An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.369; 2020

Food for Thought 2020
Food and mood: how do diet and nutrition affect mental wellbeing, joseph firth.
1 Division of Psychology and Mental Health, Faculty of Biology, Medicine and Health, Oxford Road, University of Manchester, Manchester M13 9PL, UK
2 NICM Health Research Institute, Western Sydney University, Westmead, Australia
James E Gangwisch
3 Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons, New York, USA
4 New York State Psychiatric Institute, New York, NY, USA
Alessandra Borsini
5 Section of Stress, Psychiatry and Immunology Laboratory, Institute of Psychiatry, Psychology and Neuroscience, Department of Psychological Medicine, King’s College London, London, UK
Robyn E Wootton
6 School of Psychological Science, University of Bristol, Bristol, UK
7 MRC Integrative Epidemiology Unit, Oakfield House, Bristol, UK
8 NIHR Biomedical Research Centre, University Hospitals Bristol NHS Foundation Trust and University of Bristol, Bristol, UK
Emeran A Mayer
9 G Oppenheimer Center for Neurobiology of Stress and Resilience, UCLA Vatche and Tamar Manoukian Division of Digestive Diseases, UCLA, Los Angeles, CA, USA
10 UCLA Microbiome Center, David Geffen School of Medicine, UCLA, Los Angeles, CA, USA
Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population, say Joseph Firth and colleagues
Key messages
- Healthy eating patterns, such as the Mediterranean diet, are associated with better mental health than “unhealthy” eating patterns, such as the Western diet
- The effects of certain foods or dietary patterns on glycaemia, immune activation, and the gut microbiome may play a role in the relationships between food and mood
- More research is needed to understand the mechanisms that link food and mental wellbeing and determine how and when nutrition can be used to improve mental health
Depression and anxiety are the most common mental health conditions worldwide, making them a leading cause of disability. 1 Even beyond diagnosed conditions, subclinical symptoms of depression and anxiety affect the wellbeing and functioning of a large proportion of the population. 2 Therefore, new approaches to managing both clinically diagnosed and subclinical depression and anxiety are needed.
In recent years, the relationships between nutrition and mental health have gained considerable interest. Indeed, epidemiological research has observed that adherence to healthy or Mediterranean dietary patterns—high consumption of fruits, vegetables, nuts, and legumes; moderate consumption of poultry, eggs, and dairy products; and only occasional consumption of red meat—is associated with a reduced risk of depression. 3 However, the nature of these relations is complicated by the clear potential for reverse causality between diet and mental health ( fig 1 ). For example, alterations in food choices or preferences in response to our temporary psychological state—such as “comfort foods” in times of low mood, or changes in appetite from stress—are common human experiences. In addition, relationships between nutrition and longstanding mental illness are compounded by barriers to maintaining a healthy diet. These barriers disproportionality affect people with mental illness and include the financial and environmental determinants of health, and even the appetite inducing effects of psychiatric medications. 4

Hypothesised relationship between diet, physical health, and mental health. The dashed line is the focus of this article.
While acknowledging the complex, multidirectional nature of the relationships between diet and mental health ( fig 1 ), in this article we focus on the ways in which certain foods and dietary patterns could affect mental health.
Mood and carbohydrates
Consumption of highly refined carbohydrates can increase the risk of obesity and diabetes. 5 Glycaemic index is a relative ranking of carbohydrate in foods according to the speed at which they are digested, absorbed, metabolised, and ultimately affect blood glucose and insulin levels. As well as the physical health risks, diets with a high glycaemic index and load (eg, diets containing high amounts of refined carbohydrates and sugars) may also have a detrimental effect on psychological wellbeing; data from longitudinal research show an association between progressively higher dietary glycaemic index and the incidence of depressive symptoms. 6 Clinical studies have also shown potential causal effects of refined carbohydrates on mood; experimental exposure to diets with a high glycaemic load in controlled settings increases depressive symptoms in healthy volunteers, with a moderately large effect. 7
Although mood itself can affect our food choices, plausible mechanisms exist by which high consumption of processed carbohydrates could increase the risk of depression and anxiety—for example, through repeated and rapid increases and decreases in blood glucose. Measures of glycaemic index and glycaemic load can be used to estimate glycaemia and insulin demand in healthy individuals after eating. 8 Thus, high dietary glycaemic load, and the resultant compensatory responses, could lower plasma glucose to concentrations that trigger the secretion of autonomic counter-regulatory hormones such as cortisol, adrenaline, growth hormone, and glucagon. 5 9 The potential effects of this response on mood have been examined in experimental human research of stepped reductions in plasma glucose concentrations conducted under laboratory conditions through glucose perfusion. These findings showed that such counter-regulatory hormones may cause changes in anxiety, irritability, and hunger. 10 In addition, observational research has found that recurrent hypoglycaemia (low blood sugar) is associated with mood disorders. 9
The hypothesis that repeated and rapid increases and decreases in blood glucose explain how consumption of refined carbohydrate could affect psychological state appears to be a good fit given the relatively fast effect of diets with a high glycaemic index or load on depressive symptoms observed in human studies. 7 However, other processes may explain the observed relationships. For instance, diets with a high glycaemic index are a risk factor for diabetes, 5 which is often a comorbid condition with depression. 4 11 While the main models of disease pathophysiology in diabetes and mental illness are separate, common abnormalities in insulin resistance, brain volume, and neurocognitive performance in both conditions support the hypothesis that these conditions have overlapping pathophysiology. 12 Furthermore, the inflammatory response to foods with a high glycaemic index 13 raises the possibility that diets with a high glycaemic index are associated with symptoms of depression through the broader connections between mental health and immune activation.
Diet, immune activation, and depression
Studies have found that sustained adherence to Mediterranean dietary patterns can reduce markers of inflammation in humans. 14 On the other hand, high calorie meals rich in saturated fat appear to stimulate immune activation. 13 15 Indeed, the inflammatory effects of a diet high in calories and saturated fat have been proposed as one mechanism through which the Western diet may have detrimental effects on brain health, including cognitive decline, hippocampal dysfunction, and damage to the blood-brain barrier. 15 Since various mental health conditions, including mood disorders, have been linked to heightened inflammation, 16 this mechanism also presents a pathway through which poor diet could increase the risk of depression. This hypothesis is supported by observational studies which have shown that people with depression score significantly higher on measures of “dietary inflammation,” 3 17 characterised by a greater consumption of foods that are associated with inflammation (eg, trans fats and refined carbohydrates) and lower intakes of nutritional foods, which are thought to have anti-inflammatory properties (eg, omega-3 fats). However, the causal roles of dietary inflammation in mental health have not yet been established.
Nonetheless, randomised controlled trials of anti-inflammatory agents (eg, cytokine inhibitors and non-steroidal anti-inflammatory drugs) have found that these agents can significantly reduce depressive symptoms. 18 Specific nutritional components (eg, polyphenols and polyunsaturated fats) and general dietary patterns (eg, consumption of a Mediterranean diet) may also have anti-inflammatory effects, 14 19 20 which raises the possibility that certain foods could relieve or prevent depressive symptoms associated with heightened inflammatory status. 21 A recent study provides preliminary support for this possibility. 20 The study shows that medications that stimulate inflammation typically induce depressive states in people treated, and that giving omega-3 fatty acids, which have anti-inflammatory properties, before the medication seems to prevent the onset of cytokine induced depression. 20
However, the complexity of the hypothesised three way relation between diet, inflammation, and depression is compounded by several important modifiers. For example, recent clinical research has observed that stressors experienced the previous day, or a personal history of major depressive disorders, may cancel out the beneficial effects of healthy food choices on inflammation and mood. 22 Furthermore, as heightened inflammation occurs in only some clinically depressed individuals, anti-inflammatory interventions may only benefit certain people characterised by an “inflammatory phenotype,” or those with comorbid inflammatory conditions. 18 Further interventional research is needed to establish if improvements in immune regulation, induced by diet, can reduce depressive symptoms in those affected by inflammatory conditions.
Brain, gut microbiome, and mood
A more recent explanation for the way in which our food may affect our mental wellbeing is the effect of dietary patterns on the gut microbiome—a broad term that refers to the trillions of microbial organisms, including bacteria, viruses, and archaea, living in the human gut. The gut microbiome interacts with the brain in bidirectional ways using neural, inflammatory, and hormonal signalling pathways. 23 The role of altered interactions between the brain and gut microbiome on mental health has been proposed on the basis of the following evidence: emotion-like behaviour in rodents changes with changes in the gut microbiome, 24 major depressive disorder in humans is associated with alterations of the gut microbiome, 25 and transfer of faecal gut microbiota from humans with depression into rodents appears to induce animal behaviours that are hypothesised to indicate depression-like states. 25 26 Such findings suggest a role of altered neuroactive microbial metabolites in depressive symptoms.
In addition to genetic factors and exposure to antibiotics, diet is a potentially modifiable determinant of the diversity, relative abundance, and functionality of the gut microbiome throughout life. For instance, the neurocognitive effects of the Western diet, and the possible mediating role of low grade systemic immune activation (as discussed above) may result from a compromised mucus layer with or without increased epithelial permeability. Such a decrease in the function of the gut barrier is sometimes referred to as a “leaky gut” and has been linked to an “unhealthy” gut microbiome resulting from a diet low in fibre and high in saturated fats, refined sugars, and artificial sweeteners. 15 23 27 Conversely, the consumption of a diet high in fibres, polyphenols, and unsaturated fatty acids (as found in a Mediterranean diet) can promote gut microbial taxa which can metabolise these food sources into anti-inflammatory metabolites, 15 28 such as short chain fatty acids, while lowering the production of secondary bile acids and p-cresol. Moreover, a recent study found that the ingestion of probiotics by healthy individuals, which theoretically target the gut microbiome, can alter the brain’s response to a task that requires emotional attention 29 and may even reduce symptoms of depression. 30 When viewed together, these studies provide promising evidence supporting a role of the gut microbiome in modulating processes that regulate emotion in the human brain. However, no causal relationship between specific microbes, or their metabolites, and complex human emotions has been established so far. Furthermore, whether changes to the gut microbiome induced by diet can affect depressive symptoms or clinical depressive disorders, and the time in which this could feasibly occur, remains to be shown.
Priorities and next steps
In moving forward within this active field of research, it is firstly important not to lose sight of the wood for the trees—that is, become too focused on the details and not pay attention to the bigger questions. Whereas discovering the anti-inflammatory properties of a single nutrient or uncovering the subtleties of interactions between the gut and the brain may shed new light on how food may influence mood, it is important not to neglect the existing knowledge on other ways diet may affect mental health. For example, the later consequences of a poor diet include obesity and diabetes, which have already been shown to be associated with poorer mental health. 11 31 32 33 A full discussion of the effect of these comorbidities is beyond the scope of our article (see fig 1 ), but it is important to acknowledge that developing public health initiatives that effectively tackle the established risk factors of physical and mental comorbidities is a priority for improving population health.
Further work is needed to improve our understanding of the complex pathways through which diet and nutrition can influence the brain. Such knowledge could lead to investigations of targeted, even personalised, interventions to improve mood, anxiety, or other symptoms through nutritional approaches. However, these possibilities are speculative at the moment, and more interventional research is needed to establish if, how, and when dietary interventions can be used to prevent mental illness or reduce symptoms in those living with such conditions. Of note, a recent large clinical trial found no significant benefits of a behavioural intervention promoting a Mediterranean diet for adults with subclinical depressive symptoms. 34 On the other hand, several recent smaller trials in individuals with current depression observed moderately large improvements from interventions based on the Mediterranean diet. 35 36 37 Such results, however, must be considered within the context of the effect of people’s expectations, particularly given that individuals’ beliefs about the quality of their food or diet may also have a marked effect on their sense of overall health and wellbeing. 38 Nonetheless, even aside from psychological effects, consideration of dietary factors within mental healthcare may help improve physical health outcomes, given the higher rates of cardiometabolic diseases observed in people with mental illness. 33
At the same time, it is important to be remember that the causes of mental illness are many and varied, and they will often present and persist independently of nutrition and diet. Thus, the increased understanding of potential connections between food and mental wellbeing should never be used to support automatic assumptions, or stigmatisation, about an individual’s dietary choices and their mental health. Indeed, such stigmatisation could be itself be a casual pathway to increasing the risk of poorer mental health. Nonetheless, a promising message for public health and clinical settings is emerging from the ongoing research. This message supports the idea that creating environments and developing measures that promote healthy, nutritious diets, while decreasing the consumption of highly processed and refined “junk” foods may provide benefits even beyond the well known effects on physical health, including improved psychological wellbeing.
Contributors and sources: JF has expertise in the interaction between physical and mental health, particularly the role of lifestyle and behavioural health factors in mental health promotion. JEG’s area of expertise is the study of the relationship between sleep duration, nutrition, psychiatric disorders, and cardiometabolic diseases. AB leads research investigating the molecular mechanisms underlying the effect of stress and inflammation on human hippocampal neurogenesis, and how nutritional components and their metabolites can prevent changes induced by those conditions. REW has expertise in genetic epidemiology approaches to examining casual relations between health behaviours and mental illness. EAM has expertise in brain and gut interactions and microbiome interactions. All authors contributed to, read, and approved the paper, and all the information was sourced from articles published in peer reviewed research journals. JF is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following: JF is supported by a University of Manchester Presidential Fellowship and a UK Research and Innovation Future Leaders Fellowship and has received support from a NICM-Blackmores Institute Fellowship. JEG served on the medical advisory board on insomnia in the cardiovascular patient population for the drug company Eisai. AB has received research funding from Johnson & Johnson for research on depression and inflammation, the UK Medical Research Council, the European Commission Horizon 2020, the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, and King’s College London. REW receives funding from the National Institute for Health Research Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. EAM has served on the external advisory boards of Danone, Viome, Amare, Axial Biotherapeutics, Pendulum, Ubiome, Bloom Science, Mahana Therapeutics, and APC Microbiome Ireland, and he receives royalties from Harper & Collins for his book The Mind Gut Connection. He is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and the US Department of Defense. The views expressed are those of the authors and not necessarily those of the organisations above.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of series commissioned by The BMJ. Open access fees are paid by Swiss Re, which had no input into the commissioning or peer review of the articles. T he BMJ thanks the series advisers, Nita Forouhi, Dariush Mozaffarian, and Anna Lartey for valuable advice and guiding selection of topics in the series.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Food and mood: how do...
Food and mood: how do diet and nutrition affect mental wellbeing?
Read our food for thought 2020 collection.
- Related content
- Peer review
This article has a correction. Please see:
- Food and mood: how do diet and nutrition affect mental wellbeing? - November 09, 2020
- Joseph Firth , research fellow 1 2 ,
- James E Gangwisch , assistant professor 3 4 ,
- Alessandra Borsini , researcher 5 ,
- Robyn E Wootton , researcher 6 7 8 ,
- Emeran A Mayer , professor 9 10
- 1 Division of Psychology and Mental Health, Faculty of Biology, Medicine and Health, Oxford Road, University of Manchester, Manchester M13 9PL, UK
- 2 NICM Health Research Institute, Western Sydney University, Westmead, Australia
- 3 Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons, New York, USA
- 4 New York State Psychiatric Institute, New York, NY, USA
- 5 Section of Stress, Psychiatry and Immunology Laboratory, Institute of Psychiatry, Psychology and Neuroscience, Department of Psychological Medicine, King’s College London, London, UK
- 6 School of Psychological Science, University of Bristol, Bristol, UK
- 7 MRC Integrative Epidemiology Unit, Oakfield House, Bristol, UK
- 8 NIHR Biomedical Research Centre, University Hospitals Bristol NHS Foundation Trust and University of Bristol, Bristol, UK
- 9 G Oppenheimer Center for Neurobiology of Stress and Resilience, UCLA Vatche and Tamar Manoukian Division of Digestive Diseases, UCLA, Los Angeles, CA, USA
- 10 UCLA Microbiome Center, David Geffen School of Medicine, UCLA, Los Angeles, CA, USA
- Correspondence to: J Firth joseph.firth{at}manchester.ac.uk
Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population, say Joseph Firth and colleagues
Key messages
Healthy eating patterns, such as the Mediterranean diet, are associated with better mental health than “unhealthy” eating patterns, such as the Western diet
The effects of certain foods or dietary patterns on glycaemia, immune activation, and the gut microbiome may play a role in the relationships between food and mood
More research is needed to understand the mechanisms that link food and mental wellbeing and determine how and when nutrition can be used to improve mental health
Depression and anxiety are the most common mental health conditions worldwide, making them a leading cause of disability. 1 Even beyond diagnosed conditions, subclinical symptoms of depression and anxiety affect the wellbeing and functioning of a large proportion of the population. 2 Therefore, new approaches to managing both clinically diagnosed and subclinical depression and anxiety are needed.
In recent years, the relationships between nutrition and mental health have gained considerable interest. Indeed, epidemiological research has observed that adherence to healthy or Mediterranean dietary patterns—high consumption of fruits, vegetables, nuts, and legumes; moderate consumption of poultry, eggs, and dairy products; and only occasional consumption of red meat—is associated with a reduced risk of depression. 3 However, the nature of these relations is complicated by the clear potential for reverse causality between diet and mental health ( fig 1 ). For example, alterations in food choices or preferences in response to our temporary psychological state—such as “comfort foods” in times of low mood, or changes in appetite from stress—are common human experiences. In addition, relationships between nutrition and longstanding mental illness are compounded by barriers to maintaining a healthy diet. These barriers disproportionality affect people with mental illness and include the financial and environmental determinants of health, and even the appetite inducing effects of psychiatric medications. 4

Hypothesised relationship between diet, physical health, and mental health. The dashed line is the focus of this article.
- Download figure
- Open in new tab
- Download powerpoint
While acknowledging the complex, multidirectional nature of the relationships between diet and mental health ( fig 1 ), in this article we focus on the ways in which certain foods and dietary patterns could affect mental health.
Mood and carbohydrates
Consumption of highly refined carbohydrates can increase the risk of obesity and diabetes. 5 Glycaemic index is a relative ranking of carbohydrate in foods according to the speed at which they are digested, absorbed, metabolised, and ultimately affect blood glucose and insulin levels. As well as the physical health risks, diets with a high glycaemic index and load (eg, diets containing high amounts of refined carbohydrates and sugars) may also have a detrimental effect on psychological wellbeing; data from longitudinal research show an association between progressively higher dietary glycaemic index and the incidence of depressive symptoms. 6 Clinical studies have also shown potential causal effects of refined carbohydrates on mood; experimental exposure to diets with a high glycaemic load in controlled settings increases depressive symptoms in healthy volunteers, with a moderately large effect. 7
Although mood itself can affect our food choices, plausible mechanisms exist by which high consumption of processed carbohydrates could increase the risk of depression and anxiety—for example, through repeated and rapid increases and decreases in blood glucose. Measures of glycaemic index and glycaemic load can be used to estimate glycaemia and insulin demand in healthy individuals after eating. 8 Thus, high dietary glycaemic load, and the resultant compensatory responses, could lower plasma glucose to concentrations that trigger the secretion of autonomic counter-regulatory hormones such as cortisol, adrenaline, growth hormone, and glucagon. 5 9 The potential effects of this response on mood have been examined in experimental human research of stepped reductions in plasma glucose concentrations conducted under laboratory conditions through glucose perfusion. These findings showed that such counter-regulatory hormones may cause changes in anxiety, irritability, and hunger. 10 In addition, observational research has found that recurrent hypoglycaemia (low blood sugar) is associated with mood disorders. 9
The hypothesis that repeated and rapid increases and decreases in blood glucose explain how consumption of refined carbohydrate could affect psychological state appears to be a good fit given the relatively fast effect of diets with a high glycaemic index or load on depressive symptoms observed in human studies. 7 However, other processes may explain the observed relationships. For instance, diets with a high glycaemic index are a risk factor for diabetes, 5 which is often a comorbid condition with depression. 4 11 While the main models of disease pathophysiology in diabetes and mental illness are separate, common abnormalities in insulin resistance, brain volume, and neurocognitive performance in both conditions support the hypothesis that these conditions have overlapping pathophysiology. 12 Furthermore, the inflammatory response to foods with a high glycaemic index 13 raises the possibility that diets with a high glycaemic index are associated with symptoms of depression through the broader connections between mental health and immune activation.
Diet, immune activation, and depression
Studies have found that sustained adherence to Mediterranean dietary patterns can reduce markers of inflammation in humans. 14 On the other hand, high calorie meals rich in saturated fat appear to stimulate immune activation. 13 15 Indeed, the inflammatory effects of a diet high in calories and saturated fat have been proposed as one mechanism through which the Western diet may have detrimental effects on brain health, including cognitive decline, hippocampal dysfunction, and damage to the blood-brain barrier. 15 Since various mental health conditions, including mood disorders, have been linked to heightened inflammation, 16 this mechanism also presents a pathway through which poor diet could increase the risk of depression. This hypothesis is supported by observational studies which have shown that people with depression score significantly higher on measures of “dietary inflammation,” 3 17 characterised by a greater consumption of foods that are associated with inflammation (eg, trans fats and refined carbohydrates) and lower intakes of nutritional foods, which are thought to have anti-inflammatory properties (eg, omega-3 fats). However, the causal roles of dietary inflammation in mental health have not yet been established.
Nonetheless, randomised controlled trials of anti-inflammatory agents (eg, cytokine inhibitors and non-steroidal anti-inflammatory drugs) have found that these agents can significantly reduce depressive symptoms. 18 Specific nutritional components (eg, polyphenols and polyunsaturated fats) and general dietary patterns (eg, consumption of a Mediterranean diet) may also have anti-inflammatory effects, 14 19 20 which raises the possibility that certain foods could relieve or prevent depressive symptoms associated with heightened inflammatory status. 21 A recent study provides preliminary support for this possibility. 20 The study shows that medications that stimulate inflammation typically induce depressive states in people treated, and that giving omega-3 fatty acids, which have anti-inflammatory properties, before the medication seems to prevent the onset of cytokine induced depression. 20
However, the complexity of the hypothesised three way relation between diet, inflammation, and depression is compounded by several important modifiers. For example, recent clinical research has observed that stressors experienced the previous day, or a personal history of major depressive disorders, may cancel out the beneficial effects of healthy food choices on inflammation and mood. 22 Furthermore, as heightened inflammation occurs in only some clinically depressed individuals, anti-inflammatory interventions may only benefit certain people characterised by an “inflammatory phenotype,” or those with comorbid inflammatory conditions. 18 Further interventional research is needed to establish if improvements in immune regulation, induced by diet, can reduce depressive symptoms in those affected by inflammatory conditions.
Brain, gut microbiome, and mood
A more recent explanation for the way in which our food may affect our mental wellbeing is the effect of dietary patterns on the gut microbiome—a broad term that refers to the trillions of microbial organisms, including bacteria, viruses, and archaea, living in the human gut. The gut microbiome interacts with the brain in bidirectional ways using neural, inflammatory, and hormonal signalling pathways. 23 The role of altered interactions between the brain and gut microbiome on mental health has been proposed on the basis of the following evidence: emotion-like behaviour in rodents changes with changes in the gut microbiome, 24 major depressive disorder in humans is associated with alterations of the gut microbiome, 25 and transfer of faecal gut microbiota from humans with depression into rodents appears to induce animal behaviours that are hypothesised to indicate depression-like states. 25 26 Such findings suggest a role of altered neuroactive microbial metabolites in depressive symptoms.
In addition to genetic factors and exposure to antibiotics, diet is a potentially modifiable determinant of the diversity, relative abundance, and functionality of the gut microbiome throughout life. For instance, the neurocognitive effects of the Western diet, and the possible mediating role of low grade systemic immune activation (as discussed above) may result from a compromised mucus layer with or without increased epithelial permeability. Such a decrease in the function of the gut barrier is sometimes referred to as a “leaky gut” and has been linked to an “unhealthy” gut microbiome resulting from a diet low in fibre and high in saturated fats, refined sugars, and artificial sweeteners. 15 23 27 Conversely, the consumption of a diet high in fibres, polyphenols, and unsaturated fatty acids (as found in a Mediterranean diet) can promote gut microbial taxa which can metabolise these food sources into anti-inflammatory metabolites, 15 28 such as short chain fatty acids, while lowering the production of secondary bile acids and p-cresol. Moreover, a recent study found that the ingestion of probiotics by healthy individuals, which theoretically target the gut microbiome, can alter the brain’s response to a task that requires emotional attention 29 and may even reduce symptoms of depression. 30 When viewed together, these studies provide promising evidence supporting a role of the gut microbiome in modulating processes that regulate emotion in the human brain. However, no causal relationship between specific microbes, or their metabolites, and complex human emotions has been established so far. Furthermore, whether changes to the gut microbiome induced by diet can affect depressive symptoms or clinical depressive disorders, and the time in which this could feasibly occur, remains to be shown.
Priorities and next steps
In moving forward within this active field of research, it is firstly important not to lose sight of the wood for the trees—that is, become too focused on the details and not pay attention to the bigger questions. Whereas discovering the anti-inflammatory properties of a single nutrient or uncovering the subtleties of interactions between the gut and the brain may shed new light on how food may influence mood, it is important not to neglect the existing knowledge on other ways diet may affect mental health. For example, the later consequences of a poor diet include obesity and diabetes, which have already been shown to be associated with poorer mental health. 11 31 32 33 A full discussion of the effect of these comorbidities is beyond the scope of our article (see fig 1 ), but it is important to acknowledge that developing public health initiatives that effectively tackle the established risk factors of physical and mental comorbidities is a priority for improving population health.
Further work is needed to improve our understanding of the complex pathways through which diet and nutrition can influence the brain. Such knowledge could lead to investigations of targeted, even personalised, interventions to improve mood, anxiety, or other symptoms through nutritional approaches. However, these possibilities are speculative at the moment, and more interventional research is needed to establish if, how, and when dietary interventions can be used to prevent mental illness or reduce symptoms in those living with such conditions. Of note, a recent large clinical trial found no significant benefits of a behavioural intervention promoting a Mediterranean diet for adults with subclinical depressive symptoms. 34 On the other hand, several recent smaller trials in individuals with current depression observed moderately large improvements from interventions based on the Mediterranean diet. 35 36 37 Such results, however, must be considered within the context of the effect of people’s expectations, particularly given that individuals’ beliefs about the quality of their food or diet may also have a marked effect on their sense of overall health and wellbeing. 38 Nonetheless, even aside from psychological effects, consideration of dietary factors within mental healthcare may help improve physical health outcomes, given the higher rates of cardiometabolic diseases observed in people with mental illness. 33
At the same time, it is important to be remember that the causes of mental illness are many and varied, and they will often present and persist independently of nutrition and diet. Thus, the increased understanding of potential connections between food and mental wellbeing should never be used to support automatic assumptions, or stigmatisation, about an individual’s dietary choices and their mental health. Indeed, such stigmatisation could be itself be a casual pathway to increasing the risk of poorer mental health. Nonetheless, a promising message for public health and clinical settings is emerging from the ongoing research. This message supports the idea that creating environments and developing measures that promote healthy, nutritious diets, while decreasing the consumption of highly processed and refined “junk” foods may provide benefits even beyond the well known effects on physical health, including improved psychological wellbeing.
Contributors and sources: JF has expertise in the interaction between physical and mental health, particularly the role of lifestyle and behavioural health factors in mental health promotion. JEG’s area of expertise is the study of the relationship between sleep duration, nutrition, psychiatric disorders, and cardiometabolic diseases. AB leads research investigating the molecular mechanisms underlying the effect of stress and inflammation on human hippocampal neurogenesis, and how nutritional components and their metabolites can prevent changes induced by those conditions. REW has expertise in genetic epidemiology approaches to examining casual relations between health behaviours and mental illness. EAM has expertise in brain and gut interactions and microbiome interactions. All authors contributed to, read, and approved the paper, and all the information was sourced from articles published in peer reviewed research journals. JF is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following: JF is supported by a University of Manchester Presidential Fellowship and a UK Research and Innovation Future Leaders Fellowship and has received support from a NICM-Blackmores Institute Fellowship. JEG served on the medical advisory board on insomnia in the cardiovascular patient population for the drug company Eisai. AB has received research funding from Johnson & Johnson for research on depression and inflammation, the UK Medical Research Council, the European Commission Horizon 2020, the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, and King’s College London. REW receives funding from the National Institute for Health Research Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. EAM has served on the external advisory boards of Danone, Viome, Amare, Axial Biotherapeutics, Pendulum, Ubiome, Bloom Science, Mahana Therapeutics, and APC Microbiome Ireland, and he receives royalties from Harper & Collins for his book The Mind Gut Connection. He is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and the US Department of Defense. The views expressed are those of the authors and not necessarily those of the organisations above.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of series commissioned by The BMJ. Open access fees are paid by Swiss Re, which had no input into the commissioning or peer review of the articles. T he BMJ thanks the series advisers, Nita Forouhi, Dariush Mozaffarian, and Anna Lartey for valuable advice and guiding selection of topics in the series.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Friedrich MJ
- Johnson J ,
- Weissman MM ,
- Lassale C ,
- Baghdadli A ,
- Siddiqi N ,
- Koyanagi A ,
- Gangwisch JE ,
- Salari-Moghaddam A ,
- Larijani B ,
- Esmaillzadeh A
- de Jong V ,
- Atkinson F ,
- Brand-Miller JC
- Seaquist ER ,
- Anderson J ,
- American Diabetes Association ,
- Endocrine Society
- Towler DA ,
- Havlin CE ,
- McIntyre RS ,
- Nguyen HT ,
- O’Keefe JH ,
- Gheewala NM ,
- Kastorini C-M ,
- Milionis HJ ,
- Esposito K ,
- Giugliano D ,
- Goudevenos JA ,
- Panagiotakos DB
- Teasdale SB ,
- Köhler-Forsberg O ,
- N Lydholm C ,
- Hjorthøj C ,
- Nordentoft M ,
- Yahfoufi N ,
- Borsini A ,
- Horowitz MA ,
- Kiecolt-Glaser JK ,
- Fagundes CP ,
- Andridge R ,
- Osadchiy V ,
- Martin CR ,
- O’Brien C ,
- Sonnenburg ED ,
- Sonnenburg JL
- Rampelli S ,
- Jeffery IB ,
- Tillisch K ,
- Kilpatrick L ,
- Walsh RFL ,
- Wootton RE ,
- Millard LAC ,
- Jebeile H ,
- Garnett SP ,
- Paxton SJ ,
- Brouwer IA ,
- MooDFOOD Prevention Trial Investigators
- Francis HM ,
- Stevenson RJ ,
- Chambers JR ,
- Parletta N ,
- Zarnowiecki D ,
- Fischler C ,
- Sarubin A ,
- Wrzesniewski A
- Harrington D ,
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 20 November 2023
The triple burden of malnutrition
Nature Food volume 4 , page 925 ( 2023 ) Cite this article
2647 Accesses
1 Citations
3 Altmetric
Metrics details
Today’s nutrition crisis is a manifestation of the broader malfunctioning of our global food system. The specific factors linking the two warrant further investigation.
The world is facing an unprecedented crisis in which overnutrition (overweight and obesity), undernutrition (stunting, wasting and underweight) and micronutrient deficiencies (often referred to as ‘hidden hunger’) coexist within the same population. This triple burden of malnutrition is a major public health challenge. The numbers speak for themselves: 51% of the world’s population over five years of age is predicted to be obese or overweight by 2035 if the status quo is maintained while, paradoxically, one in five children under the age of five years is stunted.

Connecting overnutrition, undernutrition and micronutrient deficiencies is the food system’s inability to provide equitable access to healthy diets for all. A recent analysis of anthropometric and demographic data from 55 low- and middle-income countries has shown that economic globalization is associated with the simultaneous occurrence of overnutrition and undernutrition, particularly among the poorest households of poorer countries (Seferidi, P. et al., Lancet Glob. Health 10 , E482–E490; 2022). Factors such as non-resilient food supply chains, persistent food loss and waste, economic crises, conflicts and extreme weather events pose additional threats. At the same time, the increasing accessibility of ultra-processed foods at lower prices than processed or unprocessed foods widens the gap in access to a healthy diet between high-income and low-income individuals.
Scientific evidence on the above factors and their interplay is key to support food system change towards ending malnutrition in all its forms. This issue of Nature Food features five primary research articles that aim to contribute to this goal.
Fadnes et al. use prospective population-based cohort data to show that sustained dietary changes can increase life expectancy by up to 10 years. The study reveals that the largest gains are associated with increased consumption of whole grains, nuts and fruits and reduced consumption of processed meats and sugar-sweetened beverages.
While these are considerable health gains, implementing dietary changes at the population level remains a challenge, given that the determinants of food choice are multifactorial — including, among others, culture, religion, personal preferences and economics (G. Leng et al., Proc. Nutr. Soc . 76 , 316–327; 2017). Recognizing that, in this issue, Grummon et al. propose an approach based on simple and actionable dietary substitutions that are more likely to be incorporated into people’s daily habits and benefit the health of the global population.
The responsibility for malnutrition lies on individual as much as collective choices. Relying solely on the former, without due consideration of what needs to be transformed in the food environment, might constrain progress towards better diets. Effective policies that make healthy food and water universally accessible while disincentivizing the consumption of unhealthy foods are essential to address these concerns on a global scale. A systematic scoping review by Alvarado et al. in this issue summarizes existing evidence on sugar-sweetened beverage taxation, an important contributor to overweight and obesity.
In addition to the obesity epidemic, micronutrient deficiencies of minerals (iodine, zinc and iron) and/or vitamins (vitamin A, vitamin B 12 and folate) have health consequences throughout the life cycle and not just in children. Based on a production–consumption–nutrition model, Wang et al. show that the food domestically available for consumption is insufficient to meet people’s needs for 9 different micronutrients in more than half of the 156 countries studied.
Finally, although biofortification of staple crops is a necessary strategy to increase accessibility to nutritious food, the latter can’t be achieved without ensuring the retention of micronutrients in food at the point of consumption. Huey et al. present an online interactive micronutrient retention dashboard that provides an overview of the retention of provitamin A, iron and zinc in food across crop processing methods. This new resource will benefit households, regulatory entities and implementers of biofortification programmes.
We hope you enjoy reading!
Rights and permissions
Reprints and permissions
About this article
Cite this article.
The triple burden of malnutrition. Nat Food 4 , 925 (2023). https://doi.org/10.1038/s43016-023-00886-8
Download citation
Published : 20 November 2023
Issue Date : November 2023
DOI : https://doi.org/10.1038/s43016-023-00886-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Home
Americans poor diet drives $50 billion a year in health care costs
An #NHLBI-funded study put a price tag on American's bad eating habits: $50 billion a year in health care costs, attributable to cardiometabolic diseases such as heart disease, stroke and type 2 diabetes. The research, reported in the journal PLoS Medicine , sought to zero in on the national health care costs of unhealthy diet habits, which are known to account for up to 45% of all cardiometabolic deaths.
The researchers examined the impact of 10 food groups - fruits, vegetables, nuts/seeds, whole grains, unprocessed red meats, processed meats, sugar-sweetened beverages, polyunsaturated fats, seafood omega-3 fats and sodium - and found that almost 20% of heart disease, stroke and diabetes costs are due to poor diet.
Three dietary factors contributed most to these costs: consumption of processed meats, low consumption of nuts/seeds, and low consumption of seafoods containing omega-3 fats.
Media Coverage
- Health Care Costs Of Unhealthy American Diet? At Least $50B A Year, Study Estimates
- Unhealthy Eating Habits Cost U.S. $50 Billion a Year: Study
- Suboptimal Diet May Drive $50 Billion in Cardiometabolic Costs
- Better diets could save billions in U.S. health care costs
- Unhealthy eating costs $50B a year in health care costs
- Poor Diet Contributes Substantially to Cardiometabolic Disease Costs
- Healthy Diet Could Save $50B in Health Care Costs
- Cardiometabolic disease costs associated with suboptimal diet in the United States: A cost analysis based on a microsimulation model
Poor Nutrition

Measure Breastfeeding Practices and Eating Patterns
Support breastfeeding in the hospital and community, offer healthier food options in early care and education facilities and schools, offer healthier food options in the workplace, improve access to healthy foods in states and communities, support lifestyle change programs to reduce obesity and type 2 diabetes risk.
Good nutrition is essential to keeping current and future generations healthy across the lifespan. A healthy diet helps children grow and develop properly and reduces their risk of chronic diseases. Adults who eat a healthy diet live longer and have a lower risk of obesity, heart disease, type 2 diabetes, and certain cancers. Healthy eating can help people with chronic diseases manage these conditions and avoid complications.
However, when healthy options are not available, people may settle for foods that are higher in calories and lower in nutritional value. People in low-income communities and some racial and ethnic groups often lack access to convenient places that offer affordable, healthier foods.
Most people in the United States don’t eat a healthy diet and consume too much sodium, saturated fat, and sugar, increasing their risk of chronic diseases. For example, fewer than 1 in 10 adolescents and adults eat enough fruits or vegetables. In addition, 6 in 10 young people aged 2 to 19 years and 5 in 10 adults consume at least one sugary drink on any given day.
CDC supports breastfeeding and works to improve access to healthier food and drink choices in settings such as early care and education facilities, schools, worksites, and communities.
In the United States:

3 IN 4 INFANTS
are not exclusively breastfed for 6 months.

9 IN 10 AMERICANS
consume too much sodium.

1 in 6 PREGNANT WOMEN
have iron levels that are too low.

NEARLY $173 BILLION
a year is spent on health care for obesity.
The Harmful Effects of Poor Nutrition
Overweight and obesity.
Eating a healthy diet, along with getting enough physical activity and sleep, can help children grow up healthy and prevent overweight and obesity. In the United States, 20% of young people aged 2 to 19 years and 42% of adults have obesity, which can put them at risk of heart disease, type 2 diabetes, and some cancers.
Heart Disease and Stroke

Two of the leading causes of heart disease and stroke are high blood pressure and high blood cholesterol. Consuming too much sodium can increase blood pressure and the risk for heart disease and stroke . Current guidelines recommend getting less than 2,300 mg a day, but Americans consume more than 3,400 mg a day on average.
Over 70% of the sodium that Americans eat comes from packaged, processed, store-bought, and restaurant foods. Eating foods low in saturated fats and high in fiber and increasing access to low-sodium foods, along with regular physical activity, can help prevent high blood cholesterol and high blood pressure.
Type 2 Diabetes
People who are overweight or have obesity are at increased risk of type 2 diabetes compared to those at a healthybecause, over time, their bodies become less able to use the insulin they make. Of US adults, 96 million—more than 1 in 3—have prediabetes , and more than 8 in 10 of them don’t know they have it. Although the rate of new cases has decreased in recent years, the number of adults with diagnosed diabetes has nearly doubled in the last 2 decades as the US population has increased, aged, and become more overweight.
An unhealthy diet can increase the risk of some cancers. Consuming unhealthy food and beverages, such as sugar-sweetened beverages and highly processed food, can lead to weight gain, obesity and other chronic conditions that put people at higher risk of at least 13 types of cancer, including endometrial (uterine) cancer, breast cancer in postmenopausal women, and colorectal cancer. The risk of colorectal cancer is also associated with eating red and processed meat.
CDC’s Work to Promote Good Nutrition
CDC’s Division of Nutrition, Physical Activity, and Obesity uses national and state surveys to track breastfeeding rates and eating patterns across the country, including fruit, vegetable, and added sugar consumption. The division also reports data on nutrition policies and practices for each state. Data from these surveys are used to understand trends in nutrition and differences between population groups.
CDC partners use this information to help support breastfeeding and encourage healthy eating where people live, learn, work, and play, especially for populations at highest risk of chronic disease.

Breastfeeding is the best source of nutrition for most infants. It can reduce the risk of some short-term health conditions for infants and long-term health conditions for infants and mothers. Maternity care practices in the first hours and days after birth can influence whether and how long infants are breastfed.
CDC funds programs that help hospitals use maternity care practices that support breastfeeding . These programs have helped increase the percentage of infants born in hospitals that implement recommended practices 1. CDC also works with partners to support programs designed to improve continuity of care and community support for breastfeeding mothers.

Nearly 56 million US children spend time in early care and education (ECE) facilities or public schools. These settings can directly influence what children eat and drink and how active they are—and build a foundation for healthy habits.
CDC is helping our nation’s children grow up healthy and strong by:
- Creating resources to help partners improve obesity prevention programs and use nutrition standards.
- Investing in training and learning networks that help child care providers and state and local child care leaders meet standards and use and share best practices .
- Providing technical assistance, such as training school staff how to buy, prepare, and serve fruits and vegetables or teach children how to grow and prepare fruits and vegetables.
The CDC Healthy Schools program works with states, school systems, communities, and national partners to promote good nutrition . These efforts include publishing guidelines and tips on how schools and parents can model healthy behaviors and offer healthier school meals, smart snacks , and water access.
CDC also works with national groups to increase the number of salad bars in schools. As of 2021, the Salad Bars to School program has delivered almost 6,000 salad bars to schools across the nation, giving over 2.9 million children and school staff better access to fruits and vegetables.
Millions of US adults buy foods and drinks while at work. CDC develops and promotes food service guidelines that encourage employers and vendors to increase healthy food options for employees. CDC-funded programs are working to make healthy foods and drinks (including water) more available in cafeterias, snack shops, and vending machines. CDC also partners with states to help employers comply with the federal lactation accommodation law and provide breastfeeding mothers with places to pump and store breast milk, flexible work hours, and maternity leave benefits.

People living in low-income urban neighborhoods, rural areas, and tribal communities often have little access to affordable, healthy foods such as fruits and vegetables. CDC’s State Physical Activity and Nutrition Program , High Obesity Program , and Racial and Ethnic Approaches to Community Health program fund states and communities to improve food systems in these areas through food hubs, local stores, farmers’ markets, and bodegas.
These programs, which also involve food vendors and distributors, help increase the variety and number of healthier foods and drinks available and help promote and market these items to customers.
CDC’s National Diabetes Prevention Program (National DPP) is a partnership of public and private organizations working to build a nationwide delivery system for a lifestyle change program proven to prevent or delay type 2 diabetes in adults with prediabetes. Participants in the National DPP lifestyle change program learn to make healthy food choices, be more physically active, and find ways to cope with stress. These changes can cut their risk of developing type 2 diabetes by as much as 58% (71% for those over 60).
Social_govd
Get Email Updates
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Open access
- Published: 08 September 2023
Nutrition interventions to address nutritional problems in HIV-positive patients: translating knowledge into practice
- Leila Rezazadeh 1 ,
- Alireza Ostadrahimi 2 ,
- Helda Tutunchi 3 ,
- Mohammad Naemi Kermanshahi 4 &
- Samira Pourmoradian 5
Journal of Health, Population and Nutrition volume 42 , Article number: 94 ( 2023 ) Cite this article
2639 Accesses
1 Citations
2 Altmetric
Metrics details
Human immunodeficiency virus (HIV) infection and malnutrition negatively reinforce each other. Malnutrition leads to further immune deficiency and accelerates disease progression. The present overview aimed to investigate the current knowledge from review articles on the role of nutrition interventions as well as food and nutrition policies on HIV-related outcomes in adults to present future strategies for strengthening food and nutrition response to HIV.
We searched PubMed/Medline, Scopus, Embase, ProQuest, and Ovid databases using the relevant keywords. The search was limited to studies published in English until April 2022. All types of reviews studies (systematic review, narrative review, and other types of review studies) which evaluated the impact of nutritional program/interventions on HIV progression were included.
Although nutrition programs in HIV care have resulted in improvements in nutritional symptoms and increase the quality life of HIV patients, these programs should evaluate the nutritional health of HIV-infected patients in a way that can be sustainable in the long term. In additions, demographic, clinical, and nutritional, social characteristics influence nutritional outcomes, which provide potential opportunities for future research.
Nutrition assessment, education and counseling, and food supplements where necessary should be an integral part of HIV treatment programs.
Human immunodeficiency virus (HIV) is a serious communicable disease characterized by immunodeficiency and other complications that increase mortality rate in these patients. In 2020, it was estimated that the people living with HIV were 37.7 million worldwide, and 1.5 million people became newly infected with HIV [ 1 ]. According to the World Health Organization, HIV-related deaths were estimated about 630,000 cases by 2022. The prevalence of malnutrition (undernutrition) in HIV patients in some African countries is over 25% [ 2 ].
HIV is known by immune system suppression which increases energy requirement to combat infection in undernourished HIV patients, leading to further nutritional problems [ 3 , 4 ]. Malnutrition is an important health issue in patients living with HIV. Malnutrition leads to physiological, psychological, and functional disorders. In addition, malnutrition contributes to further immune deficiency and accelerates disease progression. The underlying causes of malnutrition in HIV-infected person are related to reduced food intake, poor absorption, changes in metabolism, chronic infections, and illnesses [ 5 ]. Adequate nutrition, which provides sufficient calories by macronutrients (proteins, carbohydrates and fats) and micronutrients (vitamins and minerals), is important to increase resistance to infection, maintain nutritional status of patients, help to delay the progression of HIV, and improve quality of life [ 4 , 6 , 7 ].
In developing countries, poor nutrition status and food insecurity increase individuals’ susceptibility to infectious diseases, as well as viral load, sexual, and vertical transmission of HIV [ 8 ]. Nutrition interventions including supplementation with macro- and micronutrients, nutrition education, or counseling and food assistance programs are essential for HIV-positive persons to improve nutrient intake and reduce viral load by enhancing immunity [ 9 , 10 , 11 ].
To date, several review and systematic review studies have evaluated the effectiveness of such interventions on nutritional status of HIV. Considering sociodemographic, clinical and nutritional characteristics of various populations can influence the nutritional outcomes that provide potential opportunities for improvement in future research and programs. As far as we know, there is no overview to summarize the results of these review studies. Therefore, the present overview aimed to investigate the current knowledge from review articles on the role of nutrition interventions as well as food and nutrition policies on HIV-related outcomes in adults to present future strategies for strengthening food and nutrition response to HIV.
Material and methods
For the purposes of this overview, we searched PubMed/Medline, Scopus, Embase, ProQuest, and Ovid from 2000/01/01 until 2022/04/30. We developed and performed the literature search (MN, LR).
Only publications with English language were included.
Search strategy included combinations of the following terms:
“HIV” OR “human immunodeficiency virus*” OR “HIV” OR “People Living with HIV” OR “PLWHIV” OR “PLHIV” OR “HIV-positive” OR” HIV positive” AND “Nutrition program” OR “Nutritional intervention” OR “Nutrition education” OR “Micronutrient supplementation” OR “Macronutrient supplementation” OR “Ready to use Therapeutic food” OR “complementary therapy” OR “food assistance program”.
Gray literature (e.g., conference papers, theses, interviews, protocols, comments, and short communications) was obtained through Google searches and Elsevier (first 20 pages of results). Apart from electronic search, manual search of the reference lists of the eligible papers and relevant review articles were conducted to avoid missing relevant studies.
Inclusion and exclusion criteria
Two of the authors (HT and SP) screened the title and abstract of all studies found in the systematic search to identify studies that met our criteria for inclusion in the present study. Systematic review which evaluated the impact of nutritional program/interventions on HIV progression was included. However, studies which examined nutrition intervention on children with HIV and also pregnant and lactation women were excluded.

Quality assessment of included reviews
Two authors (OA and LR) assessed the quality of included SRs using A Measurement Tool to Checklist Assess Systematic Reviews 2 (AMSTAR 2). AMSTAR2 is a practical appraisal tool for SRs performed on randomized and/or nonrandomized studies of healthcare interventions. It contains16 domains. Each question was answered with “yes,” “no,” “cannot answer,” or “not applicable.” According to the answers, only the “yes” answer counted as a point in the total score for the assessed study. Thus, the meta-analyses with at least 80% of the items were categorized as high quality and those SRs between 40 and 80% scores were considered as moderate quality, and those with < 40% of the items were satisfied as low quality [ 12 ].
Characteristics of included studies
After excluding duplicates and irrelevant studies based on screening of the title and abstract, 30 full-text articles were reviewed in detail for eligibility and finally 5 studies met our specified inclusion criteria. The PRISMA flowchart of the study is shown in Fig. 1 .
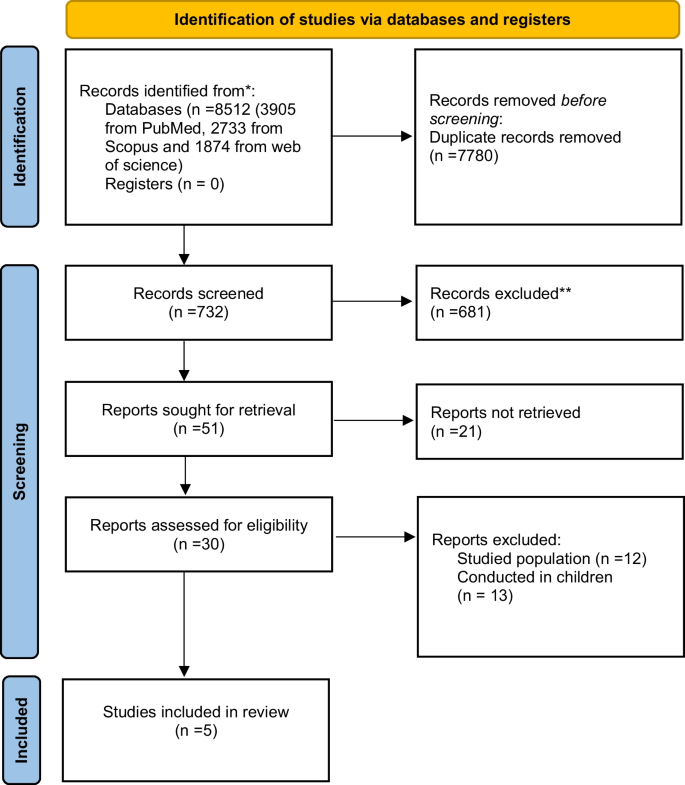
The PRISMA flowchart of the study
Table 1 shows the characteristics of the five included SRs of the effects of nutritional program/interventions in HIV-positive adults [ 10 , 13 , 14 , 15 , 16 ]. The nutrition interventions for HIV patients are classified into three groups including education/counseling, supplementation with macro- and micronutrients, and food and nutrition supporting programs. Two of five included SRs were Cochrane systematic reviews [ 13 , 15 ]. Most of the included studies were searched at least two databases including Embase and PubMed/Medline.
The three of included SRs were assessed the macronutrient supplementation in HIV-positive adults [ 13 , 14 , 15 ]. Two studies conducted by Tesfay et al. [ 10 ] and Tong et al. [ 16 ] were evaluated nutrition assessment, counseling, and support (NACS) interventions.
The primary outcomes of included studies were weight, BMI, fat-free mass, fat mass, viral load, CD4 count, and dietary intake.
The intervention location in the most of the included SRs was outpatients clinics or community-based settings [ 13 , 14 , 15 ]. Furthermore, in the two SRs, the multiple setting interventions (conducted in the hospital and outpatient clinic or community-based settings) were included [ 10 , 16 ].
Methodological quality of the included reviews
The methodological quality of included SRs articles is depicted in Table 2 . According to AMSTAR2 quality assessment tool, SRs conducted by Grobler et al. [ 13 ], Mahlungulu et al. [ 15 ] which were Cochrane systematic reviews had high quality. The Hong et al. [ 14 ] and Tang et al. [ 16 ] studies had moderate quality, and only one of them possess low quality [ 10 ] (Table 2 ).
Nutritional intervention plays a crucial role in the management of HIV infection. People living with HIV often experience malnutrition and weight loss due to various factors such as decreased appetite, nutrient malabsorption, increased energy expenditure, and opportunistic infections [ 17 ]. Nutritional intervention is a critical component of the overall management of HIV infection. It helps support immune function, prevent malnutrition, and improve overall health outcomes for individuals living with HIV. Here, we discuss our findings in three sections.
Nutrition education/counseling
Nutrition education or counseling has been shown to assist and improve dietary intake and nutritional status in HIV-positive adults in different settings by increasing individual knowledge about healthy food choices [ 10 , 13 , 14 , 15 , 16 ]. In studies conducted by Grobler et al. [ 13 ], Mahlungulu et al. [ 15 ], nutrition education or counseling was one component of the nutritional programs in HIV-positive patients.
Despite the value of nutrition education/counseling in HIV treatment programs, there is little research in this field. Nutrition counseling as a cost-effective intervention especially in developing countries with limited resources and high prevalence of nutritional deficiencies must be in the first line of nutrition intervention in HIV management [ 8 ]. To improve the health and nutrition status of people living with HIV, the expertise of a registered dietitian/nutritionist as part of the health care team should be considered.
Supplementation with macro- and micronutrients
Based on previous evidences, reduction of serum antioxidant vitamins and minerals was reported during the progression of HIV with high oxidative stress. So, intervention with foods and supplements including macro- and micronutrients is necessary for strengthen the immune system. Furthermore, people with HIV should be aware of health benefits of essential nutrients along with lifestyle changes to improve nutritional status and the immune system [ 18 ]. The effectiveness of supplementation with macro- and micronutrients was reviewed by Hong et al. to improve immune defense system and quality of life of HIV patients. They found that supplementation with selenium, zinc, iron, probiotic, vitamins A, B, C, and E improved quality of life and immunity in HIV-infected patients. Furthermore, Hong et al. [ 14 ] showed that protein-energy-fortified macronutrient supplements led to significant changes in nutritional status and immunological response in HIV disease.
Given the potential effectiveness of the supplementation of macronutrients and micronutrients in HIV, it is necessary to establish national guidelines for health care provider as well as evaluating socio-psychophysiological status to assist in their clinical decision in terms of improving nutritional status and immunologic responses [ 14 ].
Multiple interventions
Adequate nutrition is recognized as a key component in the care and support for people living with HIV due to the high prevalence of clinical undernutrition and food insecurity. There is a strong association between malnutrition and increased mortality rate in HIV-infected patients [ 19 ].
According to the nutrition requirement guideline of the World Health Organization (WHO), providing a balanced healthy diet as well as increasing energy intakes by approximately 20% to 30% to maintain body weight is vital for health and survival in individuals with HIV [ 20 ].
Nutrition assessment, counseling, and support (NACS) interventions were designed for evaluating nutritional status of undernourished people. NACS includes a wide range of interventions to prevent and treat malnutrition among HIV-infected adolescents and adults in clinical care in low-resource settings [ 16 , 21 ].
There were two review studies that examined the effect of NACS interventions on mortality, morbidity, retention in care, quality of life, prevention of HIV transmission, and weight-related nutritional outcomes [ 10 , 16 ]. In the systematic review conducted by Tang et al. [ 16 ], NACS interventions had no significant impact on all five outcomes (mortality, morbidity, retention in care, quality of life, and prevention of ongoing HIV transmission) in HIV-infected patients. Tesfay et al. showed that nutritional programs in HIV care led to some improvements in nutritional outcomes related to body weight in HIV people. However, the long-term nutrition status indicators such as food security were recommended to assess the nutritional status of people living with HIV [ 10 ]. In three narrative review studies, the multicomponent nutrition interventions including nutritional education, food aid, supplementation of macro- and micronutrients, exercise, and livelihood interventions were assessed on nutritional outcomes, quality of life, and mortality in HIV patients [ 9 , 20 , 22 ]. The available evidence suggests that nutrition education is an essential component in all settings accompanied by food assistance program as well as supplementation of macro- and micronutrients in resource-limited settings [ 20 ]. However, they reported an increase in quality of life and a decrease in mortality, as well as improvements in metabolic abnormalities and body composition following multivitamin supplementation, nutritional counseling, and exercise interventions in HIV-infected individuals [ 9 , 22 ].
Strengths and limitations
The key strength of this study is its coverage of all type of interventions in this field as well as summarizing the results of various nutrition programs in HIV patients in SRs studies. It also examines a range of HIV symptoms. However, the review has some limitations. This study only included articles published in English that may have omitted papers on a same topic that have been published in other languages. Furthermore, all reviewed studies in present review evaluated the impact of nutritional programs on undernourished individuals living with HIV in health care settings, while overnutrition as a risk factor of overweight and cardiovascular disease is important in these people and therefore this issue should be considered for future studies.
The findings of this review indicate that nutritional interventions in HIV care lead to improved nutritional symptoms and increased quality of life in these patients. However, nutritional programs on HIV care should evaluate the nutritional health of HIV-infected patients in a way that can be sustainable in the long term. In additions, demographic, clinical, nutritional, and social characteristics influence nutritional outcomes, which provide potential opportunities for future research.
Availability of data and materials
Not applicable.
Monteiro R, Azevedo I. Chronic inflammation in obesity and the metabolic syndrome. Mediato Inflamm. 2010. https://doi.org/10.1155/2010/289645 .
Article Google Scholar
Gedle D, Mekuria G, Kumera G, Eshete T, Feyera F, Ewunetu T. Food insecurity and its associated factors among people living with HIV/AIDS receiving anti-retroviral therapy at Butajira Hospital, Southern Ethiopia. J Nutr Food Sci. 2015;5(2):2–6.
Google Scholar
Obi SN, Ifebunandu NA, Onyebuchi AK. Nutritional status of HIV-positive individuals on free HAART treatment in a developing nation. J Infect Dev Ctries. 2010;4(11):745–9.
Article PubMed Google Scholar
Singhato A, Khongkhon S, Rueangsri N, Booranasuksakul U. Effectiveness of medical nutrition therapy to improve dietary habits for promoting bone health in people living with chronic HIV. Ann Nutr Metab. 2020;76(5):313–21.
Article PubMed CAS Google Scholar
Birhane M, Loha E, Alemayehu FR. Nutritional status and associated factors among adult HIV/AIDS patients receiving ART in Dilla University referral hospital, Dilla, Southern Ethiopia. J Med Physiol Biophys. 2021;70:8–15.
Kosmiski L. Energy expenditure in HIV infection. Am J Clin Nutr. 2011;94(6):1677S-S1682.
Article PubMed PubMed Central CAS Google Scholar
Musoke PM, Fergusson P. Severe malnutrition and metabolic complications of HIV-infected children in the antiretroviral era: clinical care and management in resource-limited settings. Am J Clin Nutr. 2011;94(6):1716S-S1720.
Kaye HL, Moreno-Leguizamon CJ. Nutrition education and counselling as strategic interventions to improvehealth outcomes in adult outpatients with HIV: a literature review. Afr J AIDS Res. 2010;9(3):271–83.
Aberman N-L, Rawat R, Drimie S, Claros JM, Kadiyala S. Food security and nutrition interventions in response to the AIDS epidemic: assessing global action and evidence. AIDS Behav. 2014;18(5):554–65.
Tesfay FH, Javanparast S, Gesesew H, Mwanri L, Ziersch A. Characteristics and impacts of nutritional programmes to address undernutrition of adults living with HIV in sub-Saharan Africa: a systematic review of evidence. BMJ Open. 2022;12(1):e047205.
Article PubMed PubMed Central Google Scholar
Pourmoradian S, Rezazadeh L, Tutunchi H, Ostadrahimi A. Selenium and Zinc supplementation in HIV-infected patients. Int J Vit Nutr Res. 2023:1–7.
Shea BJRB, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. bmj. 2017;21:358.
Grobler L, Siegfried N, Visser ME, Mahlungulu SS, Volmink J. Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD004536.pub3 .
Hong H, Budhathoki C, Farley JE. Effectiveness of macronutrient supplementation on nutritional status and HIV/AIDS progression: a systematic review and meta-analysis. Clin Nutr ESPEN. 2018;27:66–74.
Mahlungulu SS, Grobler L, Visser MM, Volmink J. Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database Syst Rev. 2013;2007(3):CD004536.
Tang AM, Quick T, Chung M, Wanke CA. Nutrition assessment, counseling, and support (NACS) interventions to improve health-related outcomes in people living with HIV/AIDS: a systematic review of the literature. J Acquir Immune Defic Syndr (1999). 2015;68(03):S340.
Article CAS Google Scholar
Madhu M, Udaya Kumar V, Dhingra S, Kumar N, Singh S, et al. Nutritional aspects of people living with HIV (PLHIV) amidst COVID-19 pandemic: an insight. Curr Pharmacol Rep. 2022;8(5):350–64.
Suttajit M. Advances in nutrition support for quality of life in HIV/AIDS. Asia Pac J Clin Nutr. 2007;16(1):318–22.
PubMed CAS Google Scholar
Liu E, Spiegelman D, Semu H, Hawkins C, Chalamilla G, Aveika A, et al. Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania. J Infect Dis. 2011;204(2):282–90.
Houtzager L. Nutrition in HIV: a review. Benin J Postgrad Med. 2009. https://doi.org/10.4314/bjpm.v11i1.48829 .
Kaplan JE, Hamm TE, Forhan S, Hassani AS, Bang G, Weyant E, et al. The impact of HIV care and support interventions on key outcomes in low and middle-income countries: a literature review. Introduction. J Acquir Immune Defic Syndr (1999). 2015;68(Suppl 3):S253.
Botros D, Somarriba G, Neri D, Miller TL. Interventions to address chronic disease and HIV: strategies to promote exercise and nutrition among HIV-infected individuals. Curr HIV/AIDS Rep. 2012;9(4):351–63.
Download references
Acknowledgements
We sincerely thank the financial support of the Nutrition Research Center of Tabriz University of Medical Sciences.
Author information
Authors and affiliations.
Nutrition Research Center, Faculty of Nutrition and Food Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Leila Rezazadeh
Nutrition Research Center, Department of Clinical Nutrition, Tabriz University of Medical Sciences, Tabriz, Iran
Alireza Ostadrahimi
Endocrine Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Helda Tutunchi
Student Research Committee, Nutrition Research Center, Faculty of Nutrition and Food Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Mohammad Naemi Kermanshahi
Nutrition Research Center, Department of Community Nutrition, Faculty of Nutrition and Food Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Samira Pourmoradian
You can also search for this author in PubMed Google Scholar
Contributions
The authors’ responsibilities were as follows: Two independent authors (MN and LR) systematically searched articles in PubMed/Medline, Scopus, Embase, ProQuest, and Ovid from 2000 till 2022. Two reviewers (HT and SP) independently screened and extracted study characteristics. The quality of all selected studies was assessed according to AMSTAR2 risk of bias tool (by AO and LR). SP as a supervisor contributed to paper writing and contributed to the final revision of the manuscript. All authors contributed to paper writing. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Samira Pourmoradian .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no conflict of interest in publishing this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rezazadeh, L., Ostadrahimi, A., Tutunchi, H. et al. Nutrition interventions to address nutritional problems in HIV-positive patients: translating knowledge into practice. J Health Popul Nutr 42 , 94 (2023). https://doi.org/10.1186/s41043-023-00440-z
Download citation
Received : 03 January 2023
Accepted : 29 August 2023
Published : 08 September 2023
DOI : https://doi.org/10.1186/s41043-023-00440-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Malnutrition
- Nutrition counseling
- Nutrition interventions
Journal of Health, Population and Nutrition
ISSN: 2072-1315
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Choosing sugary drinks over fruit juice for toddlers linked to risk of adult obesity
Consuming sugar-sweetened drinks in the first few years of childhood can be linked to poor diet patterns that increase the risk of obesity in later life, according to a new study by the School of Psychology at Swansea University.
Published in the European Journal of Clinical Nutrition , the study tracked the influence of diet on 14,000 British children from birth to adulthood and is believed to be the longest of its kind ever reported.
Using the Avon Longitudinal Study of Parents and Children, the research team found:
- Children who drank fizzy drinks such as cola or sugar-sweetened fruit cordials before the age of two gained more weight when they were 24 years old. Girls who had pure fruit juice gained less weight, while the weight of boys remained the same.
- At three years of age, toddlers who drank cola consumed more calories, fat, protein, and sugar but less fibre. In contrast, those given pure apple juice consumed less fat and sugar but higher amounts of fibre.
The study also highlighted corresponding differences in food choices. Children who consumed pure apple juice often followed a diet with more fish, fruit, green vegetables, and salad, whereas those drinking cola ate more burgers, sausages, pizza, french fries, meat, chocolate, and sweets.
Additionally, the team discovered a link between sugar-sweetened drinks and social deprivation, with children from affluent backgrounds more likely to have access to pure fruit juice.
Lead researcher Professor David Benton said: "The early diet establishes a food pattern that influences, throughout life, whether weight increases. The important challenge is to ensure that a child develops a good dietary habit: one that offers less fat and sugar, although pure fruit juice, one of your five a day, adds vitamin C, potassium, folate, and plant polyphenols."
Dr Hayley Young added: "Obesity is a serious health concern, one that increases the risk of many other conditions. Our study shows thatthe dietary causes of adult obesity begin in early childhood and that if we are to control it, more attention needs to be given to our diet in the first years of life."
- Diet and Weight Loss
- Children's Health
- Food and Agriculture
- Atkins Diet
- Malnutrition
- Anti-obesity drug
- Electrolyte
Story Source:
Materials provided by Swansea University . Note: Content may be edited for style and length.
Journal Reference :
- David Benton, Hayley A. Young. Early exposure to sugar sweetened beverages or fruit juice differentially influences adult adiposity . European Journal of Clinical Nutrition , 2024; DOI: 10.1038/s41430-024-01430-y
Cite This Page :
Explore More
- Genes for Strong Muscles: Healthy Long Life
- Brightest Gamma-Ray Burst
- Stellar Winds of Three Sun-Like Stars Detected
- Fences Causing Genetic Problems for Mammals
- Ozone Removes Mating Barriers Between Fly ...
- Parkinson's: New Theory On Origins and Spread
- Clash of Stars Solves Stellar Mystery
- Secure Quantum Computing at Home
- Ocean Currents: Collapse of Antarctic Ice ...
- Pacific Cities Much Older Than Previously ...
Trending Topics
Strange & offbeat.
Study at Tufts keeps patients ‘locked up’ for two weeks to unlock the mysteries of food

Jon Hamdorf is a free spirit who lives for adventure. His latest was a little different .
It started in mid-January when he checked into a 12th-floor room in a drab brick building in Boston’s Chinatown. At age 70, Hamdorf has no permanent address and spends his days traveling or living on his boat in Maine. But for this jaunt, this intrepid soul was confined to a rigid schedule, required to eat specific meals that were handed to him, and forbidden to go outside without a chaperone — all in the service of science.
“This, to me, is like going to Nepal or going to Israel. It’s like another adventure,” said Hamdorf, a retired CPA.
Advertisement
The thrill, he said, lay in the purpose. For three two-week stints, Hamdorf had agreed to become a study subject in a project seeking to answer questions that have troubled nearly every person who brings fork to mouth: What will happen in my body after I eat this food? Will it make me fat, raise my cholesterol, mess up my gut microbiome — or perhaps extend my life?
The Nutrition for Precision Health Study, a $170 million national research project seeking to enroll 10,000 people nationwide, aims to develop a way to pinpoint the optimal diet for every person. The study is being carried out by six clinical centers across the country, including the New England Clinical Center, run by Tufts University and Massachusetts General Hospital.
Current nutrition advice is based on averages, on what seems to work best for most people. But in many studies, people eating the exact same mix of nutrients have differing responses in measures like blood glucose or blood pressure, explains Holly Nicastro, the national study’s program director.
The study will try to find out exactly why, so that someday — it is hoped — people will be able to consume a diet tailored to their unique biology.
The study is also seeking to overcome the challenges that have long dogged nutrition research. Typically, nutrition data relies on asking people what they remember eating. But memories are notoriously inaccurate, and often biased by, say, embarrassment over having eaten that entire sleeve of Oreos. Nutrition for Precision Health is testing other methods of documenting what people consume, including with an app, a questionnaire, or a tiny camera mounted on eyeglasses that is activated by chewing.
“We have the technology to actually get away from the reliance on memory,” said Sarah L. Booth, director of the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University. “This is one of the exciting aspects of this study. We may be completely revolutionizing how we study nutrition.”
Participants first complete a “module” in which they follow their normal diet for 10 days and report what they ate. If they want to continue, they choose either to pick up prepackaged meals to eat at home or to enroll in the “live-in diet” module, the tightly controlled sojourn that Hamdorf selected. By keeping people inside and under watch, researchers can track — with precision and certainty — what people eat, and what effects those foods have throughout the body.
Hamdorf was among an inaugural group of four participants in the live-in diet phase in Boston. All had previously signed up for the All of Us Research Program of the National Institutes of Health, which aims to enroll 1 million or more participants to contribute their health data, including genetics, to build a database that can inform thousands of studies. Only existing All of Us members are invited to take part in the nutrition study.
On the first day, the participants gave blood and saliva samples, had their bones scanned, their metabolic rates measured, and their fat-to-muscle ratio documented. They were also equipped with blood-glucose monitors attached at the waist to continuously track fluctuations in blood sugar, and wrist bands that tracked activity and sleep.

The next day, the daily routines kicked in: 6:30 a.m. weight and vital signs taken; 8 a.m. breakfast; 12 p.m. lunch; 3 p.m. snack; 6 p.m. dinner; 11 p.m. lights out.
The strict schedule proved more liberating than confining, Hamdorf said. “It feels very good to be structured like this,” he said. “You just show up for the meals, and you don’t have to go shopping or anything.”
Between meals and tests, participants were free to use the exercise equipment on the 13th floor, stretch on the mats in the yoga room, gather in the game room, or relax in their spacious private rooms with picture windows. They loved interacting with many of the 150 people working in offices, laboratories, and the kitchen at the Human Nutrition Research Center on Aging.
Occasionally, they took a stroll outside, but only when a staff member could accompany them, lest anyone get an urge for an ice cream cone; the researchers must be able to attest that the participants ate only what they were served inside.
And what were they served?
Precisely at noon near the end of their first two-week stint, the four participants trooped to the 11th-floor dining room, accompanied by Paul J. Fuss, clinical research manager, who stayed to keep an eye on them as they ate.

The kitchen staff brought them plates wrapped in plastic and labeled with their names. Each meal is tailored to the individual’s calorie needs; participants are not supposed to gain or lose weight.
Each also has a tiny rubber spatula to scoop up every crumb. “We’re pretty much asking you to lick the plate without licking the plate,” said Kayla Airaghi, a dietitian. If they can’t finish, the staff will weigh the leftovers, tracking consumption down to a 10th of a gram.
On this day, Lori Mattheiss, 60, of Andover got a hamburger, peaches, and potato chips; her husband, Tim Carter, 63, was served two hamburger sliders. Jane Cashell, 75, of Clinton, ate broccoli, chicken nuggets, and mac and cheese. Hamdorf got Spanish rice, chicken with taco seasoning, and cheddar cheese.
“It’s not the food we normally eat,” Mattheiss said. “I’m eating things I haven’t eaten since I was a kid.” On other days she’s had a Yodel, Kool-Aid, canned fruit cocktail, Fritos.

In this two-week session, participants consumed what they called the traditional American diet. The researchers, however, resist labeling it; officially it’s described only by its contents, high in refined grains and sugar-sweetened drinks and low in fruits, vegetables, whole grains, and fish.
In the second and third two-week visits — which were spaced apart with at least two weeks in between — the participants ate high-fat and high-protein fare, and, finally, a diet replete with fruits, vegetables, beans, nuts, whole grains, and fish (the four liked this one best).
The three diets were chosen not because they’re recommended but because they are the most common diet patterns in the United States, said Sai Krupa Das, a senior scientist at the center and principal investigator for the New England branch of the study. “They are reflective of what we consume as a nation,” she said.
And the goal is not to determine which diet is best, but rather to measure individuals’ varying response to the different components.
The researchers acknowledge that it will be difficult to attract a diverse population to this phase of the project. How many people can put their lives on hold for two weeks at a time? Carter and Mattheiss, who trade stocks online, worked during their stays, and other remote workers might be able to do the same. But bus drivers? Restaurant owners? Parents of young children? Even the $6,200 stipend for completing all three two-week sessions may not be enough to compensate for lost work.
Despite the challenges, the NIH’s Nicastro said, “We do have ambitious diversity goals,” which they expect to achieve at least with “Module 1,” in which participants eat what they normally do and record it. But even for the more demanding modules — the prepackaged meals or the live-in diet — research sites are working with churches, barbershops, community centers, and other places to sign people up for All of Us, and then recruit them into the nutrition study, Nicastro said.
Rafael Pérez-Escamilla, a professor at the Yale School of Public Health, who is not involved in the study, believes the Nutrition for Precision Health will probably answer some fascinating scientific questions — but, he said, it won’t do much to improve people’s health or reach those suffering the worst effects of a poor diet.
“We live in a country where about 70 percent of adults are either overweight or obese, and 70 percent or more of their calories are coming from ultraprocessed or junk foods, including sugar-sweetened beverages,” he said. “The problem is heavily concentrated among the poor.”
Pérez-Escamilla would much prefer to see a similar investment in efforts to increase access to healthy foods, such as “produce prescription programs” that supply debit cards to purchase fresh fruits and vegetables.
Christopher Gardner, a Stanford professor who has studied the health benefits of dietary components but is not involved with the Nutrition for Precision Health study, called it an “incredibly ambitious” project. He predicted that the researchers would identify the key good and bad bacteria in the gut, and which foods promote them.
Gardner serves on the scientific advisory board for a private company, Zoe, that is offering personalized nutrition advice based on biological information. People take at-home tests and get instructions on what to eat based on the results.
This is exactly what the NIH study eventually hopes to offer, but Das, the principal investigator in Boston, said the results will have stronger scientific backing. “The market’s always ahead of the science,” she said, when asked about Zoe.

At the end of their two-week stay, the participants face two full days of testing, every aspect of their biology measured. On the last day, they drink two cups of vanilla Ensure and then sit in a chair from 8 a.m. to 1 p.m., giving blood samples at set intervals to measure how nutrients are metabolized.
The “live-in diet” sessions are expected to wrap up in mid-2026. Then, with a trove of data from each individual, multiplied across thousands of participants, the project will deploy artificial intelligence to come up with proposed algorithms for determining who should eat what. But that’s not the end: A series of studies will have to be conducted to validate those algorithms.
Nicastro is eager to learn what factors are driving individual responses. “It could be genetics, it could be microbiome, it could be something about the environment, and or probably a lot of these things mixed together,” she said. The ultimate goal is to enable doctors or dietitians to test for certain factors and then produce a personalized eating plan.
Meanwhile, the first four participants, settled back at home with their lime-green souvenir water bottles, are already finding themselves making changes in their diet. Cashell loved the third diet so much she’s trying to re-create the recipes in her kitchen. Hamdorf noticed that during the experiment he never felt hungry, yet looked forward to each meal — and realized he needed to eat more, and drink more water. Matthiess and Carter are trying to eat less in the evening and include more fruits and nuts.
All were gratified to have been part of the study.
“You don’t have many opportunities to contribute to important scientific research,” Carter said. “And I feel lucky that I am able to do that.”
Felice J. Freyer can be reached at [email protected] . Follow her @felicejfreyer .

Virtual Tour
Experience University of Idaho with a virtual tour. Explore now
- Discover a Career
- Find a Major
- Experience U of I Life
More Resources
- Admitted Students
- International Students
Take Action
- Find Financial Aid
- View Deadlines
- Find Your Rep

Helping to ensure U of I is a safe and engaging place for students to learn and be successful. Read about Title IX.
Get Involved
- Clubs & Volunteer Opportunities
- Recreation and Wellbeing
- Student Government
- Student Sustainability Cooperative
- Academic Assistance
- Safety & Security
- Career Services
- Health & Wellness Services
- Register for Classes
- Dates & Deadlines
- Financial Aid
- Sustainable Solutions
- U of I Library

- Upcoming Events
Review the events calendar.
Stay Connected
- Vandal Family Newsletter
- Here We Have Idaho Magazine
- Living on Campus
- Campus Safety
- About Moscow

The largest Vandal Family reunion of the year. Check dates.
Benefits and Services
- Vandal Voyagers Program
- Vandal License Plate
- Submit Class Notes
- Make a Gift
- View Events
- Alumni Chapters
- University Magazine
- Alumni Newsletter

U of I's web-based retention and advising tool provides an efficient way to guide and support students on their road to graduation. Login to VandalStar.
Common Tools
- Administrative Procedures Manual (APM)
- Class Schedule
- OIT Tech Support
- Academic Dates & Deadlines
- U of I Retirees Association
- Faculty Senate
- Staff Council
University of Idaho News
University Communications and Marketing
Fax: 208-885-5841
Email: [email protected]
Web: Communications and Marketing
U of I Receives Over $11 Million to Launch Research Center in Women’s Nutrition and Health
April 10, 2024.
MOSCOW, Idaho — The National Institutes of Health (NIH) has awarded University of Idaho more than $11 million toward creating a biomedical research center focused on furthering studies on women’s health and nutrition.
Shelley McGuire , professor of nutrition and director of the Margaret Ritchie School of Family and Consumer Sciences (FCS), recently received confirmation of her successful application for the NIH Center of Biomedical Research Excellence (COBRE) grant and will serve as project director and principal investigator. McGuire, a maternal-infant nutritionist with expertise in breastfeeding and lactation, was recently elected to the National Academy of Medicine .
“It’s going to bolster our ability to do high-level, federally funded research on a topic that should be important to every single human,” McGuire said. “We are hoping to have impacts in the state, region and nation.”
American women face a heightened risk of malnutrition — 12% struggle with anemia while 60% are overweight. Malnutrition is an especially serious problem in Idaho, where 12% of the general population is food insecure, compared with 10% nationally.
“The whole topic of health and nutrition in women is important from early life, through breastfeeding, through pregnancy and all the way until women get older when we have a higher risk of poor health outcomes like osteoporosis and specific types of cancer,” McGuire said.
The COBRE will span five years, retroactive to Jan. 1, in its initial phase, and U of I will be eligible to apply for two additional five-year phases of funding. Furthermore, researchers from any U of I college will be eligible to apply for up to $100,000 per year in combined funds for relevant pilot projects, and McGuire has already received inquiries about the opportunity from faculty members in four colleges.
The funds will cover two administrative staff members and four new faculty positions — two FCS faculty members, a health psychologist within the Department of Psychology and Communication Studies and an expert at analyzing large datasets or data related to nutrition and women’s health within the Department of Mathematics and Statistical Science.
The COBRE names three initial research project leaders:
- Yimin Chen , an assistant professor in FCS specializing in maternal nutrition and human milk composition, will study the impact of postpartum vitamin D supplementation on maternal depression.
- Ginny Lane , an assistant professor in FCS specializing in community and global nutrition, will study type 2 diabetes among Hispanic women living in Idaho.
- Ann Brown , an associate professor of exercise physiology and associate dean of graduate studies in the College of Education, Health and Human Sciences, will study the health ramifications for women, including college-age athletes, of having a normal body weight but still carrying excess fat tissue similar to that of an obese person.
The COBRE’s administrative team will also include Mark McGuire , university distinguished professor and associate dean of research and director of the Idaho Agricultural Experiment Station, and Janet Williams , a senior research scientist with the Department of Animal, Veterinary and Food Sciences, who will oversee a nutrition analytics lab developed for the program.
COBRE research project leaders will receive leadership training.
“My vision is that all of these people will end up in leadership roles, and they will become a voice in academic leadership that considers rigorous research and women’s health on a daily basis,” McGuire said.
The COBRE program supports the establishment and development of innovative, state-of-the-art biomedical and behavioral research centers at institutions in states with historically poor success at landing NIH awards. Idaho ranks 49th among states at obtaining NIH funds.
McGuire’s COBRE represents the fourth COBRE in U of I’s history. U of I has one other active COBRE — the Institute for Modeling Collaboration and Innovation — which is in its ninth year and is run by Holly Wichman, a university distinguished professor in the Department of Biological Sciences.
The NIH Center of Biomedical Research Excellence (COBRE) in Nutrition and Women's Health is funded with a five-year, $11,183,222 grant, of which 100% is the federal share, through the National Institute of Health under award number 1P20GM152304-01.
Media Contacts:
John O’Connell Assistant Director of Communications, College of Agricultural and Life Sciences 208-530-5959 [email protected]
Shelley McGuire Professor and Director, Margaret Ritchie School of Family and Consumer Sciences 208-885-6546 [email protected]
About the University of Idaho
The University of Idaho, home of the Vandals, is Idaho’s land-grant, national research university. From its residential campus in Moscow, U of I serves the state of Idaho through educational centers in Boise, Coeur d’Alene and Idaho Falls, nine research and Extension centers, plus Extension offices in 42 counties. Home to nearly 11,000 students statewide, U of I is a leader in student-centered learning and excels at interdisciplinary research, service to businesses and communities, and in advancing diversity, citizenship and global outreach. U of I competes in the Big Sky and Western Athletic conferences. Learn more at uidaho.edu .
- Request info
- Majors & Degrees
- Prospective Students
- Current Undergraduate Students
- Current Graduate Students
- Online Students
- Alumni and Friends
- Faculty and Staff
USM Contingent Captures Awards at Mississippi Academy of Nutrition and Dietetics Conference
Fri, 04/12/2024 - 03:17pm | By: Van Arnold

Students, faculty, and alumni from The University of Southern Mississippi’s (USM) School of Kinesiology and Nutrition earned special recognition during the Mississippi Academy of Nutrition and Dietetics annual conference held at USM’s Hattiesburg campus.
This year’s conference, held April 4-5, featured the theme: “Food for Thought – Innovation, Solutions, and Strategies for Success.”
USM honorees included:
- Outstanding Dietetic Educator of the Year: Teresa-Walker Cartwright, USM faculty member and alumna
- Outstanding Dietetic Student – Didactic Program in Dietetics: Kymberly Jackson, USM undergraduate student
- Outstanding Dietetic Student – Dietetic Internship: Eric Wicht, USM graduate student
- Emerging Dietetic Leader: Molly Edwards, USM faculty member and alumna
- Recognized Young Dietitian: Chelsey Crocker, USM alumna
The USM School of Kinesiology and Nutrition offers an undergraduate degree program in nutrition and dietetics and a graduate degree program in nutrition and foods systems.
“It was so exciting to recognize current and former students and my colleagues for these well-deserved awards,” said Dr. Holly Huye, Associate Professor of Nutrition and Dietetics and director of the undergraduate program. “It is truly inspiring to see their hard work and dedication acknowledged, and I’m thrilled to celebrate their accomplishments.”
Walker-Cartwright, a lecturer in the School of Kinesiology and Nutrition, described being chosen as the Outstanding Dietetic Educator of the Year, “an absolute honor.”
“I appreciate the recognition from my colleagues and my students as it serves as an acknowledgment of the time and energy I put into being the best educator I can be,” she said. “My students and the nutrition professionals that I work with serve as my motivation, and they make me strive to always be better and do better. They encourage me to greater effort, enthusiasm, and creativity- they inspire me every day.”
Edwards, visiting instructor and Director, Dietetic Internship program expressed surprise and gratitude upon learning that she had been nominated for the award.
“I am so honored to win this award and particularly to be nominated by a former student. The students in the internship mean the world to me,” said Edwards. “Each year we have around 10 interns enter the two-year program. They work so hard over the course of the program completing graduate courses and supervised practice hours within the community to attain their Registered Dietitian Nutritionist (RDN) credential.
She added, “It is such a joy each year to get to know the interns, watch them grow in their skills and confidence, and guide them through the process. It's also such an honor for me to see the graduates years later serving our community as RDNs.”
Members of the Mississippi Academy of Nutrition and Dietetics are dedicated professionals who volunteer their time and talents to improve the nutritional status of their clients and the public. MS-AND members are trained to deliver nutrition information in a variety of settings and practice in every area of the state.
MS-AND is a state Affiliate Association of the Academy of Nutrition and Dietetics, which has 70,000 members nationally and throughout the world. Members serve in more than 20 countries overseas. Membership is comprised of Registered Dietitians, the Registered Dietetic Technicians, and students of nutrition and food service.
Learn more about USM’s School of Kinesiology and Nutrition by calling 601.266.5358.
Categories: Education and Human Sciences
Recent News Articles
Usm's gulf and caribbean research journal gives undergraduate students publication opportunities & experiences, festivalsouth® returns, featuring southern miss performers.
Read our research on: Gun Policy | International Conflict | Election 2024
Regions & Countries
7 facts about americans and taxes.

Spring reliably brings a whirlwind of number-crunching and form-filing as Americans finish their tax returns. Altogether, the IRS expects to process more than 160 million individual and business tax returns this season.
Ahead of Tax Day on April 15, here are seven facts about Americans and federal taxes, drawn from Pew Research Center surveys and analyses of federal data.
Ahead of Tax Day 2024, Pew Research Center sought to understand Americans’ views of the federal tax system and outline some of its features.
The public opinion data in this analysis comes from Pew Research Center surveys. Links to these surveys, including details about their methodologies, are available in the text.
The external data comes from the U.S. Office of Management and Budget and the IRS Data Book . Data is reported by fiscal year, which for the federal government begins Oct. 1 and ends Sept. 30. For example, fiscal 2024 began Oct. 1, 2023, and ends Sept. 30, 2024.
A majority of Americans feel that corporations and wealthy people don’t pay their fair share in taxes, according to a Center survey from spring 2023 . About six-in-ten U.S. adults say they’re bothered a lot by the feeling that some corporations (61%) and some wealthy people (60%) don’t pay their fair share.
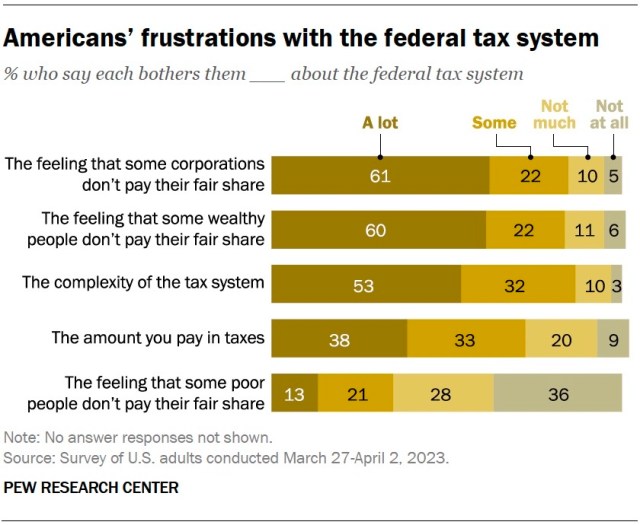
Democrats are far more likely than Republicans to feel this way. Among Democrats and Democratic-leaning independents, about three-quarters say they’re bothered a lot by the feeling that some corporations (77%) and some wealthy people (77%) don’t pay their fair share. Much smaller shares of Republicans and GOP leaners share these views (46% say this about corporations and 43% about the wealthy).
Meanwhile, about two-thirds of Americans (65%) support raising tax rates on large businesses and corporations, and a similar share (61%) support raising tax rates on households with annual incomes over $400,000. Democrats are much more likely than Republicans to say these tax rates should increase.
Just over half of U.S. adults feel they personally pay more than what is fair, considering what they get in return from the federal government, according to the same survey.
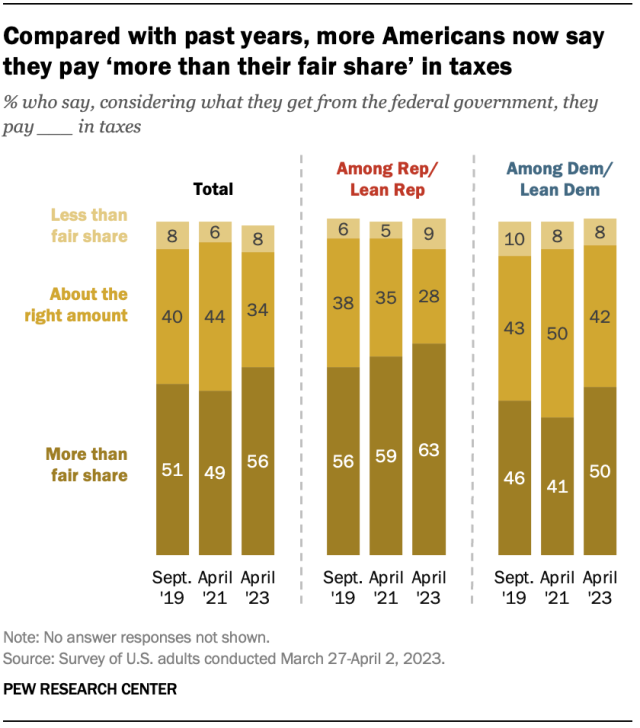
This sentiment has grown more widespread in recent years: 56% of Americans now say they pay more than their fair share in taxes, up from 49% in 2021. Roughly a third (34%) say they pay about the right amount, and 8% say they pay less than their fair share.
Republicans are more likely than Democrats to say they pay more than their fair share (63% vs. 50%), though the share of Democrats who feel this way has risen since 2021. (The share among Republicans is statistically unchanged from 2021.)
Many Americans are frustrated by the complexity of the federal tax system, according to the same survey. About half (53%) say its complexity bothers them a lot. Of the aspects of the federal tax system that we asked about, this was the top frustration among Republicans – 59% say it bothers them a lot, compared with 49% of Democrats.
Undeniably, the federal tax code is a massive document, and it has only gotten longer over time. The printed 2022 edition of the Internal Revenue Code clocks in at 4,192 pages, excluding front matter. Income tax law alone accounts for over half of those pages (2,544).
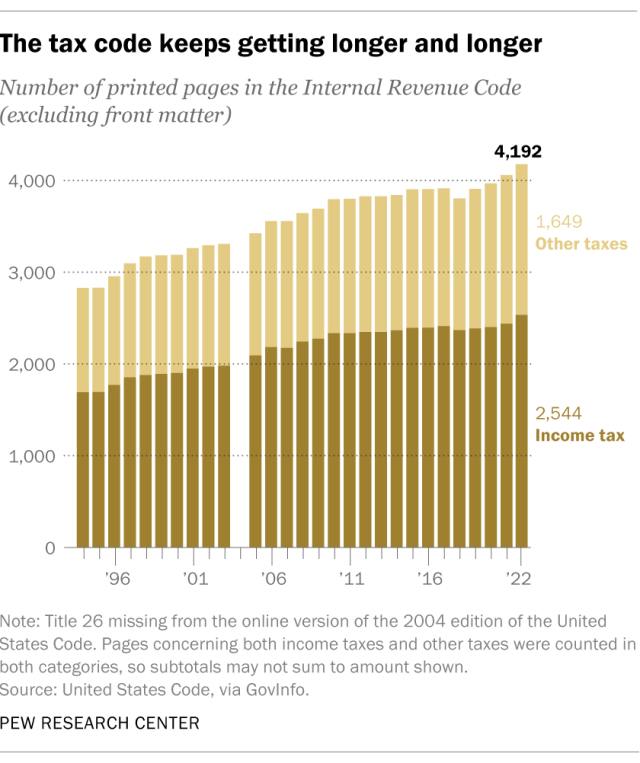
The public is divided in its views of the IRS. In a separate spring 2023 Center survey , 51% of Americans said they have an unfavorable opinion of the government tax agency, while 42% had a favorable view of the IRS. Still, of the 16 federal agencies and departments we asked about, the IRS was among the least popular on the list.
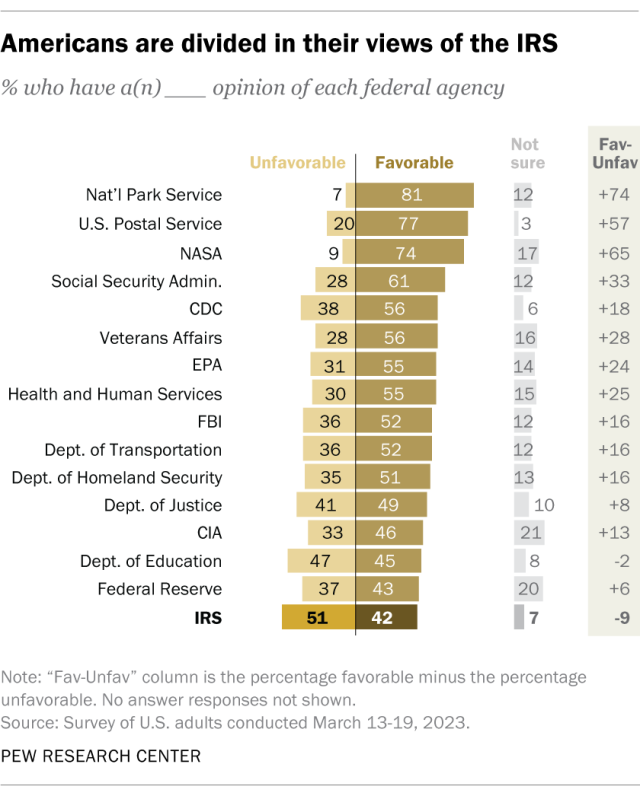
Views of the IRS differ greatly by party:
- Among Republicans, 29% have a favorable view and 64% have an unfavorable view.
- Among Democrats, it’s 53% favorable and 40% unfavorable.
On balance, Democrats offer much more positive opinions than Republicans when it comes to most of the federal agencies we asked about. Even so, the IRS ranks near the bottom of their list.
Individual income taxes are by far the government’s largest single source of revenue, according to estimates from the Office of Management and Budget (OMB).
The federal government expects to collect about $2.5 trillion in individual income taxes in fiscal year 2024. That accounts for nearly half (49%) of its total estimated receipts for the year. The next largest chunk comes from Social Security taxes (including those for disability and retirement programs), which are projected to pull in $1.2 trillion this fiscal year (24%).
By comparison, corporate income taxes are estimated to bring in $612.8 billion, or 12% of this fiscal year’s federal receipts. And excise taxes – which include things like transportation trust fund revenue and taxes on alcohol, tobacco and crude oil – are expected to come to $99.7 billion, or 2% of receipts.
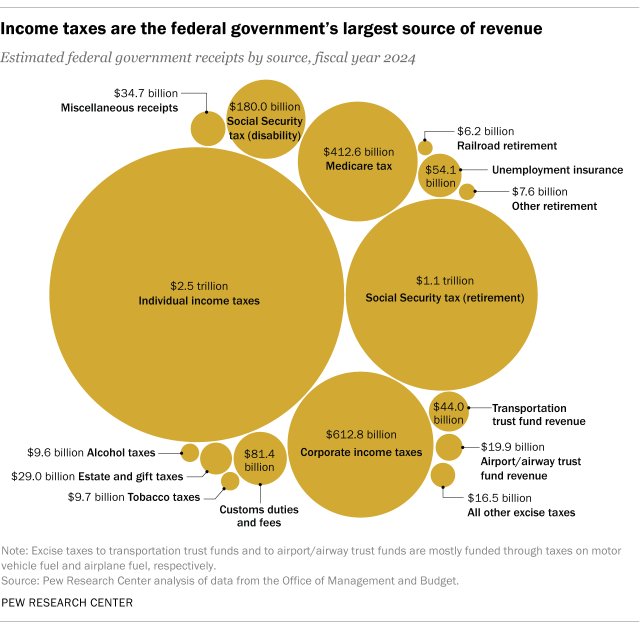
American tax dollars mostly go to social services. Human services – including education, health, Social Security, Medicare, income security and veterans benefits – together will account for 66% ($4.6 trillion) of federal government spending in fiscal 2024, according to OMB estimates.
An estimated 13% ($907.7 billion) will go toward defense spending. Another 13% ($888.6 billion) will repay net interest on government debt, and 10% ($726.9 billion) will fund all other functions, including energy, transportation, agriculture and more.
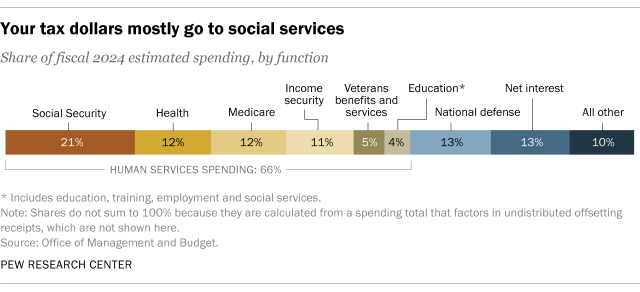
Related: 6 facts about Americans’ views of government spending and the deficit
The vast majority of Americans e-file their taxes, according to IRS data . In fiscal 2022, 150.6 million individual federal income tax returns were filed electronically, accounting for 94% of all individual filings that year.
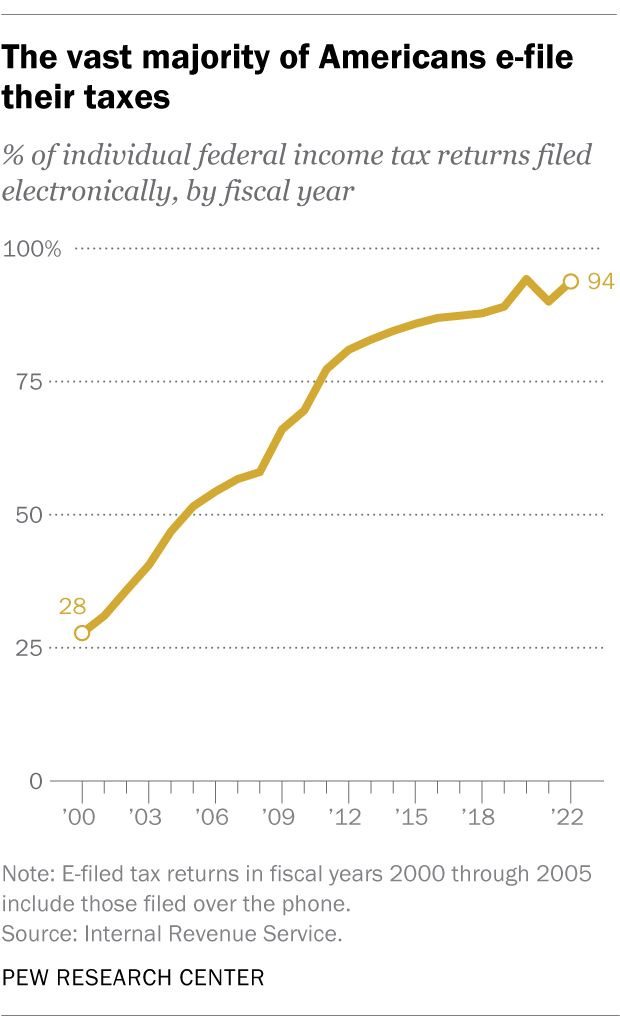
Unsurprisingly, e-filing has become more popular since the turn of the century. Fiscal 2000, the earliest year for which comparable data is available, saw 35.4 million individual income tax returns filed electronically (including those filed over the phone). These accounted for just 28% of individual filings that year.
By fiscal 2005, more than half of individual income tax returns (52%) were filed electronically.
Note: This is an update combining information from two posts originally published in 2014 and 2015.
Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Top tax frustrations for Americans: The feeling that some corporations, wealthy people don’t pay fair share
Growing partisan divide over fairness of the nation’s tax system, public has mixed expectations for new tax law, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
- Side Hustles
- Power Players
- Young Success
- Save and Invest
- Become Debt-Free
- Land the Job
- Closing the Gap
- Science of Success
- Pop Culture and Media
- Psychology and Relationships
- Health and Wellness
- Real Estate
- Most Popular
Related Stories
- Land the Job The No. 1 mistake job seekers make when using AI, says career expert
- Land the Job Don't use these phrases in a job interview, they are ‘major red flags'
- Land the Job This bad job interview habit gives hiring managers the 'biggest ick'
- Land the Job How to use ChatGPT to prep for a job interview, says ex-Disney recruiter
- Science of Success The No. 1 personality trait employers always look for
The 3 biggest red flags hiring managers look for in resumes, according to new research

If you use artificial intelligence to write your resume — or get a bit too creative with the design — you could be hurting your chances of landing a job.
The biggest red flag hiring managers look for in job candidates is an AI-generated resume, according to new research from Resume Genius, which surveyed 625 hiring managers across the U.S. Other resume faux pas include poor formatting and typos.
Here are the three biggest resume red flags that could cost you a job offer, and how to avoid them, according to a hiring expert:
AI-generated resumes
More than half (53%) of hiring managers say they have reservations about resumes that include AI-generated content, with 20% calling it a "critical issue" that might prevent them from hiring someone.
"It's extremely important that your resume is a truthful, authentic reflection of the skills and experience you bring to the table," says Michelle Reisdorf, district director at recruitment firm Robert Half. "If you use AI to write a resume for you in minutes, it tells me you didn't put a lot of time and thought into applying to my job."
Reisdorf, who has worked in recruiting and hiring for over 30 years, still encourages jobseekers to use AI to review and edit their resume — but says you should write the first draft.
"AI is great for proofreading and enhancing what you've already written, but it's not a one-stop shop to generate the perfect resume," she adds. "Recruiters will be able to tell if you're not including specific details from your past jobs or writing in a personal, human voice."
DON'T MISS: The ultimate guide to acing your interview and landing your dream job
Frequent job-hopping
Similarly, resumes showing a pattern of frequent job-hopping make 50% of hiring managers hesitant to move forward with a candidate, Resume Genius found.
This red flag is trickier to avoid: If you've switched jobs a lot, you can't lie about your employment history. Plus, hiring managers have different definitions of what constitutes excessive job-hopping.
For some, it might be changing jobs every 1-2 years, while others would argue it's a shorter timeframe (opting to move after less than a year).
You don't have to explain every time you switched roles, "as most recruiters aren't looking for that on the first pass," Reisdorf says. "They want to know if you have the skills and the experience to do the job well — your past experiences and commitment to work are usually saved for the interview."
If you have several short stints on your resume, however, Reisdorf recommends including a brief context (1-2 sentences) of your job changes elsewhere on your application.
"Most online applications will have text fields for additional comments or 'reasons for leaving' after you upload your resume," she explains. "That's a good place to acknowledge any job-hopping without drawing too much attention to it."
Otherwise, save any explanations of your career choices for the interview.
Poor formatting
Another red flag hiring managers look out for on resumes is poor formatting, whether it's a disorganized layout, using an obscure font or simply forgetting to spell-check.
Reisdorf says clean, simple resumes are the most effective as they're easy for anyone to read and understand. That means using a basic black font, trimming it to one page and having clearly labeled, organized sections.
Put simply, you want a recruiter's attention to be focused on your accomplishments — not a bold typeface choice or cluttered layout.
Proofreading for any spelling or grammar mistakes before submitting your resume is important, too, Reisdorf says, because it shows your potential employer that you're detail-oriented and conscientious.
"Ultimately, you want the hiring manager to focus on you, as the candidate, versus the mistakes on your resume," says Reisdorf. "Your resume should make them excited to interview and, hopefully, hire you."
Want to land your dream job in 2024? Take CNBC's new online course How to Ace Your Job Interview to learn what hiring managers are really looking for, body language techniques, what to say and not to say, and the best way to talk about pay. CNBC Make It readers can save 25% with discount code 25OFF.
Plus, sign up for CNBC Make It's newsletter to get tips and tricks for success at work, with money and in life.


COMMENTS
The effects of certain foods or dietary patterns on glycaemia, immune activation, and the gut microbiome may play a role in the relationships between food and mood. More research is needed to understand the mechanisms that link food and mental wellbeing and determine how and when nutrition can be used to improve mental health. 3 fig 1 4.
Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population, say Joseph Firth and colleagues ### Key messages Depression and anxiety are the most common mental health conditions worldwide, making them a leading cause of disability.1 Even beyond diagnosed conditions ...
Interestingly, such brain dysfunction most often co-occurs with metabolic disorders (e.g., obesity) and/or poor dietary habits; obesity and poor diet can lead to negative health implications ...
Nutrition health disparities include differences in incidence, prevalence, morbidity, and mortality of diet-related diseases and conditions. Often, race, ethnicity, and the social determinants of health are associated with dietary intake and related health disparities. This report describes the nutrition health disparities research supported by NIH over the past decade and offers future ...
Proper nutrition offers one of the most effective and least costly ways to decrease the burden of many diseases and their associated risk factors, including obesity. Nutrition research holds the key to increasing our understanding of the causes of obesity and its related comorbidities and thus holds promise to markedly influence global health and economies. After outreach to 75 thought leaders ...
This triple burden of malnutrition is a major public health challenge. The numbers speak for themselves: 51% of the world's population over five years of age is predicted to be obese or ...
Food insecurity and the lack of access to affordable, nutritious food are associated with poor dietary quality and an increased risk of diet-related diseases, including cardiovascular disease, diabetes, and certain types of cancer. Those of lower socioeconomic status and racial and ethnic minority groups experience higher rates of food insecurity, are more likely to live in under-resourced ...
Prevalence of poor, intermediate, and ideal scores for the dietary component of the American Heart Association's Ideal Cardiovascular Health Definition in US adults aged ≥20 years (age standardized) and selected age groups by race/ethnicity. ... Prepared by Mathematica Policy Research for the USDA Food and Nutrition Service. 2018. Available ...
December 17, 2019. An #NHLBI-funded study put a price tag on American's bad eating habits: $50 billion a year in health care costs, attributable to cardiometabolic diseases such as heart disease, stroke and type 2 diabetes. The research, reported in the journal PLoS Medicine , sought to zero in on the national health care costs of unhealthy ...
Poor nutrition on the menu: children's meals at America's top chain restaurants. Child Obes. 2012; 8: 251-254. Crossref; ... Beltsville Human Nutrition Research Center, Food Surveys Research Group, and US Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), National Center for Health Statistics. ...
Consuming too much sodium can increase blood pressure and the risk for heart disease and stroke. Current guidelines recommend getting less than 2,300 mg a day, but Americans consume more than 3,400 mg a day on average. Over 70% of the sodium that Americans eat comes from packaged, processed, store-bought, and restaurant foods.
The Journal of Nutrition invites submission of high-quality, original research manuscripts, reviews, perspectives, and systematic reviews with meta-analyses on studies that apply interdisciplinary methods to advance research on nutrition and the brain. Papers must be submitted by 15 December 2024 to be considered for this Special Collection.
Recent data show that nutrition curricula worldwide are inadequate, 6,7 and fewer than 1% of questions on medical licensing exams are related to topics in nutrition. 8 Unsurprisingly, many medical ...
Poor nutrition (substandard diet quantity and/or quality resulting in under- or overnutrition) and the lack of early learning opportunities contribute to the loss of developmental potential and life-long health and economic disparities among millions of children aged <5 y. Single-sector interventions representing either early child development (ECD) or nutrition have been linked to positive ...
January 5, 2022 by ASN Staff. 2021 has come to a close, take a look back at some trending nutrition research articles from ASN's four journals: The Journal of Nutrition, The American Journal of Clinical Nutrition, Advances in Nutrition, and Current Developments in Nutrition. Here are 15 articles that were mentioned the most in news and social ...
Poor nutrition is the leading cause of US illnesses, creating a growing burden on the nation's economy, exacerbating health disparities and impacting national security, according to a white ...
A research team has unearthed new findings which may help explain the connection between cancer risk and poor diet, as well as common diseases like diabetes, which arise from poor diet. The ...
Human immunodeficiency virus (HIV) infection and malnutrition negatively reinforce each other. Malnutrition leads to further immune deficiency and accelerates disease progression. The present overview aimed to investigate the current knowledge from review articles on the role of nutrition interventions as well as food and nutrition policies on HIV-related outcomes in adults to present future ...
Consuming sugar-sweetened drinks in the first few years of childhood can be linked to poor diet patterns that increase the risk of obesity in later life, according to a new study. Consuming sugar ...
A national research project, with the New England component based at Tufts, is seeking to understand why individuals respond differently to different nutrients. The goal is to someday enable ...
MOSCOW, Idaho — The National Institutes of Health (NIH) has awarded University of Idaho more than $11 million toward creating a biomedical research center focused on furthering studies on women's health and nutrition. Shelley McGuire, professor of nutrition and director of the Margaret Ritchie School of Family and Consumer Sciences (FCS), recently received confirmation of her successful ...
MS-AND members are trained to deliver nutrition information in a variety of settings and practice in every area of the state. MS-AND is a state Affiliate Association of the Academy of Nutrition and Dietetics, which has 70,000 members nationally and throughout the world. Members serve in more than 20 countries overseas.
A majority of Americans feel that corporations and wealthy people don't pay their fair share in taxes, according to a Center survey from spring 2023.About six-in-ten U.S. adults say they're bothered a lot by the feeling that some corporations (61%) and some wealthy people (60%) don't pay their fair share.
The biggest red flag hiring managers look for in job candidates is an AI-generated resume, according to new research from Resume Genius, which surveyed 625 hiring managers across the U.S. Other ...