- Open access
- Published: 06 April 2023

Mental health challenges, treatment experiences, and care needs of post-secondary students: a cross-sectional mixed-methods study
- Elnaz Moghimi 1 , 2 ,
- Callum Stephenson 1 ,
- Gilmar Gutierrez 1 ,
- Jasleen Jagayat 3 ,
- Gina Layzell 3 ,
- Charmy Patel 1 ,
- Amber McCart 4 ,
- Cynthia Gibney 4 ,
- Caryn Langstaff 5 ,
- Oyedeji Ayonrinde 1 ,
- Sarosh Khalid-Khan 1 ,
- Roumen Milev 1 , 3 ,
- Erna Snelgrove-Clarke 6 ,
- Claudio Soares 1 ,
- Mohsen Omrani 1 , 7 &
- Nazanin Alavi 1 , 3 , 7
BMC Public Health volume 23 , Article number: 655 ( 2023 ) Cite this article
18k Accesses
7 Citations
10 Altmetric
Metrics details
Post-secondary students frequently experience high rates of mental health challenges. However, they present meagre rates of treatment-seeking behaviours. This elevated prevalence of mental health problems, particularly after the COVID-19 pandemic, can lead to distress, poor academic performance, and lower job prospects following the completion of education. To address the needs of this population, it is important to understand students' perceptions of mental health and the barriers preventing or limiting their access to care.
A broad-scoping online survey was publicly distributed to post-secondary students, collecting demographic, sociocultural, economic, and educational information while assessing various components of mental health.
In total, 448 students across post-secondary institutions in Ontario, Canada, responded to the survey. Over a third ( n = 170; 38.6%) of respondents reported a formal mental health diagnosis. Depression and generalized anxiety disorder were the most commonly reported diagnoses. Most respondents felt that post-secondary students did not have good mental health ( n = 253; 60.5%) and had inadequate coping strategies ( n = 261; 62.4%). The most frequently reported barriers to care were financial ( n = 214; 50.5%), long wait times ( n = 202; 47.6%), insufficient resources ( n = 165; 38.9%), time constraints ( n = 148; 34.9%), stigma ( n = 133; 31.4%), cultural barriers ( n = 108; 25.5%), and past negative experiences with mental health care ( n = 86; 20.3%). The majority of students felt their post-secondary institution needed to increase awareness ( n = 231; 56.5%) and mental health resources ( n = 306; 73.2%). Most viewed in-person therapy and online care with a therapist as more helpful than self-guided online care. However, there was uncertainty about the helpfulness and accessibility of different forms of treatment, including online interventions. The qualitative findings highlighted the need for personal strategies, mental health education and awareness, and institutional support and services.
Conclusions
Various barriers to care, perceived lack of resources, and low knowledge of available interventions may contribute to compromised mental health in post-secondary students. The survey findings indicate that upstream approaches such as integrating mental health education for students may address the varying needs of this critical population. Therapist-involved online mental health interventions may be a promising solution to address accessibility issues.
Peer Review reports
Post-secondary students frequently report high levels of stress, anxiety, depression, and other mental health concerns [ 1 , 2 , 3 ]. In a national survey of Canadian post-secondary students using campus mental health services, 95% reported being overwhelmed and exhausted, 83.7% reported anxiety, 86% were depressed, and 81% experienced loneliness [ 4 ]. Further, 45.1% of post-secondary students experience higher than average stress levels, and up to 35% meet diagnostic criteria for at least one mental health disorder [ 5 , 6 ]. Compromised mental health may increase student distress, academic probations, dropouts, and challenges in finding future employment [ 2 , 7 , 8 , 9 ].
The importance of effective mental health services for all citizens, including youth and young adults is broadly recognized in Canadian society [ 10 ]. As a result, most postsecondary institutions offer several different mental health services to vulnerable groups. These may include social or peer support, promotion and outreach programs, health education, counselling services, accommodations, triage system for urgent care, and short-term therapy [ 11 , 12 ]. Campuses typically do not offer long-term therapy or off-site services [ 11 ]. Despite the services available, treatment-seeking is reported to be as low as 10% [ 5 , 13 , 14 ]. Factors such as cost, stigma, privacy concerns, heavy academic course loads, inability to distinguish between mental illness and stress or other common emotions, work priorities, and long wait times can deter students from seeking help [ 14 , 15 ]. Moreover, adequate and timely access to mental health services by students is adversely affected by a network of personal, social, cultural, and institutional barriers that vary between regions and individuals [ 15 ]. These barriers include limited resources, increased complexity in student psychopathology, fragmented services, and low funding, to name a few [ 11 , 16 ]. Indeed, many student counselling centres report increased service wait times and reduced therapy sessions [ 11 ]. These strains are worsened in smaller institutions with fewer staff and resources [ 17 ]. Treatment barriers and service use amid the COVID-19 pandemic have yet to be fully delineated.
Mental health concerns were exacerbated by the COVID-19 pandemic, affecting all profiles of post-secondary students [ 18 ]. In a recent qualitative study, students without pre-existing mental health conditions reported greater social and academic isolation than those with pre-existing mental health concerns [ 19 ]. Furthermore, a recent meta-analysis noted an increase in the prevalence of anxiety (36%) and depression (39%) during the pandemic [ 20 ]. In response, many institutions have shifted to telemental health services that encourage continued care [ 21 ]. Other universities have started to implement virtual interventions to help first-year, graduate, and professional students navigate through the changed academic and social environments [ 22 , 23 ]. When assessing support offered by institutions during prolonged campus lockdowns, 91% of Canadian post-secondary institutions offered virtual counselling services, and 84% provided general psychoeducational resources [ 24 ]. Similar services are also available in US-based institutions [ 25 ]. Nevertheless, poor wellness behaviours, mood, and attention in post-secondary students have been observed during the pandemic [ 26 ]. To better understand the efficacy and effectiveness of the available resources during this period, it is critical to investigate how students perceive their mental health challenges and use the services at hand.
The current study aimed to capture post-secondary student mental health and care needs during the post-lockdown period of the COVID-19 pandemic. Specifically, the study surveyed post-secondary students on their mental health knowledge, treatment-seeking behaviours, perception of mental health services, and perceived barriers that may have limited their access to care. Since the persistence of lockdowns and social distancing laws resulted in online therapy use becoming commonplace, this delivery format was also focused on. The findings of this needs assessment study can inform the development of targeted, effective, and equitable care initiatives for this population.
Study design
The following cross-sectional mixed-methods study collected data through a self-administered online survey. A broad-scoping mental health experience survey was publicly advertised to post-secondary students across Ontario, Canada, through social media. Paid advertisement was not utilized for this study and organic reach was obtained by posting to groups and pages that pertained to the target population. Specifically, the survey advertisement was posted on Ontario-based university and college groups and pages on Reddit and Facebook. The research team as well as Queen’s University health and wellness centres also posted the study advertisement on their Instagram, Reddit, and Facebook social media pages. Data collection occurred from May 5 to June 5, 2022. Participation was voluntary, and the survey was administered via Qualtrics (Qualtrics, Provo, UT). Post-secondary students enrolled in any public or private post-secondary institution in Ontario, Canada, were eligible to complete the survey, which entered them in a draw to receive 1 of 20 Amazon gift cards valued at $25. Students of any status, including international, domestic, part-time, full-time, certificate, or degree, were included. To verify student status, participants were asked to provide an institutional email after consenting to participate in the study. The survey link was sent to this email. The consent process informed the students that their responses were in no way linked to their institutional emails. Participants were also asked to include the name of their post-secondary institution in their survey responses. Any student involved in developing or testing the survey was not eligible to complete the survey. Ethics approval was obtained from the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (HSREB) in Kingston, Canada.
Survey development
The research team developed and disseminated the Post-Secondary Student Mental Health Experience Survey to all post-secondary students attending colleges or universities in Ontario, Canada. The decision to limit the survey to Ontario was to pilot the survey and make any necessary modifications before administering the survey to a broader population [ 27 ]. Before dissemination, the survey was reviewed with a sample of post-secondary students enrolled in different programs ( n = 10) and modifications were made based on their feedback. These students were highly involved in student affairs and leadership positions within their post-secondary institutions. The diverse sample also represented an array of equity-deserving communities, including BIPOC, 2SLGBTQ + , international students, and students with different physical and mental health conditions. The survey was then uploaded onto Qualtrics (Qualtrics, Provo, UT) and was tested by another sample of students ( n = 20) before finalization. All student reviewers were within the research team’s broad network and agreed to review the survey voluntarily. Once the necessary changes were made, the survey was made available to all post-secondary students attending colleges or universities in Ontario, except for those involved in the survey's development and testing. All participants provided informed consent online before accessing the survey. The final survey focused on specific demographic variables, knowledge of and experience with different mental health treatments and resources (including online delivery formats), perceptions of the accessibility of the current mental health treatments, motivation and likelihood of seeking various types of mental healthcare, and changes students would like to see in the current system of care (Additional file 1 ). The survey intended to capture post-secondary students' mental health needs and identify barriers and limitations to care.
Data analysis
Since participants could skip questions they preferred not to answer, data from participants who did not complete the survey in its entirety were also included in the analysis. Missing data were not imputed because the sample size was sufficient to conduct the descriptive analysis. Each item was assessed individually and reported count percentages were relevant to the total responses of each item. All descriptive analyses were conducted through the online Qualtrics (Qualtrics, Provo, UT) statistical analysis software. Data from the open-ended question at the end of the survey ( Do you have any additional feedback to share ?) were analyzed qualitatively using content analysis methods [ 28 , 29 ]. All relevant feedback was categorized under codes representing prevalent ideas and common categories across the responses. The codes were meant to provide more context on the research findings—in particular, assessing the mental health challenges and care needs of post-secondary students. In the first step, a conventional coding approach was used where coding categories were developed from direct analysis of the entire textual data [ 30 ]. To do this, participant feedbacks were read several times to capture a general sense of the data. Subsequently, primary codes explicitly representing the participant responses were developed and modified. Data coding was done semantically, staying close to the text and using the participants’ words and verbiage. After discussion and refinement by the research team, the final coding strategy was applied to the dataset by two independent coders (EM and CaS), and inter-coder reliability was assessed via Cohen’s Kappa. Before finalization, all discrepancies were resolved through a third coder (GG). A subcategory analysis was then conducted by one of the coders (EM), and any emergent secondary codes were finalized through discussion with the research team. The demographic characteristics of participants who provided qualitative data were compared to that of all survey respondents via chi-squared tests for categorical variables and independent sample t-tests for continuous variables at α = 0.05. All statistical analysis was conducted using IBM SPSS Statistics for Mac, version 24 (IBM Corp., Armonk, N.Y., USA).
Participants
In total, 448 responses were recorded from students across post-secondary institutions in Ontario, Canada. Participants who did not list their post-secondary institution or if the institution was not located in Ontario, Canada, were excluded ( n = 78). On average, participants were 21.9 years of age (SD = 4.1). Most respondents did not have children ( n = 437; 97.5%). Participants reporting their race or ethnicity were given the option to select all applicable identities. For demographic information, please see Table 1 .
Post-secondary student profile
The study respondents were enrolled in 34 different institutions across Ontario. Only one participant attended a private institution (Additional file 1 ). Respondents were mainly enrolled in universities ( n = 406; 90.6%) compared to colleges ( n = 42; 9.4%). The majority of university students attended Queen’s University ( n = 80; 17.9%), followed by the University of Toronto ( n = 43; 9.6%), Ontario Tech University ( n = 38; 8.5%), Carleton University ( n = 37; 8.4%), McMaster University ( n = 37; 8.3%), University of Waterloo ( n = 35; 7.8%), and York University ( n = 21; 4.7%). Most of the respondents attending college were enrolled at St. Lawrence College ( n = 12; 2.7%), Durham College ( n = 6; 1.3%), and Centennial College ( n = 4; 0.9%). Regarding degree type, 65% of respondents ( n = 290) were undergraduate students, and 17.9% ( n = 80) were graduate students. Further, 9.8% ( n = 44) of respondents were pursuing a professional degree, diploma ( n = 24, 5.4%), or other ( n = 9; 2%; Fig. 1 ). Most students were Ontario residents ( n = 351; 90.5%) and did not relocate from another province. Employment status was nearly equal among students, with 48.8% of respondents being employed ( n = 217) and 51.2% ( n = 228) not employed. Students who indicated their weekly employment hours ( n = 73) worked an average of 25.87 h per week (SD = 11.76). Students ( n = 77) also committed an average of 5.4 h (SD = 5.24) to weekly volunteering. See Table 2 for a summary of student profiles.
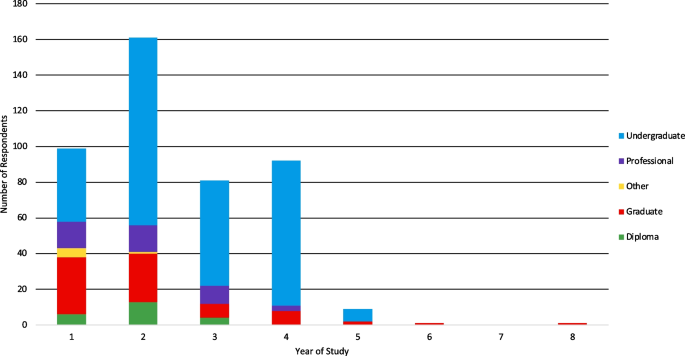
Year of study and degree type of students
Mental health disorders and symptoms
Most participants reported not being diagnosed with a mental health disorder ( n = 270; 61.4%; Fig. 2 ). Amongst those diagnosed, depression ( n = 85; 19.3%) and generalized anxiety disorder ( n = 80; 18.2%) were the most prevalent, followed by social anxiety disorder ( n = 51; 11.6%), panic disorder ( n = 40; 9.1%), and attention deficit hyperactivity disorder ( n = 34; 7.7%). Participants who were diagnosed with other mental health disorders ( n = 24; 5.5%), most frequently reported obsessive–compulsive disorder ( n = 9; 37.5%). Most participants ( n = 351; 80.7%) reported not having a disability. The most frequently reported disability was neurodevelopmental ( n = 36; 8.6%). When asked if students experienced a decline in their mental health since starting their post-secondary education, 66.5% of respondents ( n = 290) reported a decline in their mental health, 23.4% ( n = 102) did not see a difference in their mental health, and 10.1% ( n = 44) were unsure. Specifically, 66.1% of students ( n = 288) reported problems concentrating, 59.6% ( n = 260) experienced symptoms of depression (i.e., low moods, low energy, and low motivation), 58% ( n = 253) experienced daily general anxiety, 51.4% ( n = 244) experienced anxiety in social situations, 42.2% ( n = 184) had mood swings, 33.7% ( n = 147) experienced panic attacks, and 13.5% ( n = 59) engaged in problematic use of alcohol or other substances including cannabis. Other symptoms expressed by students ( n = 13; 3.0%) predominately comprised insomnia and other sleep disturbances ( n = 5; 3.8%).
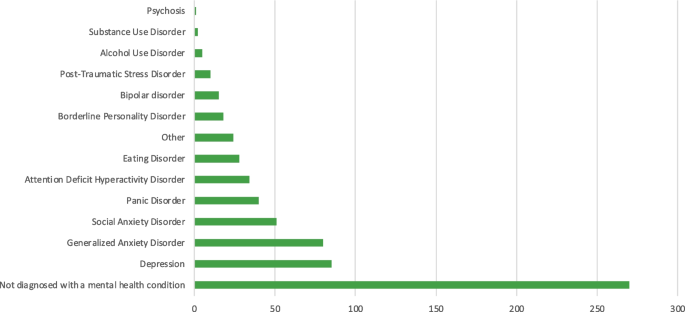
Prevalence of mental health disorders among participants
- Mental health needs
Although most students indicated that their mental health knowledge was good ( n = 283; 67.7%), the majority ( n = 261; 62.4%) agreed with the statement that they did not have enough coping strategies and tools related to mental health when starting their post-secondary studies. Many did not believe that post-secondary students have good mental health ( n = 253; 60.5%). Furthermore, not having enough time to focus on mental health during post-secondary studies was also expressed as a concern by participants ( n = 198; 47.3%). Most respondents ( n = 278; 66.5%) believed that the majority of students keep their mental health problems a secret. With respect to high school education, most ( n = 209; 50%) did not believe that the awareness and education on mental health were adequate, and others were neutral about this sentiment ( n = 71; 17%). On the other hand, many participants ( n = 307; 73.5%) believed that improving high school students’ mental health could enhance their overall functioning and well-being during their post-secondary studies.
Treatment-seeking behaviours
Concerning treatment, 70.5% ( n = 182) of respondents indicated that they were not taking medication, and 71.5% ( n = 318) were not receiving counselling or psychotherapy for their mental health. Amongst those receiving counselling or psychotherapy, the majority (52.0%; n = 66) received their sessions over online video platforms and 33.9% ( n = 43) engaged in in-person sessions. Many participants believed that digital mental health care delivery was good but not as good as in-person delivery ( n = 132; 31.1%), 18.6% ( n = 79) were unsure, 12.3% ( n = 52) believed it was no different, and 9.0% ( n = 38) believed it was better.
When asked about the campus environment and resources, most participants ( n = 321; 73.6%) indicated that they had not experienced any form of harassment on campus. However, 17.9% ( n = 78) of participants experienced verbal harassment, followed by cyber harassment ( n = 27; 6.2%), sexual harassment ( n = 25; 5.7%), and physical harassment ( n = 22; 5.0%). Most students ( n = 267; 61.7%) did not have accommodations such as extra test time or separate exam rooms. Some students ( n = 151; 34.9%) reported not using mental health services during their post-secondary studies. However, 34.6% ( n = 150) of students used the student wellness services offered by their institutions, and 25.4% ( n = 110) used mental health services provided outside their post-secondary institution. Participants also used several different strategies to cope with stress (Fig. 3 ). The most frequently used approach was distractive behaviours such as hobbies ( n = 305; 70.4%), followed by connecting with friends ( n = 258; 59.6%), food ( n = 209; 48.3%), and physical activity ( n = 208; 48.0%).
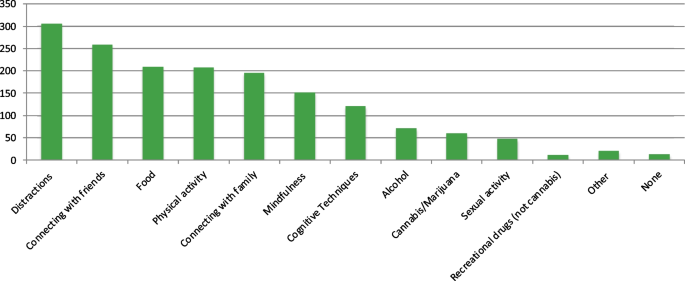
Strategies used to cope with stress
The most frequently reported barriers to mental health care were financial ( n = 214; 50.5%), long wait lists ( n = 202; 47.6%), lack of resources to address needs ( n = 165; 38.9%), inability to receive care due to school commitments ( n = 148; 34.9%), stigma ( n = 133; 31.4%), cultural barriers ( n = 108; 25.4%), and past negative experiences with mental health care ( n = 86; 20.3%). Only 8.3% ( n = 35) of respondents indicated no barriers to receiving care. Respondents who indicated “other” (5.0%, n = 21) listed accessibility issues ( n = 4; 19.0%), anxiety or social anxiety preventing treatment-seeking ( n = 2; 9.5%), work commitments ( n = 2), and apathy ( n = 2; Fig. 4 ).
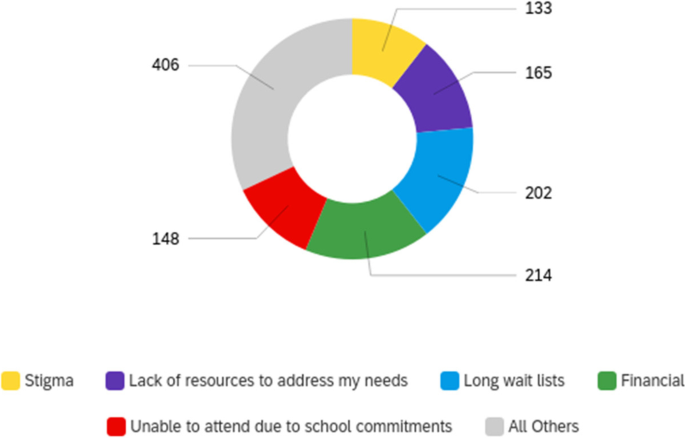
Perceived barriers to care (response count)
Mental health care
A sizeable proportion of participants were unsure about the helpfulness of different forms of mental health care (Fig. 5 ). Although in-person services were frequently rated as helpful ( n = 271; 63.9%), the perceptions of accessibility were nearly equally divided, with 42.9% finding this delivery type accessible and 37.3% finding it inaccessible (Fig. 6 ). By contrast, the fewest participants rated online psychotherapy with no therapist involved as helpful ( n = 100; 23.6%). However, 36.8% ( n = 156) found this delivery type to be accessible. Similar to perceptions of helpfulness, most respondents were unsure about the accessibility of the different care deliveries, particularly those in online or group therapy formats. Most of the individuals who were unsure about the helpfulness or accessibility of mental health care services were not receiving medication or psychotherapy (Additional file 2 ).
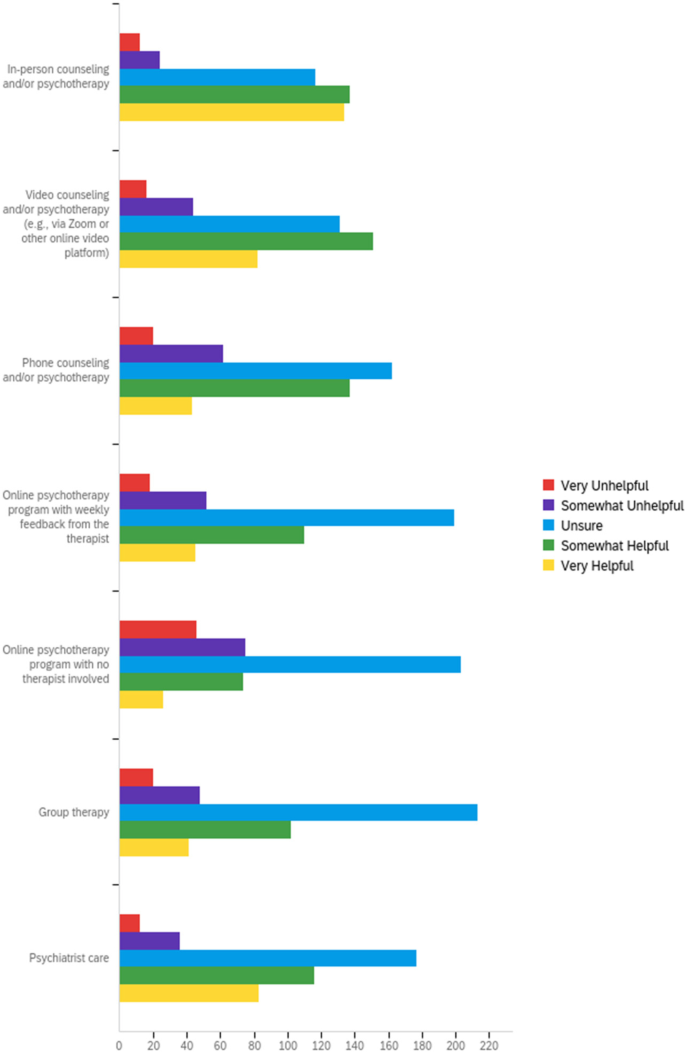
Perception of care helpfulness
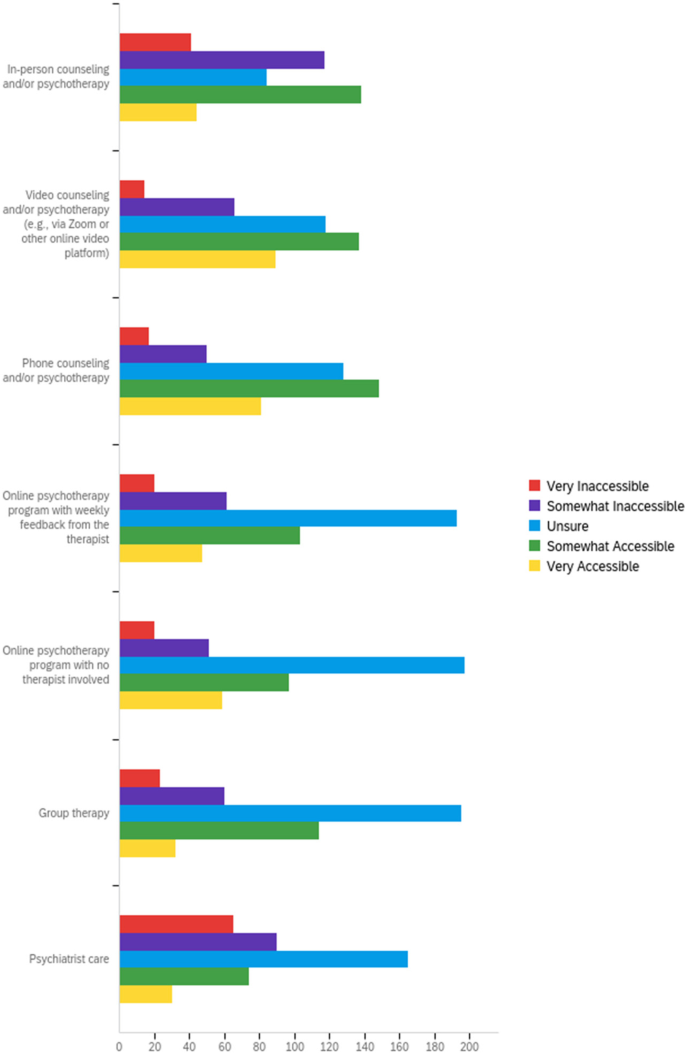
Perception of care accessibility
When focusing on post-secondary mental health services, 46.9% ( n = 196) of respondents believed they had a good understanding of the mental health resources offered by their institution. The exact number of participants ( n = 167; 40%) were either neutral or agreed that their institution's mental health programs and services were adequate. At the same time, 73.2% ( n = 306) of students believed that post-secondary mental health resources need to be increased. Most students ( n = 186; 44.5%) did not feel comfortable reaching out to faculty members or staff to access support for their mental health, although most were either neutral ( n = 137; 30.4%) or agreed ( n = 181; 43.3%) that institutional staff promoted mental health resources. Most individuals were also neutral ( n = 160; 38.3%) when asked if they prefer using services outside their institutions. At the same time, most participants ( n = 187; 45.6%) did not believe they could afford private mental health care, despite 61.2% ( n = 251) being aware of resources outside their institutions. Most participants were neutral ( n = 172; 42%) or agreed ( n = 157; 38.3%) that mental health services outside their campuses were more accessible. Most individuals ( n = 186; 45.4%) also preferred using services outside of their institution, even though most were neutral ( n = 210; 51.2%) about whether the quality of the service was superior to those on campus.
Many students ( n = 231; 56.5%) believed that greater awareness about mental health is necessary and that increasing awareness in the region could prevent mental health disorders ( n = 265; 64.6%; Fig. 7 ). Students also believed that current psychotherapy resources were insufficient and that more resources were needed ( n = 225; 54.9%).
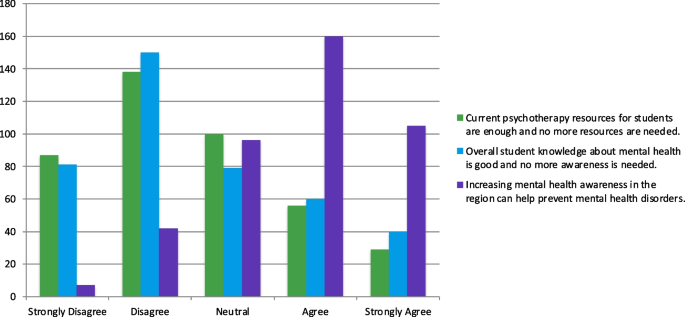
Opinions on mental health awareness and psychotherapy resources
Finally, when exploring the perception of online mental health care, students were relatively divided about their preference for online and in-person care, with most being neutral ( n = 178; 43.4%; Fig. 8 ). At the same time, most had or were willing to use online mental health care services ( n = 251; 61.2%). Although online mental health care was believed to make it easier for students to get the help they need ( n = 261; 63.7%), many thought it was easier to connect with therapists in-person than online ( n = 233; 56.8%). A large number of participants also expressed that they had privacy concerns accessing online mental health care ( n = 183; 44.6%).
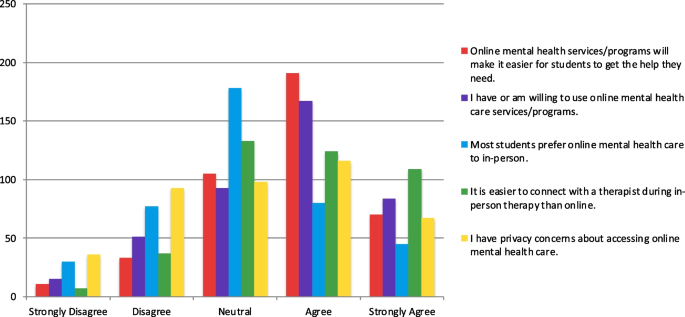
Opinions on online mental health care
Qualitative data
Initially, 155 participants (34.6%) responded when asked in the survey whether they had any additional feedback to share. After removing irrelevant content (i.e., responses with “no” or “not applicable” without follow-up statements), a final set of n = 110 (24.6%) feedback responses were coded. Agreement between the coders was moderate, κ = 0.53, (95% CI, 0.64 to 0.42), p < 0.001. After resolving discrepancies, seven categories and 24 subcategories emerged from the data (Table 3 ). Personal strategies ( n = 35; 31.82%) and the need for mental health education ( n = 29; 26.36%) were the most frequently expressed categories. Personal strategies were suggested by respondents and mostly stressed interpersonal skills ( n = 9) to improve social connections, methods to enhance self-awareness ( n = 7) and self-regulation ( n = 5), and lifestyle changes ( n = 5). Concerning mental health education, most feedback centred on the need to develop a formal course ( n = 16) with content focused on personal strategies ( n = 7). The most frequently discussed service and support focused on the need for guidance and counselling ( n = 6). Three respondents also highlighted the institution’s role, particularly the need for support from faculty and staff. The feedback about awareness mostly centred around highlighting its importance ( n = 10). The few environmental risk factors described digital online technology ( n = 1), systemic factors ( n = 2), and COVID-19 ( n = 2). Further, changes to the post-secondary learning environment were related to improving time management by extending the years needed to complete a degree and spreading out the course workload ( n = 2). One person also suggested improving institutional hardware and software. Lastly, participants who provided survey feedback ( n = 11; 10%) thanked the researchers for the survey ( n = 6) and offered suggestions to improve the survey ( n = 4). Changes pertained to a question using the term “prevention” rather than “treatment,” including an “I don’t know” option in some parts of the survey, a technical error where a blank question was visible, and the consideration of student diversity in mental health status. A comparison of demographic data between all survey respondents and those who provided qualitative feedback demonstrated significant differences (Additional file 3 ). Participants who provided feedback were mostly men, male, and single (Additional file 3 ). Furthermore, the ratio of white to black respondents was reduced from 3.75 times amongst all survey respondents to 1.74 times in participants who provided qualitative feedback.
The current study explored the mental health challenges and care needs of post-secondary students in the post-lockdown COVID-19 pandemic period (May to June 5, 2022). To capture this data, the Post-Secondary Student Mental Health Experience Survey was developed and made available to students within Ontario, Canada. Approximately 0.05% of the postsecondary population in the province (448 out of 903, 780 individuals [ 31 ]) responded to the survey. A decline in mental health was reported by post-secondary students since starting their studies. Although there was a greater preference for in-person treatments, many students used online mental health interventions. However, there was uncertainty about the helpfulness and accessibility of different in-person and online interventions. Several limitations to care were also expressed, including the need to improve mental health awareness, education, and care resources.
In line with the current body of studies, the most prevalent mental health disorders among students were depression and anxiety [ 32 ]. In students not formally diagnosed, the majority experienced mental health concerns and indicated a decline in their mental health since starting their post-secondary education. Indeed, post-secondary students are considered an at-risk population for chronic stress and poor mental health [ 33 ]. The current study provided additional details on how these symptoms present themselves—namely in the form of compromised concentration, symptoms of anxiety and depression, mood swings, panic attacks, problematic use of alcohol and other recreational drugs, and problems with sleep. Given the number of hours students work and engage in extracurricular activities, it is unsurprising that the majority surveyed lacked time to focus on their mental health. The pressures to meet the increased cost of living, combined with the competitiveness of the current job market, can put students at higher odds of experiencing anxiety and depression [ 34 ].
Much of the mental health needs of the sample focused on education, strategies, and tools. Although most students believed they had good mental health knowledge and offered personal strategies in the survey feedback, they could not effectively manage their concerns. These findings provide some insight into the importance of distinguishing between knowledge acquisition and knowledge use. Health knowledge can influence health behaviours and attitudes, even during the pandemic [ 35 ]. However, the current body of studies has presented caveats to the positive association between health knowledge and health behaviours. For example, one pilot study demonstrated that consumers of self-help books might present more significant symptoms of stress compared to nonconsumers [ 36 ]. In social media-based research, a gap was identified between health knowledge acquisition, intention, and health behaviours. This gap was influenced by several factors, including fear, trust, credibility, and perceived efficacy [ 37 ]. Moreover, nearly one in four students in the current study reported being subjected to some form of harassment on campus despite relevant policies, educational resources, and initiatives available to the community [ 38 ]. While it is beyond the scope of this study, future studies should examine the disconnect between knowledge and action—frequently termed the G.I Joe Phenomena [ 39 ]—in the context of post-secondary mental health education development. This is especially important considering that one of the most predominant feedback from participants was the need for mental health-based courses that focused on teaching personal coping strategies. In line with the theme of knowledge acquisition, most students also believed in the importance of high school mental health education. High school psychoeducation can help students transition to post-secondary school [ 40 ] by providing resources and support, enhancing student mental health literacy and hygiene, improving psychological resilience, and mitigating distorted thought processing [ 41 , 42 ]. At the same time, a more robust evidence base is needed to support effective mental health promotion strategies from a young age [ 43 ]. Taken together, how and when information should be disseminated to students to evoke actionable change requires further investigation.
Regarding treatment-seeking and care needs, many students were unsure about the accessibility and helpfulness of the treatments offered. Privacy and confidentiality, communication concerns, and the quality of resources may impact acceptability and engagement with different delivery methods [ 44 ]. In addition, most of the students surveyed were not diagnosed with a mental health disorder, which may partially explain these trends. The high level of stigma that exists in this population may also limit knowledge about the resources offered. These factors further support programs that inform students of available resources. Considering the risk of developing or worsening mental health symptoms in this population, institutions may benefit from proactive measures that increase mental health awareness and knowledge of resources. Programs with these aims have successfully reduced stigma and increased resiliency and help-seeking [ 45 ]. How these approaches impact campus accommodation use and treatment-seeking are important considerations for future research [ 46 ]. Similar to other populations [ 47 ], delivery methods with therapists were more frequently perceived as accessible and helpful. The emergent categories of interpersonal skills, peer support, and counselling and guidance within the qualitative findings also support the association between human connection and mental health. Future studies should investigate whether the same benefits exist with paraprofessionals (e.g., peer supporters, lay counsellors, and other non-clinicians) since improved outcomes have been observed in digital mental health interventions that employ such personnel [ 48 ]. Despite the greater preference for in-person mental health care and increased therapist involvement, students expressed challenges in seeking help due to financial constraints, long wait times, and lack of time to focus on mental health. Online resources benefit from integrating cost-effectiveness, time flexibility, and rapid availability to alleviate some barriers to care [ 49 , 50 ].
The study is one of few that investigates the mental health challenges and care needs of post-secondary students in the post-lockdown period of the COVID-19 pandemic. While the novelty of this study serves as its strength, some of its limitations must also be mentioned. A smaller region was used to pilot the survey before administering it to a larger population. Since all survey advertisements occurred through social media, there is the possibility of volunteer bias. A lack of paid advertisement may have also limited reach to include only students who access the groups and platforms the survey was advertised on. The substantial increase in technology use to connect with others can make social media a feasible tool for survey recruitment during the COVID-19 pandemic [ 51 ]. However, as students return to campus, future recruitment strategies should consider partnerships with teaching faculty and institutional and student organizations that can build trust and enhance reach amongst postsecondary students. Further, although the sample size and handling of missing data were adequate for the study’s descriptive analysis, some factors were not weighted similarly due to different response rates. While this may be a limitation, the pilot survey provided opportune conditions to re-assess the survey items and add “I don’t know,” “unsure,” or “prefer not to answer” options to discourage skipping items. A suggestion to include “does not apply” was also expressed by a participant in the qualitative feedback. The response rates were sufficient for all items, except when students were asked if they were taking medication for their mental health. When given only “yes” or “no” options, the response rate for this item was approximately 58%. Although the aforementioned options will be added to the next iteration of the survey, future studies should investigate the potential role of self-stigma on response rates within anonymous mental health surveys [ 52 ].
Nevertheless, the current findings indicated that mental health worsens throughout post-secondary education in the study population. Therefore, the survey will also be revised to include whether current mental health diagnoses were received before or after participants commenced their post-secondary studies. This information is critical in evaluating how symptoms and experiences manifest and differ in newly diagnosed patients versus those with longer experiences with mental health challenges. Another limitation of the study was that most respondents were not diagnosed with mental health disorders, and there were few members of equity-seeking and equity-deserving groups. Students who identify with these communities typically face additional stressors that increase their risk of mental health concerns [ 53 , 54 ]. In addition, significant differences were observed in some of the demographic characteristics of feedback providers. Namely, men and males comprised most of the qualitative responders, whereas survey responders as a whole were mostly women and female. Furthermore, the ratio of white to black respondents was substantially reduced in the group that provided additional feedback. While not the main objective of this study, these patterns highlight the importance of designing inclusive surveys that provide a platform for traditionally less vocal groups to express their mental health needs [ 55 , 56 ]. Future studies may need to implement procedures to build community trust and encourage survey completion by students in these groups. These data are critical in informing equitable mental health care and resources.
The current study highlighted the need for more accessible mental health resources for students across the mental health spectrum. Institutions may benefit from developing formal courses with coping mechanisms and other tools, skills, and strategies to inspire action-based changes in students suffering from poor mental health. Financial constraints, lack of time, stigma, and long wait times are all factors that can reduce treatment-seeking and worsen mental health. Strategic methods to enhance mental health awareness and knowledge also have the potential to clarify the uncertainty that students have about the helpfulness and accessibility of different care delivery types. Although therapist guidance was viewed positively, future studies should explore how online therapist guidance can improve sentiment towards online care—a delivery type frequently used during the pandemic.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Wiens K, Bhattarai A, Dores A, Pedram P, Williams J, Bulloch A, et al. Mental Health among Canadian Postsecondary Students: A Mental Health Crisis? Can J Psychiatry Rev Can Psychiatr. 2020;65(1):30–5.
Article Google Scholar
Evans TM, Bira L, Gastelum JB, Weiss LT, Vanderford NL. Evidence for a mental health crisis in graduate education. Nat Biotechnol. 2018;36(3):282–4.
Article CAS PubMed Google Scholar
Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. The association between depression, anxiety and substance use among Canadian post-secondary students. Neuropsychiatr Dis Treat. 2018;14:3241–51.
Article PubMed PubMed Central Google Scholar
Ogrodniczuk JS, Kealy D, Laverdière O. Who is coming through the door? A national survey of self-reported problems among post-secondary school students who have attended campus mental health services in Canada. Couns Psychother Res. 2021;21(4):837–45.
American College Health Association. National College Health Assessment [Internet]. 2017. Available from: http://www.acha-ncha.org/reports_ACHANCHAIIc.%0Dhtml .
American College Health Association. American College Health Association-National College Health Assessment II: Ontario Canada Reference Group Executive Summary Spring 2019. Silver Spring, MD: American College Health Association; 2019.
Chacón-Cuberos R, Zurita-Ortega F, Olmedo-Moreno EM, Castro-Sánchez M. Relationship between Academic Stress, Physical Activity and Diet in University Students of Education. Behav Sci. 2019;9(6):59–59.
Chiauzzi E, Brevard J, Thurn C, Decembrele S, Lord S. MyStudentBody–Stress: An Online Stress Management Intervention for College Students. J Health Commun. 2008;13(6):555–72.
Article PubMed Google Scholar
Smith L, Disler R, Watson K. Physical activity and dietary habits of first year nursing students: An Australian dual-method study. Collegian. 2020;27(5):535–41.
Ng P, Padjen M. An overview of post-secondary mental health on campuses in Ontario: challenges and successes. Int J Ment Health Addict. 2019;17(3):531–41.
Jaworska N, De Somma E, Fonseka B, Heck E, MacQueen GM. Mental Health Services for Students at Postsecondary Institutions: A National Survey. Can J Psychiatry. 2016;61(12):766–75.
Gotlib D, Saragoza P, Segal S, Goodman L, Schwartz V. Evaluation and Management of Mental Health Disability in Post-secondary Students. Curr Psychiatry Rep. 2019;21(6):43.
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–38.
Marsh CN, Wilcoxon SA. Underutilization of Mental Health Services Among College Students: An Examination of System-Related Barriers. J Coll Stud Psychother. 2015;29(3):227–43.
Dunley P, Papadopoulos A. Why Is It So Hard to Get Help? Barriers to Help-Seeking in Postsecondary Students Struggling with Mental Health Issues: a Scoping Review. Int J Ment Health Addict. 2019;17(3):699–715.
Ontario College Health Association. Towards a comprehensive mental health strategy: the crucial role of colleges and universities as partners [Internet]. 2009 [cited 2022 May 16]. Available from: http://www.oucha.ca/pdf/mental_health/2009_12_OUCHA_Mental_Health_Report.pdf
Mowbray C, Megivern D, Mandiberg J. Campus MHS: recommendations for change. Am J Orthopsychiatry. 2006;76(2):226–37.
Zhu J, Racine N, Xie EB, Park J, Watt J, Eirich R, et al. Post-secondary student mental health during COVID-19: a meta-analysis. Front Psychiatry. 2021;12:777251.
Ewing L, Hamza CA, Walsh K, Goldstein AL, Heath NL. A Qualitative Investigation of the Positive and Negative Impacts of the COVID-19 Pandemic on Post-Secondary Students’ Mental Health and Well-Being. Emerg Adulthood. 2022;10(5):1312–27.
Li Y, Wang A, Wu Y, Han N, Huang H. Impact of the COVID-19 Pandemic on the Mental Health of College Students: A Systematic Review and Meta-Analysis. Front Psychol. 2021;12:669119.
Huilgol YS, Torous J, Gold JA, Goldman ML. Telemental health policies for college students during COVID-19. J Am Coll Health J ACH. 2021;23:1–5.
Google Scholar
Kwan MYW, Brown D, MacKillop J, Beaudette S, Van Koughnett S, Munn C. Evaluating the impact of Archway: a personalized program for 1st year student success and mental health and wellbeing. BMC Public Health. 2021;21(1):59.
Wasil AR, Taylor ME, Franzen RE, Steinberg JS, DeRubeis RJ. Promoting Graduate Student Mental Health During COVID-19: Acceptability, Feasibility, and Perceived Utility of an Online Single-Session Intervention. Front Psychol. 2021;12:569785.
Seko Y, Meyer J, Bonghanya R, Honiball L. Mental health support for Canadian postsecondary students during COVID-19 pandemic: An environmental scan. J Am Coll Health. 2022;4(0):0–5.
Liu CH, Pinder-Amaker S, Hahm HC, Chen JA. Priorities for addressing the impact of the COVID-19 pandemic on college student mental health. J Am Coll Health. 2022;70(5):1356–8.
Copeland WE, McGinnis E, Bai Y, Adams Z, Nardone H, Devadanam V, et al. Impact of COVID-19 Pandemic on College Student Mental Health and Wellness. J Am Acad Child Adolesc Psychiatry. 2021;60(1):134-141.e2.
Bergman A, Chinco A, Hartzmark SM, Sussman AB. Survey curious? Start-up guide and best practices for running surveys and experiments online. Econometrics: Econometric & Statistical Methods - Special Topics eJournal. 2020:n. pag.
Krippendorff K. Content analysis: An introduction to its methodology. Thousand Oaks, CA: Sage publications; 2019.
Book Google Scholar
Neuendorf KA. Content analysis and thematic analysis. In: Advanced research methods for applied psychology. Milton Park: Routledge; 2018. p. 211–23.
Chapter Google Scholar
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Statistics Canada. Table 37-10-0011-01 Postsecondary enrolments, by field of study, registration status, program type, credential type and gender. 2022. https://doi.org/10.25318/3710001101-eng .
Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021;301:113863.
Article CAS PubMed PubMed Central Google Scholar
Linden B, Stuart H. Post-Secondary Stress and Mental Well-Being: A Scoping Review of the Academic Literature. Can J Commun Ment Health. 2020;39(1):1–32.
Posselt J. Discrimination, competitiveness, and support in US graduate student mental health. Stud Grad Postdr Educ. 2021;12(1):89–112.
Rincón Uribe FA, de Souza Godinho RC, Machado MAS, Oliveira KR da SG, Neira Espejo CA, de Sousa NCV, et al. Health knowledge, health behaviors and attitudes during pandemic emergencies: A systematic review. PLoS One. 2021;16(9):e0256731.
Raymond C, Marin MF, Hand A, Sindi S, Juster RP, Lupien SJ. Salivary cortisol levels and depressive symptomatology in consumers and nonconsumers of self-help books: a pilot study. Neural Plast. 2016;2016:3136743.
Chaoguang H, Feicheng M, Yifei Q, Yuchao W. Exploring the determinants of health knowledge adoption in social media: An intention-behavior-gap perspective. Inf Dev. 2018;34(4):346–63.
Cismaru M, Cismaru R. Protecting University Students from Bullying and Harassment: A Review of the Initiatives at Canadian Universities. Contemp Issues Educ Res. 2018;11(4):145–52.
Kristal AS, Santos LR. GI Joe phenomena: understanding the limits of metacognitive awareness on debiasing. No 21–084. Harvard Business School Working Paper; 2021. p. 1–54.
Kutcher S, Wei Y. School mental health: a necessary component of youth mental health policy and plans. World Psychiatry. 2020;19(2):174–5.
Şahin H, Türk F. The Impact of Cognitive-Behavioral Group Psycho-Education Program on Psychological Resilience, Irrational Beliefs, and Well-Being. J Ration-Emotive Cogn-Behav Ther. 2021;39(4):672–94.
Sapru I, Khalid-Khan S, Choi E, Alavi N, Patel A, Sutton C, et al. Effectiveness of online versus live multi-family psychoeducation group therapy for children and adolescents with mood or anxiety disorders: a pilot study. Int J Adolesc Med Health. 2018;30(4). https://doi.org/10.1515/ijamh-2016-0069 .
O’Reilly M, Svirydzenka N, Adams S, Dogra N. Review of mental health promotion interventions in schools. Soc Psychiatry Psychiatr Epidemiol. 2018;53(7):647–62.
Chan JK, Farrer LM, Gulliver A, Bennett K, Griffiths KM. University Students’ Views on the Perceived Benefits and Drawbacks of Seeking Help for Mental Health Problems on the Internet: A Qualitative Study. JMIR Hum Factors. 2016;3(1):e4765.
Szeto AC, Henderson L, Lindsay BL, Knaak S, Dobson KS. Increasing resiliency and reducing mental illness stigma in post-secondary students: A meta-analytic evaluation of the inquiring mind program. J Am Coll Health. 2021;1–11.
Condra M, Dineen M, Gills H, Jack-Davies A, Condra E. Academic Accommodations for Postsecondary Students with Mental Health Disabilities in Ontario, Canada: A Review of the Literature and Reflections on Emerging Issues. J Postsecond Educ Disabil. 2015;28(3):277–91.
Saddichha S, Al-Desouki M, Lamia A, Linden IA, Krausz M. Online interventions for depression and anxiety – a systematic review. Health Psychol Behav Med. 2014;2(1):841–81.
Leung C, Pei J, Hudec K, Shams F, Munthali R, Vigo D. The Effects of Nonclinician Guidance on Effectiveness and Process Outcomes in Digital Mental Health Interventions: Systematic Review and Meta-analysis. J Med Internet Res. 2022;24(6):e36004.
Donker T, Blankers M, Hedman E, Ljotsson B, Petrie K, Christensen H. Economic evaluations of Internet interventions for mental health: a systematic review. Psychol Med. 2015;45(16):3357–76.
Montagni I, Tzourio C, Cousin T, Sagara JA, Bada-Alonzi J, Horgan A. Mental health-related digital use by university students: a systematic review. Telemed E-Health. 2020;26(2):131–46.
Purewal S, Ardiles P, Di Ruggiero E, Flores JVL, Mahmood S, Elhagehassan H. Using social media as a survey recruitment strategy for post-secondary students during the COVID-19 pandemic. Inq J Med Care Organ Provis Financ. 2021;58:1–9.
Cinculova A, Prasko J, Kamaradova D, Ociskova M, Latalova K, Vrbova K, Tichackova A. Adherence, self-stigma and discontinuation of pharmacotherapy in patients with anxiety disorders–cross-sectional study. Neuroendocrinol Lett. 2017;38(6):429–36.
PubMed Google Scholar
Aguilar O, Lipson SK. A Public Health Approach to Understanding the Mental Health Needs of College Students with Disabilities: Results from a National Survey. J Postsecond Educ Disabil. 2021;34(3):273–85.
Lisnyj KT, Pearl DL, McWhirter JE, Papadopoulos A. Exploration of Factors Affecting Post-Secondary Students’ Stress and Academic Success: Application of the Socio-Ecological Model for Health Promotion. Int J Environ Res Public Health. 2021;18(7):3779.
Taylor RE, Kuo BC. Black American psychological help-seeking intention: An integrated literature review with recommendations for clinical practice. J Psychother Integr. 2019;29(4):325.
Brown JS, Sagar-Ouriaghli I, Sullivan L. Help-seeking among men for mental health problems. In: The Palgrave Handbook of male psychology and mental health. London: Palgrave Macmillan; 2019. p. 397–415.
Download references
Acknowledgements
Not applicable.
This study was funded by the Canadian Institutes of Health Research (CIHR) Healthy Cities Implementation Science (HCIS) Team Grant (File #: RN458719—473591).
Author information
Authors and affiliations.
Department of Psychiatry, Faculty of Health Sciences, Queen’s University, 166 Brock Street, Kingston, ON, K7L 5G2, Canada
Elnaz Moghimi, Callum Stephenson, Gilmar Gutierrez, Charmy Patel, Oyedeji Ayonrinde, Sarosh Khalid-Khan, Roumen Milev, Claudio Soares, Mohsen Omrani & Nazanin Alavi
Waypoint Research Institute, Waypoint Centre for Mental Health Care, Penetanguishene, Canada
Elnaz Moghimi
Centre for Neuroscience Studies, Faculty of Health Sciences, Queen’s University, Kingston, ON, Canada
Jasleen Jagayat, Gina Layzell, Roumen Milev & Nazanin Alavi
Student Wellness Services, Queen’s University, Kingston, ON, Canada
Amber McCart & Cynthia Gibney
Wellness, Accessibility & Student Success, St. Lawrence College, Kingston, ON, Canada
Caryn Langstaff
School of Nursing, Faculty of Health Sciences, Queen’s University, Kingston, ON, Canada
Erna Snelgrove-Clarke
OPTT Inc, Toronto, ON, Canada
Mohsen Omrani & Nazanin Alavi
You can also search for this author in PubMed Google Scholar
Contributions
EM, CaS, MO, and NA were responsible for the study design. EM, CaS, JJ, GL, CP and NA were responsible for developing and administering the survey. Data analysis and drafting of the manuscript were conducted by EM, CaS, and GG. Subsequent drafts of the manuscript were edited and finalized by all authors. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Nazanin Alavi .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (HSREB) in Kingston, Canada. All methods were carried out in accordance with relevant guidelines and regulations. All participants provided informed consent online before accessing the survey.
Consent for publication
Competing interests.
NA and MO cofounded an online care delivery platform (i.e., OPTT) and have ownership stakes in OPTT Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2:.
Appendix 2. Perceived helpfulness and accessibility of treatments in survey respondents currently receiving psychotherapy/counseling and medication for their mental health.
Additional file 3:
Table 4. Demographic data of qualitative respondents. Statistical analysis compared data of qualitative respondents and all survey respondents. All p values are two-tailed and α = 0.05.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Moghimi, E., Stephenson, C., Gutierrez, G. et al. Mental health challenges, treatment experiences, and care needs of post-secondary students: a cross-sectional mixed-methods study. BMC Public Health 23 , 655 (2023). https://doi.org/10.1186/s12889-023-15452-x
Download citation
Received : 29 November 2022
Accepted : 15 March 2023
Published : 06 April 2023
DOI : https://doi.org/10.1186/s12889-023-15452-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Student mental health
- Mental health treatment
- Psychotherapy
- Post-secondary students
- University and college mental health
- Young-adult mental health
- Treatment perception
- Online mental health treatment
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 14 December 2021
Bullying at school and mental health problems among adolescents: a repeated cross-sectional study
- Håkan Källmén 1 &
- Mats Hallgren ORCID: orcid.org/0000-0002-0599-2403 2
Child and Adolescent Psychiatry and Mental Health volume 15 , Article number: 74 ( 2021 ) Cite this article
89k Accesses
13 Citations
30 Altmetric
Metrics details
To examine recent trends in bullying and mental health problems among adolescents and the association between them.
A questionnaire measuring mental health problems, bullying at school, socio-economic status, and the school environment was distributed to all secondary school students aged 15 (school-year 9) and 18 (school-year 11) in Stockholm during 2014, 2018, and 2020 (n = 32,722). Associations between bullying and mental health problems were assessed using logistic regression analyses adjusting for relevant demographic, socio-economic, and school-related factors.
The prevalence of bullying remained stable and was highest among girls in year 9; range = 4.9% to 16.9%. Mental health problems increased; range = + 1.2% (year 9 boys) to + 4.6% (year 11 girls) and were consistently higher among girls (17.2% in year 11, 2020). In adjusted models, having been bullied was detrimentally associated with mental health (OR = 2.57 [2.24–2.96]). Reports of mental health problems were four times higher among boys who had been bullied compared to those not bullied. The corresponding figure for girls was 2.4 times higher.
Conclusions
Exposure to bullying at school was associated with higher odds of mental health problems. Boys appear to be more vulnerable to the deleterious effects of bullying than girls.
Introduction
Bullying involves repeated hurtful actions between peers where an imbalance of power exists [ 1 ]. Arseneault et al. [ 2 ] conducted a review of the mental health consequences of bullying for children and adolescents and found that bullying is associated with severe symptoms of mental health problems, including self-harm and suicidality. Bullying was shown to have detrimental effects that persist into late adolescence and contribute independently to mental health problems. Updated reviews have presented evidence indicating that bullying is causative of mental illness in many adolescents [ 3 , 4 ].
There are indications that mental health problems are increasing among adolescents in some Nordic countries. Hagquist et al. [ 5 ] examined trends in mental health among Scandinavian adolescents (n = 116, 531) aged 11–15 years between 1993 and 2014. Mental health problems were operationalized as difficulty concentrating, sleep disorders, headache, stomach pain, feeling tense, sad and/or dizzy. The study revealed increasing rates of adolescent mental health problems in all four counties (Finland, Sweden, Norway, and Denmark), with Sweden experiencing the sharpest increase among older adolescents, particularly girls. Worsening adolescent mental health has also been reported in the United Kingdom. A study of 28,100 school-aged adolescents in England found that two out of five young people scored above thresholds for emotional problems, conduct problems or hyperactivity [ 6 ]. Female gender, deprivation, high needs status (educational/social), ethnic background, and older age were all associated with higher odds of experiencing mental health difficulties.
Bullying is shown to increase the risk of poor mental health and may partly explain these detrimental changes. Le et al. [ 7 ] reported an inverse association between bullying and mental health among 11–16-year-olds in Vietnam. They also found that poor mental health can make some children and adolescents more vulnerable to bullying at school. Bayer et al. [ 8 ] examined links between bullying at school and mental health among 8–9-year-old children in Australia. Those who experienced bullying more than once a week had poorer mental health than children who experienced bullying less frequently. Friendships moderated this association, such that children with more friends experienced fewer mental health problems (protective effect). Hysing et al. [ 9 ] investigated the association between experiences of bullying (as a victim or perpetrator) and mental health, sleep disorders, and school performance among 16–19 year olds from Norway (n = 10,200). Participants were categorized as victims, bullies, or bully-victims (that is, victims who also bullied others). All three categories were associated with worse mental health, school performance, and sleeping difficulties. Those who had been bullied also reported more emotional problems, while those who bullied others reported more conduct disorders [ 9 ].
As most adolescents spend a considerable amount of time at school, the school environment has been a major focus of mental health research [ 10 , 11 ]. In a recent review, Saminathen et al. [ 12 ] concluded that school is a potential protective factor against mental health problems, as it provides a socially supportive context and prepares students for higher education and employment. However, it may also be the primary setting for protracted bullying and stress [ 13 ]. Another factor associated with adolescent mental health is parental socio-economic status (SES) [ 14 ]. A systematic review indicated that lower parental SES is associated with poorer adolescent mental health [ 15 ]. However, no previous studies have examined whether SES modifies or attenuates the association between bullying and mental health. Similarly, it remains unclear whether school related factors, such as school grades and the school environment, influence the relationship between bullying and mental health. This information could help to identify those adolescents most at risk of harm from bullying.
To address these issues, we investigated the prevalence of bullying at school and mental health problems among Swedish adolescents aged 15–18 years between 2014 and 2020 using a population-based school survey. We also examined associations between bullying at school and mental health problems adjusting for relevant demographic, socioeconomic, and school-related factors. We hypothesized that: (1) bullying and adolescent mental health problems have increased over time; (2) There is an association between bullying victimization and mental health, so that mental health problems are more prevalent among those who have been victims of bullying; and (3) that school-related factors would attenuate the association between bullying and mental health.
Participants
The Stockholm school survey is completed every other year by students in lower secondary school (year 9—compulsory) and upper secondary school (year 11). The survey is mandatory for public schools, but voluntary for private schools. The purpose of the survey is to help inform decision making by local authorities that will ultimately improve students’ wellbeing. The questions relate to life circumstances, including SES, schoolwork, bullying, drug use, health, and crime. Non-completers are those who were absent from school when the survey was completed (< 5%). Response rates vary from year to year but are typically around 75%. For the current study data were available for 2014, 2018 and 2020. In 2014; 5235 boys and 5761 girls responded, in 2018; 5017 boys and 5211 girls responded, and in 2020; 5633 boys and 5865 girls responded (total n = 32,722). Data for the exposure variable, bullied at school, were missing for 4159 students, leaving 28,563 participants in the crude model. The fully adjusted model (described below) included 15,985 participants. The mean age in grade 9 was 15.3 years (SD = 0.51) and in grade 11, 17.3 years (SD = 0.61). As the data are completely anonymous, the study was exempt from ethical approval according to an earlier decision from the Ethical Review Board in Stockholm (2010-241 31-5). Details of the survey are available via a website [ 16 ], and are described in a previous paper [ 17 ].
Students completed the questionnaire during a school lesson, placed it in a sealed envelope and handed it to their teacher. Student were permitted the entire lesson (about 40 min) to complete the questionnaire and were informed that participation was voluntary (and that they were free to cancel their participation at any time without consequences). Students were also informed that the Origo Group was responsible for collection of the data on behalf of the City of Stockholm.
Study outcome
Mental health problems were assessed by using a modified version of the Psychosomatic Problem Scale [ 18 ] shown to be appropriate for children and adolescents and invariant across gender and years. The scale was later modified [ 19 ]. In the modified version, items about difficulty concentrating and feeling giddy were deleted and an item about ‘life being great to live’ was added. Seven different symptoms or problems, such as headaches, depression, feeling fear, stomach problems, difficulty sleeping, believing it’s great to live (coded negatively as seldom or rarely) and poor appetite were used. Students who responded (on a 5-point scale) that any of these problems typically occurs ‘at least once a week’ were considered as having indicators of a mental health problem. Cronbach alpha was 0.69 across the whole sample. Adding these problem areas, a total index was created from 0 to 7 mental health symptoms. Those who scored between 0 and 4 points on the total symptoms index were considered to have a low indication of mental health problems (coded as 0); those who scored between 5 and 7 symptoms were considered as likely having mental health problems (coded as 1).
Primary exposure
Experiences of bullying were measured by the following two questions: Have you felt bullied or harassed during the past school year? Have you been involved in bullying or harassing other students during this school year? Alternatives for the first question were: yes or no with several options describing how the bullying had taken place (if yes). Alternatives indicating emotional bullying were feelings of being mocked, ridiculed, socially excluded, or teased. Alternatives indicating physical bullying were being beaten, kicked, forced to do something against their will, robbed, or locked away somewhere. The response alternatives for the second question gave an estimation of how often the respondent had participated in bullying others (from once to several times a week). Combining the answers to these two questions, five different categories of bullying were identified: (1) never been bullied and never bully others; (2) victims of emotional (verbal) bullying who have never bullied others; (3) victims of physical bullying who have never bullied others; (4) victims of bullying who have also bullied others; and (5) perpetrators of bullying, but not victims. As the number of positive cases in the last three categories was low (range = 3–15 cases) bully categories 2–4 were combined into one primary exposure variable: ‘bullied at school’.
Assessment year was operationalized as the year when data was collected: 2014, 2018, and 2020. Age was operationalized as school grade 9 (15–16 years) or 11 (17–18 years). Gender was self-reported (boy or girl). The school situation To assess experiences of the school situation, students responded to 18 statements about well-being in school, participation in important school matters, perceptions of their teachers, and teaching quality. Responses were given on a four-point Likert scale ranging from ‘do not agree at all’ to ‘fully agree’. To reduce the 18-items down to their essential factors, we performed a principal axis factor analysis. Results showed that the 18 statements formed five factors which, according to the Kaiser criterion (eigen values > 1) explained 56% of the covariance in the student’s experience of the school situation. The five factors identified were: (1) Participation in school; (2) Interesting and meaningful work; (3) Feeling well at school; (4) Structured school lessons; and (5) Praise for achievements. For each factor, an index was created that was dichotomised (poor versus good circumstance) using the median-split and dummy coded with ‘good circumstance’ as reference. A description of the items included in each factor is available as Additional file 1 . Socio-economic status (SES) was assessed with three questions about the education level of the student’s mother and father (dichotomized as university degree versus not), and the amount of spending money the student typically received for entertainment each month (> SEK 1000 [approximately $120] versus less). Higher parental education and more spending money were used as reference categories. School grades in Swedish, English, and mathematics were measured separately on a 7-point scale and dichotomized as high (grades A, B, and C) versus low (grades D, E, and F). High school grades were used as the reference category.
Statistical analyses
The prevalence of mental health problems and bullying at school are presented using descriptive statistics, stratified by survey year (2014, 2018, 2020), gender, and school year (9 versus 11). As noted, we reduced the 18-item questionnaire assessing school function down to five essential factors by conducting a principal axis factor analysis (see Additional file 1 ). We then calculated the association between bullying at school (defined above) and mental health problems using multivariable logistic regression. Results are presented as odds ratios (OR) with 95% confidence intervals (Cis). To assess the contribution of SES and school-related factors to this association, three models are presented: Crude, Model 1 adjusted for demographic factors: age, gender, and assessment year; Model 2 adjusted for Model 1 plus SES (parental education and student spending money), and Model 3 adjusted for Model 2 plus school-related factors (school grades and the five factors identified in the principal factor analysis). These covariates were entered into the regression models in three blocks, where the final model represents the fully adjusted analyses. In all models, the category ‘not bullied at school’ was used as the reference. Pseudo R-square was calculated to estimate what proportion of the variance in mental health problems was explained by each model. Unlike the R-square statistic derived from linear regression, the Pseudo R-square statistic derived from logistic regression gives an indicator of the explained variance, as opposed to an exact estimate, and is considered informative in identifying the relative contribution of each model to the outcome [ 20 ]. All analyses were performed using SPSS v. 26.0.
Prevalence of bullying at school and mental health problems
Estimates of the prevalence of bullying at school and mental health problems across the 12 strata of data (3 years × 2 school grades × 2 genders) are shown in Table 1 . The prevalence of bullying at school increased minimally (< 1%) between 2014 and 2020, except among girls in grade 11 (2.5% increase). Mental health problems increased between 2014 and 2020 (range = 1.2% [boys in year 11] to 4.6% [girls in year 11]); were three to four times more prevalent among girls (range = 11.6% to 17.2%) compared to boys (range = 2.6% to 4.9%); and were more prevalent among older adolescents compared to younger adolescents (range = 1% to 3.1% higher). Pooling all data, reports of mental health problems were four times more prevalent among boys who had been victims of bullying compared to those who reported no experiences with bullying. The corresponding figure for girls was two and a half times as prevalent.
Associations between bullying at school and mental health problems
Table 2 shows the association between bullying at school and mental health problems after adjustment for relevant covariates. Demographic factors, including female gender (OR = 3.87; CI 3.48–4.29), older age (OR = 1.38, CI 1.26–1.50), and more recent assessment year (OR = 1.18, CI 1.13–1.25) were associated with higher odds of mental health problems. In Model 2, none of the included SES variables (parental education and student spending money) were associated with mental health problems. In Model 3 (fully adjusted), the following school-related factors were associated with higher odds of mental health problems: lower grades in Swedish (OR = 1.42, CI 1.22–1.67); uninteresting or meaningless schoolwork (OR = 2.44, CI 2.13–2.78); feeling unwell at school (OR = 1.64, CI 1.34–1.85); unstructured school lessons (OR = 1.31, CI = 1.16–1.47); and no praise for achievements (OR = 1.19, CI 1.06–1.34). After adjustment for all covariates, being bullied at school remained associated with higher odds of mental health problems (OR = 2.57; CI 2.24–2.96). Demographic and school-related factors explained 12% and 6% of the variance in mental health problems, respectively (Pseudo R-Square). The inclusion of socioeconomic factors did not alter the variance explained.
Our findings indicate that mental health problems increased among Swedish adolescents between 2014 and 2020, while the prevalence of bullying at school remained stable (< 1% increase), except among girls in year 11, where the prevalence increased by 2.5%. As previously reported [ 5 , 6 ], mental health problems were more common among girls and older adolescents. These findings align with previous studies showing that adolescents who are bullied at school are more likely to experience mental health problems compared to those who are not bullied [ 3 , 4 , 9 ]. This detrimental relationship was observed after adjustment for school-related factors shown to be associated with adolescent mental health [ 10 ].
A novel finding was that boys who had been bullied at school reported a four-times higher prevalence of mental health problems compared to non-bullied boys. The corresponding figure for girls was 2.5 times higher for those who were bullied compared to non-bullied girls, which could indicate that boys are more vulnerable to the deleterious effects of bullying than girls. Alternatively, it may indicate that boys are (on average) bullied more frequently or more intensely than girls, leading to worse mental health. Social support could also play a role; adolescent girls often have stronger social networks than boys and could be more inclined to voice concerns about bullying to significant others, who in turn may offer supports which are protective [ 21 ]. Related studies partly confirm this speculative explanation. An Estonian study involving 2048 children and adolescents aged 10–16 years found that, compared to girls, boys who had been bullied were more likely to report severe distress, measured by poor mental health and feelings of hopelessness [ 22 ].
Other studies suggest that heritable traits, such as the tendency to internalize problems and having low self-esteem are associated with being a bully-victim [ 23 ]. Genetics are understood to explain a large proportion of bullying-related behaviors among adolescents. A study from the Netherlands involving 8215 primary school children found that genetics explained approximately 65% of the risk of being a bully-victim [ 24 ]. This proportion was similar for boys and girls. Higher than average body mass index (BMI) is another recognized risk factor [ 25 ]. A recent Australian trial involving 13 schools and 1087 students (mean age = 13 years) targeted adolescents with high-risk personality traits (hopelessness, anxiety sensitivity, impulsivity, sensation seeking) to reduce bullying at school; both as victims and perpetrators [ 26 ]. There was no significant intervention effect for bullying victimization or perpetration in the total sample. In a secondary analysis, compared to the control schools, intervention school students showed greater reductions in victimization, suicidal ideation, and emotional symptoms. These findings potentially support targeting high-risk personality traits in bullying prevention [ 26 ].
The relative stability of bullying at school between 2014 and 2020 suggests that other factors may better explain the increase in mental health problems seen here. Many factors could be contributing to these changes, including the increasingly competitive labour market, higher demands for education, and the rapid expansion of social media [ 19 , 27 , 28 ]. A recent Swedish study involving 29,199 students aged between 11 and 16 years found that the effects of school stress on psychosomatic symptoms have become stronger over time (1993–2017) and have increased more among girls than among boys [ 10 ]. Research is needed examining possible gender differences in perceived school stress and how these differences moderate associations between bullying and mental health.
Strengths and limitations
Strengths of the current study include the large participant sample from diverse schools; public and private, theoretical and practical orientations. The survey included items measuring diverse aspects of the school environment; factors previously linked to adolescent mental health but rarely included as covariates in studies of bullying and mental health. Some limitations are also acknowledged. These data are cross-sectional which means that the direction of the associations cannot be determined. Moreover, all the variables measured were self-reported. Previous studies indicate that students tend to under-report bullying and mental health problems [ 29 ]; thus, our results may underestimate the prevalence of these behaviors.
In conclusion, consistent with our stated hypotheses, we observed an increase in self-reported mental health problems among Swedish adolescents, and a detrimental association between bullying at school and mental health problems. Although bullying at school does not appear to be the primary explanation for these changes, bullying was detrimentally associated with mental health after adjustment for relevant demographic, socio-economic, and school-related factors, confirming our third hypothesis. The finding that boys are potentially more vulnerable than girls to the deleterious effects of bullying should be replicated in future studies, and the mechanisms investigated. Future studies should examine the longitudinal association between bullying and mental health, including which factors mediate/moderate this relationship. Epigenetic studies are also required to better understand the complex interaction between environmental and biological risk factors for adolescent mental health [ 24 ].
Availability of data and materials
Data requests will be considered on a case-by-case basis; please email the corresponding author.
Code availability
Not applicable.
Olweus D. School bullying: development and some important challenges. Ann Rev Clin Psychol. 2013;9(9):751–80. https://doi.org/10.1146/annurev-clinpsy-050212-185516 .
Article Google Scholar
Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: “Much ado about nothing”? Psychol Med. 2010;40(5):717–29. https://doi.org/10.1017/S0033291709991383 .
Article CAS PubMed Google Scholar
Arseneault L. The long-term impact of bullying victimization on mental health. World Psychiatry. 2017;16(1):27–8. https://doi.org/10.1002/wps.20399 .
Article PubMed PubMed Central Google Scholar
Moore SE, Norman RE, Suetani S, Thomas HJ, Sly PD, Scott JG. Consequences of bullying victimization in childhood and adolescence: a systematic review and meta-analysis. World J Psychiatry. 2017;7(1):60–76. https://doi.org/10.5498/wjp.v7.i1.60 .
Hagquist C, Due P, Torsheim T, Valimaa R. Cross-country comparisons of trends in adolescent psychosomatic symptoms—a Rasch analysis of HBSC data from four Nordic countries. Health Qual Life Outcomes. 2019;17(1):27. https://doi.org/10.1186/s12955-019-1097-x .
Deighton J, Lereya ST, Casey P, Patalay P, Humphrey N, Wolpert M. Prevalence of mental health problems in schools: poverty and other risk factors among 28 000 adolescents in England. Br J Psychiatry. 2019;215(3):565–7. https://doi.org/10.1192/bjp.2019.19 .
Article PubMed Central Google Scholar
Le HTH, Tran N, Campbell MA, Gatton ML, Nguyen HT, Dunne MP. Mental health problems both precede and follow bullying among adolescents and the effects differ by gender: a cross-lagged panel analysis of school-based longitudinal data in Vietnam. Int J Ment Health Syst. 2019. https://doi.org/10.1186/s13033-019-0291-x .
Bayer JK, Mundy L, Stokes I, Hearps S, Allen N, Patton G. Bullying, mental health and friendship in Australian primary school children. Child Adolesc Ment Health. 2018;23(4):334–40. https://doi.org/10.1111/camh.12261 .
Article PubMed Google Scholar
Hysing M, Askeland KG, La Greca AM, Solberg ME, Breivik K, Sivertsen B. Bullying involvement in adolescence: implications for sleep, mental health, and academic outcomes. J Interpers Violence. 2019. https://doi.org/10.1177/0886260519853409 .
Hogberg B, Strandh M, Hagquist C. Gender and secular trends in adolescent mental health over 24 years—the role of school-related stress. Soc Sci Med. 2020. https://doi.org/10.1016/j.socscimed.2020.112890 .
Kidger J, Araya R, Donovan J, Gunnell D. The effect of the school environment on the emotional health of adolescents: a systematic review. Pediatrics. 2012;129(5):925–49. https://doi.org/10.1542/peds.2011-2248 .
Saminathen MG, Låftman SB, Modin B. En fungerande skola för alla: skolmiljön som skyddsfaktor för ungas psykiska välbefinnande. [A functioning school for all: the school environment as a protective factor for young people’s mental well-being]. Socialmedicinsk tidskrift [Soc Med]. 2020;97(5–6):804–16.
Google Scholar
Bibou-Nakou I, Tsiantis J, Assimopoulos H, Chatzilambou P, Giannakopoulou D. School factors related to bullying: a qualitative study of early adolescent students. Soc Psychol Educ. 2012;15(2):125–45. https://doi.org/10.1007/s11218-012-9179-1 .
Vukojevic M, Zovko A, Talic I, Tanovic M, Resic B, Vrdoljak I, Splavski B. Parental socioeconomic status as a predictor of physical and mental health outcomes in children—literature review. Acta Clin Croat. 2017;56(4):742–8. https://doi.org/10.20471/acc.2017.56.04.23 .
Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. https://doi.org/10.1016/j.socscimed.2013.04.026 .
Stockholm City. Stockholmsenkät (The Stockholm Student Survey). 2021. https://start.stockholm/aktuellt/nyheter/2020/09/presstraff-stockholmsenkaten-2020/ . Accessed 19 Nov 2021.
Zeebari Z, Lundin A, Dickman PW, Hallgren M. Are changes in alcohol consumption among swedish youth really occurring “in concert”? A new perspective using quantile regression. Alc Alcohol. 2017;52(4):487–95. https://doi.org/10.1093/alcalc/agx020 .
Hagquist C. Psychometric properties of the PsychoSomatic Problems Scale: a Rasch analysis on adolescent data. Social Indicat Res. 2008;86(3):511–23. https://doi.org/10.1007/s11205-007-9186-3 .
Hagquist C. Ungas psykiska hälsa i Sverige–komplexa trender och stora kunskapsluckor [Young people’s mental health in Sweden—complex trends and large knowledge gaps]. Socialmedicinsk tidskrift [Soc Med]. 2013;90(5):671–83.
Wu W, West SG. Detecting misspecification in mean structures for growth curve models: performance of pseudo R(2)s and concordance correlation coefficients. Struct Equ Model. 2013;20(3):455–78. https://doi.org/10.1080/10705511.2013.797829 .
Holt MK, Espelage DL. Perceived social support among bullies, victims, and bully-victims. J Youth Adolscence. 2007;36(8):984–94. https://doi.org/10.1007/s10964-006-9153-3 .
Mark L, Varnik A, Sisask M. Who suffers most from being involved in bullying-bully, victim, or bully-victim? J Sch Health. 2019;89(2):136–44. https://doi.org/10.1111/josh.12720 .
Tsaousis I. The relationship of self-esteem to bullying perpetration and peer victimization among schoolchildren and adolescents: a meta-analytic review. Aggress Violent Behav. 2016;31:186–99. https://doi.org/10.1016/j.avb.2016.09.005 .
Veldkamp SAM, Boomsma DI, de Zeeuw EL, van Beijsterveldt CEM, Bartels M, Dolan CV, van Bergen E. Genetic and environmental influences on different forms of bullying perpetration, bullying victimization, and their co-occurrence. Behav Genet. 2019;49(5):432–43. https://doi.org/10.1007/s10519-019-09968-5 .
Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics. 2004;113(5):1187–94. https://doi.org/10.1542/peds.113.5.1187 .
Kelly EV, Newton NC, Stapinski LA, Conrod PJ, Barrett EL, Champion KE, Teesson M. A novel approach to tackling bullying in schools: personality-targeted intervention for adolescent victims and bullies in Australia. J Am Acad Child Adolesc Psychiatry. 2020;59(4):508. https://doi.org/10.1016/j.jaac.2019.04.010 .
Gunnell D, Kidger J, Elvidge H. Adolescent mental health in crisis. BMJ. 2018. https://doi.org/10.1136/bmj.k2608 .
O’Reilly M, Dogra N, Whiteman N, Hughes J, Eruyar S, Reilly P. Is social media bad for mental health and wellbeing? Exploring the perspectives of adolescents. Clin Child Psychol Psychiatry. 2018;23:601–13.
Unnever JD, Cornell DG. Middle school victims of bullying: who reports being bullied? Aggr Behav. 2004;30(5):373–88. https://doi.org/10.1002/ab.20030 .
Download references
Acknowledgements
Authors are grateful to the Department for Social Affairs, Stockholm, for permission to use data from the Stockholm School Survey.
Open access funding provided by Karolinska Institute. None to declare.
Author information
Authors and affiliations.
Stockholm Prevents Alcohol and Drug Problems (STAD), Center for Addiction Research and Department of Clinical Neuroscience, Karolinska Institutet, Solna, Sweden
Håkan Källmén
Epidemiology of Psychiatric Conditions, Substance Use and Social Environment (EPiCSS), Department of Global Public Health, Karolinska Institutet, Level 6, Solnavägen 1e, Solna, Sweden
Mats Hallgren
You can also search for this author in PubMed Google Scholar
Contributions
HK conceived the study and analyzed the data (with input from MH). HK and MH interpreted the data and jointly wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mats Hallgren .
Ethics declarations
Ethics approval and consent to participate.
As the data are completely anonymous, the study was exempt from ethical approval according to an earlier decision from the Ethical Review Board in Stockholm (2010-241 31-5).
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Principal factor analysis description.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Källmén, H., Hallgren, M. Bullying at school and mental health problems among adolescents: a repeated cross-sectional study. Child Adolesc Psychiatry Ment Health 15 , 74 (2021). https://doi.org/10.1186/s13034-021-00425-y
Download citation
Received : 05 October 2021
Accepted : 23 November 2021
Published : 14 December 2021
DOI : https://doi.org/10.1186/s13034-021-00425-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Adolescents
- School-related factors
- Gender differences
Child and Adolescent Psychiatry and Mental Health
ISSN: 1753-2000
- Submission enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Mental health, behavioural problems and treatment seeking among students commencing university in Northern Ireland
Roles Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing
Affiliation School of Psychology, Ulster University, Magee Campus, Derry/Londonderry, United Kingdom
Roles Conceptualization, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing
Affiliation Northern Ireland Centre for Stratified Medicine, Biomedical Sciences Research Institute Ulster University, C-TRIC, Altnagelvin Hospital, Derry/Londonderry, United Kingdom
Roles Methodology, Project administration, Writing – review & editing
Roles Conceptualization, Formal analysis, Methodology, Supervision, Writing – review & editing
Affiliation School of Psychology, Ulster University, Coleraine Campus, Coleraine, United Kingdom
Roles Conceptualization, Formal analysis, Supervision
Roles Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
- Margaret McLafferty,
- Coral R. Lapsley,
- Edel Ennis,
- Cherie Armour,
- Sam Murphy,
- Brendan P. Bunting,
- Anthony J. Bjourson,
- Elaine K. Murray,
- Siobhan M. O'Neill

- Published: December 13, 2017
- https://doi.org/10.1371/journal.pone.0188785
- Reader Comments
Mental health and behavioural problems are common among students commencing university. University life can be stressful and problems often exacerbate during their course of study, while others develop disorders for the first time. The WHO World Mental Health Surveys International College Student Project aims to conduct longitudinal research to examine and monitor student mental health and wellbeing. The Ulster University Student Wellbeing study, which commenced in September 2015 in Northern Ireland (NI), was conducted as part of this initiative (wave 1, n = 739), using the WMH-CIDI to examine psychopathology. Baseline prevalence rates of lifetime and 12-month mental health and substance disorders, ADHD and suicidality were high, with more than half of new undergraduate students reporting any lifetime disorder. Co-morbidity was common with 19.1% of students experiencing three or more disorders. Logistic regression models revealed that females, those over 21, non-heterosexual students, and those from a lower SES background were more likely to have a range of mental health and behavioural problems. Overall, 10% of new entry students received treatment for emotional problems in the previous year. However, 22.3% of students with problems said they would not seek help. The study provides important information for universities, policy makers and practice, on mental health and wellbeing in young people generally but particularly for students commencing university. The findings will assist in the development and implementation of protection and prevention strategies in the university setting and beyond.
Citation: McLafferty M, Lapsley CR, Ennis E, Armour C, Murphy S, Bunting BP, et al. (2017) Mental health, behavioural problems and treatment seeking among students commencing university in Northern Ireland. PLoS ONE 12(12): e0188785. https://doi.org/10.1371/journal.pone.0188785
Editor: Daimei Sasayama, Shinshu University School of Medicine, JAPAN
Received: April 25, 2017; Accepted: November 12, 2017; Published: December 13, 2017
Copyright: © 2017 McLafferty et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Data access restrictions apply for ethical reasons as data contain sensitive participant information. Restrictions are imposed by Ulster University Research Ethics Committee. Data are available from the Ulster University Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data (contact: [email protected] ).
Funding: This work was financed by a grant awarded to A. J. Bjourson under the European Union Regional Development Fund (ERDF) EU Sustainable Competitiveness Programme for N. Ireland & the Northern Ireland Public Health Agency (HSC R&D). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Many mental health problems emerge before the age of 18 with the period from 18 to 25 being a particularly susceptible developmental time in a person’s life [ 1 ]. For many young adults, this may coincide with their time at university. Starting university is a key life transition, which can be extremely stressful for some people. For a number of students, pre-existing mental health problems may be aggravated during this transition. These problems may persist or indeed worsen during their course of study and can have an impact on academic performance [ 2 – 4 ]. For others, however, the stress of university life and adapting to a new social environment can trigger psychopathology [ 5 , 6 ].
Recent research has revealed a high and increasing prevalence of psychopathology among students in higher education [ 7 ]. Indeed, the issue is becoming a growing concern globally [ 8 – 10 ]. For example, in 2014, a large-scale study reported that 32.6% of American students said that they were so depressed they found it difficult to function, 54% reported overwhelming anxiety and 8.1% had seriously considered suicide [ 11 ]. In 2015, depression rates had increased to 36.1%, anxiety to 58.6%, and seriously considering suicide rose to 10.3% [ 7 ]. In relation to clinical estimates, the Healthy Minds study of over 14,000 American college students reported that 17.3% met the criteria for depression, 7% for generalised anxiety disorders, 4.1% for panic disorders, 6.3% for suicide ideation and 15.3% for self-harm [ 12 ].
High prevalence rates of mental health problems and suicidality have also been found among university students in the UK. For example, when compared to their pre-entry levels, undergraduate students reported increased levels of anxiety during their first year [ 6 , 13 ], and poorer psychological wellbeing throughout their time at university [ 6 ]. Another study [ 14 ] reported that nearly a quarter of first year students had clinical levels of psychological distress. Furthermore, it has suggested that the increases in psychological problems may be related to widening participation in UK universities, with 17.3% of students having mental health problems, similar to rates found in the general population [ 15 ].
In addition to adapting to university life, many students are also adapting to their transition into adulthood. It has been suggested that the first few months at university are particularly challenging and stressful due to numerous psychosocial adjustments [ 16 ]. Some students may be living away from their family and friends for the first time. Others may be coming directly from schools, which were very structured, and they may find it difficult to adapt to a less structured academic setting [ 17 ]. Many older students often have the added responsibility of caring for family or work commitments, which can lead to added stress.
A large-scale study conducted in an Australian university reported that females, those aged 25–34, students with a low income and non-heterosexual students had the highest rates of mental health problems [ 18 ]. Additional studies corroborate that females have significantly higher rates of mental health problems [ 12 , 19 , 20 ]. Students who struggle financially also have significantly higher rates of mental health problems [ 5 , 21 ] than those who do not report financial concerns. Indeed, research has revealed that deprivation has a very negative impact on mental health in NI [ 22 ]. Furthermore, high rates of mental illnesses are especially common in those who identify as bi-sexual or homosexual [ 23 ].
Moreover, while mental health problems are highly prevalent and persistent, research has shown that many students who meet the criteria for a disorder do not receive treatment [ 2 ]. For example, a study found that only 36% of students in the US who had a mental health problem received treatment in the previous 12 months [ 24 ]. The uptake of treatment was even lower in a recent cross-national study which examined findings from 21 countries, with only 16.4% of students receiving treatment for their mental health problems in the previous year [ 4 ].
Significant gender differences in help seeking have also been found, with 11% of female students looking for help in comparison to 6% of males [ 25 ]. A global survey found that while males made up 43.8% of the student body, they only comprised of 33.9% of clients who presented to college counselling centres [ 26 ], suggesting that males tend not to seek help for mental health problems. While females generally have higher rates of mood and anxiety disorders [ 26 ] this only partially accounts for the gender difference found in help seeking.
While some studies [ 15 , 27 ] reported comparable rates of mental health disorders between the general population and university students, other studies have found significantly higher prevalence rates among students [ 21 , 28 ]. For instance, a study conducted in an Australian university reported elevated prevalence rates in the student population when compared with the general population, with a quarter of students experiencing very high levels of psychological problems [ 29 ]. The first onset of suicidal thoughts and behaviours have also been found to be higher among college students in comparison to the general population [ 3 ].
However, cross-national research carried out by the WHO World Mental Health Survey Initiative revealed that 20.3% of students had a 12-month mental health disorder in comparison to 21.4% of non-students in the population. Conversely, the highest level of 12-month mental health problems was found in those who had commenced university but failed to graduate, with 25% of those who dropped out reporting psychological problems [ 4 ]. Additionally, those with mental health problems may be less likely to get a place in university, which may partially account for the slightly higher rate of psychopathology found in some studies for non-students [ 4 ].
Studies corroborate that mental health problems can impact severely on a student’s life [ 30 ]. Indeed, mental health problems considerably disrupt learning ability [ 10 ], with psychopathology, particularly anxiety and depression, being associated with lower grades [ 31 ]. In addition, students who had lifetime suicide plans and attempts when entering university obtained significantly lower grades [ 3 ], as did those who engaged in non-suicidal self-injury [ 32 ]. Issues with attention and concentration can also impact on grades in addition to mental wellbeing. For example, ADHD is often co-morbid with a range of mental health disorders [ 33 ]. Moreover, research has found that of those with DSM IV/CIDI mental health disorders in the previous 12 months, 83.1% of disorders commenced before students started college and that pre-matriculation onset was associated with higher attrition rates and lower university entry rates [ 4 ].
It is important therefore to establish baseline prevalence rates of disorders and to understand the socio-demographic predictors of mental health and behavioural problems when students first enter universities. This point of entry information may be very beneficial for universities, helping them to provide adequate support for students and addressing problems early, minimising risk and improving grades and retention rates. A report examining the mental health of students in higher education recommends the use of longitudinal studies to gain greater insight into psychopathology in the student body [ 9 ]. Research such as that carried out by the WHO World Mental Health Surveys International College Student Project (WMH-ICS) will gather important information about the wellbeing of the student population. Conducted as part of this initiative, the Ulster University Student Wellbeing Study aims to examine and monitor student health and wellbeing during their time at university.
The main aims of the current study are to provide baseline prevalence rates of mental health problems, ADHD and suicidal behaviour among first year undergraduate students, who have newly registered at Ulster University, NI. The study also examines gender variations and age of onset in reported lifetime and 12-month disorders. Socio-demographic correlates of mental health disorders will be explored using logistic regression. Help seeking behaviour and the use of medication or counselling for mental health problems will subsequently be examined.
In September 2015, the Ulster University Student Wellbeing study (UUSWS) commenced on four campuses across Northern Ireland (Belfast, Coleraine, Derry/Londonderry and Jordanstown). The UUSWS study is being conducted as part of the WHO World Mental Health International College Student Project (WMH-ICS).An observational, longitidunal cohort study design is used for all studies. Prospective studies, such as this, can be very benefical in that recall issues are minimised, sequences or patterns of events can be established and causal relationships may be inferred. Ethical approval was obtained for the Northern Ireland study from the Ulster University Research Ethics Committee (REC/15/0004).
Overall, 4,365 first year undergraduates registered at Ulster University in the year 2015–2016. A week prior to registration an email was circulated to all new first year undergraduate students due to register at the university, with a detailed participant information sheet attached outlining the aims of the study and methodology to be employed. Students were asked to consider participating in the study. Trained researchers recruited students on the various campuses following registration. A total of 1,646 participants provided informed written consent to take part in the study. Saliva/DNA samples (4ml) were collected from each participant using the Oragene-500 (DNA Genotek) self-collection kits according to the manufacturer’s instructions and stored for genetic analysis. Each student was provided with a card containing their unique ID number and a link to the survey. The survey instrument was administered on-line using Qualtrics software. The link to the survey was also emailed to each participant. The survey was fully completed by 739 of the participants. The completed response rate was 16.95% in relation to the total number of first year students registered. While other students partially completed the survey only those who responded to all questions are included in the analyses for the current study ( N = 739), of which 462 were female, 274 were male, and three students identified as other (1 transgender male to female, 1 transgender female to male and 1 non-binary). The average age of participants was 21( M = 20.69, SD = 5.313), with an age range of 18 to 49. All participants were residents of the United Kingdom (UK) or the Republic of Ireland (ROI). International students, those repeating first year and students under the age of 18 were excluded from the study.
Diagnostic assessment
The WMH-ICS surveys use questions adapted from the WMH Composite International Diagnostic Interview (CIDI), version 3.0, [ 34 ] to explore the prevalence of mental health problemsin accordance with ICD and DSM criteria. Good concordance has been found between the WMH-CIDI and clinical assessments [ 35 ]. The instrument includes screening sections for depression, bi-polar disorder, anxiety, panic attacks or panic disorder and other serious emotional problems. The Alcohol Use Disorders Identification Test (AUDIT), developed by the WHO [ 36 ], was used to screen for probable alcohol dependence. Drug abuse and dependence was measured using The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), which has been found to be a reliable [ 37 ] and valid screening test for drug use [ 38 ]. ADHD was assessed using the WMH-CIDI screener for Attention-Deficit/Hyperactivity Disorder, with questions focusing on difficulties with attention and concentration in the previous 6 months. Suicidal thoughts, plans and attempts were assessed using items from the Self-Injurious Thoughts and Behaviour Interview, the SITBI [ 39 ], an instrument with strong psychometric properties. At the end of the survey a list of useful resources were provided for participants with links to information, help and support. If students were deemed to be at risk of suicide, due to their responses to certain questions, such as if they attempted or planned suicide in the previous year, an alert was triggered. Carecall, the university counselling provider, contacted these students by phone to establish if they required help and provided information on support available.
Help seeking and treatment for emotional problems
Questions from the WMH-CIDI services section were adapted and used to assess help seeking behaviour and receipt of treatment, including medication or counselling for emotional problems. For example, students were asked how likely they would be to go to the student counselling provider or someone else, such as a doctor or mental health professional if they developed a serious emotional problem in the coming year. Students were also asked if they had received either psychological counselling or medication for an emotional problem, how old they were when they first received treatment, if they were still in treatment and how old they were the most recent time they received treatment.
Data analysis
Weights were created using the gender and age characteristics of the first year student population at Ulster University, subsequently these were applied to analyses to ensure that the study results wererepresentative of the total student population. Lifetime and 12-month prevalence rates for a range of mental health and substance disorders, ADHD and suicidality were calculated. Any disorder included any lifetime mental health disorder or suicidality or substance disorder or 6-month ADHD. Chi-square tests for independence examined gender differences in prevalence rates. The age of onset was examined, with independent samples t-tests conducted to determine gender variations. Differences in help seeking and use of medication or counselling in the previous year between males and females and those with and without disorders were examined using chi-square tests for independence. Logistic regression analyses were used to explore relationships between mental health problems and gender, age (21 and over, under 21), sexuality (heterosexual, non-heterosexual), current finances (poor, enough, comfortable, well-to-do) and where the person grew up (large city, suburbs, small city, town or village, rural setting). All analyses were conducted using SPSS (version 23).
Lifetime prevalence rates of mental health disorders, substance disorders, suicidality and 6-month ADHD are presented in Table 1 . The highest prevalence rates were found for suicidality (31%), major depressive episode (24.2%) and generalised anxiety disorder (22.6%). Chi-square tests for independence revealed significant gender differences in reported rates. Females were significantly more likely to experience mood and anxiety problems as well as suicidality. Males had significantly higher rates of drug abuse and dependence but numbers were very low (4.8%). The overall prevalence rate for experiencing any lifetime disorders was 53.2%, with females experiencing significantly higher rates than males. Overall, 19.1% of students including the three people who identified themselves as either transgender or non-binary experienced 3 or more disorders.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0188785.t001
Table 2 reports 12-month prevalence rates for a range of mental health disorders, substance dependence or abuse, suicidality and 6-month ADHD. The number of people who met the criteria for any 12-month disorders were high at 47.5%, although rates were lower than lifetime prevalence rates. Greater variations between lifetime and 12-month prevalence rates was found for suicidality. Gender differences were found in 12-month prevalence rates for mood and anxiety disorders, with females reporting significantly higher rates than males. Significant differences were also revealed for drug abuse or dependence, with males having higher rates (3.8%) than females (0.2%). Again, it should be noted that numbers were very low. In contrast to lifetime prevalence rates for suicidality, no significant gender difference was found in 12-month rates. Additionally, no significant gender variations were found in prevalence rates for any disorders reported in the previous year. The overall rate of any disorders reported in the previous 12-months remained high however at 47.5%, with 15.3% experiencing 3 or more disorders.
https://doi.org/10.1371/journal.pone.0188785.t002
The age of onset for a range of mental health and substance disorders, suicidality and ADHD are presented in Table 3 . The average age of onset for most problems was between 14 and 17. However the average age of onset for 6-month ADHD was lower ( M = 11.5, SD = 5.36). Significant gender differences in average age on onset for ADHD were also revealed, with males having onset at a younger age ( M = 10.09, SD = 4.77) than females [ M = 12.37, SD = 5.60; t (135) = -2.484, p = .014]. Some problems started as early as 4, with absolute values of between 8 and 41.
https://doi.org/10.1371/journal.pone.0188785.t003
Results of logistic regression analyses examining associations between socio-demographic variables and lifetime mental health problems are presented in Table 4 . Females were more likely to develop mood ( OR = 1.565, p < .05), anxiety ( OR = 1.609, p < .05) or any disorder ( OR = 1.425, p < .05), compared to males. When compared to students under the age of 21, the older age group were nearly twice as likely to have experienced a major depressive episode ( OR = 1.954, p < .01). In contrast to heterosexual students, those who said they were non-heterosexual were nearly three and a half times more likely to have a MDE, nearly four and a half times more likely to have GAD and five times more likely to have any lifetime disorder. In relation to current financial position, when compared to those who said they were poor, those who were comfortable were significantly less likely to have any lifetime disorder. In comparison to those who grew up in a rural setting, students raised in a suburban setting were more likely to have any disorder ( OR = 1.886, p < .05).
https://doi.org/10.1371/journal.pone.0188785.t004
Table 5 presents findings regarding treatment for emotional problems. Overall 10% of students received treatment for an emotional problem in the year prior to commencing university. Significantly more females (13.8%) received treatment than males (5.3%). A strong association was found between receipt of treatment and lifetime (χ 2 (1, n = 738) = 66.454, p < .001) and 12-month disorders (χ 2 (1, n = 737) = 66.142, p < .001). However, less than 20% of those with mental health problems received treatment. Moreover, 18.6% of students said that they would probably not seek help for an emotional problem. Many of these students screened positively for a range of problems. Indeed, chi-square tests for independencerevealed strong associations between probably not seeking help and both lifetime (χ 2 (1, n = 733) = 7.063, p < .01) and 12-month disorders (χ 2 (1, n = 735) = 5.408, p < .05), with 22.3% of those with problems saying they would not seek help. While more males (21.4%) than females (15.8%) reported that they would not seek help, the difference was not significant. The transgender and non-binary students did not get treatment in the previous year and reported they would probably not seek help.
https://doi.org/10.1371/journal.pone.0188785.t005
The current study provides baseline estimates for mental health and substance disorders, suicidality and ADHD among students commencing study at Ulster University, NI. High lifetime and 12-month prevalence rates for a range of problems were revealed. Almost a quarter of students experienced a lifetime major depressive episode, over a fifth had GAD and more than a tenth had ADHD or endorsed probable alcohol dependence. Moreover, nearly a third of students reported experiencing suicidal thoughts, plans or attempts during their lifetime. Overall, more than a half of the students experienced some lifetime disorder. Co-morbidity of problems was common with just under a fifth experiencing three or more disorders. The findings concur with other studies which found high levels of mental health and behavioural problems in the student population [ 3 , 4 ], although the rates revealed were higher than clinical estimates from US studies [ 12 ].
Prevalence rates for the previous 12 months were slightly lower than lifetime rates as would be expected. However, the reported rates remained high, with more than a fifth of students having a major depressive episode or GAD in the year prior to commencing university. It should be remembered that many of these students completed A levels or Leaving Certificate (ROI) exams during this time which may have impacted on their mental health and wellbeing. Additionally, since the average age of participants in this study was 21, this period for many signals their transition into adulthood which may partially account for the high rates of disorders reported. Indeed, the average age of onset for most disorders in the current study was between the ages of 14 and 17. A previous epidemiological study based on the NI population found that age of onset for many mental health problems were during these formative teenage years [ 40 ]. The authors recommended that policies and interventions should be prioritised for young people to address mental health issues before they arise.
Numerous gender differences in prevalence rates were revealed in the current study. In accordance with previous studies, females had higher lifetime rates of mood and anxiety problems [ 20 ], and suicidal behaviour. However, no significant gender differences were found for any 12-month disorders or suicidality, which contradicts previous evidence that females in this age group are at higher risk of having a current mental disorder [ 12 ]. This may reflect differences in age of onset, illness severity or duration, or help seeking, and as such merits further investigation. In line with previous studies, males were more likely to report drug abuse or dependence, although no gender variation was found for alcohol dependence contrary to other research in this area [ 20 ]. Overall females were more likely to have any lifetime disorder as well as higher rates of co-morbidity. While no significant gender difference was found for the prevalence of ADHD, age of onset was significantly lower for males.
Further analyses revealed numerous significant socio-demographic risk factors for mental health problems. In accordance with previous research, the study found that females, students over 21, those with a lower income and non-heterosexual students had the highest rates of mental health problems [ 5 , 8 , 23 ]. Students over 21 were significantly more likely to have a mood disorder. A previous study [ 40 ] found that the age of onset for mood disorders in the NI population was 32. This could suggest that many of the participants in the current study may have yet to develop a mood disorder and it is important therefore to address any issues before the onset of problems. The findings indicate that universities also need to be mindful of the increasing numbers of students from disadvantaged families with low socio-economic status. Non-heterosexual students also had a heightened risk of experiencing a range of mental health disorders and it is important therefore that information, help and support is available on campus to address their needs.
A key finding from this study, which warrants careful consideration, is the fact that many students with pre-existing problems said that they did not receive treatment and that they would not seek help for an emotional problem. This may be related to the severity of their symptoms, with some having only mild symptoms that did not require treatment. Others may not be fully aware of their problems, or they may have not been diagnosed yet. However, since many students met the criteria for a disorder it is reasonable to assume that there is unmet need and that they would benefit from treatment. Females received more treatment since they were also more likely to have a mental health problem but this is likely to only partially account for the gender difference found. Males were less likely to look for help. Some would suggest that it is due to stigma, embarrassment and an unwillingness to express emotions [ 25 , 41 ]. It may also be related to how serious they perceive the illness to be. One study [ 2 ] found that while many students with psychological problems were aware that they needed help, service use was low. Others propose that stigma only partially accounts for this and that universities need to look at innovative ways to encourage behaviour change [ 12 ].
It is important therefore to carefully consider strategies to encourage help-seeking behaviour, increasing the uptake of services to address these problems. This may include anti-stigma campaigns, gatekeeper training and effective screening programmes [ 12 ]. Additionally, the quality and quantity of counselling services, which are often overstretched, needs to be addressed in all universities, with flexible opening hours, prompt responses, reduced waiting lists and free sessions to students in need [ 42 ].
While studies show that the uptake of services is low in comparison to the levels of mental health problems reported in the student population, the number of students accessing counselling services has nonetheless grown in recent years. For example, a recent report found an increase of 50% in the past 5 years [ 43 ]. Increases in awareness of mental illness may have led to an upsurge in treatment seeking. Such findings are promising, indicating that more students are getting help, with early interventions and treatment helping to alleviate problems. However, a large proportion of mental health issues remain untreated. A review of the evidence suggests that it is important to have ongoing campaigns to increase awareness among students about the services and support that is available within the university and from other external sources [ 44 ].
Limitations
While the study provides important information regarding student mental health and wellbeing, several limitations should be considered when interpreting the findings. For instance, the on-line survey utilises self-report questionnaires which are often criticised for providing inaccurate results due to recall issues. However, since many of the sample was 21 or younger, recall issues should not have a great impact. Although prevalence rates of most major mental health disorders are reported in the current study, those disorders that are not characterised easily by self-report such as psychotic disorders were not included. Another limitation of the study is that the response rate is low and hence precludes us from safely generalising to the student population within this university. Furthermore, many more females participated. Sampling weights however were applied to address these issues but possible response bias should be considered. It is difficult to determine therefore exactly how representative the current study is. Previous reports suggest that people with mental health problems may be less likely to participate in studies such as this, due to stigma or a fear that if they reveal a mental health problem that it may impact on their future career [ 45 ], which may indicate that our findings are an underestimate of the prevalence of mental health disorders. However, it is also possible that those with mental health problems may be more likely to engage in such studies due to inherent interest in the study, meaning that rates reported may be higher than the true prevalence. The rates of mental health disorders reported, however, are comparable to other studies of student mental health in the UK [ 9 ] and the general population in Northern Ireland [ 40 ].
Conclusions
Previous studies suggest that many students have mental health and behavioural problems while at university which can impact on their wellbeing and may result in elevated attrition rates. The current study extends on these findings, providing important information on baseline rates of mental health and behavioural problems, along with help seeking in a representative sample of students commencing university in NI. Such findings mean that those in need of help are identified early and provided with information on available services. This may lead to improved retention rates and academic success, as well as maintaining or improving psychological health and wellbeing beyond the university years.
A review of the evidence suggests that it is essential to increase awareness among students about the services and support that is available, as well as providing guidance for university staff to assist students with mental health difficulties [ 44 ]. Staff should be adequately equipped to make referrals and know where students can get the help they require. Improved screening for disorders and early diagnosis are also important. By intervening early and encouraging help-seeking, mental health and behavioural problems can be treated before they escalate and grades and retention rates may be improved. The UU Student Wellbeing Survey will monitor student’s health and wellbeing throughout their time at university, by conducting longitudinal research on all those who initially consented to participate, with findings helping to inform policy makers and practice within the university setting and beyond.
Acknowledgments
We thank the Northern Ireland Centre for Stratified Medicine and School of Psychology staff and postgraduate students for assistance with the recruitment during registration week. We also thank the Students Union, Student Support and Student Administration Services at Ulster University, and Inspire Students, for their assistance in this study. We would also like to thank Dr Randy Auerbach and his team at Harvard University for their assistance in data management.
- View Article
- PubMed/NCBI
- Google Scholar
- 7. Association ACH. American College Health Association-National College Health Assessment II: Fall 2015 Reference Group Undergraduates Executive Summary. Hanover, MD; 2016.
- 9. Psychiatrists TRCo. Mental health of students in higher education. London, UK; 2011.
- 11. Association ACH. American college health association-national college health assessment II: Spring 2014 reference group data report. Hanover, MD; 2014.
- 23. Higgins A, Doyle L, Downes C, Murphy R, Sharek D, DeVries J, et al. The LGBTIreland Report: national study of the mental health and wellbeing of lesbian, gay, bisexual, transgender and intersex people in Ireland. Dublin; 2016.
- 26. Reetz DR, Krylowicz B, Mistler B. The association for university and college counseling center directors annual survey. 2014.
- 34. Kessler RC, Ustun TB. The WHO world mental health surveys: global perspectives on the epidemiology of mental disorders. New York; 2008.
- 43. Yeung P, Weale S, Perraudin F. University mental health services face strain as demand rises 50%. UK: The Guardian; 2015 [Available from: https://www.theguardian.com/education/2016/sep/23/university-mental-health-services-face-strain-as-demand-rises-50 .
A survey of special education teachers and specialists in Saudi Arabia on the use of collaborative practices to support the mental health of students with disabilities
- Published: 11 April 2024
Cite this article
- Nourah Ibrahim Abdullah Albash ORCID: orcid.org/0000-0003-3547-7733 1
The current study aimed to identify the reality of collaborative practices to facilitate access to mental healthcare by students with disabilities in the Kingdom of Saudi Arabia. Descriptive survey approach was used to obtain data from 71 teachers and specialists ( n = 42 teachers; n = 29 specialists), who were identified using snowball sampling method, on the use of collaboration to support the mental health of such students. Statistical processing was done to obtain (a) the frequencies and percentages for the analysis of the participants’ responses, and (b) the means to organize these data. According to the findings, while Saudi teachers and specialists in special education agree on the importance of collaborating to provide these services to those with disabilities, the survey responses indicate that Saudi Arabia lacks clear directives in the form of regulations, laws, incentives, and training that would help facilitate the implementation of these practices as required. Based on these and other findings, a proposal is made on how to increase collaboration among stakeholders to create better access to mental healthcare, when needed, for those in the population of individuals with disabilities receiving special education support in schools in Saudi Arabia. In addition, the respondents indicated they perceive a lack of understanding of the different psychological issues individuals with disabilities may encounter and how these can be treated. The current study develops recommendations based on the findings to address these concerns as well as provides recommendations for future research.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
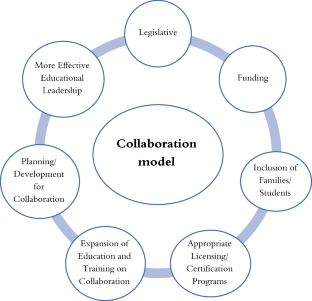
Availability of Data and Material
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Aalatawi, R. (2023). Teachers’ perceptions of the barriers to inclusive education of kindergarten students with disabilities in Saudi Arabia. International Journal of Learning, Teaching and Educational Research, 22 (2). https://doi.org/10.26803/ijlter.22.2.19
Abbas, M., Nofal, M., Al-Issa, M., & Abu Awwad, F. (2007). Introduction to research methods in education and psychology . Dar Al Masirah.
Google Scholar
Abu Fakhr, G. (2001). The cooperative relationship between parents and workers in special education institutions and its relationship to some variables. The Arab Journal of Education, Tunis, 21 (2), 34–68.
Abu Nayyan, I. (2007). Counseling and group work as one of the educational methods for providing educational difficulties services in the middle and secondary stages. Journal of the College of Education in Zagazig, Egypt, 55 , 243–282.
ADA Northeast Center. (2018). Mental health conditions in the workplace and the ADA . ADA National Network. https://adata.org/sites/adata.org/files/files/Mental_Health_Conditions_final2018.pdf . Accessed 11 Mar 2023
Alabdallat, B., Alkhamra, H., & Alkhamra, R. (2021). Special education and general education teacher perceptions of collaborative teaching responsibilities and attitudes towards an inclusive environment in Jordan. Frontiers in Education, 6 , 739384. https://doi.org/10.3389/feduc.2021.739384
Article Google Scholar
Al-Adl, A. (2013). The reference in disabilities, psychological disorders, and special education methods . Dar Al-Kitab Al-Hadith: Cairo.
Alamer, M., Alsaad, A., Al-Ghareeb, M., Almomatten, A., Alaethan, M., & AlAmeer, M. A. (2021). Mental stigma among Al-Ahsa population in Saudi Arabia. Cureus, 13 (11), e19710. https://doi.org/10.7759/cureus.19710
AlAteeq, D., AlDaoud, A., AlHadi, A., AlKhalaf, H., & Miley, R. (2018). The experience and impact of stigma in Saudi people with a mood disorder. Annals of General Psychiatry, 17 , 15. https://doi.org/10.1186/s12991-018-0221-3
Al-Battal, Z. (2019). Practice level of consultation and collaboration between learning disable students’ teachers and normal students teachers in elementary schools in Riyadh. Scientific Journal of King Faisal University, 20 (2), 161–188. https://services.kfu.edu.sa/scientificjournal/Handlers/FileHandler.ashx?file=h2028.pdf&Folder=UploadFiles . Accessed 27 Feb 2023
Algethami, R. K. (2022). Assessing the quality of training programs for teachers of students with disabilities in light of recent trends in the Kingdom of Saudi Arabia. PLoS ONE, 17 (7), e0270538. https://doi.org/10.1371/journal.pone.0270538
Alhamaudi, F. A. (1996). Attitudes toward disabilities in Saudi Arabia and their relationship to disability and responsibility framework [Doctoral dissertation, University of Illinois Institute of Technology] . ProQuest Theses 9625728. https://www.proquest.com/openview/62e2d99e79d165363100fb7f9aaf4a9f/1?pq-origsite=gscholar&cbl=18750&diss=y . Accessed 2 May 2023
Alharthi, N., & Evans, D. (2017). Special education teachers’ attitudes toward teaching students with learning disabilities in middle schools in Saudi Arabia. International Journal of Modern Education Studies, 1 (1). https://doi.org/10.51383/ijonmes.2017.13
Alhossyan, F. (2023). Collaboration between special and general education teachers: A systematic review. Information Sciences Letters , 12 (4), 1021–1029. https://doi.org/10.18576/isl/120424
Al-Natour, M., Amr, M., Al-Zboon, E., & Alkhamra, H. (2015). Examining collaboration and constrains [ sic ] on collaboration between special and general education teachers in mainstream schools in Jourdan. International Journal of Special Education , 30 (1), 1–14. https://files.eric.ed.gov/fulltext/EJ1094801.pdf . Accessed 18 May 2023
Alqahtani, R. F., Alshuayl, M., & Ryndak, D. L. (2021). Special education in Saudi Arabia: A descriptive analysis of 32 years of research. Division of International Special Education and Services, 24 (2), 76–85. https://doi.org/10.9782/JISNE-D-19-00039
Al-Quraini, T. (2015). Obstacles to the practice of collaboration between general education teachers and special education teachers in teaching students with disabilities in regular schools. Journal of Educational Sciences, Ain Shams University, (39), 215 –270. https://faculty.ksu.edu.sa/sites/default/files/bhth_wyq_lml_ljy_fy_brmj_ltrby_lkhs.pdf . Accessed 25 Jul 2023
AlShamare, A. H. (2018). Consultation and collaboration in special education programs: Adapting the American model to the Saudi Arabian context. Journal of Education and Practice , 9 (12), 69–79. https://faculty.ksu.edu.sa/sites/default/files/my_search_1.pdf . Accessed 11 Mar 2023
Al-Shammari, A. (2005). Counseling and group work and their role in forming an integrated working relationship between workers in special education programs. In Symposium on Special Education in the Kingdom of Saudi Arabia: Keeping Up with Modernization and Future Challenges , King Saud University, Riyadh, Kingdom of Saudi Arabia. https://elibrary.mediu.edu.my/books/MAL06635.pdf . Accessed 18 May 2023
Al-Tohamy, M. (2010). Ingredients and obstacles to the success of work teams. Journal of Administrative Development, 28 (129), 50–55.
Americans With Disabilities Act of 1990, 42 U.S.C. § 12101 et seq . (1990).
Amey, M. J., Eddy, P. L., & Ozaki, C. C. (2007). Demands for partnership and collaboration in higher education: A model. New Directions for Community Colleges, 2007 (139), 5–14. https://doi.org/10.1002/cc.288
Auster, E. R., Feeney-Kettler, K. A., & Kratochwill, T. R. (2006). Conjoint behavioral consultation: Application to school-based treatment of anxiety disorders. Education and Treatment of Children, 29 (2), 243–256. https://www.jstor.org/stable/42899884 . Accessed 23 Apr 2023
Bakhsh, A. (2009). The reality of training programs for special education teachers in the Kingdom of Saudi Arabia and their development in the light of their perceptions of their training needs. Educational Journal - Academic Publishing Council, Kuwait University, 23 (90), 125–178.
Bin Battal, Z. M. (2016). Special education in Saudi Arabia. International Journal of Technology and Inclusive Education (IJTIE), 5 (2), 880–886. https://doi.org/10.20533/ijtie.2047.0533.2016.0113
Bouillet, D. (2013). Some aspects of collaboration in inclusive education – Teachers’ experiences. Center for Educational Policies Journal, 3 (2), 93–117.
Bukhary, M. A. (2021). Collaboration in early intervention in Saudi Arabia: Reality and barriers. Multicultural Education, 7 (9), 447. https://doi.org/10.5281/zenodo.5528851
Carter, E. (2019). Mental health stigma in America: What it is, and how to help. GoMo Health . https://gomohealth.com/2019/mental-health-stigma-in-america-what-it-is-and-how-to-help/ .
Cook, L., & Friend, M. (1991). Principles for the practice of collaboration in schools. Preventing School Failure: Alternative Education for Children and Youth, 35 (4), 6–9. https://doi.org/10.1080/1045988X.1991.9944251
Coombs, N. C., Meriwether, W. E., Caringi, J., & Newcomer, S. R. (2021). Barriers to healthcare access among U.S. adults with mental health challenges: A population-based study. SSM Population. Health, 15 , 100847. https://doi.org/10.1016/j.ssmph.2021.100847
Council for Exceptional Children. (2015). What every special educator must know: Professional ethics and standards . https://exceptionalchildren.org/sites/default/files/2020-07/Standards%20for%20Professional%20Practice.pdf . Accessed 27 Jun 2023
Damore, S. J., & Murray, C. (2009). Urban elementary school teachers’ perspectives regarding collaborative teaching practices. Remedial and Special Education, 30 (4), 234–244. https://doi.org/10.1177/0741932508321007
Education of All Handicapped Children Act of 1975, Public Law 94–142.
Emam, M. M. (2016). Inclusive education for children with disabilities in the Gulf countries in the light of world declarations (an analytical study). Arab Childhood Journal, 17 (66), 9–36. http://search.shamaa.org/PDF/Articles/KUJac/JacVol17No66Y2016/jac_2016-v17-n66_009-036.pdf .
Gable, R. A., Mostert, M. P., & Tonelson, S. W. (2004). Assessing professional collaboration in schools: Knowing what works. Preventing School Failure, 48 (3), 4–8. https://doi.org/10.3200/PSFL.48.3.4-8
Ghorab, H. (2007). Psychological problems among disabled children in inclusive schools from the point of view of their teachers in Gaza Governorate and ways to overcome them. Journal of the Islamic University for Human Research - Scientific Research and Postgraduate Studies Affairs at the Islamic University - Gaza - Palestine, 15 (1), 533–560. https://search.mandumah.com/Record/645382 .
Grier, B. C., & Bradley-Klug, K. L. (2011). Collaborative consultation to support children with pediatric health issues: A review of the Biopsychoeducational Model. Journal of Educational & Psychological Consultation, 21 (2), 88–105. https://doi.org/10.1080/10474412.2011.571522
Hanafi, A., & Alralris, T. (2008). Views of special education teachers on the preparation of the individual educational program and the difficulties of its application in some institutes and programs of special education in the Kingdom of Saudi Arabia. Journal of Psychological Counseling, Egypt, 22 , 181–243.
Heath, C. (2023). What is descriptive research? Dovetail. https://dovetail.com/research/descriptive-research/ . Accessed 28 Feb 2023
Hernandez, S. J. (2013). Collaboration in special education: Its history, evolution, and critical factors necessary for successful implementation. U.S.-China Education Review , 3 (6), 480–498. https://eric.ed.gov/?id=ED544122 . Accessed 28 Jul 2023
Hyatt, K. J., & Filler, J. (2011). LRE re-examined: Misinterpretations and unintended consequences. International Journal of Inclusive Education, 15 (9), 1031–1045. https://doi.org/10.1080/13603116.2010.484509
Individuals With Disabilities Education Act, 20 U.S.C. § 1400 (2004).
Johnson, W. L., & Ruggles, M. (2016). Bridging the gap in early childhood special education services: Collaboration between universities and local schools. YC Young Children Journal, 71 (1), 38–43. https://www.jstor.org/stable/ycyoungchildren.71.1.38 . Accessed 27 Jun 2023
Jones, B. A. (2012). Fostering collaboration in inclusive settings: The special education students at a glance approach. Intervention in School and Clinic, 47 (5), 297–306. https://doi.org/10.1177/1053451211430113
Kaiser Family Foundation. (2023). Status of state action on the Medicaid expansion decision [Content last reviewed May 8, 2023]. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ . Accessed 15 Jun 2023
Khairuddin, K. F., Dally, K., & Foggett, J. (2016). Collaboration between general and special education teachers in Malaysia. Journal of Research in Special Educational Needs, 16 (S1), 909–913. https://doi.org/10.1111/1471-3802.12230
Kingdom of Saudi Arabia. (2016). Vision 2030. http://vision2030.gov.sa . Accessed 2 Jul 2023
Lombardi, P. (n.d.). Instructional methods, strategies and technologies to meet the needs of all learners . Granite Press Books. https://granite.pressbooks.pub/edu606-701/ . Accessed 5 Jul 2023
Mbuvha, T. (2019). Kinds of support offered by the disability unit to students with disabilities at institutions of higher learning in South Africa: A case study of the University of Venda. Journal of Student Affairs in Africa, 7 (2), 57–73. https://doi.org/10.24085/jsaa.v7i2.3825
McDaniel, S. C., Pietrantoni, Z., & Chen, S-y. (2022). Supporting students with disabilities in transition: Collaboration between school counselors and special educators. In Inclusive pedagogical practices amidst a global pandemic (pp. 177–193). https://doi.org/10.1007/978-3-031-10642-2_11
Mgumba, B. F. (2021). The status of counselling services for students with visual impairments in Tanzanian universities. Journal of Education, Humanities & Sciences, 10 (5), 23–39. https://ojs3.bongotech.info/index.php/jehs/article/view/107 .
Mgumba, B. F., & Kija, L. L. (2023). Promoting support services of special education units for enhancing educational achievements of students with disabilities in Tanzanian universities. Papers in Education and Development — Special Issue on Inclusive & Special Education –. African Journals Online (AJOL), 111–126. file:///C:/Users/HP/Downloads/ajol-file-journals_668_articles_251543_64bd4bfe7837b%20(3).pdf. Accessed 10 Feb 2023
Ministry of Health. (2023). Health care . Kingdom of Saudi Arabia. https://www.my.gov.sa/wps/portal/snp/aboutksa/HealthCareInKSA/?lang=en%3F%3F%3F . Accessed 16 May 2023
Modi, H., Orgera, K., & Grover, A. (2022). Exploring barriers to mental health care in the U.S. [Issue Brief]. The AAMC Research and Action Institute. https://www.aamc.org/advocacy-policy/aamc-research-and-action-institute/barriers-mental-health-care . Accessed 27 Jun 2023
Mostafa, A. S. (2019). Interdisciplinary collaboration in exemplary counseling-enriched high school programs: Integrating college & career readiness and mental health wellness for students with emotional disturbance [Doctoral dissertation, Brandman University]. UMass Global ScholarWorks. https://digitalcommons.umassglobal.edu/cgi/viewcontent.cgi?article=1300&context=edd_dissertations . Accessed 24 May 2023
Murata, N. M., & Tan, C. A. (2009). Collaborative teaching of motor skills for preschoolers with developmental delays. Early Childhood Education Journal, 36 (6), 483–489. https://doi.org/10.1007/s10643-007-0212-5
National Center for Learning Disabilities. (2021). Collaboration: Partnering with colleagues, families, and caregivers to promote student success . https://www.ncld.org/reports-studies/forward-together-2021/collaboration/ . Accessed 12 May 2023
Parcesepe, A. M., & Cabassa, L. J. (2013). Public Stigma of Mental Illness in the United States: A Systematic Literature Review. https://doi.org/10.1007/s10488-012-0430-z
Pufpaff, L. A., Mcintosh, C. E., Thomas, C., Elam, M., & Irwin, M. K. (2015). Meeting the health care needs of students with severe disabilities in the school setting: Collaboration between school nurses and special education teachers. Psychology in the Schools Journal, 52 (7), 684–701. https://doi.org/10.1002/pits.21849
Radić-Šestić, M., Radovanović, V., Milanović-Dobrota, B., Slavkovic, S., & Langović-Milićvić, A. (2013). General and special education teachers’ relations within teamwork in inclusive education: Socio-demographic characteristics. South African Journal of Education, 33 (3), 1–15. https://doi.org/10.15700/201503070733
Rothestein, L., & Johnson, J. (2014). Special education law . Sage Publications: U.S.A.
Salaheddin, K., & Mason, B. (2016). Identifying barriers to mental health help-seeking among young adults in the UK: A cross-sectional study. British Journal of General Practice, 66 (651). https://doi.org/10.3399/bjgp16X687313
Sileo, N. M., & Prater, M. A. T. (2011). Working with families of children with special needs: Family and professional partnerships and roles (1st ed.). Pearson.
Talbott, E., De Los Reyes, A., Power, T., Michel, J., & Racz, S. (2021). A team-based collaborative care model for youth with attention-deficit hyperactivity disorder in education and health care settings. Journal of Emotional and Behavioral Disorders, 29 (1), 24–33. https://doi.org/10.1177/1063426620949987
United Nations Convention on the Rights of Persons with Disabilities. (2006). https://www.ohchr.org/en/hrbodies/crpd/pages/conventionrightspersonswithdisabilities.aspx . Accessed 6 Feb 2023
Venianaki, A., & Zervakis, S. (2015). Collaboration practices between special education teachers and mainstream teachers in secondary education. Journal of Education, Social Policy, 2 (6), 4246. https://www.researchgate.net/publication/322369754_Collaboration_Practices_between_Special_Education_Teachers_and_Mainstream_Teachers_in_Secondary_Education_Journal_of_Education_Social_Policy_2_6_42-46 . Accessed 11 Mar 2023
Download references
The authors did not obtain funding from any entity or institution.

Author information
Authors and affiliations.
Special Education Department, College of Education, King Faisal University, Al-Ahsa, 31982, Saudi Arabia
Nourah Ibrahim Abdullah Albash
You can also search for this author in PubMed Google Scholar
Contributions
The author collected the data, analyzed the data, and wrote the paper.
Corresponding author
Correspondence to Nourah Ibrahim Abdullah Albash .
Ethics declarations
Competing interest.
The author has no conflict of interests to declare that are relevant to the content of this article.
Ethical considerations
The author obtained an approval to conduct the study from the Board of Ethics Committee at King Faisal University.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Albash, N.I.A. A survey of special education teachers and specialists in Saudi Arabia on the use of collaborative practices to support the mental health of students with disabilities. Educ Inf Technol (2024). https://doi.org/10.1007/s10639-024-12667-2
Download citation
Received : 16 August 2023
Accepted : 22 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1007/s10639-024-12667-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Collaboration
- Psychological problems
- Students with disabilities
- Saudi Arabia
- Special education
- Mental healthcare
- Find a journal
- Publish with us
- Track your research
This paper is in the following e-collection/theme issue:
Published on 9.4.2024 in Vol 26 (2024)
Moderating Effect of Coping Strategies on the Association Between the Infodemic-Driven Overuse of Health Care Services and Cyberchondria and Anxiety: Partial Least Squares Structural Equation Modeling Study
Authors of this article:

Original Paper
- Richard Huan Xu 1 , PhD ;
- Caiyun Chen 2 , PhD
1 Department of Rehabilitation Sciences, Faculty of Health and Social Sciences, Hong Kong Polytechnic University, Hung Hom, China (Hong Kong)
2 Nanjing Academy of Administration, Nanjing, China
Corresponding Author:
Richard Huan Xu, PhD
Department of Rehabilitation Sciences
Faculty of Health and Social Sciences
Hong Kong Polytechnic University
11 Yuk Choi Rd
China (Hong Kong)
Phone: 852 27664199
Email: [email protected]
Background: The COVID-19 pandemic has led to a substantial increase in health information, which has, in turn, caused a significant rise in cyberchondria and anxiety among individuals who search for web-based medical information. To cope with this information overload and safeguard their mental well-being, individuals may adopt various strategies. However, the effectiveness of these strategies in mitigating the negative effects of information overload and promoting overall well-being remains uncertain.
Objective: This study aimed to investigate the moderating effect of coping strategies on the relationship between the infodemic-driven misuse of health care and depression and cyberchondria. The findings could add a new dimension to our understanding of the psychological impacts of the infodemic, especially in the context of a global health crisis, and the moderating effect of different coping strategies on the relationship between the overuse of health care and cyberchondria and anxiety.
Methods: The data used in this study were obtained from a cross-sectional web-based survey. A professional survey company was contracted to collect the data using its web-based panel. The survey was completed by Chinese individuals aged 18 years or older without cognitive problems. Model parameters of the relationships between infodemic-driven overuse of health care, cyberchondria, and anxiety were analyzed using bootstrapped partial least squares structural equation modeling. Additionally, the moderating effects of coping strategies on the aforementioned relationships were also examined.
Results: A total of 986 respondents completed the web-based survey. The mean scores of the Generalized Anxiety Disorder-7 and Cyberchondria Severity Scale-12 were 8.4 (SD 3.8) and 39.7 (SD 7.5), respectively. The mean score of problem-focused coping was higher than those of emotion- and avoidant-focused coping. There was a significantly positive relationship between a high level of infodemic and increased overuse of health care (bootstrapped mean 0.21, SD 0.03; 95% CI 0.1581-0.271). The overuse of health care resulted in more severe cyberchondria (bootstrapped mean 0.107, SD 0.032) and higher anxiety levels (bootstrapped mean 0.282, SD 0.032) in all the models. Emotion (bootstrapped mean 0.02, SD 0.008 and 0.037, SD 0.015)- and avoidant (bootstrapped mean 0.026, SD 0.009 and 0.049, SD 0.016)-focused coping strategies significantly moderated the relationship between the overuse of health care and cyberchondria and that between the overuse of health care and anxiety, respectively. Regarding the problem-based model, the moderating effect was significant for the relationship between the overuse of health care and anxiety (bootstrapped mean 0.007, SD 0.011; 95% CI 0.005-0.027).
Conclusions: This study provides empirical evidence about the impact of coping strategies on the relationship between infodemic-related overuse of health care services and cyberchondria and anxiety. Future research can build on the findings of this study to further explore these relationships and develop and test interventions aimed at mitigating the negative impact of the infodemic on mental health.
Introduction
Covid-19–related mental health problems.
In today’s technologically advancing society, widespread and rapid digitization has led to a substantial increase in the use of social media and the internet. This, in turn, has facilitated the rapid dissemination of all types of information. Although this can be beneficial in filling information gaps quickly, it has its drawbacks. A prominent drawback is the amplification of harmful messages, which can have negative effects on individuals [ 1 , 2 ]. The World Health Organization (WHO) acknowledged the presence of an infodemic during the COVID-19 pandemic and subsequent responses. WHO defines an infodemic as an excessive amount of information, including both accurate and inaccurate content [ 3 ]. This abundance of information makes it difficult for individuals to distinguish reliable sources from unreliable sources and to find trustworthy guidance when they need it.
Excessive use of health care services can have adverse effects on individuals and the overall sustainability of health care systems. Although challenges associated with the overuse of health care services were evident before the COVID-19 pandemic [ 4 , 5 ], the urgent need for sustainable health care systems was exacerbated by the pandemic. Because large portions of the population were instructed to self-isolate at home and had limited access to health care professionals during the pandemic, the internet became the primary source of information for numerous individuals seeking answers to health-related questions. However, the abundance of web-based information, including both true and false content, can leave individuals feeling overwhelmed and struggling to make informed choices. This information overload can lead to depression because individuals bombarded with conflicting messages may feel unsure of what to believe [ 6 - 10 ].
Besides depression, cyberchondria has also emerged as a significant public health challenge since the onset of the COVID-19 pandemic. This refers to the repeated and excessive search for health-related information on the internet, leading to a significant increase in distress or anxiety [ 11 ]. Although the global emergency caused by the COVID-19 pandemic is over, telehealth remains a growing trend. An increasing number of studies have indicated that telehealth can improve health care access, outcomes, and affordability by offering a bridge to care and an opportunity to reinvent web-based care models [ 12 ]. However, increasing internet exposure increases the risk of cyberchondria, especially under conditions of uncertainty and increased risk, due to the large volume of information it contains. Thus, it is crucial to understand how to provide support and guidance to help people adopt appropriate strategies for using web-based resources safely in the context of an infodemic.
Current Research on the COVID-19–Related Infodemic
The harms of infodemic are well documented. An Italian study suggested developing early warning signals for an infodemic, which can provide important cues for implementing effective communication strategies to mitigate misinformation [ 13 ]. Other studies have shown that successful use of coping strategies can help individuals manage stressful events and reduce negative emotions during a pandemic. For example, Yang [ 14 ] found a positive correlation between emotion-focused coping and cyberbullying and depression during the COVID-19 pandemic. A large-scale UK study indicated that supportive coping was associated with a faster decrease in depression and anxiety symptoms [ 15 ]. Shigeto et al [ 16 ] emphasized the importance of training young adults to develop resilience, flexibility, and specific coping skills to offset the psychological effects of significant lifestyle changes resulting from pandemics or other health crises in the future. A recent study used machine learning technology to enhance the accuracy and efficiency of automated fact-checking and infodemic risk management at a strategic level [ 17 ]. However, the impact of coping strategies on the relationship among the infodemic, cyberchondria, and anxiety at an individual level during the COVID-19 pandemic is still unknown.
Importance of Coping Strategies
The ability of individuals to discern and adopt appropriate coping strategies can have a profound impact on their mental health, particularly in relation to conditions such as depression and anxiety. The ability to select and implement coping strategies is not uniform across all individuals, and these differences can significantly influence the trajectory of their mental health outcomes. For some, the ability to effectively choose and implement coping strategies can serve as a protective factor, mitigating the severity of the symptoms of depression or anxiety and promoting overall health and well-being. Conversely, for others, inability or difficulty in selecting and implementing effective coping strategies can exacerbate mental health conditions, leading to increased severity of depression and anxiety. This, in turn, can have detrimental effects on individuals’ overall health and well-being. Therefore, understanding the factors that influence individuals’ ability to select and implement effective coping strategies is of paramount importance in the field of mental health research and intervention [ 18 ].
Research has demonstrated the importance of appropriate coping mechanisms in managing mental health problems. Coping strategies, which are essential for dealing with stress or challenging situations, can be categorized into 3 primary types: emotion focused, problem focused, and avoidant focused [ 19 ]. Emotion-focused strategies are centered around managing and regulating emotions. They serve as a means to cope with stress or difficult situations. These strategies might involve seeking emotional support from others, using relaxation techniques, or practicing mindfulness. In contrast, problem-focused strategies actively address the problem or stressor. These strategies might encompass problem-solving, devising a plan of action, or seeking information and resources to effectively tackle the situation. Avoidant-focused strategies involve evading or distancing oneself from the stressor or problem. These strategies might include denial, distraction, or engaging in activities to escape or avoid contemplating the issue [ 18 ]. The effectiveness of different coping strategies can vary depending on the situation. Individuals often use different or a combination of strategies, tailoring their approach to their circumstances.
Coping Strategies in the COVID-19–Related Infodemic
From a social perspective, this study underscores the importance of mental health in the context of public health emergencies such as the COVID-19 pandemic. It highlights the need for society to recognize and address the mental health burden that such emergencies can place on individuals, particularly in relation to the phenomenon of cyberchondria, which is the unfounded escalation of concerns about common symptoms based on reviews of web-based literature and resources.
Practically, this study provides valuable insights for policy makers and practitioners. It emphasizes the need for the development of effective coping strategies and programs to manage the negative impact of an overload of misinformation and disinformation on mental health. This is particularly relevant in the digital age, where individuals have access to a plethora of information, not all of which is accurate or reliable. Policy makers and practitioners can use the findings of this study to design interventions that not only provide accurate information but also equip individuals with the skills to distinguish reliable sources from unreliable sources and to cope with the anxiety that misinformation can cause. From a research standpoint, this study fills a gap in the literature by assessing the impact of the infodemic on cyberchondria and the moderating effect of coping strategies in this relationship. It opens up new avenues of research into the complex interplay among public health emergencies, infodemic, cyberchondria, and coping strategies. Future research could build on the findings of this study to further explore these relationships and develop and test interventions aimed at mitigating the negative impact of infodemic on mental health.
Objective of the Study
Currently, the association between the overuse of health care services and mental health problems in the context of an infodemic remains unclear, as is the moderating effect of different coping strategies on this association. Thus, this study investigated the moderating effect of coping strategies on the relationship between the infodemic-driven misuse of health care and depression and cyberchondria.
Hypotheses of the Study
The study used a hypothesis-driven format. Specifically, there are five hypotheses: (1) a positive relationship exists between infodemic and the misuse of health care, (2) a positive relationship exists between the misuse of health care and depressive disorders, (3) a positive relationship exists between the misuse of health care and cyberchondria, (4) coping strategies mitigate the negative effect of the misuse of health care on depression, and (5) coping strategies mitigate the negative effect of the misuse of health care on cyberchondria. Hypotheses 2-5 are separately evaluated for the three types of coping strategies: problem focused (H2.1), emotion focused (H2.2), and avoidant focused (H2.3).
Study Design and Sample Size
The data used in this study were obtained from a cross-sectional and web-based survey conducted between April and May 2023 in China.
There is no gold standard for sample estimation in partial least squares structural equation modeling (PLS-SEM). Following Hair et al [ 20 ], we set the significance level at 5% and the minimum path coefficients to between 0.05 and 0.1. Based on these criteria, a minimum sample size of 619 was determined.
Data Source and Collection
A professional surveying company, WenJuanXing, was invited to collect the data through its web-based panel. The panel of WenJuanXing consists of 2.6 million members, with an average of over 1 million questionnaire respondents daily. At the beginning of the project, a survey manager collaborated with the research team to screen and recruit participants using the company’s internal social network platform. All of the eligible panel members received a survey invitation, and a voluntary response sampling method was used. The survey manager checked the data quality using WenJuanXing’s artificial intelligence data quality control system to ensure that respondents met our inclusion criteria and provided valid responses, thus ensuring a high level of data accuracy and integrity. The inclusion criteria were (1) aged older than 18 years, (2) able to understand and read Chinese, and (3) agreed to provide informed consent. All eligible respondents were invited to participate in a web-based survey. The first section of the survey was the informed consent, which the participants were required to read and agree to before proceeding. All the participants who agreed to participate in the survey were asked to complete six questionnaires covering (1) demographics and socioeconomic status, (2) COVID-19 information–related questions, (3) a cyberchondria questionnaire, (4) an eHealth literacy questionnaire, (5) an anxiety questionnaire, and (6) a coping strategy questionnaire. The English translations of the questionnaires are presented in Multimedia Appendix 1 . To ensure data quality, we collaborated with the survey company and implemented various indicators. We monitored completion time, excluding responses that took less than 6 minutes. We also tracked ID addresses, ensuring that each ID address could only complete the questionnaire once. To minimize random errors, we used an artificial intelligence formula developed by the survey company to identify and filter any response patterns that appeared to be generated in parallel.
Ethical Considerations
The study protocol and informed consent process were approved by the institutional review board of the Hong Kong Polytechnic University (HSEARS20230502006). Informed consent was collected from all participants. The survey was conducted anonymously, and no personally identifiable information was collected. No compensation was provided by the research team.
Instruments
Cyberchondria severity scale-12.
The Cyberchondria Severity Scale-12 (CSS-12), derived from the 33-item CSS, was used to measure the severity of cyberchondria. The CSS-12 exhibited equally good psychometric properties as the original version and has been validated in Chinese populations [ 21 ]. The CSS-12 items are scored on a Likert-type scale ranging from 1=“never” to 5=“always,” giving total scores ranging from 12 to 60. A higher score indicates a higher severity of suspected cyberchondria. The psychometric properties of the Chinese version of the CSS-12 were reported by Peng et al [ 22 ].
Generalized Anxiety Disorder Assessment
The Generalized Anxiety Disorder Assessment-7 (GAD-7) was used to screen for generalized anxiety disorder and related anxiety disorders [ 23 ]. This scale consists of 7 items designed to assess the frequency of anxiety symptoms during the 2 weeks preceding the survey. The GAD-7 score is calculated by assigning scores of 0, 1, 2, and 3 to the response categories of “not at all,” “several days,” “more than half the days,” and “nearly every day,” respectively. The scores of the 7 questions are then summed, giving a total ranging from 0 to 21, with higher scores indicating a higher severity of anxiety disorders. Many studies have reported the psychometric properties of the GAD-7 in Chinese populations, such as that conducted by Sun et al [ 24 ].
Coping Orientation to Problems Experienced Inventory
The Coping Orientation to Problems Experienced Inventory (Brief-COPE) is a 28-item self-report questionnaire used to measure effective and ineffective strategies for coping with a stressful life event [ 25 ]. The Brief-COPE assesses how a person deals with stressors in their daily life. The questionnaire measures 3 coping strategy dimensions: problem focused, emotion focused, and avoidant focused [ 26 ]. Each item is rated on a 4-point scale. The scores for the 3 overarching coping styles are calculated as average scores. This is done by dividing the sum of the item scores by the number of items. These average scores indicate the extent to which the respondent engages in each coping style. A higher score indicates that the respondent does not have many coping skills. The Chinese version of the Brief-COPE and its psychometric properties in Chinese populations were reported by Wang et al [ 27 ].
Infodemic- and Misinformation-Driven Overuse of Health Care Services
The COVID-19–related infodemic and misinformation-driven medical misbehavior were assessed using 2 self-developed items. The first item was “Do you believe there is an excessive amount of information regarding the COVID virus and vaccine on a daily basis?” The second item was “Has misinformation or disinformation about COVID-19 led you to engage in the overuse of health care services (eg, frequently visiting the doctor/psychiatrist or buying unnecessary medicine)?” The respondents were required to indicate their response to these 2 questions by selecting 1 of 2 options presented dichotomously: yes or no.
Statistical Analysis
Descriptive statistics were used to describe the participants’ background characteristics. Continuous variables (eg, age) were calculated as means and SDs. Categorical variables (eg, sex) were calculated as frequencies and proportions. The Pearson correlation coefficient ( r ) was used to examine the association between measures, where r ≥0.3 and r ≥0.5 indicated moderate and large effects, respectively [ 28 , 29 ].
In this study, we used PLS-SEM to estimate the research model parameters, as it works efficiently with small samples and complex models. Compared with covariance-based structural equation modeling, PLS-SEM has several advantages, such as the ability to handle non-normal data and small samples [ 30 ]. Unlike covariance-based structural equation modeling, which focuses on confirming theories, PLS-SEM is a causal-predictive approach that explains variance in the model’s dependent variables [ 31 ]. To improve the model fit, we used the bootstrapping method with 10,000 replications to obtain the estimates of the mean coefficients and 95% CIs [ 32 ]. Composite reliability rho_a (>0.7), composite reliability rho_c (>0.7), and average variance extracted (>0.5) were used to examine the model performance.
PLS-SEM encompasses measurement models that define the relationship between constructs (instruments) and indicator variables and a structural model. The structural model used in this study is presented in Figure 1 . We hypothesized that the infodemic significantly affects misinformation-driven medical misbehavior, resulting in cyberchondria and high anxiety levels. Furthermore, we speculated that coping strategies significantly modify this relationship. To test these hypotheses, we used 3 models that used the full sample to separately investigate the moderating effect of the 3 types of coping strategies (problem focused, emotion focused, and avoidant focused). We analyzed the data and estimated the PLS-SEM parameters using the “SEMinR” package in R (R Foundation for Statistical Computing). A P value of ≤.05 was considered statistically significant.

Background Characteristics of Participants
A total of 986 respondents completed the web-based survey and provided valid responses, resulting in a response rate of 84%. Among the participants, 51.7% (n=510) were female, approximately 95% (n=933) had completed tertiary education or above, and 71.2% (n=702) resided in urban areas. The participants’ background characteristics are listed in Table 1 .
a A currency exchange rate of 7.23 CNY=US $1 applies.
Mean Scores and Frequency of Responses
The mean score of the GAD-7 was 8.4 (SD 3.8), while the mean score of the CSS-12 was 39.7 (SD 7.5). Problem-focused coping had a higher mean score than emotion- and avoidant-focused coping. Respondents with active employment reported statistically significantly higher mean scores on the GAD and avoidant-focused coping subscale compared to those with nonactive employment. A higher proportion of respondents with chronic diseases experienced an infodemic and exhibited the overuse of health care services relative to those without chronic diseases ( Table 2 ). The correlations between all of the measures are presented in Multimedia Appendix 2 .
a GAD-7: Generalized Anxiety Disorder Assessment-7.
b CSS-12: Cyberchondria Severity Scale-12.
c COPE: Coping Orientation to Problems Experienced Inventory.
g P <.001.
Measurement Models
Tables 3 - 5 present the performance of the measurement models for the 3 coping strategies. The values of rho_C and rho_A were above 0.7, indicating acceptable construct reliability. All 3 constructs had Cronbach α values exceeding the cutoff of 0.7, indicating adequate reliability. Table 2 presents the models’ convergent validity. All the bootstrapped item loadings exceeded 0.3 and were significant at <.05 for the problem- and avoidant-focused models. However, for cyberchondria and the Brief-COPE, none of the average variance extracted values were above 0.5, indicating unsatisfactory model convergent validity.
a AVE: average variance extracted.
b GAD-7: Generalized Anxiety Disorder-7.
d HC: health care.
b GAD-7: Generalized Anxiety Disorder.
Structural Models
The structural model analysis involved estimating path coefficients for the conceptual model. We performed PLS-SEM on the research model 3 times to estimate path coefficients for the models with different coping strategies. We found that H1 was supported. A significant and positive relationship was observed between a high level of infodemic exposure and increased overuse of health care services (coefficient=0.212, 95% CI 0.151-0.271). In addition, the overuse of health care services was correlated with more severe cyberchondria and higher anxiety levels in all the 3 models, supporting H2 and H3. The effect of the overuse of health care services on cyberchondria was larger than its effect on anxiety. All these relationships were statistically significant ( Tables 3 - 5 ).
Moderating Effects
In our moderation analyses ( Figure 2 and Tables 6 and 7 ), we found that emotion- and avoidant-focused coping strategies significantly moderated the relationship between the overuse of health care services and cyberchondria and that between the overuse of health care services and anxiety, respectively, supporting H5 and H6. For the problem-based model (H4), the moderating effect was not significant for the relationship between the overuse of health care services and cyberchondria (coefficient=0.002, 95% CI −0.011 to 0.006), indicating that H4.1 was not supported. Compared with the direct effects on the relationship between the overuse of health care services and cyberchondria or anxiety, a strong ability to cope with difficulties can effectively mitigate the negative effects of the infodemic-driven overuse of health care services on cyberchondria and anxiety.

a HC: health care.
b GAD: Generalized Anxiety Disorder Assessment.
b CS: coping strategy.
c GAD: Generalized Anxiety Disorder Assessment.
Principal Findings
We performed a series of PLS-SEM analyses to examine the relationships between the infodemic-driven overuse of health care services and cyberchondria and anxiety and determine the moderating effects of 3 types of coping strategies on these relationships. We observed that the individuals who were exposed to an overload of COVID-19–related information were more likely to seek and use extra and unnecessary health care services during the pandemic. Such behavior may lead to a considerable wastage of health resources that are particularly limited during a public health crisis. Although some studies have indicated that during the COVID-19 pandemic individuals with increasing mental health symptoms rarely used mental health services [ 33 - 35 ], we found that the overuse of health care services may contribute to higher levels of depression and cyberchondria during a pandemic. This finding has never been reported before. However, we did not differentiate between the types of health care services, either physical or mental, that the individuals overused during the pandemic. This limitation may affect the implications of our findings for policy making purposes.
Comparisons With Previous Studies
We observed that enhanced coping strategies can mitigate the adverse effects of overusing health care on depression and cyberchondria. Studies have confirmed the association between pandemics and depression, have identified several sources of depression [ 6 , 7 , 10 , 36 , 37 ], and have determined the relationship between depression and cyberchondria [ 38 ]. However, few studies have investigated the relationship between depression or cyberchondria and the infodemic-driven overuse of health care services. Our findings demonstrate that the adverse effects of the pandemic are diverse and require the investigation of individuals’ health from multiple perspectives (ie, infodemic in health communication, the use of health care in health service research, and depression in psychiatry). These effects might not be immediately apparent, but they are all linked to each other and collectively cause harm. Thus, policy makers should develop a comprehensive and cost-effective strategy to address the potential adverse effects of pandemics on people’s health and well-being and better prepare for the next public health crisis.
This study offers new insights into the role of coping strategies in mediating the relationship between health care overuse and depression or cyberchondria during the COVID-19 pandemic. Overall, individuals with strong coping abilities were more likely to report lower levels of depression or cyberchondria than those with weak coping abilities. However, the moderating effects of different coping strategies varied slightly. We discovered that problem-focused coping strategies resulted in lower levels of depression and cyberchondria than avoidant-focused coping strategies. Additionally, emotion-focused coping strategies led to lower levels of depression than the other 2 types of coping strategies. These findings partially align with previous studies. For instance, Li [ 39 ] demonstrated that using both problem-focused and emotion-focused coping strategies was beneficial for psychological well-being. However, previous studies have reported mixed findings. For example, AlHadi et al [ 40 ] indicated that emotion-focused coping strategies were associated with increased depression, anxiety, and sleep disorders in the Saudi Arabian population. Few studies have examined the effect of avoidant-focused coping strategies. In this study, we found that respondents who reported living with chronic diseases exhibited a higher ability to use avoidant-focused coping. This finding is partially consistent with a previous study that found a positive relationship between avoidance-focused coping strategies and mental health in women with heart disease [ 41 ]. Individuals with medical conditions are more likely to adopt avoidant coping strategies. Firouzbakht et al [ 42 ] explained that avoidance is an effective strategy for handling short-term stress and is more likely to be adopted by certain patient groups.
We found that individuals who favor emotion-focused coping strategies to overcome difficulties are able to effectively mitigate the adverse effects of excessive health care use on depression and cyberchondria relative to those who opt for the other 2 coping strategies. This finding is not entirely surprising or unexpected. It is, in fact, quite reasonable when one considers that scholars and researchers in the field have previously indicated that people have a tendency to adopt emotion-focused strategies, especially when they find themselves in situations that are uncontrollable or unpredictable, such as the ongoing global pandemic [ 43 ]. Some studies have found that age can have a significant impact on an individual’s coping strategy preferences. For instance, younger adults were more likely to use emotion-focused coping strategies during the acute phase of the SARS outbreak, whereas older adults used this particular strategy several months after the outbreak had initially occurred [ 44 ]. This suggests that the coping strategies adopted by individuals can vary greatly depending on their age and the stage of the crisis they are experiencing. However, in the context of this study, we did not observe any significant differences in the coping strategy preferences of the different age groups. This could be due to a variety of factors, but a possible explanation is that our model incorporated the COVID-19 infodemic. In this context, it is understandable that providing emotional support might be more important than providing real solutions. This is particularly true in the current digital age, where the internet offers unlimited information sources for people to explore, which can often lead to information overload and increased anxiety. Therefore, emotion-focused coping strategies could be more beneficial in helping individuals navigate the sea of information and manage their emotional responses effectively.
In this study, we used self-developed items to measure the infodemic and overuse of health care services. While this approach allowed us to collect data that were directly related to the research questions, it may have introduced some potential issues. First, self-developed items may have less validity and reliability than standardized questionnaires. This could affect the accuracy of measurements and the validity of findings. Second, using self-developed items may limit comparability with other studies that use standardized questionnaires. Standardized questionnaires allow for easy comparison across studies and populations. The lack of a common metric may make it challenging to compare the findings of this study to other studies or to aggregate them in future meta-analyses. Finally, self-developed items may be more susceptible to response bias. They may not have considered factors like social desirability bias or acquiescence bias as standardized questionnaires do. This could have skewed the responses and affected the accuracy of the findings. Despite these limitations, the study’s findings provide valuable insights and pave the way for future research in this area.
Main Contributions of This Study
The importance of preparedness, prevention, and emergency response to infodemiology is highly encouraged by the WHO [ 45 ]. This study makes a significant contribution by exploring and empirically evaluating the relationship between the infodemic, the overuse of health care services, cyberchondria, and anxiety in the context of the COVID-19 pandemic. It provides empirical evidence supporting the assertion that a high level of infodemic can lead to the increased overuse of health care services, resulting in more severe cyberchondria and heightened anxiety levels. This finding adds a new dimension to our understanding of the psychological impacts of the infodemic, especially in the context of a global public health crisis. Additionally, this study highlights that adopting appropriate coping strategies can potentially reduce the severity of cyberchondria and anxiety, even among people facing high levels of the infodemic and the overuse of health care services.
Future Research
The study’s findings emphasize the importance of coping strategies in reducing the negative effects of the infodemic and the excessive use of health care. Future research could focus on developing and testing interventions to improve coping skills, such as cognitive-behavioral, mindfulness-based, or psychoeducational approaches. Additionally, other factors like social support, personality traits, or health literacy may moderate the relationship between infodemic, health care overuse, cyberchondria, and anxiety. Future research could further explore these variables. This study’s findings may not apply to all populations, so future research could investigate these relationships in different groups, including those with pre-existing mental health conditions, health care professionals, or diverse cultural contexts. By pursuing these future directions, researchers could build on this study’s findings, thereby enhancing our understanding of the psychological impact of infodemic and developing effective interventions.
Limitations
This study has several limitations that need to be addressed. A primary limitation is that the data were cross-sectional and self-reporting, which can introduce several biases. Social desirability bias may occur when respondents provide answers they believe are socially acceptable rather than truthful. Recall bias may also be present, as the respondents were asked to recall experiences from months or even a year ago. The data are also prone to response bias, as respondents may agree or disagree with statements regardless of their content. These biases may have affected the accuracy of the findings. In the future, we will try to collect data at multiple time points to reduce the biases and identify changes over time. Second, the data used in this analysis were obtained from a web-based survey, which excluded individuals who are not familiar with web-based surveys or do not have access to the internet. This could have resulted in selection bias. Additionally, due to the nature of the web-based survey, the demographic information of our sample was highly skewed. The majority of the respondents were young and highly educated and were frequent internet users who may have experienced more infodemic effects than older and less educated individuals. This may have affected the reliability of our findings. A quota sampling method could be used in future studies to improve the representativeness of the sample. Third, the study was conducted in China; thus, it is important to consider the unique context of China when interpreting the results. It is necessary to conduct further research in different cultural and regional contexts to determine the generalizability of the results. Finally, the evaluation of health care service overuse and strength of the infodemic relied on 2 self-developed items, which may have affected the measurement properties and limited the reliability of our findings. The development of standardized questionnaires to measure the infodemic and the overuse of health care services during a pandemic would be a valuable contribution to future research in this field.
Conclusions
This study is the first to demonstrate a significant correlation between the infodemic-driven overuse of health care services and high levels of depression and cyberchondria in the Chinese population during the COVID-19 pandemic. We find that 3 types of coping strategies can effectively mitigate the adverse effects of infodemic-driven health care overuse on depression and cyberchondria. Among them, emotion-focused coping strategies have stronger moderating effects than the other 2 types of coping strategies. These findings provide empirical evidence that can guide policy makers in developing strategies to reduce cyberchondria, provide accurate information about public health crises, and promote adaptive coping strategies to effectively manage future public health crises.
Data Availability
The data sets generated and analyzed during this study are available from the corresponding author on reasonable request.
Authors' Contributions
RHX contributed to developing the study concept and design, data analysis and interpretation, software, writing the original draft, and review and editing. CC contributed to data collection, software, and review and editing. Both authors approved the submitted version.
Conflicts of Interest
None declared.
English-translated questionnaire.
Correlations between measures.
- Joseph AM, Fernandez V, Kritzman S, Eaddy I, Cook OM, Lambros S, et al. COVID-19 misinformation on social media: a scoping review. Cureus. 2022;14(4):e24601. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Farsi D, Martinez-Menchaca HR, Ahmed M, Farsi N. Social media and health care (Part II): narrative review of social media use by patients. J Med Internet Res. 2022;24(1):e30379. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Health topic - Infodemic. World Health Organization. 2023. URL: https://www.who.int/health-topics/infodemic#tab=tab_1 [accessed 2023-05-14]
- Gogol M, Siebenhofer A. [Choosing wisely—against overuse in healthcare systems—activities in Germany and Austria in geriatric medicine]. Wien Med Wochenschr. 2016;166(5-6):155-160. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morgan DJ, Leppin AL, Smith CD, Korenstein D. A practical framework for understanding and reducing medical overuse: conceptualizing overuse through the patient-clinician interaction. J Hosp Med. 2017;12(5):346-351. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16(3):e0247679. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17(10):3740. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tomasoni D, Bai F, Castoldi R, Barbanotti D, Falcinella C, Mulè G, et al. Anxiety and depression symptoms after virological clearance of COVID-19: a cross-sectional study in Milan, Italy. J Med Virol. 2021;93(2):1175-1179. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tran HTT, Nguyen MH, Pham TTM, Kim GB, Nguyen HT, Nguyen NM, et al. Predictors of eHealth literacy and its associations with preventive behaviors, fear of COVID-19, anxiety, and depression among undergraduate nursing students: a cross-sectional survey. Int J Environ Res Public Health. 2022;19(7):3766. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bareeqa SB, Ahmed SI, Samar SS, Yasin W, Zehra S, Monese GM, et al. Prevalence of depression, anxiety and stress in China during COVID-19 pandemic: a systematic review with meta-analysis. Int J Psychiatry Med. 2021;56(4):210-227. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Starcevic V, Berle D. Cyberchondria: towards a better understanding of excessive health-related internet use. Expert Rev Neurother. 2013;13(2):205-213. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309-313. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gallotti R, Valle F, Castaldo N, Sacco P, De Domenico M. Assessing the risks of 'infodemics' in response to COVID-19 epidemics. Nat Hum Behav. 2020;4(12):1285-1293. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yang F. Coping strategies, cyberbullying behaviors, and depression among Chinese netizens during the COVID-19 pandemic: a web-based nationwide survey. J Affect Disord. 2021;281:138-144. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fluharty M, Bu F, Steptoe A, Fancourt D. Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Soc Sci Med. 2021;279:113958. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shigeto A, Laxman DJ, Landy JF, Scheier LM. Typologies of coping in young adults in the context of the COVID-19 pandemic. J Gen Psychol. 2021;148(3):272-304. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hang CN, Yu PD, Chen S, Tan CW, Chen G. MEGA: Machine Learning-Enhanced Graph Analytics for infodemic risk management. IEEE J Biomed Health Inform. 2023;27(12):6100-6111. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55(3):234-247. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wechsler B. Coping and coping strategies: a behavioural view. Appl Anim Behav Sci. 1995;43(2):123-134. [ FREE Full text ] [ CrossRef ]
- Hair JF, Hair J, Hult GTM, Ringle CM, Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). Thousand Oaks, CA. SAGE; 2022.
- McElroy E, Kearney M, Touhey J, Evans J, Cooke Y, Shevlin M. The CSS-12: development and validation of a short-form version of the cyberchondria severity scale. Cyberpsychol Behav Soc Netw. 2019;22(5):330-335. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peng XQ, Chen Y, Zhang YC, Liu F, He HY, Luo T, et al. The status and influencing factors of cyberchondria during the COVID-19 epidemic. a cross-sectional study in Nanyang City of China. Front Psychol. 2021;12:712703. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sun J, Liang K, Chi X, Chen S. Psychometric properties of the Generalized Anxiety Disorder Scale-7 Item (GAD-7) in a large sample of Chinese Adolescents. Healthcare (Basel). 2021;9(12):1709. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92-100. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Poulus D, Coulter TJ, Trotter MG, Polman R. Stress and coping in Esports and the influence of mental toughness. Front Psychol. 2020;11:628. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wang AWT, Cheng CP, Chang CS, Chen DR, Chen ST, Shieh V, et al. Does the factor structure of the brief COPE fit different types of traumatic events? Eur J Psychol Assess. 2018;34(3):162-173. [ FREE Full text ] [ CrossRef ]
- Brown TA. Confirmatory Factor Analysis for Applied Research, Second Edition. New York, NY. Guilford Publications; 2015.
- Nunnally JC. Psychometric Theory, 3rd Edition. New York, NY. Tata McGraw-Hill Education; 1994.
- Hair JF, Sarstedt M, Pieper TM, Ringle CM. The use of partial least squares structural equation modeling in strategic management research: a review of past practices and recommendations for future applications. Long Range Plann. 2012;45(5-6):320-340. [ FREE Full text ] [ CrossRef ]
- Streukens S, Leroi-Werelds S. Bootstrapping and PLS-SEM: a step-by-step guide to get more out of your bootstrap results. Eur Manag J. 2016;34(6):618-632. [ FREE Full text ] [ CrossRef ]
- Hair JF, Hult GTM, Ringle CM, Sarstedt M, Danks NP, Ray S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook. Cham, Switzerland. Springer International Publishing; 2021.
- Liberman JN, Bhattacharjee S, Rui P, Ruetsch C, Rothman B, Kulkarni A, et al. Impact of the COVID-19 pandemic on healthcare resource utilization in individuals with major depressive disorder. Health Serv Res Manag Epidemiol. 2022;9:23333928221111864. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saunders R, Buckman JEJ, Leibowitz J, Cape J, Pilling S. Trends in depression and anxiety symptom severity among mental health service attendees during the COVID-19 pandemic. J Affect Disord. 2021;289:105-109. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee J, Jeong HJ, Kim S. Stress, anxiety, and depression among undergraduate students during the COVID-19 pandemic and their use of mental health services. Innov High Educ. 2021;46(5):519-538. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(15):5514. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chen J, Liu X, Wang D, Jin Y, He M, Ma Y, et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc Psychiatry Psychiatr Epidemiol. 2021;56(1):47-55. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jungmann SM, Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: which factors are related to coronavirus anxiety? J Anxiety Disord. 2020;73:102239. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Li Q. Psychosocial and coping responses toward 2019 coronavirus diseases (COVID-19): a cross-sectional study within the Chinese general population. QJM. 2020;113(10):731-738. [ FREE Full text ] [ CrossRef ] [ Medline ]
- AlHadi AN, Alarabi MA, AlMansoor KM. Mental health and its association with coping strategies and intolerance of uncertainty during the COVID-19 pandemic among the general population in Saudi Arabia: cross-sectional study. BMC Psychiatry. 2021;21(1):382. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sidhu A, Arora AK. A study of mental health and coping among women with coronary heart disease and women without coronary heart disease. Int J Adv Res Dev. 2017;2(6):1-3. [ FREE Full text ]
- Firouzbakht M, Rahmani N, Nia HS, Omidvar S. Coping strategies and depression during the COVID-19 pandemic in pregnant women: a cross sectional study. BMC Psychiatry. 2022;22(1):153. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chew QH, Wei KC, Vasoo S, Chua HC, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Med J. 2020;61(7):350-356. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yeung DYL, Fung HH. Age differences in coping and emotional responses toward SARS: a longitudinal study of Hong Kong Chinese. Aging Ment Health. 2007;11(5):579-587. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wilhelm E, Ballalai I, Belanger ME, Benjamin P, Bertrand-Ferrandis C, Bezbaruah S, et al. Measuring the burden of infodemics: summary of the methods and results of the Fifth WHO Infodemic Management Conference. JMIR Infodemiology. 2023;3:e44207. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by G Eysenbach, T de Azevedo Cardoso; submitted 05.10.23; peer-reviewed by K Wang, J Chen, CN Hang, E Vashishtha, D Liu; comments to author 06.11.23; revised version received 14.11.23; accepted 22.03.24; published 09.04.24.
©Richard Huan Xu, Caiyun Chen. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 09.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
April 2, 2024
Eclipse Psychology: When the Sun and Moon Align, So Do We
How a total solar eclipse creates connection, unity and caring among the people watching
By Katie Weeman

Students observing a partial solar eclipse on June 21, 2020, in Lhokseumawe, Aceh Province, Indonesia.
NurPhoto/Getty Images
This article is part of a special report on the total solar eclipse that will be visible from parts of the U.S., Mexico and Canada on April 8, 2024.
It was 11:45 A.M. on August 21, 2017. I was in a grassy field in Glendo, Wyo., where I was surrounded by strangers turned friends, more than I could count—and far more people than had ever flocked to this town, population 210 or so. Golden sunlight blanketed thousands of cars parked in haphazard rows all over the rolling hills. The shadows were quickly growing longer, the air was still, and all of our faces pointed to the sky. As the moon progressively covered the sun, the light melted away, the sky blackened, and the temperature dropped. At the moment of totality, when the moon completely covered the sun , some people around me suddenly gasped. Some cheered; some cried; others laughed in disbelief.
Exactly 53 minutes later, in a downtown park in Greenville, S.C., the person who edited this story and the many individuals around him reacted in exactly the same ways.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
When a total solar eclipse descends—as one will across Mexico, the U.S. and Canada on April 8—everyone and everything in the path of totality are engulfed by deep shadow. Unlike the New Year’s Eve countdown that lurches across the globe one blocky time zone after another, the shadow of totality is a dark spot on Earth that measures about 100 miles wide and cruises steadily along a path, covering several thousand miles in four to five hours. The human experiences along that path are not isolated events any more than individual dominoes are isolated pillars in a formation. Once that first domino is tipped, we are all linked into something bigger—and unstoppable. We all experience the momentum and the awe together.
When this phenomenon progresses from Mexico through Texas, the Great Lakes and Canada on April 8, many observers will describe the event as life-changing, well beyond expectations. “You feel a sense of wrongness in those moments before totality , when your surroundings change so rapidly,” says Kate Russo, an author, psychologist and eclipse chaser. “Our initial response is to ask ourselves, ‘Is this an opportunity or a threat?’ When the light changes and the temperature drops, that triggers primal fear. When we have that threat response, our whole body is tuned in to taking in as much information as possible.”
Russo, who has witnessed 13 total eclipses and counting, has interviewed eclipse viewers from around the world. She continues to notice the same emotions felt by all. They begin with that sense of wrongness and primal fear as totality approaches. When totality starts, we feel powerful awe and connection to the world around us. A sense of euphoria develops as we continue watching, and when it’s over, we have a strong desire to seek out the next eclipse.
“The awe we feel during a total eclipse makes us think outside our sense of self. It makes you more attuned to things outside of you,” says Sean Goldy, a postdoctoral fellow at the department of psychiatry and behavioral sciences at Johns Hopkins University.
Goldy and his team analyzed Twitter data from nearly 2.9 million people during the 2017 total solar eclipse. They found that people within the path of totality were more likely to use not only language that expressed awe but also language that conveyed being unified and affiliated with others. That meant using more “we” words (“us” instead of “me”) and more humble words (“maybe” instead of “always”).
“During an eclipse, people have a broader, more collective focus,” Goldy says. “We also found that the more people expressed awe, the more likely they were to use those ‘we’ words, indicating that people who experience this emotion feel more connected with others.”
This connectivity ties into a sociological concept known as “collective effervescence,” Russo and Goldy say. When groups of humans come together over a shared experience, the energy is greater than the sum of its parts. If you’ve ever been to a large concert or sporting event, you’ve felt the electricity generated by a hive of humans. It magnifies our emotions.
I felt exactly that unified feeling in the open field in Glendo, as if thousands of us were breathing as one. But that’s not the only way people can experience a total eclipse.
During the 2008 total eclipse in Mongolia “I was up on a peak,” Russo recounts. “I was with only my husband and a close friend. We had left the rest of our 25-person tour group at the bottom of the hill. From that vantage point, when the shadow came sweeping in, there was not one man-made thing I could see: no power lines, no buildings or structures. Nothing tethered me to time: It could have been thousands of years ago or long into the future. In that moment, it was as if time didn’t exist.”
Giving us the ability to unhitch ourselves from time—to stop dwelling on time is a unique superpower of a total eclipse. In Russo’s work as a clinical psychologist, she notices patterns in our modern-day mentality. “People with anxiety tend to spend a lot of time in the future. And people with depression spend a lot of time in the past,” she says. An eclipse, time and time again, has the ability to snap us back into the present, at least for a few minutes. “And when you’re less anxious and worried, it opens you up to be more attuned to other people, feel more connected, care for others and be more compassionate,” Goldy says.
Russo, who founded Being in the Shadow , an organization that provides information about total solar eclipses and organizes eclipse events around the world, has experienced this firsthand. Venue managers regularly tell her that eclipse crowds are among the most polite and humble: they follow the rules; they pick up their garbage—they care.
Eclipses remind us that we are part of something bigger, that we are connected with something vast. In the hours before and after totality you have to wear protective glasses to look at the sun, to prevent damage to your eyes. But during the brief time when the moon blocks the last of the sun’s rays, you can finally lower your glasses and look directly at the eclipse. It’s like making eye contact with the universe.
“In my practice, usually if someone says, ‘I feel insignificant,’ that’s a negative thing. But the meaning shifts during an eclipse,” Russo says. To feel insignificant in the moon’s shadow instead means that your sense of self shrinks, that your ego shrinks, she says.
The scale of our “big picture” often changes after witnessing the awe of totality, too. “When you zoom out—really zoom out—it blows away our differences,” Goldy says. When you sit in the shadow of a celestial rock blocking the light of a star 400 times its size that burns at 10,000 degrees Fahrenheit on its surface, suddenly that argument with your partner, that bill sitting on your counter or even the differences among people’s beliefs, origins or politics feel insignificant. When we shift our perspective, connection becomes boundless.
You don’t need to wait for the next eclipse to feel this way. As we travel through life, we lose our relationship with everyday awe. Remember what that feels like? It’s the way a dog looks at a treat or the way my toddler points to the “blue sky!” outside his car window in the middle of rush hour traffic. To find awe, we have to surrender our full attention to the beauty around us. During an eclipse, that comes easily. In everyday life, we may need to be more intentional.
“Totality kick-starts our ability to experience wonder,” Russo says. And with that kick start, maybe we can all use our wonderment faculties more—whether that means pausing for a moment during a morning walk, a hug or a random sunset on a Tuesday. In the continental U.S., we won’t experience another total eclipse until 2044. Let’s not wait until then to seek awe and connection.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol
Children and Adolescents Mental Health: A Systematic Review of Interaction-Based Interventions in Schools and Communities
Rocío garcía-carrión.
1 Faculty of Education, Psychology and Social Work, Universitat de Lleida, Lleida, Spain
Beatriz Villarejo-Carballido
2 Faculty of Psychology and Education, University of Deusto, Bilbao, Spain
Lourdes Villardón-Gallego
Background: There is growing evidence and awareness regarding the magnitude of mental health issues across the globe, starting half of those before the age of 14 and have lifelong effects on individuals and society. Despite the multidimensional nature of this global challenge, which necessarily require comprehensive approaches, many interventions persist in seeking solutions that only tackle the individual level. The aim of this paper is to provide a systematic review of evidence for positive effects in children and adolescents' mental health resulting from interventions conducted in schools and communities in which interaction among different agents is an integral component.
Methods: An extensive search in electronic databases (Web of Knowledge, SCOPUS, ERIC, and PsycINFO) was conducted to identify interventions in which interactions between peers, teachers, families or other community members or professionals played a role. Their effects on children and adolescents' mental health were also reviewed. We carried out a systematic review of papers published from 2007 to 2017. Eleven studies out of 384 met the inclusion criteria. Seven of the articles reviewed focus on interventions conducted in schools and promote supportive interactions involving students, teachers, families and mental health professionals. Four of the articles develop interventions that engage community members in dialogic interactions with children and adolescents.
Results: Interventions in schools and communities implement strategies that foster supportive interactions among diverse actors including teachers, parents, community members, and other professionals. The effects of the mental health interventions reported on children and adolescents' problems include a decrease in disruptive behaviors and affective symptoms such as depression and anxiety, together with an increase in social skills, as well as an improvement in personal well-being.
Conclusions: There is evidence of a positive effect on the mental health of children and adolescents, both in decreasing symptoms of mental disorder and in promoting emotional well-being. Whereas, interactions among different actors seem to be a relevant aspect across the interventions, more research is needed to conclude its effect on the outcomes of the studies reviewed.
Introduction
Childhood and adolescence are critical periods to promote mental health as more than half of mental health problems start at these stages, and many of these persist throughout adult life (Kessler et al., 2005 ). Currently, this has become a priority as worldwide data shows an increase in the prevalence of mental health issues in childhood and adolescence (de la Barra M, 2009 ) and the percentage of those afflicted reaching nearly 20% (WHO, 2016 ). The situation is further exacerbated by the fact that many of these children and adolescents are not receiving the specialized care they require (Mills et al., 2006 ; Weist and Murray, 2008 ; Green et al., 2013 ).
Consequently, important efforts to bring together the best evidence about mental health have been done and raised the challenge of agreeing about fundamental issues in the field such as the definition of mental health and other related concepts (Mehta et al., 2015 ). According to WHO, mental health is understood not as a mere absence of illness, but rather, in a broader sense, as a state of well-being in which individuals develop their abilities, face the stress of daily life, perform productive and fruitful work, and contribute to the betterment of their community (WHO, 2004 ). This definition served as the basis for WHO Mental Health Action Plan, 2013–2020, which incorporates the concepts of mental health promotion, mental illness prevention and treatment, and rehabilitation. Particularly, developmental aspects of children and young people, including, for instance, the ability to manage thoughts, emotions, as well as to build social relationships, and the aptitude to learn, are emphasized in the plan as critical facets to be tackled in mental health interventions.
Mental health interventions conducted in schools and in the communities start from the premise that the problems experienced by adolescents are determined by the interaction of individual, environmental and family factors (Manjula, 2015 ). Accordingly, schools and communities offer an optimal context to intervene as children and adolescents grow and develop through social interaction. Schools and communities can make the most of its environment to foster child and youth development and to promote good mental health (Weist and Murray, 2008 ). Many of the mental health programs implemented in schools promote the development of social skills, socio-emotional competences, and learning outcomes while at the same time reducing disruptive behavior (Dowdy et al., 2010 ; Moreira et al., 2010 ; Durlak et al., 2011 ; Suldo et al., 2014 ). The school environment and climate can therefore play a critical role in encouraging the promotion of protective factors for mental health, such as social-emotional competences and skills (Osher et al., 2012 ).
Hence, social and cognitive development is enacted through social interactions in a particular cultural and social context (Vygotsky, 1978 ; Bronfenbrenner, 1979 ). Drawing on the contributions of Vygotsky's theory of cognitive development, human interaction that takes place in the social and cultural context enhances learning and is fundamental for psychological function. These cultural processes in which people learn and developed occur through interactions with others, including symmetrical (peer) as well as expert–novice (e.g., teacher–student) relations (Rogoff, 1990 ; Cole, 1996 ). Importantly, specific instruments have been produced to capture productive forms of dialogue across educational contexts (Hennessy et al., 2016 ).
Most of the research have been devoted to understanding the central role played by the quality of dialogue and interaction between students, in small group classrooms, or in whole class setting teacher-student interaction (see review by Howe and Abedin, 2013 ). Furthermore, research conducted in community-based schools has also reported the benefit of involving families and community members in learning interactions with elementary students, especially for those belonging to vulnerable populations (Flecha and Soler, 2013 ; Valls and Kyriakides, 2013 ). Accordingly, community plays a central role as human develop through their interactions in the sociocultural activities of their communities (Rogoff, 2003 ). Similar improvements have been reported among students with disabilities as a result of engaging in caring and supportive interactions among peers and with other adults when solving academic tasks in interactive groups (García-Carrión et al., 2018 ). The relevance of productive forms of dialogue and supportive interactions among peers, teachers and other community members, have also reported positive effects in 4th grade students prosocial behavior (Villardón-Gallego et al., 2018 ). These studies evidence the potential of educational interventions that draw on the potential of fostering interactions among different agents and promote productive dialogues as a tools for academic and social improvement.
However, when searching for mental health improvement through dialogic interactions, the research is scarce. The pioneering study carried out by Seikkula and Arnkil ( 2006 ) showed the psychological and social benefits of the therapy based on open and anticipation dialogues with adults and adolescents that also involved the family along with the professionals. Rather than focusing in the individual, facilitating supportive interactions among peers, professionals and family members might be an asset underpinning mental health interventions with children and adolescents. This study showed the critical role of collective interactions, which were very different from a dialogue between two individuals (Seikkula and Arnkil, 2006 ). They identified multi-system treatments (MST) characterized by engaging in close interaction professionals with adolescents, family, and other networks. Replication of these US studies in Norway found evidence of effectiveness, particularly, in the adolescents' social skills (Ogden and Halliday-Boykins, 2004 ). However, according to Seikkula and Arnkil ( 2006 , p. 181): “what ultimately caused the observed outcome was not revealed. After all, methods do not help or cure anyone as such. Psychological methods -and other interaction-based means- exist as they user activity.”
Whereas, determining the effect of the interaction itself in the outcomes obtained might be problematic, the authors of these paper aim to examine interaction-based mental health interventions, defined as those in which collective interactions, that involve professionals, family and community members with children and adolescents, are an integral component of the intervention. This systematic review focuses on those interventions conducted in schools and communities and its outcomes on children and adolescents' mental health. According to the WHO definition of mental health provided above, primary studies selected for this review will include positive outcomes in a broader sense, comprising not only the reduction of symptoms of mental disorder but also the promotion of emotional well-being.
The study carries out a systematic review (Gough et al., 2013 ), a methodology developed by the EPPI Centre of the UCL Institute of Education. We have also taken into account the recommendations by PRISMA (Moher et al., 2009 ) and checklist by Joanna Briggs Institute (JBI) (Lockwood et al., 2015 ), in order to offer transparency, validity, replicable, and updateable in this study.
Search Strategy
This systematic review has been focused and defined by the question: Do interaction-based mental health interventions in schools and communities have positive effects among children and adolescents? This question has been defined in terms of PICOS: In children and adolescents (Population) are interaction-based interventions (Intervention) effective in decreasing disruptive behaviors and affective symptoms such as depression and anxiety (in children and adolescents with mental health problems), and in increasing social skills, and improving well-being and academic engagement (in children and adolescents in general)? (Outcomes).
For the review, empirical articles published in international scientific journals in the areas of psychology, education, and mental health and focused on interventions among children and youth between 2007 and 2017 were searched and screened. To that effect, the following databases were analyzed: Web of Knowledge, SCOPUS, ERIC, and PsycINFO.
The articles were searched using the following keywords: “school-based,” “community-based,” “dialogue,” “mental health,” “well-being,” “emotional development,” “interventions,” “program,” “interaction,” and “prevention.” The exploration was completed with searches that employed synonyms or derivatives of the keywords. The keywords were also combined to refine the search. The publications containing the search criteria in the title, in the keywords and in the abstract were include.
Inclusion and Exclusion Criteria
In order to identify and select the studies most relevant to our research, inclusion and exclusion criteria were established.
The inclusion criteria were the following:
- - Special population group: children and adolescents.
- - Target age: 6 to 18 years of age, inclusive.
- - Mental health interventions in which collective interactions, including professionals, families, and community members with children and adolescents, are an integral component.
- - Studies reporting outcomes of the intervention in decreasing symptoms and/or promoting well-being.
The exclusion criteria were the following:
- - Interventions focus on early childhood, youth, or adults.
- - Target age is not specified, or the target population is below 5 or above 18 years.
- - Mental health interventions focusing on one-to-one interactions (i.e., professional-child/professional-adolescent).
- - The intervention is not described or assessed, as in trials, theoretical research or literature reviews.
Selection Process
The first part of the search yielded a total of 384 articles from indexed journals: 183 in published in the WOS database, 12 in Scopus, 33 in ERIC and 156 in PsycINFO. All these articles were entered into the Mendeley software for its screening and review. Basic information such as the title, year, authoring, and abstracts was obtained and introduced in a spreadsheet for a first screening.
From the 384 articles gathered in the initial search, the titles and their authors were subsequently revised in order to eliminate duplicates. This review was carried out by the members of the group independently in order to eliminate duplicate documents, specifically 83 were duplicates and were therefore discarded, resulting in a new total of 301 articles.
Abstracts of the 301 articles were reviewed according to the inclusion and exclusion criteria. As a result, 17 articles initially met the inclusion criteria and were eligible for the review (see Figure 1 ). The articles were downloaded for an in-depth review.

Flow diagram to show the process of study selection.
The three researchers examined the articles independently and extracted the most relevant information that was included in a spreadsheet. The information referred to: (a) study characteristics (author, country, selection criteria, design, data acquisition period), (b) population (target population, age and sample size), (c) settings, and (d) type of study. Once the articles were examined in depth against inclusion and exclusion criteria, discrepancies were discussed to reach a consensus in the final selection of the studies. This first review and discussion of the studies of the 11 articles lead to the elimination of a further six articles that did not adequately fit the inclusion criteria. Thus, a total of 11 articles were finally selected for analysis ( Figure 1 ).
Quality Assessment
The quality of the selected studies was assessed using a checklist following the methodological guidance for systematic reviews developed by the Joanna Briggs Institute (JBI) (Lockwood et al., 2015 ). The selected studies were checked against nine questions. The results of the evaluation are presented in the Table 1 .
Quality of studies.
Q1. Is there congruity between the stated philosophical perspective and the research methodology?
Q2. Is there congruity between the research methodology and the research question or objectives?
Q3. Is there congruity between the research methodology and the methods used to collect data?
Q4. Is there congruity between the research methodology and the representation and analysis of data?
Q5. Is there congruity between the research methodology and the interpretation of results?
Q6. Is the influence of the researcher on their search, and vice-versa, addressed?
Q7. Are participant, and their voices, adequately represented?
Q8. Is the research ethical according to current criteria or, for recent studies, and is there evidence of ethical approval by an appropriate body?
Q9. Do the conclusions drawn in the research report flow from the analysis or interpretation, of the data?
Data Analysis
For the analysis of the studies, the three researchers developed an analytical grid to systematize the most relevant information for the purpose of the review: study characteristics, interactions fostered during the intervention, positive effects and information for assessment of the risk of bias. Each researcher analyzed the studies independently aiming at identifying on the one hand, how the interventions promote interactions between different agents, and on the other hand, the effects of the interventions on the target population. Firstly, data was categorized following an inductive method. Secondly, researchers compared their analysis to reach a consensus to report main findings from the review.
The analysis of 11 mental health interventions targeting children and adolescents reported the benefits for both -students with mental health problems as well as healthy participants- resulting from their participation in the programs analyzed. Nine of the studies show the effects of preventive interventions aim to reduce future problems and to promote mental health among children and adolescents without mental health problems. Only two studies target children who had already contacted the school-based mental health service (Fazel, 2015 ) and adolescents who presented depressive symptoms (Connell and Dishion, 2008 ). Overall, the articles reviewed show a series of studies conducted mainly in the US context, seven out of ten, whereas the rest of the studies were carried out in the United Kingdom and Kenya. Seven of the interventions were conducted in schools and four of them were based in the community.
All the studies have shown to promote positive mental health in increasing well-being and preventing other related problems, as well as in reducing affective symptoms among those participants who were already affected. A detailed analysis of the strategies implemented across the mental health programs revealed an emphasis on fostering interactions among the children and adolescents engaging them in dialogues that involved different agents -teachers, families, community members, mental health professionals. An overview of the articles selected is provided in Table 2 .
Summary of included studies.
Supportive Interactions in Mental Health Interventions
Interactions among students, teachers, family, and community members and other professionals play an important role in the interventions analyzed. The mental health programs developed in schools and communities include specific strategies that have an emphasis on enacting peer support, partnerships and dialogic spaces for the children and adolescents to engage in supportive interactions with other relevant peers or adults.
Collaborative Interactions Among Children, Teachers and Parents in the School Context
Interactions between teachers and students underpin the strategies of the mental health interventions in different specific ways, which include tutoring, interviews, consultation meetings, peer-assisted learning strategies, interactive games, cooperative non-competitive building games, among others. (Bradshaw et al., 2009 ; Houlston et al., 2011 ; Cappella et al., 2012 ; Ohl et al., 2013 ; Atkins et al., 2015 ; Fazel, 2015 ). Overall, five of the studies implement strategies aim at developing children social skills through interaction and collaboration.
Similarly, interventions focus on “group interactions” as a preventive strategy that seek to reduce future mental health problems and to promote well-being (McWhirter and McWhirter, 2010 ). Specifically, two group-oriented prevention programs—Project Family Rejuvenation Education and Empowerment and Group-Oriented Psychological Education Prevention- are characterized by small-group discussions among students and with their mothers; in both settings participants engage in dialogue in a nonthreatening climate while encouraging cultivation of feedback and support between them (McWhirter and McWhirter, 2010 ).
Moreover, three studies promoted collaborative interactions between parents, teachers, and mental health professionals (Bradshaw et al., 2009 ; McWhirter and McWhirter, 2010 ; Atkins et al., 2015 ). Interactive features of these mental health programs include building positive peer groups and partnerships, solving problems peacefully, and fostering parent-student interactions, among others. This aligns with the need for an integration of the school ecology into program planning and the implementation of effective programs, as observed in the Link to Learning (L2L) service model instituted in classrooms and homes to support children with disruptive behavior disorders living in urban low-income communities (Atkins et al., 2015 ). In the same vein, collaboration between parents and teachers in classrooms is at the heart of the Family-School Partnership Program (Bradshaw et al., 2009 ). Discussion-based interactions include parents reading aloud to their children, with a particular emphasis in the promotion of reasoning among the students. Interaction is guided-by open-ended questions after the reading or using other materials, such as videotapes. Parents reacted to and discussed the situations and problem-solved alternative approaches. Discussions were also held on problem situations arising at home.
Fostering Communicative Skills and Home–School Interaction
Communication skills and family communication practice are a central component of READY—a family-based intervention program to prevent HIV infection and mental health problems (Puffer et al., 2016 ). The interaction and the communication skills training involved families, caregivers, children, and the community, as the intervention was carried out in religious congregations. By improving family communication as a protective factor against mental health disorders, READY draws on a promising approach to strengthen protective family processes that may prevent future negative outcomes for adolescents (Puffer et al., 2016 ). In conjunction with these activities, and while the program was being implemented, interaction was also fostered, using a voicemail system to cultivate parents' involvement and to provide consultation on an as-needed basis, and asking parents to fill in and return comment sheets indicating whether they had completed the weekly home activities and whether they had encountered any problems.
For their part, Atkins et al. ( 2010 ) carried out an intervention that targeted home-school communication and home routines that support learning, homework support, and daily readings. They promoted interaction between parents and teachers by means of two techniques: Daily Report Cards and Good News Notes. Daily Reports Cards, on the one hand, consist of cards in which teachers and parents join efforts to identify, monitor, and reinforce behaviors that interfere with learning. Teachers and parents agree on a rating system to track behaviors, a reward schedule, and a plan for monitoring intervals that will enhance both direct feedback to students and home-school communication. Good News Notes, on the other hand, are certificates that teachers send to families detailing desirable behaviors exhibited by children, as a means to provide positive weekly feedback to parents. The Notes identify students' strengths, scaffold behavior improvement by reinforcing small achievements, and balance infraction reports with positive feedback.
Overall, these studies report a multilevel approach, tackling schools, families, communities, and mental health providers and services. The three articles include programs that evidence the crucial role of family and parental engagement in promoting mental health among adolescents (Connell and Dishion, 2008 ; Puffer et al., 2016 ) and children (Atkins et al., 2015 ). According to Connell and Dishion ( 2008 ), providing family-centered services in the school environment facilitated family engagement in the program.
Engaging in Dialogue With Community Members
Engaging in dialogue with the very community members who might be at risk of suffering mental health problems is essential for the success of the intervention. Some strategies for their involvement include the creation of a local Community Advisory Committee (Puffer et al., 2016 ) or a Community Advisory Board (Kia-Keating et al., 2017 ). The latter engage participants in reciprocal dialogues on solutions for issues ranging from violence exposure and health disparities to the difficulties encountered by youth people seeking to thrive, as exemplified by the HEROES Project (Kia-Keating et al., 2017 ).
There have been other community-based organizations studied in California, aimed at promoting “cultures of health” by engaging people in building social networks, by fostering solidarity and collective efficacy, or by promoting a shared commitment to the collective well-being (Puffer et al., 2016 ). Overall, these programs promote dialogic spaces in which the voices of the minorities, who have often been excluded, are instead given prominence and listened to, in order to look for solutions that will address the inequalities affecting their communities.
The effects of the interventions carried out in schools and communities with an emphasis on fostering supportive interactions as discussed above have benefited children and adolescents as reported in the following dimensions:
- Internalizing symptomatology: Three studies include interventions that have had positive effects on the treatment and prevention of affective disorders such as depression and anxiety. Thus, Connell and Dishion ( 2008 ) ascertained, throughout 3 years, their potential to reduce and prevent the increase of depressive symptoms in at-risk early adolescents. Likewise, Ohl et al. ( 2013 ) confirmed the effectiveness of relationships for decreasing emotional symptoms. McWhirter and McWhirter ( 2010 ) garnered the results of the GOPEP intervention program (McWhirter et al., 1997 ), based on group sessions and on conjoint sessions, which entailed substantial collaboration between researchers and participants, and confirmed the effectiveness of the SOAR program (Student Optimistic Attitudes and Resilience Program) in reducing anxiety and depression. The FREE program, for its part, was effective in decreasing self-isolation among children and their mothers, survivors of domestic violence.
- Externalizing symptomatology: Four articles present improvements in aspects related to aggression and behavioral issues. Ohl et al. ( 2013 ) confirmed that the Pyramid project helped improve peer problems; however, they did not find positive effects on behavioral problems. McWhirter and McWhirter ( 2010 ) gathered evidence confirming the effectiveness of the FREE project in decreasing family conflict, and of the SCARE (Student-Created Aggression Replacement Education) program, one of the GOPEP intervention programs, in decreasing and managing aggression, anger, and violent behaviors. However, Cappella et al. ( 2012 ) did not find significative differences in behavioral regulation as an effect of their BRIDGE intervention, although children identified as having behavioral problems benefitted more than their peers in the area of social relations. On the other hand, Bradshaw et al. ( 2009 ) confirmed the long-term positive effects in reducing behavioral and mental-health problems resulting of the CC intervention.
- Personal well-being: Six of the studies reported positive effects on strengthening psychological-related aspects to well-being, including self-concept, self-esteem, self-efficacy, and empowerment, among others. Cappella et al. ( 2012 ) confirmed the existence of a positive effect of intervention on children's academic self-concept. Atkins et al. ( 2015 ) found a significantly greater improvement on social skills among children who had been involved in the intervention, whereas Ohl et al. ( 2013 ) ascertained its positive effect on prosocial behavior. Houlston et al. ( 2011 ) confirmed that peer support improves self-esteem in victims of bullying, as well as their perception of the support provided by friends and other students. Participants stated that peer support had a positive impact on students' relationships, improving and building peer networks with trained peer supporters and other students. More specifically, in bullying situations, students considered peer support to be helpful for a number of reasons, including being able to talk about it, having peers to interact with, or helping bullied students to tell others of their plight.
- Bloemraad and Terriquez ( 2016 ) gathered the opinions of people taking part in activities organized by CBOs (Community-Based Organizations). Results provide evidence of the impact that involvement in CBOs has on participants, namely when preparing to enroll and succeed in college, as well as on their self-reported civic capacity developing skills, which encompass skills as diverse as communicating with others, understanding the impact that government decisions have on the community, speaking in public, or planning events. Besides, the involvement in CBOs improves personal empowerment and self-efficacy, as participants learn to stand up for their beliefs, become more aware of health issues impacting their communities, and learn about their own culture or ethnic group. As for health and education outcomes, participants became more informed about college and career options, took better care of their personal health, and improved their school grades.
- McWhirter and McWhirter ( 2010 ) showed that the FREE project resulted in an increase in children's and women's emotional well-being, peer engagement and self-esteem in children, as well as women's self-efficacy.
- Context: Five of the interventions reported improvements on the classroom climate and teacher-student and peer interactions. The study carried out by Cappella et al. ( 2012 ), based on BRIDGE intervention, demonstrates how classroom interactions generate a positive climate where emotional support and teacher sensitivity are prominent. These interactions also promote a positive classroom climate, characterized by optimal behavior management, productivity, and instructional learning formats. Furthermore, they have been verified to help develop instructional support, more positive teacher expectations regarding children's behavior, and a more responsive teacher-student relationship. The study by McWhirter and McWhirter ( 2010 ), based on group interventions, highlights that interacting with other people helps build positive peer/adult relationships. These conclusions are shared by Puffer et al. ( 2016 ), whose study focused on family communication, and who conclude that intra-family communication improves well-being. In a similar vein, Bloemraad and Terriquez ( 2016 ) find that the interactions fostered by the intervention improve well-being in the community.
The present systematic review of studies has fulfilled the objective of identifying evidence for positive effects of interaction-based interventions in schools and communities in children's and adolescents' mental health. We have shown that mental health interventions, in which supportive interactions are fostered among different actors, have a positive effect in decreasing affective symptoms and in increasing personal wellbeing among children and adolescents.
We detected in these programs an emphasis on engaging children and adolescents in supportive interactions with other relevant adults, such as teachers, family, community members, and other professionals. Overall it showcases the benefits children and adolescents without mental health problems can reap, particularly in preventive interventions as nine of the studies focused on. Only two studies target adolescents and children with mental health problems (Connell and Dishion, 2008 ; Fazel, 2015 ). The literature analyzed sheds light on the importance of preventive interventions where different agents work together toward the common goal of promoting children's and adolescents' mental health (Atkins et al., 2015 ; Kia-Keating et al., 2017 ).
Positive effects on mental health are achieved through interventions that are culturally appropriate and culturally grounded (Bloemraad and Terriquez, 2016 ; Puffer et al., 2016 ; Kia-Keating et al., 2017 ). This is particularly important in those interventions which require the active engagement of families and community members. The role of family and community members emerges as particularly relevant and providing them with communicative skills and fostering home-school communication are assets for the mental health interventions. Schools thus become an ideal space to facilitate family and community involvement, and they consequently present a great potential for enhancing positive parent-teacher, teacher-student and student-student interactions. This is consistent with other research that has focused on the benefits of school-based mental health interventions to help them develop cognitively, socially, and emotionally (Fazel et al., 2014 ).
There is enough supporting evidence on the potential of these interventions for schools to create a positive climate based on instructional and emotional support, solidarity and friendship that improves the well-being of children and communities (McWhirter and McWhirter, 2010 ; Bloemraad and Terriquez, 2016 ; Puffer et al., 2016 ). Available evidence on the effectiveness of these studies attests to the attainment of positive gains in students' academic achievement, which will also lead to other long-term positive effects that will help prevent behavioral and mental-health problems (Bradshaw et al., 2009 ). This positive effect is particularly strong in high poverty contexts (Atkins et al., 2015 ). Particularly relevant is the reduction of anxiety and depression, especially in light of the marked increase of the latter, currently ailing 4,4% of the world population (WHO, 2017 ).
Overall, we argue that interaction-based approaches in mental health interventions, that involve diverse actors in productive forms of dialogue and supportive interactions, are consistent with the benefits reported by the sociocultural approaches to learning and development (Vygotsky, 1978 ). However, in this systematic review we have not been able to determine the effect of the interaction on the effectiveness of the intervention. This is consistent with the literature, as effective mental health interventions, which include collective interactions among different agents as a central element of the intervention, did not revealed how those interactions were linked to the positive outcomes obtained (Seikkula and Arnkil, 2006 ). Similarly, the primary studies reviewed do not established a direct link of the interaction component of the intervention with the positive mental health outcomes. This question still remains.
Limitation and Future Directions
In this systematic review we have reviewed a set of interventions for both adolescents and children, without explicitly distinguishing within the two study groups. This raises a limitation as children and adolescents can potentially show different needs in terms of mental and behavioral support. Consequently, there could be potential differences in the outcomes that have not been considered in this review. In the same vein, this study only reviewed research in English and most research was conducted in the United States, which could also limit the generalizability of the results.
On the other hand, the concept of interaction we explored it is a broad concept that presents some limitations in providing a consistent definition within the interventions. Furthermore, the primary studies reported the effects of the intervention as a whole. Therefore, their methodological designs do not allow to identify the specific effect on mental health of the interaction itself. Still there is a gap to determine the effect of the interactions on the mental health outcomes. Further research is needed to explore the particular role and potential of social interaction to promote children and adolescents' mental health.
Conclusions
This systematic review of 11 studies has focused on mental health interventions in which interaction plays an important role. Supportive interactions carried out in the framework of mental health interventions involve various contexts, agents and systems, including teachers, parents, mental-health professionals, and members of the community.
There is evidence of a positive effect on the mental health of children and adolescents, both in decreasing internalizing and externalizing symptoms, and in promoting personal well-being. Factors that foster mental health as social support or engagement also increase with interventions programs that include interaction as a main feature.
However, more research is needed into the specific impact of interaction on the mental health of children and adolescents, as well as analyzing the type of interactions that have the most beneficial effect.
Author Contributions
RG-C wrote the proposal of this systematic review with the input and contributions of the research team BV-C and LV-G. RG-C and LV-G planned the search in databases and defined exclusion and inclusion criteria for the selection of the articles. BV-C carried out the search, screen the materials and proposed a selection. All the authors checked and refined the selection of the studies. Each author drafted a section of this manuscript. All authors reviewed the whole manuscript, read and approved the submitted version.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. The work leading to this invention has received funding from the Spanish Research Grants EDU2017-88666-R and EDU2015-66395-R (MINECO/FEDER, UE).
- Atkins M. S., Hoagwood K. E., Kutash K., Seidman. E. (2010). Toward the integration of education and mental health in schools . Admin. Pol. Mental Health Mental Health Serv. Res. 37 , 40–47. 10.1007/s10488-010-0299-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Atkins M. S., Shernoff E. S., Frazier S. L, Schoenwald S. K., Cappella E., Marinez-Lora A., et al.. (2015). Redesigning community mental health services for urban children: supporting schooling to promote mental health . J. Consult. Clin. Psychol . 83 , 839–52. 10.1037/a0039661 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bloemraad I., Terriquez V. (2016). Cultures of engagement: the organizational foundations of advancing health in immigrant and low-income communities of color . Soc. Sci. Med. 165 , 214–222. 10.1016/j.socscimed.2016.02.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradshaw C. P., Zmuda J. H., Kellam S. G., Ialongo N. S. (2009). Longitudinal impact of two universal preventive interventions in first grade on educational outcomes in high school . J. Educ. Psychol . 101 , 926–37. 10.1037/a0016586 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bronfenbrenner U. (1979). The Ecology of Human Development : Experiments by Nature and Design . Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Cappella E., Hamre B. K., Kim H. Y., Henry D. B., Frazier S. L., Atkins M. S., et al.. (2012). Teacher consultation and coaching within mental health practice: classroom and child effects in urban elementary schools . J. Consult. Clin. Psychol . 80 , 597–610. 10.1037/a0027725 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cole M. (1996). Cultural Psychology : A Once and Future Discipline. Cambridge, MA: Belknap Press of Harvard University Press. [ Google Scholar ]
- Connell A. M., Dishion T. J. (2008). Reducing Depression among at-risk early adolescents: three-year effects of a family-centered intervention embedded within schools . J. Fam. Psychol. 22 , 574–585. 10.1037/0893-3200.22.3.574 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- de la Barra M F. (2009). Epidemiología de trastornos psiquiátricos en niños y adolescentes: estudios de Prevalencia . Rev. Chil. Neuro Psiquiatr. 47 , 303–314. 10.4067/S0717-92272009000400007 [ CrossRef ] [ Google Scholar ]
- Dowdy E., Ritchey K., Kamphaus R. W. (2010). School-based screening: a population-based approach to inform and monitor children's mental health needs . School Mental Health 2 , 166–176. 10.1007/s12310-010-9036-3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Durlak J. A., Weissberg R. P., Dymnicki A. B., Taylor R. D., Schellinger K.B. (2011). The impact of enhancing students' social and emotional learning: a meta-analysis of school-based universal interventions . Child Dev . 82 , 405–432. 10.1111/j.1467-8624.2010.01564.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fazel M. (2015). A moment of change: facilitating refugee children's mental health in UK schools . Int. J. Educ. Dev . 41 , 255–261. 10.1016/j.ijedudev.2014.12.006 [ CrossRef ] [ Google Scholar ]
- Fazel M., Hoagwood K., Stephan S., Ford T. (2014). Mental health interventions in schools in high-income countries . Lancet Psychiatry 1 , 377–87. 10.1016/S2215-0366(14)70312-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flecha R., Soler M. (2013). Turning Difficulties into possibilities: engaging roma families and students in school through dialogic learning . Camb. J. Educ. 43 , 451–65. 10.1080/0305764X.2013.819068 [ CrossRef ] [ Google Scholar ]
- García-Carrión R., Molina Roldán S., Roca Campos E. (2018). Interactive learning environments for the educational improvement of students with disabilities in special schools . Front. Psychol . 9 :1744. 10.3389/fpsyg.2018.01744 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gough D., Oliver S., Thomas J., Hobbs A. (2013). Learning from research: systematic reviews for informing policy decisions a quick guide , in Principal Public Health Adviser NHS Chief Scientist Office Overseas Development Institute Cabinet Office Director of Social Research & Policy , no. December: 1–36. Available online at: www.alliance4usefulevidence.org .
- Green J. G., McLaughlin K. A., Alegría M., Costello E. J., Gruber M. J., Hoagwood K., et al.. (2013). School mental health resources and adolescent mental health service use . J. Am. Acad. Child Adolesc. Psychiatry 52 , 501–510. 10.1016/j.jaac.2013.03.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hennessy S., Rojas-Drummond S., Higham R., Márquez A. M., Maine F., Ríos R. M., et al. (2016). Developing a coding scheme for analysing classroom dialogue across educational contexts . Learn. Culture Soc. Inter. 9 , 16–44. 10.1016/j.lcsi.2015.12.001 [ CrossRef ] [ Google Scholar ]
- Houlston C., Smith P. K., Jessel J. (2011). The relationship between use of school-based peer support initiatives and the social and emotional well-being of bullied and non-bullied students . Child. Soc. 25 , 293–305. 10.1111/j.1099-0860.2011.00376.x [ CrossRef ] [ Google Scholar ]
- Howe C., Abedin M. (2013). Classroom dialogue: a systematic review across four decades of research . Camb. J. Educ . 43 , 325–356. 10.1080/0305764X.2013.786024 [ CrossRef ] [ Google Scholar ]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., Walters E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication . Arch. General Psychiatry 62 , 593–602. 10.1001/archpsyc.62.6.593 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kia-Keating M., Santacrose D. E., Liu S. R., Adams J. (2017). Using community-based participatory research and human-centered design to address violence-related health disparities among Latino/a youth . Fam. Commun. Health 40 , 160–169. 10.1097/FCH.0000000000000145 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lockwood C., Munn Z., Porritt K. (2015). Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation . Int. J. Evid. Based Healthcare 13 , 179–187. 10.1097/XEB.0000000000000062 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Manjula M. (2015). Community-based mental health interventions in adolescents , in A Practical Approach to Cognitive Behaviour Therapy for Adolescents , eds Mehta M., Sagar R. (New Delhi: Springer India; ), 43–53. 10.1007/978-81-322-2241-5_3 [ CrossRef ] [ Google Scholar ]
- McWhirter J. J., Herrman D. S., Jefferys K., Quinn M. M. (1997). Tools for violence prevention . Catholic School Stud. 70 , 15–19. [ Google Scholar ]
- McWhirter P. T., McWhirter J. J. (2010). Community and school violence and risk reduction: empirically supported prevention . Group Dynamics 14 , 242–256. 10.1037/a0020056 [ CrossRef ] [ Google Scholar ]
- Mehta N., Croudace T., Davies D. S. C. (2015). Public mental health: evidenced-based priorities . Lancet . 385 , 1472–1475. 10.1016/S0140-6736(14)61400-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mills C., Stephan S. H., Moore E., Weist M. D., Daly B. P., Edwards M. (2006). The President's new freedom commission: capitalizing on opportunities to advance school-based mental health services . Clin. Child Fam. Psychol. Rev . 9 , 149–161. 10.1007/s10567-006-0003-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement . PLoS Med . 6 :e1000097 10.1371/journal.pmed.1000097 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moreira P., Crusellas L., Sa I., Gomes P., Matias C. (2010). Evaluation of a manual-based programme for the promotion of social and emotional skills in elementary school children: results from a 4-year study in Portugal . Health Promotion Int. 25 , 309–317. 10.1093/heapro/daq029 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ogden T., Halliday-Boykins C. A. (2004). Multisystemic treatment of antisocial adolescents in Norway: replication of clinical outcomes outside of the US . Child Adolesc. Mental Health 9 , 77–83. 10.1111/j.1475-3588.2004.00085.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ohl M., Fox P., Mitchell K. (2013). Strengthening socio-emotional competencies in a school setting: data from the pyramid project . Br. J. Educ. Psychol . 83 , 452–466. 10.1111/j.2044-8279.2012.02074.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Osher D., Dwyer K. P., Jimerson S. R., Brown J. A. (2012). Developing safe, supportive, and effective schools: facilitating student success to reduce school violence , in Handbook of School Violence and School Safety , eds Furlong M., Jimerson S., Nickerson A. B., Mayer M. J. (Mahwah, NJ: Lawrence Erlbaum Associates; ). Available online at: https://www.routledgehandbooks.com/doi/10.4324/9780203841372.ch3 (accessed March 10, 2018). [ Google Scholar ]
- Puffer E. S., Green E. P., Sikkema K. J., Broverman S. A., Ogwang-Odhiambo R. A., Pian J. (2016). A church-based intervention for families to promote mental health and prevent HIV among adolescents in rural Kenya: results of a randomized trial . J. Consult. Clin. Psychol . 84 , 511–525. 10.1037/ccp0000076 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rogoff B. (1990). Apprenticeship in Thinking : Cognitive Development in Social Context . New York, NY: Oxford University Press. [ Google Scholar ]
- Rogoff B. (2003). The Cultural Nature of Human Development . New York, NY: Oxford university press. [ Google Scholar ]
- Seikkula J., Arnkil T. E. (2006). Dialogical Meetings in Social Networks . London:Karnac. [ Google Scholar ]
- Suldo S. M., Gormley M. J., DuPaul G. J., Anderson-Butcher D. (2014). The impact of school mental health on student and school-level academic outcomes: current status of the research and future directions . School Mental Health 6 , 84–98. 10.1007/s12310-013-9116-2 [ CrossRef ] [ Google Scholar ]
- Valls R., Kyriakides L. (2013). The power of interactive groups: how diversity of adults volunteering in classroom groups can promote inclusion and success for children of vulnerable minority ethnic populations . Camb. J. Educ . 43 , 17–33. 10.1080/0305764X.2012.749213 [ CrossRef ] [ Google Scholar ]
- Villardón-Gallego L., García-Carrión R., Yáñez-Marquina L., Estévez A. (2018). Impact of the interactive learning environments in children's prosocial behavior . Sustainability 10 :2138 10.3390/su10072138 [ CrossRef ] [ Google Scholar ]
- Vygotsky L. S. (1978). Mind in Society: The Development of Higher Mental Process . Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Weist M. D., Murray M. (2008). Advancing school mental health promotion globally . Adv. School Mental Health Promotion 1 , 2–12. 10.1080/1754730X.2008.9715740 [ CrossRef ] [ Google Scholar ]
- WHO (2004). Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report. Geneva, World Health Organization. Retrieved . http://www.who.int/mental_health/evidence/en/promoting_mhh.pdf (accessed March 10, 2018).
- WHO (2016). “WHO| Child and Adolescent Mental Health.” WHO . World Health Organization. Available online at: http://www.who.int/mental_health/maternal-child/child_adolescent/en/
- WHO (2017). “WHO| “Depression: Let's Talk” Says WHO, as Depression Tops List of Causes of Ill Health.” WHO. World Health Organization. Available online at: http://www.who.int/mediacentre/news/releases/2017/world-health-day/en/

IMAGES
VIDEO
COMMENTS
The scale. relates to the four typ es of the mental disorders among students, such a s tired or headaches, mood swings or insomnia. Previous. results showed that more the 38% studen ts are ...
Another common mental health problem among college students is depression, with prevalence rates in college students of 7 to 9 % [1, 9]. ... Ruwaard J, et al. Efficacy and effectiveness of online cognitive behavioral treatment: a decade of interapy research. Stud Health Technol Inform. 2011; 167:9-14. [Google Scholar] 103.
COVID-19 and Student Mental Health. Empirical studies reported a high prevalence of college mental health issues during the early phase of COVID-19 around the world (Cao et al., 2020; Chang et al., 2020; Liu et al., 2020, Rajkumar, 2020; Saddik et al., 2020).In the U.S. a few, but a growing number of empirical surveys and studies were conducted to assess college students' mental health ...
found mental health concerns can cause a student to have difficulty in school. with poor academic performance, even chronic absenteeism, and disciplinary. concerns. Weist (2005) notes that in the prior two decades, "school mental health. programs have increased due to the recognition of the crisis in children's mental.
Poor mental health of students in further and higher education is an increasing concern for public health and policy [1,2,3,4].A 2020 Insight Network survey of students from 10 universities suggests that "1 in 5 students has a current mental health diagnosis" and that "almost half have experienced a serious psychological issue for which they felt they needed professional help"—an ...
Although the concept of school mental health dates back to the early 1900s, as reflected in the publication of the first recorded scientific paper on the topic, entitled "Mental Health of School Children" (Anonymous, 1906), efforts to define mental health in schools continue to be hampered by a lack of precise terminology and
The promotion of mental health among children and adolescents is a public health imperative worldwide, and schools have been proposed as the primary and targeted settings for mental health promotion for students in grades K-12. This review sought to provide a comprehensive understanding of key factors involved in models of school education ...
Background Post-secondary students frequently experience high rates of mental health challenges. However, they present meagre rates of treatment-seeking behaviours. This elevated prevalence of mental health problems, particularly after the COVID-19 pandemic, can lead to distress, poor academic performance, and lower job prospects following the completion of education. To address the needs of ...
As with youth mental health (Wilson, 2020 ), research into student mental health (and well-being) is influenced by the differing priorities of individual research teams, as well as cultural context, and policy. Moving forward, research should also represent the priorities of students and universities, including a pragmatic focus on factors ...
By nearly every metric, student mental health is worsening. During the 2020-2021 school year, more than 60% of college students met the criteria for at least one mental health problem, according to the Healthy Minds Study, which collects data from 373 campuses nationwide (Lipson, S. K., et al., Journal of Affective Disorders, Vol. 306, 2022).In another national survey, almost three quarters ...
Research paper. Trends in college student mental health and help-seeking by race/ethnicity: Findings from the national healthy minds study, 2013-2021 ... For each of the seven prevalence outcomes, annual trends reveal worsening mental health among all students. (1) For flourishing, there was a 32.5% decrease among all students from 2013 to ...
To examine recent trends in bullying and mental health problems among adolescents and the association between them. A questionnaire measuring mental health problems, bullying at school, socio-economic status, and the school environment was distributed to all secondary school students aged 15 (school-year 9) and 18 (school-year 11) in Stockholm during 2014, 2018, and 2020 (n = 32,722).
The strong relationship between mental health and quality of life among students has also been suggested by previous studies, such as that of Taylor, Bramoweth, Grieser, Tatum, and Roane (Citation 2013) which observed depression, anxiety, stress together with quality of life among students with sleeping problems; Mukhtar and Hashim (Citation ...
Mental health and behavioural problems are common among students commencing university. University life can be stressful and problems often exacerbate during their course of study, while others develop disorders for the first time. The WHO World Mental Health Surveys International College Student Project aims to conduct longitudinal research to examine and monitor student mental health and ...
Based on a prevalence of 27.2%, mental health problems among high school children in a study done in Karnataka, considering an absolute precision of 5%, the sample size was estimated to be 305. [ 5] Approval was obtained from the institutional human ethics committee, and informed consent was collected from the student's parents.
Campus acts of violence, student suicide, and the relative increase in mental-health incidents among college students are several reasons that mental health is a pressing issue for higher education. Unfortunately, negative stigma surrounding mental-health issues impacts college students and their choices about seeking help.
Abstract. The purpose of this paper is to investigate the changes in mental health among Chinese primary school students during 2001-2021. We conducted a cross-temporal meta-analysis including 93 studies (43239 Chinese primary school students) to evaluate the relationship between the year of data collection and the total MHRSP scores and the scores of each factor.
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
Purpose: The aim of this study was to examine the relationship between physical activity and mental well-being among college students. Methodology: The study adopted a desktop research methodology. Desk research refers to secondary data or that which can be collected without fieldwork. Desk research is basically involved in collecting data from existing resources hence it is often considered a ...
The aim of this review is to investigate the impacts of various forest therapy activities on the physical and mental health of college students. Additionally, it evaluates the research methodologies and existing issues in current studies, providing an important agenda for future research. Research was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses ...
1. Introduction. Young people's mental health is a major public health issue. Mental health problems among young people contribute to impaired physical and mental health extending into adulthood [1,2,3].Promoting young people's mental health is an integral component in ensuring their development and improving health and social wellbeing across their lifespan [].
The current study aimed to identify the reality of collaborative practices to facilitate access to mental healthcare by students with disabilities in the Kingdom of Saudi Arabia. Descriptive survey approach was used to obtain data from 71 teachers and specialists (n = 42 teachers; n = 29 specialists), who were identified using snowball sampling method, on the use of collaboration to support ...
Background: The COVID-19 pandemic has led to a substantial increase in health information, which has, in turn, caused a significant rise in cyberchondria and anxiety among individuals who search for web-based medical information. To cope with this information overload and safeguard their mental well-being, individuals may adopt various strategies.
Introduction. Mental health issues are the leading impediment to academic success. Mental illness can affect students' motivation, concentration, and social interactions—crucial factors for students to succeed in higher education [].The 2019 Annual Report of the Center for Collegiate Mental Health [] reported that anxiety continues to be the most common problem (62.7% of 82,685 respondents ...
This article is part of a special report on the total solar eclipse that will be visible from parts of the U.S., Mexico and Canada on April 8, 2024. It was 11:45 A.M. on August 21, 2017. I was in ...
Introduction. Childhood and adolescence are critical periods to promote mental health as more than half of mental health problems start at these stages, and many of these persist throughout adult life (Kessler et al., 2005).Currently, this has become a priority as worldwide data shows an increase in the prevalence of mental health issues in childhood and adolescence (de la Barra M, 2009) and ...