
- Previous Article
- Next Article

46-LB: A New Approach to Understand Diabetes Burnout—Examining Potential Burnout Profiles?
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Cite Icon Cite
- Get Permissions
SAMEREH ABDOLI , KATHERINE L. MILLER , DANIELLE M. HESSLER; 46-LB: A New Approach to Understand Diabetes Burnout—Examining Potential Burnout Profiles?. Diabetes 1 June 2022; 71 (Supplement_1): 46–LB. https://doi.org/10.2337/db22-46-LB
Download citation file:
- Ris (Zotero)
- Reference Manager
Aim: The study aimed to identify latent profiles of diabetes burnout and examine if there are significant differences in psychosocial well-being, diabetes outcomes, and demographic characteristics between individuals with varying burnout profiles.
Methods: A national sample of adults with T1D (n=1099) completed an online cross-sectional survey across the U.S. We used Diabetes Burnout Scale (DBS) to collect data on diabetes burnout (i.e., exhaustion, detachment, lack of control) . We also measured diabetes distress, depressive symptoms, glycemic control, and demographic characteristics. Data were analyzed using latent class analysis (LCA) , and the resulting profiles were validated using Chi-square and Kruskal Wallis test.
Results: Results showed a seven latent burnout profiles: (a) fully burned out (n=275, 25.02%) ; (b) exhausted (n=148, 13.47%) ; (c) Dissociated (n= 132, 12.56%) ; (d) overextended (n= 135, 12.28%) ; (e) disengaged (n=90, 8.18%) ; (f) loss of control (n=48, 4.37%) . Among participants, 275 (25.02%) were categorized as not having any symptoms of burnout. Examination of the profiles suggested a non-linear relationship between exhaustion, detachment, and lack of control. The results revealed that there were significant differences in diabetes distress, depressive symptoms, and demographic characteristics between individuals with different burnout profiles. Among profiles, fully burned-out profile was a stronger predictor for glycemic control.
Conclusion: This is the first study examining statistically different profiles of diabetes burnout in adults with T1D. The identification of burnout profiles and the developmental model can inform targeted interventions to address burnout in each specific profile and prevent burnout to result devastating consequences.
S. Abdoli: None. K. L. Miller: None. D. M. Hessler: None.
Email alerts
- Online ISSN 1939-327X
- Print ISSN 0012-1797
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Help & FAQ
The Value of Measuring Diabetes Burnout
- Department of Medicine
- Division of General Internal Medicine
- Department of Public Health Sciences
- Department of Humanities
Research output : Contribution to journal › Review article › peer-review
Purpose of Review: Diabetes represents a chronic illness with significant physical and psychological morbidities. This review aims to summarize current conceptualizations of diabetes burnout in individuals with diabetes and describe its associated adverse outcomes in this population while proposing possible mechanisms of action and targets of intervention. Recent Findings: “Diabetes burnout” may result in adverse long-term outcomes including poor treatment compliance, diabetes complications, and depression. Diabetes burnout may impact not only individuals, but also providers, and caregivers and family members of affected individuals. Diabetes burnout may results from sustained cognitive stresses of chronic treatment adherence, assessment of realistic treatment goals, and treatment challenges. Summary: Early screening and interdisciplinary approaches for patient-centered diabetes care are critical for sustained diabetes social support. Future work exploring these approaches may identify early support and targeted interventions for the long-term support of individuals with diabetes.
All Science Journal Classification (ASJC) codes
- Internal Medicine
- Endocrinology, Diabetes and Metabolism
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.1007/s11892-021-01392-6
Other files and links
- Link to publication in Scopus
- Link to the citations in Scopus
Fingerprint
- Psychological Burnout Medicine & Life Sciences 100%
- Patient-Centered Care Medicine & Life Sciences 25%
- Treatment Adherence and Compliance Medicine & Life Sciences 24%
- Diabetes Complications Medicine & Life Sciences 21%
- Patient Compliance Medicine & Life Sciences 20%
- Social Support Medicine & Life Sciences 20%
- Caregivers Medicine & Life Sciences 18%
- Chronic Disease Medicine & Life Sciences 15%
T1 - The Value of Measuring Diabetes Burnout
AU - Abdoli, Samereh
AU - Hessler, Danielle
AU - Doosti-Irani, Mehri
AU - Chang, Bernard P.
AU - Stuckey, Heather
N1 - Publisher Copyright: © 2021, The Author(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.
PY - 2021/8
Y1 - 2021/8
N2 - Purpose of Review: Diabetes represents a chronic illness with significant physical and psychological morbidities. This review aims to summarize current conceptualizations of diabetes burnout in individuals with diabetes and describe its associated adverse outcomes in this population while proposing possible mechanisms of action and targets of intervention. Recent Findings: “Diabetes burnout” may result in adverse long-term outcomes including poor treatment compliance, diabetes complications, and depression. Diabetes burnout may impact not only individuals, but also providers, and caregivers and family members of affected individuals. Diabetes burnout may results from sustained cognitive stresses of chronic treatment adherence, assessment of realistic treatment goals, and treatment challenges. Summary: Early screening and interdisciplinary approaches for patient-centered diabetes care are critical for sustained diabetes social support. Future work exploring these approaches may identify early support and targeted interventions for the long-term support of individuals with diabetes.
AB - Purpose of Review: Diabetes represents a chronic illness with significant physical and psychological morbidities. This review aims to summarize current conceptualizations of diabetes burnout in individuals with diabetes and describe its associated adverse outcomes in this population while proposing possible mechanisms of action and targets of intervention. Recent Findings: “Diabetes burnout” may result in adverse long-term outcomes including poor treatment compliance, diabetes complications, and depression. Diabetes burnout may impact not only individuals, but also providers, and caregivers and family members of affected individuals. Diabetes burnout may results from sustained cognitive stresses of chronic treatment adherence, assessment of realistic treatment goals, and treatment challenges. Summary: Early screening and interdisciplinary approaches for patient-centered diabetes care are critical for sustained diabetes social support. Future work exploring these approaches may identify early support and targeted interventions for the long-term support of individuals with diabetes.
UR - http://www.scopus.com/inward/record.url?scp=85108141765&partnerID=8YFLogxK
UR - http://www.scopus.com/inward/citedby.url?scp=85108141765&partnerID=8YFLogxK
U2 - 10.1007/s11892-021-01392-6
DO - 10.1007/s11892-021-01392-6
M3 - Review article
C2 - 34132905
AN - SCOPUS:85108141765
SN - 1534-4827
JO - Current diabetes reports
JF - Current diabetes reports
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
What to know about diabetes burnout

Diabetes burnout describes a feeling of physical and emotional exhaustion due to the demands of living with and managing diabetes.
People experiencing diabetes burnout may feel unmotivated to manage their diabetes . This can cause their glucose levels to rise, placing them at greater risk of hyperglycemia .
Although diabetes burnout has similarities with diabetes distress and depression , it is an experience in its own right with its own symptoms.
In this article, we will explore diabetes burnout in more detail and describe how it differs from diabetes distress and depression.

Diabetes is a demanding condition that often requires a person to engage in strict self-management and an extensive medicinal regime. It is, therefore, unsurprising that people living with diabetes may feel emotionally and mentally drained.
Diabetes burnout refers to a state of feeling overwhelmed, exhausted, and disillusioned stemming from living with and managing diabetes.
Although people may experience diabetes burnout slightly differently from each other, it typically involves a person feeling that they are unable to cope with their diabetes management.
As a result, people with diabetes burnout may disengage from their diabetes care.
Signs and symptoms
A person experiencing diabetes burnout may demonstrate the following signs and symptoms:
- feeling unable to cope with diabetes
- feeling powerless
- feeling detached from oneself
- detaching oneself from social support and healthcare systems
- feeling overwhelmed by diabetes management
- missing or skipping medication, such as insulin
- not monitoring glucose levels as frequently
- not monitoring eating habits
- not engaging in exercise
- ignoring or trying to forget about diabetes
Vs. diabetes distress
Diabetes distress is the negative emotional experience of living with and managing diabetes.
Some research suggests that 1 in 4 people living with type 1 diabetes , 1 in 5 people living with insulin-treated type 2 diabetes , and 1 in 6 people with noninsulin-treated diabetes experience elevated levels of diabetes distress.
A 2020 study exploring how people living with diabetes perceive diabetes distress and diabetes burnout notes that these individuals view them as separate but closely linked experiences.
As such, there are a number of similarities between the two concepts. This includes feelings of:
- powerlessness to manage diabetes
- anger towards diabetes and its management
- being burned-out
- being overwhelmed
- frustration
If a person experiences high levels of diabetes distress for an extended period, it may develop into diabetes burnout
Vs. depression
Depression is a mental health condition in which a person experiences a constant period of low mood, which impairs daily functioning.
Older research suggests that the prevalence of depression is three times higher in those living with type 1 diabetes and two times higher in those living with type 2 diabetes than in the general population.
Little research exists regarding how diabetes burnout specifically differs from depression. However, many reports distinguish diabetes distress from depression.
Where diabetes burnout may stem from an extended period of diabetes distress, the research exploring diabetes distress and depression may be appropriate to explain the differences between diabetes burnout and depression.
Firstly, diabetes distress, and likely diabetes burnout, are specific to the context of living with diabetes. Therefore, the feelings that come with diabetes distress and diabetes burnout may not necessarily manifest in other parts of a person’s life.
On the other hand, the diagnostic criteria for depression describe it as a general emotional state.
Another potential difference between diabetes burnout and depression is how they may impact A1C levels .
Research exploring diabetes distress consistently shows that elevated levels can negatively impact self-management behaviors, in turn leading to an increase in A1C levels. A 2021 study also suggests this may be the case for people experiencing diabetes burnout.
The association between depression, self-management, and A1C is less clear. However, studies claim no association exists. Consequently, the difference in the way depression impacts a person living with diabetes in comparison to diabetes distress and diabetes burnout implies they are distinct concepts.
There are a number of reasons why a person may experience diabetes burnout. A 2021 study suggests that the following may contribute:
- Prolonged diabetes distress: People living with diabetes must make a multitude of daily health decisions. The mental load of having to be constantly considerate of a chronic condition can become exhausting for people.
- Unrealistic treatment goals: If a person feels like they are regularly missing their target A1C or other treatment goals, this may instill a sense of failure or inadequacy.
- Treatment challenges: A person living with diabetes may experience challenges with their treatment — for example, complications, accessing the right type and amount of medication , problems with insurance plans, hypoglycemia , and hyperglycemia.
Tips to manage diabetes burnout
The Centers for Disease Control and Prevention (CDC) suggest that it can be helpful for a person experiencing diabetes burnout to consider the following:
- Involve the health care team: Whether that be a person’s primary doctor, consultant, optometrist, or nurse, these professionals are there to help. As well as reminding a person of the progress made with their diabetes management, they can also help with new strategies in managing diabetes.
- Remember that perfection is impossible: Diabetes can be an unpredictable condition, and this can make management difficult. When it comes to treatment goals, a person should try and break them down into small steps. For example, instead of aiming for a specific target A1C range, a person can focus on lowering their A1C by 1%.
- Lean on the diabetes community: Living with diabetes and diabetes burnout may feel isolating. There are a number of diabetes forums and support groups where people share similar experiences. These supportive environments can create a place for people to feel heard and share advice.
In addition to these recommendations, a person may also wish to consider changing their language and how they discuss the condition. For example, instead of referring to glucose levels as good or bad, they can describe them as high or low.
Additionally, people can seek support from their friends and family. It can be difficult to manage diabetes, and leaning on close acquaintances may help. For example, a person can ask a family member to pick up a prescription or to attend a medical appointment with them.
Supporting someone with diabetes burnout
Research suggests that higher levels of social support may help lower emotional distress in people living with diabetes. A person looking to support someone with diabetes burnout can consider:
- letting them share concerns without being judgmental
- asking the person what they need in terms of support
- acknowledging and validating the person’s feelings
- being empathetic
- celebrating wins
When a person notices that they are starting to feel stressed or overwhelmed due to diabetes and its management, they may consider taking preventive steps to avoid reaching diabetes burnout. These can include:
Taking a break
Some people may refer to this as a diabetes vacation. This refers to taking a few days off from the strict regime that people living with diabetes must adhere to each day. To do this safely, a person should discuss it with their healthcare team.
Reducing stress levels
General stress levels may trigger diabetes burnout. Some ways that can help to reduce stress include :
- getting plenty of sleep
- avoiding or limiting alcohol, tobacco, and substance use
Setting achievable treatment and management goals
A person should work with their healthcare team to create attainable treatment and management goals that work for them.
Asking about new technology
Advances in diabetes technology are providing more options for people living with diabetes. Technology such as continuous glucose monitoring , insulin pumps , and closed-loop systems may help make diabetes management easier.
A person can discuss these options with their healthcare team and figure out which options are available to them.
Diabetes burnout refers to a state of exhaustion that occurs due to the demanding nature of diabetes and its management.
While diabetes burnout is a unique experience for each individual, it usually involves a person feeling unable to cope with their diabetes management, which may cause them to disengage with aspects of their treatment.
To help prevent diabetes burnout, it is advisable that people seek support from their healthcare team, friends and family, and others in the diabetes community. Working towards achievable goals in a supportive environment can help a person to better manage their condition.
Last medically reviewed on August 10, 2022
How we reviewed this article:
- Abdoli, S., et al . (2021). Development and validation of a scale to measure diabetes burnout. https://www.sciencedirect.com/science/article/pii/S221462372100003X
- Abdoli, S., et al . (2021). The value of measuring diabetes burnout. https://link.springer.com/article/10.1007/s11892-021-01392-6
- Abdoli, S., et al . (2020). New insights into diabetes burnout and its distinction from diabetes distress and depressive symptoms: A qualitative study [Abstract]. https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(20)30699-9/fulltext
- Chapter 3: Diabetes distress. (n.d.). https://www.diabetes.org.uk/professionals/resources/shared-practice/psychological-care/emotional-health-professionals-guide/chapter-3-diabetes-distress
- Coping with stress. (2021). https://www.cdc.gov/violenceprevention/about/copingwith-stresstips.html
- Dealing with diabetes burnout. (2022). https://www.cdc.gov/diabetes/library/spotlights/diabetes-burnout.html
- Depression. (2017). https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Depression
- Diabetes distress. (2019). https://www.diabetes.org.uk/resources-s3/2019-03/0526%20Diabetes%20UK%20HCP_Distress_P3.pdf
- Fayed, A., et al . (2022). Relation between diabetes related distress and glycemic control: The mediating effect of adherence to treatment. https://www.sciencedirect.com/science/article/pii/S1751991821002205
- Helgeson, V. (2021). Diabetes burnout among emerging adults with type 1 diabetes: A mixed methods investigation. https://link.springer.com/article/10.1007/s10865-020-00198-3
- Kiriella, D., et al . (2021). Unraveling the concepts of distress, burnout, and depression in type 1 diabetes: A scoping review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8408521/#!po=1.72414
- Kreider, K. (2017). Diabetes distress or major depressive disorder? A practical approach to diagnosing and treating psychological comorbidities of diabetes. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5306125/
- Langberg, J., et al . (2022). The association of hemoglobin A1c levels and depression among adults with diabetes in the United States. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8967126/
- Ramkisson, S., et al . (2017). Social support and coping in adults with type 1 diabetes. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5566130/#__ffn_sectitle
- Roy, T., et al . (2012). Epidemiology of depression and diabetes: A systematic review [Abstract]. https://www.sciencedirect.com/science/article/abs/pii/S0165032712700046?via%3Dihub
Share this article
Latest news
- FDA delays approval of Alzheimer's drug donanemab: What experts think
- Sildenafil (Viagra) may help reduce Alzheimer's risk, study suggests
- Weight loss drug Wegovy gains FDA approval to reduce heart disease risk
- Children and eczema: How the skin condition can cause learning, memory issues
- Metabolic syndrome increases the risk of all types of cancer, study finds
Related Coverage
What are diabetic ulcers? Read on to learn more about this common diabetes complication, including causes, symptoms, treatment, and prevention options.
Brittle diabetes is a rare form of diabetes that involves severe changes in blood sugar levels. Learn about its causes, risk factors, symptoms, and…
What are some of the ways that diabetes may develop? Read on to learn more about the different types of diabetes and their potential causes.
Type 1 and type 2 diabetes can cause many of the same symptoms. Recognizing the early symptoms can help prevent diabetes complications. Learn more…
Diabetes and sleep have a dual-sided relationship, meaning that each can affect the other. Learn more about the link between them and find some tips…
Dealing With Diabetes Burnout

Over time, the emotional burden of managing diabetes can cause burnout.
So far, you’ve had diabetes; it hasn’t had you. You’ve been watching what you eat, making time for physical activity, taking meds, checking your blood sugar, checking your blood sugar again. But then something takes the wind out of your sails. Maybe you’ve been trying hard but not seeing results. Or you developed a health problem related to diabetes in spite of your best efforts.
When you feel discouraged and frustrated, you may slip into unhealthy habits, stop monitoring your blood sugar, even skip doctor’s appointments. It happens to many—if not most—people with diabetes, often after years of good management. You’re in the land of diabetes burnout. How can you get back to healthy living as soon as possible?
Get Your Team Involved
Call on your primary care doctor, eye doctor, podiatrist, dietitian, diabetes educator—anyone and everyone—to help you refocus on your goals. It’s easier for you to see what’s not working instead of what you’re doing right. Your team can remind you of the progress you’ve made and help you with new ideas and strategies.
Don’t Let Perfect be the Enemy of Good
Perfect blood sugar management isn’t necessary and may not even be possible. And sometimes seeing the little picture is better than the big one. Try taking small steps—such as lowering your A1c by 1%—instead of focusing on big goals. You’re still headed in the same direction, but you’ll have more successes along the way.
Call this confidential, free, 24-hour information service (in English and Spanish): 1-800-662-4357
Connect With People Who Get You
Tap into encouragement, insights, and support from people who’ve been there. Online communities for people with diabetes such as the American Diabetes Association’s Community page external icon and the American Association of Diabetes Educators’ Diabetes Online Community pdf icon external icon are great ways to connect with others who share your experience. If you prefer to get involved in person, this directory of diabetes support groups external icon will help you find one nearby.
- Managing Diabetes
- Living Well With Diabetes
- Diabetes and Mental Health
- Diabetes Education and Support
- CDC Diabetes on Facebook
- @CDCDiabetes on Twitter
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
ORIGINAL RESEARCH article
Working with type 1 diabetes: investigating the associations between diabetes-related distress, burnout, and job satisfaction.

- 1 Psychology Research Institute, University of Amsterdam, Amsterdam, Netherlands
- 2 Department of Experimental and Applied Psychology, Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 3 Department of Psychology, Technische Universität Chemnitz, Chemnitz, Germany
The present study investigates the association between diabetes-related distress (DD) and work outcomes (burnout and job satisfaction) among employed people with type 1 diabetes. Employed adults with type 1 diabetes ( N = 297) completed an online survey. Measures assessed emotional, social, food- and treatment-related DD, burnout, and job satisfaction, as well as the type of insulin treatment. We conducted multiple regression analyses to test our hypotheses. Emotional DD was significantly and positively associated with burnout. Social DD was significantly and negatively associated with job satisfaction. The type of treatment (insulin pen versus insulin pump) had no significant effect on the outcomes. This study sets the stage for research on the interactions between working conditions, work outcomes and illness symptoms, and problems of people with type 1 diabetes, and, generally, employees with chronic illnesses. The findings have implications for individual health and illness management, burnout prevention, and occupational health measures.
Introduction
Diabetes can negatively affect work-life, decreasing the probability of employment and increasing the likelihood of work limitations ( Tunceli et al., 2005 ). Although guidelines summarizing the safety risks of employees with diabetes exist ( American Diabetes Association [ADA], 2014 ), these are limited to the physical risks of diabetes during work (e.g., due to hypoglycemia). Many people with chronic illness continue working after being diagnosed; however, they often experience limitations in their work-life ( Vooijs et al., 2015 ). Life with a chronic health condition is not only characterized by physical symptoms and impairments but requires specific illness or health management ( Rak, 2014 ). Illness or health management refers to all activities to maintain or improve one’s health and prevent adverse health consequences, such as following a medical treatment plan and attending appointments with medical professionals ( McGonagle et al., 2020 ).
For employed people with type 1 diabetes, health management comprises controlling blood sugar levels and the intake of insulin ( Rak, 2014 ). However, the requirements and demands caused by health and illness management can present a challenge to employed people with diabetes, as they need to balance both the demands of their job as well as those of the illness when allocating their time and energy resources ( McGonagle et al., 2020 ), which poses a risk of negative work-related outcomes, in particular burnout ( Demerouti et al., 2001 ).
Burnout is associated with negative occupational consequences, such as lower retention rates ( Rabatin et al., 2016 ), lower job performance ( Taris, 2006 ), and withdrawal ( Taris et al., 2001 ), and psychological consequences, such as lower life satisfaction and depressive symptoms ( Hakanen and Schaufeli, 2012 ). Furthermore, burnout can have physical consequences, particularly affecting the metabolic and cardiovascular systems ( Kitaoka-Higashiguchi et al., 2009 ), leading to substantial health risks for people with type 1 diabetes.
Due to the early onset age and the necessity of insulin treatment ( Maahs et al., 2010 ), most employees with type 1 diabetes may face the challenge of integrating both work and illness management for most of their time as active members of the workforce. Thus, insights into the association between diabetes type 1 and burnout are crucial for developing appropriate working conditions for chronically ill people because certain working conditions (e.g., lack of autonomy in assembly-line work or customer service) make the illness management of employees with type 1 diabetes more difficult. Moreover, various preventative countermeasures in health education can be derived for different stakeholders, e.g., implementing educational training for leaders and HR managers and specific stress prevention training for employees with diabetes. However, even though the interest in mental health at work is steadily rising, to this point, there is only little insight into the association between chronic illness and work outcomes such as burnout and job satisfaction. This is problematic as people with chronic illnesses such as diabetes are often more likely to retire earlier, leading to an economic and societal burden ( Vijan et al., 2004 ), and both burnout and job satisfaction are important predictors of workplace retention ( Rumrill et al., 2004 ; Swider and Zimmerman, 2010 ). Furthermore, existing studies on work and diabetes have focused mostly on diabetes mellitus as a potential health outcome of work stress ( Cosgrove et al., 2012 ) or shift work ( Gan et al., 2015 ).
The present paper investigates the association of diabetes-related distress (DD) on burnout and job satisfaction at work compared to other work-related demands (e.g., quantitative job demands and lack of autonomy). Applying resource-based models of occupational health and burnout, namely the Job Demands-Resources Model (JDR, Bakker et al., 2014 ) and the Conservation of Resources Model (COR, Hobfoll and Freedy, 1997 ), we investigate the association between perceived illness-related distress and work-related mental health outcomes. In line with recent additions to the Job-Demands Resources model ( Demerouti et al., 2001 ) that emphasize the role of personal resources ( Schaufeli and Taris, 2014 ), we add to the literature by investigating the employees’ existing health, respectively illness status as a personal resource ( McGonagle et al., 2015 ). We tested our assumptions utilizing a cross-sectional online study amongst employed people with type 1 diabetes. Our findings offer a potential starting point to better understand employees with type 1 diabetes at work. Moreover, they could give a push to engage and research regarding counseling, medical treatment, the improvement of existing workplace health management programs, the development of new workplace health management programs aimed at providing support for chronically ill employees, and human resource development measures for supervisors and managers of a health-diverse workforce. Furthermore, our study responds to the call for more theory-driven research regarding the work-life and careers of people with chronic diseases ( Lehmann et al., 2021 ).
Diabetes-Related Distress
An important factor to consider when studying the effects of a chronic illness is that people can strongly differ regarding their individual and subjective problems with the respective disease and may experience different effects of these problems. The most prominent variable to capture the inter-individual variance regarding these experiences is assessing the level of individually perceived DD. DD comprises the “unique and hidden emotional burden or frustration that comes with living with diabetes and considers ongoing concerns, worries, and fears of diabetes management as well as diabetes complications” ( Abdoli et al., 2019 , p. 2). Although DD is often utilized and conceptualized as a construct with a single general factor, factor analyses suggest it can be differentiated into four subordinate dimensions: Emotional problems, food-related problems, treatment problems, and social problems (lack of support) ( Polonsky et al., 2005 ). The general measures of DD and the emotional and treatment-related subdimensions of DD are positively associated with glycosylated hemoglobin (HbA 1 c ) levels and blood glucose self-monitoring. The HbA 1 c level “reflects average plasma glucose over the previous eight to 12 weeks” ( World Health Organization [WHO], 2011 , p. 6) and is commonly used as a diagnostic measure for diabetes. However, it is important to note to this point there is no theoretical framework that supports the inclusion and definition of the subdimensions. Furthermore, there is conflicting evidence regarding the factor structure of DD assessments, as some studies (e.g., Graue et al., 2012 ) have failed to replicate the four-factor solution or found a one-factor general DD solution to have a better fit ( Graue et al., 2012 ; Schmitt et al., 2016 ).
People with type 1 diabetes report higher general DD compared to people with type 2 diabetes, and the level of perceived diabetes distress is higher amongst people with more diabetic complications such as kidney damage, albuminuria, retinopathy, neuropathy, heart disease, stroke, and vascular disease ( Fenwick et al., 2018 ). People with higher levels of general DD report lower subjective health, as well as more problems with self-care, dieting, and blood glucose testing ( Schmitt et al., 2016 ) as well as higher Hb1Ac ( Graue et al., 2012 ) and more fear of hyperglycemia ( Amsberg et al., 2008 ). General DD is also associated with depressive symptoms, general anxiety, and lower self-esteem ( Fenwick et al., 2018 ) and coping styles such as distractive coping, trivialization, and depressive coping ( Schmitt et al., 2016 ). Individuals experiencing higher levels of DD also tend to experience a higher stigma associated with type 1 diabetes, including the perception that they are being treated differently due to their illness and that they are blamed and judged ( Browne et al., 2017 ).
As studies investigating the effects of the subdimensions are sparse, there is little evidence of differences in their effects. All four facets are negatively correlated with well-being and positively associated with worrying about hyperglycemia and trait anxiety ( Snoek et al., 2000 ). Furthermore, all four subtypes are significantly and positively associated with depressive symptoms ( Polonsky et al., 2005 ; Martin et al., 2018 ) and negatively associated with mental health, social functioning, and vitality ( Graue et al., 2012 ). However, only emotional and treatment-related DD are significantly associated with HbA1C and self-monitoring of blood glucose ( Snoek et al., 2000 ). Individuals with higher emotional, social, and food-related DD also report significantly greater problems regarding meal planning. Furthermore, whereas food-related and interpersonal/social DD are positively associated with higher cholesterol levels, only food-related DD is associated with lower self-monitoring of blood glucose ( Polonsky et al., 2005 ).
Associations of Diabetes-Related Distress and Work Outcomes
Research on the work-life of people with type 1 diabetes is sparse, however, is evidence that “working-age adults with diabetes are more likely to be unemployed or unable to work, miss workdays, or have severe difficulty with work tasks compared to those without diabetes” ( Fritschi and Quinn, 2010 , p. 37). In a qualitative study on diabetes and work, young adult employees with type 1 diabetes reported difficulties with diabetes management during work. Especially under time pressure or when experiencing difficulties with the illness, employees with type 1 diabetes reported that they neglected or decreased the diabetes management activities ( Balfe et al., 2014 ). Previous research also indicates a negative association between the number of years since the onset of the illness and wages, whereas a stable HbA1c was positively associated with the wage level ( Brown et al., 2012 ). Furthermore, a study including people with type 1 and type 2 diabetes found that working conditions characterized by high job demands, low decision latitude, and low social support predicted fatigue amongst the study sample ( Weijman et al., 2003 ). A study on the association between burnout and receiving treatment for chronic illnesses indicates an association between burnout and treatment for diabetes. However, the authors did not indicate the diabetes type ( De Beer et al., 2016 ).
Insights into the effects of diabetes on general well-being and everyday functioning indicate two main mechanisms through which type 1 diabetes may impact employment and lead to negative work-related outcomes. The first mechanism is rooted in the effect of disease on the perceived energy and emotional well-being. Existing evidence implies that type 1 diabetes is linked to chronic fatigue, i.e., feelings of physical and emotional exhaustion ( Goedendorp et al., 2014 ; Kalra and Sahay, 2018 ). Chronic fatigue in people with type 1 diabetes is only weakly associated with blood glucose levels. It cannot be fully explained by depression ( Goedendorp et al., 2014 ), a common comorbidity of type 1 diabetes ( Gendelman et al., 2009 ). However, fatigue can have substantial effects on daily life, as it is related to reported functional impairments, such as mobility, social interactions, and work limitations ( Goedendorp et al., 2014 ). A theoretical framework on fatigue in people with diabetes ( Fritschi and Quinn, 2010 ) states that DD is one of the psychological factors associated with fatigue. However, it does not state an exact causality relation between the concepts.
The second mechanism is rooted in the burden of treatment, i.e., the time and effort required to manage a chronic illness ( Sav et al., 2015 ). To prevent potentially fatal exacerbations, type 1 diabetes requires a high and constant level of day-to-day management activities, including, but not limited to, blood glucose monitoring. The responsibility of the management activities lies mainly on the people with type 1 diabetes themselves ( Ahola and Groop, 2013 ). As diabetes self-management requires resources such as time, energy, and cognitive capacity, employed people with type 1 diabetes can experience tensions between their work and diabetes management ( Pyatak, 2011 ). Moreover, people with type 1 diabetes may experience a lack of mental, emotional, and physical energy and feelings of detachment regarding their diabetes management, a phenomenon known as diabetes burnout. Diabetes burnout is strongly and positively associated with DD. However, it is conceptually distinct ( Abdoli et al., 2020 ). In sum, both mechanisms imply that employees with type 1 diabetes experience a loss of resources in terms of time and energy due to the symptomology of the illness itself and the high and constant illness management requirements.
Individual resources are highly relevant in theories explaining work-related employee well-being and other, more distal work-related outcomes such as performance and satisfaction. Two fundamental theoretical frameworks from the field of occupational health psychology, namely the conservation of resources theory (COR) ( Hobfoll, 1989 ) and the job-demands resources model (JDR) ( Demerouti et al., 2001 ), include employee resources as an essential factor in their explanations of the etiology and processes underlying employee strain. As the development of the JDR was influenced by COR ( Bakker and Demerouti, 2017 ), both theoretical frameworks lead to similar conclusions regarding their proposed effects of employee resources, or a lack thereof, on strain, which manifests as burnout. Burnout is one of the most commonly researched work-related mental health outcomes and is mainly characterized by exhaustion, loss of energy, depletion, and detachment ( Maslach and Leiter, 2017 ).
The COR focused on the effects of the availability and investment of resources which can include material objects (e.g., money), but also personal characteristics (e.g., self-esteem), and energy resources ( Hobfoll, 1989 ; Park et al., 2014 ). According to COR, a loss of resources is stressful to individuals and predicts strain and burnout ( Hobfoll, 1989 ). As the resources of employees with type 1 diabetes resources can be limited due to the illness and its symptoms (e.g., fatigue) ( Kalra and Sahay, 2018 ), as well as the time and effort required to manage the illness (burden of treatment) ( Sav et al., 2015 ), they may have a higher risk for a resource loss cycle. Higher levels of DD should intensify this resource loss cycle and hence the level of burnout, particularly because high diabetes distress is associated with negative emotionality and perceived stress ( Coccaro et al., 2020 ).
In contrast to the COR, the JDR model considers the work characteristics as it postulates that stress and burnout are the results of direct effects and interactions of job demands and job resources. High job demands (e.g., time pressure, physical workload, shift work) directly affect employee strain. A lack of job resources (rewards, job control, support) or personal resources (resilience, self-efficacy, and intrinsic motivation) can lead to increased difficulties in meeting the job demands, thus also increasing the risk for burnout ( Demerouti et al., 2001 ; Schaufeli and Taris, 2014 ).
The JDR model is one of the most frequently applied models to explain the development of stress and burnout ( Schaufeli and Taris, 2014 ). In a recent study amongst employed people with multiple sclerosis (MS), a chronic neurological autoimmune illness, job demands and job resources predicted the experienced MS-related difficulties at work. These difficulties (e.g., cognitive and physical limitations and external barriers) mediated the effects on job demands and burnout and job demands and turnover intentions ( Lehmann et al., 2021 ). Whereas this study investigated the health-related difficulties at work as a mechanism within the JDR model, physical health status can also be conceptualized as a personal resource within the JDR framework. Thus, a pre-existing chronic illness or health impairment signifies a loss of resources or status of diminished resources, leading to a higher vulnerability toward demands and stressors ( McGonagle et al., 2015 ).
Previous research on diabetes (type 1 and type 2) shows inconclusive results on the association between diabetes (versus no diabetes) and burnout. In general, burnout seems to be more prevalent among employees with chronic medical illnesses than employees without any chronic medical condition ( Armon et al., 2014 ). A study including 7895 employees from different sectors ( De Beer et al., 2016 ) did not find a significant relationship between diabetes and levels of burnout. However, the authors did not assess or report the type of diabetes among the participants.
To our knowledge, only one existing study has investigated the effects of the individual perception of the severity of the illness in terms of DD and occupational burnout. In a sample of employees with type 2 diabetes, self-reported DD was not only significantly associated with burnout but also mediated the effect of Hb1ac levels on burnout and the effect of positive affect on burnout. Moreover, it was particularly strongly associated with the exhaustion dimension of burnout ( Han, 2008 ). According to COR and JDR, we assume that high levels of DD are associated with high levels of burnout. Moreover, we suggest that DD explains variance in burnout above and beyond other job characteristics.
Hypothesis 1: Diabetes-related distress is positively associated with burnout.
In addition to burnout, we are focusing on job satisfaction as a secondary outcome. Job satisfaction is a positive emotional attitude or state resulting from the appraisal of one’s job or experiences on the job, that is influenced by dispositions of the employee and job characteristics ( Judge et al., 2020 ). Meta-analytical evidence ( Faragher et al., 2005 ) shows strong and negative associations with burnout, positive associations with mental health outcomes (anxiety and depression), and smaller yet significant associations with subjective physical illness. Job satisfaction is also an important predictor of turnover intention and job tenure, but it also plays an important part in work adjustment and rehabilitation for people with chronic diseases ( Roessler et al., 2004 ).
Furthermore, job satisfaction is strongly and positively associated with self-esteem ( Faragher et al., 2005 ). A study on self-esteem and type 1 diabetes showed that individuals that reported feeling overwhelmed by diabetes also had low levels of self-esteem. Moreover, self-esteem and illness self-concept were positively related to diabetes-related problems. Individuals with low levels of self-esteem reported experiencing less support and more treatment- and emotional problems 5 years later ( Luyckx et al., 2008 ). As self-esteem is related to diabetes-related problems and job satisfaction, we assume that DD affects job satisfaction negatively and explains variance in job satisfaction above and beyond other job characteristics.
Hypothesis 2: Diabetes-related problems are negatively associated with job satisfaction.
Regarding the dimensionality of DD, there are no clear theoretical and empirical indicators that allow for the development of distinct hypotheses for the specific subdimensions, particularly as all four subdimensions are positively associated with mental health problems and negatively associated with social functioning ( Graue et al., 2012 ). Given the limited evidence so far, we, therefore, aim at an explorative analysis of the associations between different types of DD and work-related outcomes.
Research Question 1: Are there differences between the subdimensions regarding their association with burnout?
Research Question 2: Are there differences between the subdimensions regarding their association with job satisfaction?
Types of Diabetes Treatment
Individuals with type 1 diabetes have two main options for insulin treatment: multiple daily injections of rapid-acting insulin combined with daily basal insulin or continuous subcutaneous insulin infusion ( Maahs et al., 2010 ). Past research investigated the effect of different insulin treatments (syringe, pen, and pump) on psychological outcomes: a study on 132 patients with insulin-dependent diabetes mellitus investigated insulin therapy change. Patients who changed from traditional syringe treatment to insulin pen were more satisfied with their performance at work, life in general, and time for diabetes management and felt less restricted regarding social relationships, diet, leisure time. Patients who changed from an insulin pen to an insulin pump were more satisfied with time for diabetes management and felt less restricted regarding social relationships, diet, leisure time ( Chantelau et al., 1997 ). These findings suggest that insulin treatment with a pump can improve illness management, which should lead to less DD and hence lower levels of burnout and higher levels of job satisfaction.
Hypotheses 3a: Employees who use an insulin pump in contrast to an insulin pen report lower levels of burnout.
Hypotheses 3b: Employees who use an insulin pump in contrast to an insulin pen report higher levels of job satisfaction.
Materials and Methods
Study design.
We conducted a cross-sectional study among adult employed people with type 1 diabetes. Before starting the questionnaire, the participants had to confirm that they fulfilled the inclusion criteria (minimum age of 18 years, employment with at least 20 h per week work time, medical diagnosis of type 1 diabetes). The inclusion criteria were presented to the participants as a list and the participant and to select the option stating that they fulfilled all criteria before they could proceed with the survey.
We conducted an a priori power analysis using G ∗ Power ( Faul et al., 2007 ) to determine the sample size. Based on previous similar research on chronic illness severity, burnout, and job satisfaction ( Han, 2008 ; Siu et al., 2013 ), we chose a size of f 2 = 0.08 as the basis of our calculation resulting in a minimum sample size of N = 155 to reach a power of 0.80 and N = 238 for a power of 0.95 assuming that we would test the effects of the four DDS subdimensions and their incremental effects above and beyond six covariates. We therefore aimed at acquiring a sample size between 200 and 300.
Data collection took place in the first quarter of 2018 (early January until late March). We recruited the sample through an announcement by a German monthly magazine for people with diabetes and social media groups on diabetes. The assessment was carried out via a self-report online questionnaire and was only available in German. Participants were excluded if they did not have type 1 diabetes, suspected having type 1 diabetes yet did not have a diagnosis from a medical professional, were self-employed or unemployed, and/or did not speak German. Participants did not receive compensation for their participation in the study. The study design was submitted for a pre-review to the responsible ethics review board, which declared no necessity for a full review. 1 During the design and conduction of the study, we made sure that we adhered to the ethical guidelines of the German Psychological Association (DGPs).
We assessed burnout with the personal burnout scale of the Copenhagen Burnout Inventory (CBI, Kristensen et al., 2005 ). We used the German translation of the scale as included in the German version of the Copenhagen Psychosocial Questionnaire ( Nübling et al., 2006 ). The scale consists of 6 items answered on a 5-point Likert-type scale from 1 = does not apply at all, to 5 = applies very strongly. We calculated the mean value of the scale. Higher mean values imply more severe burnout symptoms. The scale showed very good reliability with α = 0.92, respectively ω RT = 0.94 ( Revelle, 2016 ; McNeish, 2018 ).
Job Satisfaction
We assessed job satisfaction with the eponymous subscale from the COPSOQ ( Nübling et al., 2006 ). The scale consists of nine items that ask for the participant’s satisfaction with different job-related aspects (e.g., salary, general working conditions, the way his/her abilities are used) with a 4-point Likert-type response scale from 1 = very dissatisfied to 4 very satisfied. Larger scale mean values imply higher job satisfaction. The scale showed good reliability with α = 0.86 and ω RT = 0.90.
We assessed DD with the German version of the Problem Areas in Diabetes Questionnaire (PAID, Polonsky et al., 1995 ). The PAID questionnaire is frequently used amongst individuals with type 1 diabetes to assess DD and has been translated into multiple languages ( El Achhab et al., 2008 ; Lee et al., 2015 ). The PAID has four subscales that assess the four different areas of diabetes-related problems: emotional (12 items), social (two items), food-related (three items), and therapy-related problems (three items) ( Snoek et al., 2000 ). All items were answered in a 4-point Likert-type scale from 1 = does not apply at all to 5 = applies very strongly. We calculated the mean values for each subscale, with higher values signifying higher levels of DD. The scale reliabilities were acceptable to excellent, with α = 0.93 and ω RT = 0.95 (emotional), α = 0.73 and ω RT = 0.73 (social), α = 0.76 and ω RT = 0.76 (food-related), and α = 0.70 and ω RT = 0.73 (therapy-related).
Type of Insulin Therapy
We assessed the type of insulin therapy with a single item, asking the participants to check the type of therapy they currently apply (0 = pen, 1 = pump, 2 = syringe, 3 = other). Participants that chose the “other” category were asked to describe their insulin therapy in an open text field.
Control Variables
We included age and gender as covariates as women and younger employees are more likely to experience higher emotional exhaustion ( Brewer and Shapard, 2004 ; Purvanova and Muros, 2010 ). To analyze the incremental validity of the predictors above and beyond working conditions whether the participant’s job included leadership responsibility. We assessed leadership responsibility with one item: “What is your current job position” with two response options 1 = employee with leadership responsibility and 0 = employee without leadership responsibility. Furthermore, we assessed quantitative job demands and the degree to which the participants had control over their work time using two eponymous scales from the COPSOPQ ( Nübling et al., 2006 ). The quantitative job demands scale consisted of seven items with a 5-point Likert-type response scale from 1 = never to 5 = always. Higher mean values imply higher perceived quantitative job demands. Scale reliability was excellent with α = 0.86 and ω RT = 0.90. The control over work time scale consisted of four items and was answered with the same response scale as the quantitative job demands scale. Scale reliability was good with α = 0.87 and ω RT = 0.90.
The final sample consisted of N = 237 participants. Of the study sample, 67.34% were female, and 46.80% reported having a university degree. Participants reported working an average of 35.82 h/week ( SD = 7.05). About half of the participants ( N = 156, 52.2%) were employed in the public sector, respectively worked in the fields of healthcare, education, whereas N = 46 (15.5%) worked in manufacturing, N = 29 (9.8%) worked in trade, transport, or the hospitality industry, N = 26 (8.8%) worked in the information and communication industry, and N = 24 in the financial, insurance and business services.
The rest of the sample consisted of employees from the energy, real estate, and agricultural sectors. Most participants reported having disclosed their diabetes to their line manager (93.94%) and at least some colleagues (95.96%). Fifty-nine participants (19.87%) reported having a secondary illness (38.98% diabetic retinopathy, 30.51% diabetic neuropathy, 3.39% diabetic nephropathy, and 25.42% other/not stated). 46.46% reported using a pen, and 53.53% reported using a pump. None of the participants in this sample reported using a different type of insulin therapy.
Analytical Approach
The steps of the data analysis were planned as follows: first, a confirmatory factor analysis (CFA) was to be conducted to confirm the validity of using the four DD subscales (compared to a one-factor solution), followed by a descriptive analysis of the bivariate correlations (for the numeric variables) and t -tests to analyze possible associations between dichotomous and numerically scaled variables. To test the study hypotheses, we conducted a series of multiple regression analyses for each outcome. In the baseline models, we regressed the respective outcome on age and gender only (Models 1a and 2a). In the next step, we added the work-related covariates (Models 1b and 2b) before adding the main predictors in the final step (Models 1c and 2c). All analyses except for the CFA were carried out using the psych package ( Revelle, 2021 ) for the R environment ( R Development Core Team, 2015 ), whereas the CFA was conducted using the lavaan package for R ( Rosseel, 2012 ).
Before hypothesis testing, we conducted a confirmatory factor analysis to confirm the 4-factor structure of the PAID. We compared the proposed 4-factor structure to a single-factor model. The 4-factor structure fit the data significantly better, with Δχ 2 ( 6 ) = 129.21, p < 0.001. However, it is important to note that the 4-factor model did not meet the criteria for an acceptable model fit (cf. Schermelleh-Engel et al., 2003 ), with χ 2 ( 164 ) = 592.93, CFI = 0.887, and RMSEA = 0.094 ( Table 1 ).

Table 1. Results of the confirmatory analyses testing the 4-factor structure of the PAID.
The analysis of the bivariate correlations ( Table 2 ) revealed that the number of working hours per week was not significantly associated with any of the study outcomes or predictors and was therefore not included in the further analyses. The correlation analyses further revealed positive and significant bivariate associations between all dimensions of DD and burnout and significant negative associations between DD and job satisfaction. Gender was significantly correlated with emotion-related DD and burnout, indicating that female participants reported higher levels of both variables. Control over work time was significantly and negatively correlated to all four DD dimensions, and quantitative work demands were positively correlated with food-related DD. In addition to the bivariate correlations, we conducted t-tests to investigate whether gender was associated with the study variables. Participants identifying as female reported significantly higher levels of burnout ( M = 3.15) compared to participants identifying as male ( M = 2.78), with t (295) = 3.58, p < 0.001. There was no significant difference in job satisfaction between genders, with t (295) = −1.05, p = 0.30. (See Supplementary Appendix A for the gender differences of all study variables).
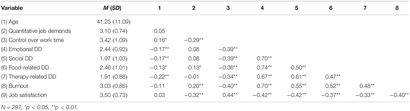
Table 2. Bivariate correlations of the numerically scaled variables.
We conducted t -tests to test for differences in the outcomes as a function of the type of insulin therapy. There were no differences in either burnout, t (295) = −0.81, p = 0.42, or job satisfaction, t (295) = 0.65, p = 0.52, between participants using a pen and participants with a pump (see Supplementary Appendix B for the differences between pen and pump for all study variables).
To test the study hypotheses, we conducted a series of multiple regression analyses for each outcome. In the baseline models, we regressed the respective outcome on age and gender only (Models 1a and 2a). In the next step, we added the work-related covariates (Models 1b and 2b) before adding the main predictors in the final step (Models 1c and 2c). The results of the regression analyses are stated in Table 3 .
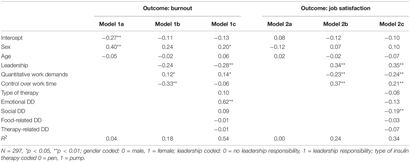
Table 3. Models regressing the standardized outcomes on standardized predictors.
Controlling for demographic variables (age and gender) as well as work-related variables, emotional DD was significantly and positively associated with burnout (β = 0.62, p < 0.001), thus supporting Hypothesis 1. Together, all DD variables explained 36% of the variance in burnout. Finally, social DD was significantly and negatively associated with job satisfaction (β = −0.19, p < 0.01), controlling for age, gender, and working conditions. Together, all DD variables explained 10% of the variance in job satisfaction. Regarding Hypotheses 3a and 3b on the association between type of insulin therapy and work-related outcomes, we did not find any indication of a difference in burnout or job satisfaction between participants using insulin pens and participants with pumps in the regression analysis. These results align with the results of the t -tests that we carried out in the descriptive analyses. Thus, we conclude that Hypotheses 3a and 3b are not supported.
Similar to the results of the bivariate correlation, participant gender had a positive and significant effect on burnout in the regression analyses, implying that female participants were more likely to report higher burnout levels. Quantitative job demands, which were included as a covariate, had a significant positive effect on burnout and a significant negative effect on job satisfaction. In contrast, control over work time was significantly and positively related to job satisfaction only.
Supplemental Analyses
Due to the cross-sectional nature of the assessment and the strong positive correlation between emotional DD and burnout, we conducted a confirmatory factor analysis to justify treating these variables as separate constructs. We tested a single factor model (emotional DD and burnout) against the 2-factor model ( Table 4 ). The 2-factor model fit the data significantly better, with Δχ 2 ( 1 ) = 417.62, p < 0.001, therefore justifying the treatment of the variables as separate constructs. However, it is noteworthy that the 2-factor model did not fulfill the criteria for acceptable model fit (cf. Schermelleh-Engel et al., 2003 ).

Table 4. Results of the confirmatory analyses testing the distinctions between emotional diabetes-related problems and symptoms of stress, respectively burnout.
The present study’s findings on employees with type 1 diabetes show that DD is associated with burnout and job satisfaction. Higher levels of DD are linked to higher levels of burnout and lower level of job satisfaction. For each of the respective outcomes, a specific facet of DD explained variance in the outcome above and beyond job demands and control over time. For burnout, the emotional facet of DD (e.g., feeling alone with diabetes) was most relevant. In contrast, the social facet of DD (e.g., worrying about reactions) was strongly related to job satisfaction.
Additionally, it is important to emphasize the extent of the variance explained by diabetes-related variables found in this study. Previous research estimates the correlations between workplace-related stress and health variables to rarely exceed r = 0.333 or R 2 = 0.10 ( Faragher et al., 2005 ). In one of the two full models of our study (Model 1c), the DD explained more variance than age, gender, and workplace variables together, indicating that diabetes-related problems may have a greater impact on job satisfaction than job characteristics. The variance explanation of job satisfaction in Model 2c is smaller compared to the variance explanation of burnout (Model 1c). However, it is important to note that in Model 2c DD still explained 10% of the variance in job satisfaction. The insulin treatment method (pump vs. pen) did not affect burnout or job satisfaction, implying the rejection of Hypotheses 3a and 3b. However, pump users, in contrast to pen users, reported less food-related DD.
Theoretical Implications
Our results align with findings on DD and burnout among people with diabetes type 2 ( Han, 2008 ). This reinforces the assumption that health status should be viewed as an individual resource that plays an important role in the development of burnout ( McGonagle et al., 2015 ). Previous research has been strongly focusing on physical health or illness as a critical outcome of burnout. Yet, systematic analyses on the exact causal nature of the association and, in particular, possible reciprocal effects are lacking ( Maslach, 2001 ). There are, to our knowledge, no existing models of occupational health and burnout (e.g., JDR and COR) that account for a possible diversity in individual employee health statuses. Thus, our study is in line with previous work that suggests an integration of occupational health and diversity research, viewing chronic illness as a dimension of organizational diversity ( Beatty and Joffe, 2006 ).
The associations found in this study support the proposition of investigating existing health status and health impairments as a personal resource within the JDR ( McGonagle et al., 2015 ). Personal resources can directly impact well-being, moderate the effects of job characteristics, mediate the effect of job characteristics, and influence the perception of job characteristics ( Schaufeli and Taris, 2014 ). Research on well-being fundamentally supports this general understanding of the impact of health ( Sonnentag, 2015 ): The current level of well-being affects the perception of job demands ( de Jonge et al., 2001 ), job resources (e.g., Reis et al., 2015 ) and personal resources ( Xanthopoulou et al., 2009 ) in the future. Taking these findings into account, it can be assumed that health impairments like DD impact the well-being of chronic-ill employees and their perception of working conditions. This study mostly focused on the direct effect of diabetes-related problems (as a proxy for impaired health) on well-being outcomes. Future research should investigate whether individuals with diabetes-related problems or individuals with health impairments in general show different reactions to job characteristics in general terms of well-being outcomes.
Moreover, future research should analyze whether the subjective perception of job characteristics, such as quantitative and cognitive job demands, depends on the health status of the perceiver, for example by comparing employees with different health statuses working the same or very similar job within the same organization or team. Insights on these aspects allow a differentiate consideration of chronic-ill employees in their organizations. This is relevant in that illness management is predominantly the task of chronic-ill employees ( Rak, 2014 ) and organizations should take more responsibility in this regard.
Further results of our study are that certain facets of DD are strongly related to burnout and job satisfaction. The emotional facet of DD (e.g., feeling alone with diabetes) was most relevant for burnout, whereas the social facet of DD (e.g., worrying about reactions) for job satisfaction. The strong association between the emotional facet of DD and burnout may be based on the common relationship to depression. Employees exposed to difficult working conditions for a long time have a higher risk for burnout, which can cause depression in the long term ( Hakanen and Schaufeli, 2012 ). However, the measurement of emotional distress in diabetes and the psychiatric diagnosis of depression shows a conceptual overlap that requires a strong association ( Gonzalez et al., 2011 ). The differences in the magnitude of explained variance between burnout and job satisfaction by the DD subdimensions is in line with the assumptions job satisfaction is a more distal outcome of work-related stressors, and a possible consequence of burnout ( Wolpin et al., 1991 ). Thus, future studies with longitudinal designs should investigate the possibility of burnout mediating the effect of DD on job satisfaction.
Additionally, it can be assumed that employees in our sample have been confronted with the consequences of diabetes for a long time, which increases the emotional burden. The specific association between the social facet of DD and job satisfaction shows parallels to the relationship of neuroticism and job satisfaction, which is one of the strongest personality factors regarding job satisfaction ( Judge et al., 2002 ). Employees with a high level of neuroticism are less satisfied with their work. The anxiety of reactions from other people is a crucial element of neuroticism and the social facet of DD. This might be an explanation for the specific association between the social facet of DD and job satisfaction.
In contrast to hypotheses 3a and b, the type of insulin therapy did not predict any work-related outcome. However, the portion of pen and pump users was relatively balanced in our sample. Despite the advantages of insulin pumps in the illness management of diabetes type 1 ( Karges et al., 2017 ), employees did not experience less burnout or more job satisfaction than employees using an insulin pen. One possible reason for this result might be the habitation of handling with the respective insulin therapy over time. People get used to dealing with the type of insulin therapy and integrate them into their daily routine. An interesting finding in the additional analyses ( Supplementary Appendix B ) was that pen users reported more control over their work time than pump users. This may imply that the choice of insulin intake could be guided my aspects of the job itself. Less control over work time could imply more difficulties regarding diabetes management (i.e., monitoring blood glucose and manually injecting), thus providing a reason to choose a pump over a pen. Future research should consider this aspect when investigating the impact of insulin therapy among employees with diabetes type 1.
Practical Implications
Our findings are highly relevant for employed or soon to be employed individuals with type 1 diabetes, diabetologists, and other diabetes-related treatment and counseling providers, as they are the main providers of diabetes-related information. Awareness of the strong associations between DD and burnout may prevent employees with high levels of burnout from using self-blame as a coping mechanism ( Spataro et al., 2016 ) and motivate them to pay close attention to warning signs of exhaustion. Furthermore, knowledge about the effects of diabetes on work-life can be crucial for the career choices of adolescent people with type 1 diabetes.
Our results indicate that employees with type 1 diabetes have additional challenges that are associated with work-related outcomes. The reduction of DD provides an interesting starting point for improving work-life and preventing burnout among employees with diabetes type 1. Current approaches to working with diabetes mainly focus on the individual as the main actor in maintaining individual health and preventing worsening of the illness or it’s symptoms. A meta-analysis on self-efficacy education programs in persons with diabetes shows positive effects on HbA1C levels, self-management behaviors, knowledge, and quality of life. However, the review notes that most of the studies are characterized by low quality, short-term follow-up periods, and deficient physiological and emotional strategies ( Jiang et al., 2019 ). The limited usage of strategies to improve the emotional state seems problematic as our findings show that the emotional facet of DD is particularly important for burnout. Other approaches, such as a specific 12-week coaching program for working individuals with chronic illness (e.g., ankylosing spondylitis, multiple sclerosis, nerve injury or neuropathy, diabetes Types 1 and 2), may provide a first starting point ( McGonagle et al., 2014 ). This coaching intervention focuses on reinforcing four central personal resources in the context of work-related health (job self-efficacy, mental resources, core self-evaluations, and resilience) to reduce work-related challenges of employees with chronic illness (e.g., coming to work when sick, disclosing illness at work, long-term sickness absence and low levels of workplace support) and hence prevent further resource losses ( Hobfoll, 1989 ).
In addition to the individual initiative of chronically ill employees to improve their illness management, organizations should support these efforts in workplace health management. However, organizations may be unaware of the prevalence of chronic illness among their employees, especially because symptoms are often invisible ( Beatty and Joffe, 2006 ). In the context of diversity, organizations should explicitly name chronic ill employees as a significant part of the organizational workforce in the mission statement and point out that their specific concerns will be considered in organizational decision-making processes (e.g., design of tasks, workflow, and roles as well as health-related offers). Chronic illness can lead to day-to-day fluctuations of the employee’s capabilities. Thus, flexibility may be a core aspect in this process, for example, regarding work schedules (e.g., flextime), task assignments (e.g., completing tasks according to the present physical condition), and methods of task performance (e.g., work from home) ( Beatty and Joffe, 2006 ). However, the respective actions must be planned and implemented with close regard to the needs and requirements of the chronically ill employees, which requires further investigation into the specific needs of employees with type 1 diabetes at work. A high level of organizational support may motivate chronically ill employees and evoke trust for illness disclosure leading to more inclusive organizations.
Strengths and Limitations
A strength of the study lies in adequately sized sample of employees with a specific chronic illness which allows us to investigate associations between health- and work factors amongst people with type 1 diabetes. Chronic illnesses are still greatly overlooked in occupational health research and organizational diversity research ( Beatty and Joffe, 2006 ). During the data collection period, we received positive feedback from participants that felt that the topic needs more attention, and several participants shared suggestions for future research topics that were rooted in their day-to-day experiences.
However, there are several limitations. First, the cross-sectional design does not allow to test for causal relations. Future studies should include prospective and longitudinal designs, e.g., to test for reciprocal effects of diabetes-related and work-related outcomes. Second, our study is based solely on self-reported data, which is why we cannot exclude the possibility of a common method bias. Further studies should combine self-reported questionnaire data with physiological indicators such as the HbA1c to increase the validity of the findings. As the inclusion criteria were also based on self-report, we cannot exclude the possibility that people without type 1 diabetes took part in the study. Although we announced the study both in social media and in a print outlet, the fact that we assessed the data via an online survey might have attracted a younger sample. Third, although the 4-factor solution of DD fit the data best, the overall fit of the model was not good and did not match the findings of previous studies on the factor structure of the PAID (e.g., Snoek et al., 2000 ). We also found less than acceptable fit indices regarding the 2-factor model of emotional DD and burnout. It is important to keep in mind that the PAID was initially developed as a unidimensional instrument, therefore further studies on the construct validity of the instrument should be carried out.
Finally, our burnout instrument assessed burnout mainly in terms of emotional exhaustion. Although emotional exhaustion is considered the core component of burnout as it is linked to physiological stress outcomes of the autonomic nervous system ( Kanthak et al., 2017 ), as well as depression ( Hakanen and Schaufeli, 2012 ), future research should investigate whether there are similar associations between DD and other subtypes of burnout. Furthermore, burnout and other measures of work-related well-being should be investigated as possible mediators for the association between type 1 diabetes and general well-being variables, such as depression.
In sum, our analyses suggest that diabetes distress is meaningfully associated with burnout and job satisfaction among employed people with type 1 diabetes, thus providing one of the first pieces of evidence of a link between type 1 diabetes and negative work outcomes and supporting similar findings amongst people with type 2 diabetes. These findings can contribute theory and research on occupational health, diabetes counseling and treatment, and career and health coaching of people with type 1 diabetes.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AC co-wrote the theory section and hypotheses, designed the study, collected the data, analyzed the data, and wrote the first draft of the manuscript and guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses. AZ co-wrote the theory and discussion sections and reviewed and edited the manuscript. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.697833/full#supplementary-material
- ^ Due to the limited capacity of the local Ethics Review Board (ERB), researchers at faculty were asked to provide a description of the study design, as well as the participant information and the consent forms for a preliminary inspection. This pre-review concluded in the statement of the ERB that a full ethics proposal was not necessary.
Abdoli, S., Hessler Jones, D., Vora, A., and Stuckey, H. (2019). Improving diabetes care. Should we reconceptualize diabetes burnout? Diabetes Educator 45, 1–11. doi: 10.1177/0145721719829066
PubMed Abstract | CrossRef Full Text | Google Scholar
Abdoli, S., Miller-Bains, K., Burr, E. M., Smither, B., Vora, A., and Hessler, D. (2020). Burnout, distress, and depressive symptoms in adults with type 1 diabetes. J. Diabetes Complications 34:107608. doi: 10.1016/j.jdiacomp.2020.107608
Ahola, A. J., and Groop, P. (2013). Barriers to self-management of diabetes. Diabetic Med. 30, 413–420. doi: 10.1111/dme.12105
American Diabetes Association [ADA] (2014). Diabetes and employment. Diabetes Care 37, 112–117.
Google Scholar
Amsberg, S., Wredling, R., Lins, P.-E., Adamson, U., and Johansson, U.-B. (2008). The psychometric properties of the Swedish version of the Problem Areas in Diabetes Scale (SwePAID-20): scale development. Int. J. Nurs. Stud. 45, 1319–1328. doi: 10.1016/j.ijnurstu.2007.09.010
Armon, G., Melamed, S., Toker, S., Berliner, S., and Shapira, I. (2014). Joint effect of chronic medical illness and burnout on depressive symptoms among employed adults. Health Psychol. 33, 264–272. doi: 10.1037/a0033712
Bakker, A. B., and Demerouti, E. (2017). Job demands–resources theory: taking stock and looking forward. J. Occupational Health Psychol. 22, 273–285. doi: 10.1037/ocp0000056
Bakker, A. B., Demerouti, E., and Sanz-Vergel, A. I. (2014). Burnout and work engagement: the JDR approach. Annu. Rev. Organ. Psychol. Organ. Behav. 1, 389–411. doi: 10.1146/annurev-orgpsych-031413-091235
CrossRef Full Text | Google Scholar
Balfe, M., Brugha, R., Smith, D., Sreenan, S., Doyle, F., and Conroy, R. (2014). Why do young adults with type 1 diabetes find it difficult to manage diabetes in the workplace? Health Place 26, 180–187. doi: 10.1016/j.healthplace.2013.12.016
Beatty, J. E., and Joffe, R. (2006). An overlooked dimension of diversity: the career effects of chronic illness. Organ. Dynamics 35, 182–195. doi: 10.1016/j.orgdyn.2006.03.006
Brewer, E. W., and Shapard, L. (2004). Employee burnout: a meta-analysis of the relationship between age or years of experience. Hum. Resour. Dev. Rev. 3, 102–123. doi: 10.1177/1534484304263335
Brown, H. S., Pérez, A., Yarnell, L. M., Hanis, C., Fisher-Hoch, S. P., and McCormick, J. (2012). “Diabetes and employment productivity: the effect of duration and management among Mexican Americans ∗ ,” in Aging, Health, and Longevity in the Mexican-Origin Population , eds J. Angel, F. Torres-Gil, and K. Markides (Boston, MA: Springer), 173–181. doi: 10.1007/978-1-4614-1867-2_13
Browne, J. L., Ventura, A. D., Mosely, K., and Speight, J. (2017). Measuring Type 1 diabetes stigma: development and validation of the Type 1 Diabetes Stigma Assessment Scale (DSAS-1). Diabetic Med. 34, 1773–1782.
Chantelau, E., Schiffers, T., Schütze, J., and Hansen, B. (1997). Effect of patient-selected intensive insulin therapy on quality of life. Patient Educ. Counseling 30, 167–173. doi: 10.1016/S0738-3991(96)00964-0
Coccaro, E. F., Lazarus, S., Joseph, J., Wyne, K., Drossos, T., Phillipson, L., et al. (2020). Emotional regulation and diabetes distress in adults with type 1 and type 2 diabetes. Diabetes Care 44, 20–25. doi: 10.2337/dc20-1059
Cosgrove, M. P., Sargeant, L. A., Caleyachetty, R., and Griffin, S. J. (2012). Work-related stress and Type 2 diabetes: systematic review and meta-analysis. Occupational Med. 62, 167–173. doi: 10.1093/occmed/kqs002
De Beer, L. T., Pienaar, J., and Rothmann, S. (2016). Job burnout, work engagement and Self-reported treatment for health conditions in South Africa. Stress Health 32, 36–46. doi: 10.1002/smi.2576
de Jonge, J., Dormann, C., Janssen, P. P. M., Dollard, M. F., Landeweerd, J. A., and Nijhuis, F. J. N. (2001). Testing reciprocal relationships between job characteristics and psychological well-being: a cross-lagged structural equation model. J. Occupat. Organ. Psychol. 74, 29–46. doi: 10.1348/096317901167217
Demerouti, E., Bakker, A. B., Nachreiner, F., and Schaufeli, W. B. (2001). The job demands-resources model of burnout. J. Appl. Psychol. 86, 499–512. doi: 10.1037/0021-9010.86.3.499
El Achhab, Y., Nejjari, C., Chikri, M., and Lyoussi, B. (2008). Disease-specific health-related quality of life instruments among adults diabetic: a systematic review. Diabetes Res. Clin. Practice 80, 171–184. doi: 10.1016/j.diabres.2007.12.020
Faragher, E. B., Cass, M., and Cooper, C. L. (2005). The relationship between job satisfaction and health: a meta-analysis. Occupat. Environ. Med. 62, 105–112. doi: 10.1136/oem.2002.006734
Faul, F., Erdfelder, E., Lang, A.-G., and Buchner, A. (2007). G ∗ Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. doi: 10.3758/BF03193146
Fenwick, E. K., Rees, G., Holmes-truscott, E., Browne, J. L., Pouwer, F., and Speight, J. (2018). What is the best measure for assessing diabetes distress? A comparison of the Problem Areas in Diabetes and Diabetes Distress Scale: results from. J. Health Psychol. 23, 667–680. doi: 10.1177/1359105316642006
Fritschi, C., and Quinn, L. (2010). Fatigue in patients with diabetes: a review. J. Psychosomatic Res. 69, 33–41. doi: 10.1016/j.jpsychores.2010.01.021
Gan, Y., Yang, C., Tong, X., Sun, H., Cong, Y., Yin, X., et al. (2015). Shift work and diabetes mellitus: a meta-analysis of observational studies. Diabetes Care 2, 72–78. doi: 10.1136/oemed-2014-102150
Gendelman, N., Wadwa, R. P., Snell-Bergeon, J. K., Bishop, F., McFann, K., Rewers, M., et al. (2009). Prevalence and correlates of depression in individuals with and without type 1 diabetes. Diabetes Care 32, 575–579. doi: 10.2337/dc08-1835
Goedendorp, M. M., Tack, C. J., Steggink, E., Bloot, L., Bazelmans, E., and Knoop, H. (2014). Chronic fatigue in type 1 diabetes: highly prevalent but not explained by hyperglycaemia or glucose variability. Diabetes Care 37, 73–80. doi: 10.2337/dc13-0515
Graue, M., Haugstvedt, A., Wentzel-larsen, T., Iversen, M. M., Karlsen, B., and Rokne, B. (2012). Diabetes-related emotional distress in adults: Reliability and validity of the Norwegian versions of the Problem Areas in Diabetes Scale (PAID) and the Diabetes Distress Scale (DDS). Int. J. Nursing Stud. 49, 174–182. doi: 10.1016/j.ijnurstu.2011.08.007
Gonzalez, J. S., Fisher, L., and Polonsky, W. H. (2011). Depression in diabetes: have we been missing something important? Diabetes care 34, 236–239. doi: 10.2337/dc10-1970
Hakanen, J. J., and Schaufeli, W. B. (2012). Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J. Affect. Disord. 141, 415–424. doi: 10.1016/j.jad.2012.02.043
Han, T. Y. (2008). A biopsychosocial perspective to the burnout of Korean workers with diabetes. Am. J. Health Behav. 32, 741–753. doi: 10.5555/ajhb.2008.32.6.741
Hobfoll, S. E. (1989). Conservation of resources. A new attempt at conceptualizing stress. Am. Psychol. 44, 513–524.
Hobfoll, S. E., and Freedy, J. (1997). “Conservation of resources: a general stress theory applied to burnout,” in Professional Burnout. Recent Developments in Theory and Research , eds W. B. Schaufeli, C. Maslach, and T. Marek (Milton Park: Taylor & Francis), 115–133.
Jiang, X., Wang, J., Lu, Y., Jiang, H., and Li, M. (2019). Self-efficacy-focused education in persons with diabetes: a systematic review and meta-analysis. Psychol. Res. Behav. Manag. 12, 67–79. doi: 10.2147/PRBM.S192571
Judge, T. A., Heller, D., and Mount, M. K. (2002). Five-factor model of personality and job satisfaction: a meta-analysis. J. Appl. Psychol. 87, 530–541. doi: 10.1037/0021-9010.87.3.530
Judge, T. A., Zhang, S. C., and Glerum, D. R. (2020). “Job satisfaction,” in Essentials of Job Attitudes and Other Workplace Psychological Constructs , eds V. I. Sessa and N. A. Bowling (Milton Park: Routledge), 207–241.
Kalra, S., and Sahay, R. (2018). Diabetes fatigue syndrome. Diabetes Ther. 9, 1421–1429. doi: 10.1007/s13300-018-0453-x
Kanthak, M. K., Stalder, T., Hill, L. K., Thayer, J. F., Penz, M., and Kirschbaum, C. (2017). Autonomic dysregulation in burnout and depression: evidence for the central role of exhaustion. Scandinavian J. Work Environ. Health 43, 475–484. doi: 10.5271/sjweh.3647
Karges, B., Schwandt, A., Heidtmann, B., Kordonouri, O., Binder, E., Schierloh, U., et al. (2017). Association of insulin pump therapy vs insulin injection therapy with severe hypoglycemia, ketoacidosis, and glycemic control among children, adolescents, and young adults with type 1 diabetes. JAMA - J. Am. Med. Assoc. 318, 1358–1366. doi: 10.1001/jama.2017.13994
Kitaoka-Higashiguchi, K., Morikawa, Y., Miura, K., Sakurai, M., Ishizaki, M., Kido, T., et al. (2009). Burnout and risk factors for arteriosclerotic disease: follow-up study. J. Occupat. Health 51, 123–131. doi: 10.1539/joh.L8104
Kristensen, T. S., Borritz, M., Villadsen, E., and Christensen, K. B. (2005). The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress 19, 192–207. doi: 10.1080/02678370500297720
Lee, J., Lee, E., Kim, C., and Hei, S. (2015). Diabetes-related emotional distress instruments: a systematic review of measurement properties. Int. J. Nurs. Stud. 52, 1868–1878. doi: 10.1016/j.ijnurstu.2015.07.004
Lehmann, A. I., Rodgers, S., Calabrese, P., Kamm, C. P., Wyl, V., and Bauer, G. F. (2021). Relationship between Job Demands-Resources and turnover intention in chronic disease – The example of multiple sclerosis. Stress Health [Online ahead of print] doi: 10.1002/smi.3054
Luyckx, K., Seiffge-Krenke, I., Schwartz, S. J., Goossens, L., Weets, I., Hendrieckx, C., et al. (2008). Identity development, coping, and adjustment in emerging adults With a chronic illness: The sample case of type 1 diabetes. J. Adolescent Health 43, 451–458. doi: 10.1016/j.jadohealth.2008.04.005
Maahs, D. M., West, N. A., Lawrence, J. M., and Mayer-Davis, E. J. (2010). Epidemiology of type 1 diabetes. Endocrinol. Metabol. Clin. North Am. 39, 481–497. doi: 10.1016/j.ecl.2010.05.011
Martin, C. E., Renn, B. N., Winderman, K. E., Hundt, N., Petersen, N. J., Naik, A. D., et al. (2018). Classifying diabetes-burden: a factor analysis of the Problem Areas in Diabetes Scale. J. Health Psychol. 23, 882–888. doi: 10.1177/1359105316678667
Maslach, C. (2001). What have we learned about burnout and health? Psychol. Health 16, 607–611. doi: 10.1080/08870440108405530
Maslach, C., and Leiter, M. P. (2017). “Understanding burnout,” in The Handbook of Stress and Health: A Guide to Research and Practice , Vol. 29, eds C. L. Cooper and J. C. Quick (Hoboken, NJ: John Wiley & Sons, Ltd), 36–56. doi: 10.1002/9781118993811.ch3
McGonagle, A. K., Barnes-Farrell, J. L., Grosch, J. W., and Fisher, G. G. (2015). Individual and work factors related to perceived work ability and labor force outcomes. J. Appl. Psychol. 100, 376–398. doi: 10.1037/a0037974
McGonagle, A. K., Beatty, J. E., and Joffe, R. (2014). Coaching for workers with chronic illness: evaluating an intervention. J. Occupat. Health Psychol. 19, 385–398. doi: 10.1037/a0036601
McGonagle, A. K., Schmidt, S., and Speights, S. L. (2020). Work-health management interference for workers with chronic health conditions: Construct development and scale validation. Occupat. Health Sci. 4, 445–470.
McNeish, D. (2018). Thanks coefficient alpha, we’ll take it from here. Psychol. Methods 23, 412–433. doi: 10.1037/met0000144
Nübling, M., Stössel, U., Hasselhorn, H.-M., Michaelis, M., and Hofmann, F. (2006). Measuring psychological stress and strain at work: evaluation of the COPSOQ Questionnaire in Germany. Psycho-Social-Medicine 3, 1–14.
Park, H. I., Jacob, A. C., Wagner, S. H., and Baiden, M. (2014). Job control and burnout: a meta-analytic test of the conservation of resources model. Appl. Psychol. 63, 607–642. doi: 10.1111/apps.12008
Polonsky, W. H., Anderson, B. J., Lohrer, P. A., Welch, G., Jacobson, A. M., Aponte, J. E., et al. (1995). Assessment of diabetes-related distress. Diabetes Care 18, 754–760. doi: 10.2337/diacare.18.6.754
Polonsky, W. H., Fisher, L., Earles, J., Dudl, R. J., Lees, J., Mullan, J., et al. (2005). Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care 28, 626–631. doi: 10.2337/diacare.28.3.626
Purvanova, R. K., and Muros, J. P. (2010). Gender differences in burnout: a meta-analysis. J. Vocational Behav. 77, 168–185. doi: 10.1016/j.jvb.2010.04.006
Pyatak, E. (2011). Participation in occupation and diabetes self-management in emerging adulthood. Am. J. Occupat. Ther. 65, 462–469. doi: 10.5014/ajot.2011.001453
R Development Core Team (2015). R: A Language and Environment for Statistical Computing, Version 3.2.3 Computer Software. Vienna: R Development Core Team.
Rabatin, J., Williams, E., Manwell, L. B., Schwartz, M. D., Brown, R. L., and Linzer, M. (2016). Predictors and outcomes of burnout in primary care physicians. J. Prim. Care Commun. Health 7, 41–43. doi: 10.1177/2150131915607799
Rak, E. C. (2014). Employment outcomes in persons with diabetes: the role of health literacy and diabetes management self-efficacy. Rehabil. Counsel. Bull. 57, 159–169. doi: 10.1177/0034355213500816
Reis, D., Hoppe, A., and Schröder, A. (2015). Reciprocal relationships between resources, work and study engagement, and mental health: evidence for gain cycles. Eur. J. Work Organ. Psychol. 24, 59–75. doi: 10.1080/1359432X.2013.834891
Revelle, W. (2016). USing R and the Psych Package to Find ω. Available online at: http://personality-project.org/r/psych/HowTo/omega.pdf (accessed January 21, 2019).
Revelle, W. (2021). Psych: Procedures for Personality and Psychological Research. Evanston, IL: Northwestern University.
Roessler, R. T., Rumrill, P. D., and Fitzgerald, S. M. (2004). Factors affecting the job satisfaction of employed adults with multiple sclerosis. J. Rehabil. 70, 42–50.
Rosseel, Y. (2012). lavaan: an R package for structural equation modeling. J. Stat. Softw. 48, 1–36.
Rumrill, P., Roessler, R., Vierstra, C., Hennessey, M., and Staples, L. (2004). Workplace barriers and job satisfaction among employed people with multiple sclerosis: an empirical rationale for early intervention. J. Vocational Rehabil. 20, 177–183.
Sav, A., King, M. A., Whitty, J. A., Kendall, E., Mcmillan, S. S., Kelly, F., et al. (2015). Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expectations 18, 312–324. doi: 10.1111/hex.12046
Schaufeli, W. B., and Taris, T. W. (2014). “A critical review of the Job Demands-Resources model: implications for improving work and health,” in Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach , eds G. F. Bauer and O. Hämmig (Berlin: Springer Sicence+Business), 43–68.
Schermelleh-Engel, K., Moosbrugger, H., and Müller, H. (2003). Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 8, 23–74. doi: 10.1002/0470010940
Schmitt, A., Reimer, A., Kulzer, B., Haak, T., Ehrmann, D., and Hermanns, N. (2016). How to assess diabetes distress: comparison of the Problem Areas in Diabetes Scale (PAID) and the Diabetes Distress Scale (DDS). Diabetic Med. 33, 835–843. doi: 10.1111/dme.12887
Siu, A. M. H., Hung, A., Lam, A. Y. L., and Cheng, A. (2013). Work limitations, workplace concerns, and job satisfaction of persons with chronic disease. Work 45, 107–115. doi: 10.3233/WOR-121550
Snoek, F. J., Pouwer, F., Welch, G. W., and Polonsky, W. H. (2000). Diabetes-related emotional distress in Dutch and U.S. diabetic patients: cross-cultural validity of the problem areas in diabetes scale. Diabetes Care 23, 1305–1309. doi: 10.2337/diacare.23.9.1305
Sonnentag, S. (2015). Dynamics of well-being. Ann. Rev. Organ. Psychol. Organ. Behav. 2, 261–293. doi: 10.1146/annurev-orgpsych-032414-111347
Spataro, B. M., Tilstra, S. A., Rubio, D. M., and McNeil, M. A. (2016). The toxicity of self-Blame: sex differences in burnout and coping in internal medicine trainees. J. Women’s Health 25, 1147–1152. doi: 10.1089/jwh.2015.5604
Swider, B. W., and Zimmerman, R. D. (2010). Born to burnout: a meta-analytic path model of personality, job burnout, and work outcomes. J. Vocational Behav. 76, 487–506. doi: 10.1016/j.jvb.2010.01.003
Taris, T. W. (2006). Is there a relationship between burnout and objective performance? A critical review of 16 studies. Work Stress 20, 316–334. doi: 10.1080/02678370601065893
Taris, T. W., Schreurs, P. J. G., and Van Iersel-Van Silfhout, I. J. (2001). Job stress, job strain, and psychological withdrawal among Dutch university staff: towards a dual-process model for the effects of occupational stress. Work Stress 15, 283–296. doi: 10.1080/02678370110084049
Tunceli, K., Bradley, C. J., Nerenz, D., Williams, L. K., Pladevall, M., and Lafata, J. E. (2005). The impact of diabetes on employment and work productivity. Diabetes Care 28, 2662–2667. doi: 10.2337/diacare.28.11.2662
Vijan, S., Hayward, R. A., and Langa, K. M. (2004). The impact of diabetes on workforce participation: results from a national household sample. Health Services Res. 39, 1653–1670. doi: 10.1111/j.1475-6773.2004.00311.x
Vooijs, M., Leensen, M. C. J., Hoving, J. L., Wind, H., and Frings-Dresen, M. H. W. (2015). Interventions to enhance work participation of workers with a chronic disease: a systematic review of reviews. Occupat. Environ. Med. 72, 820–826. doi: 10.1136/oemed-2015-103062
Weijman, I., Ros, W. J. G., Rutten, G. E. H. M., Schaufeli, W. B., Schabracq, M. J., and Winnubst, J. A. M. (2003). Fatigue in employees with diabetes: its relation with work characteristics and diabetes related burden. Occupat. Environ. Med. 60(Suppl. 1), 93–99. doi: 10.1136/oem.60.suppl_1.i93
Wolpin, J., Burke, R. J., and Greenglass, E. R. (1991). Is job satisfaction an antecedent or a consequence of psychological burnout? Hum. Relat. 44, 193–209. doi: 10.1177/001872679104400205
World Health Organization [WHO] (2011). Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus. Geneva: World Health Organization.
Xanthopoulou, D., Bakker, A. B., Demerouti, E., and Schaufeli, W. B. (2009). Reciprocal relationships between job resources, personal resources, and work engagement. J. Vocat. Behav. 74, 235–244. doi: 10.1016/j.jvb.2008.11.003
Keywords : diabetes mellitus, burnout, job satisfaction, distress, chronic illness
Citation: Cook A and Zill A (2021) Working With Type 1 Diabetes: Investigating the Associations Between Diabetes-Related Distress, Burnout, and Job Satisfaction. Front. Psychol. 12:697833. doi: 10.3389/fpsyg.2021.697833
Received: 20 April 2021; Accepted: 18 October 2021; Published: 04 November 2021.
Reviewed by:
Copyright © 2021 Cook and Zill. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra (Sasha) Cook, [email protected] ; Alexander Zill, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Diabetes distress and diabetes burnout explored in various areas of life in patients with type 1 diabetes: effect of short-term psychological intervention
- Original Article
- Published: 06 March 2024
Cite this article
- Katarzyna Cyranka ORCID: orcid.org/0000-0002-0897-9394 1 , 2 , 3 ,
- Tomasz Klupa 2 , 3 ,
- Maciej Pilecki 1 , 3 ,
- Dominika Sarna-Palacz 3 ,
- Andrzej Juryk 1 , 3 ,
- Dawid Storman 3 , 4 ,
- Dominika Dudek 1 , 3 ,
- Maciej T. Malecki 3 nAff5 &
- Bartłomiej Matejko 2 , 3
32 Accesses
Explore all metrics
Introduction
Diabetes distress (DD) and diabetes burnout (DB) are recognized psychological phenomena in patients with T1DM (type 1 diabetes mellitus). Still, there is an urgent need to create professional psychological intervention procedures to provide patients with adequate care.
The aim of the study was to assess the level of DD and DB in T1DM patients at baseline and after 5 of sessions psychological intervention in the group of participants who applied for help.
34 T1DM patients who requested psychological support (22 females, 12 males) and 30 patients in a control group (14 females, 16 males) participated in the study. At baseline clinical test results between groups were compared. Next, in the studied group measurements were repeated after a set of five psychological face-to-face individual interventions which lasted 30–60 min each. They were support sessions with elements of cognitive-behavioral interventions done by clinical psychologists. Session 1: introduction, interview and collection of test results; session 2–4: work on the indicated by the patient and test results most problematic aspect of diabetes, session 5: a summary and plan for further treatment if needed. The control group results were obtained only at baseline. Research tools: DDS; PAID, Diabetes Burnout test by Polonsky.
At the baseline, significant differences were observed between the studied group and control group: in DB/DD levels: DB (3.9 ± 1.7 vs 2.4 ± 1.6; p < 0.001); DDS (3.2 ± 1.0 vs 2.7 ± 1.0; p = 0.064); PAID (62.3 ± 14.1vs 34.4 ± 21.0; p < 0.001). There were also group differences in HbA1c levels (8.7 ± 2.4 vs 7.3 ± 1.5; p = 0.028). After psychological interventions, there was a significant improvement in DB (3.9 ± 1.7vs 2.9 ± 1.2; p < 0.001; DDS (3.2 ± 1 vs 3.0 ± 0.7; p = 0.03); PAID (62.3 ± 14.1 vs 51.8 ± 12.5; p < 0.001).
Conclusions
DD and DB constitute a significant problem in the group of T1DM patients, but providing appropriate specialist care may help them accept diabetes and improve life satisfaction, as well as regain control over their diabetes management.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

The Value of Measuring Diabetes Burnout
Samereh Abdoli, Danielle Hessler, … Heather Stuckey

Diabetes burnout among emerging adults with type 1 diabetes: a mixed methods investigation
Vicki S. Helgeson

Prevalence and predictors of diabetes-related distress in adults with type 1 diabetes
Natasa Grulovic, Martina Rojnic Kuzman & Maja Baretic
Data availability
The data that support the findings of this study are available on request from the corresponding author K.C.
T.C. Skinner, L. Joensen, T. Parkin, Twenty-five years of diabetes distress research. Diabet. Med. 37 (3), 393–400 (2020). https://doi.org/10.1111/dme.14157
Article CAS PubMed Google Scholar
F. Snoek, Mental health in diabetes care. Time to step up. Front. Clin. Diabetes Healthc., 13 , https://doi.org/10.3389/fcdhc.2022.1039192
K. Dennick, J. Sturt, J. Speight, What is diabetes distress and how can we measure it? A narrative review and conceptual model. J. Diabetes Complic. 31 (5), 898–911 (2017). https://doi.org/10.1016/j.jdiacomp.2016.12.018
Article Google Scholar
W.H. Polonsky, L. Fisher, J. Earles, R.J. Dudl, J. Lees, J. Mullan, R.A. Jackson, Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care 28 (3), 626–631 (2005). https://doi.org/10.2337/diacare.28.3.626
Article PubMed Google Scholar
S. Abdoli, D. Hessler, B. Smither, K. Miller-Bains, E.M. Burr, H.L. Stuckey, New insights into diabetes burnout and its distinction from diabetes distress and depressive symptoms: a qualitative study. Diabetes Res Clin. Pract. 169 , 108446 (2020). https://doi.org/10.1016/j.diabres.2020.108446
K. Kontoangelos, A. Raptis, V. Lambadiari, M. Economou, S. Tsiori, V. Katsi, C. Papageorgiou, S. Martinaki, G. Dimitriadis, C. Papageorgiou, Burnout related to diabetes mellitus: a critical analysis. Clin. Pract. Epidemiol. Ment. Health 18 , e174501792209010 (2022). https://doi.org/10.2174/17450179-v18-e2209010
Article PubMed PubMed Central Google Scholar
American Diabetes Association Professional Practice Committee, B. Draznin, A. VR, G. Bakris, G. Benson, B. FM et al. Facilitating behavior change and well-being to improve health outcomes: Standards of medical care in diabetes-2022. Diabetes Care 45 (Suppl 1), S60–S82 (2022). https://doi.org/10.2337/dc22-S005
E.H. Lee, Y.W. Lee, K.W. Lee et al. Measurement of diabetes-related emotional distress using the Problem Areas in Diabetes scale: psychometric evaluations show that the short form is better than the full form. Health Qual. Life Outcomes 12 , 142 (2014). https://doi.org/10.1186/s12955-014-0142-z
G.W. Welch, A.M. Jacobson, W.H. Polonsky, The problem areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care 20 (5), 760–766 (1997). https://doi.org/10.2337/diacare.20.5.760 . MayPMID: 9135939
S. Krzemińska, E. Bąk, Psychometric properties of the Polish Version of the Diabetes Distress Scale (DDS). Psychol. Res Behav. Manag. 14 , 1149–1156 (2021). https://doi.org/10.2147/PRBM.S320675
Novo Nordisk 2006. Adapted from DAWN Interactive 2. Text by Frank Snoek and Garry Welch
Diabetes burnout: what to do when you can’t take it anymore, William Polonsky, American Diabetes Association, 1999, ISBN 1580403905, 9781580403900
K. Cyranka, D. Dudek, M.T. Małecki, B. Matejko, T. Klupa, Psychological crisis intervention for COVID-19 lockdown stress in patients with type 1 diabetes mellitus: survey study and qualitative analysis. JMIR Ment. Health 8 (6), e28097 (2021). https://doi.org/10.2196/28097
K. Cyranka, B. Matejko, A. Chrobak, D. Dudek, B. Kieć-Wilk, K. Cyganek, P. Witek, M. Lushchyk, S. Krzyżowska, M.T. Małecki, T. Klupa, Assessment of the spectrum of depression and bipolarity in patients with type 1 diabetes. Diabetes Metab. Res. Rev. 21 , e3583 (2022). https://doi.org/10.1002/dmrr.3583
Article CAS Google Scholar
V. Hagger, C. Hendrieckx, F. Cameron, F. Pouwer, T.C. Skinner, J. Speight, Diabetes distress is more strongly associated with HbA1c than depressive symptoms in adolescents with type 1 diabetes: results from Diabetes MILES Youth-Australia. Pediatr. Diabetes 19 (4), 840–847 (2018). https://doi.org/10.1111/pedi.12641
A.M. Friis, M.H. Johnson, R.G. Cutfield, N.S. Consedine, Does kindness matter? Self-compassion buffers the negative impact of diabetes-distress on HbA1c. Diabet. Med 32 (12), 1634–1640 (2015). https://doi.org/10.1111/dme.12774
A. Fayed, F. AlRadini, R.M. Alzuhairi, A.E. Aljuhani, H.R. Alrashid, M.M. Alwazae, N.R. Alghamdi, Relation between diabetes related distress and glycemic control: The mediating effect of adherence to treatment. Prim. Care Diabetes 16 (2), 293–300 (2022). https://doi.org/10.1016/j.pcd.2021.12.004
L. Lašaitė, R. Dobrovolskienė, E. Danytė, I. Stankutė, D. Ražanskaitė-Virbickienė, V. Schwitzgebel, D. Marčiulionytė, R. Verkauskienė, Diabetes distress in males and females with type 1 diabetes in adolescence and emerging adulthood. J. Diabetes Complic. 30 (8), 1500–1505 (2016). https://doi.org/10.1016/j.jdiacomp.2016.08.013
I. Nishio, M. Chujo, Self-stigma of patients with type 1 diabetes and their coping strategies. Yonago Acta Med. 60 (3), 167–173 (2017)
Y.M. Jeong, L. Quinn, N. Kim, P. Martyn-Nemeth, Health-related stigma in young adults with type 1 diabetes mellitus. J. Psychosoc. Nurs. Ment. Health Serv. 56 (10), 44–51 (2018). https://doi.org/10.3928/02793695-20180503-01
J. Fuchs, R. Hovorka, Closed-loop control in insulin pumps for type-1 diabetes mellitus: safety and efficacy. Expert Rev. Med. Devices 17 (7), 707–720 (2020)
Article CAS PubMed PubMed Central Google Scholar
A. Janez, T. Battelino, T. Klupa, G. Kocsis, M. Kuricová, N. Lalić, A.P. Stoian, M. Prázný, D. Rahelić, J. Šoupal, T. Tankova, N. Zelinska, Hybrid closed-loop systems for the treatment of type 1 diabetes: a collaborative, expert group position statement for clinical use in Central and Eastern Europe. Diabetes Ther. 12 (12), 3107–3135 (2021)
B. Matejko, A. Juza, B. Kieć-Wilk, K. Cyranka, S. Krzyżowska, X. Chen, O. Cohen, J. Da Silva, M.T. Malecki, T. Klupa, Transitioning of people with type 1 diabetes from multiple daily injections and self-monitoring of blood glucose directly to minimed 780g advanced hybrid closed-loop system: a two-center, randomized, controlled study. Diabetes Care 45 (11), 2628–2635 (2022). https://doi.org/10.2337/dc22-0470
V. Serrano, L. Larrea-Mantilla, R. Rodríguez-Gutiérrez, G. Spencer-Bonilla, G. Málaga, I. Hargraves, V.M. Montori, Shared decision making in patients with diabetes mellitus. Rev. Med Chil. 145 (5), 641–649 (2017). https://doi.org/10.4067/S0034-98872017000500012
N. Hermanns, D. Ehrmann, A. Shapira, B. Kulzer, A. Schmitt, L. Laffel, Coordination of glucose monitoring, self-care behaviour and mental health: achieving precision monitoring in diabetes. Diabetologia. 2022. https://doi.org/10.1007/s00125-022-05685-7
V. Serrano, R. Rodriguez-Gutierrez, I. Hargraves, M.R. Gionfriddo, S. Tamhane, V.M. Montori, Shared decision-making in the care of individuals with diabetes. Diabet. Med 33 (6), 742–751 (2016). https://doi.org/10.1111/dme.13143
S. Tamhane, R. Rodriguez-Gutierrez, I. Hargraves, V.M. Montori, Shared decision-making in diabetes care. Curr. Diabetes Rep. 15 (12), 112 (2015). https://doi.org/10.1007/s11892-015-0688-0
J. Carretero-Gómez, J.C. Arévalo-Lorido, The meaning of words in diabetes. Language matters. Rev. Clin. Esp. 222 (8), 502–503 (2022). https://doi.org/10.1016/j.rceng.2022.07.003
N. Kuniss, U.A. Müller, C. Kloos, G. Wolf, G. Kramer, Reduction of HbA1c and diabetes-related distress after intervention in a diabetes day care clinic in people with type 2 diabetes but not with type 1 diabetes. Exp. Clin. Endocrinol. Diabetes 126 (4), 242–248 (2018). https://doi.org/10.1055/s-0043-112862
V.S. Helgeson, Diabetes burnout among emerging adults with type 1 diabetes: a mixed methods investigation. J. Behav. Med. 44 (3), 368–378 (2021). https://doi.org/10.1007/s10865-020-00198-3
E. Berry, S. Lockhart, M. Davies, J.R. Lindsay, M. Dempster, Diabetes distress: understanding the hidden struggles of living with diabetes and exploring intervention strategies. Postgrad. Med. J. 91 (1075), 278–283 (2015). https://doi.org/10.1136/postgradmedj-2014-133017
J.S. Gonzalez, M.L. Tanenbaum, P.V. Commissariat, Psychosocial factors in medication adherence and diabetes self-management: Implications for research and practice. Am. Psychol. 71 (7), 539–551 (2016). https://doi.org/10.1037/a0040388
K. Winkley, R. Upsher, D. Stahl, D. Pollard, A. Kasera, A. Brennan, S. Heller, K. Ismail, Psychological interventions to improve self-management of type 1 and type 2 diabetes: a systematic review. Health Technol. Assess. 24 (28), 1–232 (2020). https://doi.org/10.3310/hta24280
P. Khashayar, N. Shirzad, A. Zarbini, A. Esteghamati, M. Hemmatabadi, E. Sharafi, Diabetes-related distress and its association with the complications of diabetes in Iran. J. Diabetes Metab. Disord. 21 (2), 1569–1575 (2022). https://doi.org/10.1007/s40200-022-01103-2
A. Stahl-Pehe, C. Bächle, K. Bódis, O.P. Zaharia, K. Lange, R.W. Holl, M. Roden, J. Rosenbauer; GDS Group, Comparison of diabetes distress and depression screening results of emerging adults with type 1 diabetes onset at different ages: findings from the German early-onset T1D study and the German Diabetes Study (GDS). Diabetol. Metab. Syndr. 15 (1), 24 (2023). https://doi.org/10.1186/s13098-023-00994-2
Download references
Jagiellonian University Medical College grant no N41/DBS/000642.
Author information
Maciej T. Malecki
Present address: Department of Metabolic Diseases, Jagiellonian University Medical College, Krakow, Poland

Authors and Affiliations
Department of Psychiatry, Jagiellonian University Medical College, Kraków, Poland
Katarzyna Cyranka, Maciej Pilecki, Andrzej Juryk & Dominika Dudek
Department of Metabolic Diseases, Jagiellonian University Medical College, Krakow, Poland
Katarzyna Cyranka, Tomasz Klupa & Bartłomiej Matejko
University Hospital in Krakow, Kraków, Poland
Katarzyna Cyranka, Tomasz Klupa, Maciej Pilecki, Dominika Sarna-Palacz, Andrzej Juryk, Dawid Storman, Dominika Dudek, Maciej T. Malecki & Bartłomiej Matejko
Chair of Epidemiology and Preventive Medicine, Department of Hygiene and Dietetics, Jagiellonian University Medical College, Kraków, Polska
Dawid Storman
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Katarzyna Cyranka .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Ethical approval
The study received Jagiellonian University Medical College No. 1072.6120.78.202. Participants gave their informed consent to participate and consent to publish the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cyranka, K., Klupa, T., Pilecki, M. et al. Diabetes distress and diabetes burnout explored in various areas of life in patients with type 1 diabetes: effect of short-term psychological intervention. Endocrine (2024). https://doi.org/10.1007/s12020-024-03760-0
Download citation
Received : 20 November 2023
Accepted : 24 February 2024
Published : 06 March 2024
DOI : https://doi.org/10.1007/s12020-024-03760-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 1 diabetes mellitus
- Diabetes distress
- Diabetes burnout
- Psychological intervention
- Find a journal
- Publish with us
- Track your research
- News in brief
- Diabetes views
- Advocating for diabetes
- Caring for diabetes
- Living with diabetes
- Diabetes profiles
Search your topic
- Submit an article
- Middle East and North Africa
- North America and Caribbean
- South and Central America
- South-East Asia
- Western Pacific
Global perspectives on diabetes

- Visual storytelling
Diabetes burnout: a common but neglected impact of diabetes
Research conducted by t1international finds that people living with diabetes are experiencing diabetes burnout at a very high rate, with a significant impact on their health and wellbeing., share this:.
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)

Credit: T1International and Erin Lubin
In June, T1International shared a blog post outlining the phenomenon of diabetes burnout , which is the loss of strength or motivation, usually as a result of prolonged stress in regards to diabetes management and care. At the end of this post, our team included a questionnaire for people with diabetes to address burnout effects and what factors contribute to this feeling. While circumstances and realities vary for all individuals, some notable patterns emerged that everyone in our community should be aware of and concerned about.
While we were enthused by the number of participants and support, the results of the survey painted a picture of a diabetes community faced with prolific burnout that many are confronting alone. In this article, we take a look at what the data means for people facing a condition that is ever present and in the forefront of mind of a person living with diabetes.
Of the 107 people who took the questionnaire, over 74% have lived with diabetes for more than 10 years. This means that the majority of participants have been managing their condition for a significant portion of their lives.
Overall, people with diabetes are experiencing burnout at a very high rate, with over half (55%) of respondents reporting they experience burnout much or all of the time. One in seven (14%) of these consider diabetes burnout as an ongoing condition that is always present in their life.
I feel overwhelmed while taking care of diabetes tasks and remember (even though I’ve had this half of my life) that I’ll have to do this forever. I push through. But it can be exhausting. I wish we got a break sometimes!
This feeling of burnout has a clear and definite impact on the lives of people with diabetes. Over half of respondents (57%) reported a strong or overwhelming impact that takes the form of lack of sleep, feelings of depression and anxiety and neglect of blood glucose management. When sharing their experience, people noted feelings such as anger and lethargy in the face of constant stress.
Those who took the questionnaire were given free space to express their thoughts or feelings on the topic, and noted that their stress presents in different ways. Many experience stress related to their supplies, adequacy of access and insurance coverage. Others experienced poor eating habits and lapses in care as a result of their burnout. A common issue reported is the continuous presence of a condition that utterly drains their energy.
Despite this, a staggering number of people with diabetes (62% of participants) are not seeking any support from friends, family or mental health professionals. Furthermore, less than a quarter (24%) claimed they feel comfortable talking with their own doctor about this burnout. Many sacrifice seeking help from professionals at the cost of mental health. We would venture to assume that those who feel unsupported by their community have a higher chance of poor management compared to those who have a strong support system.
It’s a daily routine. When the constant lows and highs hit due to something I ate or did or didn’t even do in my daily life, it can get hard to handle. I always get past it and start a new day, but it’s not easy to deal with the mental strain of feeling a sense of failure and how that may affect me later down the line with diabetes complications.
In reviewing the information and statements provided freely by survey participants, diabetes burnout leads people with diabetes to feelings of anxiety, depression and frustration. For many, the persistent management and attention that the condition requires leads to feelings and stress that manifest in other areas of their lives.
Burnout appears very common among people with diabetes. Most of the time it remains unaddressed or untreated by healthcare professionals. In seeking solutions, a sizable number of participants (44%), reported that online communities such as T1International are helpful in terms of support for diabetes care and burnout.
It is notable and concerning that online spaces are filling gaps that healthcare systems across the world should be addressing. While inadequate access to insulin and supplies is a major cause of diabetes burnout, the survey shows that regardless of access, burnout is experienced by almost all respondents (97.1%) at some point in their life.
It becomes harder to make good decisions regarding my diabetes management because it feels overwhelming. I often also eat more, meaning more dosing/adjustment is needed. I do take care of myself, but it’s not the best care and my fatigue towards this situation bleeds over into other aspects of my daily life, especially as it pertains to mood. It is just harder for me to do things, broadly speaking.
In the future, healthcare professionals and institutions should consider the impacts chronic conditions have on other elements of the lives of people with diabetes and their ability to manage these conditions in the long term. People living with diabetes understand all too well that healthcare professionals, who do not have to contend with the condition on a daily basis, can never fully grasp how challenging it is to live with it. It is therefore important that governments and institutions around the world prioritize and dedicate more resources for mental health support for people with diabetes.
Elizabeth Pfiester and Katherine Souris contributed to this article.
Elizabeth is founder and executive director of T1International. She has lived with type 1 diabetes for over 30 years.
Katherine is a consultant with T1International. She has lived with type 1 diabetes for 17 years.

Konstantina Taki is a medical doctor and a Digital Advocate volunteer with T1International, a non-profit advocacy organisation representing people with diabetes around the world. She has lived with type 1 diabetes for 14 years. Ian Devaney is the Communications Coordinator at T1International. He has lived with type 1 diabetes for 3 years.
You may also find these interesting
No related posts.
Do you have something to say?
Your thoughts and opinions matter to us., be the first to comment.
Diabetes burnout among emerging adults with type 1 diabetes: a mixed methods investigation
Affiliation.
- 1 Psychology Department, Carnegie Mellon University, Pittsburgh, PA, 15213, USA. [email protected].
- PMID: 33566266
- DOI: 10.1007/s10865-020-00198-3
Feeling overwhelmed, exhausted, and frustrated by the daily demands of diabetes management has been referred to as diabetes burnout. The goal of the study was to develop a measure of diabetes burnout and to link this measure to psychological health and diabetes outcomes. Emerging adults with type 1 diabetes (n = 88, average age 27) completed an online questionnaire and an HbA1c assessment; a subset was interviewed by phone to obtain a more in-depth understanding of burnout. Exploratory factor analysis revealed three burnout domains: exhaustion, detachment, and powerlessness. Burnout was related to higher psychological distress, higher diabetes distress, and poorer diabetes outcomes. Burnout independently predicted higher HbA1c, independent of diabetes distress. Qualitative interviews revealed that participants defined burnout in terms of exhaustion and powerlessness and resolved burnout by acceptance and utilization of social resources. Prevention and intervention efforts might target resilience as a way to mitigate burnout.
Keywords: Burnout; HbA1c; Psychological distress; Type 1 diabetes.
Publication types
- Research Support, N.I.H., Extramural
- Burnout, Professional*
- Burnout, Psychological
- Diabetes Mellitus, Type 1* / complications
- Mental Health
- Surveys and Questionnaires
Grants and funding
- R01 DK060586/DK/NIDDK NIH HHS/United States
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Personal and Work-Related Burnout Is Associated with Elevated Diastolic Blood Pressure and Diastolic Hypertension among Working Adults in Chile
Yinxian chen.
1 Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA 02115, USA
Diana Juvinao-Quintero
Juan carlos velez.
2 Departamento de Rehabilitación, Hospital del Trabajador, Asociación Chilena de Seguridad, Santiago 8320000, Chile
Sebastian Muñoz
Jessica castillo, bizu gelaye.
3 Department of Psychiatry, Harvard Medical School, Boston, MA 02115, USA
4 The Chester M. Pierce, MD Division of Global Psychiatry, Massachusetts General Hospital, Boston, MA 02114, USA
Associated Data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
We aimed at investigating the association of personal and work-related burnout with blood pressure and hypertension among working adults in Chile. We conducted a cross-sectional study among 1872 working adults attending the Hospital del Trabajador in Santiago, Chile, between September 2015 and February 2018. The Copenhagen Burnout Inventory was used to assess personal and work-related burnout. Blood pressure was measured by medical practitioners. Multivariable linear and logistic regressions were used to estimate the association of burnout status with systolic blood pressure (SBP), diastolic blood pressure (DBP), and hypertension. After adjusting for confounders, participants with both types of burnout had a 1.66 (95% confidence interval [CI]: 0.02–3.30) mmHg higher mean DBP than those without burnout. The odds of isolated diastolic hypertension among the participants with only personal burnout and both types of burnout were 2.00-fold (odds ratio [OR] = 2.00; 95% CI: 1.21–3.31) and 2.08-fold (OR = 2.08; 95% CI: 1.15–3.78) higher than those without burnout. The odds of combined systolic/diastolic hypertension among the participants with only work-related burnout increased by 59% (OR = 1.59; 95% CI: 1.01–2.50) compared with those without burnout. Both work-related and personal burnouts were associated with increased DBP and odds of diastolic hypertension among working adults in Chile.
1. Introduction
Burnout is a state resulting from individuals being exposed to prolonged psychosocial stress [ 1 ] and presenting core features such as physical and psychological fatigue and exhaustion [ 2 ]. Although previous studies have mainly been applied in describing the status of working adults under exposure to working stress, burnout can be due to other attributes in the personal life of working adults, such as health problems and family demands.
Hypertension is a leading modifiable cause of premature mortality and a significant contributor to the global burden of cardiovascular disease (CVD) [ 3 ], contributing to 26.4% of all causes of death [ 4 ]. According to the Chilean National Health Survey, 30.8% of Chileans had hypertension in 2017, with men (31.2%) having a slightly higher prevalence than women (30.3%) [ 5 ]. For young and middle-aged adults (<60 years), isolated diastolic hypertension (IDH: SBP < 140 mmHg and DBP ≥ 90 mmHg) is more prevalent than isolated systolic hypertension (ISH: SBP ≥ 140 mmHg and DBP < 90 mmHg) [ 6 ]. Among them, elevated DBP mainly contributes to the risk of CVD [ 7 ]. In contrast, older adults (≥60 years) are more likely to have combined systolic/diastolic hypertension (SDH: SBP ≥ 140 mmHg and DBP ≥ 90 mmHg) and isolated systolic hypertension (ISH: SBP ≥ 140 mmHg and DBP < 90 mmHg) [ 6 ]. In this case, increased SBP replaces DBP as the predominant predictor of CVD [ 7 ]. Given that hypertension is highly prevalent in Chile, it is warranted to explore populations susceptible to hypertension to decrease the burden of CVD in Chile.
Burnout has shown strong potential as a target for hypertension prevention. Previous studies have indicated that burnout is associated with multiple health consequences, ranging from health behaviors (smoking [ 8 ], alcohol consumption [ 8 ], and substance abuse [ 8 ]), psychiatric disorders [ 9 , 10 ], and insomnia [ 9 ] to physical disorders (type 2 diabetes [ 9 ] and hypercholesterolemia [ 9 ]) that are well-established risk factors for hypertension [ 11 , 12 ]. However, the current evidence of burnout with hypertension among working adults is inconclusive. More studies have shown that burnout is associated [ 13 , 14 , 15 , 16 , 17 , 18 ] with higher odds or a higher proportion of hypertension than those showing no association [ 19 , 20 , 21 ]. The association between burnout and blood pressure is also heterogeneous, going from no association with SBP and DBP [ 22 ] to being associated with SBP/DBP [ 23 ] or with mean arterial pressure (MAP) [ 24 ]. The current evidence is also narrow in terms of the attributes of burnout, with only one study assessing generic burnout [ 17 ], while others have only focused on work-related burnout. Nearly all the evidence has been derived from the human service sectors, with only one exception focusing on mine workers [ 20 ]. The quality of the current evidence is also problematic, as some studies did not take into account the presence of confounding variables under their observational study design [ 13 , 14 , 16 , 20 , 25 , 26 ].
Given the gap described above, a study that systematically assesses the association between burnout and hypertension among working adults is necessary to provide new evidence and promote additional health strategies for addressing the cardiometabolic consequences of high burnout among working adults. Thus, we conducted a cross-sectional study in an ongoing cohort, recruiting working adults in Santiago, Chile, to examine the association of burnout with blood pressure and the occurrence of hypertension.
2. Materials and Methods
2.1. study population.
The present cross-sectional study drew participants from the Stress, Pain, Sleep, and Neuropsychiatric Disorders (SPLENDID) study conducted in a workers’ compensation hospital system in Chile. Details about the SPLENDID study, including the study procedures, have been previously described [ 27 ]. Briefly, the SPLENDID study aimed to examine the prevalence and correlations of pain, work-related stress, and neuropsychiatric outcomes among working adults in Chile with the goal of developing workplace wellness programs. Between September 2015 and February 2018, we collected data among patients attending the Hospital del Trabajador in Santiago, Chile. The Hospital del Trabajador is the largest workers’ compensation hospital and the referral center for trauma and professional diseases of the Asociación Chilena de Seguridad, with approximately 2.5 million affiliated workers. Individuals were eligible if they were working adults attending the hospital for the following types of injuries: burns, bone fractures, spinal cord and mild brain injury, and soft tissue injuries of various etiologies. All participants provided written informed consent prior to participation. All procedures in this study were approved by the institutional review boards of the Hospital del Trabajador, Santiago, Chile, and the Office of Human Research Administration, Harvard T.H. Chan School of Public Health, Boston, MA, USA.
2.2. Exposure
While the Maslach Burnout Inventory (MBI) [ 2 ] is the most widely used tool for assessing burnout, the personal attributes of burnout outside the work setting are not captured in it. Therefore, we chose the Copenhagen Burnout Inventory (CBI), a 19-item scale measuring burnout in 3 domains: personal burnout (6 items), work-related burnout (7 items), and client-related burnout (6 items) [ 28 ]. The CBI has been shown to have good reliability and validity among the Spanish-speaking population [ 29 , 30 ]. Since the present study was conducted among the general working population, the client domain was not included due to its inapplicability in non-human-service sectors.
The personal burnout scale included six items. The responses for each item were given on a five-point Likert scale, ranging from 0 to 4, which corresponded to never/almost never, seldom, sometimes, often, and always. The responses were then transformed into scores of 0, 25, 50, 75, and 100, consistent with the original questionnaire. The score for personal burnout was the average score of 6 items and ranged from 0 to 100. We defined scores of ≥50 as having personal burnout [ 31 , 32 ]. The work-related burnout subscale contained seven items. The responses for each item were given on a five-point Likert scale: very-high degree, high degree, somewhat, low degree, and very-low degree. Similar to personal burnout, the responses were transformed into scores of 0, 25, 50, 75, and 100. The total score for work-related burnout was the average score of the 7 items and ranged from 0 to 100. We defined scores of ≥50 as having work-related burnout [ 31 , 32 ]. To examine the independent and joint effects of the two burnout domains, we categorized participants into four groups: (1) no burnout (both subscales < 50); (2) only personal burnout (only personal subscale ≥ 50); (3) only work-related burnout (only work-related subscale ≥ 50); and (4) both burnouts (both subscales ≥ 50).
2.3. Outcome
After participants completed the structured interviews, their blood pressure was measured. Two additional blood pressure measurements were taken with 3 min elapsing between successive measurements. Following the World Health Organization’s recommendation, the mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) from the second and third measurements were analyzed. Hypertension was defined as mean SBP ≥ 140 mmHg or mean DBP ≥ 90 mmHg based on the Seventh Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure (the JNC 7) [ 33 ]. Subtypes of hypertension [ 34 ], including isolated diastolic hypertension (IDH: SBP < 140 mmHg and DBP ≥ 90 mmHg), isolated systolic hypertension (ISH: SBP ≥ 140 mmHg and DBP < 90 mmHg), and combined systolic/diastolic hypertension (SDH: SBP ≥ 140 mmHg and DBP ≥ 90 mmHg), were used as the outcomes for the secondary analysis.
2.4. Covariates
We used structured questionnaires to collect participants’ sociodemographic and behavioral characteristics. Sociodemographic characteristics included sex (men vs. women), age when interviewing (continuous and <60 years vs. ≥60 years), country (Chile vs. other), and highest education level (elementary school, high school, and college or technical training). Behavioral characteristics included body mass index (BMI) (<18.5 kg/m 2 , 18.5–24.9 kg/m 2 , 25–29.9 kg/m 2 , and ≥30 kg/m 2 ), smoking status (non-smoker, past smoker, and current smoker), alcohol consumption (never, five days/week, and ≥5 days/week), and physical activity, which was assessed by a Global Physical Activity Questionnaire (GPAQ), where participants having a Metabolic Equivalent (MET) ≥ 600 min per week were considered physically active [ 35 ] (inactive vs. active). We also measured participants’ occupational characteristics, including their work sector (construction, commercial, finance, public services, manufacturing, transportation, and others), work type (administrative, professional, manual worker, salesperson, teacher, technician, and others), and work shift (7 a.m.–7 p.m., 2 p.m.–12 a.m., and 11 p.m.–8 a.m.). All covariates were considered potential confounders in this study based on the previous evidence showing that they were associated with objective exposure (burnout) and outcome (blood pressure and hypertension).
2.5. Statistical Analysis
We interviewed a total of 2000 participants. Of these, based on the complete case analysis (CCA), sixty-six participants were excluded due to missing data on blood pressure, seven were excluded due to missing data on the CBI, and seventy-five were excluded due to missing data on relevant covariates. We included a total of 1872 participants in the final study.
We first explored the frequency distributions of participants’ sociodemographic, behavioral, and occupational characteristics. We summarized the data using numbers and percentages (%) for the categorical variables and reported group-specific means and standard deviations (SD) for the continuous variables. We used the Chi-square test or Fisher’s exact test for the categorical variables and ANOVA (normally distributed and homogeneous variance) or the Kruskal–Wallis test (non-normally distributed or heterogeneous variance) for the continuous variables to determine bivariate differences. We considered confounding variables a priori based on their hypothesized relationship with burnout and elevated BP. The covariates of interest were sex, age, country, highest education level, BMI, physical activity, work sector, work type, and work shift. For the primary analysis, we used multivariable least squares linear regression procedures to assess the association of burnout status with mean SBP and DBP before and after accounting for prior-selected putative confounders, reporting crude and adjusted coefficients (βs), 95% confidence intervals (CIs), and the p -value (P). We completed analyses for each outcome separately. In addition, we used logistic regression procedures to estimate the odds ratios (ORs) and 95% Cis of hypertension in relation to burnout status. Given the qualitative differences in the endorsement of personal burnout by sex [ 32 , 36 ], we repeated the same procedures in the primary analyses, stratifying by sex, and estimating the sex-specific βs, ORs, and 95% CIs. We also used polytomous logistic regression to estimate the ORs and 95% CIs of the association of burnout status with subtypes of hypertension (IDH vs. normal, ISH vs. normal, and SDH vs. normal). Two-side p < 0.05 was considered statistically significant. All analyses were performed using R version 4.1.2.
Table 1 shows the characteristics of the study participants ( n = 1872). The mean age (SD) of the participants was 45.8 (13.7), and most of them were men (73.7%), born in Chile (93.9%), and had at least a high school education (56.0%). About two-thirds of participants reported lifetime smoking (30.3% for past smokers and 30.6% for current smokers), while 5.5% reported alcohol consumption nearly every day.
Characteristics of working adults in Santiago, Chile, by burnout status ( n = 1872).
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; IDH, isolated diastolic hypertension; ISH, isolated systolic hypertension; SBP, systolic blood pressure; SD, standard deviation; SDH, combined systolic/diastolic hypertension. a p value was calculated by chi-square test or Fisher’s exact test for categorical variables, and ANOVA or Kruskal–Wallis test for continuous variables. b Included agriculture, education, security, cleaning services, administration, food service, automotive, mining, retired, gardener, electrical engineer, and maintenance. c Included chauffeur, conductors, concierge, security guard, food service, landlord, food distribution, telecommunication, machine operator, and cleaning services. d Hypertension was defined as mean SBP ≥ 140 mmHg or mean DBP ≥ 90 mmHg. e Isolated diastolic hypertension was defined as mean SBP < 140 mmHg and mean DBP ≥ 90 mmHg. f Isolated systolic hypertension was defined as mean SBP ≥ 140 mmHg and mean DBP < 90 mmHg. g Systolic/diastolic hypertension was defined as mean SBP ≥ 140 mmHg and mean DBP ≥ 90 mmHg.
The prevalence of hypertension was 27.2% (7.2% for IDH, 9.2% for ISH, and 10.8% for SDH). Table 1 also shows the participants’ characteristics by burnout. Those without burnout were more likely to be younger men working in construction, commercial, or professional sectors. They were more likely to report alcohol consumption below five days per week and had higher education levels compared with participants with burnout ( p < 0.005). Those without burnout were also more likely to have a lower prevalence of hypertension and SDH ( p < 0.02).
Table 2 shows that both personal and work-related burnouts were associated with a higher mean DBP. After adjusting for confounders, the participants with both types of burnout had a 1.66 (95% CI: 0.02–3.30) mmHg higher mean DBP than those without burnout. The participants with only personal (β = 0.53; 95% CI: −0.83–1.90) or work-related burnout (β = −0.10; 95% CI: −1.58–1.38) did not show an elevated mean DBP compared with the reference group. All types of burnout were not associated with an increased mean SBP. The odds of hypertension among the participants with only work-related burnout increased by 40% (OR = 1.40; 95% CI: 0.99–1.96) compared with those without burnout, with marginal significance, while personal burnout (OR = 1.21; 95% CI: 0.88–1.67) and both burnouts (OR = 1.31; 95% CI: 0.89–1.90) were not statistically significantly associated with elevated odds of hypertension.
Association between burnout status and mean systolic blood pressure, diastolic blood pressure, and hypertension among working adults in Santiago, Chile ( n = 1872).
Abbreviations: β, coefficient; CI, confidence interval; DBP, diastolic blood pressure; OR, odds ratio; Ref., reference group; SBP, systolic blood pressure. a Adjusted for sociodemographic (sex, continuous age, country, and highest education levels), behavioral (BMI, smoking status, alcohol consumption, and physical activity), and occupational characteristics (work sector, work type, and work shift).
Supplementary Table S1 shows that having both burnouts was associated with a 2.11 (95% CI: 0.06–4.15) mmHg higher DBP compared with no burnout among men after adjusting for putative confounders. Men with both burnouts and only work-related burnout had 1.65-fold (95% CI: 1.04–2.58) and 1.57-fold (95% CI: 1.07–2.28) higher odds of hypertension compared with those without burnout. However, all types of burnout were not statistically significantly associated with SBP, DBP, and the odds of hypertension among women ( Supplementary Table S1 ).
The association between burnout status and subtypes of hypertension is presented in Table 3 . After accounting for putative confounders, the odds of IDH among the participants with only personal burnout and both burnouts were 2.00-fold (OR = 2.00; 95% CI: 1.21–3.31) and 2.08-fold (OR = 2.08; 95% CI: 1.15–3.78) higher than those without burnout. The odds of SDH among the participants with only work-related burnout increased by 59% (OR = 1.59; 95% CI: 1.01–2.50) compared with those without burnout. All types of burnout were not associated with increased odds of ISH.
Association between burnout status and subtypes of hypertension among working adults in Santiago, Chile ( n = 1872).
Abbreviations: CI, confidence interval; IDH, isolated diastolic hypertension; ISH, isolated systolic hypertension; OR, odds ratio; Ref., referent group; SDH, combined systolic/diastolic hypertension. a Adjusted for sociodemographic (sex, continuous age, country, and highest education levels), behavioral (BMI, smoking status, alcohol consumption, and physical activity), and occupational characteristics (work sector, work type, and work shift).
4. Discussion
In the present study of Chilean working adults, 27.2% of the participants had hypertension, with 7.2% having IDH, 9.2% having ISH, and 10.8% having SDH. We found that the participants with both personal burnout and work-related burnout were associated with elevated DBP after adjusting for prior putative confounders. The results were consistent among men but not women. We also found that odds of IDH increased among the participants with only personal burnout and both burnouts compared with those without burnout. The elevated odds of SDH were found among the participants with only work-related burnout. Little evidence was found of an association of any status of burnout with elevated SBP and ISH.
Our study extended the findings from prior studies [ 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ], documenting that exposure to personal and work-related burnout was related to an increased DBP and higher odds of IDH. These findings are vital for working adults. Although previous evidence has indicated that an increase in SBP or having ISH or SDH is the dominant predictor of cardiovascular outcomes, and that changes in DBP and the occurrence of IDH is considered less important in preventing cardiovascular risk [ 37 ], this circumstance is age-dependent [ 7 ]. The results from The Framingham Heart Study showed that elevated DBP was the dominant predictor of coronary heart disease (CHD) among individuals <50 years, and the risk of CHD by elevated DBP and SBP was comparable among those <60 years [ 7 ]. Another piece of evidence from UK Biobank indicated that for individuals <60 years, the hazard of composite CVD events (nonfatal MI, nonfatal ischemic stroke, nonfatal hemorrhagic stroke, and CVD death) increased among those with IDH compared with those without IDH [ 38 ]. One longitudinal study recruiting adults from all age ranges (≥18 years, median = 53 years) showed that increased DBP and IDH were still independently associated with a higher hazard of adverse CVD events (first episode of myocardial infarction, ischemic stroke, or hemorrhagic stroke) [ 39 ], although yielding a smaller effect size than elevated SBP and ISH. Given that most of our participants were working adults (mean age = 45.7 years, with 82.6% <60 years), the burden of increased DBP and the odds of IDH might contribute to the younger occurrence of CVD events, yielding an inability to work and a poor quality of life. Moreover, IDH was associated with future ISH and SDH [ 40 ], leading to higher risk and worse prognosis of CVD events in later life [ 7 ]. Therefore, interventions to alleviate burnout from not only the working environment but also personal life may help decrease the risk of CVD among working adults by improving their DBP.
The substantial variability in our results and the existing evidence might account for the differences in the measurement tools of burnout and the population recruited in the studies [ 22 ]. Previous studies have mainly focused on burnout derived from work settings [ 13 , 14 , 15 , 16 , 17 , 19 , 20 , 21 , 22 , 23 , 24 ] and individuals in the human service sector (health professionals [ 13 , 14 , 15 , 19 ], university professors [ 16 ], company managers [ 21 ], and workers in elderly welfare facilities [ 17 ]). Only one study focused on personal burnout [ 17 ], and one was conducted in other sectors (mine workers [ 20 ]). We extended the current evidence to a new magnitude and broader sources of burnout and the population by assessing personal burnout and recruiting working adults from multiple sectors and occupational types.
The potential mechanism that burnout may lead to increased blood pressure and risk of hypertension usually accounts for the autonomic nervous system (ANS) and the hypothalamic–pituitary–adrenal (HPA) axis [ 41 ], which are the primary systems responding to stressors in humans. Burnout has been characterized as a prolonged psychosocial stress exposure, yielding a persistent unbalance between demands and resources [ 1 ]. This mismatch may lead to the sustained activation of the sympathetic nervous system (SNS) and suppression of the parasympathetic system (PNS) [ 41 ]. The level of catecholamines (such as adrenaline and noradrenaline) would thus persistently increase, raising the DBP and subsequently increasing the risk of IDH by causing vasoconstriction and constant peripheral resistance. The high DBP related to the prolonged activation of the SNS may also be due to an inactive reaction of the HPA axis. Existing evidence has found that hypocortisolism occurs in individuals with burnout [ 42 ], which could decrease the negative feedback from cortisol to corticotropin-releasing hormone (CRH), thus raising CRH levels persistently. CRH is a hormone that can activate the SNS [ 43 ], leading to prolonged high DBP. Sustained high peripheral resistance can increase atherosclerosis risk, impairing the structure of large arteries and making them less elastic. Together with the effect of age on increasing the stiffness of large arteries [ 44 ], IDH related to burnout may switch to SDH or ISH due to the elevation of SBP when individuals grow older [ 40 ]. Our results might manifest this progress to some extent. The participants with only personal burnout (with 17.9% ≥60 years) and both burnouts (with 14.0% ≥60 years) were younger and were associated with higher odds of IDH. In comparison, the participants with only work-related burnout (with 23.3% ≥60 years) were older and were related to higher odds of SDH. Burnout is also associated with hypercholesterolemia [ 9 ], type 2 diabetes [ 9 ], and a high risk of unhealthy behaviors such as smoking [ 8 ], alcohol consumption [ 8 ], and substance abuse [ 8 ], all of which are considered risk factors for increased blood pressure and hypertension [ 11 , 45 ].
Previous studies have shown that women have sustained excessive demands outside of their work [ 36 ] and are more likely to experience burnout compared with men [ 32 ], which was consistent with the current study, showing that women had a higher proportion of personal burnout (36.7% in women vs. 18.7% in men). However, all types of burnout, including personal burnout, did not have a statistically significant association with elevated blood pressure and odds of hypertension, which was different from the results in men. We do not have a clear explanation for this. The lack of a statistically significant association among women might be due to a lower underlying risk of hypertension than men; even though a larger proportion of women were exposed to personal burnout, they may still be less likely to have hypertension.
There were serval strengths in our study. First, we assessed burnout from both the working environment and personal life, accounting for the potential joint effect of burnout from different attributes. Second, to the best of our knowledge, this was the first study examining the association between burnout and hypertension subtypes, presenting a clearer image of how burnout might affect the occurrence of hypertension. Third, our study population comprised working adults from multiple types of occupations in different work sectors, increasing the generalizability of our results compared with previous studies.
Limitations
As a cross-sectional study, the temporality of burnout and hypertension could not be determined. Additionally, we did not collect information on the participants’ prior diagnosis of hypertension and anti-hypertensive treatment. Whether the participants had hypertension was defined only by their blood pressure, which might lead to the misclassification of the outcome because we did not recognize hypertensive patients with normal blood pressure maintained by anti-hypertensive treatment. Moreover, prior diagnosis of hypertension and medical use may be associated with current blood pressure and hypertension, as well as the emotional burden of working adults, leading to higher levels of burnout. The lack of adjustment for those factors may yield residual confounding bias. For applying self-reported measurement tools on burnout and most covariates, measurement errors might have caused bias in the results. As we drew the participants from a worker’s compensation hospital, the results of our study might not be generalizable to working adults from other bases. Finally, although the regression models were adjusted for possible confounding factors, residual confounding could have possibly remained due to these unmeasured factors.
5. Conclusions
Both work-related and personal burnouts were associated with an increased DBP and odds of diastolic hypertension among working adults in Chile. Mental health support for burnout may effectively prevent hypertension among working adults. Future researchers should consider conducting prospective cohort studies or randomized trials to determine the temporality between burnout and hypertension.
Acknowledgments
The authors wish to thank the dedicated staff members of the Hospital del Trabajador for their expert technical assistance with this research.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20031899/s1 , Table S1: Association between burnout status and mean systolic blood pressure, diastolic blood pressure, and Hypertension among working adults in Santiago, Chile, with stratification by sex (N = 1872).
Funding Statement
This research was supported by awards from the National Institutes of Health (NIH) and the National Institute of Minority Health and Health Disparities (T37-MD-001449). The NIH had no further role in the study design, the collection, analysis, and interpretation of data, the writing of the report, and the decision to submit the paper for publication.
Author Contributions
Conceptualization, Y.C., D.J.-Q. and B.G.; Methodology, Y.C., D.J.-Q. and B.G.; Software, Y.C.; Validation, Y.C., D.J.-Q. and B.G.; Formal Analysis, Y.C.; Investigation, J.C.V., S.M. and J.C.; Resources, J.C.V.; Writing—Original Draft Preparation, Y.C.; Writing—Review and Editing, Y.C., D.J.-Q., B.G., J.C.V., S.M. and J.C.; Supervision, B.G. and J.C.V.; Project Administration, B.G. and J.C.V.; Funding Acquisition, B.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the institutional review boards of the Hospital del Trabajador, Santiago, Chile, and the Office of Human Research Administration, Harvard T.H. Chan School of Public Health, Boston, MA (IRB Approval Number: IRB15-0585).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
- Open access
- Published: 14 November 2023
Non-drug interventions of traditional Chinese medicine in preventing type 2 diabetes: a review
- Jingying Liu 1 ,
- Chun Yao 3 ,
- Yitao Wang 1 ,
- Jinmin Zhao 2 &
- Hua Luo ORCID: orcid.org/0000-0002-9710-6084 1 , 2
Chinese Medicine volume 18 , Article number: 151 ( 2023 ) Cite this article
1940 Accesses
2 Altmetric
Metrics details
Traditional Chinese medicine (TCM) is increasingly used to manage type 2 diabetes and its nonpharmacological interventions are showing potential for preventing type 2 diabetes. This study mainly reviews relevant research. The most mentioned non-drug treatments for preventing type 2 diabetes in TCM are healthy diet, physical activity, emotional therapy, and acupuncture. In most studies, blood glucose status in patients with prediabetes and type 2 diabetes was significantly improved after TCM non-drug interventions, and there was no significant difference between the adverse effect of TCM and control groups or other intervention groups, while the methodological quality of the clinical trials involving TCM generally kept a low level. The effectiveness of TCM in preventing type 2 diabetes has yet to be validated in large randomized controlled trials and the underlying mechanism also needs further exploration.
Introduction
Diabetes mellitus, more simply called diabetes, manifests as continuous hyperglycemia because any or enough of the insulin cannot be made in the pancreas or efficiently used by the body; it is a severe and common chronic disease [ 1 ]. Plasma glucose criteria, either the fasting plasma glucose (FPG) value or the 2-h postload glucose (2hPG) value during a 75- g oral glucose tolerance test or glycated hemoglobin (HbA1c) criteria, is the clinical diagnostic indicator of diabetes [ 2 , 3 , 4 ] (Table 1 ).
Prediabetes is used to describe individuals who exhibit abnormal carbohydrate metabolism but do not yet satisfy the criteria for diabetes and these people present with impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT) and/or HbA1c 6–6.4% (5.7–6.4%) [ 5 , 6 ]. With prediabetes, the risk of conversion to diabetes increases, but this can be reduced by active intervention [ 7 , 8 , 9 , 10 , 11 ].
Diabetic patients are more susceptible to developing a series of health problems, which not only influence the quality of life but also threaten the life of patients. State of chronic hyperglycemia can cause serious damage to the body and various organs failure, resulting in disabling and life-threatening health complications and being a major cause of cardiovascular disease, kidney failure, lower limb amputation and blindness. However, appropriate management can help delay or prevent these. Therefore, interventions should be taken to prevent or delay this disease and associated comorbidities [ 1 , 12 ].
The global prevalence of diabetes appears to be an alarming trend, rising from 10.5% (536.6 million) of people aged 20–79 in 2021 to 12.2% (783.2 million) by 2045 [ 13 ]. Besides, it was estimated that about 44.7% (239.7 million) of adults with diabetes did not realize it [ 14 ]. Type 2 diabetes, the most common type of diabetes, accounts for almost 90% of the 536.6 million cases [ 1 ], making its prevention and treatment imperative. Although contemporary medicines control the diabetic state effectively, it is difficult to reverse the course of the disease. Better, cheaper, simpler treatments with fewer side effects to prevent type 2 diabetes, especially non-drug interventions, deserve to be explored.
Traditional Chinese Medicine (TCM) has been used and developed for more than 2000 years and has become increasingly popular in the East and West over the last several decades [ 15 ]. In China, a national survey was conducted to estimate the attitude of patients who receive TCM, Western medicine, and integrative medicine (TCM and Western medicine integrated). The results showed that 71.2% of 2748 participants preferred integrative therapeutic treatments and 18.74% favored the TCM therapeutic method as their favorite [ 16 ]. In the US, over 15 million people take herbal remedies or high-dose vitamins. Besides, visits to complementary and alternative medicine far outweighed those to primary physicians, costing more than 34 billion per year [ 17 ]. In Australia, in a wide survey targeting older people over 50 years old with chronic diseases, during the past 3 months, 8.8% of the total 2540 participants and 5.1% of 184 individuals with diabetes saw complementary and alternative medicine doctors [ 18 ].
In recent years, growing research was conducted on the prevention and management of type 2 diabetes with TCM, and the effectiveness and advantages of TCM in preventing and treating type 2 diabetes were in the process of being confirmed [ 19 ]. In addition to herbal remedies, TCM also focuses on diet adjustment and active exercise to prevent type 2 diabetes, which is consistent with modern research. This review summarizes nonpharmacological intervention studies of TCM for preventing type 2 diabetes and compares the similarities and differences between TCM and contemporary medicine, aiming to tap the potential of TCM in this regard and provide new research directions for type 2 diabetes and new non-drug therapy for clinical prevention.
- Type 2 diabetes
Although the causes of type 2 diabetes are not fully understood, several risk factors, including a complex combination of genetic, metabolic and environmental factors, have shown strong relationships with it [ 20 , 21 , 22 ], such as family history [ 23 ], obesity [ 24 , 25 ], unhealthy diet [ 26 , 27 ], physical inactivity [ 28 ], and ethnicity [ 29 , 30 ].
Insulin resistance and initial hyperglycemia are the primary pathophysiology characteristics of type 2 diabetes, followed by a gradual decline in the ability of pancreatic β cells to produce insulin [ 31 ]. In type 2 diabetic patients, adipose tissue, gastrointestinal tract, α-cell, kidney and brain all play important roles in the development of glucose intolerance, besides the traditional triumvirate of insulin resistance in muscle and liver and β-cell failure [ 32 ]. These eight core defects were later expanded to 11 mediating pathways that resulted in hyperglycemia [ 33 ] (Fig. 1 ).
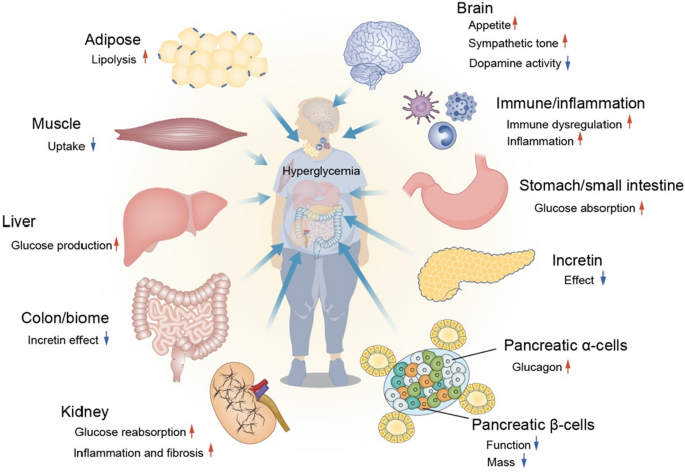
11 defects contributing to hyperglycemia
Patients with type 2 diabetes present semblable symptoms to those with type 1 diabetes, often characterized by excessive thirst, frequent urination, tiredness, blurred vision, recurrent skin infections, slow wound healing and tingling or numbness in the hands and feet [ 1 , 4 ]. However, these individuals may live with mild or absent symptoms for several years before diagnosis, making early detection and prevention important.
In ancient China, there was a disease named Xiao Ke, manifesting polydipsia, polyuria and polyphagia, accompanied by emaciation or sweetness of the urine. Due to their similar symptoms, modern TCM doctors regard diabetes as this disease during treating type 2 diabetes [ 34 , 35 ]. In the last few years, large-scale clinical trials have confirmed that TCM has made progress in hypoglycemic, delaying the transition from prediabetes to diabetes, reducing the risk of diabetic complications and delaying the progression of diabetes complications [ 19 ].
TCM thoughts
Primary prevention focuses on reducing risk factors and preventing the occurrence of type 2 diabetes. Preventing the exacerbation and complication of type 2 diabetes through early detection, early diagnosis and early treatment is the goal of secondary prevention. And delaying the progression of diabetic complications, minimizing morbidity and mortality and maximizing quality of life after a long-term type 2 diabetes or injury are major components of tertiary prevention [ 34 ]. In diabetes prevention, primary prevention could gain more preventive benefits than the other two levels of prevention and secondary prevention might obtain greater population benefits than tertiary prevention [ 36 ].
TCM holds the similar view of prevention. Huangdi Neijing, as one of four TCM classics, has a famous saying: now, when drugs are employed for therapy only after a disease has become fully developed, when attempts at restoring order are initiated only after a disorder has fully developed, this is as if a well were dug when one is thirsty, and as if weapons were cast when the fight is on. Would this not be too late, too [ 37 ]? This reflects one of the most important thinking strongly emphasized by TCM, preventive treatment, including prevention before disease onset and development [ 38 ]. For type 2 diabetes, it refers to preventing the onset of prediabetes and type 2 diabetes in healthy individuals, reversing the prediabetic state and preventing it from developing into type 2 diabetes for prediabetic individuals, and maintaining blood glucose levels and preventing further progression, comorbidity and complications for type 2 diabetes patients [ 39 ].
Non-drug TCM interventions
Type 2 diabetes is a highly preventable disease through lifestyle modification. Landmark research has shown that prevention can be achieved by physical activity and a healthy diet [ 40 , 41 ]. The Da Qing Study estimated the effect of a 6-year diet and exercise intervention in people over the age of 45 with IGT. The cumulative incidence of diabetes at 6 years was higher in the control group (67.7%) compared with the three intervention groups (diet only 43.8%, exercise only 41.1%, diet plus exercise 46.0%) [ 42 ] and during the 20 years follow-up, 80% of participants in the intervention group and 93% of the participants in the control group had developed diabetes [ 8 ]. The Finnish Diabetes Prevention Study, the first randomized controlled trial, aimed to find out whether lifestyle modification can prevent type 2 diabetes alone among people with IGT. The intervention group was given detailed personalized advice involving dietary advice and physical activity guidance. After 4 years, compared with the control group (23%), the cumulative incidence of diabetes was lower in the experimental group (11%) [ 10 ], and this result was maintained even if after the lifestyle intervention was ceased [ 43 ]. The Diabetes Prevention Program (DPP) compared the efficacy of therapeutic lifestyle changes or metformin and placebo for persons with IGT in the US. After 2.8 years, the incidence of diabetes was 4.8, 7.8 and 11.0 cases per 100 person-years respectively. Both lifestyle interventions and metformin treatment reduced the incidence of diabetes in high-risk groups, but the former was more effective than the latter [ 44 ]. This lifestyle or metformin prevention of diabetes can remain for at least a decade [ 45 ]. In fact, doing TCM therapy exercises and decreasing the intake of noodles, rice and fruit had been recommended for diabetic patients by TCM doctors, a thousand years before John Rolo, the first person to use diet intervention as a treatment for diabetes [ 35 ] (Figs. 2 , 3 and 4 ).
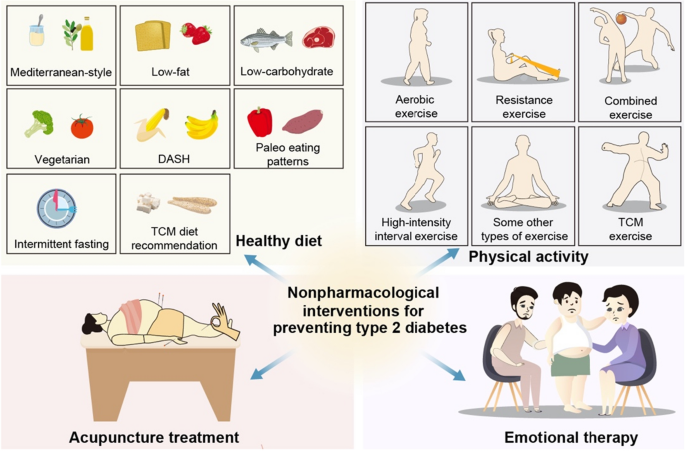
Non-drug interventions for preventing type 2 diabetes
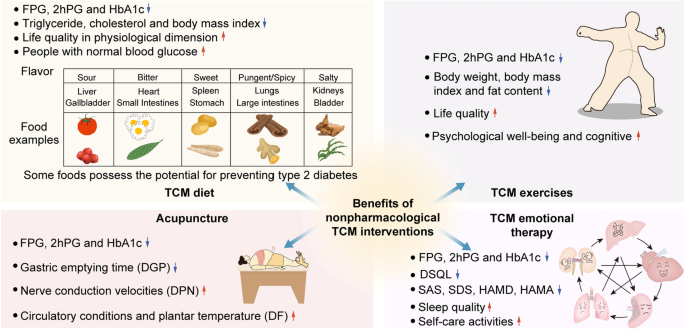
Benefits of non-drug TCM intervention
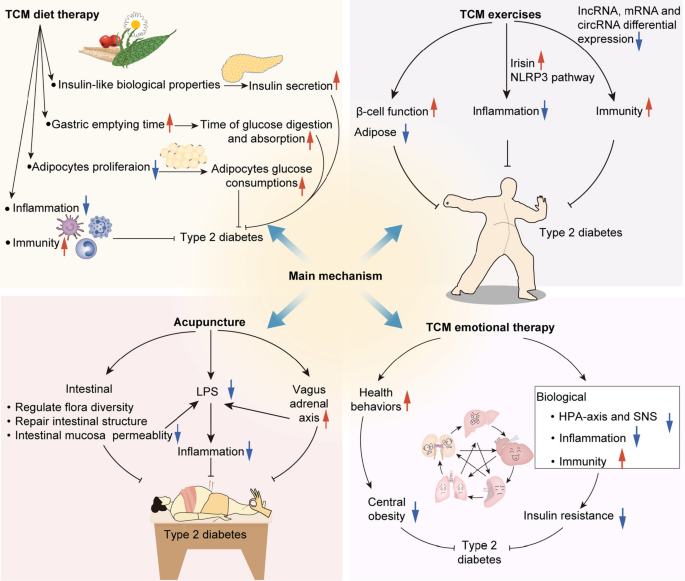
Main possible mechanism of non-drug TCM intervention
Healthy diet
Several dietary factors were found to be associated with an increased or decreased risk of type 2 diabetes, regardless of body weight change [ 40 ]. Some dietary patterns showed potential for preventing prediabetes or type 2 diabetes. The relevant research available mainly focused on Mediterranean-style, low-fat, low-carbohydrate, vegetarian, dietary approaches to stop hypertension, paleo eating patterns and intermittent fasting. Although diet may vary because of culture, food availability and personal preferences, there are some consensus recommendations on the general principles for type 2 diabetes prevention: a variety of eating patterns are acceptable. Some foods should be encouraged, such as nonstarchy vegetables, unrefined grain products with high natural fiber and nuts, legumes and fish as the source of protein. Some should be limited or reduced, such as sugar, refined grains, red meat, highly processed foods and carbohydrates [ 46 ].
In the year 652, Sun Simiao, a famous TCM doctor in the Tang dynasty, suggested that patients with Xiao Ke needed to control drinking and salty food and food made of flour intake. After that, TCM doctors gradually realized that sugar in food worsens the condition and gave some dietary advice to these patients [ 35 ]. Based on the theory of nutrition, the theory of TCM and the literature evidence of diet-related chronic disease, some principles and suggestions are put forward for the daily diet of diabetic patients by an expert group in China [ 47 ]. It is not difficult to find that the dietary guidelines recommended by TCM are very similar to contemporary medicine, which emphasizes having a bland diet and reducing sugar intake.
However, TCM has its own characteristics, that is, syndrome differentiation and treatment [ 48 ], and some food, such as Poria cocos (Fuling) and Dioscorea opposita (Shanyao), also act as Chinese herbal medicine, have great potential in preventing type 2 diabetes [ 49 , 50 , 51 ]. From this, daily meals can be combined with TCM health recipes to prevent diabetes. In the Dietary Guidelines for Adults with Diabetes, patients are divided into three main categories. Mori folium (Sangye), Cassiae Semen (Juemingzi) and Nelumbinis Semen (Lianzi) could be adopted for patients with yin deficiency heat excess syndrome to nourish yin and clear heat. Mori Fructus (Sangshen), Lycii Fructus (Gouqizi) and Puerariae lobatae Radix (Gegen) could be used for patients with qi and yin deficiency syndrome to tonify qi and yin. Dioscoreae Rhizoma (Shanyao), Poria (Fuling) and Cinnamomi Cortex (Rougui) are suggested for patients with yin and yang deficiency syndrome [ 47 ]. While treating patients with syndrome differentiation, TCM dietotherapy also pays attention to in line with seasonal and local conditions. Besides, TCM also focuses on having regular meals, which refers to the relatively fixed time of three meals a day and additional meals, because regular and quantitative meals can avoid the lethargy of satiety center response caused by excessive hunger, resulting in overeating.
Several clinical trials have proved the ability of TCM dietary therapy to prevent type 2 diabetes. In a randomized controlled trial, 80 patients with IGT were randomly divided into a control group and an intervention group. The former received general nutrient health education, while the latter was guided to take TCM medicated diets according to TCM theory and individual physique. After 1 month and 3 months of treatment, the blood glucose, triglyceride, cholesterol and body mass index in the intervention group were better than those in the control group, and the differences were statistically significant. Furthermore, 37 patients in the intervention group had normal blood glucose after 6 months of treatment, whose outcome was significantly better than that of the control group [ 52 ]. Another research explored the effect of the Jianpi Qushi Diet recipe on prediabetic patients with phlegm-dampness constitution. A total of 200 middle-aged patients with prediabetes and phlegm-dampness constitution were selected and randomly divided into two groups. Both groups were given routine health education and hypotensive and lipid-lowering drugs appropriately. Moreover, based on the food exchange method of the control group, the experimental group was given the Jianpi Qushi Diet recipe to replace part of the food. At 6 months and 12 months, the FPG and the 2hPG of the two groups were significantly lower than those before the intervention, and the reduction degree of the experimental group was significantly better than that of the control group, with statistically significant differences [ 53 ]. Besides, a meta-analysis of 12 randomized controlled trials including 1178 patients evaluated the influence of TCM diet intervention on blood glucose and life quality of type 2 diabetes. Among them, there were 593 cases in the TCM diet intervention group and 585 cases in the conventional treatment group. The results illustrated that the FPG, 2hPG and HbA1c in the intervention group were significantly lower than that in the control group. Although there was no significant difference between the two groups in psychological and social dimensions, the dietary intervention group was superior to the control group in the physiological dimension of quality of life [ 54 ].
TCM dietary therapy shows tremendous potential in improving blood glucose levels in patients with diabetes or prediabetes, the mechanism of action can be considered in the following aspects. First, some TCM medicinal diets may have insulin-like biological properties, which can promote insulin secretion and increase the sensitivity of tissue cells to insulin. Second, some TCM medicinal meals contain rich dietary fiber, so they can delay the gastric emptying time, thereby delaying the digestion and absorption of glucose. Third, the hypoglycemic effect of TCM diet recipes may be achieved by inhibiting the proliferation of adipocytes and promoting the glucose consumption of adipose cells, thus improving insulin resistance. In addition, reducing inflammation in the body and regulating the intracorporeal environment may also be the potential mechanisms [ 55 ].
Physical activity
Physical activity, also an important factor in preventing type 2 diabetes independent of body weight status [ 56 ], helps to improve insulin sensitivity [ 57 , 58 ], reduce visceral fat [ 58 , 59 ], enhance β-cell function [ 59 ] and improve gut microbiota [ 60 ]. Based on previous studies, at least 700 kcal/week, equal to a minimum of 150 min of moderate-intensity athletic activities each week like brisk walking, was adopted for DPP [ 61 ]. International Diabetes Federation has a similar recommendation for preventing type 2 diabetes by exercising at least 30 to 45 min three to 5 days a week [ 1 ]. Multiple types of physical activity have been shown benefit in glycemic management for type 2 diabetes patients, including aerobic exercise, resistance exercise, combined exercise, high-intensity interval exercise and some other types of exercise [ 62 , 63 ].
In the year 610, Chao Yuanfang, a knowledgeable imperial physician in the Sui Dynasty, proposed that Xiao Ke patients should do Daoyin, a type of TCM therapeutic exercise, and then take 120 steps even up to a thousand steps, and then eat a meal [ 35 ]. During the long history of TCM development, a variety of TCM therapeutic exercises have been formed [ 64 ], being proven to be suitable for central obesity management, thereby reducing the risk of related diseases [ 65 ], and have been recommended for the prevention and treatment of diabetes by Chinese guidelines [ 66 ]. Among them, Qigong, Tai Chi, Baduanjin and Yijinjing are most used in clinical experiments and show great potential in the prevention of type 2 diabetes [ 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 ].
A meta-analysis of nine randomized controlled trials with 485 participants included four types of TCM exercises: Baduanjin, Yijinjing, Tai Chi and Shaolin Kungfu, investigating the effects of these exercises on glycemic control in individuals with prediabetes. The results suggested that among the prediabetes patients, TCM exercises were associated with lower FPG, 2hPG and HbA1c, having potential preventive value for type 2 diabetes [ 68 ]. Similar findings were seen in patients with type 2 diabetes. Compared with the comparison group, the TCM exercises group performed better in the glycemic control and observed a significant decrease in FPG and HbA1c [ 69 ]. Several studies recommended Tai Chi as a prophylactic and therapeutic exercise prescription for type 2 diabetes [ 67 , 72 , 73 , 76 , 77 ], which not only improved FPG, 2hPG, HbA1c, triglyceride, high density lipoprotein cholesterol and life quality of people with type 2 diabetes compared with control groups (usual care, regular exercise and clinical conventional therapy) but also better played hypoglycemic effect than that of other aerobic exercises [ 72 , 73 , 76 , 77 ]. Moreover, the FPG level was lower in the Qigong group than in that of the resistance exercise group and the HbA1c level of the other aerobic exercise group, and the differences were statistically significant [ 71 ]. Baduanjin, another kind of mind-body program, got better improvements in FPG, 2hPG and HbA1c, better gains in body mass index and more positive impact on depression, anxiety and mental health compared with usual care and better improvements in HbA1c, body mass index, depression and anxiety compared with other exercises [ 75 , 78 ].
A recent randomized controlled trial evaluated the effect of engagement in Baduanjin for prediabetes patients. The results showed that a year of Baduanjin training improved blood glucose, blood lipid profile, body shape and blood pressure and protected against diabetes and atherosclerotic cardiovascular disease of these participants significantly [ 79 ]. Besides, Yijinjing combined with elastic band exercise, reducing the body weight, body mass index and fat content and improving muscle function and growth hormone secretion in patients with prediabetes, can delay muscle mass loss and diabetes development [ 80 ]. Furthermore, in a randomized clinical trial including 328 patients aged 60 and above with type 2 diabetes and mild cognitive impairment, the Tai Chi Chuan group had higher Montreal cognitive assessment scores compared with the control group and the fitness walking group at 36 weeks, suggesting its potential to prevent cognitive impairment and exacerbation in senile patients with type 2 diabetes [ 81 ]. These three recent clinical trials all manifested that adverse events unrelated to the studies did not have statistically significant differences between the TCM exercises group and the other group [ 79 , 80 , 81 ].
From a Western perspective, TCM exercises can be classified as a type of light to moderate intensity aerobic exercise that is conducive to metabolism in cells and tissues, cardiac blood reflux, improved glucose utilization and target cell reactivity, reduced glucose resistance, enhanced HbA1c decomposition and accelerated hemoglobin and oxygen binding [ 71 ]. Moreover, the potential hypoglycemic mechanism of TCM exercises in prediabetes individuals may be associated with the increase of irisin in blood and inhibition of the NLRP3 inflammatory signal pathway, which helps reduce insulin resistance and inflammation [ 82 ]. For type 2 diabetes patients, TCM exercises probably achieved preventive and therapeutic effects by the benefit of immune regulatory function [ 83 ]. It may play a role by regulating the abnormal expression of incRNA, mRNA, and circRNA in improving depression symptoms and blood glucose levels of type 2 diabetes patients with depression. [ 84 ].
Therefore, TCM exercises provided more variety of choices for type 2 diabetes prevention and could be considered to popularize with their easy to learn and no limit by time and venue nature [ 71 , 79 ].
Emotional therapy
An emerging number of the literature suggests that psychological stress and psychiatric disorders may bring on type 2 diabetes [ 85 , 86 , 87 ]. The relationship between psychological factors and the occurrence of type 2 diabetes has gotten unprecedented attention and concern from many researchers since English physician Thomas Willis observed that emotional factors such as grief or sadness could cause diabetes [ 88 ]. Although the findings were initially inconsistent, the evidence gradually moved to support this link [ 89 ].
A series of reviews and meta-analyses have revealed that compared with non-depressed individuals, there was a higher risk of developing type 2 diabetes in depression patients [ 90 , 91 , 92 , 93 ], and vice versa [ 94 , 95 ]. In addition, after investigating the relationship between anxiety and the incidence of diabetes, it was found that anxiety may be one of the risk factors for incident diabetes [ 96 , 97 ]. While prediabetes itself has been linked to the onset of diabetes, a study found that in participants with prediabetes, anxiety could boost its progression to type 2 diabetes [ 98 ]. Similar results turned out between prediabetes and depressive symptoms. A recent study illustrated that adults with depressive symptoms accompanied by prediabetes had a higher possibility for type 2 diabetes [ 99 ]. Besides, other negative psychological factors, such as posttraumatic stress disorder [ 100 ], adverse childhood experiences [ 101 , 102 ] and job strain [ 103 ] are probably correlated to an increased incidence of type 2 diabetes among the initially healthy population.
The mechanisms explaining the link between negative psychological factors and type 2 diabetes can be classified into two main categories. First, psychological stress is associated with adverse health behaviors, involving unhealthy diet, physical inactivity, smoking, sleeping disturbances and medical examination absence, which indirectly increases the risk of type 2 diabetes [ 86 , 90 , 91 , 92 , 104 ]. Second, multiple biological mechanisms are also considered to elucidate this link [ 86 , 92 , 95 ]. Poor health behaviors mentioned before and a side effect of medications can induce weight increase and obesity [ 105 , 106 , 107 ]. Furthermore, the hypothalamus-pituitary-adrenal axis and the sympathetic nervous system are activated by chronic stress, increasing the release of cortisol which results in stimulating glucose production, increasing portal and peripheral free fatty acids, decreasing insulin sensitivity and inhibiting insulin secretion [ 90 , 108 , 109 , 110 , 111 ]. Besides, systemic inflammation and immune system also may function in the relationship between negative emotional factors and the increased risk [ 85 , 86 , 90 ]. Although there is not direct evidence of a relationship between negative emotions and the causes of type 2 diabetes, the link between negative emotions and an increased risk of diabetes is increasingly being recognized, suggesting that enhancing mental welling may decrease this hazard and be beneficial to its prevention.
TCM has realized the vital impact of emotions on human health for thousands of years. According to TCM theory, there are seven main categories of emotions: joy, anger, anxiety, pensiveness, sadness, fear and fright. Disorder emotion can cause the dysfunctions of internal organs, developing into different diseases [ 112 ], which is gradually supported by some facts. More than 5.9 million people born in Denmark were included in a population-based cohort study that was followed from 2000 to 2016. Cox regression models were used to evaluate the overall hazard ratio and time-dependent hazard ratios for pairs of mental disorders and medical conditions. It was shown that most mental disorders exacerbated the risk of a subsequent illness, with hazard ratios ranging from 0.82 to 3.62, depending on the time the mental disorder was diagnosed [ 113 ]. In the etiology of type 2 diabetes, TCM not only emphasizes the important role of lifestyle such as diet and exercise but also recognizes the influence of emotional factors, proposing emotional disorder is one of the causes [ 114 ], which is consistent with modern research to some extent [ 85 , 86 , 87 , 90 , 91 , 92 , 93 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 ]. Therefore, emotion regulation is a possible intervention to treat and prevent type 2 diabetes. A new psychotropic treatment model based on rhythm regulation has been applied to the treatment of type 2 diabetes, which not only reduced FPG, 2hPG and HbA1c but also decreased the occurrence of hypothalamic–pituitary–adrenal axis abnormalities, and might forestall the progression of type 2 diabetes and played a preventive role [ 115 ]. Although some evidence reported that for type 2 diabetes, the use of antidepressants could be an independent risk factor [ 107 , 116 ]. Actually, these reports do not conflict with emotional therapy. Because the causality has not been established for some antidepressants at higher doses and longer duration are associated with worsening glucose control. And long-term prospective studies of individual antidepressants rather than class effects should be done.
TCM emotional therapy, without needing to worry about drug reactions, is different from the regulation of emotions by modern drugs. It has special emotional therapy for preventing type 2 diabetes: remind high-risk groups to avoid excessive emotional stimulation, and according to the principle of generation-inhibition in five elements, stimulate existing emotion of the individuals with corresponding emotion [ 114 ]. In several clinical trials, patients with type 2 diabetes were randomly split into a control group with routine care and an intervention group given TCM emotional nursing care based on usual care. A number of measures assessing blood glucose levels, self-management ability, quality of survival, negative emotion, symptoms and treatment compliance were compared before and after the trial. These findings suggested that TCM emotional therapy may benefit type 2 diabetics. After the treatment, firstly, the FPG, 2hPG and blood glucose fluctuation in the intervention group were lower than those in the control group, and the differences were statistically significant [ 117 , 118 ]. Secondly, in comparison with the routine care group, the TCM group had a higher measure scoring on the summary of diabetes self-care activities (SDSCA) and a lower diabetes specific quality of life scale (DSQL) [ 119 , 120 ]. Thirdly, TCM mental nursing, with lower scores on the self-rating anxiety scale (SAS) and self-rating depression scale (SDS) and a better Pittsburgh sleep quality index (PSQI), demonstrated the ability to improve negative emotions and sleep quality [ 120 , 121 , 122 ]. Finally, it was shown that patients in the treatment group had better compliance than those in the usual care group, which was more conducive to maximum therapeutic effect [ 117 , 120 , 121 ]. Besides, there were also some possible advantages for patients with diabetes complications treated by TCM emotional nursing. A few randomized controlled trials have demonstrated that the implementation of emotional nursing of TCM in diabetic patients with anxiety or depression not only contributed to controlling blood glucose, making FPG, 2hPG and HbA1c lower than the control group, but also alleviated the negative feeling. The scores of SAS, SDS, Hamilton anxiety scale (HAMA) and Hamilton depression rating scale (HAMD) were lower than those of the conventional care group [ 123 , 124 , 125 , 126 , 127 ]. For diabetic nephropathy patients, negative emotions were improved and quality of life was promoted after the TCM emotional nursing. And the differences in SAS, SDS as well as DSQL scores between the intervention group and the control group were statistically significant [ 128 , 129 ]. A study investigated the impact of psychological nursing on diabetic food patients. The results indicated that the HAMA scores, HAMD scores, hospital stays and amputation rates in the intervention group were significantly lower than those in the control group [ 130 ]. TCM emotional therapy also manifested a positive significance on the diabetic neurogenic bladder, playing a role in improving clinical symptoms, reducing bladder residual urine volume and relieving anxiety and depression [ 131 ]. However, some of the intervention groups in these trials involved TCM massage and exercise, which may have interfered with the outcome, so well-designed studies are needed to illustrate TCM emotional therapy is helpful to type 2 diabetics.
Acupuncture therapy
The benefits of acupuncture, which has a history of more than 2000 years, are also worthy of attention in type 2 diabetes prevention and treatment [ 132 ]. Sun Simiao suggested that moxibustion and acupuncture should be performed in the early stage of Xiao Ke [ 133 ]. A classic acupuncture treatment refers to needling 4–12 points and retaining them for 10 to 30 min, and some operations can be conducted to enhance its effect during this time, such as stimulating the needles manually or electrically [ 134 ]. For type 2 diabetes treatment, acupuncture therapy was included and recommended in the guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2020 Edition) issued by the Chinese Medical Association for the first time [ 135 ].
The primary prevention of type 2 diabetes is mainly targeted at the prediabetic population. A randomized controlled trial evaluated the therapeutic efficacy of point application for senile IGT. Among 64 participants, they were randomly divided into two groups: the control group received dietary intervention while the intervention group was given point application. After 2 courses of treatment, the 2hPG obviously decreased in both groups, with a lower level in the experimental group than in the control group [ 136 ]. A pilot randomized study made a comparison between the efficacy of transcutaneous auricular vagus nerve stimulation (taVNS) and pseudo stimulus in patients with IGT. The results showed that there was a significant decline in measures of FPG, 2hPG, and HbAlc in participants treated with taVNS. Only two patients experienced dizziness during or after the treatment and they could completely recover from this uncomfortable feeling after stopping the therapy [ 137 ].
However, in healthy volunteers, acupuncture did not significantly reduce random blood glucose levels [ 138 ], indicating that acupuncture does not cause hypoglycemia in normal people. Although the available evidence is not strong enough to completely prove that acupuncture intervention in prediabetes reduces the proportion of its turning into type 2 diabetes, with the characteristics of the effectiveness have been proven to some extent, easy to operate and only slight risk of mild side effects, acupuncture is a promising approach to treat prediabetes and prevent type 2 diabetes.
Acupuncture, including typical acupuncture, laser acupuncture, ear acupuncture, herbal acupuncture, electroacupuncture and transcutaneous electrical nerve stimulation, has had the potential for the secondary prevention of type 2 diabetes. It could not only show the hypoglycemic effect, reducing FPG, 2hPG and HbA1c [ 139 , 140 , 141 , 142 , 143 , 144 ], but also be helpful for controlling blood glucose, which is better than the control group in continuous glucose monitoring [ 145 ]. Besides, auricular acupuncture, improving circulatory conditions and plantar temperature of patients with type 2 diabetes effectively, attributes a preventive effect on the treatment of diabetic foot [ 146 ]. It suggested the possibility of acupuncture in preventing the occurrence and exacerbation of diabetic complications.
At present, some clinical evidence for acupuncture improving type 2 diabetes related complications mainly focuses on diabetic peripheral neuropathy [ 147 , 148 , 149 , 150 , 151 ] and diabetic gastroparesis [ 152 , 153 ]. A recent study of 172 patients with type 2 diabetes induced diabetic peripheral neuropathy evaluated the effects of needle acupuncture, laser acupuncture, or placebo laser acupuncture for them. Comparing needle acupuncture to placebo, sural sensory nerve action potential sural and tibial nerve conduction velocities were significantly improved, and needle acupuncture produced a curative effect earlier than laser acupuncture. In addition, improvement in nerve conduction studies values may prove structural nerve regeneration after acupuncture [ 148 ]. For patients with diabetic gastroparesis, both classical needle acupuncture and electroacupuncture have been demonstrated to improve clinical symptoms and reduce gastric emptying time or gastric half-emptying time [ 152 , 153 ].
Studies have proposed that impaired parasympathetic function existed in prediabetes and was aggravated as the disease developed into diabetes [ 154 ]. Immune dysregulation and excessive proinflammatory responses were regulated by the vagus through inflammatory reflex, which is related to the pathogenesis of insulin resistance and the onset of type 2 diabetes [ 155 ]. Adequate vagus nerve activity may reduce the incidence of metabolic syndromes, having an important preventative and therapeutic meaning for type 2 diabetes [ 156 ]. Thus, acupuncture may prevent type 2 diabetes by driving the vagal-adrenal axis and producing anti-inflammatory effects [ 157 , 158 ]. Besides, an avalanche of studies turned to understanding type 2 diabetes from gut flora. A research analyzed the fecal bacteria composition of type 2 diabetes and non-diabetic adults by real-time qPCR and tag-encoded amplicon pyrosequencing. Compared with the non-diabetic group, the percentages of phylum Firmicutes and class Clostridia were markedly decreased and class Betaproteobacteria was significantly enriched in the diabetic group. And a significant positive relevance with plasma glucose concentration was shown in the proportions of Bacteroidetes to Firmicutes as well as the proportions of Bacteroides-Prevotella group to C. coccoides-E. rectale group [ 159 ]. A plethora of researches have indicated gut microbiota dysbiosis not only predisposed type 2 diabetes but also shared a close relationship with a variety of diabetic complications, suggesting the approaches through modulating gut flora may have preventive and therapeutic effects on type 2 diabetes [ 160 , 161 , 162 ]. Some researchers started to interpret the esoteric TCM theory and its mechanism by intestinal flora, and regard gut flora as an approach to revealing TCM core connotation [ 163 ]. Acupuncture, as one of the TCM therapy methods, has been found to modulate the composition of intestinal flora in the progression of treating some diseases. [ 164 , 165 , 166 ]. Although there were few clinical trials exploring the mechanism of acupuncture in the management of diabetes from the perspective of intestinal flora, animal tests have manifested electroacupuncture was beneficial in increasing the diversity of gut flora and promoting colonic motility, which may be used to explain its hypoglycemic mechanism. [ 167 , 168 ].
The preventive ideas and methods of type 2 diabetes and its complications based on TCM theory, showing a strong concordance with contemporary medical views, provide several alternative nonpharmacological interventions, mainly including TCM diet recommendation, TCM exercise, TCM emotional treatment and acupuncture therapy. These TCM non-drug interventions were effective in having hypoglycemic effects in patients with prediabetes or type 2 diabetes, reducing the risk of type 2 diabetes and diabetic complication, delaying its progression and improving the life quality of these patients. There were no significant differences in adverse effects between the TCM and the control or other intervention groups. However, the methodological quality of some studies involving TCM in this article was low and the meta-analysis of TCM mentioned also suggested that most pooled clinical trials were of low methodological quality. Therefore, high-quality, large-scale randomized controlled trials involving safety assessment should be conducted before any definitive conclusions can be come on whether TCM approaches are effective and safe in preventing type 2 diabetes. Besides, given its strong potential to prevent type 2 diabetes, TCM mechanism in this regard deserves further study and exploration.
Availability of data and materials
Not applicable.
Abbreviations
Dietary approaches to stop hypertension
Diabetic foot
Diabetic gastroparesis
Diabetic peripheral neuropathy
Diabetes prevention program
Diabetes specific quality of life scale
Fasting plasma glucose
Hamilton anxiety scale
Hamilton depression rating scale
Glycated hemoglobin
Impaired fasting glucose
Impaired glucose tolerance
Lipopolysaccharide
Scores of self-rating anxiety scale
Self-rating depression scale
Transcutaneous auricular vagus nerve stimulation
- Traditional Chinese medicine
2-h postload glucose
International Diabetes Federation. IDF Diabetes Atlas, 10th edn. Brussels, Belgium. 2021. https://www.diabetesatlas.org .
Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. part 1: diagnosis and classification of diabetes mellitus. provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–53.
Article CAS PubMed Google Scholar
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. Classification and diagnosis of Diabetes: standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):19–S40. https://doi.org/10.2337/dc23-S002 .
Article Google Scholar
World Health Organization. HEARTS D: diagnosis and management of type 2 diabetes. Geneva: World Health Organization; 2020.
Google Scholar
World Health Organization. Use of glycated haemoglobin (HbA1c) in diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. Geneva: World Health Organization; 2011.
American Diabetes Association. Diagnosis and classification of Diabetes Mellitus. Diabetes Care. 2011;34(Supplement1):62–9. https://doi.org/10.2337/dc11-S062 .
Article CAS Google Scholar
Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for Diabetes development. Lancet. 2012;379(9833):2279–90. https://doi.org/10.1016/S0140-6736(12)60283-9 .
Article PubMed PubMed Central Google Scholar
Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, et al. The long-term effect of lifestyle interventions to prevent Diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008;371(9626):1783–9. https://doi.org/10.1016/S0140-6736(08)60766-7 .
Article PubMed Google Scholar
Zhang X, Gregg EW, Williamson DF, Barker LE, Thomas W, Bullard KM, et al. A1C level and future risk of Diabetes: a systematic review. Diabetes Care. 2010;33(7):1665–73. https://doi.org/10.2337/dc09-1939 .
Article CAS PubMed PubMed Central Google Scholar
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 Diabetes Mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50. https://doi.org/10.1056/nejm200105033441801 .
Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in Diabetes risk: results from the Diabetes Prevention Program outcomes Study. Lancet. 2012;379(9833):2243–51. https://doi.org/10.1016/s0140-6736(12)60525-x .
Gregg EW, Chen H, Wagenknecht LE, Clark JM, Delahanty LM, Bantle J, et al. Association of an intensive lifestyle intervention with remission of type 2 Diabetes. JAMA. 2012;308(23):2489–96. https://doi.org/10.1001/jama.2012.67929 .
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level Diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. https://doi.org/10.1016/j.diabres.2021.109119 .
Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL, Sacre JW, Karuranga S, et al. IDF Diabetes Atlas: global estimates of undiagnosed Diabetes in adults for 2021. Diabetes Res Clin Pract. 2022;183:109118. https://doi.org/10.1016/j.diabres.2021.109118 .
Hao PP, Jiang F, Chen YG, Yang J, Zhang K, Zhang MX, et al. Traditional Chinese medication for Cardiovascular Disease. Nat Rev Cardiol. 2015;12(2):115–22. https://doi.org/10.1038/nrcardio.2014.177 .
Chen KJ, Lu AP. Situation of integrative medicine in China: results from a national survey in 2004. Chin J Integr Med. 2006;12(3):161–5. https://doi.org/10.1007/bf02836514 .
Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with Cardiovascular Diseases. J Am Coll Cardiol. 2010;55(6):515–25. https://doi.org/10.1016/j.jacc.2009.07.074 .
Yen L, Jowsey T, McRae IS. Consultations with complementary and alternative medicine practitioners by older australians: results from a national survey. BMC Complement Altern Med. 2013;13:73. https://doi.org/10.1186/1472-6882-13-73 .
Tian J, Jin D, Bao Q, Ding Q, Zhang H, Gao Z, et al. Evidence and potential mechanisms of traditional Chinese medicine for the treatment of type 2 Diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2019;21(8):1801–16. https://doi.org/10.1111/dom.13760 .
Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, et al. Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21176275 .
Fletcher B, Gulanick M, Lamendola C. Risk factors for type 2 Diabetes Mellitus. J Cardiovasc Nurs. 2002;16(2):17–23. https://doi.org/10.1097/00005082-200201000-00003 .
Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 Diabetes Mellitus: an exposure-wide umbrella review of meta-analyses. PLoS ONE. 2018;13(3):e0194127. https://doi.org/10.1371/journal.pone.0194127 .
Duschek E, Forer L, Schonherr S, Gieger C, Peters A, Kronenberg F, et al. A polygenic and family risk score are both independently associated with risk of type 2 Diabetes in a population-based study. Sci Rep. 2023;13(1):4805. https://doi.org/10.1038/s41598-023-31496-w .
Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17(2):179–88. https://doi.org/10.1038/nm.2279 .
Tahrani AA, Morton J. Benefits of weight loss of 10% or more in patients with overweight or obesity: a review. Obes (Silver Spring). 2022;30(4):802–40. https://doi.org/10.1002/oby.23371 .
Hosseini F, Jayedi A, Khan TA, Shab-Bidar S. Dietary carbohydrate and the risk of type 2 Diabetes: an updated systematic review and dose-response meta-analysis of prospective cohort studies. Sci Rep. 2022;12(1):2491. https://doi.org/10.1038/s41598-022-06212-9 .
Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, et al. Alternative dietary indices both strongly predict risk of chronic Disease. J Nutr. 2012;142(6):1009–18. https://doi.org/10.3945/jn.111.157222 .
Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic Disease. Nature. 2008;454(7203):463–9. https://doi.org/10.1038/nature07206 .
Liu LL, Yi JP, Beyer J, Mayer-Davis EJ, Dolan LM, Dabelea DM, et al. Type 1 and type 2 Diabetes in Asian and Pacific Islander U.S. youth: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(Suppl 2):133–40. https://doi.org/10.2337/dc09-S205 .
Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, et al. Elevated rates of Diabetes in Pacific islanders and Asian subgroups: the Diabetes study of Northern California (DISTANCE). Diabetes Care. 2013;36(3):574–9. https://doi.org/10.2337/dc12-0722 .
Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 Diabetes. Lancet. 2022;400(10365):1803–20. https://doi.org/10.1016/S0140-6736(22)01655-5 .
Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 Diabetes Mellitus. Diabetes. 2009;58(4):773–95. https://doi.org/10.2337/db09-9028 .
Schwartz SS, Epstein S, Corkey BE, Grant SF, Gavin JR, Aguilar RB. The Time is right for a new classification system for diabetes: rationale and implications of the beta-cell-centric classification schema. Diabetes Care. 2016;39(2):179–86. https://doi.org/10.2337/dc15-1585 .
Jia W, Weng J, Zhu D, Ji L, Lu J, Zhou Z, et al. Standards of medical care for type 2 Diabetes in China 2019. Diabetes Metab Res Rev. 2019;35(6):e3158. https://doi.org/10.1002/dmrr.3158 .
Tong XL, Dong L, Chen L, Zhen Z. Treatment of Diabetes using traditional Chinese medicine: past, present and future. Am J Chin Med. 2012;40(5):877–86. https://doi.org/10.1142/S0192415X12500656 .
Bauman A, St George A, Diabetes. T2DM–will tertiary prevention solve the problem? Nat Rev Endocrinol. 2013;9(4):190–2. https://doi.org/10.1038/nrendo.2013.44 .
Unschuld PU, Huang Tessenow H, Wen Di Nei Jing Su. An annotated translation of Huang Di’s inner classic - basic questions. Berkeley: University of California Press; 2011. p. 57.
Liang F, Koya D. Acupuncture: is it effective for treatment of insulin resistance? Diabetes Obes Metab. 2010;12(7):555–69. https://doi.org/10.1111/j.1463-1326.2009.01192.x .
Shi L, Ni Q. Treating Disease before its onset in Treatise on Febrile and miscellaneous Diseases and its application in Tertiary Prevention of Diabetes Mellitus. Liaoning J Traditional Chin Med. 2018;45(07):1383–6. https://doi.org/10.13192/j.issn.1000-1719.2018.07.013 .
Schwarz PE, Greaves CJ, Lindström J, Yates T, Davies MJ. Nonpharmacological interventions for the prevention of type 2 Diabetes Mellitus. Nat Rev Endocrinol. 2012;8(6):363–73. https://doi.org/10.1038/nrendo.2011.232 .
Tuomilehto J, Schwarz P, Lindstrom J. Long-term benefits from lifestyle interventions for type 2 diabetes prevention: time to expand the efforts. Diabetes Care. 2011;34:2210–4. https://doi.org/10.2337/dc11-s222 .
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537–44. https://doi.org/10.2337/diacare.20.4.537 .
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, et al. Sustained reduction in the incidence of type 2 Diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368(9548):1673–9. https://doi.org/10.1016/s0140-6736(06)69701-8 .
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 Diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. https://doi.org/10.1056/NEJMoa012512 .
Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, et al. 10-year follow-up of Diabetes incidence and weight loss in the Diabetes Prevention Program outcomes Study. Lancet. 2009;374(9702):1677–86. https://doi.org/10.1016/s0140-6736(09)61457-4 .
Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, et al. Nutrition Therapy for adults with Diabetes or Prediabetes: a Consensus Report. Diabetes Care. 2019;42(5):731–54. https://doi.org/10.2337/dci19-0014 .
General Office of National Health Commission of the People's Republic of China. Dietary Guidelines for Adults with Hyperlipidemia. (2023 edition). http://www.nhc.gov.cn/sps/s7887k/202301/0e55a01df50c47d9a4a43db026e3afc3.shtml.shtml . Accessed 18 January 2023.
Dou Z, Xia Y, Zhang J, Li Y, Zhang Y, Zhao L, et al. Syndrome differentiation and treatment regularity in traditional Chinese medicine for type 2 diabetes: a text mining analysis. Front Endocrinol 2021;12:728032. https://doi.org/10.3389/fendo.2021.728032 .
Li WL, Zheng HC, Bukuru J, De Kimpe N. Natural medicines used in the traditional Chinese medical system for therapy of Diabetes Mellitus. J Ethnopharmacol. 2004;92(1):1–21. https://doi.org/10.1016/j.jep.2003.12.031 .
Wu T, Yue R, He M, Shaoqi W. Medication rule analysis of traditional Chinese Medicine formulas in the treatment of Prediabetes based on Data Mining. Pharmacol Clin Chin Materia Med. 2021;37(03):190–5.
Yang Q, Jing L, Li J, Wang Z, Li Z, Qin J, et al. Analysis of the medication rule of traditional Chinese medicine in the treatment of impaired glucose tolerance based on data mining. China Med. 2021;16(11):1678–82.
Huang W, Tan X, Deng X. Application of differential dietary nutrition intervention in 40 cases with impaired glucose tolerance. Chin J Ethnomed Ethnopharmacy. 2016;25(02):126–7.
Yang B, Dai N, Wu Y. Effect of Jianpi Qushi Diet recipe on pre-diabetes patients with phlegm-dampness constitution. Clin J Chin Med. 2021;13(15):31–3.
CAS Google Scholar
Dai Y, Liu W, Pang S, Yang L, Li M. A systematic evaluation of the influence of traditional Chinese medicine diet on blood glucose and quality of life in type 2 Diabetes patients. J Guangxi Univ Chin Med. 2019;22(01):140–6.
Ye B, Lin L, Zheng K. Exploration on the application of Dietotherapy in the treatment of Diabetes. Chin Med Mod Distance Educ China. 2022;20(03):199–202.
Crump C, Sundquist J, Winkleby MA, Sieh W, Sundquist K. Physical fitness among Swedish Military conscripts and Long-Term risk for type 2 Diabetes Mellitus: a Cohort Study. Ann Intern Med. 2016;164(9):577–84. https://doi.org/10.7326/m15-2002 .
Kirwan JP, Solomon TP, Wojta DM, Staten MA, Holloszy JO. Effects of 7 days of exercise training on insulin sensitivity and responsiveness in type 2 Diabetes Mellitus. Am J Physiol Endocrinol Metab. 2009;297(1):E151–6. https://doi.org/10.1152/ajpendo.00210.2009 .
Battista F, Ermolao A, van Baak MA, Beaulieu K, Blundell JE, Busetto L, et al. Effect of exercise on cardiometabolic health of adults with overweight or obesity: focus on blood pressure, insulin resistance, and intrahepatic fat-A systematic review and meta-analysis. Obes Rev. 2021;22(Suppl 4):e13269. https://doi.org/10.1111/obr.13269 .
Heiskanen MA, Motiani KK, Mari A, Saunavaara V, Eskelinen JJ, Virtanen KA, et al. Exercise training decreases pancreatic fat content and improves beta cell function regardless of baseline glucose tolerance: a randomised controlled trial. Diabetologia. 2018;61(8):1817–28. https://doi.org/10.1007/s00125-018-4627-x .
Motiani KK, Collado MC, Eskelinen JJ, Virtanen KA, Loyttyniemi E, Salminen S, et al. Exercise Training modulates Gut Microbiota Profile and improves endotoxemia. Med Sci Sports Exerc. 2020;52(1):94–104. https://doi.org/10.1249/MSS.0000000000002112 .
The Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–71. https://doi.org/10.2337/diacare.25.12.2165 .
Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/Physical activity in individuals with type 2 Diabetes: a Consensus Statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;54(2):353–68. https://doi.org/10.1249/mss.0000000000002800 .
Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 Diabetes. Cleve Clin J Med. 2017;84(7 Suppl 1):15–s21. https://doi.org/10.3949/ccjm.84.s1.03 .
Jiang Y, Zou J. Analysis of the TCM theory of traditional Chinese health exercise. J Sport Health Sci. 2013;2(4):204–8. https://doi.org/10.1016/j.jshs.2013.03.008 .
Siu PM, Yu AP, Yu DS, Hui SS, Woo J. Effectiveness of Tai Chi training to alleviate metabolic syndrome in abdominal obese older adults: a randomised controlled trial. The Lancet. 2017. https://doi.org/10.1016/s0140-6736(17)33149-5 .
Chinese Diabetes Society. Guidelines for the prevention and control of type 2 Diabetes in China(2017 Edition). Chin J Practical Intern Med. 2018;38(04):292–344.
Shi H, Wang S, Zhang Y, Liu P, Dong C, Wang D, et al. The effects of Tai Chi exercise for patients with type 2 diabetes mellitus: an overview of systematic reviews and meta-analyses. J Diabetes Res. 2022;2022:6587221.
Yu DD, You LZ, Huang WQ, Cao H, Wang FJ, Tang XQ, et al. Effects of traditional Chinese exercises on blood glucose and hemoglobin A1c levels in patients with prediabetes: a systematic review and meta-analysis. J Integr Med. 2020;18(4):292–302. https://doi.org/10.1016/j.joim.2020.04.003 .
Song G, Chen C, Zhang J, Chang L, Zhu D, Wang X. Association of traditional Chinese exercises with glycemic responses in people with type 2 Diabetes: a systematic review and meta-analysis of randomized controlled trials. J Sport Health Sci. 2018;7(4):442–52. https://doi.org/10.1016/j.jshs.2018.08.004 .
Lauche R, Peng W, Ferguson C, Cramer H, Frawley J, Adams J, et al. Efficacy of Tai Chi and qigong for the prevention of Stroke and Stroke risk factors: a systematic review with meta-analysis. Med (Baltim). 2017;96(45):e8517. https://doi.org/10.1097/md.0000000000008517 .
Meng D, Chunyan W, Xiaosheng D, Xiangren Y. The effects of Qigong on type 2 diabetes mellitus: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2018;2018:8182938. https://doi.org/10.1155/2018/8182938 .
Chao M, Wang C, Dong X, Ding M. The effects of Tai Chi on type 2 diabetes mellitus: a meta-analysis. J Diabetes Res. 2018;2018:7350567. https://doi.org/10.1155/2018/7350567 .
Xinzheng W, Fanyuan J, Xiaodong W. The effects of Tai Chi on glucose and lipid metabolism in patients with Diabetes Mellitus: a meta-analysis. Complement Ther Med. 2022;71:102871. https://doi.org/10.1016/j.ctim.2022.102871 .
Liu YN, Wang L, Fan X, Liu S, Wu Q, Qian YL. A meta-analysis of the effects of tai chi on glucose and lipid metabolism in middle-aged and elderly diabetic patients: evidence from randomized controlled trials. Evid Based Complement Alternat Med. 2021;2021:6699935. https://doi.org/10.1155/2021/6699935 .
Wen J, Lin T, Cai Y, Chen Q, Chen Y, Ren Y, et al. Baduanjin exercise for type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2017;2017:8378219.
Wang Y, Yan J, Zhang P, Yang P, Zhang W, Lu M. Tai Chi Program to Improve Glucose Control and Quality of Life for the Elderly with type 2 Diabetes: a Meta-analysis. Inquiry. 2022;59:469580211067934. https://doi.org/10.1177/00469580211067934 .
Guo S, Xu Y, Qin J, Chen Y, You Y, Tao J, et al. Effect of Tai Chi on glycaemic control, lipid metabolism and body composition in adults with type 2 Diabetes: a meta-analysis and systematic review. J Rehabil Med. 2021;53(3):jrm00165. https://doi.org/10.2340/16501977-2799 .
Kong L, Ren J, Fang S, He T, Zhou X, Fang M. Effects of traditional Chinese mind-body exercise-baduanjin for type 2 Diabetes on psychological well-being: a systematic review and meta-analysis. Front Public Health. 2022;10:923411. https://doi.org/10.3389/fpubh.2022.923411 .
Ma X, Li M, Liu L, Lei F, Wang L, Xiao W, et al. A randomized controlled trial of Baduanjin exercise to reduce the risk of atherosclerotic Cardiovascular Disease in patients with prediabetes. Sci Rep. 2022;12(1):19338. https://doi.org/10.1038/s41598-022-22896-5 .
Huang Y, Han J, Gu Q, Cai Y, Li J, Wang S, et al. Effect of Yijinjing combined with elastic band exercise on muscle mass and function in middle-aged and elderly patients with prediabetes: a randomized controlled trial. Front Med 2022;9:990100. https://doi.org/10.3389/fmed.2022.990100 .
Chen Y, Qin J, Tao L, Liu Z, Huang J, Liu W, et al. Effects of Tai Chi Chuan on cognitive function in adults 60 years or older with type 2 Diabetes and mild cognitive impairment in China: a Randomized Clinical Trial. JAMA Netw Open. 2023;6(4):e237004. https://doi.org/10.1001/jamanetworkopen.2023.7004 .
Hu S, Hu Y, Long P, Li P, Chen P, Wang X. The effect of Tai Chi intervention on NLRP3 and its related antiviral inflammatory factors in the serum of patients with pre-diabetes. Front Immunol. 2022;13:1026509. https://doi.org/10.3389/fimmu.2022.1026509 .
Yeh SH, Chuang H, Lin LW, Hsiao CY, Wang PW, Yang KD. Tai Chi Chuan exercise decreases A1C levels along with increase of regulatory T-cells and decrease of cytotoxic T-cell population in type 2 diabetic patients. Diabetes Care. 2007;30(3):716–8. https://doi.org/10.2337/dc06-1507 .
An T, He ZC, Zhang XQ, Li J, Chen AL, Tan F, et al. Baduanjin exerts anti-diabetic and anti-depression effects by regulating the expression of mRNA, lncRNA, and circRNA. Chin Med. 2019;14:3. https://doi.org/10.1186/s13020-019-0225-1 .
Hackett RA, Steptoe A. Type 2 Diabetes Mellitus and psychological stress - a modifiable risk factor. Nat Rev Endocrinol. 2017;13(9):547–60. https://doi.org/10.1038/nrendo.2017.64 .
Lindekilde N, Rutters F, Erik Henriksen J, Lasgaard M, Schram MT, Rubin KH, et al. Psychiatric disorders as risk factors for type 2 Diabetes: an umbrella review of systematic reviews with and without meta-analyses. Diabetes Res Clin Pract. 2021;176:108855. https://doi.org/10.1016/j.diabres.2021.108855 .
Lindekilde N, Scheuer SH, Diaz LJ, Rubin KH, Plana-Ripoll O, Henriksen JE, et al. Risk of developing type 2 Diabetes in individuals with a Psychiatric disorder: a Nationwide Register-based Cohort Study. Diabetes Care. 2022;45(3):724–33. https://doi.org/10.2337/dc21-1864 .
Rubin RR, Peyrot M. Was Willis right? Thoughts on the interaction of depression and Diabetes. Diabetes Metab Res Rev. 2002;18(3):173–5. https://doi.org/10.1002/dmrr.292 .
Kolb H, Martin S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 Diabetes. BMC Med. 2017;15(1):131. https://doi.org/10.1186/s12916-017-0901-x .
Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 Diabetes Mellitus. A meta-analysis. Diabetologia. 2006;49(5):837–45. https://doi.org/10.1007/s00125-006-0159-x .
Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 Diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31(12):2383–90. https://doi.org/10.2337/dc08-0985 .
Tabák AG, Akbaraly TN, Batty GD, Kivimäki M. Depression and type 2 Diabetes: a causal association? Lancet Diabetes Endocrinol. 2014;2(3):236–45. https://doi.org/10.1016/s2213-8587(13)70139-6 .
Graham EA, Deschênes SS, Khalil MN, Danna S, Filion KB, Schmitz N. Measures of depression and risk of type 2 Diabetes: a systematic review and meta-analysis. J Affect Disord. 2020;265:224–32. https://doi.org/10.1016/j.jad.2020.01.053 .
Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Roux AVD, et al. Examining a Bidirectional Association between Depressive Symptoms and Diabetes. JAMA. 2008;299(23):2751–9. https://doi.org/10.1001/jama.299.23.2751 .
Moulton CD, Pickup JC, Ismail K. The link between depression and Diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3(6):461–71. https://doi.org/10.1016/s2213-8587(15)00134-5 .
Smith KJ, Deschênes SS, Schmitz N. Investigating the longitudinal association between Diabetes and anxiety: a systematic review and meta-analysis. Diabet Med. 2018;35(6):677–93. https://doi.org/10.1111/dme.13606 .
Mersha AG, Tollosa DN, Bagade T, Eftekhari P. A bidirectional relationship between Diabetes Mellitus and anxiety: a systematic review and meta-analysis. J Psychosom Res. 2022;162:110991. https://doi.org/10.1016/j.jpsychores.2022.110991 .
Jiang L, Atasoy S, Johar H, Herder C, Peters A, Kruse J, et al. Anxiety boosts progression of prediabetes to type 2 Diabetes: findings from the prospective Cooperative Health Research in the region of Augsburg F4 and FF4 studies. Diabet Med. 2020;37(10):1737–41. https://doi.org/10.1111/dme.14232 .
Deschenes SS, McInerney A, Nearchou F, Byrne B, Nouwen A, Schmitz N. Prediabetes and the risk of type 2 diabetes: Investigating the roles of depressive and anxiety symptoms in the lifelines cohort study. Diabet Med. 2023. https://doi.org/10.1111/dme.15061 .
Vancampfort D, Rosenbaum S, Ward PB, Steel Z, Lederman O, Lamwaka AV, et al. Type 2 Diabetes among people with posttraumatic stress disorder: systematic review and Meta-analysis. Psychosom Med. 2016;78(4):465–73. https://doi.org/10.1097/psy.0000000000000297 .
Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. 2019;4(10):e517–28. https://doi.org/10.1016/s2468-2667(19)30145-8 .
Gaston SA, Riley NM, Parks CG, Woo JMP, Sandler DP, Jackson CL. Racial/Ethnic Differences in Associations between Traumatic Childhood experiences and both metabolic syndrome prevalence and type 2 Diabetes risk among a cohort of U.S. women. Diabetes Care. 2023;46(2):341–50. https://doi.org/10.2337/dc22-1486 .
Nyberg ST, Fransson EI, Heikkilä K, Ahola K, Alfredsson L, Bjorner JB, et al. Job strain as a risk factor for type 2 Diabetes: a pooled analysis of 124,808 men and women. Diabetes Care. 2014;37(8):2268–75. https://doi.org/10.2337/dc13-2936 .
Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for Diabetes development: systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. https://doi.org/10.1016/j.smrv.2015.10.002 .
Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71(10):1259–72. https://doi.org/10.4088/JCP.09r05346blu .
Semenkovich K, Brown ME, Svrakic DM, Lustman PJ. Depression in type 2 Diabetes Mellitus: prevalence, impact, and treatment. Drugs. 2015;75(6):577–87. https://doi.org/10.1007/s40265-015-0347-4 .
Barnard K, Peveler RC, Holt RI. Antidepressant medication as a risk factor for type 2 Diabetes and impaired glucose regulation: systematic review. Diabetes Care. 2013;36(10):3337–45. https://doi.org/10.2337/dc13-0560 .
Daimon M, Kamba A, Murakami H, Mizushiri S, Osonoi S, Matsuki K, et al. Dominance of the hypothalamus-pituitary-adrenal axis over the renin-angiotensin-aldosterone system is a risk factor for decreased insulin secretion. Sci Rep. 2017;7(1):11360. https://doi.org/10.1038/s41598-017-10815-y .
Otte C, Lenoci M, Metzler T, Yehuda R, Marmar CR, Neylan TC. Hypothalamic-pituitary-adrenal axis activity and sleep in posttraumatic stress disorder. Neuropsychopharmacology. 2005;30(6):1173–80. https://doi.org/10.1038/sj.npp.1300676 .
Joseph JJ, Golden SH. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 Diabetes Mellitus. Ann N Y Acad Sci. 2017;1391(1):20–34. https://doi.org/10.1111/nyas.13217 .
Kyrou I, Tsigos C. Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol. 2009;9(6):787–93.
Sun Y, Qi X. Excessive seven emotions impairing qi of five zang-viscera with the theory of chill and Fever. China J Traditional Chin Med Pharm. 2018;33(01):55–7.
Momen NC, Plana-Ripoll O, Agerbo E, Benros ME, Børglum AD, Christensen MK, et al. Association between Mental disorders and subsequent medical conditions. N Engl J Med. 2020;382(18):1721–31. https://doi.org/10.1056/NEJMoa1915784 .
Wang YW, Dehui. Prevention of Diabetes Mellitus in the perspective of emotion. J Liaoning Univ Traditional Chin Med. 2010;12(6):98–100. https://doi.org/10.13194/j.jlunivtcm.2010.06.100.wangy.123 .
Min W, Sun X, Tang N, Zhang Y, Luo F, Zhu M, et al. A new model for the treatment of type 2 Diabetes Mellitus based on rhythm regulations under the framework of psychosomatic medicine: a real-world study. Sci Rep. 2023;13(1):1047. https://doi.org/10.1038/s41598-023-28278-9 .
Yoon JM, Cho EG, Lee HK, Park SM. Antidepressant use and Diabetes Mellitus risk: a meta-analysis. Korean J Fam Med. 2013;34(4):228–40. https://doi.org/10.4082/kjfm.2013.34.4.228 .
Ma L. Influence of Chinese emotional therapy combined with health education on medication compliance of diabetic patients. World Latest Medicine Information. 2016;16(98):143–4.
Qian D, Guo Z. TCM mental nursing on the fluctuation of blood glucose of patients with type 2 Diabetes. J Changchun Univ Chin Med. 2016;32(02):371–2. https://doi.org/10.13463/j.cnki.cczyy.2016.02.055 .
He J, Pan R, Cai Y, Chen S, Guo S. The influence of emotional nursing of traditional Chinese medicine on self-management ability and quality of life of diabetic patients. Diabetes New World. 2020;23(07):155–6.
Liu L, Liang Z, Pan Y. Application of traditional Chinese medicine emotional nursing in Elderly Diabetes. J Practical Traditional Chin Intern Med. 2023;37(01):95–7.
Ma H. Observation on the effect of traditional Chinese emotional nursing on negative emotion, self-efficacy and nursing compliance in elderly patients with type 2 Diabetes. Qinghai Med J. 2022;52(05):14–6.
Peng W, Yu Y, Cheng Y. Effect of emotional nursing on negative emotion and sleep quality in elderly patients with type 2 Diabetes. Diabetes New World. 2019;22(08):149–50.
Lu R, Li Y, Li Z, Zhang Q. The clinical effect of traditional Chinese medicine emotional nursing on patients with type 2 Diabetes Mellitus accompanied by anxiety and depression. Qinghai Med J. 2021;51(05):32–4.
Li X. Application Effect of TCM Emotional Nursing on Elderly Diabetic Patients with Depression. Diabetes New World. 2020;23(13):158–60.
Li N. Application of emotional nursing of traditional Chinese medicine in anxiety of diabetic patients. J Xuzhou Med Univ. 2019;39(10):774–6.
Zuo R. Application effect of emotion nursing of traditional Chinese medicine on elderly diabetic patients with depression. Chin Community Doctors. 2018;34(18):142–3.
Li C, Sun J, Zheng X, Dai Q, Sun J, Miao J. Study on TCM emotional intervention on type 2 Diabetes patients complicated with depression. Chin Gen Pract Nurs. 2014;12(08):673–4.
Xiao L, Yang M. Influence of emotional nursing on negative emotions and self-behavior management of elderly patients with diabetic Nephropathy treated by long-term hemodialysis. China Mod Med. 2020;27(08):228–31.
Zhang F, Cao N, Wang Y. Effect of emotional nursing interveniotn on compliance behavior of traditional Chinese medicine decoction and quality of life in patients with diabetic Nephropathy. Lab Med Clin. 2019;16(08):1110–2.
Ma P. Nursing study of emotional nursing intervention combined with routine nursing in diabetic foot patients and its influence on prognosis. Biped and Health. 2017;26(23):75–.
Li F, Shi R, Yang H, Zhang N. The application of TCM emotional nursing in treating diabetic neurogenic bladder. Clin J Chin Med. 2017;9(26):66–8.
Wei JP, Wang QH, Zheng HJ, Wei F. Research Progress on non-drug treatment for blood glucose control of type 2 Diabetes Mellitus. Chin J Integr Med. 2018;24(10):723–7. https://doi.org/10.1007/s11655-018-2844-2 .
Li B, Zhao N, Sun W, Zhang Z, Yang S. Practice and benefits of acupuncture and moxibustion in the Prevention and Treatment of type 2 Diabetes. Chin J Integr Traditional Western Med. 2022;42(04):492–6.
Covington MB. Traditional Chinese medicine in the treatment of Diabetes. Diabetes Spectr. 2001;14(3):154.
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 Diabetes Mellitus in China(2020 edition)(part 2). Chin J Practical Intern Med. 2021;41(08):668–95.
Wu Y, Fei M, He Y, Zhang C, Zheng W, Wu Y, et al. Clinical observation on senile patients with impaired glucose tolerance treated by point application. J Tradit Chin Med. 2006;26(2):110–2.
PubMed Google Scholar
Huang F, Dong J, Kong J, Wang H, Meng H, Spaeth RB, et al. Effect of transcutaneous auricular vagus nerve stimulation on impaired glucose tolerance: a pilot randomized study. BMC Complement Altern Med. 2014;14:203. https://doi.org/10.1186/1472-6882-14-203 .
Mohanty S, Mooventhan A, Manjunath NK. Effect of needling at CV-12 (Zhongwan) on blood glucose levels in healthy volunteers: a pilot randomized Placebo Controlled Trial. J Acupunct Meridian Stud. 2016;9(6):307–10. https://doi.org/10.1016/j.jams.2016.08.002 .
Zhang R-x, Li H, Xiong J-w, Jiang Y-q, Li Y-t, Zhang J-b. Thirty two cases of type 2 Diabetes Mellitus of qi and Yin deficiency treated with laser acupuncture. World J Acupunct - Moxibustion. 2021;31(4):320–3. https://doi.org/10.1016/j.wjam.2021.05.006 .
Zhou X, Chen J. Efficacy and Safety of acupuncture and related techniques for type 2 diabetes mellitus: a systematic review of 21 randomised controlled trials. Metabolism. 2021. https://doi.org/10.1016/j.metabol.2020.154519 .
Chen C, Liu J, Sun M, Liu W, Han J, Wang H. Acupuncture for type 2 Diabetes Mellitus: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2019;36:100–12. https://doi.org/10.1016/j.ctcp.2019.04.004 .
Lee SW, Nam MH, Lee BC. Herbal acupuncture for type 2 Diabetes: a meta-analysis. Exp Ther Med. 2017;13(6):3249–56. https://doi.org/10.3892/etm.2017.4379 .
Tjipto BW, Saputra K, Sutrisno TC. Effectiveness of acupuncture as an adjunctive therapy for Diabetes Mellitus: a Randomized Controlled Trial. Med Acupunct. 2014;26(6):341–5. https://doi.org/10.1089/acu.2014.1058 .
Zhiyuan W, Ming Y, Jie J, Yi W, Tiansheng H, Mingfen L, et al. Effect of transcutaneous electrical nerve stimulation at acupoints on patients with type 2 Diabetes Mellitus: a randomized controlled trial. J Tradit Chin Med. 2015;35(2):134–40. https://doi.org/10.1016/s0254-6272(15)30020-0 .
Vencio S, Caiado-Vencio I, Caiado A, Morgental D, Dantas LS, Caiado-Vencio R. Acute Effect of acupuncture on Glycemic Control in type 2 Diabetes measured by continuous glucose monitoring: a pilot study. Med Acupunct. 2021;33(1):65–70. https://doi.org/10.1089/acu.2020.1457 .
de Bacelar B, de Cassia Lopes Chaves E, de Sousa L, Machado Chianca TC, Carvalho Borges JB, Silva Vilela Terra AM, et al. The effects of auricular acupuncture on vascular parameters on the risk factors for diabetic foot: a randomized clinical trial. Complement Ther Clin Pract. 2021;44:101442. https://doi.org/10.1016/j.ctcp.2021.101442 .
Wang Z, Hou Y, Huang Y, Ju F, Liang Z, Li S. Clinical efficacy and safety of electro-acupuncture combined with beraprost sodium and α-lipoic acid for diabetic peripheral neuropathy. Am J Transl Res. 2022;14(1):612–22.
CAS PubMed PubMed Central Google Scholar
Meyer-Hamme G, Friedemann T, Greten J, Gerloff C, Schroeder S. Electrophysiologically verified effects of acupuncture on diabetic peripheral neuropathy in type 2 Diabetes: the randomized, partially double-blinded, controlled ACUDIN trial. J Diabetes. 2021;13(6):469–81. https://doi.org/10.1111/1753-0407.13130 .
Shin KM, Lee S, Lee EY, Kim CH, Kang JW, Lee CK, et al. Electroacupuncture for painful Diabetic Peripheral Neuropathy: a Multicenter, Randomized, Assessor-Blinded, Controlled Trial. Diabetes Care. 2018;41(10):e141–2. https://doi.org/10.2337/dc18-1254 .
Zhang C, Ma YX, Yan Y. Clinical effects of acupuncture for diabetic peripheral neuropathy. J Tradit Chin Med. 2010;30(1):13–4. https://doi.org/10.1016/s0254-6272(10)60003-9 .
Hamza MA, White PF, Craig WF, Ghoname ES, Ahmed HE, Proctor TJ, et al. Percutaneous electrical nerve stimulation: a novel analgesic therapy for diabetic neuropathic pain. Diabetes Care. 2000;23(3):365–70. https://doi.org/10.2337/diacare.23.3.365 .
Wang L. Clinical observation on acupuncture treatment in 35 cases of diabetic gastroparesis. J Tradit Chin Med. 2004;24(3):163–5.
CAS PubMed Google Scholar
Wang CP, Kao CH, Chen WK, Lo WY, Hsieh CL. A single-blinded, randomized pilot study evaluating effects of electroacupuncture in diabetic patients with symptoms suggestive of gastroparesis. J Altern Complement Med. 2008;14(7):833–9. https://doi.org/10.1089/acm.2008.0107 .
Hadad R, Akobe SF, Weber P, Madsen CV, Larsen BS, Madsbad S, et al. Parasympathetic tonus in type 2 Diabetes and pre-diabetes and its clinical implications. Sci Rep. 2022;12(1):18020. https://doi.org/10.1038/s41598-022-22675-2 .
Pavlov VA, Tracey KJ. The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat Reviews Endocrinol. 2012;8(12):743–54. https://doi.org/10.1038/nrendo.2012.189 .
De Couck M, Mravec B, Gidron Y. You may need the vagus nerve to understand pathophysiology and to treat Diseases. Clin Sci (Lond). 2012;122(7):323–8. https://doi.org/10.1042/cs20110299 .
Liu S, Wang Z, Su Y, Qi L, Yang W, Fu M, et al. A neuroanatomical basis for electroacupuncture to drive the vagal–adrenal axis. Nature. 2021;598(7882):641–5. https://doi.org/10.1038/s41586-021-04001-4 .
Liu S, Wang Z-F, Su Y-S, Ray RS, Jing X-H, Wang Y-Q, et al. Somatotopic organization and intensity dependence in driving distinct NPY-expressing sympathetic pathways by electroacupuncture. Neuron. 2020;108(3):436–50. e7.
Larsen N, Vogensen FK, Van Den Berg FW, Nielsen DS, Andreasen AS, Pedersen BK, et al. Gut microbiota in human adults with type 2 Diabetes differs from non-diabetic adults. PLoS ONE. 2010;5(2):e9085.
Iatcu CO, Steen A, Covasa M. Gut microbiota and complications of type-2 diabetes. Nutrients. 2022. https://doi.org/10.3390/nu14010166 .
Zhou Z, Sun B, Yu DS, Zhu CS. Gut microbiota: an important player in type 2 diabetes mellitus. Front Cell Infect Microbiol. 2022. https://doi.org/10.3389/fcimb.2022.834485 .
Ma QT, Li YQ, Li PF, Wang M, Wang JK, Tang ZY, et al. Research progress in the relationship between type 2 diabetes mellitus and intestinal flora. Biomed Pharmacother. 2019. https://doi.org/10.1016/j.biopha.2019.109138 .
Li X, Wu D, Niu J, Sun Y, Wang Q, Yang B, et al. Intestinal Flora: a pivotal role in Investigation of Traditional Chinese Medicine. Am J Chin Med. 2021;49(2):237–68. https://doi.org/10.1142/s0192415x21500130 .
Sheng J, Yang G, Jin X, Si C, Huang Y, Luo Z, et al. Electroacupuncture Combined with Diet Treatment has a therapeutic effect on perimenopausal patients with abdominal obesity by improving the Community structure of Intestinal Flora. Front Physiol. 2021;12:708588. https://doi.org/10.3389/fphys.2021.708588 .
Zheng Y, Jiang X, Gao Y, Yuan L, Wang X, Wu S, et al. Microbial profiles of patients with antipsychotic-related constipation treated with electroacupuncture. Front Med 2021;8:737713. https://doi.org/10.3389/fmed.2021.737713 .
Wang TQ, Li LR, Tan CX, Yang JW, Shi GX, Wang LQ, et al. Effect of electroacupuncture on gut microbiota in participants with knee osteoarthritis. Front Cell Infect Microbiol. 2021;11:597431. https://doi.org/10.3389/fcimb.2021.597431 .
Dou D, Chen QQ, Zhong ZQ, Xia XW, Ding WJ. Regulating the enteric nervous system against obesity in mice by Electroacupuncture. Neuroimmunomodulation. 2020;27(1):48–57. https://doi.org/10.1159/000506483 .
An J, Wang LL, Song SN, Tian LG, Liu QQ, Mei MH, et al. Electroacupuncture reduces blood glucose by regulating intestinal flora in type 2 diabetic mice. J Diabetes. 2022;14(10):695–710. https://doi.org/10.1111/1753-0407.13323 .
Download references
Acknowledgements
We thank Mr. Shimin Xiao for editing the figures. Prof. Yitao Wang serves as the Editor-in-Chief of Chinese Medicine .
This work was supported by the Macao Science and Technology Development Fund (001/2023/ALC and 0006/2020/AKP), the Research Fund of University of Macau (CPG2023-00028-ICMS), Guangxi Science and Technology Major Project (GUIKEAA22096029 and AA23023035), and Macao Young Scholars Program (AM2022022).
Author information
Authors and affiliations.
Macau Centre for Research and Development in Chinese Medicine, State Key Laboratory of Quality Research in Chinese Medicine, Institute of Chinese Medical Sciences, University of Macau, Macao, 999078, People’s Republic of China
Jingying Liu, Yitao Wang & Hua Luo
College of Pharmacy, Guangxi Medical University, Nanning, 530021, People’s Republic of China
Jinmin Zhao & Hua Luo
Guangxi University of Chinese Medicine, Nanning, 530001, People’s Republic of China
You can also search for this author in PubMed Google Scholar
Contributions
JL wrote this manuscript. CY and YW conceived and supervised the study. HL and JZ revised, organized, and supervised the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding authors
Correspondence to Jinmin Zhao or Hua Luo .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
All authors approved the final manuscript and the submission to this journal.
Competing interests
The authors declare they have no competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Liu, J., Yao, C., Wang, Y. et al. Non-drug interventions of traditional Chinese medicine in preventing type 2 diabetes: a review. Chin Med 18 , 151 (2023). https://doi.org/10.1186/s13020-023-00854-1
Download citation
Received : 12 July 2023
Accepted : 23 October 2023
Published : 14 November 2023
DOI : https://doi.org/10.1186/s13020-023-00854-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nonpharmacological intervention
Chinese Medicine
ISSN: 1749-8546
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Too little sleep raises risk of type 2 diabetes, new study finds
Adults who sleep only three to five hours per day are at higher risk of developing type 2 diabetes. This is demonstrated in a new study from Uppsala University, published in JAMA Network Open . It also shows that chronic sleep deprivation cannot be compensated by healthy eating alone.
"I generally recommend prioritising sleep, although I understand it's not always possible, especially as a parent of four teenagers," says Christian Benedict, Associate Professor and sleep researcher at the Department of Pharmaceutical Biosciences at Uppsala University and leading researcher behind the study.
He and a team of researchers have examined the link between type 2 diabetes and sleep deprivation. Type 2 diabetes affects the body's ability to process sugar (glucose), hindering insulin absorption and resulting in high blood sugar levels. A report from 2020 showed that over 462 million people suffer from this disease. Over time, it can cause serious damage, particularly to nerves and blood vessels, and thus represents an escalating public health problem globally.
"Previous research has shown that repeated short daily rest increases the risk of type 2 diabetes, while healthy dietary habits such as regularly eating fruit and vegetables can reduce the risk. However, it has remained unclear whether people who sleep too little can reduce their risk of developing type 2 diabetes by eating healthily," notes Diana Noga, a sleep researcher at the Department of Pharmaceutical Biosciences at Uppsala University.
The researchers therefore used data from one of the largest population databases in the world, the UK Biobank, in which nearly half a million participants from the UK have been genetically mapped and responded to questions on health and lifestyle. They followed the participants for over ten years and found that a sleep duration of between three and five hours was linked to a higher risk of developing type 2 diabetes.
In contrast, healthy eating habits led to a lower risk of developing the disease, but even people who ate healthily but slept less than six hours a day were still at higher risk of type 2 diabetes.
"Our results are the first to question whether a healthy diet can compensate for lack of sleep in terms of the risk of type 2 diabetes. They should not cause concern, but instead be seen as a reminder that sleep plays an important role in health," explains Benedict.
He also argues that the effects of sleep deprivation vary between individuals, depending on aspects such as genetics and a person's actual need for sleep.
- Insomnia Research
- Sleep Disorder Research
- Staying Healthy
- Sleep Disorders
- Obstructive Sleep Apnea
- Disorders and Syndromes
- Sleep deprivation
- Circadian rhythm sleep disorder
- Narcolepsy (sleep disorder)
- Delayed sleep phase syndrome
- Rapid eye movement
- Sleep apnea
- Sleep disorder
- Night terror
Story Source:
Materials provided by Uppsala University . Note: Content may be edited for style and length.
Journal Reference :
- Diana Aline Nôga, Elisa de Mello e Souza Meth, André Pekkola Pacheco, Xiao Tan, Jonathan Cedernaes, Lieve Thecla van Egmond, Pei Xue, Christian Benedict. Habitual Short Sleep Duration, Diet, and Development of Type 2 Diabetes in Adults . JAMA Network Open , 2024; 7 (3): e241147 DOI: 10.1001/jamanetworkopen.2024.1147
Cite This Page :
- Economic Losses from Climate Change
- AI-Generated Food Images Look Tastier
- Giant Volcano Discovered On Mars
- Weaving Wearable Electronics Into Fabrics
- Warming Seas: Deep Whirpools in Ocean Currents?
- Alaska Dinosaur Tracks Reveal Lush Environment
- A Coral Superhighway in the Indian Ocean
- Cheetahs' Unrivalled Speed: Size Matters
- Sand Ripples On Mars and Earth: New Theory
- Peering Into the Tendrils of NGC 604

IMAGES
COMMENTS
Diabetes burnout is a mixture of emotions and behaviors where the patients can feel mentally and physically tired from the daily engagement with self-care and experience ... Stuckey H. Original research: experiences of diabetes burnout: a qualitative study among people with type 1 diabetes. Am. J. Nurs. 2019; 119 (12):22-31. doi: 10.1097/01 ...
Diabetes burnout research also resulted in the development of a reliable and valid burnout scale, Diabetes Burnout Scale (DBS), to measure diabetes burnout ( α ≥ 0.80). The DBS is a 12-item scale with a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree). The DBS addresses the main dimensions of diabetes burnout including ...
The research around diabetes burnout can be informed by more fully developed theoretical conceptualizations of burnout in other fields. In particular, the occupational burnout literature exhibits parallels to diabetes burnout. Occupational burnout is described as exhaustion, cynicism, and professional efficacy
We included all eligible adults with T1D without considering their current or previous experience of burnout for two main reasons: (1) diabetes burnout is a prevalent problem (prior research suggesting that up to 36% of adults experience diabetes burnout); , and (2) the dimensions of diabetes burnout that we identified in our preliminary ...
The results from our study highlight the need for more research on diabetes burnout to distinguish from diabetes distress. Finally, based on qualitative studies and on expert opinion, a recent publication proposed a specific scale for diabetes burnout. This scale shows high correlations with depression and diabetes distress and is a good ...
Aims: This study aimed to corroborate the main hypotetized dimensions of diabetes burnout, and its distinction from diabetes distress and depressive symptoms among adults with type 1 diabetes (T1D). Methods: A qualitative descriptive study was employed to collect data from 31 eligible participants using semi-structured individual phone interviews.
Although exhaustion is an entry point for diabetes burnout, the findings suggest that detachment from illness identity, diabetes self-care, and support systems form a core component. ... Original Research: Experiences of Diabetes Burnout: A Qualitative Study Among People with Type 1 Diabetes Am J Nurs. 2019 Dec;119(12):22-31. doi: 10.1097/01 ...
Background: Diabetes burnout is a condition when a patient with diabetes feels tired from his/her disease and neglects it for a certain period or continuously. Objective: Diabetes burnout is frequent, and there is extended literature about psychosocial stress and its negative effects on health. Methods: A search for relevant studies was conducted using PubMed, Google Scholar and ResearchGate.
The research around diabetes burnout can be informed by more fully developed theoretical conceptualizations of burnout in other fields. In particular, the occupational burnout literature exhibits parallels to diabetes burnout. Occupational burnout is described as exhaustion, cynicism, and professional efficacy [21] as the result of ...
Diabetes burnout (9 studies) Maslach Burnout Inventory-General Survey (MBI-GS), exhaustion subscale : Adults: 9: Being overextended and exhausted by one's work: ... few studies have addressed diabetes burnout. The results from our study highlight the need for more research on diabetes burnout to distinguish from diabetes distress. Finally ...
Although diabetes burnout was related to poorer diabetes outcomes (more frequent missed medical appointments, missed glycemic targets), it did not predict these outcomes independently of diabetes distress. Whereas empirical research on diabetes burnout is sparse, there is a large literature on related constructs, including diabetes distress.
Diabetes burnout is significantly associated with both depression and diabetes distress. Charman D., 2000 [11] Psychotherapeutic case presentation Enhanced self-understanding can help achieve a ...
Methods: A national sample of adults with T1D (n=1099) completed an online cross-sectional survey across the U.S. We used Diabetes Burnout Scale (DBS) to collect data on diabetes burnout (i.e., exhaustion, detachment, lack of control) . We also measured diabetes distress, depressive symptoms, glycemic control, and demographic characteristics.
s it. Objective: This study was aimed at increasing our understanding of the lived experiences of diabetes burnout among adults with type 1 diabetes. Methods: A qualitative descriptive study was conducted with a sample of 18 adults with type 1 diabetes who reported a current or previous experience of diabetes burnout. Data were collected using in-depth interviews and analyzed using qualitative ...
It differs from diabetes distress and depression, with burnout focusing on exhaustion related to management, while distress encompasses broader challenges, and depression involves feelings of sadness and hopelessness. Coping strategies include self-care, realistic goals, seeking support, and lifestyle adjustments.
Purpose of Review: Diabetes represents a chronic illness with significant physical and psychological morbidities. This review aims to summarize current conceptualizations of diabetes burnout in individuals with diabetes and describe its associated adverse outcomes in this population while proposing possible mechanisms of action and targets of intervention.
Little research exists regarding how diabetes burnout specifically differs from depression. However, many reports distinguish diabetes distress from depression.
The research around diabetes burnout can be informed by more fully developed theoretical conceptualizations of burnout in other fields. In particular, the occupational burnout literature exhibits parallels to diabetes burnout. ... Diabetes burnout differs from distress and depressive symptoms in specificity, duration and progression: Diabetes ...
Dealing With Diabetes Burnout. Over time, the emotional burden of managing diabetes can cause burnout. So far, you've had diabetes; it hasn't had you. You've been watching what you eat, making time for physical activity, taking meds, checking your blood sugar, checking your blood sugar again. But then something takes the wind out of your ...
Diabetes burnout can co-occur with depression (see Chapter 6), anxiety (see Chapter 7), and negative mood. In contrast to diabetes distress, very little research has been conducted specifically about diabetes burnout.30,34 The best way to prevent diabetes burnout is to regularly monitor for diabetes distress so that you can offer
Previous research on diabetes (type 1 and type 2) shows inconclusive results on the association between diabetes (versus no diabetes) and burnout. In general, burnout seems to be more prevalent among employees with chronic medical illnesses than employees without any chronic medical condition (Armon et al., 2014).
Introduction Diabetes distress (DD) and diabetes burnout (DB) are recognized psychological phenomena in patients with T1DM (type 1 diabetes mellitus). Still, there is an urgent need to create professional psychological intervention procedures to provide patients with adequate care. Aim The aim of the study was to assess the level of DD and DB in T1DM patients at baseline and after 5 of ...
Research by T1International finds that people with diabetes experience diabetes burnout at a very high rate, with a significant impact. Language. Español; ... While inadequate access to insulin and supplies is a major cause of diabetes burnout, the survey shows that regardless of access, burnout is experienced by almost all respondents (97.1% ...
When the literature has addressed diabetes burnout, it has overlooked how such burnout affects; people with diabetes. health care providers. family caregivers of people with diabetes. In preliminary studies among people with type 1 diabetes, Abdoli and colleagues reported that descriptions of burnout included detachment from illness identity ...
Feeling overwhelmed, exhausted, and frustrated by the daily demands of diabetes management has been referred to as diabetes burnout. The goal of the study was to develop a measure of diabetes burnout and to link this measure to psychological health and diabetes outcomes. Emerging adults with type 1 …
1. Introduction. Burnout is a state resulting from individuals being exposed to prolonged psychosocial stress [] and presenting core features such as physical and psychological fatigue and exhaustion [].Although previous studies have mainly been applied in describing the status of working adults under exposure to working stress, burnout can be due to other attributes in the personal life of ...
Compared with people who got seven to eight hours of sleep per day, those who slept less than six hours daily had a higher risk of developing type 2 diabetes later in life, according to the study ...
Traditional Chinese medicine (TCM) is increasingly used to manage type 2 diabetes and its nonpharmacological interventions are showing potential for preventing type 2 diabetes. This study mainly reviews relevant research. The most mentioned non-drug treatments for preventing type 2 diabetes in TCM are healthy diet, physical activity, emotional therapy, and acupuncture.
March 6, 2024. Source: Uppsala University. Summary: Adults who sleep only three to five hours per day are at higher risk of developing type 2 diabetes, according to a new study. Chronic sleep ...
Burnout. 45% of mental health professionals reported. burnout in 2022. Prevention is not only on worker; employers must. view causes at an organization level. People with workplace burnout have a 180%. increased risk of depression. 84% increased risk of type 2 diabetes. My experience (aka symptoms of burnout)