
NurseStudy.Net
Nursing Education Site

Community Health Nursing Diagnosis and Nursing Care Plan
Last updated on May 18th, 2022 at 06:35 am
Community Health Nursing Care Plans Diagnosis and Interventions
Community Health Nursing NCLEX Review and Nursing Care Plans
Community health nursing, also known as public health nursing, is one of the various specializations available in this professional field. Nurses who aspire to work in a setting other than a hospital and have greater control over their practice can choose to specialize in community health nursing.
A comprehensive approach to patient care is required in community health nursing. Its emphasis is on individuals, families, and groups within a particular area which focuses on the health promotion of an entire population while also preventing disease, disability, and mortality rates in a community.
Educating the community to maintain a healthy lifestyle is also one of the key objectives of community health nursing.
By taking into account the cultural beliefs, surroundings, lifestyle, and socioeconomic considerations, a community nurse should be able to adapt quickly and help people live healthier lives in their own environment.
Importance of Community Health Nursing
Community health nursing is paramount to the overall welfare and health of the population, as it enhances health outcomes and strengthens measures for disease monitoring and management.
Indeed, any healthcare system should be available to everybody. However, communities are dealing with a significantly large number of people of all ages who are unable to obtain or seek health care due to various reasons such as financial constraints.
Absence of insurance coverage, transport difficulties, inability to physically get to a doctor’s clinic or hospital, and a lack of understanding of where to go for healthcare are the other reasons why community members may not seek medical care.
As a result of a lack of access to health care, newborns, pregnant women, and other vulnerable groups have seen a significant increase in morbidity and mortality.
Underprivileged members of the community who do not have access to health care can be treated better through efficient community health nursing.
History of Nursing Involvement in the Community
Lillian Wald and Florence Nightingale were the first individuals to develop a system of health planning based on a study of the health requirements of the community they served. Nurses have also historically been active in putting other disciplines’ plans into action.
According to reputable organizations such as American Nurses Association (ANA) and American Public Health Association (APHA), community health nurses’ primary responsibility is to the community or population as a whole, and in order to fulfill this responsibility, nurses must recognize the need for comprehensive health planning.
Nurses should be involved in program planning for various reasons, in addition to professional organizations’ obligations. The majority of healthcare workers are nurses responsible for health programs where they learn a lot about what works and what does not. This experience aids in the identification of future problems that can be avoided, especially in a community.
Unlike any other healthcare provider, nurses spend more time in close touch with their patients than anybody else. They spend time in the community with clients, learning about their health, habits, needs, and what it’s like to be a member of that community firsthand.
Nurses are in a unique position to have access to vital information that may be used to plan and implement successful health programs as a result of their community involvement.
Nurses not only make up a substantial percentage of healthcare providers, but they also make up a significant fraction of healthcare consumers. Nurses are in a unique position to influence the development of population-based health programs as a result of this.
Principles of Community Health Nursing
Community Health Nursing (CHN) is an essential component of public health, and it is guided by a set of 12 principles, which include:
- Individuals, families, and communities’ identified needs are the foundation for CHN work. Its main goal is to expand the use of public health measures as part of the overall CHN approach.
- Goal attainment is facilitated by having an excellent comprehension of the agency’s goals and policies. Towards this goal, the mission statement engages Community Health Nurses to positively realize their work.
- Family is the main unit of service for CHN. The degree to which it can deal with its own challenges has an impact on its level of functioning. As a result, the most effective and accessible medium for CHN initiatives is the family.
- The efficacy of client care is strengthened by sensitivity to the client’s values, customs, and beliefs. Regardless of race, faith, color, or socioeconomic level, CHN services must be sustainable and accessible to all.
- Health education and counseling are integrated into the CHN’s. These foster and encourage community efforts to enhance people’s health by bringing concerns up for discussion.
- The achievement of goals is made easier when coworkers and members of the health team work together. Employees observe themselves on how their contributions benefit the entire organization.
- Evaluation of the degree to which CHN goals and objectives are being met can be performed on a regular and continuous basis. Through consultations, observations, and precise recording, clients are involved in the evaluation of their health program.
- To improve and maintain effective nursing practices in their context, a continuing staff education program and high-quality client services are required. The agency’s staff development programs take into account the professional interests and needs of Community Health Nurses.
- Maximizing the success of the Community Health Nurses’ activities by utilizing existing community resources. The ability to connect with existing community resources, both public and private, raises an understanding of what they require and what they are entitled to.
- The success of CHN programs is greatly determined by the active participation of the individual, family, and community in planning and making health care decisions. Participation in activities of organized community groups satisfies the needs and interests of the community.
- The task completed is guided and directed by the supervision of nursing services by qualified CHN employees. Employees’ ability to perform effectively and efficiently is enhanced.
- The basis for evaluating the progress of planned programs and activities, as well as a guide for future actions, is accurate recording and reporting. Community health records are used in studies and research as well as legal documents, thus, keeping accurate records is an essential responsibility of the community health nurse and community leaders.
Responsibilities of a Community Health Nurse
Community health nurses may have a distinct set of responsibilities due to the diversity of a community’s requirements. Clinics, churches, community health centers, non-profit organizations, private homes, and schools are just a few of the places where community health nurses work. Community health nurses have the following primary responsibilities:
- Preventive care. One of the most important concepts of community health nursing is prevention. Community health nurses can help people who do not have access to preventive or screening services from a doctor or other healthcare practitioner by providing various health services. Vaccinations, cholesterol tests, and well-baby visits that improve health and prevent disease are some of the health services they provide at a little or free cost to the public.
- Health trends monitoring. Particular health trends or illnesses have a different impact on each community. Rising rates of diabetes or hepatitis , for example, may affect just a percentage of the population, and community health nurses are trained to recognize and monitor these trends and risk factors. This data is utilized to educate and provide services specific to the community’s needs to prevent illness or disease from spreading.
- Training and education. Community health nurses may create educational programs, presentations, and training materials to distribute to vulnerable members of the community after identifying significant concerns or trends affecting a particular location or population. As part of this program, nurses may work with schools, enterprises, elder centers, health clinics, and regional healthcare groups to communicate the information to the public.
- Engagement in the underprivileged. Because public health nurses work so directly with people in a community, they are typically better able to comprehend the difficulties that affect different groups of people. As a result of their extensive understanding, they can advocate for those underserved by contacting local, state, and federal agencies to request further supplies, financing, and assistance for these groups.
- Knowledge and Skills of a Community Health Nurse
- Because community health nurses are responsible for a variety of tasks, they need to possess the following characteristics to succeed in their area.
- Versatility. Nurses must be able to improvise and adapt rapidly to their circumstances. As typical duties might vary dramatically — one day it might be giving kids immunizations, and the next day might be presenting a lecture on malnutrition — it is essential to effortlessly switch between tasks.
- Teamwork. The majority of the work of community health nurses involves collaboration with other healthcare organizations, community groups, and government leaders, although they may work independently. Nurses will be more productive if they learn to collaborate with others.
- A BSN degree holder. The American Public Health Association (APHA) acknowledges a bachelor’s degree as the entry-level education required for public health nurses due to the intricacy of anticipating and addressing the health needs of a whole community. The APHA also recommends that BSN coursework include population health, finance, and healthcare policy in addition to preventive care methods.
- Willingness and capacity to travel. There may be a frequent share of travel necessary depending on the area to reach the people. Traveling to rural, remote, or underserved places, in particular, may be prevalent. It is also possible that community health nurses will need to make arrangements with local organizations to meet them.
ADPIE Care Plan for Community Health Problems
The nursing process in a community involves health planning. It is a continual social process in which data in a certain area is collected and analyzed in order to establish a strategy for generating new ideas, meeting identified requirements, resolving health issues, and guiding changes in the delivery of health care.
The majority of nurses in the community are required to design strategies and actions for the entire community’s health needs, not just for the health of a single person. It involves the process of problem-solving which is centered on a certain group of people.
Assessments of communities are made, needs and problems are prioritized, goals are set, and methods for achieving them are developed. When planning care for a group or a population, the term program planning is frequently used to refer to the process of planning care for a community.
Community health nurses also conduct health assessments that collect a broader range of data than nurses in other fields. CHNs collect information on both individuals and families within the community.
They look at the data to see if it can be utilized to determine a population’s health, resources, or needs. They also look into how a range of community factors affect the health of the people who live there.
Collaborating with the members of the community to validate nursing diagnoses based on the assessment and enlisting community members’ support and cooperation in accomplishing change are all essential tasks. T
he program may not be successful if the community is not involved from the start. You will have a more successful program if you incorporate the community in the assessment and planning phases, just as you will have better adherence and outcomes from planning care with an individual client.
The nursing process in a community setting can be illustrated in the following scenarios:
Community Health Nursing Diagnosis
Community health nursing care plan 1.
Altered health-seeking behaviors
Assessment: The older adults are expanding rapidly in ABC County, a suburban community. According to the records, there is only one taxicab service company in the area, which causes limited public transportation.
Nursing Diagnosis: Altered health-seeking behaviors related to insufficient transport services for senior citizens.
Desired Outcome:
The community, particularly the senior citizens, will improve their health-seeking behaviors through participation in organized health activities and programs.
Community Health Nursing Care Plan 2
Risk of Cardiovascular Diseases
Assessment: According to figures from the District Health Department’s 2019 Annual Report, at least one person in every family in ABC County is obese , thereby increasing the risk of cardiovascular disease in the community.
The primary causes of this health concern are listed below:
- Lack of information about sedentary lifestyles, poor nutritional habits, and overweight/obesity as cardiovascular disease risk factors
- Lack of awareness of the risk factors, signs, and symptoms of cardiovascular diseases
- Uninformed of the risks of future complications of obesity such as cardiovascular diseases
- Limited access to fresh and nutritious food for everyone
- Inactive support from the community groups and state leaders
Nursing Diagnosis: Risk of cardiovascular diseases related to obesity among the residents of ABC County as demonstrated in an obesity rate of 40.1% and record of being the second-highest mortality risk for cardiovascular disease at 203/100,000 in their District.
Desired Outcomes:
Knowledge regarding the effects of and prevention of obesity will be dispersed to the citizens of ABC County, and the number of residents who are able to verbalize the effects of and prevention of obesity will be increased by 30% by the end of the year.
The community will have at least 5% decrease in statistical numbers of obese individuals, as measured by BMI, and consequently a reduction in deaths from cardiovascular diseases related to obesity at the end of 2025.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2017). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
16.3 Applying the Nursing Process to Community Health
Community health nurses apply the nursing process to address needs of individuals, families, vulnerable populations, and entire communities. See Figure 16.7 [1] for an illustration of the nursing process in community health nursing.

The community health nurse typically begins a community health needs assessment by determining what data is already available. [2] As previously discussed in the “ Community Health Concepts ” section, national, state, county, and local health needs assessments are widely available. Secondary analysis refers to analyzing previously collected data to determine community needs.
Community health nurses may also engage in primary data collection to better understand the community needs and/or study who may be affected by actions taken as a result of the assessment. [3] Primary data collection includes tools such as public forums, focus groups, interviews, windshield surveys, surveys, and participant observation.
Public Forums
Public forums are gatherings where large groups of citizens discuss important issues at well-publicized locations and times. Forums give people of diverse backgrounds a chance to express their views and enhance understanding of the community’s specific needs and resources. Forums should be planned in a convenient location with accessibility to public transportation and child care. They should also be scheduled at convenient times for working families to gain participation from a wide range of populations.
Focus Groups
Focus groups are a systematic method of data collection through small-group discussions led by a facilitator. Participants in focus groups are selected to represent a larger group of people. Groups of 6-10 people with similar backgrounds or interests are interviewed in an informal or formal setting. Focus groups should be scheduled at several dates and times to ensure a broad participation from members of the community. Here are advantages of focus groups:
- Community member involvement in assessing and planning community initiatives is encouraged.
- Different perceptions, values, and beliefs by community members are explored.
- Input can be obtained from specific subpopulations of the community. Example of subpopulations include young mothers caring for infants, individuals receiving home hospice care, individuals struggling to find housing, residents of the prison system, individuals coping with mental health disorders, or residents in group homes.
Interviews are structured conversations with individuals who have experience, knowledge, or understanding about a particular topic or issue. Key informant interviews are conducted with people in key positions in the community and have specific areas of knowledge and experience. These interviews can be useful for exploring specific community problems and/or assessing a community’s readiness to address those problems. [4]
Advantages of interviews include the following [5] :
- They can be conducted in a variety of settings (e.g., homes, schools, churches, stores, or community centers).
- They are low cost and generally have low dropout rates.
- Respondents define what is important from their perspective.
- It is possible to explore issues in depth, and there is an opportunity to clarify responses.
- They can provide leads to other data sources and key informants.
- They provide an opportunity to build partnerships with community members.
- Data can be compared among local government officials, citizens, and non-government leaders.
Interviews can have these disadvantages:
- Interviews can be time-consuming to schedule and perform.
- They require trained interviewers.
- There is a potential for interviewer bias to affect the data collected during the interview.
- Rapport must be established before sensitive information is shared.
- It is more time-consuming to summarize and analyze findings.
Windshield Surveys
A windshield survey is a type of direct observation of community needs while driving and literally looking through the windshield. It can be used to observe characteristics of a community that impact health needs such as housing, pollution, parks and recreation areas, transportation, health and social services agencies, industries, grocery stores, schools, and religious institutions.
View the following YouTube video of a windshield survey [6] : Windshield Survey Nursing .
Surveys use standardized questions that are relatively easy to analyze. They are beneficial for collecting information across a large geographic area, obtaining input from as many people as possible, and exploring sensitive topics. [7] Surveys can be conducted face to face, via the telephone, mailed, or shared on a website. Responses are typically anonymous but demographic information is often collected to focus on the needs of specific populations. Disadvantages of surveys can include the following [8] :
- Surveys can be time-consuming to design, implement, and analyze the results.
- The accuracy of survey results depends on who is surveyed and the size of the sample.
- Mailed surveys may have low response rates with higher costs due to postage.
- They offer little opportunity to explore issues in depth, and questions cannot be clarified.
- There is no opportunity to build rapport with respondents.
Participant Observation
Participant observation refers to nurses informally collecting data as a member of the community in which they live and work. This is considered a subjective observation because it is from the nurse’s perspective. Informal observations are made, or discussions are elicited among peers and neighbors within the community.
Sociocultural Considerations
When analyzing community health needs, it is essential to do so through a sociocultural lens. Just as an individual’s health can be influenced by a wide variety of causes, community health problems are affected by various factors in the community. For example, a high rate of cancer in one community could be related to environmental factors such as pollution from local industry, but in another community, it may be related to the overall aging of the population. Both communities have a high rate of cancer, but the public health response would be very different. Another example related to mental health is related to various situational factors affecting depression. A high rate of depression in one community may be related to socioeconomic factors such as low-paying jobs, lack of support systems, and poor access to basic needs like grocery stores, whereas in another community it may be related to lack of community resources during frequent weather disasters. The public health response would be different for these two communities.
Nurses must also recognize and value cultural differences such as health beliefs, practices, and linguistic needs of diverse populations. They must take steps to identify subpopulations who are vulnerable to health disparities and further investigate the causes and potential interventions for these disparities. For example, mental health disparities pose a significant threat to vulnerable populations in our society, such as high rates of suicide among LGBTQ+ youth, reduced access to prevention services among people living in rural areas, and elevated rates of substance misuse among Native Americans. These disparities threaten the health and wellness of these populations. [9]
Key points to consider when assessing a community using a sociocultural lens include the following:
- Have the trends of assessment data changed over time? What are the potential causes for these changes in this community?
- How does the community’s needs assessment data compare to similar communities at local, county, state, and national levels? What target goals and health initiatives have been successfully implemented in other communities?
- What vulnerable subpopulations are part of this community, and what health disparities are they experiencing? What are potential causes and solutions for these health disparities?
- Input from members of vulnerable subpopulations must be solicited regarding their perspectives on health disparities, as well as barriers they are experiencing in accessing health care.
Similar to how nurses individualize nursing diagnoses for clients based on priority nursing problems identified during a head-to-toe assessment, community health nurses use community health needs assessment data to develop community health diagnoses. These diagnoses are broad, apply to larger groups of individuals, and address the priority health needs of the community. Resources such as Healthy People 2030 can be used to determine current public health priorities.
A community diagnosis is a summary statement resulting from analysis of the data collected from a community health needs assessment. [10] A clear statement of the problem, as well as causes of the problem, should be included. A detailed community diagnosis helps guide community health initiatives that include nursing interventions.
A community diagnosis can address health deficits or services that support health in the community. A community diagnosis may also address a need for increased wellness in the community. Community diagnoses should include these four parts:
- The problem
- The population or vulnerable group
- The effects of the problem on the population/vulnerable group
- The indicators of the problem in this community
Here are some examples of community health diagnoses based on community health needs assessments:
- Community Scenario A
- Assessment data: The local high school has had a 50% increase in the number of teen pregnancies in the past year, causing high school graduation rates to decrease due to pregnant students dropping out of high school.
- Community diagnosis: Increased need for additional birth control and resources for prevention of pregnancy due to lack of current resources, as evidenced by 50% increase in teen pregnancies in the last year and a decrease in graduation rates.
- Community Scenario B
- Assessment data: Fifty percent of residents of an assisted living facility were found to have blood pressure readings higher than 130/80 mmHg during a health fair last week at the facility.
- Community diagnosis: Increased need for education about exercise and diet and referrals to primary care doctors for residents of an assisted living facility due to increased risk for mortality related to high blood pressure, as evidenced by a high number of residents with high blood pressure during a health fair.
- Community Scenario C
- Assessment data: The local high school has had two cases of suicide in the past year.
- Diagnosis: Increased need for community education regarding suicide prevention and crisis hotlines, as evidenced by an increase in adolescent suicide over the past twelve months.
Outcomes Identification
Outcomes refer to the changes in communities that nursing interventions and prevention strategies are intended to produce. Outcomes include broad overall goals for the community, as well as specific outcomes referred to as “SMART” outcomes that are specific, measurable, achievable, realistic, and with a timeline established.
Broad goals for communities can be tied to national objectives established by Healthy People 2030, as previously discussed in the “ Community Health Concepts ” section.
Healthy People objectives are classified by these five categories [11] :
- Health Conditions
- Health Behaviors
- Populations
- Settings and Systems
- Social Determinants of Health
SMART outcomes can be created based on the objectives listed under each category. For example, if an overall community goal is related to “Drug and Alcohol Use” under the “Health Behaviors” category, a SMART outcome could be based on the Healthy People objective, “Increase the proportion of people with a substance use disorder who got treatment in the past year.” [12] Based on this Healthy People objective, an example of a SMART outcome could be the following:
- The proportion of people treated for a substance disorder in Smith County will increase to 14% within the next year.
View the Healthy People 2030 Objectives and Community Objectives .
Planning Interventions
Nursing interventions for the community can be planned based on the related Healthy People category and objective. For example, based on the sample SMART outcome previously discussed, a planned nursing intervention could be the following:
- The nurse will provide education and materials regarding evidence-based screening practices for substance use disorder in local clinics.
Community health nursing interventions typically focus on prevention of illness with health promotion interventions. After performing a community health needs assessment, identifying priority problems, and establishing health goals and SMART outcomes, the nurse integrates knowledge of health disorders (e.g., diabetes, cancer, obesity, or mental health disorders) and current health risks in a community to plan prevention interventions.
There are two common public health frameworks used to plan prevention interventions. A traditional preventive framework is based on primary, secondary, or tertiary prevention interventions. A second framework, often referred to as the Continuum of Care Prevention Model, was established by the Institute of Medicine (IOM) and includes universal, selected, and indicated prevention interventions. Both frameworks are further discussed in the following sections. [13]
Primordial, Primary, Secondary, Tertiary, and Quaternary Interventions
Preventive health interventions may include primordial, primary, secondary, tertiary, and quaternary prevention interventions. These strategies attempt to prevent the onset of disease, reduce complications of disease that develops, and promote quality of life. [14]
Primordial Prevention
Primordial prevention consists of risk factor reduction strategies focused on social and environmental conditions that affect vulnerable populations. In other words, primordial prevention interventions target underlying social determinants of health that can cause disease. These measures are typically promoted through laws and national policy. An example of a primordial prevention strategy is improving access to urban neighborhood playgrounds to promote physical activity in children and reduce their risk for developing obesity, diabetes, and cardiovascular disease. [15] See Figure 16.8 [16] for an image of a neighborhood playground.

Primary Prevention
Primary prevention consists of interventions aimed at susceptible populations or individuals to prevent disease from occurring. An example of primary prevention is immunizations. [17] Nursing primary prevention interventions also include public education and promotion of healthy behaviors. [18] See Figure 16.9 [19] for an image of an immunization clinic sponsored by a student nurses’ association.

Secondary Prevention
Secondary prevention emphasizes early detection of disease and targets healthy-appearing individuals with subclinical forms of disease. Subclinical disease refers to pathologic changes with no observable signs or symptoms. Secondary prevention includes screenings such as annual mammograms, routine colonoscopies, Papanicolaou (Pap) smears, as well as screening for depression and substance use disorders. [20] Nurses provide education to community members about the importance of these screenings. See Figure 16.10 [21] for an image of a mammogram.

Tertiary Prevention
Tertiary prevention is implemented for symptomatic clients to reduce the severity of the disease and potential long-term complications. While secondary prevention seeks to prevent the onset of illness, tertiary prevention aims to reduce the effects of the disease after it is diagnosed in an individual. [22] For example, rehabilitation therapy after an individual experiences a cerebrovascular accident (i.e., stroke) is an example of tertiary prevention. See Figure 16.11 [23] for an image of a client receiving rehabilitation after experiencing a stroke.
The goals of tertiary prevention interventions are to reduce disability, promote curative therapy for a disease or injury, and prevent death. Nurses may be involved in providing ongoing home health services in clients’ homes as a component of interprofessional tertiary prevention efforts. Health education to prevent the worsening or recurrence of disease is also provided by nurses.

Quaternary Prevention
Quaternary prevention refers to actions taken to protect individuals from medical interventions that are likely to cause more harm than good and to suggest interventions that are ethically acceptable. Targeted populations are those at risk of overmedicalization. [24] An example of quaternary prevention is encouraging clients with terminal illness who are approaching end of life to seek focus on comfort and quality of life and consider hospice care rather than undergo invasive procedures that will likely have no impact on recovery from disease.
See additional examples of primordial, primary, secondary, tertiary, and quaternary prevention strategies in Table 16.3a.
Table 16.3a Examples of Prevention Interventions [25] , [26]
In the United States, several governing bodies make prevention recommendations. For example, the United States Preventive Services Task Force (USPSTF) makes recommendations for primary and secondary prevention strategies, and the Women’s Preventive Services Initiative (WPSI) makes recommendations specifically for females. The Advisory Committee on Immunizations Practices (ACIP) makes recommendations for vaccinations, and various specialty organizations such as the American College of Obstetrics and Gynecology (ACOG) and the American Cancer Society (ACS) make preventative care recommendations. Preventive services have been proven to be an essential aspect of health care but are consistently underutilized in the United States. [27] Nurses can help advocate for the adoption of evidence-based prevention strategies in their communities and places of employment.
Continuum of Care Prevention Model
A second framework for prevention interventions, referred to as the “Continuum of Care Prevention Model,” was originally proposed by the Institute of Medicine (IOM) in 1994 and has been adopted by the Substance Abuse and Mental Health Services Administration (SAMHSA). [28] See Figure 16.12 [29] for an illustration of the Continuum of Care Prevention Model.
![]”This image is derivative of the “IOM “protractor” by unknown author and is included on the basis of Fair Use. Access for free at http://www.ca-sdfsc.org/docs/resources/SDFSC_IOM_Policy.pdf Image showing a Continuum of Care Prevention Model](https://wtcs.pressbooks.pub/app/uploads/sites/35/2022/03/coc-protractor.png)
The Continuum of Care Prevention Model can be used to illustrate a continuum of mental health services for community members that includes prevention, treatment, and maintenance care:
- Universal prevention : Interventions designed to reach entire groups, such as those in schools, workplaces, or entire communities. [30] , [31] For example, wellness sessions regarding substance misuse can be planned and implemented at a local high school.
- Selected prevention : Interventions that target individuals or groups with greater risk factors (and perhaps fewer protective factors) than the broader population. [32] , [33] For example, a research study showed that wellness programs implemented for adolescents who were already using alcohol or drugs reduced the quantity and frequency of their alcohol use and reduced episodes of binge drinking. [34]
- Indicated prevention : Interventions that target individuals who have a high probability of developing disease. [35] For example, interventions may be planned for adolescents who show early signs of substance misuse but have not yet been diagnosed with a substance use disorder. Interventions may include referrals to community support services for adolescents who have violated school alcohol or drug policies. [36]
- Treatment refers to identification of a mental health disorder and standard treatment for the known disorder. Treatment also includes interventions to reduce the likelihood of future co-occurring disorders. [37]
- Maintenance refers to long-term treatment to reduce relapse and recurrence, as well as provision of after-care services such as rehabilitation. [38]
See additional examples of prevention strategies using the Continuum of Care Prevention Model in Table 16.3b.
Table 16.3b Examples of Continuum of Care Prevention Strategies
Read A Guide to SAMHSA’s Strategic Prevention Framework PDF for more about planning prevention strategies for substance misuse and related mental health problems.
Culturally Competent Interventions
To overcome systemic barriers that can contribute to health disparities, nurses must recognize and value cultural differences of diverse populations and develop prevention programs and interventions in ways that ensure members of these populations benefit from their efforts. [39]
SAMHSA identified the following cultural competence principles for planning prevention interventions [40] :
- Include the targeted population in needs assessments and prevention planning
- Use a population-based definition of community (i.e., let the community define itself)
- Stress the importance of relevant, culturally appropriate prevention approaches
- Promote cultural competence among program staff
Review additional concepts related to culturally responsive care in the “ Diverse Patients ” chapter of Open RN Nursing Fundamentals .
Evidence-Based Practice
It is essential to incorporate evidence-based practice when planning community health interventions. SAMHSA provides an evidence-based practice resource center for preventive practices related to mental health and substance abuse. See these resources, as well as examples of evidence-based programs and practices in the following box.
Examples of Evidence Based Prevention Practices related to Mental Health and Substance Misuse [41]
- Blueprints for Healthy Youth Development : Youth violence, delinquency, and drug prevention and intervention programs that meet a strict scientific standard of program effectiveness
- Evidence-Based Behavioral Practice (EBBP) : A project that creates training resources to help bridge the gap between behavioral health research and practice
- SAMHSA’s Suicide Prevention Research Center (SPRC) : A best practices registry that identifies, reviews, and disseminates information about best practices that address specific objectives of the National Strategy for Suicide Prevention
- The Athena Forum: Prevention 101 : Substance misuse prevention programs and strategies with evidence of success from the Washington State Department of Social and Health Services
- National Institute on Drug Abuse: Preventing Drug Use Among Children and Adolescents : Research-based drug abuse prevention principles and an overview of program planning, including universal, selected, and indicated interventions
View the SAMHSA Evidence-Based Practice Resource Center .
Implementation
Community health nurses collaborate with individuals, community organizations, health facilities, and local governments for successful implementation of community health initiatives. Depending on the established community health needs, goals, outcomes, and target group, the implementation of nursing interventions can be categorized as clinical, behavioral, or environmental prevention:
- Clinical prevention : Interventions are delivered one-on-one to individuals in a direct care setting. Examples of clinical prevention interventions include vaccine clinics, blood pressure monitoring, and screening for disease.
- Behavioral prevention : Interventions are implemented to encourage individuals to change habits or behaviors by using health promotion strategies. Examples of behavioral prevention interventions include community exercise programs, smoking cessation campaigns, or promotion of responsible alcohol drinking by adults.
- Environmental prevention : Interventions are implemented for the entire community when laws, policies, physical environments, or community structures influence a community’s health. Examples of environmental prevention strategies include improving clean water systems, establishing no-smoking ordinances, or developing community parks and green spaces.
When evaluating the effectiveness of community health initiatives, nurses refer to the established goals and SMART outcomes to determine if they were met by the timeline indicated. In general, the following questions are asked during the evaluation stage:
- Did the health of the community improve through the interventions put into place?
- Are additional adaptations or changes to the interventions needed to improve outcomes in the community?
- What additional changes are needed to improve the health of the community?
- Have additional priority problems been identified?
- “ Nursing Process in Community Health Nursing ” by Open RN project is licensed under CC BY 4.0 ↵
- Community Tool Box by Center for Community Health and Development at the University of Kansas is licensed under CC BY NC SA 3.0 ↵
- A Guide to SAMHSA’s Strategic Prevention Framework by Substance Abuse and Mental Health Services Administration is available in the Public Domain . ↵
- Medrea, R. (2014, July 20). Windshield survey nursing [Video]. YouTube. All rights reserved. https://youtu.be/aAzW1bW_Dbw ↵
- McDonald, L. (2006). Florence Nightingale and public health policy: Theory, activism and public administration. University of Guelph. https://cwfn.uoguelph.ca/nursing-health-care/fn-and-public-health-policy/ ↵
- Office of Disease Prevention and Health Promotion. Healthy People 2030: Building a healthier future for all. U.S. Department of Health and Human Services. https://health.gov/healthypeople ↵
- Savage, C. L. (2020). Public/community health and nursing practice: Caring for populations (2nd ed.). FA Davis. ↵
- This work is a derivative of StatPearls by Kisling and Das and is licensed under CC BY 4.0 ↵
- “ Playground_at_Hudson_Springs_Park.jpg ” by Kevin Payravi is licensed under CC BY-SA 3.0 ↵
- “ 10442934136_1f910af332_b ” by Lower Columbia College (LCC) is licensed under CC BY_NC-ND 2.0 ↵
- “ US_Navy_021025-N-6498N-001_Mammogram_technician,_aids_a_patient_in_completing_her_annual_mammogram_evaluation.jpg ” by U.S. Navy photo by Ensign Ann-Marie Al Noad is in the Public Domain . ↵
- “ tech_zerog.jpg ” by unknown author at Gaylord.org is included on the basis of Fair Use ↵
- National Research Council (US); Institute of Medicine (US) Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults; and Research Advances and Promising Interventions. Defining the scope of prevention. (2009). In M. E. O’Connell & Warner B. T. (Eds). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. In Research advances and promising interventions. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK32789/ ↵
- This image is a derivative of the “IOM protractor” by unknown author and is included on the basis of Fair Use. Access for free at http://www.ca-sdfsc.org/docs/resources/SDFSC_IOM_Policy.pdf ↵
- A Guide to SAMHSA’s Strategic Prevention Framework by Substance Abuse and Mental Health Services Administration is available in the Public Domain. ↵
- Werch, C., Moore, M. J., DiClemente, C. C., Bledsoe, R., & Jobli, E. (2005). A multihealth behavior intervention integrating physical activity and substance use prevention for adolescents. Prevention Science, 6 (213). https://doi.org/10.1007/s11121-005-0012-3 ↵
- Substance Abuse and Mental Health Services Administration. (2019, July 19). Finding evidence-based programs and practices. https://www.samhsa.gov/sites/default/files/20190719-samhsa-finding_evidence-based-programs-practices.pdf ↵
Analyzing previously collected data to determine community needs.
Data collection that occurs through public forums, focus groups, interviews, windshield surveys, surveys, and participant observation.
Gatherings where large groups of citizens discuss important issues at well-publicized locations and times.
Systematic method of data collection through small-group discussions led by a facilitator.
Structured conversations with individuals who have experience, knowledge, or understanding about a particular topic or issue.
Interviews conducted with people in key positions in the community and have specific areas of knowledge and experience.
Type of direct observation of community needs while driving and literally looking through the windshield.
Standardized questions that are relatively easy to analyze.
A summary statement resulting from analysis of the data collected from a community health needs assessment.
Risk factor reduction strategies focused on social and environmental conditions that affect vulnerable populations.
Interventions aimed at susceptible populations or individuals to prevent disease from occurring.
The early detection of disease and targets healthy-appearing individuals with subclinical forms of disease.
Implemented for symptomatic clients to reduce the severity of the disease and potential long-term complications.
Actions taken to protect individuals from medical interventions that are likely to cause more harm than good and to suggest interventions that are ethically acceptable.
Interventions designed to reach entire groups, such as those in schools, workplaces, or entire communities.
Interventions that target individuals or groups with greater risk factors (and perhaps fewer protective factors) than the broader population.
Interventions that target individuals who have a high probability of developing disease.
Interventions are delivered one-on-one to individuals in a direct care setting.
Interventions are implemented to encourage individuals to change habits or behaviors by using health promotion strategies.
Interventions are implemented for the entire community when laws, policies, physical environments, or community structures influence a community’s health.
Nursing: Mental Health and Community Concepts Copyright © 2022 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
📕 Studying HQ
Exploring community health nursing research topics: a comprehensive guide for nursing students, carla johnson.
- August 25, 2023
- Essay Topics and Ideas
Community health nursing is a dynamic and vital field within the nursing profession, focused on providing holistic care to populations within a defined community. This specialized branch of nursing goes beyond individual patient care, extending its reach to families, groups, and entire communities. This article will delve into community health nursing, explore its significance, and provide valuable resources for nursing students to engage in research, evidence-based practice (EBP) projects, capstone projects, research paper topics, research questions, and essay ideas.
What You'll Learn
Understanding Community Health Nursing: A Holistic Approach
Community health nursing emphasizes preventive care , health promotion, and disease prevention within a specific community. This holistic approach involves understanding the community’s unique needs, cultures, and challenges to provide targeted interventions that improve health outcomes. As nursing students, you will find this field to be a gateway to understanding the broader healthcare landscape and the interconnectedness of various factors that influence health.

PICOT Questions on Community Health Nursing
- P: Adult population in psychiatric care ; I: Implementation of daily RS questionnaire; C: Units without the daily survey; O: Reduction in utilization of restraint and seclusion; T: 6 months. Can the implementation of a daily RS (Restraint and Seclusion) questionnaire for adults in psychiatric care lead to a significant decrease in the utilization of restraint and seclusion within a period of 6 months?
- P: Pediatric population in school settings; I: Introduction of daily exercise regimen; C: Schools without daily exercise; O: Improvement in BMI and overall fitness; T: 1 academic year. Does introducing a daily exercise regimen in school settings for pediatric populations result in a noticeable improvement in BMI and overall fitness over the course of 1 academic year?
- P: Elderly population in assisted living facilities; I: Implementation of fall prevention program; C: Facilities without fall prevention program; O: Reduction in fall-related injuries; T: 1 year. Is there a significant reduction in fall-related injuries among the elderly residing in assisted living facilities after the implementation of a comprehensive fall prevention program within 1 year?
- P: Low-income pregnant women; I: Provision of prenatal education classes; C: Those without access to prenatal education; O: Increase in prenatal knowledge and healthier pregnancy outcomes; T: Throughout gestation. Can providing prenatal education classes to low-income pregnant women lead to increased prenatal knowledge and improved pregnancy outcomes when compared to those without access to such education?
- P: Diabetic population within the community; I: Establishment of a mobile diabetic clinic; C: No mobile clinic available; O: Enhanced diabetic management and reduced hospitalizations; T: 2 years. Does the establishment of a mobile diabetic clinic within the community lead to better diabetic management and a decrease in hospitalizations over a span of 2 years?
- P: Adolescent population in schools; I: Implementation of comprehensive sexual education; C: Schools with standard sexual education; O: Reduction in teen pregnancies and sexually transmitted infections (STIs); T: 3 years. Over a period of 3 years, does the implementation of comprehensive sexual education in schools result in a significant decrease in the rates of teen pregnancies and STIs among adolescents compared to schools with standard sexual education?
- P: Homeless population; I: Launch of mobile healthcare unit; C: No access to regular healthcare; O: Improvement in overall health status and decrease in emergency room visits; T: 1 year. Can the introduction of a mobile healthcare unit for the homeless population improve their overall health status and a noticeable reduction in emergency room visits within a year?
- P: Rural elderly population; I: Initiation of telehealth services ; C: Lack of telehealth services; O: Enhanced access to healthcare and better management of chronic conditions; T: 18 months. Does the introduction of telehealth services for the rural elderly population lead to increased access to healthcare services and improved management of chronic conditions over the course of 18 months?
- P: New mothers; I: Implementation of postpartum support groups; C: No postpartum support groups available; O: Reduction in postpartum depression rates and improved maternal well-being; T: 1 year. Can the implementation of postpartum support groups for new mothers lead to a significant reduction in postpartum depression rates and an overall improvement in maternal well-being within a year?
- P: LGBTQ+ youth; I: Creating safe spaces in schools; C: Absence of designated safe spaces; O: Decreased mental health challenges and higher academic achievement; T: Ongoing. Does creating safe spaces within schools for LGBTQ+ youth lead to a noticeable decrease in mental health challenges and a rise in academic achievement over an ongoing period?
Evidence-Based Practice Projects Ideas
- Evaluating the effectiveness of community-wide vaccination drives in reducing vaccine-preventable diseases.
- Assessing the impact of a smoke-free policy in public spaces on community members’ respiratory health.
- Investigating the outcomes of a nutrition education program in improving dietary habits among low-income families.
- Analyzing the effectiveness of a community-based mental health awareness campaign in reducing stigma and increasing help-seeking behavior.
- Exploring the outcomes of a diabetes management intervention using mobile health apps in urban communities.
- Studying the effects of a community gardening initiative on physical activity levels and nutrition awareness.
- Investigating the utilization and impact of telemedicine services in remote rural areas.
- Assessing the benefits of a community fitness program on cardiovascular health and overall well-being.
- Evaluating the effectiveness of a school-based anti-bullying campaign on students’ mental health.
- Analyzing the outcomes of a community-driven initiative to increase access to clean drinking water in underserved areas.
Nursing Capstone Project Ideas
- Developing a comprehensive disaster preparedness plan for a local community.
- Designing and implementing a culturally sensitive prenatal care program for immigrant populations.
- Creating a curriculum for training community health workers in identifying and addressing social determinants of health.
- Establishing a support network for caregivers of elderly individuals living at home.
- Designing a mental health first aid training program for community leaders and volunteers.
- Implementing a community-based program to promote physical activity among children with obesity.
- Creating a resource guide for LGBTQ+ youth to access healthcare services without discrimination.
- Developing a community-wide initiative to combat opioid misuse and overdose.
- Establishing a telehealth platform for remote health consultations in underserved regions.
- Designing a comprehensive sexual education curriculum for high schools to address varying cultural norms.
Nursing Research Paper Topics
- The impact of community health nursing interventions on reducing health disparities .
- Exploring the role of community health nurses in disaster response and recovery.
- Analyzing the effectiveness of school-based health clinics in improving student health outcomes.
- Investigating the barriers and facilitators of healthcare access in underserved rural communities.
- The role of community health nursing in promoting healthy aging and elderly care.
- Addressing mental health stigma through community-based interventions led by nurses.
- Analyzing the outcomes of community health education programs on reducing tobacco use .
- Exploring the relationship between community engagement and positive maternal-child health outcomes.
- The effectiveness of telehealth services in bridging healthcare gaps in remote areas.
- Investigating the impact of community health nursing in preventing and managing chronic diseases.
Community Health Nursing Research Questions
- How does the presence of community health nurses influence health outcomes in underserved urban neighborhoods?
- What are the key components of successful school-based vaccination programs , and how do they impact disease prevention?
- How do cultural competence and sensitivity affect the effectiveness of community health nursing interventions?
- What are the main challenges community health nurses face in addressing social determinants of health ?
- How does community engagement contribute to the sustainability of community health initiatives led by nurses?
- What strategies effectively promote mental health awareness and reduce stigma within communities?
- How do telehealth services improve access to healthcare for individuals in geographically isolated regions?
- What role do community health nurses play in detecting and managing chronic diseases ?
- How do community health interventions impact healthcare utilization patterns and costs?
- What are the outcomes of community health nursing programs focused on improving maternal and child health?
Essay Topic Ideas & Examples
- The Role of Community Health Nursing in Promoting Population Health.
- Addressing Health Disparities: The Impact of Community Health Nursing.
- Community-Based Approaches to Preventing Teenage Pregnancy .
- Telehealth: Bridging Healthcare Gaps in Underserved Communities.
- Cultural Competence in Community Health Nursing: Challenges and Strategies.
- Disaster Preparedness and Response: The Critical Role of Community Health Nurses.
- The Influence of Social Determinants of Health on Community Health Nursing Interventions.
- Community Health Education: Strategies for Promoting Healthy Lifestyles.
- Exploring the Connection Between Mental Health and Community Well-being.
- Innovations in Community Health Nursing: Harnessing Technology for Better Outcomes.
As nursing students, you are poised to become the next generation of community health nurses, armed with the knowledge and skills to impact the health and well-being of diverse populations positively. Community health nursing offers numerous opportunities for research, practice, and advocacy. By delving into PICOT questions, evidence-based practice projects, capstone projects, research paper topics, and research questions, you can deepen your understanding of this vital field and contribute to its growth. Don’t hesitate to seek our writing services if you need assistance with your community health nursing assignments or essays. We understand the demands of nursing education and are here to support you in your academic journey. Your dedication to improving community health is commendable, and together, we can pave the way for healthier, more vibrant communities.
Frequently Asked Questions (FAQs) About Community Health Nursing
- Is community health nursing the same as nursing? Community health nursing is a specialized branch of nursing that focuses on providing holistic care to populations within specific communities. While nursing is a broader field encompassing various specialties, community health nursing is distinct in its emphasis on preventive care and health promotion within communities.
- What are the qualifications of a community health nursing? To practice community health nursing, one typically needs a registered nurse (RN) license. Many community health nurses also hold a Bachelor of Science in Nursing (BSN) degree, and advanced practice may require additional education such as a Master of Science in Nursing (MSN) with a specialization in community health.
- Do community health nurses work in hospitals? While community health nurses primarily work in community settings like public health departments, schools, and clinics, they can also collaborate with hospitals to provide education, preventive care, and continuity of care to patients transitioning from hospital to home.
- Can a community health nurse become a doctor? Community health nurses can certainly pursue further education and career advancement, but the path to becoming a doctor is different. Becoming a doctor requires completing medical school and earning a medical degree (MD) or a doctor of osteopathic medicine (DO) degree, whereas community health nursing involves nursing education and training.
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Have a subject expert write for you now, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular topics.
Business StudyingHq Essay Topics and Ideas How to Guides Samples
- Nursing Solutions
- Study Guides
- Free Study Database for Essays
- Privacy Policy
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- How to Guides
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- Terms and Conditions
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
- Degree Completion Plans
- Course Guides
- Supplemental Instruction
- IT Helpdesk
- Academic Departments
- Doctoral Degrees
- Communications
- Criminal Justice
- Public Policy
- Strategic Leadership
- Worship Studies
- More Programs >
- Masters Degrees
- Applied Psychology
- Business Administration
- Clinical Mental Health Counseling
- Executive Leadership
- Healthcare Administration
- Political Science
- Public Administration
- Social Work
- Bachelor's Degrees
- Graphic Design
- Information Technology
- Paralegal Studies
- Sports Management
- Associate Degrees
- Christian Counseling
- Creative Writing
- Early Childhood Education
- Information Systems
- Interdisciplinary Studies
- Medical Office Assistant
- STEM Mathematics
- Undergraduate
- Christian Ministry
- Data Networking
- Project Management
- Biblical Studies
- Educational Tech. & Online Instruction
- General Business
- Health Promotion
- Theological Studies
- Curriculum and Instruction
- Instructional Design
- Higher Ed. Administration
- Special Education
- New Programs
- Biblical Counseling (BS)
- Chaplaincy (MA)
- Christian Leadership – Faith-Based Consulting (PhD)
- Educational Research (PhD)
- Fire Administration – Emergency Medical Services (BS)
- Geographic Information Systems – Commercial Logistics (MS)
- Healthcare Law and Compliance (MBA)
- Instructional Design and Technology (EdS)
- Interdisciplinary Research (MA)
- International Relations – Human Rights (MS)
- Philosophy, Politics, and Economics (BS)
- Special Education (EdD)
- Who Are We?
- Our Three A's
- Virtual Tour of Liberty's Campus
- What is a Nonprofit University?
- Why Choose Liberty?
- Accreditation
- Top 10 Reasons to Choose Liberty University
- Video Testimonials
- Annual Security Report
- Annual Security Report 2023
- Admission Information
- Getting Started With Liberty
- Admission Process
- Admission FAQs
- Academic Calendar
- Admission Resources
- Common Forms and Documents
- Technical Requirements
- Official Transcript Request Form
- Textbooks and Software
- Transferring to Liberty
- Transfer Students
- Experience Plus – Credit for Life Experience
- Transfer FAQs
- University Transcript Request Links
- Tuition Assistance
- First Responder Discount
- Military Tuition Discount
- Small Business Discount
- Corporate Tuition Assistance
- Corporate Tuition Affiliates
- Financial Basics
- Tuition & Fees
- Payment Plans
- Military Benefits
- Financial Check-In
- Financial Aid
- Financial Aid Process
- Financial Aid FAQs
- Grants & Loans
- Scholarship Opportunities
- Military Homepage
- Military Benefits Guide
- Discount on Tuition
- Doctoral Military Rate
- Veterans Benefits
- Academics and Programs
- Military Programs and Partnerships
- Military Benefits and Scholarships
- Community and Resources
- Top Used Links
- Upcoming Events
- Academic Advising
- Jerry Falwell Library
- Policies and Deadlines
- Liberty University Academic Calendar Online
- Academic Policies
- Information Technology (IT)
- Online Writing Center
- Honor Societies
- Student Advocate Office
- Flames Pass (Student ID)
- Online Student Life
- Office of Disability Accommodation Support
- Commonly Used Forms
- learn.liberty.edu
Strategies for Community Health Care – NURS 440
CG • Section 8WK • 11/08/2019 to 04/16/2020 • Modified 02/09/2022
Request Info
Course Description
For information regarding prerequisites for this course, please refer to the Academic Course Catalog .
To develop a broad-based understanding of nursing in today’s changing environment, the student must be aware of historical, ethical, and professional developments relevant to nursing beyond the acute care setting. Community health nursing integrates all aspects of the nursing process and considers the holistic care needs of a variety of populations and community groups. It is an integral part of baccalaureate education and is congruent with one of the nursing major’s objectives, the promotion of optimum health for individuals, families, and communities.
Course Assignment
After reading the Course Syllabus and Student Expectations , the student will complete the related checklist found in the Course Overview.
Discussions (2)
Discussions are collaborative learning experiences. Therefore, the student is required to create a thread in response to the provided prompt for each discussion. Each thread must be at least 300 words and demonstrate course-related knowledge. For each thread, the student must support his/ her assertions with at least 2 citations in current APA format and 1 biblical reference. In addition to the thread, the student is required to reply to 2 other classmates’ threads. Each reply must be at least 200 words and incorporate at least 1 citation and 1 biblical reference.
Measurable Learning Outcomes: 1; RN-BSN PLOs-1 and 3; BSN Essentials- I, III, and V
Community Clinical Location Submission Assignment
The student will choose a location and preceptor for the Community Clinical Experience and Log and submit it to the instructor for approval in Canvas.
Health Education Program Assignments
This assignment will be submitted in 2 parts. The student will outline a Community Health Plan and Health Education Lesson Plan for his/her community and implement this in his/her community.
HEP Part 1: Topic and Site Selection
The student will research a social issue that is affecting the health of your community. Submit a Word document that includes: a 100 – 250-word rationale addressing why you chose your topic and presentation site; discuss how you will work with the community to address the issue via an education program; discuss further the presentation site and how it was chosen as it relates to the identified community health issue.
HEP Part 2: Program Presentation
Using the CDC- HECAT, the student will devise Health Education Lesson Plan. Using the Health Education Lesson Plan, the student will deliver a 30-minute presentation, including a 10-minute question and answer period at a chosen community venue. The student will create a survey and hand it out to the audience upon completion of the presentation. Students will then write a minimum 500-word synopsis of the presentation and survey results. Current APA format must be used with at least 4 scholarly sources cited.
Measurable Learning Outcomes: 1 and 3; RN-BSN PLOs-1, 2, 3, 4, and 7; BSN Essentials- I, II, III, VI, VII, and VIII
Community Assessments
This assignment will be submitted in 3 parts. Using the student’s own community, subjective and objective information will be gathered to develop 2 community diagnoses. The nursing process will be further utilized to devise a plan to implement and evaluate for 1 of the devised diagnoses.
Part 1 – Community Assessment: Windshield Survey (Subjective Data)
The student will complete a windshield survey to assess the community.
Part 2 – Community Assessment: Objective Data Collection and Community Interview Assignment
After completing the windshield survey, the student will research information to gather objective data for the community. The student will further research the environmental health of their community. Finally, the student will interview 3 community members to gather insight regarding the community’s health.
Part 3 – Community Health Nursing Process Assignment
Using all of the information identified in Parts 1 – 2, the student will write 2 community health nursing diagnoses. Then, the student will use the ADPIE model to address 1 of the diagnoses.
Measurable Learning Outcomes: 2; RN-BSN PLOs- 3, 4, 6, and 7; BSN Essentials- I, II, VII, and VIII
Epidemiology Case Study Assignment
The student will review and complete an epidemiology case study.
Measurable Learning Outcomes: 1; RN-BSN PLOs- 3 and 6; BSN Essentials I, II, III and VII
Family Assessment Assignment
The student will identify and interview a multi-problem family (this may not be a personal friend or family member) as defined and described in the textbook. Information collected will be used to complete a Genogram or EcoMap diagram. Using the provided discussion topics, the student will further write a narrative summarizing the assessment of the family. The student will devise diagnoses based on the family information, as well as consider the role of the community health nurse in family case management.
Measurable Learning Outcomes: 2, 3, and 5; RN-BSN PLOs- 1, 2, 3, 4, 5, 6 and 7; BSN Essentials I, II, III, VI, VII and VIII
Disaster Response PowerPoint Assignment
Utilizing the textbook and at least 4 other scholarly sources, the student will develop a 10 – 15-slide (excluding the title and reference slide) PowerPoint presentation that addresses the steps of disaster management continuum, as well as the roles of the community nurse in a disaster.
Measurable Learning Outcomes: 1; RN-BSN PLOs- 3, 5, 6 and 7; BSN Essentials I, II, VII and VIII
Patient Education Assessment Assignment
Using the Simple Measure of Gobbledygook (SMOG) method, the student must select and analyze a piece of patient education literature. The student will discuss the SMOG method, research health literacy statistics and other vital statistics in his/her community, and then analyze the results to determine if the literature is appropriate. In addition, the student will write a narrative discussing the findings.
Measurable Learning Outcomes: 1 and 3; RN-BSN PLOs- 1 and 3; BSN Essentials I, II, III and V
Community Clinical Experience and Log Assignment
The student will complete 2 eight-hour shifts at a designated community location or with a community preceptor. All clinical experiences are subject to faculty approval. Completion of this clinical component and ALL course assignments is required to pass the course. The student will submit a clinical log documenting their experience using the template provided in the course. The student must note that since the course assignments contribute to the clinical requirement (even though they are not part of the 2 eight-hour shifts), completion of ALL assignments in the course is required to satisfactorily pass the clinical component of this course.
Measurable Learning Outcomes: 1 and 3; RN-BSN PLOs- 1, 2, 3, 4, 5, 6, and 7; BSN Essentials I, II, III, VI, VII and VIII
Almost there! How may we contact you?
Our Admissions team is ready to answer any additional questions you may have.
By submitting contact information through this form, I agree that Liberty University and its affiliates may call and/or text me about its offerings by any phone number I have provided and may provide in the future, including any wireless number, using automated technology.
Message and data rates may apply. For additional information, text HELP to 49595 or 49596. You may opt-out at any time by sending STOP to 49595 or 49596. Visit for Terms & Conditions and Privacy Policy.
- Get My Results
Discover what Liberty can do for you!
Get your personalized guide on how to start with liberty..
In 60 seconds or less!
Become a Champion for Christ
Estimate your Cost
Cost Per Credit Hour Per Semester for 7 to 15 Credits* Per Semester for 9 to 15 Credits* i Visit the Tuition and Financing page for more information.
Additional program fees may apply. See program page for details.
Disclaimer: This calculator is a tool that provides a rough estimate of the total cost of tuition, and should not be relied upon to determine overall costs, as pricing may vary by program and tuition/fees are subject to change. Estimates are not final or binding, and do not include potential financial aid eligibility.
Your Cost Estimate:
View All Tuition & Fees Go Back
For eligibility requirements for military discounts at the doctoral level, please review the online benefits page .
Request Information
Learn More About Liberty University Online
You will be automatically taken to the application once you submit your request for information
Message and data rates may apply. For additional information, text HELP to 49595 or 49596. You may opt-out at any time by sending STOP to 49595 or 49596. Visit for Terms & Conditions and Privacy Policy .
You have to have a lot of self-motivation and self-discipline when you are going to school online, but the amazing thing is at Liberty you do not need to do it by yourself. You really do have resources like someone who is going to school on campus.
– Janae Fleming ’15, B.S. in Education
What to Know about the Role of a Community Health Nurse
Community health/public health nurses are the largest segment of the U.S. public health workforce, so they play a vital role in creating healthy, equitable communities. They positively influence population health and can grow rewarding careers outside traditional healthcare settings.
Keep reading to learn about the role of a community health nurse, how they make a difference, and how you can embark on a fulfilling career in community-based nursing.
What Is Community Health Nursing?
According to the American Public Health Association (APHA), community health nursing is the “practice of promoting and protecting the health of populations.” Also known as public health nursing , it strives to further social justice and equity so that every population achieves optimal health.
Community health nurses serve individuals, families, and communities. They provide preventative and primary care and participate in advocacy, policy development, and planning to address the many environmental, physical, and social determinants of health.
Community-based nursing promotes health and well-being, maintains population health, and prevents illness, injury, and disability.
What Does a Community Health Nurse Do?
The role of a community health nurse is multifaceted. Generally, community health nurses may carry out any of the 10 Essential Public Health Services , including:
- Assessing and monitoring population health.
- Strengthening, supporting, and mobilizing communities and partnerships.
- Creating, championing, and implementing policies, plans, and laws.
The day-to-day activities of a community health nurse depend on where they work. A few examples are direct patient care, community outreach, and policy and advocacy.
Direct Patient Care
The role of a community health nurse can involve providing direct patient care .
Many community health nurses serve at-risk populations, such as people experiencing homelessness, people of color, and individuals with chronic diseases. These groups have an increased risk of poor health outcomes due to the disparities they face.
Community health nurses provide culturally competent, patient-centered care. They recognize and respect the diversity of the individuals and communities they serve, tailoring their approach to meet the unique needs of each person.
The direct patient care duties of community health nurses include:
- Performing health assessments and screenings to identify risk factors and social determinants of health.
- Educating patients on disease prevention and self-care so they can adopt healthy behaviors and manage chronic conditions.
- Triaging patients and providing medical care during natural disasters or humanitarian crises.
- Coordinating care with other healthcare providers and connecting patients to community resources and social services.
Community Outreach
Community health nurses partner with organizations and other healthcare providers to promote healthy behaviors and improved outcomes. Collaborative efforts take many forms, from health promotion and essential healthcare to community health assessment, such as:
- Developing and implementing health promotion activities, such as workshops and support groups, to empower community members to make healthy choices and improve their well-being.
- Delivering essential healthcare services to improve access and meet the community’s health needs, including blood drives and mobile clinics.
- Collaborating on health assessments, surveys, and research studies to collect data that develops programs addressing community health needs.
Policy and Advocacy
Another role of a community health nurse is promoting health equity.
Health equity refers to the presence of fair and just opportunities for everyone to attain optimal health. A society achieves health equity by changing the systems and policies that have created racial and ethnic health disparities.
Community health nurses advocate for policies that improve population health. They participate in policy analysis and development, legislative advocacy, and other activities that support the health and well-being of individuals and communities:
- Analyzing current policies about public health to identify strengths and opportunities for improvement.
- Communicating the health needs and experiences of vulnerable populations to planners and policymakers.
- Engaging with legislators to advocate for policies aligned with public health principles.
- Providing testimony and comment at legislative hearings and public meetings to influence policy making.
Where Do Community Health Nurses Work?
Community health nurses work in various settings across the public and private sectors, including:
- State and local health departments
- Schools, colleges, and universities
- Home health agencies
- Community centers
- Correctional facilities
- Advocacy groups
- Faith-based organizations
The responsibilities and role of a community health nurse vary depending on community needs and the organization's goals. However, they share a commitment to promoting health, addressing health disparities, and advancing health equity.
Why Become a Community Health Nurse?
There are many reasons to become a nurse. Community-based nursing is an attractive career path because of the opportunities to make a wide-ranging difference, pursue diverse jobs, and enjoy job stability.
Influence Population Health
Community health nurses make a meaningful difference by improving the health of individuals, families, and their communities. They promote health, prevent disease, and improve health outcomes while reducing disparities in healthcare outcomes. Many community health nurses derive great satisfaction from creating healthier, more equitable societies.
Explore Diverse Jobs
Community health nurses have many career prospects, from government and healthcare to schools and international non-profit organizations. They work with diverse populations in the U.S. and around the world. The role of a community health nurse could focus on many different areas of public health, including direct care, public policy, or leadership.
Experience Steady Employment
The number of community health nurses has declined, creating a high demand for the profession. The percentage of RNs employed in a community or public health setting decreased from approximately 7% in 2000 to 3% in 2018. Starting a career in community-based nursing can provide job stability.

How to Become a Community Health Nurse?
There are a few steps to becoming a community health nurse. You will need to complete nursing education and then obtain nursing licensure, which involves passing a national nursing exam. Licensed RNs can apply for community-based nursing positions and pursue an optional certification in public health.
Step 1: Earn a Nursing Degree
The first step in becoming a community health nurse is earning a degree in nursing. The APHA recommends that community health nurses have a minimum of a Bachelor of Science in Nursing (BSN) because it equips nurses with foundational knowledge and skills for community nursing care:
- Clinical prevention
- Population health
- Healthcare policy
- Regulatory environments
- Interprofessional collaboration
As a BSN student, you will grow your nursing expertise through coursework, simulations, and in-person clinical experiences .
Traditional BSN programs take four years to complete. If you have a bachelor’s degree in a non-nursing discipline, you can graduate from an accelerated BSN (ABSN) program in 11 to 18 months . ABSN programs take less time because they build on previous learning experiences, allowing students to start nursing coursework faster.
Step 2: Obtain Nursing Licensure
After graduating from a BSN program, you will need to acquire nursing licensure from the state where you plan to practice.
You will apply for licensure through your state board of nursing . The board of nursing will review your application and determine your eligibility to take the national nurse licensure exam, called the National Council Licensure Examination (NCLEX).
When you pass the NCLEX, you will become a licensed RN.
Step 3: Apply for Community Nursing Care Jobs
As a licensed RN, you can apply for community health nursing jobs. The Association of Public Health Nurses ( APHN ) and the American Public Health Association ( APHA ) are valuable resources for job opportunities. Both maintain large job listing directories.
Step 4 (Optional): Get Certified in Public Health
Community health nurses can obtain an optional certification in public health called the Certified in Public Health (CPH) credential . Administered by the National Board of Public Health Examiners, the CPH demonstrates knowledge of public health sciences and a commitment to the field.
There are several eligibility pathways for the CPH. RNs with a BSN are eligible once they have at least five years of public health work experience.
Start Your Career in Community Nursing Care with Saint Joseph’s College of Maine
Community-based nursing is a versatile and stable career path for improving social justice, health equity, and population health outcomes. Does the role of a community health nurse interest you?
You can change careers and become a BSN-prepared nurse in 15 months through the Hybrid Accelerated Bachelor of Science in Nursing (ABSN) program from Saint Joseph’s College of Maine (SJC). The accredited program is designed for individuals with a bachelor’s degree in any field, and no nursing experience is required.
Aspiring nurses choose SJC because of its emphasis on community. SJC welcomes people of all faiths, ages, and backgrounds. Together, students, faculty, and staff recognize learning as a tool for lifting themselves up in service to others.
Students learn in a community built on mutual respect and receive individualized attention, guidance, and mentoring from a team of passionate, experienced educators. Saint Joseph’s College of Maine’s BSN graduates have a first-time NCLEX pass rate of over 90%, demonstrating their readiness for a meaningful and rewarding career in nursing.
Start your path to promoting community health as a nurse. For more information, obtain your ABSN program guide today.

- Registered Nurse to Master of Science in Nursing in Administrative Leadership in Nursing
- Registered Nurse to Master of Science in Nursing in Nursing Education
- Registered Nurse to Master of Science in Nursing in Nursing Informatics
- Master of Science in Nursing in Administrative Leadership in Nursing
- Master of Science in Nursing in Nursing Education
- Master of Science in Nursing in Nursing Informatics
- Graduate Nursing Certificate in Administrative Leadership
- Graduate Nursing Certificate in Nursing Education
- Graduate Nursing Certificate in Nursing Informatics
- Accreditations, Accolades & Quick Facts
- Faculty Profiles
- Student Services
Welcome to our website! How did you hear about us? Take Survey »
Home » Degrees » RN to BSN » The Nurse's Role in Community Health
The Nurse’s Role in Community Health
- Published On: September 20, 2017
In the past, caregivers journeyed on horseback to the homes of their neighbors to provide medical services. These caregivers were crucial to reducing the mortality rates in their communities. After the civil war, hospitals were built. This began the implementation of organized healthcare. Today, nurses practice in a variety of settings and community health is again re-emerging as an integral part of providing care to everyone.
What Is Community Health Nursing?
Community health nursing is a discipline that incorporates evidenced-based research along with advances in science and new approaches for improving the health The practice takes into consideration the cultural and socioeconomic backgrounds of the people in the community to ensure appropriate interaction and sensitivity when working with them.
A community is a group of people in a specific location, which includes places where people live, work and go to school. Most people belong to multiple types of communities. Community health nursing is commonly practiced in geographic locations like cities and rural areas.
What Is the Goal of Community Health Nursing?
The goal of community health nursing is to promote, protect and preserve the health of the public. Community health nursing involves these basic concepts:
- Promote healthy lifestyle
- Prevent disease and health problems
- Provide direct care
- Educate community about managing chronic conditions and making healthy choices
- Evaluate a community’s delivery of patient care and wellness projects
- Institute health and wellness programs
- Conduct research to improve healthcare
What Is the Role of a Community Health Nurse?
The primary role of community health nurses is to provide treatment to patients. Additionally, community health nurses offer education to community members about maintaining their health so that they can decrease the occurrence of diseases and deaths. They plan educational assemblies, hand -out fliers, conduct health screenings, dispense medications and administer immunizations.
Nurses also may distribute health-related items like condoms and pregnancy tests. Examples of some health issues that community health nurses try to control or eliminate are:
- Infectious and sexually transmitted diseases
- Poor nutrition
- Substance abuse
- Teen pregnancy
Where Do Community Health Nurses Work?
Community health nurses work in hospitals, community centers, clinics, schools and government health agencies. Community health nurses are important to regions where healthcare is not easily accessible, so they can travel to remote places and isolated areas of a city.
How Do You Become a Community Health Nurse?
To become a community health nurse you must first work as a registered nurse. If you only have an associate degree you might want to consider completing a Bachelor of Science in Nursing (BSN) degree program. Many schools like Northeastern State University (NSU) offer RN to BSN programs .
NSU has an online RN to BSN program that includes the course Community Health Nursing. This course examines the theory and research used in nursing and the public health practice, which promotes and preserves the health of communities. Students are given the opportunity to apply their current knowledge and what they learn in the course. They are paired with a community and other healthcare professionals to experience community health nursing.
Nursing care should be available to every American. Throughout the country, there are entire communities of people prone to chronic illnesses, infectious diseases and economic hardships. Community health nurses have the ability to improve the welfare of individuals and their communities. They are at the forefront of bringing quality patient care to the most vulnerable and underserved members of society.
Learn more about Northeastern State University’s online RN to BSN program .
EveryNurse.org: Becoming a Community Health Nurse
Centers for Disease Control and Prevention: Benefits of Community Health
Government of the Northwest Territories: Community Health Nurses
ScienceDirect: What Is “Community Health”? Examining the Meaning of an Evolving Field in Public Health
Houston Chronicle: What Are the Primary Roles of the Community Nurse?
National Women’s History Museum: The Evolution of Nursing
Related Articles
Our commitment to content publishing accuracy.
Articles that appear on this website are for information purposes only. The nature of the information in all of the articles is intended to provide accurate and authoritative information in regard to the subject matter covered.
The information contained within this site has been sourced and presented with reasonable care. If there are errors, please contact us by completing the form below.
Timeliness: Note that most articles published on this website remain on the website indefinitely. Only those articles that have been published within the most recent months may be considered timely. We do not remove articles regardless of the date of publication, as many, but not all, of our earlier articles may still have important relevance to some of our visitors. Use appropriate caution in acting on the information of any article.
Report inaccurate article content:
- Email Address *
REQUEST INFORMATION
Submit this form, and an Enrollment Specialist will contact you to answer any questions.
*All fields required.
- Program of Interest * Program of Interest* Graduate Nursing Certificate in Administrative Leadership Graduate Nursing Certificate in Nursing Education Graduate Nursing Certificate in Nursing Informatics MSN in Administrative Leadership in Nursing MSN in Nursing Education MSN in Nursing Informatics RN to BSN RN to MSN in Administrative Leadership RN to MSN in Nursing Education RN to MSN in Nursing Informatics
- First Name *
- Last Name *
- How did you hear about us? * How did you hear about us?* Coworker Email Employer Family/Friend Information Session Magazine/Newspaper Online Professional Organization Radio/TV
- Comments This field is for validation purposes and should be left unchanged.
Or call 844-351-6656
By submitting this form, I am providing my digital signature agreeing that Northeastern State University (NSU) and its agent, Academic Partnerships, may email me or contact me regarding educational services by telephone and/or text message utilizing automated technology or a pre-recorded message at the telephone number(s) provided above. I understand this consent is not a condition to attend NSU or to purchase any other goods or services.

Begin Application Process
for help with any questions you have.

- Social Media
- Direct mail
- Search Engine
- Event/Conference
- This is my first time
- Within the last 30 days
- 1-2 months ago
- 3+ months ago
Request Information
- Portfolio Profile
Community Health Nursing: Self-Reflection Narrative
- Individual Strengths Statement
- Nursing Philosophy Statement
- Sample Course
- Internships
- Achievements

Self Reflection for Community Health Nursing
Community health nursing focus on health promotion, disease prevention and maintenance of health. The foundation of community-base nursing is evidence-based care.Information about the concerns, conditions and strengths of the populations and the community are gathered through community assessment which are then analyzed and identified. Community assets and their accessibility are also identified. Diversity in cultural, ethnic, economic, educational, linguistic, medical, physical, and social are recognized during the community assessment. I have the opportunity to practice as a community health nurse at the Stein Senior Center. This is a very interesting clinical experience because I was able to work with seniors not a critical or illness level. I learn to see and know what activity and program they are interested in during their leisure time when they relatively healthy. As mentioned in the beginning of the paragraph, community health nursing is able health promotion, disease prevention and maintenance of health, my clinical group conducted a health fair event beneficial to the seniors at the Stein Senior Center. Following are the objectives that I have met during the participation as a community health nurse at the Stein Senior Center.
Objective 1: Demonstrates individual professionalism through personal behaviors and appearance.
Maintaining client confidentiality is part of demonstrations of individual professionalism. I’m obligated to all information shared with me by the seniors confidential unless it causes harm to the persons. Individual professionalism also involves dressing professional to the work setting. I dress in business casual and wear sneaker to the clinical as per the request of the facility. This is not a hospital setting that requires scrub or lab coat. I dress who I represent, a nurse. Punctuality is important part of individual professionalism. It is also a respect to the facility as well as to the seniors. We as a class met with Robert F. Doxsey, the Deputy Director of the Stein Senior Center, every morning and discussed the upcoming events and changes at the center. The mission of the center is “to cultivate friendly relations among the members of the Stein Senior Center and the general public; the provide services with an emphasis on group growth; to share the strengths, and wisdom of senior citizens; and referral services, and to safeguard the health and wellness of senior citizens”. I assumed responsibility for my own learning by reading the materials, information, textbooks and nursing journals that help me prepare and practice better as the community health nurse. I completed all assignments given by the professor which further enhanced my learning. My professor was always available and provided me guidance.
Objective 2: Employ analytical reasoning and critical thinking skills when providing care to individuals and families in the community setting.
Analytical reasoning and critical thinking skills are important when providing care to clients. Analytical reasoning involves analyzing a situation, being able to look through the problem and think in a multi-dimensional way of the situation. Critical thinking is the objective analysis and evaluation of a situation with the intention to form a judgment or solution to the situation. There wasn’t much opportunity for hands on experience at the senior center. There was neither medical record for the seniors attended the center. Client information was collected through interview and information shared with by the seniors. I have done blood pressure screening. I was pleased to know that most of the seniors check their blood pressure at home regularly. They know what their normal blood pressure reading is and their medications for treating their hypertension. There was no opportunity to administer medications or treatments to the seniors: however, I assessed and reviewed the medications with the seniors. I emphasized to the seniors the indications and importance to adhere to their medication regimen. I also advised them not to stop taking any medication without notifying their care providers.
Objective 3: Effectively communicate with diverse groups and disciplines using a variety of strategies regarding the health needs of individuals and families in the community setting.
Therapeutic communication involves using broad opening statements, reflecting, sharing observations, acknowledging the seniors feelings, using silence, giving information, clarifying, verbalizing implied thoughts and feelings, exploring, presenting reality and validating. When approaching and interacting with the seniors at the center, I always greet them with a smile. I always introduce my name and profession to them. I have effectively communicated with the seniors by sharing, clarifying and validating their knowledge of health. Seniors may not process the information given to them at the same speed that they used to be; therefore, I talk to the seniors at the speed that they can follow. Paying attention to senior’s nonverbal cues is also important. I have met couple of the Asian seniors at the center. I approached to them and learned that they speak Chinese and limited English. I started interviewing them using their primary language. The seniors were very pleased that they have someone speak their language at the center. They were more opened up and willing to share their thoughts and concerns.
Objective 4: Establish environment conducive to learning and use a plan for learners based on evidence-based practice.
We have established environment conducive to learning for the seniors. During the health fair event, there were many health care providers participated and engaged in screening the seniors. The event provided the opportunity for the seniors to consult these health care providers with the questions that they have. Brochures containing health information were distributed to the seniors. The seniors were advised and referred to follow up with the health care providers as needed. During blood pressure screening, one to one learning opportunity was provided. Seniors are encouraged to ask questions that they may have. Medications and indications of the medications are reviewed with the seniors.
Objective 5: Utilize informational technology when managing individual and families in the community.
The center has computer lab for seniors to use which they can have access to internet and vital information. We also used the computers to do community research to prepare for the health fair event that we coordinated at the center. We used the computer to communicate with vendors, to create flyers, and to print out invitation letters to the vendor. Since this is a senior center, there is no electronical medical records of the members. Yet, all information shared with me by the seniors was kept confidential. I did not disclose information about the seniors to anyone else in or outside of the center. I would only disclose information if it would cause a health concern on the seniors.
Objective 6: Demonstrate a commitment to professional development.
To demonstrate the commitment to professional development, I completed all the required written assignments which enhanced my learning experience. I reflected upon my clinical experience with my classmates on my weekly blog. When caring for the seniors at the center, I always keep aware of my own cultural beliefs and values that vary from the seniors. Professional development also include using appropriate current literature in planning care. To assume responsibility for lifelong learning as a health profession, I must stay informed of evidence based practice to support my clinical practice through reading and researching.
Objective 7: Incorporate professional nursing standards and accountability into practice.
As a nurse, it is crucial to know and remember my nursing scope of practice and nursing code of ethics. It is important to check with American Nurse Association Standards to learn and update the professional nursing standards in clinical practice. The standards of professional nursing practice include assessing, diagnosing, planning, implementing and evaluating in a patient care. Ethical practice is pertinent in provide nursing care. According to the code of ethic in nusring, nurses have the duty to advocate for equitable care for their clients, Nurses have the obligation to keep client confidentiality within legal and regulatory parameters. Nurses also have to deliver care in a manner that preserves and protects client’s autonomy, dignity, rights, values and beliefs. Lastly , nurses should know and aware of the assigned agency’s mission. As I mentioned earlier in this self reflection, the mission of the Stein Senior Center is to “cultivate friendly relations among the members of the Stein Senior Center and the general public; the provide services with an emphasis on group growth; to share the strengths, and wisdom of senior citizens; and referral services, and to safeguard the health and wellness of senior citizens.”
Objective 8: Collaborate with clients, significant support persons and members of the health care team.
My clinical group set up, planned, coordinated and carried out a health fair event for the senior citizens at the Stein Senior Center. The staffs and the deputy director at the center were very helpful by giving us the contact list of the potential vendors. Works were disseminated among the group. We have created our own flyer of the event to the vendors and the members in the community. We were responsible for calling and emailing the invitation letter to all the vendors. We were also responsible for confirming the date with them. We also went out to the community and asked for donations to the seniors at the center. The community members were very nice and supportive to the event. On the day of the health fair, we set up the tables, table cloths, balloons and signs. We directed the seniors to each vendor and made sure that they visited all the vendors for needed health information. There were hearing screening, blood pressure screening, dental screening and many other more screenings at the health fair that the seniors could take advantage of.
Objective 9: Recognized the impact of economic, political, social and demographic forces that affect the delivery of health care services.
The impact of economic, political, social and demographic forces that affect the delivery of health care services were recognized in the research of the community. Through research, my clinical group has identified the major health problems that were needed in the community include but no limited to cancer, hypertension, diabetes mellitus, cardiovascular disease and Alzheimer’s Disease. I have recognized that not all seniors are insured or are under insured. There are many services are denied by insurances that used to cover. This is the gap in care system where seniors failed to receive needed care due to noncoverage. Many insurance companies such as Health First, BlueCross BlueShield and VNS were present at the health fair event to answer questions and provide details of the insurance coverage. Health educational information and brochures were provided and distributed to the senior citizens as well. We advocated for our members who need additional resources and helps they need in order to assist them in the delivery of health care services.
I have a wonderful opportunity to practice as a community health nurse at the Stein Senior Center. The service learning project has broaden my knowledge and clinical experience at a different level of care where clients are stable, active and relatively healthy. Community health nursing is evidence based practice care that focus on health promotion, disease prevention and maintain a healthy living. Community health nursing involve assessment of a community, diagnosis of needs in the community, planning how to increase health awareness in the community, implementing of the plan and evaluating the outcome of the plan. Professional nursing standards apply in all settings with the emphasis on keeping client confidentiality, advocating equitable healthcare to clients, and deliver care to clients in manner to preserve and protect client’s autonomy, dignity, rights, cultural values and beliefs.
- Write a brief paragraph to introduce yourself to your visitors and explain what they will find on this site. Be sure to add more developed content to your About Me page. (Edit this paragraph in Dashboard > Widgets > Text)
- Search for:
Learning Blog Archives
Recent posts, the openlab at city tech: a place to learn, work, and share.
The OpenLab is an open-source, digital platform designed to support teaching and learning at City Tech (New York City College of Technology), and to promote student and faculty engagement in the intellectual and social life of the college community.

New York City College of Technology | City University of New York
Accessibility
Our goal is to make the OpenLab accessible for all users.
Learn more about accessibility on the OpenLab
Creative Commons
- - Attribution
- - NonCommercial
- - ShareAlike

© New York City College of Technology | City University of New York
- Toggle navigation
The purpose of this course is to introduce students to community health nursing, health promotion and disease prevention across the life span. A major focus of this course is for students to critically think about and discuss the role of community health care nurse within a global environment. Nursing students will be exposed to the culturally diverse population, health disparities that exist in the United States and countries around the world, and some of the efforts by individuals, groups, organizations, and countries to deal with disparities. In addition, students will be provided with information and tools that nurses and nursing can use to confront health and health care challenges. Students will enhance critical thinking skills by planning and implementing a service-learning project in the vulnerable population community.
Upon completion of this course, the student will be able to:
- Analyze comprehensive and focused assessments (physical, psychosocial, socioeconomic, political, developmental, spiritual, cultural, educational, health care, and environmental) of diverse communities, groups, and populations.
- Evaluate one’s role and participation in emergency preparedness and disaster response with an awareness of environmental factors and the risks they pose to self, patients/clients, communities, groups, and populations in a multicultural environment.
- Use decision making skills, including the nursing process and problem solving processes, to deliver evidence-based care in the health promotion, maintenance, and restoration, disease and injury prevention, and rehabilitation of health and during disasters/ emergencies, mass casualties, and other crises that impact communities, groups, and populations, using developmentally and culturally appropriate approaches.
- Critically analyze evidence-based practice guidelines/research, nursing theories and theories from other disciplines that support the identification of clinical problems, prioritization of activities, implementation of nursing skills, and quality outcomes in the care of diverse communities, groups, and populations.
- Develop clinical prevention and population-focused interventions, using appropriate technological aids, with attention to effectiveness, efficiency, cost-effectiveness, and equity.
- Engage in purposeful collaboration and communication within a team to develop plans of care for communities, groups, and populations that take into account determinants of health, available resources, and the range of activities that contribute to health promotion, prevention of disease and injury, and emergency preparedness.
- Examine professional nursing concepts of social justice, advocacy, autonomy, human dignity, integrity, and altruism related to the health of vulnerable communities, groups, and populations and elimination of health disparities in a multicultural global environment.
- Online group discussions/forums
- Case studies
- Written assignments; individual and group
- PowerPoint presentations of textbook information
- Guest lecturers/presentations
Written examinations, submitted group papers, community project, group presentation, service-learning reflection paper.
The email feature is external communication that allows users to send emails to users enrolled in the course including the instructor and other students. Emails are sent to the student's FIU email on record.
Keep in mind that forum discussions are public, and care should be taken when determining what to post.
In order to mitigate any issues with your computer and online assessments, it is very important that you take the "Practice Quiz" from each computer you will be using to take your graded quizzes and exams. It is your responsibility to make sure your computer meets the minimum hardware requirements . Please note assessments in this course are not compatible with mobile devices and should not be taken through a mobile phone or a tablet. If you need further assistance please contact FIU Online Support Services .
Grading Criteria for the Community Health Nursing Theory
Grading Criteria for the Community Service-Learning Project Groups (selected the first week of class) will present their community project during the last few weeks of class. Criteria for grading and content of community project can be accessed on the Blackboard site for NUR 4636C.
F0 Below 60%

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

16.3: Applying the Nursing Process to Community Health
- Last updated
- Save as PDF
- Page ID 65651

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
Community health nurses apply the nursing process to address needs of individuals, families, vulnerable populations, and entire communities. See Figure 16.7 [1] for an illustration of the nursing process in community health nursing.

The community health nurse typically begins a community health needs assessment by determining what data is already available. [2] As previously discussed in the “ Community Health Concepts ” section, national, state, county, and local health needs assessments are widely available. Secondary analysis refers to analyzing previously collected data to determine community needs.
Community health nurses may also engage in primary data collection to better understand the community needs and/or study who may be affected by actions taken as a result of the assessment. [3] Primary data collection includes tools such as public forums, focus groups, interviews, windshield surveys, surveys, and participant observation.
Public Forums
Public forums are gatherings where large groups of citizens discuss important issues at well-publicized locations and times. Forums give people of diverse backgrounds a chance to express their views and enhance understanding of the community’s specific needs and resources. Forums should be planned in a convenient location with accessibility to public transportation and child care. They should also be scheduled at convenient times for working families to gain participation from a wide range of populations.
Focus Groups
Focus groups are a systematic method of data collection through small-group discussions led by a facilitator. Participants in focus groups are selected to represent a larger group of people. Groups of 6-10 people with similar backgrounds or interests are interviewed in an informal or formal setting. Focus groups should be scheduled at several dates and times to ensure a broad participation from members of the community. Here are advantages of focus groups:
- Community member involvement in assessing and planning community initiatives is encouraged.
- Different perceptions, values, and beliefs by community members are explored.
- Input can be obtained from specific subpopulations of the community. Example of subpopulations include young mothers caring for infants, individuals receiving home hospice care, individuals struggling to find housing, residents of the prison system, individuals coping with mental health disorders, or residents in group homes.
Interviews are structured conversations with individuals who have experience, knowledge, or understanding about a particular topic or issue. Key informant interviews are conducted with people in key positions in the community and have specific areas of knowledge and experience. These interviews can be useful for exploring specific community problems and/or assessing a community’s readiness to address those problems. [4]
Advantages of interviews include the following [5] :
- They can be conducted in a variety of settings (e.g., homes, schools, churches, stores, or community centers).
- They are low cost and generally have low dropout rates.
- Respondents define what is important from their perspective.
- It is possible to explore issues in depth, and there is an opportunity to clarify responses.
- They can provide leads to other data sources and key informants.
- They provide an opportunity to build partnerships with community members.
- Data can be compared among local government officials, citizens, and non-government leaders.
Interviews can have these disadvantages:
- Interviews can be time-consuming to schedule and perform.
- They require trained interviewers.
- There is a potential for interviewer bias to affect the data collected during the interview.
- Rapport must be established before sensitive information is shared.
- It is more time-consuming to summarize and analyze findings.
Windshield Surveys
A windshield survey is a type of direct observation of community needs while driving and literally looking through the windshield. It can be used to observe characteristics of a community that impact health needs such as housing, pollution, parks and recreation areas, transportation, health and social services agencies, industries, grocery stores, schools, and religious institutions.
View the following YouTube video of a windshield survey [6] : Windshield Survey Nursing .
Surveys use standardized questions that are relatively easy to analyze. They are beneficial for collecting information across a large geographic area, obtaining input from as many people as possible, and exploring sensitive topics. [7] Surveys can be conducted face to face, via the telephone, mailed, or shared on a website. Responses are typically anonymous but demographic information is often collected to focus on the needs of specific populations. Disadvantages of surveys can include the following [8] :
- Surveys can be time-consuming to design, implement, and analyze the results.
- The accuracy of survey results depends on who is surveyed and the size of the sample.
- Mailed surveys may have low response rates with higher costs due to postage.
- They offer little opportunity to explore issues in depth, and questions cannot be clarified.
- There is no opportunity to build rapport with respondents.
Participant Observation
Participant observation refers to nurses informally collecting data as a member of the community in which they live and work. This is considered a subjective observation because it is from the nurse’s perspective. Informal observations are made, or discussions are elicited among peers and neighbors within the community.
Sociocultural Considerations
When analyzing community health needs, it is essential to do so through a sociocultural lens. Just as an individual’s health can be influenced by a wide variety of causes, community health problems are affected by various factors in the community. For example, a high rate of cancer in one community could be related to environmental factors such as pollution from local industry, but in another community, it may be related to the overall aging of the population. Both communities have a high rate of cancer, but the public health response would be very different. Another example related to mental health is related to various situational factors affecting depression. A high rate of depression in one community may be related to socioeconomic factors such as low-paying jobs, lack of support systems, and poor access to basic needs like grocery stores, whereas in another community it may be related to lack of community resources during frequent weather disasters. The public health response would be different for these two communities.
Nurses must also recognize and value cultural differences such as health beliefs, practices, and linguistic needs of diverse populations. They must take steps to identify subpopulations who are vulnerable to health disparities and further investigate the causes and potential interventions for these disparities. For example, mental health disparities pose a significant threat to vulnerable populations in our society, such as high rates of suicide among LGBTQ+ youth, reduced access to prevention services among people living in rural areas, and elevated rates of substance misuse among Native Americans. These disparities threaten the health and wellness of these populations. [9]
Key points to consider when assessing a community using a sociocultural lens include the following:
- Have the trends of assessment data changed over time? What are the potential causes for these changes in this community?
- How does the community’s needs assessment data compare to similar communities at local, county, state, and national levels? What target goals and health initiatives have been successfully implemented in other communities?
- What vulnerable subpopulations are part of this community, and what health disparities are they experiencing? What are potential causes and solutions for these health disparities?
- Input from members of vulnerable subpopulations must be solicited regarding their perspectives on health disparities, as well as barriers they are experiencing in accessing health care.
Similar to how nurses individualize nursing diagnoses for clients based on priority nursing problems identified during a head-to-toe assessment, community health nurses use community health needs assessment data to develop community health diagnoses. These diagnoses are broad, apply to larger groups of individuals, and address the priority health needs of the community. Resources such as Healthy People 2030 can be used to determine current public health priorities.
A community diagnosis is a summary statement resulting from analysis of the data collected from a community health needs assessment. [10] A clear statement of the problem, as well as causes of the problem, should be included. A detailed community diagnosis helps guide community health initiatives that include nursing interventions.
A community diagnosis can address health deficits or services that support health in the community. A community diagnosis may also address a need for increased wellness in the community. Community diagnoses should include these four parts:
- The problem
- The population or vulnerable group
- The effects of the problem on the population/vulnerable group
- The indicators of the problem in this community
Here are some examples of community health diagnoses based on community health needs assessments:
- Community Scenario A
- Assessment data: The local high school has had a 50% increase in the number of teen pregnancies in the past year, causing high school graduation rates to decrease due to pregnant students dropping out of high school.
- Community diagnosis: Increased need for additional birth control and resources for prevention of pregnancy due to lack of current resources, as evidenced by 50% increase in teen pregnancies in the last year and a decrease in graduation rates.
- Community Scenario B
- Assessment data: Fifty percent of residents of an assisted living facility were found to have blood pressure readings higher than 130/80 mmHg during a health fair last week at the facility.
- Community diagnosis: Increased need for education about exercise and diet and referrals to primary care doctors for residents of an assisted living facility due to increased risk for mortality related to high blood pressure, as evidenced by a high number of residents with high blood pressure during a health fair.
- Community Scenario C
- Assessment data: The local high school has had two cases of suicide in the past year.
- Diagnosis: Increased need for community education regarding suicide prevention and crisis hotlines, as evidenced by an increase in adolescent suicide over the past twelve months.
Outcome Identification
Outcomes refer to the changes in communities that nursing interventions and prevention strategies are intended to produce. Outcomes include broad overall goals for the community, as well as specific outcomes referred to as “SMART” outcomes that are specific, measurable, achievable, realistic, and with a timeline established.
Broad goals for communities can be tied to national objectives established by Healthy People 2030, as previously discussed in the “ Community Health Concepts ” section.
Healthy People objectives are classified by these five categories [11] :
- Health Conditions
- Health Behaviors
- Populations
- Settings and Systems
- Social Determinants of Health
SMART outcomes can be created based on the objectives listed under each category. For example, if an overall community goal is related to “Drug and Alcohol Use” under the “Health Behaviors” category, a SMART outcome could be based on the Healthy People objective, “Increase the proportion of people with a substance use disorder who got treatment in the past year.” [12] Based on this Healthy People objective, an example of a SMART outcome could be the following:
- The proportion of people treated for a substance disorder in Smith County will increase to 14% within the next year.
View the Healthy People 2030 Objectives and Community Objectives .

Planning Interventions
Nursing interventions for the community can be planned based on the related Healthy People category and objective. For example, based on the sample SMART outcome previously discussed, a planned nursing intervention could be the following:
- The nurse will provide education and materials regarding evidence-based screening practices for substance use disorder in local clinics.
Community health nursing interventions typically focus on prevention of illness with health promotion interventions. After performing a community health needs assessment, identifying priority problems, and establishing health goals and SMART outcomes, the nurse integrates knowledge of health disorders (e.g., diabetes, cancer, obesity, or mental health disorders) and current health risks in a community to plan prevention interventions.
There are two common public health frameworks used to plan prevention interventions. A traditional preventive framework is based on primary, secondary, or tertiary prevention interventions. A second framework, often referred to as the Continuum of Care Prevention Model, was established by the Institute of Medicine (IOM) and includes universal, selected, and indicated prevention interventions. Both frameworks are further discussed in the following sections. [13]
Primordial, Primary, Secondary, Tertiary, and Quaternary Interventions
Preventive health interventions may include primordial, primary, secondary, tertiary, and quaternary prevention interventions. These strategies attempt to prevent the onset of disease, reduce complications of disease that develops, and promote quality of life. [14]
Primordial Prevention
Primordial prevention consists of risk factor reduction strategies focused on social and environmental conditions that affect vulnerable populations. In other words, primordial prevention interventions target underlying social determinants of health that can cause disease. These measures are typically promoted through laws and national policy. An example of a primordial prevention strategy is improving access to urban neighborhood playgrounds to promote physical activity in children and reduce their risk for developing obesity, diabetes, and cardiovascular disease. [15] See Figure 16.8 [16] for an image of a neighborhood playground.

Primary Prevention
Primary prevention consists of interventions aimed at susceptible populations or individuals to prevent disease from occurring. An example of primary prevention is immunizations. [17] Nursing primary prevention interventions also include public education and promotion of healthy behaviors. [18] See Figure 16.9 [19] for an image of an immunization clinic sponsored by a student nurses’ association.

Secondary Prevention
Secondary prevention emphasizes early detection of disease and targets healthy-appearing individuals with subclinical forms of disease. Subclinical disease refers to pathologic changes with no observable signs or symptoms. Secondary prevention includes screenings such as annual mammograms, routine colonoscopies, Papanicolaou (Pap) smears, as well as screening for depression and substance use disorders. [20] Nurses provide education to community members about the importance of these screenings. See Figure 16.10 [21] for an image of a mammogram.

Tertiary Prevention
Tertiary prevention is implemented for symptomatic clients to reduce the severity of the disease and potential long-term complications. While secondary prevention seeks to prevent the onset of illness, tertiary prevention aims to reduce the effects of the disease after it is diagnosed in an individual. [22] For example, rehabilitation therapy after an individual experiences a cerebrovascular accident (i.e., stroke) is an example of tertiary prevention. See Figure 16.11 [23] for an image of a client receiving rehabilitation after experiencing a stroke.
The goals of tertiary prevention interventions are to reduce disability, promote curative therapy for a disease or injury, and prevent death. Nurses may be involved in providing ongoing home health services in clients’ homes as a component of interprofessional tertiary prevention efforts. Health education to prevent the worsening or recurrence of disease is also provided by nurses.

Quaternary Prevention
Quaternary prevention refers to actions taken to protect individuals from medical interventions that are likely to cause more harm than good and to suggest interventions that are ethically acceptable. Targeted populations are those at risk of overmedicalization. [24] An example of quaternary prevention is encouraging clients with terminal illness who are approaching end of life to seek focus on comfort and quality of life and consider hospice care rather than undergo invasive procedures that will likely have no impact on recovery from disease.
See additional examples of primordial, primary, secondary, tertiary, and quaternary prevention strategies in Table 16.3a.
Table 16.3a Examples of Prevention Interventions [25] , [26]
In the United States, several governing bodies make prevention recommendations. For example, the United States Preventive Services Task Force (USPSTF) makes recommendations for primary and secondary prevention strategies, and the Women’s Preventive Services Initiative (WPSI) makes recommendations specifically for females. The Advisory Committee on Immunizations Practices (ACIP) makes recommendations for vaccinations, and various specialty organizations such as the American College of Obstetrics and Gynecology (ACOG) and the American Cancer Society (ACS) make preventative care recommendations. Preventive services have been proven to be an essential aspect of health care but are consistently underutilized in the United States. [27] Nurses can help advocate for the adoption of evidence-based prevention strategies in their communities and places of employment.
Continuum of Care Prevention Model
A second framework for prevention interventions, referred to as the “Continuum of Care Prevention Model,” was originally proposed by the Institute of Medicine (IOM) in 1994 and has been adopted by the Substance Abuse and Mental Health Services Administration (SAMHSA). [28] See Figure 16.12 [29] for an illustration of the Continuum of Care Prevention Model.
![]”This image is derivative of the “IOM “protractor” by unknown author and is included on the basis of Fair Use. Access for free at http://www.ca-sdfsc.org/docs/resources/SDFSC_IOM_Policy.pdf Image showing a Continuum of Care Prevention Model](https://med.libretexts.org/@api/deki/files/39124/coc-protractor.png?revision=1)
The Continuum of Care Prevention Model can be used to illustrate a continuum of mental health services for community members that includes prevention, treatment, and maintenance care:
- Universal prevention: Interventions designed to reach entire groups, such as those in schools, workplaces, or entire communities. [30] , [31] For example, wellness sessions regarding substance misuse can be planned and implemented at a local high school.
- Selected prevention: Interventions that target individuals or groups with greater risk factors (and perhaps fewer protective factors) than the broader population. [32] , [33] For example, a research study showed that wellness programs implemented for adolescents who were already using alcohol or drugs reduced the quantity and frequency of their alcohol use and reduced episodes of binge drinking. [34]
- Indicated prevention: Interventions that target individuals who have a high probability of developing disease. [35] For example, interventions may be planned for adolescents who show early signs of substance misuse but have not yet been diagnosed with a substance use disorder. Interventions may include referrals to community support services for adolescents who have violated school alcohol or drug policies. [36]
- Treatment refers to identification of a mental health disorder and standard treatment for the known disorder. Treatment also includes interventions to reduce the likelihood of future co-occurring disorders. [37]
- Maintenance refers to long-term treatment to reduce relapse and recurrence, as well as provision of after-care services such as rehabilitation. [38]
See additional examples of prevention strategies using the Continuum of Care Prevention Model in Table 16.3b.
Table 16.3b Examples of Continuum of Care Prevention Strategies
Read A Guide to SAMHSA’s Strategic Prevention Framework PDF for more about planning prevention strategies for substance misuse and related mental health problems.
Culturally Competent Interventions
To overcome systemic barriers that can contribute to health disparities, nurses must recognize and value cultural differences of diverse populations and develop prevention programs and interventions in ways that ensure members of these populations benefit from their efforts. [39]
SAMHSA identified the following cultural competence principles for planning prevention interventions [40] :
- Include the targeted population in needs assessments and prevention planning
- Use a population-based definition of community (i.e., let the community define itself)
- Stress the importance of relevant, culturally appropriate prevention approaches
- Promote cultural competence among program staff
Review additional concepts related to culturally responsive care in the “ Diverse Patients ” chapter of Open RN Nursing Fundamentals .
Evidence-Based Practice
It is essential to incorporate evidence-based practice when planning community health interventions. SAMHSA provides an evidence-based practice resource center for preventive practices related to mental health and substance abuse. See these resources, as well as examples of evidence-based programs and practices in the following box.
Examples of Evidence Based Prevention Practices related to Mental Health and Substance Misuse [41]
- Blueprints for Healthy Youth Development : Youth violence, delinquency, and drug prevention and intervention programs that meet a strict scientific standard of program effectiveness
- Evidence-Based Behavioral Practice (EBBP) : A project that creates training resources to help bridge the gap between behavioral health research and practice
- SAMHSA’s Suicide Prevention Research Center (SPRC) : A best practices registry that identifies, reviews, and disseminates information about best practices that address specific objectives of the National Strategy for Suicide Prevention
- The Athena Forum: Prevention 101 : Substance misuse prevention programs and strategies with evidence of success from the Washington State Department of Social and Health Services
- National Institute on Drug Abuse: Preventing Drug Use Among Children and Adolescents : Research-based drug abuse prevention principles and an overview of program planning, including universal, selected, and indicated interventions
View the SAMHSA Evidence-Based Practice Resource Center .
Implementation
Community health nurses collaborate with individuals, community organizations, health facilities, and local governments for successful implementation of community health initiatives. Depending on the established community health needs, goals, outcomes, and target group, the implementation of nursing interventions can be categorized as clinical, behavioral, or environmental prevention:
- Clinical prevention: Interventions are delivered one-on-one to individuals in a direct care setting. Examples of clinical prevention interventions include vaccine clinics, blood pressure monitoring, and screening for disease.
- Behavioral prevention: Interventions are implemented to encourage individuals to change habits or behaviors by using health promotion strategies. Examples of behavioral prevention interventions include community exercise programs, smoking cessation campaigns, or promotion of responsible alcohol drinking by adults.
- Environmental prevention: Interventions are implemented for the entire community when laws, policies, physical environments, or community structures influence a community’s health. Examples of environmental prevention strategies include improving clean water systems, establishing no-smoking ordinances, or developing community parks and green spaces.
When evaluating the effectiveness of community health initiatives, nurses refer to the established goals and SMART outcomes to determine if they were met by the timeline indicated. In general, the following questions are asked during the evaluation stage:
- Did the health of the community improve through the interventions put into place?
- Are additional adaptations or changes to the interventions needed to improve outcomes in the community?
- What additional changes are needed to improve the health of the community?
- Have additional priority problems been identified?
- “ Nursing Process in Community Health Nursing ” by Open RN project is licensed under CC BY 4.0 ↵
- Community Tool Box by Center for Community Health and Development at the University of Kansas is licensed under CC BY NC SA 3.0 ↵
- A Guide to SAMHSA’s Strategic Prevention Framework by Substance Abuse and Mental Health Services Administration is available in the Public Domain . ↵
- Medrea, R. (2014, July 20). Windshield survey nursing [Video]. YouTube. All rights reserved. https://youtu.be/aAzW1bW_Dbw ↵
- McDonald, L. (2006). Florence Nightingale and public health policy: Theory, activism and public administration. University of Guelph. https://cwfn.uoguelph.ca/nursing-health-care/fn-and-public-health-policy/ ↵
- Office of Disease Prevention and Health Promotion. Healthy People 2030: Building a healthier future for all. U.S. Department of Health and Human Services. https://health.gov/healthypeople ↵
- Savage, C. L. (2020). Public/community health and nursing practice: Caring for populations (2nd ed.). FA Davis. ↵
- This work is a derivative of StatPearls by Kisling and Das and is licensed under CC BY 4.0 ↵
- “ Playground_at_Hudson_Springs_Park.jpg ” by Kevin Payravi is licensed under CC BY-SA 3.0 ↵
- “ 10442934136_1f910af332_b ” by Lower Columbia College (LCC) is licensed under CC BY_NC-ND 2.0 ↵
- “ US_Navy_021025-N-6498N-001_Mammogram_technician,_aids_a_patient_in_completing_her_annual_mammogram_evaluation.jpg ” by U.S. Navy photo by Ensign Ann-Marie Al Noad is in the Public Domain . ↵
- “ tech_zerog.jpg ” by unknown author at Gaylord.org is included on the basis of Fair Use ↵
- National Research Council (US); Institute of Medicine (US) Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults; and Research Advances and Promising Interventions. Defining the scope of prevention. (2009). In M. E. O’Connell & Warner B. T. (Eds). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. In Research advances and promising interventions. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK32789/ ↵
- This image is a derivative of the “IOM protractor” by unknown author and is included on the basis of Fair Use. Access for free at http://www.ca-sdfsc.org/docs/resources/SDFSC_IOM_Policy.pdf ↵
- A Guide to SAMHSA’s Strategic Prevention Framework by Substance Abuse and Mental Health Services Administration is available in the Public Domain. ↵
- Werch, C., Moore, M. J., DiClemente, C. C., Bledsoe, R., & Jobli, E. (2005). A multihealth behavior intervention integrating physical activity and substance use prevention for adolescents. Prevention Science, 6 (213). https://doi.org/10.1007/s11121-005-0012-3 ↵
- Substance Abuse and Mental Health Services Administration. (2019, July 19). Finding evidence-based programs and practices. https://www.samhsa.gov/sites/default/files/20190719-samhsa-finding_evidence-based-programs-practices.pdf ↵

Assignment: Community Health Nurse
Assignment: Community Health Nurse ORDER NOW FOR AN ORIGINAL PAPER ASSIGNMENT: Assignment: Community Health Nurse Assignment: Community Health Nurse Culture and the values learned within a cultural group are critical to how people perceive health, health care, and nursing care providers (Maurer, Smith, 2013). A community health nurse be educated in the cultural values, beliefs, views and their accepted way of life in order to provide care in a manner that the patient population will accept and understand. Whether community/public health nurses focus on an individual, group, or community as the unit of care, these concepts must be understood to provide the best possible nursing care (Maurer, Smith, 2013) The deliberate act of keeping cultural heritage from the present for the future is known as preservation (Maurer, Smith, 2013) . These are practices that have been past down through multiple generations and provide a sense of pride to that culture. The Chinese culture of acupuncture to relive pain is a cultural preservation practice (americannursetoday.com, 2017). This has been shown to proven to control pain and can be used as part of the care plan for pain control. They risk infections, organ damage and bleeding if not preformed correctly(mayoclinic.org , 2017). The nurse may not believe in the practice and try to encourage medication only. Assignment: Community Health Nurse Assignment: Community Health Nurse Cultural accommodation is respecting a practice of a culture that has not been proven to work but does not cause harm to the patient (Maurer, Smith, 2013) . The Mexican culture places a metal object on the navel of a sick newborn because it is believed assist in healing (americannursetoday.com, 2017). . This has no evidenced based research proving any type of healing nor places the new born in danger. The nurse will incorporate this practice in the care plan of the new born showing respect for the cultural practice. May prevent the parents from seeking medical interventions in a timely manner resulting in a very ill newborn when seeking care. The care giver may not fully understand this practice and perceived the parents as neglectful and possible case for protective services. Cultural repatterning is changing a practice that may interact in medical treatment (Maurer, Smith, 2013) . The African American Culture believes in prayers and folk medicines for healing. This may prevent the patient from compliance with their treatment plan that has a proven positive outcome. A cancer diagnosis brings increased prayers, home made medicine that has been past down from previous generations and refusal of medical treatment. My culture believes that air causes cancer to spread and will refuse recommended proven medical intervention. Having little to no understand, faith or trust medical practice because Jesus heals the sick. No matter how much information is given or who presents it the cultural practice of prayer over rules all. Culture brokering gives professionals the tools to assess cultural factors so they can work more productively with clients from diverse backgrounds (Jezewski, 1990) . If a patient does not speak or understand English a culture broker will translate the information between the care giver and patient. . As the medical professional explains a cardiac cauterization to a patient, the broker can use a brochure with pictures of the procedure as a visual tool. Translating each step in correlation with the doctor, pictures, terms the patient understands being mindful of cultural implication of medical care by strangers. The patient may not have trust in the broker if no prior relationship existed and refuse treatment. I NEED YOU TO COMMENT FROM THIS POST, NO MORE THAN 150 WORDS NEEDED AND A REFERENCE PLEASE. You must proofread your paper. But do not strictly rely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort on your part and you can expect your grade to suffer accordingly. Papers with numerous misspelled words and grammatical mistakes will be penalized. Read over your paper – in silence and then aloud – before handing it in and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes. Use a standard 10 to 12 point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages. Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor. The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting hard copy, be sure to use white paper and print out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument. Get a 10 % discount on an order above $ 50 :
Is this the question you were looking for? If so, place your order here to get started!

Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts
Nurs – 6630n psychopharmacologic approaches to treatment of psychopathology.
NURS – 6630N Psychopharmacologic Approaches to Treatment of Psychopathology NURS – 6630N Psychopharmacologic Approaches to Treatment of Psychopathology Walden – NURS 6630 – Psychopharmacologic Approaches To Treatment Of Psychopathology Essay Assignment At times, psychotherapy is not enough to alleviate...
New Technologies in Nursing
New Technologies in Nursing New Technologies in Nursing Introduction The current nursing technologies have transformed how nurses conduct their duties. Evidently, such technologies and new healthcare systems have endured establishing better services to patients. According to the reports of...
Blog , Nursing Blog
Experience of Disorder Symptoms Nursing Research Paper
Experience of Disorder Symptoms Nursing Research Paper Experience of Disorder Symptoms The study was approved by an Institutional Review Board as it is a requirement of the journal where it was published. Notably, the article is peer-reviewed. Though it...
- Open access
- Published: 11 April 2024
Impact of training on knowledge, confidence and attitude amongst community health volunteers in the provision of community-based palliative care in rural Kenya
- Hussein Elias 1 , 2 ,
- Evelyne Kisembe 2 ,
- Sarah Nyariki 2 ,
- Ivan Kiplimo 2 ,
- James Amisi 1 , 2 ,
- Juli Boit 3 ,
- Allison Tarus 3 ,
- Naseem Mohamed 4 &
- Kenneth Cornetta 1 , 2 , 5
BMC Palliative Care volume 23 , Article number: 97 ( 2024 ) Cite this article
Metrics details
Existing literature suggests multiple potential roles for community health volunteers (CHVs) in the provision of palliative care (PC) in low- and middle-income countries. In Kenya the role of CHV in the provision of PC has not been reported. The objective of this study was to assess knowledge, confidence, attitude, and clinical practice of community health volunteers after attending a novel palliative care (PC) training program.
A total of 105 CHVs participated in a 3-day in person training followed by a 1-month in person and telephone observation period of the palliative care activities in the community. Structured questionnaires were used pre- and post-training to assess knowledge acquisition, impact on practice, and content delivery. A mixed method study design was conducted 12-month post training to assess impact on clinical practice.
Immediately after training, CHV provided positive ratings on relevance and content delivery. In the month following training, CHVs evaluated 1,443 patients, referred 154, and conducted 110 and 129 tele consults with the patients and PC providers respectively. The follow up survey at 12 months revealed improved knowledge and confidence in various domains of palliative care including symptom and spiritual assessment and provision of basic nursing and bereavement care. Focus group discussions revealed the CHVs ability to interpret symptoms, make referrals, improved communication/ interpersonal relationships, spiritual intervention, patient comfort measures and health care practices as newly learned and practiced skills.
Conclusions
We noted improved knowledge, new skills and change in practice after CHVs participation in a novel training curriculum. CHVs can make important contributions to the PC work force and be first line PC providers in the community as part of larger hub and spoke care model.
Peer Review reports
In 2014, the World Health Assembly WHA 67.19 called upon the World Health Organization (WHO) and Member States to improve access to palliative care (PC), with an emphasis on primary healthcare and community/home-based care [ 1 ]. Approximately 800,000 people in Kenya are in need of PC while only 14,552 accessing the service [ 2 ]. Similar to other countries in Africa, the need of PC in Kenya is escalating with the increasing burden of noncommunicable diseases and the ageing of the population [ 3 , 4 , 5 ].
In Kenya most patients are diagnosed in advanced stages of disease and many who present early cannot afford or lack access to curative treatments [ 5 , 6 ]. Also, an increase in life expectancy and decrease in communicable diseases have led to an increase in chronic disease, such as heart failure and chronic obstructive pulmonary disease putting additional strain on the limited available PC resources [ 6 ].
In Kenya, Community Health Volunteers (CHV) receive limited training (324 contact hours and 160 h of practical experience), and are then assigned to provide services to a community unit by the local Ministry of Health (MOH) [ 7 ]. On average, 10 CHVs are assigned to a community unit of approximately 1,000 households (5,000 people) within a defined geographical area [ 7 , 8 , 9 ]Since the 1980s, CHVs have played a major role in the delivery of community-based healthcare in rural areas with activities focused on (a) home visits to determine health situations, deliver key messages and undertake necessary actions, (b) health improvement and prevention, (c) treatment of common diseases and minor injuries, (d) protocol implementation for maternal and newborn health efforts, and (e) case management of childhood illnesses [ 7 , 8 , 9 ].
Existing literature indicates multiple potential roles for Community Health Volunteers (CHVs) in the provision of PC in low- and middle-income countries (LMIC) [ 10 ]. The scope of practice can vary in different LMIC’s, some of which have shown the potential of CHVs to raising awareness and identifying patients in need of PC, assist in pain management, and provide home-based care including psychological and spiritual support [ 10 , 11 ]. In Kenya, the role of CHV in the provision of PC has not been reported. One of the emerging themes in a recently published qualitative study on Kenyan palliative care providers and leaders perception of palliative care research needs and support to facilitate rigorous research was to evaluate the role of CHVs in the provision of PC [ 12 ].
There is paucity of local data regarding CHVs and palliative care. This project aimed to train CHVs in community based palliative care and equip them with tools to assist them to identify, assess, support and refer community members in need of palliative care. Hence, the broad objective of this study was to assess knowledge, confidence, attitude and clinical practice after attendance at the training program.
We developed a curriculum focused on key PC skills and included connections to PC providers within the county of residence. The training involved two components, a 3-day classroom training including practicum and a one-month observation in the community. Because of their limited medical background, CHV were linked to palliative care providers for teleconsultation and facilitate referrals to palliative care clinics. Providers included a primary care physician and clinical officers (equivalent to physician assistant who have prescription authority). Providers have more than 3 years of working experience in a palliative and hospice care unit.
CHV Selection
The training was developed in collaboration with county health officials from Uasin Gishu and Bungoma counties, Kenya. As the course was delivered prior to widespread COVID19 vaccinations, the officials requested the inclusion of COVID19 education in the curriculum and required training session be limited to < 12 CHV. The county officials selected 2 CHV from a community unit within their jurisdiction. CHVs were invited from 43 community units.
Training Implementation
The curriculum was developed by PC providers at Moi University School of Medicine and Academic Model Providing Access To Healthcare (AMPATH www.ampathkenya.org ), Eldoret Kenya and aimed to teach PC skills appropriate for the CHV scope of practice. The Knowledge Based Curriculum Components are listed in Table 1 . Training included a three-day in person combination of didactic and practicum learning followed by a one-month observation period. The training was delivered by experienced clinical officers and nurses working in PC facilities within the county. The training was supervised by a primary care physician. The in-person training was hosted at the hospitals where the trainers work. The skill-based components were delivered using role play. For the observation period, CHVs were provided with a training manual, patient assessment forms, telephone contacts of the trainers and 400 Kenya Shillings (kshs) (approximately $4 US) airtime for the month. Participants were linked to a PC provider within their region who during the observation period met with them weekly in the community to review symptom assessment forms and document activities. In addition, the PC providers visited the households with the CHVs and observed the CHV encounters with the community members. The observation was also done remotely in between the weekly visits using a telephone. The CHVs were called by the trainers and asked about the encounters with the community members and use of the tools. The PC providers were also provided with 800 kshs airtime for the month. A total of 10 training sessions were conducted between August 5th, 2020 and April 6th 2021, with 105 CHVs completing the 3-day training.
Curriculum Assessment
Efforts to document the impact of training were conducted at two timepoint. An initial assessment was performed at the time of training. Pre- and post-questionnaires assessed trainees on confidence, relevance, and content delivery. Approximately one year after training, all trained CHV were invited to participate in a mixed method designed study to assess knowledge retention, impact on practice, and challenges to PC delivery. Participation was voluntary, 79 out of 105 trained CHVs chose to participate in the survey and FGDs. The survey was carried out at the sites where the original training was conducted. The focus group discussions were conducted in groups of ≤ 12 participants. A total of 10 FGDs were held. The participants in a training cohort were selected from the participants in the original training cohort. All the participants who accepted and signed the informed consent were asked to complete a self-administered survey and participate in a focus group discussion (FGD). Data collection was designed using Kirkpatrick taxonomy [ 13 ] (Table 2 ). Level 1 Reaction: participants reaction to the training was assessed using the anonymized information from post-training evaluation taken at the time of initial training. Level 2 Learning: acquired knowledge was assessed 12 months after the using Likert type questions derived from the Knowledge Based Curriculum Components. Participants were also asked to rate their confidence level on performing clinical skills. Level 3 Behavior: 12 months post-training a structured questionnaire and FGD assessed how training changed CHV practice. Level 4 Results: at 12 months a questionnaire and FGD evaluated (a) CHVs confidence in their ability to identify patients in need of PC, (b) ability to refer palliative patients, (c) cope with the very sick patients and (d) provide home-based care and (e) train other CHVs. The CHVs were also questioned regarding their use of the training manual and the assessment forms. The number of consultation requests from the community where the trained CHVs practiced was also assessed. The questionnaires used were developed for this study (see supplementary file 1 ).
Data from the survey was extracted into Redcap for compiling and reviewing. All the data was anonymized, and stored in a password protected server. The FGD interviews were held in English and audio-recorded. The data was transcribed using NVivo software for coding into meaning oriented interpretations. In instances where the participants chose to speak in Swahili, the data analyst translated the wording into English. Statistical analysis of pre- and post- questionnaires was performed using two-tail paired t-test.
The data was maintained under Institutional Research and Ethics Committee (IREC) guidelines to respect confidentiality as data moved through the stages of capture, storage, entry, cleaning, coding, analysis. (A) Data was stored in files using a naming convention to maintain confidentiality of the participants by delinking identifiers. The naming conventions identifies file content without opening the file. The naming conventions carried four components: study phase, participant group, participant ID, file type; (B) Data and recording files were saved in a password protected computer and stored in a locked cabinet when not in use by study personnel.
The study was approved by the Moi University IREC (IREC 2021/203) and was determined to be exempt by Indiana University Institutional Review Board. The survey was conducted in accordance with the relevant guidelines and regulations and an informed consent was obtained from all the participants.
The demographics of the participants are provided in Table 3 . The majority of participants were female (66%), 34 to 54 years of age, (70%), and worked as CHVs for more than 5 years (76%). As CHV is a volunteered position, two-thirds indicated they were employed. In the month-long observation period immediately after the training, CHV evaluated 1,443 individuals. Of these, 154 were referred and received at the PC clinic and an additional 58 home visits were conducted jointly by the CHV and a PC provider. Telephone conversations were also conducted with CHVs making 110 calls to a patient and 129 calls to a PC provider. One year follow-up assessment was conducted between March 2022 and May 2022, with 79 CHVs returning to participate in a face-to-face knowledge assessment and FGD.
The impact assessment was divided into 4 Levels which were assessed at the time of training and at the one-year follow-up.
Level 1 Reaction
This was assessed at the time of initial training (see Fig. 1 ). Most of the 105 participants agreed or strongly agreed that the training was relevant (90.8%), will be useful to them in their work (99%), and the training materials were helpful (98%). Approximately two third (70%) of the participants agreed or strongly agreed that the duration of the training was sufficient.
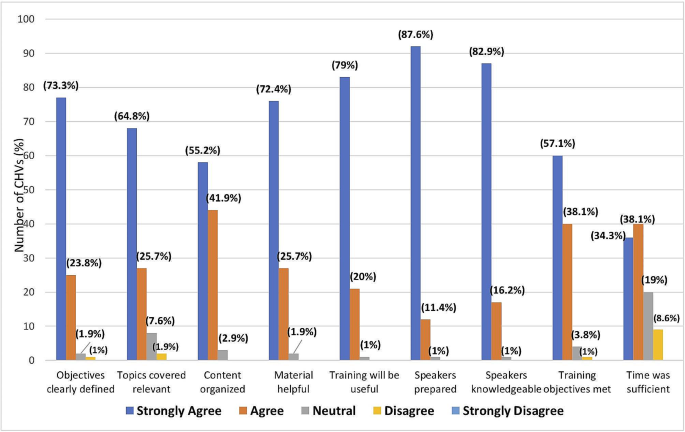
Training evaluation. Abbreviations CHVs - Community health volunteers
Level 2 Learning
Table 4 shows the levels of self-assessed knowledge on various domains of PC including physical symptom assessment, spiritual issue assessment, provision of basic nursing care, and bereavement care. There was an overall statistically significant improvement in all the domains when comparing pre- and post-training values.
Table 5 shows self-assessed confidence levels on pain assessment, change of urine bag, prevention and care of bedsores, turning a patient in bed, feeding procedures, patient referral, spiritual assessment, communication skills, ethical principles pre–and post–training. Statistically significant Improved confidence was reported in all domains except for patient referral.
Level 3 behavior
The average number of assessments performed during the month after training varied with a third of CHVs assessed ≤ 10, approximately half assessed between 11 and 20, and the remaining assessing over 20 community members. Figure 2 shows the average number of selected activities performed first month after training. During this period, approximately 6 or more patients were referred to PC clinics, linked to other organizations and tele–consulted with CHV by approximately 50%, 40% and 76% of the CHVs respectively. In addition, approximately more than two third CHV tele consulted with PCU 6 or more times and more than half invited a PC provider to accompany them on a home visit.
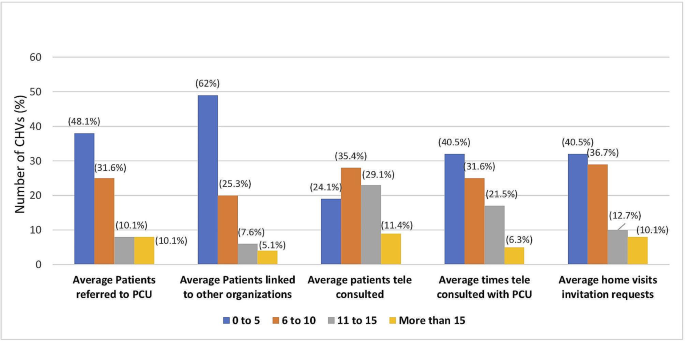
Some of the activities performed by CHVs during the first 4 weeks after the training. Abbreviations PCU – palliative care unit, CHVs – community health volunteers
Level 4 Results: During the training a copy of the training manual was given to all the CHVs. Two thirds of the CHV’s were using the training manual either most or all the time during their community visits. Approximately 90% of the participants reported that they saw the relevance of the training most or all the time during their community visits. Approximately 90% CHVs reported that they used the assessment tool while assessing community members most or all the time and 99% felt the assessment tool was helpful to assess the condition of the community member. When asked about the ease of use of the assessment tool, only 6% found it difficult to use.
All of the CHVs reported an increase in the number of consultations from the community and 94% reporting that they facilitated community education on PC. Part of the training program was to enable participants to train other CHVs in their community units. 97% felt they could utilize the training manual to train others and 97% reporting they trained other CHVs and 94% trained members of their community.
In addition to the quantitative assessments, 79 CHV returned one year after the initial training to participate in a semi-structured interview in which six questions were used to obtain feedback. The major themes that arouse from the FGD are listed in Table 6 and details are available in Table 1 , supplemental data. Attentive listening and counseling were improved and led to open discussion of illness, confidence in addressing misinformation, better symptom assessment and medication adherence interventions. The training also improved caregiver interactions and spiritual care. The CHV felt empowered to make referrals to PC providers, encourage patients to use technology in their care, and educate family on basic care issues for ill patients. The communication skills were noted to improve interpersonal relationship with patients and family and helped the CHV deal with the stress of caring for patients at the end of life.
The WHO and other organizations have encouraged CHV involvement in palliative care delivery. In 2020, MacRae et al. addressed this issue in LMIC and found only 13 studies appropriate for their review [ 10 ]. For a more recent evaluation, we performed an OVID search ( https://www.wolterskluwer.com/en/solutions/ovid ) on February 14, 2024 using the keywords Community Health Workers (CHW), CHV, and Palliative Care and found 27 references. Searching CHW, CHV and Hospice did not add any additional references. The majority of publications were from high income countries where CHV expressed a positive attitude towards end-of-life care and including CHV in PC delivery may decrease medical costs [ 14 , 15 ]. CHV were successful in to promoting advance care planning, utilization of hospice and palliative medicine, particularly in underserved populations [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ]. Culturally based care was also an important factor in improving PC outcomes [ 25 ]. Most of the CHV in high income countries were supplementing an existing palliative care workforce. In contrast, CHV may be the only resource available for home-based care in LMIC and there are few publications addressing their role in palliative care delivery. Over a decade ago, Uganda developed national policies that included adding palliative care to the scope of CHV activities and other countries have followed suit [ 26 ] (2). A national PC policy in South Africa promotes CHV involvement but a report in 2022 recommended a needs assessment [ 27 ]. The study also noted CHV expressed uncertainty regarding their role in home-based palliative care. In general, publications recognize that adding PC to CHV practice represents a change from their current focus on preventative and general primary care needs. While publications have highlighted the need for research studies [ 10 , 12 , 27 ], our report is one of the few addressing CHV PC training and implementation in the LMIC setting.
The training curriculum described here was designed to cover the three main domains of PC which include physical symptom assessment and treatment, spiritual and social care and grief and bereavement care. Special emphasis was placed on the communication skills used in discussing difficult topics. The manuscript present pre- and post-assessments of training. CHV found the training of value, increased referrals to PC providers, and empowered the CHVs to alter their practice by providing a variety of PC services.
CHVs live within the community they serve and have been selected by the members of the same community, speak the same language and are from the same cultural background which is an added advantage in performing their roles [ 8 ]. In Kenya, their key roles and responsibilities include making home visits to assess health situations, share health improvement and prevention information from the MOH, treat common minor illnesses and injuries, and address maternal, newborn health and childhood health issues [ 8 , 9 ]. The study found that with additional training and linkage to palliative care providers, CHVs can identify the PC needs of their community and appropriately act within their scope of practice. This includes a role in providing psychosocial and spiritual support as well as newly learned clinical care skill.
Following the training the CHVs used the training manuals and assessment forms provided to them during their community visits. We believe that these documents provided a stepwise guide to community member assessment and intervention and positively impacted the knowledge and confidence to initiate telephone consultations with PC mentors.
CHVs reported that through the training they have learnt new skills and the importance of biopsychosocial nature of chronic illnesses which they incorporated into their practice. They also appropriately identified patients for referral. At one year follow up, the CHVs also reported an increase in the number of PC consults they received from community members. In the FGD, several CHVs commented that by applying their new skills the respect shown to them by the community improved. The CHVs recognized the benefit of tapping into the existing community resources to help the sick community members. The CHVs trained caregivers who were then able to care for their sick family member and others in the community. This is consistent with the study by Soderhamn et al. showing a network of volunteers (beyond CHVs) can address patient needs and mobilized resources in the community [ 14 ].
This survey has shown a statistically significant overall improvement in knowledge and confidence in conducting basic nursing procedures like cleaning and dressing of wounds, stoma care, change of urine bag and feeding procedures except for patient referral. We believe that this can reduce unnecessary hospital visits especially for bedbound patients and reduce transport and procedure costs, but the clinical and financial impact will require further study. Greater access to home PC has the potential to allow patients with no access to home hospice to remain at home as they near end-of-life. A population-based study done in Kenya reported that approximately 50% favored dying at home [ 15 ]. Interestingly, 23.7% stated dying at home was the least preferred place, which some credited to the low availability of resources. This suggests an unmet care needs that CHVs could fulfill [ 15 ].
There were a number of limitations to our study. CHVs are familiar with patient referral as this is part of their monthly reporting requirements. They rated this skill the highest in terms of pre training confidence. This could explain the reason patient referral was not statistically significant and suggests this part of the training curriculum could be revised in future trainings. CHVs embraced teleconsultation which was facilitated by the robust telecommunication infrastructure in Kenya where the number of subscribers per capita is higher than most countries, including the United States ( https://data.worldbank.org/indicator/IT.CEL.SETS.P2 ). The provision of PC by CHV may be less effective in countries will limited telecommunication coverage. Our training also empowered CHVs to train other CHVs but the impact of the peer training on patient care is unknown. CHV also were within counties that had an active palliative care clinic that was part of a larger hub and spoke model of PC support, areas where access to PC providers is limited may decrease the effectiveness of training. The availability of a 24-hour PC hotline and the small amount of financial support for phone fees are also components that could impact replication of our findings. We also had cooperation from the MOH in allowing CHV to participate in the training, which was likely influence by the Kenya Palliative Care Policy 2021–2030 which sets goals for increasing access to PC. Sustainability will require continued support by the MOH in allowing CHVs to incorporate PC into their other duties. Adding palliative care services to the CHV skill set may cause a negative impact on performing existing responsibilities as an unintended consequence. While this was not directly assessed in questionnaires, CHVs did not mention this as a limitation during semi-structured interviews.
Conclusion and recommendations
PC specific training which includes practicum, provision of support material and mentorship is relevant and it improves skills, knowledge, and confidence amongst CHVs which changes their practice and behavior. This change has been reported by the CHVs to benefit the community. The components of this training can prepare CHVs on PC task shifting in the community. In addition, the training led to increase referrals to palliative care providers. Our study suggests CHVs can play an important role in a hub and spoke model of PC provision in resource limited settings. Further studies are warranted to assess the impact of the CHV activities from the community perspective, reduction in unnecessary hospital visits, reduced costs and also to review the role of CHVs in performing specific activities like increasing access to morphine for pain management.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
World Health Organization. Palliative care. [Online]. 2020 [cited 2022 October 8. Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care .
Ministry of Health. Kenya community health policy 2020–2030: Ministry of Health.
Kirton BA, Birakurateki J, Merriman J. A. A bridge to the hospice: the impact of Community Health Volunteer Programme in Uganda. SAGE Journals. 2011 March; 25(7).
Powell RA, Ali Z, Luyirika E, Harding R, Radbruch L, Mwangi-Powell FN. Out of the shadows: non-comunicable diseases and palliative care in Africa. BMJ Support Palliat Care. 2017; 7(2).
Zubairi H, Tulshian P, Villegas S, Nelson BD, Ouma K, Burke TF. Assessment of palliative care services in western Kenya. Annals Palliat Med. 2017 April; 6(2).
Ali Z. Kenya Hospices and Palliative Care Association: integrating palliative care in public hospitals in Kenya. Ecancermedicalscience. 2016; 10.
Ministry of Health. Community Health Volunteers (CHVs) Basic Modules Handbook; 2013.
Njiraini R, Hussein S. Kenya’s community health volunteer program. [Online].; 2020 [cited 2022 November 8. Available from: https://chwcentral.org/kenyas-community-health-volunteer-program/ .
MacRae MC, Fazal O, O’Donovan J. Community health workers in palliative care provision in low-income and middle-income countries: a systematic scoping review of the literature. BMJ Global Health. 2020 April; 5.
Nesbit K, Gombwa S, Ngalande A. Rehabilitation training for home-based palliative care community health workers: a pilot study. Progress Palliat Care. 2015; 23(5).
Cartmell KB, Doherty EA, Gikaara N, Ali Z, Qanungo S, Melikam ES et al. Kenyan palliative care providers’ and leaders’ perceptions of palliative care research needs and support to facilitate rigorous research. Res Square. 2022 October.
Smidt A, Balandin S, Sigafoos J, Reed VA. The kirkpatrick model: a useful tool for evaluating training outcomes. J Intellect Dev Disabil. 2009; 34(3).
Patel MI, Ramirez D, Agajanian R, Agajanian H, Bhattacharya J, Bundorf KM. Lay Health Worker-Led Cancer Symptom Screening intervention and the Effect on patient-reported satisfaction, Health Status, Health Care Use and total costs: results from a Tri-part collaboration. JCO Oncol Pract. 2020; 16.
Lee KT, Zale AD, Ibe CA, Johnston FM. Patient Navigator and Community Health Worker attitudes towards End-of-life-care. J Palliat Med. 2021; 24.
Siddiqi A, Monton O, Woods A, Masroor T, Fuller S, Owczarzak J et al. Dissemination and implementation of a Community Health Worker Intervention for Disparities in Palliative Care (DeCIDE PC): a study protocol for hybrid type 1 randomized controlled trial. BMC Palliat Care. 2023; 22.
Patel MI, Murilo A, Agarwal M, Coker T. Health Care professionals persectives on implementation, Adoption and Maintenance of a Community Health Worker-Led Advance Care Planning and Cancer Symptom Screening intervention: a qualiative study. JCO Oncol Pract. 2023; 19.
Patel MI, Kapphahn K, Dewland M, Aguilar V, Sanchez B, Sisay E et al. Effect of a Community Health Worker intervention on Acute Care Use, Advance Care Planning and patient-reported outcomes among adults with Advanced stages of Cancer: a Randomized Clinical Trial. JAMA Oncol. 2022; 8.
Goebel JR, Bird MN, Martinez IL. Empowering the latino community realted to Palliative Care and Chronic Disease Manageemnt through Promotores De Salud (Vommunity Health Workers). J Palliat Med. 2021; 24.
Sedhom R, Nudotor R, Freund KM, Smith TJ, Cooper LA, Owczarzak JT et al. Can Community Health workers Icrease Palliative Care Use for African American patients? A pilot study. JCO ONcol Pract. 2021; 17.
Kubi B, Enumah ZO, Lee KT, Feund KM, Smith TJ, Cooper LA et al. Theory-Basd Development of an Implementation Intervention Using Community Health Workers to increase Palliative Care Use. J Pain Symptom Manage. 2020; 60.
Johnston FM, Neiman JH, Parmley LE, Conca-Cheng A, Freund KM, Concannon TW et al. Stakeholder perspectives on the Use of Community Health Workers to improve Palliative Care use by African americans with Cancer. J Palliat Med. 2019; 22.
Britt HR, Jaka MM, Fernstom KM, Bingham PE, Betzner AE, Taghon JR et al. Quasi-experimental evaluation of LIfecourse on utilization and Palient and caregiver quality of LIfe and experience. Am J Hosp Palliat Care. 2019; 36.
Poulos RG, Harkin D, Poulos CJ, Cole A, Macleod R. Can specially trained community care workers effectively support patients and their families in the home setting at the end of life? Health Soc Care Community. 2018; 26.
Fischer SM, Cervantes L, Fink RM, Kutner JS. Apoyo con Carino: a pilot randomized controlled trial of a patient navigator intervention to improve palliative care outcomes for latinos with serious illness. J Pain Symptom Manage. 2015; 49.
Nabudere H, Asiimwe D, Amandua J. Improving access to skilled attendance at delivery: a policy brief for Uganda. Int J Technol Assess Health Care. 2013; 29.
Van Heerden EM, Jenkins LS. The role of community health workers in palliative care in a rural subdistrict in South Africa. Afr J Prim Health Care Fam Med. 2022; 14.
Soderhamn U, Fkateland S, Fensli M, Skaar R. To be trained and supported volunteer in palliatie care - a phenomenological study. BMC Palliat Care. 2017; 16(18).
Downing J, Gomes B, Gikaara N, Munene G, Daveson BA, Powell RA et al. Public preferences and priorities for end-of-life care in Kenya: a population-based street survey. BMC Palliative Care. 2014 February; 4.
Rouse D. Employing kirkpatrick’s evaluation framework to determine the effectiveness of health information management courses and programs. Perspect Health Inf Manag. 2011 April; 8.
Download references
Acknowledgements
We would like to acknowledge the financial support from Pfizer foundation, the CHVs who participated in the training, Webuye county referral hospital for and living room international for providing conference facilities for face-to-face training.
Funding for this analysis was supported by a grant from the Pfizer Foundation (Principal Investigator K.C.). Additional support was provided for partial salary support by the Indiana University Foundation (H.E.) and a Fulbright Scholar award (K.C.). The funding body played no role in the design of the study and collection, analysis, interpretation of data, and in writing the manuscript.
Author information
Authors and affiliations.
Department of Family Medicine, College of Health Sciences, Moi University, Eldoret, Kenya
Hussein Elias, James Amisi & Kenneth Cornetta
Academic Model Providing Access to Healthcare (AMPATH), Eldoret, Kenya
Hussein Elias, Evelyne Kisembe, Sarah Nyariki, Ivan Kiplimo, James Amisi & Kenneth Cornetta
Living Room International Hospital, Eldoret, Kenya
Juli Boit & Allison Tarus
Webuye County Referral Hospital, Webuye, Kenya
Naseem Mohamed
Department of Medical and Molecular Genetics, School of Medicine, Indiana University, Indianapolis, IN, USA
Kenneth Cornetta
You can also search for this author in PubMed Google Scholar
Contributions
H.E: Curriculum development, coordinating and facilitating the training, writing, review and editing and supervision. K.C: Curriculum development, supervision, writing, review and editing, fund acquisition. S.N: project coordinator, writing, review and editing. E.K: qualitative data analysis, writing, review and editing. J.A: project administration, writing review and editing. J.B: training facilitator, supervision, writing, review and editing. A.T: training facilitator, supervision, writing review and editing. N.M: training facilitator, supervision, writing, review and editing. I.K: quantitative data manager, writing, review and editing.
Corresponding author
Correspondence to Hussein Elias .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from Moi University Institutional Research and Ethics Committee (IREC 2021/203) and all methods were performed in accordance with the relevant guidelines and regulations and an informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Elias, H., Kisembe, E., Nyariki, S. et al. Impact of training on knowledge, confidence and attitude amongst community health volunteers in the provision of community-based palliative care in rural Kenya. BMC Palliat Care 23 , 97 (2024). https://doi.org/10.1186/s12904-024-01415-5
Download citation
Received : 21 April 2023
Accepted : 21 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s12904-024-01415-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community health volunteers
- Community based palliative care
- Teleconsult
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Bureaus and Offices
- Contact HRSA
- Continuation Funding
- Apply for Transitions in Care for Justice-Involved Populations (QIF-TJI)
QIF-TJI Project Plan Form Guide
You will complete a Project Plan Form to provide an overview of your proposed project as part of the Quality Improvement Fund - Transitions in Care for Justice Involved Populations (QIF-TJI) application in the HRSA Electronic Handbooks (EHBs).
We provide this guide for reference purposes only. It does not represent the form as EHBs formats it.
Review the Project Plan Form sections
How to fill out the project overview section, how to fill out the project details section.
The Project Plan Form has two sections:
- Project Overview Provide information that applies to the entire project, including project name, carceral setting partner, problem statement, population of focus, and community engagement approach.
- Project Details Describe your proposed project and innovative activities in detail.
Align all sections of the Project Plan Form with your responses in the Project Narrative.
Project name
Provide a brief title for your entire project.
Narrative field, up to 100 characters.
Carceral setting partner
Provide the Name, Street Address, City, State, and ZIP Code for the carceral setting, such a jail, prison, or other correctional facility, with whom you will collaborate to implement the proposed project.
NOTE: You must include the ZIP code of the carceral setting on your health center’s Form 5B service area ZIP codes.
Problem statement
Briefly describe the current barriers and challenges your proposed project will address.
Narrative field, up to 400 characters.
Population of focus
Briefly describe your population of focus for the proposed project. The description should align with the information you provided in the NEED section of the Project Narrative.
Community engagement approach
Briefly describe your plan to gather input from, and meaningfully engage with patients, community members, and community partners throughout the period of performance.
Narrative field, up to 1,000 characters.
In EHBs you’ll find the following instructions for completing the Project Details section of the Project Plan Form:
Use the “Add Project” button to open a separate window and add information about your proposed project. After you save information about the project, you'll be redirected to this screen. You must add information for at least one project. You can add multiple projects by selecting the “Add Project” button again.
Provide a detailed description of the proposed project.
- A brief overview of your project, including the evidence-based model(s) you’ll use
- Goals you intend to accomplish
- Critical health and health-related social needs the project will address
- The innovative activities you’ll implement
- The evaluative measures you’ll use to assess the success of the project
Descriptions in the Project Details section should align with your responses in the Project Narrative and with the Project Overview section of this Project Plan Form.
After you have entered all information about your project, select “Save and Continue” to return to the Project Plan Form. The information you entered will appear in a table format on the main Project Plan Form. You may add more than one project. The system will assign projects a number according to the order in which you add them.
Project overview
Provide a brief narrative overview of the proposed project, including the evidence-based model(s) you plan to implement.
Narrative field, up to 2,000 characters.
Briefly describe the goal(s) of your proposed project. Tell us how the project will address needs and barriers and improve transitions in care for your population of focus.
Goals should:
- Be specific and measurable
- Reflect input from health center patients and community members who have lived experience with incarceration
Needs summary
Select the needs your project will address. You must select at least one critical health need and at least one health-related social need. You may select multiple.
Select at least one of the following critical health needs your project will address:
- Managing chronic conditions
- Prevention, screening, diagnosis and treatment of HCV, HIV, and other infectious disease
- Reducing risk of drug overdose
- Addressing mental health and substance use disorder treatment needs
Select at least one of the following health-related social needs your project will address:
- Housing insecurity
- Food insecurity
- Financial strain
- Lack of transportation or access to public transportation
- Intimate partner violence
- Other – please describe
Innovative activities
List and describe the specific activities you’ll implement to adapt or build upon evidence-based model(s) of care to address the identified needs and barriers for your population of focus.
Narrative field, up to 4,000 characters.
Evaluative measures
List the evaluative measures you plan to use to assess the success of your project. You must include at least one measure of patient experience and one measure of community engagement.
This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
This is a member publication of Imperial College London (Jisc)
Regulatory Standards and Guidance for the Use of Health Apps for Self-Management in Sub-Saharan Africa: Scoping Review
Authors of this article:

- Benard Ayaka Bene 1, 2 , MBBS, MPH ;
- Sunny Ibeneme 3 , MD, PhD ;
- Kayode Philip Fadahunsi 1 , MBBS, MPH ;
- Bala Isa Harri 4 , MBBS, MPH, MSc ;
- Nkiruka Ukor 5 , MSc ;
- Nikolaos Mastellos 1 , BSc, PhD ;
- Azeem Majeed 1 , MD ;
- Josip Car 1, 6 , MSc, MD, PhD
1 Department of Primary Care and Public Health, School of Public Health, Imperial College London, London, United Kingdom
2 Department of Public Health, Federal Ministry of Health, Abuja, Nigeria
3 Digital Health Specialist, UNICEF East Asia Pacific Regional Office, Bangkok, Thailand
4 Department of Health Planning, Research and Statistics, Federal Ministry of Health, Abuja, Nigeria
5 Strategic Health Information Cluster, World Health Organization, Abuja, Nigeria
6 School of Life Course & Population Sciences, King’s College London, London, United Kingdom
Corresponding Author:
Benard Ayaka Bene, MBBS, MPH
Department of Primary Care and Public Health
School of Public Health
Imperial College London
The Reynolds Building
St Dunstan’s Road
London, W6 8RP
United Kingdom
Phone: 44 7598439185
Email: [email protected]
Background: Health apps are increasingly recognized as crucial tools for enhancing health care delivery. Many countries, particularly those in sub-Saharan Africa, can substantially benefit from using health apps to support self-management and thus help to achieve universal health coverage and the third sustainable development goal. However, most health apps published in app stores are of unknown or poor quality, which poses a risk to patient safety. Regulatory standards and guidance can help address this risk and promote patient safety.
Objective: This review aims to assess the regulatory standards and guidance for health apps supporting evidence-based best practices in sub-Saharan Africa with a focus on self-management.
Methods: A methodological framework for scoping reviews was applied. A search strategy was built and applied across the following databases, gray literature sources, and institutional websites: PubMed, Scopus, World Health Organization (WHO) African Index Medicus, OpenGrey, WHO Regional Office for Africa Library, ICTworks, WHO Directory of eHealth policies, HIS Strengthening Resource Center, International Telecommunication Union, Ministry of Health websites, and Google. The search covered the period between January 2005 and January 2024. The findings were analyzed using a deductive descriptive content analysis. The policy analysis framework was adapted and used to organize the findings. The Reporting Items for Stakeholder Analysis tool guided the identification and mapping of key stakeholders based on their roles in regulating health apps for self-management.
Results: The study included 49 documents from 31 sub-Saharan African countries. While all the documents were relevant for stakeholder identification and mapping, only 3 regulatory standards and guidance contained relevant information on regulation of health apps. These standards and guidance primarily aimed to build mutual trust; promote integration, inclusion, and equitable access to services; and address implementation issues and poor coordination. They provided guidance on systems quality, software acquisition and maintenance, security measures, data exchange, interoperability and integration, involvement of relevant stakeholders, and equitable access to services. To enhance implementation, the standards highlight that legal authority, coordination of activities, building capacity, and monitoring and evaluation are required. A number of stakeholders, including governments, regulatory bodies, funders, intergovernmental and nongovernmental organizations, academia, and the health care community, were identified to play key roles in regulating health apps.
Conclusions: Health apps have huge potential to support self-management in sub-Saharan Africa, but the lack of regulatory standards and guidance constitutes a major barrier. Hence, for these apps to be safely and effectively integrated into health care, more attention should be given to regulation. Learning from countries with effective regulations can help sub-Saharan Africa build a more robust and responsive regulatory system, ensuring the safe and beneficial use of health apps across the region.
International Registered Report Identifier (IRRID): RR2-10.1136/bmjopen-2018-025714
Introduction
Health apps are the most widely used digital health products globally [ 1 , 2 ]. Harnessing the potential of health apps creates a huge opportunity in providing support for health care delivery, including patient communication, patient education, and decision support for self-management [ 3 - 8 ]. Health apps can be an effective tool to strengthen health systems worldwide, especially in low- and middle-income countries including those in sub-Saharan Africa [ 4 , 5 , 9 ]. As a result, the attainment of universal health coverage (UHC) and sustainable development goal (SDG) 3, good health and well-being, can be accelerated [ 8 , 10 ].
Many health apps fall below the expected quality threshold [ 11 ]. Several studies have found that widely used health apps are often technically unreliable and clinically unsafe [ 12 - 14 ] and do not comply with ethical standards and the principles of confidentiality of information and data privacy [ 15 , 16 ]. In addition, many commercially available health apps were not developed using interoperability standards that are widely accepted in sub-Saharan Africa (eg, Fast Healthcare Interoperability Resources [FHIR]) [ 17 - 20 ]. Consequently, it becomes difficult to integrate these apps into a clinical workflow.
Hence, regulation through robust mechanisms is crucial to enhance the development, implementation, and adoption of health apps. Regulatory standards and guidance are essential for the safety of patients as they ensure quality assurance of any new technology in health care and contribute to building mutual trust while promoting the optimal use of the technology [ 21 - 23 ]. Therefore, to ensure that health apps that are used to support the self-management of patients are technically reliable and clinically safe, interoperable across systems, and compliant with the principles of confidentiality of information and data privacy, there is a need for effective regulatory standards. Furthermore, effective regulation can help ensure that health apps for self-management are culturally functional and competent and are accessible to those who need them regardless of gender, ethnicity, geographical location, or financial status [ 24 - 31 ].
Since 2005, there have been ongoing efforts to strengthen digital health governance at both the national and international levels [ 32 , 33 ]. In 2018, the World Health Organization (WHO) member states renewed their commitment to using digital health technologies (DHTs) to advance UHC and SDG 3 [ 33 ]. However, to date, the extent to which the use of health apps for self-management is regulated across countries within the WHO African Region (also known as sub-Saharan Africa) remains unclear. Therefore, this review was conducted to identify available regulatory standards and guidance and assess the extent to which they regulate health apps for self-management in sub-Saharan Africa. The review also mapped out the key stakeholders and their roles in regulating health apps for self-management across sub-Saharan Africa.
Review Questions
The review attempted to answer the following questions: (1) What regulatory standards and guidance are available for regulating health apps for self-management across sub-Saharan Africa? (2) To what extent do regulatory standards and guidance regulate health apps for self-management in terms of what aspects are regulated; why, how, and for whom; and what aspects are not regulated? (3) Who are the key stakeholders and what are their roles in regulating health apps for self-management?
Study Design
The process of this scoping review followed the methodological framework for conducting a scoping study originally described by Arksey and O’Malley [ 34 ] and the updated methodological guidance for conducting a Joanna Briggs Institute scoping review [ 34 - 37 ]. The reporting of the review was guided by the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist [ 38 ]. A completed PRISMA-ScR checklist is provided in Multimedia Appendix 1 . The protocol of this scoping review was published in BMJ Open [ 30 ].
Identifying Relevant Documents
Two reviewers (BAB and SI) developed the search strategy with the assistance of a librarian and in consultation with other research team members (KPF, BIH, NU, NM, AM, and JC). The following key terms were included: policy, legislation, strategy, regulation, standard, criterion, framework, guidance, guideline, digital health, eHealth, app, WHO African Region, and sub-Saharan Africa, and the names of all sub-Saharan African countries.
Owing to the absence of regulatory standards and guidance in scientific databases, the search focus was narrowed down to gray literature sources and institutional websites, including OpenGrey, WHO Regional Office for Africa (AFRO) Library, repositories for digital health policies (ICTworks, WHO’s Directory of eHealth Policies, and Health Information System Strengthening Resource Center), as well as the websites of WHO, International Telecommunication Union (ITU), and Ministries of Health (MOHs). The only scientific databases searched were PubMed, Scopus, and WHO AIM. PubMed was not included in the protocol. We also conducted a systematic search on Google. We used truncation to increase the yield of the results. The search strategy was then applied across PubMed, Scopus, and WHO AIM databases using Boolean terms (mainly OR and AND ) to combine search results. Gray literature sources and institutional websites were searched using phrases containing ≥2 keywords such as “eHealth regulation,” “digital health regulatory standard,” “eHealth regulatory standard,” “digital health regulation,” “digital health policy,” “eHealth policy,” “digital health strategy,” and “eHealth strategy.” For Google search, we added the names of the country to the phrases (eg, “digital health regulation Nigeria”). The reference lists of the included documents were also searched, and key individuals at the MOHs, WHO Country Offices, and the WHO AFRO were contacted for related documents. When our search was conducted, the WHO Directory of eHealth policies website was unavailable, and the WHO AFRO Library was undergoing reconstruction. The search strategies for PubMed, Scopus, and WHO AIM are provided in Multimedia Appendix 2 . The search was conducted between 2005 and January 2024.
Study Selection
The search results obtained from PubMed, Scopus, and WHO AIM were imported into Mendeley (Elsevier) [ 39 ] to remove duplicates. The search conducted on OpenGrey did not yield any results, whereas relevant records obtained from institutional websites, repositories, and Google were downloaded as PDF copies and uploaded to Mendeley. After removing duplicates, the remaining results were imported into Covidence (Veritas Health Innovation) [ 40 ] for screening. Two reviewers (BAB and SI) applied the predefined eligibility criteria ( Textbox 1 ) to screen the documents in 2 stages (title and abstract or executive summary). All discrepancies were discussed until the reviewers reached agreement.
Inclusion criteria
- Type of document: Regulatory standards, guidance, policies, strategies, and committee or government reports that address regulatory issues related to the use of health apps for self-management
- Location: Documents developed and implemented in countries within sub-Saharan Africa
- Date of publication: Documents developed since 2005; the global efforts toward promoting standards to minimize variability and potential harms that could arise from poorly regulated use of digital health began in 2005 [ 33 ]
- Language: Documents written in English language and other official languages of sub-Saharan African countries (Portuguese and French)
Exclusion criteria
- Type of document: Standards, guidance, policies, strategies, and reports not related to regulation of health apps
- Location: Documents from countries outside sub-Saharan Africa
- Date of publication: Documents developed before 2005
- Language: None
Data Charting (Extraction)
Two reviewers (BAB and SI), in consultation with the other members of the research team, developed the data extraction forms using an iterative process that included piloting data extraction and refinement until a consensus was reached.
We proposed in the study protocol [ 30 ] that data extraction would be conducted by the 2 reviewers independently. However, owing to the approach adopted for data extraction (deductive qualitative content analysis), 1 reviewer, rather than 2, initially extracted data from the included documents, and any concerns were discussed with a second reviewer [ 41 ]. Unresolved issues were then discussed and resolved with a third reviewer in a steering group meeting.
Collating, Summarizing, and Reporting Results
To address the research questions (particularly question 2), we adopted a deductive descriptive qualitative content analysis method to analyze and report the key findings. The policy analysis framework by Walt and Gilson [ 42 ] was adapted and applied to ensure that there was a consistent way of organizing the key findings: (1) Content (which aspects are regulated and which aspects are not?)—these are the components that directly or indirectly address regulatory issues related to the use of health apps for self-management, including areas that have not been addressed. (2) Context (why are those aspects regulated?)—this characterizes the rationale indicated for addressing regulatory issues related to the use of health apps for self-management. (3) Process (how are the regulatory standards developed and implemented?)—this describes the methods or approaches used to develop and implement regulatory standards. (4) Actors (who are the regulatory standards targeted toward?)—these are the key actors targeted by the standards.
Using a deductive descriptive qualitative content analysis approach, we examined each included document to systematically identify texts for concepts, patterns, and other relevant information. We then categorized them under content, context, process, or actors in relation to regulating health apps for self-management. The findings under content and context were further organized based on 4 predefined regulatory categories or themes as documented in the literature, namely (1) technical and clinical safety [ 12 - 14 ], (2) data protection and security [ 15 , 16 ], (3) standards and interoperability [ 28 , 31 ], and (4) inclusion and equitable access [ 24 - 29 ].
To address the third research question, the Reporting Items for Stakeholder Analysis (RISA) tool [ 41 ] was used as a guide to group key stakeholders based on role categorization as recognized globally by the WHO, the ITU, and UNESCO [ 32 , 33 , 43 ].
Ethical Considerations
Primary data were not collected in this study. Therefore, no ethics approval was required.
Search Results
A total of 2900 records were obtained after removing duplicates. Although the literature search was conducted in English, the search also yielded documents written in French and Portuguese from the ICTworks repository [ 44 ]. Following the initial screening of the title and abstract (or executive summaries), 73 documents were retrieved for full-text assessment. After applying the inclusion criteria for the full-text assessment, 49 documents were found eligible for inclusion in the review.
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram [ 45 ] showing the study selection process is presented in Figure 1 .

Types of Documents
On the basis of the inclusion criteria, 3 categories of documents were considered for this review, namely “stand-alone regulatory standards and guidance that potentially regulate health apps for self-management,” “national policies and strategies on digital health,” and “other national documents that relate to the regulation of health apps for self-management.” Table 1 presents the types of documents obtained for each country within sub-Saharan Africa.
Characteristics of the Included Documents
Stand-alone regulatory standards and guidance.
We identified and included 6 stand-alone regulatory standards [ 18 , 19 , 46 - 49 ] from 3 countries (Ethiopia, Kenya, and Nigeria). All 6 documents were written in English. The years of development ranged between 2013 and 2021, as indicated in Multimedia Appendix 3 . The years of implementation were not specifically stated.
Although none of the included regulatory standards were exclusively developed to regulate health apps for self-management, 3 of them (Kenya Standards and Guidelines for mHealth Systems [ 18 ], Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ], and Health Sector Information and Communications Technology Standards and Guidelines [ 48 ]) provided concept and information relevant to the regulation of health apps and were included in the qualitative content analysis. The Kenya Standards and Guidelines for mHealth Systems [ 18 ] provides standards and guidelines on the design, development, and implementation of mobile health (mHealth) solutions to ensure they are interoperable, scalable, and sustainable. The Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ] outlines the principles, requirements, and standards for eHealth systems interoperability in Kenya. The Health Sector Information and Communications Technology Standards and Guidelines [ 48 ] provide guidance and a consistent approach across the health sector in Kenya for establishing, acquiring, and maintaining current and future information systems and information and communications technology (ICT) infrastructure that foster interoperability across systems. These 3 documents are a good combination of regulatory standards and guidance that provide content and context relevant to the regulation of health apps in sub-Saharan Africa.
The remaining 3 standards (standard for electronic health record [EHR] system in Ethiopia [ 19 ], standards and guidelines for electronic medical record systems in Kenya [ 46 ], and the health information exchange standard operating procedure and guideline [ 49 ]) were exclusively developed for EHRs or electronic medical records. However, they contain information relevant for mapping stakeholders with potential roles in regulating health apps for supporting self-management.
National Policies and Strategies on Digital Health
This review includes 35 national policies and strategies that are related to digital health (potentially covering health apps) [ 50 - 84 ] from 31 countries written in English, French, and Portuguese (Benin, Botswana, Burkina Faso, Burundi, Cameroon, Comoros, Côte d’Ivoire [Ivory Coast], Democratic Republic of the Congo, Eswatini, Ethiopia, Gabon, Ghana, Kenya, Liberia, Madagascar, Malawi, Mali, Mauritius, Mozambique, Namibia, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, South Africa, Tanzania, Togo, Uganda, Zambia, and Zimbabwe). Although the literature search was conducted in English, it also yielded documents written in French and Portuguese from the ICTworks repository. The years of development and implementation range between 2005 and 2030. Policies and strategies written in French and Portuguese were translated into English using Google Translate. Documents labeled as national development plans, strategic plans, and strategic development plans were considered as national strategies.
National policies and strategies do not offer specific standards or guidance, but rather outline the country’s vision, policy directions, and strategies for using digital technologies in health care. They provide useful information for identifying digital health stakeholders who can play a role in regulating health apps for self-management. For example, Nigeria has a separate National Digital Health Policy [ 72 ] and a National Digital Health Strategy [ 71 ]. Both documents were developed by building on the lessons learned from the end-term evaluation of the previous National Health ICT Strategic Framework [ 85 ]. They describe Nigeria’s renewed vision, mission, goals, objectives, and strategies for the development and implementation of digital health with the aim to improve the quality, efficiency, and effectiveness of health service delivery and health outcomes.
It is worth noting that for countries with >1 policy or strategy, we included only the most recent versions. For instance, as mentioned earlier, Nigeria now has both a national digital health policy and a national digital health strategy. These 2 documents supersede and thus replace the old National Health ICT Strategic Framework [ 86 ]. Details of included documents are presented in Multimedia Appendix 3 .
Other Related National Documents
We included 8 other documents [ 20 , 85 , 87 - 92 ] from 6 countries (Ethiopia, Kenya, Liberia, Nigeria, South Africa, and Tanzania) that did not fall under either stand-alone regulatory standards and guidance or national policies and strategies. These were mostly frameworks, road maps, and reports that potentially provide information relevant to the use of health apps. The years of development and implementation range from 2016 to 2025. These documents do not provide standards or guidance, but they contain information that can help map the digital health stakeholders that potentially play a role in regulating health apps for self-management. When multiple versions of a document exist, only the latest version was taken into consideration. Multimedia Appendix 3 provides details of the included documents.
Content: Aspects That Are Regulated and Aspects That Are Not
Technical and clinical safety.
Technical and clinical safety standards are required to prevent or minimize the harm that may arise from the use of the health ICT systems (including mHealth systems) as well as to improve the health outcomes and user satisfaction. As shown in Figure 2 , two subthemes were generated from included standards [ 18 , 47 , 48 ] as content under technical and clinical safety: v(1) guidance on system quality and (2) guidance on software or app development, acquisition, support, and maintenance.

Notably, 2 of the included standards [ 18 , 47 ] provide guidance on system quality to ensure the quality, security, reliability, performance, and maintenance of eHealth and mHealth systems. The Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ] recommend the implementation of a data quality protocol to ensure that the data collection, collation, analysis, interpretation, dissemination, and use are managed in accordance with the quality standards. Similarly, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] recommends the inclusion of the following requirements in the technical manual: (1) minimum hardware requirements that should incorporate the preferred hardware architecture, (2) minimum software requirements that should include the minimum version of the underlying operating system as well as acceptable versions of related software, and (3) a detailed list of software dependencies (external libraries) necessary for the system to function properly.
The included standards [ 18 , 48 ] cover guidance on software or app development, acquisition, support, and maintenance, which aim to ensure the efficiency and effectiveness of eHealth and mHealth systems. The Kenya Standards and Guidelines for mHealth Systems [ 18 ] recommends a technical manual to provide a detailed description of the system’s installation and maintenance processes for system administrators and implementers; a developer’s guide for software developers and programmers to provide them with an overview of the system, description of the software design methodologies, description of the system architecture, and technical design diagrams; and a user manual to aid users in understanding how the system works and how each feature operates; in addition, the technical manual contains instructions for operating the software; entering and updating data; and generating, saving, and printing reports.
Although the contents generated here provide guidance that is relevant to health apps, they are not specific to health apps. Moreover, there are no clear measures to enable individuals or organizations that use health apps to manage clinical risk appropriately.
Data Protection and Security
Data protection and security are crucial aspects of managing patient information, thus ensuring the confidentiality, integrity, and availability of data as well as the rights and interests of the patient. Two subthemes related to data protection and security are (1) security measures for adequate protection of patients’ digital records and (2) guidance on data exchange.
The included standards [ 18 , 48 ] provide security measures for eHealth or mHealth systems to ensure the adequate protection of digitally accessible patient records. These measures include authentication, accountability, identification, authorization, integrity, confidentiality, availability, security, administration, and audit. This will help to achieve confidentiality, integrity, availability, and nonrepudiation of patient data or health records. Additional levels of security such as data encryption are required when there is a need to store sensitive information on removable devices or media or outside the MOH premises.
The Kenya Standards and Guidelines for mHealth Systems [ 18 ] provide the following guidance on data exchange to ensure privacy: (1) anonymize client data as much as possible before they can be shared; (2) where possible, use pseudonyms for the client data before they can be shared; (3) aggregate client data before they can be shared to reduce possibilities of tracing the data back to the client; and (4) minimize data so that access is available only to the data set required for that particular use. With regard to privacy rules, the Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ] propose that a notice of privacy practices should be given to patients describing how their information may be used or shared while also specifying their legal rights.
Standards and Interoperability
Standards and interoperability are essential concepts in the field of IT, especially for systems that need to communicate and exchange data, as seen in the use of health apps for self-management. Two subthemes related to standards and interoperability are (1) interoperability as a basic requirement and (2) minimum standards to enable integration.
All the regulatory standards [ 18 , 47 , 48 ] highlight the importance of having interoperability as a basic requirement when selecting software products or services for use within the health system. This facilitates interaction across systems. For instance, to facilitate seamless interaction between mHealth systems and primary information systems for data capture, reporting, and decision support in various domains of the health system, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] recommends the incorporation of at least 3 types of interoperability, namely, technical interoperability, semantic interoperability, and process interoperability.
Furthermore, 2 regulatory standards [ 18 , 47 ] proposed minimum interoperability standards to enable the integration of services and data exchange between various systems in health care. For instance, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] suggests standards (for interoperability) for mHealth systems that are consistent with the recommendations in internationally accepted standards. They include the following: (1) clinical messaging—ensuring mHealth systems conform to Health Level 7 (HL7) version 3 standards and corresponding implementation guideline; (2) clinical terminology—ensuring terminologies and classifications for clinical concepts (eg, International Classification of Diseases, tenth revision—for diseases; Systemized Nomenclature of Medicine—for clinical data coding; Logical Observation Identifiers Names and Codes—for laboratories; and RxNorm—for Pharmacies); (3) the mHealth system must use the latest versions of international standards, such as HL7 Clinical Document Architecture for electronic sharing of clinical documents; (4) concepts—mHealth systems will use the idea of “concepts” so that information can be transmitted between systems without losing meaning or context, and HL7 Reference Implementation Model or other appropriate standards are recommended for implementing concepts; (5) architecture—to develop mHealth systems, developers should define the system architecture that should include data elements and business logic. Furthermore, to define how mHealth systems interact with other systems, developers of mHealth solutions must provide application programming interfaces. FHIR is the preferred application programming interface interoperability standard.
Inclusion and Equitable Access
Inclusion and equitable access are essential principles to ensure that health apps are culturally appropriate and relevant and accessible to everyone, regardless of gender, ethnicity, location, or economic status.
All the included regulatory standards [ 18 , 47 , 48 ] indicate that they were developed based on a combination of participatory and consultative approaches involving multiple actors or stakeholders, thus promoting inclusion. However, there are no specific measures or guidance to ensure adequate engagement and representation of all the relevant stakeholders and to sustain that engagement.
The Kenya Standards and Guidelines for mHealth Systems [ 18 ] proposes the following systems attributes to ensure equitable access to mHealth services at all times and from anywhere: (1) allocation of adequate storage and bandwidth capacity; (2) fast response time; (3) fast recovery capabilities; (4) performance monitoring; (5) business continuity processes, for example, backups; and (6) redundant sites and links. Furthermore, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] prescribes the following metrics for measuring system availability: (1) downtime per year, (2) mean time between failure, (3) mean time to repair, and (4) failure in time.
Although the abovementioned systems attributes and metrics for measuring system availability are important, the included standards do not offer any concrete guidance or model for achieving a sustainable funding mechanism for health apps to ensure that they are readily available and accessible to those who need them.
Context: Reasons Why Those Aspects Are Regulated
The 3 standards [ 18 , 47 , 48 ] were developed to address unsafe, isolated, and inconsistent implementation. The Health Sector ICT Standards and Guidelines [ 48 ] suggest that although there has been a lot of ICT investment in the health sector leading to improvement in service delivery and information exchange, there remains the challenge of inconsistency in ICT implementation and harmonization of the health sector system requirements. Hence, there is a need to adopt global best practices for software development, acquisition, support, and maintenance by the MOH. In addition, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] indicates that standards and guidelines are necessary to ensure a consistent approach to the development of ICT systems. Similarly, the Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ] recognize the need to ensure that the processes of collecting, collating, analyzing, interpreting, disseminating, and using data are consistent with data quality standards.
To build mutual trust and maximize the benefits of eHealth information exchange, the Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ] reiterate that as health data are constantly being exchanged across health information systems, robust security standards are required to maintain their integrity and confidentiality. This will build the trust of service users and consequently help to maximize the benefits of eHealth information exchange such as in self-management.
Two of the included regulatory standards [ 47 , 48 ] indicate that the context for standards and interoperability was (1) to address poor coordination, duplication of efforts, and inefficient use of resources and (2) to promote the integration of ICT systems.
The Kenya Standards and Guidelines for E-Health Systems Interoperability [ 47 ] acknowledge that the absence of interoperability standards over the years has led to the duplication of efforts and the inefficient use of ICT resources in health care. Now that ICT has become increasingly relevant in improving efficiency in health service delivery, the Kenya MOH recognizes the need to adopt a standardized approach, hence the development of interoperability standards for eHealth systems. In addition, the Health Sector ICT Standards and Guidelines [ 48 ] emphasize the relevance of interoperability as a requirement for addressing the inconsistency in implementing ICT in the health sector.
The Health Sector ICT Standards and Guidelines [ 48 ] consider “integration of ICT systems” as one of its key guiding principles, acknowledging the lack of information systems integration as a challenge experienced by ICT services across Kenya.
The contexts for inclusion and equitable access as generated from included standards [ 18 , 47 , 48 ] were (1) to promote inclusion and (2) to promote equitable access to services.
To promote inclusion, the standards [ 18 , 47 , 48 ] highlight the importance of involving and engaging multiple actors and stakeholders during the development process. However, no emphasis was placed on the need to sustain stakeholder engagement during the implementation process.
Pertaining to equitable access, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] acknowledges that the public health care system is largely unavailable to most of the population in many developing countries because of geographical location, resource constraints, inefficiencies, and lack of awareness. Hence, it recognizes the importance of ensuring that mHealth services are always accessible by users and from anywhere as well as the need to put in place mechanisms to make this happen.
Process: How the Regulations Are Developed and Implemented
Two themes were generated from the included standards: development and implementation processes [ 18 , 47 , 48 ].
Development Process
All the included standards [ 18 , 47 , 48 ] indicate that they were developed through a participatory process and in consultation with a range of subject experts and interest groups. In addition, the standards [ 18 , 47 , 48 ] adopted a multisectoral approach to engage health-related stakeholders from government ministries or agencies and development partners and a range of subject experts and interest groups. It has also been reported that these standards [ 18 , 47 , 48 ] were developed based on international best practices and with reference to international standards. However, there is no indication that a stakeholder engagement strategy was adopted to sustain the engagement of stakeholders through the entire development and implementation process.
Implementation Process
The 3 regulatory standards [ 18 , 47 , 48 ] identify the key requirements to ensure effective implementation of IT services in the health sector. These are (1) legal authority, (2) coordination, (3) building capacity, and (4) monitoring and evaluation.
The included standards [ 18 , 47 , 48 ] were established based on the legal provisions enshrined in the health and other related acts and laws of Kenya as well as the relevant policies and strategies. Hence, it is expected that their implementation will comply with and be backed by those legal provisions. For example, the Health Sector ICT Standards and Guidelines [ 48 ] indicate that its implementation will be supported by the authority from the Kenya Communications Act 2009, E-Government Strategy, and National ICT Policy. Similarly, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] asserts that it will be implemented by complying with existing and relevant national policies, legal frameworks, strategies, and standards, including the Health Information Policy, ICT Standards, and System Interoperability Principles.
The included standards [ 18 , 47 , 48 ] report that the implementation of regulations will require robust coordination mechanisms. For instance, the Health Sector ICT Standards and Guidelines [ 48 ] indicate that, as the Ministry’s ICT resource manager, the principal secretary (also the head of ICT), in collaboration with the ICT Governance Committee, is responsible for coordinating the implementation of the standard. The ICT Governance Committee comprises representatives from the heads of departments and ICT development partners in the health sector. The committee’s responsibilities include overseeing, enforcing, and reviewing standards as well as initiating ICT projects.
The Health Sector ICT Standards and Guidelines [ 48 ] highlight the need for capacity building or training of the MOH staff and stakeholders who are the primary users of the Ministry’s ICT services. This will enhance their capacity to implement the guidelines provided in the document in line with the ministry’s human resource development policies, regulations, and rules. However, it is acknowledged that building capacity for health ICT is a challenge given that there is low adoption of ICT among health providers, and ICT is not routinely included in the course content of most training programs. The Kenya Standards and Guidelines for mHealth Systems [ 18 ] listed the “number of mHealth practitioners trained on the standards and guidelines” as one of the indicators for monitoring and evaluating mHealth interventions.
The Health Sector ICT Standards and Guidelines [ 48 ] assert that monitoring and evaluation is an essential role of the MOH to ensure efficiency, accountability, and transparency throughout the implementation period. It further stresses that all those who use the Ministry’s ICT services are required to adhere to the provisions in the standard as the MOH will carry out quarterly monitoring exercises on the use of the standard to ensure compliance based on clear indicators. Furthermore, the ICT Governance Committee will periodically review and amend the standard to keep it relevant and effective. Similarly, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] establishes the following key indicators for effectively monitoring and evaluating the implementation of the standards and guidelines: (1) the number of counties in which the MOH has disseminated the standards and guidelines, (2) the number of counties successfully implementing the standards and guidelines, (3) the number of mHealth practitioners trained on the standards and guidelines, (4) the number of mHealth practitioners accessing the standards and guidelines, (5) the number of mHealth practitioners who correctly understand the standards and guidelines, (6) the number of stakeholders who adhere to the standards and guidelines, (7) the number of mHealth systems that follow the required development steps, and (8) the number of mHealth practitioners who have implemented their systems by using the standards and guidelines. In addition, the Kenya Standards and Guidelines for mHealth Systems [ 18 ] indicates that the outlined standards will be reviewed every 3 years to ensure they are up to date with new changes including the changes in policies and systems upgrades.
Although all the abovementioned indicators are relevant, the implementation process is not explicit on the approach for regulating health apps and ensuring compliance with regulatory standards and guidance.
Actors: Those the Regulations Are Targeted at
The included standards [ 18 , 47 , 48 ] identified 2 main groups of actors for whom the regulations and guidance were targeted. They included (1) those who provide digital health services and (2) those who use the ICT infrastructure of the MOH.
Two of the standards [ 47 , 48 ] indicated that the regulations should be implemented by all individuals and organizations that provide ICT-related health care services to the public. Similarly, the Health Sector ICT Standards and Guidelines [ 48 ] state that all those who access or use the MOH ICT infrastructure are expected to adhere to the guidelines outlined in the document.
Mapping of Stakeholders
To address the third research question, we conducted a stakeholder mapping guided by the RISA tool [ 41 ].
A total of 11 categories of key stakeholders were identified from all 49 included documents (6 stand-alone regulatory standards and guidance, 35 national policies or strategies, and 8 other related documents). These categories are consistent with the digital health stakeholders recognized by the WHO, ITU, and UNESCO [ 32 , 33 , 43 ]. Table 2 presents the mapping of stakeholders according to their role categorization. A more detailed table with a potential role description with regard to regulating health apps for self-management is presented in Multimedia Appendix 4 .
a WHO: World Health Organization.
This paper presents the findings of a scoping review of regulatory standards and guidance for the use of health apps for self-management in sub-Saharan Africa. To the best of our knowledge, this is the first study that attempted to identify and assess the extent to which regulatory standards and guidance regulate and guide the use of health apps for self-management in sub-Saharan Africa as well as map out the key stakeholders and their potential roles.
Our findings reveal that only 1 country (Kenya) in sub-Saharan Africa currently has national regulatory standards that could potentially regulate the use of health apps for self-management. The included standards failed to adequately address adequate attention to inclusion and equitable access. This is concerning given the growing need to promote the adoption of culturally appropriate and relevant health apps and to ensure that they are available to those who need them regardless of gender, ethnicity, geographical location, or financial status [ 24 - 29 ]. Consequently, this review provides insights into the regulation of health apps for self-management in sub-Saharan Africa, which needs to be given more attention if the potential of these apps is to be harnessed in the region.
Principal Findings
We identified 49 documents from 31 countries in sub-Saharan Africa. Although none of the included standards provided a specific set of regulations on health apps for self-management, we identified 3 standards [ 18 , 47 , 48 ] that provided relevant information regarding the regulation of health apps. The included national policies and strategies, in contrast, only outline the goals and commitments made by national governments to promote the adoption of digital technologies in the health sector and the plans and paths set forth to achieve these goals. However, the information they provided was relevant for identifying and mapping digital health stakeholders who potentially have vital roles in regulating the use of health apps for self-management.
The policy analysis framework (content, context, process, and actors) [ 42 ] was adapted and applied to organize the key findings. The content covered the following areas: guidance on systems quality; guidance on software and app development, acquisition, support, and maintenance; security measures for adequate protection of patients’ digital records; guidance on data exchange; interoperability as a basic requirement; minimum standards to enable integration; involvement and engagement of relevant stakeholders; and system attributes for equitable access to services. Meanwhile, the context was to address unsafe, isolated, and inconsistent implementation; to build mutual trust and maximize the benefits of eHealth information exchange; to address poor coordination, duplication of efforts, and inefficient use of resources; to promote the integration of ICT systems; and to promote inclusion and equitable access to services. The process involved the development process (which covers participatory and consultative processes and multisectoral approach, with reference to international standards and best practices) and the implementation process (which covers legal authority, coordination, capacity building, and monitoring and evaluation). The targeted actors were those who provided digital health services and those who used the ICT infrastructure of the MOH.
Furthermore, key stakeholders with potential roles in regulating health apps for self-management were identified. They include the government, regulatory bodies, funders, intergovernmental and nongovernmental organizations, academia, and the health care community.
Implications of the Study Findings for Practice
Regulatory standards and guidance act as a bridge between technological innovation and its safe and effective use in health care. They ensure that while technology continues to advance, the safety and trust of patients are never compromised. Among the plethora of health apps on the market, the over-the-counter, nonregulated apps such as wellness and fitness apps are the most mainstream [ 93 - 95 ]. On the other side of the spectrum, there are regulated health apps that are classified under medical devices or software as medical device products [ 94 , 95 ]. Some of these are prescription-only apps, such as digital therapeutics (DTx) apps for managing substance dependence [ 95 , 96 ].
Although some high-income countries have made significant strides in ensuring the safety, effectiveness, and accessibility of health apps, the journey has indeed not been without challenges and hurdles. Sub-Saharan Africa, although dealing with its own unique set of challenges, has the opportunity to learn from the experiences of these high-income countries. This could potentially allow the region to bypass some of the hurdles encountered by high-income countries in their journeys.
Technical and clinical safety are essential requirements that health apps must meet before they can be considered for use for self-management to minimize the risk of harm to patients. It is well documented that health apps that function poorly pose a serious threat to the safety of patients. An example illustrating how health apps used for self-management can threaten patient safety is evident in a study [ 12 ]. This study [ 12 ] revealed that widely used health apps designed to calculate and estimate insulin doses could endanger patients by providing incorrect or inappropriate dose recommendations. Similarly, 2 successive studies that assessed the contents and tools of apps for asthma discovered that none of the apps in the first study offered comprehensive information or adequate tools for asthma self-management, whereas the follow-up study, which was conducted 2 years later, showed a 2-fold increase in the number of asthma apps, yet there was no improvement in the content and tools offered by the newer apps. In fact, many apps recommended self-management procedures that were not supported by evidence [ 13 , 14 ]. Accordingly, some health apps that support the self-management of long-term conditions do not adhere to evidence-based guidelines and are unresponsive to the evolving health needs of patients.
Although the context of included regulatory standards with regard to technical and clinical safety was to address unsafe, isolated, and inconsistent implementation, the guidance provided by these regulatory standards is not specific to health apps, and they do not provide appropriate guidance and standards for health organizations and other key stakeholders to establish a framework for managing the clinical risks associated with deploying and implementing self-management health apps. Considering the rapid advancements in digital health (including artificial intelligence [AI] or machine learning and big data), health apps will increasingly play a crucial role in supporting self-management through digitally enabled care pathways that will improve personalized care and health outcomes [ 97 , 98 ]. Therefore, it is imperative to ensure the technical reliability and clinical safety of health apps for self-management through robust regulatory standards and guidance. For instance, a guide on the criteria for health app assessment, developed by the UK government, includes technical stability and clinical safety as criteria for deciding whether health apps should be considered for use in the National Health Service (NHS) [ 99 ]. In addition, medical device apps are required to conform to the NHS clinical risk management standards as part of the clinical safety requirements [ 99 , 100 ]. In the event of any concerns regarding the safety of a medical device app, the Yellow Card reporting system can be used by a responsible clinical safety officer or any other individual to notify the Medicines and Healthcare products Regulatory Agency (MHRA) [ 101 , 102 ].
To adequately manage patient information when health apps are used for self-management, data protection and security standards and guidance are required. They guarantee that data are kept and handled safely and responsibly within the provisions of the law and that patients’ rights and interests are respected.
There have been ongoing concerns about compliance with ethical standards, the principles of confidentiality of information, and data privacy. For example, an assessment of apps that had previously been endorsed by the former UK NHS Apps Library revealed substantial gaps in compliance with data protection principles regarding the collection, storage, and transmission of personal information. This has raised a fundamental concern about the credibility of developer disclosures and whether these disclosures can be trusted by certification programs [ 15 ]. A study assessed the privacy practices of the 36 most popular apps for depression and smoking cessation for Android and iOS in the United States and Australia [ 16 ]. The findings revealed that although only 69% (25/36) of the apps included a privacy policy, 92% (33/36) of the apps shared data with a third party, and only 92% (23/25 with privacy policy) of the apps disclosed sharing data with a third party in their policy. Although 81% (29/36) of the apps shared data with Google and Facebook for the purposes of advertising, marketing, or analytics, only 43% (12/28) of the apps that shared data with Google and 50% (6/12) of the apps that shared data with Facebook disclosed this in their policy [ 16 ].
In this regard, health app developers and providers in the United Kingdom are required to conduct a data protection risk assessment before they launch or update their apps to ensure compliance with the United Kingdom General Data Protection Regulation (GDPR) and other relevant regulations, including the Data Protection Act 2018 [ 103 ]. By conducting a data protection risk assessment, health app developers and providers can demonstrate that they are accountable; they respect the privacy and dignity of their users; and that they deliver safe, effective, and ethical solutions [ 104 ].
Health apps are expected to play an increasingly important role in supporting self-management. However, this ambition can only be achieved if citizens trust that these apps are collecting and analyzing data safely and in accordance with robust regulatory standards and guidance. It is also crucial that these apps provide reliable information that clinicians can act on [ 98 ]. The context of the standards included in this study regarding data protection and security was to build mutual trust and maximize the benefits of eHealth information exchange. Trust is a key factor in the successful adoption and use of health apps, and transparency in data handling and clinical decision-making is essential to build and maintain that trust. This is also paramount for the widespread acceptance and impact of health apps on health care outcomes in sub-Saharan Africa.
We acknowledge the existence of numerous national laws related to data protection and security outside the health sector. Hence, guidelines that link these legislations together must be provided to ensure compliance with all relevant laws and guidance when using patient data. An example of how to achieve this is the United Kingdome’s guide to good practice for digital and data-driven health technologies that provides guidelines on how to abide by the laws and principles that govern data security and protection in the United Kingdom, including the GDPR, Data Protection Act 2018, and Caldicott Principles [ 105 ].
Standards and interoperability are essential for effectively developing, deploying, and implementing health apps to support self-management in sub-Saharan Africa. Interoperability is the ability of different systems, devices, or applications to communicate and exchange data with each other in a coordinated manner, thus providing timely and seamless portable information across organizational, regional, and national boundaries and optimizing both individual and population health [ 106 ]. In the same vein, standards enable interoperability between systems or devices through a common language and a common set of expectations [ 106 ].
Interoperability is crucial in improving the quality, safety, and efficiency of care delivery as well as empowering patients and providers with access to relevant and timely information [ 99 ]. One of the most widely used and accepted interoperability standards for health care data exchange is FHIR [ 106 , 107 ]. FHIR is a global industry standard developed by HL7 International. FHIR is designed to be quick to learn and implement and to support a variety of use cases, including self-management [ 108 ]. By using apps that are based on an FHIR standard, patients can benefit from data analytics that show how their health data relate to their chronic conditions or wellness goals [ 109 ]. They could also access all their health information from one place, even if they visit different health professionals who use different electronic medical records or EHR, thus promoting integrated care [ 28 , 31 , 33 , 109 - 115 ]. As a result, patient care can easily be coordinated.
The context of the included regulatory standards with regard to standards and interoperability was to address poor coordination, duplication of efforts, and inefficient use of resources and to promote the integration of ICT systems. However, in sub-Saharan Africa, there are many challenges and barriers to the adoption and implementation of interoperability standards, such as the lack of awareness or knowledge of the benefits and requirements of interoperability standards among stakeholders; lack of incentives or regulations to encourage or enforce the adoption of interoperability standards by app developers and vendors; lack of resources or capacity to implement interoperability standards, including technical expertise, infrastructure, funding, or governance; and lack of alignment or coordination among the different actors and initiatives involved in developing, deploying, and implementing the digital health interventions [ 30 , 116 - 119 ]. To address these challenges, some possible solutions may include raising awareness and education on the importance and value of interoperability standards for health apps among all relevant actors; developing and implementing policies and guidelines that promote or mandate the use of interoperability standards by app developers and vendors; providing technical assistance and support for app developers and vendors to adopt and implement interoperability standards, such as tools, frameworks, testing, certification, or accreditation; and establishing and strengthening collaboration and coordination among the different stakeholders and initiatives involved in health app development, deployment, and implementation in sub-Saharan Africa. In addition, the Digital Health Platform Handbook, a toolkit developed by the collaborative efforts of the WHO and ITU [ 120 ], can help countries in sub-Saharan Africa to develop and implement digital health platforms as the underlying infrastructure for interoperable and integrated national digital health systems. The digital health platform is a system-wide approach to developing digital health solutions with the aim to overcome the problems of siloed, vertical, and isolated applications and systems that hamper data management, innovation, efficiency, and impact in the health sector.
Inclusion and equitable access are crucial to ensuring that health apps and related services are culturally appropriate and relevant as well as accessible to all who need them, regardless of gender, ethnicity, geographical location, ability, or financial status [ 24 - 29 ]. This is the key to promoting a “sense of belonging” and “ownership” and thus underscoring the importance of stakeholder mapping and involvement or engagement through the development and implementation process [ 22 ].
In this study, the included regulatory standards demonstrate the importance of inclusion by adopting both a participatory and consultative approach involving multiple stakeholders from different sectors. However, the standards do not provide clear guidance to ensure the adequate participation and sustained engagement of all relevant stakeholders. The lack of concise guidance to ensure the adequate participation and engagement of all relevant stakeholders, especially the susceptible and disadvantaged groups, can increase the risk of tokenistic tendencies, which can undermine the cultural appropriateness of health apps [ 25 , 121 ]. Some susceptible groups, such as women and people with low socioeconomic status, may face additional barriers to accessing and using health apps, such as lack of digital literacy, privacy concerns, cultural norms, or stigma [ 25 ]. Similarly, the cost of developing, maintaining, and updating health apps may not be covered by public or private health insurance schemes, which could limit their affordability and availability for low-income or uninsured populations [ 95 ]. However, there is no specific guidance or model for an effective funding mechanism for health apps in the included regulatory standards.
To address these challenges and ensure equitable access to health apps for self-management in sub-Saharan Africa, possible measures may include developing policies and regulations that support integrating health app interventions into existing health systems and financing mechanisms and engaging with stakeholders from different sectors and backgrounds (including health professionals, patients, communities, governments, civil society, academia, and industry) to co-develop and co-implement frameworks or models that promote the use of health apps for self-management in ways that are responsive to the local context and needs. Moreover, establishing regulations that provide appropriate financing or reimbursement options will reduce the risk of developers of good quality health apps turning to data mining for revenue, thus increasing privacy concerns [ 95 ]. For instance, in Germany, the reimbursement of health apps classified as medical devices (Digitale Gesundheitsanwendungen) was introduced in 2021 under the statutory health insurance [ 122 , 123 ]. When a medical device is prescribed by a physician or a physiotherapist, the manufacturer must submit an application to the German Federal Institute for Drugs and Medical Devices (Bundesinstitut für Arzneimittel und Medizinprodukte) for approval [ 123 ]. The Federal Association of the Statutory Health Insurance Funds (Spitzenverband Bund der Krankenkassen) determines and negotiates the reimbursement thresholds following approval. However, the manufacturer must demonstrate that the app is safe, functional, and of good quality; complies with data protection requirements; and benefits patient care [ 123 ].
The process of regulating health apps essentially involves the development and implementation of regulatory standards and guidance. According to our study, the development process comprises a participatory and consultative process, a multisectoral approach, and a reference to international standards and best practices. In contrast, the implementation process is ongoing and requires appropriate legal authority, coordination, capacity building, and monitoring and evaluation.
We recognize that health apps can be accessed and used by patients from different parts of the world, and this means that countries need to carefully consider whether health apps that are accessed and used by their citizens meet the national or regional legal and ethical requirements, including their cultural and linguistic needs [ 23 ]. For countries in sub-Saharan Africa, a cross-border or regional collaboration between national legal authorities through the coordination of agencies such as the African Medicines Regulatory Harmonization (AMRH) may help to ensure that health apps built for the region are safe, effective, and user-friendly for everyone, considering the contextual differences of the countries [ 23 ]. For instance, all medical device companies that want to sell their products in the European market must obtain a Conformité Européenne (CE) mark for their devices, which indicates that they meet the legal requirements and can be freely circulated within the European Union [ 124 ]. Although the European Union member states regulate medical devices, the European Medicines Agency is involved in the regulatory process.
The regulation of health apps is extremely complex and involves a wide range of stakeholders. Therefore, a robust coordination mechanism is essential to reduce the risk of fragmentation and duplication of efforts and to promote the efficient use of resources. Most countries in sub-Saharan Africa have units in health ministries that coordinate and oversee the regulation of medical products. These units should be autonomous, full-fledged departments with legal authority (boards or commissions) to ensure independent, transparent, and accountable decision-making, but this is often not the case [ 125 ]. These units are recognized by the national authorities as regulators (eg, the National Medicines Regulatory Authority [NMRA]) [ 126 ]. Such organizational structures hinder the effectiveness of the national regulatory authorities in fulfilling their mandate and prevent the establishment of quality management systems to ensure transparent and accountable decision-making [ 125 ].
Furthermore, Essén et al [ 23 ] analyzed health app policy or regulation in 9 high-income countries (Sweden, Norway, Denmark, Netherlands, Belgium, Germany, England, the United States, and Singapore) and found that most of these countries adopted centralized approaches to app evaluation. Although centralized approaches might have advantages over self-evaluation, they may create bottlenecks and limit the availability of high-quality health apps for users. As suggested by Essén et al [ 23 ], a decentralized approach, such as the accreditation of evaluation agencies, maybe a worthwhile solution. However, this will require adequate coordination to ensure the consistency and reliability of the evaluation criteria and methods across different agencies as well as the transparency and accountability of the accreditation process. A possible way to achieve this is to adopt a common framework that can guide the evaluation and accreditation of health apps.
Similarly, the postmarket surveillance (PMS) system, which is a new regulation for medical devices in Europe, is a process of collecting and analyzing data on medical devices after they have been launched into the market to ensure their safety and performance and to identify any problems or need for improvements [ 127 , 128 ]. The PMS system is important because premarket data, which are obtained from testing a medical device before it is launched, have limitations in capturing the long-term performance and risks of the device [ 128 ]. Currently, the PMS system does not cover fitness and wellness apps, which are commonly used in self-management. Hence, Yu [ 93 ] proposed that the PMS system should also be applied to DHTs, such as fitness and wellness apps. They argue that the postmarket data would help regulators periodically review and adjust the regulatory standards for these groups of health apps based on their risks and benefits.
Drawing on the experience of the United Kingdom, it can be clearly demonstrated that the regulation of health apps is a complex, a multifaceted, and an evolving process that involves different regulators and criteria depending on the nature and function of the app. For instance, a centralized NHS Apps Library was launched as a beta site in April 2017 to provide patients with a collection of trusted and easy-to-use digital health tools [ 129 ]. The library provided access to a range of health apps that were reviewed and approved by the NHS, including apps that could help patients manage conditions such as diabetes, mental health, and chronic obstructive pulmonary disease [ 130 ]. However, the library was closed in December 2021 [ 131 ]. Although no reason for the closure was provided on the website, it is likely because of persistent concerns regarding the safety of patients and data privacy involving multiple apps including those listed in the library [ 12 , 14 - 16 , 131 , 132 ]. The NHS App was introduced in January 2019 before the closure of the NHS Apps Library to serve as the gateway for accessing NHS services including ordering repeat prescriptions and booking or managing appointments [ 133 ].
Furthermore, the United Kingdom Health Security Agency, formerly known as Public Health England, issued a guidance on criteria for health app assessment in October 2017 [ 99 ]. The purpose of this guidance was to ensure that all health apps built for the UK population work well and provide clear information about their functions, benefits, and intended outcomes for patients and health care professionals. On the basis of this guidance, those intending to build an app are required to conform to certain regulations before being considered for the app assessment process. The 2 main regulations are the medical device regulation and the Care Quality Commission (CQC) registration. Apps that are considered as medical devices must register with the MHRA and have a CE mark. Apps providing health or social care that fit into 1 of 14 regulated activities are required to register with the CQC before they can be assessed [ 134 ]. CQC is an independent regulator of health and social care services in England.
Similarly, the Organisation for the Review of Care and Health Apps (ORCHA) is a UK-based organization that independently evaluates and distributes health apps. It provides services such as app review, accreditation, curation, and recommendation within the United Kingdom and across the world [ 135 ]. ORCHA also enables organizations (including the NHS) to build a decentralized web-based digital health library of consumer-friendly over-the-counter apps [ 135 - 137 ]. These apps are continuously assessed by ORCHA against the standards and regulations in clinical and professional assurance, data quality and privacy, and usability and accessibility [ 137 ].
In addition, the Digital Technology Assessment Criteria (DTAC) were introduced in beta in October 2020, and its first official version was subsequently launched in February 2021 [ 138 ]. The DTAC plays a crucial role in ensuring that digital health tools meet the necessary standards in areas such as clinical safety, data protection, technical security, interoperability, usability, and accessibility. By serving as the national baseline criteria for DHTs in the NHS and social care, it provides a valuable framework for health care organizations during procurement. It also offers guidance for developers on the expectations for their digital technologies within the NHS and social care. This is an example of how a harmonized framework can help ensure the quality and safety of DHTs, including health apps.
In addition, the National Institute for Health and Care Excellence Evidence Standards Framework is a set of evidence standards for a wide range of DHTs designed to help evaluators and decision makers in the health care system to consistently identify DHTs that are likely to offer benefits to the users and the health care system [ 139 ]. The Evidence Standards Framework was first published in March 2019 and is ideally used before DHTs (including health apps) are considered for commissioning or procurement by the NHS [ 140 ]. It is a crucial tool for ensuring that DHTs are clinically effective and offer value to the health and care system in the United Kingdom. In August 2022, the framework was updated to include AI and data-driven technologies with adaptive algorithms [ 140 ].
Furthermore, DTx apps, which are a type of medical device, are not allowed into the UK market unless they comply with the UK GDPR and meet the requirements of DTAC. In addition, they must bear the CE or UK Conformity Assessed marks [ 141 ]. This means that DTx apps must demonstrate their safety and efficacy through clinical trials and comply with the relevant regulations for data protection and quality standards as regulated by the MHRA. DTx products are also recognized as DHTs under the National Institute for Health and Care Excellence Evidence Standards Framework [ 142 ]. DTx incorporates software to treat, prevent, or manage specific diseases or conditions [ 143 , 144 ]. The fact that DTx products typically focus on a narrow clinical indication and generate evidence of clinical efficacy underscores their potential to make a substantial contribution to self-management and health care delivery in general. The increasing recognition of the role of DTx in patient care by regulators is also noteworthy, and the creation of regulatory and reimbursement pathways for approved apps further enables DTx products to continue to play an important role in impacting health care delivery [ 1 , 143 ]. This is a testament to the potential of regulated health apps to revolutionize health care and improve patient outcomes.
Among the many lessons to learn from the experience of the United Kingdom is that the regulation of health apps must evolve to keep pace with advances in DHTs and adapt to the changing needs and demands of digital health. Moreover, efforts are being made to streamline the multifaceted approaches to simplify app regulation and access in the United Kingdom [ 23 ]. Therefore, a robust and dynamic coordination mechanism, along with political will, skilled personnel, reliable funding, and a robust framework for monitoring and evaluating progress and aligning key performance indicators, is essential for countries in sub-Saharan Africa to keep pace with the advancement in the regulation of health apps. There is also a need to strengthen collaboration and ensure regulatory harmonization among national regulatory authorities and continental bodies such as the regional economic communities, AMRH, and the WHO AFRO [ 126 ].
Capacity building and monitoring and evaluation are important factors for ensuring effective regulation of health apps given the complex nature of the process. The regulation of medical products (including health apps) in sub-Saharan Africa generally includes licensing and accreditation, evaluation, inspection, quality control, information dissemination and promotion, and monitoring of adverse events [ 125 ]. Therefore, high-level skills as well as effective monitoring and evaluation will be required to ensure the success of the process. For most countries in sub-Saharan Africa, the NMRA is responsible for coordinating and overseeing the regulatory system of medical products [ 125 , 126 ]. However, in most cases, NMRAs are unable to perform the core regulatory functions expected of them [ 145 ]. More than 90% of African countries have limited or no capacity to regulate medical products, with only 7% having moderately developed capabilities [ 145 ]. The lack of effective NMRAs in Africa exposes the citizens to potential harm by allowing unsafe, low-quality, and fake medical products to circulate and be used [ 145 ].
Although it is the responsibility of governments to establish functional regulatory systems and ensure effective monitoring and evaluation of the regulatory process, the involvement of international and continental organizations to support sub-Saharan African countries improve the regulatory capacity of their national regulatory agencies would be extremely beneficial. For instance, the African Medicines Agency (AMA) was established in November 2019 as a treaty adopted by the African Union Member States to help address the concerns arising from weak regulatory systems on the continent. At present, 37 countries have signed the AMA treaty, including 26 countries that have ratified it [ 146 ]. The main objective of the AMA is to enhance the capacity of States Parties and regional economic communities to regulate medical products to improve the quality, safety, and efficacy of medical products on the continent [ 147 ]. The AMA, in collaboration with other existing capacity building initiatives or organizations, such as the WHO Global Initiative on Digital Health, ITU, AMRH, WHO AFRO, and United Nations Children’s Fund, can assist sub-Saharan African countries in aligning their regulatory requirements with available resources and support them to acquire the necessary tools and skills to build effective and sustainable regulatory systems for health apps. This can be achieved by adopting a decentralized approach to engage a network of technical experts across the African Union similar to the model of the European Medicines Agency [ 148 ].
Actors or Stakeholders
The regulation of health apps often requires working with a wide range of actors or stakeholders. However, in this review, we identified only 2 main actor groups (those who provide digital health services and those who use the ICT infrastructure of the health ministry). These are the groups that are targeted by the included regulatory standards.
From a broader perspective, 12 categories of stakeholders according to their potential role in regulating health apps for the self-management were mapped in this study. The potential contribution of these stakeholders to the regulation of health apps for self-management in sub-Saharan Africa not only depends on their roles and responsibilities but also on their interests, needs, expectations, and influence [ 41 , 149 - 151 ]. Thus, a robust stakeholder analysis is paramount as it can help define the scope of the regulatory process, prioritize the requirements, manage the expectations, and ensure the engagement and participation of stakeholders throughout the regulatory process [ 41 , 152 - 156 ]. Our stakeholder mapping, as presented in Table 2 (refer to Multimedia Appendix 4 for more details), lays the foundation for national governments to conduct a robust stakeholder analysis and to adopt an all-inclusive stakeholder engagement strategy to manage and sustain the engagement and participation of all relevant stakeholders [ 157 , 158 ].
Recommendations
Our review found that the regulation of health apps in sub-Saharan Africa is especially poor and almost nonexistent, as only Kenya has national standards that could address some of the regulatory issues related to health apps. Therefore, we recommend the following actions to help sub-Saharan African countries improve the regulation of health apps to support self-management:
- Establish a clear and consistent definition of what constitutes a health app (considering AI or machine learning) and what level of regulation is required for different types of apps.
- Develop and implement criteria and guidelines that ensure the quality, safety, and usability of health apps.
- Engage with independent app evaluators, such as ORCHA, to adopt a common framework that can guide the evaluation and accreditation of health apps and use the framework to create and maintain decentralized and transparent platforms that showcase and evaluate health apps for users and health care professionals.
- Develop and implement policies and regulations that enable sustainable funding for health apps such as integrating the use of health apps for self-management into existing health systems and financing pathways or mechanisms.
- Support and facilitate innovation and collaboration across the sub-Saharan Africa region, especially in areas including but not limited to data security and privacy, interoperability standards, usability, accessibility, funding, capacity building, and monitoring and evaluation of the regulatory process.
- Manage and sustain the engagement, involvement, and participation of all relevant stakeholders in the regulatory process by conducting a robust stakeholder analysis and adopting an all-inclusive stakeholder engagement strategy.
Strengths and Limitations of the Study
This study has several strengths, which include an extensive search of gray literature and repositories, contact with key individuals, and the use of a systematic approach. Given that regulatory standards and guidance are unavailable in scientific databases, a wide range of gray literature and repositories were searched. In addition, contact was made with key staff members to obtain relevant documents, including those at the MOHs, the WHO country offices, and the WHO AFRO. Second, to enhance the strength of the study, a policy analysis framework was adapted and used to systematically organize the key study findings, whereas a deductive descriptive qualitative content analysis approach was used to identify and analyze texts that contained relevant concepts and other related information based on the 4 predefined themes. Third, the RISA tool was used to guide the mapping of key stakeholders. This has further increased the robustness of the study findings.
The limitations of this study include the fact that our literature search was conducted in English. Although the literature search was conducted in English, it yielded documents written in French and Portuguese from the ICTworks repository. Second, regulatory standards and guidance are not readily available on scientific databases; hence, it is possible that some relevant documents might have been missed. However, efforts were made to obtain these documents by contacting key stakeholders including key contact persons at the WHO AFRO, WHO country offices, and MOHs. In addition, contacting key individuals only for the purposes of requesting documents rather than conducting direct interviews was one of the limitations of this study. Interviewing key contact persons and stakeholders to obtain additional information could have strengthened the review; however, we did not interview any key individuals or stakeholders because it was beyond the scope of this review. Nonetheless, we recommend that future studies consider incorporating interviews to explore the perspectives of key stakeholders.
Conclusions
Health apps are increasingly being used by patients to manage their health, and sub-Saharan African countries can leverage these apps to advance their progress toward achieving SDG 3 (good health and well-being) and UHC, especially given the rapid advancement of AI and big data. However, our study has established that the regulation of health apps in sub-Saharan Africa is inadequate to ensure that health apps are technically reliable and clinically safe; interoperable across systems; compliant with the principles of confidentiality of information and data privacy; culturally appropriate and relevant; and accessible to everyone regardless of gender, ethnicity, location, or income. Therefore, the region can learn from the experiences of some high-income countries such as the United Kingdom and Germany to develop and implement a robust and responsive regulatory system that supports the widespread adoption of safe, effective, and beneficial health apps for its population.
Following the publication of this review, a summary of the findings will be disseminated to the relevant organizations. In addition, the key findings will be summarized and presented at national, regional, and international conferences.
Acknowledgments
The authors would like to thank Rebecca Jones, the Library Manager and Liaison Librarian at Charing Cross Library, who advised and assisted with the search strategy for this study. This work is part of the PhD research of BAB, which is sponsored by the government of Nigeria. AM and JC were supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration Northwest London (NIHR200180). The views expressed in this publication are those of the authors and not necessarily those of the government of Nigeria or the NIHR or the Department of Health and Social Care. In the Results and Discussion sections, Microsoft Copilot in Bing [ 159 ] was used to help summarize and modify a few texts as well as suggest some citations.
Data Availability
The search strategy for PubMed, Scopus, and the World Health Organization AIM is presented in Multimedia Appendix 1 . All data generated or analyzed during this study are included in this published article (and its supplementary information files). The documents analyzed are available directly from the relevant institutional websites, ICTworks repository [ 44 ] or upon request from the relevant government departments in each country. Additionally, documents in the list of references that are not accessible on the web can be solicited from the corresponding author on reasonable request.
Authors' Contributions
BAB and JC conceived the study. BAB designed the study with contributions from JC and NM. BAB drafted the manuscript, and JC, NM, AM, SI, KPF, BIH, and NU read and contributed to it. AM was the clinical lead, and JC acted as a guarantor for this study. The final manuscript was read and approved by all the authors.
Conflicts of Interest
None declared.
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist.
Database search strategy.
Details of included documents.
Mapping of the stakeholders according to their potential role in regulating health apps for self-management.
- Aitken M, Nass D. Digital health trends 2021: innovation, evidence, regulation, and adoption. IQVIA Institute for Human Data Science. 2021. URL: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/digital-health-trends-2021/iqvia-institute-digital-health-trends-2021.pdf?&_=1669449368070 [accessed 2022-11-26]
- Mobile app threat landscape report. RiskIQ. 2020. URL: https://www.riskiq.com/2020-mobile-threat-landscape-report-thank-you/ [accessed 2021-07-19]
- El-Sappagh S, Ali F, Hendawi A, Jang JH, Kwak KS. A mobile health monitoring-and-treatment system based on integration of the SSN sensor ontology and the HL7 FHIR standard. BMC Med Inform Decis Mak. May 10, 2019;19(1):97. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Labrique AB, Vasudevan L, Kochi E, Fabricant R, Mehl G. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract. Aug 06, 2013;1(2):160-171. [ FREE Full text ] [ CrossRef ]
- Adepoju IOO, Albersen BJA, De Brouwere V, van Roosmalen J, Zweekhorst M. mHealth for clinical decision-making in sub-Saharan Africa: a scoping review. JMIR Mhealth Uhealth. Mar 23, 2017;5(3):e38. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vegesna A, Tran M, Angelaccio M, Arcona S. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed J E Health. Jan 2017;23(1):3-17. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Use of appropriate digital technologies for public health: Report by the Director-General. World Health Organization. 2016. URL: https://iris.who.int/handle/10665/274134 [accessed 2023-05-06]
- El-Osta A, Rowe C, Majeed A. Developing a shared definition of self-driven healthcare to enhance the current healthcare delivery paradigm. J R Soc Med. Nov 2022;115(11):424-428. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hussein R. A review of realizing the universal health coverage (UHC) goals by 2030: part 2- what is the role of eHealth and technology? J Med Syst. Jul 2015;39(7):72. [ CrossRef ] [ Medline ]
- Sustainable development goal 3: Ensure healthy lives and promote well-being for all at all ages. United Nations. URL: https://sdgs.un.org/goals/goal3 [accessed 2023-05-07]
- Coronavirus: apps to help the elderly. Organisation for the Review of Care and Health Apps. 2020. URL: https://orchahealth.com/coronavirus-apps-to-help-the-elderly/ [accessed 2021-07-19]
- Huckvale K, Adomaviciute S, Prieto JT, Leow MKS, Car J. Smartphone apps for calculating insulin dose: a systematic assessment. BMC Med. May 06, 2015;13:106. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huckvale K, Car M, Morrison C, Car J. Apps for asthma self-management: a systematic assessment of content and tools. BMC Med. Nov 22, 2012;10:144. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huckvale K, Morrison C, Ouyang J, Ghaghda A, Car J. The evolution of mobile apps for asthma: an updated systematic assessment of content and tools. BMC Med. Mar 23, 2015;13:58. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huckvale K, Prieto JT, Tilney M, Benghozi PJ, Car J. Unaddressed privacy risks in accredited health and wellness apps: a cross-sectional systematic assessment. BMC Med. Sep 07, 2015;13:214. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huckvale K, Torous J, Larsen ME. Assessment of the data sharing and privacy practices of smartphone apps for depression and smoking cessation. JAMA Netw Open. Apr 05, 2019;2(4):e192542. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ndlovu K, Mars M, Scott RE. Interoperability frameworks linking mHealth applications to electronic record systems. BMC Health Serv Res. May 13, 2021;21(1):459. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kenya standards and guidelines for mHealth systems. Kenya Ministry of Health. 2017. URL: https://www.health.go.ke/wp-content/uploads/2020/02/Revised-Guidelines-For-Mhealth-Systems-May-Version.pdf [accessed 2023-03-21]
- Standard for electronic health record system (EHRs) in Ethiopia. Ethiopia Minister of Health. 2021. URL: https://registry.betterehealth.eu/ehealth-policies/standard-electronic-health-record-system-ehrs-ethiopia [accessed 2023-04-21]
- National health normative standards framework for digital health interoperability in South Africa. South Africa Department of Health. 2021. URL: https://www.health.gov.za/wp-content/uploads/2022/10/HNSF_Gazette_21_October_2022.pdf [accessed 2023-05-15]
- Ferretti A, Ronchi E, Vayena E. From principles to practice: benchmarking government guidance on health apps. Lancet Digit Health. Jun 2019;1(2):e55-e57. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Diao JA, Venkatesh KP, Raza MM, Kvedar JC. Multinational landscape of health app policy: toward regulatory consensus on digital health. NPJ Digit Med. May 11, 2022;5(1):61. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Essén A, Stern AD, Haase CB, Car J, Greaves F, Paparova D, et al. Health app policy: international comparison of nine countries' approaches. NPJ Digit Med. Mar 18, 2022;5(1):31. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care. Feb 2002;25(2):259-268. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chaney SC, Mechael P. Self-Care Trailblazer Group. 2020. URL: https://media.psi.org/wp-content/uploads/2020/09/31000510/Digital-Self-Care-Final.pdf [accessed 2021-05-20]
- Kanzaveli T. Healthcare: shiftingfrom “one size fits all” to “one size fits one”. Medium. 2017. URL: https://tkanzaveli.medium.com/healthcare-shifting-from-one-size-fits-all-to-one-size-fits-one-d56136ded705 [accessed 2022-03-04]
- Myth 1 – one app will fit all!. Organisation for the Review of Care and Health Apps. URL: https://orchahealth.com/myth-1-one-app-will-fit-all/ [accessed 2022-03-04]
- Aitken M, Lyle J. Patient adoption of mHealth: use, evidence and remaining barriers to mainstream acceptance. IQVIA Institute for Human Data Science. Sep 2015. URL: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/patient-adoption-of-mhealth.pdf [accessed 2021-05-21]
- Mechael P, Batavia H, Kaonga N. Barriers and gaps affecting mhealth in low and middle income countries: policy white paper. Center for Global Health and Economic Development Earth Institute, Columbia University. 2010. URL: http://www.globalproblems-globalsolutions-files.org/pdfs/mHealth_Barriers_White_Paper.pdf [accessed 2021-03-24]
- Bene BA, Ibeneme S, Fadahunsi KP, Harri BI, Ukor N, Mastellos N, et al. Regulatory standards and guidance for the use of health applications for self-management in Africa: scoping review protocol. BMJ Open. Feb 11, 2022;12(2):e058067. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Aitken M, Gauntlett C. Patient apps for improved healthcare: from novelty to mainstream. IMS Institute for Healthcare Informatics. 2013. URL: https://ignacioriesgo.es/wp-content/uploads/2014/03/iihi_patient_apps_report_editora_39_2_1.pdf [accessed 2024-03-10]
- National eHealth Strategy Toolkit. World Health Organization, International Telecommunication Union. 2012. URL: https://www.itu.int/pub/D-STR-E_HEALTH.05-2012 [accessed 2021-06-28]
- Global strategy on digital health 2020-2025. World Health Organization. 2021. URL: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf [accessed 2021-06-23]
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. Feb 2005;8(1):19-32. [ FREE Full text ] [ CrossRef ]
- Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst. Jul 09, 2008;6:7. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. Sep 20, 2010;5:69. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. Oct 2020;18(10):2119-2126. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. Oct 02, 2018;169(7):467-473. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leitner C, Potenziani D. Mendeley reference manager. Mendeley. 2022. URL: https://www.mendeley.com/reference-management/reference-manager [accessed 2022-08-03]
- Better systematic review management. Covidence. URL: https://www.covidence.org/ [accessed 2023-02-13]
- Franco-Trigo L, Fernandez-Llimos F, Martínez-Martínez F, Benrimoj SI, Sabater-Hernández D. Stakeholder analysis in health innovation planning processes: A systematic scoping review. Health Policy. Oct 2020;124(10):1083-1099. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan. Dec 1994;9(4):353-370. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Digital health: a call for government leadership and cooperation between ICT and health. Broadband Commission. 2017. URL: https://broadbandcommission.org/wp-content/uploads/2021/09/WGHealth_Report2017-.pdf [accessed 2021-06-28]
- Vota W. Every African country’s national eHealth strategy or digital health policy. ICT works. 2019. URL: https://www.ictworks.org/african-national-ehealth-strategy-policy/ [accessed 2023-12-10]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. Jul 21, 2009;6(7):e1000097. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Standards and guidelines for electronic medical record systems in Kenya. Kenya Ministry of Medical Services, Kenya Ministry of Public Health and Sanitation. 2010. URL: http://guidelines.health.go.ke:8000/media/Standards_and_Guidelines_for_EMR_Systems.pdf [accessed 2023-04-21]
- Kenya standards and guidelines for E-health systems interoperability. Kenya Ministry of Health, AfyaInfo Project. 2014. URL: https://pdf.usaid.gov/pdf_docs/PA00TB2K.pdf [accessed 2023-03-21]
- Health sector ICT standards and guidelines. Kenya Ministry of Health. 2013. URL: https://www.medbox.org/pdf/5e148832db60a2044c2d2895 [accessed 2023-03-21]
- Health information exchange standard operating procedure (SOP) and guideline. Nigeria Federal Ministry of Health. Jul 2020.
- National eHealth strategy 2018-2022. Benin Ministry of Health. 2017.
- The eHealth strategy of botswana 2020-2024. Botswana Ministry of Health. URL: https://ehealth.ub.bw/bhdc/Docs/MOH%20ehealth%20Strategy%20Book%20A4.pdf [accessed 2023-04-22]
- Health sector digital strategy 2016-2020. Burkina Faso Ministry of Health.
- National health informatics development plan of Burundi. Burundi Ministry of Public Health. 2015.
- The 2020-2024 national digital health strategic plan. Cameroon Ministry of Public Health. 2020.
- National eHealth strategy 2017-2021. Comoros Ministry of Health. 2016.
- eHealth strategic plan. Cote d’Ivoire Minister of Health and Public Hygiene. 2011.
- National development plan for health informatics. Democratic Republic of Congo Ministry of Public Health. 2014.
- Kingdom of Swaziland eHealth strategy 2016 - 2020. Kingdom of Swaziland Ministry Of Health. 2016.
- Information revolution strategic plan (2018-2025). Ethiopia Ministry of Health. 2018.
- Strategic master plan of the health information system of the Gabon. Gabon Ministry of Public Health and Population. 2017.
- National e-Health strategy. Ghana Ministry of Health. 2010.
- Kenya national e-Health strategy. Kenya Ministry of Medical Services, Kenya Ministry of Public Health & Sanitation. 2011.
- Kenya national eHealth policy 2016-2030. Kenya Ministry of Health. 2016.
- National strategy - Liberia - 2016-2021. Liberia Ministry of Health. 2016.
- Strategic plan for strengthening the health information system of Madagascar 2018–2022. Madagascar Ministry of Public Health. 2017.
- National digital health strategy 2020-2025. Malawi Ministry of Health. 2020.
- National eHealth policy in Mali. Mali Ministry of Health and Public Hygiene. 2013.
- Health 2015: seamless continuity of care. Mauritius Ministry of Health and Quality of Life. 2015.
- Strategic plan of information system for health 2009-2014. Mozambique Ministry of Health. 2009.
- National eHealth strategy 2019-2023. Niger Ministry of Public Health. 2018.
- National digital health strategy 2021-2025. Nigeria Federal Ministry of Health. 2021.
- National digital health policy. Nigeria Federal Ministry of Health. 2021.
- National digital health strategic plan 2018-2023. Rwanda Ministry of Health. 2018. URL: https://elearning.helinanet.org/mod/resource/view.php?id=890 [accessed 2023-05-09]
- Strategic plan for digital health 2018-2023. Senegal Ministry of Health and Social Action. 2018.
- National digital health strategy 2018-2023. Sierra Leone Ministry of Health and Sanitation, Sierra Leone Ministry of Information and Communication. 2018.
- The national digital health strategy 2019 – 2024. Tanzania Ministry of Health, Community Development, Gender, Elderly and Children. 2019.
- National digital health strategy for South Africa 2019 - 2024. South Africa Department of Health. 2019.
- Strategic plan for the development of eHealth in Togo 2013-2015. Togo Ministry of Health. 2012.
- Uganda national eHealth policy. Uganda Ministry of Health. 2016.
- Uganda national eHealth strategy 2017 - 2021. Uganda Ministry of Health. URL: https://health.go.ug/sites/default/files/National%20e_Health%20Strategy_0.pdf [accessed 2023-05-16]
- National eHealth strategy 2017-2021. Zambia Ministry of Health. 2017.
- Zimbabwe’s E-Health strategy 2012-2017. Ministry of Health and Child Welfare. 2012.
- National eHealth strategy 2021-2025. Namibia Ministry of Health & Social Services. 2021. URL: https://www.scribd.com/document/639371316/eHealth-Strategy-Namibia-2021# [accessed 2023-05-13]
- Health sector ICT policy and strategy. Ghana Ministry of Health. 2005. URL: https://www.moh.gov.gh/wp-content/uploads/2016/02/Health-Sector-ICT-Policy-and-Strategy.pdf [accessed 2023-05-08]
- Adebola OJ. Beyond national digital health strategy: final report of end term evaluation for the National Health ICT Strategic Framework 2015-2020. Nigeria Federal Ministry of Health. May 2021.
- National Health ICT Strategic Framework 2015 - 2020. Nigeria Federal Ministry of Health. 2016. URL: https://www.health.gov.ng/doc/HealthICTStrategicFramework.pdf [accessed 2023-05-16]
- Digital health blueprint. Ethiopia Ministry of Health. 2021. URL: http://repository.iifphc.org/bitstream/handle/123456789/1658/Ethiopian-Digital-Health-Blueprint.pdf?sequence=1&isAllowed=y [accessed 2023-05-16]
- Kenya health information systems interoperability framework. Kenya Ministry of Health. 2020. URL: https://www.data4sdgs.org/sites/default/files/services_files/Kenya%20Health%20Information%20Systems%20Interoperability%20Framework.pdf [accessed 2023-05-16]
- National community health digitization strategy 2020-2025. Kenya Ministry of Health, Division of Community Health Services. 2021. URL: https://www.eahealth.org/sites/www.eahealth.org/files/content/attachments/2021-08-02/eCHIS-Strategy-2020-2025.pdf [accessed 2023-05-16]
- Leitner C, Potenziani D. Health information systems interoperability in Liberia. IntraHealth International. 2016. URL: https://elearning.helinanet.org/mod/resource/view.php?id=938 [accessed 2023-05-16]
- Narrative for 2022 national digital health annual operational plan (AOP). Nigeria Federal Ministry of Health. 2022.
- Tanzania digital health investment road map 2017-2023. Tanzania Ministry of Health, Community Development, Gender, Elderly and Children, President’s Office Regional Administration and Local Government. 2017.
- Yu H. Regulation of digital health technologies in the European Union: intended versus actual use. In: Cohen GI, Minssen T, Price II NW, Robertson C, Shachar C, editors. The Future of Medical Device Regulation: Innovation and Protection. Cambridge. Cambridge University Press; Mar 31, 2022;103-114.
- Policy for device software functions and mobile medical applications: guidance for industry and Food and Drug Administration staff. U.S. Food and Drug Administration. 2022. URL: https://www.fda.gov/media/80958/download [accessed 2023-10-10]
- Gordon WJ, Landman A, Zhang H, Bates DW. Beyond validation: getting health apps into clinical practice. NPJ Digit Med. 2020;3:14. [ FREE Full text ] [ CrossRef ] [ Medline ]
- FDA clears mobile medical app to help those with opioid use disorder stay in recovery programs. U.S. Food and Drug Administration. 2018. URL: https://www.fda.gov/news-events/press-announcements/fda-clears-mobile-medical-app-help-those-opioid-use-disorder-stay-recovery-programs [accessed 2021-01-27]
- Digital maturity model: achieving digital maturity to drive growth. Deloitte. 2018. URL: https://www2.deloitte.com/content/dam/Deloitte/global/Documents/Technology-Media-Telecommunications/deloitte-digital-maturity-model.pdf [accessed 2021-10-20]
- May E. How digital health apps are empowering patients. Deloitte. 2021. URL: https://www2.deloitte.com/us/en/blog/health-care-blog/2021/how-digital-health-apps-are-empowering-patients.html [accessed 2023-10-06]
- Guidance: criteria for health app assessment. Public Health England. 2017. URL: https://www.gov.uk/government/publications/health-app-assessment-criteria/criteria-for-health-app-assessment [accessed 2023-10-16]
- Clinical risk management standards. National Health Service Digital. 2020. URL: https://digital.nhs.uk/services/clinical-safety/clinical-risk-management-standards [accessed 2023-10-28]
- Report a problem with a medicine or medical device. Gov.uk. URL: https://www.gov.uk/report-problem-medicine-medical-device [accessed 2023-11-07]
- Digital technology assessment criteria for health and social care (DTAC) - Version 1.0. National Health Service X. 2021. URL: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Ftransform.england.nhs.uk%2Fmedia%2Fdocuments%2FDTAC_version_1.0_FINAL_updated_16.04.odt&wdOrigin=BROWSELINK [accessed 2023-11-07]
- Data protection impact assessment: NHS login - formerly Citizen Identity. National Health Service Digital. 2022. URL: https://digital.nhs.uk/services/nhs-login/data-protection-impact-assessment [accessed 2023-11-07]
- Risks and data protection impact assessments (DPIAs). Information Commissioner’s Office. URL: https://ico.org.uk/for-organisations/uk-gdpr-guidance-and-resources/accountability-and-governance/accountability-framework/risks-and-data-protection-impact-assessments-dpias/ [accessed 2023-11-07]
- A guide to good practice for digital and data-driven health technologies. Department of Health and Social Care. 2021. URL: https://www.gov.uk/government/publications/code-of-conduct-for-data-driven-health-and-care-technology/initial-code-of-conduct-for-data-driven-health-and-care-technology [accessed 2023-10-30]
- Interoperability in healthcare. Healthcare Information and Management Systems Society (HIMSS). 2023. URL: https://www.himss.org/resources/interoperability-healthcare [accessed 2023-10-17]
- DAPB4020: UK core Fast Healthcare Interoperability Resources (FHIR) release 4 (R4) governance. National Health Service Digital. 2022. URL: https://digital.nhs.uk/data-and-information/information-standards/information-standards-and-data-collections-including-extractions/publications-and-notifications/standards-and-collections/dapb4020-uk-core-fhir-r4-governance [accessed 2023-10-17]
- Fast Healthcare Interoperability Resources (FHIR). National Health Service Digital. 2022. URL: https://digital.nhs.uk/services/fhir-apis [accessed 2023-10-17]
- FHIR Interoperability Basics: 4 things to know. Health IT Analytics. 2022. URL: https://healthitanalytics.com/news/4-basics-to-know-about-the-role-of-fhir-in-interoperability [accessed 2023-11-07]
- Giordanengo A, Bradway M, Pedersen R, Grøttland A, Hartvigsen G, Årsand E. Integrating data from apps, wearables and personal electronic health record (pEHR) systems with clinicians’ electronic health records (EHR) systems. Int J Integr Care. Nov 09, 2016;16(5):16. [ FREE Full text ] [ CrossRef ]
- A plan for digital health and social care. Department of Health & Social Care. 2022. URL: https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care [accessed 2022-12-01]
- Ryu B, Kim N, Heo E, Yoo S, Lee K, Hwang H, et al. Impact of an electronic health record-integrated personal health record on patient participation in health care: development and randomized controlled trial of MyHealthKeeper. J Med Internet Res. Dec 07, 2017;19(12):e401. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Winter A, Takabayashi K, Jahn F, Kimura E, Engelbrecht R, Haux R, et al. Quality requirements for electronic health record systems*. A Japanese-German information management perspective. Methods Inf Med. Aug 07, 2017;56(7):e92-e104. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wachter RM. Making IT work: harnessing the power of health information technology to improve care in England. National Advisory Group on Health Information Technology. 2016. URL: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/550866/Wachter_Review_Accessible.pdf [accessed 2021-07-22]
- Framework on integrated people-centred health services (IPCHS). World Health Organisation. 2023. URL: https://www.who.int/teams/integrated-health-services/clinical-services-and-systems/service-organizations-and-integration [accessed 2023-06-05]
- Ibeneme S, Karamagi H, Muneene D, Goswami K, Chisaka N, Okeibunor J. Strengthening health systems using innovative digital health technologies in Africa. Front Digit Health. 2022;4:854339. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ibeneme S, Ukor N, Ongom M, Dasa T, Muneene D, Okeibunor J. Strengthening capacities among digital health leaders for the development and implementation of national digital health programs in Nigeria. BMC Proc. 2020;14(Suppl 10):9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Delivering safe digital health. Organisation for the Review of Care and Health Apps. URL: https://orchahealth.com/ [accessed 2023-10-22]
- Mamuye AL, Yilma TM, Abdulwahab A, Broomhead S, Zondo P, Kyeng M, et al. Health information exchange policy and standards for digital health systems in Africa: a systematic review. PLOS Digit Health. Oct 2022;1(10):e0000118. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Digital health platform handbook: Building a digital information infrastructure (infostructure) for health. World Health Organization, International Telecommunication Union. 2022. URL: https://www.itu.int/dms_pub/itu-d/opb/str/D-STR-E_HEALTH.10-2020-PDF-E.pdf [accessed 2021-05-22]
- Framework for involving patients in patient safety 2021. National Health Service England. 2021. URL: https://www.england.nhs.uk/patient-safety/framework-for-involving-patients-in-patient-safety/ [accessed 2023-03-23]
- Olesch A. Towards harmonised EU landscape for digital health: summary of the roundtable discussions in selected EIT Health InnoStars countries. EIT Health InnoStars. Jan 2023. URL: https://eithealth.eu/wp-content/uploads/2023/02/EIT_Health_DiGA_report_Jan2023.pdf [accessed 2023-10-10]
- Grieb J, Tschammler D, Färber C, Woitz S. Digital health laws and regulations germany. Global Legal Group. 2023. URL: https://iclg.com/practice-areas/digital-health-laws-and-regulations/germany [accessed 2023-11-03]
- Human regulatory: medical devices. European Medicines Agency. URL: https://www.ema.europa.eu/en/human-regulatory/overview/medical-devices [accessed 2023-10-12]
- Strengthening the capacity for regulation of medical products in the African region. World Health Organization Regional Office for Africa. 2013. URL: https://iris.who.int/bitstream/handle/10665/94308/AFR_RC63_7.pdf?sequence=1 [accessed 2023-10-17]
- Ncube BM, Dube A, Ward K. Establishment of the African Medicines Agency: progress, challenges and regulatory readiness. J Pharm Policy Pract. Mar 08, 2021;14(1):29. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Post market surveillance system. European Union Medical Device Regulation. 2023. URL: https://eumdr.com/post-market-surveillance-system/ [accessed 2023-10-31]
- Dayal R. Effective post-market surveillance for medical devices: An essential part of medical devices regulation (MDR). Capgemini. 2020. URL: https://www.capgemini.com/insights/expert-perspectives/effective-post-market-surveillance-for-medical-devices-an-essential-part-of-mdr/ [accessed 2023-10-31]
- NHS app library reaches 70 apps in honour of the NHS birthday. Northampton General Hospital NHS Trust. 2018. URL: https://www.northamptongeneral.nhs.uk/News/News-Archive/2018/NHS-App-Library-reaches-70-apps-in-honour-of-the-NHS-birthday.aspx [accessed 2023-09-21]
- Developers invited to add to NHS apps library. National Health Service Digital. 2018. URL: https://digital.nhs.uk/news/2018/developers-invited-to-add-to-nhs-apps-library [accessed 2023-09-22]
- The NHS apps library has closed. National Health Service Digital. 2021. URL: https://digital.nhs.uk/services/nhs-apps-library#:~:text=The%20NHS%20Apps%20Library%20was%20decommissioned%20in%20December%202021.&text=Further%20information%20can%20be%20found%20on%20the%20NHS.UK%20website [accessed 2023-09-22]
- Larsen ME, Huckvale K, Nicholas J, Torous J, Birrell L, Li E, et al. Using science to sell apps: evaluation of mental health app store quality claims. NPJ Digit Med. 2019;2:18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- About the NHS app. National Health Service. Dec 4, 2023. URL: https://www.nhs.uk/nhs-app/about-the-nhs-app/ [accessed 2023-09-22]
- Scope of registration: regulated activities. Care Quality Commission. 2022. URL: https://www.cqc.org.uk/guidance-providers/scope-registration-regulated-activities [accessed 2023-11-05]
- Distributing great apps into health and care services across the world. Organisation for the Review of Care and Health Apps. 2020. URL: https://orchahealth.com/wp-content/uploads/2020/12/Health-and-Care-1.pdf [accessed 2023-10-09]
- Our founder, our story and our values: we exist to make digital health healthy. Organisation for the Review of Care and Health Apps. URL: https://orchahealth.com/about-us/ [accessed 2023-10-09]
- Health app library: empower your community with safe access to health apps and digital health products. Organisation for the Review of Care and Health Apps. URL: https://orchahealth.com/our-products/health-app-library/#:~:text=A%20Health%20App%20Library%20is,on%20the%20Health%20App%20Library [accessed 2023-10-09]
- Digital technology assessment criteria (DTAC). National Health Service X. URL: https://www.nhsx.nhs.uk/key-tools-and-info/digital-technology-assessment-criteria-dtac/ [accessed 2023-10-09]
- Evidence standards framework (ESF) for digital health technologies. National Institute for Health and Care Excellence. 2023. URL: https://www.nice.org.uk/about/what-we-do/our-programmes/evidence-standards-framework-for-digital-health-technologies [accessed 2023-10-08]
- Tsang L, Kerr-Peterson H. UK NICE updates its evidence standards framework for data-driven digital health technologies. Ropes & Gray. 2022. URL: https://www.ropesgray.com/en/insights/alerts/2022/10/uk-nice-updates-its-evidence-standards-framework-for-data-driven-digital-health-technologies [accessed 2023-10-09]
- Guidance: medical device stand-alone software including apps (including IVDMDs). Medicines and healthcare products regulatory agency. 2023. URL: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1168485/Medical_device_stand-alone_software_including_apps__including_IVDMDs_.pdf [accessed 2023-10-09]
- Digital therapeutics in the United Kingdom. Digital Therapeutics Alliance. 2021. URL: https://dtxalliance.org/wp-content/uploads/2021/06/DTA_DTx-Overview_UK.pdf [accessed 2023-10-09]
- Transforming global healthcare by advancing digital therapeutics. Digital Therapeutics Alliance. 2023. URL: https://dtxalliance.org/ [accessed 2023-10-10]
- International Organization for Standardization (ISO) digital therapeutic definition. Digital Therapeutic Alliance. Jun 2023. URL: https://dtxalliance.org/wp-content/uploads/2023/06/DTA_FS_ISO-Definition.pdf [accessed 2023-10-09]
- Ndomondo-Sigonda M, Miot J, Naidoo S, Dodoo A, Kaale E. Medicines regulation in Africa: current state and opportunities. Pharmaceut Med. 2017;31(6):383-397. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chinele J. East Africa shows solid support for African Medicines Agency treaty. Health Policy Watch. Aug 16, 2023. URL: https://healthpolicy-watch.news/east-africa-shows-solid-support-for-african-medicines-agency-treaty/ [accessed 2023-10-09]
- Treaty for the establishment of the African Medicines Agency 2019. African Union. 2019. URL: https://au.int/sites/default/files/treaties/36892-treaty-0069_-_ama_treaty_e.pdf [accessed 2023-10-17]
- European Medicines Agency: about us. European Medicines Agency. Mar 1, 2023. URL: https://www.ema.europa.eu/en/documents/other/about-us-european-medicines-agency-ema_en.pdf [accessed 2023-10-18]
- Bryson JM. What to do when stakeholders matter. Public Adm Rev. Mar 2004;6(1):21-53. [ FREE Full text ] [ CrossRef ]
- Iyawa G, Herselman M, Botha A. Potential stakeholders and perceived benefits of a digital health innovation ecosystem for the Namibian context. Procedia Computer Science. 2017;121:431-438. [ CrossRef ]
- Ferretti V. From stakeholders analysis to cognitive mapping and multi-attribute value theory: an integrated approach for policy support. European Journal of Operational Research. Sep 2016;253(2):524-541. [ CrossRef ]
- Brugha R, Varvasovszky Z. Stakeholder analysis: a review. Health Policy Plan. Sep 2000;15(3):239-246. [ CrossRef ] [ Medline ]
- Schmeer K. Guidelines for conducting a stakeholder analysis 1999. Partnerships for Health Reform, Abt Associates. 1999. URL: https://www.ktecop.ca/wordpress/wp-content/uploads/guidelines-stakeholder-analysis-PHR-1999.pdf [accessed 2023-10-17]
- Gilmour J, Beilin R. Stakeholder mapping for effective risk assessment and communication. Australian Centre of Excellence for Risk Analysis, University of Melbourne. Apr 2007. URL: https://cebra.unimelb.edu.au/__data/assets/pdf_file/0006/2220990/gilmour0609.pdf [accessed 2023-10-17]
- Quality, service improvement and redesign tools: stakeholder analysis. National Health Service England, National Health Service Improvement. 2022. URL: https://www.england.nhs.uk/wp-content/uploads/2022/02/qsir-stakeholder-analysis.pdf [accessed 2023-10-20]
- Craven MP, Lang AR, Martin JL. Developing mHealth apps with researchers: multi-stakeholder design considerations. Springer; 2014. Presented at: Third International Conference, DUXU 2014, held as a part of HCI International; June 22-27, 2014;15-24; Heraklion, Greece. URL: https://doi.org/10.1007/978-3-319-07635-5_2 [ CrossRef ]
- How to encourage stakeholder participation. SustaiNet Software International. URL: https://sustainet.com/how-to-encourage-stakeholder-participation/ [accessed 2023-10-20]
- Stakeholder engagement. Organisation for Economic Cooperation and Development. URL: https://www.oecd.org/governance/better-international-rulemaking/compendium/keyprinciples/stakeholderengagement.htm [accessed 2023-10-20]
- Microsoft Copilot in Bing. Microsoft. URL: https://www.bing.com/chat?form=NTPCHB [accessed 2023-03-15]
Abbreviations
Edited by A Mavragani; submitted 19.05.23; peer-reviewed by N O'Brien, A Essén; comments to author 07.09.23; revised version received 08.12.23; accepted 23.02.24; published 11.04.24.
©Benard Ayaka Bene, Sunny Ibeneme, Kayode Philip Fadahunsi, Bala Isa Harri, Nkiruka Ukor, Nikolaos Mastellos, Azeem Majeed, Josip Car. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

- President's Cabinet
- Executive Office of the President
- USA Freedom Corps
- Faith-Based & Community
- Office of Management and Budget
- National Security Council
- Citizens' Handbook
- Federal Agencies & Commissions
- Federal Statistics
- Application
- Nominations
- Afghanistan
- Budget Management
- Environment
- Global Diplomacy
- Health Care
- Homeland Security
- Immigration
- International Trade
- Judicial Nominations
- Middle East
- National Security
- Current News
- Press Briefings
- Proclamations
- Executive Orders
- Setting the Record Straight
Thomas Graham Special Assistant to the President and Senior Director for Russian Affairs

Mr. Graham served as a a Foreign Service Officer from 1984 until 1998. His assignments included two tours of duty at the U.S. Embassy in Moscow, where he served as head of the political/internal unit and acting political counselor. Between tours in Moscow, he worked on Russian and Soviet affairs on the Policy Planning Staff of the Department of State and as a policy assistant in the Office of the Undersecretary of Defense for Policy.
Mr. Graham holds a Ph.D. in political science from Harvard University and a B.A. in Russian studies from Yale University.


IMAGES
VIDEO
COMMENTS
A. The community health nurse continuously develops himself personally and professionally. B. Health education and community organizing are necessary in providing community health services. C. Community health nursing in intended primarily for health promotion and prevention and treatment of disease. D.
Studying N493 Community Health Nursing II at Aspen University? On Studocu you will find 14 assignments, practice materials, lecture notes, coursework, summaries and. Skip to main content. ... Module 8 assignment. 10 pages 2020/2021 100% (6) 2020/2021 100% (6) Save. Module 1 Assignment. 7 pages 2020/2021 67% (9) 2020/2021 67% (9) Save. Final ...
A comprehensive approach to patient care is required in community health nursing. Its emphasis is on individuals, families, and groups within a particular area which focuses on the health promotion of an entire population while also preventing disease, disability, and mortality rates in a community. Educating the community to maintain a healthy ...
different assignments: Windshield Survey 10%, Project Plan 5%, Presentation (see rubric) 25% Peer review in class discussion 5%. Students will use the five-step community health nursing process (Maurer & Smith) with communities to develop a plan to improve or maintain the health of a small population. The steps
Week 2 Sentinel City Assignment 3: Subsystem-Health and Social Services . Epidemiological studies to identify health issues and trends are known as the Epidemiological Triangle. The Community/Public Health nurse utilizes the concept of the Epidemiological Triangle to identify vulnerable populations and intervene to decrease or eliminate risk.
The community health nurse typically begins a community health needs assessment by determining what data is already available. [2] As previously discussed in the " Community Health Concepts " section, national, state, county, and local health needs assessments are widely available.
Community health nursing is a dynamic and vital field within the nursing profession, focused on providing holistic care to populations within a defined community. This specialized branch of nursing goes beyond individual patient care, extending its reach to families, groups, and entire communities. This article will delve into community health ...
Community health Nursing is the synthesis of nursing and public health practice applied to promote and protect the health of population. It combines all the basic elements of professional, clinical nursing with public health and community practice. Community health nursing is essential particularly at this point
Part 3 - Community Health Nursing Process Assignment. Using all of the information identified in Parts 1 - 2, the student will write 2 community health nursing diagnoses. Then, the student ...
Community health nursing is a vital part of the healthcare system. The CDC reports that 6 in 10 adults in the U.S. suffer from health problems that originate from chronic conditions and diseases acquired in the community, such as obesity, heart disease, and cancer. By working within the community, CHNs provide services for these conditions while helping to educate people on how best to prevent ...
The role of a community health nurse is multifaceted. Generally, community health nurses may carry out any of the 10 Essential Public Health Services, including: Assessing and monitoring population health. Strengthening, supporting, and mobilizing communities and partnerships. Creating, championing, and implementing policies, plans, and laws.
By giving individuals in need of care and education, the community health nurse has an influence on the community. She. also explained that it was important to ensure that services are accessible to people in need and to speak up for the community's health. She stated, "Being a patient advocate as a community health nurse is crucial."
The goal of community health nursing is to promote, protect and preserve the health of the public. Community health nursing involves these basic concepts: Promote healthy lifestyle. Prevent disease and health problems. Provide direct care. Educate community about managing chronic conditions and making healthy choices.
Self Reflection for Community Health Nursing . Community health nursing focus on health promotion, disease prevention and maintenance of health. ... textbooks and nursing journals that help me prepare and practice better as the community health nurse. I completed all assignments given by the professor which further enhanced my learning. My ...
Community Health Assessment. Alexander Cur琀椀s Galen College of Nursing NSG 3480 Dr. Rachael Benne琀琀, DNP, RNC-NIC November 30th, 2022. Community Health Assessment Cancer 391. Heart disease- 126. Numbers are per 100, Live Births- Community Data General Death- Mortality- Infant- 5. Cancer 391. Heart disease- 126.
4 credits. Clock Hours: 3 credits theory (2 ½ hours); 1 credit clinical (2 hours) Course Description and Purpose. The purpose of this course is to introduce students to community health nursing, health promotion and disease prevention across the life span. A major focus of this course is for students to critically think about and discuss the ...
Community Health II Assignments Module 1: Community Educational Project Site Selection and Letter Most community educational projects are developed in collaboration with other healthcare professionals and the affected population, rather than by community ... The community health nursing intervention strategies—promote social and recreational ...
Assessment. The community health nurse typically begins a community health needs assessment by determining what data is already available. [2] As previously discussed in the "Community Health Concepts" section, national, state, county, and local health needs assessments are widely available. Secondary analysis refers to analyzing previously collected data to determine community needs.
Simulation activities have proven to be a valuable resource for nursing education, providing students with the opportunity to practice physical assessment and technical skills. Most published simulation scenarios have focused on traditional medical specialties. However, there is a recent trend in which entry-level nurses are increasingly engaged outside the traditional acute care setting.
Assignment: Community Health Nurse. Culture and the values learned within a cultural group are critical to how people perceive health, health care, and nursing care providers (Maurer, Smith, 2013). A community health nurse be educated in the cultural values, beliefs, views and their accepted way of life in order to provide care in a manner that ...
In 2014, the World Health Assembly WHA 67.19 called upon the World Health Organization (WHO) and Member States to improve access to palliative care (PC), with an emphasis on primary healthcare and community/home-based care [].Approximately 800,000 people in Kenya are in need of PC while only 14,552 accessing the service [].Similar to other countries in Africa, the need of PC in Kenya is ...
The World Bank, WHO, Partnerships for Health Reform, USAID, and. 3 Lewis, M. (2005) Addressing the Challenge of HIV/AIDS: Macroeconomic, Fiscal and Institutional Issues, Center for Global Development, Washington, DC. 4 Lewis (2005) and World Bank (2005). bilateral donors are all struggling for the best way to deal with this issue.
You will complete a Project Plan Form to provide an overview of your proposed project as part of the Quality Improvement Fund - Transitions in Care for Justice Involved Populations (QIF-TJI) application in the HRSA Electronic Handbooks (EHBs). We provide this guide for reference purposes only. It does not represent the form as EHBs formats it.
Approved for publication by the 201st WMA Council Session Moscow, Russia, 16th October 2015. This toolkit for doctors working in situations of conflicts and other emergencies has been developed for the WMA by the British Medical Association within the framework of the project Health Care in Danger (ICRC).
digital transformation of health systems and increasing digitalization of everyday life mean the availability and ubiquity of health-related information has increased rapidly and substantially over recent decades. So far, school health promotion has only partially tapped the potential and challenges of digital media. We therefore:
Background: Health apps are increasingly recognized as crucial tools for enhancing health care delivery. Many countries, particularly those in sub-Saharan Africa, can substantially benefit from using health apps to support self-management and thus help to achieve universal health coverage and the third sustainable development goal. However, most health apps published in app stores are of ...
His assignments included two tours of duty at the U.S. Embassy in Moscow, where he served as head of the political/internal unit and acting political counselor. Between tours in Moscow, he worked on Russian and Soviet affairs on the Policy Planning Staff of the Department of State and as a policy assistant in the Office of the Undersecretary of ...