

A ‘Havana Syndrome’ Investigation in Congress Rests on Politics, Not Science
Lawmakers should look in the mirror if they want answers to who hyped dubious reports of Havana syndrome. Instead they are investigating the spy agencies telling them the truth about the mystery
Robert Bartholomew
Growth Hormone Injections May Have ‘Seeded’ Alzheimer’s in Some People, Study Suggests
Injections of no-longer-used growth hormone derived from cadavers may have “seeded” Alzheimer’s in some people, small study suggests
Carissa Wong, Nature magazine

Elon Musk’s Neuralink Has Implanted Its First Chip in a Human Brain. What’s Next?
The wealthiest person on Earth has taken the next step toward a commercial brain interface
Ben Guarino

Zapping the Vagus Nerve Could Relieve Some Long COVID Symptoms
Ongoing research shows electrical vagus nerve stimulators could relieve some long COVID symptoms. But are the expensive devices worth the price?

A Rare Visual Disorder Twists Faces Out of Shape
New studies unlock the mysteries of prosopometamorphopsia, a disorder that distorts faces. One woman’s condition improves when she wears orange-tinted glasses
Jaimie Seaton
Could Blood Transfusions and Tissue Transplants Spread Certain Dementias?
Scattered evidence suggests that aberrant proteins act as “seeds” to transmit neurodegenerative disease, but the jury is still out
Esther Landhuis

Transgender People’s Neurological Needs Are Being Overlooked
Migraine, stroke and epilepsy disproportionately affect members of the transgender community—but neurologists are often unprepared to respond
Z Paige L'Erario
How Does Your Brain Remember and Retrieve Words?
Here's a look at how the brain uses its mental dictionary to remember and retrieve language
Nichol Castro, The Conversation

Man with Parkinson’s Walks Smoothly thanks to an Experimental Spinal Implant
Electrical stimulation to the lower spine has improved the mobility of a man with Parkinson’s disease for the past two years, but researchers say larger clinical trials are needed to assess the device
Emily Waltz, Nature magazine

Scientists Tickle Rats and Discover Brain’s ‘Play Spot’
By inhibiting part of rats’ brain stem, scientists may have found the play center of the brain
Timmy Broderick

How Dangerous Are Soccer Concussions? They May Cause Lasting Damage
As the 2023 Women’s World Cup kicks off, repeated concussions and head injuries in the sport raise discussion about the lifelong consequences on the brain
Lauren J. Young

The First Person to Be Diagnosed with Autism Has Died at 89
A 1943 paper highlighted “Donald T.” as “Case 1” of 11 children with “autistic disturbances of affective contact”
Shaena Montanari, Spectrum
Neuroscience News
Top headlines, latest headlines.
- Synaptic Protein Change During Development
- AI to Locate Damage to Brain After Stroke?
- Making Long-Term Memories: Nerve-Cell Damage
- Different Autism Types: Shared Mechanism
- Risk Factors for Faster Brain Aging
- Brain Expansion in Humans
- Want to Feel Young? Protect Your Sleep
- Self-Test App for Early Alzheimer's
- Hidden Brain Changes With Heart Disease
- Developmental Crossroads in the Brain
Earlier Headlines
Tuesday, march 26, 2024.
- New Treatment Target Identified for Alzheimer's Disease
- Common Degenerative Brain Disease May Begin to Develop in Middle Age
- xCT Protein Is Key Link in Inhibiting Pancreatic Cancer Growth and Limiting Mood Disturbances
- Large-Scale Animal Study Links Brain pH Changes to Wide-Ranging Cognitive Issues
- Common Household Chemicals Pose New Threat to Brain Health, Study Finds
Monday, March 25, 2024
- Human Brains Are Getting Larger: That May Be Good News for Dementia Risk
- New Archive of Ancient Human Brains Challenges Misconceptions of Soft Tissue Preservation
- Artificial Nanofluidic Synapses Can Store Computational Memory
Friday, March 22, 2024
- The Aging Brain: Protein Mapping Furnishes New Insights
- Researchers Describe Tools to Better Understand CaMKII, a Protein Involved in Brain and Heart Disease
- Movement Disorder ALS and Cognitive Disorder FTLD Show Strong Molecular Overlaps, New Study Shows
- Researchers Propose a New Way to Identify When Babies Become Conscious
- Early Intervention After the First Seizure May Prevent Long-Term Epilepsy and Associated Cognitive Deficits
Thursday, March 21, 2024
- High-Resolution Brain Created With 3D Printer
- The Power of Neighbors: Neighboring Synapses Shape Learning and Memory
- Immune Cells Identified as Key Players in Brain Health
- Research Offers Hope for Preventing Post-COVID 'brain Fog' By Targeting Brain's Blood Vessels
Wednesday, March 20, 2024
- Metformin During Pregnancy Affects the Brain Development in Offspring Mice, Study Finds
- Cellular Architecture of Lesions in Multiple Sclerosis Now Mapped out
- In Flies, a Single Brain Cell Can Drive Multiple Movements of the Body
- Social Bonding Gets People on the Same Wavelength
- Craving Snacks After a Meal? It Might Be Food-Seeking Neurons, Not an Overactive Appetite
- Keto Diet Prevents Early Memory Decline in Mice
Tuesday, March 19, 2024
- Brain Recordings in People Before Surgery Reveal How All Minds Plan What to Say Prior to Speaking
- Is the Secret to Anxiety in Young Women Hidden in Our Brain Chemistry?
- Brain-Inspired Wireless System to Gather Data from Salt-Sized Sensors
- Biomarkers of the Middle-Aged Brain Predict Cognitive Health in Old Age
- How Neurochemicals Affect fMRI Readings
Monday, March 18, 2024
- Five Factors to Ensure an Infant Thrives
- Deciphering the Role of Bitter and Astringent Polyphenols in Promoting Well-Being
- Researchers Find Unanticipated Complexity in Aging Brain's Memory Decline
- Landmark Study Shows That 'transcendent' Thinking May Grow Teens' Brains Over Time
Friday, March 15, 2024
- Fatty Food Before Surgery May Impair Memory in Old, Young Adults
- Abnormal Brain Structure Identified in Children With Developmental Language Problems
- New Study Reveals Breakthrough in Understanding Brain Stimulation Therapies
- How the Brain Translates Motivation Into Goal-Oriented Behavior, According to New Study
Thursday, March 14, 2024
- How Fear Unfolds Inside Our Brains
- A Healthier Diet Is Linked With a Slower Pace of Aging, Reduced Dementia Risk, Study Shows
- Even Cells Know the Importance of Recycling
Wednesday, March 13, 2024
- Blast-Related Concussions Linked to Higher Alzheimer's Risk
- Interactions With Dogs Can Increase Brainwaves Associated With Stress Relief and Heightened Concentration
- Researchers Identify Brain Connections Associated With ADHD in Youth
- Integrity of Blood-Brain Barrier Depends on Protein That Is Altered in Some Neurodegenerative Diseases
- 'Dual-Target' Cell Therapy Appears to Shrink Brain Tumors, Research Finds
- Middle-Age Obesity Is Caused by Changes in the Shape of Neurons in the Brain
- First Recognition of Self in the Mirror Is Spurred by Touch
Tuesday, March 12, 2024
- The Surprising Effect of Presence Hallucinations on Social Perception
- 'Curved' Walking and a Depth Camera: New Tool Detects Early Cognitive Decline
- Researchers Expand Our Understanding of How the Body and Brain Communicate
Monday, March 11, 2024
- Researchers Uncover Protein Responsible for Cold Sensation
- Researchers Identify Gene Involved in Neuronal Vulnerability in Alzheimer's Disease
- AI May Predict Spread of Lung Cancer to Brain
- Wrist Device That Monitors Activity Could Help Provide Early Warning of Alzheimer's
- 'Study Drugs' Set the Stage for Other Drug Use and Mental Health Decline
- Shared Blueprint in Brain Development Across Different Functional Areas
- For People Who Speak Many Languages, There's Something Special About Their Native Tongue
Friday, March 8, 2024
- Brain Waves Travel in One Direction When Memories Are Made and the Opposite When Recalled
- Zika Virus Vaccine Emerges as an Unlikely Hero in Battling Brain Cancer
- Lack of Focus Doesn't Equal Lack of Intelligence -- It's Proof of an Intricate Brain
Thursday, March 7, 2024
- How the Brain Coordinates Speaking and Breathing
- Doctors Can Now Watch Spinal Cord Activity During Surgery
- Foot-Eye Coordination: How Our Vision Changes in Rhythm With Our Walking
Wednesday, March 6, 2024
- Virtual Reality Exposure Plus Electric Brain Stimulation Offers a Promising Treatment for PTSD
- Earliest-Yet Alzheimer's Biomarker Found in Mouse Model Could Point to New Targets
- A Noninvasive Treatment for 'chemo Brain'
- Hearing Study: Each Nerve Fiber Trains on It's Own
- Study Takes Wider View at Household Size, Children's Development
- Schizophrenia and Aging May Share a Common Biological Basis
- New Microscopy Tech Answers Fundamental Questions
- Amyloid Blood Levels Associated With Brain Changes in Alzheimer's Study
- Does Iron Accumulate in Brain After Concussions?
Monday, March 4, 2024
- Exposure to Different Kinds of Music Influences How the Brain Interprets Rhythm
- Opening a Window on the Brain
- Your Brain in the Zone: A New Neuroimaging Study Reveals How the Brain Achieves a Creative Flow State
- Sleep Apnea Symptoms Linked to Memory and Thinking Problems
Friday, March 1, 2024
- AI Outperforms Humans in Standardized Tests of Creative Potential
- Early Vocabulary Size Is Genetically Linked to ADHD, Literacy, and Cognition
Thursday, February 29, 2024
- Tiny Magnetic Particles in Air Pollution Linked to Development of Alzheimer's
- Study Sheds Light on How Neurotransmitter Receptors Transport Calcium
- Scientists Identify New 'regulatory' Function of Learning and Memory Gene Common to All Mammalian Brain Cells
- A Holistic Framework for Studying Social Emotions
- Mutations in Hereditary Alzheimer's Disease Damage Neurons Without 'usual Suspect' Amyloid Plaques
- Poor Spatial Navigation Could Predict Alzheimer's Disease Years Before the Onset of Symptoms
- Study Detects Cognitive Changes in Older Drivers Using in-Vehicle Sensors
- Molecular Clusters on Glial Cells Show They Are More Than Our Brain's 'glue'
Wednesday, February 28, 2024
- Continued Cocaine Use Disrupts Communication Between Major Brain Networks
- Neurons Help Flush Waste out of Brain During Sleep
- In Fight Against Brain Pathogens, the Eyes Have It
- Could We Assess Autism in Children With a Simple Eye Reflex Test?
- More Than Just Neurons: A New Model for Studying Human Brain Inflammation
- How 40Hz Sensory Gamma Rhythm Stimulation Clears Amyloid in Alzheimer's Mice
- How Ketamine Acts Fast and Slow
Tuesday, February 27, 2024
- CBD Shown to Ease Anxiety Without the Risks That Can Come With THC
- Sniffing Our Way to Better Health
- Addressing Societal Concerns of Genetic Determinism of Human Behavior by Linking Environmental Influences and Genetic Research
- New Study Links Placental Oxygen Levels to Fetal Brain Development
- Long-Term Memory and Lack of Mental Images
- Learning and Memory Problems in Down Syndrome Linked to Alterations in Genome's 'dark Matter'
Monday, February 26, 2024
- Gut-Brain Communication Turned on Its Axis
- Live Music Emotionally Moves Us More Than Streamed Music
- LATEST NEWS
- Top Science
- Top Physical/Tech
- Top Environment
- Top Society/Education
- Health & Medicine
- Mind & Brain
- Disorders and Syndromes
- ADD and ADHD
- Alzheimer's
- Bipolar Disorder
- Borderline Personality Disorder
- Brain Injury
- Hearing Impairment
- Huntington's Disease
- Mad Cow Disease
- Multiple Sclerosis
- Obstructive Sleep Apnea
- Parkinson's
- Schizophrenia
- Sleep Disorders
- Education & Learning
- Brain-Computer Interfaces
- Educational Psychology
- Infant and Preschool Learning
- Intelligence
- K-12 Education
- Language Acquisition
- Learning Disorders
- Illegal Drugs
- Crystal Meth
- Psychedelic Drugs
- Living Well
- Anger Management
- Child Development
- Consumer Behavior
- Dieting and Weight Control
- Gender Difference
- Nutrition Research
- Racial Issues
- Relationships
- Spirituality
- Mental Health
- Eating Disorders
- Smoking Addiction
- Neuroscience
- Child Psychology
- Social Psychology
- Space & Time
- Matter & Energy
- Computers & Math
- Plants & Animals
- Earth & Climate
- Fossils & Ruins
- Science & Society
- Business & Industry
Strange & Offbeat
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- Cell Division Quality Control 'Stopwatch'
- What Controls Sun's Differential Rotation?
- Robot, Can You Say 'Cheese'?
- Researchers Turn Back the Clock On Cancer Cells
- A Solar Cell You Can Bend and Soak in Water
- 'Cosmic Cannibals': Fast-Moving Jets in Space
Trending Topics
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neurol Res Int
- v.2022; 2022

Managing Chronic Neuropathic Pain: Recent Advances and New Challenges
Namrata hange.
1 National University of Singapore, Singapore
Sujan Poudel
2 National Medical College, Tribhuvan University, Birgunj, Nepal
Saleha Ozair
3 Department of Research & Academic Affairs, Larkin Community Hospital, South Miami, FL, USA
Trissa Paul
4 Larkin Community Hospital, Miami, Florida, USA
Meghna Nambakkam
5 Department of Neurology, University of Kansas Medical Center, Kansas City, KS, USA
Rakchhya Shrestha
6 Department of Internal Medicine, Ascension St. Agnes Hospital, Baltimore, MD, USA
Farrah Greye
Sangam shah.
7 Tribhuvan University, Institute of Medicine, Maharajgunj, Kirtipur 44600, Nepal
Yagya Raj Adhikari
Sangharsha thapa.
8 University of Minnesota, Minneapolis, MN, USA
Pooja Patel
9 Department of Internal Medicine, Larkin Community Hospital, South Miami, FL, USA
Associated Data
All the data used to support the findings of the study are included within the article.
Neuropathic pain affects 7–10% of the population, with most of the patients receiving inadequate and incomplete treatment. Owing to the high financial burden and the poor quality of life of the patients and their caretakers, there is a dire need to address the challenges in diagnosing and treating chronic neuropathic pain.
This literature review was conducted to review novel treatments and related challenges through a systematic search from sources such as PubMed, Google Scholar with the combination of MESH words such as neuropathic pain, management of neuropathic pain. Articles from non-English literature, reports without human subjects, animal studies, and abstracts/posters were excluded. However, human studies and studies published in English were included.
This review article discusses novel treatment modalities while acknowledging the challenges medical workers face while encountering neuropathic pain. Despite the recent advances in diagnosis and treatment modalities, several challenges still exist. Hence, there is still a need to explore the various treatment modalities, emphasizing the cause and underlying pathophysiology of neuropathic pain.
We recommend integrated multimodal treatment with the current treatment facility, including various medical disciplines. However, a personalized approach would work the best depending on the 'patient's medical history. Therefore, this article recommends an integrated, cause-specific, cost-effective approach to address this problem of chronic neuropathic pain.
1. Introduction
Globally, neuropathic pain is prevalent in 7%–10% of the general population, among which 20–30% have chronicity [ 1 ]. Chronic neuropathic pain was redefined in 2011 by the International Association for the Study of Pain (IASP) as: “pain arising as a direct consequence of a lesion or disease affecting the somatosensory system including peripheral fibers” (A β , A δ , and C fibers) and central neurons [ 2 ]. Neuropathic pain has been categorized into a broad range of clinical conditions depending upon etiology (degenerative, traumatic, infectious, metabolic, and toxic) and site of neurological lesion (peripheral vs. central lesion) [ 2 ]. Painful peripheral neuropathies, post-herpetic neuralgia, and traumatic nerve injury are all common causes of peripheral neuropathic pain. Positive features, such as aberrant non-painful sensations (e.g., tingling, numbness, pins, and needles) with paresthesia and/or dysesthesia, and negative phenomena, such as neurological sensory deficiencies in the painful area, describe neuropathic pain syndromes clinically [ 2 ]. Existing treatment modalities (pharmacological, nonpharmacological, and interventional therapies) essentially provide only symptomatic relief [ 3 ]. Pharmacological treatments recommended as the first-line treatment include antidepressants (tricyclic agents, serotonin-norepinephrine reuptake inhibitors) and anticonvulsants (gabapentin and pregabalin). Effective nonpharmacological treatment modalities for chronic pain include behavioral therapy for short-term pain relief; cognitive behavioral therapy for reducing long-term pain and disability; hypnosis as an adjunctive therapy; guided imagery, diaphragmatic breathing, and music therapy for peripheral neuropathy.
Chronic neuropathic pain is associated with a substantial economic burden. It unequally affects females, older ages, and people with low education levels leading to increased labor absenteeism. Compared to other chronic pain, neuropathic pain seems to be more challenging to treat, with the quality of treatment being low as only a few patients receive recommended medication in effective doses [ 4 ]. While the total cost of neuropathic pain has not been determined, neuropathic pain boasts substantial costs to society as direct medical costs, reduced ability to work, reduced ability of caregivers to work, and greater need for institutionalization [ 5 ]. While pharmacological treatment of neuropathic pain has been widely explored with guidelines such as NICE and NeuPSIG recommendations, inadequate response to such treatment is still a significant unmet need in neuropathic pain patients [ 6 ]. There is increased advocacy for developing novel pharmacological approaches addressing the current issue of low efficacy and impaired health-related quality of life [ 7 ]. Interventional, psychological, and physical therapy are recommended for drug-refractory cases [ 8 ]. Neuropathic pain is also widely underdiagnosed and underrated [ 9 ]. Current pharmacological treatments are mainly palliative, and although they temporarily relieve the pain, they do not address the underlying mechanisms of the pain. Over the past two decades, numerous studies on various animal models and extensive clinical research on neuropathic pain have led to a new conceptualization for chronic neuropathic pain syndrome management. Individualized multidisciplinary patient care entails careful consideration of pain-related disability (such as depression and occupational dysfunction) and patient education, as well as repeat follow-up and strategic referral to appropriate medical/surgical subspecialties, as well as physical and psychological therapies [ 10 ]. This review summarizes the epidemiology, definition, assessment scales, current treatment options and recent advances, nonpharmacological treatment options, and the challenges of managing these patients. Additionally, the challenges in the diagnosis are also being overviewed.
This literature review was conducted to review novel treatments and related challenges through a systematic search from sources such as PubMed, Google Scholar with the combination of MESH words such as neuropathic pain, management of neuropathic pain: nonpharmacological and pharmacological modalities “neuropathic pain,” “neuralgia,” “chronic pain,” “recent advances,” “management,” “treatment,” “pharmacological modalities,” “nonpharmacological modalities.” Articles from non-English literature, reports without human subjects, animal studies, and abstracts/posters were excluded. However, human studies and studies published in English were included. This article aims to review the most recent advances in diagnosing and managing patients with chronic neuropathic pain and the challenges involved in managing patients with chronic neuropathic pain.
3. Result and Discussion
Successful Management of chronic neuropathic pain involves identifying the underlying cause and requires an integrated management approach using pharmacological and nonpharmacological approaches.
3.1. Diagnosing Chronic Neuropathic Pain (CNP)
Precise diagnostic modalities for chronic neuropathic pain, which consider location and etiology, are crucial for holistic management with improved quality of life, especially in the elderly population [ 11 ]. Taking a detailed history should be at the forefront of the diagnostic workup, typically inclusive of location, onset, duration, radiation, characteristics, frequency of pain, intensity, or severity of pain on a scale of 0–10, mode of injury (if any), relieving and aggravating factors. In addition, any associated symptoms, such as decreased range of motion, weakness, stiffness, muscle spasms, and decreased sensation or muscle strength, should be assessed [ 12 ]. Autoimmune syndromes like systemic lupus erythematosus or rheumatoid arthritis are common misdiagnoses for peripheral neuropathy, causing a domino effect of incorrect drug treatment and further worsening of the condition.
The physical examination of neuropathic pain includes the examination of cranial nerves (I–XII), muscle strength, the functionality of the autonomic nerves, and light and pin prick (sharp) touch sensations [ 13 ].
Laboratory investigations should include testing for vitamin B12 and folate deficiencies, thyroid, liver, and kidney abnormalities, glycosylated hemoglobin, glucose tolerance, lyme disease, hepatitis B and C, celiac disease, anti-MAG antibodies, autoimmune conditions, tox screen, among many others to find a source for neuropathic pain [ 13 ]. EMG studies estimate the extent of nerve damage and determine the root cause of neuropathy. A definitive diagnosis would possibly need spinal taps. Radiographic investigations, including computed tomography (CT) and magnetic resonance imaging (MRI), help to diagnose the criticality of disease depending upon the presentation and signs [ 13 ]. Another advanced autonomic study, the quantitative sensory test (QST), is used to target certain neuropathies. Small nerve endings which detect temperature and large nerve endings which sense vibrations are checked for damage. This is a non-invasive test regulated by a computer system that recognizes how the isolated nerves respond to vibration and variations in temperature. The results of normal patients and the patient's unaffected side are used as variables to be compared to the patient's affected side to assess for any abnormalities [ 13 ]. The most common causes of chronic neuropathic pain can be classified into four categories: trauma, disease, infection, and limb amputation. However, other causes of neuropathic pain include thyroid insufficiency, carpal tunnel syndrome, spinal arthritis, radiculopathies, spondylolisthesis, vitamin B deficiency, and facial nerve palsy [ 14 ]. The method-based approach to diagnose neuropathic pain holds tremendous potential for ensuring a better quality of life for patients with neuropathic pain.
3.2. Pharmacological Management of Chronic Neuropathic Pain: Recent Advances
The challenges in the treatment of chronic neuropathic pain are such that despite the availability of various therapeutic regimens, treatment efficacy remains abysmally low. The comprehensive algorithm for the management of chronic neuropathic pain published in 2019 outlines the proposed therapy progression from the first line through the sixth line wherein five of the six phases are mainly pharmacological. A summary of the comprehensive algorithm is presented in Figure 1 [ 15 ]. Similarly, the consensus statement for the management of chronic neuropathic pain by the Canadian Pain Society has pharmacologic agents constituting the first through the fourth line of management. A summary of the comprehensive algorithm is presented in Figure 2 [ 16 ]. Irving et al. estimated that despite optimization of therapy, only 50% of patients could attain a 30–50% reduction in their pain sensation, while the other half remain refractory to therapeutic management [ 17 ]. These dismal statistics leave much to be improved in the domain of pain management in chronic neuropathy. As a result, new pharmacological agents are continually being developed and tested. The study reports recent advances in pharmacological therapy to treat chronic neuropathic pain, not limited to cancer, chemotherapy, or post-surgical causes. These include recently approved drugs, drugs for which clinical trial results have been published, drugs and pharmacological agents undergoing clinical trials, and pharmacological agents in preclinical testing phases.

The comprehensive algorithm for the management of chronic neuropathic pain published in 2019.

Consensus statement for the management of chronic neuropathic pain by the Canadian Pain Society.
3.3. Approved Drugs
3.3.1. qutenza (target: trpv1 channel).
An 8% Capsaicin patch (640 mcg per cm 2 ; total 179 mg), Qutenza, is a transient receptor potential vanilloid (TRPV1) receptor agonist. Initially approved for the treatment of post-herpetic neuralgia in 2009, a supplemental new drug approval for using Qutenza in the treatment of painful peripheral diabetic neuropathy was released in July 2020 [ 18 ]. The drug's efficacy was supported by the results of two 12-week, double-blind, randomized, dose-controlled multicenter clinical trials. In the first study, 29% ± 2% of the treatment group demonstrated a ≥50% reduction in average pain at the primary assessment during week 8 [ 19 , 20 ]. Only 18% ± 2% of the control group had a ≥50% reduction in average pain at the same assessment point. The second study had comparable results, with 33% ± 2% of the treatment group showing a ≥50% reduction in average pain and a ≥50% reduction in average pain in 26% ± 2% of the control group [ 17 , 20 ]. The recommended dosage is up to 4 patches applied over the most painful skin areas in an office setting with a minimum interval for repeat dosing as warranted by the return of pain is three months. The most common adverse effects are limited to the application site and include erythema, pain, pruritus, and papules [ 18 ].
3.3.2. Mirogabalin (Target: α 2 δ 1 Subunit of Voltage-Gated Ca 2+ Channel)
A gabapentinoid therapy, Mirogabalin besylate modulates pain by binding to the α 2 δ 1 subunit of voltage-gated Ca 2+ channels in the dorsal root ganglion [ 21 ]. Mirogabalin was approved to treat peripheral neuropathic pain in Japan in January 2019. A phase III clinical trial (AMELA) conducted in Japan, Taiwan, and South Korea was completed in December 2020 [ 22 ]. Preliminary analysis of the results found that Mirogabalin was superior to placebo when participants were assessed for change in average daily pain score (ADPS) from baseline to week 14 [ 23 ]. These results mirrored results from earlier studies, including results from the 14-week, randomized, double-blind, placebo-controlled phase 3 study in Asian patients published in January 2019. At the point of assessment, the difference in average daily pain score least-squares mean vs. placebo in this study was −0.41, −0.47, and −0.77 for Mirogabalin 15, 20, and 30 mg/day, respectively [ 24 ]. Subsequently, an extension study assessing the long-term safety and efficacy over 52 weeks was conducted. The results from the extension study showed that adverse effects ranged from mild to moderate and most commonly included nasopharyngitis, somnolence, dizziness, weight increase, and edema [ 25 ].
3.4. Drugs under Clinical Trials
3.4.1. ipidacrine (neiromidine) (target: acetylcholinesterase).
A 4-aminopyridine derivative, Ipidacrine is a reversible inhibitor of acetylcholinesterase [ 26 ]. A phase II randomized control trial published in 2019 concluded that adding Ipidacrine to the traditional therapy for tunnel syndrome resulted in the regression of neuropathic pain syndrome. This regression was quantitatively assessed using VAS, DN4, and pain detect scales, the indexes of which decreased significantly ( p < 0.01).
3.4.2. Bumetanide (Target: Na + -K + -2Cl − Cotransporter)
Bumetanide has been proposed as an adjunctive treatment in the treatment of neuropathic pain resulting from spinal cord injury (SCI). An open-label, single-arm pilot trial of bumetanide (2 mg/day) as an add-on treatment was conducted in 14 SCI patients for 19 weeks. Pain scores were assessed using the numeric rating scale (NRS) and the short-form McGill pain questionnaire. Published in November 2020, the study results demonstrated a significant reduction in the average pain intensity measured by the aforementioned pain scores [ 27 ].
3.4.3. Minocycline (Target: Toll-Like Receptor 4)
A tetracycline that is primarily marketed as an antibiotic, minocycline has been shown to alleviate neuropathic pain through microglial inhibition [ 28 ]. This is thought to be due to its antagonistic effect on the expression of the toll-like receptor 4, a receptor implicated in the neuroinflammation mediated by microglia [ 29 ]. In addition, a placebo-controlled double-blind drug-crossover study demonstrated that [ 30 ].
3.4.4. Dietary Agmatine Sulfate
A metabolite of arginine, dietary agmatine sulfate has been proposed by multiple studies as a dietary adjunct in the treatment of refractory chronic neuropathic pain [ 31 ]. A pilot open-label consecutive case series study was conducted to demonstrate the effectiveness of agmatine sulfate in patients with painful small fiber neuropathy. Participants showed varied responses with average decrease in pain intensity of 26.0 rating points, corresponding to a 46.4% reduction in overall pain ( p < 0.00001) [ 32 ].
3.4.5. IV Immunoglobulin
Intravenous immunoglobulin is an immune-modulating, blood-derived product that may decrease neuropathic pain by decreasing neuroinflammatory processes [ 33 ]. A double-blind, randomized, placebo-controlled, multicenter trial was designed such that 0.4 g/Kg/day, administered intravenously over five consecutive days to the treatment group with primary endpoint assessment of pain intensity and quality of life. Four weeks after IVIG, ≥50% pain reduction was reported in seven of 11 patients (63.6%) in the IVIG group vs. zero of 12 in the placebo group ( P =0.0013). The only adverse effect reported in the treatment group was mild “dermatitis psoriasiform” in one patient [ 34 ].
3.4.6. Topical Cannabidiol Oil
A placebo-controlled, randomized crossover study looking at the effectiveness of topical cannabidiol oil in the symptomatic relief of peripheral neuropathy in the lower extremities found a significant improvement of pain symptoms with the topical application of 250 mg CBD/3fl. oz, as assessed by the neuropathic pain scale. In addition, the treatment group reported a reduction in intense pain, sharp pain, cold, and itchy sensations and no adverse events [ 35 ].
3.4.7. Dextromethorphan Post-Ketamine (Target: NMDA-R Antagonist)
Intravenous ketamine is an NMDA antagonist often used to treat refractory neuropathic pain [ 36 ]. Though effective, administration of IV ketamine requires trained personnel in a controlled setting. Using an adjunctive oral NMDA antagonist following the procedure would theoretically extend the interval period between office visits. A multicenter randomized controlled clinical trial tested this hypothesis with a three-arm study; dextromethorphan 90 mg/day, memantine 20 mg/day, and placebo. Results collected at one month showed that dextromethorphan-maintained pain relief induced by ketamine while memantine and placebo increased pain intensity scores. Adverse events included drowsiness and nausea in the dextromethorphan group and dizziness, drowsiness, and constipation in the memantine group [ 37 ]. Another study compared the anti-nociceptive effects of dextromethorphan to placebo and concluded that because dextromethorphan had no intrinsic anti-nociceptive effect in acute pain on healthy skin, the N-methyl-D-aspartate receptor may need to be sensitized by pain for dextromethorphan to be effective [ 38 ].
3.4.8. Micronized Palmitoylethanolamide (Target: Direct PPAR- α , Multiple Receptors Indirectly)
Palmitoylethanolamide (PEA) is a neurotrophic-antinociceptive nutraceutical that exerts its effects directly through the PPAR- α receptor and indirectly through the TRPV1, CB1, and CB2 receptors [ 38 ]. Analysis of a study on micronized PEA in patients with low back pain/sciatica revealed that it significantly reduces the neuropathic pain component of sciatica. The NNT for 600 mg/die of PEA was 1.7 (95% confidence interval: 1.4–2) for pain, and 1.5 (95% confidence interval: 1.4–1.7) for function. PEA was also extremely well-tolerated, with the calculated NNH non-significant [ 39 ].
3.4.9. Cetuximab (Target: EGFR-1 Antagonist)
It is hypothesized that cetuximab exerts its effects in reducing neuropathic pain by directly inhibiting MAP-kinase in neuronal or glial cells [ 40 ]. Several case series and reports have been published wherein treatment with cetuximab resulted in significant alleviation of neuropathic pain, an open-label randomized proof of concept failed to demonstrate a significant confidence interval for the reduction of pain scores; however, 36% of patients in the treatment group reported ≥50% reduction in average pain three to seven days after cetuximab compared to 14% among the placebo group. This warrants further investigation. The only adverse event reported was grade 1–2 skin rashes among 86% of the participants [ 41 ].
3.4.10. Nano Curcumin (Target: Proinflammatory Cytokine Inhibitor)
Curcumin is an antioxidant that inhibits the production of proinflammatory cytokines like TNF- α and Interleukin-1 (IL-1) and prevents NO synthesis [ 42 ]. A double-blind, randomized, placebo-controlled clinical trial conducted in 2019 concluded that curcumin supplementation for two months improved and reduced the severity of DSPN in patients with T2DM [ 42 ]. Supplementation of nano curcumin was accounted for a significant reduction in Glycated hemoglobin (HbA1c) ( p < 0.001) and fast blood sugar (FBS) ( p =0.004), total score of neuropathies ( p < 0.001), total reflex score ( p =0.04), and temperature ( p =0.01) compared to placebo group [ 42 ].
3.4.11. PF-06372865 (Target: α 2/ α 3/ α 5 Subtype-Selective GABA A Partial Agonist)
A novel α 2/ α 3/ α 5 gamma-aminobutyric acid A (GABA A ) subunit selective partial positive allosteric modulator (PAM) [ 43 ]. In a randomized placebo-controlled crossover study published in 2019, researchers found that a dose of 15 mg PF-06372865 enhanced pain tolerance thresholds (PTTs) for pressure pain by a ratio of 1.11 (90% confidence interval [CI]: 1.02, 1.22) when compared to placebo [ 43 ]. PTT for the cold pressor increased by 1.17 (90% CI: 1.03, 1.32), and pressure pain task increased by 1.11 (90% CI: 1.01, 1.21) after a dose of 65 mg PF-06372865. [ 43 ]
3.4.12. Topical Fisionerv® (Target: Multimechanistic NeuP Modulator)
An emulgel obtained from the combination of Carbopol 990 Polymer (which gels water) and Carbopol Ultrez 20 (which emulsifies ozonated olive oil) [ 44 ]. A double-blind, randomized controlled clinical trial was conducted in 2019 on patients with lumbar sciatica or lumbar disk herniation and/or lumbar canal stenosis, or with carpal tunnel syndrome with two treatment arms: group A: in Fisionerv® in combination with physiotherapy and group B: placebo in combination with physiotherapy. A significant ( p < 0.05) improvement was observed group A (VAS mean 5.3 (1.10)) compared to group B (VAS mean 6.17 (0.80)), already after four weeks of treatment [ 44 ]. A further VAS reduction was recorded at eight treatment weeks, with a significant difference between the treatments (group A: VAS mean = 1.89 (0.77); group B: VAS mean = 3.79 (1.20) ( p < 0.001) [ 44 ]. No adverse drug reaction was observed [ 44 ].
3.4.13. Lacosamide (Target: Na Channel Blocker)
The anticonvulsant lacosamide specifically acts on Nav1.3, Nav1.7, and Nav1.8 which play a significant role in the modulation of neuropathic pain in small fiber neuropathy [ 45 ]. The lacosamide-efficacy-“N”-safety in SFN (LENSS) randomized, placebo-controlled, double-blind, crossover-design study was carried out between November 2014 and July 2016 [ 45 ]. It showed that lacosamide has a significant effect on pain, general wellbeing, and sleep quality [ 45 ]. In 58.3% of patients receiving lacosamide, mean average pain decreased by at least 1 point, compared to 21.7% in the placebo group [sensitivity analyses, odds ratio 5.65 (95% confidence interval: 1.83–17.41); P =0.0045] [ 45 ]. In the lacosamide group, 33.3% reported that their general condition improved versus 4.3% in the placebo group ( P -value = 0.0156) [ 45 ]. Lacosamide was well-tolerated and safe, suggesting that it can be used for pain treatment in Nav1.7-related small-fiber neuropathy [ 45 ].
3.4.14. Intrathecal Baclofen (Target: GABA Analogue)
A GABA analogue that has analgesic effects on all subtypes of neuropathic pain and can improve interference of neuropathic pain with activities of daily living [ 46 ]. In a randomized controlled trial conducted in 2018, neuropathic pain was proven to be improved significantly in the intrathecal baclofen (ITB) group based on assessments such as the numerical rating scale, brief pain inventory, and neuropathic pain system inventory, which revealed an effect on all subtypes of pain [ 46 ].
3.4.15. Sustained Release Sodium Nitrite
Oral formulation of NaNO 2 improves vascular function by restoring NO bioavailability and mediating vasodilation resulting in potential effectiveness as a therapeutic agent in diabetic peripheral neuropathy and endothelial dysfunction [ 47 ]. In a double-blind, randomized placebo-controlled clinical trial conducted in 2018, 24 patients were randomized to 40 mg or 80 mg of sustained-release nitrite or placebo twice daily for 12 weeks [ 47 ]. The NPSI assessment of patients in the 40 mg and 80 mg dose group reported a 12.7% and 22.0% reduction in pain, respectively, compared to an 8.4% reduction by patients in the placebo group [ 47 ]. In addition, SR-nitrite eliminates the headache and dizziness observed in the immediate release of nitrite [ 47 ].
3.4.16. α -Lipoic Acid
Lipoic acid, a potential antioxidant, improves diabetic neuropathy by improving blood flow, reducing oxidative stress, and improving distal nerve conduction [ 48 ]. A prospective interventional study conducted in 2015–2016 concluded that lipoic acid administration was associated with reduced neuropathic symptoms and improved quality of life in painful diabetic neuropathy patients [ 49 ]. Patients noted statistically significant reductions in neuropathic symptoms following a 40-day administration of 600 mg a-lipoic acid, indicated by changes in NSS, SPNSQ, and DN4 scores. [ 49 ]
3.4.17. Lidocaine Infusion
Lidocaine, a widely used local anesthetic and class Ib antiarrhythmic, has effectively treated neuropathic pain [ 50 ]. A prospective, randomized, double-blind, placebo-controlled, parallel study concluded that patients with lidocaine infusion therapy (3 mg/kg of lidocaine administered over 1 hour once a week for four weeks) showed a significant percentage reduction in NRS pain scores after the final infusion compared to the control group [ 50 ]. However, the pain reduction was not maintained at the 4-week follow-up [ 50 ].
3.4.18. l-4 Chlorokynurenine (AV-101)
AV-101 (l-4 chlorokynurenine): it is a novel oral agent which is converted into a potent, selective GlyB site antagonist of the NMDAR, and demonstrated to be active in neuropathic pain [ 51 ]. The randomized, double-blind, placebo-controlled two phase 1 studies conducted in 2017 concluded that although AV-101 did not reach statistical significance in reducing pain, there were consistent reductions for allodynia pain and mechanical and heat hyperalgesia. [ 51 ] The excellent pharmacokinetic and safety profile warrants further clinical trials [ 51 ].
3.4.19. Turpentine Oil
Turpentine oil is a safe topical analgesic and skin protectant observed to relieve neuropathic pain [ 52 ]. A randomized control trial conducted in 2016 concluded that patients treated with commercially available turpentine oil had a VAS of 7.83 ± 1.012 at baseline and 5.20 ± 1.187 after three months of treatment ( P -value 0.0001) [ 52 ].
3.4.20. Dronabinol
Dronabinol is a purified active compound of medical cannabis, which acts primarily upon CB 1 and CB 2 receptors resulting in a wide range of medical indications, including analgesia [ 53 ]. A randomized, double-blind, placebo-controlled parallel-group design for 16 weeks was followed by a 32 weeks open-label period [ 53 ]. In addition, a subgroup of patients participated in the open-label long-term safety follow-up for up to an additional 96 weeks [ 53 ]. This trial demonstrated that dronabinol is a safe long-term treatment option as there were no reported signs of drug abuse with only one possible case of dependency [ 53 ].
3.4.21. Neublastin
Neublastin targets proteins that belong to a group of glial cell-derived neurotrophic factors that act on sensory neurons and assist in the regeneration of sensory nerve cells relieving neuropathic pain [ 54 ]. Study designs consisted of clinical trials reporting minimal pain relief with the lowest injection dose of 50 μ g/kg for lumbosacral radiculopathy [ 54 ]. Approximately 50% of the non-placebo group reported pruritus unrelated to any specific doses [ 54 ].
3.4.22. Botulinum Toxin A
It binds to presynaptic cholinergic nerve terminals and decreases the release of acetylcholine, causing neuromuscular block [ 55 ]. A randomized controlled trial reflects significant relief in neuropathic pain with subcutaneous injections [ 55 ]. Complaints of pain during injection administration for 30% were the only side effect noted [ 55 ].
3.4.23. Cebranopadol
This opioid alternative analgesic that combines nociceptin/orphanin FQ peptide (NOP receptors) receptor reduces afferent neuronal excitability, a critical pathway for pain transmission [ 56 ]. The clinical trial with higher doses of 400–600 μ g had 50% of participants with pain relief (3/10) but had high dropout rates in trials with chronic low back pain [ 56 ]. In addition, higher doses of 400–600 μ g reported adverse effects during titration and discontinuation of the drug [ 56 ]. Dizziness, nausea, vomiting, somnolence, constipation, fatigue, headache, and hyperhidrosis were common side effects [ 56 ].
3.4.24. BG00010 (Neurotrophic Factor) (Target: GFR α 3 Co-Receptor)
A protein in the glial cell line-derived neurotrophic factor (GDNF) family, BG00010 is a selective ligand for the GDNF family receptor alpha-3 (GFR α 3) co-receptor [ 57 ]. This receptor normalizes cellular changes resulting from damage or disease and potentially alleviates neuropathic pain [ 57 ]. A randomized, blinded, placebo-controlled multiple-dose study in subjects with sciatica showed that higher dose regimens of BG00010 resulted in a more significant pain reduction than placebo or lower dose regimens. The most adverse effects were mild and included headache, feeling hot, and pruritus [ 57 ].
3.4.25. Sativex®
Sativex, a combination of delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), may be effective in improving MS-related neuropathic pain [ 58 ]. This is possible through its action on specific cortical pathways. A small-scale clinical trial assessed the clinical (such as VAS) and neurophysiological (using laser-evoked potentials and transcranial magnetic stimulation) parameters before and after four weeks of Sativex administration [ 58 ]. The study showed that one month of drug administration in MS patients with neuropathic pain successfully reduced pain rating and improved quality of life [ 58 ].
3.4.26. Topical Ketamine (Target: N-Methyl-D-Aspartate Antagonist)
The assessment of the efficacy and safety of an alternative route of administration of ketamine, an open-label trial, showed that subjects who applied topical ketamine 10% three times a day for two weeks had a decrease in their numerical pain scale by the end of two weeks, ranging from 14% to 63% [ 36 ]. No adverse effects were reported in the trial [ 59 ].
3.5. Nonpharmacological Management of Chronic Neuropathic Pain: Recent Advances
Nonpharmacological pain management methods for chronic neuropathic pain proved to be valuable in a multimodal approach, combined with pharmacotherapy concurrently or separately [ 60 , 61 ].
3.5.1. Neurostimulation and Neuromodulation Techniques
Although usually invasive, neurostimulation techniques provide effective pain control in patients with chronic neuropathic pain due to paraplegia and above-knee amputation [ 60 , 62 ]. Neuromodulation therapies can positively impact underlying disease mechanisms and move from a palliative treatment paradigm to a disease prevention model. Neuromodulation is a non-addictive, drug-free clinical tool for treating chronic neuropathic pain [ 62 ]. It works by sending controlled physical energy to pre-identified neural targets in the central nervous system, either by actively stimulating nerves to produce a natural biological response or by applying targeted pharmaceutical agents in tiny doses directly to the site of action. Neuromodulation for pain is divided into peripheral and CNS modulation, as well as invasive and non-invasive interface types [ 62 ]. Electrodes are applied to the brain, spinal cord, or peripheral nerves in neurostimulation devices.
3.5.2. Epidural Motor Cortex Stimulation (EMCS)
It is known to be a safe, efficacious, therapeutic option for chronic neuropathic and drug-resistant pain. Neurosurgeons specifically prefer it for such cases [ 63 ]. In addition, surgically-implanted EMCS has emerged as an alternative in the advanced management of facial neuropathic pain and is proven to relieve refractory neuropathic pain effectively [ 63 ].

3.5.3. Spinal Cord Stimulation (SCS)
It was a commonly used invasive technique for pain relief of various neuropathic pain conditions. It works through the stimulation of the dorsal columns of the spinal cord by administering electrical impulses at frequencies of approximately 50 Hz (by an implanted pulse generator-PG) and the electrodes (or lead). It can suppress the central neuronal hyperexcitability with a remarkable reduction of pain intensity scores. Despite being well known for a relatively lower side effect profile such as excessive sedation or cognitive impairment, SCS has been associated with serious adverse events such as infection, dural puncture leading to a subdural hematoma, and subsequently death in one of the patients [ 64 , 65 ]. Nevertheless, SCS is considered a valid, effective, and safe treatment option in patients suffering from neuropathic pain and those resistant to pharmacological treatment. Technical advancements to improve the clinical efficacy and novel waveform paradigms, such as Burst-SCS and KHFSCS (Kilohertz-frequency spinal cord stimulation)—a novel paresthesia-free treatment for chronic pain—have contributed significantly towards innovations in lead design, improvements in IPG capabilities to increase battery lifetime, reduce invasiveness, and provides closed-loop stimulation. These innovations and decades of clinical experience have produced potentially powerful therapies to improve the lives of patients suffering from chronic pain. Nevertheless, the level of efficacy for SCS in chronic pain is still classified as “moderate” and with minimal side effects. In case of failure of SCS in pain management or central origin pain, clinicians switch to deep brain stimulation or motor cortex stimulation [ 66 ].
3.5.4. Deep Brain Stimulation (DBS)
It is used to treat neuropathic pain in post-peripheral nerve injury, post-spinal cord injury, brain stem disease and thalamic pain, pain after amputation, either phantom or stump, cranial and facial pain, including anesthesia dolorosa, and plexopathies. DBS trials with lead externalization have been used extensively over the last 50 years to treat chronic pain. However, spinal cord and/or peripheral nerve stimulation have overshadowed DBS in the pain arena. Laser thermal ablation and radiosurgery provide cost-effective, efficacious therapy and an ablation-based alternative to DBS, possibly used with magnetic resonance imaging guidance to resolve neuropathic pain, especially in advanced stages of cancer [ 67 ].
3.5.5. Peripheral Nerve Stimulation
It has been proven to be helpful in the treatment of several chronic pain conditions, including peripheral nerve dysfunctions, complex regional pain syndrome, and cranial neuralgias. These peripheral nerve stimulators allow external pulse generators to transmit impulses wirelessly to the implanted electrode, and their implantation is lesser invasive. Lately, TIMWAVE, Bioness, and SPR Therapeutics have produced a new generation of devices that allow for external pulse generators to transmit impulses wirelessly to the implanted electrode. In a study conducted by Mobbs et al., significant improvement in symptoms and lifestyle quality was reported post-implantation of peripheral nerve stimulators; [ 68 ] while Deer et al. has demonstrated significant relief for severe intractable chronic pain with the application of an externally powered peripheral nerve stimulator in a prospective, multicentric, randomized, double-blinded, partial crossover study [ 69 ]. In addition, PNS utilizing percutaneously inserted electrodes was shown to be effective in occipital neuralgia, trigeminal neuropathic pain, and cervicogenic headache [ 70 – 74 ].
3.5.6. Transcutaneous Electrical and Electromagnetic Stimulation
Transcutaneous electrical nerve stimulation (TENS) is an expensive, non-invasive, self‐adhesive to relieve pain in CNP, PNP, complex regional pain syndrome, phantom limb pain, and fibromyalgia [ 75 ]. The administered technique delivers pulsed low voltage electrical current.
3.5.7. Electroceuticals
These devices deliver therapeutic electrical stimulation, often at very high frequencies, to different parts of the body. Techniques for chronic pain are being developed, including epidural stimulation and vagal nerve stimulation, which can be quite invasive and expensive. In addition, the analgesic mechanisms of TENS can be evaluated with advanced neuroimaging techniques, such as electroencephalography, magnetoencephalography, and magnetic resonance imaging [ 76 ].
3.5.8. Repetitive Magnetic Stimulation
The use of implanted epidural stimulation to treat persistent, drug-resistant neuropathic pain has been proposed. Various investigations have shown that recurrent transcranial magnetic stimulation (rTMS) administered to the motor cortex can reduce neuropathic pain, at least temporarily [ 77 ]. Additionally, adjuvant static magnetic field therapy can significantly decrease exercise-induced pain in patients with diabetic polyneuropathy (level II evidence).
3.5.9. Transcranial Direct Current Stimulation (tDCS)
It is a recently developed, non-invasive, painless brain stimulation treatment that uses direct electrical currents to stimulate specific brain parts. MRI-guided transcranial focused ultrasound is a nascent, minimally invasive method of targeted tissue thermal ablation that may be used to treat central neuropathic pain with current and potential intracranial applications. Transcranial magnetic-resonance-imaging-guided focused ultrasound is a very precise and a radiation-free neurosurgical technique for treating neuropathic pain [ 78 ]. In addition, adjuvant repetitive transcranial magnetic stimulation of the motor cortex effectively reduces the overall pain intensity in patients with diabetic polyneuropathy (level II evidence).
3.5.10. Remote Electrical Neuromodulation (REN)
Remote electrical neuromodulation has proven to be a novel acute treatment modality for migraine by stimulating the upper arm peripheral nerves to induce conditioned pain modulation (CPM) [ 79 ]. This technique utilizes an endogenous analgesic mechanism in which conditioning stimulation inhibits pain in remote body areas.
3.6. Novel Innovative Techniques
3.6.1. immersive virtual reality (ivr).
Therapy, an emerging technique, has not been made widely available yet as the equipment is expensive and possibly challenging for clinicians, especially those with limited technological experience. However, with the development of “plug and play,” low-cost IVR devices such as the Oculus Rift, Gear VR, and Google Cardboard, IVR no longer requires such specific technical proficiency. Therefore, IVR may be a feasible and affordable option for adjuvant therapy of neuropathic pain. A preliminary study was conducted to review the application of a new virtual reality method and 3D augmented reality mirror visual feedback therapy in persistent, unilateral upper extremity neuropathic pain, and a significant reduction of pain was reported [ 80 ].
3.6.2. Breathing Controlled Electrical Stimulation (BreEStim)
It is a novel, nonpharmacological intervention for neuropathic pain wherein a single-pulse electrical stimulation (EStim) was delivered transcutaneously to a peripheral nerve study.
3.6.3. Scrambler Therapy (Marketed as Calmare™ Therapy in the United States)
It is a novel form of superficial neuromodulation, electro-analgesia therapy for non-invasive pain relief in chronic neuropathic and cancer pain, based on a new generation of medical devices that use a rapidly changing electrical impulse to send a “non-pain” signal along the same pain fibers that are sending the “pain” stimulus. This is predicted to potentially treat chronic neuropathic pain and cancer pain resistant to opioids. Scrambler Therapy was created to trap C-fibers and relieve neuropathic pain, but it has also been shown to help with numbness and tingling caused by various nerve fibers [ 81 , 82 ].
3.6.4. Optogenetics
It is an upcoming alternative strategy to reduce pain using genetically encoded and optically active proteins, opsin, to control signaling events by directly manipulating somatosensory pathways. Evidence from animal models shows that optogenetics is an efficient approach to alleviating inflammatory and neuropathic pain. Considering that gene therapy techniques are already at the clinical stage for several pathological conditions, analgesia by phototherapy could be a promising strategy to treat chronic pain [ 83 ].
3.6.5. Photon Stimulation or Pulsed Infrared Light Therapy
Management of patients with painful diabetic peripheral neuropathy (PDPN) is done by photon stimulation delivered using LEDs. Photo biomodulation or low-level laser therapy (LLLT) utilizes electromagnetic technology, which significantly improves the quality of pain and QOL outcomes in patients with a significant amount of pain and disability due to diabetes [ 84 ]. Furthermore, the application of photo biomodulation in nerve injury and pain control has also been associated with a decrease in inflammatory cytokine levels and facilitation of neuronal regeneration, as demonstrated by the levels of TNF-a, IL-1b, and GAP-43 [ 85 ].
3.6.6. Vibration Stimulation: (WBV) has recently been shown to improve strength, balance, endurance, and blood and lymph fluid circulation in patients with stroke and peripheral neuropathy associated with Parkinson's disease [ 86 ]. WBV improves sensory perceptions like pain and vibration, neuropathy disability score, balance measures, and the general health in painful diabetic peripheral neuropathy [ 87 ]. Vibration causes local myorelaxation, which behaves like a massage and enhances the overall analgesic effects [ 86 ].
3.6.6. Molecular Modalities
Proposed molecular modalities for treating chronic neuropathic pain include ion channel expressions, immune reactions, and inflammatory substrate diffusions. Recent advances in RNA sequence analysis have discovered specific ion channel expressions in nociceptors such as transient receptor potential (TRP) channels, voltage-gated potassium, and sodium channels. G protein-coupled receptors (GPCRs) also play an essential role in triggering the surrounding immune cells. Multiple protein expressions are thought to complicate the therapeutic development of neuropathic pain. Recent progress in optogenetics and pharmacogenetics may herald the development of novel therapeutics for incurable pain. Optogenetics and designer receptors exclusively activated by designer drugs (DREADDS) provide hope in controlling intractable pain in patients suffering from debilitating neuropathic pain. Based on the underlying cause of neuropathic pain, it may be possible to improve pain management by using a combination of therapies and drugs targeting specific molecular targets. With continued development and refinement of this technique combined with viral vector-mediated safe and efficient gene therapy, there is a hope to develop a satisfactory treatment for otherwise intractable neuropathic pain [ 88 ].
3.6.7. Possible Stem Cell Regenerative Therapeutic Dimension with Transplantation
This is a new approach to repair damaged nervous system-induced neuropathic pain syndromes rather than simply providing palliation. Stem cells offer a totipotent cellular source for replacing injured or lost neural cells. Stem cells have the ability to stop degenerative processes, suppress apoptotic pathways, and let wounded and uninjured nerves survive and regenerate. The ability of stem cells to change cellular processes, when combined with their ability to release neurotrophic factors, creates a protective and restorative milieu that has the potential to reverse the source of neuropathic pain. Stem cells can play many functions in the damaged microenvironment, such as peripheral, central, and spinal cord disinhibition, which greatly reduces clinical symptoms including spontaneous pain and hyperalgesia [ 89 – 91 ]. The proposed mechanism replaces the damaged neuronal tissue, protects against progressive nerve damage, and releases paracrine and endocrine factors, which repair the underlying pathology of genesis and propagation of damage within the somatosensory system. Previous studies have shown that fetal GABAergic neuron precursors can also provide substantial pain relief. Lastly, GABAergic neuron transplants have been found to survive long-term in an injured spinal cord, which can possibly treat neuropathic pain along with synaptic integration.
3.6.8. Oxygen and Ozone Therapy
O 2 , O 3 therapy is considered a promising conservative and mini-invasive intervention that can be used independently or in combination with other treatments to reduce neuropathic pain and improve pain function in patients affected by musculoskeletal disorders such as low back pain and knee osteoarthritis [ 92 ].
3.6.9. Aptiva
Aptiva is an innovative non-drug option that uses a frequency rhythmic electrical modulation system (FREMS) to treat painful diabetic neuropathy. It uses modulated electrical pulses, which differ from those used in percutaneous electrical nerve stimulation (PENS), and it is intended to improve the supply of oxygen to nerve cells to reduce pain. However, current evidence regarding efficacy is limited due to the high costs of this type of therapy. Possibly because of underlying huge cost [ 93 ].
3.6.10. Cognitive Behavioral Therapy (CBT)
A biopsychosocial approach used in several multidisciplinary pain management programs for reducing the severity of pain associated with diabetic peripheral neuropathy. CBT encourages patients to take control of their pain and lead a fulfilling life despite it [ 94 ]. Addressing the psychological component of chronic neuropathic pain is central to success. CBT strategies comprise 8 to 12 sessions, lasting 30 to 50 minutes, including psychoeducation, relaxation, cognitive restructuring, stress management, activity pacing, behavioral activation, anger control, and relapse prevention techniques [ 95 ].
3.6.11. Complementary and Integrative Medicine (CIM)
This includes nonconventional treatments such as acupuncture, meditation, massage, cupping, movement therapies, and relaxation techniques that may be used in conjunction with or in place of other medical treatments.
3.6.12. Acupuncture
A minimally invasive procedure using traditional Chinese therapy based on real experiences has proven beneficial and cost-effective in managing diabetic peripheral neuropathy, back pain, and shoulder pain [ 96 , 97 ]. This involves the stimulation of specific points on the body, most often by inserting thin needles through the skin, promoting the body's natural self-healing process. Acupuncture also stimulates blood flow to restore nerve damage. Acupuncture was found to be an effective treatment option for diabetic and human immunodeficiency virus-related peripheral neuropathy, especially in Bell's palsy and carpal tunnel syndrome [ 98 – 100 ]. Battlefield acupuncture (BFA) is an emerging method of easing neuropathic pain, purported to influence central nervous system pain processing through the release of β -endorphins and its effect on a somatotopic organization of the body represented in the auricle.
3.6.13. Aromatherapy
One of the most widely used complementary therapies in clinical practices involves the use of essential oils extracted from plants that reduce neuropathic pain scores and improve the QoL, resulting in a positive impact on physical, emotional, and mental health [ 101 ]. Preclinical research studies have reported that the essential oil obtained from bergamot (BEO) fruit (Citrus bergamia, Risso) modifies the normal and pathological synaptic plasticity implicated, for instance, in nociceptive and neuropathic pain. In addition, BEO modulates the sensitive perception of pain in different models of nociceptive, inflammatory, and neuropathic pain modulating endogenous systems.
3.7. Challenges in Managing Chronic Neuropathic pain
A good treatment strategy might take several trials of combining pharmacological and nonpharmacological therapeutic options. Pain management counseling and frequent communication is a must to target the right fit of regimes. The best outcomes have shown improvement over time with experimentation, much like a sliding scale for pain management.
3.7.1. Tolerability and Safety
The most common adverse effects of various therapeutic options discussed above were constipation, nausea, drowsiness, and dizziness. An increase in the frequency of serious adverse events occurred with chronic treatment and polypharmacy.
3.7.2. Precautions
Precautions are warranted in patients with a history of substance abuse and other significant comorbidities like heart disease and dementia. A dosage adjustment is essential in renal failure or CYP450 enzyme-inhibitor interactions.
3.7.3. Noncompliance and Quality of Life
Inadequate pharmacological response significantly contributes to drug non-compliance. In the context of neuropathic pain, minimal to no relief of pain can potentially lead to sleep disturbance, depression, fatigue, reduction in quality of life and driving ability.
4. Limitations
- Many of the newer drugs that we mentioned in the study are in phase I and II. So, these drugs are not approved for use.
- We could not formulate new treatment modalities for the treatment of neuropathic pain
- Our study does not include articles comparing superiority of combining pharmacological and nonpharmacological treatment modalities over pharmacological.
- Disease-specific treatment modalities are not clear.
- Limited articles on recent advances in psychological treatment modalities.
5. Conclusion
The increasing prevalence of chronic neuropathic pain and its poor impact on the quality of life prompts the need for an early diagnosis and intervention. Recent advances in various pharmacological modalities have been primarily limited by the side effect profile of certain drugs and the cost incurred in making them available to the masses. Research addressing nonpharmacological measures might help to come up with cost-effective solutions with minimal side effects. A mixed approach consisting of symptomatic management during an acute episode and a simultaneous multidisciplinary approach for long-term pain management is thus warranted.
Data Availability
Conflicts of interest.
The authors declare no conflicts of interest.
MIT Technology Review
- Newsletters
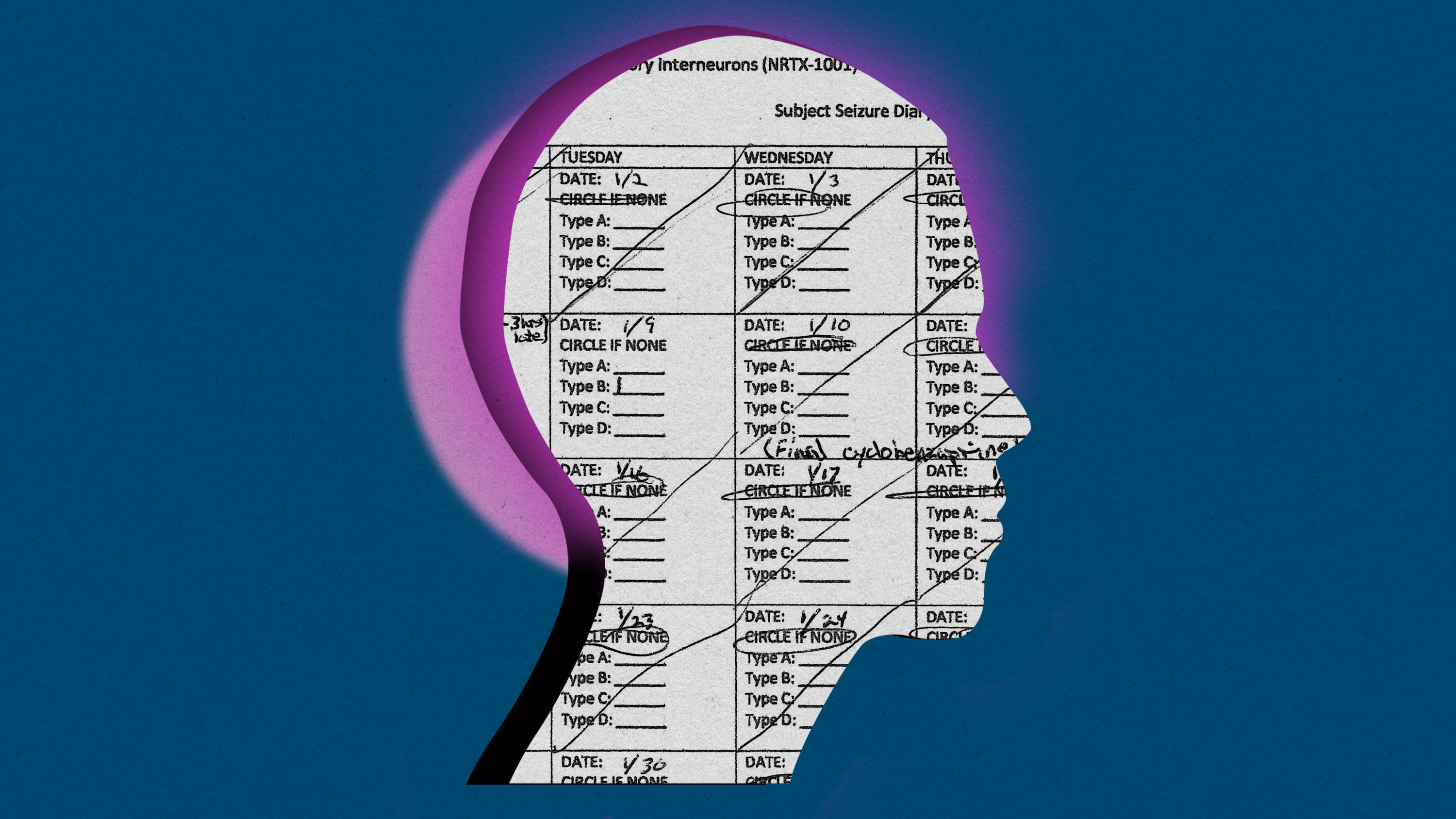
Brain-cell transplants are the newest experimental epilepsy treatment
Neurona Therapeutics’ epilepsy treatment could be a breakthrough for stem-cell technology.
- Antonio Regalado archive page
This article first appeared in The Checkup, MIT Technology Review’s weekly biotech newsletter. To receive it in your inbox every Thursday, and read articles like this first, sign up here .
Justin Graves was managing a scuba dive shop in Louisville, Kentucky, when he first had a seizure. He was talking to someone and suddenly the words coming out of his mouth weren’t his. Then he passed out. Half a year later he was diagnosed with temporal-lobe epilepsy.

Graves’s passion was swimming. He’d been on the high school team and had just gotten certified in open-water diving. But he lost all that after his epilepsy diagnosis 17 years ago. “If you have ever had seizures, you are not even supposed to scuba-dive,” Graves says. “It definitely took away the dream job I had.”
You can’t drive a car, either. Graves moved to California and took odd jobs, at hotels and dog kennels. Anywhere on a bus line. For a while, he drank heavily. That made the seizures worse.
Epilepsy, it’s often said, is a disease that takes people hostage.
So Graves, who is now 39 and two and half years sober, was ready when his doctors suggested he volunteer for an experimental treatment in which he got thousands of lab-made neurons injected into his brain.
“I said yes, but I don’t think I understood the magnitude of it,” he says.
The treatment, developed by Neurona Therapeutics, is shaping up as a breakthrough for stem-cell technology. That's the idea of using embryonic human cells, or cells converted to an embryonic-like state, to manufacture young, healthy tissue.
And stem cells could badly use a win. There are plenty of shady health clinics that say stem cells will cure anything, and many people who believe it. In reality, though, turning these cells into cures has been a slow-moving research project that, so far, hasn’t resulted in any approved medicines .
But that could change, given the remarkable early results of Neurona’s tests on the first five volunteers. Of those, four, including Graves, are reporting that their seizures have decreased by 80% and more. There are also improvements in cognitive tests. People with epilepsy have a hard time remembering things, but some of the volunteers can now recall an entire series of pictures.
“It’s early, but it could be restorative,” says Cory Nicholas, a former laboratory scientist who is the CEO of Neurona. “I call it activity balancing and repair.”
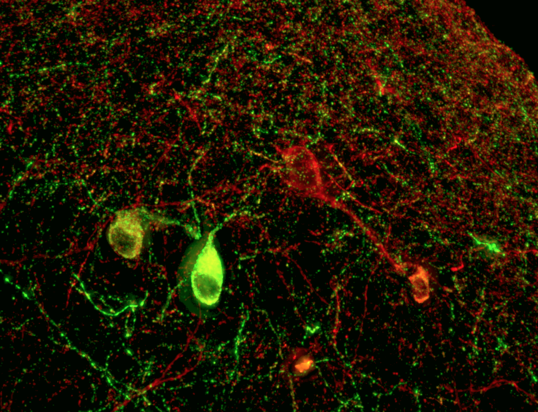
Starting with a supply of stem cells originally taken from a human embryo created via IVF, Neurona grows “inhibitory interneurons.” The job of these neurons is to quell brain activity—they tell other cells to reduce their electrical activity by secreting a chemical called GABA.
Graves got his transplant in July. He was wheeled into an MRI machine at the University of California, San Diego. There, surgeon Sharona Ben-Haim watched on a screen as she guided a ceramic needle into his hippocampus, dropping off the thousands of the inhibitory cells. The bet was that these would start forming connections and dampen the tsunami of misfires that cause epileptic seizures.
Ben-Haim says it’s a big change from the surgeries she performs most often. Usually, for bad cases of epilepsy, she is trying to find and destroy the “focus” of misbehaving cells causing seizures. She will cut out part of the temporal lobe or use a laser to destroy smaller spots. While this kind of surgery can stop seizures permanently, it comes with the risk of “major cognitive consequences.” People can lose memories, or even their vision.
That’s why Ben-Haim thinks cell therapy could be a fundamental advance. “The concept that we can offer a definitive treatment for a patient without destroying underlying tissue would be potentially a huge paradigm shift in how we treat epilepsy,” she says.
Nicholas, Neurona’s CEO, is blunter. “The current standard of care is medieval,” he says. “You are chopping out part of the brain.”
For Graves, the cell transplant seems to be working. He hasn’t had any of the scary “grand mal” attacks, that kind can knock you out, since he stopped drinking. But before the procedure in San Diego, he was still having one or two smaller seizures a day. These episodes, which feel like euphoria or déjà vu, or an absent blank stare, would last as long as half a minute.
Now, in a diary he keeps as part of the study to count his seizures, most days Graves circles “none.”
Other patients in the study are also telling stories of dramatic changes. A woman in Oregon, Annette Adkins , was having seizures every week; but now hasn't had one for eight consecutive months, according to Neurona. Heather Longo, the mother of another subject, has also said her son has gone for periods without any seizures. She's hopeful his spirits are picking up and said that his memory, balance, and cognition, are improving.
Getting consistent results from a treatment made of living cells is not going to be easy, however. One volunteer in the study saw no benefit, at least initially, while Graves’s seizures tapered away so soon after the procedure that it’s unclear whether the new cells could have caused the change, since it can takes weeks for them to grow out synapses and connect to other cells.
“I don’t think we really understand all the biology,” says Ben-Haim.
Neurona plans a larger study to help sift through cause and effect. Nicholas says the next stage of the trial will enroll 30 volunteers, half of whom will undergo “sham” surgeries. That is, they’ll all don surgical gowns, and doctors will drill holes into their skulls. But only some will get the cells; for the rest it will be play-acting. That is to rule out a placebo effect or the possibility that, somehow, simply passing a needle into the brain has some benefit.

Graves tells MIT Technology Review he is sure the cells helped him. “What else could it be? I haven’t changed anything else,” he says.
Now he is ready to believe he can get parts of his life back. He hopes to swim again. And if he can drive, he plans to move home to Louisville to be near his parents. “Road trips were always something I liked,” he says. “One of the plans I had was to go across the country. To not have any rush to it and see what I want.”
Now read the rest of The Checkup
Read more from mit technology review ’s archive.
This summer, I checked into what 25 years of research using embryonic stem cells had delivered. The answer: lots of hype and no cures …yet.
Earlier this month, Cassandra Willyard wrote about the many scientific uses of “organoids.” These blobs of tissue (often grown from stem cells) mimic human organs in miniature and are proving useful for testing drugs and studying viral infections.
Our 2023 list of young innovators to watch included Julia Joung , who is discovering the protein factors that tell stem cells what to develop into.
There’s a different kind of stem cell in your bone marrow—the kind that makes blood. Gene-editing these cells can cure sickle-cell disease. The process is grueling, though. In December, one patient, Jimi Olaghere, told us his story.
From around the web
The share of abortions that are being carried out with pills in the US continues to rise, reaching 63%. The trend predates the 2022 Supreme Court decision allowing states to bar doctors from providing abortions. Since then, more women may have started getting the pills outside the formal health-care system. ( New York Times )
Excitement over pricey new weight-loss drugs is causing “pharmaco-amnesia,” Daniel Engber says. People are forgetting there were already some decent weight-loss pills that he says were “half as good … for one-30th the price.” ( The Atlantic )
Biotechnology and health
This baby with a head camera helped teach an ai how kids learn language.
A neural network trained on the experiences of a single young child managed to learn one of the core components of language: how to match words to the objects they represent.
- Cassandra Willyard archive page
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The next generation of mRNA vaccines is on its way
Adding a photocopier gene to mRNA vaccines could make them last longer and curb side effects.
Stay connected
Get the latest updates from mit technology review.
Discover special offers, top stories, upcoming events, and more.
Thank you for submitting your email!
It looks like something went wrong.
We’re having trouble saving your preferences. Try refreshing this page and updating them one more time. If you continue to get this message, reach out to us at [email protected] with a list of newsletters you’d like to receive.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
The following represent additions to UpToDate from the past six months that were considered by the editors and authors to be of particular interest. The most recent What's New entries are at the top of each subsection.
CEREBROVASCULAR DISEASE
Mechanical thrombectomy for extremely large core infarcts (March 2024)
Randomized controlled trials have shown that mechanical thrombectomy (MT) improves outcomes for patients with acute anterior circulation ischemic stroke due to large vessel occlusion who have a large ischemic core, as defined by an Alberta Stroke Program Early Computed Tomography Score (ASPECTS) of 3 to 5 or by a core volume ≥50 mL. Emerging evidence now suggests that even patients with extremely large core infarcts (ie, a baseline ASPECTS of 0 to 2) may benefit from MT [ 1,2 ]. These data also support studies suggesting that the clinical and imaging parameters (eg, APSECTS, CT perfusion) used to differentiate irreversible core infarction from the salvageable ischemic penumbra are imperfect. However, further trials are needed to confirm the benefit of MT for patients with extremely large core infarcts. (See "Mechanical thrombectomy for acute ischemic stroke", section on 'Benefit for large core infarcts' .)
Cerebral amyloid angiopathy as a risk for isolated subdural hematoma (February 2024)
Cerebral amyloid angiopathy (CAA) commonly presents with acute intracerebral hemorrhage that may extend into the subarachnoid or subdural spaces in some instances, but the risk of isolated spontaneous subdural hematoma (SDH) from CAA is uncertain. In a retrospective study of data from two large population-based cohorts, CAA was associated with an elevated risk of SDH after adjustment for patient demographics, cardiovascular risks, and antithrombotic medication use [ 3 ]. Leptomeningeal amyloid deposition may predispose such patients to spontaneous SDH. These results expand our understanding of the varied hemorrhagic presentations associated with CAA. (See "Cerebral amyloid angiopathy", section on 'Imaging features' .)
Time window to start dual antiplatelet therapy for high-risk TIA or minor ischemic stroke (January 2024)
There is evidence from several randomized trials that early initiation of short-term dual antiplatelet therapy (DAPT) for select patients with high-risk transient ischemic attack (TIA) or minor ischemic stroke reduces the risk of recurrent ischemic stroke. The evidence comes from trials that started DAPT within 12 to 24 hours of symptom onset. Results from the recent INSPIRES trial suggest that DAPT is still beneficial when started up to 72 hours after symptom onset [ 4 ]. Although the time window is extended by the results from INSPIRES, we start DAPT as soon as possible for patients with high-risk TIA or minor ischemic stroke. (See "Early antithrombotic treatment of acute ischemic stroke and transient ischemic attack", section on 'High-risk TIA and minor ischemic stroke' .)
Management of CADASIL (November 2023)
A recent American Heart Association (AHA) scientific statement reviews various clinical aspects of cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) [ 5 ]. The AHA statement notes that safety and efficacy of thrombolysis are unknown for patients with CADASIL presenting with small vessel stroke, while mechanical thrombectomy without thrombolysis may be preferred for patients presenting with large vessel stroke unrelated to CADASIL. The AHA also suggests specific perioperative measures to avoid cerebral ischemia during anesthesia and surgery, and recommends avoidance of catheter angiography except for patients with acute ischemic stroke due to large vessel occlusion. (See "Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)", section on 'Management' .)
Risk of intracerebral hemorrhage in transfusion recipients (September 2023)
In an explorative study using a database of blood donors and >100,000 individuals who received a transfusion, the risk of spontaneous intracerebral hemorrhage (ICH) was slightly more than twofold greater in transfusion recipients whose donors later developed two or more episodes of ICH [ 6 ]. ICH is the most common manifestation of cerebral amyloid angiopathy, which is seen in Alzheimer disease, and the study also found an increased risk of ICH in patients who received a transfusion from a donor with a single previous episode of ICH plus dementia. These findings do not demonstrate causality, and a plausible mechanism for transmission of ICH has not been identified. Further study is needed to confirm or refute this finding. (See "Blood donor screening: Medical history", section on 'Neurodegenerative and other neurologic disorders' .)
Adult-onset ADHD and dementia (December 2023)
Individuals with adult-onset attention deficit hyperactivity disorder (ADHD) may have difficulties compensating for deficits from neurodegenerative or cerebrovascular processes, but any association with dementia has been inconsistent. In a prospective study including over 100,000 adults without ADHD or dementia at baseline, those who were subsequently diagnosed with adult-onset ADHD were more likely to receive a diagnosis of dementia (adjusted relative risk 2.8) [ 7 ]. Whether symptoms that resulted in the ADHD diagnosis were early or prodromal dementia symptoms is uncertain; nevertheless, these findings suggest that caregivers be alert for signs of dementia in individuals with adult-onset ADHD. (See "Attention deficit hyperactivity disorder in adults: Epidemiology, clinical features, assessment, and diagnosis", section on 'Comorbidity' .)
DEMYELINATING DISEASE
Cerebral cortical encephalitis as a manifestation of MOGAD (November 2023)
Myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) was originally described as a demyelinating disease often presenting as acute disseminated encephalomyelitis. Over time, additional MOGAD phenotypes have emerged, including a novel syndrome termed cerebral cortical encephalitis. Clinical manifestations include seizures, aphasia, stroke-like episodes, headache, and fever [ 8 ]. Most episodes are unilateral with ipsilateral symptoms and cortical swelling, T2 hyperintensity, and leptomeningeal enhancement on magnetic resonance imaging. A recent report describes children with bilateral cerebral cortical encephalitis and more fulminant disease, including critical illness, severe encephalopathy, seizures, and worse outcomes [ 9 ]. Thus, the clinical spectrum of MOGAD continues to expand. (See "Myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD): Clinical features and diagnosis", section on 'Cerebral cortical encephalitis' .)
Acute encephalopathy with biphasic seizures and late reduced diffusion (November 2023)
Acute encephalopathy with biphasic seizures and late reduced diffusion (AESD) is a parainfectious syndrome characterized by presentation with febrile status epilepticus (FSE) followed by a brief seizure-free period before recurrence of seizures in clusters. In a retrospective study from Japan of 55 patients presenting with FSE, the development of AESD in 11 patients was associated with longer time from seizure onset to hospital arrival, presence of hypoxia, and later treatment with antiseizure medications [ 10 ]. These findings suggest that shortening the seizure duration by early effective treatment and preventing hypoxia during ambulance transportation might reduce the risk of AESD. (See "Clinical features and evaluation of febrile seizures", section on 'Acute encephalopathy with biphasic seizures and late reduced diffusion' .)
Expert panel on epilepsy with eyelid myoclonia (November 2023)
Epilepsy with eyelid myoclonia (EEM; Jeavons syndrome) is a female-predominant generalized epilepsy syndrome with onset from 3 to 12 years of age characterized by eyelid myoclonia, photosensitivity, and eye closure-induced seizures or paroxysms on electroencephalography (EEG). Recently, an international expert panel found a strong consensus that EEM is often underdiagnosed, that a correct diagnosis can only be made with EEG including photic stimulation, and that an earlier age at onset is associated with an increased risk of intellectual disability and drug-resistant epilepsy [ 11 ]. Management generally involves reducing exposure to provoking factors (eg, visual stimuli, various sources of natural and artificial light) and use of antiseizure medication such as levetiracetam or valproate [ 12 ]. (See "Photosensitive epilepsies", section on 'Epilepsy with eyelid myoclonia (Jeavons syndrome)' .)
New guidelines for the treatment of neonatal seizures (October 2023)
New guidelines from the International League Against Epilepsy (ILAE) recommend phenobarbital as first-line antiseizure medication (ASM) therapy for treating most etiologies of neonatal seizures [ 13 ]. The one exception is that sodium channel blockers ( phenytoin / fosphenytoin or carbamazepine ) are considered a first-line therapy for neonates with a channelopathy. Phenytoin, levetiracetam , midazolam , and lidocaine are considered second-line ASMs for infants who continue to have seizures despite first-line therapy. Our approach is in accordance with the ILAE guidelines. (See "Treatment of neonatal seizures", section on 'Phenobarbital for most etiologies' .)
Early use of ubrogepant to abort migraine headache (November 2023)
Acute migraine treatments, including calcitonin gene-related peptide (CGRP) antagonists, are typically given at headache onset, but the benefit of earlier dosing is uncertain. In a trial of 477 patients with migraine who were treated at the onset of prodromal symptoms (prior to headache), ubrongepant improved the proportion of patients who remained free of moderate to severe headache at 24 hours compared with placebo (46 versus 29 percent) [ 14 ]. Enrolled patients had migraines that consisted of prodromal symptoms (eg, photophobia, fatigue, neck pain) occurring one to six hours before headache onset in at least 75 percent of attacks. These results support our practice to administer acute migraine treatments, such as ubrogepant , early in the course of migraine symptoms. (See "Acute treatment of migraine in adults", section on 'CGRP antagonists' .)
Low-dose dexamethasone for severe migraine in adults (October 2023)
Parenteral dexamethasone is used along with short-acting abortive therapies to reduce migraine recurrence for patients with severe symptoms, but optimal dosing is uncertain. Prior trials have reported benefit at doses ranging from 8 to 24 mg. In a recent trial of 209 adults with moderate to severe migraine presenting to the emergency department treated with metoclopramide and intravenous (IV) dexamethasone, rates of sustained relief at 48 hours were similar between groups randomly assigned to 4 versus 16 mg of dexamethasone [ 15 ]. Rates of immediate headache relief and medication use in the week following discharge were also similar. These results support our preference for adjunctive dexamethasone at a dose of 4 mg IV to reduce migraine recurrence. (See "Acute treatment of migraine in adults", section on 'Abortive therapy plus parenteral dexamethasone' .)
MOVEMENT DISORDERS
Suicidality in Parkinson disease (February 2024)
Patients with Parkinson disease (PD) are at risk for suicidality, but the magnitude of risk has been uncertain. In a meta-analysis that included 28 observational studies and more than 500,000 patients with PD, the pooled prevalence of suicidal ideation was 22 percent [ 16 ]. The risk of suicidal behavior was low (1.25 percent) but nonetheless elevated relative to the general population or patients with nonneurologic diseases (hazard ratio 1.7). Other studies indicate that risk is primarily mediated by depression; whether treatments for PD, including dopaminergic agents and deep brain stimulation, contribute to excess risk remains uncertain. Depression screening and treatment are important components of longitudinal care in all patients with PD. (See "Clinical manifestations of Parkinson disease", section on 'Depression' and "Management of nonmotor symptoms in Parkinson disease", section on 'Depression' .)
Botulinum toxin injections for essential head tremor (November 2023)
Botulinum toxin (BoNT) injections have been used for refractory head tremor in patients with essential tremor (ET) based on limited data. In a randomized trial of 117 patients with essential or isolated head tremor, BoNT type A injections into each splenius capitis muscle improved subjective and objective head tremor severity measurements compared with placebo injections, with expected waning of response by 12 weeks after each injection [ 17 ]. Adverse effects were more frequent with BoNT (47 versus 16 percent), most commonly headache or neck pain, dysphagia, and posterior neck weakness. BoNT type A injections are an option for patients with bothersome head tremor due to ET who do not tolerate oral medications or whose tremor does not respond, but side effects are common and may outweigh potential benefits in some patients. (See "Essential tremor: Treatment and prognosis", section on 'Administration and efficacy' .)
Neurostimulation device for restless legs syndrome (November 2023)
Noninvasive neuromodulation techniques are of interest for treatment of restless legs syndrome (RLS). One new device, tonic motor activation (TOMAC), delivers peroneal nerve stimulation via bilateral therapy units worn externally just below the knee, over the head of the fibula. In a randomized sham-controlled trial of TOMAC in 133 adults with medication-refractory RLS, TOMAC improved clinician-rated responses and RLS severity scores at 4 weeks [ 18 ], and the device was well tolerated for up to 24 weeks [ 19 ]. TOMAC received marketing approval in the United States in 2023 [ 20 ], and availability is anticipated in 2024. (See "Management of restless legs syndrome and periodic limb movement disorder in adults", section on 'Neurostimulation' .)
NEUROMUSCULAR DISEASE
Vamorolone for Duchenne muscular dystrophy (December 2023)
Glucocorticoid treatment with prednisone or deflazacort for Duchenne muscular dystrophy (DMD) is associated with improved motor function, but adverse effects include weight gain, slowing of growth, and bone loss. Vamorolone , a novel steroid, was designed to reduce adverse effects of glucocorticoid therapy for DMD. In the VISION-DMD trial, vamorolone treatment led to improvement on several motor outcomes compared with placebo, while efficacy was similar compared with prednisone [ 21 ]. Prednisone treatment (but not vamorolone) led to growth deceleration and bone biomarker abnormalities. Based on these findings, the US Food and Drug Administration approved vamorolone for children age ≥2 years with DMD [ 22 ]. We suggest glucocorticoid treatment for children with DMD and anticipate using vamorolone as an alternative to prednisone and deflazacort. (See "Duchenne and Becker muscular dystrophy: Glucocorticoid and disease-modifying treatment", section on 'Benefits of glucocorticoid therapy' .)
Eplontersen for polyneuropathy related to hereditary transthyretin amyloidosis (November 2023)
Hereditary transthyretin amyloidosis (ATTR) is a rare but serious form of amyloidosis that can cause a rapidly progressive, sensory-motor and autonomic polyneuropathy. The efficacy of eplontersen , an antisense oligonucleotide that inhibits hepatic production of transthyretin (TTR), was evaluated in an open-label trial in nearly 170 patients with ATTR amyloidosis and polyneuropathy who received this agent for up to 66 weeks [ 23 ]. Patients treated with eplontersen had greater reductions in serum TTR concentrations, less neuropathy-related impairment, and better quality of life compared with historical controls receiving placebo. This trial contributed to US Food and Drug Administration approval of eplontersen in December 2023 for treatment of polyneuropathy of ATTR in adults [ 24 ]. (See "Overview of amyloidosis", section on 'Therapies for individual amyloid types' .)
Fatal immune reaction after gene therapy for Duchenne muscular dystrophy (September 2023)
Recombinant adeno-associated virus (rAAV) vectors used to deliver gene therapy can be associated with a risk of severe immune reactions. This was illustrated by a report of a 27-year-old patient with advanced Duchenne muscular dystrophy (DMD) and impaired cardiopulmonary function who was treated with a high dose of rAAV containing a CRISPR-based transgene designed to upregulate dystrophin [ 25 ]. After treatment, he developed worsening cardiac dysfunction, acute respiratory distress syndrome, and fatal cardiac arrest. Laboratory and postmortem studies suggested his death was due to an innate immune reaction. Further research to develop safer approaches and identify high-risk patients may help to mitigate the acute toxic effects of rAAV gene therapy. (See "Overview of gene therapy, gene editing, and gene silencing", section on 'Potential concerns with gene therapy' and "Duchenne and Becker muscular dystrophy: Glucocorticoid and disease-modifying treatment", section on 'Risk of immune reactions with AAV vectors' .)
NEUROONCOLOGY
Osimertinib and chemotherapy in EGFR-mutated NSCLC with brain metastases (March 2024)
Trials are investigating systemic treatment options for those with epidermal growth factor receptor ( EGFR )-mutated non-small cell lung cancer (NSCLC) with central nervous system (CNS) disease. In a randomized trial, among the 222 patients with baseline CNS disease from EGFR -mutated NSCLC, osimertinib plus chemotherapy resulted in a 24-month CNS progression-free survival of 74 percent versus 54 percent with chemotherapy alone, but the difference was not statistically significant (hazard ratio 0.58, 95% CI 0.33-1.01) [ 26 ]. Results in the overall study population (with and without CNS disease) also favored combination therapy, with a trend towards improved overall survival [ 27 ]. For patients with EGFR -mutated NSCLC and brain metastases, we now suggest osimertinib and chemotherapy, but consider osimertinib alone a reasonable alternative. (See "Brain metastases in non-small cell lung cancer", section on 'Osimertinib with chemotherapy' .)
No role for central nervous system prophylaxis with high-dose methotrexate in diffuse large B cell lymphoma (February 2024)
Patients with diffuse large B cell lymphoma (DLBCL) are at substantial risk for central nervous system (CNS) relapse, but there is controversy about whether adding high-dose methotrexate (HD-MTX) prophylaxis to CD20-based induction chemoimmunotherapy can reduce this risk. In a recent observational study that included 2418 patients, administration of HD-MTX prophylaxis (at the discretion of the treating physician) was not associated with a clinically meaningful reduction in two-year risk of CNS relapse [ 28 ]. Toxicity with HD-MTX includes encephalopathy, hepatotoxicity, and kidney toxicity. Based on this and other studies, we do not routinely add HD-MTX prophylaxis to induction chemoimmunotherapy for DLBCL. (See "Initial treatment of advanced stage diffuse large B cell lymphoma", section on 'CNS management' .)
Intraoperative techniques for glioblastoma resection (December 2023)
Several intraoperative neurosurgical techniques are available to improve the extent of glioblastoma resection while minimizing damage to normal brain, but little comparative data exist. In a multicenter parallel-group trial that included over 300 patients undergoing resection of a newly diagnosed glioblastoma, rates of complete resection were comparable with use of either intraoperative magnetic resonance imaging (iMRI) or 5-aminolevulinic acid (ALA; 81 and 78 percent, respectively) [ 29 ]. In both groups, absence of any enhancing tumor postoperatively was associated with improved progression-free and overall survival. These results further support use of adjunctive tools like iMRI and ALA to facilitate maximal safe resection; selection of a specific operative plan is individualized based on neurosurgeon preference, tumor location, and availability of various technologies. (See "Clinical presentation, diagnosis, and initial surgical management of high-grade gliomas", section on 'Intraoperative techniques' .)
Systemic therapy for brain metastases from NSCLC (October 2023)
Trials are evaluating systemic therapy as an initial treatment option for subsets of patients with non-small cell lung cancer (NSCLC) with brain metastases:
● In a single-arm trial of single-agent targeted therapy in 19 patients with KRAS G12C-mutated NSCLC and untreated measurable intracranial disease, adagrasib was associated with an intracranial objective response rate of 42 percent and progression-free survival (PFS) of 5.4 months [ 30 ].
● In a single-arm trial of chemoimmunotherapy in 40 patients with advanced nonsquamous NSCLC with asymptomatic brain metastases, atezolizumab plus carboplatin and pemetrexed was associated with an intracranial median PFS of 6.9 months and response rate of 43 percent [ 31 ].
We consider either of these options to be reasonable initial systemic strategies in the patient populations in the respective trials; nevertheless, radiation is appropriate in such patients with untreated brain metastases, pending further comparative data between radiation and systemic therapy as an initial treatment strategy. (See "Brain metastases in non-small cell lung cancer", section on 'KRAS G12C' .)
BRAF/MEK targeted therapy in pediatric low-grade glioma (September 2023)
Targeted therapy is preferred for many children with BRAF V600E-mutant low-grade gliomas who require treatment beyond surgery. In a randomized, open-label, phase 2 trial in 110 such children requiring treatment after surgery for either symptoms or progression, first-line targeted BRAF/MEK inhibition ( dabrafenib plus trametinib ) improved overall response rate compared with carboplatin plus vincristine chemotherapy (47 versus 11 percent); it also improved median progression-free survival (20.1 versus 7.4 months) and was better tolerated [ 32 ]. Overall survival data are not yet mature. Although not compared with radiation therapy, targeted therapy has the advantage of avoiding or at least delaying the long-term neurologic and cognitive consequences of radiation, which are of particular concern in younger patients. (See "Uncommon brain tumors", section on 'Ganglioglioma and gangliocytoma' .)
PEDIATRIC NEUROLOGY
N-acetyl-l-leucine (NALL) for Niemann-Pick disease type C (February 2024)
Niemann-Pick disease type C (NPD-C) is a rare lysosomal disease with a wide phenotypic spectrum; most patients have onset in childhood with cerebellar ataxia and slowly progressive neurologic deterioration. Investigational therapies include N-acetyl-l-leucine (NALL), a putative neuroprotective agent that improves cellular energy production and reduces neuroinflammation. In a recent placebo-controlled, 12-week crossover trial of 60 patients (age ≥4 years) with NPD-C, treatment with NALL was well tolerated and led to improved neurologic status on a scale that measures ataxia and other neurologic signs and symptoms [ 33 ]. While these results are promising, longer-term trials are needed to determine if NALL is beneficial for patients with NPD-C. (See "Overview of Niemann-Pick disease", section on 'Experimental therapies' .)
Benign acute childhood myositis (January 2024)
Benign acute childhood myositis (BACM) is a self-limited syndrome associated with calf pain and creatinine kinase elevation, often following infection with influenza. In a retrospective study of 65 patients with BACM, the median age was 6.6 years and 66 percent of patients were male [ 34 ]. The most common symptoms were bilateral calf pain, refusal to walk, and diffuse weakness. The median creatinine kinase was 1827 U/L, which normalized after an average of seven days. Early recognition of this syndrome allows the clinician to avoid an unnecessary evaluation for other muscle diseases. (See "Overview of viral myositis", section on 'Benign acute childhood myositis' .)
Intrapartum magnesium sulfate before preterm birth and cerebral palsy (October 2023)
Magnesium sulfate is typically administered to pregnant women with impending preterm birth <32 weeks of gestation to decrease the incidence and severity of cerebral palsy in offspring. However, the recent MAGENTA trial comparing the effects of magnesium sulfate versus placebo administered before impending preterm birth between 30 and 34 weeks of gestation found that it did not prevent cerebral palsy among surviving infants [ 35 ]. These findings do not change our current practice because the trial used a single 4 g bolus of magnesium sulfate alone, whereas we also provide an ongoing 1 g/hour infusion until delivery and do not use the medication after 32 weeks; the trial was likely underpowered to find a significant difference. (See "Neuroprotective effects of in utero exposure to magnesium sulfate", section on 'Lower and upper gestational age' .)
Management of spinal deformities in children with NF1 (September 2023)
New consensus-based guidelines on the management of spinal deformities, including scoliosis in children with neurofibromatosis type 1 (NF1), have been published [ 36 ]. The guidelines recommend screening for spine deformity by physical examination at diagnosis and yearly thereafter. To limit radiation exposure in the pediatric population, diagnostic spine imaging is suggested only if clinical suspicion for a spinal abnormality arises from patient history or physical examination. Spinal tumor burden must be assessed preoperatively in any patient with NF1 undergoing surgery for scoliosis because instrumentation that impedes visualization of spinal tumors by magnetic resonance imaging is not recommended when spinal tumor burden is high. (See "Neurofibromatosis type 1 (NF1): Management and prognosis", section on 'Scoliosis' .)
OTHER NEUROLOGY
Updated guideline on postoperative delirium in adults (February 2024)
The European Society of Anaesthesiology and Intensive Care Medicine has published an updated guideline on postoperative delirium (POD) [ 37 ]. Recommendations include preoperatively screening older adults for risk factors for POD and multicomponent nonpharmacological interventions for all patients with risk factors. In addition, review of recent evidence showed that perioperative use of dexmedetomidine was associated with a lower incidence of POD, particularly when administered postoperatively in the intensive care unit. We agree with the recommendations and often use dexmedetomidine in the perioperative period to reduce the incidence of POD in high-risk patients. (See "Perioperative neurocognitive disorders in adults: Risk factors and mitigation strategies", section on 'Intravenous agents associated with lower risk' .)
Fusarium meningitis associated with epidural anesthesia (February 2024)
In early 2023, there was an outbreak of Fusarium spp meningitis in 33 immunocompetent patients who received epidural anesthesia at two clinics in Mexico. In a review of 13 cases, hospital admission was delayed by a median of 39 days after symptom onset [ 38 ]. Severe neurovascular complications, such as aneurysm, intracranial hemorrhage, stroke, and hydrocephalus, occurred despite initial improvement on antifungal therapy. Susceptibility testing was performed on one isolate and revealed resistance to all antifungals approved in the United States; however, it was susceptible to fosmanogepix, an investigational agent. Nine patients (69 percent) died from the infection; of the four survivors, three received compassionate-use fosmanogepix. Understanding the clinical features and management challenges of Fusarium meningitis are important to providing effective care should future outbreaks occur. (See "Clinical manifestations and diagnosis of Fusarium infection", section on 'Outbreaks of meningitis' .)
- Katsanos AH, Catanese L, Shoamanesh A. Endovascular Thrombectomy in Patients With Very Low ASPECTS Scores: A Systematic Review and Meta-analysis. Neurology 2023; 101:e2043.
- Almallouhi E, Zandpazandi S, Anadani M, et al. Outcomes of mechanical thrombectomy in stroke patients with extreme large infarction core. J Neurointerv Surg 2023.
- Rivier CA, Kamel H, Sheth KN, et al. Cerebral Amyloid Angiopathy and Risk of Isolated Nontraumatic Subdural Hemorrhage. JAMA Neurol 2024; 81:163.
- Gao Y, Chen W, Pan Y, et al. Dual Antiplatelet Treatment up to 72 Hours after Ischemic Stroke. N Engl J Med 2023; 389:2413.
- Meschia JF, Worrall BB, Elahi FM, et al. Management of Inherited CNS Small Vessel Diseases: The CADASIL Example: A Scientific Statement From the American Heart Association. Stroke 2023; 54:e452.
- Zhao J, Rostgaard K, Lauwers E, et al. Intracerebral Hemorrhage Among Blood Donors and Their Transfusion Recipients. JAMA 2023; 330:941.
- Levine SZ, Rotstein A, Kodesh A, et al. Adult Attention-Deficit/Hyperactivity Disorder and the Risk of Dementia. JAMA Netw Open 2023; 6:e2338088.
- Valencia-Sanchez C, Guo Y, Krecke KN, et al. Cerebral Cortical Encephalitis in Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease. Ann Neurol 2023; 93:297.
- Kannan V, Sandweiss AJ, Erickson TA, et al. Fulminant Anti-Myelin Oligodendrocyte Glycoprotein-Associated Cerebral Cortical Encephalitis: Case Series of a Severe Pediatric Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease Phenotype. Pediatr Neurol 2023; 147:36.
- Arai Y, Okanishi T, Kanai S, et al. Risk Factors of Prehospital Emergency Care for Acute Encephalopathy in Children With Febrile Status Epilepticus. Pediatr Neurol 2023; 147:95.
- Smith KM, Wirrell EC, Andrade DM, et al. Clinical presentation and evaluation of epilepsy with eyelid myoclonia: Results of an international expert consensus panel. Epilepsia 2023; 64:2330.
- Smith KM, Wirrell EC, Andrade DM, et al. Management of epilepsy with eyelid myoclonia: Results of an international expert consensus panel. Epilepsia 2023; 64:2342.
- Pressler RM, Abend NS, Auvin S, et al. Treatment of seizures in the neonate: Guidelines and consensus-based recommendations-Special report from the ILAE Task Force on Neonatal Seizures. Epilepsia 2023; 64:2550.
- Dodick DW, Goadsby PJ, Schwedt TJ, et al. Ubrogepant for the treatment of migraine attacks during the prodrome: a phase 3, multicentre, randomised, double-blind, placebo-controlled, crossover trial in the USA. Lancet 2023; 402:2307.
- Friedman BW, Solorzano C, Kessler BD, et al. Randomized Trial Comparing Low- vs High-Dose IV Dexamethasone for Patients With Moderate to Severe Migraine. Neurology 2023; 101:e1448.
- Mai AS, Chao Y, Xiao B, et al. Risk of Suicidal Ideation and Behavior in Individuals With Parkinson Disease: A Systematic Review and Meta-Analysis. JAMA Neurol 2024; 81:10.
- Marques A, Pereira B, Simonetta-Moreau M, et al. Trial of Botulinum Toxin for Isolated or Essential Head Tremor. N Engl J Med 2023; 389:1753.
- Bogan RK, Roy A, Kram J, et al. Efficacy and safety of tonic motor activation (TOMAC) for medication-refractory restless legs syndrome: a randomized clinical trial. Sleep 2023; 46.
- Roy A, Ojile J, Kram J, et al. Long-term efficacy and safety of tonic motor activation for treatment of medication-refractory restless legs syndrome: A 24-Week Open-Label Extension Study. Sleep 2023; 46.
- US Food and Drug Administration (FDA) device classification under section 513(f)(2)(de novo) available at: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/denovo.cfm?id=DEN220059 (Accessed on October 26, 2023).
- Guglieri M, Clemens PR, Perlman SJ, et al. Efficacy and Safety of Vamorolone vs Placebo and Prednisone Among Boys With Duchenne Muscular Dystrophy: A Randomized Clinical Trial. JAMA Neurol 2022; 79:1005.
- Muscular Dystrophy Association-supported drug Agamree (vamorolone) approved for the treatment of Duchenne muscular dystrophy by the FDA. Available at: https://www.mda.org/press-releases/mda-supported-drug-agamree-vamorolone-approved-for-the-treatment-of-duchenne-muscular-dystrophy-by-the-fda (Accessed on December 07, 2023).
- Coelho T, Marques W Jr, Dasgupta NR, et al. Eplontersen for Hereditary Transthyretin Amyloidosis With Polyneuropathy. JAMA 2023; 330:1448.
- Wainua (eplontersen) injection, for subcutaneous use. US Food and Drug Administration (FDA) approval information. Revised December 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/217388s000lbl.pdf (Accessed on January 03, 2024).
- Lek A, Wong B, Keeler A, et al. Death after High-Dose rAAV9 Gene Therapy in a Patient with Duchenne's Muscular Dystrophy. N Engl J Med 2023; 389:1203.
- Jänne PA, Planchard D, Kobayashi K, et al. CNS Efficacy of Osimertinib With or Without Chemotherapy in Epidermal Growth Factor Receptor-Mutated Advanced Non-Small-Cell Lung Cancer. J Clin Oncol 2024; 42:808.
- Planchard D, Jänne PA, Cheng Y, et al. Osimertinib with or without Chemotherapy in EGFR-Mutated Advanced NSCLC. N Engl J Med 2023; 389:1935.
- Lewis KL, Jakobsen LH, Villa D, et al. High-Dose Methotrexate as CNS Prophylaxis in High-Risk Aggressive B-Cell Lymphoma. J Clin Oncol 2023; 41:5376.
- Roder C, Stummer W, Coburger J, et al. Intraoperative MRI-Guided Resection Is Not Superior to 5-Aminolevulinic Acid Guidance in Newly Diagnosed Glioblastoma: A Prospective Controlled Multicenter Clinical Trial. J Clin Oncol 2023; 41:5512.
- Negrao MV, Spira AI, Heist RS, et al. Intracranial Efficacy of Adagrasib in Patients From the KRYSTAL-1 Trial With KRASG12C-Mutated Non-Small-Cell Lung Cancer Who Have Untreated CNS Metastases. J Clin Oncol 2023; 41:4472.
- Nadal E, Rodríguez-Abreu D, Simó M, et al. Phase II Trial of Atezolizumab Combined With Carboplatin and Pemetrexed for Patients With Advanced Nonsquamous Non-Small-Cell Lung Cancer With Untreated Brain Metastases (Atezo-Brain, GECP17/05). J Clin Oncol 2023; 41:4478.
- Bouffet E, Hansford JR, Garrè ML, et al. Dabrafenib plus Trametinib in Pediatric Glioma with BRAF V600 Mutations. N Engl J Med 2023; 389:1108.
- Bremova-Ertl T, Ramaswami U, Brands M, et al. Trial of N-Acetyl-l-Leucine in Niemann-Pick Disease Type C. N Engl J Med 2024; 390:421.
- Attaianese F, Costantino A, Benucci C, et al. Benign acute children myositis: 5 years experience in a tertiary care pediatric hospital. Eur J Pediatr 2023; 182:4341.
- Crowther CA, Ashwood P, Middleton PF, et al. Prenatal Intravenous Magnesium at 30-34 Weeks' Gestation and Neurodevelopmental Outcomes in Offspring: The MAGENTA Randomized Clinical Trial. JAMA 2023; 330:603.
- Xu AL, Suresh KV, Gomez JA, et al. Consensus-Based Best Practice Guidelines for the Management of Spinal Deformity and Associated Tumors in Pediatric Neurofibromatosis Type 1: Screening and Surveillance, Surgical Intervention, and Medical Therapy. J Pediatr Orthop 2023; 43:e531.
- Aldecoa C, Bettelli G, Bilotta F, et al. Update of the European Society of Anaesthesiology and Intensive Care Medicine evidence-based and consensus-based guideline on postoperative delirium in adult patients. Eur J Anaesthesiol 2024; 41:81.
- Strong N, Meeks G, Sheth SA, et al. Neurovascular Complications of Iatrogenic Fusarium solani Meningitis. N Engl J Med 2024; 390:522.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 20 March 2024
COVID’s toll on the brain: new clues emerge
- Claudia López Lloreda
You can also search for this author in PubMed Google Scholar
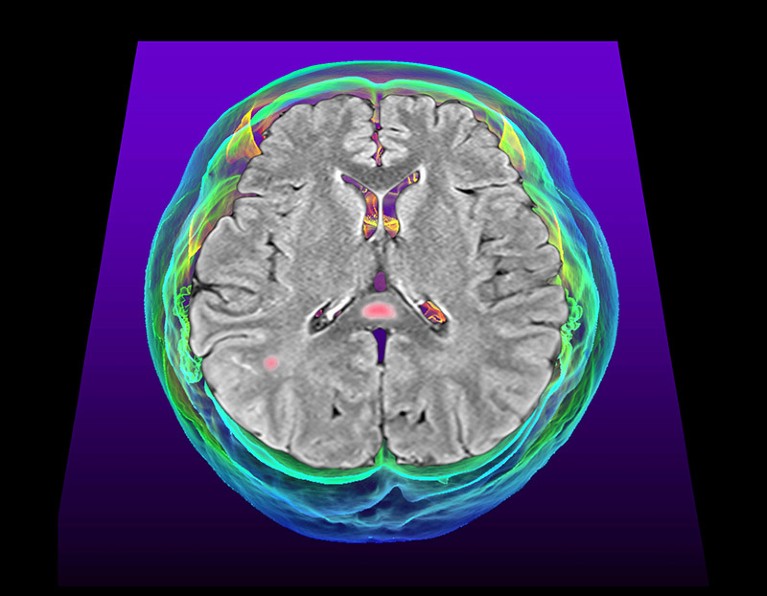
Tissue damage (pink, artificially coloured) dots the brain of a person with COVID-19 and the related disorder called multisystem inflammatory syndrome. Credit: K H Fung/Science Photo Library
Loss of smell , headaches , memory problems: COVID-19 can bring about a troubling storm of neurological symptoms that make everyday tasks difficult. Now new research adds to the evidence that inflammation in the brain might underlie these symptoms .
Not all data point in the same direction. Some studies suggest that SARS-CoV-2 , the virus that causes COVID-19, directly infects brain cells. Those findings bolster the hypothesis that direct infection contributes to COVID-19-related brain problems. But the idea that brain inflammation is key has received fresh support: one study, for example, has identified specific brain areas prone to inflammation in people with COVID-19 1 .
“The whole body of literature is starting to come together a little bit more now and give us some more concrete answers,” says Nicola Fletcher, a neurovirologist at University College Dublin.
Immunological storm
When researchers started looking for a culprit for the brain problems caused by COVID-19, inflammation quickly became a key suspect. That’s because inflammation — the flood of immune cells and chemicals that the body releases against intruders — has been linked to the cognitive symptoms caused by other viruses , such as HIV. SARS-CoV-2 stimulates a strong immune response throughout the body, but it was unclear whether brain cells themselves contributed to this response and, if so, how.

Severe COVID could cause markers of old age in the brain
Helena Radbruch, a neuropathologist at the Charité — Berlin University Medicine, and her colleagues looked at brain samples from people who’d died of COVID-19. They didn’t find any cells infected with SARS-CoV-2. But they did find these people had more immune activity in certain brain areas than did people who died from other causes. This unusual activity was noticeable in regions such as the olfactory bulb , which is involved in smell, and the brainstem, which controls some bodily functions, such as breathing. It was seen only in the brains of people who had died soon after catching the virus.
To Radbruch, these observations suggest that inflammation caused by COVID-19 outside the brain triggers an immune response in specific brain areas early during infection, which could contribute to neurological symptoms. The team suspects that if neuroinflammation persists, it could result in the brain symptoms linked to long COVID , the complex constellation of symptoms that can last for months or years after infection. The findings were published in Nature Neuroscience 1 .
Leaky barrier
But how would molecules from the rest of the body influence inflammation in the brain? Research from neuroscientist Matthew Campbell and neurologist Colin Doherty at Trinity College Dublin has found that the blood–brain barrier , which separates the brain from the rest of the body, can break down during SARS-CoV-2 infection.
The team found that this barrier is more permeable in people with both long COVID and ‘ brain fog ’ — problems with memory, concentration and decision-making — than in uninfected people or people who have long COVID but not brain fog. The results, reported in Nature Neuroscience 2 , point to a clear route for immune molecules to enter the brain, where they could lead to brain fog.
The team found that these individuals’ blood was teeming with inflammatory molecules, which could potentially cross into the brain through the leaky barrier.
Brain invasion
Although most evidence points to neuroinflammation as the source of symptoms, some studies back the direct-infection theory.
For instance, a different team at University College Dublin has found that human neurons and other brain cells in laboratory dishes can become infected with SARS-CoV-2, and even release infectious virus into their surroundings. The researchers also found that blocking a particular protein on brain cells protected them from SARS-CoV-2 infection. The virus needs to bind to the very same protein to infect other cell types, including lung cells. “This supports a model where the virus is able to directly affect the brain,” Fletcher says. The work was posted on the bioRxiv preprint server 3 and has not yet been peer reviewed.
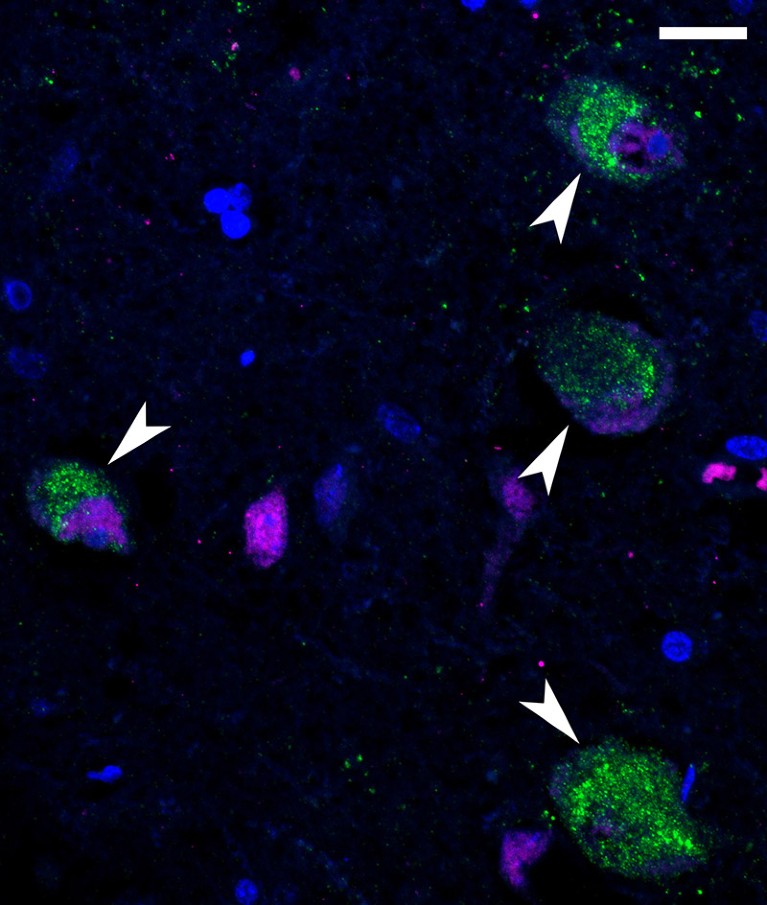
SARS-CoV-2 components (green) dot the neurons (magenta) of a person who died of COVID-19. Credit: NIAID (CC BY 2.0)
Another team successfully infected dopaminergic neurons, which use the signalling molecule dopamine to communicate. Neuroscientist Shuibing Chen at Cornell University in Ithaca, New York, and her team found that infection triggered these neurons, but not others, to enter a state called senescence , which is associated with ageing and has a characteristic gene-activity pattern that prompts cells to release immune molecules.
When the researchers analysed autopsy tissue from people who had died of COVID-19, they again saw the senescence-related gene pattern in a brain area riddled with dopaminergic neurons. Chen thinks that senescence and the resulting secretion of inflammatory factors from these cells might underlie COVID-19-induced brain damage and possibly neurological effects. The study was published in Cell Stem Cell 4 .
Complex factors
But only a small number of brain cells became infected in the lab dishes, and conclusive evidence of viral infection of the brain in people with COVID-19 is lacking.
Even Fletcher, whose study provides support for direct neuron infection, recognizes the significant contribution of immune cells. “There are data to support both theories,” she says, but “the symptoms that people are experiencing would fit with the inflammatory response.”
Ultimately, all of these studies point to potential therapeutic targets and biomarkers. For example, the diabetes medication metformin blocked viral-induced senescence in neurons in Chen’s study, making it a possible therapeutic option. But COVID-19’s brain symptoms are probably caused by a combination of factors, which would complicate treatment of cognitive problems, particularly in long COVID. “There are multiple things occurring at once,” says Campbell. “I just don’t think there’s a golden bullet.”
doi: https://doi.org/10.1038/d41586-024-00828-9
Radke, J. et al. Nature Neurosci. 27 , 409–420 (2024).
Article PubMed Google Scholar
Greene, C., et al. Nature Neurosci. 27 , 421–432 (2024).
Haverty, R. et al. Preprint at bioRxiv https://doi.org/10.1101/2023.11.21.568132 (2024).
Yang, L. et al. Cell Stem Cell 31 , 196–211 (2024).
Download references
Reprints and permissions
Related Articles

- Neuroscience

Google AI could soon use a person’s cough to diagnose disease
News 21 MAR 24

Mobile delivery of COVID-19 vaccines improved uptake in rural Sierra Leone
News & Views 13 MAR 24

Massive public-health experiment sends vaccination rates soaring
News 13 MAR 24

Innate immunity in neurons makes memories persist
News & Views 27 MAR 24

Formation of memory assemblies through the DNA-sensing TLR9 pathway
Article 27 MAR 24

A brainstem–hypothalamus neuronal circuit reduces feeding upon heat exposure

Memories are made by breaking DNA — and fixing it
News 27 MAR 24

Ketamine is in the spotlight thanks to Elon Musk — but is it the right treatment for depression?
News Explainer 20 MAR 24
Tenure-track Assistant Professor in Ecological and Evolutionary Modeling
Tenure-track Assistant Professor in Ecosystem Ecology linked to IceLab’s Center for modeling adaptive mechanisms in living systems under stress
Umeå, Sweden
Umeå University
Faculty Positions in Westlake University
Founded in 2018, Westlake University is a new type of non-profit research-oriented university in Hangzhou, China, supported by public a...
Hangzhou, Zhejiang, China
Westlake University
Postdoctoral Fellowships-Metabolic control of cell growth and senescence
Postdoctoral positions in the team Cell growth control by nutrients at Inst. Necker, Université Paris Cité, Inserm, Paris, France.
Paris, Ile-de-France (FR)
Inserm DR IDF Paris Centre Nord
Zhejiang Provincial Hospital of Chinese Medicine on Open Recruitment of Medical Talents and Postdocs
Director of Clinical Department, Professor, Researcher, Post-doctor
The First Affiliated Hospital of Zhejiang Chinese Medical University
Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Warmly Welcomes Talents Abroad
“Qiushi” Distinguished Scholar, Zhejiang University, including Professor and Physician
No. 3, Qingchun East Road, Hangzhou, Zhejiang (CN)
Sir Run Run Shaw Hospital Affiliated with Zhejiang University School of Medicine
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Neurological Illness and National Security : Lessons to Be Learned
- 1 Department of Medicine, Stanford University School of Medicine, Stanford, California
- 2 Department of Microbiology & Immunology, Stanford University School of Medicine, Stanford, California
- 3 Center for International Security and Cooperation, Stanford University, Stanford, California
- 4 Infectious Diseases Section, Veterans Affairs Palo Alto Health Care System, Palo Alto, California
- Original Investigation Neuroimaging Findings in Individuals Involved in Anomalous Health Incidents Carlo Pierpaoli, MD, PhD; Amritha Nayak, ME; Rakibul Hafiz, PhD; M. Okan Irfanoglu, PhD; Gang Chen, PhD; Paul Taylor, PhD; Mark Hallett, MD; Michael Hoa, MD; Dzung Pham, PhD; Yi-Yu Chou, MS; Anita D. Moses, MSN; André J. van der Merwe, BS; Sara M. Lippa, PhD; Carmen C. Brewer, PhD; Chris K. Zalewski, PhD; Cris Zampieri, PhD; L. Christine Turtzo, MD, PhD; Pashtun Shahim, MD, PhD; Leighton Chan, MD, MPH; NIH AHI Intramural Research Program Team; Brian Moore, DMSc, MPH; Lauren Stamps, BS; Spencer Flynn, BA; Julia Fontana, BS; Swathi Tata, BS; Jessica Lo, BS; Mirella A. Fernandez, BS; Annie Lori-Joseph, BS; Jesse Matsubara, DPT; Julie Goldberg, MA; Thuy-Tien D. Nguyen, MS; Noa Sasson, BS; Justine Lely, BS; Bryan Smith, MD; Kelly A. King, AuD, PhD; Jennifer Chisholm, AuD; Julie Christensen, MS; M. Teresa Magone, MD; Chantal Cousineau-Krieger, MD; Louis M. French, PsyD; Simge Yonter, MD; Sanaz Attaripour, MD; Chen Lai, PhD JAMA
- Original Investigation Clinical, Biomarker, and Research Findings in Individuals With Anomalous Health Incidents Leighton Chan, MD, MPH; Mark Hallett, MD; Chris K. Zalewski, PhD; Carmen C. Brewer, PhD; Cris Zampieri, PhD; Michael Hoa, MD; Sara M. Lippa, PhD; Edmond Fitzgibbon, MD; Louis M. French, PsyD; Anita D. Moses, MSN; André J. van der Merwe, BS; Carlo Pierpaoli, MD, PhD; L. Christine Turtzo, MD, PhD; Simge Yonter, MD; Pashtun Shahim, MD, PhD; NIH AHI Intramural Research Program Team; Brian Moore, DMSc, MPH; Lauren Stamps, BS; Spencer Flynn, BA; Julia Fontana, BS; Swathi Tata, BS; Jessica Lo, BS; Mirella A. Fernandez, BS; Annie-Lori Joseph, BS; Jesse Matsubara, DPT; Julie Goldberg, MA; Thuy-Tien D. Nguyen, MS; Noa Sasson, BS; Justine Lely, BS; Bryan Smith, MD; Kelly A. King, AuD, PhD; Jennifer Chisholm, AuD; Julie Christensen, MS; M. Teresa Magone, MD; Chantal Cousineau-Krieger, MD; Rakibul Hafiz, PhD; Amritha Nayak, ME; Okan Irfanoglu, PhD; Sanaz Attaripour, MD; Chen Lai, PhD; Wendy B. Smith, MA, PhD, BCB JAMA
In 2016, a set of troubling neurological symptoms was reported through confidential channels by US government personnel based at the US Embassy in Havana, Cuba. As the number of cases in Havana escalated and then similar cases occurred over the next 5 years in other locations around the globe, efforts to understand this syndrome, now known as anomalous health incidents (AHIs), were hampered by their unusual features, incomplete information, nonstandardized clinical testing, delayed reporting, and the sensitive nature of the circumstances, individuals, and their work. A subset of individuals described the abrupt onset, sometimes in the middle of the night, of a loud, grinding, clicking, buzzing, or high-pitched piercing sound inside the head, occasionally likened to a slide whistle, and a sensation of pressure, sometimes in one ear, on one side of the head, or in the face or chest. Most strikingly, these phenomena often displayed strong location dependence, in that they quickly dissipated when the individuals vacated their initial location, and then returned when the location was revisited. In some cases, this location dependence was reported to occur repeatedly by the same individual or by multiple individuals as they moved away from and then returned within minutes to a specific location, such as part of a room. These abrupt-onset sensory phenomena were followed by a mix of vertigo, dizziness, imbalance, blurry vision, tinnitus, headache, nausea, and cognitive dysfunction, sometimes leading to chronic disability.
Read More About
Relman DA. Neurological Illness and National Security : Lessons to Be Learned . JAMA. Published online March 18, 2024. doi:10.1001/jama.2023.26818
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
New neurologic issues less likely after severe COVID than flu, research suggests
sudok1 / iStock
Adults hospitalized for COVID-19 were at lower risk of needing medical care for migraine, epilepsy, neuropathy, movement disorders, stroke, and dementia in the next year than matched patients with influenza, researchers from Yale University and the University of Michigan report in Neurology .
They point out, however, that their study did not assess the effects of long COVID.
The investigators analyzed the electronic medical records of 77,272 COVID-19 patients hospitalized from April 2020 to November 2021 and the same number of flu patients admitted from 2016 to 2019 to quantify neurologic diagnoses and related healthcare use in the year after infection. The average patient age was 51 years, 57.7% were women, and 41.5% were White.
36% lower odds of movement disorders
New-onset neurologic conditions were diagnosed in 2.8% of the COVID-19 group and 4.9% of flu patients (HR, 0.62). A lower proportion of COVID-19 patients than flu patients needed care for migraine (2.0% vs 3.2%, respectively; hazard ratio [HR], 0.65 ), epilepsy (1.6% vs 2.1%; HR, 0.78 ), neuropathy (1.9% vs 3.6%; HR, 0.57 ), movement disorders (1.5% vs 2.5%; HR, 0.64 ), stroke (2.0% vs 2.4%; HR, 0.90 ), and dementia (2.0% vs 2.3%; HR, 0.93 ).
While the results were not what we expected to find, they are reassuring in that we found being hospitalized with COVID did not lead to more care for common neurologic conditions when compared to being hospitalized with influenza.
Brian Callaghan, MD, MS
After adjustment for potential confounding factors, COVID-19 patients had a lower risk of requiring care for migraine (-35%), epilepsy (-22%), neuropathy (-44%), movement disorders (-36%), stroke (-10%), and dementia (-7%) than the flu cohort.
The study didn't specifically examine long-COVID outcomes, and the findings don't necessarily conflict with those of previous studies showing increased neurologic symptoms in long-COVID patients, the authors noted. Also, the results may not apply to all COVID-19 survivors because the studied sample wasn't nationally representative.
"While the results were not what we expected to find, they are reassuring in that we found being hospitalized with COVID did not lead to more care for common neurologic conditions when compared to being hospitalized with influenza," coauthor Brian Callaghan, MD, MS, of the University of Michigan Health at Ann Arbor, said in a press release from the American Academy of Neurology, publisher of Neurology .
It's reassuring that COVID-19 behaves similarly to other respiratory viruses with respect to the studied neurologic conditions, the authors said. "There was concern that the already limited access to neurologic care would further shrink if we had a dramatic increase in neurologic care after COVID-19 infection," lead author Adam de Havenon, MD, MSc, of Yale, said in the release.
Related news
States that lean republican report more covid vaccine-related adverse events, study finds.

Study: COVID booster cuts severe COVID risk by a third in patients with weak immune systems

Study: Kids with COVID but no symptoms play key role in household spread

Survey identifies unmet child medical needs in first 2 US COVID pandemic waves

Race, geography defined telemedicine use early in pandemic, data reveal

New data show Paxlovid outperforms molnupiravir against severe COVID-19 outcomes

Probe links COVID spread to school bus riders from sick driver

Simple AI tool can predict COVID vaccine uptake, researchers report

This week's top reads
Sick cows in 2 states test positive for avian flu.
Dead wild birds were found on the affected farms.

Avian flu detected for first time in US livestock
Minnesota veterinary officials said animals with weakened or immature immune systems, such as goat kids, are at increased risk.

Avian flu detections in dairy cows raise more key questions
Experts wonder if the virus is responsible for all of the symptoms, if the virus can spread from cow to cow, and how the findings might shape farm biosecurity.

After being told to quarantine following exposure to the virus, the driver continued to ferry passengers on a public bus, school bus, and charter bus.

CDC releases ventilation guidance for curbing indoor respiratory virus spread
Advice includes optimizing HVAC systems and other steps to improve air quality and circulation.
The clinical secondary attack rate for asymptomatic COVID-positive children was more than 10%.

Puerto Rico declares dengue a public health emergency
The territory last declared an emergency owing to dengue in 2012.
Climate change unleashing torrent of infectious disease threats, physicians caution
Healthcare providers must stay current on climate-related changes in the geographic range, seasonality, and frequency of transmission of infectious diseases, the authors say.

DR Congo mpox outbreak expands, becomes deadlier
Mpox spread is occurring alongside a refugee crisis, internal violence, and a host of other disease outbreaks.

More measles cases detected in Illinois, New York as US total climbs to 64
In all of 2023, US cases of the vaccine-preventable disease totaled 58.

Our underwriters
Unrestricted financial support provided by.

- Antimicrobial Resistance
- Chronic Wasting Disease
- All Topics A-Z
- Resilient Drug Supply
- Influenza Vaccines Roadmap
- CIDRAP Leadership Forum
- Roadmap Development
- Coronavirus Vaccines Roadmap
- Antimicrobial Stewardship
- Osterholm Update
- Newsletters
- About CIDRAP
- CIDRAP in the News
- Our Director
- Osterholm in the Press
- Shop Merchandise
Advertisement
Supported by
Use of Abortion Pills Has Risen Significantly Post Roe, Research Shows

By Pam Belluck
Pam Belluck has been reporting about reproductive health for over a decade.
- Share full article
On the eve of oral arguments in a Supreme Court case that could affect future access to abortion pills, new research shows the fast-growing use of medication abortion nationally and the many ways women have obtained access to the method since Roe v. Wade was overturned in June 2022.
The Details

A study, published on Monday in the medical journal JAMA , found that the number of abortions using pills obtained outside the formal health system soared in the six months after the national right to abortion was overturned. Another report, published last week by the Guttmacher Institute , a research organization that supports abortion rights, found that medication abortions now account for nearly two-thirds of all abortions provided by the country’s formal health system, which includes clinics and telemedicine abortion services.
The JAMA study evaluated data from overseas telemedicine organizations, online vendors and networks of community volunteers that generally obtain pills from outside the United States. Before Roe was overturned, these avenues provided abortion pills to about 1,400 women per month, but in the six months afterward, the average jumped to 5,900 per month, the study reported.
Overall, the study found that while abortions in the formal health care system declined by about 32,000 from July through December 2022, much of that decline was offset by about 26,000 medication abortions from pills provided by sources outside the formal health system.
“We see what we see elsewhere in the world in the U.S. — that when anti-abortion laws go into effect, oftentimes outside of the formal health care setting is where people look, and the locus of care gets shifted,” said Dr. Abigail Aiken, who is an associate professor at the University of Texas at Austin and the lead author of the JAMA study.
The co-authors were a statistics professor at the university; the founder of Aid Access, a Europe-based organization that helped pioneer telemedicine abortion in the United States; and a leader of Plan C, an organization that provides consumers with information about medication abortion. Before publication, the study went through the rigorous peer review process required by a major medical journal.
The telemedicine organizations in the study evaluated prospective patients using written medical questionnaires, issued prescriptions from doctors who were typically in Europe and had pills shipped from pharmacies in India, generally charging about $100. Community networks typically asked for some information about the pregnancy and either delivered or mailed pills with detailed instructions, often for free.
Online vendors, which supplied a small percentage of the pills in the study and charged between $39 and $470, generally did not ask for women’s medical history and shipped the pills with the least detailed instructions. Vendors in the study were vetted by Plan C and found to be providing genuine abortion pills, Dr. Aiken said.
The Guttmacher report, focusing on the formal health care system, included data from clinics and telemedicine abortion services within the United States that provided abortion to patients who lived in or traveled to states with legal abortion between January and December 2023.
It found that pills accounted for 63 percent of those abortions, up from 53 percent in 2020. The total number of abortions in the report was over a million for the first time in more than a decade.
Why This Matters
Overall, the new reports suggest how rapidly the provision of abortion has adjusted amid post-Roe abortion bans in 14 states and tight restrictions in others.
The numbers may be an undercount and do not reflect the most recent shift: shield laws in six states allowing abortion providers to prescribe and mail pills to tens of thousands of women in states with bans without requiring them to travel. Since last summer, for example, Aid Access has stopped shipping medication from overseas and operating outside the formal health system; it is instead mailing pills to states with bans from within the United States with the protection of shield laws.
What’s Next
In the case that will be argued before the Supreme Court on Tuesday, the plaintiffs, who oppose abortion, are suing the Food and Drug Administration, seeking to block or drastically limit the availability of mifepristone, the first pill in the two-drug medication abortion regimen.
The JAMA study suggests that such a ruling could prompt more women to use avenues outside the formal American health care system, such as pills from other countries.
“There’s so many unknowns about what will happen with the decision,” Dr. Aiken said.
She added: “It’s possible that a decision by the Supreme Court in favor of the plaintiffs could have a knock-on effect where more people are looking to access outside the formal health care setting, either because they’re worried that access is going away or they’re having more trouble accessing the medications.”
Pam Belluck is a health and science reporter, covering a range of subjects, including reproductive health, long Covid, brain science, neurological disorders, mental health and genetics. More about Pam Belluck

IMAGES
VIDEO
COMMENTS
Neurology is a medical specialty that is concerned with the study of structure, function and disorders of the nervous system. Clinical disease trajectories that describe neuropsychiatric symptoms ...
N Engl J Med 2024;390:1129-1139. An 84-year-old man was evaluated at the hospital for a fall and admitted for treatment of a presumed urinary tract infection. On hospital day 4, severe chest pain ...
Sarah AFriedman, Matthew SRobbins. November 29, 2023. Research Article. The Role of Deployment History on the Association Between Epilepsy and Traumatic Brain Injury in Post-9/11 Era U.S. Veterans. Amy KHenion, Chen-PinWang, MeganAmuan, et al. November 29, 2023.
Formerly Archives of Neurology. Explore the latest in brain science including dementia, traumatic brain injury, cerebellar stroke, restless arms, herpes ... Economics, and Policy Promoting EDI in Genetics Research PTSD and Cardiovascular Disease Red Blood Cell Transfusion: 2023 AABB International Guidelines Reimagining Children's Rights in ...
Latest Articles. Filters. 51910 Results. Failed to save your search, ... Sex and gender diverse (SGD) neurology trainees include transgender, nonbinary, and intersex people. There has been historical exclusion of SGD trainees from participating in clinical care, medical research, and academic training programs. ... Research Articles. 15 March 2024.
Cecilia Åkerlund and David Nelson. Cecilia Åkerlund and David Nelson join The Lancet Neurology to discuss their research on clinical variables that might distinguish how the disease process progresses in people with traumatic brain injury. The Article is published in the January issue of The Lancet Neurology. Follow us.
Explore Neurology/Neurosurgery articles from The New England Journal of Medicine ... Research 1152; Clinical Cases 746; Other 537; Review 534; Commentary 526; Media 257; Perspective 197; By Date.
Neurology ®. The most widely read and highly cited peer-reviewed neurology journal. José G. Merino, MD, MPhil, FAAN, Editor-in-Chief. View latest issue
Research Article. 14 Mar 2024 Open Access. Membrane Proteome-Wide Screening of Autoantibodies in CIDP Using Human Cell Microarray Technology. Marta Caballero-Ávila, ... Transforming health care delivery in neurology. Latest Blog Post. 24 May 2023. Accelerate, Innovate, Learn.
Neurology June 22, 2023 The First Person to Be Diagnosed with Autism Has Died at 89 A 1943 paper highlighted "Donald T." as "Case 1" of 11 children with "autistic disturbances of ...
Study Finds High Prevalence of Hidden Brain Changes in People With Heart Disease. Mar. 26, 2024 — A new analysis involving over 13,000 people has found changes to blood vessels in the brain that ...
1. Introduction. Globally, neuropathic pain is prevalent in 7%-10% of the general population, among which 20-30% have chronicity [].Chronic neuropathic pain was redefined in 2011 by the International Association for the Study of Pain (IASP) as: "pain arising as a direct consequence of a lesion or disease affecting the somatosensory system including peripheral fibers" (Aβ, Aδ, and C ...
Neurona Therapeutics' epilepsy treatment could be a breakthrough for stem-cell technology. This article first appeared in The Checkup, MIT Technology Review's weekly biotech newsletter. To ...
Neurology Today reports on breaking news, issues, and trends in the practice and science of neurology, reaching more than 36,000 professionals. It delivers credible, up-to-the-minute, balanced, cutting-edge reporting and commentary for today's busy neurology professionals. Published in print twice a month with the latest developments and online-only coverage on NeurologyToday.com, Neurology ...
What's new in neurology. Authors: John F Dashe, MD, PhD. April F Eichler, MD, MPH. Richard P Goddeau, Jr, DO, FAHA. Janet L Wilterdink, MD. Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan 2024.
November 10, 2023. Research Article. Increased Intracranial Pressure in Pediatric Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease. Linda Nguyen, Darryl K. Miles, Lana Harder, et al. November 02, 2023. Clinical/Scientific Note. Early Neuroaxonal Damage in Neurologic Disorders Associated With GAD65 Antibodies.
Research Article Abnormal Neurologic Findings in Patients With Sickle Cell Disease Without a History of Major Neurologic Events Mohammed B. Nawaiseh , Ahmed M. Yassin , Mohammed Q. Al-Sabbagh , et al.
Loss of smell, headaches, memory problems: COVID-19 can bring about a troubling storm of neurological symptoms that make everyday tasks difficult. Now new research adds to the evidence that ...
A major new study released by The Lancet Neurology shows that, in 2021, more than 3 billion people worldwide were living with a neurological condition. The World Health Organization (WHO) contributed to the analysis of the Global Burden of Disease, Injuries, and Risk Factor Study (GBD) 2021 data. Neurological conditions are now the leading cause of ill health and disability worldwide.
A new study highlights the importance of middle age in understanding and predicting future cognitive health. Researchers emphasize that this period, traditionally between 40 and 65 years, is pivotal for identifying risk factors for dementia and represents a crucial phase for interventions. Featured Neurology Neuroscience.
In 2016, a set of troubling neurological symptoms was reported through confidential channels by US government personnel based at the US Embassy in Havana, Cuba. As the number of cases in Havana escalated and then similar cases occurred over the next 5 years in other locations around the globe,...
Archive of all articles across the Neurology ... Research Articles. 21 March 2024 Video. Expanding the Clinical Spectrum of DRP2 -Associated Charcot-Marie-Tooth Disease. ... Please login to be able to save your searches and receive alerts for new content matching your search criteria.
Neuroscience News Home. Neuroscience News is an independent open access science magazine. Since 2001, we have featured neuroscience research news from labs, universities, hospitals and news departments around the world. Topics include brain research, AI, psychology, neuroscience, mental health and neurotech.
Vaccines that protect against severe illness, death and lingering long Covid symptoms from a coronavirus infection were linked to small increases in neurological, blood, and heart-related ...
Adults hospitalized for COVID-19 were at lower risk of needing medical care for migraine, epilepsy, neuropathy, movement disorders, stroke, and dementia in the next year than matched patients with influenza, researchers from Yale University and the University of Michigan report in Neurology.. They point out, however, that their study did not assess the effects of long COVID.
Among the Institute's achievements of which Remuzzi is most proud is the training of more than 9200 people through professional training courses, master's degrees, and research doctorates; today, many research organisations in Italy are led by individuals who have received training at the Mario Negri Institute, with the Director reeling off a ...
The News. On the eve of oral arguments in a Supreme Court case that could affect future access to abortion pills, new research shows the fast-growing use of medication abortion nationally and the ...