Pragmatic Case Studies in Psychotherapy
PCSP is a peer reviewed, open-access journal and database. It provides innovative, quantitative and qualitative knowledge about psychotherapy process and outcome. PCSP is published by the National Register of Health Service Psychologists.
January, 2024 -- see our newest case, "The Commitment of a Lifetime": The Role of Emotionally Focused Couple Therapy in Strengthening Attachment Bonds and Improving Relationship Health in Later-Life Couples—The Teletherapy Case of "Alice" and "Steve."
Click on the upper left button for the “Newest Case" or the button labeled "Current." Click on "CE Exams On Case Studies" below for an Exam on the current issue's case study and on past issues' case studies.

The Case Studies
Autism spectrum, cognitive difficulties, medical conditions, obsessive compulsive, personality disorders, psychosis/schizophrenia, trauma/ptsd, specific features in case studies, methodology of case studies, approaches and theories in case studies, ce exams on case studies.
January 23, 2024 -- FROM THE EDITOR
ANNOUNCING THE PUBLICATION OF OUR 67th ISSUE (Vol. 20, Module 1)
"The Commitment of a Lifetime": The Role of Emotionally Focused Couple Therapy in Strengthening Attachment Bonds and Improving Relationship Health in Later-Life Couples --The Teletherapy Case of "Alice" and "Steve"
*** Drew Mendelson, Rutgers University-New Brunswick, NJ
Commentaries
*** Karen Skean and Elisabeth Brown, Rutgers University-New Brunswick, NJ
*** Shalonda Kelly, Rutgers University-New Brunswick, NJ
EDITOR'S NOTE
A healthy marriage is a crucial protective factor for adapting to the challenges of late life. Emotionally Focused Couple Therapy (EFCT) for couples is an attachment-based model of psychotherapy that emphasizes here-and-now processing of emotion in a safe holding environment; enhanced understanding of the patterned interactions between self and other; and a non-pathologizing, growth-oriented approach toward couples’ difficulties. This case study examines the benefits of EFCT for addressing issues specific to late life, including existential concerns such as aging, illness, and mortality; caregiving burdens and stress; cumulative relational trauma over the lifespan; and forgiveness and healing from emotional injuries. Specifically, this case study involves a 20-session, teletherapy treatment of a couple named “Alice” and “Steve,” aged 74 and 75, respectively, with Steve suffering from advanced Parkinson’s Disease. The couple presented with hopelessness and resentment about their caregiving situation, unresolved traumas from early childhood fueling their relationship’s sore spots, and unprocessed grief and fears concerning losses at the end stage of life. The EFCT-guided treatment focused on promoting transformational and corrective experiences of secure attachment bonding and was importantly successful in resolving their presenting problems.
*** For a Table of Contents and pdf links to the articles, click on the upper left button labeled "Newest Case" or the button labeled "Current."

- Request new password
- Create a new account
Doing Research in Counselling and Psychotherapy
Student resources, carrying out a systematic case study.
The key messages of this chapter are:
- case study analysis makes a distinctive contribution to the evidence base for counselling and psychotherapy
- case studies are ethically sensitive, so need to be carried out with care and sensitivity
- it is important to be aware of how different types of research question require different case study approaches.
The following sources are intended to help you to explore issues covered in the chapter in more depth.
Methodological issues and challenges associated with case study research
Flyvbjerg, B. (2006). Five misunderstandings about case-study research . Qualitative Inquiry, 12 , 219 – 245.
Essential reading – a highly influential paper that clarifies the value of case study methods
Fishman, D. B. (2005). Editor's Introduction to PCSP--From single case to database: a new method for enhancing psychotherapy practice. Pragmatic Case Studies in Psychotherapy, 1(1), 1 – 50.
The rationale for the pragmatic case study approach
Foster, L.H. (2010). A best kept secret: single-subject research design in counseling. Counseling Outcome Research and Evaluation, 1, 30 – 39
An accessible and informative introduction to n=1 single subject case study methodology
McLeod, J. (2013). Increasing the rigor of case study evidence in therapy research. Pragmatic Case Studies in Psychotherapy, 9 , 382 – 402
Explores further possibilities around the development of case study methodology
Different types of therapy case study
Bloch-Elkouby, S., Eubanks, C. F., Knopf, L., Gorman, B. S., & Muran, J. C. (2019). The difficult task of assessing and interpreting treatment deterioration: an evidence-based case study. Frontiers in Psychology , 10, 1180.
Systematic case study that combines qualitative and quantitative information to explore a theoretically-significant case of apparent client deterioration. Case was drawn from dataset of a larger study
Brezinka, V., Mailänder, V., & Walitza, S. (2020). Obsessive compulsive disorder in very young children–a case series from a specialized outpatient clinic. BMC Psychiatry , 20(1), 1 – 8.
Example of how a series of n=1 case studies can be used
Faber, J., & Lee, E. (2020). Cognitive-Behavioral Therapy for a refugee mother with depression and anxiety. Clinical Case Studies , 19(4), 239 – 257.
A hybrid theory-building/pragmatic case study that seeks to develop new understanding of therapy in situations of client-therapist cultural difference. Clinical Case Studies is a major source of case study evidence – this study is a typical example of the kind of work that it publishes
Gray, M.A. & Stiles, W.B. (2011). Employing a case study in building an Assimilation Theory account of Generalized Anxiety Disorder and its treatment with Cognitive-Behavioral Therapy. Pragmatic Case Studies in Psychotherapy , 7(4), 529 – 557
An example of a theory-building case study focused on the development of the assimilation model of change
Kramer, U. (2009). Between manualized treatments and principle-guided psychotherapy: illustration in the case of Caroline. Pragmatic Case Studies in Psychotherapy , 5(2), 45 – 51
A pragmatic case study that also seeks to address important theoretical issues associated with the use of exposure techniques in CBT
McLeod, J. (2013). Transactional Analysis psychotherapy with a woman suffering from Multiple Sclerosis: a systematic case study. Transactional Analysis Journal, 43 , 212 – 223.
A hybrid case study – mainly aims to develop a theory of therapy in long-term health conditions, but also includes elements of pragmatic, narrative and HSCED approaches. Good example of the use of the Client Change Interview in case study research
Powell, M.L. and Newgent, R.A. (2010) Improving the empirical credibility of cinematherapy: a single-subject interrupted time-series design. Counseling Outcome Research and Evaluation , 1, 40 – 49.
Example of a series of n=1 case studies
Stige, S. H., & Halvorsen, M. S. (2018). From cumulative strain to available resources: a narrative case study of the potential effects of new trauma exposure on recovery. Illness, Crisis & Loss , 26(4), 270 – 292.
A narrative case study based on client interviews
Kellett, S., & Stockton, D. (2021). Treatment of obsessive morbid jealousy with cognitive analytic therapy: a mixed-methods quasi-experimental case study. British Journal of Guidance & Counselling , 1 – 19.
Example of an n=1 case study of a single case. Useful demonstration of how this approach can be used to study non-behavioural therapy
Wendt, D. C., & Gone, J. P. (2016). Integrating professional and indigenous therapies: An urban American Indian narrative clinical case study. The Counseling Psychologist , 44(5), 695 – 729.
A narrative case study based on client interviews
Werbart, A., Annevall, A., & Hillblom, J. (2019). Successful and less successful psychotherapies compared: three therapists and their six contrasting cases. Frontiers in Psychology . DOI: 10.3389/fpsyg.2019.00816.
Combined narrative, theory-building and cross-case analysis, based on interviews with client and therapist dyads
Widdowson, M. (2012). TA treatment of depression: A hermeneutic single-case efficacy design study-case three: 'Tom'. International Journal of Transactional Analysis Research , 3(2), 15 – 27.
Example of an HSCED study that also includes elements of theory-building. Supplementary information on journal website includes full details of the Change Interview and judges’ case analyses. This open access journal has also published many other richly-described HSCED studies
Issues and possibilities associated with quasi-judicial methodology
Bohart, A.C., Tallman, K.L., Byock, G.and Mackrill, T. (2011). The “Research Jury” Method: The application of the jury trial model to evaluating the validity of descriptive and causal statements about psychotherapy process and outcome. Pragmatic Case Studies in Psychotherapy, 7 (1) ,101 – 144.
Miller, R.B. (2011). Real Clinical Trials (RCT) – Panels of Psychological Inquiry for Transforming anecdotal data into clinical facts and validated judgments: introduction to a pilot test with the Case of “Anna”. Pragmatic Case Studies in Psychotherapy, 7(1), 6 – 36.
Stephen, S. and Elliott, R. (2011). Developing the Adjudicated Case Study Method. Pragmatic Case Studies in Psychotherapy, 7(1), 230 – 224.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- March 15, 2024 | VOL. 77, NO. 1 CURRENT ISSUE pp.1-42
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Recovery in First-Episode Psychosis: A Case Study of Metacognitive Reflection and Insight Therapy (MERIT)
- Bethany L. Leonhardt , Psy.D. ,
- Kristen Ratliff , M.S. ,
- Jenifer L. Vohs , Ph.D.
Search for more papers by this author
Despite historically pessimistic views from both the professional community and lay public, research is emerging that recovery from psychosis is possible. Recovery has evolved to include not only a reduction in symptoms and return to functioning, but a sense of agency and connection to meaningful roles in life. The development of a more comprehensive conceptualization of recovery has particular importance in the treatment of first-episode psychosis, because early intervention may avoid some of the prolonged dysfunction that may make recovery difficult. As the mental health field moves to intervene early in the course of psychosis and to support recovery for individuals with severe mental illness, it is essential to develop and assess interventions that may promote a more comprehensive recovery. This case illustration offers an account of a type of integrative psychotherapy that may assist individuals in achieving recovery: metacognitive reflection and insight therapy (MERIT).
Despite early pessimism about the chronicity and course of schizophrenia spectrum disorders in psychiatry, there has been a shift in discussion in research, treatment, and policy suggesting that recovery from severe mental illness is possible. Various factors have contributed to this shift, including long-term outcomes studies that show a heterogeneous course for those with schizophrenia spectrum disorders ( 1 ), as well as a shift in the conceptualization of recovery in serious mental illness. Due to a grassroots movement of activists and scholars embracing a broadened view of recovery, recovery now includes a process of regaining autonomy over one’s life and a return to meaningful life roles, even in the face of persisting symptoms or difficulties ( 2 , 3 ). This aspect of recovery is called many things, including recovery as process and subjective recovery. Included in this definition of recovery is that individuals see themselves as more than a mental health patient, feel empowered to make decisions about their lives and health care, and can participate in aspects of their community that are meaningful to them ( 2 ).
This broadened view of recovery has several implications for interventions offered to individuals with schizophrenia spectrum disorders. In particular, with a recent emphasis on intervening early in the course of illness, or first-episode psychosis (FEP), a broadened view of recovery has implications for the types of interventions offered in FEP clinics. The literature to date has shown that early intervention in FEP is related to a range of improved outcomes ( 4 ), yet these outcomes are often more objectively defined, such as symptom remission, use of acute services, and level of functioning. While these outcomes are important, it remains unanswered how early intervention can assist individuals with FEP to attain subjective recovery.
One promising intervention that may assist in promoting recovery in FEP is metacognitive reflection and insight therapy (MERIT; 5 ). MERIT is an integrative psychotherapy that targets metacognition. Metacognition refers to a range of cognitive activities that allow one to form complex, flexible accounts of one’s own life, as well as of significant others, and to use this knowledge to respond to a range of psychosocial problems ( 6 ). Deficits in metacognition have been found to exist in schizophrenia spectrum disorders ( 7 , 8 ), to be stable ( 9 ), and to be present across all phases of illness, including FEP ( 10 ). Promoting metacognition may assist persons in moving toward subjective recovery because it may be necessary to think in a sophisticated way about oneself to obtain this type of recovery. For example, thinking flexibly and coherently about oneself may allow one to see oneself as more than a mental health patient, to identify a range of passions and life roles that would make one’s life fulfilling, and to be able to respond flexibly to psychosocial distress.
There is some evidence to suggest that higher metacognition is related to an improved sense of subjective recovery in those with schizophrenia spectrum disorders ( 11 ), and offering interventions such as MERIT that specifically target metacognition may assist in promoting recovery. In fact, in a sample of individuals with prolonged psychosis, metacognitively oriented psychotherapy was found to assist in forming a coherent sense of self and to ultimately promote recovery ( 12 ). Additionally, case studies have been reported examining the use of MERIT as an intervention to target and promote insight in FEP ( 13 , 14 ). The following case builds upon this work to illustrate the use of MERIT as an intervention promoting recovery in FEP.
Presenting Problem and Client Background
The client for this case will be referred to as Grohl. All identifying information has been altered to protect his confidentiality. Grohl is a single male in his early to mid-20s who was diagnosed as having schizophrenia two years prior to his engagement in therapy. He grew up as the eldest of three children in a middle-class family and reported no developmental concerns or delays. Grohl described himself as having many friends during his childhood and reported he was involved in extracurricular activities and performed well in school. Prior to his diagnosis of schizophrenia, he had no other mental health diagnoses or mental health treatment. He was a talented artist and was active in his high school’s art community. He and his parents noted a change after high school in which Grohl became less social and struggled academically in his college classes. Immediately after high school, Grohl relocated from living with his family of origin to living with his grandfather in a different city in the same state. He had limited contact with his family of origin during that time and began to experience a change in his level of psychosocial functioning: socially withdrawing, failing to keep jobs, and eventually dropping out of school. Grohl’s grandfather struggled with substance abuse during this time and was actively using substances while Grohl lived with him. Grohl and his parents reported that there were often verbal and physical fights as a result of Grohl’s grandfather’s substance use and overall this was a tumultuous time for Grohl. Grohl’s own substance use included occasional marijuana and alcohol in high school, and he reported drinking alcohol several times per week while living with his grandfather. He had legal charges related to an arrest for underage drinking.
During the onset of Grohl’s illness, he began to believe a range of persecutory delusions that often centered on his physical health, stating that others were poisoning him and noting strange physical sensations that he believed were a result of the poison he was administered. His grandfather took him to a behavioral health center where Grohl was diagnosed as having schizophrenia and an oral second-generation antipsychotic was prescribed, which he took intermittently. Grohl lived with his grandfather and occasionally sought medical assistance for physical sensations for one-and-a-half years before he visited emergency rooms in several states, attempting to convince hospital staff that he was being poisoned and requesting medical attention. Grohl would leave the emergency room before care could be administered. He was eventually detained by the police due to erratic behavior and was transferred to an inpatient hospital close to his parents’ residence. It was following this hospitalization that Grohl was linked to the early psychosis clinic. While on the inpatient unit, Grohl was involuntarily committed due to his refusal to take medications and his attempts to leave the unit against medical advice. He began receiving an injection of paliperidone palmitate. Grohl eventually moved to a supported living environment and attended an outpatient clinic, receiving case management and medication services for six months before agreeing to psychotherapy. He remained on a stable dose of his medications during the duration of the therapy presented below, and he received services from a multidisciplinary team, including case management and supported employment services. In addition, because of Grohl’s somatic complaints, he received care at several primary and specialty care clinics to evaluate his health. He received a diagnosis of gastroesophageal reflux disease and was treated for this condition. He received no other medical diagnoses.
When Grohl began therapy, he was primarily experiencing negative symptoms. He experienced thought blocking, prolonged response latency, anhedonia, and flat affect. He described that his mind was “empty” and noted that he spent much of his day lying in his bed. Grohl was unemployed at the time and saw his family once per week when his parents picked him up for a family Sunday dinner. He had no other social contact. He endorsed avolition, noting that despite being bored much of the time he was not motivated to engage in any behaviors that he used to find enjoyable, such as creating art, spending time in Internet forums, or spending time with his friends. Grohl was quiet, rarely made eye contact, and often came to his psychotherapy session appearing disheveled.
Case Conceptualization
Grohl’s deficits in metacognition were assessed with the Metacognition Assessment Scale-Abbreviated (MAS-A; 15 ), which is an adaptation of the original MAS ( 16 ) and includes four domains of metacognition: self-reflectivity, awareness of others, decentration, and mastery. Each part of the scale is hierarchical, with higher scores representing increased capacity to perform the complex mental tasks of each domain. Self-reflectivity refers to the ability to acknowledge and identify internal states and to ultimately form flexible understandings of oneself and one’s unique life events over time. Grohl initially had low self-reflectivity. Although he was able to distinguish a range of cognitive operations, he was unable to name a nuanced range of emotions or recognize that his thoughts were fallible, giving him a score of 3 out of 9 on the self-reflectivity scale. For example, Grohl remained convinced that he was being poisoned by an unnamed entity and remained adamant that he had holes in his head that were causing discomfort in his body. Awareness of others refers to the ability to consider other people’s internal states and to make guesses about their intentions. Grohl also scored low in this capacity. He recognized that others had their own internal states but was unable to name a range of emotions significant others in his life might experience and struggled to guess their intentions. He was evaluated at a 3 out of a possible score of 7 on this subscale of the MAS-A. Decentration refers to the ability to recognize that one is not the center of all activities and that other people have differing, valid opinions separate from one’s own. Grohl tended to view events as being connected to him, often believing that others wished him harm, and failed to consider that others in his life had lives outside of his. He scored 0 out of 3 on this scale. Finally, mastery refers to the ability to use knowledge about oneself to respond in increasingly complex ways to psychological problems. Grohl initially came to therapy without a clear psychological problem, often stating that something had gone wrong in his life but attributing that distress to the malicious, unnamed individuals who he believed were causing his physical sensations. Thus, his score on mastery was a 1.5 out of 9.0 because he did not meet the criteria of articulating a plausible psychological problem.
Course of Treatment
The therapy described below refers to an 18-month period of weekly individual psychotherapy utilizing MERIT. MERIT is an integrative psychotherapy with eight core elements incorporated into each session. These elements can be used along with a range of therapeutic approaches and offer therapists a method of building upon existing skills and conceptualizations and employing a flexible framework that centers on increasing the client’s metacognitive capacity ( 17 ). Each of these elements is briefly defined below, along with a description of how that element was addressed in Grohl’s psychotherapy.
Element 1: The Preeminent Role of the Client’s Agenda
This element refers to, first and foremost, establishing what the client wants from the session that day. Agendas are often not clearly articulated, and it is possible for clients to have multiple, and at times conflicting, agendas at once. For example, a client could wish that a therapist agree that he or she is a victim of a jealous neighbor or may want the therapist to view him or her as independent and capable. Attending to these agendas requires that therapists be curious about and attentive to the ways in which the client’s desires pull for a reaction in a session, whether it is to be viewed a certain way or for the therapist to take a certain action.
Initially, Grohl’s agenda appeared to be to convince the therapist that he did not have a mental illness and to get her to agree with his belief that others were causing his physical symptoms through attacks on him in his sleep. Grohl often was adversarial with his psychiatrist, asserting that he did not have schizophrenia and noting his anger at being forced to take medications he did not believe he needed. The therapist responded to these agendas with curiosity about Grohl’s physical symptoms and attempted to gather a timeline and narrative episodes surrounding the onset of these symptoms. When Grohl would directly ask the therapist to align with him against his psychiatrist by asking whether she agreed that he did not have schizophrenia but was the victim of a conspiracy, she responded by reflecting on the dynamics of Grohl’s agenda and with curiosity about what her agreement would mean to him. The therapist would then request more information about Grohl’s experience to better understand what he was experiencing. It seemed important to the therapist that she remain open to and curious about Grohl’s agenda rather than attempting to promote her own agenda (such as improving insight or adherence to treatment). The therapist’s openness seemed to allow Grohl to move at a pace with which he was comfortable, which ultimately seemed to promote trust and further exploration of Grohl’s life story. However, at times moving at Grohl’s pace was difficult, and often the treatment team would experience impatience or anxiety as Grohl continued to attempt to get body scans or other medical procedures to address his somatic experiences.
Element 2: Introduction of the Therapist’s Thoughts as Dialogue
This element refers to the therapist offering his or her own reflections and reactions throughout the session to promote dialogue. The therapist’s mental contents are fodder for reflection and not presented as fact or a more accurate view of reality but to encourage the client to react to the therapist’s reflections so the two can think together about them.
The therapist initially achieved this element with Grohl by stating her confusion about the claims he was asserting regarding his physical sensations. As Grohl provided more information and reflected upon the events surrounding the onset of these sensations, it occurred to the therapist that Grohl often experienced these strange sensations when he felt unsafe. He reported that the sensations began while living with his grandfather, who was unpredictable and often verbally and physically abusive to Grohl, including attacking him in his sleep. Since then, Grohl had moved into a supported living home with individuals with psychiatric needs in a neighborhood in the city that was known for being unsafe. Grohl often reported being most bothered by these physical symptoms when he was around others living in the home, and he reported that he did not experience these symptoms at his parents’ home. The therapist responded to Grohl by offering reflections such as “When you share these stories, it makes me wonder if you felt threatened,” and, “I have a thought that you felt unsafe staying with your grandfather.” The therapist would then invite Grohl to comment on her reflections.
Element 3: Eliciting Narrative Episodes
The third element of MERIT emphasizes the importance of eliciting narrative episodes to assist clients in developing a storied sense of their lives over time. This element was particularly important with Grohl and was challenging in the beginning due to his barren account of his life. Grohl described his life as being successful and positive until the physical sensations began, to which he attributed all his dissatisfaction with his current circumstances. The therapist elicited narratives by asking for more details about the onset of his physical symptoms and attempting to gather information about where he was living and with whom he was interacting. Eventually, she began to compile a timeline of Grohl’s life. He often responded to the therapist’s inquiries by stating that he could not remember his life. By revisiting the few narratives he could offer, Grohl eventually was able to provide more details to these narratives and slowly, narratives of other times arose. A richer picture of his life emerged, including his account of the abuse he endured while living with his grandfather, his sense of having failed at becoming an independent adult, his social discomfort in high school, and his remembering of his love and dedication to art. With this richer picture of his life, Grohl’s account of having experienced a perfect life prior to the onset of physical symptoms was challenged and evolved into a rich, storied sense of his unique life, including his challenges and triumphs. This richer version of Grohl’s life often caused him pain and discomfort, as he grappled with a sense of loss of dreams he previously had for himself and struggled with acceptance of painful interactions with significant others. Likewise, this process was difficult at times for the therapist as she watched Grohl struggle with painful aspects of his life and continued to encourage him to reflect and explore potentially distressing narratives. Despite the discomfort that often accompanied the increased reflectivity, Grohl appeared better able to make sense of his life. Exploring narratives seemed to allow Grohl to finally come to terms with experiencing psychiatric difficulties as well as to see himself as a full being and not only a psychiatric patient.
Element 4: The Psychological Problem
The fourth element refers to assisting clients in forming a plausible, mutually agreed upon psychological problem. The psychological problem often emerges from the understanding of the client’s agenda and narratives and may include a range of difficulties not restricted to a mental disorder. Examples of these difficulties could include struggling to connect with others in an adaptive manner or difficulty in understanding the intentions of others and thus navigating interactions.
Initially, Grohl struggled to form a plausible psychological problem and focused on implausible explanations for the distress he was experiencing. He often stated that others were poisoning him or performing operations on him while he was sleeping, leaving no trace of surgical scars when he woke. These expressions often left the therapist in a difficult position, because she could not join Grohl in these explanations of his difficulties. However, through exploration of the development of these physical sensations and the narratives he offered, Grohl began to articulate a psychological problem that something had gone wrong in his life and that he had gotten off track. He considered factors that could have influenced the course of his life, expanding these factors from his suspicions of others to include his decreased self-esteem caused by perceived failures, such as of losing jobs, dropping out of college, and new difficulties in connecting with others. Grohl’s understanding of his psychological problem continued to evolve as he discussed various narrative episodes in his life and considered what had changed. He began to acknowledge difficulties occurring earlier in his life and in particular reflected on the impact of his grandfather’s abuse. He described themes of feeling unsafe, struggling to perceive the intentions of others, and feeling left behind in life, as his peers and siblings established their autonomy in young adulthood in ways in which Grohl felt he should but was unable.
Element 5: Reflecting on Interpersonal Processes
This element requires attention to and reflection on the interpersonal dynamics occurring within the therapy sessions by both the therapist and client. This element was difficult with Grohl, who would struggle to describe his reactions to the therapist. He seemed initially unsure of the therapist and her intentions and would state that he was not sure what to talk about during the sessions. Grohl often noted surprise at having talked through the entire session.
Another significant interpersonal process in Grohl’s psychotherapy was seen in his attempts to convince his therapist that he did not have a mental illness and should not have to be in treatment. At times he would experience the therapist’s curiosity as challenging the legitimacy of what he was experiencing and would offer statements attempting to legitimize his experiences, such as “This isn’t all in my head” and “There is something seriously wrong with my body, and I’m afraid I’m going to die.” At times he perceived his therapist as being on his side and would attempt to recruit her help in procuring a body scan that would “prove” the damage he was sure was happening to his body. The therapist described her experience during these moments as feeling pulled in different directions by Grohl, and she would invite him to reflect on how he perceived her during these moments as well and to react to her reflections.
Element 6: Reflecting on the Process of Therapy Within and Across Sessions
In practicing element 6, the therapist invites feedback from the client on how the session has gone each time as well as to reflect on the therapy process as a whole. In MERIT, the process of therapy is viewed as an opportunity for reflection and dialogue about the connection between two individuals over time and how this connection can evolve. Initially, Grohl described that sessions went well but also noted his discomfort in knowing what to talk about. As he reflected on more of his life and developed a conceptualization of his psychological problem, Grohl would describe that he was thinking about his life differently as a result of therapy. He noted that these reflections were at times painful, particularly when describing memories of his earliest experiences of psychosis and traumatic interactions with his grandfather. The therapist would often observe a change in Grohl in the sessions following exploration of his relationship with his grandfather. Specifically, Grohl tended to describe his grandfather in an overwhelmingly positive manner in the sessions following his disclosure of painful moments with him. The therapist would note this change between sessions and explore with Grohl his ambivalence about his relationship with his grandfather and about discussing and reflecting on painful moments in his life.
Element 7: Stimulating Reflectivity of Self and Others
One of the hallmarks of MERIT is the stimulation of reflective activity at the appropriate level of metacognition. This stimulation requires the therapist to continuously assess clients’ current level of metacognitive capacity to reflect on the internal states of themselves and others. The therapist then offers interventions at that level or attempts to assist them to the next highest level through scaffolding. Offering interventions that are either too metacognitively complex or simple is viewed as ineffective as the client is being asked to reflect at a level that does not match his or her current capacity. Of note, metacognitive capacity is dynamic and changes between sessions and often even within sessions ( 18 ), so to effectively perform this element, therapists must frequently assess the client’s metacognitive capacity.
In this case, the therapist first needed to intervene to provide a scaffold for Grohl to express a range of nuanced emotions, as Grohl could describe a range of cognitive operations but could not identify how he was feeling in various narratives. The therapist performed this intervention by inviting Grohl to describe the circumstances around the beginning of his physical symptoms. This encouragement led him to describe narrative episodes that, while initially barren, gave some material for Grohl and the therapist to reflect upon. The therapist would stimulate self-reflectivity by asking Grohl to describe his reactions to events in these narratives and the various feelings within his body during those moments. The therapist would offer labels for emotions and at times would describe her own guesses about how she might feel if she were experiencing the narrative Grohl described, exploring how those guesses fit or did not fit for Grohl, fine-tuning his understanding of how he was feeling. During the exploration of these initial barren narratives, Grohl began offering narratives from earlier periods in his life, and more details emerged, particularly his complicated and traumatic interactions with his grandfather. As Grohl developed his ability to reflect on a range of emotions, the therapist also began to scaffold the fallibility of thoughts, assisting Grohl in exploring how his thoughts had changed over time. He was most able to do this when thinking about events in the past, and he struggled to recognize that his current thoughts were also fallible. To address this, the therapist would invite Grohl to reflect on his certainty within the moment and how that differed from times in the past when his thoughts had changed. Ultimately, as Grohl began reflecting on his life in more detail and began to integrate the circumstances of significant points of his life, he developed a more complex understanding of himself and the psychosocial events he had experienced.
When Grohl began to offer narrative episodes that included significant others in his life, the therapist targeted his ability to understand the internal states of other people. Grohl initially struggled to recognize a range of nuanced emotion in others. As he developed the capacity to describe his own nuanced emotional states, he began to consider the emotional states of others. When Grohl considered his family dynamics, the therapist would often stimulate reflectivity of others by asking Grohl how he thought his parents viewed or reacted to significant events. He began to articulate, and form guesses about how certain events, such as the onset of his illness, had affected others in his family. As Grohl considered the impact his relationship with his grandfather had upon him, he was receptive to interventions that invited him to reflect upon aspects of his grandfather’s life that may have influenced his grandfather’s behavior. Grohl began to think flexibly about an individual who had caused him much pain and developed some hypotheses about what may have influenced his grandfather’s behavior.
Element 8: Stimulating Psychological Mastery
The eighth and final element of MERIT requires the therapist to offer interventions to stimulate metacognitive mastery, or the use of knowledge of self and others to respond to psychological distress. Similar to stimulating reflectivity of self and others at the correct metacognitive level, mastery interventions also must be tailored to the metacognitive capacity of the client. Stimulation of mastery includes assisting clients to form a plausible psychological problem and then to develop increasingly complex ways to master the problem. Interventions become more complex as they include the knowledge gained in reflection about self and others to navigate difficulties in life.
For Grohl, the therapist first began to stimulate mastery by offering interventions to promote reflectivity about what his plausible psychological problem might be. As discussed in the fourth element, Grohl initially struggled to articulate a problem that was plausible, but through exploration of the onset of his physical problems, he was eventually able to describe that his life had gotten off track and to acknowledge his difficulty in assessing others’ intentions and interacting successfully. As Grohl became more reflective of significant moments in his past, he began to describe the fulfillment he found while creating art. He began to create again and engaged this part of himself, eventually even agreeing to do contracted pieces of art as he had in the past. Being paid to create caused Grohl great anxiety initially, as he wondered whether he would perform to his past abilities and feared he might disappoint those who were paying him. However, he was successful with his first few pieces, and this success improved his self-esteem and sense of agency over aspects of his life.
As Grohl began to gain self-confidence and continued to reflect on the change he noticed in his life’s trajectory, his explanation of his psychological problem again evolved. He began to describe narratives he had previously not mentioned and acknowledged experiencing psychotic symptoms, which he had formerly denied. What emerged was a more complex understanding of the unique life circumstances that had led him to experience a high level of stress and a sense of being lost. He reflected on his history of being anxious as a child and as a rebellious teenager, and he noted how he had often overcompensated for his insecurity by acting out while in high school. Grohl abandoned the narrative that he had previously stated, that all was perfect in his life prior to his physical sensations and described a childhood of uncertainty that included moments of strength and happiness. Describing the moments of happiness led him to conclude that it was important to connect more with his family of origin and with the passions he had, including art.
Clinical Outcomes
Significantly, Grohl appears to have made gains in his personal recovery. At the beginning of therapy, he was unemployed and isolated, and much of his focus (including interactions with his family) was on his physical experiences. Within two years of starting therapy, Grohl’s life looked considerably different. He has been employed for 18 months at one job and recently added a second job. He has reconnected with his family members and sees them several times every week. He has reestablished an old friendship and begun two new ones. He engages with his community by creating murals for the church he attends and taking other offers to generate art. Additionally, he lives independently in an apartment, has bought a car, has gotten a pet, and has other accomplishments that seem to illustrate a dynamic life. As Anthony ( 19 ) points out, the meaning of recovery for each individual is deeply personal, and thus Grohl’s own subjective sense of recovery is the best marker for whether or not he is in recovery from his severe mental illness. Grohl describes in therapy sessions that he has an improved quality of life, expressing that while he still feels anxious and unsure about taking chances on his future, he feels more fulfilled with his current life than he did two years ago. He articulates an improved sense of self-esteem and appears to experience himself as an agent, even making decisions about his mental health care and how and when he will engage in it. He seems to rely less on his parents to make decisions for him, although he considers their advice. Grohl is actively pursuing higher education opportunities and has been reflecting on what type of career he would like. He is planning to start college within the next year.
Thus, while this case has results similar to other case studies using MERIT for patients with FEP, such as an increase in insight and decrease in symptoms ( 14 ), Grohl’s case also illustrates the movement from being dominated by a mental health condition to living a more fulfilling and enriched life in recovery. While this case occurred within clinical practice and thus other contributing and confounding factors cannot be ruled out, it seems likely that the use of MERIT promoted Grohl’s recovery. We posit that MERIT promotes recovery for two reasons: first, each of its elements supports the core values of recovery, and second, metacognitive capacity may be necessary to achieve many of the subjective elements of recovery.
By starting with the first of these two assertions, that the eight elements of MERIT support the tenets of recovery, we see that elements 1, 4, 5, 6, 7, and 8 all position the client as an agent with an agenda, a mind for dialogue, and an active participant in care, thus encouraging self-direction. Element 1, or the preeminent role of the client’s agenda, places importance on understanding what the client wants in a given moment, creating a therapeutic environment with multiple pathways to recovery, tailored to what is important to the individual and allowing for self-direction. MERIT promotes an open stance, in which the therapist does not operate as an expert but rather as a consultant, serving as a guide to explore the content of one’s own mind. The MERIT therapist does not merely mirror the client, but in addition to providing reflections of the client’s mind, actively offers his or her own thoughts to discuss and react to within the therapy encounter (elements 2 and 5). MERIT also supports recovery through the therapist’s interest in the client’s story and life before and after illness, helping the client recapture a sense of self rather than just focusing on symptom relief or eradication of unhealthy thoughts and behaviors (element 3). Thus, all eight elements of MERIT support the core values of recovery.
Turning to the second assertion, MERIT may assist persons in the types of sense-making that are necessary to achieve subjective recovery. For example, having a storied sense of one’s life as having good moments as well as challenges aligns with the recovery tenets of seeing oneself as more than a mental health patient, feeling empowered to make decisions about one’s life, and ultimately recapturing a sense of self. By contrast, having significant metacognitive deficits may make achieving subjective elements of recovery difficult if one is struggling to identify one’s own hopes and dreams and to understand and respond to psychological challenges. Thus, it may be that by promoting metacognitive capacity through the eight elements of MERIT, therapists are able to assist clients in forming flexible, coherent understandings of themselves, others, and their unique challenges in life and begin to respond to them.
Significantly, Grohl made gains on each of the four metacognition subscales. Grohl began to describe and recognize a range of nuanced emotions; began to view his thoughts as fallible and thus changeable; believed that his expectations were not always reality; and began to integrate his thoughts, feelings, and behaviors when thinking about specific narrative episodes of his life. Thus, Grohl moved from a 3 to a 6.5 on self-reflectivity. He also began to see other people as having rich internal experiences and began to make guesses about their intentions using unique information about them, thus moving from a 3 to a 5 on awareness of others. Grohl initially scored a 0 on decentration, as he thought all others were somehow tied to a conspiracy against him. He developed a different view, however, and was able to see others as having their own lives separate from him, and he even began to consider that other people have valid but differing opinions from him, placing him at 1.5 on the scale. Finally, Grohl developed a plausible psychological problem and began to use behavioral strategies, such as engaging in artistic endeavors, to manage his distress, moving him from a 1.5 to a 5 on the mastery scale.
Although case studies provide in-depth examinations of an individual’s experience, they have limitations. The findings from this case study may not be generalizable to other individuals. More work is needed with individuals of differing demographic characteristics and phases of illness to assess the generalizability of these findings. Additionally, other factors external to Grohl’s psychotherapy may have had an impact on his ability to recover, including other services he received, such as medication management and supported employment services. Despite these limitations and given the larger body of literature and the findings of this case, MERIT appears to be a promising intervention that may help promote recovery for patients with FEP.
The authors report no financial relationships with commercial interests.
1 Harding CM, Brooks GW, Ashikaga T, et al. : The Vermont longitudinal study of persons with severe mental illness, I: methodology, study sample, and overall status 32 years later . Am J Psychiatry 1987 ; 144:718–726 Crossref , Medline , Google Scholar
2 Davidson L, Roe D : Recovery from versus recovery in serious mental illness: one strategy for lessening confusion plaguing recovery . J Mental Health 2007 ; 16:459–470 Crossref , Google Scholar
3 Silverstein SM, Bellack AS : A scientific agenda for the concept of recovery as it applies to schizophrenia . Clin Psychol Rev 2008 ; 28:1108–1124 Crossref , Medline , Google Scholar
4 Dixon LB, Goldman HH, Bennett ME, et al. : Implementing coordinated specialty care for early psychosis: the RAISE Connection Program . Psychiatr Serv 2015 ; 66:691–698 Crossref , Medline , Google Scholar
5 Van Donkersgoed RJM, De Jong S, Van der Gaag M, et al. : A manual-based individual therapy to improve metacognition in schizophrenia: protocol of a multi-center RCT . BMC Psychiatry 2014 ; 14:27–45 Crossref , Medline , Google Scholar
6 Lysaker PH, Vohs JL, Ballard R, et al. : Metacognition, self-reflection and recovery in schizophrenia . Future Neurol 2013 ; 8:103–115 Crossref , Google Scholar
7 Hasson-Ohayon I, Avidan-Msika M, Mashiach-Eizenberg M, et al. : Metacognitive and social cognition approaches to understanding the impact of schizophrenia on social quality of life . Schizophr Res 2015 ; 161:386–391 Crossref , Medline , Google Scholar
8 Lysaker PH, Leonhardt BL, Brüne M, et al. : Capacities for theory of mind, metacognition, and neurocognitive function are independently related to emotional recognition in schizophrenia . Psychiatry Res 2014 ; 219:79–85 Crossref , Medline , Google Scholar
9 Hamm JA, Renard SB, Fogley RL, et al. : Metacognition and social cognition in schizophrenia: stability and relationship to concurrent and prospective symptom assessments . J Clin Psychol 2012 ; 68:1303–1312 Crossref , Medline , Google Scholar
10 Vohs JL, Lysaker PH, Francis MM, et al. : Metacognition, social cognition, and symptoms in patients with first episode and prolonged psychoses . Schizophr Res 2014 ; 153:54–59 Crossref , Medline , Google Scholar
11 Kukla M, Lysaker PH, Salyers MP : Do persons with schizophrenia who have better metacognitive capacity also have a stronger subjective experience of recovery? Psychiatry Res 2013 ; 209:381–385 Crossref , Medline , Google Scholar
12 Bargenquast R, Schweitzer RD : Enhancing sense of recovery and self-reflectivity in people with schizophrenia: a pilot study of Metacognitive Narrative Psychotherapy . Psychol Psychother 2014 ; 87:338–356 Crossref , Medline , Google Scholar
13 Hillis JD, Leonhardt BL, Vohs JL, et al. : Metacognitive reflective and insight therapy for people in early phase of a schizophrenia spectrum disorder . J Clin Psychol 2015 ; 71:125–135 Crossref , Medline , Google Scholar
14 Leonhardt BL, Benson K, George S, et al. : Targeting insight in first episode psychosis: a case study of metacognitive reflective insight therapy (MERIT) . J Contemp Psychother 2016 ; 46:207–216 Crossref , Google Scholar
15 Lysaker PH, Leonhardt BL, Pijnenborg M, et al. : Metacognition in schizophrenia spectrum disorders: methods of assessment and associations with neurocognition, symptoms, cognitive style and function . Isr J Psychiatry Relat Sci 2014 ; 51:54–61 Medline , Google Scholar
16 Semerari A, Carcione A, Dimaggio G, et al. : How to evaluate metacognitive function in psychotherapy? The metacognition assessment scale and its applications . Clin Psychol Psychother 2003 ; 10:238–261 Crossref , Google Scholar
17 Lysaker PH, Buck KD, Leonhardt B, et al. : Metacognitively focused psychotherapy for persons with schizophrenia: eight core elements that define practice ; in Metacognition and Social Cognition in Schizophrenia . Edited by Lysaker PH, Dimaggio G, Brune M . New York, Elsevier, 2014 Crossref , Google Scholar
18 Lysaker PH, Buck KD, Ringer JM : The recovery of metacognitive capacity in schizophrenia across 32 months of individual psychotherapy: a case study . Psychother Res 2007 ; 17:713–720 Crossref , Google Scholar
19 Anthony WA : Recovery from mental illness: the guiding vision of the mental health service system in the 1990s . Psychosoc Rehabil J 1993 ; 16:11–23 Crossref , Google Scholar
- Metacognitive Reflection and Insight Therapy (MERIT) Delivered Virtually During the COVID-19 Pandemic: An Illustration of Two Cases 10 August 2022 | Journal of Contemporary Psychotherapy, Vol. 53, No. 1
- Metacognitive Reflection and Insight Therapy with a Patient with Low Medication Adherence: The Interplay Between Personal, Functional and Clinical Recovery 13 September 2022 | Journal of Contemporary Psychotherapy, Vol. 53, No. 1
- A Guide for the Implementation of Group-Based Metacognitive Reflection and Insight Therapy (MERITg) 16 September 2022 | Journal of Contemporary Psychotherapy, Vol. 53, No. 1
- Recovery-Focused Metacognitive Interpersonal Therapy (MIT) for Adolescents with First-Episode Psychosis 22 September 2022 | Journal of Contemporary Psychotherapy, Vol. 53, No. 1
- The Phenomenological Perspective and Metacognitive Psychotherapy in Addressing Psychosis 26 April 2023
- Addressing Schizotypy in Metacognitive Reflection and Insight Therapy 10 October 2023
- The Recovery Process for Individuals With Schizophrenia in the Context of Evidence-Based Psychotherapy and Rehabilitation European Psychologist, Vol. 26, No. 2
- Trauma and Personal Recovery in Serious Mental Illness: A Case Report of Integrative Psychotherapy 19 February 2020 | Journal of Psychosocial Rehabilitation and Mental Health, Vol. 7, No. 1
- Metacognitive function and fragmentation in schizophrenia: Relationship to cognition, self-experience and developing treatments Schizophrenia Research: Cognition, Vol. 19
- <p>Metacognitive Reflection and Insight Therapy: A Recovery-Oriented Treatment Approach for Psychosis</p> 1 April 2020 | Psychology Research and Behavior Management, Vol. Volume 13
- Metacognitive deficits and social functioning in schizophrenia across symptom profiles: A latent class analysis 27 March 2019 | Journal of Experimental Psychopathology, Vol. 10, No. 1
- Jay A. Hamm , Psy.D. , and
- Paul H. Lysaker , Ph.D.
- Promoting recovery from severe mental illness: Implications from research on metacognition and metacognitive reflection and insight therapy World Journal of Psychiatry, Vol. 8, No. 1
- Psychotherapy, Psychosis
- Schizophrenia Spectrum
- Metacognition
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
Case Study Research Method in Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, Ph.D., is a qualified psychology teacher with over 18 years experience of working in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews).
The case study research method originated in clinical medicine (the case history, i.e., the patient’s personal history). In psychology, case studies are often confined to the study of a particular individual.
The information is mainly biographical and relates to events in the individual’s past (i.e., retrospective), as well as to significant events that are currently occurring in his or her everyday life.
The case study is not a research method, but researchers select methods of data collection and analysis that will generate material suitable for case studies.
Freud (1909a, 1909b) conducted very detailed investigations into the private lives of his patients in an attempt to both understand and help them overcome their illnesses.
This makes it clear that the case study is a method that should only be used by a psychologist, therapist, or psychiatrist, i.e., someone with a professional qualification.
There is an ethical issue of competence. Only someone qualified to diagnose and treat a person can conduct a formal case study relating to atypical (i.e., abnormal) behavior or atypical development.
Famous Case Studies
- Anna O – One of the most famous case studies, documenting psychoanalyst Josef Breuer’s treatment of “Anna O” (real name Bertha Pappenheim) for hysteria in the late 1800s using early psychoanalytic theory.
- Little Hans – A child psychoanalysis case study published by Sigmund Freud in 1909 analyzing his five-year-old patient Herbert Graf’s house phobia as related to the Oedipus complex.
- Bruce/Brenda – Gender identity case of the boy (Bruce) whose botched circumcision led psychologist John Money to advise gender reassignment and raise him as a girl (Brenda) in the 1960s.
- Genie Wiley – Linguistics/psychological development case of the victim of extreme isolation abuse who was studied in 1970s California for effects of early language deprivation on acquiring speech later in life.
- Phineas Gage – One of the most famous neuropsychology case studies analyzes personality changes in railroad worker Phineas Gage after an 1848 brain injury involving a tamping iron piercing his skull.
Clinical Case Studies
- Studying the effectiveness of psychotherapy approaches with an individual patient
- Assessing and treating mental illnesses like depression, anxiety disorders, PTSD
- Neuropsychological cases investigating brain injuries or disorders
Child Psychology Case Studies
- Studying psychological development from birth through adolescence
- Cases of learning disabilities, autism spectrum disorders, ADHD
- Effects of trauma, abuse, deprivation on development
Types of Case Studies
- Explanatory case studies : Used to explore causation in order to find underlying principles. Helpful for doing qualitative analysis to explain presumed causal links.
- Exploratory case studies : Used to explore situations where an intervention being evaluated has no clear set of outcomes. It helps define questions and hypotheses for future research.
- Descriptive case studies : Describe an intervention or phenomenon and the real-life context in which it occurred. It is helpful for illustrating certain topics within an evaluation.
- Multiple-case studies : Used to explore differences between cases and replicate findings across cases. Helpful for comparing and contrasting specific cases.
- Intrinsic : Used to gain a better understanding of a particular case. Helpful for capturing the complexity of a single case.
- Collective : Used to explore a general phenomenon using multiple case studies. Helpful for jointly studying a group of cases in order to inquire into the phenomenon.
Where Do You Find Data for a Case Study?
There are several places to find data for a case study. The key is to gather data from multiple sources to get a complete picture of the case and corroborate facts or findings through triangulation of evidence. Most of this information is likely qualitative (i.e., verbal description rather than measurement), but the psychologist might also collect numerical data.
1. Primary sources
- Interviews – Interviewing key people related to the case to get their perspectives and insights. The interview is an extremely effective procedure for obtaining information about an individual, and it may be used to collect comments from the person’s friends, parents, employer, workmates, and others who have a good knowledge of the person, as well as to obtain facts from the person him or herself.
- Observations – Observing behaviors, interactions, processes, etc., related to the case as they unfold in real-time.
- Documents & Records – Reviewing private documents, diaries, public records, correspondence, meeting minutes, etc., relevant to the case.
2. Secondary sources
- News/Media – News coverage of events related to the case study.
- Academic articles – Journal articles, dissertations etc. that discuss the case.
- Government reports – Official data and records related to the case context.
- Books/films – Books, documentaries or films discussing the case.
3. Archival records
Searching historical archives, museum collections and databases to find relevant documents, visual/audio records related to the case history and context.
Public archives like newspapers, organizational records, photographic collections could all include potentially relevant pieces of information to shed light on attitudes, cultural perspectives, common practices and historical contexts related to psychology.
4. Organizational records
Organizational records offer the advantage of often having large datasets collected over time that can reveal or confirm psychological insights.
Of course, privacy and ethical concerns regarding confidential data must be navigated carefully.
However, with proper protocols, organizational records can provide invaluable context and empirical depth to qualitative case studies exploring the intersection of psychology and organizations.
- Organizational/industrial psychology research : Organizational records like employee surveys, turnover/retention data, policies, incident reports etc. may provide insight into topics like job satisfaction, workplace culture and dynamics, leadership issues, employee behaviors etc.
- Clinical psychology : Therapists/hospitals may grant access to anonymized medical records to study aspects like assessments, diagnoses, treatment plans etc. This could shed light on clinical practices.
- School psychology : Studies could utilize anonymized student records like test scores, grades, disciplinary issues, and counseling referrals to study child development, learning barriers, effectiveness of support programs, and more.
How do I Write a Case Study in Psychology?
Follow specified case study guidelines provided by a journal or your psychology tutor. General components of clinical case studies include: background, symptoms, assessments, diagnosis, treatment, and outcomes. Interpreting the information means the researcher decides what to include or leave out. A good case study should always clarify which information is the factual description and which is an inference or the researcher’s opinion.
1. Introduction
- Provide background on the case context and why it is of interest, presenting background information like demographics, relevant history, and presenting problem.
- Compare briefly to similar published cases if applicable. Clearly state the focus/importance of the case.
2. Case Presentation
- Describe the presenting problem in detail, including symptoms, duration,and impact on daily life.
- Include client demographics like age and gender, information about social relationships, and mental health history.
- Describe all physical, emotional, and/or sensory symptoms reported by the client.
- Use patient quotes to describe the initial complaint verbatim. Follow with full-sentence summaries of relevant history details gathered, including key components that led to a working diagnosis.
- Summarize clinical exam results, namely orthopedic/neurological tests, imaging, lab tests, etc. Note actual results rather than subjective conclusions. Provide images if clearly reproducible/anonymized.
- Clearly state the working diagnosis or clinical impression before transitioning to management.
3. Management and Outcome
- Indicate the total duration of care and number of treatments given over what timeframe. Use specific names/descriptions for any therapies/interventions applied.
- Present the results of the intervention,including any quantitative or qualitative data collected.
- For outcomes, utilize visual analog scales for pain, medication usage logs, etc., if possible. Include patient self-reports of improvement/worsening of symptoms. Note the reason for discharge/end of care.
4. Discussion
- Analyze the case, exploring contributing factors, limitations of the study, and connections to existing research.
- Analyze the effectiveness of the intervention,considering factors like participant adherence, limitations of the study, and potential alternative explanations for the results.
- Identify any questions raised in the case analysis and relate insights to established theories and current research if applicable. Avoid definitive claims about physiological explanations.
- Offer clinical implications, and suggest future research directions.
5. Additional Items
- Thank specific assistants for writing support only. No patient acknowledgments.
- References should directly support any key claims or quotes included.
- Use tables/figures/images only if substantially informative. Include permissions and legends/explanatory notes.
- Provides detailed (rich qualitative) information.
- Provides insight for further research.
- Permitting investigation of otherwise impractical (or unethical) situations.
Case studies allow a researcher to investigate a topic in far more detail than might be possible if they were trying to deal with a large number of research participants (nomothetic approach) with the aim of ‘averaging’.
Because of their in-depth, multi-sided approach, case studies often shed light on aspects of human thinking and behavior that would be unethical or impractical to study in other ways.
Research that only looks into the measurable aspects of human behavior is not likely to give us insights into the subjective dimension of experience, which is important to psychoanalytic and humanistic psychologists.
Case studies are often used in exploratory research. They can help us generate new ideas (that might be tested by other methods). They are an important way of illustrating theories and can help show how different aspects of a person’s life are related to each other.
The method is, therefore, important for psychologists who adopt a holistic point of view (i.e., humanistic psychologists ).
Limitations
- Lacking scientific rigor and providing little basis for generalization of results to the wider population.
- Researchers’ own subjective feelings may influence the case study (researcher bias).
- Difficult to replicate.
- Time-consuming and expensive.
- The volume of data, together with the time restrictions in place, impacted the depth of analysis that was possible within the available resources.
Because a case study deals with only one person/event/group, we can never be sure if the case study investigated is representative of the wider body of “similar” instances. This means the conclusions drawn from a particular case may not be transferable to other settings.
Because case studies are based on the analysis of qualitative (i.e., descriptive) data , a lot depends on the psychologist’s interpretation of the information she has acquired.
This means that there is a lot of scope for Anna O , and it could be that the subjective opinions of the psychologist intrude in the assessment of what the data means.
For example, Freud has been criticized for producing case studies in which the information was sometimes distorted to fit particular behavioral theories (e.g., Little Hans ).
This is also true of Money’s interpretation of the Bruce/Brenda case study (Diamond, 1997) when he ignored evidence that went against his theory.
Breuer, J., & Freud, S. (1895). Studies on hysteria . Standard Edition 2: London.
Curtiss, S. (1981). Genie: The case of a modern wild child .
Diamond, M., & Sigmundson, K. (1997). Sex Reassignment at Birth: Long-term Review and Clinical Implications. Archives of Pediatrics & Adolescent Medicine , 151(3), 298-304
Freud, S. (1909a). Analysis of a phobia of a five year old boy. In The Pelican Freud Library (1977), Vol 8, Case Histories 1, pages 169-306
Freud, S. (1909b). Bemerkungen über einen Fall von Zwangsneurose (Der “Rattenmann”). Jb. psychoanal. psychopathol. Forsch ., I, p. 357-421; GW, VII, p. 379-463; Notes upon a case of obsessional neurosis, SE , 10: 151-318.
Harlow J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39 , 389–393.
Harlow, J. M. (1868). Recovery from the Passage of an Iron Bar through the Head . Publications of the Massachusetts Medical Society. 2 (3), 327-347.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Further Information
- Case Study Approach
- Case Study Method
- Enhancing the Quality of Case Studies in Health Services Research
- “We do things together” A case study of “couplehood” in dementia
- Using mixed methods for evaluating an integrative approach to cancer care: a case study
Psychology: Research and Review
- Open access
- Published: 19 March 2021
Appraising psychotherapy case studies in practice-based evidence: introducing Case Study Evaluation-tool (CaSE)
- Greta Kaluzeviciute ORCID: orcid.org/0000-0003-1197-177X 1
Psicologia: Reflexão e Crítica volume 34 , Article number: 9 ( 2021 ) Cite this article
7109 Accesses
3 Citations
5 Altmetric
Metrics details
Systematic case studies are often placed at the low end of evidence-based practice (EBP) due to lack of critical appraisal. This paper seeks to attend to this research gap by introducing a novel Case Study Evaluation-tool (CaSE). First, issues around knowledge generation and validity are assessed in both EBP and practice-based evidence (PBE) paradigms. Although systematic case studies are more aligned with PBE paradigm, the paper argues for a complimentary, third way approach between the two paradigms and their ‘exemplary’ methodologies: case studies and randomised controlled trials (RCTs). Second, the paper argues that all forms of research can produce ‘valid evidence’ but the validity itself needs to be assessed against each specific research method and purpose. Existing appraisal tools for qualitative research (JBI, CASP, ETQS) are shown to have limited relevance for the appraisal of systematic case studies through a comparative tool assessment. Third, the paper develops purpose-oriented evaluation criteria for systematic case studies through CaSE Checklist for Essential Components in Systematic Case Studies and CaSE Purpose-based Evaluative Framework for Systematic Case Studies. The checklist approach aids reviewers in assessing the presence or absence of essential case study components (internal validity). The framework approach aims to assess the effectiveness of each case against its set out research objectives and aims (external validity), based on different systematic case study purposes in psychotherapy. Finally, the paper demonstrates the application of the tool with a case example and notes further research trajectories for the development of CaSE tool.
Introduction
Due to growing demands of evidence-based practice, standardised research assessment and appraisal tools have become common in healthcare and clinical treatment (Hannes, Lockwood, & Pearson, 2010 ; Hartling, Chisholm, Thomson, & Dryden, 2012 ; Katrak, Bialocerkowski, Massy-Westropp, Kumar, & Grimmer, 2004 ). This allows researchers to critically appraise research findings on the basis of their validity, results, and usefulness (Hill & Spittlehouse, 2003 ). Despite the upsurge of critical appraisal in qualitative research (Williams, Boylan, & Nunan, 2019 ), there are no assessment or appraisal tools designed for psychotherapy case studies.
Although not without controversies (Michels, 2000 ), case studies remain central to the investigation of psychotherapy processes (Midgley, 2006 ; Willemsen, Della Rosa, & Kegerreis, 2017 ). This is particularly true of systematic case studies, the most common form of case study in contemporary psychotherapy research (Davison & Lazarus, 2007 ; McLeod & Elliott, 2011 ).
Unlike the classic clinical case study, systematic cases usually involve a team of researchers, who gather data from multiple different sources (e.g., questionnaires, observations by the therapist, interviews, statistical findings, clinical assessment, etc.), and involve a rigorous data triangulation process to assess whether the data from different sources converge (McLeod, 2010 ). Since systematic case studies are methodologically pluralistic, they have a greater interest in situating patients within the study of a broader population than clinical case studies (Iwakabe & Gazzola, 2009 ). Systematic case studies are considered to be an accessible method for developing research evidence-base in psychotherapy (Widdowson, 2011 ), especially since they correct some of the methodological limitations (e.g. lack of ‘third party’ perspectives and bias in data analysis) inherent to classic clinical case studies (Iwakabe & Gazzola, 2009 ). They have been used for the purposes of clinical training (Tuckett, 2008 ), outcome assessment (Hilliard, 1993 ), development of clinical techniques (Almond, 2004 ) and meta-analysis of qualitative findings (Timulak, 2009 ). All these developments signal a revived interest in the case study method, but also point to the obvious lack of a research assessment tool suitable for case studies in psychotherapy (Table 1 ).
To attend to this research gap, this paper first reviews issues around the conceptualisation of validity within the paradigms of evidence-based practice (EBP) and practice-based evidence (PBE). Although case studies are often positioned at the low end of EBP (Aveline, 2005 ), the paper suggests that systematic cases are a valuable form of evidence, capable of complimenting large-scale studies such as randomised controlled trials (RCTs). However, there remains a difficulty in assessing the quality and relevance of case study findings to broader psychotherapy research.
As a way forward, the paper introduces a novel Case Study Evaluation-tool (CaSE) in the form of CaSE Purpose - based Evaluative Framework for Systematic Case Studies and CaSE Checklist for Essential Components in Systematic Case Studies . The long-term development of CaSE would contribute to psychotherapy research and practice in three ways.
Given the significance of methodological pluralism and diverse research aims in systematic case studies, CaSE will not seek to prescribe explicit case study writing guidelines, which has already been done by numerous authors (McLeod, 2010 ; Meganck, Inslegers, Krivzov, & Notaerts, 2017 ; Willemsen et al., 2017 ). Instead, CaSE will enable the retrospective assessment of systematic case study findings and their relevance (or lack thereof) to broader psychotherapy research and practice. However, there is no reason to assume that CaSE cannot be used prospectively (i.e. producing systematic case studies in accordance to CaSE evaluative framework, as per point 3 in Table 2 ).
The development of a research assessment or appraisal tool is a lengthy, ongoing process (Long & Godfrey, 2004 ). It is particularly challenging to develop a comprehensive purpose - oriented evaluative framework, suitable for the assessment of diverse methodologies, aims and outcomes. As such, this paper should be treated as an introduction to the broader development of CaSE tool. It will introduce the rationale behind CaSE and lay out its main approach to evidence and evaluation, with further development in mind. A case example from the Single Case Archive (SCA) ( https://singlecasearchive.com ) will be used to demonstrate the application of the tool ‘in action’. The paper notes further research trajectories and discusses some of the limitations around the use of the tool.
Separating the wheat from the chaff: what is and is not evidence in psychotherapy (and who gets to decide?)
The common approach: evidence-based practice.
In the last two decades, psychotherapy has become increasingly centred around the idea of an evidence-based practice (EBP). Initially introduced in medicine, EBP has been defined as ‘conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients’ (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996 ). EBP revolves around efficacy research: it seeks to examine whether a specific intervention has a causal (in this case, measurable) effect on clinical populations (Barkham & Mellor-Clark, 2003 ). From a conceptual standpoint, Sackett and colleagues defined EBP as a paradigm that is inclusive of many methodologies, so long as they contribute towards clinical decision-making process and accumulation of best currently available evidence in any given set of circumstances (Gabbay & le May, 2011 ). Similarly, the American Psychological Association (APA, 2010 ) has recently issued calls for evidence-based systematic case studies in order to produce standardised measures for evaluating process and outcome data across different therapeutic modalities.
However, given EBP’s focus on establishing cause-and-effect relationships (Rosqvist, Thomas, & Truax, 2011 ), it is unsurprising that qualitative research is generally not considered to be ‘gold standard’ or ‘efficacious’ within this paradigm (Aveline, 2005 ; Cartwright & Hardie, 2012 ; Edwards, 2013 ; Edwards, Dattilio, & Bromley, 2004 ; Longhofer, Floersch, & Hartmann, 2017 ). Qualitative methods like systematic case studies maintain an appreciation for context, complexity and meaning making. Therefore, instead of measuring regularly occurring causal relations (as in quantitative studies), the focus is on studying complex social phenomena (e.g. relationships, events, experiences, feelings, etc.) (Erickson, 2012 ; Maxwell, 2004 ). Edwards ( 2013 ) points out that, although context-based research in systematic case studies is the bedrock of psychotherapy theory and practice, it has also become shrouded by an unfortunate ideological description: ‘anecdotal’ case studies (i.e. unscientific narratives lacking evidence, as opposed to ‘gold standard’ evidence, a term often used to describe the RCT method and the therapeutic modalities supported by it), leading to a further need for advocacy in and defence of the unique epistemic process involved in case study research (Fishman, Messer, Edwards, & Dattilio, 2017 ).
The EBP paradigm prioritises the quantitative approach to causality, most notably through its focus on high generalisability and the ability to deal with bias through randomisation process. These conditions are associated with randomised controlled trials (RCTs) but are limited (or, as some argue, impossible) in qualitative research methods such as the case study (Margison et al., 2000 ) (Table 3 ).
‘Evidence’ from an EBP standpoint hovers over the epistemological assumption of procedural objectivity : knowledge can be generated in a standardised, non-erroneous way, thus producing objective (i.e. with minimised bias) data. This can be achieved by anyone, as long as they are able to perform the methodological procedure (e.g. RCT) appropriately, in a ‘clearly defined and accepted process that assists with knowledge production’ (Douglas, 2004 , p. 131). If there is a well-outlined quantitative form for knowledge production, the same outcome should be achieved regardless of who processes or interprets the information. For example, researchers using Cochrane Review assess the strength of evidence using meticulously controlled and scrupulous techniques; in turn, this minimises individual judgment and creates unanimity of outcomes across different groups of people (Gabbay & le May, 2011 ). The typical process of knowledge generation (through employing RCTs and procedural objectivity) in EBP is demonstrated in Fig. 1 .
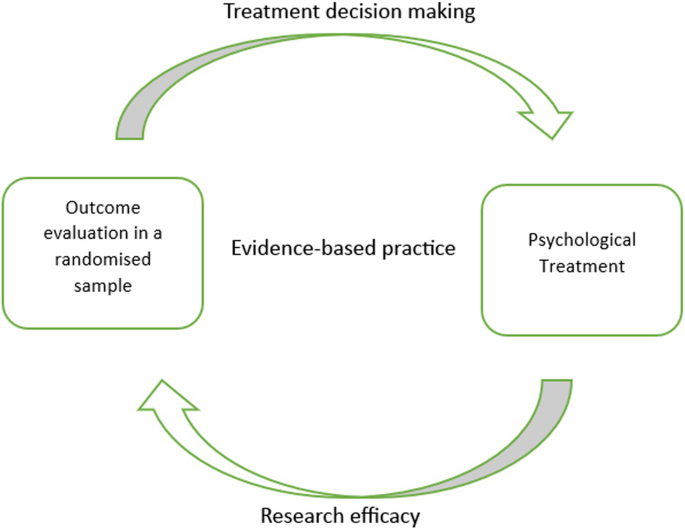
Typical knowledge generation process in evidence–based practice (EBP)
In EBP, the concept of validity remains somewhat controversial, with many critics stating that it limits rather than strengthens knowledge generation (Berg, 2019 ; Berg & Slaattelid, 2017 ; Lilienfeld, Ritschel, Lynn, Cautin, & Latzman, 2013 ). This is because efficacy research relies on internal validity . At a general level, this concept refers to the congruence between the research study and the research findings (i.e. the research findings were not influenced by anything external to the study, such as confounding variables, methodological errors and bias); at a more specific level, internal validity determines the extent to which a study establishes a reliable causal relationship between an independent variable (e.g. treatment) and independent variable (outcome or effect) (Margison et al., 2000 ). This approach to validity is demonstrated in Fig. 2 .
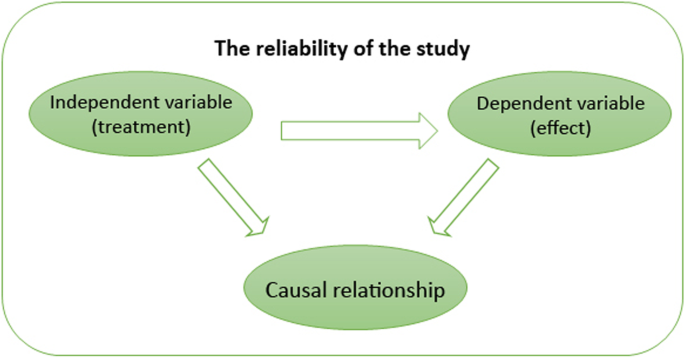
Internal validity
Social scientists have argued that there is a trade-off between research rigour and generalisability: the more specific the sample and the more rigorously defined the intervention, the outcome is likely to be less applicable to everyday, routine practice. As such, there remains a tension between employing procedural objectivity which increases the rigour of research outcomes and applying such outcomes to routine psychotherapy practice where scientific standards of evidence are not uniform.
According to McLeod ( 2002 ), inability to address questions that are most relevant for practitioners contributed to a deepening research–practice divide in psychotherapy. Studies investigating how practitioners make clinical decisions and the kinds of evidence they refer to show that there is a strong preference for knowledge that is not generated procedurally, i.e. knowledge that encompasses concrete clinical situations, experiences and techniques. A study by Stewart and Chambless ( 2007 ) sought to assess how a larger population of clinicians (under APA, from varying clinical schools of thought and independent practices, sample size 591) make treatment decisions in private practice. The study found that large-scale statistical data was not the primary source of information sought by clinicians. The most important influences were identified as past clinical experiences and clinical expertise ( M = 5.62). Treatment materials based on clinical case observations and theory ( M = 4.72) were used almost as frequently as psychotherapy outcome research findings ( M = 4.80) (i.e. evidence-based research). These numbers are likely to fluctuate across different forms of psychotherapy; however, they are indicative of the need for research about routine clinical settings that does not isolate or generalise the effect of an intervention but examines the variations in psychotherapy processes.
The alternative approach: practice-based evidence
In an attempt to dissolve or lessen the research–practice divide, an alternative paradigm of practice-based evidence (PBE) has been suggested (Barkham & Mellor-Clark, 2003 ; Fox, 2003 ; Green & Latchford, 2012 ; Iwakabe & Gazzola, 2009 ; Laska, Motulsky, Wertz, Morrow, & Ponterotto, 2014 ; Margison et al., 2000 ). PBE represents a shift in how we think about evidence and knowledge generation in psychotherapy. PBE treats research as a local and contingent process (at least initially), which means it focuses on variations (e.g. in patient symptoms) and complexities (e.g. of clinical setting) in the studied phenomena (Fox, 2003 ). Moreover, research and theory-building are seen as complementary rather than detached activities from clinical practice. That is to say, PBE seeks to examine how and which treatments can be improved in everyday clinical practice by flagging up clinically salient issues and developing clinical techniques (Barkham & Mellor-Clark, 2003 ). For this reason, PBE is concerned with the effectiveness of research findings: it evaluates how well interventions work in real-world settings (Rosqvist et al., 2011 ). Therefore, although it is not unlikely for RCTs to be used in order to generate practice-informed evidence (Horn & Gassaway, 2007 ), qualitative methods like the systematic case study are seen as ideal for demonstrating the effectiveness of therapeutic interventions with individual patients (van Hennik, 2020 ) (Table 4 ).
PBE’s epistemological approach to ‘evidence’ may be understood through the process of concordant objectivity (Douglas, 2004 ): ‘Instead of seeking to eliminate individual judgment, … [concordant objectivity] checks to see whether the individual judgments of people in fact do agree’ (p. 462). This does not mean that anyone can contribute to the evaluation process like in procedural objectivity, where the main criterion is following a set quantitative protocol or knowing how to operate a specific research design. Concordant objectivity requires that there is a set of competent observers who are closely familiar with the studied phenomenon (e.g. researchers and practitioners who are familiar with depression from a variety of therapeutic approaches).
Systematic case studies are a good example of PBE ‘in action’: they allow for the examination of detailed unfolding of events in psychotherapy practice, making it the most pragmatic and practice-oriented form of psychotherapy research (Fishman, 1999 , 2005 ). Furthermore, systematic case studies approach evidence and results through concordant objectivity (Douglas, 2004 ) by involving a team of researchers and rigorous data triangulation processes (McLeod, 2010 ). This means that, although systematic case studies remain focused on particular clinical situations and detailed subjective experiences (similar to classic clinical case studies; see Iwakabe & Gazzola, 2009 ), they still involve a series of validity checks and considerations on how findings from a single systematic case pertain to broader psychotherapy research (Fishman, 2005 ). The typical process of knowledge generation (through employing systematic case studies and concordant objectivity) in PBE is demonstrated in Fig. 3 . The figure exemplifies a bidirectional approach to research and practice, which includes the development of research-supported psychological treatments (through systematic reviews of existing evidence) as well as the perspectives of clinical practitioners in the research process (through the study of local and contingent patient and/or treatment processes) (Teachman et al., 2012 ; Westen, Novotny, & Thompson-Brenner, 2004 ).
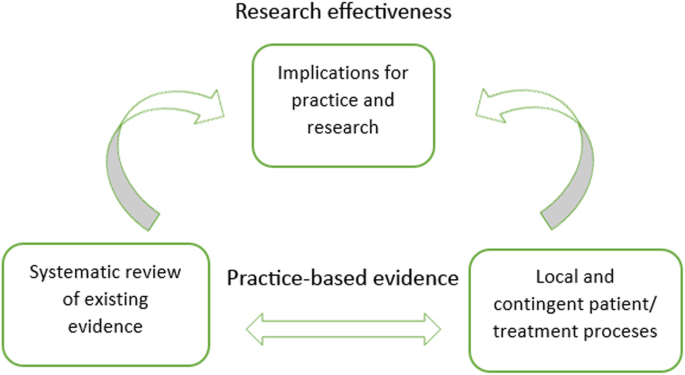
Typical knowledge generation process in practice-based evidence (PBE)
From a PBE standpoint, external validity is a desirable research condition: it measures extent to which the impact of interventions apply to real patients and therapists in everyday clinical settings. As such, external validity is not based on the strength of causal relationships between treatment interventions and outcomes (as in internal validity); instead, the use of specific therapeutic techniques and problem-solving decisions are considered to be important for generalising findings onto routine clinical practice (even if the findings are explicated from a single case study; see Aveline, 2005 ). This approach to validity is demonstrated in Fig. 4 .
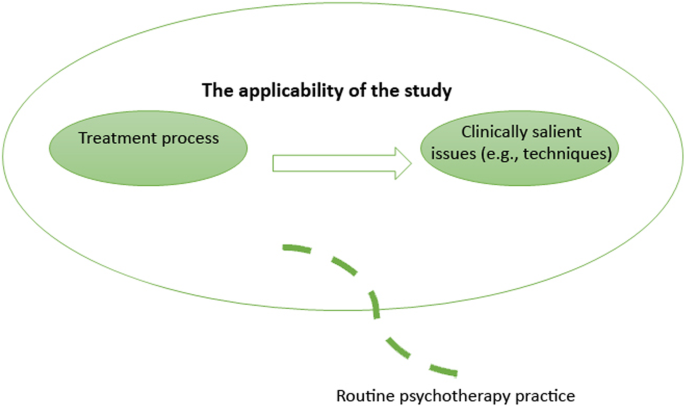
External validity
Since effectiveness research is less focused on limiting the context of the studied phenomenon (indeed, explicating the context is often one of the research aims), there is more potential for confounding factors (e.g. bias and uncontrolled variables) which in turn can reduce the study’s internal validity (Barkham & Mellor-Clark, 2003 ). This is also an important challenge for research appraisal. Douglas ( 2004 ) argues that appraising research in terms of its effectiveness may produce significant disagreements or group illusions, since what might work for some practitioners may not work for others: ‘It cannot guarantee that values are not influencing or supplanting reasoning; the observers may have shared values that cause them to all disregard important aspects of an event’ (Douglas, 2004 , p. 462). Douglas further proposes that an interactive approach to objectivity may be employed as a more complex process in debating the evidential quality of a research study: it requires a discussion among observers and evaluators in the form of peer-review, scientific discourse, as well as research appraisal tools and instruments. While these processes of rigour are also applied in EBP, there appears to be much more space for debate, disagreement and interpretation in PBE’s approach to research evaluation, partly because the evaluation criteria themselves are subject of methodological debate and are often employed in different ways by researchers (Williams et al., 2019 ). This issue will be addressed more explicitly again in relation to CaSE development (‘Developing purpose-oriented evaluation criteria for systematic case studies’ section).
A third way approach to validity and evidence
The research–practice divide shows us that there may be something significant in establishing complementarity between EBP and PBE rather than treating them as mutually exclusive forms of research (Fishman et al., 2017 ). For one, EBP is not a sufficient condition for delivering research relevant to practice settings (Bower, 2003 ). While RCTs can demonstrate that an intervention works on average in a group, clinicians who are facing individual patients need to answer a different question: how can I make therapy work with this particular case ? (Cartwright & Hardie, 2012 ). Systematic case studies are ideal for filling this gap: they contain descriptions of microprocesses (e.g. patient symptoms, therapeutic relationships, therapist attitudes) in psychotherapy practice that are often overlooked in large-scale RCTs (Iwakabe & Gazzola, 2009 ). In particular, systematic case studies describing the use of specific interventions with less researched psychological conditions (e.g. childhood depression or complex post-traumatic stress disorder) can deepen practitioners’ understanding of effective clinical techniques before the results of large-scale outcome studies are disseminated.
Secondly, establishing a working relationship between systematic case studies and RCTs will contribute towards a more pragmatic understanding of validity in psychotherapy research. Indeed, the very tension and so-called trade-off between internal and external validity is based on the assumption that research methods are designed on an either/or basis; either they provide a sufficiently rigorous study design or they produce findings that can be applied to real-life practice. Jimenez-Buedo and Miller ( 2010 ) call this assumption into question: in their view, if a study is not internally valid, then ‘little, or rather nothing, can be said of the outside world’ (p. 302). In this sense, internal validity may be seen as a pre-requisite for any form of applied research and its external validity, but it need not be constrained to the quantitative approach of causality. For example, Levitt, Motulsky, Wertz, Morrow, and Ponterotto ( 2017 ) argue that, what is typically conceptualised as internal validity, is, in fact, a much broader construct, involving the assessment of how the research method (whether qualitative or quantitative) is best suited for the research goal, and whether it obtains the relevant conclusions. Similarly, Truijens, Cornelis, Desmet, and De Smet ( 2019 ) suggest that we should think about validity in a broader epistemic sense—not just in terms of psychometric measures, but also in terms of the research design, procedure, goals (research questions), approaches to inquiry (paradigms, epistemological assumptions), etc.
The overarching argument from research cited above is that all forms of research—qualitative and quantitative—can produce ‘valid evidence’ but the validity itself needs to be assessed against each specific research method and purpose. For example, RCTs are accompanied with a variety of clearly outlined appraisal tools and instruments such as CASP (Critical Appraisal Skills Programme) that are well suited for the assessment of RCT validity and their implications for EBP. Systematic case studies (or case studies more generally) currently have no appraisal tools in any discipline. The next section evaluates whether existing qualitative research appraisal tools are relevant for systematic case studies in psychotherapy and specifies the missing evaluative criteria.
The relevance of existing appraisal tools for qualitative research to systematic case studies in psychotherapy
What is a research tool.
Currently, there are several research appraisal tools, checklists and frameworks for qualitative studies. It is important to note that tools, checklists and frameworks are not equivalent to one another but actually refer to different approaches to appraising the validity of a research study. As such, it is erroneous to assume that all forms of qualitative appraisal feature the same aims and methods (Hannes et al., 2010 ; Williams et al., 2019 ).
Generally, research assessment falls into two categories: checklists and frameworks . Checklist approaches are often contrasted with quantitative research, since the focus is on assessing the internal validity of research (i.e. researcher’s independence from the study). This involves the assessment of bias in sampling, participant recruitment, data collection and analysis. Framework approaches to research appraisal, on the other hand, revolve around traditional qualitative concepts such as transparency, reflexivity, dependability and transferability (Williams et al., 2019 ). Framework approaches to appraisal are often challenging to use because they depend on the reviewer’s familiarisation and interpretation of the qualitative concepts.
Because of these different approaches, there is some ambiguity in terminology, particularly between research appraisal instruments and research appraisal tools . These terms are often used interchangeably in appraisal literature (Williams et al., 2019 ). In this paper, research appraisal tool is defined as a method-specific (i.e. it identifies a specific research method or component) form of appraisal that draws from both checklist and framework approaches. Furthermore, a research appraisal tool seeks to inform decision making in EBP or PBE paradigms and provides explicit definitions of the tool’s evaluative framework (thus minimising—but by no means eliminating—the reviewers’ interpretation of the tool). This definition will be applied to CaSE (Table 5 ).
In contrast, research appraisal instruments are generally seen as a broader form of appraisal in the sense that they may evaluate a variety of methods (i.e. they are non-method specific or they do not target a particular research component), and are aimed at checking whether the research findings and/or the study design contain specific elements (e.g. the aims of research, the rationale behind design methodology, participant recruitment strategies, etc.).
There is often an implicit difference in audience between appraisal tools and instruments. Research appraisal instruments are often aimed at researchers who want to assess the strength of their study; however, the process of appraisal may not be made explicit in the study itself (besides mentioning that the tool was used to appraise the study). Research appraisal tools are aimed at researchers who wish to explicitly demonstrate the evidential quality of the study to the readers (which is particularly common in RCTs). All forms of appraisal used in the comparative exercise below are defined as ‘tools’, even though they have different appraisal approaches and aims.
Comparing different qualitative tools
Hannes et al. ( 2010 ) identified CASP (Critical Appraisal Skills Programme-tool), JBI (Joanna Briggs Institute-tool) and ETQS (Evaluation Tool for Qualitative Studies) as the most frequently used critical appraisal tools by qualitative researchers. All three instruments are available online and are free of charge, which means that any researcher or reviewer can readily utilise CASP, JBI or ETQS evaluative frameworks to their research. Furthermore, all three instruments were developed within the context of organisational, institutional or consortium support (Tables 6 , 7 and 8 ).
It is important to note that neither of the three tools is specific to systematic case studies or psychotherapy case studies (which would include not only systematic but also experimental and clinical cases). This means that using CASP, JBI or ETQS for case study appraisal may come at a cost of overlooking elements and components specific to the systematic case study method.
Based on Hannes et al. ( 2010 ) comparative study of qualitative appraisal tools as well as the different evaluation criteria explicated in CASP, JBI and ETQS evaluative frameworks, I assessed how well each of the three tools is attuned to the methodological , clinical and theoretical aspects of systematic case studies in psychotherapy. The latter components were based on case study guidelines featured in the journal of Pragmatic Case Studies in Psychotherapy as well as components commonly used by published systematic case studies across a variety of other psychotherapy journals (e.g. Psychotherapy Research , Research In Psychotherapy : Psychopathology Process And Outcome , etc.) (see Table 9 for detailed descriptions of each component).
The evaluation criteria for each tool in Table 9 follows Joanna Briggs Institute (JBI) ( 2017a , 2017b ); Critical Appraisal Skills Programme (CASP) ( 2018 ); and ETQS Questionnaire (first published in 2004 but revised continuously since). Table 10 demonstrates how each tool should be used (i.e. recommended reviewer responses to checklists and questionnaires).
Using CASP, JBI and ETQS for systematic case study appraisal
Although JBI, CASP and ETQS were all developed to appraise qualitative research, it is evident from the above comparison that there are significant differences between the three tools. For example, JBI and ETQS are well suited to assess researcher’s interpretations (Hannes et al. ( 2010 ) defined this as interpretive validity , a subcategory of internal validity ): the researcher’s ability to portray, understand and reflect on the research participants’ experiences, thoughts, viewpoints and intentions. JBI has an explicit requirement for participant voices to be clearly represented, whereas ETQS involves a set of questions about key characteristics of events, persons, times and settings that are relevant to the study. Furthermore, both JBI and ETQS seek to assess the researcher’s influence on the research, with ETQS particularly focusing on the evaluation of reflexivity (the researcher’s personal influence on the interpretation and collection of data). These elements are absent or addressed to a lesser extent in the CASP tool.
The appraisal of transferability of findings (what this paper previously referred to as external validity ) is addressed only by ETQS and CASP. Both tools have detailed questions about the value of research to practice and policy as well as its transferability to other populations and settings. Methodological research aspects are also extensively addressed by CASP and ETQS, but less so by JBI (which relies predominantly on congruity between research methodology and objectives without any particular assessment criteria for other data sources and/or data collection methods). Finally, the evaluation of theoretical aspects (referred to by Hannes et al. ( 2010 ) as theoretical validity ) is addressed only by JBI and ETQS; there are no assessment criteria for theoretical framework in CASP.
Given these differences, it is unsurprising that CASP, JBI and ETQS have limited relevance for systematic case studies in psychotherapy. First, it is evident that neither of the three tools has specific evaluative criteria for the clinical component of systematic case studies. Although JBI and ETQS feature some relevant questions about participants and their context, the conceptualisation of patients (and/or clients) in psychotherapy involves other kinds of data elements (e.g. diagnostic tools and questionnaires as well as therapist observations) that go beyond the usual participant data. Furthermore, much of the clinical data is intertwined with the therapist’s clinical decision-making and thinking style (Kaluzeviciute & Willemsen, 2020 ). As such, there is a need to appraise patient data and therapist interpretations not only on a separate basis, but also as two forms of knowledge that are deeply intertwined in the case narrative.
Secondly, since systematic case studies involve various forms of data, there is a need to appraise how these data converge (or how different methods complement one another in the case context) and how they can be transferred or applied in broader psychotherapy research and practice. These systematic case study components are attended to a degree by CASP (which is particularly attentive of methodological components) and ETQS (particularly specific criteria for research transferability onto policy and practice). These components are not addressed or less explicitly addressed by JBI. Overall, neither of the tools is attuned to all methodological, theoretical and clinical components of the systematic case study. Specifically, there are no clear evaluation criteria for the description of research teams (i.e. different data analysts and/or clinicians); the suitability of the systematic case study method; the description of patient’s clinical assessment; the use of other methods or data sources; the general data about therapeutic progress.
Finally, there is something to be said about the recommended reviewer responses (Table 10 ). Systematic case studies can vary significantly in their formulation and purpose. The methodological, theoretical and clinical components outlined in Table 9 follow guidelines made by case study journals; however, these are recommendations, not ‘set in stone’ case templates. For this reason, the straightforward checklist approaches adopted by JBI and CASP may be difficult to use for case study researchers and those reviewing case study research. The ETQS open-ended questionnaire approach suggested by Long and Godfrey ( 2004 ) enables a comprehensive, detailed and purpose-oriented assessment, suitable for the evaluation of systematic case studies. That said, there remains a challenge of ensuring that there is less space for the interpretation of evaluative criteria (Williams et al., 2019 ). The combination of checklist and framework approaches would, therefore, provide a more stable appraisal process across different reviewers.
Developing purpose-oriented evaluation criteria for systematic case studies
The starting point in developing evaluation criteria for Case Study Evaluation-tool (CaSE) is addressing the significance of pluralism in systematic case studies. Unlike RCTs, systematic case studies are pluralistic in the sense that they employ divergent practices in methodological procedures ( research process ), and they may include significantly different research aims and purpose ( the end - goal ) (Kaluzeviciute & Willemsen, 2020 ). While some systematic case studies will have an explicit intention to conceptualise and situate a single patient’s experiences and symptoms within a broader clinical population, others will focus on the exploration of phenomena as they emerge from the data. It is therefore important that CaSE is positioned within a purpose - oriented evaluative framework , suitable for the assessment of what each systematic case is good for (rather than determining an absolute measure of ‘good’ and ‘bad’ systematic case studies). This approach to evidence and appraisal is in line with the PBE paradigm. PBE emphasises the study of clinical complexities and variations through local and contingent settings (e.g. single case studies) and promotes methodological pluralism (Barkham & Mellor-Clark, 2003 ).
CaSE checklist for essential components in systematic case studies
In order to conceptualise purpose-oriented appraisal questions, we must first look at what unites and differentiates systematic case studies in psychotherapy. The commonly used theoretical, clinical and methodological systematic case study components were identified earlier in Table 9 . These components will be seen as essential and common to most systematic case studies in CaSE evaluative criteria. If these essential components are missing in a systematic case study, then it may be implied there is a lack of information, which in turn diminishes the evidential quality of the case. As such, the checklist serves as a tool for checking whether a case study is, indeed, systematic (as opposed to experimental or clinical; see Iwakabe & Gazzola, 2009 for further differentiation between methodologically distinct case study types) and should be used before CaSE Purpose - based Evaluative Framework for Systematic Case Studie s (which is designed for the appraisal of different purposes common to systematic case studies).
As noted earlier in the paper, checklist approaches to appraisal are useful when evaluating the presence or absence of specific information in a research study. This approach can be used to appraise essential components in systematic case studies, as shown below. From a pragmatic point view (Levitt et al., 2017 ; Truijens et al., 2019 ), CaSE Checklist for Essential Components in Systematic Case Studies can be seen as a way to ensure the internal validity of systematic case study: the reviewer is assessing whether sufficient information is provided about the case design, procedure, approaches to inquiry, etc., and whether they are relevant to the researcher’s objectives and conclusions (Table 11 ).
CaSE purpose-based evaluative framework for systematic case studies
Identifying differences between systematic case studies means identifying the different purposes systematic case studies have in psychotherapy. Based on the earlier work by social scientist Yin ( 1984 , 1993 ), we can differentiate between exploratory (hypothesis generating, indicating a beginning phase of research), descriptive (particularising case data as it emerges) and representative (a case that is typical of a broader clinical population, referred to as the ‘explanatory case’ by Yin) cases.
Another increasingly significant strand of systematic case studies is transferable (aggregating and transferring case study findings) cases. These cases are based on the process of meta-synthesis (Iwakabe & Gazzola, 2009 ): by examining processes and outcomes in many different case studies dealing with similar clinical issues, researchers can identify common themes and inferences. In this way, single case studies that have relatively little impact on clinical practice, research or health care policy (in the sense that they capture psychotherapy processes rather than produce generalisable claims as in Yin’s representative case studies) can contribute to the generation of a wider knowledge base in psychotherapy (Iwakabe, 2003 , 2005 ). However, there is an ongoing issue of assessing the evidential quality of such transferable cases. According to Duncan and Sparks ( 2020 ), although meta-synthesis and meta-analysis are considered to be ‘gold standard’ for assessing interventions across disparate studies in psychotherapy, they often contain case studies with significant research limitations, inappropriate interpretations and insufficient information. It is therefore important to have a research appraisal process in place for selecting transferable case studies.
Two other types of systematic case study research include: critical (testing and/or confirming existing theories) cases, which are described as an excellent method for falsifying existing theoretical concepts and testing whether therapeutic interventions work in practice with concrete patients (Kaluzeviciute, 2021 ), and unique (going beyond the ‘typical’ cases and demonstrating deviations) cases (Merriam, 1998 ). These two systematic case study types are often seen as less valuable for psychotherapy research given that unique/falsificatory findings are difficult to generalise. But it is clear that practitioners and researchers in our field seek out context-specific data, as well as detailed information on the effectiveness of therapeutic techniques in single cases (Stiles, 2007 ) (Table 12 ).
Each purpose-based case study contributes to PBE in different ways. Representative cases provide qualitatively rich, in-depth data about a clinical phenomenon within its particular context. This offers other clinicians and researchers access to a ‘closed world’ (Mackrill & Iwakabe, 2013 ) containing a wide range of attributes about a conceptual type (e.g. clinical condition or therapeutic technique). Descriptive cases generally seek to demonstrate a realistic snapshot of therapeutic processes, including complex dynamics in therapeutic relationships, and instances of therapeutic failure (Maggio, Molgora, & Oasi, 2019 ). Data in descriptive cases should be presented in a transparent manner (e.g. if there are issues in standardising patient responses to a self-report questionnaire, this should be made explicit). Descriptive cases are commonly used in psychotherapy training and supervision. Unique cases are relevant for both clinicians and researchers: they often contain novel treatment approaches and/or introduce new diagnostic considerations about patients who deviate from the clinical population. Critical cases demonstrate the application of psychological theories ‘in action’ with particular patients; as such, they are relevant to clinicians, researchers and policymakers (Mackrill & Iwakabe, 2013 ). Exploratory cases bring new insight and observations into clinical practice and research. This is particularly useful when comparing (or introducing) different clinical approaches and techniques (Trad & Raine, 1994 ). Findings from exploratory cases often include future research suggestions. Finally, transferable cases provide one solution to the generalisation issue in psychotherapy research through the previously mentioned process of meta-synthesis. Grouped together, transferable cases can contribute to theory building and development, as well as higher levels of abstraction about a chosen area of psychotherapy research (Iwakabe & Gazzola, 2009 ).
With this plurality in mind, it is evident that CaSE has a challenging task of appraising research components that are distinct across six different types of purpose-based systematic case studies. The purpose-specific evaluative criteria in Table 13 was developed in close consultation with epistemological literature associated with each type of case study, including: Yin’s ( 1984 , 1993 ) work on establishing the typicality of representative cases; Duncan and Sparks’ ( 2020 ) and Iwakabe and Gazzola’s ( 2009 ) case selection criteria for meta-synthesis and meta-analysis; Stake’s ( 1995 , 2010 ) research on particularising case narratives; Merriam’s ( 1998 ) guidelines on distinctive attributes of unique case studies; Kennedy’s ( 1979 ) epistemological rules for generalising from case studies; Mahrer’s ( 1988 ) discovery oriented case study approach; and Edelson’s ( 1986 ) guidelines for rigorous hypothesis generation in case studies.
Research on epistemic issues in case writing (Kaluzeviciute, 2021 ) and different forms of scientific thinking in psychoanalytic case studies (Kaluzeviciute & Willemsen, 2020 ) was also utilised to identify case study components that would help improve therapist clinical decision-making and reflexivity.
For the analysis of more complex research components (e.g. the degree of therapist reflexivity), the purpose-based evaluation will utilise a framework approach, in line with comprehensive and open-ended reviewer responses in ETQS (Evaluation Tool for Qualitative Studies) (Long & Godfrey, 2004 ) (Table 13 ). That is to say, the evaluation here is not so much about the presence or absence of information (as in the checklist approach) but the degree to which the information helps the case with its unique purpose, whether it is generalisability or typicality. Therefore, although the purpose-oriented evaluation criteria below encompasses comprehensive questions at a considerable level of generality (in the sense that not all components may be required or relevant for each case study), it nevertheless seeks to engage with each type of purpose-based systematic case study on an individual basis (attending to research or clinical components that are unique to each of type of case study).
It is important to note that, as this is an introductory paper to CaSE, the evaluative framework is still preliminary: it involves some of the core questions that pertain to the nature of all six purpose-based systematic case studies. However, there is a need to develop a more comprehensive and detailed CaSE appraisal framework for each purpose-based systematic case study in the future.
Using CaSE on published systematic case studies in psychotherapy: an example
To illustrate the use of CaSE Purpose - based Evaluative Framework for Systematic Case Studies , a case study by Lunn, Daniel, and Poulsen ( 2016 ) titled ‘ Psychoanalytic Psychotherapy With a Client With Bulimia Nervosa ’ was selected from the Single Case Archive (SCA) and analysed in Table 14 . Based on the core questions associated with the six purpose-based systematic case study types in Table 13 (1 to 6), the purpose of Lunn et al.’s ( 2016 ) case was identified as critical (testing an existing theoretical suggestion).
Sometimes, case study authors will explicitly define the purpose of their case in the form of research objectives (as was the case in Lunn et al.’s study); this helps identifying which purpose-based questions are most relevant for the evaluation of the case. However, some case studies will require comprehensive analysis in order to identify their purpose (or multiple purposes). As such, it is recommended that CaSE reviewers first assess the degree and manner in which information about the studied phenomenon, patient data, clinical discourse and research are presented before deciding on the case purpose.
Although each purpose-based systematic case study will contribute to different strands of psychotherapy (theory, practice, training, etc.) and focus on different forms of data (e.g. theory testing vs extensive clinical descriptions), the overarching aim across all systematic case studies in psychotherapy is to study local and contingent processes, such as variations in patient symptoms and complexities of the clinical setting. The comprehensive framework approach will therefore allow reviewers to assess the degree of external validity in systematic case studies (Barkham & Mellor-Clark, 2003 ). Furthermore, assessing the case against its purpose will let reviewers determine whether the case achieves its set goals (research objectives and aims). The example below shows that Lunn et al.’s ( 2016 ) case is successful in functioning as a critical case as the authors provide relevant, high-quality information about their tested therapeutic conditions.
Finally, it is also possible to use CaSE to gather specific type of systematic case studies for one’s research, practice, training, etc. For example, a CaSE reviewer might want to identify as many descriptive case studies focusing on negative therapeutic relationships as possible for their clinical supervision. The reviewer will therefore only need to refer to CaSE questions in Table 13 (2) on descriptive cases. If the reviewed cases do not align with the questions in Table 13 (2), then they are not suitable for the CaSE reviewer who is looking for “know-how” knowledge and detailed clinical narratives.
Concluding comments
This paper introduces a novel Case Study Evaluation-tool (CaSE) for systematic case studies in psychotherapy. Unlike most appraisal tools in EBP, CaSE is positioned within purpose-oriented evaluation criteria, in line with the PBE paradigm. CaSE enables reviewers to assess what each systematic case is good for (rather than determining an absolute measure of ‘good’ and ‘bad’ systematic case studies). In order to explicate a purpose-based evaluative framework, six different systematic case study purposes in psychotherapy have been identified: representative cases (purpose: typicality), descriptive cases (purpose: particularity), unique cases (purpose: deviation), critical cases (purpose: falsification/confirmation), exploratory cases (purpose: hypothesis generation) and transferable cases (purpose: generalisability). Each case was linked with an existing epistemological network, such as Iwakabe and Gazzola’s ( 2009 ) work on case selection criteria for meta-synthesis. The framework approach includes core questions specific to each purpose-based case study (Table 13 (1–6)). The aim is to assess the external validity and effectiveness of each case study against its set out research objectives and aims. Reviewers are required to perform a comprehensive and open-ended data analysis, as shown in the example in Table 14 .
Along with CaSE Purpose - based Evaluative Framework (Table 13 ), the paper also developed CaSE Checklist for Essential Components in Systematic Case Studies (Table 12 ). The checklist approach is meant to aid reviewers in assessing the presence or absence of essential case study components, such as the rationale behind choosing the case study method and description of patient’s history. If essential components are missing in a systematic case study, then it may be implied that there is a lack of information, which in turn diminishes the evidential quality of the case. Following broader definitions of validity set out by Levitt et al. ( 2017 ) and Truijens et al. ( 2019 ), it could be argued that the checklist approach allows for the assessment of (non-quantitative) internal validity in systematic case studies: does the researcher provide sufficient information about the case study design, rationale, research objectives, epistemological/philosophical paradigms, assessment procedures, data analysis, etc., to account for their research conclusions?
It is important to note that this paper is set as an introduction to CaSE; by extension, it is also set as an introduction to research evaluation and appraisal processes for case study researchers in psychotherapy. As such, it was important to provide a step-by-step epistemological rationale and process behind the development of CaSE evaluative framework and checklist. However, this also means that further research needs to be conducted in order to develop the tool. While CaSE Purpose - based Evaluative Framework involves some of the core questions that pertain to the nature of all six purpose-based systematic case studies, there is a need to develop individual and comprehensive CaSE evaluative frameworks for each of the purpose-based systematic case studies in the future. This line of research is likely to enhance CaSE target audience: clinicians interested in reviewing highly particular clinical narratives will attend to descriptive case study appraisal frameworks; researchers working with qualitative meta-synthesis will find transferable case study appraisal frameworks most relevant to their work; while teachers on psychotherapy and counselling modules may seek out unique case study appraisal frameworks.
Furthermore, although CaSE Checklist for Essential Components in Systematic Case Studies and CaSE Purpose - based Evaluative Framework for Systematic Case Studies are presented in a comprehensive, detailed manner, with definitions and examples that would enable reviewers to have a good grasp of the appraisal process, it is likely that different reviewers may have different interpretations or ideas of what might be ‘substantial’ case study data. This, in part, is due to the methodologically pluralistic nature of the case study genre itself; what is relevant for one case study may not be relevant for another, and vice-versa. To aid with the review process, future research on CaSE should include a comprehensive paper on using the tool. This paper should involve evaluation examples with all six purpose-based systematic case studies, as well as a ‘search’ exercise (using CaSE to assess the relevance of case studies for one’s research, practice, training, etc.).
Finally, further research needs to be developed on how (and, indeed, whether) systematic case studies should be reviewed with specific ‘grades’ or ‘assessments’ that go beyond the qualitative examination in Table 14 . This would be particularly significant for the processes of qualitative meta-synthesis and meta-analysis. These research developments will further enhance CaSE tool, and, in turn, enable psychotherapy researchers to appraise their findings within clear, purpose-based evaluative criteria appropriate for systematic case studies.
Availability of data and materials
Not applicable.
Almond, R. (2004). “I Can Do It (All) Myself”: Clinical technique with defensive narcissistic self–sufficiency. Psychoanalytic Psychology , 21 (3), 371–384. https://doi.org/10.1037/0736-9735.21.3.371 .
Article Google Scholar
American Psychological Association (2010). Evidence–based case study. Retrieved from https://www.apa.org/pubs/journals/pst/evidence–based–case–study.
Google Scholar
Aveline, M. (2005). Clinical case studies: Their place in evidence–based practice. Psychodynamic Practice: Individuals, Groups and Organisations , 11 (2), 133–152. https://doi.org/10.1080/14753630500108174 .
Barkham, M., & Mellor-Clark, J. (2003). Bridging evidence-based practice and practice-based evidence: Developing a rigorous and relevant knowledge for the psychological therapies. Clinical Psychology & Psychotherapy , 10 (6), 319–327. https://doi.org/10.1002/cpp.379 .
Berg, H. (2019). How does evidence–based practice in psychology work? – As an ethical demarcation. Philosophical Psychology , 32 (6), 853–873. https://doi.org/10.1080/09515089.2019.1632424 .
Berg, H., & Slaattelid, R. (2017). Facts and values in psychotherapy—A critique of the empirical reduction of psychotherapy within evidence-based practice. Journal of Evaluation in Clinical Practice , 23 (5), 1075–1080. https://doi.org/10.1111/jep.12739 .
Article PubMed Google Scholar
Bower, P. (2003). Efficacy in evidence-based practice. Clinical Psychology and Psychotherapy , 10 (6), 328–336. https://doi.org/10.1002/cpp.380 .
Cartwright, N., & Hardie, J. (2012). What are RCTs good for? In N. Cartwright, & J. Hardie (Eds.), Evidence–based policy: A practical guide to doing it better . Oxford University Press. https://doi.org/10.1093/acprof:osobl/9780199841608.003.0008 .
Critical Appraisal Skills Programme (CASP). (2018). Qualitative checklist. Retrieved from https://casp–uk.net/wp–content/uploads/2018/01/CASP–Qualitative–Checklist–2018.pdf .
Davison, G. C., & Lazarus, A. A. (2007). Clinical case studies are important in the science and practice of psychotherapy. In S. O. Lilienfeld, & W. T. O’Donohue (Eds.), The great ideas of clinical science: 17 principles that every mental health professional should understand , (pp. 149–162). Routledge/Taylor & Francis Group.
Douglas, H. (2004). The irreducible complexity of objectivity. Synthese , 138 (3), 453–473. https://doi.org/10.1023/B:SYNT.0000016451.18182.91 .
Duncan, B. L., & Sparks, J. A. (2020). When meta–analysis misleads: A critical case study of a meta–analysis of client feedback. Psychological Services , 17 (4), 487–496. https://doi.org/10.1037/ser0000398 .
Edelson, M. (1986). Causal explanation in science and in psychoanalysis—Implications for writing a case study. Psychoanalytic Study of Child , 41 (1), 89–127. https://doi.org/10.1080/00797308.1986.11823452 .
Edwards, D. J. A. (2013). Collaborative versus adversarial stances in scientific discourse: Implications for the role of systematic case studies in the development of evidence–based practice in psychotherapy. Pragmatic Case Studies in Psychotherapy , 3 (1), 6–34.
Edwards, D. J. A., Dattilio, F. M., & Bromley, D. B. (2004). Developing evidence–based practice: The role of case–based research. Professional Psychology: Research and Practice , 35 (6), 589–597. https://doi.org/10.1037/0735-7028.35.6.589 .
Erickson, F. (2012). Comments on causality in qualitative inquiry. Qualitative Inquiry , 18 (8), 686–688. https://doi.org/10.1177/1077800412454834 .
Fishman, D. B. (1999). The case for pragmatic psychology . New York University Press.
Fishman, D. B. (2005). Editor’s introduction to PCSP––From single case to database: A new method for enhancing psychotherapy practice. Pragmatic Case Studies in Psychotherapy , 1 (1), 1–50.
Fishman, D. B., Messer, S. B., Edwards, D. J. A., & Dattilio, F. M. (Eds.) (2017). Case studies within psychotherapy trials: Integrating qualitative and quantitative methods . Oxford University Press.
Fox, N. J. (2003). Practice–based evidence: Towards collaborative and transgressive research. Sociology , 37 (1), 81–102. https://doi.org/10.1177/0038038503037001388 .
Gabbay, J., & le May, A. (2011). Practice–based evidence for healthcare: Clinical mindlines . Routledge.
Green, L. W., & Latchford, G. (2012). Maximising the benefits of psychotherapy: A practice–based evidence approach . Wiley–Blackwell. https://doi.org/10.1002/9781119967590 .
Hannes, K., Lockwood, C., & Pearson, A. (2010). A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qualitative Health Research , 20 (12), 1736–1743. https://doi.org/10.1177/1049732310378656 .
Hartling, L., Chisholm, A., Thomson, D., & Dryden, D. M. (2012). A descriptive analysis of overviews of reviews published between 2000 and 2011. PLoS One , 7 (11), e49667. https://doi.org/10.1371/journal.pone.0049667 .
Article PubMed PubMed Central Google Scholar
Hill, A., & Spittlehouse, C. (2003). What is critical appraisal? Evidence–Based Medicine , 3 (2), 1–8.
Hilliard, R. B. (1993). Single–case methodology in psychotherapy process and outcome research. Journal of Consulting and Clinical Psychology , 61 (3), 373–380. https://doi.org/10.1037/0022-006X.61.3.373 .
Horn, S. D., & Gassaway, J. (2007). Practice–based evidence study design for comparative effectiveness research. Medical Care , 45 (10), S50–S57. https://doi.org/10.1097/MLR.0b013e318070c07b .
Iwakabe, S. (2003, May). Common change events in stages of psychotherapy: A qualitative analysis of case reports. In Paper presented at the 19th Annual Conference of the Society for Exploration of Psychotherapy Integration, New York .
Iwakabe, S. (2005). Pragmatic meta–analysis of case studies. Annual Progress of Family Psychology , 23 , 154–169.
Iwakabe, S., & Gazzola, N. (2009). From single–case studies to practice–based knowledge: Aggregating and synthesizing case studies. Psychotherapy Research , 19 (4-5), 601–611. https://doi.org/10.1080/10503300802688494 .
Jimenez-Buedo, M., & Miller, L. (2010). Why a Trade–Off? The relationship between the external and internal validity of experiments. THEORIA: An International Journal for Theory History and Foundations of Science , 25 (3), 301–321.
Joanna Briggs Institute (JBI). (2017a). Critical appraisal checklist for qualitative research. Retrieved from https://joannabriggs.org/sites/default/files/2019–05/JBI_Critical_Appraisal–Checklist_for_Qualitative_Research2017_0.pdf
Joanna Briggs Institute (JBI). (2017b). Checklist for case reports. Retrieved from https://joannabriggs.org/sites/default/files/2019–05/JBI_Critical_Appraisal–Checklist_for_Case_Reports2017_0.pdf
Kaluzeviciute, G. (2021). Validity, Evidence and Appraisal in Systematic Psychotherapy Case Studies . Paper presented at the Research Forum of Department of Psychosocial and Psychoanalytic Studies, University of Essex, Colchester, UK. https://doi.org/10.13140/RG.2.2.33502.15683
Kaluzeviciute, G., & Willemsen, J. (2020). Scientific thinking styles: The different ways of thinking in psychoanalytic case studies. The International Journal of Psychoanalysis , 101 (5), 900–922. https://doi.org/10.1080/00207578.2020.1796491 .
Katrak, P., Bialocerkowski, A. E., Massy-Westropp, N., Kumar, S. V. S., & Grimmer, K. (2004). A systematic review of the content of critical appraisal tools. BMC Medical Research Methodology , 4 (1), 22. https://doi.org/10.1186/1471-2288-4-22 .
Kennedy, M. M. (1979). Generalising from single case studies. Evaluation Quarterly , 3 (4), 661–678. https://doi.org/10.1177/0193841X7900300409 .
Laska, K. M., Gurman, A. S., & Wampold, B. E. (2014). Expanding the lens of evidence–based practice in psychotherapy: A common factors perspective. Psychotherapy , 51 (4), 467–481. https://doi.org/10.1037/a0034332 .
Levitt, H. M., Motulsky, S. L., Wertz, F. J., Morrow, S. L., & Ponterotto, J. G. (2017). Recommendations for designing and reviewing qualitative research in psychology: Promoting methodological integrity. Qualitative Psychology , 4 (1), 2–22. https://doi.org/10.1037/qup0000082 .
Lilienfeld, S. O., Ritschel, L. A., Lynn, S. J., Cautin, R. L., & Latzman, R. D. (2013). Why many clinical psychologists are resistant to evidence–based practice: root causes and constructive remedies. Clinical Psychology Review , 33 (7), 883–900. https://doi.org/10.1016/j.cpr.2012.09.008 .
Long, A. F., & Godfrey, M. (2004). An evaluation tool to assess the quality of qualitative research studies. International Journal of Social Research Methodology , 7 (2), 181–196. https://doi.org/10.1080/1364557032000045302 .
Longhofer, J., Floersch, J., & Hartmann, E. A. (2017). Case for the case study: How and why they matter. Clinical Social Work Journal , 45 (3), 189–200. https://doi.org/10.1007/s10615-017-0631-8 .
Lunn, S., Daniel, S. I. F., & Poulsen, S. (2016). Psychoanalytic psychotherapy with a client with bulimia nervosa. Psychotherapy , 53 (2), 206–215. https://doi.org/10.1037/pst0000052 .
Mackrill, T., & Iwakabe, S. (2013). Making a case for case studies in psychotherapy training: A small step towards establishing an empirical basis for psychotherapy training. Counselling Psychotherapy Quarterly , 26 (3–4), 250–266. https://doi.org/10.1080/09515070.2013.832148 .
Maggio, S., Molgora, S., & Oasi, O. (2019). Analyzing psychotherapeutic failures: A research on the variables involved in the treatment with an individual setting of 29 cases. Frontiers in Psychology , 10 , 1250. https://doi.org/10.3389/fpsyg.2019.01250 .
Mahrer, A. R. (1988). Discovery–oriented psychotherapy research: Rationale, aims, and methods. American Psychologist , 43 (9), 694–702. https://doi.org/10.1037/0003-066X.43.9.694 .
Margison, F. B., et al. (2000). Measurement and psychotherapy: Evidence–based practice and practice–based evidence. British Journal of Psychiatry , 177 (2), 123–130. https://doi.org/10.1192/bjp.177.2.123 .
Maxwell, J. A. (2004). Causal explanation, qualitative research, and scientific inquiry in education. Educational Researcher , 33 (2), 3–11. https://doi.org/10.3102/0013189X033002003 .
McLeod, J. (2002). Case studies and practitioner research: Building knowledge through systematic inquiry into individual cases. Counselling and Psychotherapy Research: Linking research with practice , 2 (4), 264–268. https://doi.org/10.1080/14733140212331384755 .
McLeod, J. (2010). Case study research in counselling and psychotherapy . SAGE Publications. https://doi.org/10.4135/9781446287897 .
McLeod, J., & Elliott, R. (2011). Systematic case study research: A practice–oriented introduction to building an evidence base for counselling and psychotherapy. Counselling and Psychotherapy Research , 11 (1), 1–10. https://doi.org/10.1080/14733145.2011.548954 .
Meganck, R., Inslegers, R., Krivzov, J., & Notaerts, L. (2017). Beyond clinical case studies in psychoanalysis: A review of psychoanalytic empirical single case studies published in ISI–ranked journals. Frontiers in Psychology , 8 , 1749. https://doi.org/10.3389/fpsyg.2017.01749 .
Merriam, S. B. (1998). Qualitative research and case study applications in education . Jossey–Bass Publishers.
Michels, R. (2000). The case history. Journal of the American Psychoanalytic Association , 48 (2), 355–375. https://doi.org/10.1177/00030651000480021201 .
Midgley, N. (2006). Re–reading “Little Hans”: Freud’s case study and the question of competing paradigms in psychoanalysis. Journal of the American Psychoanalytic Association , 54 (2), 537–559. https://doi.org/10.1177/00030651060540021601 .
Rosqvist, J., Thomas, J. C., & Truax, P. (2011). Effectiveness versus efficacy studies. In J. C. Thomas, & M. Hersen (Eds.), Understanding research in clinical and counseling psychology , (pp. 319–354). Routledge/Taylor & Francis Group.
Sackett, D. L., Rosenberg, W. M., Gray, J. A. M., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: what it is and what it isn’t. BMJ , 312 (7023), 71–72. https://doi.org/10.1136/bmj.312.7023.71 .
Stake, R. E. (1995). The art of case study research . SAGE Publications.
Stake, R. E. (2010). Qualitative research: Studying how things work . The Guilford Press.
Stewart, R. E., & Chambless, D. L. (2007). Does psychotherapy research inform treatment decisions in private practice? Journal of Clinical Psychology , 63 (3), 267–281. https://doi.org/10.1002/jclp.20347 .
Stiles, W. B. (2007). Theory–building case studies of counselling and psychotherapy. Counselling and Psychotherapy Research , 7 (2), 122–127. https://doi.org/10.1080/14733140701356742 .
Teachman, B. A., Drabick, D. A., Hershenberg, R., Vivian, D., Wolfe, B. E., & Goldfried, M. R. (2012). Bridging the gap between clinical research and clinical practice: introduction to the special section. Psychotherapy , 49 (2), 97–100. https://doi.org/10.1037/a0027346 .
Thorne, S., Jensen, L., Kearney, M. H., Noblit, G., & Sandelowski, M. (2004). Qualitative metasynthesis: Reflections on methodological orientation and ideological agenda. Qualitative Health Research , 14 (10), 1342–1365. https://doi.org/10.1177/1049732304269888 .
Timulak, L. (2009). Meta–analysis of qualitative studies: A tool for reviewing qualitative research findings in psychotherapy. Psychotherapy Research , 19 (4–5), 591–600. https://doi.org/10.1080/10503300802477989 .
Trad, P. V., & Raine, M. J. (1994). A prospective interpretation of unconscious processes during psychoanalytic psychotherapy. Psychoanalytic Psychology , 11 (1), 77–100. https://doi.org/10.1037/h0079522 .
Truijens, F., Cornelis, S., Desmet, M., & De Smet, M. (2019). Validity beyond measurement: Why psychometric validity is insufficient for valid psychotherapy research. Frontiers in Psychology , 10 . https://doi.org/10.3389/fpsyg.2019.00532 .
Tuckett, D. (Ed.) (2008). The new library of psychoanalysis. Psychoanalysis comparable and incomparable: The evolution of a method to describe and compare psychoanalytic approaches . Routledge/Taylor & Francis Group. https://doi.org/10.4324/9780203932551 .
van Hennik, R. (2020). Practice based evidence based practice, part II: Navigating complexity and validity from within. Journal of Family Therapy , 43 (1), 27–45. https://doi.org/10.1111/1467-6427.12291 .
Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004). The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin , 130 (4), 631–663. https://doi.org/10.1037/0033-2909.130.4.631 .
Widdowson, M. (2011). Case study research methodology. International Journal of Transactional Analysis Research & Practice , 2 (1). https://doi.org/10.29044/v2i1p25 .
Willemsen, J., Della Rosa, E., & Kegerreis, S. (2017). Clinical case studies in psychoanalytic and psychodynamic treatment. Frontiers in Psychology , 8 (108). https://doi.org/10.3389/fpsyg.2017.00108 .
Williams, V., Boylan, A., & Nunan, D. (2019). Critical appraisal of qualitative research: Necessity, partialities and the issue of bias. BMJ Evidence–Based Medicine . https://doi.org/10.1136/bmjebm-2018-111132 .
Yin, R. K. (1984). Case study research: Design and methods . SAGE Publications.
Yin, R. K. (1993). Applications of case study research . SAGE Publications.
Download references
Acknowledgments
I would like to thank Prof Jochem Willemsen (Faculty of Psychology and Educational Sciences, Université catholique de Louvain-la-Neuve), Prof Wayne Martin (School of Philosophy and Art History, University of Essex), Dr Femke Truijens (Institute of Psychology, Erasmus University Rotterdam) and the reviewers of Psicologia: Reflexão e Crítica / Psychology : Research and Review for their feedback, insight and contributions to the manuscript.
Arts and Humanities Research Council (AHRC) and Consortium for Humanities and the Arts South-East England (CHASE) Doctoral Training Partnership, Award Number [AH/L50 3861/1].
Author information
Authors and affiliations.
Department of Psychosocial and Psychoanalytic Studies, University of Essex, Wivenhoe Park, Colchester, CO4 3SQ, UK
Greta Kaluzeviciute
You can also search for this author in PubMed Google Scholar
Contributions
GK is the sole author of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Greta Kaluzeviciute .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Kaluzeviciute, G. Appraising psychotherapy case studies in practice-based evidence: introducing Case Study Evaluation-tool (CaSE). Psicol. Refl. Crít. 34 , 9 (2021). https://doi.org/10.1186/s41155-021-00175-y
Download citation
Received : 12 January 2021
Accepted : 09 March 2021
Published : 19 March 2021
DOI : https://doi.org/10.1186/s41155-021-00175-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic case studies
- Psychotherapy research
- Research appraisal tool
- Evidence-based practice
- Practice-based evidence
- Research validity
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Hum Neurosci
A clinical case study of a psychoanalytic psychotherapy monitored with functional neuroimaging
Anna buchheim.
1 Institute of Psychology, University of Innsbruck, Innsbruck, Austria
Karin Labek
Steffen walter.
2 Department of Psychosomatic Medicine and Psychotherapy, University of Ulm, Ulm, Germany
Roberto Viviani
3 Department of Psychiatry and Psychotherapy III, University of Ulm, Ulm, Germany
This case study describes 1 year of the psychoanalytic psychotherapy using clinical data, a standardized instrument of the psychotherapeutic process (Psychotherapy process Q-Set, PQS), and functional neuroimaging (fMRI). A female dysthymic patient with narcissistic traits was assessed at monthly intervals (12 sessions). In the fMRI scans, which took place immediately after therapy hours, the patient looked at pictures of attachment-relevant scenes (from the Adult Attachment Projective Picture System, AAP) divided into two groups: those accompanied by a neutral description, and those accompanied by a description tailored to core conflicts of the patient as assessed in the AAP. Clinically, this patient presented defense mechanisms that influenced the relationship with the therapist and that was characterized by fluctuations of mood that lasted whole days, following a pattern that remained stable during the year of the study. The two modes of functioning associated with the mood shifts strongly affected the interaction with the therapist, whose quality varied accordingly (“easy” and “difficult” hours). The PQS analysis showed the association of “easy” hours with the topic of the involvement in significant relationships and of “difficult hours” with self-distancing, a defensive maneuver common in narcissistic personality structures. In the fMRI data, the modes of functioning visible in the therapy hours were significantly associated with modulation of the signal elicited by personalized attachment-related scenes in the posterior cingulate ( p = 0.017 cluster-level, whole-volume corrected). This region has been associated in previous studies to self-distancing from negatively valenced pictures presented during the scan. The present study may provide evidence of the possible involvement of this brain area in spontaneously enacted self-distancing defensive strategies, which may be of relevance in resistant reactions in the course of a psychoanalytic psychotherapy.
INTRODUCTION
The empirical investigation of the psychoanalytic process and outcome is of great importance to advance our knowledge of the psychoanalytic theory of treatment. Several studies have demonstrated the efficacy of long-term and short-term psychoanalytic treatment in randomized controlled trials (e.g., Gabbard et al., 2002 ; Leichsenring et al., 2004 ; Leichsenring and Rabung, 2008 , 2011 ). Nevertheless, many clinicians and researchers argue that detailed single case studies, a time-honored instrument of psychoanalytic inquiry and knowledge dissemination ( Donnellan, 1978 ; Edelson, 1985 ; Kächele et al., 2009 ) are still an essential complement to clinical trials in furthering our understanding of the psychoanalytic process and its relation to outcome (e.g., Kächele et al., 2006 , 2009 ). Single case research has been often indicated as one of the most suitable approach for evaluating psychoanalytic treatments ( Wallerstein and Sampson, 1971 ; Edelson, 1988 ; Hilliard, 1993 ). Recently, single case studies based on operationalized instruments have been developed in different domains (e.g., Kazdin, 1982 ). These efforts have produced psychotherapy studies focusing on computerized text-analytic measures (e.g., Mergenthaler and Kächele, 1996 ), process and outcome research (e.g., Hilliard, 1993 ; Orlinsky et al., 2004 ; Gullestad and Wilberg, 2011 ), and the combination of psychotherapy research and fMRI ( Schiepek et al., 2009 , 2013 ).
The aim of the present study was exploring for the first time the feasibility of single case research of an ongoing psychoanalysis in a neurobiological context using repeated fMRI measurements. We pursued the integration of clinical presentation, of operationalized formal instruments to describe the individual psychotherapeutic process, and of neuroimaging techniques to monitor the psychotherapeutic process on both the clinical and the neural levels. To this end, we collected functional neuroimaging data at monthly intervals from a patient undergoing psychoanalytic psychotherapy during exposure to attachment-relevant pictures ( Buchheim et al., 2006 , 2008 ). The main question we wanted to address was the extent to which the data from functional neuroimaging could be brought to bear on our theoretical understanding of the psychoanalytic process. Likewise, we were interested in verifying if existing interpretations of cortical activity gained in controlled experimental settings from neuroimaging studies would maintain their explanatory power in the context of the single case study of a psychoanalytic process. A crucial issue was therefore the existence of an association between symptoms, the character of the relationship with the therapist in individual therapy hours, and variation in the signal from the attachment-relevant scenes probe in the scanner.
MATERIALS AND METHODS
One year of psychoanalytic therapy of a patient with a chronic depressive disorder and narcissistic traits was assessed at monthly intervals ( N = 12 sessions) with an established measure for the characterization of therapy (The Psychotherapy Process Q-Set, PQS; Jones, 2000 ), and with a functional neuroimaging probe that was successfully used to elicit signal in an adult attachment context in a previous study of the psychoanalytic treatment of recurrent depression ( Buchheim et al., 2012 ).
The patient, a 42-years-old female lawyer, suffered from rapidly fluctuating affective states. Waking up the morning she knew that “this will be an easy day” or “this will be a difficult day.” Her capacity for successful work and concentration was reduced when she felt depressed and in a “difficult day mood.” During these occasions she isolated herself, tended to withdraw from relationships, and worked hard to hide her emotional vulnerability. This chronic and fluctuating depressive pathology and a fragile, vulnerable perception of self and others brought her in psychoanalytic treatment.
In order to obtain an objective assessment of the psychotherapy process describing the psychodynamic pattern of the patient and the interaction between the patient and the therapist, one session every 4 weeks (first session of the week) at regular intervals (compatible with interruptions due to vacations and illnesses) was audiotaped, transcribed, and analyzed with the PQS approach (12 sessions in all). The PQS ( Jones, 2000 ; German version: Albani et al., 2007 ) is a rating instrument designed to provide a basic vocabulary for the description and classification of psychotherapy processes in a form suitable to quantitative analysis (Q-sort methodology). The PQS captures a wide range of events in the psychotherapeutic session attributable to both the therapist’s activity and the patient, including transference manifestations, resistance, and the accompanying affective states.
Functional neuroimaging scans were taken on the same days as the recorded therapy hours. As in a previous study ( Buchheim et al., 2012 ), attachment-relevant scenes were used to capture individual attachment-related features relevant for the psychotherapeutic relationship. In the scanner, the patient looked at the scenes used in a formal measure for the assessment of adult attachment representations (Adult Attachment Projective Picture System, AAP; Buchheim et al., 2006 , 2008 ; George and West, 2012 ). These scenes were alternately accompanied by sentences neutrally describing their content, or by sentences that referred to the personally relevant content evoked by them as extracted by a previous AAP interview. The contrast of interest was the difference between the signal evoked by the personalized and the neutral textual descriptions of the scenes. This contrast detected neural substrates activated by the appraisal of the personal element in the attachment scenes, at the net of generic activations due to the perceptual encoding of the scenes and reading the textual description.
Note that we did not have access to changes in brain function during therapy, since the functional neuroimaging sessions necessarily took place after, and not during, therapy hours. However, we were aided in our attempt in establishing a link between mind states, therapy, and neural substrates by the oscillations of the patient between “difficult” and “easy” days, a change in mood that may have been relatively stable from the therapy hour to the functional neuroimaging session. Hence, the data we present document changes in these modes of emotional functioning that had consequences on the quality of the therapy hours, rather than the therapy hours themselves. The question of interest was the extent to which clinical data from the therapy hours and neural activation were reciprocally informative of the mental states at the base of the “easy” and “difficult” moods. This focus also allowed us to sidestep the issue of change over the course of therapy, which would possibly be confounded by habituation or learning effects in the neuroimaging data.
PARTICIPANTS
The analyst was a very experienced training analyst with an interest in research. She agreed to take part in our study and to audiotape one therapy session a month for the PQS analysis. She works in a private practice as a psychiatrist.
The patient also agreed to take part in the study. She was given information about the study and signed a declaration of her willingness to participate for 1 year and to be assessed with several questionnaires and the functional neuroimaging scans. The treatment was paid by the health insurance. This study was approved by the ethical committee by the University of Ulm in the context of the Hanse-Neuro-Psychoanalysis Study ( Buchheim et al., 2008 , 2012 ). The patient gave written informed consent to the publication of the data. However, the case report should be written taking into consideration the need to protect the identity of the patient.
This patient was treated with a standard long-term psychoanalysis with a frequency of two face-to-face sessions per week. Standard key techniques included exploration, clarification, and interpretation. Interpretive interventions aimed to enhance the patient’s insight into her repetitive conflicts sustaining her problems; supportive interventions aimed to strengthen abilities that were temporarily inaccessible to the patient’s owing to acute stress (e.g., traumatic events) or were not sufficiently developed (e.g., Fonagy and Kächele, 2009 ; Shedler, 2010 ). The establishment of a helping (or therapeutic) alliance is regarded as an important component of supportive interventions. Transference, defined as the repetition of past experiences in present interpersonal relations, constitutes another important dimension of the therapeutic relationship. In psychodynamic psychotherapy, transference is regarded as a primary source of understanding and therapeutic change (e.g., Fonagy and Kächele, 2009 ). In this low frequency therapy, the analyst followed an intersubjective approach, characterized by the focus on the inner and outer reality of the patient’s self and object representations and the aim to increase the patient’s capacity to differentiate between reality and fantasy by enhancing self-reflection (e.g., Ogden, 1977 , 1989 ; Fonagy et al., 2004 ; Dreyer and Schmidt, 2008 ).
CLINICAL AND BEHAVIORAL OUTCOME VARIABLES
The clinical and behavioral outcome data served different purposes. First, the monitoring of symptoms with self-rating scales documented changes in affective symptoms at the days of the data collection. In clinical studies, these data describe the level of symptoms and document changes during therapy (in the present case study, these measures indicated a substantially stable state over the year of the study, as detailed below). Second, the clinical rating of the hour by the therapist and the PQS documented the exchange between patient and analyst during therapy through the clinical impression and an operationalized assessment instrument. Variation in these data provided correlates to explore with the neuroimaging probe. Third, the AAP interview provided material on core attachment issues specific to the patient for the preparation of the stimuli used in the neuroimaging sessions. Almost as a side product, it also provided an assessment of the attachment pattern of this patient at the beginning of study. The AAP interview, however, is not administrable on a monthly basis and for this reason could not be used as a clinical correlate of the neuroimaging data in the present setting. Fourth, a post-scan self-rating questionnaire was administered to evaluate reported involvement with the stimuli presented during the scan session. These data were meant as an aid in interpreting the fMRI analysis. Finally, the results section also reports on the patient using a more customary clinical description informed by psychoanalytic views. We considered the clinical description an integral part of the results, this being a single case study. This description is meant to provide guidance on the psychopathology of this patient, to be compared with the functional role of neural structures identified in the neuroimaging study.
Clinical rating of the hour by the therapist
The analyst rated on a clinical level dichotomously if the 12 sessions were “difficult” or “easy.” According to her documentation the classification in “difficult” or “easy” was very clearly identifiable. The “difficult” sessions started with silence and remained quiet and inhibited. The “easy” sessions started fluently and remained talkative.
Psychopathology monitoring with self-rating scales
At each scanning session, the patient filled a number of self-rating scales documenting her psychopathological state. State depressiveness was rated with the Collegium Internationale Psychiatriae Scalarum (CIPS)-depressiveness scale ( Zerssen, 1976 ). This is a self-rating depressiveness scales provided in two parallel series of questions, which may be used in alternative turns in sequential assessments. The general burden of symptoms was gaged with the outcome questionnaire (OQ)-burden subscale (German version: Haug et al., 2004 ).
Psychotherapy process Q-set
The PQS is an operationalized instrument for the characterization of therapy hours ( Jones, 2000 ). It consists of 100 items covering a wide range of aspects in the behavior of the patient and her interaction with the therapist. Unlike most rating instruments, the items are not arranged in predefined groups that considered together provide scores on clinical dimensions identified a priori . Instead, a typical use of this instrument in psychotherapy research is the identification of hallmark of hours with specific characteristics. For example, one may attempt to identify items correlating with a negative therapeutic reaction, ascertained clinically in a carefully monitored therapy sample. Among their uses, these items can identify both the unity and coherence of treatment sessions, and detects changes between hours and patients. The PQS-instrument shows excellent inter-rater reliability, item reliability, concurrent, and predictive validity for several studies and various types of treatment samples (see Levy et al., 2012 ). The inter-rater reliability, assessed for all 100 items and tested by correlating the Q-sorts of multiple raters, is high as evidenced by levels of inter-rater agreement/reliability (kappa ranges from 0.83 to 0.89). Reliability varies from adequate to excellent for individual items, giving values between 0.50 and 0.95 (see Levy et al., 2012 ). In this study verbatim transcribed sessions were coded by two independent raters, who were blind to all therapy hours. Two independent trained judges rated all 12 psychotherapy sessions and achieved a correspondence of kappa between 0.80 and 0.97.
Statistical analysis of behavioral data
Because of the inherently correlational and explorative character of data obtained with the PQS, we investigated the tendency of PQS scores to covary across items with a principal component analysis. To compute significance levels of principal components, we carried out 2000 Monte Carlo simulations in which principal component analyses were computed on data with the same item range and distribution, but varying independently from each other. Significance values were computed as quantiles of the first and second components of the simulations (to test the significance of the first and second component, respectively). Significant components provide evidence that a set of therapy characteristics occur together, suggesting the existence of recurrent interaction dynamics.
Hypothesis testing on PQS items were conducted on the linear trend (the months of therapy from 1 to 12) and on the classification of “easy” and “difficult” hours provided by the analyst. The first test documented the existence of a change in the tendency of these interaction dynamics to occur with different frequencies at the beginning and at the end of the period of the study. The second test constituted an objective verification of the clinical impression of the analyst. Tests were carried out independently on each PQS item, correcting for the multiple comparison using a permutation method with 2000 steps ( Blair et al., 1994 ). In this approach, at each permutation the maximal (minimal) t -value obtained from conducting the test on the PQS item was recorded. The significance levels of high (low) t -values, with adjustment for multiple testing, were given by the quantiles of the recorded maximal (minimal) t -values.
Self-rating questionnaire after fMRI sessions
To monitor the extent of emotional involvement and autobiographical character of the three core sentences during the course of the psychotherapy, we administered a self-rating questionnaire to the patient after each fMRI session. In the questionnaire the patient was asked to rate the personalized sentences from the AAP scenes used in the scanner by answering the following two questions: “How much of the sentence applies to you autobiographically?” and “How strong did this sentence move you emotionally?” The patient had to assign a score between 1 and 7, where 1 meant not at all, 4 meant middle intensity, and 7 meant very much.
AAP interview
Attachment classification and fMRI-stimuli were derived from the AAP ( George and West, 2012 ), an established and validated interview to assess attachment representations, based on a set of eight picture stimuli. The stimuli are line drawings of a neutral scene and seven attachment scenes (e.g., illness, separation, solitude, death, and threat). The AAP classification system designates the four main adult attachment groups identified using the AAI classification system (secure, dismissing, preoccupied, unresolved). Classifications are based on the rating of several scales (e.g., agency of self, connectedness, synchrony, deactivation) on the basis of verbatim transcripts of the stories to the seven attachment activating stimuli.
Administration involves asking participants in a semi-structured format to describe the scene in the picture, including what characters are thinking or feeling, and what they think might happen next. Three core sentences that represented the attachment pattern of the participants were extracted from the audiotaped responses to each AAP picture stimulus by two independent certified judges (e.g., “A girl is incarcerated in that big room,” “My mother suffered until the end and the ambulance came often”). These sentences were paired to the respective picture to constitute the “personally relevant” trials tailored to each participant. These same pictures, paired to sentences describing only the environment of the depicted situation (e.g., “There is a window with curtains on the left and right,” “There is a bed with a big blanket”) constituted the “neutral” trials (see also Buchheim et al., 2012 ).
NEUROIMAGING OUTCOME VARIABLES
The neuroimaging session took place on the same day as the recorded psychotherapy hour. It consisted of the task in the scanner and in the administration of a rating instrument to assess the patient’s reaction to the items presented in the scanner.
Neuroimaging task
In each trial, the patient looked at pictures of attachment-relevant AAP scenes, accompanied by a short descriptive text. Each picture was presented for 20 s, followed by a fixation point for about the same duration ( Figure Figure1 1 ). The AAP consists of a set of seven of such pictures; this set was repeated 12 times, for a total of 84 trials. Repetitions of the set were divided into two groups: those in which the descriptive text was a neutral rendering of the figures appearing in the scene ( neutral trials ), and those where the description was tailored to core conflicts of the patient as assessed in the initial AAP interview ( personally relevant trials ).

Schematic representation of the AAP scenes and sentences used in the functional neuroimaging study (example of a personalized trial) .
Image acquisition
MRI data were recorded using a 3-T Magnetom Allegra head scanner (Siemens, Erlangen, Germany), equipped with a standard head coil. In each session, 508 EPI T 2 *-weighted whole brain volumes were acquired (TR/TE = 2500/30 ms, flip angle 90°, FOV 192 mm, matrix 64 × 64, voxel size 3 mm × 3 mm, slice thickness 3 mm, 44 slices, standard AC–PC orientation). Sessions were repeated in monthly intervals for a year, for a total of 12 sessions.
Preprocessing and statistical analysis of neuroimaging data
Data were analyzed with the Statistical Parametric Mapping (SPM) package ( Frackowiak et al., 2003 ), using a voxelwise approach. After realignment and normalization into Montreal Neurological Institute (MNI) space, volumes were smoothed with a Gaussian isotropic kernel (8 mm full width-half maximum). The blood oxygenation level-dependent (BOLD) response function was modeled by convolving the trial onsets with a standard hemodynamic response function. Effects of interest were estimated for each session separately (in a model that included presentation of the scene + textual description combination and whether the combination was personalized or not) and brought to the second level to account for a random effect of sessions ( Penny and Holmes, 2007 ). At the second level, main effects were tested with one-sample t -tests. The interaction between quality of the hour and personalized effect was given by an additional second-level regressor indicating whether the hour was “easy” or “difficult.” This regressor is orthogonal to the one-sample t -test of the personalized effect ( Viviani, 2010 ).
The main effect of interest of the study was given by the contrast personally relevant vs. neutral, and its interaction with the index of the quality of the session, as indicated by the therapist and its operational characterization through the PQS scores. To identify regions associated with the presentation of the personalized trials, we performed a whole-brain estimation of the model voxel by voxel. The significance levels reported in the text of section “Results” are corrected at cluster level ( Poline and Mazoyer, 1993 ; Friston et al., 1994 ) for the whole volume.
The post-scan self-rating scales were analyzed separately from neuroimaging data using the freely available package R (The R Foundation for Statistical Computing, www.r-project.org , Vienna, Austria; repeated measures regression: function lmer , package lme4, version 2.13.1; Bates and Maechler, 2009 ). The dependent variable (emotional involvement or extent of autobiographical character of the scene–sentence couple) was modeled in a repeated measurements linear model as an effect of the hour character (“easy” or “difficult”) and the personally relevant AAP scene as fixed effects, and the session and the sentences as grouping variables for the random effects.
CLINICAL DESCRIPTION OF THE PATIENT
The patient, a 42-years-old lawyer, suffered since the birth of her first daughter from rapidly fluctuating affective states. From a clinical point of view, the patients had a moderate functioning level. During the so-called “difficult day”-states she isolated herself and tended to withdraw herself in relationships and hide her emotional vulnerability in contrast to the so-called “easy days”-states, where the patient felt self-conscious and full of personal strength. Regarding her personality structure she showed some narcissistic features ( Kernberg, 1984 ; Cain et al., 2008 ; Pincus and Lukowitsky, 2010 ), being self-centered and rather achievement oriented. She defined herself frequently via money, success, and reputation. When she felt in her job that clients were not as satisfied with her work as she expected from herself she broke down and was ruminating anxiously if they will come back. This pattern demonstrated that her self-esteem fluctuated according to the gratifying or frustrating experiences in relationships and how she evaluated the distance between the goals and aspirations. Because of her harsh super-ego demand for perfection she was in an instable inner state and self-esteem could be diminished rapidly.
The patient lived in a long-lasting relationship. However, she characterized the relationship with her husband as competitive with respect to their tendency to experience rivalry and envy. Moreover, there was a clear discrepancy between her self-perception and the perception that significant others had of the patient. Although easier days were subjectively felt more pleasant by the patient, her husband reportedly found it very difficult to deal with her. This often led to constant, seemingly unsolvable conflicts and to repeatedly considering separation.
One of her major unconscious defensive structure seemed to circle around fantasies of success and grandiosity, leading to her dependency to be admired by others and to bouts of insecurity disrupting her sense of grandiosity or specialness (for a description of the related dynamic, see Kernberg and Yeomans, 2013 ).
According to the observations of the analyst collected over 1 year of clinical work, the following topics may be considered key to the psychodynamic understanding of the patient and her treatment:
1. On “difficult” days the patient showed a severely inhibited capacity to think and to express feelings and thoughts and fell into silence. On “easy” days the patient talked expansively and her personality appeared strong.
2. The association of the fluctuating symptoms with unresolved loss experiences and fear due to uncontrollable guilt-feelings.
As we shall see later, these two core issues could be retrieved in the formal assessment of the interaction between the patient and the therapist using the PQS methodology.
From a psychodynamic and biographic perspective the analyst suggested that two events of death were useful to understand the nature of the patient’s symptoms. These events revealed the underlying vulnerability of the patient with respect to this issue and the related latent feelings of helplessness and impotence. When the patient was 30-years old her mother died unexpectedly. She felt guilty, because she was unable to call the emergency doctor in time. Moreover, the tragic loss through death of a colleague some years previously coincided with the birth of her first child, a son. Again the patient felt guilty, because she was not able to reach her colleague in time to be able to help her. Her fluctuating depressive symptoms might be interpreted as the outcome of this defensive structure. On “easy days” her functioning was predominantly characterized by externalization with an increase of activity and personal strength, while on “difficult days” internalization led to inhibition of activity and severe self-doubts. These latter phases were characterized by affective distance between the patient and her object world in an effort to preserve the illusion of control relative to object loss ( Modell, 1975 ).
Since the patient demonstrated a complex chronic affective disorder with difficult personality traits and a rigid defensive structure, there was an indication for long-term psychoanalytic treatment with two sessions per week ( Leichsenring and Rabung, 2011 ). The treatment setting was face-to-face, thus creating a positive stable counterpole to her mood changes. The positive stabilizing effect of the therapy was noticeable early in the treatment even though the total process was taking a very long time. The treatment centered on the deeper understanding of her uncontrollable mood-shifts and her impaired self-perception and perception of others. The question of failure and/or the continuing of the analytic work were constantly present. The transference relationship was mirrored by her experiences of loss: she failed to prevent the unexpected deaths, and for a long time the analyst and the patient failed to prevent the unexpected mood-shifts and to find ways how she could regulate and stabilize her affective instability. Gradually, the patients internalized a better perception of herself and it became easier for the patient to succeed regulating her mood toward the state characterizing “easy” days. One major focus of the treatment was to increase the patient’s ability to react timely in case of severe events like illness or death, and therefore to be able to process these potential traumatic events in a more controlled and integrated way.

ATTACHMENT DATA
The patient was administered the AAP interview at the beginning of the fMRI experiments and 1 year later. The AAP interview had two purposes. On the one hand we assessed the patient’s attachment representation at the beginning of the fMRI assessment and on the other hand we extracted core sentences of the patient’s narratives in the AAP interview as the personalized stimulus material in the fMRI setting (see Section “Neuroimaging Task”). The patient was classified as unresolved (i.e., disorganized). Unresolved stories typically leave characters without protection, describe feelings of extreme mental distress that have not been diminished or transformed, or leave threatening images looming without addressing them further. The patient demonstrated a lack of resolution especially in the AAP Picture “Cemetery” where the loss of the father was associated with mourning, loneliness and a present dialogue with the dead father, which indicated a spectral quality.
ANALYSIS OF SELF-RATING SCALES
Analysis of the CIPS-depressiveness score gave a mean value of 12.2 (SD 5.2, range 8–19), indicating affective symptoms of moderate intensity. The regression of the scores over time failed to demonstrate the existence of changes. Nominally, in the examined monthly sessions the patient became more depressed during the year she was monitored ( Figure Figure2 2 ), but the result was far from significant ( t = 1.05; df = 10, p = 0.34, two-tailed).

Plot of depressiveness scores ( y -axis) over the 12 months of the study ( x -axis) .
The general burden of symptom, as measured by the OQ subscale, was on average 41.75 (SD 5.0, range 33.53), indicating alternating degree of symptom severities crossing the line of norm values ( Haug et al., 2004 ). Like depressiveness, the symptom burden also increased lightly, but not significantly, during this period ( t = 1.16, df = 10, p = 0.27, two-tailed).
The analysis of the PQS scores took place in three steps. In the first step, we undertook an explorative analysis to answer the question of whether there were consistent changes over therapy hours across different items of the PQS, by carrying out a principal component analysis of the PQS scores. This analysis aimed at detecting items that were high or low together in the same hour, without imposing a priori constraints on what these items should be, as would be the case if items had been grouped into preformed scores. We also looked at whether these changes were consistent with a linear trend (i.e., a gradual change over time). In the second step, we looked at the existence of items that were associated with the analyst’s classification of the hours in good and bad. In the final step, we looked at whether changes detected during the explorative analysis related to the changes associated with the analyst’s judgment.
In the principal component analysis of PQS scores, the first detected component, which explained about 32% of the variance of PQS items over time, was highly significant ( p < 0.001). A second component only reached trend significance ( p = 0.06), explaining 16.7% of the overall variance over time. Further components, explaining 13% of the variance of less, failed to reach significance even at trend level. The 10 items scoring highest in the first and second components are shown in Table Table1 1 .
Ten highest scoring items from the principal component analysis of the PQS.
Several items in the principal component analysis scored negative values. The PQS manual contains specific indications to score items as distinctively low. In the first component, a low score on item 54 is given for rambling or incoherent communications, and on item 23 for lack of a guiding discourse thread; on item 13 for the patients appearing bored or dull, and on item 74 grave or somber. Considered together with items with high scores (whose interpretation is immediate), they show that component one prevalently collected items suggesting difficult or inhibited communication of the patient toward the analyst, with frequent phases of silence. These occurred together with other items suggesting the presence of a tense, sober mood (items 7, 13, 74).
The second component appears to characterize form and content of the intervention of the analyst (items 31, 40, 45, 63, 66) and the sometimes difficult reaction of the patient to them (items 1, 49, 95).
We then tested the existence of a linear trend in the changes over time in these component scores. This would have been the case, for example, if the character of the hours changed over the year of therapy, and these components reflected this systematic change. However, the regression of the component scores on the time trend was not significant (first component: t = 0.99, df = 9, p = 0.35, two-tailed; second component: t = 0.82, df = 9, p = 0.43, two-tailed), suggesting that they did not change over time ( Figure Figure3 3 ). Even if the main components did not appear to reflect a change over time, it is conceivable that some other isolated item did. To verify this hypothesis, we tested the regression of each item score over time separately, correcting the significance level for the 100 tests. Also this analysis failed to detect items reflecting a change over the year of therapy. The item that was most associated with time was item 76 (“Therapist suggests that patient accept responsibility for his or her problems,” which however failed to reach significance ( t = 4.22, p = 0.14, two-tailed corrected for multiple comparisons). In summary, change over time in the PQS scores did not document a systematic change after 1 year of therapy relative to the beginning of the monitoring period.

Plot of first component scores over time, together with the respective linear trends (on the x -axis by the monthly session). In blue, first component scores; in green, second component scores. Both component scores display a small tendency to increase over time, which however was not significant.
In the second step of the analysis we looked at the existence of items that were associated with the analyst’s classification of the hours in “easy” and “difficult.” Both easy and difficult hours occurred during this year, and a logistic regression of the occurrence of easy hours over time showed the absence of a significant time trend ( z = -0.53, p = 0.60). The separate regression of each PQS item on the analyst indicator of the quality of the hour detected three significant items, after correcting significance levels for multiple comparisons: item 12 (“Silences occur during the hour”), t = -9.16, p = 0.004 (two-tailed, corrected); item 61 (“Patient feels shy and embarrassed (vs. un-self-conscious and assured.),” t = -5.76, p = 0.03; item 54 (“Patient is clear and organized in self-expression”), t = 5.39, p = 0.04. A fourth item reached trend significance, item 7 (“Patient is anxious or tense (vs. calm and relaxed).”), t = -4.95, p = 0.063.
Finally, we looked at whether changes detected during the explorative principal component analysis in the form of component scores related to the changes associated with the analyst’s judgment. There was a significant association between the first component scores and the analyst’s indicator of the quality of the hour ( t = -5.03, df = 9, p = 0.0006). The second component, in contrast, was not significantly associated ( t = 1.01, df = 9, p = 0.33).
In summary, there was at least one set of PQS items that changed together across therapy hours. These changes were not associated with a time trend, indicating stability of the underlying psychotherapy pattern; however, they were associated with the occurrence of “easy” and “difficult” days. This result did not change if the PQS items were regressed individually on time and day difficulty.
CORE PSYCHODYNAMIC FEATURES OF THE PATIENT AND PQS RESULTS: AN EXPLORATORY COMPARISON
We compared the clinical features of “difficult” and “easy” days with the first component from the PQS, obtained independently from information on the day difficulty (see Table Table2 2 ). This comparison revealed convergent patterns. The clinical description of the analyst, emphasizing the difficulties of expression of the patient, is consistent with the items in the first component detailing inhibited communication, silence, or ineffective content on difficult days. The identification by the analyst of unresolved feelings of loss corresponds to the items related to tense and sober mood. We conclude that the PQS analysis could validate the subjective evaluations of the analyst.
Clinical characteristics compared to PQS-items (principal component analysis).
ANALYSIS OF POST-SCAN SELF-RATING QUESTIONNAIRE
The patient was asked after each fMRI session to rate personalized sentences from the fMRI task with respect of self-involvement and autobiographical content (see Section “Materials and Methods”). The analysis of emotional self-involvement revealed that the rating was on the whole significantly higher in the fMRI sessions that followed “easy” therapy hours ( t = 2.08, df = 9, p = 0.03, one-tailed). This result did not change if the autobiographical rating was added as a confounding covariate to the model ( t = 2.08). This expanded model also revealed that the autobiographical rating was in the individual items associated with the level of emotional involvement rating ( t = 3.9, df = 193, p < 0.001). In contrast, there was no significant change in ratings of the autobiographical character of the personalized sentences in association of the quality of the hour ( t = 1.27, df = 9, p = 0.12 one-tailed).
In summary, these self-rating data confirmed the existence of a qualitative difference between “easy” and “difficult” days that involved the stimuli presented in the scanner through the tendency of a higher self-rated emotional involvement on “easy” days. However, over and above this association, there was an even stronger association at each individual rating between the level of self-involvement and the level of autobiographical character of the scene + text combination.
NEUROIMAGING RESULTS
When viewing the pictures described by personalized text, relative to those with neutral descriptions, the patient activated several areas, prevalently on the left. The most prominent activations involved the ventrolateral and the dorsolateral prefrontal cortex, the perigenual portion of the medial prefrontal cortex, the posterior cingulate and precuneus, the middle temporal gyrus, and the anterior tip of the inferior temporal gyrus, and the occipital/calcarine cortex (see Figure Figure4A 4A and Table Table3 3 ). No area was significantly more active when looking at the neutral scenes.

(A) Parametric maps of activations detected in the personally relevant vs. neutral contrast, overlaid on a template image. (B) Parametric maps of the interaction of the same contrast with hour quality, as rated by the therapist. Slices positioned at MNI coordinates x = -6 (left) and z = 40 (right). For illustration purposes, the parametric map was thresholded at p < 0.005, uncorrected, and a cluster size of 150 voxels (1.2 cm 3 ). a, precuneus and posterior cingulate, active at both the contrast personally relevant vs. neutral and its interaction with hour quality; b, calcarine cortex; c, perigenual medial prefrontal cortex; d, dorsolateral prefrontal cortex. Areas a and c (labeled in green) belong to the “default network system”; area d to the dorsal attentional network (in blue). The red label b refers to primary visual areas.
Activations for the contrast personalized vs. neutral.
The interaction of the effect of personal relevance with goodness of therapy hours was significant in the posterior cingulate/precuneal region (MNI coordinates, x , y , z : -6, -60, 40, t = 6.7, cluster size in voxels: 633, p = 0.017). Here, the signal while looking at personalized scenes was higher when the therapy hour was bad. This area, shown in Figure Figure1B 1B , was part of the medial prefrontal network that was associated with viewing personalized scenes ( Figure Figure1A 1A ). Other, smaller areas detected in the interaction failed to reach significance. No significant interaction was observed in the opposite direction.
We also tested the interaction between the effect of personal relevance and a linear time trend, to detect changes in activation that developed during the year of therapy. In the interaction with the positive time trend, a cluster extending from the left post-central gyrus to the middle frontal gyrus was significant (MNI coordinates, x , y , z : -54, -12, 40, t = 10.2, cluster size in voxels: 1410, p < 0.001). This interaction partially overlapped with the prefrontal interaction in Figure Figure4A 4A (d, dorsolateral prefrontal cortex). No effect was observed in the interaction with a negative time trend.
Recently, the issue of the relationship between Freudian thought or psychoanalytic theory and technique more generally and neuroscience has been the object of renewed interest ( Carhart-Harris et al., 2008 ; Carhart-Harris and Friston, 2010 ; Solms and Panksepp, 2012 ; Zellner, 2012 ; Schmeing et al., 2013 ). In the present study, we attempted to integrate a clinical description of the psychoanalytic process with two empirical instruments, one providing an operationalized assessment of the therapeutic interaction, and the other information on brain activity based on a functional neuroimaging probe. Our aim was to explore the extent to which the two main mental states of the patient and their effect on the psychoanalytic interaction could be observed not only at the clinical level, but also through the data delivered by these two additional instruments.
Analysis of the symptomatic scales gave the picture of a patient with affective symptom severity of moderate intensity, occurring in a patient with a personality with narcissistic features, as described in detail in Section “Results.” The unresolved attachment pattern emerging from the AAP interview is consistent with the analyst’s clinical presentation and with recent attachment data on patients, comorbid with borderline personality disorder and narcissistic personality disorder ( Diamond et al., 2012 ).
The analysis of the PQS data showed that sessions differed along a main axis, defined by the first component. This component was highly correlated with the judgment of the analyst on the quality of the sessions. This analysis revealed that “easy” hours were associated with items describing the deeper understanding of relationship issues, “difficult” hours with silence in the therapy hours and difficulties of the patient to feel at ease. Furthermore, there was no evidence in the PQS data of a linear trend over time that reflected systematic changes from the initial to the final phases of the year monitored by the study. In summary, the main change across sessions present in the PQS data was the one documented by the analyst through her judgment in a phase of therapy where the patient remained stable. This source of change was not associated with a time trend, as “easy” or “difficult” days did not occur more often at the beginning or end of the observation year. This allows excluding the confounds of habituation or learning effects from the regressor representing quality of the hour.
The activation pattern in the contrast of the main effect personally relevant vs. neutral ( Figure Figure4A 4A ) was characterized by the presence of two main groups of areas. The first included areas that are often active in functional neuroimaging studies and that are known to be active while carrying out a focused task ( Duncan and Owen, 2000 ). This group includes the ventrolateral and the dorsolateral prefrontal cortex, and the occipital/calcarine cortex (for visually presented stimuli). The second group may be considered more specific for the material used in the present study, and included areas in the medial wall (anterior cingulate, and the posterior cingulate and precuneus). The activation pattern of these areas was consistent with the activation found in studies in the literature in which participants were asked to judge the degree to which stimuli presented during the scan were attributed to the self, or were felt to be part on oneself/one’s own description ( Figure Figure5 5 ; for a systematic review and meta-analysis of the literature, see van der Meer et al., 2010 ; Qin and Northoff, 2011 ). The medial prefrontal cortex may also be associated with changes after the therapy of affective disorders ( Messina et al., 2013 ). We therefore considered the areas in this second group as those most likely involved in processing the personally relevant content of the stimuli.

Areas in the medial face of the brain associated with self-representation. This image synthesizes data in the neuroimaging literature of studies concerned with self-referentiality using automated keyword search and meta-analytic methods (from www.neurosynth.org , search key “self-referential”; Yarkoni et al., 2011 ). Slices positioned at MNI coordinates x = -6 (left) and z = 40 (right). The comparison with the activation detected in the study in the contrast personally relevant vs. neutral contrast ( Figure Figure4 4 ) shows correspondence of activation in the areas in the medial aspect of the brain: the precuneus and posterior cingulate (a) and the perigenual medial prefrontal cortex (c).
Within this pattern of activation of areas associated to the self and personal relevance, the posterior cingulate cortex was modulated by the interaction with the quality of the therapy hours that had immediately preceded the scan. This association represent evidence of a neural substrates accompanying opposing mental states that, as shown in the self-rating scales, the judgment of the analyst on the quality of the hour, and the formal instrument for assessing the therapeutic exchange, represented a coherent constellation of internally experienced and interpersonally exchanged affect.
The posterior cingulate cortex has been shown in other studies to be modulated by self-distancing from negatively valenced pictures presented during the scan ( Koenigsberg et al., 2010 ) or when down-regulating the reaction to a negative stimulus by self-distraction ( Kanske et al., 2011 ). Of particular interest in the present context is the study by van Reekum et al. (2007) , in which gaze fixations were recorded while participants viewed aversive scenes and were left free to choose the down-regulating strategy. This area highly correlated with the amount of eye movements of the participants, who were directing their gaze so as to avoid the focal area of the image where the disturbing content was represented. This area was also reported to be active in regulation strategies adopted by patients with personality disorders characterized by poor emotion regulation ( Koenigsberg et al., 2009 ; Doering et al., 2012 ; Lang et al., 2012 ).
The self-rating data collected after the scan confirmed the association between the enactment of a self-distancing strategy from the material and the quality of the hour. On “difficult” days, the patient indicated that her overall emotional involvement with the visuotextual material was lower than on the “easy” days. This corresponded to a higher activity in the posterior cingulate area, associated in the previous studies with self-distancing emotion regulation strategies. In view of the documented association between the quality of the hour and the quality of the interaction with the therapist, and the clinical judgment of the therapist himself, the present study provides evidence on the possible involvement of the posterior cingulate area in spontaneously enacted self-distancing emotion-handling strategies representing defensive maneuvers in the course of a psychoanalytic therapy.
Among the areas active in the contrast personally relevant vs. neutral there were also areas prevalently involved in attentional processes (dorsolateral prefrontal cortex; Figure Figure4A 4A letter c). Also this area was modulated during the year of therapy, showing a progressive increase of the signal due to personally relevant trials. This suggests a dissociation of the areas detected in the contrast personally relevant vs. neutral, with the posterior medial area associating with quality of the hour, and the dorsolateral prefrontal areas associating with change over time. The change over time in the dorsolateral prefrontal cortex might be due to a progressive loss of attentional pull of the non-relevant trials, or to the increased recruitment of attentional resources in looking at scenes in the personally relevant trials. From a clinical point of view it could mean that the patient was more effective in appraising and reflecting on her own personal core attachment-related issues.
There are several noteworthy limitations of this study. First, treatment did not follow a manualized psychoanalytic psychotherapy. However, it was conducted by adhering to specific core techniques, as described in section “Materials and Methods,” by a very experienced psychoanalyst. Second, in the attachment paradigm used in the scanner no pictures without attachment content were present. This is consistent with the choice to investigate personal relevance in the context of material likely to evoke core emotional issues, as in previous work ( Buchheim et al., 2012 ). Future work will have to address the issue of the neural response to attachment pictures of the kind used in the AAP in comparison with neutral pictures of similar content and complexity, but differing attachment relevance and interpersonal quality or emotionality, and its capacity to capture affective psychopathology. Third, the fluctuation between two cognitive–emotional states (easy and difficult days, easy and difficult sessions) may have been indicative of pattern transitions that may be analyzed with approaches focusing on self-organization and non-linear dynamics in psychotherapy (see e.g., Boston Change Process Study Group, 2005 ; Schiepek et al., 2009 , 2013 ). However, this aspect of the psychotherapeutic interaction fell outside of the scope of the present study.
In summary, this case report gives indications on the interplay between activity in neural circuits and quality of the psychotherapeutic sessions in the context of psychoanalytic process research. In this specific single case, major characteristics of the patient’s defensive structure could be demonstrated on a behavioral and neural level and validated the subjective evaluation of the analyst. Specifically, affective distancing has been identified in the literature as a hallmark defensive maneuver in personality organization with narcissistic traits ( Modell, 1975 ). Using functional neuroimaging, we were able to objectify the defensive structure of this patient during this phase of psychoanalytic treatment and the occurrence of difficult sessions.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was in part funded by the German Psychoanalytic Association, whose generous support is here gratefully acknowledged. The authors declare no conflict of interest. We thank Prof. Dr. Horst Kächele, International Psychoanalytic University Berlin, for his encouragement and the inspiration for initiating this research. We are also grateful to Dr. Carolina Seybert, International Psychoanalytic University Berlin, for training and supervising the PQS scoring.
- Albani C., Ablon S., Kächele H. (2007). Der “Psychotherapie Prozess Q-Set” von Enrico E. Jones . Deutsche Version und Anwendungen . Ulm: Ulmer Textbank [ Google Scholar ]
- Bates D. M., Maechler M. (2009). lme4: Linear Mixed-effects Models Using S4 Classes. R Package Version 0.999375-31. Available at: http://CRAN.R-project.org/package=lme4 (accessed December 12, 2011) [ Google Scholar ]
- Blair R. C., Higgins J. J., Karniski W., Kromrey J. D. (1994). A study of multivariate permutation tests which may replace Hotelling’s T2 test in prescribed circumstances. Multivariate Behav. Res. 29 141–163 10.1207/s15327906mbr2902_2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boston Change Process Study Group. (2005). The “something more” than interpretation revisited: sloppiness and co-creativity in the psychoanalytic encounter. J. Am. Psychoanal. Assoc. 53 693–729 10.1177/00030651050530030401 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buchheim A., Erk S., George C., Kächele H., Kircher T., Martius P., et al. (2008). Neural correlates of attachment trauma in borderline personality disorder: a functional magnetic resonance imaging study. Psychiatry Res. 163 223–235 10.1016/j.pscychresns.2007.07.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buchheim A., Erk S., George C., Kächele H., Ruchsow M., Spitzer M., et al. (2006). Measuring attachment representation in an fMRI environment: a pilot study. Psychopathology 39 144–152 10.1159/000091800 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buchheim A., Viviani R., Kessler H., Kächele H., Cierpka M., Roth G., et al. (2012). Changes in prefrontal-limbic function in major depression after 15 months of long-term psychotherapy. PLoS ONE 7 : e33745 10.1371/journal.pone.0033745 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cain N. M., Pincus A. L., Ansell E. B. (2008). Narcissism at the crossroads: phenotypic description of pathological narcissism across clinical theory, social/personality psychology, and psychiatric diagnosis. Clin. Psychol. Rev. 28 638–656 10.1016/j.cpr.2007.09.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carhart-Harris R. L., Friston K. J. (2010). The default mode, ego-functions and free-energy: a neurobiological account of Freudian ideas. Brain 133 1265–1283 10.1093/brain/awq010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carhart-Harris R. L., Mayberg H. S., Malizia A. L., Nutt D. (2008). Mourning and melancholia revisited: correspondence between principles of Freudian metapsychology and empirical findings in neuropsychiatry. Ann. Gen. Psychiatry 7 9 10.1186/1744-859X-7-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Diamond D., Clarkin J., Horz S., Levy K., Fisher-Kern M., Cain N., et al. (2012). Attachment and reflective function in patients with co-morbid NPD/BPD. Paper presented at the 2nd International Congress on Borderline Personality Disorder and Allied Disorders Amsterdam, The Netherlands: September 29, 2012 [ Google Scholar ]
- Doering S., Enzi B., Faber C., Hinrichs J., Bahmer J., Northoff G. (2012). Personality functioning and the cortical midline structures. An exploratory fMRI study. PLoS ONE 7 : e49956 10.1371/journal.pone.0049956 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donnellan G. J. (1978). Single-subject research and psychoanalytic theory. Bull. Menninger Clin. 42 352–357 [ PubMed ] [ Google Scholar ]
- Dreyer K.-A., Schmidt M. G. (2008). Niederfrequente psychoanalytische Psychotherapie . Theorie, Technik, Therapie Stuttgart: Klett Cotta [ Google Scholar ]
- Duncan J., Owen A. M. (2000). Common regions of the human frontal lobe recruited by diverse cognitive demands. Trends Neurosci. 23 475–483 10.1016/S0166-2236(00)01633-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Edelson M. (1985). The hermeneutic turn and the single case study in psychoanalysis. Psychoanal. Contemp. Thought 8 567–614 [ Google Scholar ]
- Edelson M. (1988). Psychoanalysis: A Theory in Crisis . Chicago: University of Chicago Press [ Google Scholar ]
- Fonagy P., György G, Elliot L. J., Target M. (2004). Affect Regulation, Mentalization, and the Development of the Self . New York: Other Press [ Google Scholar ]
- Fonagy P., Kächele H. (2009). “Psychoanalysis and other long-term dynamic psychotherapies,” in New Oxford Textbook of Psychiatry 2nd Edn. Vol. 2 eds Gelder M. G., Lopez-Ibor J. J., Andreasen N. (Oxford University Press; ) 1337–1349 [ Google Scholar ]
- Frackowiak R. S. J., Friston K. J., Frith C., Dolan R., Price C. J., Zeki S., et al. (2003). Human Brain Function . London: Academic Press [ Google Scholar ]
- Friston K. J., Worsley K. J., Frackowiak R. S. J., Mazziotta J. C., Evans A. C. (1994). Assessing the significance of focal activations using their spatial extent. Hum. Brain Mapp. 1 214–220 [ PubMed ] [ Google Scholar ]
- Gabbard G. O., Gunderson J. G., Fonagy P. (2002). The place of psychoanalytic treatments within psychiatry. Arch. Gen. Psychiatry 59 505–510 10.1001/archpsyc.59.6.505 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- George C., West M. (2012). The Adult Attachment Projective Picture System. Attachment Theory and Assessment in Adults . New York: The Guilford Press [ Google Scholar ]
- Gullestad F., Wilberg T. (2011). Change in reflective functioning during psychotherapy: a single-case study. Psychother. Res. 21 97–111 10.1080/10503307.2010.525759 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haug S., Puschner B., Lambert M. J., Kordy H. (2004). Veränderungsmessung in der Psychotherapie mit dem Ergebnisfragebogen (EB-45). Z. Differentielle Diagn. Psychol. 25 141–151 10.1024/0170-1789.25.3.141 [ CrossRef ] [ Google Scholar ]
- Hilliard R. B. (1993). Single-case methodology in psychotherapy process and outcome research. J. Cogn. Clin. Psychol. 61 373–380 10.1037/0022-006X.61.3.373 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones E. E. (2000). Therapeutic Action. A Guide to Psychoanalytic Therapy . Nothvale, NJ: Jason Aronson Inc [ Google Scholar ]
- Kächele H., Albani C., Buchheim A., Hölzer M., Hohage R., Jimenez J. P., et al. (2006). The German specimen case amalia X: empirical studies. Int. J. Psychoanal. 87 1–18 10.1007/3-540-29882-7_1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kächele H., Schachter J., Thomä H. (eds) (2009). .From Psychoanalytic Narrative to Empirical Single Case Research. Implications for Psychoanalytic Practice . New York: Routledgse [ Google Scholar ]
- Kanske P., Heissler J., Schönfelder S., Bongers A., Wessa M. (2011). How to regulate emotion? Neural networks for reappraisal and distraction. Cereb. Cortex 21 1379–1388 10.1093/cercor/bhq216 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kazdin A. E. (1982). Single Case Research Designs: Methods for Clinical and Applied Settings . Oxford: Oxford University Press [ Google Scholar ]
- Kernberg O. F. (1984). Severe Personality Disorders: Psychotherapeutic Strategies . New Haven, CT: Yale University Press; 10.1521/bumc.2013.77.1.1 [ CrossRef ] [ Google Scholar ]
- Kernberg O. F., Yeomans F. E. (2013). Borderline personality disorder, bipolar disorder, depression, attention deficit/hyperactivity disorder, and narcissistic personality disorder: practical differential diagnosis. Bull. Menninger Clin. 77 1–22 [ PubMed ] [ Google Scholar ]
- Koenigsberg H. W., Fan J., Ochsner K. N., Liu X., Guise K., Pizzarello S., et al. (2010). Neural correlates of using distancing to regulate emotional responses to social situations. Neuropsychologia 48 1813–1822 10.1016/j.neuropsychologia.2010.03.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koenigsberg H. W., Fan J., Ochsner K. N., Liu X., Guise K. G., Pizzarello S., et al. (2009). Neural correlates of the use of psychological distancing to regulate responses to negative social cues: a study of patients with borderline personality disorder. Biol. Psychiatry 66 854–863 10.1016/j.biopsych.2009.06.010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lang S., Kotchoubey B., Frick C., Spitzer C., Grabe H. J., Barnow S. (2012). Cognitive reappraisal in trauma-exposed women with borderline personality disorder. Neuroimage 59 1727–1734 10.1016/j.neuroimage.2011.08.061 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leichsenring F., Rabung S. (2008). Effectiveness of long-term psychodynamic psychotherapy: a meta-analysis. JAMA 13 1551–1565 10.1001/jama.300.13.1551 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leichsenring F., Rabung S. (2011). Long-term psychodynamic psychotherapy in complex mental disorders: update of a meta-analysis. Br. J. Psychiatry 199 15–22 10.1192/bjp.bp.110.082776 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leichsenring F., Rabung S., Leibing E. (2004). The efficacy of short-term psychodynamic psychotherapy in specific psychiatric disorders. A meta-analysis. Arch. Gen. Psychiatry 61 1208–1216 10.1001/archpsyc.61.12.1208 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levy R. A., Ablon J., Thomae H., Kaechele M. D., Ackerman H., Erhardt I., et al. (2012). “A session of psychoanalysis as analyzed by the psychotherapy process Q-set: Amalia X, session 152,” in Psychodynamic Psychotherapy Research: Practice Based Evidence and Evidence Based Practice eds Raymond A., Levy J., Ablon S., Kaechele H. (New York: Springer) [ Google Scholar ]
- Mergenthaler E., chele H. (1996). Applying multiple computerized text-analytic measures to single psychotherapy cases. J. Psychother. Pract. Res. 5 307–317 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Messina I., Sambin M., Palmieri A., Viviani R. (2013). Neural correlates of psychotherapy in anxiety and depression: a meta-analysis. PLoS ONE 8 : e74657 10.1371/journal.pone.0074657 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Modell A. H. (1975). A narcissistic defence against affects and the illusion of self-sufficiency. Int. J. Psycho-Anal. 56 275–282 [ PubMed ] [ Google Scholar ]
- Ogden T. H. (1977). Projective Identification and Psychotherapeutic Technique . Lanham, MD: Jason Aronson [ Google Scholar ]
- Ogden T. H. (1989). The Primitive Edge of Experience . Northvale, NJ: Jason Aronson [ Google Scholar ]
- Orlinsky D. E., Ronnestad M. H., Willutzki U. (2004). “Fifty years of psychotherapy process-outcome research: continuity and change,” in Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change ed. Lambert M. J. (New Jersey: Wiley & Sons; ) 307–389 [ Google Scholar ]
- Penny W. D., Holmes A. J. (2007). “Random-effects analysis,” in Human Brain Function eds Frackowiak R. S., Friston K. J., Frith C. D., Dolan R. J., Price C. J., Zeki S., Ashburner J., Penny W. D. (San Diego: Elsevier Academic Press; ) 156–165 [ Google Scholar ]
- Pincus A. L., Lukowitsky M. R. (2010). Pathological narcissism and narcissistic personality disorder. Annu. Rev. Clin. Psychol. 6 421–446 10.1146/annurev.clinpsy.121208.131215 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Poline J.-B., Mazoyer B. M. (1993). Analysis of individual positron emission tomography activation maps by detection of high signal-to-noise pixel clusters. J. Cereb. Blood Flow Metab. 13 425–437 10.1038/jcbfm.1993.57 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qin P., Northoff G. (2011). How is our self related to midline regions and the default-mode network? Neuroimage 57 1221–1233 10.1016/j.neuroimage.2011.05.028 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schiepek G., Tominschek I., Karch S., Lutz J., Mulert C., Meindl T., et al. (2009). A controlled single case study with repeated fMRI measures during the treatment of a patient with obsessive-compulsive disorder: testing the nonlinear dynamics approach to psychotherapy. World J. Biol. Psychiatry 10 658–668 10.1080/15622970802311829 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schiepek G., Tominschek I., Heinzel S., Aigner M., Dold M., Unger A., et al. (2013). Discontinuous patterns of brain activation in the psychotherapy process of obsessive compulsive disorder: converging results from repeated fMRI and daily self-reports. PLoS ONE 8 : e71863 10.1371/journal.pone.0071863 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shedler J. (2010). The efficacy of psychodynamic psychotherapy. Am. Psychol. 65 98–109 10.1037/a0018378 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmeing J. B., Kehyayan A., Kessler H., Do Lam A. T. A., Fell J., Schmidt A. C., et al. (2013). Can the neural basis of repression be studies in the MRI scanner? New insights from two free association paradigms. PLoS ONE 8 : e62358 10.1371/journal.pone.0062358 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Solms M., Panksepp J. (2012). The ‘Id’ knows more than the ‘ego’ admits: neuropsychoanalytic and primal consciousness perspectives on the interface between affective and cognitive neuroscience. Brain Sci. 2 147–175 10.3390/brainsci2020147 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van der Meer L., Costafreda S., Aleman A., David A. S. (2010). Self-reflection and the brain: a theoretical review and meta-analysis of neuroimaging studies with implications for schizophrenia. Neurosci. Biobehav. Rev. 34 935–946 10.1016/j.neubiorev.2009.12.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van Reekum C. M., Johnstone T., Urry H. L., Thurow M. E., Schaefer H. S., Alexander A. L., et al. (2007). Gaze fixations predict brain activation during the voluntary regulation of picture-induced negative affect. Neuroimage 36 1041–1055 10.1016/j.neuroimage.2007.03.052 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Viviani R. (2010). Unbiased ROI selection in neuroimaging studies of individual differences. Neuroimage 50 184–189 10.1016/j.neuroimage.2009.10.085 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wallerstein R. S., Sampson H. (1971). Issues in research in the psychoanalytic process. Int. J. Psychoanal. 52 11–50 [ PubMed ] [ Google Scholar ]
- Yarkoni T., Poldrack R. A., Nichols T. N., Van E. D. C., Wager T. D. (2011). Large-scale automated synthesis of human functional neuroimaging data. Nat. Methods 8 665–670 10.1038/nmeth.1635 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zellner M. R. (2012). Toward a materialist metapsychology: major operating principles of the brain provide a blueprint for a fundamentally psychodynamic infrastructure. Psychoanal. Rev. 99 563–588 10.1521/prev.2012.99.4.563 [ CrossRef ] [ Google Scholar ]
- Zerssen D. V. (1976). Depressivitäts-Skala . Weinheim: Beltz [ Google Scholar ]
- Open access
- Published: 09 March 2024
How is trauma-focused therapy experienced by adults with PTSD? A systematic review of qualitative studies
- Solveig Flem Gjerstad 1 , 5 ,
- Linda Nordin 2 , 3 ,
- Stig Poulsen 1 ,
- Erminio Francesco Antares Spadaro 1 &
- Sabina Palic 2 , 4
BMC Psychology volume 12 , Article number: 135 ( 2024 ) Cite this article
1164 Accesses
1 Altmetric
Metrics details
Trauma-focused therapies (TFTs) are first-line treatments for posttraumatic stress disorder (PTSD). However, TFTs are under-utilised, partly due to clinicians’ and patients' fear that TFT is too challenging or harmful. We review the qualitative studies on how adults with PTSD experience TFTs to enhance the understanding of user perspectives, therapeutic processes, and outcomes.
PubMed, PsychINFO and PTSDPubs were searched between October 1st and November 30th, 2021. Study quality assessments were undertaken, and studies were analysed using a descriptive-interpretative approach. Nine studies were included.
The analysis resulted in the identification of four key domains, representing a temporal sequence of TFT stages: Overcoming ambivalence towards TFT, Experience of treatment elements, Motivation for dropout/retention, and Perceived changes post-treatment.
Although many participants reported high levels of distress and considered dropping out, only a minority did eventually drop out and most patients expressed that the hardships in therapy were necessary for PTSD improvement. Establishing a safe therapeutic environment and working with the ambivalence towards treatment was essential for retention. This review serves a dual purpose, to shed light on diverse TFT experiences found to be important for treatment satisfaction, and to elucidate common treatment patterns. The results can be used in preparing patients for therapy and in training TFT therapists. Studies had moderate to high quality, and more studies of experiences of TFT non-responders and dropouts in a non-veteran population are needed to further our understanding of the utility and limitations of TFTs.
Peer Review reports
Posttraumatic Stress Disorder (PTSD) is a highly prevalent psychological disorder characterised by symptoms of re-experiencing trauma-related memories, avoidance, and elevated arousal [ 1 ]. The disorder is more commonly reported in high-income countries; however, the symptoms, personal and socioeconomic consequences are consistent globally [ 2 ]. Several types of therapies have been developed with various degrees of proven efficacy. Trauma-focused therapies (TFTs) are suggested as the first-line treatment for PTSD [ 3 ]. In a summary of the major Clinical Practice Guidelines (CPGs), Hamblen et al. [ 4 ] found that all guidelines [ 5 , 6 , 7 , 8 , 9 ] strongly recommended trauma-focused cognitive behavioural therapy (TF-CBT), including cognitive processing therapy (CPT) [ 10 ] and prolonged exposure (PE) [ 11 ]. Eye movement desensitisation and reprocessing (EMDR) [ 12 ] was strongly recommended by all except one guideline [ 5 ].
For this review, TFT is defined as “any therapy that uses cognitive, emotional or behavioural techniques to facilitate the processing of a traumatic experience and in which the trauma focus is a central component of the therapeutic process” [ 13 ]. Specific types of TFT include, but are not limited to, cognitive-behavioural therapies such as PE, CPT, cognitive therapy for PTSD (CT-PTSD) [ 14 ], and narrative exposure therapy (NET) [ 15 ], as well as EMDR, an alternative format of delivering exposure therapy in association with cognitive and emotional components [ 13 ]. In the literature, TF-CBT has both been described as a category encompassing the various cognitive-behavioural therapies mentioned above, or as a specific type of TFT [ 16 ]. In this review, TF-CBT will be referred to as an overarching category of cognitive-behavioural treatments, and TFT will be used as a broader category including TF-CBTs and EMDR.
The distinctive TFTs utilise different interventions. However, they are thought to create change in the same underlying mechanisms, targeting emotion, cognitions, and avoidance of trauma memories [ 17 ]. The cognitive model of PTSD [ 18 ] explains exposure, i.e., imaginal or written reliving and in-vivo exposure, as essential because it modifies negative trauma appraisals. The emotional processing theory [ 19 ] further posits that inhibition of the exaggerated fear response occurs when the patient experiences an optimal emotional activation while experiencing information contradicting their fears. Thus, TFT is theorised and expected to be challenging, as it requires high levels of activation of negative emotions during exposure.
Despite TFTs being the recommended first-line treatments for PTSD, they are often not utilised in clinical practice [ 20 ]. A review by Finch et al. [ 21 ] found that three of the most important clinician-related barriers to the use of the evidence-informed interventions are fear of re-traumatising patients, fear of increasing patients’ symptoms, and a disliking of the inflexibility of the manualized approaches. Therapists further often believed TFT to be unsuitable for patients in case of comorbidity or more complex trauma histories [ 21 ]. However, evidence does not support the concerns regarding the retraumatization and un-suitability of TFTs in cases with comorbidity, for example for psychosis [ 22 ], dissociative symptoms [ 23 ] and major depressive disorder [ 24 ]; see also Ennis et al. [ 25 ] and Voorendonk et al. [ 26 ].
Smith et al. [ 27 ] reviewed barriers to help-seeking in adults with PTSD, including barriers to initiating TFT. The findings revealed complex patterns, where some participants reported not being emotionally ready to talk about trauma or believing PE or CPT to be ineffective or harmful [ 28 , 29 , 30 ], and others having a strong preference for exposure therapy [ 31 ]. Importantly, the patients’ treatment preferences impacted therapists’ willingness to offer TFT [ 21 ]. Hence, systematic reviews [ 21 , 27 ] find that fear of negative experiences and reactions to TFT in both patients and therapists alike is a central barrier to its application.
Finally, TFT has been associated with higher drop-out rates than non-TFT [ 32 , 33 ], and the non-response rate to TFTs is often reported around 50% percent. This has been unchanged over the last two decades [ 33 , 34 ] despite extensive quantitative research into predictors and moderators of outcome as well as therapy effectiveness and dismantling studies. Therefore, a qualitative review of TFT users’ experiences may inform us on how to more efficiently approach the TFT concerns of therapists and patients, as well as the questions of drop-out and nonresponse. Further, users’ experiences with TFTs may lead to new research questions and designs, which can not be deduced from quantitative associations between variables.
Hence, investigating similarities and discrepancies in how patients experience the TFTs might be essential in understanding how to close the gap between current clinical practice and treatment guidelines for PTSD. While reviews studying this question have been conducted for populations of children and youths [ 35 ] and patients’ experience with EMDR [ 36 ], as of today, no review has investigated adult patient experiences with TFTs.
This qualitative review aims to synthesise adult patients’ reported experiences of TFTs to broaden the understanding of common and relevant treatment experiences, themes and trajectories in the therapeutic processes that can inform ways to more efficient and successful delivery of TFT.
Eligibility criteria
The study inclusion and exclusion criteria for this analysis were defined a priori, using the SPIDER mnemonic: Sample, Phenomenon of Interest, Design, Evaluation and Research type [ 37 ]. The final inclusion criteria were: English-language, published, peer-reviewed, qualitative and mixed-method studies reporting on the experience of receiving TFT for patients aged 17 or above with a primary diagnosis of PTSD. The inclusion age was modified from 18 to 17 years during the screening process since one identified article [ 38 *] with participants aged 17– 25 years (M = 20.0, SD = 2.61) was assessed to provide important qualitative information. Since the mean age was 20 and only a few participants were below the age of 18, it was decided that the study should be included. Studies describing both positive and negative experiences of receiving TFT were included to ensure variation in the phenomenon and strengthen the fidelity to the subject matter [ 39 ]. Some studies were excluded from the analysis because they had been discussed in a prior systematic review, exploring patients’ experiences with EMDR [ 36 ]. Their findings are included in the discussion of the current review. However, as the review by Whitehouse [ 36 ] only included studies with clients identified as potentially benefiting from EMDR, older studies that did not meet the inclusion criteria for the review by Whitehouse [ 36 ] were considered for the current review. Therefore, studies involving EMDR published before Whitehouse’s review were also included.
Search strategy
The systematic search consisted of three phases. The first phase involved a preliminary search in PubMed and Google Scholar to identify keywords within the abstract of relevant articles. The SPIDER [ 37 ] tool was applied to define search terms from the review question and develop a standardised search strategy. The second phase consisted of systematic searches using the identified keywords. The searches were conducted in three databases: Pubmed (Medline), PsycINFO (EBSCOHost) and PTSDPubs (Proquest) between October 1st and November 30th, 2021. Some of the search terms were modified to fit the different databases (e.g., using truncation and wildcards). The final phase consisted of hand searches in the chosen studies’ reference lists. The key search terms are presented in Table 1 . For a comprehensive presentation of the search process for each database, see Additional file 1 .
Study selection
Studies were screened and reviewed by the first author with the aid of Covidence. First, duplicates were removed. Titles and abstracts were then screened for inclusion. Studies were retrieved and full-text assessed for eligibility. To limit the possibility of excluding relevant articles, credibility checks were conducted by auditing [ 40 ], meaning that the inclusion of some articles was discussed by three of the authors.
Quality assessment
The quality of the included studies was ensured by including published, peer-reviewed studies [ 39 ]. Further quality assessment was undertaken using the Critical Appraisal Skills Programme [ 41 ], the most used quality checklist in health-related qualitative synthesis [ 42 ]. CASP does not provide a scoring system but allows for a systematic quality assessment through 10 questions with elaborative prompts. To summarise the quality assessment, questions 1 through 9 were evaluated with the following score: Yes/clearly described = 1; Partially described = 0.5; No/insufficient information = 0 (adapted from Neelakantan et al. [ 35 ]). The total scores were categorised as low quality (scores 0 – 3), moderate quality (scores 4 – 8) and high quality (scores 8—9). Studies identified as lower quality by the checklist were not excluded. The quality assessments were used to assess potential biases, reliability, and value in the review’s findings [ 43 ].
Data analysis and synthesis
Descriptive-interpretative qualitative analysis [ 40 ] was applied to provide a comprehensive description of patients’ experience of receiving TFT, including ambiguities and differences found in the primary studies. This approach is suggested for qualitative meta-analyses because it minimises two opposite types of risks that qualitative studies face. One risk is being too relativistic but with insightful findings, meaning that the findings are relative to the interpreter of the analysis and cannot lead to a generalizable framework. Another risk is that the studies are too realistic but with superficial results, because the results simply reproduce the participants’ words true to their original form but lack essential comparisons and interpretation of importance across different studies [ 44 , 45 ]. A qualitative systematic review not only provides a synthesis but also an interpretation of experiences, enabling the presentation of shared, divergent, or significant themes across various modalities of Trauma-Focused Therapies (TFT), group or individual settings, and spanning different types of trauma.
The analysis consisted of four steps, described by Timulak [ 40 ]. First, the collected data were assigned into domains, informed and adjusted by the data of the primary studies. The identified domains created a conceptual framework and represented a temporal sequence of participants’ experiences of trauma-focused therapy. Second, meaning units (the smallest units of the data that conveyed a clear meaning) were identified. Third, meaning units were clustered based on similarities, generating categories and sub-categories. Lastly, the main findings were abstracted in narratives, exemplified through direct quotes.
The analysis was guided by a realist epistemology, assuming a unidirectional relationship between patients’ reports and experiences [ 46 ]. Categories were identified at a semantic level, that is the explicit meaning of the data was identified and organised into patterns [ 46 ]. The patterns were interpreted in terms of their significance and broader meaning. The interpretation included assessing how the methodology in the primary studies may have influenced the results.
All contextual information, including direct quotes, descriptions, and discussions, were considered data. The rationale for including contextual information was to retain the meaning of the results and minimise the risk of overlooking the context of the primary studies, to which qualitative research is sensitive [ 40 ]. Only accounts available in the published versions were included. In mixed methods studies, only qualitative information was used as data. To minimise the risk of overgeneralizing findings, means were taken to address the representativeness of the results in the final review by reporting: (i) how many primary studies were included in each domain, category, sub-category and (ii) how many categories were identified in each study, to account for the degree that each study was represented in the final review [ 47 ].
The analysis and synthesis were initially conducted by the primary author. The fourth author then conducted a separate analysis and synthesis. The process of reaching consensus included making sure that the synthesis represented both analyses and that the final synthesis was adjusted to fit the categories of the independent analysis. Consensus of the domains, categories, meaning units and extracted data were reached in collaboration [ 48 ].
The database search identified 163 studies, where 57 duplicates were removed. The resulting 106 records were screened based on title and abstract. After excluding 95 studies, 11 studies were retrieved and assessed for eligibility. Five studies were excluded during full-text screening, resulting in six studies identified from database-search. Three additional studies were identified through hand searches. All three studies were kept during the screening of title and abstract and the full-text eligibility assessment. The process resulted in nine included studies, three identified through hand-search and six from database searches. Details of the screening process are provided in a PRISMA Flow Diagram (Fig. 1 ).
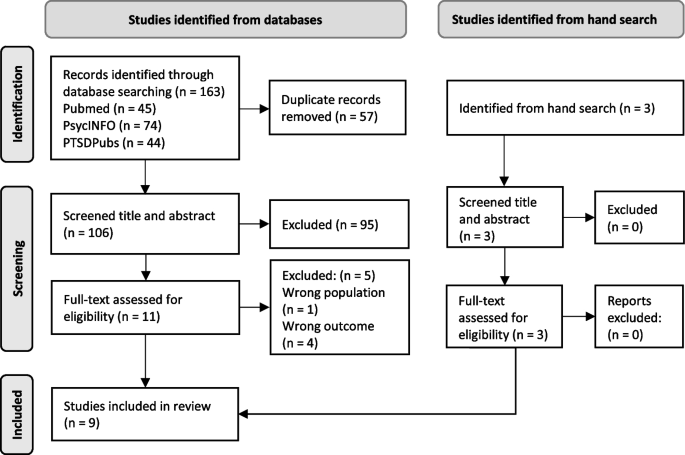
PRISMA flow diagram. Note: Articles excluded based on full-text assessment: Hundt et al. [ 28 ], König et al. [ 49 ], Sherril et al. [ 50 ], Tong et al. [ 51 ] and Wise & Marich [ 52 ]. From: Page, M. J. et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372 , n71. https://doi.org/10.1136/bmj.n71
The reasons for exclusion were wrong population ( n = 1) and wrong objective ( n = 4), i.e., not meeting the criteria for PTSD [ 51 ], investigating pre-treatment criteria [ 28 ], comparing the importance of treatment elements in two treatments without describing the experience [ 49 ], and not including qualitative information about how the patients’ experienced the treatment [ 50 , 52 ]. For a more detailed description of the in- and exclusion process, see Additional file 2 .
Study characteristics
Table 2 provides details of study characteristics. The service contexts included trauma outpatient treatment services, a centre for anxiety disorders, veteran PTSD clinics, a youth mental health service and a primary care service. The studies described using TF-CBT, PE, CPT, Imaginary Rescripting (ImRs), EMDR, reliving, on-site-visits, Imaginal Reliving and/or Adapted Testimony within a TF-CBT framework. Two studies included group CPT, while the rest were delivered as individual therapy. Eight studies used qualitative interviews and one study used a questionnaire with free-text items. All samples consisted of adults, with one study focusing on young adults between 17 and 25 years. Reported traumatic events varied: physical and sexual assault or abuse, gang rape, road traffic accidents, medical trauma, military trauma, witnessing a murder, witnessing others or family members being killed, harmed or captured, finding a child murdered, physical torture, imprisonment, physical threat, domestic and childhood abuse, acts of terrorism, assaults with a weapon. The nine studies comprised 174 participants, with 38 dropping out of treatment (21.8%). Three studies reported interviews with dropouts. The rest of the studies recruited participants that had completed therapy.
Synthesis of the results
The analysis resulted in a conceptual framework representing a temporal sequence of experiences and dilemmas in different stages of TFT. There were four key domains: Overcoming ambivalence towards TFT , Experience of treatment elements , Motivation for dropout or retention and Perceived changes post-treatment , with three categories for each domain. Each category was represented by several sub-categories (see Fig. 2 for a visual representation of experiences and dilemmas in different stages of TFT and Table 3 for a comprehensive summary of the distribution of the articles within each category and which studies are represented by the themes described below).
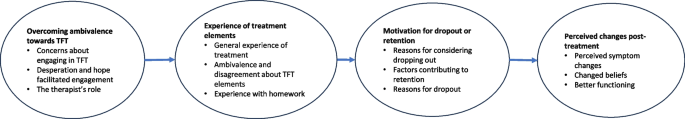
Experiences and dilemmas in different stages of TFT
Overcoming ambivalence towards TFT
Overcoming ambivalence towards TFT was identified as a major theme for all participants. This domain was further divided into three categories: Concerns about engaging in TFT, Desperation and hope facilitated engagement and The therapist’s role.
Concerns about engaging in TFT: fear and scepticism
Participants described experiencing ambivalence about engaging in TFT. More specifically, participants expressed fear, anxiety, and avoidance. “I’d been avoiding it for ages and ages and ages, […]. And it wasn’t until I’d spoken, I’d thought it through, that I realised that I was scared of things, it was just kind of instinctive reaction of like horror, not wanting to go there” [ 53 *] and “I am absolutely afraid I will get depressed again. In fact, I expect it” [ 60 *].
Desperation and hope facilitated engagement
Most of the studies described motivating factors that facilitated initiating TFT. Being desperate and hitting rock bottom was identified as a central factor for encountering the anticipated distress. Conversely, one study [ 53 *] also identified being in a good place as essential for choosing to engage in TFT. Many highlighted the importance of having positive attitudes towards TFT. Three sub-groups emerged. One group reported feelings of hope, determination, commitment and being intrinsically motivated. A second group described emotional doubt but intellectual confidence in the effectiveness of therapy, which was promoted through the understanding of the treatment rationale and therapy process. The last group experienced scepticism and belief simultaneously.
The therapist’s role
Most of the studies highlighted the therapists’ role in helping the patients overcome anticipatory anxiety and engage in trauma-focused interventions. Many studies emphasised the importance of the collaborative relationship, for example feeling that the therapist “facilitated” rather than “directed” the patients [ 55 *] and experiencing being both pushed and respected [ 54 *]. Furthermore, trusting the therapist was considered a significant factor in both empowering patients to manage complicated feelings [ 53 *], expressing concerns about treatment [ 60 *] and gaining a sense of self-efficacy [ 54 *]. Participants identified several valuable characteristics of the therapist that facilitated trust: transparency regarding the content [ 38 *], flexibility within therapy sessions [ 55 *], attentive listening [ 54 *], and empathy, understanding and non-judgement [ 58 *].
Experience of treatment elements
All the studies described patients’ positive or negative experiences of specific elements of TFT, including perceptions of what aspects of therapy they valued or disliked. Despite some differences between the various types of interventions (TF-CBT, PE, CPT, reliving and site-visits as part of TF-CBT, ImRs and EMDR), most participants expressed they had changed their thoughts/beliefs (cognitive-behavioural element) and learned affective coping skills (affective modulation strategies). They also valued exposure and experiencing habituation (trauma-focused elements) and felt that homework generalised learning (homework assignments).
General experience of treatment
Most of the studies included positive reports regarding cognitive-behavioural elements. Cognitive techniques such as questioning one’s thought processes and identifying cognitive biases were emphasised by participants as valuable in gaining a greater understanding of themselves, their triggers, symptoms, traumatic experiences, and were experienced as contributing to positive changes in thoughts/beliefs and better coping skills. In addition to cognitive strategies, affective modulation strategies and psychoeducation were both described as vital for change and helped the participants gain a sense of control. Regarding the length of therapy, there are mixed results. Some participants reported wanting more sessions, some were satisfied, and others were reported as finishing treatment early. See Table 3 for an overview of what articles report which of the reported themes.
Ambivalence and disagreement about trauma-focused elements
Trauma-focused interventions received the most negative evaluation, but were also described as the most essential and critical parts of recovery. Since this category accounted for a large part of the analysis, it was separated into conflicting but complementary subcategories. The following subthemes show a disagreement in how the participants experienced trauma-focused interventions.
Harder than expected versus unfounded fears
Participants’ encounters with trauma-focused interventions varied and were categorised into three groups: (i) easier than anticipated, (ii) more challenging than expected, and (iii) difficult, as expected. Those individuals who perceived trauma-focused interventions as easier than anticipated described them as painful yet manageable, as their worst fears were proven unfounded. In the words of a participant, “Although it was very, very painful to relive it, I didn’t lose control, I didn’t scream, cry, or lash out” [ 53 *]. A few studies reported experiences where treatment proved more challenging than expected, as expressed by a participant in Doran et al. [ 60 *]: “I simply didn’t anticipate my reactions. I didn’t expect it to be this difficult”. In contrast, a majority experienced distress during the trauma processing, but recognized it as an expected and necessary part of the recovery process.
Difficulty tolerating trauma work versus importance of hardship
All studies consistently reported emotional distress among patients undergoing trauma-focused therapy (TFT), emphasising its demanding nature in addressing negative emotions and content. Common adverse reactions included initial symptom worsening, including nightmares, flashbacks, intrusive thoughts, and increased substance use [ 38 *, 53 *, 54 *, 56 , 57 ,*– 58 *].
Feeling overwhelmed during trauma-related exposures and re-experiencing the events was also frequently reported. Notably, one participant described the resurfacing of trauma-related emotions as “even more traumatic” than the original event, attributing this distress to an inability to disengage from the traumatic memories [ 38 *]. Another participant conveyed a sense of dissociation during trauma work, stating, “… I was actually back when it was, all the stuff [the trauma] was happening. So I was like actually, I was scared and I’d leave, like obviously we’d stop because [the therapist] could see that I was not in the room” [ 38 *].
Nonetheless, despite the distress experienced, discussing the trauma was described as “cathartic” and deemed essential [ 54 *]. A majority of participants credited therapeutic progress to trauma work, emphasizing that the short-term pain was outweighed by the eventual benefits. One participant continued therapy even after relapsing into substance use during trauma narration, regarding it as a necessary part of their healing journey [ 58 *]. However, it is important to note that not all participants shared this perspective, and dropout from treatment was often linked to an inability to manage the emotional distress associated with trauma work, which will be discussed separately.
Life-consuming versus habituation
Several participants reported that trauma work consumed every facet of their lives. This immersion manifested itself as persistent rumination and enduring low mood in the intervals between therapy sessions, which had adverse effects on their social, occupational, and academic aspects of life. For instance, one participant articulated their experience, stating, “I was very dark and depressed… constantly thinking about it, bringing up suppressed memories…” [ 38 *]. Nonetheless, a prevalent pattern surfaced where participants progressively found the trauma-work more manageable over time, experiencing habituation and improved coping. They likened it to desensitisation, making it easier to discuss and express their experiences.
Piecing together traumatic experiences versus wanting less repetition
Participants generally had positive concluding remarks on trauma processing. Repeatedly discussing the “original event” facilitated memory reconstruction, changed beliefs [ 57 *], memory vividness [ 56 *], and “moving forward” [ 59 *]. However, some wanted to address multiple events, patients who dropped out cited feeling overwhelmed by the repetitive sessions [ 60 *], and some viewed discussing trauma as “dwelling on the past” and potentially hindering recovery [ 38 *].
Experience with homework
Most participants found homework beneficial for practice and generalised learning [ 55 *]. Positive experiences with homework served as positive feedback that the therapy was working [ 57 *]. Challenges included finding the homework assignments confusing or having problems completing it due to other commitments [ 57 *, 60 *].
Motivation for dropout or retention
The third domain that emerged from the analysis was “Motivation for dropout or retention”. Although a minority of participants dropped out, many participants described wanting to drop out at some point. The domain was divided into the categories “Reasons for considering dropping out”, “Factors contributing to retention”, and “Reasons for dropout”.
Reasons for considering dropping out
The primary reason for considering ending therapy was unresolved ambivalence about treatment, primarily rooted in doubts regarding therapy effectiveness, difficulty tolerating treatment, and avoidance behaviours, as indicated by one participant: “I thought about quitting because I was avoiding writing about my traumatic experience” [ 57 *]. Stigma and cultural stereotypes surrounding seeking mental health prevailed and were a central theme for participants’ ambivalence about treatment. Concerns about treatment duration, especially its brevity, added to ambivalence, as participants questioned the adequacy of the allocated time. Uncertainty about the future, notably among asylum seekers awaiting decisions on their asylum claim, also led to doubts about the worth of continuing therapy. Furthermore, participants cited practical barriers, including transportation challenges and family responsibilities, as hindrances to therapy.
Factors contributing to retention
Despite considering discontinuing treatment, most participants chose to continue therapy. Support from family and friends was mentioned by many as a primary reason for retention. For those lacking social support, the therapeutic relationship held great importance and openly discussing concerns with the therapist reinforced commitment. Additionally, perceived early progress, symptom improvement, relief and shifts in perspectives, inspired the patients’ persistence. Lastly, dedication to the therapy process, oneself, and the therapist was recognized as crucial during challenging phases, with some participants attributing their decision to continue to their “commitment” [ 57 *].
Reasons for dropout
Participants dropped out of therapy for four main reasons: external barriers, therapy-related difficulties, therapeutic alliance issues and lack of social support.
External barriers such as therapists lacking dedicated offices, scheduling conflicts, and limited health plan coverage, often led to disengagement. Therapy-related difficulties mirrored the concerns of those considering dropout. Many quit when they didn't see improvement or had doubts about the therapy approach, finding it too formal or preferring to learn coping skills. Some started therapies recommended by their therapists despite reservations [ 58 *]. Interestingly, some dropped out despite believing in the benefits of trauma work due to an inner conflict between avoidance and recognizing the need for therapy [ 60 *].
Participants expressed their willingness to consider returning to therapy if it were possible to develop a stronger therapeutic relationship, acquire enhanced coping skills, or resolve practical barriers [ 54 *, 58 *]. Importantly, those facing therapy-related challenges often cited issues with the therapist-patient relationship and a lack of social support [ 38 *, 58 *].
Perceived changes post-treatment
Participants reported noteworthy positive changes: reduction in symptoms, changed beliefs about the trauma, themselves and the future and better functioning. A few reported negative outcomes, which will be discussed within these categories.
Perceived symptom changes
Positive symptom changes included reduced re-experiencing symptoms, improved sleep, mood, concentration, fewer nightmares, and less avoidance and hyperarousal. Most commonly, participants reported mood and functional improvements, a reduction in symptom intensity and frequency, while also acquiring coping skills to better manage residual symptoms. Yet, some saw no improvements, and a few felt worse, experiencing symptom exacerbation, nightmares, and substance abuse relapses [ 60 *].
Changed beliefs
Participants experienced profound shifts in their beliefs about trauma, themselves, and the future. These changes involved developing a new relationship with traumatic memories, reinterpreting the traumatic experiences, and gaining insights into their impact on life challenges. The changes extended to participants regaining a sense of agency, and experiencing bolstered confidence in handling trauma and reduced self-blame, exemplified by a participant recognizing they were allowed to be angry about what was done to them [ 53 *]. This transformation indicated a profound shift in self-identity [ 38 *, 57 *].
Notably, asylum-seekers differed in their responses. They expressed feelings of weakness and illness due to their therapy needs, contrary to the more common experience of relief from shame and guilt. Accepting new perspectives was challenging for some asylum-seekers, leading to negative changes in self-understanding and beliefs about others [ 54 *].
Despite these variations, most participants adopted a positive outlook on life following therapy. They expressed renewed hope for a meaningful future and a preference for life over death, representing a significant shift in their perspective.
Better functioning
Symptom improvements, increased hope, and enhanced symptom management had a positive effect on various aspects of participants’ lives. They reported improved social relationships, occupational functioning, and a rekindled interest in previously enjoyed activities. For instance, one participant mentioned increased participation in family events [ 57 *]. Another credited therapy with helping them open up about their experiences, which allowed for a sense of connection and social support [ 38 *].
Representativeness of findings
The representativeness of the findings in the review is presented in Table 3 . Representativeness was assessed as (a) how many studies were represented in each category and sub-category, and (b) how many categories were identified in each study. Assessing the representativeness of each study in the findings was conducted by calculating the total amount of categories each study identified.
Critical appraisal
The quality of the included studies was high and moderate, with six studies rated as high quality and three studies rated as moderate quality according to CASP. All studies gave a clear statement of the research aims, and qualitative research was justified and considered to be the suitable methodology for addressing the research goal. Recruitment bias was widespread throughout all the studies. For instance, two of the studies did not provide sufficient information about how the participants were selected [ 56 *, 57 *], and one study used self-selecting recruitment but did not discuss the implications of this method [ 53 *]. Despite the presence of recruitment bias, most authors discussed their recruitment strategy (e.g., recruiting participants from one treatment facility or choosing participants who were thought to benefit from the treatment), which demonstrated systematic appraisal of study limitations. All the studies described and justified the data collection procedures. Five studies did not discuss the relationship between researcher and participants. This was mostly not considered to create a high risk of bias, as different individuals conducted the therapy, data collection and analysis. However, in two studies, participants might have been reluctant to disclose negative therapy experiences due to the nature of the data collection [ 54 *, 55 *]. Three studies did not provide sufficient details to assess whether ethical standards were maintained [ 53 *, 55 *, 56 *]. All studies described data analysis rigorously. All except one study [ 56 *] offered a comprehensive statement of findings. See Additional file 3 for a detailed description of the quality assessments.
The purpose of the present review was to understand and summarise patients’ experiences and dilemmas in trauma-focused therapy. The synthesis across patients with different trauma and six different types of TFT resulted in a common pattern, which provides insight into common experiences likely to occur throughout TFT. Comparing the experiences reported by those who considered dropping out but chose to stay and those who did drop out may help to illuminate, which aspects of TFT that are experienced as too challenging for patients [ 21 , 27 ].
Trajectories of treatment experiences
Different trajectories of how patients experienced the process of TFT emerged. Patients’ concerns about starting therapy, described in this review, concur with the common characteristics of PTSD, including avoidance and negative beliefs about the self, future, and trauma [ 18 ]. At the beginning of therapy, most participants experienced scepticism and fear of talking about the trauma. Despite the commonly held belief in both patients and therapists that the patients’ should be in “a good place in life” in order to engage in TFT, the most prevalently reported patient-experience in the study was that desperation (i.e., “hitting rock bottom”) was important for deciding to engage in TFT in the first place. Thus, apparently a combination of desperation and hope might compel patients to begin treatment.
Next, patients’ experiences with trauma-focused interventions were mixed. Importantly, most considered dropping out at some point, due to the hardship of trauma-focused interventions and doubts about its efficacy. This finding has important clinical implications, because while most TFT manuals prescribe motivational strategies before the initiation of trauma-focused exposure, to the best of our knowledge, none deal explicitly with retention strategies once exposure has begun (NET (15); CT-PTSD (14); CPT (10); PE (11)). Thus, therapists are currently left to devise their own retention strategies to the best of their ability.
Despite the high distress levels involved, difficulty tolerating treatment and overcoming the discomfort was found to be essential for recovery. Furthermore, overall the patient experiences did not support patients’ and therapists’ concerns that TFT might be ineffective or harmful. To the contrary, some described TFT to be effective, despite dropping out of therapy.
Factors associated with retention
Factors associated with retention included buy-in to treatment, symptom improvement, fewer external barriers, social support, and a strong therapeutic relationship. Buy-in to treatment was crucial, often achieved through psychoeducation and therapist support.
The results indicated that buy-in to treatment can be divided into a rational, emotional and desperate buy-in. A rational buy-in was accomplished through thorough psychoeducation. An emotional buy-in was described as based on a trust in the therapists, facilitated by feeling both respected and pushed. When respected, patients were allowed time to understand the treatment rationale and take breaks, due to emotional limits. The experience of being pushed in a constructive way encompassed being exposed to trauma-interventions even when they did not believe they could tolerate it. The last group of clients, characterised by what we have termed desperate buy-in, preferred starting trauma intervention as soon as possible to limit the risk of them backing out. Despite not necessarily understanding the treatment approach, early trauma interventions allowed them to experience early symptom improvement. This exemplifies the complexities of trauma treatment and the all-important balancing of providing psychoeducation, ensuring “buy-in to treatment”, and early introduction of trauma-focused interventions. Hence, if we are to get better at preventing drop-out from TFT, designing explicit manualized strategies, which help therapists to recognize and address the above patterns, might be a way forward.
Patients perceived certain aspects of TFT as too inflexible, including the treatment content and process, consistent with concerns raised by therapists [ 21 ]. However, participants experiencing both being pushed and respected reported positive sentiments about its flexibility. Thus, although flexible sessions that adapt to individual needs while staying true to treatment goals may be beneficial, trusting the therapist might result in a more positive attitude towards the treatment manual. Overall, in order to improve retention, the expectations of treatment services regarding the pace and length of TFTs need to be flexible enough to allow for adaptations and good enough working alliances between therapists and patients, as well as good enough working conditions for those providing the treatments.
Social issues such as external stressors, logistical barriers and unstable living conditions often interfered with treatment. However, those reporting external barriers who simultaneously had a strong therapeutic relationship or good social support were more inclined to stay in therapy. Moreover, participants reporting both external barriers and lack of social support specifically emphasised the therapist’s support as a central factor in their decision to stay in therapy. For those experiencing alliance issues, discussing concerns about the treatment with their therapist often facilitated retention. This is in line with prior research that points to the significance of acknowledging factors related to the therapeutic alliance (i.e., the therapeutic relationship, empathy, support, and shared goals) as potential mediators of symptom change [ 61 ]. Finally, an important dynamic is demonstrated in the trajectory from the initial need to be in a place desperate enough to consider starting TFT, to the finding that those same social issues may become a hindrance in later phases of treatment. A clinical implication of this sequence might be that we should not wait for patients’ lives to become more “stable” before initiating TFT as has been suggested to reduce patients’ fear [ 62 ], but rather provide effective social counselling in parallel with TFT to alleviate the worst social stressors and improve retention during the exposure phase.
The findings shared similarities with the qualitative review of EMDR experiences among patients identified as benefiting from EMDR [ 36 ]. Similarities included the significance of a trusting therapeutic relationship to create a sense of safety and alleviate doubts and scepticism about therapy. Additionally, a common theme that emerged included experiencing a broader transformation through therapy, leading to an enhanced quality of life and changed beliefs about oneself.
Treatment rationale of trauma-focused therapies
Patients’ experiences both aligned with and challenged the assumptions about common mechanisms promoting change in TFT through the targeting of emotion, cognition and avoidance, i.e., psychoeducation, exposure, memory processing and habituation [ 17 ].
Psychoeducation not only seemed to increase participants’ commitment to treatment but also positively influenced most patients’ self-perceptions and how they viewed their symptoms. These shifts in how they appraised their traumatic experiences were mainly attributed to cognitive techniques, while exposure interventions played a crucial role in memory modification and discrimination. Although a minority of patients did not experience habituation to their trauma memories or symptom improvement despite completing treatment, many still reported significant improvements representing an increase in quality of life [ 63 ], including better symptom management, increased sense of control, improved social relationships, and enhanced work and daily functioning.
While the positive outcomes might be attributed to or moderated by non-specific therapeutic factors, such as the therapeutic relationship [ 64 ], patients attributed the changes to the process of addressing their trauma. The key elements that patients valued in therapy included experiencing catharsis and relief through discussing their trauma, transforming their beliefs about trauma, the world, and themselves, and having a trustworthy and genuine therapist to facilitate these changes. In accordance with the theoretical framework proposed by Ehlers and Clark [ 18 ], the results indicate that from a patient perspective, trauma-focused work was essential for regaining trauma memory, achieving a new perspective on the trauma, and managing their symptoms.
Diverse experiences within subgroups
The findings of the study indicate that Trauma-Focused Therapy (TFT) was experienced as beneficial for veterans and asylum seekers; however, the results suggest that these groups exhibit distinct and somewhat less favourable responses to TFT when compared to other populations. Notably, despite Clinical Practice Guidelines recommending TFT as the primary treatment for PTSD, recent research has uncovered inconsistent findings with regard to its superiority, particularly in the context of military-related PTSD [ 65 , 66 , 67 , 68 ].
These variations in treatment outcomes may stem from various external, cultural, or trauma-specific factors and the results underscore the imperative of cultural sensitivity when working with trauma survivors [ 69 , 70 ]. Both veteran and asylum seeker groups encountered significant challenges related to stigma, shame, and guilt. Stigma could exacerbate negative appraisals of trauma and self-perception, subsequently impeding help-seeking behaviour. This, in turn, could contribute to the persistence and severity of symptoms, as noted in prior research [ 71 ]. Moreover, limited help-seeking behaviour among these groups may lead to reduced social support, a factor which has been identified as crucial for maintaining engagement and retention in treatment.
Asylum seekers’ difficulties in acknowledging past traumas and altering their beliefs about themselves and the world pose a crucial challenge in the context of most TFTs. Among the other study samples, gaining a new perception of the trauma memory appeared as essential for improving symptom management, aligning with existing studies demonstrating that alterations in appraisals mediate the change of PTSD symptoms [ 72 ]. This observed subgroup difference might reflect significant cultural variations in the perception of psychiatric diagnoses and trauma experiences. However, it might be that current threats moderate this relationship. Notably, the fear of repatriation emerged as a significant barrier hindering engagement for asylum seekers. This aligns with theoretical models suggesting that the perception of current threats sustains PTSD symptoms [ 18 ]. Despite evidence supporting the effectiveness of TFT for individuals at high risk of re-exposure [ 25 ], the results suggest that the coexistence of cultural stigma and current threats may increase the likelihood of treatment dropout among these patient populations. More qualitative studies of refugee-patients’ experiences with TFT are needed to better understand the obstacles to effective implementation of TFT in this group.
Clinical implications
Creating a safe therapeutic environment is crucial to enhance the effectiveness and tolerability of Trauma-Focused Therapy (TFT). Addressing and working through ambivalence plays a central role in building trust in treatment and influencing patient engagement and retention. Trust encompasses both a rational understanding of the treatment rationale and an emotional reliance on the therapeutic process and therapist.
Therapists should prioritise building trust, considering the client's unique subjective and cultural perspectives. It is particularly important to inform the patient about the treatment principles, to present a clear rationale for the exposure component that acknowledges that revisiting the trauma memories may seem counterintuitive, and to provide realistic expectations for both positive and negative experiences throughout therapy. It is important to anticipate and openly discuss common reactions like fear, ambivalence, and symptom exacerbation, reassuring clients that these are typical and not indicative of treatment failure. Finally, anticipating patients’ ambivalence during treatment and manualizing retention strategies in TFTs might be a way of improving their effectiveness.
For individuals hesitant to engage in treatment due to apprehension, the awareness of shared experiences or the recognition that encountering challenges like relapse and symptom worsening has been reported as worthwhile by others may be reassuring. Follow-up sessions aimed at discussing re-engagement are recommended, as most dropouts express a willingness to retry TFT.
Some participants, particularly refugees and veterans, express a desire to move on from traumatic events, which contrasts with TFT's core element of revisiting trauma for processing. Therapists should explain this counterintuitive approach and address client scepticism through education and preparation, both in sessions and through written or online materials. Patients across the studies emphasised the importance of understanding the treatment rationale, suggesting a need for adaptations like translated materials or culturally relevant language for minority groups [ 73 ].
Clinicians should address the potential stigma and increased sense of guilt associated with psychiatric diagnosis for multiple marginalised groups. Challenges including shame, isolation and cultural stereotypes suggest that a group-oriented approach focusing on these aspects as part of psychoeducation, could be beneficial. Recognizing that cultural context shapes trauma experiences, the results suggest that the treatment should address the perception of current stressors alongside past trauma, rather than exclusively concentrating on a single traumatic event. The findings suggest that patients with many social stressors might benefit from more short-term intensive treatment [ 74 , 75 ], or/and treatments that focus on alleviating social stressors in parallel with provision of TFT.
This review informs psychoeducation by shedding light on TFT experiences and elucidating common treatment patterns. Referring to how other patients respond can assist clinicians and patients in developing trust in TFT. Recognizing that ambivalence and fear can deter both patients and therapists, this review may mitigate treatment dropouts and enhance willingness to engage in TFT.
Strengths and limitations
A strength of this review is the pre-defined inclusion and exclusion criteria. The wide range of search terms and the inclusion of hand-searched articles enhanced the likelihood to detect a large proportion of existing papers relating to patients’ experiences of TFT. The studies represented both positive and negative experiences, providing a nuanced picture of patients’ experiences. The studies included a diversity of sub-groups (veterans, asylum seekers, youths, and patients with various index traumas), allowing for a more comprehensive understanding of typical and distinct experiences seen across these groups, e.g., difficulties with completing TFT. The studies reviewed were conducted in the US, UK, Australia, Germany and Netherlands, with a wide range of ethnicities represented.
The included studies covered a variety of therapeutic methods (imaginal reliving, site-visits, PE, CPT, Adapted Testimony, ImRe and EMDR). Furthermore, the quality of this systematic review was strengthened through credibility checks. The authors amongst themselves encompassed a broad range of therapeutic experiences and preferences, including both TFT-practitioners and non-TFT practitioners. Lastly, the representativeness of the findings in this systematic review was assessed [ 47 ].
Nonetheless, certain limitations affect the generalizability of the findings. Participants with a positive experience could have been more inclined to participate in the research. Also, the use of purposive sampling might have contributed to sampling bias, resulting in overly optimistic reports about TFT experiences. For example, certain studies included patients who completed at least eight sessions of therapy [ 57 *], who found the treatment to be a positive experience [ 55 *], or who were believed to benefit from exposure interventions [ 56 *, 60 *]. Furthermore, interviews conducted in the setting where the participants received therapy might have impacted to what degree the participants were willing to disclose negative experiences [ 54 *]. Finally, the included studies do not represent the perspectives of patients who have refused to start in TFT. It is likely that studies investigating the expectations and concerns of patients who are not willing to enter into a therapy including an exposure component would have further added to the understanding of patient perspectives on TFT.
Despite the possibility that some studies contributed to disproportionately positive results, it was also evident in the studies that most participants shared both negative and positive experiences. Furthermore, certain of the included studies actively reduced the possibility of overgeneralizing positive findings in the review by focusing on those who had dropped out of TFT [ 38 *, 58 *, 60 *]. Even when bearing in mind the impact of the potential methodological biases, the themes reflecting positive and negative experiences were similar across different types of study populations. Moreover, dropouts from all three studies reported positive feelings about TFT, and many were willing to try TFT again.
Despite the inclusion of several therapeutic interventions, most studies examined therapies related to TF-CBT and no studies examined the experience of narrative exposure therapy. Approximately half of the sample and 70% of the dropouts were veterans. The exclusion criteria could have biased the reported results, as non-English language studies and studies not published in peer-reviewed publications were excluded. The exclusion of grey literature could have contributed to a publication bias of the reported experiences. Furthermore, the reporting of the results (a few, some, many, several and most) might represent a bias. Due to a lack of accurate descriptions in some of the studies, it was impossible to provide a precise number of participants reporting different experiences. Two authors selected relevant “quotations” from the original studies, and although means were taken to stay close to the language of the original studies when describing the results, both the original researchers of the primary studies and the authors of the current review might have overlooked some information. Nevertheless, by conducting rigorous and systematic analysis, the findings are likely to offer a comprehensive and in-depth picture of patients’ experiences.
Future research
First, it is evident that there is a lack of studies involving TFT experiences of multiply marginalised groups. Future research should prioritise investigating how these specific populations experience TFTs. Given that most existing studies focus on TF-CBT, it is crucial to expand our understanding by exploring how patients experience Narrative Exposure Therapy (NET). It would be relevant to focus such studies on refugees or asylum seekers, as this group did not experience the common trajectory of altered beliefs about themselves, the trauma and the world, and because NET was developed to treat trauma within this population and has demonstrated effectiveness [ 76 ]. The literature search also identified a lack of studies investigating therapists’ experience with conducting TFTs. Further research should investigate both patients’ and therapists’ experiences, making it possible to compare their experiences and to what extent they align.
Overall, participants reported high levels of distress and re-emergence of symptoms during trauma work. Still, despite negative experiences, most patients were grateful and perceived the hardship as essential for improvement. At the beginning of therapy, most participants experienced scepticism and fear of talking about the trauma. Most participants expressed a reduction in ambivalence throughout therapy due to experiencing symptom improvement, understanding the treatment rationale, and trusting the therapist’s empathy and expertise. Some expressed persistent ambivalence about the effectiveness of the treatment as an essential factor for dropping out. Also, it seems that it is vital for participants to be informed about the treatment principles and the rationale for the exposure component of the therapy. Clinicians should emphasise that therapy will be challenging and that symptom exacerbations may occur during trauma exposure, but that these experiences do not imply that treatment does not work. Instead, experiencing difficulties with the treatment and overcoming these could be essential for recovery. Most participants experienced significant improvements in symptoms and quality of life. Realistic expectations of symptom improvements post-therapy should be emphasised, as many still experienced some symptoms post-treatment. However, therapy helped them gain coping skills, a sense of control, agency and a better outlook on life. The results also emphasised that participants’ appreciated hearing about other people’s experiences, as it helped them overcome their ambivalence about staying in therapy.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
Cognitive processing therapy
Cognitive therapy for post-traumatic stress disorder
Eye movement desensitisation and reprocessing
Narrative exposure therapy
Prolonged exposure
Post-traumatic stress disorder
Trauma-focused cognitive behaviour therapy
- Trauma-focused therapy
The studies marked with an asterisk were included in the systematic review.
World Health Organization. International statistical classification of diseases and related health problems (11th ed.). 2019. https://icd.who.int/ .
Silove D, Klein L. Culture, Trauma, and Traumatic Stress among Refugees, Asylum Seekers, and Postconflict Populations. In: Friedman MJ, Schnurr PP, Keane TM, (Eds.). Handbook of PTSD: Science and practice (3rd ed.). New York, NY: Guilford Press; 2021. p. 483–500.
Olff M, Monson CM, Riggs DS, Lee C, Ehlers A, Forbes D. Psychological Treatments Core and Common Elements of Effectiveness. In: Forbes D, Bisson JI, Monson CM, Berliner L, (Eds.), Effective Treatments for PTSD (3rd ed.). New York, NY: Guilford Press; 2020. p. 164–184.
Hamblen JL, Norman SB, Sonis JH, Phelps AJ, Bisson JI, Nunes VD, Megnin-Viggars O, Forbes D, Riggs DS, Schnurr PP. A guide to guidelines for the treatment of posttraumatic stress disorder in adults: an update. Psychotherapy. 2019;56(3):359–73. https://doi.org/10.1037/pst0000231 .
Article PubMed Google Scholar
American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Washington, DC: 2017. Retrieved from: https://www.apa.org/ptsd-guideline .
Department of Veterans Affairs and Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Washington, DC: Department of Veterans Affairs and Department of Defense; 2017.
Google Scholar
International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: Methodology and recommendations. 2018. Retrieved from: www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_PreventionTreatmentGuidelines_FNL.pdf.aspx .
National Institute for Health and Care Excellence. Guideline for post-traumatic stress disorder. National Institute for Health and Clinical Practice. [NICE guideline NG116]. 2018. www.nice.org.uk/guidance/ng116 .
Phoenix Australia Centre for Posttraumatic Mental Health. Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne: Phoenix Australia Centre for Posttraumatic Mental Health; 2013.
Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD: a comprehensive manual. New York, NY: Guilford Press; 2017.
Foa EB, Hembree E, Rothbaum B. Prolonged Exposure Therapy for PTSD: Therapist Guide. Oxford: Oxford University Press; 2007. https://doi.org/10.1093/med:psych/9780195308501.001.0001 .
Article Google Scholar
Shapiro F. Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols, and procedures. New York, NY: Guilford Press; 1995.
Schnurr PP. Focusing on trauma-focused psychotherapy for posttraumatic stress disorder. Curr Opin Psychol. 2017;14:56–60. https://doi.org/10.1016/J.COPSYC.2016.11.005 .
Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behav Res Ther. 2005;43(4):413–31. https://doi.org/10.1016/j.brat.2004.03.006 .
Schauer M, Schauer M, Neuner F, Elbert T. Narrative exposure therapy: A short term treatment for traumatic stress disorders. Boston: Hogrefe; 2011.
Friedman MJ, Schnurr PP, Keane TM. PTSD from DSM-III to DSM-5 Progress and challenges. In: Friedman MJ, Schnurr PP, Keane TM, (Eds.). Handbook of PTSD: Science and practice (3rd ed.). New York, NY: Guilford Press; 2021. p. 3–18.
Schnyder U, Ehlers A, Elbert T, Foa EB, Gersons BPR, Resick PA, Shapiro F, Cloitre M. Psychotherapies for PTSD: what do they have in common? Eur J Psychotraumatol. 2015;6(1):28186. https://doi.org/10.3402/ejpt.v6.28186 .
Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38(4):319–45. https://doi.org/10.1016/S0005-7967(99)00123-0 .
Article CAS PubMed Google Scholar
Foa EB, Kozak MJ. Emotional Processing of Fear. Psychol Bull. 1986;99(1):20–35. https://doi.org/10.1037/0033-2909.99.1.20 .
Kline AC, Klein AB, Bowling AR, Feeny NC. Exposure Therapy Beliefs and Utilization for Treatment of PTSD: A Survey of Licensed Mental Health Providers. Behav Ther. 2021;52(4):1019–30. https://doi.org/10.1016/j.beth.2021.01.002 .
Finch J, Ford C, Grainger L, Meiser-Stedman R. A systematic review of the clinician related barriers and facilitators to the use of evidence-informed interventions for post traumatic stress. J Affect Disord. 2020;263:175–86. https://doi.org/10.1016/j.jad.2019.11.143 .
Swan S, Keen N, Reynolds N, Onwumere J. Psychological interventions for post-traumatic stress symptoms in psychosis: a systematic review of outcomes. Front Psychol. 2017;8:341. https://doi.org/10.3389/fpsyg.2017.00341 .
Article PubMed PubMed Central Google Scholar
Zoet HA, de Jongh A, van Minnen A. Somatoform dissociative symptoms have no impact on the outcome of trauma-focused treatment for severe PTSD. J Clin Med. 2021;10(8):1553. https://doi.org/10.3390/jcm10081553 .
Kline AC, Cooper AA, Rytwinski NK, Feeny NC. The effect of concurrent depression on PTSD outcomes in trauma-focused psychotherapy: a meta-analysis of randomized controlled trials. Behav Ther. 2021;52(1):250–66. https://doi.org/10.1016/j.beth.2020.04.015 .
Ennis N, Sijercic I, Monson CM. Trauma-focused cognitive-behavioral therapies for posttraumatic stress disorder under ongoing threat: A systematic review. Clin Psychol Rev. 2021;88:102049. https://doi.org/10.1016/j.cpr.2021.102049 .
Voorendonk EM, de Jongh A, Rozendaal L, van Minnen A. Trauma-focused treatment outcome for complex PTSD patients: results of an intensive treatment programme. Eur J Psychotraumatol. 2020;11(1):1783955. https://doi.org/10.1080/20008198.2020.1783955 .
Smith JR, Workneh A, Yaya S. Barriers and facilitators to help-seeking for individuals with posttraumatic stress disorder: a systematic review. J Trauma Stress. 2020;33(2):137–50. https://doi.org/10.1002/jts.22456 .
Hundt NE, Mott JM, Miles SR, Arney J, Cully JA, Stanley MA. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7(6):539–46. https://doi.org/10.1037/tra0000035 .
Sayer F-S, G., Spoont, M., Murdoch, M., Parker, L. E., Chiros, C., & Rosenheck, R. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72(3):238–55. https://doi.org/10.1521/psyc.2009.72.3.238 .
Stecker S, B., Watts, B. V., Jones, M., & Conner, K. R. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64(3):280–3. https://doi.org/10.1176/appi.ps.001372012 .
Simiola V, Neilson EC, Thompson R, Cook JM. Preferences for trauma treatment: A systematic review of the empirical literature. Psychological Trauma. 2015;7(6):516–24. https://doi.org/10.1037/tra0000038 .
Edwards-Stewart A, Smolenski DJ, Bush NE, Cyr B, Beech EH, Skopp NA, Belsher BE. Posttraumatic stress disorder treatment dropout among military and veteran populations: a systematic review and meta-analysis. J Trauma Stress. 2021;34(4):808–18. https://doi.org/10.1002/jts.22653 .
Lewis C, Roberts NP, Gibson S, Bisson JI. Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. Eur J Psychotraumatol. 2020;11(1):1709709. https://doi.org/10.1080/20008198.2019.1709709 .
Sripada RK, Blow FC, Rauch SA, Ganoczy D, Hoff R, Harpaz-Rotem I, Bohnert KM. Examining the nonresponse phenomenon: Factors associated with treatment response in a national sample of veterans undergoing residential PTSD treatment. J Anxiety Disord. 2019;63:18–25. https://doi.org/10.1016/j.janxdis.2019.02.001 .
Neelakantan L, Hetrick S, Michelson D. Users’ experiences of trauma-focused cognitive behavioural therapy for children and adolescents: a systematic review and metasynthesis of qualitative research. Eur Child Adolesc Psychiatry. 2019;28(7):877–97. https://doi.org/10.1007/S00787-018-1150-Z .
Whitehouse J. What do clients say about their experiences of EMDR in the research literature? A systematic review and thematic synthesis of qualitative research papers. Eur J Trauma Dissociation. 2021;5(3):100104. https://doi.org/10.1016/j.ejtd.2019.03.002 .
Cooke A, Smith D, Booth A. Beyond PICO. Qual Health Res. 2012;22(10):1435–43. https://doi.org/10.1177/1049732312452938 .
* Eastwood O, Peters W, Cohen J, Murray L, Rice S, Alvarez-Jimenez M, Bendall S. “Like a huge weight lifted off my shoulders”: Exploring young peoples’ experiences of treatment in a pilot trial of trauma-focused cognitive behavioral therapy. Psychother Res. 2021;31(6):737–51. https://doi.org/10.1080/10503307.2020.1851794 .
Levitt HM. How to conduct a qualitative meta-analysis: Tailoring methods to enhance methodological integrity. Psychother Res. 2018;28(3):367–78. https://doi.org/10.1080/10503307.2018.1447708 .
Timulak L. Meta-analysis of qualitative studies: A tool for reviewing qualitative research findings in psychotherapy. Psychother Res. 2009;19(4–5):591–600. https://doi.org/10.1080/10503300802477989 .
Critical Appraisal Skills Programme. CASP (Qualitative Study Checklist) Checklist. 2018. Available at: https://casp-uk.net/casp-tools-checklists/ . Accessed: 20.10.21.
Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci. 2020;1(1):31–42. https://doi.org/10.1177/2632084320947559 .
Stenfors T, Kajamaa A, Bennett D. How to … assess the quality of qualitative research. Clin Teach. 2020;17(6):596–9. https://doi.org/10.1111/tct.13242 .
Elliott R. A linguistic phenomenology of ways of knowing and its implications for psychotherapy research and psychotherapy integration. J Psychother Integr. 2008;18(1):40–65. https://doi.org/10.1037/1053-0479.18.1.40 .
Rennie DL, Fergus KD. Embodied categorizing in the grounded theory method. Theory Psychol. 2006;16(4):483–503. https://doi.org/10.1177/0959354306066202 .
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Sandelowski M, Barroso J. Creating metasummaries of qualitative findings. Nurs Res. 2003;52(4):226–33. https://doi.org/10.1097/00006199-200307000-00004 .
Hill CE, Thompson BJ, Williams EN. A guide to conducting consensual qualitative research. Couns Psychol. 1997;25(4):517–72. https://doi.org/10.1177/0011000097254001 .
König J, Unterhitzenberger J, Calmer C, Kohout P, Karl R, Rosner R, Butollo W. What was helpful in today’s session? Responses of clients in two different psychotherapies for posttraumatic stress disorder. Psychotherapy. 2020;57(3):437–43. https://doi.org/10.1037/pst0000295 .
Sherrill AM, Maples-Keller JL, Yasinski CW, Loucks LA, Rothbaum BO, Rauch SAM. Perceived benefits and drawbacks of massed prolonged exposure: A qualitative thematic analysis of reactions from treatment completers. Psychol Trauma Theory Res Pract Policy. 2020. https://doi.org/10.1037/tra0000548 .
Tong J, Simpson K, Alvarez-Jimenez M, Bendall S. Distress, psychotic symptom exacerbation, and relief in reaction to talking about trauma in the context of beneficial trauma therapy: perspectives from young people with post-traumatic stress disorder and first episode psychosis. Behav Cogn Psychother. 2017;45(6):561–76. https://doi.org/10.1017/S1352465817000236 .
Wise A, Marich J. The Perceived effects of standard and addiction-specific EMDR therapy protocols. J EMDR Pract Res. 2016;10(4):231–44. https://doi.org/10.1891/1933-3196.10.4.231 .
* Shearing V, Lee D, Clohessy S. How do clients experience reliving as part of trauma-focused cognitive behavioural therapy for posttraumatic stress disorder? Psychol Psychother Theory Res Pract. 2011;84(4):458–75. https://doi.org/10.1111/j.2044-8341.2010.02012.x .
* Vincent F, Jenkins H, Larkin M, Clohessy S. Asylum-seekers’ experiences of trauma-focused cognitive behaviour therapy for post-traumatic stress disorder: a qualitative study. Behav Cogn Psychother. 2013;41(5):579–93. https://doi.org/10.1017/S1352465812000550 .
* Lowe C, Murray C. Adult service-users’ experiences of trauma-focused cognitive behavioural therapy. J Contemp Psychother. 2014;44(4):223–31. https://doi.org/10.1007/S10879-014-9272-1 .
* Murray H, Merritt C, Grey N. Clients’ experiences of returning to the trauma site during PTSD treatment: an exploratory study. Behav Cogn Psychother. 2016;44(4):420–30. https://doi.org/10.1017/S1352465815000338 .
* Hundt NE, Barrera TL, Arney J, Stanley MA. “It’s Worth It in the End”: Veterans’ experiences in prolonged exposure and cognitive processing therapy. Cogn Behav Pract. 2017;24(1):50–7. https://doi.org/10.1016/j.cbpra.2016.02.003 .
* Hundt NE, Ecker AH, Thompson K, Helm A, Smith TL, Stanley MA, Cully JA. “It Didn’t Fit for Me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17(4):414–21. https://doi.org/10.1037/ser0000316 .
* Boterhoven de Haan KL, Lee CW, Correia H, Menninga S, Fassbinder E, Köehne S, Arntz A. Patient and therapist perspectives on treatment for adults with PTSD from childhood trauma. J Clin Med. 2021;10(5):954. https://doi.org/10.3390/jcm10050954 .
* Doran JM, O’Shea M, Harpaz-Rotem I. In their own words: veteran experiences with evidence-based treatments for ptsd in the veterans health administration. Psychiatr Q. 2021;92(3):961–80. https://doi.org/10.1007/s11126-020-09861-z .
Baier AL, Kline AC, Feeny NC. Therapeutic alliance as a mediator of change: A systematic review and evaluation of research. Clin Psychol Rev. 2020;82:101921–101921. https://doi.org/10.1016/j.cpr.2020.101921 .
Harned MS, Schmidt SC. Perspectives on a stage-based treatment for posttraumatic stress disorder among dialectical behavior therapy consumers in public mental health settings. Community Ment Health J. 2019;55(3):409–19. https://doi.org/10.1007/S10597-018-0358-1 .
Gladis MM, Gosch EA, Dishuk NM, Crits-Christoph P. Quality of life: Expanding the scope of clinical significance. J Consult Clin Psychol. 1999;67(3):320–31. https://doi.org/10.1037/0022-006X.67.3.320 .
Forbes D, Bisson JI, Monson CM, Berliner L. Effective Treatments for PTSD: Guiding Current Practice and Future Innovation. In: Forbes D, Bisson JI, Monson CM, Berliner L, (eds.). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies (3rd ed.). New York, NY: Guilford Press; 2020. p. 3–12.
Dillon KH, LoSavio ST, Henry TR, Murphy RA, Resick PA. The impact of military status on cognitive processing therapy outcomes in the community. J Trauma Stress. 2019;32(2):330–6. https://doi.org/10.1002/jts.22396 .
Steenkamp MM, Litz BT, Marmar CR. First-line Psychotherapies for Military-Related PTSD. JAMA. 2020;323(7):656. https://doi.org/10.1001/jama.2019.20825 .
Straud CL, Siev J, Messer S, Zalta AK. Examining military population and trauma type as moderators of treatment outcome for first-line psychotherapies for PTSD: A meta-analysis. J Anxiety Disord. 2019;67:102133. https://doi.org/10.1016/j.janxdis.2019.102133 .
Varker T, Jones KA, Arjmand H-A, Hinton M, Hiles SA, Freijah I, Forbes D, Kartal D, Phelps A, Bryant RA, McFarlane A, Hopwood M, O’Donnell M. Dropout from guideline-recommended psychological treatments for posttraumatic stress disorder: A systematic review and meta-analysis. J Affect Disord Rep. 2021;4:100093. https://doi.org/10.1016/j.jadr.2021.100093 .
Crenshaw K. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. University of Chicago Legal Forum. 1989(8):139–67. https://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8/ .
Marsella AJ. Ethnocultural aspects of PTSD: An overview of concepts, issues, and treatments. Traumatology. 2010;16(4):17–26. https://doi.org/10.1177/1534765610388062 .
Corrigan PW, Druss BG, Perlick DA. The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychol Sci Public Interest. 2014;15(2):37–70. https://doi.org/10.1177/1529100614531398 .
Kleim B, Grey N, Wild J, Nussbeck FW, Stott R, Hackmann A, Clark DM, Ehlers A. Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. J Consult Clin Psychol. 2013;81(3):383–93. https://doi.org/10.1037/a0031290 .
d’Ardenne P, Heke S. Patient-reported outcomes in post-traumatic stress disorder. Part I: focus on psychological treatment. Dialogues Clin Neurosci. 2014;16(2):213–26. https://doi.org/10.31887/DCNS.2014.16.2/sheke .
Dell L, Sbisa A, Forbes A, O'Donnell M, Bryant R, Hodson S, . . . Forbes D. Effect of massed v. standard prolonged exposure therapy on PTSD in military personnel and veterans: A non-inferiority randomised controlled trial. Psychol Med. 2023;53(9): 4192–4199. https://doi.org/10.1017/S0033291722000927
Rauch SAM, Yasinski CW, Post LM, Jovanovic T, Norrholm S, Sherrill AM, et al. An intensive outpatient program with prolonged exposure for veterans with posttraumatic stress disorder: Retention, predictors, and patterns of change. Psychol Serv. 2021;18(4):606–18. https://doi.org/10.1037/ser0000422 .
Gwozdziewycz N, Mehl-Madrona L. Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. Perm J. 2013;17(1):70–8. https://doi.org/10.7812/TPP/12-058 .
Download references
Acknowledgements
The authors would like to thank the participants from the primary studies for their contribution.
Open access funding provided by Copenhagen University
Author information
Authors and affiliations.
Department of Psychology, University of Copenhagen, 2A Oester Farimagsgade, 1353, Copenhagen, Denmark
Solveig Flem Gjerstad, Stig Poulsen & Erminio Francesco Antares Spadaro
DIGNITY- Danish Institute Against Torture, Copenhagen, Denmark
Linda Nordin & Sabina Palic
Department of Psychology, Lund University, Lund, Sweden
Linda Nordin
Department for Treatment of Borderline Personality Disorder and Self-Harm, Psychiatric Centre Glostrup, Mental Health Services in the Capitol Region of Denmark, Copenhagen, Denmark
Sabina Palic
Clinical Department of Eating Disorders, Mental Health Centre Ballerup, Mental Health Services in the Capitol Region of Denmark, Copenhagen, Denmark
Solveig Flem Gjerstad
You can also search for this author in PubMed Google Scholar
Contributions
SFG completed the systematic search, reviewed, analysed and synthesised the data. SaPa designed the study and LN and SaPa screened articles for inclusion for credibility checks. StPo reviewed the manuscript through the initial preparation. EFAS conducted an independent analysis and synthesis of the data. All authors read, made amendments to, and approved the final manuscript.
Authors’ information
Solveig Flem Gjerstad is a clinical psychologist. She earned her Master's degree in clinical psychology at University of Copenhagen and her Bachelor’s degree in General Psychology at University of Bergen, including a scholarship semester at University of Sydney. Currently she practises Dialectical Behavioural Therapy in a treatment facility for eating disorders. ORCID: 0000-0001-6744-8262.
Linda Nordin is a clinical psychologist and a researcher at DIGNITY - Danish Institute Against Torture with an affiliation at Lund University, Department of Psychology. Her main focuses of research are trauma, PTSD, refugees, and pain. ORCID: 0000-0002-8533-520X.
Stig Poulsen is Professor in Clinical Psychology and Psychotherapy at the Department of Psychology, University of Copenhagen. His main area of research is the process and outcome of psychotherapy and he has a particular focus on qualitative research in client experiences of psychotherapy. ORCID: 0000-0002-0536-1820.
Erminio Francesco Antares Spadaro graduated in Psychology at Università degli Studi di Messina (IT) (Bachelor program) and in Clinical Psychology at Università degli Studi di Palermo (IT) (Master program). He was trained as a Counselor in Family Constellations with Ad Vitam Geminos Association. He currently works as a research assistant at the Department of Psychology, University of Copenhagen.
Sabina Palic is a clinical psychologist and senior researcher at DIGNITY - Danish Institute against Torture and at Department for Treatment of Borderline Personality Disorder and Self-harm, Psychiatric Centre Glostrup. Her main areas of clinical and research interest is treatment of trauma and complex PTSD. She practises trauma-focused therapy, namely Prolonged Exposure (PE) and Narrative Exposure Therapy (NET). ORCID: 0000-0002-9686-9370.
Corresponding author
Correspondence to Stig Poulsen .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary materials 1., supplementary materials 2., supplementary materials 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gjerstad, S.F., Nordin, L., Poulsen, S. et al. How is trauma-focused therapy experienced by adults with PTSD? A systematic review of qualitative studies. BMC Psychol 12 , 135 (2024). https://doi.org/10.1186/s40359-024-01588-x
Download citation
Received : 16 January 2023
Accepted : 12 February 2024
Published : 09 March 2024
DOI : https://doi.org/10.1186/s40359-024-01588-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Qualitative research
- Patient experience
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
ORIGINAL RESEARCH article
“you can’t really have a relationship with them because they just ask you questions”: understanding adolescent dropout – an empirical single case study.

- 1 Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom
- 2 Anna Freud National Centre for Children and Families, London, United Kingdom
Introduction: High dropout rates are common in youth psychotherapy, including psychoanalytic psychotherapy, yet the reasons behind this trend remain obscure. A critical focus to enhance adolescent engagement could be the therapeutic alliance, particularly in resolving alliance ruptures. This study sought to clarify the complex relationships between the therapeutic alliance, encompassing alliance ruptures and resolutions, and dropout within the context of poor outcome. It investigated a single case of an adolescent with depression who dropped-out of Short-Term Psychoanalytic Psychotherapy, without showing clinical improvement.
Method: Data was garnered from diverse sources, including questionnaires, interviews, and session recordings, and analyzed through a mixed-method longitudinal framework. This encompassed views from the adolescent, therapist, parents, and external evaluators.
Results: The study identifies several factors impacting the decision to drop out, including initial profound distrust toward the therapist, a complex and difficult therapeutic relationship characterized by unresolved alliance ruptures, and sporadic attendance. External factors including minimal parental engagement with therapy were also seen as detrimental to the adolescent’s involvement and progress.
Discussion: The research underscores the challenges in engaging adolescents, especially when there may be distrust of professionals, and in the absence of parental involvement with treatment.
1 Introduction
Dropout from psychological treatment is a pressing issue in mental health services and is acknowledged as a significant challenge for clinicians ( Leibovich et al., 2019 ), particularly when working with young people. Defined as a client discontinuing therapy without their therapist’s agreement, dropout is estimated to impact around 45% of young people commencing therapy ( De Haan et al., 2013 ). It is often linked to dissatisfaction with the treatment ( O’Keeffe et al., 2019b ), and those who drop out may not fully reap the benefits of the treatment ( Cooper et al., 2018 ), underlining the importance of understanding what causes dropout and how it can be avoided.
A number of factors have been examined in previous research as contributing to treatment dropout. While variables such as symptom severity, socioeconomic status, and ethnicity show inconsistent predictive power regarding dropout in youth therapy ( O’Keeffe et al., 2018 ), the establishment of a strong therapeutic alliance early in treatment consistently appears as a significant factor when trying to prevent dropout. The alliance, as conceptualized within therapeutic contexts, pertains to the collaborative facets of the relationship between the patient and therapist, facilitating their joint efforts toward shared goals and the cultivation of a positive rapport ( Bordin, 1979 ). A strong alliance has been found to be consistently associated with increased engagement and positive treatment outcomes across various treatment types for adolescents ( Daly et al., 2010 ; Gersh et al., 2017 ; Schenk et al., 2019 ; Cirasola et al., 2022 ). On the contrary, poor alliance and unresolved issues within the therapeutic relationship, including alliance ruptures, have been found to be significantly linked with reduced engagement and a higher likelihood of dropout ( Eubanks et al., 2018 ; O’Keeffe et al., 2020 ).
Alliance ruptures refer to difficulties in working together toward therapy goals and breakdowns in the therapeutic bond ( Safran and Muran, 2000 ; Muran and Eubanks, 2020 ). These ruptures manifest through withdrawal or confrontation markers. Withdrawal rupture markers can be considered as ‘movements away’ from the therapist and/or the therapy and arise when clients either distance themselves from the therapist or the therapeutic process, for instance, by giving minimal responses, evasive storytelling, or exhibiting self-criticism and hopelessness. They may also involve moving toward the therapist, but in a way that disguises and distances them from their true feelings, such as through denial, separating content from emotion, or deferential behaviors. Conversely, confrontation markers can be considered as ‘movements against’ the therapist and/or the therapy and involve actions against the therapeutic work, including complaints, criticism, resistance, or attempts to control the session. A rupture is deemed resolved when the client and therapist re-establish a positive emotional connection and resume collaborative therapy.
Effectively addressing these relational issues is particularly vital when working with adolescents, a group with high incidence of ruptures and dropout ( Schenk et al., 2019 ; O’Keeffe et al., 2019a ; Cirasola et al., 2022 ). The unique developmental challenges of adolescence, such as increased individuation, identity exploration, and emerging autonomy, significantly influence these dynamics ( DiGiuseppe et al., 1996 ; Binder et al., 2008 ; Schenk et al., 2019 ; Cirasola et al., 2022 ). Adolescence is marked by a push-pull between seeking autonomy and needing support and guidance, often leading to difficulties in forming and sustaining a therapeutic alliance with an adult clinician. Additionally, factors like evolving self-perception, changing interpersonal relationships, risk-taking behaviors, and cognitive development add to the complexities of engaging adolescents in therapy ( Gulliver et al., 2010 ; Schenk et al., 2019 ; Cirasola and Midgley, 2023 ).
Understanding and effectively managing alliance ruptures is vital for successful psychotherapy, but research in this area has predominantly centered on adults, leaving a considerable knowledge gap in youth psychotherapy. Building a robust alliance and resolving ruptures is especially pertinent in psychodynamic treatments with young people. Empirical studies have identified frequent alliance ruptures in this context ( Halfon et al., 2019 ; Schenk et al., 2019 ; Cirasola et al., 2022 ) and lower alliance ratings compared to other therapeutic modalities ( Cirasola et al., 2021 ). This could be attributed to the psychoanalytic approach’s emphasis on creating a space where negative emotions, often manifested through negative transference, are openly expressed ( Cregeen et al., 2017 ). Therapists in this framework strive to recognize and support the expression of these negative emotions toward the therapist, showing tolerance and acceptance. The deliberate encouragement of expressing negative emotions, along with other aspects of psychoanalysis that intentionally induce some frustration (e.g., not directly answering personal questions), may lead to more pronounced alliance ruptures, reflected in lower alliance ratings. The impact of this on treatment outcomes remains a subject for further investigation.
In psychoanalytic therapy, it is also critical to consider that certain techniques might challenge the therapeutic relationship. Unlike some other therapies, psychoanalytic psychotherapy often adopts a less directive approach, emphasizing the young person’s autonomy in exploring their own thoughts and emotions ( Cregeen et al., 2017 ). This means therapists typically refrain from structuring sessions rigidly and limit self-disclosure, adopting a more ‘neutral’ stance to facilitate the young person’s exploration of their internal world, including transference. This approach can lead to prolonged silences, where therapists encourage young people to uncover their thoughts and feelings independently rather than providing immediate explanations or reassurance. While these techniques are fundamental to the psychoanalytic method, they may pose challenges for young people unaccustomed to this style of therapy. Research suggests that extended periods of silence, particularly when a young person is withdrawing or having difficulty expressing emotions, can adversely affect the therapeutic relationship ( Acheson et al., 2020 ). Further research is needed to guide therapists in applying these techniques effectively, fostering a strong therapeutic relationship and addressing potential ruptures.
To address this need, this study utilizes a case study approach to investigate the complex relationships between therapeutic alliance, dropout rates, and unfavorable outcomes in adolescents with depression undergoing Short-Term Psychodynamic Psychotherapy (STPP). Specifically, this study aims to:
• Describe the development of the therapeutic alliance, including its ruptures and resolutions, within the context of a single STPP case involving an adolescent with depression who dropped out of therapy, and exhibited a poor treatment outcome.
• Explore the factors influencing the young person’s decision to discontinue treatment, with a specific focus on the role of the therapeutic relationship, particularly the alliance and its rupture and resolutions.
The case study design was selected for its ability to offer a detailed and context-rich examination of the intricate dynamics in patient-therapist interactions, providing insights that are not readily obtained through group-based analyses ( McLeod, 2013 ). This focused methodology allows for an in-depth investigation, illuminating the complexities of the therapeutic relationship and its influence on treatment outcomes.
2 Materials and methods
This study adopted a longitudinal, mixed-methods case study approach, examining a single case from the IMPACT-ME study ( Midgley et al., 2014 ), the qualitative component of the IMPACT clinical trial, evaluating the effectiveness of three psychological treatments of depression in adolescents ( Goodyer et al., 2017 ). Comprehensive details of the methods and procedures of the clinical trial and associated qualitative investigation are detailed in Goodyer et al. (2017) and Midgley et al. (2014) .
2.2 Ethical considerations
The research protocol was approved by the Cambridgeshire 2 Research Ethics Committee (REC Reference: 09/HO308/137). Informed written consent was obtained from all participants, including parental consent. To maintain confidentiality, all identifying personal information has been anonymised.
2.3 Case selection
To select a suitable case, the IMPACT-ME database was examined to identify:
a. Cases referred for Short-Term Psychoanalytic Psychotherapy (STPP);
b. With available post-therapy interviews with the adolescent, their caregiver, and the therapist, to provide a comprehensive exploration of their views on the therapeutic relationship, process, and outcome;
c. Recorded as ‘drop out’ in the study database, indicating therapy was ended prematurely without therapist agreement;
d. Negative outcomes, indicated by scores consistently above the clinical threshold (27 or above) on the primary outcome measure, the Moods and Feelings Questionnaire (MFQ), at both the end of therapy and the one-year follow-up;
e. With complete audio recordings of therapy sessions, to allow a thorough and comprehensive evaluation of changes in the therapeutic alliance;
Of the 27 STPP cases in the IMPACT-ME study, 18 had complete interviews. Among these, 9 were identified as dropouts, and of these 5 had poor outcome, but only the chosen case had the full set of sessions audio recordings. Further details of the case are provided, below.
In respecting the privacy of the individuals involved, certain specifics about the backgrounds of the young person and their family have been omitted or changed. However, all pertinent information relevant to the therapeutic alliance and its dynamics remains unaltered.
2.4 Treatment
Short-Term Psychodynamic Psychotherapy (STPP) as described by Cregeen et al. (2017) , is a structured therapy consisting of up to 28 sessions over a period of 30 weeks. Parents were also given the opportunity to engage in up to seven sessions of parent work with a separate clinician. Based on psychoanalytic principles, STPP views behavioral and emotional issues as linked to early relational experiences and current developmental challenges. By actively engaging with both transference and countertransference, STPP seeks to reveal the deeper dynamics underlying symptoms, aiming to enhance adolescents’ ability to regulate emotions and develop and maintain healthy relationships.
The therapist offering the STPP, referred to here as Dr. P, was a male child and adolescent psychoanalytic psychotherapist, accredited by the Association of Child Psychotherapists in the UK. No further demographic information about the therapist was available.
2.5 Measures
2.5.1 alliance.
The therapeutic alliance was assessed using the Working Alliance Inventory Short-form (WAI-S; Horvath and Greenberg, 1989 ; Tracey and Kokotovic, 1989 ) from both the adolescent and therapist perspectives at 6, 12, and 36 weeks post-randomization. The WAI-S comprises 12 items, rated on a 7-point Likert scale, measuring three dimensions: (1) goals agreement, (2) tasks agreement, and (3) emotional bond between client and therapist, with higher ratings indicating a stronger alliance. It demonstrates good construct validity ( r = 0.74 to r = 0.80) and strong internal consistency in adult ( α = 0.93) and youth samples ( α = 0.94). In the IMPACT study also showed robust internal consistency ( α = 0.95).
2.5.2 Outcome
Aligned with the IMPACT study, this research used the 33-item MFQ ( Angold et al., 1987 ) to assess self-reported depression symptoms. A score of 27 on the MFQ signifies the clinical threshold for a major depressive episode ( Wood et al., 1995 ). Assessments occurred at baseline, and post-randomization at 6 and 12 weeks (during treatment), 36 weeks (end of treatment), and 52 and 86 weeks (post-treatment follow-ups). The MFQ demonstrates good reliability ( r = 0.78), strong internal consistency ( α = 0.82), and criterion validity ( α = 0.89) for identifying adolescent depression episodes ( Wood et al., 1995 ; Kent et al., 1997 ).
2.5.3 Alliance rupture and resolutions
The latest version of the Rupture Resolution Rating System (3RS v2022; Eubanks et al., 2022 ) was used to identify alliance ruptures and resolutions. This observer-based measure codes ruptures and resolutions in recorded therapy sessions. Ruptures, categorized as withdrawal and confrontation, are assessed on a 5-point scale using the 3RS, with 1 indicating ‘Not present/salient’ and 5 indicating ‘Present, very salient.’ The salience reflects the impact on the alliance. Tables 1 , 2 provide detailed descriptions of withdrawal and confrontation rupture markers, along with resolution strategies. Resolution effectiveness is indicated by repair anchors, ranging from 1 (Ruptures not successfully repaired, alliance worsened) to 5 (Ruptures well repaired).
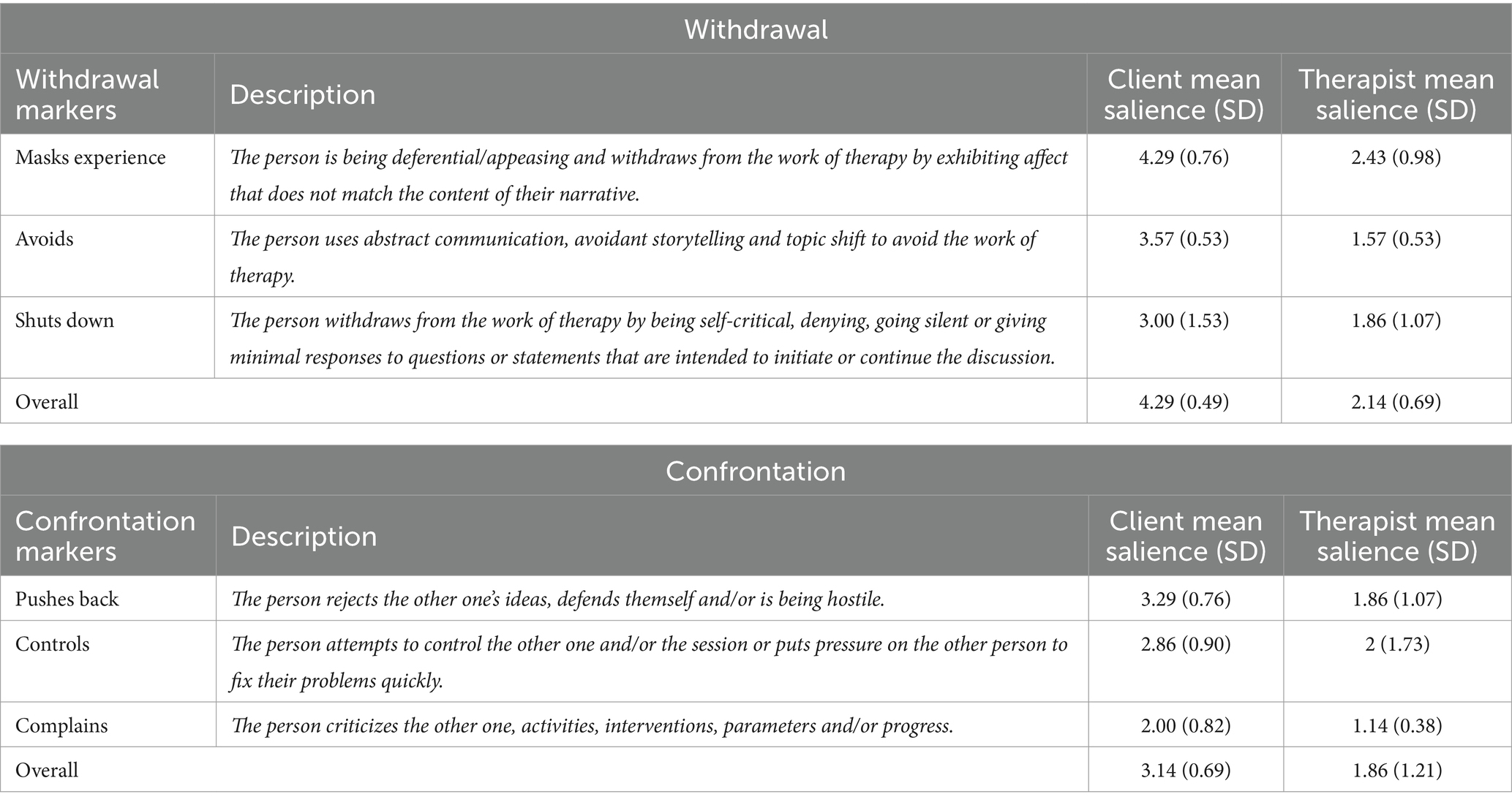
Table 1 . Description and mean salience of 3RS withdrawal and confrontation rupture markers.
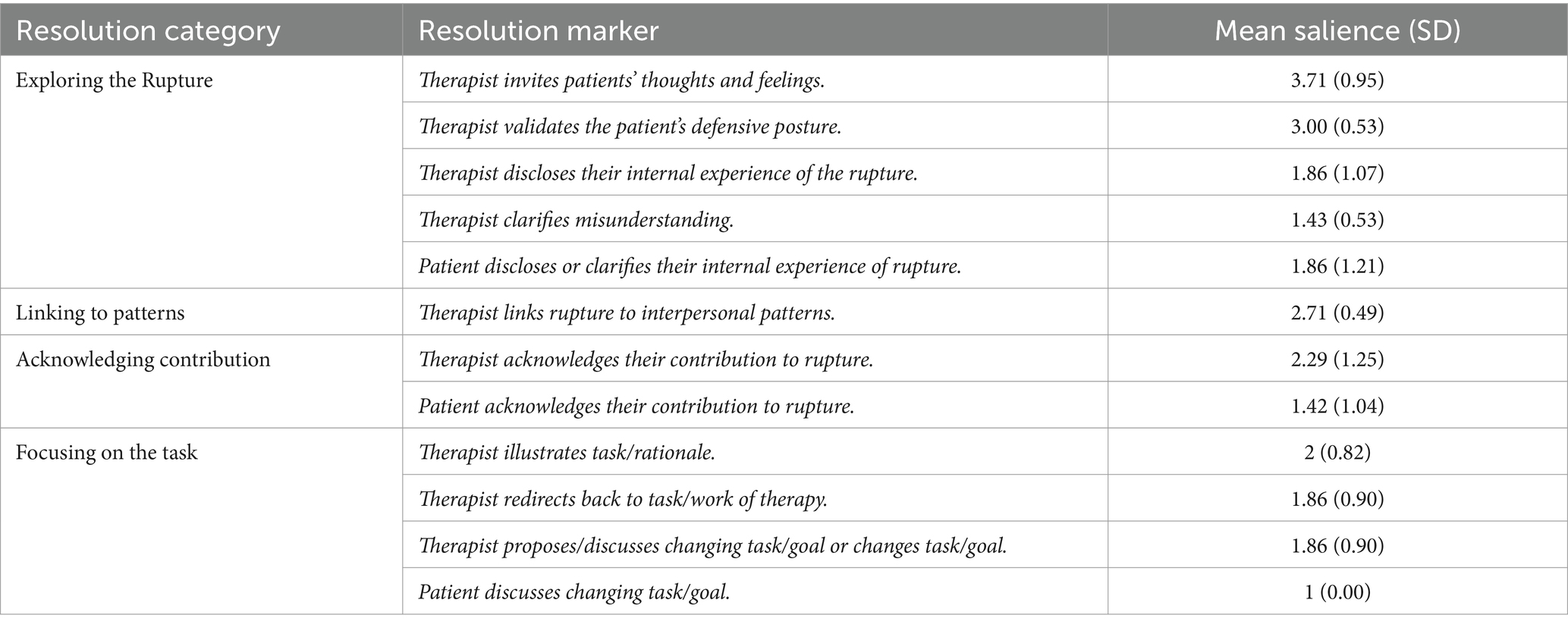
Table 2 . Description and mean salience of 3RS resolution markers.
The 3RS incorporates a Working Together (WT) subscale, based on Bordin’s (1979) alliance model. This subscale assesses goal agreement and task collaboration, trust, and contributions of the therapist and patient to their relationship on a 5-point scale. A score of 1, ‘Not salient,’ indicates ineffective collaboration, while 5, ‘Very salient,’ suggests a high level of collaborative effort. An average score of 3 indicates some degree of collaboration between the patient and therapist, possibly involving cooperative efforts or engagement in a shared task toward a common goal.
2.5.4 Therapy interviews
Semi-structured interviews using the Experience of Therapy Interview ( Midgley et al., 2011 ) were conducted at three time points: baseline (T1, before therapy started), 36 weeks post-randomization (T2, end of therapy), and 86 weeks post-randomization (T3, 1 year follow-up). An independent research psychologist conducted separate interviews with adolescents and their primary caregivers at all time points. Additionally, the therapist was interviewed at T2 only with the young person’s consent. These interviews aimed to capture diverse perspectives on the therapeutic process and outcomes from the therapist, patient, and caregiver.
2.6 Data analysis
To describe the alliance and its rupture and resolutions over the course of treatment, all session recordings were analyzed by two independent raters using the 3RS to evaluate the occurrence and type of alliance rupture resolutions. To achieve a comprehensive understanding of the therapeutic relationship and its influence on therapy outcomes and processes from multiple perspectives, we employed a dual-method approach. First, we used self-reported alliance ratings (WAI-S and WAI-T) obtained from both patients and therapists. Second, we conducted qualitative analyses of transcripts derived from seven interviews, conducted at different time-points, and involving the therapist, client, and caregiver. The interviews underwent independent analysis by two raters utilizing the framework analysis method, as outlined by Parkinson et al. (2016) . Framework Analysis entailed the construction of an analytical framework, incorporating predefined research topics and emerging themes from the data (refer to Supplementary Table 1 ). Ultimately, the information gathered from these diverse sources was synthesized in a narrative form to comprehensively address the study’s aims using a multi-perspective approach.
2.6.1 Epistemological position and reflexivity
This single case study employs a mixed-methods design from a critical realist epistemological perspective ( McEvoy and Richards, 2006 ). Critical realism suggests that research data provide insights into reality but do not directly access it, thus necessitating a combination of various observations and analyses for a comprehensive understanding ( Edgley et al., 2016 ). This approach underscores the importance of utilizing multiple measures and observations, which, despite potential errors, collectively enhance understanding and mitigate biases ( Creamer and Reeping, 2020 ).
Given the variability of the alliance construct in youth psychotherapy, influenced by unique patient and therapist characteristics, therapy type, and dynamic interactions throughout treatment, this study employs a mixed method approached and various sources of information. These include questionnaires, interviews, and audio recordings of therapy sessions, gathered from various perspectives (e.g., adolescent, therapist, parent, observers).
From this epistemological position, we approached the data with a sense of curiosity and objectivity, seeking to mitigate the influence of subjective biases. To achieve this, not only did at least two independent researchers look at each set of data, but reflective accounts were diligently composed subsequent to the analysis of each therapy session and interview. Furthermore, multiple meetings were convened among the researchers and senior authors, fostering an environment conducive to the thorough exploration of the data. Despite the inherent potential for subjectivity in the analysis process, meticulous efforts were exerted to ensure the provision of a transparent and comprehensive portrayal of the case.
2.6.2 Raters, inter-rater reliability and credibility checks
With regards to the sessions assessments, the first author, a qualified clinical psychologist, assessed each therapy session using the 3RS. To confirm the inter-rater reliability of these ratings, the second author independently re-evaluated sessions using the 3RS, but only after completing the interview analyses to minimize biases. Cohen’s linearly weighted kappa (κ) and the Intraclass Correlation Coefficient (ICC) were calculated to assess their level of agreement on the 3RS ratings. The results indicated excellent agreement on client withdrawal ruptures ( κ = 1), substantial agreement on therapist withdrawal ruptures ( κ = 0.81), rupture resolution ( κ = 0.84), and the Working Together score (ICC = 0.81; using a two-way model with absolute agreement). Moderate agreement was observed for client confrontation ruptures ( κ = 0.76) and therapist confrontation ruptures ( κ = 0.71).
For the post-therapy interviews, the transcripts were independently examined by two post-graduate students, which included the second author and another independent researcher. Both were MSc psychology students and were blind to any information pertaining to the specific case. Subsequently, the different elements of the data underwent a comprehensive review and audit conducted by the first and last authors.
3.1 Case overview
‘Morgan’ was 17 at the start of treatment, and was assessed as having severe depressive symptoms, including suicidal thoughts, sleep disturbances, and a downturn in academic performance. Due to the severity of her symptoms, alongside being referred to Child and Adolescent Mental Health Services (CAMHS), she was prescribed SSRI medication. As part of the IMPACT study, she was randomly assigned to attend Short-Term Psychodynamic Psychotherapy (STPP).
In the interviews, both the therapist and Morgan’s parents expressed serious concern about Morgan’s condition at the time of referral. Although Morgan expressed willingness to be “sorted out,” she also revealed hesitations and mistrust toward mental health professionals. Out of 28 planned sessions, Morgan attended only seven, and then dropped out of treatment after 15 weeks without formal agreement or communication with her therapist.
As displayed in the last column of Table 3 , Morgan exhibited a high MFQ score at baseline, signifying severe depression. Although the score initially decreased after 12 weeks, it later increased and consistently remained within the clinical range at all time points. Therefore, Morgan aligns with the profile of a ‘halted improver’– essentially a non-responder to treatment, mirroring a pattern observed in approximately 15% of cases in the IMPACT study ( Davies et al., 2019 ). In line with the persistently high MFQ scores, Morgan, her parents, and Dr. P. were all in agreement that Morgan did not experience significant benefits from the therapy. Yet, Dr. P. harbored the hope that through therapy, Morgan, at the very least, had a positive experience where someone actively advocated for her well-being.
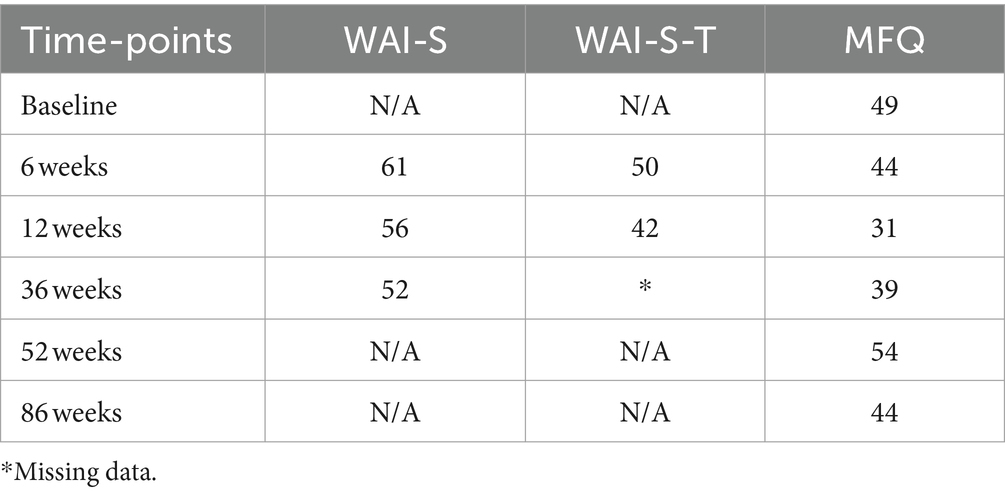
Table 3 . MFQ, WAI-S and WAI-S-T ratings at all time points.
3.2 The alliance and its dynamics in this case
As shown in the first two columns of Table 3 , both Morgan (WAI-S) and Dr. P. (WAI-S-T) consistently rated the alliance just above average across all assessment points, with a gradual decline over time, which suggests a potential weakening of the alliance. While Table 3 indicates a decline in the alliance over time and a lack of improvement in symptoms, this pattern cannot in itself establish a direct causal link between a worsening in the alliance and therapeutic outcomes.
The challenges to developing and maintaining a good therapeutic alliance, as demonstrated by the WAI ratings, was further supported by the session-by-session 3RS ratings. Table 4 presents the ratings for 3RS Salience Ratings for the observed rupture and resolutions events, including overall resolution and working together scores, for each session. Furthermore, the last row displays the average salience scores for alliance ruptures, resolutions, and collaborative work (3RS) across all sessions. In alignment with the self-reported alliance ratings, the observer-based 3RS ‘Working Together’ scale indicates an overall average level of collaboration, with subtle decline in the later sessions compared to the initial ones, signifying a diminishing ability for Morgan and Dr. P. to work together and trust each other.
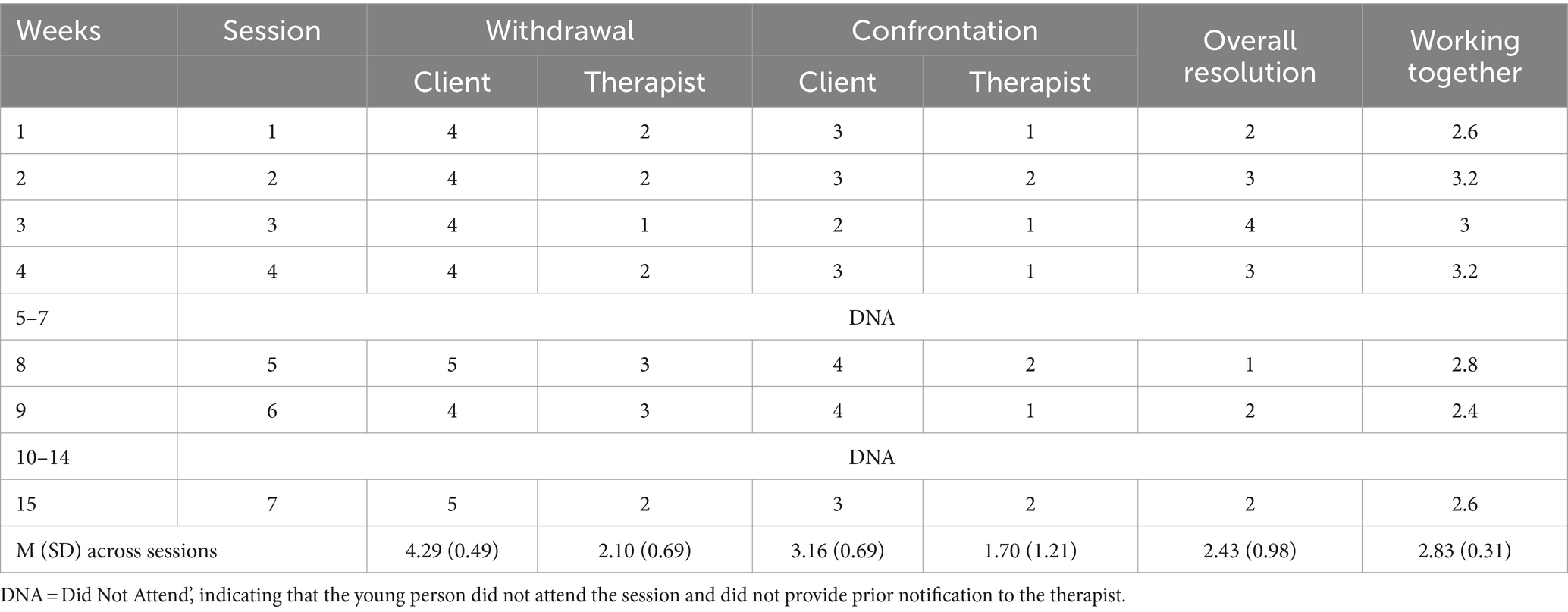
Table 4 . 3 RS salience ratings scores for each session and mean (M) and standard deviation (SD) scores across all sessions.
Morgan’s consistent display of rupture markers and limited engagement throughout the treatment, as demonstrated by the 3RS scoring of the sessions, serves to support the identified patterns. Over the course of seven attended sessions, Morgan showed a large number of rupture markers, averaging 22 markers per session. Notably, withdrawal emerged as the predominant type, constituting 66% of the total rupture markers observed. These withdrawal markers had a notably higher impact on the therapeutic alliance compared to confrontational markers, as evidenced by ratings of 4 or above on the 3RS rupture salience scale across sessions.
Although confrontation rupture markers were less prevalent, they still exerted a moderate to high impact on the therapeutic alliance, particularly in later sessions, where they were rated 3 or above on the 3RS rupture salience scale. This observation aligns with the self-ratings of the alliance provided by both Morgan and Dr. P., confirming a potential deterioration in the alliance and an escalation of tension in the therapeutic relationship as therapy progressed, ultimately leading to dropout.
Furthermore, an analysis of the 3RS ratings of the resolution of the ruptures within and across sessions reveals that approximately 58% of the sessions scored 2 or below on the overall resolution scale, indicating suboptimal resolution of ruptures in the majority of sessions. This is particularly evident in sessions preceding dropout, where most ruptures remained unresolved.
Table 1 outlines rupture markers and their average impact in all sessions. Morgan’s most salient withdrawal rupture marker, ‘mask her real experience,’ reflected her tendency to disengage by expressing incongruent emotions, often through sarcasm, especially in challenging situations. An example of this is illustrated in the following session excerpt, where the corresponding 3RS markers are noted in parentheses:
Therapist (T): I’ve noticed that— this is going to sound like a criticism— but I’ve noticed that you do not have a routine, that you do not sort of manage your own life in a sense.
Morgan (M): Nope! (loud and funny tone) [mask her real experience].
T: No. And that’s a bit, like, It’s a bit like you are kind of floating about like a bit of a mess sometimes.
M: (laughs) I am like a cloud! (funny, loud tone) [content-affect split].
Morgan also frequently showed indications of withdrawal ruptures in therapy by (a) evading through actions like switching topics, going off on tangents, and using abstract language, or (b) shutting down with minimal responses and inadequate engagement in discussions. An example is provided below, where Morgan used vague language when asked about her feelings toward a friend:
T: You seem to be very close to her, how is she?
M: She’s how you’d imagine her to be [abstract communication & minimal response].
T: How is that? [invites thoughts and feelings].
M: Its (long pause) [minimal response].
T: People have all different types of friends, do not they? [invites thoughts and feelings].
M: Like (pause) nice and (pause) friendly (pause) (laughs) [abstract communication].
Although less frequent than withdrawal markers, Morgan regularly exhibited confrontation rupture markers too, which were rated as moderately affecting the therapeutic alliance, as indicated by 3RS salience ratings (see Tables 1 , 4 ). The most salient confrontation marker involved Morgan pushing back against therapy or the therapist’s interventions. An example is provided below, where Morgan reacted to the therapist’s remarks with a mix of disbelief and humor:
T: So, you are sort of being critical of yourself for that… Is it like a voice in your head, like your thoughts telling you that you are--.
M: What a peculiar way of putting it! (loudly with an exaggerated tone, then chuckles) [rejects intervention].
T: (laughs) Is it? [Invites thoughts and feelings].
M: Yeah! (continues laughing) A voice in my head?? Yes, there is a voice in my head! I’ve gone mental! (Loudly, with a funny tone) [masks real experience, indirect complaints].
Morgan also demonstrated confrontation rupture markers when attempting to exert pressure or control over the therapist, particularly when asking him personal questions about his age or his work. These instances persisted despite the therapist’s efforts to steer the conversation back to other topics. Moreover, there were moments when Morgan expressed dissatisfaction with the therapist, indirectly indicating her preference for a female psychiatrist she had previously consulted.
Despite the therapist’s ongoing efforts to repair ruptures (averaging 21.4 attempts per session), their effectiveness was generally limited, with most sessions scoring 2 or below on the 3RS overall resolution scale, indicating a lack of resolution. Not only were Dr. P.’s efforts to repair ruptures mostly rated as unsuccessful, but he also displayed withdrawal rupture markers on some occasions (an average of 5.7 per session), even if these markers had minimal impact on the alliance (scoring below 2 on the 3RS salience score). These primarily involved ‘masking his real experience.’ For example, there were times when Dr. P.’s emotional responses seemed misaligned with the content being discussed, such as laughing when he appeared uncomfortable. This was most noticeable in response to Morgan’s personal questions. Dr. P. typically adhered to what might be considered a traditional psychoanalytic stance, avoiding direct personal disclosure (e.g., by replying ‘this is more about you than about me’ when asked a personal question), which was sometimes rated on the 3RS as a movement away from the young person (withdrawal rupture). Alternatively, he focused on exploring the underlying motives behind Morgan questions instead of directly answering them. Both approaches often resulted in increased withdrawal markers from Morgan, as shown in the following excerpt following Morgan’s query about the therapist’s life at her age:
T: Maybe you are wondering if erm I was like you at your age?
M: Not really, just trying to make conversation. [long silence] [rejects intervention, minimal response].
Table 2 presents a summary of Dr. P’s strategies for addressing ruptures, including their average significance. He mainly used exploratory strategies, which involved delving into the rupture and its underlying reasons or patterns. This typically included encouraging the young person to explore her thoughts and feelings and validating her experiences. For example, when Morgan discussed upsetting issues with humor, the therapist promoted further exploration (e.g., ‘Oh gosh, what’s it like for you?’). In situations involving confrontational ruptures, such as Morgan expressing dissatisfaction with an intervention made by Dr. P., he responded by acknowledging and validating Morgan’s feelings, regardless of their negativity, as in the following example where he addressed Morgan’s challenges in engaging with therapy:
T: I get that, therapy is a really strange process to get used to, is not it? […] And it takes a bit of getting used to it because normally you know, you do not usually say everything that’s in your mind, do you? [validate defense].
Dr. P. also used immediate resolution strategies aimed at steering the therapy back on course or reducing the emotional intensity. For instance, when Morgan deviated from a topic in an avoidant manner, Dr. P. redirected the conversation to more pertinent subjects. Moreover, when facing signs of Morgan’s withdrawal ruptures, such as minimal responses, he showed flexibility by shifting to a different topic, as demonstrated in the following exchange:
T: Hmm. Probably more importantly, how are you feeling? (both laugh).
M: Yeah. (quietly) I’m okay. (long silence) [minimal response].
T: So, painting is something that you have always done for pleasure, is not it? [change topic].
Despite the therapist’s continued efforts to address ruptures, few ruptures were successfully repaired. Of these, a notable instance of rupture resolution occurred when the therapist authentically shared his feelings. This not only repaired the rupture but also actively involved Morgan in the resolution process.
T: — And I noticed that it was, um, it was after I told you that we were going to have a break over the holiday, that you did not come. [invites thoughts and feelings].
M: Yeeeaah aaaand???? (exaggerated, loud tone) [controls/puts pressure on the T].
T: Um, I was thinking about what you were saying about feeling abandoned and I was wondering if sometimes, without thinking, that you wanted to give me an experience of being abandoned. [invites thoughts and feelings].
M: Nooo! (exaggerated, loud tone) [pushes back/rejects idea].
T: Not consciously […] and I might not have explained myself correctly [acknowledge contribution].
M: Yeah! I wasn’t trying to make you feel abandoned! [rejects intervention].
T: No, I’m not saying it was like “right! I’m going to” [clarify misunderstanding].
M: “I’m going to abandon him!” (Loudly, with an exaggerated tone).
T: […] I just mean sometimes people do things without thinking, and it’s kind of giving me the personal experience of what it’s like [clarify misunderstanding]. And I wonder…
M: Did you feel abandoned? (Exaggerated tone) [puts some pressure on the therapist].
T: I felt concerned about where you were and… um… worried and… yeah I suppose, maybe abandoned is not quite the right word, but yeah, it certainly was an experience of not knowing what was going on [disclose internal experience].
M: Hm. Sorry for not turning up on those days. It wasn’t intentional. [P acknowledges contribution].
Despite the therapist’s persistent efforts, such as in the extract above, effectively engaging Morgan proved to be a persistent challenge as evidenced by her repeated session absences and sustained withdrawal rupture behaviors that remained unresolved. The ratings on the 3RS align with findings obtained from qualitative analysis of interviews conducted with both Morgan and the therapist. As elaborated below, both parties characterized their relationship as inherently challenging, offering insightful perspectives on the factors contributing to the intricacies of their interaction and how these dynamics may have impacted the overall therapeutic outcome.
3.3 Therapeutic relationship and treatment drop-out
Morgan’s decision to end the therapy prematurely without informing Dr. P. seems to be consistent with her tendency to withdraw when faced by alliance ruptures, as emerged from the session ratings. In her interview, she explained her decision to end therapy without first speaking to the therapist, stating: “It would have made me feel really guilty, so I just did not go.” Various factors influenced this decision, encompassing, but not limited to, a challenging relationship with Dr. P.
In the post-therapy interviews, Morgan identified a number of issues that contributed to her decision to drop out of therapy, including: (a) perceiving the therapy as unhelpful, (b) feeling inherent mistrust of mental health professionals, and (c) challenges in her relationship with Dr. P. From the therapist’s perspective, potential contributors to the decision were (a) Morgan’s difficulty in making use of the offered interventions, (b) challenges in their relationship, and (c) external circumstances in Morgan’s life, especially the lack of parental involvement in the therapy. The parents’ interviews did not uncover any additional factors. Morgan’s parents mainly mentioned the lack of progress and appeared to have limited knowledge about Morgan’s therapy experiences. They only shared Morgan’s reason for discontinuing therapy when she expressed, ‘It’s making me feel terrible. I do not want to continue.’ Moreover, the parents stressed that they were dealing with family issues, which hindered their ability to engage actively in Morgan’s treatment and they did not attend any of the parent sessions offered to them.
A key impediment to treatment engagement appeared to be Morgan’s skepticism toward mental health professionals. She openly conveyed her belief that clinicians, including Dr. P., could not fully understand or genuinely care about her difficulties. She acknowledged how this created a barrier from the onset of therapy, stating that her difficulty in trusting people “probably pre-determined that [she] wasn’t gonna open up.” This sense of distrust persisted over time, evident in her sentiments during the one-year follow-up interview: ‘I do not know…what they [mental health professionals] do but it just they make you feel so small and insignificant…(sighs)… (pause)… acting like they care.” This underscores how her initial reluctance to trust the therapist remained a persistent issue even after the therapy had ended.
Both Morgan and Dr. P. characterized the therapeutic relationship as challenging, and this dynamic appeared to have influenced the lack of engagement. While both parties acknowledged challenges in their relationship and found common ground on some contributing factors, they also highlighted unique elements that played a role in exacerbating these difficulties.
Morgan expressed dissatisfaction with the therapeutic relationship, particularly noting what she felt was its one-sidedness. She emphasized the lack of personal disclosure from the therapist, hindering the formation of a meaningful connection. She even said that she was not able to provide an in-depth description of their relationship, since she felt: “you cannot really have a relationship with them because they just ask you questions… but I wanna know what they are like as a person.” According to her, what impeded the formation of a meaningful relationship was the lack of personal disclosure from the therapist. Morgan conveyed a wish for a more “friendly” and “open” relationship with Dr. P. She desired open conversation and responsiveness to her inquiries instead of feeling like she was being “interrogated.” She reflected that her need to know more about the therapist possibly stemmed from her trust issues: “I have awful trust issues, so to talk to someone I actually have to… sort of know what they are like… personally….” The perceived lack of personal sharing from the therapist made the therapeutic interaction seem impersonal, making it “harder [for her] to talk about [her] feelings with Dr. P.”
Dr. P. also described the relationship with Morgan as challenging, marked by difficulties in engaging her and an awkward dynamic. He noted challenges arising from Morgan’s personal questions and his reluctance to disclose personal information. He talked about the difficulties he experienced in managing Morgan’s ‘intrusive’ questions while trying to establish a therapeutic connection. He explained that he struggled to find a balance between avoiding counterproductive dynamics while being sensitive to ‘her very strong sense of rejection.’ This complex interplay added to the challenges of their therapeutic relationship, which already suffered from a lack of engagement. Despite his continues efforts, Dr. P. acknowledged that their relationship did not get easier, and in his interview he consistently described their interaction as ‘awkward’ and ‘uncomfortable.’
Morgan’s fear of abandonment also emerged as a factor hindering the establishment of a positive and strong relationship with Dr. P., as acknowledged by both parties. In her interview, Morgan explicitly stated, “Dr. P. is gonna fucking abandon me too,” expressing the belief that opening up to him would be pointless. This fear intensified with the awareness of the time-limited treatment, causing disappointment when reminded in the sessions by Dr. P. of the “amount of weeks left.” Additionally, Morgan’s sporadic attendance, frequently addressed by the therapist, became a sensitive issue triggering guilt in her and reducing motivation, ultimately contributing to ruptures in the therapeutic alliance.
Dr. P. also acknowledged the impact of Morgan’s fear of abandonment on their relationship, especially during therapy breaks. Accordingly, he said that he tried to approach these breaks with sensitivity, recognizing their significance. However, he recognized that addressing Morgan’s poor attendance while avoiding making her feel criticized, became a delicate matter. He reflected on a particular session where his response to Morgan’s non-attendance at the previous session, his words might have been perceived as criticism by Morgan, potentially exacerbating the challenges in her therapy creating tension (or ruptures) in their relationship and potentially contributing to her decision not to continue with therapy. Notably, Morgan also acknowledged the difficulty posed by therapy breaks, impacting her motivation to continue the sessions. In fact, her decision to end therapy followed an extended break, as she reflected, ‘basically the break was about 3 weeks… and after that, I did not see the point in going anymore.’
In addressing the challenges encountered in establishing a meaningful therapeutic alliance with Morgan, Dr. P. emphasized the detrimental impact of her poor attendance, unresponsiveness to messages, and difficulty in ‘engaging with the session structure.’ Dr. P., while perceiving that Morgan, to a certain extent, appreciated his efforts to connect, described what he saw as her inability “to use what was offered to her.”
According to Dr. P., external factors also significantly impacted Morgan’s ultimate decision to stop going to therapy, underscoring common complexities in adolescent complex cases. These factors included Morgan’s difficulties at college, and especially, the absence of parental involvement in the therapy. Dr. P. clarified that Morgan’s parents neither attended any offered sessions nor responded to the therapist’s attempts to communicate or gather information about Morgan’s attendance issues. According to Dr. P., this lack of parental engagement played a crucial role in hindering Morgan’s involvement in therapy. These factors collectively created substantial barriers to consistent therapy attendance, and as Dr. P. concluded: “It was unrealistic to expect her to be able to get to therapy.”
4 Discussion
This case study offers an in-depth analysis of the therapeutic relationship and the factors contributing to a decision to drop out of psychoanalytic psychotherapy with Morgan, an adolescent who was experiencing depression. The study highlights the complexities inherent in engaging an adolescent in therapy.
The exploration of the relationship between Morgan and Dr. P. revealed several issues and a considerable number of alliance ruptures, predominantly of the withdrawal type. These ruptures were marked by Morgan’s tendency to disengage from the therapeutic process, manifesting in behaviors such as avoidance, giving minimal responses, and communicating in abstract terms. The prevalence of withdrawal over confrontation ruptures aligns with findings from previous research in youth psychotherapy ( Gersh et al., 2017 ; Schenk et al., 2019 ; O’Keeffe et al., 2019b ; Cirasola et al., 2023 ). This pattern suggests that withdrawal ruptures may be more characteristic of youth populations, who may find it challenging to engage in therapy and are often more inclined toward withdrawal behaviors ( Johnson et al., 2009 ; Constantino et al., 2010 ).
The majority of the withdrawal ruptures in Morgan’s case persisted without resolution, which may have been a significant factor in the difficulties encountered in establishing a robust therapeutic alliance. This unresolved state likely contributed to Morgan’s decision to stop going to therapy. This observation is in line with existing research suggesting that unresolved ruptures can lead to poorer engagement and treatment outcomes ( Eubanks et al., 2018 ). Additionally, these findings resonate with other studies highlighting that adolescents, when dissatisfied with therapy or the therapeutic relationship, tend to withdraw and drop out of treatment, often without explicitly expressing their dissatisfaction to the therapist ( O’Keeffe et al., 2019a , 2020 ).
Our findings align with research in adult therapy, suggesting that both therapists and clients in unsuccessful cases tend to report less positive client-therapist relationships and therapy experiences compared to successful cases ( Gazzillo et al., 2014 ; Hayes et al., 2015 ; Werbart et al., 2019a ). However, our results diverge somewhat from another study conducted with therapists of non-improved young adults. That study showed these therapists described therapy outcomes favorably, noting increased insight and mitigated problems, yet they also reported an incoherent, split picture of the therapeutic process ( Werbart et al., 2019b ). In our case, the therapist demonstrated awareness of difficulties in the therapeutic relationship and process, as well as the lack of patients’ improvement. Since even the most skilled therapists can encounter unsuccessful treatments—patients who do not improve— further research is needed to assess the therapist’s impact on the therapeutic process in both successful and unsuccessful cases to understand what makes a difference. This is particularly relevant in youth therapy, given the challenges in engaging young people and their high dropout rates.
The results of this study also emphasize the importance of trust in the therapeutic process. Epistemic mistrust refers to a deep-seated skepticism or lack of confidence in the knowledge, intentions, or expertise of others, particularly in the context of mental health professionals and therapeutic relationships ( Fonagy and Allison, 2014 ). Morgan’s epistemic mistrust, evident in her overt expressions of distrust toward mental health professionals, presented a significant barrier to her engagement from the onset of therapy. In psychotherapy, individuals with epistemic mistrust may be reluctant to disclose personal information, question the competence of their therapist, or harbor doubts about the effectiveness of the therapeutic process. Addressing and understanding epistemic mistrust is vital in mental health care, as it profoundly affects the dynamics of the therapeutic relationship and can significantly hinder successful treatment outcomes ( Fonagy et al., 2015 ).
Morgan’s struggles with relating to and trusting the therapist shed light on her underlying issues and internal world. For example, her frequent withdrawal ruptures and distrust may suggest difficulties in social interaction, possibly stemming from negative or ambivalent attitudes toward self and others. Hence, ruptures can be viewed as coping mechanisms in response to the tension between two fundamental human motivations: agency and relatedness ( Blatt, 2008 ). Through an examination of these ruptures, therapists can glean insights into patients’ personality traits and internal struggles. Therefore, it might be helpful for therapists to identify and interpret ruptures as glimpses into their clients’ inner worlds. Addressing and resolving these ruptures offers an opportunity to address maladaptive relational patterns and find a balance between self-definition and relatedness.
It is challenging to identify precisely what might have fostered a greater sense of trust in Morgan’s therapeutic relationship and aided in resolving ruptures. However, her explicit remarks about Dr. P’s refusal to answer more personal questions may be significant. Morgan expressed desire to know more about her therapist as a person and the absence of such information from Dr. P. likely contributed to her feeling of being treated impersonally. In the context of this STPP case, the lack of therapist self-disclosure is not surprising, aligning with the historical standpoint in psychoanalysis where self-disclosure is actively discouraged. This skepticism arises from the fundamental principles of psychoanalysis, where therapeutic focus traditionally centers on the patient’s exploration of their unconscious mind and dynamics. Within this framework, therapists traditionally maintain a neutral and objective stance, refraining from personal revelations to prevent potential interference with the patient’s introspective process ( Campos, 2020 ). Contemporary psychoanalytic perspectives challenge the historical stance on therapist self-disclosure, highlighting potential benefits such as promoting authenticity and aiding clients in overcoming impasses and resistance ( Malan and Coughlin Della Selva, 2007 ; Campos, 2020 ). This is especially relevant when working with clients like Morgan, who display epistemic mistrust, resulting in negative expectations of the therapist. Whilst this may be taken up as ‘negative transference,’ there appears to be a risk that it can contribute to treatment dropout, when there is not a fundamental sense that the therapist is ‘on my side.’ Therefore, appropriate self-disclosure and responsiveness to personal questions can foster honesty and authenticity, offering information that proves instrumental in overcoming therapeutic impasses and resistance ( Gorkin, 1987 ).
In contrast to the historical perspective in psychoanalysis, contemporary alliance literature recognizes the therapist’s disclosure of their internal experience in the patient-therapist interaction as a reparative strategy ( Eubanks et al., 2015 , 2019 ). When employed with sensitivity, this strategy is seen as a means to flexibly negotiate distance and closeness based on the patient’s needs, rather than rigidly adhering to a specific treatment manual. Specifically, it is argued that judicious and well-considered self-disclosure can enhance the therapeutic relationship by offering clients insight into the therapist’s humanity, thereby fostering a more genuine connection ( Muran and Eubanks, 2020 ). This approach is also endorsed in mentalization-based therapies, where therapists are encouraged to engage in careful self-disclosure as a vital means for both client and therapist to understand each other by sharing their respective thinking and emotional processes in listening and reacting to each other ( Bateman and Fonagy, 2004 ). Although further research is required on this subject, it appears that, especially for clients with trust issues and signs of withdrawal ruptures (i.e., movement away from the therapist or therapy), both of which are common among adolescents, therapists who disclose personal information may be perceived as initiating a “movement toward” the clients. This could enhance the therapist’s authenticity and approachability, possibly leading to increased trust and greater engagement in therapy.
Another factor that likely influenced the difficulty in establishing trust with Morgan was the brief and time-limited nature of the treatment. The predetermined number of sessions in short-term therapy might have unintentionally intensified Morgan’s existing trust issues. Her fear of abandonment, heightened by the knowledge that the treatment had a set endpoint, mirrors a common challenge in time-limited psychotherapy ( Norcross and Wampold, 2018 ). The constraint of a fixed number of sessions can present particular challenges for clients with histories of abandonment or difficulties in establishing trust and more research is needed on the topic.
In addition to the inherent complexities of the therapeutic relationship, this case study underscores the crucial role of external factors in shaping engagement with psychotherapy. Morgan’s numerous challenges, coupled with the absence of parental support for treatment—both indirect (such as endorsing therapy) and direct involvement—seemed to create substantial additional obstacles in the therapy process, especially when Morgan herself was struggling to engage. This aligns with an expanding body of research that underscores the importance of establishing a parental alliance when working with adolescents, particularly in complex cases ( Novick and Novick, 2013 ; Forsberg et al., 2014 ; Feder and Diamond, 2016 ; Malberg, 2021 ). This approach can be instrumental in navigating external challenges and highlights the criticality of not only addressing internal psychological factors, especially issues in the therapeutic relationship, but also engaging with and leveraging external support systems to provide a comprehensive and effective therapeutic approach for adolescents struggling with complex mental health needs.
4.1 Strengths and limitations
The study exhibits several notable strengths, primarily evident in its comprehensive mixed-methods design from a critical realist epistemological perspective. By employing multiple methods, including questionnaires, interviews, and audio recordings of therapy sessions, the study was able to gather rich and diverse data from multiple perspectives, enhancing the depth of understanding. Another strength lies in the engagement of multiple assessors for rating alliance rupture-resolution events and conducting post-therapy interviews. This multifaceted approach, coupled with the adoption of blind raters for the 3RS, enhances the methodological rigor of the investigation.
However, there are also certain limitations in the study. The focus on a singular case warrants caution regarding the generalizability of findings. While such an approach offers in-depth insight into the intricacies of a particular therapeutic dyad, it restricts the ability to generalize findings to broader populations or contexts. Each therapeutic relationship is unique, influenced by a multitude of factors such as individual personalities, therapeutic techniques, and external circumstances. Therefore, extrapolating conclusions from a solitary case may overlook the variability present in different therapeutic settings. Additionally, the subjective nature of qualitative analysis implies that interpretations may vary between researchers. However, to mitigate biases, this study employed multiple independent raters and utilized reflective practices and collaborative discussions across various raters. Future research should aim to replicate these findings across multiple cases to enhance their applicability.
4.2 Conclusion
In conclusion, this single-case study provides valuable insights into the nuanced dynamics contributing to dropout from short-term psychoanalytic therapy among depressed adolescents. It elucidates the intricate interaction between therapeutic processes and a variety of external and internal factors. It highlights the role of the therapeutic relationship, especially alliance ruptures, highlighting the significance of identifying and addressing ruptures while mitigating epistemic mistrust to enhance the likelihood of therapeutic engagement. Establishing an alliance and repairing ruptures necessitates a flexible negotiation of distance and closeness tailored to the patient’s needs, and some aspects of a psychoanalytic approach may need to be adapted accordingly. While the study’s results may bear the unique characteristics of this specific case, the lessons derived from it can be instructive for therapists working with other cases. Notably, strategic self-disclosure emerges as a promising avenue for fostering connection with adolescents exhibiting epistemic mistrust and its associated challenges. These insights advocate for a reconsideration of clinical methodologies and therapist training, tailored to better equip practitioners to navigate ruptures with adolescents, especially those experiencing poor engagement and epistemic mistrust.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data comprises audio recordings of sessions, which cannot be shared due to ethical and confidentiality considerations. Further inquiries can be directed to the corresponding author.
Ethics statement
The research protocol was approved by the Cambridgeshire 2 Research Ethics Committee (REC Reference: 09/HO308/137). Informed written consent was obtained from all participants, including parental consent. To maintain confidentiality, all identifying personal information has been anonymised. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DS: Formal analysis, Writing – review & editing. PF: Supervision, Writing – review & editing. NM: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank the young person, their parents and the therapist who took part in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1381901/full#supplementary-material
Acheson, R., Verdenhalven, N., Avdi, E., and Midgley, N. (2020). Exploring silence in short-term psychoanalytic psychotherapy with adolescents with depression .
Google Scholar
Angold, A., Costello, E. J., Pickles, A., Winder, F., and Silver, D. (1987). The development of a questionnaire for use in epidemiological studies of depression in children and adolescents . London: Medical Research Council Child Psychiatry Unit.
Bateman, A., and Fonagy, P. (2004). Psychotherapy for borderline personality disorder: mentalization based treatment .
Binder, P.-E., Holgersen, H., and Høstmark Nielsen, G. (2008). Re-establishing contact: a qualitative exploration of how therapists work with alliance ruptures in adolescent psychotherapy. Couns. Psychother. Res. 8, 239–245. doi: 10.1080/14733140802363167
Crossref Full Text | Google Scholar
Blatt, S. J. (2008). Polarities of experience: relatedness and self-definition in personality development, psychopathology, and the therapeutic process . American Psychological Association.
Bordin, E. S. (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychother. Theory Res. Pract. 16, 252–260. doi: 10.1037/h0085885
Campos, P. (2020). Self-disclosure in psychotherapy and psychoanalysis. Psychol. Psychol. Res. Int. J. 5:000257. doi: 10.23880/pprij-160002574
Cirasola, A., Martin, P., Fonagy, P., Eubanks, C., Muran, C. J., and Midgley, N. (2022). Alliance ruptures and resolutions in short-term psychoanalytic psychotherapy for adolescent depression: an empirical case study. Psychother. Res. 32, 951–968. doi: 10.1080/10503307.2022.2061314
PubMed Abstract | Crossref Full Text | Google Scholar
Cirasola, A., and Midgley, N. (2023). The alliance with young people: where have we been, where are we going? Psychotherapy 60, 110–118. doi: 10.1037/pst0000461
Cirasola, A., Midgley, N., Fonagy, P., and Martin, P.IMPACT Consortium (2021). The therapeutic alliance in psychotherapy for adolescent depression: differences between treatment types and change over time. J. Psychother. Integr. 32, 326–341. doi: 10.1037/int0000264
Cirasola, A., Midgley, N., Muran, J. C., Eubanks, C. F., Hunter, E. B., and Fonagy, P. (2023). Repairing alliance ruptures in psychodynamic psychotherapy with young people: the development of a rational–empirical model to support youth therapists. Psychotherapy . doi: 10.1037/pst0000514, [Online ahead of print]
Constantino, M. J., Castonguay, L. G., Zack, S. E., and DeGeorge, J. (2010). Engagement in psychotherapy: Factors contributing to the facilitation, demise, and restoration of the therapeutic alliance .
Cooper, A. A., Kline, A. C., Baier, A. L., and Feeny, N. C. (2018). Rethinking research on prediction and prevention of psychotherapy dropout: a mechanism-oriented approach. Behav. Modif. 47, 1195–1218.
Creamer, E. G., and Reeping, D. (2020). Advancing mixed methods in psychological research. Methods Psychol. 3:100035. doi: 10.1016/j.metip.2020.100035
Cregeen, S., Hughes, C., Midgley, N., Rhode, M., and Rustin, M. (2017). Short-term psychoanalytic psychotherapy for adolescents with depression: a treatment manual . London: Karnac Books.
Daly, A. M., Llewelyn, S., McDougall, E., and Chanen, A. M. (2010). Rupture resolution in cognitive analytic therapy for adolescents with borderline personality disorder. Psychol. Psychother. Theory Res. Pract. 83, 273–288. doi: 10.1348/147608309X481036
Davies, S. E., Neufeld, S. A. S., van Sprang, E., Schweren, L., Keivit, R., Fonagy, P., et al. (2019). Trajectories of depression symptom change during and following treatment in adolescents with unipolar major depression. J. Child Psychol. Psychiatry Allied Discip. 61, 565–574. doi: 10.1111/jcpp.13145
De Haan, A. M., Boon, A. E., De Jong, J. T. V. M., Hoeve, M., and Vermeiren, R. R. J. M. (2013). A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin. Psychol. Rev. 33, 698–711. doi: 10.1016/j.cpr.2013.04.005
DiGiuseppe, R., Linscott, J., and Jilton, R. (1996). Developing the therapeutic alliance in child-adolescent psychotherapy. Appl. Prev. Psychol. 5, 85–100. doi: 10.1016/S0962-1849(96)80002-3
Edgley, A., Stickley, T., Timmons, S., and Meal, A. (2016). Critical realist review: exploring the real, beyond the empirical. J. Furth. High. Educ. 40, 316–330. doi: 10.1080/0309877X.2014.953458
Eubanks, C. F., Lubitz, J., Muran, C. J., and Safran, J. D. (2019). Rupture resolution rating system (3RS): development and validation. Psychother. Res. 29, 306–319. doi: 10.1080/10503307.2018.1552034
Eubanks, C. F., Muran, C. J., and Safran, J. D. (2015). Rupture resolution rating system (3RS): manual. Res. Gate . doi: 10.13140/2.1.1666.8488
Eubanks, C. F., Muran, C. J., and Safran, J. D. (2018). Alliance rupture repair: a meta-analysis. Psychotherapy 55, 508–519. doi: 10.1037/pst0000185.supp
Eubanks, C. F., Muran, JC, and Safran, J. (2022). Rupture resolution rating system (3RS): manual version 2022 . Unpublished manuscript. Mount Sinai-Beth Israel Medical Center: New York.
Feder, M. M., and Diamond, G. M. (2016). Parent-therapist alliance and parent attachment-promoting behaviour in attachment-based family therapy for suicidal and depressed adolescents. J. Fam. Ther. 38, 82–101. doi: 10.1111/1467-6427.12078
Fonagy, P., and Allison, E. (2014). The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy 51, 372–380. doi: 10.1037/a0036505
Fonagy, P., Luyten, P., and Allison, E. (2015). Epistemic petrification and the restoration of epistemic trust: a new conceptualization of borderline personality disorder and its psychosocial treatment. J. Personal. Disord. 29, 575–609. doi: 10.1521/pedi.2015.29.5.575
Forsberg, S., Lotempio, E., Bryson, S., Fitzpatrick, K. K., Le Grange, D., and Lock, J. (2014). Parent-therapist alliance in family-based treatment for adolescents with anorexia nervosa. Eur. Eat. Disord. Rev. 22, 53–58. doi: 10.1002/erv.2242
Gazzillo, F., Waldron, S., Genova, F., Angeloni, F., Ristucci, C., and Lingiardi, V. (2014). An empirical investigation of analytic process: contrasting a good and poor outcome case. Psychotherapy 51, 270–282. doi: 10.1037/a0035243
Gersh, E., Hulbert, C. A., McKechnie, B., Ramadan, R., Worotniuk, T., and Chanen, A. M. (2017). Alliance rupture and repair processes and therapeutic change in youth with borderline personality disorder. Psychol. Psychother. Theory Res. Pract. 90, 84–104. doi: 10.1111/papt.12097
Goodyer, I. M., Reynolds, S., Barrett, B., Byford, S., Dubicka, B., Hill, J., et al. (2017). Cognitive-behavioural therapy and short-term psychoanalytic psychotherapy versus brief psychosocial intervention in adolescents with unipolar major depression (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled trial. Health Technol. Assess. 21, 1–94. doi: 10.3310/hta21120
Gorkin, M. (1987). The uses of countertransference . Jason Aronson.
Gulliver, A., Kathleen, M. G., and Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 10:113. doi: 10.1186/1471-244X-10-113
Halfon, S., Ozsoy, D., and Cavdar, A. (2019). Therapeutic alliance trajectories and associations with outcome in psychodynamic child psychotherapy. J. Consult. Clin. Psychol. 87, 603–616. doi: 10.1037/ccp0000415
Hayes, J. A., Nelson, D. L. B., and Fauth, J. (2015). Countertransference in successful and unsuccessful cases of psychotherapy. Psychotherapy 52, 127–133. doi: 10.1037/a0038827
Horvath, A. O., and Greenberg, L. S. (1989). Development and validation of the working Alliance inventory. J. Couns. Psychol. 36, 223–233. doi: 10.1037/0022-0167.36.2.223
Johnson, E., Mellor, D., and Brann, P. (2009). Factors associated with dropout and diagnosis in child and adolescent mental health services. Australian New Zealand J. Psychiatry 43, 431–437. doi: 10.1080/00048670902817687
Kent, L., Vostanis, P., and Feehan, C. (1997). Detection of major and minor depression in children and adolescents: evaluation of the mood and feelings questionnaire. J. Child Psychol. Psychiatry Allied Discip. 38, 565–573. doi: 10.1111/j.1469-7610.1997.tb01543.x
Leibovich, L., Front, O., McCarthy, K. S., and Zilcha-Mano, S. (2019). How do supportive techniques bring about therapeutic change: the role of therapeutic alliance as a potential mediator. Psychotherapy 57, 151–159. doi: 10.1037/pst0000253
Malan, D., and Coughlin Della Selva, P. (2007). Lives transformed: a revolutionary method of dynamic psychotherapy . Rev. Ed. London: Karnac Books.
Malberg, N. T. (2021). Working with autistic children and their families from a mentalization based therapy for children (MBT-C) approach. Psychoanal. Perspect. 18, 22–42. doi: 10.1080/1551806X.2021.1845033
McEvoy, P., and Richards, D. (2006). A critical realist rationale for using a combination of quantitative and qualitative methods. J. Res. Nurs. 11, 66–78. doi: 10.1177/1744987106060192
McLeod, J. (2013). Case study research in counselling and psychotherapy Sage Publications.
Midgley, N., Ansaldo, F., Parkinson, S., Holmes, J., Stapley, E., and Target, M. (2011). Experience of therapy interview (young person, parent and therapist versions) . Unpublished Manuscript. Anna Freud Centre: London.
Midgley, N., Ansaldo, F., and Target, M. (2014). The meaningful assessment of therapy outcomes: incorporating a qualitative study into a randomized controlled trial evaluating the treatment of adolescent depression. Psychotherapy 51, 128–137. doi: 10.1037/a0034179
Muran, C. J., and Eubanks, C. F. (2020). Therapist performance under pressure: negotiating emotion, difference, and rupture American Psychological Association.
Norcross, J. C., and Wampold, B. E. (2018). A new therapy for each patient: evidence-based relationships and responsiveness. J. Clin. Psychol. 74, 1889–1906. doi: 10.1002/jclp.22678
Novick, K. K., and Novick, J. (2013). Concurrent work with parents of adolescent patients. Psychoanal. Study Child 67, 103–136. doi: 10.1080/00797308.2014.11785491
O’Keeffe, S., Martin, P., Goodyer, I. M., Kelvin, R., Dubicka, B., Goodyer, I. M., et al. (2019a). Prognostic implications for adolescents with depression who drop out of psychological treatment during a randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 58, 983–992. doi: 10.1016/j.jaac.2018.11.019
O’Keeffe, S., Martin, P., Goodyer, I. M., Wilkinson, P., Consortium, I., and Midgley, N. (2018). Predicting dropout in adolescents receiving therapy for depression. Psychother. Res. 28, 708–721. doi: 10.1080/10503307.2017.1393576
O’Keeffe, S., Martin, P., and Midgley, N. (2020). When adolescents stop psychological therapy: rupture- repair in the therapeutic alliance and association with therapy ending. Psychotherapy 57, 471–490. doi: 10.1037/pst0000279
O’Keeffe, S., Martin, P., Target, M., and Midgley, N. (2019b). “I just stopped going”: a mixed methods investigation into types of therapy dropout in adolescents with depression. Front. Psychol. 10, 1–14. doi: 10.3389/fpsyg.2019.00075
Parkinson, S., Eatough, V., Holmes, J., Stapley, E., and Midgley, N. (2016). Framework analysis: a worked example of a study exploring young people’s experiences of depression. Qual. Res. Psychol. 13, 109–129. doi: 10.1080/14780887.2015.1119228
Safran, J. D., and Muran, C. J. (2000). Negotiating the therapeutic alliance: a relational treatment guide . Guilford Press.
Schenk, N., Zimmermann, R., Fürer, L., Krause, M., Weise, S., Kaess, M., et al. (2019). Trajectories of alliance ruptures in the psychotherapy of adolescents with borderline personality pathology: timing, typology and significance. Res. Psychother. Psychopathol. Process Outcome 22, 199–211. doi: 10.4081/ripppo.2019.348
Tracey, T. J., and Kokotovic, A. M. (1989). Factor structure of the working alliance inventory. Psychol. Assess. 1, 207–210. doi: 10.1037/1040-3590.1.3.207
Werbart, A., Annevall, A., and Hillblom, J. (2019a). Successful and less successful psychotherapies compared: three therapists and their six contrasting cases. Front. Psychol. 10:816. doi: 10.3389/fpsyg.2019.00816
Werbart, A., von Below, C., Engqvist, K., and Lind, S. (2019b). “It was like having half of the patient in therapy”: therapists of nonimproved patients looking back on their work. Psychother. Res. 29, 894–907. doi: 10.1080/10503307.2018.1453621
Wood, A., Kroll, L., Moore, A., and Harrington, R. (1995). Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: a research note. J. Child Psychol. Psychiatry 36, 327–334. doi: 10.1111/j.1469-7610.1995.tb01828.x
Keywords: unsuccessful treatments, dropout, youth psychotherapy, alliance, Short-Term Psychoanalytic Psychotherapy, single case, adolescent depression
Citation: Cirasola A, Szegedi D, Fonagy P and Midgley N (2024) “You can’t really have a relationship with them because they just ask you questions”: understanding adolescent dropout – an empirical single case study. Front. Psychol . 15:1381901. doi: 10.3389/fpsyg.2024.1381901
Received: 04 February 2024; Accepted: 23 February 2024; Published: 12 March 2024.
Reviewed by:
Copyright © 2024 Cirasola, Szegedi, Fonagy and Midgley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nick Midgley, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

Sport and Competition
Functional imagery training for athletic consistency, this cognitive framework has helped athletes go from good to world-class..
Posted March 20, 2024 | Reviewed by Ray Parker
- Functional imagery training combines motivational interviewing and imagery for peak performance.
- Using a minimum of three senses enhances athletic execution.
- Consistent debriefing refines performance strategies.
In the thrilling world of sports, where every sprint, jump, and victory dance is a heartbeat in the rhythm of competition , the pursuit of greatness demands more than just physical prowess. It demands an unyielding mental fortitude that transforms athletes, seemingly, into legends. Picture Simone Biles gracefully dominating the gymnastics floor while mentally choreographing the symphony of her routine, predicting every twist and turn before she defies gravity.
Now, imagine LeBron James not just slam-dunking with sheer athleticism but mentally rehearsing the perfect shot in the heat of the game. This isn't mere speculation; it's the power of imagery, and we're about to explore a groundbreaking approach: functional imagery training (FIT), a psychological game-changer that's rewriting the sport psychology and performance enhancement playbooks for athletes (doctors, even business executives) worldwide.
What Is Functional Imagery Training?
Discussed on The Sport Psych Show podcast, FIT isn't your run-of-the-mill mental training for athletes; it's a dynamic fusion of motivational interviewing ( empathic communication) and imagery—a concoction of mental gymnastics that metamorphosizes dreams into tangible actions and victories. This isn't reserved for the elite; it's the vital ingredient for anyone aiming to defy their limits.
The University of Plymouth's researchers have developed the approach out of years of research. In one study, the research team turned self-proclaimed non-athletes into ultramarathon runners. In another, they enhanced soccer players' performance, and in another, they worked with the military to improve soldier success during arduous training. They’ve even been helping individuals with weight loss and exercise adherence .
The Components of FIT: Motivational Interviewing and Imagery Training
Now, let's examine the heart of FIT. Imagine this: You're seated with a psychologist or mental skills coach, not just talking about your athletic dreams but embarking on an empathic process of self-discovery. It's like plotting your athletic manifesto with a mental pen, engaging in deep conversation with someone genuinely curious about you and what fuels your fire. This is where imagery comes in, a tool that turns this conversation into a blockbuster movie in your mind, which is then converted into a tangible action plan.
It's not just about seeing; it's about feeling the adrenaline, hearing the roar of the crowd, and experiencing the triumphs and setbacks in a multi-sensory format—visual, auditory, taste, smell, touch, motion, emotion —all working together to plan for achievement. It's your mental GPS, navigating the twists and turns of your athletic journey in the most immersive way imaginable. Imagery is used in different ways. Initially, we employ it to delve into overarching goals , then we refine the plan, and ultimately, we zoom in on individual immediate tasks. These tasks might encompass seemingly minor details, such as a technical thought about footwork, which are meticulously played out in vivid detail to immerse ourselves in the experiential process.
Case Study: Three-Point Routine
Working with professional basketballers, the seamless application of imagery for technical (and tactical developments) yields nearly instantaneous results. To maintain a steadfast focus and consistent performance, we distill the power of imagery into a three-phase performance routine. Now, let's take FIT from the academic research papers and put it into action with a real-life example, a basketball player called Zak’s three-point routine.
Phase 1: Locating the Cue
Zak's ritual begins with a gentle bounce of the ball before he takes his shot, a seemingly mundane action that acts as his cue, marking the start of his mental performance routine. This cue, intentional and purposeful, serves to focus attention on the forthcoming task and kickstart the process of mental planning. Studies (e.g., Mendelsohn et al., 2014 ) have demonstrated that such cues not only prompt planning but also stimulate vivid imagery, enhancing overall performance.
Phase 2: Activating Imagery
During this phase, Zak engages in the activation of multisensory imagery. He meticulously envisions each detail: a fluid and relaxed movement, a deep breath as he prepares, the sensation of bending his knees, arm extension and releasing the ball, its graceful flight through the air, and the satisfying swooshing sound as it elegantly lands inside the net. While leveraging all seven senses could potentially enhance performance, research has identified a trio of essential components: movement, visual, and emotional imagery. This combination has been shown ( Cregg et al., 2011 ; Rhodes et al., 2020 ) to boost performance outcomes consistently.

Phase 3: Perform and Debrief
Now, it's showtime. Zak begins his routine: a bounce of the ball, a focused breath, and a subtle bend of his knees, all in alignment with his imagery. At this stage, execution is about unwavering commitment to the plan. The culmination of his preparation unfolds seamlessly as he executes the shot exactly as envisioned. Whether Zak scores or misses, he conducts a quick debrief of the outcome—what have I learned?—returning to phase one to refine his approach. Thus, the cycle perpetuates, each iteration refining his performance further.
Applying FIT in Your Sport: Consistency Is Key
Zak's three-point routine is a testament to the power of FIT, and the beauty is that you can adopt a similar performance routine in any sport. It's about consistency—refining a series of thoughts and behaviors that develop a mental framework for thinking, especially when under pressure.
Navigating the application of FIT as you step into the spotlight of your sport requires a touch of refinement. To jumpstart your application, you can take on an imagery test. A swift exploration to uncover the secrets your mind harbors for optimal performance. Following this, carve out dedicated time to fully immerse yourself in multi-sensory imagery, seamlessly linking it with your pre-competition routine. While aiming for all seven senses is ideal, starting with three or four will suffice. Remember, this isn't merely a training technique; it's how you write the script of how you think and perform, refining your thoughts into your most reliable teammate on the field.
https://www.imagerycoaching.com/

Jonathan Rhodes, Ph.D. , is a chartered British psychologist, author, performance consultant, and researcher who helped develop Functional Imagery Training.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Is the use of secukinumab after anti-TNF therapy greater than expected for the risk of developing inflammatory bowel disease?
Affiliations.
- 1 Department of Internal Medicine, Division of Rheumatology, Dr. Ersin Arslan Training and Research Hospital, Şehitkamil, Gaziantep, Turkey. Electronic address: [email protected].
- 2 Department of Internal Medicine, Division of Rheumatology, Fırat University Faculty of Medicine, Elazığ, Turkey.
- 3 Department of Rheumatology, Gaziantep Sanko Hospital, Şehitkamil, Gaziantep, Turkey.
- PMID: 38494303
- DOI: 10.1016/j.reumae.2023.11.002
Objective: In this study, our objective was to present real-life data on the incidence of inflammatory bowel disease (IBD) among patients receiving secukinumab treatment.
Methods: The study consisted of 209 patients who had prior exposure to anti-tumor necrosis factor (TNF) or were biologically naive. Patients with a pre-existing history of IBD were excluded from the study.
Results: Of the 209 patients in the study, 176 (84.3%) had ankylosing spondylitis, while 33 (15.7%) had psoriatic arthritis. 112 (53.6%) patients had prior exposure to at least one anti-TNF treatment before initiating secukinumab. IBD developed in 10 (4.8%) of the 209 patients. The incidence of IBD among patients who initiated secukinumab as their first biologic agent was 1%. For patients who had previously received any anti-TNF treatment and subsequently transitioned to secukinumab, the incidence of IBD was 8% (p=0.018, odds ratio (OR): 8.38, 95% CI: 1.04-67.45). A mean of 3.67 months (±4.3) after anti-TNF use, whereas IBD symptoms developed in the biologically naive patient after 15 months.
Conclusion: Our study observed IBD incidence in 4.8% of patients using secukinumab. Patients who initiated secukinumab after previous anti-TNF treatment exhibited a significantly higher rate and risk of developing IBD. The onset of IBD occurred earlier in these patients (mean 3.67 months), whereas a single case of IBD showed a longer duration (15 months). Further studies with larger patient numbers are warranted to provide a more comprehensive understanding of our findings.
Keywords: Ankylosing spondylitis; Artritis psoriásica; Datos del mundo real; Enfermedad inflamatoria intestinal; Espondilitis anquilosante; Inflammatory bowel disease; Psoriatic arthritis; Real-world data; Secukinumab.
Copyright © 2023 Elsevier España, S.L.U. and Sociedad Española de Reumatología y Colegio Mexicano de Reumatología. All rights reserved.
- Antibodies, Monoclonal, Humanized / adverse effects
- Inflammatory Bowel Diseases* / drug therapy
- Spondylitis, Ankylosing* / complications
- Spondylitis, Ankylosing* / drug therapy
- Tumor Necrosis Factor Inhibitors / adverse effects
- Tumor Necrosis Factor-alpha
- secukinumab
- Tumor Necrosis Factor Inhibitors
- Antibodies, Monoclonal, Humanized

IMAGES
VIDEO
COMMENTS
Her more recent episodes related to her parents' marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT). Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response.
Clinical Case Studies (CCS), peer-reviewed & published bi-monthly electronic only, is the only journal devoted entirely to innovative psychotherapy case studies & presents cases involving individual, couples, & family therapy.The easy-to-follow case presentation format allows you to learn how interesting & challenging cases were assessed & conceptualized, & how treatment followed such ...
Pragmatic Case Studies in Psychotherapy. PCSP is a peer reviewed, open-access journal and database. It provides innovative, quantitative and qualitative knowledge about psychotherapy process and outcome. PCSP is published by the National Register of Health Service Psychologists. January, 2024 -- see our newest case, "The Commitment of a ...
Narrative case studies tell the story of therapy from the point of view of the client or therapist. Murase's (2015) case of "Mr. R" provides a powerful example of the potential of this form of case inquiry, as a means of enabling reflection and deeper understanding around the practice and process of therapy. The distinctive contribution of the case of Mr. R is discussed in relation to the ...
Case-based knowledge forms an essential element of the evidence base for counselling and psychotherapy practice. This book provides the reader with a unique introduction to the conceptual and practical tools required to conduct high quality case study research that is grounded in their own therapy practice or training.
Emphasis is on the unfolding of the client-therapist interaction and the development of the therapeutic relationship in their case study, rather than on discrete relationship variables (e.g., empathy, alliance, self-disclosure) or on schools of psychotherapy. In examining the process of change in the case studies, the authors of each chapter ...
Pragmatic Case Studies in Psychotherapy, 7(4), 529-557. An example of a theory-building case study focused on the development of the assimilation model of change Kramer, U. (2009). Between manualized treatments and principle-guided psychotherapy: illustration in the case of Caroline. Pragmatic Case Studies in Psychotherapy, 5(2), 45-51
Over recent years, an increasing number of systematic case-based investigations of the process and outcomes of counseling and psychotherapy has been published. Nevertheless, case study knowledge continues to have a limited impact on therapy training, practice and policy. It is argued that improvement in the status of case study evidence requires further attention to ways of enhancing the rigor ...
The latter components were based on case study guidelines featured in the journal of Pragmatic Case Studies in Psychotherapy as well as components commonly used by published systematic case studies across a variety of other psychotherapy journals (e.g. Psychotherapy Research, Research In Psychotherapy: Psychopathology Process And Outcome, etc ...
Evidence-Based Case Study. Parallel in purpose to the Practice Review articles, I would like to issue an open invitation for authors to submit an Evidence-Based Case Study for possible publication in Psychotherapy. I believe developing such a series of Evidence-Based Case Studies will be extremely useful in several ways.
The therapy described below refers to an 18-month period of weekly individual psychotherapy utilizing MERIT. MERIT is an integrative psychotherapy with eight core elements incorporated into each session. ... Although case studies provide in-depth examinations of an individual's experience, they have limitations. The findings from this case ...
A case study in psychotherapy serves to empirically investigate the processes involved in psychotherapy. The questions can be both hypothesis-testing and hypothesis-generating. The "object" of the investigation ("case") can include - analogously to CS in sociology - questions concerning processes, efficacy, as well as queries ...
An important step toward the development of a framework is Kaluzeviciute's Case Study Evaluation-tool (CaSE), the first tool that offers a framework and a checklist to evaluate the evidential value of case studies in the field of psychotherapy. This tool needs to be completed, disseminated, and implemented more broadly.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
Four Case Studies. One of the best ways to understand what psychotherapy involves is to read accounts of what happened to people when they went: the problems they came in with, the discussions that were had, and how things changed as a result. What follow are four representative case studies of the therapeutic process:
Challenging Emotions in Psychotherapy: Case Studies. It is impossible to take a cookbook approach to understanding transference and countertransference. Each psychotherapist-client dyad is af ected by the unique personal histories of both participants. Nonetheless, this document will provide a few examples of common transference and ...
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews). The case study research method originated in clinical medicine (the case history, i.e., the patient's personal history). In psychology, case studies are ...
The book is organized into nine chapters in two parts that together pro-vide a foundation in evidence-based, integrative psychotherapy case for-mulation, including specific formulation steps and criteria for evaluating a formulation. Part I sets the context for the description of the general case formulation model and Part II describes the model.
The purpose of this study was to gain preliminary evidence for the use of meta-emotion therapy (MET) in the treatment of comorbid complex posttraumatic stress disorder (PTSD) and binge eating disorder (BED) using a case study design. Our study revealed that MET led to noteworthy reductions in symptoms associated with both PTSD and BED, and the participant reported good tolerance of the treatment.
Finally, this case study's methodology offers constructive questions that clinical practitioners can apply to specific psychotherapy approaches as well as theological concepts. ... integrating the client's concerns with specific narrative therapy interventions or practices and the theological/spiritual concepts of immanence-transcendence ...
Systematic case studies are often placed at the low end of evidence-based practice (EBP) due to lack of critical appraisal. This paper seeks to attend to this research gap by introducing a novel Case Study Evaluation-tool (CaSE). First, issues around knowledge generation and validity are assessed in both EBP and practice-based evidence (PBE) paradigms. Although systematic case studies are more ...
The Rutgers University Libraries no longer publish the journal of Pragmatic Case Studies In Psychotherapy. Future issues of this journal will be published by the National Register of Health Service Psychologists. For back issues and future issues of this journal, please visit
Abstract. This case study describes 1 year of the psychoanalytic psychotherapy using clinical data, a standardized instrument of the psychotherapeutic process (Psychotherapy process Q-Set, PQS), and functional neuroimaging (fMRI). A female dysthymic patient with narcissistic traits was assessed at monthly intervals (12 sessions).
Therapists further often believed TFT to be unsuitable for patients in case of comorbidity or more complex trauma histories . ... while the rest were delivered as individual therapy. Eight studies used qualitative interviews and one study used a questionnaire with free-text items. All samples consisted of adults, with one study focusing on ...
These factors collectively created substantial barriers to consistent therapy attendance, and as Dr. P. concluded: "It was unrealistic to expect her to be able to get to therapy." 4 Discussion. This case study offers an in-depth analysis of the therapeutic relationship and the factors contributing to a decision to drop out of psychoanalytic ...
To our knowledge, this is the first case report of boxing therapy in the rehabilitation of visual field loss and impaired visuospatial attention. Boxing movements require motor activation and advanced coordination of the upper body, as well as visuomotor coordination when patients are instructed to hit visual targets. ... In a single case study ...
Case Study: Three-Point Routine Working with professional basketballers, the seamless application of imagery for technical (and tactical developments) yields nearly instantaneous results.
Expert reasoning in psychotherapy case formulation. Psychotherapy Research, 21, 385-399. Eells, T. D. (2013). The case formulation approach to psychotherapy research revisited. Pragmatic Case Studies in Psychotherapy, 9, 426-447. APA Videos. Case Formulation in Emotion-Focused Therapy: Addressing Unfinished Business Rhonda N. Goldman
Caregiver empowerment may help support families to uphold their child's rights and access suitable education and support. This study aimed to examine the perceptions on empowerment of caregivers of autistic children in Argentina. This was a phenomenological, qualitative study. We conducted 32 semi-structured individual interviews remotely.
Objective: In this study, our objective was to present real-life data on the incidence of inflammatory bowel disease (IBD) among patients receiving secukinumab treatment. Methods: The study consisted of 209 patients who had prior exposure to anti-tumor necrosis factor (TNF) or were biologically naive. Patients with a pre-existing history of IBD were excluded from the study.