124 ]. Achieving sustainable health in children and adolescents, at best, would target overweight/obesity with lifestyle factors that appear every day, naturally [ 23 ]. Lifestyle factors, such as physical activity level and diet, can improve health immediately for benefits that also carry over into adulthood and older adulthood and could pass on to following generations as well [ 19 , 25 ]. Considering the cumulative benefits to overall health, a dual-approach of PA with a plant-based diet appears most promising [ 1 , 3 , 6 , 7 , 9 , 10 , 25 , 28 – 31 , 39 , 114 , 115 , 117 – 120 , 125 ].
A large number of school-based interventions have targeted health behaviors, including diet and/or PA [ 10 , 28 – 31 , 108 , 112 , 126 – 139 ]. Based on our cumulative expertise, a variety of research on school-based PA interventions or dietary interventions exists. However, from the authors´ experience, the focus of plant-based dietary intervention is expected to be low. Future school-based health interventions should therefore consider investigating the PA and plant-based diet dual-approach. On an international scale, there has yet to be a compilation of interventions on PA, diet/diet type, and both for comparing the most effective strategies to improve BMI and/or BW in school pupils. This review aims to determine the best practice of PA, dietary, or combined PA and dietary intervention in primary and secondary school pupils for improving BMI and/or BW. Therefore, the primary objectives of this investigation are to assess: (i) whether compulsory (curriculum mandated) physical education (PE) is associated with BMI in school pupils; (ii) the minimum duration for compulsory PE to cause a change in BW or BMI in school pupils; (iii) whether additional PA, sports, or exercise intervention (beside compulsory PE) in the school setting is associated with a healthy BMI in pupils; (iv) whether there are differences in the efficacy of school-based physical exercise intervention versus diet intervention in promoting a healthy BMI in pupils. The secondary objectives of this investigation are based on sub-analyses regarding: (a) if the kind of dietary intervention* (Omnivorous: animal products; Whole Food Plant-Based: fruits, vegetables, legumes, and/or whole grains; Other: not related to diet type, e.g., soft drink) implemented in school programs is associated with a healthy BMI in pupils; (b) the long term (one year or more) association of interventional discipline (PA, diet, or dual-approach) with healthy sustainable BW management; (c) considering the dual-approach, whether there are differences in the efficacy of specific diet scheme types (omnivore vs. vegetarian vs. vegan; diet type definitions based on the Academy of Nutrition and Dietetics [ 85 ]) linked to PE for maintaining healthy BW.
Materials and methods
This protocol follows the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocol (PRISMA-P) guidelines [ 140 , 141 ].
Inclusion criteria (2.1)
Types of studies (2.1.1)..
We will include all types of randomized controlled trials (RCTs), including factorial, cluster, crossover, and parallel designs. As school settings clearly differ from clinical settings, we will also include non-randomized trials if none of the research questions can be addressed by available randomized controlled trials [ 142 ]. The following types of non-randomized trials will be included, if necessary: quasi-randomized controlled trials, controlled before-after studies, and follow-up studies such as inception cohort studies and non-randomized controlled trials.
Types of participants (2.1.2).
This review will consider all articles on human pupils aged 5–19 years only in primary school and secondary school levels I and II (or equivalent), with systematic review parts 1 (secondary schools) and 2 (primary schools) separated by school level. The subjects must have a stable or compensated medical condition without physical or cognitive disability (e.g., cannot follow all the amount and magnitude of lessons and exercises planned in PE lessons) and no prescribed medication. Unless results are separated, the following studies will be excluded as we cannot guarantee a bias-free result for these subjects (as they would likely add extreme values to the data): (i) studies addressing both pupils and adults (ii) studies with a whole school approach based on the inclusion aspect of people with disabilities unable to fully participate.
Types of intervention (2.1.3).
Interventions of focus must be only school-based and include those related to:
- PE–compulsory lessons as part of the curriculum (state mandate).
- PA–body movements produced by skeletal muscles that result in energy expenditure, not related to PE (e.g., brain/active break: allows bouts of in-class PA without education, or physically active lessons during the learning task at hand, unrelated to the lesson but occurs simultaneously) [ 143 ].
- Physical exercise–planned, structured, and repetitive sessions with a final or intermediate objective to improve or maintain physical fitness (physical fitness is a set of attributes that are either health- or skill-related) [ 143 ].
- Sports–related to the development of humans that require physical effort, skills (development of human capacities), a contest including a contract that is rule-governed, institutionalized, and parties have shared values and interests.
- Various combinations of (a)–(d).
- Dietary: aimed at regulating certain nutrition-related activities or actions that have an impact on food choices and health outcomes, which are not related to increasing BMI in anorexic or underweight youth (e.g. canteen-based, dietary supplement, soft drink reduction) [ 144 ].
- Dual-approach: combination of PA and dietary as one intervention.
Types of outcomes (2.1.4).
The main outcomes of interest include BMI and BW and must be calculated or measured by the testers, not self-reported. BMI is defined as body mass (BW) in kilograms divided by height in meters squared (kg/m 2 ), or by using imperial units with the equivalent calculation [ 39 , 41 , 42 ]. BMI percentile or Z-score will be accepted if BMI (kg/m 2 ) is not available.
The priority of outcomes includes BMI and BW because these measures are typically assessed in school health-related interventions, as they are cost-efficient, fast, and non-invasive. Moreover, BMI is likely related to the individuals’ PA level and diet, and BW is necessary to control for BMI.
Timing (2.1.5).
No restriction on years considered.
Language (2.1.6).
We will include articles reported in English or German language.
Exclusion criteria (2.1.7).
- Classes with an extraordinary pedagogical approach focusing on the needs of one or two pupils.
- Specialized school branches targeting physical exercise, sports in general, or a specific discipline of sport.
- Intervention groups targeting only overweight and/or obese pupils.
- Interventions outside of regular school hours.
- Multi-component interventions that are based on theoretical approaches–except in cases where PA and/or dietary is the predominant focus, and the intervention is only supplemented with additional health-related content.
- No comparator/no control group.
- No outcome on BMI or BW.
Information sources (2.2)
The following databases will be searched for articles published in English/German: PubMed, EMBASE, Education Source. Planned dates of completing the search include from October 2020 –December 2021.
To aid in the integrity of the search coverage, reference lists of included studies will be scanned as well as relevant reviews identified by the search. A bibliography of included articles will be sent to each member of the review team. PROSPERO (International Prospective Register of Systematic Reviews: https://www.crd.york.ac.uk/PROSPERO/ ) will be searched to identify similar reviews in progress as well as recently completed reviews to avoid review duplication.
Search Strategy (2.3)
Only quantitative, published studies will be sought. There will be no study design, date, or language restrictions included as part of the search. Although the databases may vary in the definition of a text word or standardized subject terms search (e.g., Medical Subject Headings [MeSH]), each database search will follow as closely as possible to that of the given PubMed Advanced search in Table 1 . To ensure the most accurate coverage of EMBASE, truncation will be used on singular key terms to remove all additional endings (e.g., plural forms) within the search (e.g., Pupil* instead of pupil OR pupils). The only limit used will be to exclude conference abstracts from the final hits of EMBASE. The specific search strategy will be created by the team, which includes expertise in sport science, nutrition science, and specialized statisticians, and peer-reviewed by the University of Innsbruck Library to assist in the structure of the search. Five columns: population 1, population 2, intervention, outcome, and study design will be used to include all related articles. The following steps will be used to search each database:
- all terms will be searched independently (e.g., “boy”) and combined with “or” for each column to create five separate search strings
- the columns will be combined into one search with “and” linking the five columns (all terms from Population 1 in one string “and” all terms from Population 2 in one string “and” all terms from Intervention in one string “and” all terms from Outcome in one string “and” all terms from Study design in one string).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0275012.t001
Study records (2.4)
All retrieved articles from each database will be transferred to Covidence (a systematic review management site: covidence.org ), and all hits will be shared with all authors. On Covidence, title/abstract and full-text screening will be performed by the two reviewers working independently with the protocol. Covidence will remove most duplicates of the same report. If there are any conflicts, the reviewers will solve these by discussion using an online audio application. If the conflict cannot be solved, a third reviewer will help make the final decision. Following the title/abstract screening, an included article will move to a full-text screening by two reviewers working independently for agreement with the eligibility criteria.
Assessment will be made of the author’s names, institutions, journal of publication, and results, and multiple reports of the same study will be linked. Contact with authors will be made by email or phone, if necessary, to identify missing information or clarifications for eligibility. Reasons for exclusion will be noted by both reviewers.
Data collection process (2.5)
Two reviewers will collect data extraction through standardized electronic data forms within Covidence (online) platform, and the results of the articles will be collected in MS Office Excel (Version 16.0.14131.20278). The second reviewer will check the outcome extracted to be sure of no missing information or errors in the outcome data collected.
The reviewers are both content area experts, and disagreements will be handled by a third reviewer. If important information cannot be found within the text, the study authors will be contacted by email or phone. Table 2 displays the data items that will be extracted.
https://doi.org/10.1371/journal.pone.0275012.t002
Risk of bias (2.6)
If necessary to include non-randomized study designs, the ROBINS-I tool will be used to assess the risk of bias in non-randomized studies as well as quasi-randomized trials and all of the included domains will be assessed for bias with no additional domains [ 145 , 146 ]. The bias domains include pre-intervention confounding bias, pre-intervention selection bias, at-intervention information bias, post-intervention confounding bias, post-intervention selection bias, post-intervention information bias, and post-intervention reporting bias [ 146 ].
Possible confounding domains include age, sex, BMI pre-intervention, BW pre-intervention, school level, school type, school policies on PA and diet, socioeconomic status, school environment, home environment, active transport, food availability, or baseline PA and dietary pattern.
Possible co-interventions include PA education sessions (without performing PA), health counseling unrelated to PA or diet (e.g. drug awareness), cognitive training, or other youth clubs unrelated to PA or diet (e.g. religious groups).
The Cochrane tool as a part of Covidence will be used to assess the risk of bias in randomized studies [ 147 ]. Two reviewers will assess included studies independently based on the following:
- Quality of allocation sequence generation
- Quality of treatment allocation concealment from study participants, clinicians, and other health care personnel from enrollment
- Appropriate blinding of the intervention allocation for team members assessing outcomes and data analysis during the trial
- Quality in the completeness of outcome data addressed in the published report for participant exclusions, attrition, and incomplete outcome data
- Quality of outcome reporting and if there exists evidence of selective outcome reporting which may have affected the study results
- Other possible trial problems that could cause a high risk of bias
We will include a description of the procedure for each domain of bias assessment for every study, including quotes when possible. For each domain, the judgment of the bias will be ranked as “high risk”, “low risk”, or “unclear”. Disagreements will be settled by discussion using an online audio application and, if necessary, a third reviewer. The reviewers will not be blinded to the studies, and agreement between reviewers will not be evaluated.
Data synthesis (2.7)
Data will be synthesized separately for randomized and non-randomized studies (if included). A descriptive summary of included studies will be incorporated into tables based upon the population (average age of participants), intervention (PA, dietary, combination), comparator (type of diet, active control, passive control), outcome (BW, BMI), and study design (PICOS structure). To answer our research questions and sub-analyses, data will be quantitatively synthesized by meta-analysis, if appropriate. For BW and BMI outcomes, the effect size of the interventions will be calculated using standardized mean difference or mean difference analyses (95% confidence intervals (95%-CI)) with a fixed- or random-effects meta-analysis (depending on the level of heterogeneity assessed by I 2 statistic or methodology). If important data (standard deviation, post-values, change scores, etc.) is not reported in the included articles, calculations will be performed from the available data (standard error, p-value, 95%- CI, etc.), or we will contact the authors. A narrative synthesis will also be performed to explore the relationship and findings both within and between the included studies for the research questions and sub-analyses.
Children and adolescents face significant health challenges today, and above all, two globally-scaled health issues of urgent concern have been identified by health experts who coined overweight/obesity as an „epidemic”and physical inactivity/insufficient levels of PA as a „crisis”[ 22 , 37 , 50 , 59 , 60 , 124 , 148 – 152 ]. Since children cannot achieve good health alone, they need support from adults to help them fulfill their potential and thrive [ 21 – 23 , 26 , 117 , 153 ]. Children are key to a nation’s present and future, considering their future roles in raising families and becoming decision- and policy-makers in different settings. Patterns of behavior and lifestyle are established during childhood and adolescence, affecting health for good or bad based on personal choices immediately and in the future [ 22 , 105 , 119 , 154 , 155 ]. Currently, poor health behavior and the direction of the development of poor health behavior are public health concerns [ 1 , 26 , 50 , 117 , 153 , 156 ].
According to the Global Burden of Disease Study, dietary risks account for 22% of all deaths among adults (≥ 25 years) in Western countries, with more than half of all diet-related deaths linked to low intakes of fruits and whole grains and the high intake of sodium [ 86 , 120 ]. The five highest-ranked risk factors of premature death worldwide include: (1) hypertension (13%), (2) tobacco use (9%), (3) high blood glucose (6%), (4) physical inactivity (6%), and (5) overweight/obesity (5%) [ 57 – 61 , 120 , 157 , 158 ]. Physical inactivity raises a serious concern because it also supports excess energy intake from unhealthy food products and items [ 45 , 50 , 53 , 58 , 159 ], but physical inactivity is not the only source of the NCD problem, as NCDs have been shown to develop in highly physically active people [ 160 ].
In addition, BMI is related to health, but a person having a BMI within the normal range can still develop other NCDs (e.g., heart disease, cancer, and/or type II diabetes) [ 1 , 35 , 36 ].
Healthy behavior is learned during childhood, and the window for adopting new healthy behaviors diminishes as people grow older [ 22 , 105 , 122 , 154 , 155 , 161 ]. There are tremendous benefits of living a healthy lifestyle, such as the reduced risk for developing NCDs like cancer, diabetes, and heart disease but also, increased lifespan with a decreased period of disabled years, especially at the end of life [ 3 , 48 , 82 , 117 , 155 , 162 , 163 ]. It is, therefore, crucial to teach children a healthy lifestyle as early as possible and offer healthy options in parallel [ 2 , 3 , 6 , 7 , 9 , 23 , 27 , 45 , 162 – 165 ]. Therefore, early intervention to prevent severe health conditions known to track over time from early childhood into adulthood is key [ 120 ].
Although PA is known as an effective tool for improving and shaping good health, PA interventions in schools have been shown to be insufficient to reverse overweight/obesity in the majority of pupils with the disease [ 47 , 104 , 106 ]. More appropriately, without the proper diet, the health benefits of PA are less pronounced [ 25 , 120 , 160 ]. Diet and PA are considered crucial in the fight against overweight/obesity [ 91 ], even in children [ 166 ], with plant-based diets considered particularly effective to fight overweight/obesity [ 70 , 91 , 102 , 103 , 120 , 166 – 170 ]. Moreover, information regarding current nutritional trends in children and adolescents (10–19) is limited [ 25 , 120 , 171 , 172 ]. To yield maximal health benefits alongside a proper health-promoting diet, PA raises the bar for health even further [ 1 , 3 , 6 , 7 , 9 , 10 , 25 , 108 , 114 , 115 , 117 – 120 , 125 , 173 ]. However, current PA opportunities during regular school hours through curricular PE lessons are limited, or even very low in many countries (up to 2 h per week) [ 57 , 59 , 60 , 174 ], mainly due to the primary time resource allocation to other equally major school subjects like Mathematics, English, and/or Science [ 175 – 177 ].
Diet is very important for health, but permanently linking it with PA, sports, and exercise as another lifestyle factor that is a well-known health tool as a minimum recommendation to achieve sustainable, lifelong health and wellbeing generally creates a permanent linkage from childhood to adulthood with greater cumulative lasting effects [ 6 , 7 , 25 , 94 , 111 , 114 , 115 , 117 , 122 , 155 ]. This review aims to determine the best practice of PA, dietary, or combined PA and dietary intervention in primary and secondary school pupils for improving BMI and/or BW.
Limitations (3.1)
As school settings are different from clinical settings, it is unknown whether non-randomized study designs will be included in order to address all of our research questions.
Strengths (3.2)
This protocol follows the PRISMA-P guidelines to peak the accuracy, transparency, frequency, and completeness of systematic review and meta-analysis methodology within the multidisciplinary field of sport science, nutrition science, pedagogy, and specialized statistics [ 140 , 141 ].
Amendments (3.3)
In the event of protocol amendments, the date of each amendment will be accompanied by a description of the change and the rationale.
Supporting information
S1 checklist..
https://doi.org/10.1371/journal.pone.0275012.s001
Acknowledgments
There are no professional relationships with companies or manufacturers who will benefit from the results of the present study.
- View Article
- Google Scholar
- 2. Campbell TC & Campbell TM II. The China study . Ashland, OR: Blackstone Audio; 2016.
- PubMed/NCBI
- 9. World Health Organization. Preventing noncommunicable diseases . Available at: https://www.who.int/activities/preventing-noncommunicable-diseases . [ accessed 19.01.2020].
- 11. The World Health Organization. The top 10 causes of death . Available at: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death . [12.04.2020].
- 12. The World Health Organization. Noncommunicable diseases . Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases . [accessed 29.06.2020].
- 25. Wirnitzer K. Therapeutic , Probiotic , and Unconventional Foods . Chapter 21 : Vegan Nutrition : Latest Boom in Health and Exercise . Elsevier London, UK. (2018).
- 27. Grant C. The Impact of School Health Programmes . K4D Helpdesk Report. Brighton, UK: Institute of Development Studies. (2017).
- 37. The Wold Health Organization. Report of the commission on ending childhood obesity. Implementation plan: executive summary. 2017;1–24. Available at: https://apps.who.int/iris/bitstream/handle/10665/259349/WHO-NMH-PND-ECHO-17.1-eng.pdf . [accessed 23.07.2021].
- 39. The World Health Organization. Body mass index–BMI . Available at: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi . [accessed 02.07.2020]
- 41. Centers for Disease Control and Prevention. Body Mass Index (BMI) . Available at: https://www.cdc.gov/healthyweight/assessing/bmi/index.html . [accessed 10.04.2020]
- 42. The World Health Organization. BMI-for-age (5–19 years) . Available at: https://www.who.int/growthref/who2007_bmi_for_age/en/ . [accessed 02.07.2020]
- 57. The World Health Organization. G lobal recommendations on physical activity for health 9–10 . Available at: https://www.who.int/dietphysicalactivity/global-PA-recs-2010.pdf . [accessed 07.08.2020].
- 58. Euractiv-Special-Report. Physical inactivity costs estimated at € 80 bn per year . Available at: https://www.euractiv.com/section/sports/news/physical-inactivity-costs-estimated-at-80bn-per-year/ . [accessed 12.09.2020].
- 59. The World Health Organization. G lobal recommendations on physical activity for health 7–8 . Available at: https://www.who.int/dietphysicalactivity/global-PA-recs-2010.pdf . [accessed 07.08.2020].
- 60. The World Health Organization. G lobal recommendations on physical activity for health 15–34 . Available at: https://www.who.int/dietphysicalactivity/global-PA-recs-2010.pdf . [accessed 07.08.2020].
- 61. The World Health Organization. Physical activity strategy for the WHO European region . Regional committee for Europe 65th session. Available at: https://www.euro.who.int/__data/assets/pdf_file/0010/282961/65wd09e_PhysicalActivityStrategy_150474.pdf . [accessed 24.03.2020]
- 62. Department of Health and Human Services, Washington, DC: USA. 2018 Physical Activity Guidelines Advisory Committee Scientific Report . Available at: https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf . [accessed 22.05.2020].
- 88. Esselstyn CB Jr. Prevent and Reverse Heart Disease . The Revolutionary , Scientifically Proven , Nutrition-Based Cure . London: Penguin Books; 2008.
- 92. Ornish D. Dean Ornish’s Program for Reversing Heart Disease : The Only System Scientifically Proven to Reverse Heart Disease Without Drugs or Surgery . New York: Ivy Books; 1996
- 116. European Commission. Nutrition and physical activity. 2021 Available at: https://ec.europa.eu/health/nutrition_physical_activity/overview_en . [accessed 23.07.2021].
- 145. The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions (version 6 . 0) . Available at: www.training.cochrane.org/handbook .
- 153. Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public’s Health in the 21st Century . Washington (DC): National Academies Press (US); 2002. Chapter 2: Understanding Population health and Its Determinants. Available at: https://www.ncbi.nlm.nih.gov/books/NBK221239/ . https://doi.org/10.17226/10548 [accessed 02.12.2020].
- 165. Physicians Committee for Responsible Medicine. Nutrition for Kids . A Dietary Approach of Lifelong Health (2018-e) . Available at: http://www.pcrm.org/sites/default/files/pdfs/health/Nutrition_for_Kids.pdf . [accessed [06.07.2020].
- 168. Physicians Committee for Responsible Medicine. Plant-Based Diets . The power of a plant-based diet for good health . 2021. Available at: https://www.pcrm.org/good-nutrition/plant-based-diets . [accessed 12.01.2021].
- 171. Ipsos Retail Performance. (2020). Exploring the explosion of veganism in the United States . Available at: https://www.ipsos-retailperformance.com/en/vegan-trends/ . [accessed 03.10.2020]
- 175. New Public Middle School Curriculum Austria (Lehrplan der Neuen Mittelschule [NMS, 2018]. Inkraftretungsdatum: 1. September 2018. Anlage 1: Erster Teil. Allgemeines Bildungsziel, Punkt 5. Bildungsbereiche. Gesundheit und Bewegung. Seite 5. Sowie: Sechster Teil. Lehrpläne der einzelnen Unterrichtsgegenstände. Pflichtgegenstand Bewegung und Sport. Beiträge zu Bildungsbereichen. Seite 102.) German. Available at: https://www.ris.bka.gv.at/Dokumente/Bundesnormen/NOR40199276/NOR40199276.pdf . [accessed 01.08.2022].
- 176. Public High School Curriculum Austria (Lehrplan AHS Oberstufe (Sekundarstufe II) (AHS, 2018b) Inkraftretungsdatum: 9. Jänner 2018. Anlage D: Erster Teil. Allgemeines Bildungsziel, Punkt 5. Bildungsbereiche. Gesundheit und Bewegung. Seite 10.). German. Available at: https://www.bmbwf.gv.at/Themen/schule/schulpraxis/lp/lp_ahs.html . [accessed 01.08.2022].
- 177. Austrian Federal Ministry–Education, Science and Research. New Competence-Oriented Curriculum for Primary and Middle Schools. (Bundesministerium–Bildung, Wissenschaft un Forschung [2021]. Pädagogik-Paket–Teilprojeckt Lehrpläne NEU: Neue kompetenzorientierte Lehrpläne für Primar- und Sekundarstufe I und Kompetenzraster). German.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Short Communication
- Published: 23 March 2011
A school-based program of physical activity may prevent obesity
- Y Shofan 1 ,
- O Kedar 2 ,
- D Branski 3 ,
- E Berry 4 &
- M Wilschanski 3
European Journal of Clinical Nutrition volume 65 , pages 768–770 ( 2011 ) Cite this article
1198 Accesses
10 Citations
Metrics details
- Disease prevention
- Paediatrics
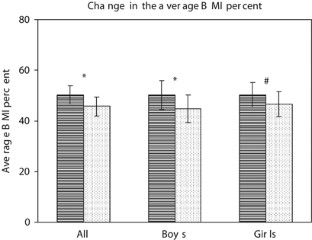
An organized intervention program in pre-pubertal children based on increased physical education and activity together with nutritional advice to the children and their families may prevent obesity. Children aged 9 to 11 received double hours of weekly physical education lessons and additional nutritional advice for 2 years. They were compared with a similar group who received standard physical education lessons only. A total of 82 study and 26 control children completed the 2 years of the project. Boys in the control group gained significantly more weight than the corresponding study group (8.4 kg vs 3.2 kg, respectively ( P <0.016)), control delta body mass index (BMI) 1.02 vs study 0.44 ( P <0.012). There was no significant change in the weight or BMI in the girls. We conclude that the prevention of obesity may be attained by similar programs. Hormonal effects and compliance at this age may be responsible for the sex differences in this study.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Skeletal muscle energy metabolism during exercise
Mark Hargreaves & Lawrence L. Spriet
Life expectancy can increase by up to 10 years following sustained shifts towards healthier diets in the United Kingdom
Lars T. Fadnes, Carlos Celis-Morales, … John C. Mathers

Effect of gut microbiome modulation on muscle function and cognition: the PROMOTe randomised controlled trial
Mary Ni Lochlainn, Ruth C. E. Bowyer, … Claire J. Steves
American academy of pediatrics (2003). Policy statement. Prevention of Pediatric overweight and obesity. Pediatrics 112 , 424–430.
Article Google Scholar
Baranowski T, Cullen K, Nicklas T (2002). School-based obesity prevention: a blueprint for tamping the epidemic. Am J Health Behav 26 , 486–493.
Broyles S, Katzmarzyk PT, Srinivasan SR, Chen W, Bouchard C, Freedman DS et al . (2010). The pediatric obesity epidemic continues unabated in Bogalusa, Louisiana. Pediatrics 125 , 900–905.
Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R (2001a). Increasing fruit and vegetableintake and decreasing fat and sugar intake in family at risk for childhood obesity. Obes Res 9 , 171–178.
Article CAS Google Scholar
Epstein LH, Roemmich JN, Raynor HA (2001b). Behavioral therapy in the treatment of pediatric obesity. Pediatr Clin North Am 48 , 981–993.
Golan M, Crow S (2004). Parents are key players in the prevention and treatment of weight related problems. Nutr Rev 62 , 39–51.
Golan M, Weizman A. (2001). Famillial aprocoach to the treatment of childhood obesity: conceptual model. J Nutr Educ Behav 33 , 102–107.
Guo SS, Wu W, Chumla WC, Roche AF (2002). Predicting overweight and obesity in Adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr 76 , 653–658.
Kain J, Uauy R, Vio F (2004). School based obesity prevention in Chilean primary school children: methodology and evaluation of controlled study. Int J of Obes 28 , 483–493.
Reinehr T, Kersting M, Alexy U, Andeler W (2003). Long-term follow up of overweight children: after training, after a single consultation session, and without treatment. J Ped Gastroenterol Nutr 37 , 72–74.
Download references
Acknowledgements
This study was supported by an educational grant from Danone International.
Author information
Authors and affiliations.
Maccabi Health Fund, Jerusalem, Israel
Braun School of Public Health, Hebrew University-Hadassah Medical School, Jerusalem, Israel
Pediatric Gastroenterology Unit, Hadassah University Hospitals, Jerusalem, Israel
D Branski & M Wilschanski
Department of Human Nutrition & Metabolism, WHO Collaborating Centre for Capacity Building in Public Health, Braun School of Public Health, Hebrew University-Hadassah Medical School, Jerusalem, Israel
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to M Wilschanski .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Shofan, Y., Kedar, O., Branski, D. et al. A school-based program of physical activity may prevent obesity. Eur J Clin Nutr 65 , 768–770 (2011). https://doi.org/10.1038/ejcn.2011.25
Download citation
Received : 22 April 2010
Revised : 07 February 2011
Accepted : 07 February 2011
Published : 23 March 2011
Issue Date : June 2011
DOI : https://doi.org/10.1038/ejcn.2011.25
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- physical activity
This article is cited by
Effective strategies for childhood obesity prevention via school based, family involved interventions: a critical review for the development of the feel4diabetes-study school based component.
- Christina-Paulina Lambrinou
- Odysseas Androutsos
- Yannis Manios
BMC Endocrine Disorders (2020)
Tackling overweight and obesity: does the public health message match the science?
- Katherine Hafekost
- David Lawrence
- Stephen R Zubrick
BMC Medicine (2013)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
San Marin Pony Express
Student-run publication bringing community & campus news to our readers, students reflect on use of bmi test in physical education.
- by Anna Kilgariff
- Posted on January 12, 2020 October 1, 2020
For some students, the Body Mass Index (BMI) test is one of the most anxiety-provoking assessments required in their school career, but for others, it is just another test mandated by the school district. The BMI test is given by NUSD to fifth, seventh and ninth graders for the purpose of collecting data on students’ wellness, and for high schoolers as one of the five tests they need to pass to complete Physical Education. The school BMI test takes a student’s height and weight and calculates if they are in the “healthy fit” zone, or the “needs improvement” zone. More broadly, it allows researchers to see the average wellness rate in a given county, state or even country.
According to the U.S. National Library of Medicine, “[The BMI test] has become the most commonly used measure of weight status due to its simplicity of calculation when collecting data for large population surveys.”
The BMI formula was invented by a Belgian mathematician whose goal was to measure the collective weight of a population, more specifically the male population. The test does not account for muscle mass, bone density, genetics, gender, biology, or ethnicity, as it was never intended for measuring the wellness of a singular person.
The BMI at San Marin
Currently, San Marin applies the BMI formula to singular students even though the formula was created to receive results that made an average. Because of this, the test often incorrectly reflects a student’s body mass which, according to an anonymous student, “puts stress on kids who are self conscious on their physical appearance, and this is most likely more unhealthy than what any BMI test may show.”
The BMI test has links to suicide and eating disorders in all genders, according to a study conducted in 2005 by the American Medical Association. Marin County’s eating disorder rates are double the national average, and in 2016, Marin had the highest suicide rate in the Bay Area.
“If we have reliable statistics telling us that it’s causing more problems than it’s solving, then I think we need to take a hard look at that,” Health teacher Cory Boyd said.
In a survey conducted by the Pony Express, 59 percent of students on campus reported that they do not believe the BMI test is a good measure of their physical fitness and wellness. “Teenagers are extremely susceptible to judgement and criticism, making this test just another medium for scrutiny of our physical appearance,” senior Kelsey McIvor said. McIvor is the president of Bring Change to Mind, which is a club that focuses on raising awareness about mental health.
Some students also feel the test violates their privacy. The test is taken in the corner of the gym with students less than four feet away waiting to be measured. After being measured, the student must verbally inform the teachers of their weight.
“The test could be conducted in a much more private setting in order to keep the data collected completely confidential,’’ McIvor said.
The fact that most students near the test site are able to hear others’ weight is one of the more stressful aspects of the test.
“I have mainly felt like I may be judged, or hearing others weights that are less than mine make me feel self-conscious,” an anonymous student said.
The anxiety that comes along with the worry of being judged by peers, and being judged by one’s self puts an unhealthy focus on one’s height and weight.
“This test is anxiety-provoking as it almost measures our worth as a number, a number that shouldn’t define us yet somehow manages to do so,” McIvor said. Sophmore Anthony Vo agreed.
“You are surrounding your whole lifestyle around your body image,” Vo said.
Grading on the BMI scale
The BMI test is an important test for students who want to opt out of PE after freshman year. To test out of PE, one must pass four out of the five components, and to pass the BMI test one must fall in the “healthy fit” zone. “The fact that students are graded on their body is sickening,” McIvor said. Students often feel the need to take advanced and unnecessary precautions to ensure they pass the test, not from a mental health and disordered eating standpoint, but the fact that they are now being graded on that aspect of their wellness.
“I thought about cheating. Everyone was like, just put coins in your pockets; bring fishing weights,” sophomore Sally Ćesko, who did not pass the BMI test due to being underweight, said.
Staff members also disagree with attaching a grade to a student’s BMI.
“If we are attaching a grade to it, I can see how that can confound and potentially make it worse for a lot of student who already don’t have very good body image, or have the skills to continually develop their own self esteem,” Boyd said.
Share this:
Leave a comment cancel reply.

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Shots - Health News
Arkansas led the nation sending letters home from school about obesity. did it help.
Kavitha Cardoza

Since Arkansas started sending the obesity letters to parents, the state's childhood obesity rates rose to nearly 24% from 21%. During the pandemic, the state obesity rate hit a high of more than 26%. M. Spencer Green/AP hide caption
Since Arkansas started sending the obesity letters to parents, the state's childhood obesity rates rose to nearly 24% from 21%. During the pandemic, the state obesity rate hit a high of more than 26%.
LITTLE ROCK, Ark. — Sixth-grade boys were lining up to be measured in the Mann Arts and Science Magnet Middle School library. As they took off their shoes and emptied their pockets, they joked about being the tallest.
"It's an advantage," said one. "You can play basketball," said another. "A taller dude can get more girls!" a third student offered.
Everyone laughed. What they didn't joke about was their weight.
Anndrea Veasley, the school's registered nurse, had them stand one by one. One boy, Christopher, slumped as she measured his height. "Chin up slightly," she said. Then Veasley asked him to stand backward on a scale so he didn't see the numbers. She silently noted his height as just shy of 4 feet, 7 inches, and his weight as 115.6 pounds.

Lifesaving or stigmatizing? Parents wrestle with obesity treatment options for kids
His parents later would be among thousands to receive a letter beginning, "Many children in Arkansas have health problems caused by their weight." The letter includes each student's measurements as well as their calculated body mass index. The BMI number categorizes each child as "underweight," "normal," "overweight," or "obese." Christopher's BMI of 25.1 put him in the obese range.
In 2003, Arkansas became the first state to send home BMI reports about all students as part of a broader anti-obesity initiative. But in the 20 years since, the state's childhood obesity rates have risen to nearly 24% from 21%, reflecting a similar, albeit higher, trajectory than national rates. During the pandemic, the state obesity rate hit a high of more than 26%.
Still, at least 23 states followed Arkansas' lead and required height and weight assessments of students. Some have since scaled back their efforts after parents raised concerns.
One school district in Wyoming used to include a child's BMI score in report cards , a practice it has since stopped. Ohio allows districts to opt in, and last year just two of 611 school districts reported BMI information to the state. And Massachusetts stopped sending letters home . Even Arkansas changed its rules to allow parents to opt out.
Multiple studies have shown that these reports, or "fat letters" as they're sometimes mockingly called, have had no effect on weight loss. And some nutritionists, psychologists, and parents have criticized the letters, saying they can lead to weight stigma and eating disorders.
BMI as a tool has come under scrutiny, too, because it does not consider differences across racial and ethnic groups, sex, gender, and age. In 2023, the American Medical Association called the BMI "imperfect" and suggested it be used alongside other tools such as visceral fat measurements, body composition, and genetic factors.
All that highlights a question: What purpose do BMI school measurements and letters serve? Nearly 20% of American children were classified as obese just before the pandemic — up from only 5% some 50 years ago — and lockdowns made the problem worse. It's unclear what sorts of interventions might reverse the trend.
Joe Thompson, a pediatrician who helped create Arkansas' program and now leads the Arkansas Center for Health Improvement , said BMI letters are meant to be a screening tool, not a diagnostic test, to make parents aware if their child is at risk of developing serious health issues, such as heart disease, diabetes, and respiratory problems.
Sharing this information with them is critical, he said, given that many don't see it as a problem because obesity is so prevalent. Arkansas is also a rural state, so many families don't have easy access to pediatricians, he said.

Don't Focus On Kids' Weight Gain. Focus On Healthy Habits Instead
Thompson said he's heard from many parents who have acted on the letters. "To this day, they are still our strongest advocates," he said.
The program also led to new efforts to reduce obesity. Some school districts in Arkansas have instituted " movement breaks ," while others have added vegetable gardens , cooking classes , and walking trails . One district sought funding for bicycles . The state does not study whether these efforts are working.
Researchers say the BMI data also serves an important purpose in illuminating population-level trends , even if it isn't helpful to individuals.
Parents are generally supportive of weighing children in school, and the letters have helped increase their awareness of obesity, research shows. At the same time, few parents followed up with a health care provider or made changes to their child's diet or physical activity after getting a BMI letter, several other studies have found.
In what is considered the gold-standard study of BMI letters , published in 2020, researchers in California found that the letters home had no effect on students' weight. Hannah Thompson , a University of California-Berkeley assistant professor who co-authored the study, said most parents didn't even remember getting the letters. "It's such a tiny-touch behavioral intervention," she said.
Arkansas now measures all public school students in even grades annually — except for 12th graders because by that stage, the pediatrician Joe Thompson said, the students are "beyond the opportunities for schools to have an impact." The change also came after many boys in one school wore leg weights under their jeans as a prank, he said.
Kimberly Collins, 50, remembers being confused by the BMI letters sent to her from the Little Rock School District stating that all her children were overweight, and that one daughter was considered obese.
"It offended me as a mama," she said. "It made me feel like I wasn't doing my job."
She didn't think her children looked overweight and the family pediatrician had never brought it up as a concern.
Hannah Thompson, the researcher from California, said that's the biggest problem with BMI letters: Parents don't know what to do with the information. Without support to help change behavior, she said, the letters don't do much.
"You find out your child is asthmatic, and you can get an inhaler, right?" she said. "You find out that your child is overweight and where do you even go from there? What do you do?"
Kevin Gee , a professor at the University of California-Davis, who has studied BMI letters , said the mailings miss cultural nuances. In some communities, for example, people prefer their children to be heavier, associating it with comfort and happiness. Or some eat foods that they know aren't very nutritious but are an important way of expressing love and traditions.
"There's a lot of rich contextual pieces that we know influences rates of obesity," Gee said. "And so how do we balance that information?"
Collins' daughter, now 15, said that as she's grown older she increasingly feels uncomfortable about her weight. People stare at her and sometimes make comments. (Collins' mother asked that her daughter's name not be published because of her age and the sensitive nature of the subject.)
"On my birthday, I went to get my allergy shots and one of the nurses told me, 'You are getting chubbier,'" she said. "That didn't make me feel the best."

How Doctors Can Stop Stigmatizing — And Start Helping — Kids With Obesity
Collins said it pains her to see her soft-spoken daughter cover herself with her arms as if she's trying to hide. The teenager has also begun sneaking food and avoids the mirror by refusing to turn on the bathroom light, Collins said. The girl signed up for tennis but stopped after other children made fun of her, her mother said.
Looking back, Collins said, while she wishes she had paid more attention to the BMI letters, she also would have liked practical suggestions on what to do. Collins said she had already been following the short list of recommended healthy practices, including feeding her children fruits and vegetables and limiting screen time. She isn't sure what else she could have done.
Now everyone has an opinion on her daughter's weight, Collins said. One person told her to put a lock on the fridge. Another told her to buy vegan snacks. Her mother bought them a scale.
"It's a total uphill climb," Collins said with a sigh.
This article was produced as a part of a project for the Spencer Education Journalism Fellowship .
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.
Weight Loss in Short-Term Interventions for Physical Activity and Nutrition Among Adults With Overweight or Obesity: A Systematic Review and Meta-Analysis
SYSTEMATIC REVIEW — Volume 21 — April 4, 2024
Wendi Rotunda, PhD 1 ; Caroline Rains, MPH 1 ; Sara R. Jacobs, PhD 1 ; Valerie Ng, BS 1 ; Rachael Lee, MSPH 1 ; Stephanie Rutledge, PhD 2 ; Matt C. Jackson, PhD, MPH 3 ; Kristopher Myers, PhD 2 ( View author affiliations )
Suggested citation for this article: Rotunda W, Rains C, Jacobs SR, Ng V, Lee R, Rutledge S, et al. Weight Loss in Short-Term Interventions for Physical Activity and Nutrition Among Adults With Overweight or Obesity: A Systematic Review and Meta-Analysis. Prev Chronic Dis 2024;21:230347. DOI: http://dx.doi.org/10.5888/pcd21.230347 .
PEER REVIEWED
Introduction
Acknowledgments, author information.
What is already known on this topic?
Long-term lifestyle change programs can be effective at achieving weight loss for adults with overweight or obesity and can lower their risks for developing chronic diseases, such as type 2 diabetes. However, enrollment and retention are challenging in long-term interventions.
What is added by this report?
We demonstrated that multicomponent nutrition and physical activity interventions of 6 months or less can achieve weight loss by the end of the intervention period.
What are the implications for public health practice?
Short-term lifestyle change programs can produce weight loss that may be associated with reduced risk of chronic diseases. Providing both short-term and long-term options could increase enrollment in such programs.
Reaching, enrolling, and retaining participants in lengthy lifestyle change interventions for weight loss is a major challenge. The objective of our meta-analysis was to investigate whether lifestyle interventions addressing nutrition and physical activity lasting 6 months or less are effective for weight loss.
We searched for peer-reviewed studies on lifestyle change interventions of 6 months or less published from 2012 through 2023. Studies were screened based on inclusion criteria, including randomized controlled trials (RCTs) for adults with overweight or obesity. We used a random-effects model to pool the mean difference in weight loss between intervention and control groups. We also performed subgroup analyses by intervention length and control type.
Fourteen RCTs were identified and included in our review. Half had interventions lasting less than 13 weeks, and half lasted from 13 to 26 weeks. Seven were delivered remotely, 4 were delivered in person, and 3 used combined methods. The pooled mean difference in weight change was −2.59 kg (95% CI, −3.47 to −1.72). The pooled mean difference measured at the end of the intervention was −2.70 kg (95% CI, −3.69 to −1.71) among interventions lasting less than 13 weeks and −2.40 kg (95% CI, −4.44 to −0.37) among interventions of 13 to 26 weeks.
Short-term multicomponent interventions involving physical activity and nutrition can achieve weight loss for adults with overweight or obesity. Offering short-term interventions as alternatives to long-term ones may reach people who otherwise would be unwilling or unable to enroll in or complete longer programs.
Approximately 60% of US adults have a chronic disease, and approximately 40% have 2 or more (1). Chronic diseases are a leading cause of death and disability (2) and contribute substantially to the $3.8 trillion in annual health care costs in the US (1). Multicomponent lifestyle change programs are known to be effective in reducing the risk of developing chronic diseases and largely focus on losing weight (3,4). Weight loss is an important objective for many lifestyle change interventions given the increased risk for people with overweight or obesity to develop chronic diseases, including type 2 diabetes (5), cardiovascular disease (6), and cancer (7). However, enrolling and remaining in such interventions are a challenge, particularly for those of longer duration (8,9). Thus, short-term interventions may have the potential to both enroll more participants and achieve higher retention (8,9). In addition, evidence indicates that most people achieve their greatest weight loss in the first 3 to 6 months of a lifestyle change intervention (10).
Previous systematic reviews examined interventions of various lengths for weight change (11–14) but did not look at whether the intervention length itself substantially affected body weight. Although 1 prior meta-analysis examined weight change in an intervention that lasted 6 months or less compared with 12 months or more, the study’s population was specific to adults with overweight or obesity who were also diagnosed with a mental illness (15). That analysis found, however, that the weight change effect size was similar in interventions of 6 months or less compared with interventions of 12 months or more.
Although weight loss is associated with preventing or delaying the onset of chronic conditions (3,4), long-term interventions have challenges in enrolling and retaining participants (8,9). We sought to understand the extent to which multicomponent interventions of 6 months or less were effective at achieving weight loss among adults with overweight or obesity.
Data sources
We searched PubMed via Medline, Web of Science, APA PsycInfo, Embase, CINAHL, and Cochrane Library for peer-reviewed studies on lifestyle change interventions of 6 months or less that were published from January 2012 through January 2023. We selected these years to ensure that the use of technology that might affect intervention length in the delivery of these interventions was reflected in the studies. Our search strategy ( Table 1 ) used a combination of key terms including 1) a health condition or lifestyle and behavior term (eg, physical activity, overweight), 2) a program or intervention term (eg, lifestyle change, intervention), and 3) an outcome term (eg, weight loss). We also hand-searched systematic reviews identified in the searches.
Study selection
We included peer-reviewed primary research studies published in English that reported on lifestyle change interventions of 6 months or less (operationalized as 26 weeks) for adults aged 18 years or older with overweight or obesity. Studies had to report weight loss outcomes to be eligible for inclusion. We excluded studies in which participants were already diagnosed with a chronic condition, such as hypertension or diabetes, but included studies that were intended for populations with heightened risks for developing chronic conditions. We also excluded studies without an intervention component focused on nutrition or physical activity.
We included randomized controlled trials (RCTs) only and excluded other study designs, such as observational studies, given that other designs are more susceptible to bias or confounding, and studies that did not conduct an intention-to-treat analysis, because complete case analysis may lead to bias in the intervention effect estimates (16). Studies also had to be conducted in countries rated as very high in development based on the United Nations Human Development Index (17), so that findings would be more generalizable to US adults with overweight or obesity.
For studies with multiple intervention arms, we selected a primary arm to include in the analysis. We selected the primary intervention arm based on several factors, such as the intervention included either nutrition or physical activity with the goal of weight loss (some of the alternative interventions did not include a lifestyle change component) or the intervention included multiple methods such as in-person sessions and an online forum meant to maximize participation and retention. In cases where multiple intervention arms met the above criteria, we included 1 intervention arm in the main analysis and the other intervention arm in a sensitivity analysis.
Data extraction and critical appraisal
We used Covidence Systematic Review Software (Veritas Health Innovation) to help manage the systematic review process. Two team members used the study selection criteria to independently review each title and abstract. All conflicts at the title and abstract stage were advanced to the full-text review. Full-text articles were also reviewed independently by 2 reviewers. Conflicts were resolved by a third senior reviewer, who also confirmed inclusion of all final articles.
Reviewers used a standardized extraction form to extract key data. The extraction form was programmed in REDCap (REDCap Consortium) (18,19), and each article was extracted by one reviewer and checked for accuracy by a senior reviewer. Data on body weight change were extracted in the reported units, either kilograms or pounds, and then standardized into kilograms for all studies. We used the National Heart, Lung, and Blood Institute’s Study Quality Assessment Tool ( Box ) (20) to document the methodologic quality of the included studies. Studies were scored and classified as poor (0–5 points), fair (6–12 points), or high (13,14 points). All 5 reviewers were trained on the extraction and study quality assessment tools before they completed the full-text extractions.
Box. National Heart Lung, and Blood Institute’s Study Quality Assessment Tool (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools)
Answer options are yes, no, neither (cannot determine, not reported, or not applicable).
1. Was the study described as randomized, a randomized trial, a randomized clinical trial, or an RCT?
2. Was the method of randomization adequate (ie, use of randomly generated assignment)?
3. Was the treatment allocation concealed (so that assignments could not be predicted)?
4. Were study participants and providers blinded to treatment group assignment?
5. Were the people assessing the outcomes blinded to the participants’ group assignments?
6. Were the groups similar at baseline on important characteristics that could affect outcomes (eg, demographics, risk factors, comorbid conditions)?
7. Was the overall dropout rate from the study at endpoint 20% or lower of the number allocated to treatment?
8. Was the differential dropout rate (between treatment groups) at endpoint 15 percentage points or lower?
9. Was there high adherence to the intervention protocols for each treatment group?
10. Were other interventions avoided or similar in the groups (eg, similar background treatments)?
11. Were outcomes assessed using valid and reliable measures, implemented consistently across all study participants?
12. Did the authors report that the sample size was sufficiently large to be able to detect a difference in the main outcome between groups with at least 80% power?
13. Were outcomes reported or subgroups analyzed prespecified (ie, identified before analyses were conducted)?
14. Were all randomized participants analyzed in the group to which they were originally assigned (ie, did they use an intention-to-treat analysis)?
Statistical analysis
We used the mean body weight change from baseline to the end of the intervention time point for both the intervention and comparison groups. When these data were not reported, we used other data provided in the study for calculating the change (21). We used Stata, version 17 (StataCorp LLC) to calculate the pooled mean difference in weight change (in kilograms) by using a random effects model with the inverse variance weighting method described by DerSimonian and Laird (22).
We assessed statistical heterogeneity (ie, variability resulting from differences in the study effects) in pooled estimates by examining I 2 statistics and P values. We considered I 2 values of 0% to 40% to indicate unimportant heterogeneity, 30% to 60% to indicate moderate heterogeneity, 50% to 90% to indicate substantial heterogeneity, and 75% to 100% to indicate considerable heterogeneity (23). When we observed moderate, substantial, or considerable heterogeneity (23), we conducted sensitivity analyses after removing outlier studies. We also visually examined plots for effects of different study characteristics and intervention factors, including the intervention method, proportion of female participants, average age of participants, average baseline weight of participants, and the percentage of participants completing the intervention.
Subgroup analyses were performed based on intervention length (<13 wk or 13–26 wk) and the type of comparison group described as low touch, usual care, or wait list. Low-touch comparison groups could entail a minimal amount of intervention for lifestyle change; for example, participants may have received informative emails (24) or printed information related to healthy habit formation (25). Usual-care groups were encouraged to engage in their regular behaviors without changing their usual routine. Wait-list or clinical-care comparison groups would eventually receive the intervention after data collection. We made the distinction between groups because a comparison group that included some engagement with participants could limit the ability to detect true intervention effects on weight loss compared with comparison groups that were considered usual care or were delayed in receiving the intervention.
Study characteristics
We screened 1,251 unique citations and identified 14 RCTs for inclusion in our review ( Figure 1 ). Among the 14 studies included, half had a wait-list comparison group (26–32), 5 had low-touch comparison groups (24,25,33–35), and 2 had usual-care comparison groups (36,37).
Five of the 14 studies were conducted in the US (26,28,32,34,35), 5 in Australia (27,29–31,36), 2 in the United Kingdom (33,37), 1 in Canada (25), and 1 in Turkey (24) ( Table 2 ). Seven studies had interventions lasting less than 13 weeks with a median of 12 weeks (24,25,27–31), and the other 7 studies lasted from 13 to 26 weeks, with a median of 24 weeks (26,32–37). The average age of study participants ranged from 40 to 52 years (24,25,27–31). Two studies included only women (28,35), and 3 studies included only men (29,30,32). Average baseline weight of study participants across all studies ranged from 82 kg to 139 kg. Seven of the 14 studies were delivered virtually, which included the use of websites, telephone, and email (24,29–31,34,36,37); 3 were a mix of both virtual and in-person components (27,32,35); and 4 were delivered exclusively in person (25,26,28,33). Among the 7 in-person and mixed-delivery intervention arms, 2 were conducted in a health care setting (28,33), 2 were conducted in a community setting (25,26), 1 was conducted in a university setting (27), 1 was conducted in the workplace (35), and 1 did not specify a setting (32).
For most of the 14 studies, the intervention focus was on both improving nutrition and increasing physical activity. Two interventions focused only on improving nutrition (34,35). Across the 14 studies that included a focus on nutrition, 7 described the nutritional component (28–30,32,34–36), 3 recommended a specific caloric value (eg, 1,200 calories per day) (28,29,34), 3 recommended participant-tailored guidance regarding calorie intake (30,32,35), and 1 allocated participants to a specific diet (36). Four studies described the physical activity component (28,32,33,36). One study reported structured group exercise in the form of 4 supervised circuit training sessions per week (28), and 3 reported providing participants with physical activity minute-count or step-count goals (32,33,36).
All 14 interventions also included more than 1 intervention component. For example, participants in 1 study (31) received a face-to-face information session, access to a study website to report daily diet and exercise, weight-loss education resources, a pedometer, and financial incentives. Another study (24) provided components that included access to an internet-based program, weekly lesson videos, food diaries, and both personalized and automatic messages. Eleven of the 14 studies provided participants with educational resources, such as booklets or access to information on a website (24,27–33,35–37); 10 studies provided participants with support tools, such as pedometers, scales, or access to food tracking logs (24,26–31,34,35,37); and 9 studies offered group or individual classes (25–27,31–35,37). Five studies supported participants by helping them set personalized exercise or calorie intake goals (29,30,32,33,35), 3 provided peer mentors or access to online discussion boards or forums where participants could work with other participants (26,30,36), and 3 sent automatic messages to participants that were not personalized, for example, messages reminding them to exercise or keep up their goals (24,30,32). In addition, 1 study provided financial incentives to participants who were part of a cohort that achieved the highest mean percentage weight loss after 1 month and at the end of the intervention (31).
Weight change
The pooled mean difference for weight change was less than −2.59 kg (95% CI, −3.47 to −1.72; 14 RCTs; 2,407 participants; I 2 = 69%) ( Figure 2 ). The negative difference in mean weight change indicates that people in the intervention groups lost more weight than those in the comparison groups. For the studies with interventions lasting less than 13 weeks, the pooled mean difference for weight change was −2.70 kg (95% CI, −3.69 to −1.71; 7 RCTs, 1,051 participants, I 2 = 73%). For the studies with interventions lasting 13 to 26 weeks, the pooled mean difference for weight change was −2.40 kg (95% CI, −4.44 to −0.37; 7 RCTs, 1,356 participants, I 2 = 69%) ( Figure 3 ). We conducted a moderator analysis with intervention duration and found a significant difference based on intervention duration ( P =.046).
Heterogeneity and sensitivity analyses
The pooled results had substantial heterogeneity overall and when stratified by intervention duration. We conducted a sensitivity analysis by removing studies with high attrition (> 20%) (24–26,33,35–37) ( Figure 4 ). From the 7 studies with interventions of less than 13 weeks, we dropped 2 low-touch comparison group studies with high attrition (24,25). Among the 5 remaining studies, heterogeneity improved ( I 2 = 0%, P =.91) and resulted in a larger mean difference for weight change: −3.48 kg (95% CI, −4.09 to −2.87). From the 7 studies with interventions of 13 to 26 weeks, we dropped 1 wait-list control study (26), 2 low-touch comparison group studies (33,35), and 2 usual-care comparison group studies (36,37) with high attrition. Among the 2 remaining studies (32,34), heterogeneity improved ( I 2 = 0%, P = .97) and resulted in a larger mean difference for weight change: −4.79 kg (95% CI: −6.30 to −3.25).
We also assessed heterogeneity by intervention method and participant characteristics. We examined results by delivery method (in person, online or other distance learning, or mixed) and gender of study participants (all men, >75% women, or a balanced mix of men and women). For results by delivery method, we found that the 7 studies conducted via online or other distance learning (24,29–31,34,36,37) had a larger effect size (−3.26 kg, I 2 = 75%) compared with the 3 studies conducted by using both online or other distance learning and in-person components (27,32,35) (−1.85 kg, I 2 = 60%), and the 4 studies conducted in person (25,26,28,33) (−0.84 kg, I 2 = 0%). We also found that for results by gender, the 3 studies conducted with all male participants (29,31,32) had a larger effect size (−3.82 kg) and minimal heterogeneity ( I 2 = 0%) compared with the 8 studies with more than 75% female participants (24–28,34–36) (−2.06 kg; I 2 = 69%) and the 3 studies with a more balanced mix of male and female participants (−3.16 kg; I 2 = 0%) (30,33,37). Baseline average age and baseline weight were similar across studies, so we do not report results by these subgroups. Intervention focus was also similar across studies (ie, most interventions focused on nutrition and exercise), so we do not report results by these characteristics.
We also conducted a sensitivity analysis that included alternative intervention arms for studies with more than 1 intervention group (25,27–30,34,36,37). The mean difference in pooled weight loss was slightly smaller than that of the selected primary intervention arm overall (−2.10 kg, 95% CI, −2.92 to −1.28) and by intervention time point (−2.16 kg; 95% CI, −3.02 to −1.31 for 13 weeks duration and −2.05 kg; 95% CI, −4.11 to 0 for 13–26 weeks duration). Heterogeneity was substantial overall ( I 2 = 69%) and for interventions of less than 13 weeks ( I 2 = 67%) and 13 to 26 weeks ( I 2 = 73%).
This meta-analysis of 14 RCTs found that interventions lasting 6 months or less were effective at achieving weight loss. Each study showed weight loss relative to control groups. The pooled mean difference in weight change was −2.59 kg compared with controls but may be further diminished when interventions are translated into real-world practice. However, adults with overweight and obesity tend to gain weight over time in the real world (eg, ~1% for >6 y) (38), such that lifestyle change interventions that slow or reverse weight gain trajectories are important in reducing the risk for developing chronic diseases. Thus, a key contribution of our study is bolstering the evidence that short-term lifestyle change interventions may result in weight change benefits in adults with overweight or obesity and could provide an alternative to longer interventions that some people may be unable or unwilling to complete (8,39,40). However, we do not know whether participants in these short-term interventions benefit, either in terms of weight change or chronic disease prevention. Our findings may have important health implications. Although the mean difference of approximately 2 kg among participants in the lifestyle change interventions relative to controls is modest, it can be clinically meaningful, because a lifestyle modification RCT reported a 16% reduction in 3-year diabetes risk for every kilogram of weight loss in the intervention group through lifestyle change (41).
All lifestyle interventions included in our meta-analysis were multicomponent, which may aid weight loss. This is consistent with findings from a recent meta-analysis where authors found that overall multicomponent lifestyle interventions were effective at achieving weight loss ranging from −1.3 kg to −8.2 kg at 5 to 6 months (42). The interventions included in that meta-analysis used various components to promote weight loss. The most frequent intervention components were educational resources, followed by support tools, such as pedometers and food and exercise diaries. Such components may facilitate self-monitoring of diet and body weight, which other studies have shown is a key to achieving healthy lifestyle behaviors (43) and preventing regain of weight lost (44). Our analysis did not examine which intervention components individually contributed to weight change. However, a recent systematic review and meta-analysis assessed the contribution of individual intervention components of lifestyle change programs, finding that change in diet, offering partial or total meal replacements, delivery by a psychologist–counselor or dietitian, and delivery in a home setting were associated with significant benefit in weight change (45). Additional research may be needed to disentangle the intervention components that drive weight change for interventions of shorter durations, such as the type of dietary guidance or the frequency and nature of physical activity recommendations. Additionally, future work should explore how social determinants of health, such as access to affordable and quality healthy food or safe places for physical activity, affect program and health outcomes (46). Understanding how different components of weight loss interventions can be adapted, tailored, or enhanced in response to contextual social determinants of health factors will help to ensure these types of interventions are equitable and accessible. Finally, 12 of the 14 included studies focused on improving both nutrition and physical activity to achieve weight loss. Therefore, we were unable to compare the effect of weight-loss interventions focused on nutrition alone versus physical activity alone. However, 1 systematic review and meta-analysis suggested that lifestyle change interventions that involved both diet and physical activity were associated with greater weight loss than those focused on diet (mean difference: –1.72 kg) or physical activity (mean difference: −5.33 kg) alone (47).
An important finding of our meta-analysis is that the interventions that lasted less than 13 weeks appear to be at least as effective for weight loss as those lasting from 13 to 26 weeks. One possible explanation for this finding is that interventions with a shorter duration showed a greater retention rate (~80%) than interventions of longer duration (~70%) in our analysis. This is consistent with other work that reported that programs of longer duration may experience higher dropout rates (48). In turn, high retention was important to increase weight loss from ~2 kg to ~4 kg in our sensitivity analysis where high attrition studies were removed, even when the intervention was relatively short in duration. This finding emphasizes that among interventions similar in length where higher retention is correlated with more significant weight loss (49,50), the success of these interventions also depends on sustained participant engagement. Future research should focus on determining which elements, such as personalized feedback or flexible scheduling, enhance retention.
Findings related to the effect of intervention duration in other meta-analyses are mixed. For example, 1 prior meta-analysis demonstrated that interventions lasting 12 months or more yielded slightly more weight loss for people with overweight or obesity compared with interventions lasting 6 months or less (15), whereas other meta-analyses reported no difference in weight loss by intervention duration (51,52). Nonetheless, interventions that require long-term engagement from participants may preclude some people from ever enrolling (53). Lengthier interventions can also be more challenging to disseminate and sustain because of the burden they place on the organizations that provide them (48).
Limitations
Our review has some limitations. First, in our meta-analysis we examined only weight change at the end of the intervention period and did not analyze any follow-up weight change that may have been reported; therefore, we could not make any conclusions about the ability of short-term interventions to sustain weight loss or reduce diabetes risk. Additional research could examine the effect of short-term interventions on sustained weight loss. Although 7 studies had substantial dropout rates at the end of the intervention (24–26,33,35–37), our sensitivity analysis showed that excluding these studies did not substantively change the overall findings. Also, given the multicomponent nature of nearly all the interventions we examined, we were unable to conclude which specific components are essential to driving weight loss. Future work should aim to disentangle the intervention components that may drive weight change for interventions of short duration. Although we improved heterogeneity by grouping studies according to their comparison group, weight loss possibly may be affected by other factors that vary between studies, such as different intensity and frequency of the interventions or differences in participant characteristics. For example, the included studies contained limited or no information on participant race or ethnicity and socioeconomic status, and some populations might respond differently to lifestyle interventions. Ensuring that interventions reduce existing health inequities is important but can be a challenge with long-term interventions that have resulted in better weight loss outcomes for participants who are non-Hispanic White and of higher socioeconomic status (39).
Short-term multicomponent interventions can possibly be effective in achieving clinically significant weight loss for adults with overweight or obesity. Participating in longer interventions may lead to more substantial results but may not be feasible for some people because of work schedules, caregiving responsibilities, transportation requirements, or other factors. Our findings can be used to inform a person’s decision making when offered a choice of programs, and by clinicians and researchers who can continue developing short-term alternatives to long interventions. Providing both short- and long-term options could increase opportunities for people to begin lifestyle changes and facilitate their choosing a program that best suits their schedule, needs, and available resources.
This work was supported by funding from the Centers for Disease Control and Prevention, contract no. HHSD2002013M53964B. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors received no external financial support for the research, authorship, or publication of this article. The authors declared no potential conflicts of interest with respect to the research, authorship, or publication of this article. No copyrighted material, surveys, instruments, or tools were used in this research.
Corresponding author: Wendi Rotunda, PhD, 3040 East Cornwallis Road, Durham North Carolina 27709 ( [email protected] ).
Author Affiliations: 1 RTI International, Research Triangle Park, North Carolina. 2 Centers for Disease Control and Prevention, Atlanta, Georgia. 3 CyberData Technologies, Herndon, Virginia.
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. About chronic diseases. July 21, 2022. Accessed November 14, 2022. https://www.cdc.gov/chronicdisease/about/index.htm
- Raghupathi W, Raghupathi V. An empirical study of chronic diseases in the United States: a visual analytics approach to public health. Int J Environ Res Public Health . 2018;15(3):431. PubMed doi:10.3390/ijerph15030431
- Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med . 2013;44(4 suppl 4):S346–S351. PubMed doi:10.1016/j.amepre.2012.12.009
- Unick JL, Beavers D, Jakicic JM, Kitabchi AE, Knowler WC, Wadden TA, et al. ; Look AHEAD Research Group. Effectiveness of lifestyle interventions for individuals with severe obesity and type 2 diabetes: results from the Look AHEAD trial. Diabetes Care . 2011;34(10):2152–2157. PubMed doi:10.2337/dc11-0874
- Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes . 2014;7:587–591. PubMed doi:10.2147/DMSO.S67400
- Jokinen E. Obesity and cardiovascular disease. Minerva Pediatr . 2015;67(1):25–32. PubMed
- De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. J Obes . 2013;2013:291546. PubMed doi:10.1155/2013/291546
- Cannon MJ, Masalovich S, Ng BP, Soler RE, Jabrah R, Ely EK, et al. . Retention among participants in the National Diabetes Prevention Program lifestyle change program, 2012–2017. Diabetes Care . 2020;43(9):2042–2049. PubMed doi:10.2337/dc19-2366
- Ely EK, Gruss SM, Luman ET, Gregg EW, Ali MK, Nhim K, et al. . A national effort to prevent type 2 diabetes: participant-level evaluation of CDC’s National Diabetes Prevention Program. Diabetes Care . 2017;40(10):1331–1341. PubMed doi:10.2337/dc16-2099
- Butryn ML, Call CC, Schumacher LM, Kerrigan SG, Forman EM. Time to peak weight loss during extended behavioral treatment. Obesity (Silver Spring) . 2018;26(4):658–664. PubMed doi:10.1002/oby.22127
- Aceves-Martins M, Robertson C, Cooper D, Avenell A, Stewart F, Aveyard P, et al. ; REBALANCE team. A systematic review of UK-based long-term nonsurgical interventions for people with severe obesity (BMI ≥35 kg m 2 ). J Hum Nutr Diet . 2020;33(3):351–372. PubMed doi:10.1111/jhn.12732
- Batsis JA, Gill LE, Masutani RK, Adachi-Mejia AM, Blunt HB, Bagley PJ, et al. . Weight loss interventions in older adults with obesity: a systematic review of randomized controlled trials since 2005. J Am Geriatr Soc . 2017;65(2):257–268. PubMed doi:10.1111/jgs.14514
- Patel ML, Wakayama LN, Bennett GG. Self‐monitoring via digital health in weight loss interventions: a systematic review among adults with overweight or obesity. Obesity (Silver Spring) . 2021;29(3):478–499. PubMed doi:10.1002/oby.23088
- LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA . 2018;320(11):1172–1191. PubMed doi:10.1001/jama.2018.7777
- Naslund JA, Whiteman KL, McHugo GJ, Aschbrenner KA, Marsch LA, Bartels SJ. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: a systematic review and meta-analysis. Gen Hosp Psychiatry . 2017;47:83–102. PubMed doi:10.1016/j.genhosppsych.2017.04.003
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions . 2nd edition. John Wiley & Sons; 2019:205–228.
- United Nations Development Programme. Human development insights. United Nations Development Programme. Accessed December 22, 2022. http://hdr.undp.org/en/content/latest-human-development-index-ranking
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. ; REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform . 2019;95:103208. PubMed doi:10.1016/j.jbi.2019.103208
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform . 2009;42(2):377–381. PubMed doi:10.1016/j.jbi.2008.08.010
- National Institutes of Health. Study quality assessment tools. Updated July 2021. Accessed December 22, 2022. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- The Cochrane Collaboration. 7.7.3.2 Obtaining standard deviations from standard errors and confidence intervals for group means. In: Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions . The Cochrane Collaboration; 2011.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials . 1986;7(3):177–188. PubMed doi:10.1016/0197-2456(86)90046-2
- The Cochrane Collaboration. 9.5.2 Identifying and measuring heterogeneity. In: Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions . The Cochrane Collaboration; 2011.
- Hepdurgun C, Özalay Ö, Pırıldar Ş, Rudarlı Rudarli Nalçakan G, Saygılı LF, Seçkiner S, et al. . Testing an internet-based Turkish obesity behavioral therapy program: a randomized study. Turk Psikiyatri Derg . 2020;31(1):41–47. PubMed
- Padwal RS, Klarenbach S, Sharma AM, Fradette M, Jelinski SE, Edwards A, et al. . The evaluating self-management and educational support in severely obese patients awaiting multidisciplinary bariatric care (EVOLUTION) trial: principal results. BMC Med . 2017;15(1):46. PubMed doi:10.1186/s12916-017-0808-6
- Mayer VL, Vangeepuram N, Fei K, Hanlen-Rosado EA, Arniella G, Negron R, et al. . Outcomes of a weight loss intervention to prevent diabetes among low-income residents of East Harlem, New York. Health Educ Behav . 2019;46(6):1073–1082. PubMed doi:10.1177/1090198119868232
- Cleo G, Glasziou P, Beller E, Isenring E, Thomas R. Habit-based interventions for weight loss maintenance in adults with overweight and obesity: a randomized controlled trial. Int J Obes . 2019;43(2):374–383. PubMed doi:10.1038/s41366-018-0067-4
- Baetge C, Earnest CP, Lockard B, Coletta AM, Galvan E, Rasmussen C, et al. . Efficacy of a randomized trial examining commercial weight loss programs and exercise on metabolic syndrome in overweight and obese women. Appl Physiol Nutr Metab . 2017;42(2):216–227. PubMed doi:10.1139/apnm-2016-0456
- Morgan PJ, Callister R, Collins CE, Plotnikoff RC, Young MD, Berry N, et al. . The SHED-IT community trial: a randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med . 2013;45(2):139–152. PubMed doi:10.1007/s12160-012-9424-z
- Collins CE, Morgan PJ, Jones P, Fletcher K, Martin J, Aguiar EJ, et al. . A 12-week commercial web-based weight-loss program for overweight and obese adults: randomized controlled trial comparing basic versus enhanced features. J Med Internet Res . 2012;14(2):e57. PubMed doi:10.2196/jmir.1980
- Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, et al. . The impact of a workplace-based weight loss program on work-related outcomes in overweight male shift workers. J Occup Environ Med . 2012;54(2):122–127. PubMed doi:10.1097/JOM.0b013e31824329ab
- Crane MM, Lutes LD, Ward DS, Bowling JM, Tate DF. A randomized trial testing the efficacy of a novel approach to weight loss among men with overweight and obesity. Obesity (Silver Spring) . 2015;23(12):2398–2405. PubMed doi:10.1002/oby.21265
- Hardcastle SJ, Taylor AH, Bailey MP, Harley RA, Hagger MS. Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: a randomised controlled trial with a 12-month post-intervention follow-up. Int J Behav Nutr Phys Act . 2013;10(1):40. PubMed doi:10.1186/1479-5868-10-40
- Arterburn LM, Coleman CD, Kiel J, Kelley K, Mantilla L, Frye N, et al. . Randomized controlled trial assessing two commercial weight loss programs in adults with overweight or obesity. Obes Sci Pract . 2018;5(1):3–14. PubMed doi:10.1002/osp4.312
- Carnie A, Lin J, Aicher B, Leon B, Courville AB, Sebring NG, et al. . Randomized trial of nutrition education added to internet-based information and exercise at the work place for weight loss in a racially diverse population of overweight women. Nutr Diabetes . 2013;3(12):e98. PubMed doi:10.1038/nutd.2013.39
- Jane M, Foster J, Hagger M, Ho S, Kane R, Pal S. Psychological effects of belonging to a Facebook weight management group in overweight and obese adults: Results of a randomised controlled trial. Health Soc Care Community . 2018;26(5):714–724. PubMed doi:10.1111/hsc.12584
- Yardley L, Ware LJ, Smith ER, Williams S, Bradbury KJ, Arden-Close EJ, et al. . Randomised controlled feasibility trial of a web-based weight management intervention with nurse support for obese patients in primary care. Int J Behav Nutr Phys Act . 2014;11(1):67. PubMed doi:10.1186/1479-5868-11-67
- Campione JR, Ritchie ND, Fishbein HA, Mardon RE, Johnson MC Jr, Pace W, et al. . Use and impact of type 2 diabetes prevention interventions. Am J Prev Med . 2022;63(4):603–610. PubMed doi:10.1016/j.amepre.2022.04.002
- Gruss SM, Nhim K, Gregg E, Bell M, Luman E, Albright A. Public health approaches to type 2 diabetes prevention: the US National Diabetes Prevention Program and beyond. Curr Diab Rep . 2019;19(9):78. . Erratum in: Curr Diab Rep . 2020;20(8):36 PubMed doi:10.1007/s11892-019-1200-z
- Sauder KA, Ritchie ND, Crowe B, Cox E, Hudson M, Wadhwa S. Participation and weight loss in online National Diabetes Prevention programs: a comparison of age and gender subgroups. Transl Behav Med . 2021;11(2):342–350. PubMed doi:10.1093/tbm/ibaa048
- Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. . Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care . 2006;29(9):2102–2107. PubMed doi:10.2337/dc06-0560
- Gallagher R, Armari E, White H, Hollams D. Multi-component weight-loss interventions for people with cardiovascular disease and/or type 2 diabetes mellitus: a systematic review. Eur J Cardiovasc Nurs . 2013;12(4):320–329. PubMed doi:10.1177/1474515112471002
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol . 2009;28(6):690–701. PubMed doi:10.1037/a0016136
- Madigan CD, Aveyard P, Jolly K, Denley J, Lewis A, Daley AJ. Regular self-weighing to promote weight maintenance after intentional weight loss: a quasi-randomized controlled trial. J Public Health (Oxf) . 2014;36(2):259–267. PubMed doi:10.1093/pubmed/fdt061
- Hartmann-Boyce J, Ordóñez-Mena JM, Theodoulou A, Butler AR, Freeman SC, Sutton AJ, et al. . Impact of program characteristics on weight loss in adult behavioral weight management interventions: systematic review and component network meta-analysis. Obesity (Silver Spring) . 2022;30(9):1778–1786. PubMed doi:10.1002/oby.23505
- Centers for Disease Control and Prevention. Social determinants of health at CDC. Accessed December 22, 2022. https://www.cdc.gov/about/sdoh/
- Johns DJ, Hartmann-Boyce J, Jebb SA, Aveyard P; Behavioural Weight Management Review Group. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet . 2014;114(10):1557–1568. PubMed doi:10.1016/j.jand.2014.07.005
- Ritchie ND. Solving the puzzle to lasting impact of the National Diabetes Prevention Program. Diabetes Care . 2020;43(9):1994–1996. PubMed doi:10.2337/dci20-0031
- Nhim K, Gruss SM, Porterfield DS, Jacobs S, Elkins W, Luman ET, et al. . Using a RE-AIM framework to identify promising practices in National Diabetes Prevention Program implementation. Implement Sci . 2019;14(1):81. PubMed doi:10.1186/s13012-019-0928-9
- Herman WH, Villatoro C, Joiner KL, McEwen LN. Retention and outcomes of National Diabetes Prevention Program enrollees and non-enrollees with prediabetes: The University of Michigan experience. J Diabetes Complications . 2023;37(8):108527. PubMed doi:10.1016/j.jdiacomp.2023.108527
- Speyer H, Jakobsen AS, Westergaard C, Nørgaard HCB, Jørgensen KB, Pisinger C, et al. . Lifestyle interventions for weight management in people with serious mental illness: a systematic review with meta-analysis, trial sequential analysis, and meta-regression analysis exploring the mediators and moderators of treatment effects. Psychother Psychosom . 2019;88(6):350–362. PubMed doi:10.1159/000502293
- Cai X, Qiu S, Luo D, Wang L, Lu Y, Li M. Mobile application interventions and weight loss in type 2 diabetes: a meta‐analysis. Obesity (Silver Spring) . 2020;28(3):502–509. PubMed doi:10.1002/oby.22715
- Zhang J, Van Spall HGC, Wang Y, Thabane L, Wang R, Li G. Twenty-year trends in racial and ethnic enrollment in large diabetes randomized controlled trials. BMC Med . 2022;20(1):294. PubMed doi:10.1186/s12916-022-02501-2
a This search strategy was initially developed as part of a broader systematic review.
Abbreviations: I, intervention; C, comparator; BMI, body mass index; CVD, cardiovascular disease; NIH, National Institutes of Health; UK, United Kingdom. a Study was determined to be low quality because of high participant attrition (>20%).
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review
Hidayet suha yuksel.
1 Faculty of Sport Sciences, Ankara University, 06830 Ankara, Turkey
Fatma Neşe Şahin
Nebojsa maksimovic.
2 Faculty of Sport and Physical Education, University of Novi Sad, 21000 Novi Sad, Serbia
Patrik Drid
Antonino bianco.
3 Department of Psychology, Educational Science and Human Movement, University of Palermo, 90144 Palermo, Italy
Associated Data
With the significant decrease in physical activity rates, the importance of intervention programs in the schools, where children spend a significant part of the day, has become indisputable. The purpose of this review is to systematically examine the possibility of school-based interventions on promoting physical activity and physical fitness as well as preventing obesity. A systematic approach adopting PRISMA statement was implemented in this study. Three different databases (2010–2019) were screened and primary and secondary school-based intervention programs measuring at least one variable of obesity, physical activity, or physical fitness were included. The risk of bias was assessed using the validated quality assessment tool for quantitative studies. Among 395 potentially related studies, 19 studies were found to meet the eligibility criteria. A general look at the studies examined reveals that among the outcomes, of which most (18/19) were examined, a significant improvement was provided in at least one of them. When the program details are examined, it can be said that the success rate of the physical activity-oriented programs is higher in all variables. School-based interventions can have important potential for obesity prevention and promotion of physical activity and fitness if they focus more on the content, quality, duration and priority of the physical activity.
1. Introduction
Physical activity (PA) is one of the most effective ways of preventing cardiovascular and mental illnesses and improving physical fitness (PF). Regular PA reduces the risk factors of many diseases such as high blood pressure, diabetes and obesity [ 1 ]. On the other hand, inactivity may cause obesity and a low level of cardiovascular fitness and increase the risk of high blood pressure and cholesterol with children. This situation also may lead to the development of chronic diseases such as high blood pressure and diabetes during adulthood [ 2 ]. In the systematic study of Janssen and Leblanc [ 3 ] where the relationship between PA, PF, and health of school-age children and adolescents were examined, it was found that PA contributed significantly to health, especially in high-risk youth, and that PA should be continued at least moderately to maintain health benefits and that vigorous activities provided more benefits. In another systematic study examining the interventions to increase moderate-to-vigorous (MVPA) PA in physical education classes, it was concluded that the intervention could increase MVPA levels throughout the course and provide significant benefits to public health [ 4 ].
To achieve health benefits, it is recommended to exercise with MVPA intensity for five days a week or more for at least 30 min, or with vigorous intensity for at least 20 min for 3 days [ 5 ]. The World Health Organization (WHO) [ 6 ] recommends MVPA for children and adolescents for at least 60 min per day. Despite the importance of regular PA, PA levels have started to decrease together with the new tools such as smartphones, computers, tablets, video games and social media, that have come into our lives in relation to technology [ 1 ]. PF of children has also declined with low levels of PA [ 7 ]. High levels of PF in children and adolescents are linked to physical and mental health [ 8 ]. At this point, the role of schools, where children and adolescents spend a significant portion of their days, in providing PA opportunities has reached an even more critical point. Despite this critical situation, the scope, quantity and quality of physical education courses, as well as the participation rates in extracurricular physical activities are not at the desired levels and differ significantly from school to school [ 9 , 10 , 11 ]. Schools are easy and provide accessible settings to promote engagement in PA because it is related to the objectives of the physical education curriculum. Children can learn the knowledge, skills and attitudes necessary for lifelong PA habits in schools. WHO [ 6 ] maintained that “all children and young people should be physically active with the support of schools or public institutions through games, sports, recreation, physical education and planned physical activities” and underlined the mission of schools regarding PA. School-based PA interventions include various categories such as physical education curriculum, classroom activity breaks, active commuting to school, modified playgrounds and comprehensive multi-component approaches. Along with learning in psychomotor, cognitive and affective domains, PA and PF levels will be promoted and obesity will be prevented over time. In this context, the priority is that children have meaningful learning experiences during their school years. Considering the seriousness of problems, which may occur related to inactivity in children, increasing school-based PA options of children and ensuring that children spend time with PA at schools should be considered a vital task.
Although PA programs in schools are one of the primary sources for promoting PA and FP, children are not active enough and their obesity/overweight levels have reached alarming levels [ 12 , 13 , 14 , 15 ]. A sedentary lifestyle and changing dietary habits have significantly increased obesity among children and adolescents [ 16 ]. Overweight and obesity are operationally defined as ‘‘abnormal or excessive fat accumulations that negatively affect health’’ [ 17 ]. WHO accepts childhood obesity as one of the most important global problems of the 21st century [ 18 ]. Overweight or obesity is a very complex phenomenon with many different causes. Although it is widely accepted that the increase in obesity stamps from the imbalance between energy intake and expenditure, it is known that there are many other genetic, environmental and behavioral reasons. The ecological model, as described by Davison et al., suggests that child risk factors for obesity include dietary intake, PA, and sedentary behavior [ 19 ]. In addition, environmental and socio-cultural factors such as family characteristics and parents’ lifestyle, school policies, and screen culture affect eating and activity behaviors [ 20 ]. Therefore, school-based intervention programs to prevent obesity should be designed and diversified in a comprehensive and multicomponent way. Physical inactivity is one of the most important factors in the emergence of obesity [ 21 , 22 ]. Traditional interventions for overweight or obesity include training in healthy nutrition and changing lifestyles by increasing PA. In this context, interventions based on increasing PA are often considered to be the most effective method, not only because they help in weight control but also because of health benefits such as the strengthening of bones and muscles, better sleep, improving mental health and reducing the risk of cardiovascular disease [ 3 , 23 ]. In a longitudinal study performed on more than 6000 children at the age of 7 years doing regular PA, it was concluded that performing PA was associated with the body fat percentage of children at the age of 11 years [ 24 ]. Again, researches conducted on children aged between 4 and 18 show that being engaged in regular PA has basic health benefits such as the increasing of bone density, good blood pressure and the improving of metabolic or cardiopulmonary health [ 3 , 25 ]. Apart from these, the benefits of PA can be stated as increased attention span, healthy functioning of cognitive processes, mental health and a general state of being healthy [ 26 , 27 ]. Regardless of the intensity, PA is associated with better health, motor skills and positive cognitive outcomes [ 28 ].
School-based PA is a necessary process that requires the structuring of all the time spent in the school, beginning with the planning of the child starting the day actively as s/he comes to school. In order to increase the participation of children in PA in schools and to prevent obesity effectively, it is necessary to increase the active time in physical education courses, to diversify the content of the course, to reevaluate the teacher qualifications and the number of students, to examine the effectiveness of programs for recess, in-school activity, extracurricular activities and school teams. Some systematic studies conducted in this respect have shown that school-based interventions can be effective in preventing obesity and promoting PA [ 29 , 30 , 31 ]. On the other hand, there are also studies in which variables such as obesity, PA and sedentary behavior are measured and no significant development can be observed [ 23 , 32 , 33 ]. In a significant part of the studies carried out in the literature, the differentiation of the success of situations in terms of the variables examined necessitates the examination of the studies conducted in this field from different aspects [ 34 , 35 , 36 ]. In this systematic review, it is aimed to contribute to the literature from different perspectives by including variables such as the content, type and duration of the physical activity which can directly affect the success of the school-based programs and are not sufficiently emphasized in other systematic review studies. Additionally, more studies are needed to evaluate the different contexts regarding the potential of school-based interventions. In this context, the study aims to systematically examine the possibility of school-based interventions for preventing obesity and promoting PA and PF.
2. Materials and Methods
The framework used analytically by Kahn et al. [ 37 ] and modified by Demetriou and Honer [ 30 ] was organized and used particularly in this study. In this sense, the expected characteristics of the school-based interventions, the expected outcomes and the interventions that are accepted to be used outside of PA in such programs are presented in Figure 1 . The systematic review does not include content that violates human rights, in compliance with the Helsinki Declaration; therefore, ethical approval was not needed.

General framework of the systematic review. PA: Physical activity.
2.1. Literature Search and Study Selection
In order to fully incorporate the relevant literature, a thorough electronic screening was conducted. The following databases were used to scan the data: (1) PubMed, (2) Web of Science, (3) Scopus. The scanning was focused on the following four key elements: population (children, adolescents), study design (trial), behavior (physical activity, walking, running, games, sports, etc.), and intervention (behavior change, higher BMI, level of physical activity, fitness). Focusing on these 4 elements, combinations of the terms school-based, physical activity, health, child, adolescent, intervention, overweight and obese were used in searching concepts ( Supplementary File S2 ).
After the first screening based on databases, the title and abstracts were exported to an Excel file and records were screened by two researchers. At this stage, researchers excluded studies if they did not include physical activity and primary or secondary school students, and if it were not clearly indicated that the program was in a school setting. After the title and abstract review, the full texts of potentially related studies in the databases were recorded.
2.2. Eligibility Criteria
The main criteria used for inclusion in this study were the application of at least one of the programs presented in Figure 1 within the scope of school-based PA, and that the results of this intervention regarding at least one variable among the components of body composition, waist circumference, skinfold, PA level, and PF were measured. In addition to this, the studies consisted of primary or secondary school students as a sample and were published between the years 2010–2019, with English accepted as a criterion. Studies published in languages other than English were excluded. Besides, studies that did not take place within the scope of school-based PA and that did not involve intervention were excluded from the study even if the age group matched. The studies that did not include clear information regarding the measurement of outcomes about obesity and PA level or how PA was implemented were also excluded.
2.3. Data Extraction and Risk of Bias
The researchers initially summarized the abstracts of each article in the Excel file in order to serve the purpose of the research. At this stage, two different researchers examined the studies according to the criteria to be included in the study and articles that did not meet the criteria for inclusion in the study were extracted. The research design, population, intervention type, intervention details, data collection process, measured characteristics and findings of the studies remaining after this stage were filed. At the next stage, two independent researchers evaluated the quality of the full text of the studies through the “validated quality assessment tool for quantitative studies” developed in the Effective Public Health Practice Project (EPHPP) ( Supplementary Table S1 ) [ 38 ].
The EPHPP quality assessment tool gives the six study components a strong, moderate or weak assessment ( Table 1 ). Based on these ratings, a global quality rating is made. Powerful studies have no weak components. Moderate studies have only one weak component. Weak studies have two or more weak components.
Quality assessment for studies.
In the first screening based on databases, 395 studies (PubMed: 188, WoS: 134, Scopus: 73) were obtained. After the exclusion of 58 repeated studies, 337 remaining titles and abstracts were read and evaluated by the researchers. In addition, systematic studies were examined, and the 12 studies found were included in the review process at this stage. After the title and summary review, the full texts of 71 studies in the databases were recorded. Nineteen studies were included in the final process after the studies that did not fit the criteria were excluded following the full-text review. The process was summarized and presented in the PRISMA flow diagram [ 39 ] ( Figure 2 ).

Flow diagram of studies through the review process.
Nineteen studies from 14 different countries (USA, Australia, England, France, Czech Republic, Iceland, Switzerland, Norway, Scotland, South Africa, China, India, Pakistan, Israel) met the eligibility criteria. 42.10% of these studies were identified as cluster randomized controlled trials, 21.05% as a non-randomized controlled trial, 15.78% quasi-experimental design, 10.52% randomized controlled trial and 10.52% as one-group, repeated measures design and mixed-effects model. An examination of the distribution of the schools studied revealed that 68.42% of the school-based intervention was realized in primary schools and 31.57% in secondary schools.
3.1. Description of Intervention and Study Quality
When the studies were evaluated according to the focus of the school-based program, the ratio of the physical activity-oriented studies (at least a direct intervention) was determined to be 73.68% and the ratio of the studies with education, guidance, counseling, and orientation support was determined to be 26.31%. The state of PA intervention being focused was evaluated according to whether it has a strategy or practice aimed at direct implementation of PA after the program details were examined. Among these studies, PA interventions have been in the form of increasing the duration of physical education or changing its content, performing extracurricular physical activities, doing activities during breaks or lunch breaks or giving activity breaks in the lessons other than physical education. In some researches, school-based interventions were in the form of examining the effects of a general project, while in some other researches it was in the form of directly intervening in a special group. In the control groups, nothing was changed. Two independent researchers helped to evaluate the quality of the studies. The results of the evaluation are given in Table 2 .
Summary of school-based intervention studies.
IG: Intervention group; CG: Control group; PF: Physical fitness.
Besides, evaluation details are provided in the Supplementary Material . According to the evaluation results, 10 of the studies were evaluated as strong [ 40 , 47 , 49 , 50 , 52 , 54 , 55 , 56 , 57 , 58 ] and the remaining nine studies were evaluated as moderate. There were no studies evaluated as weak. In the general evaluation, the studies where two researchers made different decisions were discussed by them and the final decision was made. The efficiency and details of the studies are presented in Table 3 and Table 4 .
Summary results of studies.
The “+” symbol indicates significant difference, the “−” symbol indicates no significant difference, and the abbreviation “NA” indicates that the relevant variable has not been examined in the study.
Details of the studies.
3.2. Main Outcomes Regarding Obesity Parameters, Physical Activity and Physical Fitness
The studies revealed the main outcomes, including: BMI (kg/m 2 ), waist circumference, skinfold and body fat percentage related to obesity parameters [ 40 , 41 , 42 , 43 , 45 , 46 , 47 , 49 , 50 , 51 , 52 , 53 , 56 ], the level of PA [ 45 , 48 , 49 , 50 , 51 , 52 , 54 , 55 , 57 , 58 ] and various variables related to PF components [ 42 , 49 , 52 , 53 , 54 , 56 ] during school years. Measurements of MVPA recommended in these studies were interpreted by measuring with the survey method in some studies [ 40 , 50 , 57 ] and by way of pedometer or accelerometer in some others [ 44 , 45 , 47 , 48 , 49 , 51 , 52 , 54 , 55 , 58 ]. In the studies where BMI (kg/m 2 ) measurements were reported, it was found that body mass index was measured by taking height and weight measurements with standard tools. Three studies were also interpreted by measuring waist circumference [ 42 , 46 , 56 ]. Skinfold measurements were also performed in three studies [ 49 , 50 , 57 ]. In these studies, results regarding variables such as aerobic endurance, flexibility, muscular strength, muscular endurance, power, and speed which belong to fitness components were stated [ 42 , 45 , 49 , 52 , 53 , 54 , 56 ]. See Table 4 for details.
3.2.1. Obesity
Although the values considered in the studies conducted within the scope of school-based intervention are all related to obesity, in this section, it will be focused on the studies where variables such as BMI, waist circumference and skinfold are measured, which may give a clearer idea. In this sense, body composition was evaluated in 15 studies [ 40 , 41 , 42 , 43 , 45 , 46 , 47 , 49 , 50 , 51 , 52 , 53 , 56 , 57 , 58 ]. In addition, in eight studies, body fat percentage was calculated by skinfold thickness, waist circumference thickness, or digital measurements [ 41 , 42 , 46 , 49 , 50 , 53 , 56 , 57 ]. While in eight of 15 studies in total (53.33%) there was a significant difference in favor of the intervention group in terms of BMI variable [ 40 , 41 , 43 , 45 , 47 , 49 , 50 , 58 ], there was no significant difference in six of them (40%) [ 42 , 51 , 52 , 53 , 56 , 57 ]. In the study conducted by Grydeland, Bjelland, Anderssen, Klepp, Bergh, Andersen, Ommundsen and Lien [ 46 ], while a significant difference was found in girls, no significant difference was found in boys ( p > 0.05).
Significant improvement was observed in four (50%) of the eight studies (skinfold, waist circumference or digital measurement) in which body fat percentage was measured [ 41 , 42 , 49 , 50 ]; no significant difference was found in three studies (37.5%) [ 46 , 56 , 57 ]. However, while no significant difference was found in waist circumference and skinfold values in the study conducted by Magnusson, Hrafnkelsson, Sigurgeirsson, Johannsson and Sveinsson [ 53 ] ( p > 0.05), the difference between the increases in fat percentage was found to be significant in favor of the experimental group ( p < 0.05).
When the BMI variable was examined in studies more focused on PA, the success rate was 72.72% (8/11) [ 40 , 42 , 43 , 45 , 46 , 47 , 49 , 50 , 52 , 56 , 57 ]; and the success rate was found to be 50% (2/4) in studies using PA only as support [ 41 , 51 , 53 , 58 ]. These results indicate that physical activity-oriented interventions are more likely to be successful in the BMI variable.
Obesity is also a variable directly related to the duration of intervention. In this context, when the studies lasting less than 6 months and the studies lasting longer than 6 months are compared according to the duration of the intervention [ 40 , 41 , 42 , 46 , 49 , 52 , 53 , 56 ], the success rate of the BMI variable was 62.5% (5/8); in studies less than 6 months [ 43 , 45 , 47 , 50 , 51 , 57 ] this rate was 66.66% (4/6). This result shows that shorter interventions can achieve similar success in the BMI variable.
There are 11 studies where children who are obese or overweight are in the study group [ 41 , 42 , 43 , 46 , 47 , 48 , 49 , 50 , 53 , 56 , 58 ]. While significant progress was made in the intervention group in six of these studies [ 41 , 43 , 47 , 49 , 50 , 58 ], no significant difference was found in five studies [ 42 , 46 , 48 , 53 , 56 ].
In brief, it is understood that in almost half of the studies, there was an improvement in BMI (53.33%), waist circumference or skinfold (50%) values. It was determined that, in line with the type of intervention, the BMI variable improved significantly in 72.77% (8/11) of the physical activity-oriented studies and that a success rate of 50% (2/4) could be achieved in interventions focused on training, guidance, orientation or providing support.
3.2.2. Physical Activity
Measurements regarding PA level were made in 13 studies [ 42 , 44 , 45 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 55 , 57 , 58 ]. In three of these studies, the evaluation was based on surveys, [ 42 , 50 , 57 ], a pedometer was used in four studies [ 45 , 51 , 54 , 58 ] and an accelerometer was used in five studies [ 44 , 47 , 48 , 49 , 52 ]. In the study conducted by Sigmund, El Ansari and Sigmundova [ 55 ], both accelerometer and pedometer were used. Since a substantial part of these studies was measured by objective methods, it was easier to evaluate them. In a substantial number of the studies conducted (61.53%), it was concluded that there was a significant increase in the PA levels of children compared to the control group [ 42 , 44 , 45 , 49 , 50 , 54 , 55 , 58 ].
Apart from that, while PA levels increased significantly in seven of the studies with the physical activity-oriented intervention [ 42 , 44 , 45 , 49 , 50 , 54 , 55 ], no significant development was observed in three of them [ 47 , 52 , 57 ]. Whereas PA levels increased significantly in one of the studies predominantly based on education and orientation [ 58 ], no significant increase was observed in the other two studies [ 48 , 51 ]. In addition, while PA levels increased significantly in two of the studies conducted through surveys [ 42 , 50 ]; the number of studies showing a significant increase in the studies measured by pedometer or accelerometer was determined to be four [ 49 , 54 , 55 , 58 ]. When evaluated in terms of duration, while a significant increase was observed in three of the studies where the intervention period lasted 6 months or less [ 45 , 50 , 54 ], no significant increase was observed in one study [ 51 ]. In the studies, which lasted over 6 months, while a significant increase was found in PA levels in five studies [ 42 , 44 , 49 , 55 , 58 ], development was not found to be significant in four studies [ 47 , 48 , 52 , 57 ].
In brief, although the type and extent of the interventions were different, PA levels of children increased in a significant proportion of the studies. While 70% (7/10) of the physical activity-oriented studies showed a significant increase, that 33.33% (1/3) success rate was achieved in studies focused on training and orientation. This result demonstrates the importance of applying PA strategies at the focus of the intervention program to increase the levels of PA.
3.2.3. Physical Fitness
In seven studies examined, components related to fitness were analyzed [ 42 , 45 , 49 , 52 , 53 , 54 , 56 ]. As the first variable, the property of aerobic endurance was evaluated in terms of shuttle run, 1-mile run test and ergometer bike. It was concluded that in four of the studies examining the aerobic endurance, this variable increased significantly compared to the control group [ 45 , 49 , 53 , 56 ]. No significant development was observed in two studies [ 52 , 54 ]. Considering the type of intervention, significant improvement was observed in four intervention physical activity-oriented studies [ 42 , 45 , 49 , 56 ] and no significant improvement was observed in terms of aerobic endurance in two studies [ 52 , 54 ]. In the study, which was focused on education and orientation, significant developmental findings were found [ 53 ]. When evaluated in terms of intervention duration, the rate of studies that provided significant improvement in aerobic endurance in the intervention performed at 6 months or less was determined to be 66.66% (2/3) [ 45 , 56 ]. No significant difference was found in the study conducted by Shore, Sachs, DuCette and Libonati [ 54 ]. In studies with intervention over 6 months, the rate of studies, in which aerobic capacity increased significantly, was determined to be 66.66% (2/3) [ 49 , 53 ]. In the study conducted by Madsen, Linchey, Gerstein, Ross, Myers, Brown and Crawford [ 52 ], the change in the aerobic capacities of children was not found to be significant ( p > 0.05).
Apart from aerobic endurance, four studies, most of which belong to health-related PF components, were examined in variables such as flexibility, speed, power, muscular strength and muscular endurance [ 42 , 45 , 54 , 56 ]. Among these, in the study conducted by Bhave, Pandit, Yeravdekar, Madkaikar, Chinchwade, Shaikh, Shaikh, Naik, Marley-Zagar and Fall [ 42 ], there was a significant improvement in favor of the intervention group in running, long jump, sit-up and push- up tests. In the study conducted by Eather, Morgan and Lubans [ 45 ], different variables related to PF were evaluated and significant improvement was observed in flexibility and muscular fitness properties in favor of the intervention group. In another study of Shore, Sachs, DuCette and Libonati [ 54 ], measurements were made regarding muscular strength, endurance and flexibility, but no significant difference was found compared to the control group. In the study where anaerobic capacity was measured in addition to health-related components, Thivel, Isacco, Lazaar, Aucouturier, Ratel, Dore, Meyer and Duche [ 56 ] found a significant difference in anaerobic fitness capacity in favor of the intervention group.
In brief, it is seen that in interventions based in school, measurements regarding all the health-related PF components (body mass index was examined in previous sections) were performed. Significant improvements were found in most of the studies predominantly focusing on aerobic capacity (66.66%). Improvements were observed in two of the three studies examining the different components of health-related PF. These improvements related to health-related PF parameters are valuable in terms of highlighting the importance of PA in improving children’s health.
4. Discussion
The purpose of this systematic review is to examine the potential of school-based interventions for obesity parameters (BMI, waist circumference, skinfold), PA level, and PF. Overall, 18 of the 19 studies examined were able to achieve significant improvements in at least one variable. It can be said that the content and details of the school-based intervention program are the most important factors in determining the efficiency in the studies examined. When the studies were classified according to the focus of PA in the program details, in 14 studies a strategy for direct PA and focus within the program was found [ 40 , 42 , 43 , 44 , 45 , 46 , 47 , 49 , 50 , 52 , 54 , 55 , 56 , 57 ]. Additionally, in five studies, it was understood that the education, guidance, orientation, and support in material of the staff and teachers in subjects such as health, nutrition and healthy life were in focus [ 41 , 48 , 51 , 53 , 58 ]. When the variables examined are considered, it can be said that the success rates in the physical activity-oriented studies are higher in all variables compared to those that are multicomponent but not centered on PA. This reveals the necessity of centralizing strategies aimed at PA to prevent obesity, promote PA and PF. Of course, the priority of programs for lifelong PA and health should be to prepare appropriate learning environments. Health-based physical education curriculum models aiming at a physically active life lead to the preparation of appropriate learning environments [ 59 ]. However, the relationship between the curriculum and pedagogy needs to be well understood in order to adopt more available approaches and not to neglect the enjoyable aspects of school-based PA [ 60 ]. From a holistic perspective, school-based PA programs can be more successful in promoting PA and PF. Castelli et al. [ 61 ] listed some of the properties that schools should have in order to educate physically active children: (a) a holistic approach and (b) effective and diversified pedagogy. Measuring of multicomponent interventions involving environmental and educational strategies is a complex and challenging process [ 62 ]. In this sense, although evaluations of different variables were made in school-based PA studies, only variables related to physiological dimensions were considered in this systematic research in line with the purpose.
Health promotion was the primary emphasis in school-based intervention programs. When health was evaluated from the physical aspect, the importance of school-based PA programs in improving health was revealed in this study. Similarly, in the systematic review made by Naylor et al. [ 63 ], most of the school-based intervention studies (11/15) were found to be positively associated with at least one health outcome. Of course, any program structured so as not to compromise health in relation to PA will contribute positively to health, but programs that are more comprehensive, centered on PA and games can be more helpful in this sense. In support of this situation, in the systematic study conducted by De Bourdeaudhuij et al. [ 64 ], it was suggested that the school environment should be rendered appropriate for PA, and PA durations should be increased in order to promote health. It would be more appropriate to integrate school-based programs into curriculum models in health promotion [ 59 ]. Curriculum models will ensure the persistence of effective and cognitive learning, which is crucial for the development of healthy living habits [ 65 , 66 ].
In eight of the 15 studies that evaluated obesity-related parameters, significant improvements were observed in variables such as BMI, skinfold, waist circumference and body fat; in seven studies, no significant development was observed regarding the whole group. In this sense, failure to achieve full success in almost half of the studies (46.66%) reveals that both the applied program and environmental conditions should be re-evaluated. Regarding this issue, in some systematic studies examining the effect of school-based PA on obesity parameters, it was concluded that it has no positive effect [ 23 , 67 ]. Although PA interventions are of great value in terms of short-term benefits in the fight against obesity or overweight, comprehensive programs are needed to have healthy living habits in the long term. At this point, it was understood that in most of the studies conducted to prevent obesity, multicomponent programs focusing on more than one dimension were applied [ 64 , 68 ]. These multicomponent programs should focus on content, teacher training and curriculum design to help children learn knowledge, skills and attitudes. In the study conducted by Brown and Summerbell [ 69 ], it was stated that the combination of programs based on nutrition and PA might be more effective in the struggle with obesity in the long term. For a more effective and permanent solution against the struggle with obesity, such comprehensive programs should include at least 60 min of MDVA, and interventions should be aimed at healthy diet and healthy living habits. Regarding the duration of the intervention, there was no difference in efficiency between the studies that lasted less than 6 months and more. In a meta-analysis by Harris et al., the shorter or longer duration of the intervention did not change the outcome of obesity [ 23 ].
Significant reductions in PA levels increase the importance of schools in providing a diversity of PA. In this sense, the use of different types of physical activities in school can increase children’s interest and encourage them to be more active [ 70 , 71 ]. In our study, improvement has been achieved in eight (61.53%) of the 13 studies aimed at increasing the level of PA. Similarly, in the systematic compilation conducted by Demetriou and Honer [ 30 ], it was concluded that in PA interventions in the school environment, 56.8% success was achieved in terms of increasing the level of PA. In the studies, in which PA intervention was predominantly in the center, development success on PA level reached higher rates (70–33.33%). An increase in the level of PA is important in every aspect, but when considered in relation to health, it is also important to indicate the intensity of PA. PA for at least 60 min per day with MDVA is suggested in order to improve health [ 3 , 6 ]. As interventions are very heterogeneous in terms of type, intensity and extent, there are difficulties in evaluating them at the point of MVPA. However, school-based PA programs have the potential to provide MVPA with high-intensity activity types [ 4 ]. In some of the studies evaluating the intensity of PA, interventions were found to be associated with MVPA [ 44 , 48 ]. Fairclough and Stratton stated that students engaged in MVPA for 27% to 47% of physical education class time [ 72 ]. To increase the intensity and duration of PA, it should be ensured that children are active when coming to school in the morning, during the break time, lunch break, in other lessons or at the extracurricular activities other than the physical education class. Physical education can be an effective influence on promoting PA [ 73 ]. Physical education courses should be the most complementary part of school-based PA, but this course only is not sufficient and more comprehensive programs are needed for lifelong activity [ 73 ]. The use of school-based interventions to increase the PA level of today’s children is very valuable. Some studies clearly demonstrate this potential [ 74 , 75 ].
The last variable considered in the study was the concept of PF. In seven of the studies conducted on this subject, components related to PF were evaluated and positive developments were observed in many of these studies. The primary objective of school-based PA programs is to reach and maintain health-related PF. Therefore, in the studies reviewed, the focus was rather on health-related fitness components. These are factors including components such as health-related PF, BMI, cardiorespiratory endurance (aerobic endurance), muscular strength, muscular endurance and flexibility [ 8 ]. While the feature that is mainly desired to be improved in the studies examined is aerobic endurance, it was found that there were also evaluations regarding the other components. In some studies, conducted in this sense, there are findings concerning the potential of school-based programs in improving PF [ 29 , 76 ]. There are also studies demonstrating the potential of the developed curricula for fitness education [ 59 , 77 ]. The results of our study show that even if the programs are multicomponent, the way of PA intervention is the most decisive factor at this point. In this sense, PA and games are essential for promoting PF in such programs [ 78 ].
The problems in evaluating the efficiency of such studies include: (1) the presence of very heterogeneous groups in general, and (2) the implementation of many interventions without adequate supervision, focusing only on guidance in schools, not long-term, and some of the measurement methods used are not objective. In order to prevent these problems, programs should be continued from preschool to the end of high school so that children have lifelong healthy living habits and they also should be based on a theoretical framework. The results obtained indicate that school-based intervention programs can have important potential for preventing obesity and promoting PA and PF if these problems are overcome and they focus more on PA.
The limitations of this study can be classified as follows:
- (1) In this research, publications other than articles (theses, papers, books, etc.) and studies published in languages other than English were not included.
- (2) Although many variables are measured in school-based PA programs, it was focused only on measurements related to obesity, PA, and PF in this study.
- (3) Since the contents and the type of implementation of PA programs are generally multi-component, it is difficult to understand what the most effective way is in such studies.
- (4) Evaluation of the focus of school-based intervention programs was determined according to the details given in the articles.
- (5) Besides, some variables were measured by questionnaire and some studies did not provide enough details.
- (6) In this study, variables such as curriculum, teaching models and teacher competencies related to the learning process in PA, and PF developmental processes were excluded.
Practical Implications
The main purpose of the studies related to school-based PA programs and should be used to develop the motor skills necessary for children to be active throughout their lives, and also to educate children who exhibit positive social behaviors while improving their PA and fitness levels. In this sense, physical education teachers such as school sports leaders should consider different learning domains and include administration, family and other courses in the programs. Health professionals or experts should carry out PA interventions with sports scientists. In most of the studies examined, it was seen that the intensity of exercise was not planned before the interventions. In order to increase health-related contributions, interveners need to pay attention to this issue. Nowadays, school time is more precious than ever. Sports scientists should have more contact with this field and participate more actively in designing school-based intervention programs.
5. Conclusions
School-based interventions can have important potential in the health promotion of children in terms of obesity, PA level and PF. However, the quality, duration, and priority of PA intervention in comprehensive school-based programs and teacher capacity are some of the most important factors for preventing obesity and promoting PA and PF. If more impact is desired in school-based intervention programs, the focus of the program should be PA and, as far as possible, physical activities should be implemented directly. To prevent obesity and to promote PA and PF, the characteristics of more effective programs should be examined in detail and appropriate intervention programs should be designed. Such programs should be multicomponent and longitudinal to foster children’s lifelong PA habits. This habit requires knowledge, skills and attitudes. Our study focuses on the aspect of skill (physical). Furthermore, future studies should also focus on knowledge and attitudes in order to demonstrate holistic understanding. At the same time, for children to adopt a habit of PA, issues such as motivation, physical competence and interaction with the environment, which are at the basis of the cycle according to physical literacy, are also important. In this sense, the role of school-based interventions in improving children’s physical literacy should also be examined.
Acknowledgments
We would like to thank Hakan Karabıyık and Özkan Güler from the Faculty of Sport Sciences at Ankara University for helping us do the quality assessments.
Supplementary Materials
Supplementary materials can be found at https://www.mdpi.com/1660-4601/17/1/347/s1 , Table S1: Quality assessment of 19 studies, File S2: Examples of Search Strategy.
Author Contributions
H.S.Y. participated in study design and conceptualization, contributed to methodology, validation, original draft preparation, and review and editing. F.N.Ş. contributed to the methodology and original draft preparation. N.M. contributed to the investigation, analysis, and data curation. P.D. contributed to the investigation, analysis, and visualization. A.B. participated in review and editing, contributed to visualization and supervision. The final manuscript has been approved by H.S.Y., F.N.Ş., N.M., P.D., and A.B. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.

IMAGES
VIDEO
COMMENTS
Sports in schools are important to maintain physical fitness among high school students and the quality of school physical education must be improved. During childhood and adolescence, sports participation in childhood is linked to Health-Related Quality of Life (HRQoL) in young adulthood, whether it is in the form of individual or team sports ...
Expanding physical education programs in schools should be considered an effective means of ... of 15 original studies involving randomized and nonrandomized trials with 13,003 children found a lack of favorable BMI outcomes for physical activity-based school interventions. ... This project was supported, in part, by Fundação de Amparo à ...
The relation between teaching physical education and discourses on body weight - an integrative review of research ... this crisis discourse problematises people's bodies and projects 'slim and slender' as the way to be healthy. The slim, ... which in turn is likely to lead to health-related fitness not seldom measured as BMI (Wrynn ...
There are ways to measure body fat percentage, such as skin fold tests or using BIA (Bioelectrical Impedance Analysis) device. Examples of a BIA device include a Tanita Scale or handheld device. Below is a tool to help you calculate your BMI and longer-term weight/health goals. BMI is calculated using only your height and weight. Keep in mind ….
schoolchildren spend only 9-42% of PE time engaged in moderate to vigorous physical activity 2 For children, overweight is defined as a body mass index (BMI) above the historic 85th percentile of the BMI distribution for youth of the same age and gender, and obesity is defined as a BMI above the historic 95th percentile (Barlow et al., 2007).
project was to answer the question: In school-aged children, how does school-based, structured, family-oriented physical activity education affect body mass index (BMI) compared to usual education over an eight-week time period? The Stetler Model of EBP and the health belief model were used to guide this project in a rural, Northwest Indiana
In physical education, Body Mass Index (BMI) is a measure of body fat based on height and weight. An individual with a BMI below 18.5 is considered underweight. Being underweight can result in health issues such as malnutrition, anemia, and weakened immune system.
This calculator provides BMI and the corresponding BMI-for-age percentile on a CDC BMI-for-age growth chart. Use this calculator for children and teens, aged 2 through 19 years old. The Children's BMI Tool for Schools. School staff, child care leaders, and other professionals can use this spreadsheet to compute BMI for as many as 2,000 children.
Body Mass Index (BMI) = Body weight / (height × height) Here the weight of the individual is measured in kilograms and the height is taken in metres. Example: Suppose an individual's body weight is 70 kg and his/her height is 1.60 m. Now compute these values. BMI = 70 / (1.60 x 1.60) = 70 / 2.56 = 27.34 kg/m2.
Therefore, the primary objectives of this investigation are to assess: (i) whether compulsory (curriculum mandated) physical education (PE) is associated with BMI in school pupils; (ii) the minimum duration for compulsory PE to cause a change in BW or BMI in school pupils; (iii) whether additional PA, sports, or exercise intervention (beside ...
There are two types of BMI measurement programs and each serves a specific purpose. ... Many factors beyond physical education and health education courses influence a student's weight, so it is not appropriate to hold students or teachers accountable for changes in BMI percentiles. ... the Cincinnati School Health Demonstration Project. J ...
This updated synthesis of obesity prevention interventions for children aged 6-18 years, found a small beneficial impact on child BMI for school-based obesity prevention interventions. A more comprehensive assessment of interventions is required to identify mechanisms of effective interventions to inform future obesity prevention public health policy, which may be particularly salient in for ...
Increasing the amount of time in PE up to the recommended amount of 150 minutes per week would lower BMI z-scores by 8% of a standard deviation, which is 12% of the mean, and would reduce the probability of obesity by four percentage points. Looking at gender we find that the reduction in BMI and obesity occurs only for boys.
These outcomes were primarily focused on BMI and/or body composition as primary outcomes of efficacy (10 studies), as well as secondary outcomes including health behaviours (12 studies), physical ...
Therefore, the primary objectives of this investigation are to assess: (i) whether compulsory (curriculum mandated) physical education (PE) is associated with BMI in school pupils; (ii) the minimum duration for compulsory PE to cause a change in BW or BMI in school pupils; (iii) whether additional PA, sports, or exercise intervention (beside ...
A total of 82 study and 26 control children completed the 2 years of the project. Boys in the control group gained significantly more weight than the corresponding study group (8.4 kg vs 3.2 kg ...
The BMI test is given by NUSD to fifth, seventh and ninth graders for the purpose of collecting data on students' wellness, and for high schoolers as one of the five tests they need to pass to complete Physical Education. The school BMI test takes a student's height and weight and calculates if they are in the "healthy fit" zone, or the ...
The Carol M. White Physical Education Program Project Implementation During Year 1 of the Grant . This brief was prepared for the U.S. Department of Education under Contract Number ED-04-CO-0025/0018 with the ... (BMI) data, a new PEP competitive preference priority. 1 •
Christopher's BMI of 25.1 put him in the obese range. In 2003, Arkansas became the first state to send home BMI reports about all students as part of a broader anti-obesity initiative.
Weekly group nutrition education sessions for the first 3 months, monthly for the last 3 months: Low a: Cleo et al, 2019, Australia (27) Mixed: In-person: university; Online: email: Participants aged 18-75 y, able to consent, BMI ≥25, could attend all required appointments, had access to email or telephone, and free from exercise-limiting ...
The Teruel Orthorexia Scale (TOS) defines two related but distinct constructs: Orthorexia Nervosa (OrNe), a pathological fixation on a healthy diet, and Healthy Orthorexia (HeOr), an interest in a healthy diet independent of psychopathology. Here, we (a) assessed both types of Orthorexia in a large North American sample using the TOS and (b) explored if engaging in regular physical activity ...
2. Materials and Methods. The framework used analytically by Kahn et al. [] and modified by Demetriou and Honer [] was organized and used particularly in this study.In this sense, the expected characteristics of the school-based interventions, the expected outcomes and the interventions that are accepted to be used outside of PA in such programs are presented in Figure 1.
Compared with people with BMI a < 25 in the group who were aged 65 years or younger, those with a BMI of 25.0-29.9 had a 13% higher risk for cardiovascular death.