Health Is Wealth Essay for Students and Children
500+ words health is wealth essay.
Growing up you might have heard the term ‘Health is Wealth’, but its essential meaning is still not clear to most people. Generally, people confuse good health with being free of any kind of illness. While it may be part of the case, it is not entirely what good health is all about. In other words, to lead a healthy life , a person must be fit and fine both physically and mentally. For instance, if you are constantly eating junk food yet you do not have any disease, it does not make you healthy. You are not consuming healthy food which naturally means you are not healthy, just surviving. Therefore, to actually live and not merely survive, you need to have the basic essentials that make up for a healthy lifestyle.


Introduction
Life is about striking a balance between certain fundamental parts of life. Health is one of these aspects. We value health in the same way that we value time once we have lost it. We cannot rewind time, but the good news is that we can regain health with some effort. A person in good physical and mental health may appreciate the world to the fullest and meet life’s problems with ease and comfort. Health is riches implies that health is a priceless asset rather than money or ownership of material possessions. There is no point in having money if you don’t have good health.
Key Elements Of A Healthy Lifestyle
If you wish to acquire a healthy lifestyle, you will certainly have to make some changes in your life. Maintaining a healthy lifestyle demands consistent habits and disciplined life. There are various good habits that you can adopt like exercising regularly which will maintain your physical fitness. It also affects your mental health as when your appearance enhances, your confidence will automatically get boosted.
To live a healthy life, one must make some lifestyle modifications. These modifications can include changes to your food habits, sleeping routines, and lifestyle. You should eat a well-balanced, nutrient-dense diet for your physical wellness.
Further, it will prevent obesity and help you burn out extra fat from your body. After that, a balanced diet is of great importance. When you intake appropriate amounts of nutrition, vitamins, proteins, calories and more, your immune system will strengthen. This will, in turn, help you fight off diseases powerfully resulting in a disease-free life.
Above all, cleanliness plays a significant role in maintaining a healthy lifestyle. Your balanced diet and regular exercise will be completely useless if you live in an unhealthy environment. One must always maintain cleanliness in their surroundings so as to avoid the risk of catching communicable diseases.
Get the huge list of more than 500 Essay Topics and Ideas
Benefits Of A Healthy Lifestyle
As it is clear by now, good health is a luxury which everyone wants but some of them cannot afford. This point itself states the importance of a healthy lifestyle. When a person leads a healthy lifestyle, he/she will be free from the tension of seeking medical attention every now and then.

On the contrary, if you have poor health, you will usually spend your time in a hospital and the bills will take away your mental peace. Therefore, a healthy lifestyle means you will be able to enjoy your life freely. Similarly, when you have a relaxed mind at all times, you will be able to keep your loved ones happy. A healthy individual is more likely to fulfil all of his goals because he can easily focus on them and has the energy to complete them. This is why the proverb “Health is Wealth” carries so much weight.
A socially healthy individual is one who is able to interact effectively and readily connect with others. Without his ego, he can easily blend with the person in front of him, exuding a nice feeling and energy.
Every human being should participate in sports and activities to get away from the monotony of daily life. It is because sports and games assist in instilling a sense of oneness in people, build leadership skills, and make a person absolutely disciplined.
Moreover, a healthy lifestyle will push you to do better in life and motivate you to achieve higher targets. It usually happens that people who are extremely wealthy in terms of money often lack good health. This just proves that all the riches in the world will do you no good if there is an absence of a healthy lifestyle.
In short, healthy life is the highest blessing that must not be taken for granted. It is truly the source of all happiness. Money may buy you all the luxuries in the world but it cannot buy you good health. You are solely responsible for that, so for your well-being and happiness, it is better to switch to a healthy lifestyle.
Good Health for Children
Childhood is an ideal period to inculcate healthy behaviours in children. Children’s health is determined by a variety of factors, including diet, hydration, sleep schedule, hygiene, family time, doctor visits, and physical exercise. Following are a few key points and health tips that parents should remember for their children:
- Never allow your children to get by without nutritious food. Fruits and vegetables are essential.
- Breakfast is the most important meal of the day, therefore teach them to frequently wash their hands and feet.
- Sleep is essential for your child.
- Make it a habit for them to drink plenty of water.
- Encourage physical activity and sports.
- Allow them enough time to sleep.
- It is critical to visit the doctor on a regular basis for checks.
Parents frequently focus solely on their children’s physical requirements. They dress up their children’s wounds and injuries and provide them with good food. However, they frequently fail to detect their child’s deteriorating mental health. This is because they do not believe that mental health is important.
Few Lines on Health is Wealth Essay for Students
- A state of physical, mental, emotional, and social well-being is referred to as health. And all of this is linked to one another.
- Stress, worry, and tension are the leading causes of illness and disease in today’s world. When these three factors are present for an extended period of time, they can result in a variety of mental difficulties, which can lead to physical and emotional illnesses. As a result, taking care of your own health is critical.
- Unhealthy food or contaminated water, packed and processed food and beverages, unsanitary living conditions, not getting enough sleep, and a lack of physical activity are some of the other primary causes of health deterioration.
- A well-balanced diet combined with adequate exercise and hygienic habits, as well as a clean environment, can enhance immunity and equip a person to fight most diseases.
- A healthy body and mind are capable of achieving things that a sick body and mind are incapable of achieving, including happiness.
- It is also vital to seek medical and professional assistance when necessary because health is our most valuable asset.
- Activities such as playing an instrument, playing games, or reading provide the brain with the required exercise it requires to improve health.
Maintaining healthy behaviours improves one’s outlook on life and contributes to longevity as well as success.
Frequently Asked Questions
Question 1: What are the basic essentials of a healthy life? Answer: A healthy life requires regular exercise, a balanced diet, a clean environment, and good habits.
Question 2: How can a healthy life be beneficial? Answer: A healthy lifestyle can benefit you in various ways. You will lead a happier life free from any type of disease. Moreover, it will also enhance your state of mind.
Question 3: When is World Health Day celebrated?
Answer: Since 1950, World Health Day has been observed on the 7th of April by the World Health Organization (WHO), after a decision made at the first Health Assembly in 1948. It is observed to raise awareness about people’s overall health and well-being around the world.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Home — Essay Samples — Nursing & Health — Childhood Obesity — Importance Of Good Health
Importance of Good Health
- Categories: Childhood Obesity
About this sample

Words: 649 |
Published: Mar 14, 2024
Words: 649 | Page: 1 | 4 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1163 words
4 pages / 1719 words
5 pages / 2053 words
4 pages / 1991 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Childhood Obesity
Childhood obesity is a growing epidemic that has raised significant concerns among health professionals, parents, and policymakers alike. With the rise of sedentary lifestyles, increased consumption of processed foods, and lack [...]
Buzzell, L. (2019, August 13). Benefits of a Healthy Lifestyle. Johns Hopkins Medicine. https://www.healthline.com/health/healthy-eating-on-a-budget#1.-Plan-meals-and-shop-for-groceries-in-advance
With obesity rates on the rise, and student MVPA time at an all time low, it is important, now more than ever, to provide students with tools and creative opportunities for a healthy and active lifestyle. A school following a [...]
In conclusion, while Zinczenko's analysis in "Don't Blame the Eater" offers valuable insights into the rise of childhood obesity and the role of the fast-food industry, it is necessary to critically examine his claims. While [...]
Throughout recent years obesity has been a very important topic in our society. It has continued to rise at high rates especially among children. This causes us to ask what are the causes of childhood obesity? There are many [...]
It is well known today that the obesity epidemic is claiming more and more victims each day. The Centers for Disease Control and Prevention writes “that nearly 1 in 5 school age children and young people (6 to 19 years) in the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Talk to our experts
1800-120-456-456
- Health is Wealth Essay

Importance of Working Towards Good Health
Health is God’s gift to us. Health refers to the physical and mental state of a human being. To stay healthy is not an option but a necessity to live a happy life. The basic laws of good health are related to the food we eat, the amount of physical exercise we do, our cleanliness, rest, and relaxation. A healthy person is normally more confident, self-assured, sociable, and energetic. A healthy person views things calmly, and without prejudice.
Introduction
“The Dalai Lama, when asked what surprised him most about humanity, answered "Man! Because he sacrifices his health to make money. Then he sacrifices money to recuperate his health. And then he is so anxious about the future that he does not enjoy the present; the result being that he does not live in the present or the future; he lives as if he is never going to die, and then dies having never really lived.” This signifies that individuals don’t prioritise their mental health to earn money. Some even work 24 hours a day or seven days a week.
However, you have the option to remain balanced. So, balance work and fitness daily. Always strive to keep a cheerful as well as a concentrated routine. It is necessary to plan ahead of time. In any case, one must maintain a good mental, bodily, and emotional state, and no professional or counsellor can assist you unless you desire to live. The will to live in the moment and make the most of it awakens the ideal strength within you, and you are the only one who can never let yourself fall apart.
Importance of Maintaining Health
We live in a super-fast age. The Internet has shrunk the world dramatically and people are connected 24x7. Multitasking is the order of the day, as we struggle to fulfill our responsibilities for everyone in life. In this fight, we often forget to spare time for ourselves. The stress levels continue to build up until one day a major collapse may make us realize that in all this hectic activity, we have forgotten to take care of one important thing – our health.
As we spend days shuttling between hospital and home, putting our body through one test after another, trying to find out what has gone wrong, we are forced to remember that ‘Health is indeed Wealth’.
In earlier days, life was very simple. People worked for a stipulated time, often walked everywhere, ate more homemade food, did household chores, and enjoyed a healthy balance in life.
Now people have cars and bikes to commute, so they walk less. With the demand for more working hours, people are awake till late at night and indulge in more junk food than home-cooked food. Modern equipment at home has reduced the labour work and increased dependency on this equipment. People don’t have enough time to exercise or even get enough sunlight. Nowadays people are living very unhealthy lifestyles.
Unhealthy living conditions have increased the contraction of people to various diseases like obesity, diabetes, heart attacks, hypertension, etc. This has alarming implications in the near future. So it is very important to focus on our health as much as we focus on our work. Moderation in food habits, daily exercise, and balanced work-life can surely make a big difference to our health and body. When a person stays mentally and physically fit, his actions and decisions are more practical and logical and hence he is more successful in life. Furthermore, good health has a direct impact on our personality.
It's crucial to consider how much self-control you have to keep a healthy lifestyle. Research reveals that changing one's behaviour and daily patterns are quite tough. According to the data, whether a person has a habit of smoking, drinking alcohol, doing drugs, or any other substance, it is extremely difficult to quit. A study found that 80% of smokers who tried to quit failed, with only 46% succeeding.
Importance of Good Health
A healthy body has all the major components that help in the proper functioning of the body. The essential component is the state of physical health. Your life term extends when you maintain good physical fitness. If you are committed to exercising with a sensible diet, then you can develop a sense of well-being and can even prevent yourself from chronic illness, disability, and premature death.
Some of the benefits of increased physical activity are as follows.
It Improves Our Health
1. It increases the efficiency of the heart and lungs.
2. A good walk can reduce cholesterol levels.
3. Good exercise increases muscle strength.
4. It reduces blood pressure.
5. It reduces the risk of major illnesses such as diabetes and heart disease.
Improved Sense of Well-being
1. It helps in developing more energy.
2. It reduces stress levels.
3. Quality of sleep improves.
4. It helps in developing the ability to cope with stress.
5. It increases mental sharpness.
Improved Appearances
1. Weight loss contributes to a good physique.
2. Toned muscles generate more energy.
3. Improved posture enhances our appearance.
Enhanced Social Life
1. It improves self-image
2. It increases opportunities to make new friends.
3. It increases opportunities to share an activity with friends or family members.
Increased Stamina
1. Increased productivity.
2. Increased physical capabilities.
3. Less frequent injuries.
4. Improved immunity to minor illnesses.
Along with physical fitness, a good mental state is also essential for good health. Mental health means the emotional and psychological state of an individual. The best way to maintain good mental health is by staying positive and meditating.
However, unlike a machine, the body needs rest at regular intervals. A minimum of six to seven hours of sleep is necessary for the body to function optimally. Drinking plenty of water and a balanced diet is also very important for your body. If you violate the basic laws of good health, like working late hours, ignoring physical exercise, eating junk food, it will lead to various ailments like hypertension, heart attacks, and other deadly diseases.
What is National Health Day?
Every year on April 7th, World Health Day is celebrated. The World Health Organization (WHO) hosted the inaugural World Health Day on April 7, 1950, to draw the entire world’s attention to global health.
Every year, the World Health Organization (WHO) comes up with a new theme for public awareness, such as "Support Nurses and Midwives" in 2020. This supports the situation of COVID-19, where healthcare workers are saving lives day and night without worrying about their health.
The WHO also operates a global health promotion initiative to align equality so that individuals can take control of their lives, "every life matters," and consider their fitness. The government promotes numerous health policies, including food security, workplace quality, and health literacy, in schools, colleges, workplaces, and various community activities.
Good Health for Children
Children need to maintain good physical and mental health. With an increase in the pressure of studies and over-indulgence in modern gadgets, children are losing the most precious thing, which is health. These days, they barely play in the playgrounds, they are more inclined towards junk food and spend more time on the screen. These unhealthy activities are slowly sabotaging their health. Parents should concentrate on the physical and mental health of their children, and inculcate good habits for maintaining a healthy lifestyle from a tender age.
Cleanliness also has a major role to play in maintaining good health. Taking a bath every day, washing hands before eating meals, brushing twice a day, changing clothes regularly, etc. are important habits to maintain good health.
Society is witnessing gloomy faces as a result of children and their parents' excessive usage of a computer, mobile phone, and the Internet. They are constantly using these technological items, oblivious to the fact that they may harm their health. Teenagers are frequently discovered engrossed in their electronic devices, resulting in mishaps.
The usage of electronic devices frequently results in anxiety and hostility. Excessive usage of these products has been linked to cancer, vision loss, weight gain, and insomnia.
Emotional development is another crucial component that should not be disregarded because it determines whether or not a person is healthy. An emotionally healthy person should have a solid sense of logic, realisation, and a realistic outlook.
Conclusion
Health is Wealth because if we are not healthy then all our wealth, fame and power can bring no enjoyment. Keeping fit and healthy is indeed not an option but a necessity.

FAQs on Health is Wealth Essay
1. Why is Health Considered as Wealth?
Health is wealth because it is one of God’s most precious gift to human beings. Good health refers to a balanced and healthy physical and mental state of an individual. If any individual is not healthy, wealth, fame, and power can bring no enjoyment. So health has more value than materialistic things.
2. When is World Health Day Celebrated?
World Health Day is celebrated on 7 th April to raise awareness about health and fitness.
3. How Can You Maintain Good Health?
You can maintain good health by following a balanced and healthy diet. Have a good lifestyle by balancing work and life. You should have a moderate physical fitness regime every day. Go for brisk walks regularly or do other forms of exercise. Also, meditate and be positive to take care of your mental health.
4. Who came up with the phrase "health is wealth"?
If a man begins to live a lifestyle without a plan or unhealthy manner, he will confront numerous difficulties. He'd be depressed on the inside, untidy and filthy on the outside, and emotionally unstable all the time. A person who lives an unhealthy lifestyle will wake up late at night and early in the morning. Not only would this affect their mental condition, but it would also poison their surroundings.
There would be a lot of wrath and sadness, and they would have fits from time to time.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical Literature
- Classical Reception
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Archaeology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Agriculture
- History of Education
- History of Emotions
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Variation
- Language Families
- Language Acquisition
- Language Evolution
- Language Reference
- Lexicography
- Linguistic Theories
- Linguistic Typology
- Linguistic Anthropology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Modernism)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Culture
- Music and Religion
- Music and Media
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Society
- Law and Politics
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Oncology
- Medical Toxicology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Medical Ethics
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Games
- Computer Security
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Neuroscience
- Cognitive Psychology
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business History
- Business Strategy
- Business Ethics
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Methodology
- Economic Systems
- Economic History
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Theory
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

18 The Value of Health
Daniel M. Hausman earned his philosophy PhD in 1978 at Columbia University, and has taught at the University of Maryland at College Park, Carnegie Mellon University, and since 1988 at the University of Wisconsin-Madison
- Published: 07 April 2015
- Cite Icon Cite
- Permissions Icon Permissions
Health is valuable both instrumentally, in terms of its consequences for autonomy, opportunity, and well-being, and intrinsically, at least with respect to the mental states it encompasses. Quantifying the value of health is problematic, because there are many different ways in which people may suffer diminished health. Because of this multidimensionality, the “healthier than” relation is incomplete, and health has no quantity or magnitude. Health must be measured by its value. But it has different values, and the same token health states will have different values in different environments or for people who have different goals and activities. The value of types of health states must thus be some sort of average of the varying values of tokens. Assigning those average values is challenging, and actual techniques, which rely on preference surveys, are problematic.
This chapter will be concerned exclusively with the value of human health. In particular, I shall be concerned with the value of a person’s health to that person, with the ways in which health is good for people. One important way in which health is good for a person is if health contributes to that person’s well-being. But I shall not assume that the only way that health can be good for someone is through its bearing on well-being. Health may, for example, also contribute to freedom and independence, or it may constitute a personal good of its own kind.
It is uncontroversial that health is extremely valuable. Every culture values health highly, even as cultures disagree on details concerning what constitutes health. Health is not, however, always good for people. Those German men who were too unhealthy to serve in the Nazi armies were fortunate to miss out on the Eastern Front. Yet exceptions such as this one do not impugn the generalization that health is usually very good for people.
One obvious explanation of this generalization is that a minimal level of health is required for action, consciousness, and life itself. Without some minimal level of health, nothing else can make people’s lives go well. Health beyond what is required for life and basic functioning is also of great value. Why? Three immediate answers come to mind, all of which are correct as far as they go. First, health is an extremely important cause of well-being. But this answer tells us little until we have some account of how health contributes to well-being. A second quick answer is that people value health. But this claim, true as it is, does not tell us much without an account of health that explains and justifies the value that people place on health. A third answer is that health promotes other values such as opportunity and autonomy. But again one must ask how health does so.
To understand the value of health, one needs to clarify what health is. That will be the task of the first two sections. Section 18.3 begins the task of explaining what constitutes better health and whether health has a scalar value, and section 18.4 considers whether preferences can serve as measures of better health, as is assumed by most of those working on health measurement. Section 18.5 addresses the question of whether a measurable scalar value can be assigned to health, and section 18.6 assesses three accounts of the value of health. Section 18.7 concludes.
18.1. Evaluative Views of Health
There is a large literature concerning the concept of health. Most of it takes health to be the absence of physical or mental disease or impairment. Although I shall take for granted this negative characterization of health, it is not uncontested. In 1947, the World Health Organization famously defined health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (1948: 100). But this definition conflates health and well-being, and, without ever explicitly repudiating it, the World Health Organization itself relies on narrower characterizations of health. Lennart Nordenfelt defends a positive “holistic” view of health as a second-order ability to realize one’s goals (2000: 79–81). Carol Ryff has written extensively on positive health, which she identifies primarily with possessing purpose in life and quality relations with other people, although in her view other goods such as self-esteem and mastery are closely connected. She writes, “Positive health is ultimately about engagement in living” ( Ryff and Singer 1998 : 10).
Rather than interpreting those who see health as well-being (or a generalized ability to realize one’s goals or as engagement with living) as disagreeing about the properties of some single thing called “health,” I think these contrasting claims reveal that there are multiple notions of health. According to the broad concept of health I shall discuss—health as the absence of pathology—which is the concept employed by pathologists and physiologists, health depends on the functioning of the parts and processes within people’s bodies and minds. Although being Jewish was likely to be fatal condition if one lived in Eastern Europe in the early 1940s, it was not itself a physical or mental pathology (though some Nazis mistakenly believed otherwise). Even those who maintain that there is a great deal more to health than what is “within the skin” can recognize a “negative” notion of health as the absence of pathology.
Having in this way limited the notion of health under discussion, controversies remain concerning what constitutes pathology. The many detailed accounts are of two general kinds: naturalist and evaluative. According to evaluative views, it is part of the concept of health that it is good for an organism, and our evaluative standards—particularly concerning well-being—help to define health. It might appear that evaluative theorists are obviously right. 1 Whether something is a disease apparently depends on whether it is bad for an organism in ordinary environments. 2 Tristram Engelhardt provides a memorable example of the way in which values have affected disease classification in his discussion of the history of masturbation, which for a couple of centuries was widely regarded as a disease in Europe and the United States ( Engelhardt 1974 ). Consensus was never complete, and there were disputes about whether masturbation is a physical or a mental disease and about whether masturbation is a cause of disease rather than a disease itself. But much of the medical community regarded it as a medical disorder, and doctors prescribed treatments ranging from opium, cold baths, and visits to prostitutes for men to clitoridectomies for women. It is obvious in retrospect and was obvious at the time that moral judgment influenced disease classification. Tissot’s influential mid-eighteenth-century treatise asserts, “We have seen that masturbation is more pernicious than excessive intercourse with females. Those who believe in a special providence account for it by a special ordinance of the Deity to punish this crime” (1758; quoted in Engelhardt 1974 : 239).
Engelhardt sums up as follows:
Insofar as a vice is taken to be a deviation from an ideal of human perfection, or “well-being,” it can be translated into disease language. . . . The shift is from an explicitly ethical language to a language of natural teleology. To be ill is to fail to realize the perfection of an ideal type; to be sick is to be defective rather than to be evil. . . . The notion of the “deviant” structures the concept of disease providing a purpose and direction for explanation and for action, that is, for diagnosis and prognosis, and for therapy. A “disease entity” operates as a conceptual form organizing phenomena in a fashion deemed useful for certain goals. The goals, though, involve choice by man and are not objective facts, data “given” by nature. They are ideals imputed to nature. ( Engelhardt 1974 : 247–48)
Engelhardt concludes that health is the absence of defect or deviance, where defect and deviance are evaluative notions that depend on views of well-being, perfection, virtue, and duty.
It is, however, questionable whether the case of masturbation supports an evaluative view of health such as Engelhardt’s ( Boorse 1997 : 72–78). Whether historical claims concerning attitudes toward masturbation are true depends on what people in the nineteenth century believed and why they believed what they did, rather than the definition of health. If one believes that masturbation involves physical or mental states that are bad for people, then according to the evaluative theorist, one ought to believe masturbation is a disease. Thus evaluative theorists regard nineteenth-century physicians as justified in their belief that masturbation (as an activity that issues from and causes harmful physical or mental states) is a disease, given their belief that masturbation is bad for people. The naturalist in contrast denies that harmful physical and mental states are automatically diseases and that diseases must be harmful. In some circumstances heresy is a fatal mental condition and flat feet a life-saving escape from the draft. Yet flat feet are pathological, while heresy may be healthy.
There has, of course, been a huge change in values concerning masturbation, and that change in values has been both a cause and an effect of a change in attitudes toward whether masturbation is a disease. But when one looks more closely, it turns out that the claim that masturbation is a disease was not defended by normative condemnation. The case rested instead on a long list of false assertions about the effects of masturbation on the functioning of other organ systems and about the mechanisms through which masturbation had these effects. Those false assertions were no doubt often motivated by moral objections to masturbation, but the causal connections show only that moral commitments can cause people to make false factual claims, not that morality defines pathology. The effects of masturbation were supposed to derive from debilitation caused by the loss of semen. But the loss of semen is not debilitating and has few effects on other organ systems. Masturbation does not result in the loss of more semen than intercourse, which was held to be harmless (apart from the risks of venereal disease), and some other theory had to be concocted to generate a mechanism whereby female masturbation diminished the functioning of body parts. Whether via the loss of semen or in some other way, masturbation does not cause stomach aches, epilepsy, blindness, deafness, vertigo, heart irregularities, or rickets—all of which were alleged to be its effects. If masturbation had these effects, then masturbation would be a disease or a cause of disease such as anorexia or cutting oneself. To the extent that those who regarded masturbation as a disease felt it incumbent on them to show that it had other physiological consequences than a morally condemnable self-induced orgasm, they seem to be repudiating rather than presupposing the view that Engelhardt defends. They apparently did not believe that it was sufficient to point out that masturbation is “a deviation from an ideal of human perfection.”
Even though those who regarded masturbation as a disease were not content to point out that it was a normative defect, Engelhardt might still be right. Why shouldn’t someone who regards masturbation as a defect regard masturbators as sick, just as most Americans are inclined to regard necrophiliacs as sick? 3 If God or evolution designed our sexuality exclusively to lead us to seek intercourse with living members of the opposite sex, then there is a malfunction in those who masturbate or have homosexual encounters or have intercourse with animals or cadavers, just as there is a malfunction in those who prefer a meal of mouse droppings to a decent dinner. (But notice that this thought shifts from a view of disease as morally, prudentially, or aesthetically bad to a view of disease as malfunction.)
Evaluative theorists maintain that it is a conceptual truth that health matters to what people value (see, for example, Cooper 2002 ; Engelhardt 1974 ; Reznek 1987 ). Poor health is supposedly an automatic excuse for certain behavior, a justification for sympathy and the provision of care, and something that diminishes overall well-being. But these claims appear to be false. 4 For example, infertility in young adults is unquestionably pathological. It is a failure of the reproductive system to do what it is designed to do. It may justify medical treatment. Yet many people seek infertility, at least temporarily. Women who are reversibly infertile because they are taking birth-control pills (and by virtue of lacking normal capacities thus not fully healthy) or men who have had vasectomies after having fathered as many children as they want are typically not worse off all things considered. They do not have a condition requiring medical treatment or excusing behavior that would ordinarily be condemned, and their condition does not call for sympathy or care from others.
An evaluative theorist has three possible ways of conceding that apparently better health can be worse for a person. First, even if circumstances are such that better health in a particular regard has harmful consequences, it might still be better in other respects. Second, evaluative theorists might question whether the physical and mental states that people take to be healthy are, regardless of the circumstances, always in fact healthy. On this view, premenopausal women who are sexually active and want to avoid pregnancy are healthier if infertile, because infertility is better for them than fertility, while infertility is unhealthy in those premenopausal women in whom it is involuntary and unsought. A third possibility for the evaluative theorist is to maintain that it is a conceptual truth that states of better health are typically or usually better for people rather than invariably so. Cases in which it is better to be less healthy do not constitute counterexamples to these loose conceptual connections.
These three ways in which the evaluative theorist can meet the challenge posed by cases in which it seems that it is worse to be healthier, leave one wondering how substantial the disagreements between evaluative and nonevaluative views of health actually are. On the first alternative, it is a conceptual truth that setting aside their consequences (which may in unusual cases be harmful) states of better health are better for people. Most nonevaluative theorists agree that apart from unusual circumstances, better health is typically better. So the disagreement turns on whether it is a conceptual or contingent truth that health is a good thing. If evaluative theorists protect their claim in the second way by labeling physical and mental states that serve people’s purposes as states of better health regardless of the functional deficiencies they may involve, then it seems that the evaluative theorist is concerned with a different notion of health than the one that is employed in pathology and physiology. The disagreement collapses into an argument about how to use the word “health.” With the proper translation manual, it is questionable whether the evaluative theorist is asserting anything that the nonevaluative theorist denies. On the third alternative, it is also doubtful whether any important disagreement remains between evaluative and nonevaluative or naturalistic views of health. The evaluative theorist maintains that it is a conceptual truth that good health is generally good for people. The naturalist agrees that good health is generally good for people, but denies that this is a conceptual truth. What is at issue?
Perhaps the source of disagreement lies in the independent characterization of health that the naturalist provides and to which we shall now turn. Notice that evaluative views of health make it difficult to see how the term “health” can be used univocally to refer to states of people, animals, plants, or (more debatably) ecosystems. Health is usually a very good thing both intrinsically and instrumentally, and an evaluative view is defensible. But, as we have seen, to mount a successful defense of a conceptual connection between health and benefit requires some fancy footwork.
18.2. Naturalistic Views of Health
The leading nonevaluative “naturalistic” view of health is Christopher Boorse’s biostatistical view (1977, 1987, 1997; see also Wakefield 1992 and Hausman 2012a ). In Boorse’s view, a pathology obtains when the functioning of parts or processes of the body or mind is appreciably less efficient than what is statistically normal in the relevant reference class in typical environments. Boorse defends a goal-contribution view of functions, whereby the function of a part of a directively organized system consists of the contribution that the part makes to how well or how probably the system achieves its goals. A directively organized system is one that shows resilience in the pursuit of its goals, where that resilience is explained by the structure of the system. Central goals of human beings, like other living things, are survival and reproduction. These goals are not determined by moral or prudential considerations. They are instead enforced by evolution. The functions of parts of human beings are the contributions those parts make to survival or reproduction or to the achievement of narrower goals of particular subsystems to which the parts belong. The functioning of the parts of people is healthy when it is not much below the median level of functional efficiency in a typical environment for the relevant reference class. Reference classes are narrower than whole populations, because unimpaired capacities of male and female and of different age groups differ. Infertility is not pathological in seventy-year-old women, and men who are unable to breastfeed have no disease.
Figure 18.1 , drawn by Boorse (1987 : 370 and 1997 : 8), 5 helps clarify the view. Although Boorse draws what looks roughly like a normal distribution, there is no reason why the distribution of functional efficiency should be symmetrical, single-peaked, or continuous. There might be a small number of discrete levels. Median functional efficiency (which in a skewed distribution could be less than or greater than the mode) defines what is statistically normal.
The Biostatistical Theory
Although the median in the distribution of levels of functional efficiency (in a typical environment) determines a benchmark, the distribution plays no further role in locating the line between pathological and healthy part function. Among the levels of functional efficiency that are lower than the median level, the level of functioning (as determined by the contribution the part makes to the goal-achievement of the systems to which the part belongs) determines whether functional efficiency is adequate and hence healthy or not. Functional efficiency that is “significantly” worse than the median level is pathological. Although functional efficiency is a matter of how well a part is functioning and is thus an evaluative notion, the standards of good functioning depend on a part’s contribution to the systems to which it belongs and ultimately to survival and reproduction. Considerations of well-being, aesthetics, and virtue are irrelevant.
In denying that there is any conceptual connection between health and well-being or other human values, naturalistic theories need not maintain that the relationship between health and well-being is solely instrumental. Health states may also be constituents of well-being, but whether certain levels of functional efficiency contribute to or constitute elements of well-being or other human values in specific environments is a separate question from their contribution to system goals and ultimately survival or reproduction.
18.3. Why Is It Better to Be Healthier?
What is it that makes it better to be healthier? To answer this question, more needs to be said about what it is to be healthier. This turns out to be trickier than it might at first appear, because pathology and health are multidimensional. One person may be in pain, another suffering a cognitive deficiency, a third unable to see. How are these different health states to be compared? To impose some order and to value these health states, health economists have constructed health state classifications and have then assigned values to the health states so classified. 6 Unlike someone’s health, which depends not just on her instantaneous physical and mental states, but on their trajectories through time, health economists take a person’s health state to be a snapshot at a moment, without reference to past or future. Just as the distance an object travels over an interval is the time integral of its instantaneous velocity, so a person’s health during a period is the time integral of the person’s health states. So, for example, the health state now of a woman with a symptomless cancer that will kill her in a few weeks could be little different from the health state of someone in full health. The fact that her health (as opposed to her instantaneous health state) is very poor shows up in her expected trajectory through increasingly terrible health states. Once one has classified the instantaneous health states, one can define people’s health in terms of actual or expected trajectories through these health states. The classification of health states is fundamental to this way of describing people’s health. For an example, the Health Utilities Index distinguishes eight “dimensions” of health: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain, and distinguishes five or six levels of severity of deficiencies along each dimension, for a total of 972,000 health states.
As health-classification systems such as the Health Utilities Index recognize, people’s health states are multidimensional. In this regard health states are analogous to consumption bundles in consumer choice theory. A person’s consumption bundle consists of quantities of fruits, fish, water, wine, haircuts, home heating, and so forth, and though one bundle of commodities and services may cost more than another or provide an individual with greater happiness, there is no way to say that one bundle of commodities is literally larger than another, apart from the special case of dominance in which one bundle contains at least as much of each commodity as another and more of some commodities. Although Mitt Romney is much richer than most readers of this volume and consumes a more expensive bundle of commodities, as a Mormon, his beer consumption is probably much lower than that of an average college student. The bundle of commodities he consumes is probably neither literally larger nor smaller than the bundles of commodities and services consumed by different readers of this essay.
Just as one person’s commodity bundle is often neither larger nor smaller than the commodity bundle of another, so it is frequently the case that one person has no larger or smaller quantity of health than another. One can compare how happy people are in various health states or what their median income is or how much on average they prefer one health state to another, but there is no way to say that Jack has literally more health than George, unless Jack’s health state dominates George’s—that is, unless Jack’s health state is no worse than George’s along any dimension and better along at least one dimension. It is tempting to suppose that one might make comparisons in terms of something like “overall functioning,” but this is an illusion. 7 How is one to judge whether Jack, who has a very limited short-term memory, is healthier than Jane, who needs a walker to get around, or Jessica, who is very hard of hearing? What evidence bears on this question?
The relation “is at least as healthy as” is massively incomplete : most health states cannot be compared in their quantity or magnitude of health. It is not just that we cannot tell: there is no truth condition for the claim that one set of functional deficiencies constitutes a greater quantity or magnitude of health than another, unless the former dominates the latter. There is no such thing as a quantity or magnitude of health, just as there is no such thing as the “size” of a commodity bundle.
But, of course, we compare people’s health all the time. If Jack is bedridden, senile, and deaf but has good vision, he seems to be clearly less healthy than George, who is color-blind, but otherwise healthy. Health comparisons such as this one are, I suggest, in fact comparisons of the value of different health states, of how good different health states are. When we say that one person is healthier than another, we usually mean that the first person’s health is better . Similarly, when we say that Mitt Romney has more goods than the typical steelworker, we mean that his goods are more expensive or that most people would gladly trade the steelworker’s bundle of commodities for Romney’s. Though one person rarely possesses literally more or less health than another, it is often the case that one person’s health is better or worse than another’s.
Rather than finding a basis for the value of health in clarifying the measure of health, we have found that there is no measure of health apart from its value. So we might as well ask directly: what is it for one person’s health to be better than another’s or for someone’s health to be better at one time than at another? One finds different answers in the literature. Norman Daniels cashes out the value of health in terms of opportunity (1985, 2007). In his view, someone’s health at t is better than their health at t ′ (or than someone else’s health at some time) if he or she has greater access to the normal opportunity range for someone of that age and sex in that social position and with those talents. Paul Dolan disagrees. He maintains that the value of a health state consists in the quality of subjective experience it involves ( Dolan and Kahneman 2008 ). John Broome (2002 : 94) and Dan Brock (2002 : 117) assert that how good someone’s health is is a matter of the contribution that their health makes to their well-being either as cause or component. The health measure in use in England and some other European countries takes the value of health to be a component of well-being, which health economists call “health-related quality of life.” In practice, health economists usually take one health state to be better than another if and only if people prefer the former to the latter, regardless of the reasons for the preference.
None of these views seems satisfactory. The value of health cannot be cashed out entirely in terms of opportunities. Subjective experience is also important, whether or not it affects opportunities. But opportunity and capacities are important: health cannot be measured entirely in terms of subjective experience either. Subjective experiences are often good indicators of our health—indeed one can conjecture that the evolutionary point of many of our feelings is precisely to indicate what states of our bodies are healthy or diseased. But if our evidence is faulty or we have nervous, cognitive, or affective disabilities, our subjective experience may be excellent when our health is poor. Those with congenital analgesia (an inability to feel pain) are not in better health than those who feel pain.
Nor does the measure of health consist in its bearing on well-being. People with disabilities such as deafness who have coped successfully with their disability may be as well off as people without any disabilities. Whether deafness is a disability does not depend on whether it diminishes the quality of life. It sounds more plausible to maintain that the value of health consists in health-related quality of life, but I suspect that this view appears to be more plausible mainly because it is unclear what health-related quality of life is. What would it mean to say of someone who is deaf and is living an excellent life that her “health-related quality of life” is worse than someone who can hear? As John Broome has argued (2002), there is no way to decompose someone’s well-being into some set of components, with a subset constituted or caused by the person’s health. For example, as Allotey and coauthors (2003) vividly document, the extent to which paraplegia diminishes the quality of life differs dramatically depending on whether one confronts social, natural, and technological circumstances like those in Australia or like those in Cameroon.
18.4. Preferences and the Value of Health
What about preferences? Do they enable health economists to value health states sensibly? Economists do not typically define what they mean by preferences, and when they do offer definitions, they often make indefensible claims that are inconsistent with their own practices. In Preference, Value, Choice and Welfare (2012), I argue that the interpretation of preferences that best fits the practice of economists takes preferences to be subjective total comparative evaluations. What this means is the following:
Preferences are subjective states that combine with beliefs to explain choices. They cannot be defined by behavior. Even in the simplest case in which Sally faces a choice between just two alternatives, x and y , one cannot infer that she prefers x over y from her choice of x without making assumptions about her beliefs. If Sally mistakenly believes that the choice is between x and some alternative other than y , then she might choose x from the set {x, y} despite preferring y to x .
Preferences are comparative evaluations . To prefer x to y is to judge how good x is in some regard as compared to y . To say that Sally prefers x is elliptical. If Sally prefers x , she must prefer x to something else.
Third, preferences are total comparative evaluations—that is, comparative evaluations with respect to every factor that the individual considers to be relevant. Unlike everyday language where people regard factors such as duties as competing with preferences in determining choices, economists take preferences to encompass every factor influencing choices other than beliefs and constraints.
Fourth, as total comparative evaluations , preferences are cognitively demanding. Like judgments, they may be well or poorly supported and correct or incorrect.
On this understanding of preferences, there are strong reasons to deny that one health state H is better than another, H ′, if and only if people prefer H to H ′. First, people might prefer H to H ′, despite believing that H ′ was a state of better health. For example, a manic-depressive may prefer not to treat her disease, because of what she is able to achieve during manic periods, without believing that she is in better health when not medicated.
Health economists might respond that cases in which people judge that H ′ is a better health state than H but prefer H are unusual and may be ignored. Though not defining what it is for one health state to be better than another, perhaps preferences are reliable indicators of how good or bad health is. But it is questionable whether preferences are reliable indicators of health, because people’s preferences among health states are likely to be mistaken. When economists measure people’s preferences among flavors of ice cream or makes of cars, they are asking people for their comparative evaluations of alternatives that the respondents understand well, that they have had ample opportunity to consider, and concerning which they have a great deal of information. When, in contrast, health economists ask people to express their preferences among health states, they are asking people to appraise unfamiliar alternatives concerning which respondents typically have no secure preferences at all.
This concern about the reliability of survey respondent’s comparative evaluations is not just a theoretical qualm. Consider, for example, the “quality weights” that are assigned to health states as classified by the EQ-5D, a health classification system used in Europe, including by the National Institute for Health and Clinical Excellence in England (which uses these weights to determine whether treatments are sufficiently cost-effective to be paid for by the National Health Service). The EQ-5D has five dimensions along which health states vary: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Along each dimension, there are three levels: no problems, moderate problems, and severe problems. There are thus 3 5 , or 243 distinguishable health states, to which “quality weights” are assigned. Death is assigned a quality weight of zero, and 1 is assigned to full health—that is, to no problems along any of the five dimensions. Apart from a few health states that may be worse than death, health states have some value between zero and 1. To assign values or “quality weights,” members of the population are asked questions such as the following:
Suppose that you faced a choice between (a) ten years of life remaining in health state 11112 (that is, with no problems on any of the dimensions of health except for moderate anxiety/depression) or (b) eight years of life with no problems on any of the dimensions of health. Which would you prefer?
This is not a choice that people have previously faced. It is far from well defined. What constitutes a “moderate” problem of anxiety or depression? If one actually faced such a choice—perhaps if one were faced with a choice of whether to take an antianxiety drug that would shorten one’s life by two years—it would be an extremely important choice that would demand serious reflection. One would want to know more about how disabling the anxiety or the depression would be. Exactly what counts as “moderate” anxiety or depression? Would one still be able to work, to live independently? How would it affect one’s social life or one’s income? What sort of burdens would it impose on one’s family and friends? To make a serious total comparative evaluation of these two alternatives—eight years in full health versus ten years with moderate anxiety or depression—one would need to gather a great deal of information and deliberate with care.
In fact, when those surveyed are asked whether they would prefer eight years in full health to ten years with moderate anxiety, they answer in a few seconds. What cognitive processes enable them to give immediate answers to questions that are unfamiliar, not well defined, and extremely difficult? They are probably substituting some easier question for the incredibly difficult question they have been asked ( Kahneman 2011 ). Why should one take their answers as good measures of the value of health states? These problems with surveys have no easy solution. Rational survey respondents are never going to invest the effort that is required in order to have settled and well-supported preferences among alternatives such as these. 8
These reasons to deny that H is a better state of health than H ′ if and only if people prefer H to H ′ raise a further question: Why defer to the judgment of survey respondents concerning the values of health states rather than making the judgment oneself? Unable themselves to figure out how to value health states, health economists instead elicit the views of people whose off-the-cuff answers show that they have not grappled seriously with the problems.
So the proposal to measure the values of health states by preferences fares no better than the proposals to measure the values of health states by opportunity, feelings, or well-being. The preferences people express should not be taken seriously as comparative evaluations to which they are committed. One should also wonder why, when faced with the difficult problem of providing a comparative evaluation of the health states defined by the EQ-5D, health economists should rely on the judgments of laypeople who know less about the health states and have had less opportunity to think about them.
18.5. Do Health States Have Values?
Regardless of whether one holds an evaluative or a naturalistic view of health, there is a serious additional problem with the proposal to measure health in terms of the value of health. If two individuals are in the same physical and mental state, then their health is the same. If their health is the same, then any acceptable measure of their health must assign the same number to their health. If health is measured by its value, then if health states are the same, their value must be the same. But the same health state has different values for different people in different environments. Being unable to walk is a devastating blow if one lives in an impoverished swampy or mountainous country with few paved roads. Its impact on well-being or opportunity is far less serious in a wealthy country with wheelchair-accessible transportation and buildings. A strained tendon that most people would find trivial may cost a violinist her career. If, as these examples illustrate, the same health states often have different values, then their values cannot be measures of health. But it is only in terms of their values that health states are generally comparable. So it appears that health is not measurable at all!
There is a way out of this conundrum ( Hausman 2012b ). One can distinguish between token health states—that is the health state of a particular individual at a particular time and place—and kinds or types of health states. The argument above shows that the values of tokens of the same type differ depending on the environment and the values and interests of individuals. Rather than concluding that kinds of health states have no single value, one can instead assign to health state types either the average value of their tokens weighted by the frequency of different circumstances or the value of their tokens in some “standard” context.
If the value of token health states were uniformly extremely sensitive both to the environment and to individual interests, there would be little point to considering their weighted average or the token value in some standard context, because these would tell us little about the values of the actual token health states. Fortunately the values of many token health states are not widely dispersed. A broken toe is a very serious injury to some dancers and athletes, but it has much the same value to a large majority of the population. A migraine headache is pretty much just as miserable whether one is walking through a rainforest or skiing across frozen tundra, whether one is a doctor, a dogcatcher, or a dockworker. But it is questionable whether average or standard values will serve all the purposes for which health measures are designed.
If the values of health state types are the values of tokens in some “standard” environment or averages of the values of tokens, then our inquiry into the value of health leads us to inquire about what constitutes or determines the value of token health states. That value depends jointly on the “within-the-skin” functioning of parts and processes as described by some system of health state classification, on the individual’s specific environment—cultural, technological, biological, and geographical, and on the interests and values of the individual.
18.6. Valuing Token Health States
What makes a token health state better or worse? What constitutes its value? There are three main answers in the literature. Philosophers have argued that the value of health lies in its contribution to well-being, to opportunity, or to capability. Defenders of these three accounts take them as competing, but it is possible to regard the value of health as arising from some combination of its bearing on all three.
18.6.1. Health and Well-Being
Health obviously contributes to well-being, and minimal levels of health are a necessary condition to possessing a life worth living. Most health economists probably see the value of health as deriving from its contribution to well-being. Though they measure the value of health in terms of preferences, they implicitly take greater preference satisfaction to indicate greater well-being. Some philosophers such as Brock (2002) and Broome (2002) have also defended the view that the value of health lies in its bearing on well-being.
Yet, as already argued, health does not always contribute to well-being. Health improvements are not necessarily improvements in well-being both because of perverse environments such as wars, which may reward health deficiencies, and because certain disabilities, such as deafness, need not limit an individual’s overall prospects of living well, despite limiting the variety of good lives that are open to them.
There are two responses to these objections. First, those who find the value of health in its contribution to well-being might argue that even if overall well-being is not necessarily lowered by poor health, the health-related aspect of well-being—the “health-related quality of life”—is diminished. This response seems merely to paper over the difficulty without seriously addressing it. Second, one might concede that poor health does not always diminish well-being, while insisting that it typically does, and that one is consequently justified in measuring the value of a health state by its bearing on well-being.
It is sensible to maintain that better health generally improves well-being, but health has value even when it does not promote well-being. Even if losing one’s hearing does not make one worse off, it is a loss of something of value. A further problem with locating the value of health in its contribution to well-being is that it is no easier to understand or measure well-being than it is to understand or measure health. For the same reasons that one cannot identify the value of health with the quality of mental states, one cannot identify well-being with the quality of mental states. For many of the same reasons that preference satisfaction does not constitute health, it does not constitute well-being either. Like health, well-being is multidimensional, and assigning a scalar measure (for example, in terms of preferences or subjective experience) is problematic.
At the end of the day, one can still say that it is usually the case that those whose health is better are, other things being equal, better off, and if their health is much better, then, other things being equal, they are usually much better off. But these platitudes are not very informative.
18.6.2. Health and Opportunity
As Norman Daniels has argued, health is critical for opportunity. Indeed one way to understand how impairments such as deafness, blindness, or paraplegia can count as disabilities, even when they do not diminish well-being, is to point out their consequences for opportunity. Regardless of the social accommodations society may provide, those who are blind cannot be bus drivers and those who cannot walk cannot be Navy Seals.
The value of health is not exclusively a matter of the bearing of health on occupational opportunities, and Daniels never intended to make such a claim. He uses “opportunity” in a broader sense as the range of valuable activities and experiences available to individuals. Even though poor health may not limit the occupational opportunities of someone who is past a mandatory retirement age, it may limit her opportunities for social interactions, recreation, or enjoyment.
One could stretch the notion of opportunity still further than Daniels does, so that physical or mental states that do not limit activities also count as limiting opportunities, such as opportunities to be free of pain, to avoid anxiety, or to have normal sensory or cognitive functioning. Unless we are to stretch opportunity all the way to include these, Daniels’s account of the value of health will not be adequate. Bouts of pain constitute health deficits regardless of whether they affect opportunities for activities. But if (unlike Daniels) one stretches opportunity so as to include opportunities not to be in pain, then the account is uninformative. It says that health states are bad insofar as they involve subnormal part functioning—that is to say that health states are bad insofar as they are unhealthy.
18.6.3. Health and Capability
Amartya Sen’s proposal (1992, 1993; Robeyns 2005 ) to conceptualize what is of value to human beings in terms of various kinds of functioning (which he takes to be activities as well as states of affairs) and in terms of capabilities (which he takes to be sets of functionings that are available to people) has had a significant influence on contemporary thinking concerning health and its value. Health is one of the ten central human capabilities that Martha Nussbaum identifies (2000). Jennifer Prah Ruger argues that what is of value is not just health but “health capability,” which consists of both health and the capability to pursue health (2010). Sridhar Venkatapuram (2011) argues that health is a “meta-capability”—a capability to acquire other capabilities—and that its value derives from the value of those capabilities, which is in part a matter of freedom and in part a matter of the value of the functionings that the capabilities make possible. Without using the language of capabilities, I have argued elsewhere that the value of health states depends jointly on the feelings they entail and on the activities they permit ( Hausman 2010 ).
Unlike the claims that the value of health states consists in their bearing on well-being or in their consequences for opportunity, the claim that the value of health states depends on the capabilities they imply or, in my variant ( Hausman, 2015 ), on the feelings and activity limitations they involve seems to be true. But one may reasonably question whether it is useful. Sen offers no way to evaluate functionings or capabilities except when capability sets are nested or all relevant evaluative criteria point in the same direction. Indeed he is skeptical about both the possibility and the desirability of scalar measures, which he believes lead people to overlook the complexities of evaluating ways of being and acting. Such skepticism is reasonable, and it may be that the best answer to the question “What is the value of health?” is to insist that health has many different values for different people in different circumstances. But Sen’s skepticism does not respond to the practical need for measures that will help identify the diseases and risks that most diminish health or that will guide the allocation of health-related resources. That practical need does not demand a single context-independent measure of health, but it does demand some function from contexts to health state values, and Sen is skeptical about even such a context-sensitive measure.
18.7. Conclusions
The thrust of this discussion should be discouraging to those, like the staff at the Institute for Health Metrics and Evaluation, who seek to generate summary measures of population health and to measure the burden of different diseases, accidents, and risk factors. It is similarly unhelpful to others, like those at the National Institute for Health and Clinical Excellence in England, who need a scalar measure of the health benefits of alternative treatments in order to determine their cost effectiveness. But Sen has good reason to be skeptical of scalar measures of capabilities because all of the existing systems that purport to measure health or the burden of disease have serious flaws.
The questions that the Institute for Health Metrics and Evaluation address are important and real: how large a contribution to ill health do different diseases, injuries, and risk factors make? Without a scalar measure of health, one can only look at rough indicators, such as the contribution different diseases make to premature mortality. Similarly, within the constraints set by considerations of fairness, if the United Kingdom wants to allocate healthcare resources so as to improve health as much as possible, it apparently needs a scalar measure of health.
What is needed for health measurement or scalar evaluation is unfortunately not necessarily forthcoming. There is no good way to put the many values of different health states on a single scale that will serve all the purposes for which a generic health measure is intended. Those concerned to measure health have to make do with rough indicators of the values of health states.
Philosophers who are not concerned to measure health need not be discouraged by the incompleteness of health comparisons or the difficulties of locating health states along some single scale. If the concern is to understand the values of health rather than to measure health, no scalar unit is required. Neither is there any need for complete comparisons. Health states differ in many ways and have different values. Some health states may have aesthetic values. Consider upright posture or a clear speaking voice. The values of some states of mental health are akin to the values of traditional virtues such as courage or moderation. Other health deficiencies, both physical and mental, are unpleasant in a variety of ways. Others undermine the possibilities of undertaking various activities or pursuing certain objectives. These variegated values are real and palpable, even if there is no good way to put them all on any single scale.
Acknowledgments
I have had a great deal of help thinking through the issues in this chapter from many people over a long period of time. I am particularly indebted to Andrew Altman, Christopher Boorse, Dan Brock, Norm Fost, Paul Kelleher, Elselijn Kingma, Peter Schwartz, Russ Shafer-Landau, Alan Sidelle, and Reuben Stern.
That is Dominic Murphy’s view. He assumes that everyone concedes that part of what defines a disease is harm (2009) and that the debate between “objectivists” and “constructivists” (neither of whom accepts a naturalistic view) turns on whether objective malfunction is a necessary condition for the existence of disease or pathology.
By an “ordinary” environment, I mean to rule out environments like the Nazi wartime draft or the systematic slaughter of Jews, in which traits that usually enhance well-being and opportunity or that are irrelevant to them can be very harmful.
According to the fourth edition of Diagnostic and Statistical Manual of the American Psychiatric Association , necrophilia is not a mental disorder unless it causes distress to the individual or harm to others. Earlier versions of the DSM did classify it as a disorder. What constitutes a mental disorder is much more controversial than what constitutes a physical disorder. Some societies have approved of intercourse with the dead under certain circumstances.
One central desideratum for an account of the concept of health is that it conform to the judgments of pathologists and physiologists. Their judgments are, however, fallible, and some are more central and more firmly held than others. So an account of the concept of health may conflict with some of the claims physiologists or pathologists make. This essay does not document its uncontroversial claims about their views.
Boorse accidentally mislabels the axes.
The methods employed in the global burden of disease studies carried out by the World Health Organization (2000) and the Institute for Heath Metrics and Evaluation ( Murray et al. 2012–13 ) are somewhat different, but the differences are not material to the issues in this chapter.
One might resist this claim by arguing that fitness permits one to compare health states. But comparisons of fitness are not comparisons of health, if for no other reason than the much greater importance of reproduction to fitness than to health.
In addition there are systematic differences in the way individuals value health states, with those with experience of disabilities such as deafness judging them to be far less bad than those without those disabilities. So at least one of these groups has to be mistaken in their valuations. There is no good reason to believe that the values gleaned from preference surveys are correct.
Allotey, P. , D. Reidpath , A. Kouamé , and R. Cummins . ( 2003 ). “ The DALY, Context and the Determinants of the Severity of Disease: An Exploratory Comparison of Paraplegia in Australia and Cameroon. ” Social Science and Medicine 57: 949–58.
Google Scholar
American Psychiatric Association. ( 2000 ). Diagnostic and Statistical Manual of the American Psychiatric Association IV . Arlington, VA: American Psychiatric Association.
Google Preview
Boorse, C. ( 1977 ). “ Health as a Theoretical Concept. ” Philosophy of Science 44: 542–73.
Boorse, C. ( 1987 ). “Concepts of Health.” In D. VanDeVeer and T. Regan (eds.), Health Care Ethics: An Introduction. Philadelphia: Temple University Press, 359–93.
Boorse, C. ( 1997 ). “A Rebuttal on Health.” In J. M. Humber and R. F. Almeder (eds.), What Is Disease? Totowa, NJ: Humana Press, 1–134.
Brock, D. ( 2002 ). “The Separability of Health and Well-Being.” In C. Murray , J. Salomon , C. Mathers , and A. Lopez (eds.), Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications . Geneva: World Health Organization, 115–20.
Broome, J. ( 2002 ). “Measuring the Burden of Disease by Aggregating Well-Being.” In C. Murray , J. Salomon , C. Mathers , and A. Lopez (eds.), Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications . Geneva: World Health Organization, 91–113.
Cookson, R. ( 2005 ). “ QALYs and the Capability Approach. ” Health Economics 14: 817–829.
Cooper, R. ( 2002 ). “ Disease. ” Studies in History and Philosophy of Biological and Biomedical Science 33: 263–82.
Daniels, N. ( 1985 ). Just Health Care. Cambridge: Cambridge University Press.
Daniels, N. ( 2007 ). Just Health. Cambridge: Cambridge University Press.
Dolan, P. , and D. Kahneman . ( 2008 ). “ Interpretations of Utility and Their Implications for the Valuation of Health. ” Economic Journal 118: 215–34.
Engelhardt, H. T. ( 1974 ). “ The Disease of Masturbation: Values and the Concept of Disease. ” Bulletin of the History of Medicine 48: 234–48.
Hausman, D. ( 2010 ). “ Valuing Health: A New Proposal. ” Health Economics 19: 280–96.
Hausman, D. ( 2012 a). “ Health, Naturalism, and Functional Efficiency. ” Philosophy of Science 79: 519–41.
Hausman, D. ( 2012 b). “ Health, Well-Being and Measuring the Burden of Disease. ” Population Health Metrics 10: 1–7.
Hausman, D. ( 2012 c). Preference, Value, Choice and Welfare. Cambridge: Cambridge University Press.
Hausman, D. ( 2015 ). Valuing Health: Well-Being, Freedom, and Suffering. New York: Oxford University Press.
Kahneman, D. ( 2011 ). Thinking, Fast and Slow. New York: Farrar, Straus and Giroux.
Murray, C. , et al. ( 2012 –13). “ The Global Burden of Disease Study 2010. ” The Lancet 380 (9859): 2053–260.
Murphy, D. ( 2009 ). “Concepts of Disease and Health.” In E. N. Zalta (ed.), Stanford Encyclopedia of Philosophy , Summer 2009 ed. http://plato.stanford.edu/archives/sum2009/entries/health-disease/ .
Nordenfelt, L. ( 1987 ). On the Nature of Health: An Action-Theoretic Approach . Dordrecht: Reidel.
Nordenfelt, L. ( 2000 ). Action, Ability and Health: Essays in the Philosophy of Action and Welfare . Dordrecht: Kluwer.
Nussbaum, M. ( 2000 ). Women and Human Development: The Capabilities Approach. Cambridge: Cambridge University Press.
Prah Ruger, J. ( 2010 ). Health and Social Justice . Oxford: Oxford University Press.
Reznek, L. ( 1987 ). The Nature of Disease . London: Routledge and Kegan Paul.
Robeyns, I. ( 2005 ). “ The Capability Approach: A Theoretical Survey. ” Journal of Human Development 6: 93–114.
Ryff, C. , and B. Singer . ( 1998 ). “ The Contours of Positive Human Health. ” Psychological Inquiry 9: 1–28.
Sen, A. ( 1992 ). Inequality Reexamined . Oxford: Clarendon Press.
Sen, A. ( 1993 ). “Capability and Well-Being.” In M. Nussbaum and A. Sen (eds.), The Quality of Life . Oxford: Clarendon Press, 30–53.
Venkatapuram, S. ( 2011 ). Health Justice: An Argument from the Capabilities Approach . London: Polity Press.
Wakefield, J. ( 1992 ). “ The Concept of Mental Disorder: On the Boundary between Biological Facts and Social Values. ” American Psychologist 47: 373–88.
World Health Organization. ( 1948 ). “Preamble to the Constitution of the World Health Organization.” Official Records of the World Health Organization , no. 2. Geneva: World Health Organization.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Essay on Health Is Wealth
Students are often asked to write an essay on Health Is Wealth in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Health Is Wealth
Introduction.
Health is our most precious wealth. It’s a vital aspect of life, as it influences our ability to enjoy, work, and live happily.
The Importance of Health
Good health allows us to perform our tasks with energy and enthusiasm. It helps us stay active, both physically and mentally.
Health and Happiness
Health is the key to happiness. Without health, wealth or success doesn’t have much meaning.
In conclusion, health is wealth because it provides us the strength to achieve our dreams. So, let’s prioritize our health.
Also check:
- 10 Lines on Health Is Wealth
- Paragraph on Health Is Wealth
- Speech on Health Is Wealth
250 Words Essay on Health Is Wealth
Understanding the proverb: health is wealth.
The adage “Health is wealth” underscores the fundamental concept of prioritizing health above all else, including wealth. As college students, we often find ourselves caught in the whirlwind of academic pressures, forgetting the importance of maintaining good health.
Health as a Prerequisite for Success
Health is not merely the absence of disease but also a state of complete physical, mental, and social well-being. It is the cornerstone of a fulfilling life, enabling individuals to pursue their goals effectively. Without good health, even the wealthiest person cannot enjoy their riches. Conversely, a healthy person, despite having less wealth, can lead a more enjoyable and productive life.
The Interplay of Health and Wealth
While wealth can provide better healthcare facilities, the pursuit of wealth at the expense of health can lead to a vicious cycle of illnesses and medical bills. Thus, it’s crucial to strike a balance, securing wealth without compromising health.
Investing in Health
Investing in health is not just about regular exercise and a balanced diet; it also includes mental health care. This involves stress management, maintaining a positive outlook, and fostering healthy relationships. As students, we must be proactive about our health, integrating healthy habits into our daily routines.
In conclusion, the proverb “Health is wealth” serves as a reminder that health is the most significant wealth one can possess. It is an investment that yields lifelong returns, enabling us to lead a fulfilling life. Therefore, as we strive for academic and professional success, let’s not forget to invest in our health, our true wealth.
500 Words Essay on Health Is Wealth
Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. This comprehensive definition underlines the complex nature of health and its profound impact on our lives. The axiom “Health is Wealth” encapsulates this idea, emphasizing the intrinsic value of health over material wealth.
The Primacy of Health
The importance of health in our lives cannot be overstated. It is the foundation upon which all other aspects of our lives are built. Without good health, even the most significant achievements or wealth can lose their meaning. A healthy body is a fertile ground for a sound mind, enabling us to think clearly, perform tasks efficiently, and enjoy life to its fullest.
Health and Productivity
Good health directly correlates with productivity, an essential factor for economic prosperity. Healthy individuals contribute more effectively to their communities and workplaces, driving economic growth. On the contrary, poor health can lead to decreased productivity, increased healthcare costs, and a diminished quality of life. Thus, investing in health is akin to investing in wealth.
The Socio-Economic Dimensions of Health
Health is also a social determinant that can influence one’s socio-economic status. Individuals with poor health often face obstacles in education and employment, leading to a cycle of poverty and further health deterioration. Conversely, those with good health have better opportunities for upward mobility. Therefore, health and wealth are interdependent, each influencing the other.
Health, Lifestyle, and Choices
Health is not a static state but a dynamic process influenced by our lifestyle choices. Regular physical activity, balanced nutrition, adequate sleep, and stress management are key factors in maintaining good health. These healthy habits are an investment in our future, just as saving and investing money contribute to future wealth.
The Role of Public Health
Public health initiatives play a crucial role in promoting health and, by extension, wealth. They aim to prevent disease and promote health at a population level through policies, education, and interventions. Investment in public health not only saves lives but also contributes to economic stability by reducing healthcare costs and increasing productivity.
In conclusion, health is indeed wealth. It is the foundation of a fulfilling life and a thriving society. It influences our productivity, socio-economic status, and overall quality of life. By adopting healthy lifestyles and supporting public health initiatives, we can invest in our health, thereby creating wealth not just for ourselves, but for our communities and societies as well. As we navigate through the complexities of the 21st century, let us remember this timeless wisdom and strive to make health a priority in our personal lives and public policies.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Hawa Mahal
- Essay on Handlooms
- Essay on Guitar
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Global health and moral values
Sabina alkire.
a Global Equity Initiative, Harvard University, 1033 Massachusetts Avenue, Cambridge, MA 02138, USA
Lincoln Chen
Soon after assuming office on July 21, 2003, the new Director-General of WHO, Lee Jong-wook, announced plans to launch several global health initiatives: re-energising primary health care to achieve the Millennium Development Goals (MDGs), launching the ambitious 3 by 5 initiative to expand access to antiretroviral drug treatment to 3 million HIV-positive people by 2005, 1 , 2 and accelerating country-based action through strengthening human resources. A similar pattern of new global initiatives characterised the opening phase of the previous WHO administration led by Gro Harlem Brundtland, launching programmes such as Roll Back Malaria, Stop TB, tobacco control, polio eradication, and partnerships such as GAVI (Global Alliance for Vaccines and Immunization). 3
Ethics and moral values are invariably invoked to mobilise support for these global initiatives. Earlier on in May, 2003, Lee used the terms social justice and security in his address to the World Health Assembly. 2 On assuming office, he underscored that “global health work must be guided by an ethical vision”. Recently, he wrote: “Both technical excellence and political commitment have no value … unless they have an ethically sound purpose.” 1
If ethics are the foundation for global health initiatives, how should moral philosophy guide policy choices and shape the way such programmes are undertaken? In this essay we argue that clarity regarding morality underlying global health initiatives is important, both for why and how programmes should be undertaken. Common moral values might be used to justify new global programmes, suggesting that the programmes might be shaped differently depending on the morals espoused. A rights-based or equity approach, for example, would be expected to differ from a utilitarian or humanitarian approach. Also, an initiative is only partly justified by its moral expediency. Of critical importance are factors shaped by knowledge and by institutional interests. Moral soundness about why particular global programmes should be advanced may need to be balanced against the imperative of achieving consensus among people of many different moral views. Yet, as we argue in the conclusion, moral clarity—as well as knowledge and institutional interests—can usefully shape what, when, and how health initiatives should best proceed.
Schools of moral thought
To stimulate discussion, we have selected four major schools of moral values commonly used to justify global health initiatives: humanitarianism, utilitarianism, equity, and rights. We could have analysed other schools, but these four, we believe, encompass a good range of moral positions. There are, of course, both large and important variations within each school.
Humanitarianism: acting virtuously towards those in need
The appeal for charitable acts to meet pressing humanitarian needs is arguably the most common ethical basis for global health action. Humanitarianism can be a form of virtue ethics but it also often a humanistic response to evident social problems. The ethos of humanitarianism is embedded in nearly all religions. In a humanitarian approach, people respond to human suffering and realise human fulfilment by acting in a virtuous manner based on compassion, empathy, or altruism. The virtues might be specific or broad. Examples of specific acts are charitable tithing among Baptists or zakat (charitable donations) among Muslims. Broadly proscribed virtues encompass such human qualities as generosity, honesty, trustworthiness, integrity, and fairness. Among the wealthy, these virtues might be expressed as philanthropy, which often focuses on health. 4
Humanitarianism provides the primary ethical basis of voluntary action undertaken by non-governmental organisations (NGOs), and is also an important base of public support for official foreign aid. US president George Bush in announcing US$15 billion in assistance for HIV/AIDS control described the pledge as a “work of mercy”. Public opinion polls in the USA consistently show that alleviating world hunger and providing drinking water are worthy of foreign aid from the USA. Emphasis on voluntary generosity and self-expression (rather than on duties or obligations) gives humanitarianism a broad appeal to many social groups, corporations, and governments.
Contemporary appeals to people's humanitarian impulses focus on the giver: who a person becomes by acting well, and how a person realises a sense of accomplishment or fulfilment. There are dangers that those who are helped can be placed in a dependent position, treated as victims not agents. Also, the underlying societal rules and structures that generate the social ills are not necessarily addressed. This approach might be more relevant to humanitarian catastrophes than structural approaches that attempt to correct the root causes of social problems.
Utilitarianism: maximising aggregate subjective happiness
In a utilitarian framework, the value of health is determined by the subjective utility (happiness, pleasure, or desire satisfaction) that it creates for an individual. 5 Across all individuals in a society, the ideal state is one that maximises the aggregate utility. Health could be valued because it generates utility directly, or because good health is instrumental to other utility-generating states, including opulence, or both. Many contemporary health policies are based on a form of utilitarianism in which good health is valued as instrumental to maximising aggregate utility. For example, the WHO Commission on Macroeconomics and Health calculated the costs and benefits of burdens of disease and argued that investing in health would generate economic growth, thereby enhancing incomes and aggregate utility. 6
The utilitarian approach underscores important interconnections between health and other variables. It can show how improving the health of the deprived can be “in everybody's interest”—including the self-interest of people not inclined to altruism. Its difficulties, however, are several. First, the instrumental valuation of health demeans it as an intrinsically valued goal in all societies. Second, people's self-assessments do not necessarily match their observed health status. For example, the self-reported morbidity rates in the Indian state of Kerala, where life expectancy is 70–75 years, are significantly higher than in Bihar, where life expectancy is significantly lower; and self-reported morbidity in the USA is higher still. 7 Third, it is rather difficult, even theoretically, to aggregate very different kinds of utility together into a single entity. Finally, a utility-maximising approach is not directly sensitive to distributional concerns.
Equity: achieving a fairer distribution of health capabilities
Equity is a relational concept in which ethical assessments are—at least in part—based on distributional features of one or more variable. 8 Fortunately, considerable intellectual work has recently been done on health equity and social justice. 9 , 10
Building on the work of political philosopher John Rawls, Amartya Sen has addressed some key features of health equity. 11 First, he poses the question of “equity of what?” Should equity be evaluated with reference to health achievement or access to health care? Sen argues that equity in health should be assessed in terms of health capabilities and achievements rather than health-care activities. After all, health care is a human activity; what people actually value is the capability to attain good health. He further notes that equitable social processes should inform evaluations of equity in the health space. In some equity domains, such as gender, completely equal distribution of health achievement could be considered unfair because women—whose lifespan in the absence of gender discrimination exceeds that of men—should, under an equity framework, enjoy longer life expectancies.
An equity-based evaluation considers not only allocation of a fixed set of health resources, but also allocation of resources between health and other social objectives. Equitable approaches to health have carried considerable power in mobilising support for health components of international development. Striking disparities in health achievement and emotively powerful arguments of preventable suffering can animate the public and political leaders. An example is the recent call for public funds to expand antiretroviral treatment to HIV-positive people in poor countries. The disparity between the health of those with access to life-saving drugs and the avoidable deaths among all others evokes the moral imperative to alleviate preventable human suffering caused by the inequitable access to antiretroviral drug therapy.
Rights: fulfilling our obligations so others are dignified
Human rights in health are embedded in several UN declarations, and they have deep and wide moral bases. Legal formulations were created to specify what was argued in the 17th century to be an inalienable moral claim grounded in the ontological dignity of human beings. Human rights can be described as “things which are owed to man because of the very fact that he is man”. 12 Some human rights can be expressed in the space of capabilities—for example rights to health, or to inclusion. Yet rights also add to the capability perspective by invoking duties and obligations on the part of others. Because each human being is recognised as an “end”, human rights demand obligatory behaviour on the part of the state, firms, groups, and individuals. Obligations may be “perfect” (as enshrined in law) or “imperfect” (a general duty to do what one can to help). 13
Calls for a rights-based approach to global health have recently grown. Extensions of human rights to children and women both contain references to freedom from preventable suffering and freedom to exercise health choices. 14 , 15 The application of human rights to good health has drawn attention to the duties and obligations that people and institutions have towards human beings, viewed squarely as an “end” worthy of dignity. A human rights approach often assumes some health minimum that all people should be able to realise for human dignity. The challenge is to implement the corresponding “incomplete obligations” among communities, institutions, and states where good health depends upon resources, knowledge, technologies, and social action.
Knowledge and institutions
These ethical schools do not track precisely to any specific health initiative. None of the schools dominates any specific health action, and several schools are often relevant to any single initiative. At present, whether the 3 by 5 initiative was evaluated according to aggregate utility (increasing the utility of people with HIV/AIDS) or distributional equity (increasing the numbers of people in developing countries who are given antiretroviral treatment), human rights (for health care), or the need for humanitarianism (to alleviate the suffering of those with HIV/AIDS), in all cases action is morally imperative. Ensuring a minimal threshold of health might similarly fit well with humanitarianism and human rights, and equity and justice values will require action on behalf of the most disadvantaged. Beyond moral values, the selection of global health initiatives is shaped by other, often implicit but no less valid, factors. Among these are knowledge and institutions.
To a large degree, ethical assessments will rest not only on the ethical perspective chosen, but also on the information selected for examination. 16 The selection of information is shaped by political and scientific forces as well as by moral theories. Paul Farmer 17 has written eloquently about the selective scrutiny of information that shapes health action. Tuberculosis, especially multidrug-resistant tuberculosis, became recognised as a health crisis when it achieved rapid transmission in New York City. Yet tuberculosis—before, during, and after the New York crisis—kills 2 million people annually, most of whom are poor. Because of informational selectivity, tuberculosis is a silent crisis among the world's poor, invisible to the rich and powerful. Similarly, severe acute respiratory syndrome (SARS) achieved front-page news because of its lethal nature and the paralysing effect it had on global commerce. Yet, “SARS-like” health catastrophes take place daily in thousands of rural villages in low-income countries. These health problems likewise severely affect families and communities, who are invisible to better-off and protected communities.
Scientific knowledge provides the basis for research and development of health technologies, such as vaccines and drugs. Breakthroughs in health research raise moral challenges because they make feasible treatment for conditions that were hitherto incurable—for example, antiretroviral drugs for HIV. Morally, there is a big difference between inevitable human calamity and suffering that can be prevented by modern technology. Growing knowledge gaps between technological potentiality and health realities present huge ethical challenges. Contention is further fuelled if the gap is accentuated by commercial interest. Recent debates over affordable access to life-saving antiretroviral drugs have focused on the fairness of international regimes of intellectual property rights that are perceived to favour commerce over human health.
Global health, like other fields, has a cluster of institutional stakeholders. Governments and intergovernmental agencies like the UN and the World Bank are mandated to play technical, financial, and operational roles. Since health is a major component of the global economy, corporations have interests in profits as well as in protecting their public reputations. Civil society organisations have many roles, ranging from the direct delivery of services to advocacy on public policies. Institutions, like all actors, are endowed with certain capabilities and also seek to advance their bureaucratic, political, and financial agendas. One typical driver of organisational behaviour is to gain command over resources that can translate into more jobs, higher status, and more numerous activities. Tracking of financial flows in global health initiatives can help reveal institutional winners and losers.
Historical studies have examined these institutional motivations in global health. The work of the Rockefeller Foundation overseas, for example, was often linked to corporate interests and political propagation of capitalism. 18 In an excellent historical analysis of tuberculosis control in mid-20th century, Sunil Amrith postulated that the conduct of tuberculosis programmes was primarily shaped by the state of knowledge and the capabilities of global institutions. 19 Field research had shown that directly observed therapy (DOTS) was highly effective in curing tuberculosis in home-based settings. Endowed with new knowledge, yet limited by institutional capacity and scarce funding, WHO decided to pursue tuberculosis control through vertical programmes involving cadres of specifically tasked field workers rather than attempt to build holistic village-based primary services. The latter approach would have been far more demanding institutionally and financially.
Consensus and advocacy
A common usage of moral values is to mobilise public support. Sometimes, however, advocates of global health do not give an accurate representation of distinct ethical schools, simply because they want everyone to agree. Braveman and Groskins, 20 for example, argued that the concepts of equity and rights are essentially identical, and lead to similar strategies. Their aim seems to have been advocacy for certain types of health actions rather than for clarification of distinctive moral schools. De Cock 21 argued that a public health rather than a human rights approach should frame responses to HIV/AIDS in Africa, but again this analysis is based on a very narrow example of both ethical schools. We argue that clarity in thinking is essential, because different moral schools do indeed raise distinct considerations and it can be useful to evaluate these carefully. At the same time, the urge to seek consensus is also valid, and can be sought without either exaggerating differences, or claiming (inaccurately) that differences between moral schools do not exist.
A common usage of moral values is advocacy, often to rich and powerful leaders, institutions, and nation states with the goal of mobilising resources—finance, political will, human motivations—on behalf of particular health action.
But here we run into an apparent paradox: how can one use moral values as advocacy tools, when the moral schools are distinct, and when people argue passionately among them? In order to achieve the support, global health programmes also must build consensus among a diverse constituency of resource-holders as to the central value of the initiative. So when it comes to the language of why support for global health is important, we recognise, with Cass Sunstein, 22 the wisdom of seeking “incompletely theorized agreements” in the moral discourse surrounding global health. 23
In his 1994 Tanner Lectures in human values, Sunstein 22 argued that in some cases consensus can be achieved if participants refrain from elaborating their moral positions, because if they scrutinised these positions in depth, consensus could fracture. By contrast, he advocates an approach that “enlists silence, on certain basic questions, as a device for producing convergence despite disagreement, uncertainty, limits of time and capacity, and heterogeneity”. Sunstein's approach has the advantage of opening space for dialogue, exchange, and discussion, thereby promoting deliberative democracy, political accountability, and reason-giving. Incompletely theorised agreements satisfy diverse constituencies who might have very different reasons, including incompatible values, for supporting a particular activity.
There is a further point against requiring everyone to agree on only one ethical justification for global health. For not only might different approaches appeal to different groups, different people might also have distinct understandings of what the terms “rights”, “equity”, or “humanitarianism”, actually mean. After all, the support base of global health initiatives is diverse, ranging from heads of state to private-sector executives to religious leaders to activists from NGOs to opinion-setters and journalists. It is highly unlikely that these constituencies will share an identical understanding of ethical terms.
A global health initiative can receive emphatic support from people who do not necessarily agree on the ethical foundations for their support, and in fact may very clearly disagree with one another as to why a programme should proceed—ie, its ethical or metaphysical justification. Advocates of global health initiatives would thus do well to proceed with a general appeal to moral concepts such as social justice and compassion, and this generality belies prudence rather than a lack of moral rigour.
Moral clarity
Yet an eclectic appeal to moral values in order to garner support of global health initiatives is not to imply that distinctions among moral values are trivial. Beyond clarifying why an action is important, adopting a particular moral approach can influence health action in other deeply important ways.
First is the scope of health action. An example is the programmatic implication of pursuing access to health care versus equitable distribution of health outcomes. In the former case, the programme would invest heavily in building health clinics and outposts, and perhaps in increasing the ratio of medical personnel per citizen. This sounds very appealing until one recognises that a country may have many rural health outposts, and many doctors on salary role, but if these doctors do not turn up to work, and the outposts do not have adequate pharmaceutical supplies, the population's health outcomes might remain very poor. On the contrary, to achieve an equitable distribution of health outcomes it would be necessary to make sure that the investment in health care results in better health across the population. It would also then be necessary to address broader social determinants of health, such as that raised in Michael Marmot's 24 intriguing research on the under-recognised relation between socioeconomic inequality and health.
Second, different ethical schools (and different groups within them) may shape how global health programmes are undertaken. Charitable acts might treat people as passive recipients of generosity, whereas rights-based approaches would encourage “voice” and participation to strengthen the agency of people for achieving their inherent rights.
Third, advocacy might use moral values to advance a global health agenda—because they are effective in advancing a global agenda. To mobilise a compassionate response, a picture of a feeble, emaciated, and large-eyed child might be used to stir pity among donors. Such advertisements tend to view the poor as helpless victims, rather than people who could be empowered to care for themselves. Arguably, much harm has been done by such dehumanising advocacy techniques. Yet, it could be argued that such moral approaches are legitimate to use because they are more effective in evoking public support than other moral approaches.
When people speak of ethics, the contribution that most readily leaps to mind is motivational: that an appeal to moral values will motivate people to support a set of actions. Yet this is only one of the ways in which moral values can support global health initiatives, and is not necessarily the most powerful. Discussions on whether to frame the objective of global health initiatives in terms of access to health care, or capabilities for good health, or utility maximisation, help to clarify what global health initiatives seek to accomplish. Criteria such as efficiency, or equitable treatment for men and women, clarify which alternative actions to realise similar goals should be selected. Consideration of how health activities contribute to or block non-health objectives such as the support of agency, or the rights to self-determination, clarify the importance of how health initiatives are carried forward. Thus global health may be far easier to achieve if we pause to follow through different moral analyses and thereby clarify what, which, and how global health initiatives can best proceed.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
Student Essays
Essays-Paragraphs-Speeches
Essay on Health & Importance of Health for Students
Health is defined as the state of body physically and mentally sound. Health is the prime source of happiness and comfort.
List of Topics
Read Following Best written Essays on Topic Health, importance & benefits of maintaining good health in life. These short and long essays are quite helpful for children & students.
Essay on Health, Importance, Benefits For Children & Students
Good health is the key to success. It is something which is neither bought nor sold but maintained. One who is sick remains confined to the bed.
Someone has said that there are four layers of energies which gives us good health, they are physical energy, mental energy, emotional energy and spiritual energy.
Benefits & Importance of Good Health
Health is very important aspect of life. The physical and mental well being of a person plays an important role in the life of a person. The absence of disease in life makes man able to achieve desired aims and objectives.
Related Post: Paragraphs on Health is Wealth
One can work effectively when he enjoys good health. An unhealthy person can’t enjoy life, can’t ho out and can’t embrace the beauty of nature fully. Those who are healthy can work better and can excel in life. One who doesn’t have good health, he owns nothing.
There are numerous benefits of good health, only a healthy person can bounce back difficult experiences, can adapt to adversity, can achieve balance in life and can feel secure and safe.
How to Stay Healthy
To maintain good health one must go to bed early and wake up early. As it is said that early to bed, early to rise makes a man healthy, wealthy and wise. One who aspire to be healthy, he must adopt this law.
Regular exercise also help maintain good health. Exercise keeps body fit and makes man active and energetic. Jogging and walking are good forms of exercise.
One must eat balanced diet, hygienic food and keep oneself neat and clean. Cleanliness is the sign of good health. To enjoy a healthy life we must reduce the level of consumption of fast foods because fast foods are not good for health. Eat green leafy vegetables and fresh fruits to keep yourself healthy.
Those who smoke and drink excessively, they must reduce or quit smoking and drinking because these are injurious to health. In this modern period people have become more mechanized and are dependent on machines, they have become inactive and lazy. Physical activity is very for good health.
The surroundings and environment plays an important role in maintaining good health, one must keep the surroundings clean. Pollution free environment is the sole panacea of avoiding diseases.
Related Post: Health is Wealth Speech For Students
Many diseases are caused by environmental pollution therefore it is necessary to keep environment clean and hygiene before maintaining good health. Nowadays temperatures of earth is increasing due to green house gases, one must avoid being out during noon time specially in summer season because sun’s harmful rays can cause skin cancer and can damage skin. Specially keep children indoor while sun is hot.
Related Posts:
Reader Interactions
September 25, 2021 at 7:11 am
Wow, what an excellent note it is! I m really happy to see this writing formation really this writing is so easy to understand & so simple to explain really impressive. Well done❣️❣️
September 26, 2021 at 9:51 am
Thanks for appreciation!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Essay on Health
Life is all about the precious moments that we cherish, the memories that make us smile, the people we feel grateful for and the things that move our soul. The most precious things in life cannot be bought or sold, and are not tangible. Health is one of them. It is the most precious things in everyone’s life that cannot be bought but have a very diverse effect throughout the life of a person. Health is crucial component that decides the whole lifestyle of any individual. To focus more on effects of good and bad health, today we will discuss it in detail.
Short and Long Health Essay in English
Here, we are presenting long and short essays on Health in English for students under word limits of 100 – 150 Words, 200 – 250 words, and 500 – 600 words. This topic is useful for students of classes 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, and 12 in English. These provided essays on Health will help you to write effective essays, paragraphs, and speeches on this topic.
Health Essay 10 Lines (100 – 150 Words)
1) A good health is desire of every human on the earth.
2) Health plays a vital role in the lifestyle of human beings.
3) A good health is very necessary for a good lifestyle.
4) Eating nutritious foods that are rich in vitamins and minerals is essential for good health.
5) Regular physical activity is an important part of maintaining a good health.
6) Regular check-ups are important for early diagnosis and treatment of health problems.
7) A bad health can invite lots of physical, social and mental illness to a person.
8) Maintaining a good health should be on the priority of daily routine.
9) Bad addictions like smoking and drinking can greatly cause heart disease, and other health problems.
10) Health is something that we can’t buy with money; we have to work on it continuously.
Short Essay on Health (250 – 300 Words)
Introduction
Health is the most important thing we can possess. It determines how we interact with the world and enjoy our lives. Having a balanced diet, getting enough sleep and regular exercise, is an important part of living a healthy lifestyle. It is vital that we strive to keep our bodies and minds healthy.
Physical Health
Living a healthy lifestyle includes eating a balanced diet of fresh fruits and vegetables, lean meats or fish, complex carbohydrates and healthy fats. Eating a variety of foods helps ensure we are getting all the important vitamins and minerals our bodies need. Exercise is also essential for maintaining a healthy lifestyle. Getting out and enjoying activities such as walking, jogging, cycling, swimming or playing a sport is an excellent way to get our bodies moving and keep our minds active.
Mental Health
Mental health nowadays is more important than physical health. It is essential to have a good sense of emotional, psychological, and social well-being. Taking the time to key in to your feelings and how you are feeling inside is an important part of your mental health. Taking part in activities that help you relax such as yoga and meditation are great ways to help tune in to our mental health.
To be healthy requires taking a holistic approach to life. Eating a balanced diet, exercising regularly and having a positive outlook are essential components in creating a healthy and well-rounded lifestyle. Taking care of our physical, mental and social wellbeing helps ensure a peaceful and fulfilled life.
Long Essay on Health (500 Words)
Health is an integral part of our lives, and there could be no life on earth without health. It is usually accepted that health is not just about physical well-being but also about mental and emotional states. Health is therefore a holistic concept that encompasses all aspects of our lives.
Different Aspects of Health
When we talk about physical health, it largely stands for the absence of illnesses or disorders. It is characterised by a state of optimum growth, development and functioning of the body. Generally speaking, physical health is maintained through proper nutrition, exercise, and adequate rest.
Mental and emotional health refers to the ability of a person to think rationally, control their emotions and behaviour and cope with the regular demands of life. To sustain good mental and emotional health, it is essential to nurture healthy relationships, get enough sleep, have meaningful connections with people, and take part in activities that make us feel good.
How to achieve a good health?
In regard to health and wellbeing, there is a long list of daily activities we can do to make sure we stay healthy and well. A good nutrition is absolutely essential. This includes consuming a well-balanced diet that provides all the necessary macronutrients and micronutrients, eating fruits and vegetables, limiting processed foods, and drinking enough water. Engaging in physical activity is another key element of staying healthy and physically fit.
How to maintain Mental Health?
Adequate rest is also crucial for maintaining good health. Sleep is a prerequisite for good physical, emotional and mental health. Not getting enough rest leads to higher risk for a range of physical and mental health conditions. Fourthly, stress management is an important part of looking after our wellbeing. Taking time to rest, relax and paying attention to thoughts and feelings can help to manage stressful situations in life. Finally, looking after emotional health is important too. It is important to practice emotional intelligence, use emotional regulation skills and build awareness of one’s emotions.
How Bad Health Can Effect Human?
There are many diseases, illnesses, and disorders that affect individuals’ health. Illnesses such as diabetes, heart disease, cancer, and arthritis have become increasingly prevalent in recent decades. Additionally, mental health illnesses like depression, anxiety, PTSD, bipolar, and eating disorders can have negative impacts on one’s physical health as well. These illnesses and disorders can be prevented and managed to enhance our health and wellbeing. Prevention is the key to achieving and maintaining good health and it requires individuals to pay close attention to their lifestyle choices, physical activity, sleep and stress levels and overall mental wellbeing.
Health is a multidimensional concept in which all aspects of life play a role and it is therefore essential to strive for good health in all its aspects. Good physical health can be attained through proper nutrition, exercise and adequate rest, while good mental and emotional health is sustained through managing stress, nurturing and sustaining healthy relationships, and engaging in activities that make us feel good.
I hope the above provided essay on Health will be helpful for you to know the benefits of having a good health.
FAQs: Frequently Asked Questions on Health
Ans. A healthy diet can help to improve your overall physical and mental health, maintain a healthy weight, reduce your risk of chronic diseases, provide essential vitamins and minerals, including long-term benefits to body and mind.
Ans. It is important to maintain an active lifestyle for your overall health and well-being. Regular physical activity can help reduce the risk of several diseases.
Ans. The best way to reduce your risk of getting sick is to practice good hygiene, including washing your hands frequently with soap and water; avoid close contact with sick people; and stay home when not feeling well.
Ans. Good mental health is important for your overall wellbeing. There are a number of steps you can take to maintain good mental health; including getting enough sleep, managing stress, and engaging in positive activities, such as physical activity and spending time with loved ones.
Related Posts
Essay on digital india, cashless india essay, essay on child is father of the man, essay on causes, effects and prevention of corona virus, essay on dr. sarvepalli radhakrishnan, durga puja essay, essay on summer vacation, essay on my plans for summer vacation, essay on holiday.

Essay on Importance of Health – Tips for Healthy Lifestyle
Essay on Importance of Health – Health is defined as a state of complete mental and physical well-being. It may also be defined as the ability to adjust physical, mental, and social challenges throughout our life.
As Health and Wellness is a very wide topic and we are not able, to sum up, everything in one article, so, we are trying to give you an idea on Importance of Health in our day to day life as a student point of view.
Table of Contents

100 Words Essay on Importance of Health

Maintaining good health is one of the best practices as it gives us a feeling of complete physical, mental and social well-being. Living a healthy lifestyle can prevent long-term illnesses like such as Asthma, Diabetes, heart diseases, and many more.
It provides us freedom from almost all diseases. It is very necessary for all of us to maintain a healthy lifestyle in order to be fit and fearless of diseases. We must eat healthy food and do regular physical exercises to stay fit always. Being healthy brings happiness to our lives and helps us to live a stress-free and disease-free life.
200 Words Essay on Importance of Health
According to the World Health Organisation, better health is the reason behind human happiness and well-being. It also contributes to the economic progress of the world as healthy populations are more productive and live longer.
There are so many different factors that influence the health status of a person. Some of them are discussed below.
Regular physical exercise and a balanced diet is the only way to stay fit & healthy. It reduces the risk of Heart Attack and Type 2 Diabetes. Moreover, to have strong bones and muscles, physical activity is a must-needed thing.
We must maintain a healthy weight in order to stay fit. By doing this, we can reduce the risk of stroke, heart disease, and anemia among many others. It also helps us in controlling non-insulin-dependent diabetes and increasing our energy levels along with optimizing our immune system.
We must get enough sleep in order to stay healthy and fit. Most of us need daily 7 to 8 hours of sound sleep to keep our health and minds healthy. It has a strong effect on our ability to think and work in our lives. Getting sufficient time of quality sleep at the right times helps us to protect our both physical and mental health.
Wildlife Conservation Essay
Long Essay on Importance of Health

Joyce Meyer said, “I believe that the greatest gift you can give to your family and the world is a healthy you”.
If a person stays healthy physically, he will stay healthy mentally too. Physical and mental health is linked fundamentally. If we are able to keep our bodies fit and healthy by taking the right food and doing physical activities regularly, our bodies will definitely help us to deal with daily stress.
Our body cells are made up of a variety of chemical substances and they move from place to place. Moreover, there are lots of other activities are happening in our body, for which, our body needs lots of energy and raw material. For the well-functioning of our cells and tissues, food is necessary.
For living a healthy lifestyle, good nutrition is one of the best things we should make habit of. If we combine good nutrition with regular physical activities, we are able to maintain a healthy weight which may reduce our risk of chronic diseases like heart disease and cancer. Below are some of the possible ways to do things right to have good health.
Eating and drinking the right things – Eating and drinking the right things can make our health better. Though it is not an easy task to keep a healthy diet in this world of Junk Food, we must maintain a balance in our diet of each food group.
Our balanced diet must include carbohydrates, protein from non-dairy sources, fruit, vegetables, etc. A balanced diet includes the right drinks also as our body needs to stay hydrated to keep ourselves healthy. We must avoid caffeine and sugary drinks as they can cause mood swings and affect our energy levels.
Along with good eating & drinking habits, physical activity & exercise can improve our health and reduce the risk of several diseases like Type 2 diabetes and cardiovascular disease, etc. Regular physical activity can boost our endurance and improve our muscle strength. It also stimulates our health and increases our feelings of happiness and calm.
Final Words – In this “Essay on Importance of Health”, we tried to cover the things like, what are the importance of Health in our life, how to maintain a healthy lifestyle, etc.
Though it is a very general topic, and covering each and everything related to Health and Fitness is next to impossible in a single article, we tried our best to cover as much as we can from a student’s point of view.
Essay on Wildlife Conservation: From 50 Words to Long Essay
Essay on Environmental Protection: 100 to 500 Words Long
1 thought on “Essay on Importance of Health – Tips for Healthy Lifestyle”
හොඳයි. දැනුම ගොඩක් වර්ධනය වුණා. ඉදිරියටත් මේ වගේ essays පල කරන්න. Thank you!!!!
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
- EssayBasics.com
- Pay For Essay
- Write My Essay
- Homework Writing Help
- Essay Editing Service
- Thesis Writing Help
- Write My College Essay
- Do My Essay
- Term Paper Writing Service
- Coursework Writing Service
- Write My Research Paper
- Assignment Writing Help
- Essay Writing Help
- Call Now! (USA) Login Order now
- EssayBasics.com Call Now! (USA) Order now
- Writing Guides
Importance Of Good Health (Essay Sample)
The importance of good health.
Good health is crucial to everything we do in our everyday lives. The importance of good health can be clearly seen in how we function as human beings in the daily tasks that define our functionality in the society. Without good health, we are not able to reach our individual potentials and this can hinder us from achieving our personal goals in the social environment that we exist in.
True enough, defining good health moves beyond the physical sense; it also includes emotional and mental. Good health means the different aspects of well-being which are mold together. For one individual to function properly, he or she should be physically fit, as well as emotionally and mentally. Having one missing aspect in an individual’s health can have heavy implications for an individual.
In both home and work, health is also required in building social relationships. If we are unfit to build these connections, it can imply that we are depriving ourselves of social stimulation that can help in improving our outlook and disposition in everything we do. In most cases, it can be said that good health can be equated to an individual’s self-actualization. An individual who is actualized has a nurtured sense of disposition in the society which makes him or her energetic enough to be able to face different problems that may arise during the day.
At home, good health can be a collective concept for it is also crucial to the well-being of the good family. This means that healthy relationships are required in order for families to function as a single organ. Without health, relationships may fall apart and this can bring both short term and long term damages to how we perceive life.
In professional spaces, health is crucial in dealing with different workplace situations and conflicts. If one is unfit in any of the mentioned aspects above, this can heavily affect how an individual becomes productive in the workplace. Of course, good health can be equated to productivity in this context and without it, more conflicts may arise that may be very hard to deal with.
To achieve good health, we as individuals should know the proper steps in nurturing ourselves. We need to be able to take care of ourselves in order to also know how to take care of others around us. Knowing to take the right meals, eat healthy food, drink the proper amount of water and get the right hours of sleep are the basic things that we need to master. What comes after these are more self-conscious steps that can then nourish our mental health; this includes engaging in healthy discussions with other people as well as lively and productive conversations that nurture positivity instead of negativity. We must also know to surround ourselves with the right people so that we can continue living a live with less worry. Emotional health is also a crucial part in us, as individuals. This is heavily influenced by our social relationships as well as our perception of our own selves. The key in ensuring emotional health is to always gauge our feelings and knowing how to deal with it properly. If our own selves are not capable of ensuring all these, seeking our family, friends and even professionals for help is always an option. The worst thing that we can do is to deprive ourselves of good health. Good health is not a myth; it is something that we can rally achieve as long as we put our minds in it and as long as we remember how to properly value ourselves. All it takes is the right perception of our self-worth and some self-esteem.

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 March 2020
A philosophy of health: life as reality, health as a universal value
- Julian M. Saad ORCID: orcid.org/0000-0002-9323-1021 1 &
- James O. Prochaska 1
Palgrave Communications volume 6 , Article number: 45 ( 2020 ) Cite this article
42k Accesses
3 Citations
5 Altmetric
Metrics details
- Health humanities
- Medical humanities
Emphases on biomarkers (e.g. when making diagnoses) and pharmaceutical/drug methods (e.g. when researching/disseminating population level interventions) in primary care evidence philosophies of health (and healthcare) that reduce health to the biological level. However, with chronic diseases being responsible for the majority of all cause deaths and being strongly linked to health behavior and lifestyle; predominantly biological views are becoming increasingly insufficient when discussing this health crisis. A philosophy that integrates biological, behavioral, and social determinants of health could benefit multidisciplinary discussions of healthy publics. This manuscript introduces a Philosophy of Health by presenting its first five principles of health. The philosophy creates parallels among biological immunity, health behavior change, social change by proposing that two general functions— precision and variation —impact population health at biological, behavioral, and social levels. This higher-level of abstraction is used to conclude that integrating functions, rather than separated (biological) structures drive healthy publics. A Philosophy of Health provides a framework that can integrate existing theories, models, concepts, and constructs.
Similar content being viewed by others

A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions
Julian Packheiser, Helena Hartmann, … Frédéric Michon

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers
Joseph M. Rootman, Pamela Kryskow, … Zach Walsh

Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls
Joseph M. Rootman, Maggie Kiraga, … Zach Walsh
A philosophy of health
What is health? Is it a state of the body or the mind? Is health primarily a natural, biological state or a holistic, value-laden state? Naturalistic and holistic philosophies of health have provided very important, but very different, perspectives of population health. Naturalistic views (e.g. as seen in Boorse, 1997 ) provide insight into physical, natural, biological, or physiological processes that are tangible (in the material sense), observable, and measurable with modern technology. Complementarily, holistic views contend that value-laden phenomena (e.g. vital goals, meaning, and purpose) play a central role in population health (Nordenfeldt, 2007 ).
A dialog, or as we see it, an important dialectic among naturalistic and holistic perspectives plays out between the Biostatistical Theory of Health (BST) and the Holistic Theory of Health (HTH). The BST posits that a person is healthy if and only if, all natural organs function normally given a statistically normal environment (Boorse, 1997 ). The HTH posits that a person is healthy if and only if (given standard circumstances) he/she has the ability to attain their vital goals (Nordenfeldt, 2007 ).
In addition to defining health, each philosophy defines disease. The BST poses that disease is the internal state of impairment to the normal functioning of organs (Boorse, 1997 ). In the HTH, an organ dysfunction is a disease if and only if the organ’s process reduces the person’s ability to pursue vital goals or life-purpose (Nordenfelt, 2007 ). In BST health is the absence of disease; and in HTH, health is not the absence of biological disease, but is the whole person’s ability to function in relation to vital goals.
Both naturalistic and holistic perspectives guide important observations of health and disease. When one considers health through the BST one pays close attention to the functions of the internal, biological functioning of the human being. When one considers health through the HTH, one pays close attention to the functioning of an individual, in relation to their external, societal/cultural functions. Is there a hybrid model that accounts for both internal and external functioning?
Wakefield’s ( 2014 ) harmful dysfunction analysis (HDA) creates a hybrid model that integrates natural- and value-laden phenomena when conceptualizing disease. HDA asserts that a person suffers from a disorder/disease if (1) the condition causes harm (as judged by the standards of the person’s culture); or if (2) the person’s internal, natural processes cannot perform normal functioning (as judged by the standards set by evolution). HDA creates a hybrid model that can integrate perspectives of the BST (i.e. by considering internal organ functioning); and the HTH (i.e. by considering external societal/goal functioning). However, while HDA may define health processes in relation to disease, it serves primarily as an integrative model of disease . Is there an integrative model of health that can account for natural and value-laden functions?
Schroeder ( 2012 ) identifies a significant, common thread among these competing (or perhaps complementing) philosophies: functionalism . The researcher suggests that each philosophy is concerned with the functioning of organisms. Although the BST, HTH, and the HDA might not agree on which functions inform the first principles of health, Schroder ( 2012 ) uses higher-level abstraction to identify one common first principle: the state of functioning in an organism impacts its state of health . When paralleling the three philosophies based upon functioning one might observe that (1) BST declares an individual healthy if its organs function normally; (2) HTH declares an individual healthy if he/she can function in relation to vital goals; and (3) HDA declares an individual unhealthy if internal mechanisms cannot perform natural, evolutionary functions, and/or when a condition prevents a person from functioning in relation to goals/norms/values. Through this higher-level abstraction, an integration of seemingly separate philosophies of health is made possible.
Learning from leaders in the field
As we attend to these philosophies of health, we too observe how discussions about functions and functioning produce integrative perspectives. Although a definition of “function” is not explicitly stated in the above research, it appears that Nordenfeldt ( 2007 ), Boorse ( 1997 ), Wakefield ( 2014 ), and Schroeder ( 2012 ) are each discussing functions as pre-existent (i.e. either from evolution, personal goal-setting, cultural tradition) processes - with - purposes . Whether one is describing a value-laden function (e.g. decision-making in pursuit of a valuable career) or an evolutionary-biological function (e.g. the heart beating for circulation), each process (i.e. decision-making processes or cardiac processes) serves identifiable purposes (e.g. maintained financial stability or maintained blood flow). Whether an organ is functioning normally in relation to the body or a human being is functioning in relation to vital goals, it appears that both perspectives consider if an active “process” (i.e. an organ’s activity, an individual’s activity) can express its “purpose” (i.e. evolutionary-purpose, life-purpose).
In the present manuscript we will propose that naturalistic and holistic perspectives can be integrated within a single philosophy of health. We will propose two universal functions—termed precision and variation —that can account for both natural functions and value-laden functions of the existing philosophies. This functional language will support a higher level of abstraction that integrates, rather than separates, biological functions, behavioral functions, and social functions under A Philosophy of Health.
The need for new perspectives in population health
The chronic disease crisis beckons the need for an updated philosophy of health that can account for biological, behavioral, and social functioning. Why? Chronic diseases, which account for 60% of all-cause deaths worldwide (Chartier and Cawthorpe, 2016 ), do not emerge from naturalistic, biological, or physical contact with an illness. Rather, chronic diseases do emerge in biological functions (e.g. tumor proliferation in an organ) after prolonged contact with health risk behaviors and lifestyle factors that active the conditions (Mokdad et al., 2018 ; Edington, 2009 ; Li et al., 2018 ). Chronic diseases are not curable by purely naturalistic or biological means (e.g. pharmaceuticals). Rather, some diseases may be effectively prevented or intervened on through healthy behavior (Dansinger et al., 2005 ; Daubenmier et al., 2007 ).
Population health risk behaviors are unique determinants of population health because researchers can actively observe how they simultaneously alter biological functioning (e.g. chronic smoking alters cells in lung tissue), behavioral functioning (e.g. chronic smoking alters decision-making and daily habits) and social functioning (e.g. chronic smoking creates an economic, social, and healthcare burden) of the population. These behaviors not only have biological, behavioral, and social implications for the individual doing the behavior, but also have intergenerational and interpersonal effects. The individual who binges on refined sugar not only puts themselves at risk of diabetes, but can put their future offspring at risk. The individual who smokes two packs of cigarettes per day not only puts themselves at risk of lung cancer, but can put their housemates at risk of lung cancer from second-hand smoke. Therefore, the chronic disease crisis is neither purely naturalistic, nor purely value-laden; rather it reflects an integration of natural and value-laden phenomena. There remains a real need for principles of health that can integrate existing naturalistic and holistic perspectives of population health.
The principles
Since April 7, 1948, the Constitution of the World Health Organization ( 2010 ) has utilized an intuitive definition of health by suggesting that health is “a state of complete physical, mental, and social well-being.” While this definition might be intuitive and even accessible to a wide audience; the defininition is not necessarily researchable across health disciplines. Integrating principles of health might begin with a common-sense definition of health that can also be upheld across existing naturalistic and holistic perspectives. Without operationally defining functions that drive physical, mental, and social well-being, it is a challenge for multidisciplinary collaborators to unite under the WHO mission. Further, without a common definition of health, important communications from patients to doctors, from subjects to researchers, from researchers to collaborators, and from peer-reviewers to peer-reviewees, can become fragmented or lost in translation. In the proceeding sections, a common-sense definition of health is used to present the first principles of A Philosophy of Health.
Principle 1: “Health” is the state of maintainable-ease of functioning . A “disease” is a state of prolonged-dysfunction that prevents ease
Chronic diseases emerge from prolonged exposure to dysfunctional behaviors like smoking, alcohol abuse, unhealthy diet, and inactivity (Mokdad et al., 2018 ) that also create dysfunctional expressions of life functions. Smoking creates dysfunctional breathing; alcohol abuse creates dysfunctional drinking; sugar binging creates dysfunctional eating; and sedentary behavior creates dysfunctional moving. When these health risk behaviors lead to chronic disease, they have already prolonged dysfunctional breathing, drinking, eating, and/or moving.
The chronic smoker breathes in smoke so frequently that he no longer experiences an ease-of-breathing. Rather, his breathing becomes short and shallow. Prior to the emergence of lung tumors, the chronic smoker prolongs dysfunctional patterns of breathing. The “couch potato” sits so frequently that he no longer experiences an ease-of-movement. Rather his movement becomes rigid and limited. Prior to the emergence of cardiovascular dysfunction or obesity, the sedentary person prolongs dysfunctional patterns of movement.
If chronic smoking facilitates prolonged-dysfunction in breathing, and sedentary behavior facilitates prolonged-dysfunction in movement, what do functional breathing and moving look like? Healthy breathing and moving (as well as eating and drinking) are characteristic of an ease of one’s functioning that can be maintained in normal conditions. For example, the chronic smoker and the “couch potato” might report momentary-ease in breathing and posture when engaging in their health risk behaviors; but they do not maintain that ease outside of smoking or sitting. Conversely, the yogi might report that their yoga practices expose them to momentary dis-ease in breathing and moving that lead to maintainable-ease in breathing and movement in everyday life. In contrast to disease as a prolonged-dysfunction, healthy functioning can be commonly sensed as a maintainable - ease of functioning .
When observing a disease, perhaps we are observing a prolonged-dysfunction that prevents ease. Rather than define health as the absence of disease (as seen in BST), notice here how we instead define disease in relation to health; and we define health in relation to maintainability , ease , and functioning . Consideration of “maintainable-ease of functioning” will allow us to consider how not all “dis-ease” is bad (i.e. exposure to acute dis-ease/stress maintains healthy functioning in the long-term); and not all “ease” is good (i.e. avoidance of stress and prolonged “comfort” creates fragility seen in sedentary behavior). We propose that:
Dysfunction parallels a state of “dis-ease”; and prolonged -dysfunction parallels the state of Disease.
Function parallels a state of “ease”; and maintainable-ease of functioning parallels the state of Health.
This definition of health will be applied in the proceeding principles to integrate naturalistic and holistic perspectives of population health.
Principle 2: Health emerges from maintainable-ease of functioning at multiple levels . Maintainable-ease of functioning in the general population can be observed at the level of the cell , the self , and the society simultaneously
Cooperation across multiple levels of functioning is required for the organization and adaptation of living systems (Nowak and Sigmund, 2005 ; Antonucci and Webster, 2014 ). When developing an integrative model of health, it is important to consider how biological cells, individuals, and the larger society simultaneously play a role in population health (Xavier da Silveira dos Santos and Liberali, 2019 ; Antonucci and Webster, 2014 ). In this philosophy, we define health from three levels: cells , selves, and societies . What happens when these levels do not function in cooperation?
When the functioning of cells disrupts the functioning of the self, a state dis-ease in the self can follow. For example, prolonged dysfunction in autoimmune conditions can lead to prolonged dysfunction for the (individual’s sense of) self by triggering depression, decreased motivation, or anxiety (Lougee et al., 2000 ; Garud et al., 2009 ). The reverse can also be true. When the functioning of the self (i.e. one individual) disrupts the functioning of their cells, a state dis-ease in the cells can also follow. For example, prolonged sugar binging and addictive eating can lead to prolonged high blood sugar and pancreatic dysfunction seen in diabetes (De Koning et al., 2011 ; Imamura et al., 2015 ). Cells and selves are not separate.
When the functioning of the self disrupts the functioning of the society we observe a state dis-ease in the society. For example, one person’s unprotected sex with multiple partners can also lead to epidemics and social conflicts. The reverse can also be true. When the functioning of the society disrupts the functioning of the individual, a state dis-ease in the self can follow. For example, dysfunctional social conditions (as seen in Rutter, 1998 ), can lead to prolonged psychological and behavioral dysfunctions of individuals. Selves and societies are not separate.
When the functioning of society disrupts the functioning of cells, a state of dis-ease in the cells can also follow. For example, prolonged dysfunction in society in the form of misguided values about cleanliness, can lead to over-sanitization practices that create superbugs and antibiotic-resistant bacteria (Zaccheo et al., 2017 ; Finkelstein et al., 2014 ; Bower and Daeschel, 1999 ). The reverse can also be true. When the functioning of cells disrupts the functioning of the society, a state of dis-ease in the society can follow. Prolonged dysfunction in cells from naturally occurring parasites (e.g. Yersinia pestis [Cui et al., 2013 ]) can lead to prolonged dysfunctions like the economic collapse following 14th century Black Death (Haensch et al., 2010 ). Cells and societies are not separate.
What does health look like when these levels work together? Recent reports on the Blue Zones (i.e. the areas of the world where populations live significantly longer and healthier than the average) demonstrate that healthy functioning at these levels enhances physical longevity and mental wellbeing in populations (Buettner, 2012 ; Poulain et al., 2013 ). Buettner ( 2012 ) reports on how Blue-Zone populations intentionally and habitually enrich their physical bodies with healthy eating and physical activity. In addition to integrating physical and behavioral practices, these communities also integrate behavioral and social practices, such as, goal-setting, meditations/prayer, social engagement, pursuit of purpose, and community gathering. Humor is used by individuals and groups as a means to practice ease when challenges present themselves (Buettner, 2012 ). Blue Zone communities place value upon physical/natural, behavioral and social processes, generating them intentionally and habitually.
Both states of ease and dis-ease can teach us about the contributions of cells, selves, and societies to population health. Although it is important to be able to observe the levels separately to describe their contributions, it is also important to consider how the levels integrate to impact healthy publics. We acknowledge that meaningful changes can be observed above and below these levels (e.g. at the level of the biosphere and genome). However, this initial paper will introduce levels that are most proximal and accessible to the experience of a general readership (Fig. 1 ).
Principle 3: Health emerges from systems whose primary purpose is to generate maintainable-ease of functioning at a respective level
We propose that systems exist at each level with the purpose of generating maintainable-ease of functioning at that level. The biological immune system, an individual’s system of health behaviors, and the social system will be observed as systems that generate maintainable-ease of functioning in cells, selves, and societies respectively (Fig. 2 ).
Principle 3a: The biological immune system is directly responsible for maintainable-ease of functioning at the level of the cell
Throughout the course of human evolution, the complexity and biodiversity of the human body continued to increase (Rodríguez et al., 2012 ). What keeps the trillions of cells and microorganisms in cooperation in a human body? The biological immune system maintains functional cells (Rodríguez et al., 2012 ). Although it is documented that the functioning of the biological immune system has implications for behavioral functioning (Ader, 1974 , 2000 ; Johnston et al., 1992 ; CDC, 2016 ) and social functioning (CDC, 2016 ; Reidel, 2005 ; Cutler and Miller, 2005 ) the system’s primary purpose is supporting functioning in the cellular/biological system.
Principle 3b: Health behavior is directly responsible for maintainable-ease of functioning at the level of the self
Throughout the course of time, the complexity of human behavior, has continued to increase (Boulding and Khalil, 2002 ). What keeps an individual in a state of balance during times of rapid change? One’s system of health behaviors (e.g. one’s practices of breathing, drinking, eating, and moving) maintain a functional self. Although it is well documented that the behavior of the individual impacts biological functioning (Fadel, 2013 , 2015 ) and social functioning (Omer et al., 2009 ), one’s system of health behaviors directly impacts one’s experience of (or one’s ‘sense of’) their “self”.
Principle 3c: The social system is directly responsible for maintainable-ease of functioning at the level of the society
Throughout history, the social diversity of human societies continued to increase. During periods of rapid increases in social diversity and cultural integration, what supported cooperation in the society? Social systems (e.g. public governments, private social organizations, religious/spiritual organizations) emerge to maintain a functional society. Although it is well documented that a social system can impact biological functioning (CDC, 2016 ; Riedel, 2005 ; Cutler and Miller, 2005 ) and behavioral functioning (Buettner, 2012 ), the social system’s primary role is to maintain functions at the level of the society.
Principle 3d: By considering health as maintainable-ease of functioning generated by systems , we have the ability generalize health across levels
To observe health at the level of the cell, the self, and the society simultaneously, we consider systems that support maintainable-ease of biological, behavioral, and social functioning. The biological immune system, an individual’s system of health behaviors, and the social system make meaningful contributions to the functioning of cells, selves, and societies, respectively. While these systems are not the only systems that impact each level (e.g. one’s cardiovascular system impacts cells, one’s “personality” impacts the self, the environment impacts society), the biological immune system, health behavior, and the social system have great implications for population health from their respective levels; and they can be operationalized at these levels based upon their functions .
By considering health as maintainable-ease of functioning (rather than maintained biological structures) at multiple levels, we set a point of reference from which to integrate important determinants of population health. When taking the structuralist’s perspective, the biological immune system, health behavior, and social systems appear as distinctly separated. When taking a functionalist’s perspective, the biological immune system (i.e. the integration of host defense functions and microbiota functions), one’s (system of) health behaviors (i.e. the integration of decision-making/executive functions and habits/habitual life functions), and the social system (i.e. the integration of population values and population behaviors) appear together in A Philosophy of Health.
Principle 4: Each system employs two general functions— variation and precision —to generate maintainable-ease of functioning at a level
The functionalist perspective allows us to observe systems based upon their functions . The biological immune system will be observed as an integration of host defense functions and microbiota functions (Hooper and Littman Macpherson, 2012 ); (2) an individual’s system of health behaviors will be observed as an integration of decisions/executive functions and habits/habitual life functions (de Bruin et al., 2016 ; Verplankern, 2005 ; Norman et al., 1998 ; Prochaska et al., 1994 ; Prochaska et al., 1991 ); and the social system will be observed as an integration of actively functioning values and population-wide behaviors that function in relation to those values (Dowling and Pfeffer, 1975 ; Cotgrove and Duff, 1981 ).
By researching the role of these functions at each level, we distilled two general functions of each system: variation and precision. Variation appears in the functions of each system that generate a range of abilities, the “varied-abilities”, that sustain health in presently changing conditions. The microbiota, habits/habitual life functions and population behaviors will be observed (in Principle 4a) as the variation-functions of the biological immune system, health behavior, and the social system, respectively. Precision appears in those functions that prioritize and organize the patterns of variation that can sustain health at a level in future, changing conditions. The host-defense functions, decision-making/executive functions, and values systems will be observed (in Principle 4b) as the precision-functions in the biological immune system, health behavior, and the social system, respectively.
Consideration of a complementary relationship among precision and variation is not novel. Precision and variation have been discussed as central to the development of neural and biological systems (Hiesinger and Bassem, 2018 ). Discussions of precision and variation have also provided important insight into research on the biological immune system (Albert-Vega et al., 2018 ; Brodin et al., 2015 ). Through this philosophy, one can go beyond biological systems to observe how precision (in the form of host-defense functions, decision-making/executive functions, and values) and variation (in the form of microbiota functions, habits/habitual life functions, and population-wide behaviors) integrate to generate to maintainable-ease of functioning in cells, selves, and societies simultaneously (Fig. 3 ).
Principle 4a: Variation is responsible for generating the range of abilities, the “varied-abilities”, that can express ease-of-functioning in presently changing conditions
Without functional variation, life is fragile because the present environment is always changing (Taleb and Blyth, 2011 ). Fragile systems’ inability to experience changing conditions (in part) relates to limited variability. Conversely, adaptive system’s ability to experience changing conditions (in part) relates to functional variability (Taleb, 2012 ). When one microorganism in the microbiome takes over, biological fragility reflects a state of infection. When one habit takes over, behavioral fragility reflects a state of an addiction/dependence. When one population behavior takes over (e.g. when economic participation or access to food is restricted to a small percentage of the population) social fragility reflects a state of social/civil unrest.
The human microbiota is comprised of trillions of microorganisms, such as bacteria, fungi, and viruses. When variability in the human microbiota exists, an ease of functioning, or “homeostasis” in cells can be expressed in the present biological/ecological environment (Parfrey and Knight, 2012 ; Bogaert et al., 2011 ; Claesson et al., 2011 ). Research demonstrates that variation in the microbiota impacts the health of human cells by metabolizing complex carbohydrates, converting proteins to neural signals, and modulating diurnal rhythms that maintain biological homeostasis (Clemente et al., 2012 ; Rothe and Blaut, 2012 ; Blaut and Clavel, 2007 ; De Vadder et al., 2014 ). When variation in the microbiota is dramatically limited or changed (e.g. following antibiotic overuse), cellular tissue in the human body is fragile and vulnerable to infections, allergies, and inflammatory outbreaks (Francino, 2016 ).
When one’s habitual life functions (e.g. breathing, drinking, eating, and moving) and one’s healthy habits (e.g. one’s weekly exercise schedule, or weekly meal preparation) can be expressed freely, an ease of functioning is felt by one-self in the present environment. When life functions are no longer expressed with ease (e.g. breathing and movement are compromised due to prolonged sedentary lifestyle), or when a single habit takes over one’s lifestyle (e.g. smokes breaks “must” occur every 30 min), an individual is vulnerable to stressful outbreaks and chronic states (Al’Absi, 2011 ; Conrad et al., 2007 ; Suess et al., 1980 ; León and Sheen, 2003 ; Parrott, 1999 ; Koob, 2008 ).
When the basic human rights in a society are preserved in the present (e.g. right to life, freedom of speech; right to property), human populations have the ability to freely engage in the population - wide behaviors (e.g. health behaviors, social behaviors, economic behaviors) that support a functioning society. Health behaviors drive health and longevity. Social behaviors drive communication and cooperation. Economic behaviors drive goods and resources. When these population-wide behaviors are chronically restricted in a population (e.g. poor access to health care, oppression of free-speech, economic crash), societies become vulnerable to social/civil unrest [as commented historically by Victor Frankl ( 1985 ), Alexander Solzhenitsyn ( 2003 ), Franklin D. Roosevelt ( 1941 ), and Dr. Martin Luther King ( 1985 )].
Variation is essential so that a system has varied-abilities that can express ease-of-functioning in present environmental conditions . Dramatic and prolonged restrictions to variation in the microbiota, habits/habitual life functions, and population-wide behaviors characterize fragile and vulnerable states in cells, selves, and societies. Conversely, functional-variation supports resilience, robustness, and antifragility (Taleb, 2012 ). This does not mean that infinite variation is desirable; however, in this philosophy, precision is responsible for organizing expressions of variation so that the system does not degrade into unpredictably random variation or chaos (see Principle 4b).
Principle 4b: Precision is responsible for prioritizing and organizing the patterns of variation that maintain ease-of-functioning in future, changing conditions
Some environmental changes are too challenging for ease to be expressed in the present. However, following an exposure to challenging conditions, some systems adapt and become more functional (Taleb, 2012 ). Without the ability to functionally organize after stressors, a system degrades into disorder or chaos over time. Host-defense functions, decision-making/executive functions and values systems prioritize and organize variation in the microbiota, habits/habitual life functions, and population behaviors respectively.
When a pathogen invades the biological system, precise responses must occur to organize this potentially chaotic situation. At the level of the cell, a functional host-defense system (comprised of the innate, adaptive and complement immune system branches) organizes the biological system so that functional invaders (i.e. symbionts) and healthy cells are maintained and dysfunctional invaders (i.e. pathogens) and damaged cells are removed (Hoeb et al., 2004 ; Janeway, 1992 ; Janeway and Medzhitov, 2002 ; Janeway et al., 2014 ). When precision is dysfunctional, the host-defense system may (1) fail to prioritize responses to a costly invasion, leading to a state of infection; or (2) the host-defense system might prioritize dysfunctional responses to the cells of body that prolong a state of autoimmunity (Naor and Tarcic, 1982 ).
When a bad habit emerges, precise responses must occur to organize this potentially chaotic situation. At the level of the self, functional decision-making (or at smaller scales executive functioning) prioritizes and organizes behavior so that functional expressions of habit (or at smaller scales, habitual life functions) are prioritized regularly, and dysfunctional ones are replaced or minimized (de Bruin et al., 2016 ; Prochaska et al., 1994 ; Prochaska and Prochaska, 2016 ; Prochaska et al., 1988 ; Redding et al., 2011 ; Weissenborn and Duka, 2003 ; Bickel et al., 2012 ). When dysfunctional, decisions may (1) fail to prioritize responses that remove a costly expression of habit (e.g. a teen started smoking cigarettes to “be cool” and now has to smoke in the bathroom before each class to get through the day; by not deciding to move at work, one’s breathing becomes shallow and movement becomes rigid); or decisions may (2) prioritize habits that prolong dysfunction despite knowing the dangerous consequences (e.g. an adult continues smoking cigarettes despite knowing the family’s history of lung cancer; an adolescent continues binge on sugar despite a diabetes diagnosis).
When dangerous population-wide behaviors threaten life in a society, precise responses must occur to organize this potentially chaotic situation. At the level of society, the agreed upon values organize the social system so that functional population behaviors are prioritized and dysfunctional population behaviors are minimized. Functional values prioritize behaviors that support the society (e.g. as seen when societies mandate that students get certain vaccines before attending University), while also setting standards that remove/replace behaviors that threaten the society (e.g. new laws create legal repercussions for risk behaviors in society). Without values that functionally prioritize population-wide behavior, society may (1) fail to prioritize responses to a dysfunctional population behavior (e.g. as seen during AIDS epidemic of the 1980s due to insufficient public health values around safe sex); or society may (2) prioritize dangerous behaviors that can prolong societal dysfunction (e.g. the antibiotic resistance crisis (Ventola, 2015 ; Michael et al., 2014 ) has been attributed in part to the over-valuing or over-use of antibiotic medications in healthcare practices).
Precision is essential so that a system can maintain ease-of-functioning in future, changing conditions . When precision does not adequately detect the presence of costly conditions, a response may not be prioritized (e.g. as seen during acute infection, addiction/dependence following a surgery, the AIDs outbreak in the 1980s). When precision prioritizes responses that prevent ease longitudinally, dysfunction is prolonged (e.g. autoimmunity, continued smoking despite family history of cancer, misguided values that create an antibiotic-resistant bacteria). Through dysfunctional -precision, the conditions for life in cells, selves, and societies becomes disordered over time. Through functional -precision, a system prioritizes responses that maintain ease-of-functioning in future conditions. Prioritizing functional microorganisms (i.e. symbionts) supports the developing life of cells; prioritizing functional habits (e.g. weekly exercise) and habitual life functions (e.g. diaphragmatic breathing and relaxed movement) supports the developing life of the self; and prioritizing functional population behaviors (e.g. access to functional health care, economic resources; access to social support) supports the developing life of the society.
Principle 5: Health is valued by a system when precision-and-variation generate maintainable-ease of functioning. Health is de-valued by a system when precision or variation prevent maintainable-ease of functioning
By defining precision-and-variation, we can better understand maintainable-ease of functioning in population health:
Functional-Variation generates ease-of-functioning in the present (e.g. fluid and variable motion reflects an ease and variability of one’s movement); while Functional-Precision prioritizes expressions that can maintain ease-of-functioning in the future (e.g. prioritizing challenging exercise for 20 min each day may lead to an ease in bodily movement long term).
Dysfunctional-Variation prevents ease-of-functioning in the present (e.g. prolonged sitting might lead to rigid movement and shallow breathing); while Dysfunctional-Precision might prioritize expressions that prevent ease in the future (e.g. rather than focus on relaxing breathing and movement on work breaks, one decides to drink alcohol to relax).
Without functional-variation, life is fragile and vulnerable to changing conditions of the present. Without functional-precision, life becomes disorganized from the system’s exposure to changing conditions across time. When functional-and-integrated, precision-and-variation value maintainable-ease of functioning in cells, selves, and societies. When dysfunctional or fragmented, precision or variation can de-value maintainable-ease of functioning in cells, selves, or societies. If maintainable-ease of functioning can be valued in cells, selves, and societies, we will likely observe healthy publics.
Five principles of health are presented: (1) Health is the maintainable-ease of functioning; (2) Maintainable-ease of functioning emerges from multiple levels ; (3) At each level, maintainable-ease of functioning is generated by systems ; (4) Each system employs two functions, precision - and - variation , that generate maintainable-ease of functioning ; and (5) Health is valued by a system if precision-and-variation generate maintainable-ease of functioning. Through these five principles, both naturalistic and holistic perspectives can be considered simultaneously because maintainable-ease of functioning is relevant to biological functioning (e.g. as described in BST) and personal/social, goal-oriented functioning (e.g. as described in HTH). This philosophy can also be used to investigate how naturalistic and holistic phenomena have informed past healthcare interventions. What do vaccine interventions, behavior change interventions, and social change interventions have in common? When successful, these interventions enhance both precision and variation.
Vaccine interventions can enhance both the precision of the host-defense functions and variation in the microbiome. During a vaccine intervention, the microbiome is exposed to a new variation in the form of a new virus (Reidel, 2005 ). Through this exposure, the precision of host defense functions can adapt to prioritize maintainable-ease of functioning in the microbiome in the future. How? The host-defense system produces antibodies that allow the immune system to respond effectively and efficiently to this virus when exposed to it again in the future (Janeyway, 2014 ). Although the precision of the immune system has been enhanced to handle historical threats through vaccines (e.g. for small pox, chickenpox, measles), new viruses like the coronavirus can still emerge. With this philosophy, vaccine developers and public health officials might not only ask the question, “How do we combat the coronavirus?” Researchers, vaccine developers and public health officials may also ask the functional question: “How do we enhance the precision of the host-defense system and the variation of the human microbiome to adapt following an exposure to the coronavirus?”
Behavior change interventions can enhance both the precision in one’s decisions and the variation in one’s habits. During a behavior change intervention, a person’s existing habits are exposed to a new variation in habit. For example, the beginning of a new exercise intervention exposes the individual’s current habits/habitual functioning to changes in movement and breathing (i.e. exercise) that may also change their patterns of eating and hydration. Through this exposure, a person’s decision-making might adapt to prioritize maintainable-ease of functioning in the individual’s lifestyle. How? Some behavior change interventions train one’s decision-making to remove or “counter-condition” unhealthy habits, by replacing them with healthy habits (Prochaska et al., 1988 ). Although modern behavior change interventions have shaped the precision of decision-making during health behavior change (e.g. of smoking, diet, alcohol use, inactivity), new problems for health behavior still emerge when the individual is exposed to a new, potentially addictive technology. With this philosophy, behavior change interventionists and health officials might not only ask the question, “How do we support good decision-making of individuals?” Researchers, behavior change technology developers, and public health officials may also ask the functional question: “How do we enhance the precision of one’s decisions and the variation of one’s habits following the exposure to a new, potentially addictive technology?”
Public health campaigns disseminated by social organizations can enhance the precision of the population’s health values and variation in population-wide health behaviors. Leading up to first Surgeon General’s Advisory Committee on Smoking and Health (1964), the U.S. Department of Health had become increasingly aware of (i.e. exposed to) variations in a population health behavior. If populations smoked, then populations were more likely to develop lung cancer, laryngeal cancer, or chronic bronchitis (CDC, 2018 ). Following this exposure to (the consequences of) population smoking behavior, society’s values shifted to prioritize health. How? The Federal Cigarette Labeling and Advertising Act of 1965 was adopted, and the Public Health Cigarette Smoking Act of 1969 was adopted to create new health values. This shift in values prioritized new variations in population health behavior by: (1) requiring a health warning on cigarette packages; (2) banning cigarette advertising in the broadcasting media; and (3) calling for an annual report on the health consequences of smoking (CDC, 2018 ). Since these first initiatives adult smoking rates have fallen from about 43% (in 1965) to about 18% today; and mortality rates from lung cancer, the leading cause of cancer death, are declining (Department of Health and Human Services, 2014 ). Although the precision of the population’s values has been enhanced to impact population behaviors (e.g. the tobacco laws described above supported healthy change), new chronic states can still emerge following exposure to social changes (e.g. the invention of the Juul impacted high school and college aged populations). With this philosophy, public policy officials and public health researchers might not only ask the question, “How do we create new laws to protect population health from nicotine addiction?” They may also ask the functional question: “How do we enhance the precision of the population’s values and the variation of the population’s behavior following the invention of a new nicotine delivery system technology (e.g. flavored Juuls)?”
Previously we described that without functional variation, life is fragile when exposed to present changing conditions; and without functional precision, life becomes disorganized from exposure to changing conditions across time. When successful, the above interventions upon biological, behavioral, and social functioning have a common theme: each facilitates exposures to biological, behavioral or social conditions that support (1) increasingly complex/diverse variation; and (2) increasingly organizable precision. Exposure, not avoidance , has facilitated population health in these interventions. While healthcare systematically prioritizes biological exposures in the form of vaccine interventions, they do not systematically prioritize behavioral or social exposures. However, it is documented that exposure to healthy behaviors in youth prevents risk behaviors in adolescence (Velicer et al., 2000 ); and exposure to community-based health initiatives can support population health (Dulin et al., 2018 ; CDC, 2018 ). Given that systematic biological exposures in the form of vaccination have led to a global control of some acute infectious diseases (Tangermann et al., 2007 ); might systematic behavioral and social exposures (especially in youth) be needed to enhance global campaigns toward the control of chronic disease?
A functional language of health is central to the success of a Philosophy of Health. Why? The levels are not separate, but rather are continuously connecting with one another. A good philosophy of health should have the ability to discuss assessment, diagnosis, intervention, and prevention across levels, across systems, across cultural populations, and across time. Using the common language of precision and variation creates discussions that connect the levels and integrate research disciplines.
A case (to) study: mental health as between-level functioning in this philosophy
Historically, and still too often, health professionals have an expertise at one level, that limits their prescription of interventions to that level. This can actually create barriers to a complete solution when a health problem is multileveled. While a person’s mental health is typically assessed based upon their first-person experience of thoughts, feelings, and behaviors; symptoms can be triggered by biological, physiological, behavioral, psychological, and/or social dysfunction. Most clinicians typically do not have the ability to assess and address all forms functioning. So if one person, John, is meeting with a clinician who specializes in primary care medicine, he may only be prescribed a biological intervention like medication. If John is meeting with a clinician who specializes in behavioral medicine, he may only be prescribed a health behavior change intervention. If John is meeting with a clinician who specializes in a certain theory of psychotherapy, he may only be prescribed a psychotherapy intervention based on the clinician’s training. If John is meeting with a clinician who specializes in social work, he may only be prescribed a group, community or social intervention. While the above specializations have been helpful in establishing an empirical bases for mental health interventions, over-specialization can be problematic when a multi-leveled solution is needed. In addition, it can also be problematic when a level-specific solution is needed that the clinician cannot provide (e.g. when psychotherapy is needed but a clinician only has the ability to prescribe psychiatric medication).
Technology poses a multileveled issue for population mental health in 2020. Selves have more social connection then ever in history, yet societies are characterized by increasing rates of depression and loneliness (Sum et al., 2008 ; Hammond, 2020 ; Srivastava and Tiwari, 2013 ; Twenge, 2017 ). Researchers might use this Philosophy of Health to facilitate between-level conversations that address seemingly paradoxical outcomes that emerge during this new age of rapid technological growth. To do this, a researcher might first begin by asking questions about functioning at each level ; second , ask questions about processes between the levels ; and third , concurrently ask questions at and between levels .
First: Begin by asking questions at each level
Novel challenges face the iGeneration (and their parents) due to technology’s novel impacts on the development of individual and social functioning (Twenge, 2017 ). For example, if John’s decisions (self-precision) and habits (self-variation) remain consistent during school hours because his parents do not let him have a phone; but his class’ social behaviors around him (society-variation) change dramatically because everyone else at school uses the newest smartphone application to talk during class; will John’s mental health suffer? Although his parents’ intentions are to protect John, the contrast between his behavior (self’s precision-and-variation) and the population social behavior (society-variation) can impact John’s health. Notice here how we have not yet considered functions that connect the self to the society (e.g. John’s thoughts and feelings). Rather we first consider (or contrast) functioning at the level of the self (i.e. John’s decisions-and-habits) and the society (i.e. population social behavior) in accordance with Principles 1–5 (see Figs 1 – 3 ).
Second: Look for functional processes that connect the levels
One person’s thoughts and emotions/feelings are processes that help to integrate the functioning of one-self within the functioning of a society. How might John’s thoughts and feelings connect his (sense of) self to his society? Perhaps John’s parents teach him that it is important to feel separate from his classmates during class so he can think clearly in class; and that he can feel connected to his friends by inviting them over to communicate together after school. This parenting may impact John’s thoughts and feelings during school. If John’s parents do not talk with him about this topic, John may experience different thoughts and feelings during school hours. When kept to one-self, thoughts and emotions are foundational to an internal sense of self as one functions in the larger society; and, when acted upon, thoughts and feelings can become verbal communication (e.g. speech) and non-verbal communication (e.g. body language, facial expressions) that form an external sense of self that is visible to the society. The (internal) experience of and (external) communication of thoughts, feelings and actions form the foundation of all systems of psychotherapy (Prochaska and Norcross, 2018 ). This view can be particularly helpful as researchers begin to investigate how smart technology impacts developmental changes to the self within the society beginning in youth.
Third: Concurrently ask questions at and between levels
Perhaps, a clinical researcher is interested in investigating protective mental health factors in the iGeneration; and they hypothesize that lower rates of loneliness, anxiety, and depression will be seen in subjects that do not respond to text messages immediately. The researcher might investigate further by using the philosophy to develop questions for the research subjects: “(1) Do you use conscious decision-making (self-precision) to prevent yourself from habitually responding to your phone when a text appears (self-variation)? (2) How fast do other’s in your social group typically respond to texts (society-variation)? (3) What changes in thoughts and feelings are experienced (internal self-society connection) after you communicate via text (external self-society connection)?” Perhaps this researcher also wants to investigate how those who are addicted to the technology perceive non-responders. The clinical researcher might again apply the philosophy: “(1) How fast do other’s in your social group typically respond to your texts (society-variation)? (2) Do you experience changes in thought and feeling (internal self-society connection) when others do not respond to you within an hour (society-variation)? (3) How do you communicate those thoughts and feelings (external self-society connection) with others when they do not respond for a prolonged period of time (society-variation)?” Future research might use this method to gather and organize levels of information on mental health factors across different self- and societal-conditions.
The processes that form our mental health form a functional connection between self and society. If mental health is a reflection of the self–society connection, what might be a reflection of the self–cell connection? Physiological health evidences a functional connection between our sense of self and our cells. For example, aerobic exercise is a health behavior that stimulates changes to variations in breathing and movement. By engaging in this behavior, the biological cells of the body are also stimulated via various physiological processes. Breathing will stimulate cellular functioning via the cardiovascular and respiratory systems; and movement will stimulate cellular functioning via the cardiovascular, musculoskeletal, and central nervous systems. While all physiological systems are working in collaboration in the body, certain changes to behavioral and biological functioning will stimulate certain physiological systems. By viewing health through this lens, between-level observations join the philosophy: biological functions emerge at the level of the cell; physiological functioning emerges as the cell–self connection; behavioral functions emerge at the level of the self; psychological/mental functioning emerges as the self–society connection; and social functions emerge at the level of the society. Future papers will explore maintainable-ease of functioning at and between levels.
Future directions: new images of healthcare integration and new perspectives of healthcare innovation
By considering this integrative philosophy, one can define health based upon a tangible connectedness, rather than separateness, of cells, selves, and societies. We provide Image 4 as a way to visualize the common paths to the health of healthy publics. When researchers observe that a host defense system is changing cellular functions following an infection, they may also expect these changes to have an impact [along Path 1] on expressions of habitual or physiological functions (e.g. immune function can stimulate the sensation of “achiness” or “pain” altering one’s physical movement, breath rate, hydration, and hunger) (Kelley, 2003 ; Johnson et al., 1992 ; Danzer, 2009 ). When researchers observe an individual deciding to engage in health behavior change following an addiction, they may also expect these changes to have an impact [along Path 2] on the group-behavior of their family system or social systems. When researchers observe changes to society’s values following a newly detected problem (e.g. laws ban Cigarette Advertising in broadcasting media; public health standards mandate certain vaccines before attending school), they may also expect that these changes can have an impact on behavioral functions of individuals [along Path 2] and biological functions of cells/organs [along Path 3]. These levels are continually integrating along these common paths to the health of healthy publics (Fig. 4 ).
When attending to this connectedness new, important questions can have new answers. What function does modern technology serve in population health and healthcare? If technology algorithms prioritize variations in population behaviors, then they fulfill a role as society-level precision. When modern technologies like machine learning (ML) technology and Computer Tailored Interventions (CTI) prioritize patterns of population behavior, we can see profound impacts on social change in a society. Although one might argue that technologies can be used by individual-level functions, the algorithms that are currently deployed and updated on devices interface with big-data gathered on population behaviors (Manogaran and Lopez, 2017 ; Dinov, 2016 ; Mullainathan and Spiess, 2017 ; Cheng et al., 2017 ).
In this paper, we identified that precision can be functional or dysfunctional. Similarly, technologies can support or prevent healthy population behavior. Some technologies prioritize health behavior in populations by tracking physical activity and providing feedback on activity progress; while others prevent healthy behavior by prioritizing sedentary behavior through video-gaming. Some social media technologies facilitate social communication with distant friends and relatives that supports wellbeing; while others facilitate conflictual communication that diminishes wellbeing. Given that modern technology can support or hinder health, we believe it is important that healthcare can prioritize technological innovations that value health in cells, selves, and societies. To do this, technology innovators might seek to value a higher order construct (e.g. maintainable-ease of functioning) in their algorithms.
Medical technology is currently used to titrate the doses of vaccines so that maintainable-ease of biological functioning (i.e. inoculation) is made available to the general population. When biological exposures are not properly titrated, infections can become active in the population and health is no longer valued at the level of the cell. Similarly, when behavioral and social exposures are not tailored to the needs of individuals and groups, populations can become resistant to healthy change, and health is no longer valued at the level of the self and the society. Behavior change researchers Prochaska and Prochaska ( 2016 ) report that when individuals and populations are not ready for a change, interventions that force individuals or populations to take action can increase resistance and prolong dysfunction. By tailoring (or what they term “staging”) behavioral and social level interventions, Computer Tailored Interventions upon behavioral and social functioning are made possible (Prochaska et al., 2001 ; Velicer et al., 2000 , Prochaska and Prochaska, 2016 ). Despite these advances, there remains a need for technological advances that can make maintainable-ease of behavioral and social functioning available to the general population.
Future healthcare interventions could benefit from ML algorithms that tailor behavioral and social exposures to enhance precision-and-variation. Research already demonstrates that tailoring interventions for biological precision (Albert-Vega et al., 2018 ) and biological variation (Brodin et al., 2015 ) can impact long-term biological functioning. Future innovations might seek to use technology to tailor behavioral and social interventions to generate maintainable-ease of functioning. Through the functional language used in this paper we hope readers are inspired to present new questions, new comments, and new perspectives about needed healthcare innovations.
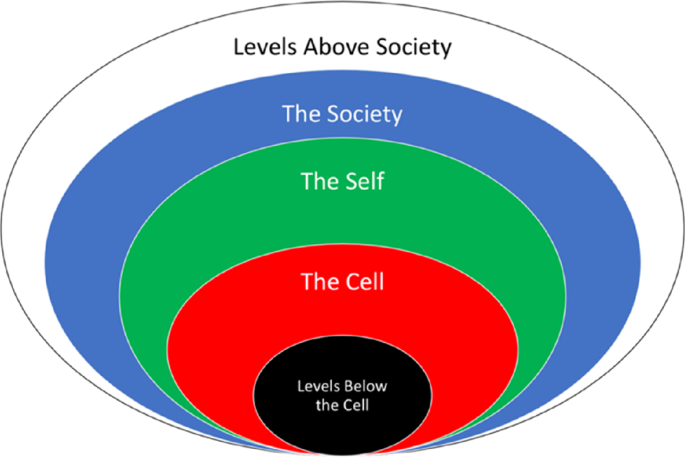
This philosophy of health investigates three levels of health: cell, self, and society. The level of the cell accounts for biological functioning within human beings. The level of the self accounts for first-person functioning of each human being. The level of the society accounts for group functioning of human beings.
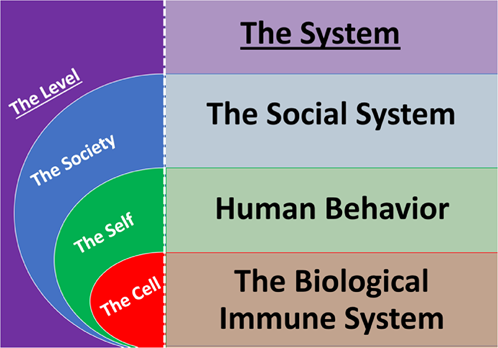
Each system is responsible for generating maintainable-ease of functioning at a level. The biological immune system is responsible at the level of the cell. A human's system of health behaviors is responsible at the level of the self. The social system is responsible at the level of the society.
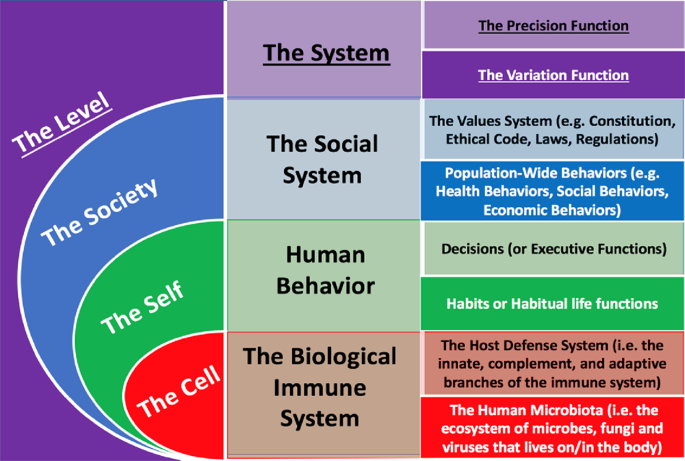
Maintainable-ease of functioning is generated by two functions in each system: precision and variation. The human microbiota, habits, and population-wide behaviors evidence variation in cells, selves and societies respectively. The host defense system, decisions, and values evidence precision in cells, selves and societies respectively.
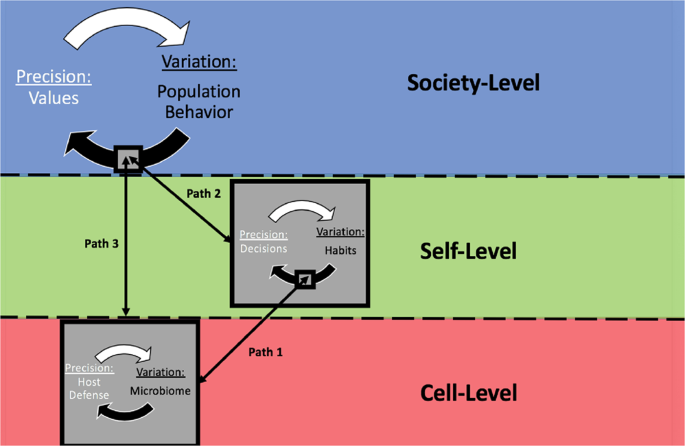
Population health is generated along common paths that integrate the levels. The biological functioing of cells impacts fluctuations of habits/habitual functioning; and vice versa. The behavioral functioning of each self impacts fluctuations in population behavior; and vice versa. The biological functioning of cells also can impact fluctations in population behavior; and vice versa.
Ader R (1974) Behaviorially conditioned immunosuppression. Psychosom Med 36(2):183–184
Article CAS PubMed Google Scholar
Ader R (2000) On the development of psychoneuroimmunology. Eur J Pharmacol 405(1–3):167–176
Al’Absi M (2011) Stress and addiction: biological and psychological mechanisms. Elsevier
Albert-Vega C, Tawfik DM, Trouillet-Assant S, Vachot L, Mallet F, Textoris J (2018) Immune functional assays, from custom to standardized tests for precision medicine. Front Immunol 9:2367
Article CAS PubMed PubMed Central Google Scholar
Antonucci TC, Webster NJ (2014) Rethinking cells to society. Res Hum Dev 11(4):309–322
Article PubMed PubMed Central Google Scholar
Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM, McClure SM (2012) Are executive function and impulsivity antipodes? A conceptual reconstruction with special reference to addiction. Psychopharmacology 221(3):361–387
Blaut M, Clavel T (2007) Metabolic diversity of the intestinal microbiota: implications for health and disease. J Nutr 137(3):751–755
Article Google Scholar
Bogaert D, Keijser B, Huse S, Rossen J, Veenhoven R, Van Gils E, Bruin J, Montijn R, Bonten M, Sanders E (2011) Variability and diversity of nasopharyngeal microbiota in children: a metagenomic analysis. PLoS ONE 6(2):e17035
Article ADS CAS PubMed PubMed Central Google Scholar
Boorse C (1997) A rebuttal on health. In: What is disease? Humana Press, Totowa. Springer. pp. 1–134
Boulding K, Khalil E (2002) Evolution, order and complexity. Routledge
Bower CK, Daeschel MA (1999) Resistance responses of microorganisms in food environments. Int J food Microbiol 50(1-2):33–44
Brodin P, Jojic V, Gao T, Bhattacharya S, Lopez Angel CJ, Furman D, Shen-Orr S, Dekker CL, Swan GE, Butte AJ, Maecker HT, Davis MM (2015) Variation in the human immune system is largely driven by non-heritable influences. Cell 160(1–2):37–47
Buettner D (2012) The blue zones: 9 lessons for living longer from the people who’ve lived the longest. National Geographic Books
Centers for Disease Control and Prevention (2016) CDC history of smallpox. https://www.cdc.gov/smallpox/history/history.html
Centers for Disease Control and Prevention (2018) History of the Surgeon General’s reports on smoking and health 2(28), 07. https://www.cdc.gov/tobacco/data_statistics/sgr/history/index.htm
Chartier G, Cawthorpe D (2016) From ‘Big 4’to ‘Big 5’: a review and epidemiological study on the relationship between psychiatric disorders and World Health Organization preventable diseases. Curr Opin Psychiatry 29(5):316–321
Article PubMed Google Scholar
Cheng Q, Li TM, Kwok CL, Zhu T, Yip PS (2017) Assessing suicide risk and emotional distress in Chinese social media: a text mining and machine learning study. J Med Internet Res 19(7):e243
Claesson MJ, Cusack S, O'Sullivan O, Greene-Diniz R, de Weerd H, Flannery E (2011) Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci USA 108:4586–4591
Article ADS PubMed Google Scholar
Clemente JC, Ursell LK, Parfrey LW, Knight R (2012) The impact of the gut microbiota on human health: an integrative view. Cell 148(6):1258–1270
Conrad A, Müller A, Doberenz S, Kim S, Meuret AE, Wollburg E, Roth WT (2007) Psychophysiological effects of breathing instructions for stress management. Appl Psychophysiol Biofeedback 32(2):89–98
Cotgrove S, Duff A (1981) Environmentalism, values, and social change. Br J Sociol 1:92–110
Cui Y, Yu C, Yan Y, Li D, Li Y, Jombart T, Weinert LA, Wang Z, Guo Z, Xu L, Zhang Y (2013) Historical variations in mutation rate in an epidemic pathogen, Yersinia pestis. Proc Natl Acad Sci 110(2):577–582
Cutler D, Miller G (2005) The role of public health improvements in health advances: the twentieth-century United States. Demography 42(1):1–22
Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ (2005) Comparison of the atkins, ornish, weight watchers, and zone diets for weight loss and heart disease risk reduction. JAMA 293(1):43
Dantzer R (2009) Cytokine, sickness behavior, and depression. Immunol Allergy Clin North Am 29(2):247–264
Daubenmier JJ, Weidner G, Sumner MD, Mendell N, Merritt-Worden T, Studley J, Ornish D (2007) The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the Multisite Cardiac Lifestyle Intervention Program. Ann Behav Med 33(1):57–68
de Bruin EI, van der Zwan JE, Bögels SM (2016) A RCT comparing daily mindfulness meditations, biofeedback exercises, and daily physical exercise on attention control, executive functioning, mindful awareness, self-compassion, and worrying in stressed young adults. Mindfulness 7(5):1182–1192
De Koning L, Malik VS, Rimm EB, Willett WC, Hu FB (2011) Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes in men. Am J Clin Nutr 93(6):1321–1327
De Vadder F, Kovatcheva-Datchary P, Goncalves D, Vinera J, Zitoun C, Duchampt A, Bäckhed F, Mithieux G (2014) Microbiota-generated metabolites promote metabolic benefits via gut–brain neural circuits. Cell 156(1–2):84–96
Dinov ID (2016) Volume and value of big healthcare data. J Med Stat Inform 4(1):3
Dowling J, Pfeffer J (1975) Organizational legitimacy: social values and organizational behavior. Pac Sociol Rev 18(1):122–136
Dulin A, Risica PM, Mello J, Ahmed R, Carey KB, Cardel M, Howe CJ, Nadimpalli S, Gans KM (2018) Examining neighborhood and interpersonal norms and social support on fruit and vegetable intake in low-income communities. BMC Public Health 18(1):455
Edington DW (2009). Zero trends: health as a serious economic strategy. UM-HMRC
Fadel PJ (2013) Neural control of the circulation during exercise in health and disease Front Physiol 4:224
Fadel PJ (2015) Reflex control of the circulation during exercise. Scand J Med Sci sports 25:74–82
Finkelstein JA, Dutta-Linn M, Meyer R, Goldman R (2014) Childhood infections, antibiotics, and resistance: what are parents saying now? Clin Pediatr 53(2):145–150
Francino MP (2016) Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front Microbiol 6:1543
Frankl VE (1985) Man’s search for meaning. Simon and Schuster
Garud S, Leffler D, Dennis M, Edwards‐George J, Saryan D, Sheth S, Schuppan D, Jamma S, Kelly CP (2009) Interaction between psychiatric and autoimmune disorders in coeliac disease patients in the Northeastern United States. Aliment Pharmacol Ther 29(8):898–905
Haensch S, Bianucci R, Signoli M, Rajerison M, Schultz M, Kacki S, Vermunt M, Weston DA, Hurst D, Achtman M, Carniel E (2010) Distinct clones of Yersinia pestis caused the black death. PLoS Pathog 6(10):e1001134
Hammond C (2020) https://www.bbc.co.uk/programmes/articles/2yzhfv4DvqVp5nZyxBD8G23/who-feels-lonely-the-results-of-the-world-s-largest-loneliness-study
Hiesinger PR, Hassan BA (2018) The evolution of variability and robustness in neural development. Trends Neurosci 41(9):577–586
Hooper LV, Littman DR, Macpherson AJ (2012) Interactions between the microbiota and the immune system. Science 336(6086):1268–1273
Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, Forouhi NG (2015) Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 351:h3576
Janeway CA (1992) The immune system evolved to discriminate infectious nonself from noninfectious self. Immunol Today 13(1):11–16
Janeway CA, Medzhitov R (2002) Innate immune recognition. Annu Rev Immunol 20(1):197–216
Janeway Jr CA, Travers P, Walport M, Shlomchik MJ (2014) Immunobiology: the immune system in health and disease, vol. 2001. Garland Science, New York, pp. 620–626
Google Scholar
Johnson EO, Kamilaris TC, Chrousos GP, Gold PW (1992) Mechanisms of stress: a dynamic overview of hormonal and behavioral homeostasis. Neurosci Biobehav Rev 16(2):115–130
Kelley KW, Bluthé RM, Dantzer R, Zhou JH, Shen WH, Johnson RW, Broussard SR (2003) Cytokine-induced behavior. Brain Behav Immun 17(1):112–118
King ML (1985) I have a dream: a speech. Thee Hellbox Press
Koob GF (2008) A role for brain stress systems in addiction. Neuron 59(1):11–34
León P, Sheen J (2003) Sugar and hormone connections. Trends Plant Sci 8(3):110–116
Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC, Hu FB (2018) Impact of healthy lifestyle factors on life expectancies in the US population. Circulation 138(4):345–355
Lougee L, Perlmutter SJ, Nicolson R, Garvey MA, Swedo SE (2000) Psychiatric disorders in first-degree relatives of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). J Am Acad Child Adolesc Psychiatry 39(9):1120–1126
Manogaran G, Lopez D (2017) A survey of big data architectures and machine learning algorithms in healthcare. Int J Biomed Eng Technol 25(2–4):182–211
Michael CA, Dominey-Howes D, Labbate M (2014) The antimicrobial resistance crisis: causes, consequences, and management. Front Public Health 2:145
Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, Kasaeian A (2018) The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 319(14):1444–1472
Mullainathan S, Spiess J (2017) Machine learning: an applied econometric approach. J Econ Perspect 31(2):87–106
Naor D, Tarcic N (1982) Control of autoimmune responses induced with modified self antigens. Ann NY Acad Sci 392(1):178–190
Article ADS CAS PubMed Google Scholar
Nordenfelt L (2007) The concepts of health and illness revisited. Med Health Care Philos 10(1):5
Norman GJ, Velicer WF, Fava JL, Prochaska JO (1998) Dynamic typology clustering within the stages of change for smoking cessation. Addict Behav 23(2):139–153
Nowak MA, Sigmund K (2005) Evolution of indirect reciprocity. Nature 437(7063):1291–1298
Omer SB, Salmon DA, Orenstein WA, Dehart MP, Halsey N (2009) Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med 360(19):1981–1988
Parfrey LW, Knight R (2012) Spatial and temporal variability of the human microbiota. Clin Microbiol Infect 18:5–7
Parrott AC (1999) Does cigarette smoking cause stress? Am Psychol 54(10):817
Poulain M, Herm A, Pes G (2013) The Blue Zones: areas of exceptional longevity around the world. Vienna Yearb Popul Res 11(1):87–108
Prochaska JO, Norcross JC, DiClemente CC (1994) Changing for good. Avon Books, New York
Prochaska JO, Velicer WF, DiClemente CC, Fava J (1988) Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol 56(4):520
Prochaska JO, Velicer WF, Guadagnoli E, Rossi JS, DiClemente CC (1991) Patterns of change: dynamic typology applied to smoking cessation. Multivar Behav Res 26(1):83–107
Article CAS Google Scholar
Prochaska JO, Velicer WF, Fava JL, Rossi JS, Tsoh JY (2001) Evaluating a population-based recruitment approach and a stage-based expert system intervention for smoking cessation. Addict Behav 26(4):583–602
Prochaska JO, Norcross JC (2018) Systems of psychotherapy: a transtheoretical analysis. Oxford University Press
Prochaska JO, Prochaska JM (2016) Changing to thrive: using the stages of change to overcome the top threats to your health and happiness. Simon and Schuster
Redding CA, Prochaska JO, Paiva A, Rossi JS, Velicer W, Blissmer BJ, Greene GW, Robbins ML, Sun X (2011) Baseline stage, severity, and effort effects differentiate stable smokers from maintainers and relapsers. Subst Use Misuse 46(13):1664–1674
Riedel S (2005) Edward Jenner and the history of smallpox and vaccination. In: Baylor University Medical Center Proceedings, January 1, vol. 18(1). Taylor & Francis, pp. 21–25
Rodríguez RM, López-Vázquez A, López-Larrea C (2012) Immune systems evolution. Sensing in nature. Springer, New York, pp. 237–251
Book Google Scholar
Roosevelt FD (1941) Message to congress. Retrieved 20 Mar 2012
Rothe M, Blaut M (2012) Evolution of the gut microbiota and the influence of diet. Benef Microbes 4(1):31–37
Rutter M (1998) Developmental catch-up, and deficit, following adoption after severe global early privation. J Child Psychol Psychiatry 39(4):465–476
Schroeder SA (2012) Rethinking health: healthy or healthier than? Br J Philos Sci 64(1):131–159
Solzhenitsyn A (2003) The Gulag Archipelago, 1918–56: an experiment in literary investigation. Random House
Srivastava A, Tiwari RP (2013) Effect of excess use of cell phone on adolescent’s mental health and quality of life. Int Multidiscip e-J 2(1):1–0
Suess WM, Alexander AB, Smith DD, Sweeney HW, Marion RJ (1980) The effects of psychological stress on respiration: a preliminary study of anxiety and hyperventilation. Psychophysiology 17(6):535–540
Sum S, Mathews RM, Hughes I, Campbell A (2008) Internet use and loneliness in older adults. CyberPsychol Behav 11(2):208–211
Taleb NN, Blyth M (2011) The black swan of Cairo: how suppressing volatility makes the world less predictable and more dangerous. Foreign Aff 2011:33–39
Taleb NN (2012) Antifragile: things that gain from disorder. Random House Incorporated
Tangermann RH, Nohynek H, Eggers R (2007) Global control of infectious diseases by vaccination programs. In: Pediatric infectious diseases revisited: Birkhäuser advances in infectious diseases BAID, Springer. vol. 1. pp. 1–41
Twenge JM (2017) iGen: Why today’s super-connected kids are growing up less rebellious, more tolerant, less happy–and completely unprepared for adulthood–and what that means for the rest of us. Simon and Schuster.
US Department of Health and Human Services (2014) The health consequences of smoking—50 years of progress. A report of the Surgeon General
Velicer WF, Prochaska JO, Fava JL, Rossi JS, Redding CA, Laforge RG, Robbins ML (2000) Using the transtheoretical model for population-based approaches to health promotion and disease prevention. Homeost Health Dis 40:174–195
Ventola CL (2015) The antibiotic resistance crisis: part 1: causes and threats. Pharm Ther 40(4):277
Verplanken B (2005) Habits and implementation intentions. The ABC of behavioural change. Elsevier, pp. 99–109
Wakefield JC (2014) The biostatistical theory versus the harmful dysfunction analysis, part 1: is part-dysfunction a sufficient condition for medical disorder? J Med Philos 39(6):648–682
Weissenborn R, Duka T (2003) Acute alcohol effects on cognitive function in social drinkers: their relationship to drinking habits. Psychopharmacology 165(3):306–312
World Health Organization (2010) Basic documents. World Health Organization
Xavier da Silveira dos Santos A, Liberali P (2018) From single cells to tissue self‐organization. FEBS J 286(8):1495–1513
Zaccheo A, Palmaccio E, Venable M, Locarnini-Sciaroni I, Parisi S (2017) Biocides and “superbugs”. Anthropological cross cultural perspectives, vol. 1. Springer, Cham, pp. 63–72
Download references
Acknowledgements
This research was supported by funding from the National Institutes of Health’s (NIH) National Cancer Institute (NCI).
Author information
Authors and affiliations.
Cancer Prevention Research Center, The University of Rhode Island, 130 Flagg Rd, Kingston, RI, 02881, USA
Julian M. Saad & James O. Prochaska
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Julian M. Saad .
Ethics declarations
Competing interests.
The authors declared the following potential competing interests: JOP, Ph.D. is a founder of the Transtheoretical Model (TTM) of Behavior Change, and is the Director of the Cancer Prevention Research Center at the University of Rhode Island. JMS, M.Ed. is currently a Ph.D. student conducting dissertation research on population health and behavior change under JOP’s supervision at the University of Rhode Island.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Saad, J.M., Prochaska, J.O. A philosophy of health: life as reality, health as a universal value. Palgrave Commun 6 , 45 (2020). https://doi.org/10.1057/s41599-020-0420-9
Download citation
Received : 28 September 2019
Accepted : 27 February 2020
Published : 18 March 2020
DOI : https://doi.org/10.1057/s41599-020-0420-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Short Essay on Health [100, 200, 400 Words] With PDF
In today’s lesson, I will discuss how you can write short essays on Health within different word limits. All the essays will be written here with a simplistic approach for a better understanding of all students.

Short Essay on Health in 100 Words
Health is an important aspect of one’s life. A person is considered healthy when he or she is free from illness or injury. Health can be categorised as physical health, mental health, emotional health, social health, et cetera. However, all these categories are interrelated.
While low physical activity can impact overall mental health, mental stress can adversely affect heart health and poor emotional health can deteriorate one’s quality of life. Being in good health enables a person to function optimally and live their life happily.
Some of the basic rules for maintaining good health include going to bed and waking up on time, exercising regularly, eating healthily and drinking at least eight glasses of water daily.
Short Essay on Health in 200 Words
Health is one of the most important aspects of one’s life. One can be a billionaire but if he is not in good health, he can not enjoy the luxuries that money can buy. Thus, health is considered as the real wealth. Health can be categorised as physical health, mental health, emotional health, social health, et cetera.
However, all these categories are interrelated and impact each other. For example, not exercising regularly can make a person irritable and cause mental health problems, while chronic stress can lead to health diseases and diabetes. Poor emotional and psychological health can also make people withdrawn and impact their overall health.
Being in good health enables a person to function optimally and live their life happily. When one feels healthy and is not troubled by pain or discomfort in the body, he can be more active, participate in various activities and be more present in the daily happenings. Being mentally in good health is also very important as suffering from anxiety, depression and other issues can severely deteriorate one’s quality of life.
One can easily improve his health by making some changes in his lifestyle. Some of the basic rules for maintaining good health include going to bed and waking up on time, exercising regularly, eating healthily and drinking a lot of water.
Short Essay on Health in 400 Words
Health is a key aspect of one’s life. A person is considered healthy when he is free from all illness and injury and can conduct his life well. One can be a billionaire but if he is not in good health, he can not enjoy the luxuries that money can buy. Thus, health is considered as the real wealth and being in good health is very important. Health can be categorised as physical health, mental health, emotional health, social health, et cetera.
Everyone can be healthy but good health does not come without the necessary discipline and care. Going to bed and waking up on time, exercising regularly, avoiding junk food, eating healthily, drinking a lot of water and getting some sunlight are a few good habits that can improve one’s health. However, it cannot be achieved in a day. One needs to change their lifestyle and practice healthy habits daily.
Sometimes, one’s external environment can also be the reason for their poor health. Living in shabby conditions, breathing in heavily polluted air, consuming unhygienic food and contaminated water can more often than not, result in bacterial, fungal and viral diseases. Hence, cleanliness is an important factor if one wants to be healthy. One should also take care of their diet and include greens and other nutritious food, limit their caffeine intake, stop smoking and drinking as well as follow the basic health protocols.
Good health is necessary if one wants to achieve their goal in life. One cannot study well or work hard when they are not feeling at ease or are suffering from pain. Adopting a healthy lifestyle makes us healthy and boosts our energy as well as immunity. Thus, good health is the key to enjoying a good life.
In this session above, I have mentioned everything that could be necessary to write short essays on Health. Through the simple words and sentences, I hope now you have understood the entire context. If you still have any doubts regarding this session, kindly let me know through some quick comments. If you want to read more such essays on various important topics, keep browsing our website.
Join our Telegram channel to get the latest updates on our upcoming sessions. Thank you.
More from English Compositions
- 100, 200, 400 Words Paragraph and Short Essay [With PDF]
- Write a Letter to the Editor Highlighting the Increasing Stress Faced by Students
- Madhyamik English Writing Suggestion 2022 [With PDF]
- Write a Letter to the Editor about Exam Stress
- Write a Letter to Your Friend Complimenting on his/her Recovery from Serious Illness
- [FREE PDF] From The Diary Of Anne Frank MCQs | CBSE Class 10 English Chapter 4 [TERM 1]
- Write an Application to the Principal for Your Mother’s Illness
- [FREE PDF] Nelson Mandela MCQs | CBSE Class 10 English Chapter 2 [TERM 1]
- Notice Writing Format, Type, Writing Tips, Examples [PDF]
- Short Essay on School games [100, 200, 400 Words] With PDF
- Short Essay on Our Class Teacher [100, 200, 400 Words] With PDF
- Short Essay on My Waste My Responsibility [100, 200, 400 Words] With PDF
- Share full article
Advertisement
Supported by
Guest Essay
Many Patients Don’t Survive End-Stage Poverty

By Lindsay Ryan
Dr. Ryan is an associate physician at the University of California, San Francisco, department of medicine.
He has an easy smile, blue eyes and a life-threatening bone infection in one arm. Grateful for treatment, he jokes with the medical intern each morning. A friend, a fellow doctor, is supervising the man’s care. We both work as internists at a public hospital in the medical safety net , a loose term for institutions that disproportionately serve patients on Medicaid or without insurance. You could describe the safety net in another way, too, as a place that holds up a mirror to our nation.
What is reflected can be difficult to face. It’s this: After learning that antibiotics aren’t eradicating his infection and amputation is the only chance for cure, the man withdraws, says barely a word to the intern. When she asks what he’s thinking, his reply is so tentative that she has to prompt him to repeat himself. Now with a clear voice, he tells her that if his arm must be amputated, he doesn’t want to live. She doesn’t understand what it’s like to survive on the streets, he continues. With a disability, he’ll be a target — robbed, assaulted. He’d rather die, unless, he says later, someone can find him a permanent apartment. In that case, he’ll proceed with the amputation.
The psychiatrists evaluate him. He’s not suicidal. His reasoning is logical. The social workers search for rooms, but in San Francisco far more people need long-term rehousing than the available units can accommodate. That the medical care the patient is receiving exceeds the cost of a year’s rent makes no practical difference. Eventually, the palliative care doctors see him. He transitions to hospice and dies.
A death certificate would say he died of sepsis from a bone infection, but my friend and I have a term for the illness that killed him: end-stage poverty. We needed to coin a phrase because so many of our patients die of the same thing.
Safety-net hospitals and clinics care for a population heavily skewed toward the poor, recent immigrants and people of color. The budgets of these places are forever tight . And anyone who works in them could tell you that illness in our patients isn’t just a biological phenomenon. It’s the manifestation of social inequality in people’s bodies.
Neglecting this fact can make otherwise meticulous care fail. That’s why, on one busy night, a medical student on my team is scouring websites and LinkedIn. She’s not shirking her duties. In fact, she’s one of the best students I’ve ever taught.
This week she’s caring for a retired low-wage worker with strokes and likely early dementia who was found sleeping in the street. He abandoned his rent-controlled apartment when electrolyte and kidney problems triggered a period of severe confusion that has since been resolved. Now, with little savings, he has nowhere to go. A respite center can receive patients like him when it has vacancies. The alternative is a shelter bed. He’s nearly 90 years old.
Medical textbooks usually don’t discuss fixing your patient’s housing. They seldom include making sure your patient has enough food and some way to get to a clinic. But textbooks miss what my med students don’t: that people die for lack of these basics.
People struggle to keep wounds clean. Their medications get stolen. They sicken from poor diet, undervaccination and repeated psychological trauma. Forced to focus on short-term survival and often lacking cellphones, they miss appointments for everything from Pap smears to chemotherapy. They fall ill in myriad ways — and fall through the cracks in just as many.
Early in his hospitalization, our retired patient mentions a daughter, from whom he’s been estranged for years. He doesn’t know any contact details, just her name. It’s a long shot, but we wonder if she can take him in.
The med student has one mission: find her.
I love reading about medical advances. I’m blown away that with a brain implant, a person who’s paralyzed can move a robotic arm and that surgeons recently transplanted a genetically modified pig kidney into a man on dialysis. This is the best of American innovation and cause for celebration. But breakthroughs like these won’t fix the fact that despite spending the highest percentage of its G.D.P. on health care among O.E.C.D. nations, the United States has a life expectancy years lower than comparable nations—the U.K. and Canada— and a rate of preventable death far higher .
The solution to that problem is messy, incremental, protean and inglorious. It requires massive investment in housing, addiction treatment, free and low-barrier health care and social services. It calls for just as much innovation in the social realm as in the biomedical, for acknowledgment that inequities — based on race, class, primary language and other categories — mediate how disease becomes embodied. If health care is interpreted in the truest sense of caring for people’s health, it must be a practice that extends well beyond the boundaries of hospitals and clinics.
Meanwhile, on the ground, we make do. Though the social workers are excellent and try valiantly, there are too few of them , both in my hospital and throughout a country that devalues and underfunds their profession. And so the medical student spends hours helping the family of a newly arrived Filipino immigrant navigate the health insurance system. Without her efforts, he wouldn’t get treatment for acute hepatitis C. Another patient, who is in her 20s, can’t afford rent after losing her job because of repeated hospitalizations for pancreatitis — but she can’t get the pancreatic operation she needs without a home in which to recuperate. I phone an eviction defense lawyer friend; the young woman eventually gets surgery.
Sorting out housing and insurance isn’t the best use of my skill set or that of the medical students and residents, but our efforts can be rewarding. The internet turned up the work email of the daughter of the retired man. Her house was a little cramped with his grandchildren, she said, but she would make room. The medical student came in beaming.
In these cases we succeeded; in many others we don’t. Safety-net hospitals can feel like the rapids foreshadowing a waterfall, the final common destination to which people facing inequities are swept by forces beyond their control. We try our hardest to fish them out, but sometimes we can’t do much more than toss them a life jacket or maybe a barrel and hope for the best.
I used to teach residents about the principles of internal medicine — sodium disturbances, delirium management, antibiotics. I still do, but these days I also teach about other topics — tapping community resources, thinking creatively about barriers and troubleshooting how our patients can continue to get better after leaving the supports of the hospital.
When we debrief, residents tell me how much they struggle with the moral dissonance of working in a system in which the best medicine they can provide often falls short. They’re right about how much it hurts, so I don’t know exactly what to say to them. Perhaps I never will.
Lindsay Ryan is an associate physician at the University of California, San Francisco, department of medicine.
Source photographs by Bettmann and Fred W. McDarrah via Getty Images.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
- International edition
- Australia edition
- Europe edition

Mental health is a measure of success, not a reason for politicians to sneer

Rishi Sunak’s attack on ‘overmedicalisation’ is ignoring the value we should be placing on our wellbeing
T here’s more to life than money, but societies can struggle to express it. When we talk about the state of nations and their citizens, we tend ultimately to boil it down to a few economic indicators. These can tell us a great deal, but they don’t quite tell us everything. The untouched stretch of ancient woodland, the arts in education, the close-knit community, the healthy childhood: there are plenty of valuable things that cannot always be weighed on this scale.
And this is a problem, particularly for people who want to hang on to those valuable things. Here’s a rule of thumb: if you can’t measure how much something is worth, it becomes tricky to protect it. Those who do not want to see a bluebell wood destroyed or another humanities subject ditched can find it hard to argue their case against the cold logic of pounds and pence. What yardstick can they use that will be taken seriously?
It’s not just activists for whom this is an issue. Governments have long flirted with the idea of an alternative to GDP, a way to capture what really matters to citizens. A “ happiness index ” was at one point a fashionable idea, but has proved too narrow and ambiguous. People often misunderstood what surveys were asking them – happiness can be hard to pin down. How do you weigh pleasure against contentment? What about meaning?
But I wonder whether over the past few years a solution has presented itself, almost without us noticing. Little by little, a sturdier, better evidenced and more widely applicable unit of value has emerged in public life: that of mental health. We all use it already.
Is it good for your mental health? This is the question by which increasingly large parts of our lives are evaluated. The language of psychology has spread so that it covers almost all human activity, from the quality of our workplaces, to the state of teenagers, to the way we spend our free time, to the manner in which we engage with our friends. If politicians are looking for a new way to measure what is important to us, they only have to open their ears.
Take, for example, the simple hobby. People no longer merely go for a walk, take up birdwatching, adopt a pet or learn to bake cakes. Instead, they discover a form of self-care that conquers their anxiety, changes their life or saves their marriage. This is what we aspire to, now, in our free time – a radical overhaul of our mental health. Just look at the books hobbyists are writing these days. Sample: Hooked: How Crafting Saved My Life ; Thirty-Thousand Steps: A Memoir of Sprinting Toward Life After Loss ; Dinner for One: How Cooking in Paris Saved Me .
The arts, too, are increasingly framed as aides to wellbeing. Why invest in a gallery pass ? It’s good for your mental health. Why take up an instrument or learn to paint ? It’s good for your mental health. Where once art was dedicated to the glory of God, now it is laid on the altar of mental wellbeing, which might well be the religion of our secular age. (The archbishop of Canterbury once complained that Christ the saviour had become Christ the counsellor .)
Even fictional characters are these days evaluated in terms of their mental health. The writer Parul Sehgal has noted the rise of the trauma plot , which does not “direct our curiosity toward the future (will they or won’t they?) but back into the past (what happened to her?).” And we do this to real-life characters too. Channel 4’s recent The Rise and Fall of Boris Johnson is one in a long series of probes into the former prime minister that attempts to locate his future actions somewhere in his childhood. Tabloids used to fill their pages with claims about what gives you cancer (intermittent fasting, red wine, hot tea) or helps stave it off (intermittent fasting, red wine, hot tea). Now the story is wellbeing. What helps? What hinders?
Now, it is easy to scoff at all this, and plenty do. Many are turned off by the spread of this newfangled language and what they see as the co-option of common sense. (What happened to just going for a swim or seeing your mates? Isn’t this “mental health” stuff all rather obvious?) Indeed, this scepticism was probably the basis for a nascent culture war launched last week by Rishi Sunak, who announced a plan to withdraw disability benefits from some people with mental health conditions , in a bid to tackle the “overmedicalising [of] the everyday challenges of life”.
But these critics – and that solution – badly miss the mark. Learning more about our mental health, what helps and what doesn’t, is in fact rather useful. This knowledge was once the preserve of academics and those who could afford therapy; now anyone can get hold of it.
This can only be a good thing. The evidence base may not be complete, but it is weighty and increasing all the time. The solution to “overmedicalisation” is surely not to ditch people in need but to continue to improve our understanding of mental health. And we shouldn’t presume, either, that complex large-scale societies always proceed in a healthy “commonsense” direction; it is new research into mental health that is guiding us back to “commonsense” practices – seeing your mates more, going for a swim outside – that we were in danger of leaving in the past.
If we want an alternative unit of value by which to assess and guide a society, we could do worse than the mental health of its citizens. In a way, we’ve already adopted it. Despite Sunak’s posturing, mental health is a potent political tool. It was only recently that he launched a crackdown on mobile phones in schools on the basis that they harm children’s mental health.
Mental health impact is the reason we now take loneliness seriously . It is the metric by which we increasingly judge workplaces; the government has previously urged employers to improve support. It is the justification for keeping hold of green spaces and, increasingly, for caring about the environment in the first place. We already measure ourselves by our mental health. Time to put that to use.
- Mental health
Most viewed
- Open access
- Published: 18 April 2024
Implementation of an audit and feedback module targeting low-value clinical practices in a provincial trauma quality assurance program: a cost-effectiveness study
- Blanchard Conombo 1 , 2 ,
- Jason R. Guertin 1 ,
- Jeffrey S. Hoch 3 ,
- Jeremy Grimshaw 4 ,
- Mélanie Bérubé 2 , 5 ,
- Christian Malo 5 ,
- Simon Berthelot 2 , 6 , 7 ,
- François Lauzier 8 ,
- Henry T. Stelfox 9 ,
- Alexis F. Turgeon 2 , 8 ,
- Patrick Archambault 10 , 6 ,
- Amina Belcaid 2 &
- Lynne Moore 1 , 2
BMC Health Services Research volume 24 , Article number: 479 ( 2024 ) Cite this article
90 Accesses
Metrics details
Audit and Feedback (A&F) interventions based on quality indicators have been shown to lead to significant improvements in compliance with evidence-based care including de-adoption of low-value practices (LVPs). Our primary aim was to evaluate the cost-effectiveness of adding a hypothetical A&F module targeting LVPs for trauma admissions to an existing quality assurance intervention targeting high-value care and risk-adjusted outcomes. A secondary aim was to assess how certain A&F characteristics might influence its cost-effectiveness.
We conducted a cost-effectiveness analysis using a probabilistic static decision analytic model in the Québec trauma care continuum. We considered the Québec Ministry of Health perspective. Our economic evaluation compared a hypothetical scenario in which the A&F module targeting LVPs is implemented in a Canadian provincial trauma quality assurance program to a status quo scenario in which the A&F module is not implemented. In scenarios analyses we assessed the impact of A&F characteristics on its cost-effectiveness. Results are presented in terms of incremental costs per LVP avoided.
Results suggest that the implementation of A&F module (Cost = $1,480,850; Number of LVPs = 6,005) is associated with higher costs and higher effectiveness compared to status quo (Cost = $1,124,661; Number of LVPs = 8,228). The A&F module would cost $160 per LVP avoided compared to status quo. The A&F module becomes more cost-effective with the addition of facilitation visits; more frequent evaluation; and when only high-volume trauma centers are considered.
A&F module targeting LVPs is associated with higher costs and higher effectiveness than status quo and has the potential to be cost-effective if the decision-makers’ willingness-to-pay is at least $160 per LVP avoided. This likely represents an underestimate of true ICER due to underestimated costs or missed opportunity costs. Results suggest that virtual facilitation visits, frequent evaluation, and implementing the module in high-volume centers can improve cost-effectiveness.
Peer Review reports
Introduction
Low-value practices (LVPs) are tests and treatments that are not supported by evidence and may expose patients to physical and psychological harm [ 1 , 2 ]. They have been estimated to consume up to 30% of healthcare resources in Canada [ 3 ] and in the US [ 4 ]. In 2013, an estimated $270 billion was wasted on excess healthcare services in the US [ 2 ]. From a patient and caregiver perspective, LVPs expose patients to physical and psychological harms, delays to effective treatment, and direct and indirect expenses [ 2 , 5 , 6 , 7 , 8 ]. From a healthcare system perspective, they put strain on tight healthcare budgets and decrease the availability of scarce resources.
Recent literature suggests that interventions targeting the de-implementation of ineffective or harmful health interventions have the potential to reduce overuse and improve clinically important outcomes [ 9 ]. Among these are Audit and Feedback (A&F) interventions, defined as ‘a summary of clinical performance of healthcare over a specified period aimed at providing information to health professionals to allow them to assess and adjust their performance’ [ 10 ]. We now have extensive evidence of the effectiveness of A&F interventions, including those targeting de-implementation of LVPs. A systematic review including 140 randomized controlled trials (RCTs) estimated that A&F interventions resulted in close to 4.3% absolute increase in adherence to evidence-based care (IQR 0.5% to 16.0%) [ 11 ]. The effect of an A&F intervention appears to be larger when it targets de-implementation of low-value practices (absolute decrease of 10.5%). This review also revealed that A&F effectiveness is influenced by its design and delivery [ 11 ]. The World Health Organisation recently expressed concern about the major knowledge gap on the cost and cost-effectiveness of A&F interventions [ 12 ], and recommended that implementation of these interventions be informed by data on their cost-effectiveness [ 13 ]. Despite this, most A&F interventions, including those used across Canadian trauma systems, are implemented without evidence on their cost-effectiveness [ 12 , 14 ]. A 2022 systematic review summarized evidence on the economic value of A&F interventions in healthcare [ 15 ] and found that they have a high potential to be cost-effective. However, authors only identified economic evaluations for 6% of A&F trials, methodological quality of these evaluations was low, and authors concluded that model-based simulations were urgently needed to assess the impact of A&F characteristics on cost-effectiveness to inform optimal A&F design.
Trauma systems are a favorable setting for de-implementation interventions as they possess many documented facilitators including quality improvement teams with medical leadership, routinely-collected clinical data, and performance linked to accreditation [ 16 ]. Furthermore, potential gains are huge due to the resource-intensive nature of trauma care. Trauma systems are thus the ideal setting to advance knowledge on de-implementation. Our research team recently published a list of quality indicators targeting LVPs in acute trauma care [ 17 , 18 ]. We aim to evaluate the cost-effectiveness of an A&F module targeting the de-implementation of these LVPs in an integrated Canadian trauma system and to assess the impact of A&F characteristics on cost-effectiveness.
We conducted an economic evaluation according to the Canadian guidelines for the Economic Evaluation of Health Technologies [ 19 ], and results are reported following the CHEERS 2022 statement [ 20 ]. The study protocol was developed with a project advisory committee including two emergency physicians (CM, EM), two trauma surgeons (TR, NY), three critical care physicians (FL, AFT, HTS), a neurosurgeon (PLB), a spine surgeon (JP), an orthopedic surgeon (ML), two trauma service managers (MB, CR), a trauma registry co-ordinator (AB), and epidemiologist (LM), and two health economists (JRG, JSH). The protocol was approved a priori by all co-authors, members of the advisory committee, a granting agency peer-review committee (Canadian Institutes of Health Research project #353374) and the CHU-de Québec – Université Laval research ethics committee.
Our economic evaluation is based on a hypothetical A&F module embedded in the Québec Trauma Care Continuum , a provincial regionalized trauma system comprising 57 adult trauma centers of which 3 are level I (highly specialized urban centers), 5 are level II (similar capacity to level I but in smaller cities), 21 are level III (hospitals in small towns transferring most major trauma to level I/II centers after stabilization), and 28 are level IV (rural community hospitals). All centers undergo mandatory, periodic verifications in line with designation, conducted by the provincial healthcare quality agency, Institut national d’excellence en santé et services sociaux ( INESSS ) and overseen by the Ministry of Health and Social Services [ 21 ]. Verification includes A&F on adherence to high-value care and risk-adjusted outcomes. Local trauma committees in each center are required to ensure the quality of the trauma program according to designation requirements. Committees include the program medical director (Chair), the program manager, heads of critical care, emergency and surgical departments, heads of multidisciplinary services, and a hospital administrator. Quality improvement activities include trimestral committee meetings with chart review, development of local care protocols, and discussions with clinical and administrative leads locally and at referring centers to identify improvement strategies. Formal letters of agreement are signed by heads of clinical departments to operate changes in their services when required.
Intervention and comparator
We compared a hypothetical scenario in which an A&F module targeting LVPs is implemented in the Québec trauma system to a status quo scenario in which the A&F module is not implemented.
Comparator (status quo scenario)
The study comparator is the A&F intervention currently in place in the Québec Trauma Care Continuum, designed by the provincial healthcare quality agency using the US Agency for Healthcare Research and Quality guidelines [ 22 ]. This A&F intervention targets trauma committees in each trauma center and, as explained above, currently includes modules for adherence to high-value practices (15 quality indicators) and optimal outcomes (3 quality indicators). The A&F intervention currently in place consists of:
Quality reports disseminated via a Web platform to local trauma committees and hospital boards of directors produced using trauma registry data.
Web links to user-friendly information sheets including definitions for quality indicators and references supporting each indicator.
Information sheets and Web capsules with guidelines on how the results should be interpreted and acted upon.
A case revision tool integrated into the trauma registry.
Within 6 months of reception of the report, committees are required to submit an action plan proposing improvement strategy for quality indicators for which they are identified as negative outliers.
Intervention
The study intervention is an A&F module targeting LVPs (6 quality indicators) ( http://www.ohri.ca/auditfeedback/laboratories/ ). The 6 quality indicators were selected using the results of an expert consensus study [ 23 ] and an indicator validation study using data from the Quebec trauma registy [ 24 ].
In the base case scenario, the module includes the components already in place described in the status quo scenario, applied to quality indicators on LVPs. We attributed a 5-year lifespan to the A&F module as current literature recommends that quality indicators be updated every five years [ 25 ]. To account for the 5-year lifespan of the A&F module and its potential benefits one year beyond its lifespan, we used a 6-year time horizon.
Type of economic evaluation
For this early economic evaluation, i.e., an evaluation prior to the implementation of the module, a probabilistic static decision analytic model was developed to estimate the incremental cost-effectiveness ratio (ICER) of the A&F module compared with status quo scenario in which the A&F module is not implemented for patients with acute injury (Fig. 1 ). We considered the Québec Ministry of Health perspective.
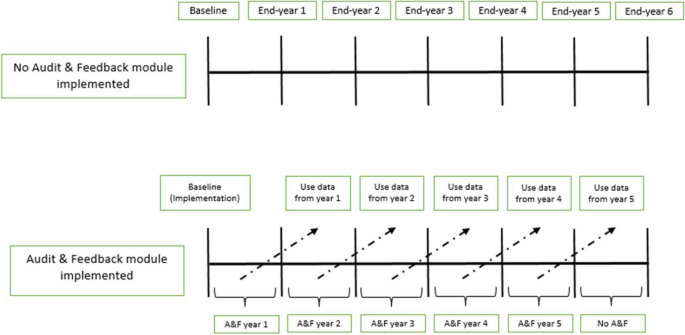
Decision-analytic model. In the status quo scenario, there is no implementation of the A&F module targeting LVPs. In the intervention scenario, an A&F module targeting LVPs is implemented at baseline (at the beginning of the 1st year). “Use data from year 1” means that data on the effectiveness and costs of A&F module from the 1st year are available at the beginning of the second year and so on for the following years
Effectiveness
The incremental effectiveness of the A&F module was estimated as the incremental number of LVPs avoided. Plausible ranges of percent reductions in LVPs were obtained from the 2012 Cochrane review, which presented effectiveness of A&F interventions as medians and interquartile ranges [ 26 ]. Specifically, we used the pooled estimate of effectiveness specific to deimplementation interventions based on 29 studies. For the purposes of our analysis, these values were used to estimate mean effectiveness and associated standard errors using a method based on highly-cited recommendations [ 27 , 28 ].
The incremental costs of the A&F module over the comparator were estimated by summing the implementation costs of the A&F module over its 5-year lifespan and the potential reduction in resource utilization for all LVPs, valued in costs and estimated between years 2 and 6. The implementation costs were determined by identifying all non-recurrent and recurrent costs related to the implementation of the A&F module including data validation and analyses, report production and validation, administrative costs, and follow-up in local trauma committees (Table 1 ). The potential reduction in resource utilization was estimated by multiplying the hypothesized reduction in the frequency of the LVPs by their average costs. Detailed information on how practices were costed are available elsewhere [ 29 ]. Briefly, we estimated direct healthcare costs for each LVP from the Ministry of Health perspective using an activity-based costing approach. Activity-based costing involves multiplying unit costs of specific activity centres by the corresponding units of resources used. This method provides an estimate of hospital resource use by activity center, consistent with Grading of Recommendations Assessment, Development and Evaluations guidelines [ 30 , 31 , 32 ]. All costs are expressed in 2020 Canadian dollars. We report our study following the Consolidated Health Economic Evaluation Reporting Standards statement [ 29 ].
Incremental cost-effectiveness ratio
The incremental cost-effectiveness ratio (ICER) was estimated by dividing the incremental costs (or savings) of the A&F module by its incremental effectiveness. Results are reported as the incremental cost per LVP avoided.
Discount rate
All future costs and benefits were discounted at a rate of 1.5% as recommended by current Canadian guidelines [ 19 ].
Scenario analyses
Our advisory committee identified 6 scenario-specific sensitivity analyses based on published evidence of A&F effectiveness and context-specific considerations (#1, 2, 3, 6) [ 24 , 26 ] as well as Canadian guidelines on economic evaluation (#4, 5):
Adding a virtual facilitation visit once per cycle to help trauma committees identify barriers and facilitators and use them to identify improvement strategies for their action plan; [ 15 , 26 ]
Increasing feedback frequency from annually to monthly, as assessed in the systematic review; [ 26 ]
Implementing the module only in high-volume trauma centers (i.e., level I and II);
Varying the discount rate between 0 and 5%, as recommended by current Canadian guidelines; [ 19 ]
Increasing the lifespan of the A&F module to 10 years (Supplementary Fig. 1 ) to take into account the effect of time on module effectiveness.
Increasing the costs of LVPs by 100% to account for lack of complete data on physician billing and unit costs that underestimate market prices. This is based on evidence that physician billing represents approximately 56% of hospital costs in Canada ( https://www.cihi.ca/sites/default/files/document/nhex-trends-2020-narrative-report-en.pdf ).
We present the ICER based on the results of probabilistic sensitivity analysis (PSA) as recommended in the Canadian Guidelines for the Economic Evaluation of Health Technologies [ 19 ]. In the PSA, model parameters were represented by distributions of possible values rather than point estimates to address parameter uncertainty. All parameters and their distributions are presented in Table 2 . Parameter distributions were randomly sampled 10,000 times. Results were summarized using cost-effectiveness acceptability curves (CEACs) and the cost-effectiveness acceptability frontier (CEAF) [ 33 ]. We used Excel software (Microsoft Office 2019 Professional Plus) to construct a decision model, to analyze base case results, and conduct PSA.
The mean costs of the A&F module and status quo scenario were $1,480,850 and $1,124,661 respectively. The associated average number of LVPs were 6,005 for the A&F module and 8,228 for status quo scenario. The implementation of the A&F module is associated with a reduction of approximately 2,223 LVPs. The ICER for the A&F module versus status quo scenario was $160 per LVP avoided (Table 3 ). The results of the PSA plotted on a cost-effectiveness plane (Fig. 2 ) show that most of the points in the scatter plot are located in the Northeast quadrant, indicating that the A&F module has a potential to be cost-effective given a decision maker’s willingness-to-pay (WTP). The cost-effectiveness acceptability frontier indicates that A&F module is cost-effective in 50% of our iterations at a WTP of $160 per LVP avoided (Fig. 3 ).
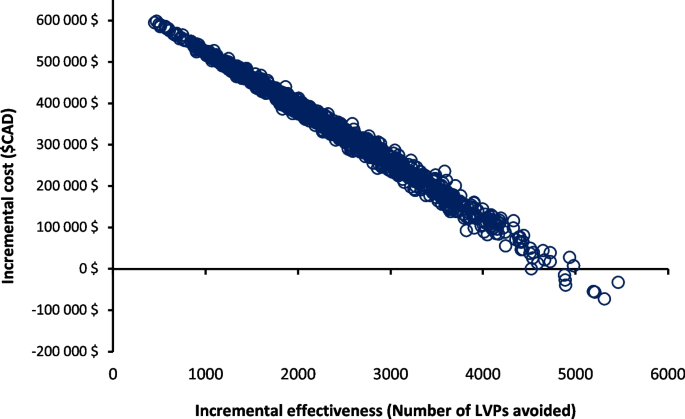
Probabilistic sensitivity analysis comparing A&F module and status quo scenario (no A&F module targeting LVPs). The x-axis represents the incremental effectiveness, number of LVPs avoided. The y-axis represents the incremental costs between A&F module and status quo scenario. Each circle represents a single simulation for a total of 10,000 simulations
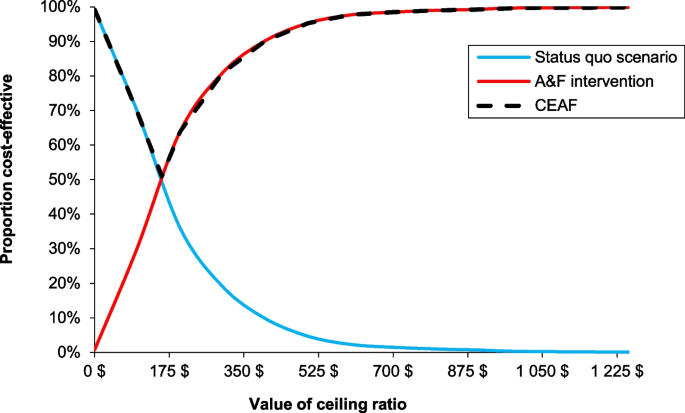
Cost-effectiveness acceptability curve (CEAC) between A&F module and status quo scenario and cost-effectiveness acceptability frontier (CEAF). The x-axis represents the willingness-to-pay (WTP) for each LVP avoided. The y-axis represents the percentage of simulations in which the A&F module is cost-effectiveness relative to the status quo scenario at different WTP threshold. The switch point where the A&F module became a cost-effective intervention corresponds to $160 per LVP avoided, equal to the ICER estimate. A&F module became 100% cost-effective at a WTP of $1000 per LVP avoided. The A&F module had the highest expected net benefit, for all values of WTP greater than the ICER. At our ICER estimate, 50% of the distribution of ICERs were cost-effective
Adding a virtual facilitation visit to the A&F module (one visit per A&F cycle) would reduce the estimated ICER (improve its cost-effectiveness profile compared to the base case scenario) to $108 per LVP avoided (Table 4 ). More frequent feedback (monthly) is associated with a slight improvement in its cost-effectiveness profile ($154 per LVP avoided). The A&F module is more cost-effective ($48 per LVP avoided) when only high-volume trauma centers are considered for the implementation of the module. Similarly, an increase in the costs of LVPs by 100% and a longer time horizon would lead to a reduction in the ICER to $10 and $106 per LVP avoided, respectively. On the other hand, a discount rate of 5% increases the ICER to $199 per LVP avoided (Table 4 ).
The results of this early economic evaluation suggest that the addition of an A&F module targeting LVPs to a provincial trauma quality assurance program over a time horizon of 6 years is associated with an ICER of $160 per LVP avoided. In analyses that simultaneously accounted for uncertainty in all key model parameters, 50% of simulations were cost-effective at a WTP of $160 per LVP avoided. The A&F module is more cost-effective with the addition of facilitation visits, frequent evaluation and if restricted to high-volume trauma centers.
Our study fills a major knowledge gap on the potential cost-effectiveness of A&F interventions to de-implement low-value care. Comparison of our results with the literature on acute trauma care is difficult, because there are no studies that have assessed the cost-effectiveness profile of A&F interventions in the context of acute injury care. However, a 2022 systematic review on the economic value of A&F interventions in various health areas summarized results of 35 studies that compared different A&F strategies targeting health professionals compliance with desire practices or patient health outcomes [ 15 ]. The results of this systematic review mirror our findings. Of 14 cost-effectiveness analyses based on changes in compliance to desired practice from the public healthcare payer perspective, 12 (86%) studies found that the A&F interventions were more costly but more effective than the comparator [ 15 ]. From studies assessing de-implementation of LVPs [ 34 , 35 ], A&F interventions were associated with a reduction in the overuse of LVPs and had the potential to be cost-effective [ 34 , 35 ]. Four (28%) studies included in the review conducted simulations to assess the influence of A&F characteristics on cost-effectiveness in scenario analyses [ 34 , 35 , 36 , 37 ]. Despite having different comparator groups (do-nothing scenario), these studies also observed improved cost-effectiveness when facilitation visits are added to A&F intervention [ 35 ] and the time horizon of the intervention is increased to 9 months (4 to 9 months) [ 34 ]. In addition, our study provides evidence that cost-effectiveness of A&F interventions may be improved by increasing frequency and restricting the intervention to high volume hospitals.
Strengths and limitations
Our study is based on effectiveness parameters from a meta-analysis on over 140 RCTs on the effectiveness of A&F interventions in different healthcare settings [ 11 ], on observed data on the frequency of LVPs [ 24 ], and on costs based on a mature, province-wide quality assurance program ( https://www.donneesquebec.ca/recherche/dataset/as-471-rapports-financiers-annuels-des-etablissements ). In addition, we conducted extensive sensitivity analyses and a range of scenario analyses to evaluate the robustness of our results and to assess the influence of key A&F characteristics on its cost-effectiveness profile. Despite these strengths, our results should be interpreted within the context of the study’s limitations. First, our evaluation is based on estimates of effectiveness from a meta-analysis published in 2012. While this study represents the most up-to-date evidence synthesis available (the Cochrane review is yet to be updated [ 38 ] and systematic reviews published more recently have not included meta-analyses) [ 39 ], it does not include the most recent evidence. Furthermore, while we used estimates specific to deimplementation interventions from the review, none of the studies were specific to trauma, none evaluated an intervention delivered in the context of accreditation, and none compared a deimplementation module in a system with an A&F intervention already in place. Furthermore, risk of bias was low for only 31% of included studies. The estimate used may therefore represent an underestimate or overestimate of the true effectiveness. Second, we conducted an early economic evaluation to assess if a hypothetical A&F module could be cost-effective and, if so, under which conditions. As such, the results of our economic evaluation provide encouragement that the true ICER of the intervention were it to be designed and implemented in the Québec trauma system might be promising as well. We used a broad range of scenarios and parameter values within our probabilistic sensitivity analyses but attributed the same weight to all scenarios analyzed. The base-case scenario will not necessarily be the one that will be implemented. However, intervention costs were based on resources currently used in the Québec trauma care continuum and opportunity costs related to LVPs avoided were based on observed baseline frequencies. We plan to conduct an economic evaluation after our cluster randomized trial (funded and currently underway) to assess the true (observed) cost-effectiveness of the intervention in a pragmatic setting. Third, opportunity costs of LVPs avoided did not fully account for physician fees and were based on unit costs that are known to underestimate their true costs. In addition, we did not account for potential resource repercussions of LVPs, for example, re-imaging due to uncertain findings or treatment of clinically nonsignificant incidental findings. Our scenario analysis where costs associated with LVPs were increased by 100% probably better reflects the Québec Ministry of Health perspective; the large decrease in the ICER ($160 to $10) suggest that opportunity costs related to LVPs are an important determinant of the cost-effectiveness of an A&F module targeting de-implementation. Furthermore, we only considered direct healthcare costs associated with the two competing strategies and did not factor in the effects of indirect costs (e.g., time off work for patients) from LVPs, which would also have led to an underestimation of the intervention’s cost-effectiveness. Fourth, our study is based on the single healthcare payer model, and it is uncertain if our findings would be applicable to other jurisdictions with alternate payer systems. Also, physicians in Canada receive payments based on fee for service that is periodically negotiated [ 40 ], so our results are dependent on current unit costs in our system and may not apply well in non-universal health systems or other jurisdictions with different structures. Fifth, in the absence of evidence indicating otherwise, our base case scenario was based on the strong assumption that effectiveness was the same for all 6 indicators. However, in probabilistic sensitivity analyses, we allowed the effectiveness of LVP to vary independently. Sixth, we were unable to take account of the uncertainty of the cost estimates of implementing the A&F module, derived from expert consultation, which we anticipate may have been underestimated. Finally, we deliberately focused on adherence to desired practice (LVPs avoided) rather than health outcomes (e.g., adverse events) due to lack of available data associated with utility/disutility of LVPs for trauma patients. Nevertheless, a strong argument can be made for focus on the measurement of LVPs avoided for assessment of the quality of our A&F intervention, as they relate most closely to actions that are within the control of healthcare professionals. Indeed, economic evaluations of similar A&F interventions have obtained more meaningful results with similar intermediate outcomes than with Quality-Adjusted Life Years (QALYs) [ 41 ]. Studies have also demonstrated that reducing LVPs will reduce physical harms and adverse events [ 42 , 43 , 44 ]. However, this probably led to an underestimation of the true cost-effectiveness profile of our A&F module as health outcomes or negative health consequences of LVPs are not considered in the measure of effectiveness [ 15 ].
Potential impact
The outcome parameter used in decision model (LVPs avoided) is unique and does not have an explicit cost-effectiveness threshold associated with it. Therefore, the decision to invest in the intervention will be based on the decision-makers willingness-to-pay, i.e., would they be prepared to invest 160$ per LVP avoided? However, the decision should also be based on other considerations, e.g., opportunity costs are likely to be greater than those estimated, cost-effectiveness may be increased if virtual facilitation visits are added, if the frequency of evaluations are increased, and if the intervention is restricted to high-volume trauma centers (level I and II). The intervention has the potential to lead to a global awareness of healthcare overuse and therefore a decrease in other LVPs [ 24 ].
Our economic evaluation suggests that an A&F module targeting de-implementation, integrated into a provincial quality-assurance program, has a high potential to reduce LVPs while increasing total healthcare costs, with an ICER of $160 per LVP avoided. Results suggest that virtual facilitation visits, frequent evaluation and implementing the intervention only in high-volume centers increase cost-effectiveness. However, its economic potential is likely underestimated in this study due to opportunity costs that were underestimated (costs of LVPs) or not accounted for (indirect costs, health outcomes, and long-term consequences). The findings of the present study may inform the development of A&F interventions targeting de-implementation and they demonstrate the feasibility of conducting early economic evaluations to inform optimal A&F intervention design.
Availability of data and materials
Quebec Trauma Registry is subject to a third-party restriction (Quebec Ministry of Health and Social Services).
Abbreviations
Low-value practices
Audit and Feedback
Randomized Controlled Trial
Willingness-to-pay
Computed tomography
Interquartile Range
Cost-effectiveness acceptability curve
Cost-effectiveness acceptability frontier
Probability sensitivity analysis
Choosing Wisely. Home page. Accessed February 21, 2022. https://www.choosingwisely.org/ .
Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156–68.
Article PubMed PubMed Central Google Scholar
Canadian Institute for Health Information. CIHI. unnecessary care in Canada: technical report. Ottawa, ON: CIHI, 2017.
Lown Institute. Low-value care. https://lowninstitute.org/lown-issues/low-value-care/ . Accessed 20 Dec 2022.
Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–6.
Article CAS PubMed Google Scholar
Boat TF, Chao SM, O’Neill PH. From waste to value in health care. JAMA. 2008;299(5):568–71.
Reilly BM, Evans AT. Much ado about (doing) nothing. Ann Intern Med. 2009;150(4):270–1.
Article PubMed Google Scholar
Hauser CJ, Adams CA Jr, Eachempati SR. Surgical Infection Society guideline: prophylactic antibiotic use in open fractures: an evidence-based guideline. Surg infect. 2006;7(4):379–405.
Article Google Scholar
Niven DJ, Mrklas KJ, Holodinsky JK, et al. Towards understanding the de-adoption of low-value clinical practices: a scoping review. BMC Med. 2015;13:255.
World Health Organization. Using audit and feedback to health professionals to improve the quality and safety of health care. https://apps.who.int/iris/handle/10665/332014 . Accessed 20 Dec 2022.
Noah I. Optimizing Audit and Feedback Interventions to Improve Quality in Primary Care. 2014.
Flottorp S, Jamtvedt G, Gibis B, McKee M. Using audit and feedback to health professionals to improve the quality and safety of health care. http://www.euro.who.int/__data/assets/pdf_file/0003/124419/e94296.pdf . Published 2010. Accessed.
Soleymani F, Rashidian A, Dinarvand R, Kebriaeezade A, Hosseini M, Abdollahi M. Assessing the effectiveness and cost-effectiveness of audit and feedback on physician’s prescribing indicators: study protocol of a randomized controlled trial with economic evaluation. Daru. 2012;20(1):88–88.
Avery AJ, Rodgers S, Cantrill JA, et al. A pharmacist-led information technology intervention for medication errors (PINCER): a multicentre, cluster randomised, controlled trial and cost-effectiveness analysis. Lancet. 2012;379(9823):1310–9.
Moore L, Guertin JR, Tardif P-A, et al. Economic evaluations of audit and feedback interventions: a systematic review. BMJ Qual Saf. 2022;31(10):754.
Squires JE, Sullivan K, Eccles MP, Worswick J, Grimshaw JM. Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement Sci. 2014;9(1):152.
Fitch K, Bernstein JS, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User's Manual. https://www.rand.org/pubs/monograph_reports/MR1269.html . Published 2001. Accessed 17 Sept 2018.
Heyworth J. Trauma services in a district general hospital. BMJ (Clinical research ed). 1990;300(6728):876–7.
CADTH. Guidelines for the economic evaluation of health technologies: Canada. 4th edition. Ottawa: CADTH; 2017.
Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BMJ (Clinical research ed). 2022;376:e067975.
PubMed Google Scholar
Ministère de la Santé et des Services sociaux. Trajectoire - Traumatologie. https://www.msss.gouv.qc.ca/professionnels/soins-et-services/guide-urgences-trajectoire-traumatologie/ . Published 2022. Accessed 13 Sept 2022.
Developing a framework and research agenda for overuse and appropriateness measures. Agency for Healthcare Research and Quality Appropriateness Small Conference. Published 2009. Accessed 17 Sept 2018.
Moore L, Bérubé M, Tardif PA, et al. Quality Indicators targeting low-value clinical practices in trauma care. JAMA Surg. 2022;157(6):507–14.
Moore L, Bérubé M, Tardif PA, et al. Validation of quality indicators targeting low-value trauma care. JAMA Surg. 2022;157(11):1008–16.
Stelfox HT, Straus SE. Measuring quality of care: considering measurement frameworks and needs assessment to guide quality indicator development. J Clin Epidemiol. 2013;66(12):1320–7.
Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Datab Syst Rev. 2012;6:Cd000259.
Google Scholar
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135.
Conombo B, Guertin JR, Hoch JS, et al. Potential avoidable costs of low-value clinical practices in acute injury care in an integrated canadian provincial trauma system. JAMA Surg. 2023;158(9):977–9.
Canby JBT. Applying activity-based costing to healthcare settings. Healthc Financ Manag. 1995;49(2):50–2 54-56.
Chan YC. Improving hospital cost accounting with activity-based costing. Health Care Manage Rev. 1993;18(1):71–7.
Guyatt GH, Oxman AD, Kunz R, et al. Incorporating considerations of resources use into grading recommendations. BMJ. 2008;336(7654):1170–3.
Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001;10(8):779–87.
Ling R, Giles M, Searles A. Administration of indwelling urinary catheters in four Australian Hospitals: cost-effectiveness analysis of a multifaceted nurse-led intervention. BMC Health Serv Res. 2021;21(1):897.
Gandjour A, Lauterbach KW. When is it worth reducing overuse of health care services? The example of prescribing expensive antihypertensives. Med Klin (Munich). 2005;100(9):535–41.
Barasa EW, Ayieko P, Cleary S, English M. A multifaceted intervention to improve the quality of care of children in district hospitals in Kenya: a cost-effectiveness analysis. PLoS Med. 2012;9(6):e1001238.
Huis A, Schoonhoven L, Grol R, Donders R, Hulscher M, van Achterberg T. Impact of a team and leaders-directed strategy to improve nurses’ adherence to hand hygiene guidelines: a cluster randomised trial. Int J Nurs Stud. 2013;50(4):464–74.
Crawshaw J, Meyer C, Antonopoulou V, et al. Identifying behaviour change techniques in 287 randomized controlled trials of audit and feedback interventions targeting practice change among healthcare professionals. Implement Sci. 2023;18(1):63.
Dunsmore J, Duncan E, MacLennan S, N’Dow J, MacLennan S. Effectiveness of de-implementation strategies for low-value prescribing in secondary care: a systematic review. Implement Sci Commun. 2023;4(1):115.
Ridic G, Gleason S, Ridic O. Comparisons of health care systems in the United States. Germany Canada Mater Sociomed. 2012;24(2):112–20.
Elliott RA, Putman Kd Fau - Franklin M, Franklin M Fau - Annemans L, et al. Cost effectiveness of a pharmacist-led information technology intervention for reducing rates of clinically important errors in medicines management in general practices (PINCER). (1179–2027 (Electronic)).
Elliott RA, Putman KD, Franklin M, et al. Cost effectiveness of a pharmacist-led information technology intervention for reducing rates of clinically important errors in medicines management in general practices (PINCER). Pharmacoeconomics. 2014;32(6):573–90.
Johri M, Ng ESW, Bermudez-Tamayo C, Hoch JS, Ducruet T, Chaillet N. A cluster-randomized trial to reduce caesarean delivery rates in Quebec: cost-effectiveness analysis. BMC Med. 2017;15(1):96.
Rodriguez-Martinez CE, Sossa-Briceño MP, Castro-Rodriguez JA. Cost-effectiveness of the utilization of “good practice” or the lack thereof according to a bronchiolitis evidence-based clinical practice guideline. J Eval Clin Pract. 2019;25(4):682–8.
Download references
Acknowledgements
We thank Natalie Yanchar, Éric Mercier, Jérôme Paquet, Tarek Razek, Martin Lesieur, Paule Lessard Boneaventure and Christine Rizzo for their role as members of the advisory committee.
Role of funder/sponsor
The funders had no role in developing this manuscript.
This research was supported by the Canadian Institutes of Health Research (Foundation grant, #353374).
Author information
Authors and affiliations.
Department of Social and Preventative Medicine, Université Laval, Québec City, Québec, Canada
Blanchard Conombo, Jason R. Guertin & Lynne Moore
Population Health and Optimal Health Practices Research Unit, Trauma – Emergency – Critical Care Medicine, Quebec University Hospital, Centre de Recherche du CHU de Québec-Université Laval, 18E Rue, Local H-012a, Québec City, Québec, 1401G1J 1Z4, Canada
Blanchard Conombo, Mélanie Bérubé, Simon Berthelot, Alexis F. Turgeon, Amina Belcaid & Lynne Moore
Division of Health Policy and Management, Department of Public Health Sciences, University of California at Davis, Davis, CA, USA
Jeffrey S. Hoch
Department of Medicine, University of Ottawa, Ottawa, ON, Canada
Jeremy Grimshaw
Faculty of Nursing, Université Laval, Québec City, Québec, Canada
Mélanie Bérubé & Christian Malo
Department of Family Medicine and Emergency Medicine, Université Laval, Québec City, Québec, Canada
Simon Berthelot & Patrick Archambault
Centre de Recherche Intégrée Pour Un Système Apprenant en Santé Et Services Sociaux, Centre Intégré de Santé Et de Services Sociaux de Chaudière-Appalaches, Lévis, Québec, Canada
Simon Berthelot
Department of Anesthesiology and Critical Care Medicine, Division of Critical Care Medicine, Université Laval, Québec City, Québec, Canada
François Lauzier & Alexis F. Turgeon
Department of Critical Care Medicine, Medicine and Community Health Sciences, O’Brien Institute for Public Health, University of Calgary, Calgary, AB, Canada
Henry T. Stelfox
VITAM-Centre de Recherche en Santé Durable, Québec City, Québec, Canada
Patrick Archambault
You can also search for this author in PubMed Google Scholar
Contributions
BC, LM, JRG, JSH, HTS, PA, SB, FL, AFT, JG, MB, CM and AB developed the original research concept and developed the study design. BC, LM, FL, AFT, JSH, HTS, AB, MB and JRG have contributed to the data acquisition, analysis, or interpretation. JH, HTS and SB oversaw the analysis and provided feedback. BC and LM developed the draft manuscript. All authors made substantial contributions to the manuscript development, critical revision and approved the final version of the manuscript.
Corresponding author
Correspondence to Lynne Moore .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the CHU-de Québec – Université Laval research ethics committee and patient consent is not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Conombo, B., Guertin, J.R., Hoch, J.S. et al. Implementation of an audit and feedback module targeting low-value clinical practices in a provincial trauma quality assurance program: a cost-effectiveness study. BMC Health Serv Res 24 , 479 (2024). https://doi.org/10.1186/s12913-024-10969-2
Download citation
Received : 09 October 2023
Accepted : 09 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12913-024-10969-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Audit and feedback
- Cost-effectiveness analysis
- Low-value care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
More From Forbes
Forget “doctors’ day.” here’s how to really value doctors.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
National Doctor’s Day has become a national phenomenon. Should it be?
You’d be forgiven if, on March 30, you didn’t set aside time to celebrate Doctors’ Day. Admittedly, it’s not the most important holiday on the national calendar. On my end, I heard from a few friends and colleagues, and we all expressed our appreciation for the well wishes and cards.
And then we discussed what it’s really like to practice medicine these days.
Which leads me to posit that it’s time to focus less on “days” and more on showing consistent appreciation for the work of healthcare workers—skilled professionals who work in the service of others.
I’m not alone. Several people told me that while they appreciate trinkets bearing corporate logos, greeting cards and even gift cards, they simultaneously feel like the existence of these “days” offers organizations absolution for their working conditions.
Physicians in particular seemed to express this sentiment. Perhaps that’s not surprising. The notion of physician burnout has been well-discussed. Different reasons for it have been proposed, but I stick to the idea that the main cause is invisibility —which is to say, in an industry increasingly dominated by large, vertically integrated companies, doctors feel small and powerless. This idea is backed up by some interesting data: nearly 75% of physicians are employed by a hospital, health system or corporate entity. At the same time, research that finds that burnout rates are lower among physicians who own their own practices.
No wonder, then, that cheery Doctors’ Day notes ring hollow in the context of broader professional devaluation.
But it doesn’t have to be this way. Here are five steps that the hospitals, health systems and other entities that employ physicians and other healthcare professionals can revalue their work and give it the prominent place of honor it deserves.
Gervonta Davis’ Next Fight: ‘Tank’ Has An Opponent For His Return
Warner bros reveals 115 million investment in harry potter attraction, how the dallas mavericks can win their series with the los angeles clippers.
1) Welcome and invite clinical perspectives into organizational decision-making . People who work in healthcare systems know that too often, they are run by career administrators without medical degrees. In and of itself, that’s not a bad thing. I’ve worked with and been mentored by several talented administrative executives without clinical training who were expert at putting patient care at the forefront of their organizations’ priorities. On the other hand, a well-known study shows that “Hospitals in physician-led hospital systems had higher quality ratings across all specialties.” Too many health systems treat clinical leaders as employees to be managed instead of bold thinkers who bring expertise to the table. Involving them in top-level decision making would go a long way to showing them that they’re not merely cogs in an impersonal system.
2) Compensate physicians fairly against market wages for their roles and levels of expertise. Let’s be honest: physicians aren’t starving. And yet, that doesn’t mean they’re always fairly compensated for their work, especially when one takes into account their training and expertise.
It might surprise people to know that 38% of physicians say they’re unsatisfied with their pay and 52% say physician pay itself is not fair or equitable.
Why do doctors feel undervalued? They say they’re not compensated for the time they spend with patients—particularly those whose conditions they manage outside of office visits. They also note that peers in other industries without the same levels of education, training and seniority often make more than they do. Also, they point out that physician pay usually fails to keep pace with the rate of inflation. To be clear: there is no healthcare without physicians, and that’s as true for a primary care doctor in a large health system as it is for a superstar surgeon with a half dozen fellowships under her belt. Both should be rewarded for their value—and a simple way to do that is to pay them what they’re worth.
3. Cease labor arbitrage practices in which physicians are replaced by less expensive, less skilled professionals . If you’ve booked an appointment with your physician lately, you may have been surprised to find that you were evaluated and treated by someone else. In the face of rising wages, labor shortages and increased demand—particularly on the heels of the pandemic, when many people forwent treatment—many healthcare companies have taken to supplanting physicians with other, lower-paid clinicians. Sometimes this makes sense. Much work done today by RN’s for example, would have been done by physicians 25 years ago, and we’ve seen no negative effect on patient health.
However, healthcare is defined as much by complexity as anything else, a fact many systems ignore when they place patient care under the purview of individuals with different levels of professional training, and without clearly defined parameters delineating where and how patients are best served—other than cost, of course. In these cases, patient care suffers, physicians are demeaned and their worth is devalued. Ensuring that complex cases are treated by highly trained people prepared to address complexity—which is to say, physicians—is one way to restore dignity to the profession and improve outcomes.
4. Recognize and acknowledge the moral tensions healthcare professionals live with every day.
Is end of life care appropriate for the patient?
Should an expensive treatment be tried when less expensive options have been exhausted?
Should I perform a diagnostic treatment on an elderly patient?
How do I tell my patient’s family that the diagnosis is terminal?
These questions represent a small fraction of the difficult choices healthcare professionals face every day. And yet, especially inside large health systems, it’s assumed that a series of protocols is sufficient to navigate these thorny issues. I’m not calling for health systems to make decisions for health professionals; but I am calling for them to acknowledge the moral and ethical complexity inherent in the practice of healthcare, and to honor the people whose job it is to make difficult decisions by acknowledging repeatedly both the difficulty of making those decisions and the sheer bravery it takes to confront them.
5. Ensure that all healthcare workers have access to excellent healthcare benefits . Many companies struggle to determine how much of the cost of healthcare their employees should bear. Healthcare companies shouldn’t be among them. Pricing your own employees out of your life-saving product makes little moral sense. It also doesn’t make economic sense, since healthy workers are more productive and therefore more likely to produce better outcomes.
Additionally, making their core products affordable to the people they employ is an obvious way for employers to demonstrate their appreciation for their work. To burden them with high costs is as misguided as it is insulting.
The “Days” Ahead
I’m not a curmudgeon. I like celebrating colleagues and being celebrated by them. And I’ll admit that special “days” have a place in the fabric of appreciation for clinicians of all kinds. Nevertheless, I can’t tell you how many people quietly complain that “days” often feel like from a cynical deflection from some of the bigger issues plaguing the health professions.
It’s those issues we should fix before we run out to buy greeting cards.

- Editorial Standards
- Reprints & Permissions

IMAGES
VIDEO
COMMENTS
500+ Words Essay on Health. Essay on Health: Health was earlier said to be the ability of the body functioning well. However, as time evolved, the definition of health also evolved. It cannot be stressed enough that health is the primary thing after which everything else follows. When you maintain good health, everything else falls into place.
500+ Words Health Is Wealth Essay. Growing up you might have heard the term 'Health is Wealth', but its essential meaning is still not clear to most people. Generally, people confuse good health with being free of any kind of illness. While it may be part of the case, it is not entirely what good health is all about.
Physical health. A person who has good physical health is likely to have bodily functions and processes working at their peak. This is not only due not only to an absence of disease. Regular ...
Importance of Good Health. In today's fast-paced world, where stress levels are high and unhealthy habits run rampant, the importance of good health cannot be overstated. From physical well-being to mental resilience, good health impacts every aspect of our lives, shaping our experiences and determining our quality of life. This essay will ...
Importance of Working Towards Good Health. Health is God's gift to us. Health refers to the physical and mental state of a human being. To stay healthy is not an option but a necessity to live a happy life. The basic laws of good health are related to the food we eat, the amount of physical exercise we do, our cleanliness, rest, and relaxation.
Health is like money; we learn it's the value when it's lost. A Healthy person can achieve happiness and success quickly than a weak and unhealthy person. Staying fit and healthy is truly a blessing. 10 Lines on Health is Wealth Essay in English. The famous proverb 'Health is Wealth' means health is the most significant wealth, not money
In the proceeding sections, a common-sense definition of health is used to present the first principles of A Philosophy of Health. Principle 1: "Health" is the state of maintainable-easeof functioning. A "disease" is a state of prolonged-dysfunction that prevents ease.
The process of formulating the CFP and reviewing proposals surfaced important challenges for research on creating and sustaining shared values to foster and maintain a Culture of Health. In this essay, we describe these considerations and provide examples from funded projects regarding how challenges can be addressed.
Abstract. Health is valuable both instrumentally, in terms of its consequences for autonomy, opportunity, and well-being, and intrinsically, at least with respect to the mental states it encompasses. Quantifying the value of health is problematic, because there are many different ways in which people may suffer diminished health.
Committee definition of health: Health is a state of well-being and the capability to function in the face of changing circumstances. Health is, therefore, a positive concept emphasizing social and personal resources as well as physical capabilities. Improving health is a shared responsibility of health care providers, public health officials ...
500 Words Essay on Health Awareness What is Health Awareness? Health awareness is knowing about the state of your body, how to keep it healthy, and what can harm it. It is like a guide to help you live a healthy life. It tells you about good habits like eating right, exercising, and getting enough sleep. It also warns you about bad things like ...
Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. This comprehensive definition underlines the complex nature of health and its profound impact on our lives. The axiom "Health is Wealth" encapsulates this idea, emphasizing the intrinsic value of health over material wealth.
Health Essay 5 (500 words) Introduction. Health is the most valuable asset a person possesses. It is a state of complete physical, mental, and social well-being, not merely the absence of disease or infirmity. ... Understanding and respect for various cultural groups' ideas, values, customs, and practices, while accepting that opinions on ...
In this essay we argue that clarity regarding morality underlying global health initiatives is important, both for why and how programmes should be undertaken. Common moral values might be used to justify new global programmes, suggesting that the programmes might be shaped differently depending on the morals espoused.
Benefits & Importance of Good Health. Health is very important aspect of life. The physical and mental well being of a person plays an important role in the life of a person. The absence of disease in life makes man able to achieve desired aims and objectives. Related Post: Paragraphs on Health is Wealth.
Published on behalf of the International Society for Pharmacoeconomics and Outcomes Research Value in Health is an international, indexed journal that publishes original research and health policy articles that advance the field of health economics and outcomes research to help healthcare leaders make evidence-based decisions. The Society's flagship journal, Value in Health is a monthly ...
Health Essay 10 Lines (100 - 150 Words) 1) A good health is desire of every human on the earth. 2) Health plays a vital role in the lifestyle of human beings. 3) A good health is very necessary for a good lifestyle. 4) Eating nutritious foods that are rich in vitamins and minerals is essential for good health. 5) Regular physical activity is ...
A framework for valuing improvements in health is developed and applied to past and prospective reductions in mortality in the United States, finding social values of increased longevity over the twentieth century, progress against various diseases after 1970, and potential future progress against major diseases. We develop a framework for valuing improvements in health and apply it to past ...
Good Essays. 1100 Words. 5 Pages. 4 Works Cited. Open Document. The Value of Health Care The development of value based healthcare reimbursement systems between healthcare payers and healthcare providers is evolving from the need to provide patients with beneficial healthcare technologies under conditions of significant economic uncertainty.
100 Words Essay on Importance of Health. Maintaining good health is one of the best practices as it gives us a feeling of complete physical, mental and social well-being. Living a healthy lifestyle can prevent long-term illnesses like such as Asthma, Diabetes, heart diseases, and many more. It provides us freedom from almost all diseases.
The Importance of Good Health. Good health is crucial to everything we do in our everyday lives. The importance of good health can be clearly seen in how we function as human beings in the daily tasks that define our functionality in the society. Without good health, we are not able to reach our individual potentials and this can hinder us from ...
This shift in values prioritized new variations in population health behavior by: (1) requiring a health warning on cigarette packages; (2) banning cigarette advertising in the broadcasting media ...
Good physical health means fitness of one's body is maintained by good nutrition and exercises. This will leads to an efficient circulation, healthy immune system and strong musculoskeletal strength. As a result, an active life is allowed and risk of chronic disease is reduced. This is not the only benefit we can require from good physical ...
Short Essay on Health in 100 Words . Health is an important aspect of one's life. A person is considered healthy when he or she is free from illness or injury. Health can be categorised as physical health, mental health, emotional health, social health, et cetera. However, all these categories are interrelated.
Many Patients Don't Survive End-Stage Poverty. Dr. Ryan is an associate physician at the University of California, San Francisco, department of medicine. He has an easy smile, blue eyes and a ...
Readers respond to First Opinion essays on nonprofit hospitals and taxes, diversity in health care, ADHD in women and girls, and more.
This essay explores three specific ways in which the American mental health care system protects potentially "visible" individuals at the expense of "invisible victims" and otherwise fails to meet the needs of great numbers of people with serious psychiatric conditions: prioritization of the wrong patients, incentivization of excessive ...
Mental health impact is the reason we now take loneliness seriously. It is the metric by which we increasingly judge workplaces; the government has previously urged employers to improve support.
Low-value practices (LVPs) are tests and treatments that are not supported by evidence and may expose patients to physical and psychological harm [1, 2].They have been estimated to consume up to 30% of healthcare resources in Canada [] and in the US [].In 2013, an estimated $270 billion was wasted on excess healthcare services in the US [].From a patient and caregiver perspective, LVPs expose ...
But it doesn't have to be this way. Here are five steps that the hospitals, health systems and other entities that employ physicians and other healthcare professionals can revalue their work and ...