
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics

Obesity Research
Language switcher.
Over the years, NHLBI-supported research on overweight and obesity has led to the development of evidence-based prevention and treatment guidelines for healthcare providers. NHLBI research has also led to guidance on how to choose a behavioral weight loss program.
Studies show that the skills learned and support offered by these programs can help most people make the necessary lifestyle changes for weight loss and reduce their risk of serious health conditions such as heart disease and diabetes.
Our research has also evaluated new community-based programs for various demographics, addressing the health disparities in overweight and obesity.
NHLBI research that really made a difference
- In 1991, the NHLBI developed an Obesity Education Initiative to educate the public and health professionals about obesity as an independent risk factor for cardiovascular disease and its relationship to other risk factors, such as high blood pressure and high blood cholesterol. The initiative led to the development of clinical guidelines for treating overweight and obesity.
- The NHLBI and other NIH Institutes funded the Obesity-Related Behavioral Intervention Trials (ORBIT) projects , which led to the ORBIT model for developing behavioral treatments to prevent or manage chronic diseases. These studies included families and a variety of demographic groups. A key finding from one study focuses on the importance of targeting psychological factors in obesity treatment.
Current research funded by the NHLBI
The Division of Cardiovascular Sciences , which includes the Clinical Applications and Prevention Branch, funds research to understand how obesity relates to heart disease. The Center for Translation Research and Implementation Science supports the translation and implementation of research, including obesity research, into clinical practice. The Division of Lung Diseases and its National Center on Sleep Disorders Research fund research on the impact of obesity on sleep-disordered breathing.
Find funding opportunities and program contacts for research related to obesity and its complications.
Current research on obesity and health disparities
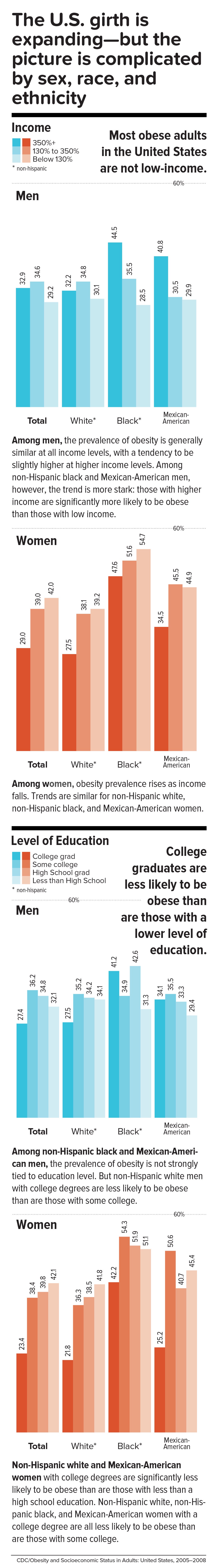
Health disparities happen when members of a group experience negative impacts on their health because of where they live, their racial or ethnic background, how much money they make, or how much education they received. NHLBI-supported research aims to discover the factors that contribute to health disparities and test ways to eliminate them.
- NHLBI-funded researchers behind the RURAL: Risk Underlying Rural Areas Longitudinal Cohort Study want to discover why people in poor rural communities in the South have shorter, unhealthier lives on average. The study includes 4,000 diverse participants (ages 35–64 years, 50% women, 44% whites, 45% Blacks, 10% Hispanic) from 10 of the poorest rural counties in Kentucky, Alabama, Mississippi, and Louisiana. Their results will support future interventions and disease prevention efforts.
- The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is looking at what factors contribute to the higher-than-expected numbers of Hispanics/Latinos who suffer from metabolic diseases such as obesity and diabetes. The study includes more than 16,000 Hispanic/Latino adults across the nation.
Find more NHLBI-funded studies on obesity and health disparities at NIH RePORTER.

Read how African Americans are learning to transform soul food into healthy, delicious meals to prevent cardiovascular disease: Vegan soul food: Will it help fight heart disease, obesity?
Current research on obesity in pregnancy and childhood
- The NHLBI-supported Fragile Families Cardiovascular Health Follow-Up Study continues a study that began in 2000 with 5,000 American children born in large cities. The cohort was racially and ethnically diverse, with approximately 40% of the children living in poverty. Researchers collected socioeconomic, demographic, neighborhood, genetic, and developmental data from the participants. In this next phase, researchers will continue to collect similar data from the participants, who are now young adults.
- The NHLBI is supporting national adoption of the Bright Bodies program through Dissemination and Implementation of the Bright Bodies Intervention for Childhood Obesity . Bright Bodies is a high-intensity, family-based intervention for childhood obesity. In 2017, a U.S. Preventive Services Task Force found that Bright Bodies lowered children’s body mass index (BMI) more than other interventions did.
- The NHLBI supports the continuation of the nuMoM2b Heart Health Study , which has followed a diverse cohort of 4,475 women during their first pregnancy. The women provided data and specimens for up to 7 years after the birth of their children. Researchers are now conducting a follow-up study on the relationship between problems during pregnancy and future cardiovascular disease. Women who are pregnant and have obesity are at greater risk than other pregnant women for health problems that can affect mother and baby during pregnancy, at birth, and later in life.
Find more NHLBI-funded studies on obesity in pregnancy and childhood at NIH RePORTER.
Learn about the largest public health nonprofit for Black and African American women and girls in the United States: Empowering Women to Get Healthy, One Step at a Time .
Current research on obesity and sleep
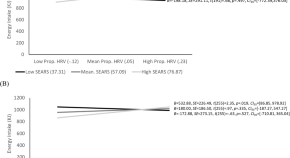
- An NHLBI-funded study is looking at whether energy balance and obesity affect sleep in the same way that a lack of good-quality sleep affects obesity. The researchers are recruiting equal numbers of men and women to include sex differences in their study of how obesity affects sleep quality and circadian rhythms.
- NHLBI-funded researchers are studying metabolism and obstructive sleep apnea . Many people with obesity have sleep apnea. The researchers will look at the measurable metabolic changes in participants from a previous study. These participants were randomized to one of three treatments for sleep apnea: weight loss alone, positive airway pressure (PAP) alone, or combined weight loss and PAP. Researchers hope that the results of the study will allow a more personalized approach to diagnosing and treating sleep apnea.
- The NHLBI-funded Lipidomics Biomarkers Link Sleep Restriction to Adiposity Phenotype, Diabetes, and Cardiovascular Risk study explores the relationship between disrupted sleep patterns and diabetes. It uses data from the long-running Multiethnic Cohort Study, which has recruited more than 210,000 participants from five ethnic groups. Researchers are searching for a cellular-level change that can be measured and can predict the onset of diabetes in people who are chronically sleep deprived. Obesity is a common symptom that people with sleep issues have during the onset of diabetes.
Find more NHLBI-funded studies on obesity and sleep at NIH RePORTER.

Learn about a recent study that supports the need for healthy sleep habits from birth: Study finds link between sleep habits and weight gain in newborns .
Obesity research labs at the NHLBI
The Cardiovascular Branch and its Laboratory of Inflammation and Cardiometabolic Diseases conducts studies to understand the links between inflammation, atherosclerosis, and metabolic diseases.
NHLBI’s Division of Intramural Research , including its Laboratory of Obesity and Aging Research , seeks to understand how obesity induces metabolic disorders. The lab studies the “obesity-aging” paradox: how the average American gains more weight as they get older, even when food intake decreases.
Related obesity programs and guidelines
- Aim for a Healthy Weight is a self-guided weight-loss program led by the NHLBI that is based on the psychology of change. It includes tested strategies for eating right and moving more.
- The NHLBI developed the We Can! ® (Ways to Enhance Children’s Activity & Nutrition) program to help support parents in developing healthy habits for their children.
- The Accumulating Data to Optimally Predict obesity Treatment (ADOPT) Core Measures Project standardizes data collected from the various studies of obesity treatments so the data can be analyzed together. The bigger the dataset, the more confidence can be placed in the conclusions. The main goal of this project is to understand the individual differences between people who experience the same treatment.
- The NHLBI Director co-chairs the NIH Nutrition Research Task Force, which guided the development of the first NIH-wide strategic plan for nutrition research being conducted over the next 10 years. See the 2020–2030 Strategic Plan for NIH Nutrition Research .
- The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) , which is a public–private partnership to accelerate progress in reducing childhood obesity.
- The NHLBI has been providing guidance to physicians on the diagnosis, prevention, and treatment of obesity since 1977. In 2017, the NHLBI convened a panel of experts to take on some of the pressing questions facing the obesity research community. See their responses: Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (PDF, 3.69 MB).
- In 2021, the NHLBI held a Long Non-coding (lnc) RNAs Symposium to discuss research opportunities on lnc RNAs, which appear to play a role in the development of metabolic diseases such as obesity.
- The Muscatine Heart Study began enrolling children in 1970. By 1981, more than 11,000 students from Muscatine, Iowa, had taken surveys twice a year. The study is the longest-running study of cardiovascular risk factors in children in the United States. Today, many of the earliest participants and their children are still involved in the study, which has already shown that early habits affect cardiovascular health later in life.
- The Jackson Heart Study is a unique partnership of the NHLBI, three colleges and universities, and the Jackson, Miss., community. Its mission is to discover what factors contribute to the high prevalence of cardiovascular disease among African Americans. Researchers aim to test new approaches for reducing this health disparity. The study incudes more than 5,000 individuals. Among the study’s findings to date is a gene variant in African Americans that doubles the risk of heart disease.
Explore more NHLBI research on overweight and obesity
The sections above provide you with the highlights of NHLBI-supported research on overweight and obesity . You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity
Affiliations.
- 1 Centre for Software Technology and Management, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia.
- 2 Centre for Software Technology and Management, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia. Electronic address: [email protected].
- 3 RIADI Laboratory, University of Manouba, Manouba, Tunisia; College of Computer Science and Engineering, Taibah University, Medina, Saudi Arabia.
- 4 Center for Artificial Intelligence Technology, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia.
- PMID: 34426171
- DOI: 10.1016/j.compbiomed.2021.104754
Obesity is considered a principal public health concern and ranked as the fifth foremost reason for death globally. Overweight and obesity are one of the main lifestyle illnesses that leads to further health concerns and contributes to numerous chronic diseases, including cancers, diabetes, metabolic syndrome, and cardiovascular diseases. The World Health Organization also predicted that 30% of death in the world will be initiated with lifestyle diseases in 2030 and can be stopped through the suitable identification and addressing of associated risk factors and behavioral involvement policies. Thus, detecting and diagnosing obesity as early as possible is crucial. Therefore, the machine learning approach is a promising solution to early predictions of obesity and the risk of overweight because it can offer quick, immediate, and accurate identification of risk factors and condition likelihoods. The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this study initially recognized the significant potential factors that influence and cause adult obesity. Next, the main diseases and health consequences of obesity and overweight are investigated. Ultimately, this study recognized the machine learning methods that can be used for the prediction of obesity. Finally, this study seeks to support decision-makers looking to understand the impact of obesity on health in the general population and identify outcomes that can be used to guide health authorities and public health to further mitigate threats and effectively guide obese people globally.
Keywords: Diseases; Machine learning; Obesity; Overweight; Risk factors.
Copyright © 2021 The Author(s). Published by Elsevier Ltd.. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Systematic Review
- Machine Learning
- Metabolic Syndrome*
- Obesity* / epidemiology
- Risk Factors
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Research articles
The effect of GLP-1 receptor agonist use on negative evaluations of women with higher and lower body weight
- Stacy M. Post
- Susan Persky

Association of body-mass index with physiological brain pulsations across adulthood – a fast fMRI study
- Lauri Raitamaa
- Joona Kautto
- Vesa Kiviniemi
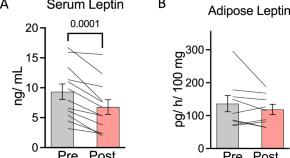
Calorie restriction-induced leptin reduction and T-lymphocyte activation in blood and adipose tissue in men with overweight and obesity
- Rebecca L. Travers
- William V. Trim
- Dylan Thompson

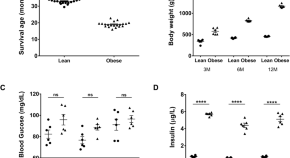
Effects of prenatal THC vapor exposure on body weight, glucose metabolism, and feeding behaviors in chow and high-fat diet fed rats
- Catherine Hume
- Samantha L. Baglot
- Matthew N. Hill
Obesity-related glomerulopathy is associated with elevated WT1 expression in podocytes
- Sneha Jakhotia
- Rajesh Kavvuri
- G. Bhanuprakash Reddy
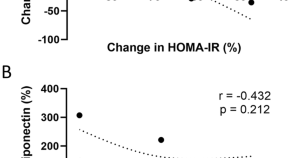
Identification of circulating apolipoprotein M as a new determinant of insulin sensitivity and relationship with adiponectin
- Laurie Frances
- Mikaël Croyal
- Nathalie Viguerie
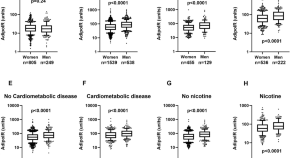
Sex differences in adipose insulin resistance are linked to obesity, lipolysis and insulin receptor substrate 1
- Peter Arner
- Daniel Peter Andersson
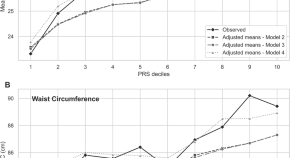
Obesity risk in young adults from the Jerusalem Perinatal Study (JPS): the contribution of polygenic risk and early life exposure
- Hagit Hochner
- Rachely Butterman
- Michal Linial

Serum IL-36β levels are associated with Insulin sensitivity in paediatric patients with obesity
- Paloma Narros-Fernández
- Andrew O’Donnell
- Patrick T. Walsh

Role of IL-18 in adipose tissue remodeling and metabolic dysfunction
- Jaqueline Pereira Lana
- Marina Chaves de Oliveira
- Adaliene Versiani Matos Ferreira
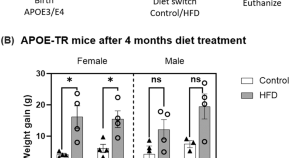
Obesity affects brain cortex gene expression in an APOE genotype and sex dependent manner
- Harshul Pandit
- Nahdia S. Jones
- G. William Rebeck

miR-548ag promotes DPP4 expression in hepatocytes through activation of TLR(7/8)/NF-κB pathway
- Jianyu Xiong
- Chaoyue Sun
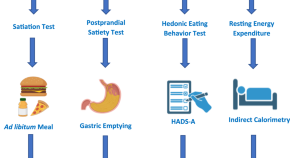
Cumulative effect of obesity phenotypes on body weight and body mass index
- Wissam Ghusn
- Lizeth Cifuentes
- Andres Acosta
The effects of acute social ostracism on subsequent snacking behavior and future body mass index in children
- Aimee E. Pink
- Bobby K. Cheon
Supplementation with antioxidant micronutrients in pregnant women with obesity: a randomized controlled trial
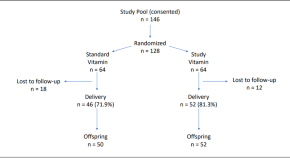
- Sarbattama Sen
- Sara Cherkerzian
- Simin N. Meydani

Tetra methyl bisphenol F: another potential obesogen
- Misha Singh
- Jennifer Crosthwait
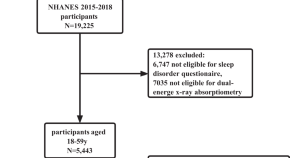
Obstructive sleep apnea (OSA) is associated with increased risk of early-onset sarcopenia and sarcopenic obesity: Results from NHANES 2015-2018
- Changqin Liu
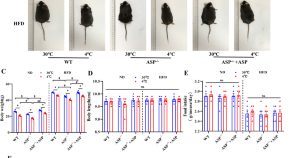
Asprosin contributes to pathogenesis of obesity by adipocyte mitophagy induction to inhibit white adipose browning in mice
- Wanwan Yuan
- Qiren Huang
Familial confounding of internalising symptoms and obesity in adolescents and young adults; a co-twin analysis
- Alexander Charles Campbell
- Lucas Calais-Ferreira
- Jesse T. Young
Body weight in childhood, adolescence, and young adulthood in relation to later risk of disabilities and early retirement among Danish female nurses
- Hanna Kruse Reiband
- Rikke Tannenberg Klemmensen
- Berit Lilienthal Heitmann
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 21 June 2021
The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies
- Emma Farrell ORCID: orcid.org/0000-0002-7780-9428 1 ,
- Marta Bustillo 2 ,
- Carel W. le Roux 3 ,
- Joe Nadglowski 4 ,
- Eva Hollmann 1 &
- Deirdre McGillicuddy 1
Systematic Reviews volume 10 , Article number: 181 ( 2021 ) Cite this article
5930 Accesses
9 Altmetric
Metrics details
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the effectiveness of health interventions. This review aims to systematically locate, assess and synthesise qualitative studies in order to develop a more comprehensive understanding of the lived experience of people with obesity.
This is a protocol for a qualitative evidence synthesis of the lived experience of people with obesity. A defined search strategy will be employed in conducting a comprehensive literature search of the following databases: PubMed, Embase, PsycInfo, PsycArticles and Dimensions (from 2011 onwards). Qualitative studies focusing on the lived experience of adults with obesity (BMI >30) will be included. Two reviewers will independently screen all citations, abstracts and full-text articles and abstract data. The quality of included studies will be appraised using the critical appraisal skills programme (CASP) criteria. Thematic synthesis will be conducted on all of the included studies. Confidence in the review findings will be assessed using GRADE CERQual.
The findings from this synthesis will be used to inform the EU Innovative Medicines Initiative (IMI)-funded SOPHIA (Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy) study. The objective of SOPHIA is to optimise future obesity treatment and stimulate a new narrative, understanding and vocabulary around obesity as a set of complex and chronic diseases. The findings will also be useful to health care providers and policy makers who seek to understand the experience of those with obesity.
Systematic review registration
PROSPERO CRD42020214560 .
Peer Review reports
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health and quality of life, increases the risk of long-term medical complications and reduces lifespan [ 1 ]. Operationally defined in epidemiological and population studies as a body mass index (BMI) greater than or equal to 30, obesity affects more than 650 million adults worldwide [ 2 ]. Its prevalence has almost tripled between 1975 and 2016, and, globally, there are now more people with obesity than people classified as underweight [ 2 ].
Obesity is caused by the complex interplay of multiple genetic, metabolic, behavioural and environmental factors, with the latter thought to be the proximate factor which enabled the substantial rise in the prevalence of obesity in recent decades [ 3 , 4 ]. This increased prevalence has resulted in obesity becoming a major public health issue with a resulting growth in health care and economic costs [ 5 , 6 ]. At a population level, health complications from excess body fat increase as BMI increases [ 7 ]. At the individual level, health complications occur due to a variety of factors such as distribution of adiposity, environment, genetic, biologic and socioeconomic factors [ 8 ]. These health complications include type 2 diabetes [ 9 ], gallbladder disease [ 10 ] and non-alcoholic fatty liver disease [ 11 ]. Excess body fat can also place an individual at increased cardiometabolic and cancer risk [ 12 , 13 , 14 ] with an estimated 20% of all cancers attributed to obesity [ 15 ].
Although first recognised as a disease by the American Medical Association in 2013 [ 16 ], the dominant cultural narrative continues to present obesity as a failure of willpower. People with obesity are positioned as personally responsible for their weight. This, combined with the moralisation of health behaviours and the widespread association between thinness, self-control and success, has resulted in those who fail to live up to this cultural ideal being subject to weight bias, stigma and discrimination [ 17 , 18 , 19 ]. Weight bias, stigma and discrimination have been found to contribute, independent of weight or BMI, to increased morbidity or mortality [ 20 ].
Thomas et al. [ 21 ] highlighted, more than a decade ago, the need to rethink how we approach obesity so as not to perpetuate damaging stereotypes at a societal level. Obesity research then, as now, largely focused on measurable outcomes and quantifiable terms such as body mass index [ 22 , 23 ]. Qualitative research approaches play a key role in understanding patient experiences, how factors facilitate or hinder the effectiveness of interventions and how the processes of interventions are perceived and implemented by users [ 24 ]. Studies adopting qualitative approaches have been shown to deliver a greater depth of understanding of complex and socially mediated diseases such as obesity [ 25 ]. In spite of an increasing recognition of the integral role of patient experience in health research [ 25 , 26 ], the voices of patients remain largely underrepresented in obesity research [ 27 , 28 ].
Systematic reviews and syntheses of qualitative studies are recognised as a useful contribution to evidence and policy development [ 29 ]. To the best of the authors’ knowledge, this will be the first systematic review and synthesis of qualitative studies focusing on the lived experience of people with obesity. While systematic reviews have been carried out on patient experiences of treatments such as behavioural management [ 30 ] and bariatric surgery [ 31 ], this review and synthesis will be the first to focus on the experience of living with obesity rather than patient experiences of particular treatments or interventions. This focus represents a growing awareness that ‘patients have a specific expertise and knowledge derived from lived experience’ and that understanding lived experience can help ‘make healthcare both effective and more efficient’ [ 32 ].
This paper outlines a protocol for the systematic review of qualitative studies based on the lived experience of people with obesity. The findings of this review will be synthesised in order to develop an overview of the lived experience of patients with obesity. It will look, in particular, at patient concerns around the risks of obesity and their aspirations for response to obesity treatment.
The review protocol has been registered within the PROSPERO database (registration number: CRD42020214560) and is being reported in accordance with the reporting guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement [ 33 , 34 ] (see checklist in Additional file 1 ).
Information sources and search strategy
The primary source of literature will be a structured search of the following electronic databases (from January 2011 onwards—to encompass the increase in research focused on patient experience observed over the last 10 years): PubMed, Embase, PsycInfo, PsycArticles and Dimensions. There is no methodological agreement as to how many search terms or databases out to be searched as part of a ‘good’ qualitative synthesis (Toye et al. [ 35 ]). However, the breadth and depth of the search terms, the inclusion of clinical and personal language and the variety within the selected databases, which cover areas such as medicine, nursing, psychology and sociology, will position this qualitative synthesis as comprehensive. Grey literature will not be included in this study as its purpose is to conduct a comprehensive review of peer-reviewed primary research. The study’s patient advisory board will be consulted at each stage of the review process, and content experts and authors who are prolific in the field will be contacted. The literature searches will be designed and conducted by the review team which includes an experienced university librarian (MB) following the methodological guidance of chapter two of the JBI Manual for Evidence Synthesis [ 36 ]. The search will include a broad range of terms and keywords related to obesity and qualitative research. A full draft search strategy for PubMed is provided in Additional file 2 .
Eligibility criteria
Studies based on primary data generated with adults with obesity (operationally defined as BMI >30) and focusing on their lived experience will be eligible for inclusion in this synthesis (Table 1 ). The context can include any country and all three levels of care provision (primary, secondary and tertiary). Only peer-reviewed, English language, articles will be included. Studies adopting a qualitative design, such as phenomenology, grounded theory or ethnography, and employing qualitative methods of data collection and analysis, such as interviews, focus groups, life histories and thematic analysis, will be included. Publications with a specific focus, for example, patient’s experience of bariatric surgery, will be included, as well as studies adopting a more general view of the experience of obesity.
Screening and study selection process
Search results will be imported to Endnote X9, and duplicate entries will be removed. Covidence [ 38 ] will be used to screen references with two reviewers (EF and EH) removing entries that are clearly unrelated to the research question. Titles and abstracts will then be independently screened by two reviewers (EF and EH) according to the inclusion criteria (Table 1 ). Any disagreements will be resolved through a third reviewer (DMcG). This layer of screening will determine which publications will be eligible for independent full-text review by two reviewers (EF and EH) with disagreements again being resolved by a third reviewer (DMcG).
Data extraction
Data will be extracted independently by two researchers (EF and EH) and combined in table format using the following headings: author, year, title, country, research aims, participant characteristics, method of data collection, method of data analysis, author conclusions and qualitative themes. In the case of insufficient or unclear information in a potentially eligible article, the authors will be contacted by email to obtain or confirm data, and a timeframe of 3 weeks to reply will be offered before article exclusion.
Quality appraisal of included studies
This qualitative synthesis will facilitate the development of a conceptual understanding of obesity and will be used to inform the development of policy and practice. As such, it is important that the studies included are themselves of suitable quality. The methodological quality of all included studies will be assessed using the critical appraisal skills programme (CASP) checklist, and studies that are deemed of insufficient quality will be excluded. The CASP checklist for qualitative research comprises ten questions that cover three main issues: Are the results of the study under review valid? What are the results? Will the results help locally? Two reviewers (EF and EH) will independently evaluate each study using the checklist with a third and fourth reviewer (DMcG and MB) available for consultation in the event of disagreement.
Data synthesis
The data generated through the systematic review outlined above will be synthesised using thematic synthesis as described by Thomas and Harden [ 39 ]. Thematic synthesis enables researchers to stay ‘close’ to the data of primary studies, synthesise them in a transparent way and produce new concepts and hypotheses. This inductive approach is useful for drawing inference based on common themes from studies with different designs and perspectives. Thematic synthesis is made up of a three-step process. Step one consists of line by line coding of the findings of primary studies. The second step involves organising these ‘free codes’ into related areas to construct ‘descriptive’ themes. In step three, the descriptive themes that emerged will be iteratively examined and compared to ‘go beyond’ the descriptive themes and the content of the initial studies. This step will generate analytical themes that will provide new insights related to the topic under review.
Data will be coded using NVivo 12. In order to increase the confirmability of the analysis, studies will be reviewed independently by two reviewers (EF and EH) following the three-step process outlined above. This process will be overseen by a third reviewer (DMcG). In order to increase the credibility of the findings, an overview of the results will be brought to a panel of patient representatives for discussion. Direct quotations from participants in the primary studies will be italicised and indented to distinguish them from author interpretations.
Assessment of confidence in the review findings
Confidence in the evidence generated as a result of this qualitative synthesis will be assessed using the Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research (GRADE CERQual) [ 40 ] approach. Four components contribute to the assessment of confidence in the evidence: methodological limitations, relevance, coherence and adequacy of data. The methodological limitations of included studies will be examined using the CASP tool. Relevance assesses the degree to which the evidence from the primary studies applies to the synthesis question while coherence assesses how well the findings are supported by the primary studies. Adequacy of data assesses how much data supports a finding and how rich this data is. Confidence in the evidence will be independently assessed by two reviewers (EF and EH), graded as high, moderate or low, and discussed collectively amongst the research team.
Reflexivity
For the purposes of transparency and reflexivity, it will be important to consider the findings of the qualitative synthesis and how these are reached, in the context of researchers’ worldviews and experiences (Larkin et al, 2019). Authors have backgrounds in health science (EF and EH), education (DMcG and EF), nursing (EH), sociology (DMcG), philosophy (EF) and information science (MB). Prior to conducting the qualitative synthesis, the authors will examine and discuss their preconceptions and beliefs surrounding the subject under study and consider the relevance of these preconceptions during each stage of analysis.
Dissemination of findings
Findings from the qualitative synthesis will be disseminated through publications in peer-reviewed journals, a comprehensive and in-depth project report and presentation at peer-reviewed academic conferences (such as EASO) within the field of obesity research. It is also envisaged that the qualitative synthesis will contribute to the shared value analysis to be undertaken with key stakeholders (including patients, clinicians, payers, policy makers, regulators and industry) within the broader study which seeks to create a new narrative around obesity diagnosis and treatment by foregrounding patient experiences and voice(s). This synthesis will be disseminated to the 29 project partners through oral presentations at management board meetings and at the general assembly. It will also be presented as an educational resource for clinicians to contribute to an improved understanding of patient experience of living with obesity.
Obesity is a complex chronic disease which increases the risk of long-term medical complications and a reduced quality of life. It affects a significant proportion of the world’s population and is a major public health concern. Obesity is the result of a complex interplay of multiple factors including genetic, metabolic, behavioural and environmental factors. In spite of this complexity, obesity is often construed in simple terms as a failure of willpower. People with obesity are subject to weight bias, stigma and discrimination which in themselves result in increased risk of mobility or mortality. Research in the area of obesity has tended towards measurable outcomes and quantitative variables that fail to capture the complexity associated with the experience of obesity. A need to rethink how we approach obesity has been identified—one that represents the voices and experiences of people living with obesity. This paper outlines a protocol for the systematic review of available literature on the lived experience of people with obesity and the synthesis of these findings in order to develop an understanding of patient experiences, their concerns regarding the risks associated with obesity and their aspirations for response to obesity treatment. Its main strengths will be the breadth of its search remit—focusing on the experiences of people with obesity rather than their experience of a particular treatment or intervention. It will also involve people living with obesity and its findings disseminated amongst the 29 international partners SOPHIA research consortium, in peer reviewed journals and at academic conferences. Just as the study’s broad remit is its strength, it is also a potential challenge as it is anticipated that searchers will generate many thousands of results owing to the breadth of the search terms. However, to the best of the authors’ knowledge, this will be the first systematic review and synthesis of its kind, and its findings will contribute to shaping the optimisation of future obesity understanding and treatment.
Availability of data and materials
Not applicable.
Abbreviations
Body mass index
Critical appraisal skills programme
Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research
Innovative Medicines Initiative
Medical Subject Headings
Population, phenomenon of interest, context, study type
Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. Can Med Assoc J. 2020;192(31):E875–91. https://doi.org/10.1503/cmaj.191707 .
Article Google Scholar
World Health Organisation. Fact sheet: obesity and overweight. Geneva: World Health Organisation; 2020.
Google Scholar
Mechanick J, Hurley D, Garvey W. Adiposity-based chronic disease as a new diagnostic term: the American Association of Clinical Endocrinologists and American College Of Endocrinology position statement. Endocrine Pract. 2017;23(3):372–8. https://doi.org/10.4158/EP161688.PS .
Garvey W, Mechanick J. Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. Obesity. 2020;28(3):484–92. https://doi.org/10.1002/oby.22727 .
Article PubMed Google Scholar
Biener A, Cawley J, Meyerhoefer C. The high and rising costs of obesity to the US health care system. J Gen Intern Med. 2017;32(Suppl 1):6–8. https://doi.org/10.1007/s11606-016-3968-8 .
Article PubMed PubMed Central Google Scholar
Department of Health and Social Care. Healthy lives, healthy people: a call to action on obesity in England. London: Department of Health and Social Care; 2011.
Di Angelantonio E, Bhupathiraju SN, Wormser D, Gao P, Kaptoge S, de Gonzalez AB, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. https://doi.org/10.1016/S0140-6736(16)30175-1 .
Sharma AM. M, M, M & M: a mnemonic for assessing obesity. Obesity Reviews. 2010;11(11):808–9. https://doi.org/10.1111/j.1467-789X.2010.00766.x .
Article PubMed CAS Google Scholar
Asnawi A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract 2010;89:309-19. Diab Res Clin Pract. 2010;89:309–19.
Dagfinn A, Teresa N, Lars JV. Body mass index, abdominal fatness and the risk of gallbladder disease. 2015;30(9):1009.
Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20(9).
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. 2003;289(2):187-193.
Grover SA, Kaouache M, Rempel P, Joseph L, Dawes M, Lau DCW, et al. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study. 2015;3(2):114-122.
Ackerman S, Blackburn O, Marchildon F, Cohen P. Insights into the link between obesity and cancer. Curr Obes Rep. 2017;6(2):195–203. https://doi.org/10.1007/s13679-017-0263-x .
Wolin K, Carson K, Colditz G. Obesity and cancer. Oncol. 2010;15(6):556–65. https://doi.org/10.1634/theoncologist.2009-0285 .
Resolution 420: Recognition of obesity as a disease [press release]. 05/16/13 2013.
Brownell KD. Personal responsibility and control over our bodies: when expectation exceeds reality. 1991;10(5):303-10.
Puhl RM, Latner JD, O'Brien K, Luedicke J, Danielsdottir S, Forhan M. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. 2015;39(7):1166-1173.
Browne NT. Weight bias, stigmatization, and bullying of obese youth. 2012;7(3):107-15.
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. 2015;26(11):1803-11.
Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being “fat” in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. 2008;11(4):321-30.
Ogden K, Barr J, Rossetto G, Mercer J. A “messy ball of wool”: a qualitative study of the dimensions of the lived experience of obesity. 2020;8(1):1-14.
Ueland V, Furnes B, Dysvik E, R¯rtveit K. Living with obesity-existential experiences. 2019;14(1):1-12.
Avenell A, Robertson C, Skea Z, Jacobsen E, Boyers D, Cooper D, et al. Bariatric surgery, lifestyle interventions and orlistat for severe obesity: the REBALANCE mixed-methods systematic review and economic evaluation. 2018;22(68).
The PLoS Medicine Editors. Qualitative research: understanding patients’ needs and experiences. Plos Med. 2007;4(8):1283–4.
Boulton M, Fitzpatrick R. Qualitative methods for assessing health care doi:10.1136/qshc.3.2.107. Qual Health Care. 1994;3:107–13.
Johnstone J, Herredsberg C, Lacy L, Bayles P, Dierking L, Houck A, et al. What I wish my doctor really knew: the voices of patients with obesity. Ann Fam Med. 2020;18(2):169–71. https://doi.org/10.1370/afm.2494 .
Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006;56(530):666–72.
PubMed PubMed Central Google Scholar
Brown I, Gould J. Qualitative studies of obesity: a review of methodology. Health. 2013;5(8A3):69–80.
Garip G, Yardley L. A synthesis of qualitative research on overweight and obese people’s views and experiences of weight management. Clin Obes. 2011;1(2-3):10–126.
Coulman K, MacKichan F, Blazeby J, Owen-Smith A. Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obes Rev. 2017;18(5):547–59. https://doi.org/10.1111/obr.12518 .
European Patients’ Forum. “Patients’ Perceptions of Quality in Healthcare”: Report of a survey conducted by EPF in 2016 Brussels: European Patients’ Forum; 2017.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349(jan02 1):g7647. https://doi.org/10.1136/bmj.g7647 .
Toye F, et al. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 2014;14(80).
Lockwood C, Porrit K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Chapter 2: Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis: JBI; 2020, doi: https://doi.org/10.46658/JBIMES-20-03 .
Methley AM, et al. PICO, PICOS and SPIDER: a comparison study of spcificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Res. 2014;14.
Covidence. Cochrane Community; 2020. Available from: https://www.covidence.org .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. https://doi.org/10.1186/1471-2288-8-45 .
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(1):2. https://doi.org/10.1186/s13012-017-0688-3 .
Download references
Acknowledgements
Any amendments made to this protocol when conducting the study will be outlined in PROSPERO and reported in the final manuscript.
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement No 875534. The JU receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA and T1D Exchange, JDRF and Obesity Action Coalition. The funding body had no role in the design of the study and will not have a role in collection, analysis and interpretation of data or in writing the manuscript.
Author information
Authors and affiliations.
School of Education, University College Dublin, Belfield, Dublin 4, Ireland
Emma Farrell, Eva Hollmann & Deirdre McGillicuddy
University College Dublin Library, Dublin, Ireland
Marta Bustillo
Diabetes Complications Research Centre, University College Dublin, Dublin, Ireland
Carel W. le Roux
Obesity Action Coalition, Tampa, USA
Joe Nadglowski
You can also search for this author in PubMed Google Scholar
Contributions
EF conceptualised and designed the protocol with input from DMcG and MB. EF drafted the initial manuscript. EF and MB defined the concepts and search items with input from DmcG, CleR and JN. MB and EF designed and executed the search strategy. DMcG, CleR, JN and EH provided critical insights and reviewed and revised the protocol. All authors have approved and contributed to the final written manuscript.
Corresponding author
Correspondence to Emma Farrell .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:..
PRISMA-P (Preferred Reporting Items for Systematic review and Meta-Analysis Protocols) 2015 checklist: recommended items to address in a systematic review protocol*.
Additional file 2: Table 1
. Search PubMed search string.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Farrell, E., Bustillo, M., le Roux, C.W. et al. The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies. Syst Rev 10 , 181 (2021). https://doi.org/10.1186/s13643-021-01706-5
Download citation
Received : 28 October 2020
Accepted : 14 May 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13643-021-01706-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lived experience
- Patient experience
- Obesity treatment
- Qualitative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Obesity: The Journal of The Obesity Society

Seeking groundbreaking scientific information on obesity? Looking for leading-edge, peer-reviewed research? Then Obesity is your essential source.
By reading Obesity , the official journal of The Obesity Society, you will stay informed about vital developments in this quickly evolving field. You will also get the latest reviews and commentaries from colleagues around the globe, representing a range of interests, ideas and viewpoints.
You can receive access to Obesity as a member of The Obesity Society.* Non-members can view abstracts of recent articles and full text of articles older than 12 months.
Access Obesity now!
*ALSO NOTE: Student and early career members do not automatically receive access to Obesity . These members are able to receive online and/or print access to Obesity for additional fees. Visit our membership page for more information.
Having Obesity login issues? Please call 301-563-6526 or email [email protected] .
Submit your research to Obesity today!
Submit your best research and join the community of thought leaders in the fight against obesity. Read more about Obesity .
Obesity editorial staff
Editor-in-Chief : Michael Jensen, MD Associate Editor-In-Chief : Leanne Redman, PhD
Obesity Journal Symposium
Leading papers from the journal are presented at the annual Obesity Journal Symposium at ObesityWeek® each November. You can review these papers in the December issue of Obesity and read papers from previous competitions.
Thank you for your interest in joining a TOS Committee.
Your request has been sent..
Cookies on Obesity.org
By using Obesity.org, you agree to our use of cookies. We use cookies to provide you with a great experience and to help our website run effectively.
Your payment has been processed successfully!
We’re sorry. we could not process your payment..

Prevention, prevention, prevention.
Losing weight is hard to do.
In the U.S., only one in six adults who have dropped excess pounds actually keep off at least 10 percent of their original body weight. The reason: a mismatch between biology and environment. Our bodies are evolutionarily programmed to put on fat to ride out famine and preserve the excess by slowing metabolism and, more important, provoking hunger. People who have slimmed down and then regain their weight don’t lack willpower—their bodies are fighting them every inch of the way.
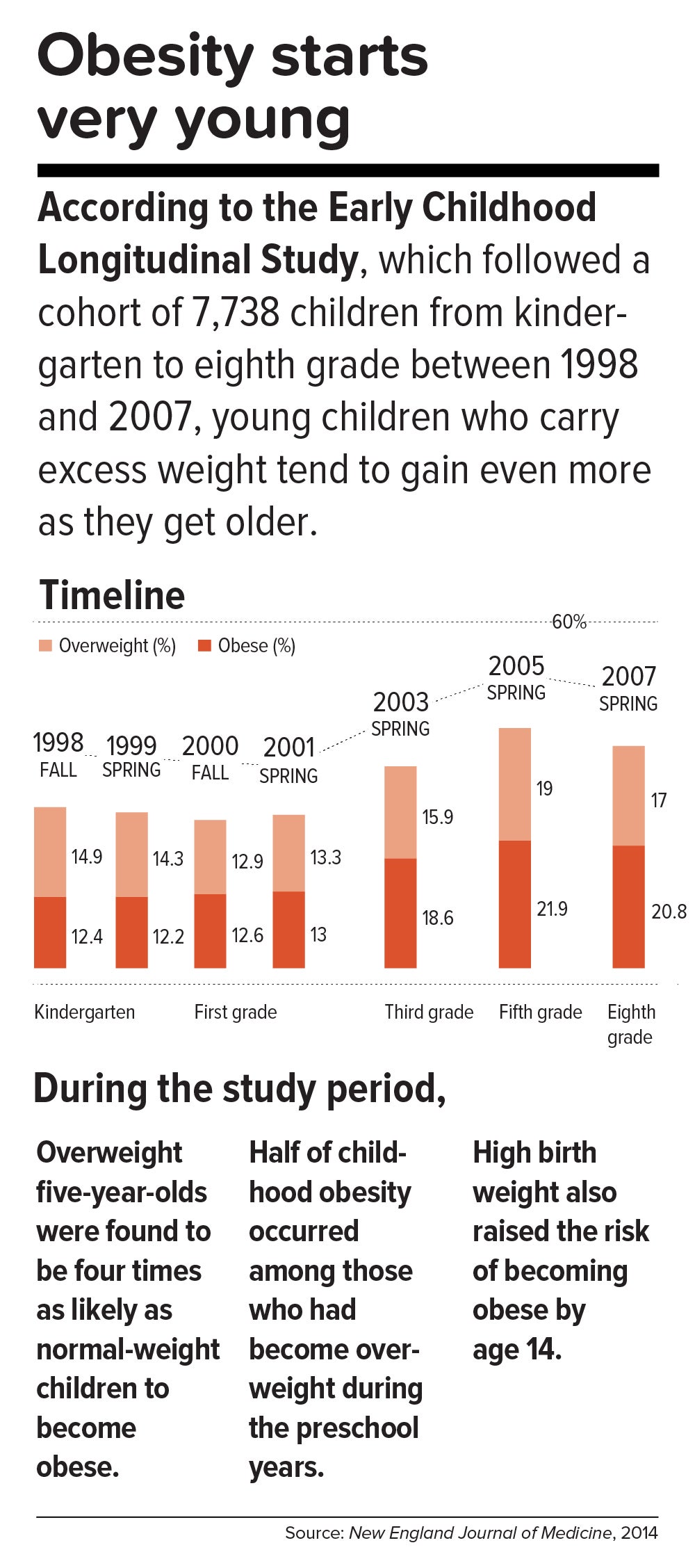
This inborn predisposition to hold on to added weight reverberates down the life course. Few children are born obese, but once they become heavy, they are usually destined to be heavy adolescents and heavy adults. According to a 2016 study in the New England Journal of Medicine , approximately 90 percent of children with severe obesity will become obese adults with a BMI of 35 or higher. Heavy young adults are generally heavy in middle and old age. Obesity also jumps across generations; having a mother who is obese is one of the strongest predictors of obesity in children.
All of which means that preventing child obesity is key to stopping the epidemic. By the time weight piles up in adulthood, it is usually too late. Luckily, preventing obesity in children is easier than in adults, partly because the excess calories they absorb are minimal and can be adjusted by small changes in diet—substituting water, for example, for sugary fruit juices or soda.
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, “Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55. During this time, people gain fat mass, not muscle mass. When they reach age 55 or so, they begin to lose their existing muscle mass and gain even more fat mass. That’s when all the metabolic problems appear: insulin resistance, high cholesterol, high blood pressure.”
Adds Walter Willett, Frederick John Stare Professor of Epidemiology and Nutrition at Harvard Chan, “The first 5 pounds of weight gain at age 25—that’s the time to be taking action. Because someone is on a trajectory to end up being 30 pounds overweight by the time they’re age 50.”
The most realistic near-term public health goal, therefore, is not to reverse but rather to slow down the trend—and even this will require strong commitment from government at many levels. In May 2017, the Trump administration rolled back recently-enacted standards for school meals, delaying a rule to lower sodium and allowing waivers for regulations requiring cafeterias to serve foods rich in whole grains. If recent expansions in food entitlements and school meals are undermined, “It would be a ‘disaster,’ to use the president’s word,” says Marlene Schwartz, director of the Rudd Center for Obesity & Food Policy at the University of Connecticut. “The federal food programs are incredibly important, not just because of the food and money they provide families, but because supporting better nutrition in child care, schools, and the WIC [Women, Infants, and Children] program has created new social norms. We absolutely cannot undo the progress that we’ve made in helping this generation transition to a healthier diet.”
Get the science right.
It is impossible to prescribe solutions to obesity without reminding ourselves that nutrition scientists botched things decades ago and probably sent the epidemic into overdrive. Beginning in the 1970s, the U.S. government and major professional groups recommended for the first time that people eat a low-fat/high-carbohydrate diet. The advice was codified in 1977 with the first edition of The Dietary Goals for the United States , which aimed to cut diet-related conditions such as heart disease and diabetes. What ensued amounted to arguably the biggest public health experiment in U.S. history, and it backfired.
At the time, saturated fat and dietary cholesterol were believed to be the main factors responsible for cardiovascular disease—an oversimplified theory that ignored the fact that not all fats are created equal. Soon, the public health blitz against saturated fat became a war on all fat. In the American diet, fat calories plummeted and carb calories shot up.
“We can’t blame industry for this. It was a bandwagon effect in the scientific community, despite the lack of evidence—even with evidence to the contrary,” says Willett. “Farmers have known for thousands of years that if you put animals in a pen, don’t let them run around, and load them up with grains, they get fat. That’s basically what has been happening to people: We created the great American feedlot. And we added in sugar, coloring, and seductive promotion for low-fat junk food.”
Scientists now know that whole fruits and vegetables (other than potatoes), whole grains, high-quality proteins (such as from fish, chicken, beans, and nuts), and healthy plant oils (such as olive, peanut, or canola oil) are the foundations of a healthy diet.
But there is also a lot scientists don’t yet know. One unanswered question is why some people with obesity are spared the medical complications of excess weight. Another concerns the major mechanisms by which obesity ushers in disease. Although surplus body weight can itself directly cause problems—such as arthritis due to added load on joints, or breast cancer caused by hormones secreted by fat cells—in general, obesity triggers myriad biological processes. Many of the resulting conditions—such as atherosclerosis, diabetes, and even Alzheimer’s disease—are mediated by inflammation, in which the body’s immune response becomes damagingly self-perpetuating. In this sense, today’s food system is as inflammagenic as it is obesigenic.
Scientists also need to ferret out the nuanced effects of particular foods. For example, do fermented products—such as yogurt, tempeh, or sauerkraut—have beneficial properties? Some studies have found that yogurt protects against weight gain and diabetes, and suggest that healthy live bacteria (known as probiotics) may play a role. Other reports point to fruits being more protective than vegetables in weight control and diabetes prevention, although the types of fruits and vegetables make a difference.
A 2017 article in the American Journal of Clinical Nutrition showed that substituting whole grains for refined grains led to a loss of nearly 100 calories a day—by speeding up metabolism, cutting the number of calories that the body hangs on to, and, more surprisingly, by changing the digestibility of other foods on the plate. That extra energy lost daily—by substituting, say, brown rice for white rice or barley for pita bread—was equivalent to a brisk 30-minute walk. One hundred calories a day, sustained over years, and multiplied by the population is one mathematical equivalent of the obesity epidemic.
A companion study found that adults who ate a whole-grain-rich diet developed healthier gut bacteria and improved immune responses. That particular foods alter the gut microbiome—the dense and vital community of bacteria and other microorganisms that work symbiotically with the body’s own digestive system—is another critical insight. The microbiome helps determine weight by controlling how our bodies extract calories and store fat in the liver, and the microbiomes of obese individuals are startlingly efficient at harvesting calories from food. [To learn more about Harvard Chan research on the gut microbiome, read “ Bugs in the System .”] The hormonal effects of sleep deprivation and stress—two epidemics concurrent and intertwined with the obesity trend—are other promising avenues of research.
And then there are the mystery factors. One recent hypothesis is that an agent known as adenovirus 36 partly accounts for our collective heft. A 2010 article in The Royal Society described a study in which researchers examined samples of more than 20,000 animals from eight species living with or around humans in industrialized nations, a menagerie that included macaques, chimpanzees, vervets, marmosets, lab mice and rats, feral rats, and domestic dogs and cats. Like their Homo sapiens counterparts, all of the study populations had gained weight over the past several decades—wild, domestic, and lab animals alike. The chance that this is a coincidence is, according to the scientists’ estimate, 1 in 10 million. The stumped authors surmise that viruses, gene expression changes, or “as-of-yet unidentified and/or poorly understood factors” are to blame.
Master the art of persuasion.
A 2015 paper in the American Journal of Public Health revealed the philosophical chasm that hampers America’s progress on obesity prevention. It found that 72 to 98 percent of obesity-related media reports emphasize personal responsibility for weight, compared with 40 percent of scientific papers.
A recent study by Drexel University researchers also quantified the political polarization around public health measures. From 1998 through 2013, Democrats voted in line with recommendations from the American Public Health Association 88.3 percent of the time, on average, while Republicans voted for the proposals just 21.3 percent of the time.
Clearly, we can’t count on bipartisan goodwill to stem the obesity crisis. But we can ask what kinds of messages appeal to politically divergent audiences. A stealth strategy may be to avoid even uttering the word “obesity.” On January 1 of this year, Philadelphia’s 1.5-cents-per-ounce excise tax on sugar-sweetened and diet beverages took effect. When Philadelphia Mayor Jim Kenney lobbied voters to approve the tax, his bid centered not on improving health—the unsuccessful pitch of his predecessor—but on raising $91 million annually for prekindergarten programs.
“That’s something lots of people care about and can get behind—it’s a feel-good policy, and it makes sense,” says psychologist Christina Roberto, assistant professor of medical ethics and health policy at the University of Pennsylvania, and a former assistant professor of social and behavioral sciences and nutrition at Harvard Chan. The provision for taxing diet beverages was also shrewd, she adds, because it spread the tax’s pain; since wealthier people are more likely than less-affluent individuals to buy diet drinks, the tax could not be slapped with the label “regressive.”
But Roberto sees a larger lesson in the Philadelphia story. Public health messaging that appeals to values that transcend the individual is less fraught, less stigmatizing, and perhaps more effective. As she puts it, “It’s very different to hear the message, ‘Eat less red meat, help the planet’ versus ‘Eat less red meat, help yourself avoid saturated fat and cardiovascular disease.’”
Supermarket makeovers
Supermarket aisles are other places where public health can shuffle a deck stacked against healthy consumer choices.
With slim profit margins and 50,000-plus products on their shelves, grocery stores depend heavily on food manufacturers’ promotional incentives to make their bottom lines. “Manufacturers pay slotting fees to get their products on the shelf, and they pay promotion allowances: We’ll give you this much off a carton of Coke if you put it on sale for a certain price or if you put it on an end-of-aisle display,” says José Alvarez, former president and chief executive officer of Stop & Shop/Giant-Landover, now senior lecturer of business administration at Harvard Business School. Such promotional payments, Alvarez adds, often exceed retailers’ net profits.
Healthy new products—like flash-frozen dinners prepared with heaps of vegetables and whole grains, and relatively little salt—can’t compete for prized shelf space against boxed mac and cheese or cloying breakfast cereals. One solution, says Alvarez, is for established consumer packaged goods companies to buy out what he calls the “hippie in the basement” firms that have whipped up more nutritious items. The behemoths could apply their production, marketing, and distribution prowess to the new offerings—and indeed, this has started to happen over the last five years.
Another approach is to make nutritious foods more convenient to eat. “We have all of these cooking shows and upscale food magazines, but most people don’t have the time or inclination—or the skills, quite frankly—to cook,” says Alvarez. “Instead, we should focus on creating high-quality, healthy, affordable prepared foods.”
An additional model is suggested by Jeff Dunn, a 20-year veteran of the soft drink industry and former president of Coca-Cola North America, who went on to become an advocate for fresh, healthy food. Dunn served as president and chief executive officer of Bolthouse Farms from 2008 to 2015, where he dramatically increased sales of baby carrots by using marketing techniques common in the junk food business. “We operated on the principles of the three 3 A’s: accessibility, availability, and affordability,” says Dunn. “That, by the way, is Coke’s more-than-70-year-old formula for success.”
Show them the money.
Obesity kills budgets. According to the Campaign to End Obesity, a collaboration of leaders from industry, academia, public health, and policymakers, annual U.S. health costs related to obesity approach $200 billion. In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the rise in health care spending from 1987 to 2007 was linked to obesity. And the U.S. Centers for Disease Control and Prevention (CDC) found that full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million more days of work each year than do healthy employees—upward of $153 billion in lost productivity annually.
But making the money case for obesity prevention isn’t straightforward. For interventions targeting children and youth, only a small fraction of savings is captured in the first decade, since most serious health complications don’t emerge for many years. Long-term obesity prevention, in other words, doesn’t fit into political timetables for elected officials.
Yet lawmakers are keen to know how “best for the money” obesity-prevention programs can help them in the short run. Over the past two years, Harvard Chan’s Steve Gortmaker and his colleagues have been working with state health departments in Alaska, Mississippi, New Hampshire, Oklahoma, Washington, and West Virginia and with the city of Philadelphia and other locales, building cost-effectiveness models using local data for a wide variety of interventions—from improved early child care to healthy school environments to communitywide campaigns. “We collaborate with health departments and community stakeholders, provide them with the evidence base, help assess how much different options cost, model the results over a decade, and they pick what they want to work on. One constant that we’ve seen—and these are very different political environments—is a strong interest in cost-effectiveness,” he says.
In a 2015 study in Health Affairs , Gortmaker and colleagues outlined three interventions that would more than pay for themselves: an excise tax on sugar-sweetened beverages implemented at the state level; elimination of the tax subsidy for advertising unhealthy food to children; and strong nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, by 2025. The projected net savings to society in obesity-related health care costs for each dollar invested: $31, $33, and $4.60, respectively.
Gortmaker is one of the leaders of a collaborative modeling effort known as CHOICES—for Childhood Obesity Intervention Cost-Effectiveness Study—an acronym that seems a pointed rebuttal to the reflexive conservative argument that government regulation tramples individual choice. Having grown up not far from Des Plaines, Illinois, site of the first McDonald’s franchise in the country, he emphasizes to policymakers that at this late date, America cannot treat its way out of obesity, given current medical know-how. Only a thoroughgoing investment in prevention will turn the tide. “Clinical interventions produce too small an effect, with too small a population, and at high cost,” Gortmaker says. “The good news is that there are many cost-effective options to choose from.”
While Gortmaker underscores the importance of improving both food choices and options for physical activity, he has shown that upgrading the food environment offers much more benefit for the buck. This is in line with the gathering scientific consensus that what we eat plays a greater role in obesity than does sedentary lifestyle (although exercise protects against many of the metabolic consequences of excess weight). “The easiest way to explain it,” Gortmaker says, “is to talk about a sugary beverage—140 calories. You could quickly change a kid’s risk of excess energy balance by 140 calories a day just by switching from a sugary drink a day to water or sparkling water. But for a 10-year-old boy to burn an extra 140 calories, he’d have to replace an hour-and-a-half of sitting with an hour-and-a-half of walking.”
Small tweaks in adults’ diets can likewise make a big difference in short order. “With adults, health care costs rise rapidly with excess weight gain,” Gortmaker says. “If you can slow the onset of obesity, you slow the onset of diabetes, and potentially not only save health care costs but also boost people’s productivity in the workforce.”
One of Gortmaker’s most intriguing calculations spins off of the food industry’s estimated $633 million spent on television marketing aimed at kids. Currently, federal tax treatment of advertising as an ordinary business expense means that the government, in effect, subsidizes hawking of junk food to children. Gortmaker modeled a national intervention that would eliminate this subsidy of TV ads for nutritionally empty foods and beverages aimed at 2- to 19-year-olds. Drawing on well-delineated relationships between exposure to these advertisements and subsequent weight gain, he found that the intervention would save $260 million in downstream health care costs. Although the effect would probably be small at the individual level, it would be significant at the population level.
Level the playing field through taxes and regulation.
When public health took on cigarette smoking, starting in the 1960s, it did so with robust policies banning television ads and other marketing, raising taxes to increase prices, making public places smoke-free, and offering people treatment such as the nicotine patch. In 1965, the smoking rate for U.S. adults was 42.2 percent; today, it is 16.8 percent.
Similarly, America reduced the rate of deaths caused by motor vehicle accidents—a 90 percent decrease over the 20th century, according to the CDC—with mandatory seat belt laws, safer car designs, stop signs, speed limits, rumble strips, and the stigmatization of drunk driving.
Change the product. Change the environment. Change the culture. That is also the policy recipe for stopping obesity.
Laws that make healthy behaviors easier are often followed by positive changes in those behaviors. And people who are trying to adopt healthy behaviors tend to support policies that make their personal aspirations achievable, which in turn nudges lawmakers to back the proposals.
One debate today revolves around whether recipients of federal Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as food stamps) should be restricted from buying sodas or junk food. The largest component of the USDA budget, SNAP feeds one in seven Americans. A USDA report, issued last November, found that the number-one purchase by SNAP households was sweetened beverages, a category that included soft drinks, fruit juices, energy drinks, and sweetened teas, accounting for nearly 10 percent of SNAP money spent on food. Is the USDA therefore underwriting the soda industry and planting the seeds for chronic disease that the government will pay to treat years down the line?
Eric Rimm, a professor in the Departments of Epidemiology and Nutrition at the Harvard Chan School, frames the issue differently. In a 2017 study in the American Journal of Preventive Medicine , he and his colleagues asked SNAP participants whether they would prefer the standard benefits package or a “SNAP-plus” that prohibited the purchase of sugary beverages but offered 50 percent more money for buying fruits and vegetables. Sixty-eight percent of the participants chose the healthy SNAP-plus option.
“A lot of work around SNAP policy is done by academics and politicians, without reaching out to the beneficiaries,” says Rimm. “We haven’t asked participants, ‘What’s your say in this? How can we make this program better for you?’” To be sure, SNAP is riddled with nutritional contradictions. Under current rules, for example, participants can use benefits to buy a 12-pack of Pepsi or a Snickers bar or a giant bag of Lay’s potato chips but not real food that happens to be heated, such as a package of rotisserie chicken. “This is the most vulnerable population in the country,” says Rimm. “We’re not listening well enough to our constituency.”
Other innovative fiscal levers to alter behavior could also drive down obesity. In 2014, a trio of strong voices on food industry practices—Dariush Mozaffarian, DrPH ’06, dean of Tufts University’s Friedman School of Nutrition Science and Policy and former associate professor of epidemiology at the Harvard Chan School; Kenneth Rogoff, professor of economics at Harvard; and David Ludwig, professor in the Department of Nutrition at Harvard Chan and a physician at Boston Children’s Hospital—broached the idea of a “meaningful” tax on nearly all packaged retail foods and many chain restaurants, with the proceeds used to pay for minimally processed foods and healthier meals for school kids. In essence, the tax externalizes the social costs of harmful individual behavior.
“We made a straightforward proposal to tax all processed foods and then use the income to subsidize whole foods in a short-term, revenue-neutral way,” explains Ludwig. “The power of this idea is that, since there is so much processed food consumption, even a modest tax—in the 10 to 15 percent range—is not going to greatly inflate the cost of these foods. Their price would increase moderately, but the proceeds would not disappear into government coffers. Instead, the revenue would make healthy foods affordable for virtually the entire population, and the benefits would be immediately evident. Yes, people will pay moderately more for their Coke or for their cinnamon bear claw but a lot less for nourishing, whole foods.”
Another suggestion comes from Sandro Galea, dean of the Boston University School of Public Health, and Abdulrahman M. El-Sayed, a public health physician and epidemiologist. In a 2015 issue of the American Journal of Public Health , they called for “calorie offsets,” similar to the carbon offsets used to mitigate environmental harm caused by the gas and oil industries. A “calorie offset” scheme could hand the food and beverage industries a chance at redemption by inviting them to invest in such undertakings as city farms, cooking classes for parents, healthy school cafeterias, and urban green spaces.
These ambitious proposals face almost impossibly high hurdles. Political battle lines typically pit public health against corporations, with Big Food casting doubt on solid nutrition science, deeming government regulation a threat to free choice, and making self-policing pledges that it has never kept. On the website for the Americans for Food and Beverage Choice, a group spearheaded by the American Beverage Association, is the admonition: “[W]hether it’s at a restaurant or in a grocery store, it’s never the government’s job to decide what you choose to eat and drink.”
Yet surprisingly, many public health professionals are convinced that the only way to stop obesity is to make common cause with the food industry. “This isn’t like tobacco, where it’s a fight to the death. We need the food industry to make healthier food and to make a profit,” says Mozaffarian. “The food industry is much more diverse and heterogeneous than tobacco or even cars. As long as we can help them—through carrots and sticks, tax incentives and disincentives—to move towards healthier products, then they are part of the solution. But we have to be vigilant, because they use a lot of the same tactics that tobacco did.”
Sow what we want to reap.
Americans overeat what our farmers overproduce.
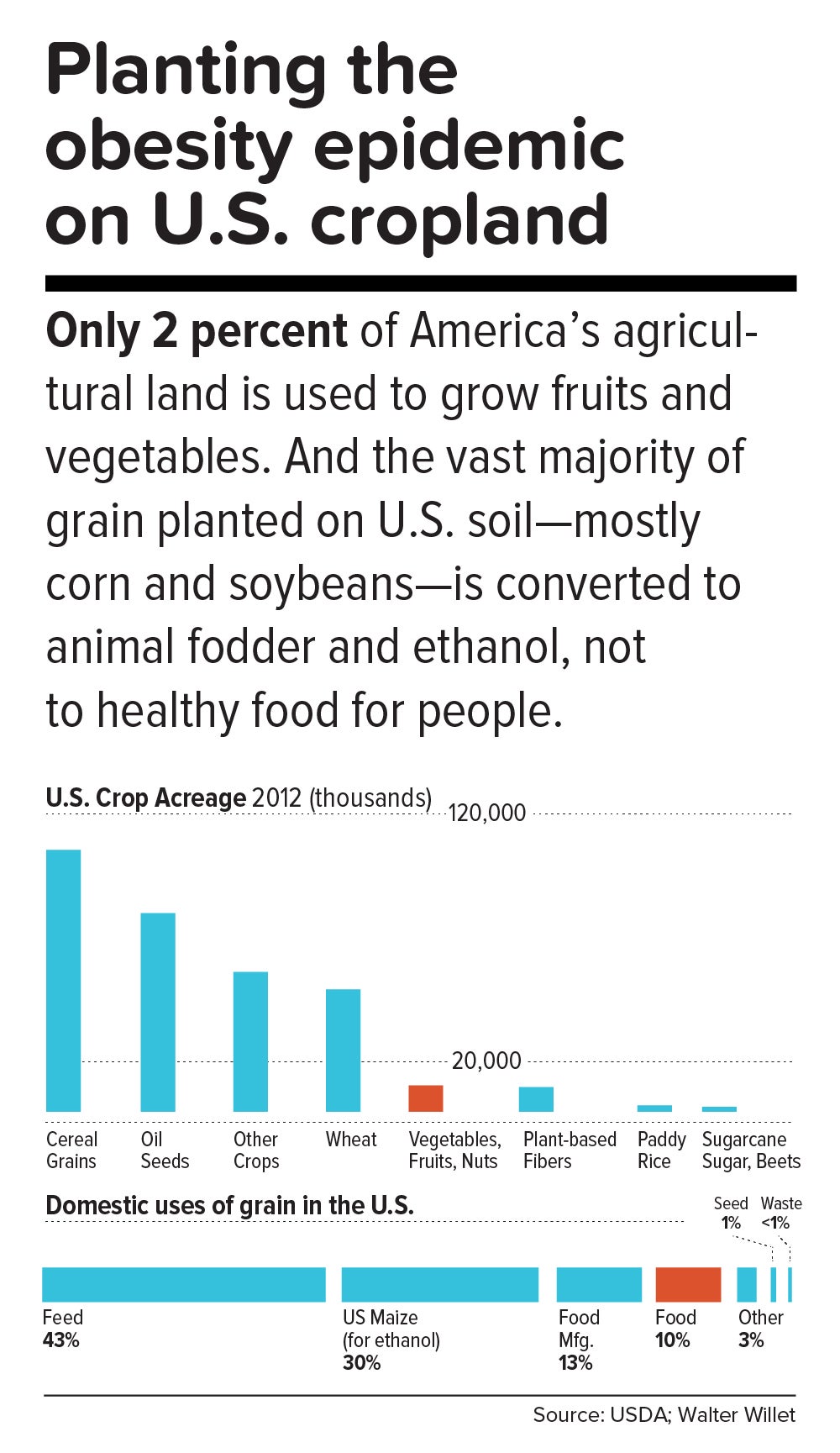
“The U.S. food system is egregiously terrible for human and planetary health,” says Walter Willett. It’s so terrible, Willett made a pie chart of American grain production consumed domestically. It shows that most of the country’s agricultural land goes to the two giant commodity crops: corn and soy. Most of those crops, in turn, go to animal fodder and ethanol, and are also heavily used in processed snack foods. Today, only about 10 percent of grain grown in the U.S. for domestic use is eaten directly by human beings. According to a 2013 report from the Union of Concerned Scientists, only 2 percent of U.S. farmland is used to grow fruits and vegetables, while 59 percent is devoted to commodity crops.
Historically, those skewed proportions made sense. Federal food policies, drafted with the goal of alleviating hunger, preferentially subsidize corn and soy production. And whereas corn or soybeans could be shipped for days on a train, fruits and vegetables had to be grown closer to cities by truck farmers so the produce wouldn’t spoil. But those long-ago constraints don’t explain today’s upside-down agricultural priorities.
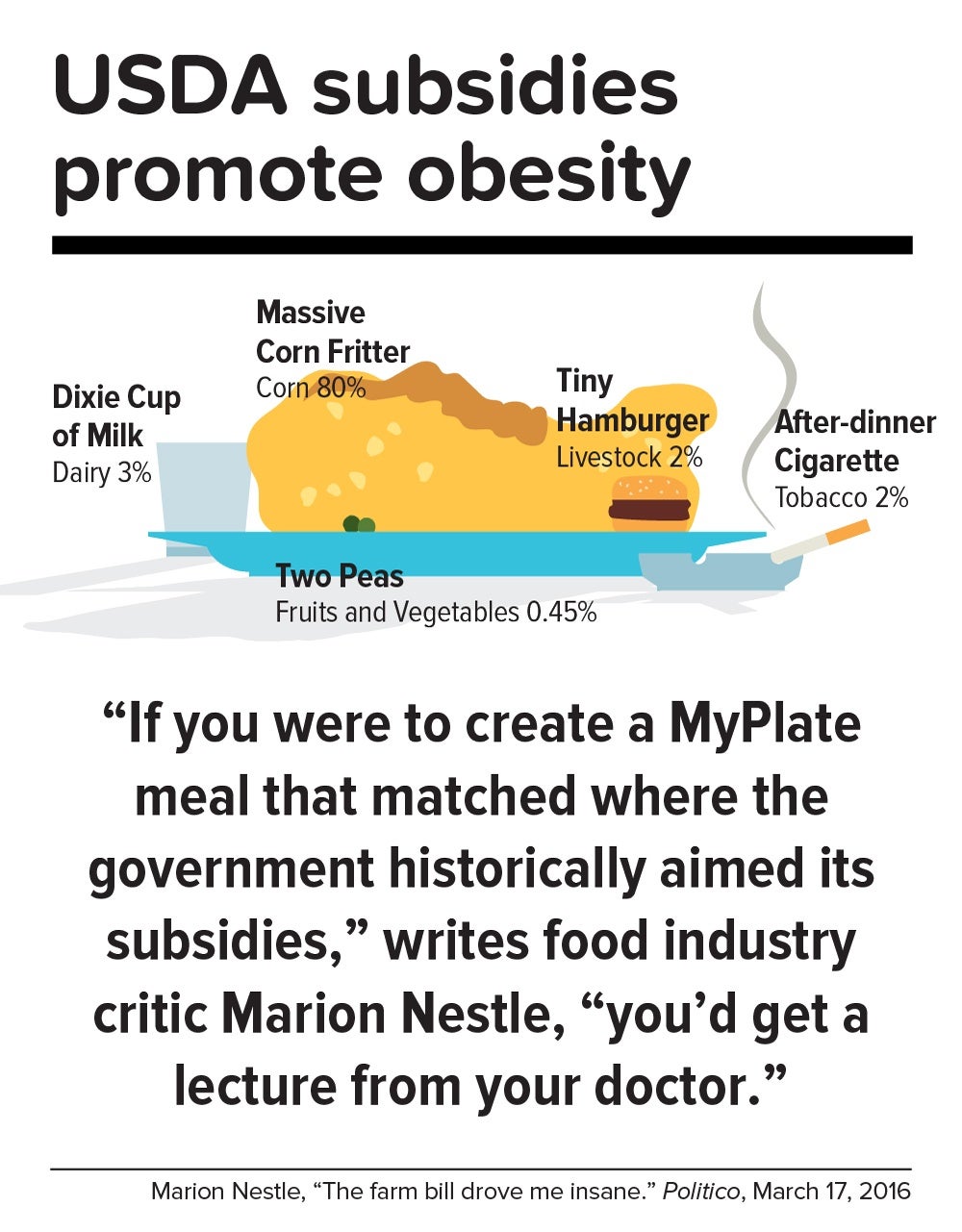
In a now-classic 2016 Politico article titled “The farm bill drove me insane,” Marion Nestle illustrated the irrational gap between what the government recommends we eat and what it subsidizes: “If you were to create a MyPlate meal that matched where the government historically aimed its subsidies, you’d get a lecture from your doctor. More than three-quarters of your plate would be taken up by a massive corn fritter (80 percent of benefits go to corn, grains and soy oil). You’d have a Dixie cup of milk (dairy gets 3 percent), a hamburger the size of a half dollar (livestock: 2 percent), two peas (fruits and vegetables: 0.45 percent) and an after-dinner cigarette (tobacco: 2 percent). Oh, and a really big linen napkin (cotton: 13 percent) to dab your lips.”
In this sense, the USDA marginalizes human health. Many of the foods that nutritionists agree are best for us—notably, fruits, vegetables, and tree nuts—fall under the bureaucratic rubric “specialty crops,” a category that also includes “dried fruits, horticulture, and nursery crops (including floriculture).” Farm bills, which get passed every five years or so, fortify the status quo. The 2014 Farm Bill, for example, provided $73 million for the Specialty Crop Block Grant Program in 2017, out of a total of about $25 billion for the USDA’s discretionary budget. (The next Farm Bill, now under debate, will be coming out in 2018.)
By contrast, a truly anti-obesigenic agricultural system would stimulate USDA support for crop diversity—through technical assistance, research, agricultural training programs, and financial aid for farmers who are newly planting or transitioning their land into produce. It would also enable farmers, most of whom survive on razor-thin profit margins, to make a decent living.
In the early 1970s, Finland’s death rate from coronary heart disease was the highest in the world, and in the eastern region of North Karelia—a pristine, sparsely populated frontier landscape of forest and lakes—the rate was 40 percent worse than the national average. Every family saw physically active men, loggers and farmers who were strong and lean, dying in their prime.
Thus was born the North Karelia Project, which became a model worldwide for saving lives by transforming lifestyles. The project was launched in 1972 and officially ended 25 years later. While its initial goal was to reduce smoking and saturated fat in the diet, it later resolved to increase fruit and vegetable consumption.
The North Karelia Project fulfilled all of these ambitions. When it started, for example, 86 percent of men and 82 percent of women smeared butter on their bread; by the early 2000s, only 10 percent of men and 4 percent of women so indulged. Use of vegetable oil for cooking jumped from virtually zero in 1970 to 50 percent in 2009. Fruit and vegetables, once rare visitors to the dinner plate, became regulars. Over the project’s official quarter-century existence, coronary heart disease deaths in working-age North Karelian men fell 82 percent, and life expectancy rose seven years.
The secret of North Karelia’s success was an all-out philosophy. Team members spent innumerable hours meeting with residents and assuring them that they had the power to improve their own health. The volunteers enlisted the assistance of an influential women’s group, farmers’ unions, homemakers’ organizations, hunting clubs, and church congregations. They redesigned food labels and upgraded health services. Towns competed in cholesterol-cutting contests. The national government passed sweeping legislation (including a total ban on tobacco advertising). Dairy subsidies were thrown out. Farmers were given strong incentives to produce low-fat milk, or to get paid for meat and dairy products based not on high-fat but on high-protein content. And the newly established East Finland Berry and Vegetable Project helped locals switch from dairy farming—which had made up more than two-thirds of agriculture in the region—to cultivation of cold-hardy currants, gooseberries, and strawberries, as well as rapeseed for heart-healthy canola oil.
“A mass epidemic calls for mass action,” says the project’s director, Pekka Puska, “and the changing of lifestyles can only succeed through community action. In this case, the people pulled the government—the government didn’t pull the people.”
Could the United States in 2017 learn from North Karelia’s 1970s grand experiment?
“Americans didn’t become an obese nation overnight. It took a long time—several decades, the same timeline as in individuals,” notes Frank Hu. “What were we doing over the past 20 years or 30 years, before we crossed this threshold? We haven’t asked these questions. We haven’t done this kind of soul-searching, as individuals or society as a whole.”
Today, Americans may finally be willing to take a hard look at how food figures in their lives. In a July 2015 Gallup phone poll of Americans 18 and older, 61 percent said they actively try to avoid regular soda (the figure was 41 percent in 2002); 50 percent try to avoid sugar; and 93 percent try to eat vegetables (but only 57.7 percent in 2013 reported they ate five or more servings of fruits and vegetables at least four days of the previous week).
Individual resolve, of course, counts for little in problems as big as the obesity epidemic. Most successes in public health bank on collective action to support personal responsibility while fighting discrimination against an epidemic’s victims. [To learn more about the perils of stigma against people with obesity, read “ The Scarlet F .”]
Yet many of public health’s legendary successes also took what seems like an agonizingly long time to work. Do we have that luxury?
“Right now, healthy eating in America is like swimming upstream. If you are a strong swimmer and in good shape, you can swim for a little while, but eventually you’re going to get tired and start floating back down,” says Margo Wootan, SD ’93, director of nutrition policy for the Center for Science in the Public Interest. “If you’re distracted for a second—your kid tugs on your pant leg, you had a bad day, you’re tired, you’re worried about paying your bills—the default options push you toward eating too much of the wrong kinds of food.”
But Wootan has not lowered her sights. “What we need is mobilization,” she says. “Mobilize the public to address nutrition and obesity as societal problems—recognizing that each of us makes individual choices throughout the day, but that right now the environment is stacked against us. If we don’t change that, stopping obesity will be impossible.”
The passing of power to younger generations may aid the cause. Millennials are more inclined to view food not merely as nutrition but also as narrative—a trend that leaves Duke University’s Kelly Brownell optimistic. “Younger people have been raised to care about the story of their food. Their interest is in where it came from, who grew it, whether it contributes to sustainable agriculture, its carbon footprint, and other factors. The previous generation paid attention to narrower issues, such as hunger or obesity. The Millennials are attuned to the concept of food systems.”
We are at a public health inflection point. Forty years from now, when we gaze at the high-resolution digital color photos from our own era, what will we think? Will we realize that we failed to address the obesity epidemic, or will we know that we acted wisely?
The question brings us back to the 1970s, and to Pekka Puska, the physician who directed the North Karelia Project during its quarter-century existence. Puska, now 71, was all of 27 and burning with big ideas when he signed up to lead the audacious effort. He knows the promise and the perils of idealism. “Changing the world may have been utopic,” he says, “but changing public health was possible.”
News from the School

Bethany Kotlar, PhD '24, studies how children fare when they're born to incarcerated mothers

Soccer, truffles, and exclamation points: Dean Baccarelli shares his story

Health care transformation in Africa highlighted at conference

COVID, four years in
More than one billion people around the globe are facing obesity
Researchers tracked bmi measurements gathered from more than 3,600 population-based studies since 1990.
Obesity is now the most common form of malnutrition in most countries, with the rates rising in all categories of men, women, children and adolescents since 1990. Obesity rates in adult men have nearly tripled since 1990, with obesity rates in woman doubling in that time. The rates of obesity in children and adolescents quadrupled in that time frame, as well. As of 2022, nearly 880 million adults and nearly 160 million children were living with obesity.
The prevalence of malnutrition across the globe was shared by the NCD Risk Factor Collaboration, a network of health scientists from around the world who provide and evaluate data on major risk factors for all countries, in collaboration with the World Health Organization. Dr. Peter Katzmarzyk, Associate Executive Director of the Population and Public Health Sciences department of Pennington Biomedical Research Center in Baton Rouge, was an author contributor to this publication.
The network participants reviewed body mass index data from more than 3,600 studies from 1990 to 2022, determining the rates of malnutrition, either from obesity or underweight, for all countries, and the degree to which the data has changed through the years.
"The current rates of obesity appear overwhelming, but the trend has been moving in this direction for more than three decades," said Dr. Katzmarzyk. "With more than 1 billion people living with obesity, it is important that we do not talk about obesity in a vacuum. We know that obesity can directly lead to comorbidities, including high blood pressure, heart disease, diabetes, cancer, and obstructive sleep apnea. By better understanding the root causes of obesity, we can identify ways to prevent, treat or even reverse its adverse effects."
Out of the 190-plus countries represented in this study, the United States ranked 10th highest in the world for the prevalence of obesity in men, with an increase in percentage of men from 16.9 percent in 1990 to 41.6 percent in 2022. For women, the obesity rate in 1990 was 21.2 percent, climbing to 43.8 percent in 2022, with ranking 36th highest in the world. For boys, the rate of obesity increased from 11.5 percent in 1990 to 21.7 percent in 2022, ranking the U.S. 26th highest in the world. The rate of obesity for girls in the U.S. ranked 22nd highest in the world, with the rate climbing from 11.6 percent in 1990 to 19.4 percent in 2022.
The results echo the prevalence of obesity on granular levels, as in 2020, 38 percent of adults in Louisiana are facing obesity, according to County Health Rankings and Roadmaps.
"The results of this study resoundingly affirm the value of Pennington Biomedical's mission," said Dr. John Kirwan, Executive Director of Pennington Biomedical. "With the prevalence of obesity growing through the decades, we remain steadfast in our commitment to promote metabolic health, eliminate metabolic disease, discover the triggers of obesity and improve the health of all people. I extend my appreciation and applaud the contribution that Dr. Katzmarzyk made to this important global study."
Over the same period, the rates of children, adolescents and adults being underweight fell on a global scale, with the rate of underweight of men in some African countries falling steeply. Both obesity and underweight are forms of malnutrition, with obesity rates higher than the rates of underweight for boys and girls in two thirds of the world's countries.
The Pennington Biomedical-led study "International Study of Childhood Obesity, Lifestyle and the Environment," is among the thousands of studies to have informed these results. The study involved more than 6,000 children from all inhabited continents.
- Diet and Weight Loss
- Chronic Illness
- Public Health
- World Development
- Travel and Recreation
- Social Issues
- Malnutrition
- Body mass index
- Influenza pandemic
- Public health
- Scientific misconduct
- Scientific method
Story Source:
Materials provided by Pennington Biomedical Research Center . Note: Content may be edited for style and length.
Journal Reference :
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults . The Lancet , 2024; 403 (10431): 1027 DOI: 10.1016/S0140-6736(23)02750-2
Cite This Page :
Explore More
- Speed of Visual Perception Ranges Widely
- 3D Printed Replica of an Adult Human Ear
- Extremely Fast Wound Healing: New Treatment
- Micro-Lisa! Novel Nano-Scale Laser Writing
- Simple Brain-Computer Link: Gaming With Thoughts
- Clinical Reasoning: Chatbot Vs Physicians
- Understanding People Who Can't Visualize
- Illuminating Oxygen's Journey in the Brain
- DNA Study IDs Descendants of George Washington
- Heart Disease Risk: More Than One Drink a Day
Trending Topics
Strange & offbeat.
- Open access
- Published: 21 March 2024
Prevalence and risk factors of obesity among undergraduate student population in Ghana: an evaluation study of body composition indices
- Christian Obirikorang 1 , 2 ,
- Evans Asamoah Adu 1 , 2 ,
- Enoch Odame Anto 3 , 4 ,
- Anthony Afum-Adjei Awuah 1 , 2 ,
- Angela Nana Bosowah Fynn 2 ,
- George Osei-Somuah 3 ,
- Patience Nyarkoa Ansong 5 ,
- Alexander Owusu Boakye 1 , 2 ,
- Ivy Ofori-Boadu 3 ,
- Yaa Obirikorang 5 ,
- Austin Gideon Adobasom-Anane 2 ,
- Eric NY Nyarko 6 &
- Lois Balmer 4
BMC Public Health volume 24 , Article number: 877 ( 2024 ) Cite this article
412 Accesses
Metrics details
Obesity is a classified risk factor for several of the world’s leading causes of death. In this study, we combined information contained in body mass index (BMI), total percentage body fat (TPBF) and relative fat mass (RFM) to estimate obesity prevalence and examine the risk factors associated with obesity.
The study recruited 1027 undergraduate students aged between 16 and 25 years using a cross-sectional study design and two-stage stratified random sampling between January and April 2019 from the Kwame Nkrumah University of Science and Technology, Kumasi, Ghana. Demographic, lifestyle, and family history of chronic disease data, were collected using a structured questionnaire. Bioelectrical impedance, along with height, weight, age, and gender, were used to estimate BMI and TPBF. The RFM was calculated using a published equation. The TPBF and RFM ranges were evaluated based on standard BMI thresholds and an informative combined obesity prevalence estimated in a Bayesian framework. Multiple logistic regression analysis was used to evaluate potential risk factors of overweight/obesity.
Concordance between BMI, TPBF and RFM for obesity classification was 84% among female and 82.9% among male students. The Bayesian analysis revealed a combined prevalence means of obesity of 9.4% (95%CI: 6.9-12.2%) among female students and 6.7% (95%CI:4.3-9.5%) among male students. The odds of obesity were increased between 1.8 and 2.5 for females depending on the classification index. A significant increasing trend of obesity was observed with university-level. A family history of obesity was associated with a high estimate of general, central, and high TPBF.
Using multiple adiposity indicators conjointly in a Bayesian framework offers a greater power to examine obesity prevalence. We have applied this and reported high obesity prevalence, especially among female students. University level and family history of obesity were key determinants for obesity among the student population.
Peer Review reports
Introduction
Obesity is a classified risk factor for several of the world’s leading causes of death including cardiovascular diseases, diabetes, and various types of cancers [ 1 ]. It represents the 5th and 6th major level two public health problem among women and men, respectively, leading to the toll of death and disability worldwide [ 2 ]. Obesity stands out among the top leading causes of attributable disability-adjusted life years (DALYs) this is due to the rate of exposure increasing by more than 0.5% per year [ 3 ]. The prevalence of obesity has increased in pandemic dimensions over the past 50 years [ 4 ] with 650 million adults, 340 million adolescents and 39 million children classified as obese [ 5 ]. As the obesity pandemic continues, estimates indicate that approximately 167 million adults and children will become less healthy due to being overweight or obese by 2025 [ 4 ]. Especially in developing countries, the possible implications of obesity on current and future population health and healthcare spending are likely to be enormous [ 6 ].
According to existing nationwide data, the prevalence of being overweight and obese is estimated at 25.4% and 17.1%, respectively [ 7 ]. Among the adult Ghanaian population, obesity is higher in women than men and mimics the level of urbanization [ 7 ]. A meta-analysis involving 29,160 Ghanaian children (≤ 19 years) across sixteen studies reported 8.6% obesity and 10.7% overweight [ 8 ]. There exists a significant number of studies that quantify the burden of obesity in Ghana with a special focus on the general adult population [ 9 , 10 , 11 , 12 , 13 , 14 ], women [ 15 , 16 , 17 , 18 , 19 , 20 , 21 ], school-aged children [ 22 , 23 , 24 ], adolescents [ 25 , 26 , 27 ], healthcare workers [ 28 , 29 , 30 , 31 , 32 ], civil servants [ 33 , 34 , 35 , 36 , 37 , 38 ] and commercial workers [ 39 ]. However, knowledge and data about the experiences of being overweight and obese among young Ghanaian adults are inadequate. Among the few existing studies in Ghana [ 20 , 40 , 41 , 42 ], there is an inconclusive estimate of those who are overweight/obese (4.2-39.3%) among the young adult population. This is due to population non-representativeness, that is, varying lifestyle habits and health-related behaviours of these age groups.
Among undergraduate students, which mainly represent the young adult population group, poor lifestyle habits, including decreased quality of diet and physical activity, sedentary lifestyle, alcohol use and smoking, as well as decreased quality sleep, are associated with obesity [ 42 , 43 , 44 ]. Also, the concurrence of altered eating behaviours (emotional eating, uncontrolled eating, and restrained eating), depression and poor sleep are estimated to be high among undergraduate students, mainly females [ 45 ]. These are fundamental factors driving the obesity epidemic [ 1 ]. Thus, exploring obesity experiences using representative sampling among undergraduate students will allow for the acquisition of information related to young Ghanaian adults. This knowledge will go a long way in informing strategies to combat the obesity epidemic and hopefully, related medical conditions among university students and the general young adult population.
We have mainly relied on the routine use of the body mass index (BMI) as an obesity measure. However, BMI has a limitation in differentiating between body composition and body fat distribution [ 46 , 47 , 48 , 49 ]. Alternative measures, including the bioelectrical impedance analysis (BIA) and BIA-derived body fat indices [ 50 ], like the body adiposity index [ 51 ] and relative fat mass (RFM) [ 52 ], have been proposed. These measures claim to adjust the limitations of BMI and alternatively represent cost-effective indices to appropriately identify individuals with accuracy close to that of underwater weighing [ 53 ] and dual-energy X-ray absorptiometry [ 54 ]. In particular, RFM and total percentage body fat (TPBF) have been validated as being a more accurate measure compared to BMI to estimate whole-body fat percentage, in addition to improving body fat-defined obesity misclassification among different population groups [ 55 ].
In this study, we have combined information contained in body mass index (BMI), TPBF and relative fat mass (RFM) to estimate an informative obesity prevalence. Because there is no single universally accepted measure of adiposity and each index has its drawbacks, we performed an evaluation analysis of waist-to-height derived RFM, corresponding to central fatness and TPBF corresponding to overall adiposity based on the routinely used weight-to-height derived BMI thresholds. By using data from the evaluation analysis assessing concordance and the estimate of measurement properties of TPBF and RFM with BMI, we combined this classification in a Bayesian framework. Thus, we reported an informative obesity prevalence corresponding to central and general adiposity, with much power. Our governing hypothesis was that a combined estimate of obesity in a Bayesian framework does not offer a more representative estimate than commonly used BMI, RFM and TPBF in isolation.
Because it is common in population surveys to have one or multiple measures investigating the same condition, the Bayesian framework has been useful in drawing inferences on disease prevalence and measurement properties while adjusting for the possibility of conditional dependence between several disease measures [ 56 , 57 , 58 ]. In practice, two aspects exist, that can be used to estimate uncertainty and improve the accuracy of population estimate of prevalence. The first is to use the prior information from existing studies, while the second requires the integration of multiple population-based measures into one estimate [ 57 , 58 ]. In our case, we employed the second approach for this study.
Methodology
This was a cross-sectional study undertaken at the Kwame Nkrumah University of Science and Technology (KNUST), Kumasi, between August 2018 and July 2019. All students provided written informed consent for their participation in the study. Ethical approval with reference ID (CHRPE/AP/030/19) was obtained from the Committee on Human Research, Publications and Ethics (CHRPE), School of Medicine and Dentistry, Kwame Nkrumah University of Science & Technology.
Sample design
A two-stage stratified random sampling was used to select 1027 first to fourth-year undergraduate students aged 16–25 years. These students were selected to cover the six Colleges in KNUST including the College of Science (CoS), Art and Built Environment (CABE), Humanities and Social Sciences (CoHSS), Health Sciences (CoHS), Engineering (CoE), and Agric and Natural Resources (CANR). Students who were feverish, bodybuilders or highly trained athletes, and students with osteoporosis or oedema (swelling in the body) were excluded.
The targeted population consisted of undergraduate students’ population from 1st to 4th year of their academic level, across the six colleges of KNUST. The operational definition of a student’s year directly depended on the recruitment dates between January and April 2019. This period represents the second semester where first-year students have spent at least one complete semester in the college. We used a two-stage stratified cluster survey design. The study population and sampling consisted of the entire student population at KNUST (43,757) during the 2018/2019 academic year. Considering the low probability of sampling 5th and 6th -year students, available only for health sciences, were excluded from the sample. The first stage of clustering involved censoring all colleges with probabilities relative to the number of departments. From each selected college, a fixed number of departments was sampled. Eight students (two students, male and female, from levels 1st, 2nd, 3 rd, and 4th year) are sampled at random at the department level.
Sample size
The required sample size to assess overweight/obesity prevalence among students was calculated assuming p = 0.18 [ 41 ], level of acceptable precision d = 0.05 (or ± 5%) at 95% CI corresponds to 227 which relate to 28 departments of 8 students in each. Using analysis of data from a previous study [ 41 ] within the same KNUST student population, the design effect was estimated at 1.9 for overweight/obesity. This was based on 6 clusters with an average of 50 students per cluster (n = 300) and an intra-cluster coefficient of 0.1. Considering these figures and while assuming a college response rate of 90% and individual students response rate at 85%, the actual sample size was estimated to be 83 departments of 8 students each (n = 664) with male and female students having equal proportion of being sampled. In the end, we recruited 1027 participants to increase the power of our estimate. Table 1 illustrates the minimum possible sampling expectations.
The equation for sample size calculation:
\(n=(z^2 \times p(1-p\left)\right(DEEF\left)\right)/\left(\right(j\left)\right(k\left)\right(l\left)\right(d^2\left)\right)\) [ 59 ].
Z was taken at 1.96, j = is the expected response rate as a proportion (0.85 × 0.9); k is the average department size (n = 8). The proportion of the student population accounted for by the targeted of interest (l) was set at 0.8. DEFF is the design effect.

Data collection and anthropometric measurement
A structured questionnaire was used to collect data on socio-demographic characteristics, lifestyle risk factors and family history of obesity, diabetes and hypertension (Table 2 ). socio-demographic data included age, sex, year of study, and college. Lifestyle data included alcohol intake, smoking and exercise history. Height was measured with a portable height rod Stadiometer with students in a straight posture, feet placed together and flat on the ground. Waist circumference (WC) was measured using a tape measure at the point of the umbilicus and maximum gluteal protrusion. Each participant was asked to stand straight on the main unit of the OMRON BF511 Clinically Validated Full Body Composition Monitor with 8 high-precision sensors for hand-to-foot measurement (OMRON HEALTHCARE Co., Ltd.), looking straight, barefooted and with arms horizontally raised holding a display unit, extended at a 90° angle for weight, body fat mass (BFM) and TPBF estimation. The machine conforms to EN60601-1-2:2015 Electro Magnetic Compatibility (EMC) standard and uses the bioelectrical impedance, along with height, weight, age and gender information to generate results based on the OMRON’s data of body composition [ 60 ]. The Omron Full Body Sensor Body Composition Monitor and Scale estimates the TPBF by the Bioelectrical Impedance Method. The instrument sends an extremely weak electrical current of 50 kHz and less than 500 µA through the participant’s body to determine the amount of water in each tissue. The instrument takes measurements from both hands and feet to reduce the influence of water movement on body composition results. The output of the OMRON BF511 monitor included TPBF, relative visceral fat content, body mass index (BMI), and skeletal muscle. We included the TPBF and BMI output together with RFM for the analysis. RFM was calculated from WC and height:
Obesity was defined based on BMI thresholds for overweight (≥ 25 Kg/m 2 ), and obesity (≥ 30 Kg/m 2 ) according to the World Health Organization’s criteria [ 1 ].
Statistical analyses
Patient characteristics were stratified by primary clusters (colleges). Counts and corresponding percentages were used to describe categorical variables and compared using the Chi-square test. Mean and standard deviations were used to describe continuous variables if they followed the Gaussian normal distribution. Median and interquartile ranges were used if otherwise distributed. Either the One-way analysis of variance or Kruskal-Willi’s test was used to compare continuous variables among primary clusters. Multiple comparison analysis with Bonferroni correction was performed when the probability value was < 0.05. Sex-stratified prevalence estimates for obesity were determined according to BMI thresholds and the corresponding TPBF and RFM thresholds for age. The Passing and Bablok regression analysis was used to evaluate the measurement agreement and possible systematic bias for TPBF and RFM against BMI [ 61 ]. The diagnostic accuracy of TPBF and RFM was estimated based on the optimal cut-off, sensitivity, and specificity analysis, considering the area under the curve (AUC) estimated with the receiver-operating characteristic curves (ROC) analysis. We integrated the results from TPBF and RFM for obesity definition based on BMI threshold in a Bayesian framework, to report a combined obesity prevalence. Twenty chains were used to sample 50,000 samples per chain (25,000 warmups and 25,000 post warmups). Posterior densities were estimated using the Hamiltonian Monte Carlo (HMC) method. Summaries of posterior distributions including the mean and 95% credible interval were used to interpret the results. Multiple logistic regression analysis was used to evaluate potential risk factors of overweight/obesity. A two-sided p -value of 0.05 was considered statistically significant. Statistical analyses were performed using R version 4.3.0 (2023-04-21 ucrt) and MedCalc software Bvba, version 18.9.1.
Table 2 displays the characteristics of the study participants by sampling strata. There was a significant over-representation of female students at CoHSS and underrepresentation at CABE and CoE (p-value < 0.001). The proportion of students that consume alcohol was comparatively low in CoHS (p-value = 0.039). Compared with CANR and CoHSS, a significant proportion of students from CoHS (31.2%), CoE and CoS (18.4% each) never engaged in regular exercise (p-value < 0.001). We observed significant variance in TPBF% measurements compared across the colleges (p-value < 0.001).
Prevalence of being overweight and Obese based on standard BMI thresholds
Using BMI ≥ 25.0 Kg/m 2 , approximately 31% and 15% of female and male students were classified as overweight/obese. However, only 2.4% of male students and 8.0% of female students were classified as obese using BMI ≥ 30.0 Kg/m 2 (Table 3 ). We observed a trend towards increased overweight/obesity with age. Among students < 20 years, 26.3% and 13.6% female and male, respectively, were classified as being overweight and/or obese. Among ≥ 20 years female and male students, 34.5% and 15.5% were classified as overweight and/or obese.
Evaluation of RFM and BAI-derived TPBF based on BMI
Passing and Bablok regression analysis are shown in Table S1 . Here we emphasised the interpretation based on the observed random difference. The null assumption was that the observed random differences within ± 1.96 residual standard deviation (RSD) > 10%. Linearity between the variables was evaluated based on the custom test for linearity probability value (Table S1 , Figure S1 ). Concordance was observed between TPBF and BMI (RSD = 1.60, ± 1.96 = -3.14 to 3.14) compared with RFM (RSD = 2.64, ± 1.96 = -5.17 to 5.17) among male students. Similarly, among female students, TPBF demonstrated good agreement with BMI (RSD = 2.23, ± 1.96 = -4.37 to 4.37) compared to RFM (RSD = 2.98, ± 1.96 = -5.83 to 5.83). The linearity test revealed a significant deviation from linearity between TPBF and BMI (p-value < 0.01) and between BMI and RFM (p-value > 0.05). The ROC curve analysis (Fig. 1 ) identified TPBF threshold values of > 20.3% and > 20.8% and was associated with high information values for defining being overweight (BMI > 29.9 Kg/m 2 ) among male students: 15–19 years (AUC = 0.941, sensitivity = 100.0%, specificity = 87.8%) and 20–25 years (AUC = 0.942, sensitivity = 94.4%, specificity = 89.6%), respectively. Also, TPBF threshold values for defining obesity (BMI ≥ 30.0 Kg/m 2 ) among 15–19 years and 20–25 years female students were > 35.4% and > 35.2%, respectively (Fig. 1 ).
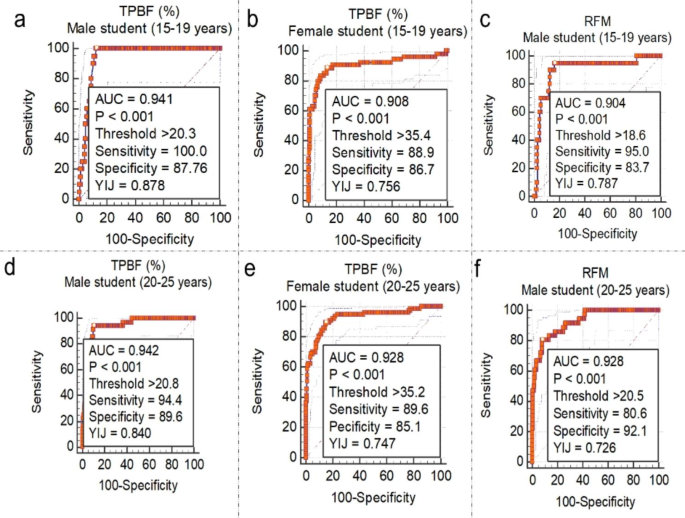
Threshold of TPBF and RFM estimates corresponding to WHO-defined BMI thresholds for overweight among male and female students
An optimal threshold value for TPBF > 26.2% (AUC = 0.981, sensitivity = 100.0%, specificity = 95.2%) for males (15–19 years) and > 24.4% (AUC = 0.938, sensitivity = 80.0%, specificity = 92.0%) had exceptional diagnostic accuracy for obesity (BMI ≥ 29.9 Kg/m 2 ) among male students (Fig. 2 ). The TPBF threshold of > 35.4% and > 35.2 was optimal for defining overweight female students 15–19 years and 20–25 years, respectively. TPBF values > 41.8% and 44.3% were optimal for defining obesity among female students 15–19 years and 20–25 years.
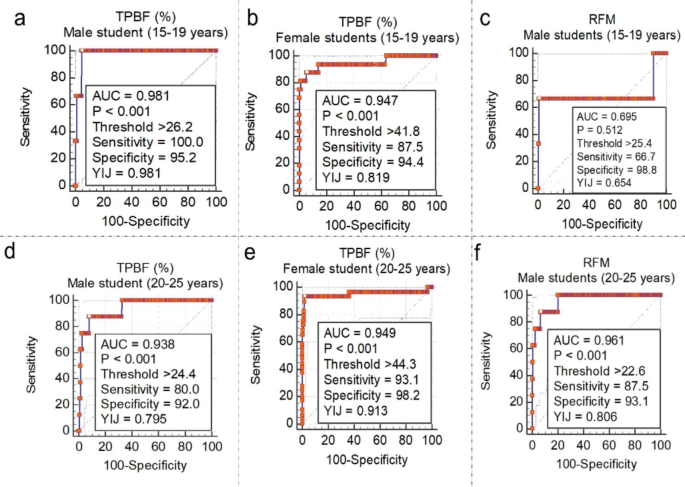
Threshold of TPBF and RFM estimates corresponding to WHO-defined BMI thresholds for obesity among male and female students
The ROC curve analysis of RFM for defining overweightness revealed an optimal cut-off of > 18.6 and > 20.5 among 15–19 years and 20–25 years male students, respectively (Fig. 1 c and f). RFM thresholds for defining obesity were > 25.4 and > 22.6 among male students 15–19 years and 20–25 years respectively (Fig. 2 a and f). Among female students (Fig. 3 a and b), RFM thresholds of > 20.7 and > 20.9 were associated with high information values for defining overweight among 15–19 years and 20 − 15 years, respectively. Moreover, obesity definition thresholds were > 24.5 and > 25.2, respectively among female students 15–19 years and 20 − 15 years (Fig. 3 c and d).
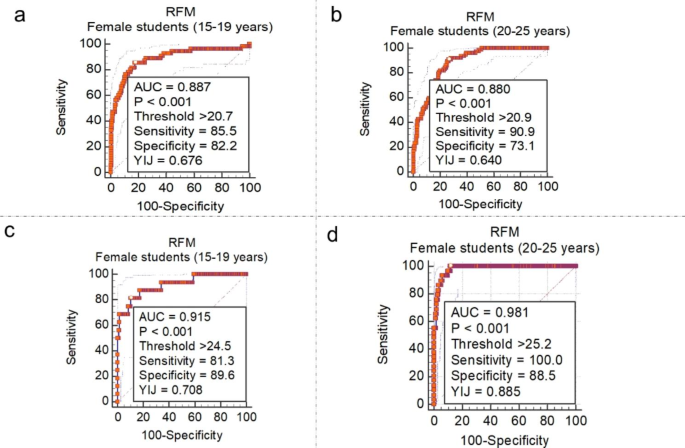
Threshold of RFM estimates corresponding to WHO-defined BMI thresholds for overweight and obesity among female students
The concordance between BMI, TPBF and RFM for obesity classification was 84% (95% lower limit = 82.0%) among female students and 82.9% (95% lower limit = 80.5%) among male students. The findings of the posterior predictive checks using the simulated data are presented in Figure S3 . The results of the Bayesian analysis suggest that the combined prevalence mean of overweight/obesity for TPBF and RFM were 33.8% (95%CI: 29.2-38.6%) among female students and 17.0% (95%CI: 13.1-21.3%) among male students. The combined prevalence mean of obesity for TPBF and RFM was 9.4% (95%CI: 6.9-12.2%) among female students and 6.7% (95%CI: 4.3-9.5%) among female students (Fig. 4 ).
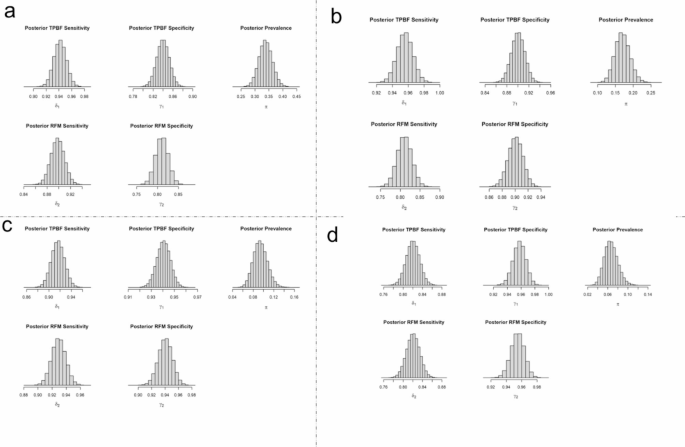
Marginal posterior density for the prevalence of obesity using combined data from TBPF and RFM. Note: π represents posterior prevalence using both TPBF and RFM data, δ1 represents sensitivity for TPBF data, γ1 represents specificity for TPBF data, δ2 represents sensitivity for RFM data, and γ2 represents specificity for RFM data
Factors associated with overweight/obesity among students
From the Multiple Logistic Regression analysis sex and family history of education were found to be consistent factors associated with general and central adiposity and percentage body fat distribution. The odds of being overweight were increased between 1.8 and 2.5, for women, depending on the classification criteria (Table 4 ). Family history of obesity was associated with increased odds of general obesity (OR = 3.48, 95%CI: 2.04–5.91), central obesity (OR = 1.98, 95%CI: 1.18–3.30) and high percentage body fat distribution (OR = 2.36, 95%CI: 1.42–3.94). Compared with first years students, the odds of central obesity and high percentage body fat were increased among third year students: OR = 2.77(1.59–4.82) and OR = 1.79(1.05–3.08), and fourth year students: OR = 3.26(1.76–6.04) and OR = 2.34(1.29–4.23), respectively.
This study sought to investigate the prevalence and risk factors of obesity among undergraduate students using multiple adiposity indices in a Byersian framework. In general the prevalence of being overweight/obese in this age group of young adults was high: 33.8% among female students and 17.0% among male students. Significant association were found between being overweight/obese and potential factors including sex, family history of obesity and university level.
Using the combined informative estimate, we observed an obesity prevalence of 6.7% among male students and 9.4% among female students. More generally, 17.0% of male students and 33.8% of female students were classified as having weight status corresponding to abnormal central and general adiposity as well as high body fat accumulation. These estimates are within the obesity prevalence range of 1.7–19.0% as estimated by a previous study in the same population group using different anthropometric indices [ 41 ]. Among the university student population in Botswana [ 43 ] and Ghana [ 44 ], similar estimates of overweight and/or obesity prevalence have been reported. In a larger study representing university students from 22 countries [ 62 ], 14.1% and 5.2% of female students and 18.9% and 5.8% of male students were reported to be overweight and obese, respectively. These data highlight the significant burden of obesity among undergraduate university students, which has a potential future health impact. In line with the current 16.2%, tertiary enrolment rate in Ghana [ 63 ], the current estimate of obesity reflects a significant national obesity problem among the young adult population with significant future health consequences.
We believe our estimate may be a true reflection of the obesity burden among student populations. First, TPBF and RFM contain high information values for obesity and fat distribution classification. Second, RFM is less accurate than BMI in lean individuals [ 64 ] whiles BAI-derived TPBF is less accurate than BMI in obese individuals [ 65 ]. Thus, combining these measures in a population estimation of obesity would provide a value informed by a broader distribution of obesity and fat distribution among the population group. Third, we relied on prior information from the concordance between both RFM and TPBF with standard BMI thresholds and a previous study from the same population [ 41 ]. Finally, the method adapted for the estimation of the combined prevalence of obesity has been successfully applied elsewhere [ 66 ]. Because this approach could be more flexible and adaptable, there is a need to test its performance in other settings with other related adiposity estimates.
An important observation of concern was the proportion of overweight/obese female students, which was higher compared with male students. This observation is consistent in several other studies [ 40 , 41 , 43 , 62 ], suggesting an increased risk for weight gain in young women and the critical need for interventions to prevent obesity and the host of associated adverse health outcomes. The evidence has been confirmed in several nationally representative surveys, where greater increases in weight are observed in young women aged 18 to 35 years compared with those seen in older women [ 67 ]. In a study among young Ghanain women aged between 15 and 24 years [ 20 ], overweight/obesity increased by 49% between 1993 and 2014 and projected a future prevalence of 35% by the year 2040. Fat deposition in women usually begins with the onset of puberty and continues unless consciously controlled [ 68 ]. Some studies has reported that female transition from adolescence to adulthood is associated with certain obesogenic dietary and physical activity behaviours to satisfy a historic valorization of large body size as a function of beauty, sexual attraction, prosperity, health and prestige [ 20 , 69 , 70 ].
In a prospective analysis of mother-daughter dyads and father-son dyads, the study reported a large and concerning increase in obesity rates over two generations of young adults, especially females [ 71 ]. These findings indicate that young adulthood represents periods of crucial importance regarding the establishment of life-long lifestyle habits and skills to control obesity. Studies have attributed this to a lack of knowledge and skills around food and nutrition, depression, anxiety, stress, satiety, neural responses, and possibly sleep patterns and premenstrual cravings [ 42 , 43 , 44 , 67 , 72 ]. Thus, there is the need to study these factors and their relationship with obesity among undergraduate students in Ghana, which can benefit future interventions.
We observed a trend in increasing obesity prevalence with academic level such that third- and fourth-year students had significantly increased obesity prevalence than first- and second-year students. Similar findings have been observed in other related studies [ 41 , 73 , 74 ] but not all [ 75 ]. This relationship may suggest the role of other factors of obesity associated with progressive academic level, which was not the focus of this study. We recommend future research to focus on changing lifestyle and eating habits of students related to progressive academic level. We replicated the association between obesity and family history and increased risk of obesity prevalence. This finding contributes to the evidence that genetics play an important role in the onset of obesity and the severity of obesity [ 76 , 77 ]. In several studies, sendentary life has been strsongly associated with being overweight/obese [ 11 , 17 , 27 , 28 ]. However, we did not find a significant association between being overweight/obese and students engagement in regular physical activity.
We would like to acknowledge some limitations of this study. First, Bayesian modelling is reliance on prior information, in our case we used the prior prevalence, concordance and diagnostic estimates obtained from the linked data and previous studies within the same population. As such, our analyses are limited by the accuracy of standard BMI thresholds for classifying obesity. Second, female students were over-represented in the dataset, which could bias the estimation of obesity prevalence. Although, we considered this in the analysis by reporting sex-specific prevalence estimates. Also, the generalizability of our estimate may be limited as data were obtained from only one tertiary institution in Ghana. This approach is significant to fill a gap in the current lack of consensus on the appropriate adiposity index and serves as the opportunity to unique data linkage and novel analytical techniques to improve obesity surveillance.
As different adiposity indices become increasingly available, multiple indicators used in combination may offer a greater power to examine obesity prevalence. We have demonstrated this by integrating central adiposity and percentage body fat criteria relative to standard BMI thresholds in a Bayesian framework and reported high obesity prevalence, especially among female students. We also demonstrated that obesity prevalence increases with university level and among students with a family history of obesity. The study suggests that the prevalence of being overweight or obese is expected to increase in the coming years, leading to several health issues. It emphasizes the requirement for public health efforts and interventions at a national level to control the problem and its associated costs and co-morbidities. Furthermore, interventions against obesity should be customized to target the socio-demographic disparities highlighted in the study.
Data Availability
The datasets and codes used and/or analysed during the current study are within the manuscript, and available at the GitHub repository ( https://github.com/EvansKCCR/obesity_among_students ).
Abbreviations
Relative fat mass
Total percentage of body fat
Body mass index
Bioelectrical impedance analysis
Kwame Nkrumah University of Science and Technology
Design effect
Receiver operative characteristics curve
Area under the curve
Hamiltonian Monte Carlo
Residual standard deviation
Obesity. and overweight. In: Department of Sustainable Development and Healthy Environments World Health Organization; 2021.
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019:a systematic analysis for the global burden of Disease Study 2019. The Lancet. 2020;396(10258):1223–49.
Murray CJL, Abbafati C, Abbas KM, Abbasi M, Abbasi-Kangevari M, Abd-Allah F, Abdollahi M, Abedi P, Abedi A, Abolhassani H, et al. Five insights from the global burden of Disease Study 2019. The Lancet. 2020;396(10258):1135–59.
Article Google Scholar
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Reviews Endocrinol. 2019;15(5):288–98.
World Obesity Day. 2022 – Accelerating action to stop obesity. In.: World Health Organization; 2022.
Nugent R. Chronic Diseases in developing countries: health and economic burdens. Ann N Y Acad Sci. 2008;1136(1):70–9.
Article PubMed Google Scholar
Ofori-Asenso R, Agyeman AA, Laar A, Boateng D. Overweight and obesity epidemic in Ghana—a systematic review and meta-analysis. BMC Public Health. 2016;16(1):1–18.
Akowuah PK, Kobia-Acquah EJJoN. Metabolism: Childhood obesity and overweight in Ghana: a systematic review and meta-analysis. Journal of Nutrition Metabolism 2020, 2020.
Amegah A, Lumor S, Vidogo FJAJF. Agriculture, Nutrition, Development: prevalence and determinants of overweight and obesity in adult residents of Cape Coast, Ghana: a hospital-based study. Afr J Food Agric Nutr Dev 2011, 11(3).
Anderson AK. Prevalence of anemia, overweight/obesity, and undiagnosed Hypertension and Diabetes among residents of selected communities in Ghana. Int J Chronic Dis 2017, 2017.
Boateng GO, Adams EA, Odei Boateng M, Luginaah IN, Taabazuing M-M. Obesity and the burden of health risks among the elderly in Ghana: a population study. PLoS ONE. 2017;12(11):e0186947.
Article PubMed PubMed Central Google Scholar
Nyakotey DA, Ananga AS, Apprey C. Assessing physical activity, nutrient intake and obesity in middle-aged adults in Akuse, Lower Manya Krobo, Ghana. J Health Res. 2022;36(2):199–208.
Obirikorang C, Osakunor DNM, Anto EO, Amponsah SO, Adarkwa OK. Obesity and cardio-metabolic risk factors in an urban and rural population in the Ashanti Region-Ghana: a comparative cross-sectional study. PLoS ONE. 2015;10(6):e0129494.
William K. Obesity and cardiovascular risk factors in a Pentecostal population in Kumasi-Ghana. J Med Sci. 2008;8(8):682–90.
Agbeko MP, Akwasi K-K, Andrews DA, Gifty OB. Predictors of overweight and obesity among women in Ghana. Open Obes J 2013, 5(1).
Asosega KA, Adebanji AO, Abdul IW. Spatial analysis of the prevalence of obesity and overweight among women in Ghana. BMJ open. 2021;11(1):e041659.
Asosega KA, Aidoo EN, Adebanji AO, Owusu-Dabo E. Examining the risk factors for overweight and obesity among women in Ghana: A multilevel perspective. Heliyon 2023.
Marquis GS, Colecraft EK, Bannerman B, Thompson-Colón T. Overweight and obesity among women in a predominantly rural district of Ghana. The FASEB Journal 2016, 30:667.669-667.669.
Tuoyire DA. Television exposure and overweight/obesity among women in Ghana. BMC Obes. 2018;5(1):1–10.
Tuoyire DA. Overweight/obesity among 15-to 24-year-old women in Ghana: 21-year trend, future projections and socio-demographic correlates. J Biosoc Sci. 2021;53(6):839–55.
Tuoyire DA, Kumi-Kyereme A, Doku DT. Socio-demographic trends in overweight and obesity among parous and nulliparous women in Ghana. BMC Obes. 2016;3(1):1–14.
Adom T, De Villiers A, Puoane T, Kengne AP. Prevalence and correlates of overweight and obesity among school children in an urban district in Ghana. BMC Obes. 2019;6:1–11.
Aryeetey R, Lartey A, Marquis GS, Nti H, Colecraft E, Brown P. Prevalence and predictors of overweight and obesity among school-aged children in urban Ghana. BMC Obes. 2017;4:1–8.
Mogre V, Gaa PK, Abukari RNS. Overweight, obesity and thinness and associated factors among school-aged children (5–14 years) in Tamale, Northern Ghana. Eur Sci J 2013, 9(20).
Akoto S, Tandoh MA, Nsiah K, Asamoah-Boakye O, Annaful VT. Lifestyle habits, macronutrient intake, and obesity prevalence among adolescents in rural-periurban community senior high schools in the Ho municipality of Ghana. Front Nutr 2022, 9.
Peltzer K, Pengpid S. Overweight and obesity and associated factors among school-aged adolescents in Ghana and Uganda. Int J Environ Res Public Health. 2011;8(10):3859–70.
Amoh I, Appiah-Brempong E. Prevalence and risk factors of obesity among senior high school students in the Adansi North district of Ghana. Int J Community Med Public Health. 2017;4(10):3762–9.
Aryee P, Helegbe G, Baah B, Sarfo-Asante R, Quist-Therson R. Prevalence and risk factors for overweight and obesity among nurses in the tamale metropolis of Ghana. J Med Biomedical Sci. 2013;2(4):13–23.
Duodu C, Awuni TK, Attito P, Zotor FB. Assessment of overweight and obesity prevalence among practicing nurses and midwives in the Hohoe Municipality of the Volta Region, Ghana. Sci J Public Health. 2015;3(6):842–51.
Obirikorang Y, Obirikorang C, Enoch O, Acheampong E, Tuboseiyefah P, Miriam A, Emmanuella N. Prevalence and risk factors of obesity among practicing nurses at three selected hospitals in Kumasi Metropolis, Ghana. J Med Biomedical Sci. 2016;5(3):45–55.
Amo-Mensah P, Vanotoo L, Davies-Teye B. Prevalence of overweight and Obesity among Health Personnel in an urban Ghana: a descriptive cross-sectional study, 2017. Value in Health. 2017;20(9):A544.
Abubakar MB, Uthman YA, Ibrahim KG. Prevalence of overweight and obesity among health-care workers in Ghana: a systematic review. Nigerian J Experimental Clin Biosci. 2021;9(1):47.
Addo J, Smeeth L, Leon D. Obesity in urban civil servants in Ghana: association with pre-adult wealth and adult socio-economic status. Public Health. 2009;123(5):365–70.
Article CAS PubMed Google Scholar
Addo P. Prevalence of obesity and overweight and Associated factors among Financial Institution workers in Accra Metropolis, Ghana: a Case Control Study. Value in Health. 2016;19(7):A579.
Addo PN, Nyarko KM, Sackey SO, Akweongo P, Sarfo B. Prevalence of obesity and overweight and associated factors among financial institution workers in Accra Metropolis, Ghana: a cross sectional study. BMC Res Notes. 2015;8(1):1–8.
Atuahene M, Ganle JK, Adjuik M, Atuahene NF, Kampitib GB. Overweight and obesity prevalence among public servants in Nadowli district, Ghana, and associated risk factors: a cross-sectional study. BMC Obes. 2017;4(1):1–8.
Kumah DB. Prevalence of overweight and obesity among staff of a Tertiary Institution in Kumasi, Ghana. EC Nutr. 2016;5:1277–81.
Google Scholar
Nuertey BD, Alhassan AI, Nuertey AD, Mensah IA, Adongo V, Kabutey C, Addai J, Biritwum RB. Prevalence of obesity and overweight and its associated factors among registered pensioners in Ghana; a cross sectional studies. BMC Obes. 2017;4(1):1–12.
Anto EO, Owiredu W, Adua E, Obirikorang C, Fondjo LA, Annani-Akollor ME, Acheampong E, Asamoah EA, Roberts P, Wang W. Prevalence and lifestyle-related risk factors of obesity and unrecognized Hypertension among bus drivers in Ghana. Heliyon. 2020;6(1):e03147.
Mogre V, Nyaba R, Aleyira S. Lifestyle risk factors of general and abdominal obesity in students of the school of medicine and health science of the University of Development Studies, Tamale, Ghana. International Scholarly Research Notices 2014, 2014.
Obirikorang C, Anto EO, Addai P, Obirikorang Y, Acheampong E. Prevalence and risks factors of overweight/obesity among undergraduate students: an institutional based cross-sectional study, Ghana. J Med Biomedical Sci. 2017;6(1):24–34.
Agyei A, Yorke E, Boima V. Prevalence of overweight and obesity and its relation to Diet and physical activity among medical students in Accra, Ghana. Afr J Health Sci. 2022;35(2):99–113.
Tapera R, Merapelo MT, Tumoyagae T, Maswabi TM, Erick P, Letsholo B, Mbongwe B. The prevalence and factors associated with overweight and obesity among University of Botswana students. Cogent Med. 2017;4(1):1357249.
Mogre V, Nyaba R, Aleyira S. Lifestyle risk factors of general and abdominal obesity in students of the school of medicine and health science of the University of Development Studies, Tamale, Ghana. ISRN obesity 2014, 2014.
Amoako M, Amoah-Agyei F, Du C, Fenton JI, Tucker RM. Emotional Eating among Ghanaian University Students: Associations with Physical and Mental Health Measures. 2023, 15(6):1526.
Dolan CM, Kraemer H, Browner W, Ensrud K, Kelsey JL. Associations between body composition, anthropometry, and mortality in women aged 65 years and older. Am J Public Health. 2007;97(5):913–8.
Kontogianni MD, Panagiotakos DB, Skopouli FN. Does body mass index reflect adequately the body fat content in perimenopausal women? Maturitas. 2005;51(3):307–13.
Obirikorang C, Obirikorang Y, Acheampong E, Anto EO, Toboh E, Asamoah EA, Amakwaa B, Batu EN, Brenya P. Association of wrist circumference and waist-to-height ratio with cardiometabolic risk factors among type II diabetics in a Ghanaian population. Journal of diabetes research 2018, 2018.
Frankenfield DC, Rowe WA, Cooney RN, Smith JS, Becker D. Limits of body mass index to detect obesity and predict body composition. Nutrition. 2001;17(1):26–30.
Sun SS, Chumlea WC, Heymsfield SB, Lukaski HC, Schoeller D, Friedl K, Kuczmarski RJ, Flegal KM, Johnson CL, Hubbard VS. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr. 2003;77(2):331–40.
Freedman DS, Thornton JC, Pi-Sunyer FX, Heymsfield SB, Wang J, Pierson RN Jr, Blanck HM, Gallagher D. The body adiposity index (hip circumference ÷ height1. 5) is not a more accurate measure of adiposity than is BMI, waist circumference, or hip circumference. Obesity. 2012;20(12):2438–44.
Senkus KE, Crowe-White KM, Locher JL, Ard JD. Relative fat mass assessment estimates changes in adiposity among female older adults with obesity after a 12-month exercise and diet intervention. Ann Med. 2022;54(1):1160–6.
Article CAS PubMed PubMed Central Google Scholar
Brodowicz GR, Mansfield RA, McClung MR, Althoff SA. Measurement of body composition in the elderly: dual energy x-ray absorptiometry, underwater weighing, bioelectrical impedance analysis, and anthropometry. Gerontology. 1994;40(6):332–9.
Bi Y, Wang R. Application of DEXA to body composition measurement. Sports Sci Res. 2008;29(1):17.
Woolcott OO, Bergman RN. Relative fat mass (RFM) as a new estimator of whole-body fat percentage a cross-sectional study in American adult individuals. Sci Rep. 2018;8(1):10980.
Joseph L, Gyorkos TW, Coupal L. Bayesian estimation of Disease Prevalence and the parameters of diagnostic tests in the absence of a Gold Standard. Am J Epidemiol. 1995;141(3):263–72.
Erkanli A, Soyer R, Stangl D. Hierarchical bayesian analysis for Prevalence Estimation. Case studies in bayesian statistics: 1997// 1997; New York. NY: Springer New York; 1997. pp. 325–46.
Chapter Google Scholar
Speybroeck N, Devleesschauwer B, Joseph L, Berkvens DJI. Misclassification errors in prevalence estimation: bayesian handling with care. 2013, 58:791–5.
Arya R, Antonisamy B, Kumar SJTIJP. Sample size estimation in prevalence studies. 2012, 79:1482–8.
Manual OI. Full body Sensor Body Composition Monitor and Scale Model HBF–510. China: Omron Healthcare 2008.
Passing H, Bablok. A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, part I. J Clin Chem Clin Biochem Z fur Klinische Chemie Und Klinische Biochemie. 1983;21(11):709–20.
CAS Google Scholar
Peltzer K, Pengpid S, Samuels TA, Özcan NK, Mantilla C, Rahamefy OH, Wong ML, Gasparishvili A. Prevalence of overweight/obesity and its associated factors among university students from 22 countries. Int J Environ Res Public Health. 2014;11(7):7425–41.
Ghana - Gross. enrolment ratio in tertiary education [ https://knoema.com/atlas/Ghana/topics/Education/Tertiary-Education/Gross-enrolment-ratio-in-tertiary-education ].
Woolcott OO, Bergman RN. Relative Fat Mass as an estimator of whole-body fat percentage among children and adolescents: a cross-sectional study using NHANES. Sci Rep. 2019;9(1):15279.
Li YC, Li CI, Lin WY, Liu CS, Hsu HS, Lee CC, Chen FN, Li TC, Lin CC. Percentage of body fat assessment using bioelectrical impedance analysis and dual-energy X-ray absorptiometry in a weight loss program for obese or overweight Chinese adults. PLoS ONE. 2013;8(4):e58272.
Edwards J, Pananos AD, Thind A, Stranges S, Chiu M, Anderson KK. A bayesian approach to estimating the population prevalence of mood and anxiety disorders using multiple measures. Epidemiol Psychiatric Sci. 2021;30:e4.
Pegington M, French DP, Harvie MN. Why young women gain weight: a narrative review of influencing factors and possible solutions. 2020, 21(5):e13002.
Ersoy C, Imamoglu S. Comparison of the obesity risk and related factors in employed and unemployed (housewife) premenopausal urban women. Diabetes Res Clin Pract. 2006;72(2):190–6.
Cohen E, Boetsch G, Palstra FP, Pasquet P. Social valorisation of stoutness as a determinant of obesity in the context of nutritional transition in Cameroon: the Bamiléké case. Social science & medicine ( 1982 ) 2013, 96:24–32.
Jokela M, Elovainio M, Kivimäki M. Lower fertility associated with obesity and underweight: the US National Longitudinal Survey of Youth. Am J Clin Nutr. 2008;88(4):886–93.
Alati R, Betts KS, Williams GM, Najman JM, Zalbahar N, Mamun A. Generational increase in obesity among young women: a prospective analysis of mother–daughter dyads. Int J Obes. 2016;40(1):176–80.
Article CAS Google Scholar
Eating Patterns of Young Women (18–25 y) with Overweight and Obesity: A Preliminary Investigation. 2023, 15(7):1652.
Elham AA, Anas A, Ikram K, Jayakumary M. Obesity among university students: a cross-sectional study in Ajman, UAE. 2015.
Ghazawy ER, Mahfouz EM, Rahman A-E, Ahmed T. Emam SAJMJoMR: Obesity/Overweight among University students. Minia Egypt. 2022;33(3):30–6.
Boukrim M, Obtel M, Lahlou L, Razine R. University students’ perceptions and factors contributing to obesity and overweigh in Southern of Morocco. Afr Health Sci. 2021;21(2):942–50.
Corica D, Aversa T, Valenzise M, Messina MF, Alibrandi A, De Luca F. Wasniewska MJFie: Does family history of obesity, cardiovascular, and metabolic diseases influence onset and severity of childhood obesity? 2018, 9:187.
van der Sande MA, Walraven GE, Milligan PJ, Banya WA, Ceesay SM, Nyan OA. McAdam KPJBotWho: family history: an opportunity for early interventions and improved control of Hypertension, obesity and Diabetes. 2001, 79(4):321–8.
Download references
Acknowledgements
We would like to thank the students of KNUST who dedicated their time and participation to this study. We also express our gratitude to the KNUST Counselling unit and the University Hospital for their support during the data collection.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Molecular Medicine, School of Medical Science, Kwame Nkrumah University of Science and Technology (KNUST), Kumasi, Ghana
Christian Obirikorang, Evans Asamoah Adu, Anthony Afum-Adjei Awuah & Alexander Owusu Boakye
Kumasi Centre for Collaborative Research, Kumasi, Ghana
Christian Obirikorang, Evans Asamoah Adu, Anthony Afum-Adjei Awuah, Angela Nana Bosowah Fynn, Alexander Owusu Boakye & Austin Gideon Adobasom-Anane
Department of Medical Diagnostics, Faculty of Allied Health Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Enoch Odame Anto, George Osei-Somuah & Ivy Ofori-Boadu
Centre for Precision Health, School of Medical and Health Sciences, Edith Cowan University, Western Australia, Australia
Enoch Odame Anto & Lois Balmer
Department of Nursing, Faculty of Health Sciences, Garden City University College, Kumasi, Ghana
Patience Nyarkoa Ansong & Yaa Obirikorang
Department of Chemical Pathology, University of Ghana Medical School, University of Ghana, Accra, Ghana
Eric NY Nyarko
You can also search for this author in PubMed Google Scholar
Contributions
CO, LB, and AAA conceptualized, designed the study, and edited the manuscript. EAA, EOA and AOB analyzed, interpreted the data, and drafted the paper. ANB, GOS and PNA assisted in data acquisition and measurement. YO, IOB, ENYN and AGA contributed to writing and editing the manuscript. All authors have read and approved the final version before submission.
Corresponding author
Correspondence to Christian Obirikorang .
Ethics declarations
Ethical approval and consent to participate.
Ethical approval with reference ID (CHRPE/AP/030/19) was obtained from the Committee on Human Research, Publications and Ethics (CHRPE), School of Medicine and Dentistry, Kwame Nkrumah University of Science & Technology. Written informed consent was obtained from participants 18 years and above and assent from minors (< 18 years) who opted to participate in the study. Additionally, informed consent to participate was taken from the legal guardians of minor participants. All methods were performed following the guidelines and regulations of the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Obirikorang, C., Adu, E.A., Anto, E.O. et al. Prevalence and risk factors of obesity among undergraduate student population in Ghana: an evaluation study of body composition indices. BMC Public Health 24 , 877 (2024). https://doi.org/10.1186/s12889-023-17175-5
Download citation
Received : 26 June 2023
Accepted : 07 November 2023
Published : 21 March 2024
DOI : https://doi.org/10.1186/s12889-023-17175-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Body composition
- Undergraduate students
- Risk factors
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Free school meals for all may reduce childhood obesity, while easing financial and logistical burdens for families and schools
Ph.D. Candidate in Health Services, University of Washington
Associate Professor of Health Systems and Population Health, Epidemiology, University of Washington
Disclosure statement
Jessica Jones-Smith receives funding from the National Institutes of Health.
Anna Localio does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University of Washington provides funding as a member of The Conversation US.
View all partners
School meals are critical to child health. Research has shown that school meals can be more nutritious than meals from other sources, such as meals brought from home.
A recent study that one of us conducted found the quality of school meals has steadily improved, especially since the 2010 Healthy, Hunger-Free Kids Act strengthened nutrition standards for school meals. In fact, by 2017, another study found that school meals provided the best diet quality of any major U.S. food source.
Many American families became familiar with universal free school meals during the COVID-19 pandemic. To ease the financial and logistical burdens of the pandemic on families and schools, the U.S. Department of Agriculture issued waivers that allowed schools nationwide to provide free breakfast and lunch to all students. However, these waivers expired by the 2022-23 school year.
Since that time, there has been a substantial increase in schools participating in the Community Eligibility Provision , a federal policy that allows schools in high poverty areas to provide free breakfast and lunch to all attending students. The policy became available as an option for low-income schools nationwide in 2014 and was part of the Healthy, Hunger-Free Kids Act . By the 2022-23 school year, over 40,000 schools had adopted the Community Eligibility Provision, an increase of more than 20% over the prior year.
We are public health researchers who study the health effects of nutrition-related policies, particularly those that alleviate poverty. Our newly published research found that the Community Eligibility Provision was associated with a net reduction in the prevalence of childhood obesity .
Improving the health of American children
President Harry Truman established the National School Lunch Program in 1946, with the stated goal of protecting the health and well-being of American children. The program established permanent federal funding for school lunches, and participating schools were required to provide free or reduced-price lunches to children from qualifying households. Eligibility is determined by income based on federal poverty levels, both of which are revised annually .
In 1966, the Child Nutrition Act piloted the School Breakfast Program , which provides free, reduced-price and full-price breakfasts to students. This program was later made permanent through an amendment in 1975.
The Community Eligibility Provision was piloted in several states beginning in 2011 and became an option for eligible schools nationwide beginning in 2014. It operates through the national school lunch and school breakfast programs and expands on these programs.

The policy allows all students in a school to receive free breakfast and lunch, rather than determine eligibility by individual households. Entire schools or school districts are eligible for free lunches if at least 40% of their students are directly certified to receive free meals, meaning their household participated in a means-based safety net program, such as the Supplemental Nutrition Assistance Program , or the child is identified as runaway, homeless, in foster care or enrolled in Head Start. Some states also use Medicaid for direct certification .
The Community Eligibility Provision increases school meal participation by reducing the stigma associated with receiving free meals, eliminating the need to complete and process applications and extending access to students in households with incomes above the eligibility threshold for free meals. As of 2023, the eligibility threshold for free meals is 130% of the federal poverty level, which amounts to US$39,000 for a family of four.
Universal free meals and obesity
We analyzed whether providing universal free meals at school through the Community Eligibility Provision was associated with lower childhood obesity before the COVID-19 pandemic.
To do this, we measured changes in obesity prevalence from 2013 to 2019 among 3,531 low-income California schools. We used over 3.5 million body mass index measurements of students in fifth, seventh and ninth grade that were taken annually and aggregated at the school level. To ensure rigorous results, we accounted for differences between schools that adopted the policy and eligible schools that did not. We also followed the same schools over time, comparing obesity prevalence before and after the policy.

We found that schools participating in the Community Eligibility Provision had a 2.4% relative reduction in obesity prevalence compared with eligible schools that did not participate in the provision. Although our findings are modest, even small improvements in obesity levels are notable because effective strategies to reduce obesity at a population level remain elusive . Additionally, because obesity disproportionately affects racially and ethnically marginalized and low-income children, this policy could contribute to reducing health disparities.
The Community Eligibility Provision likely reduces obesity prevalence by substituting up to half of a child’s weekly diet with healthier options and simultaneously freeing up more disposable income for low-to-middle-income families. Families receiving free breakfast and lunch save approximately $4.70 per day per child, or $850 per year. For low-income families, particularly those with multiple school-age children, this could result in meaningful savings that families can use for other health-promoting goods or services.
Expanding access to school meals
Childhood obesity has been increasing over the past several decades. Obesity often continues into adulthood and is linked to a range of chronic health conditions and premature death .
Growing research is showing the benefits of universal free school meals for the health and well-being of children. Along with our study of California schools, other researchers have found an association between universal free school meals and reduced obesity in Chile , South Korea and England , as well as among New York City schools and school districts in New York state .
Studies have also linked the Community Eligibility Provision to improvements in academic performance and reductions in suspensions .
While our research observed a reduction in the prevalence of obesity among schools participating in the Community Eligibility Provision relative to schools that did not, obesity increased over time in both groups, with a greater increase among nonparticipating schools.
Universal free meals policies may slow the rise in childhood obesity rates, but they alone will not be sufficient to reverse these trends. Alongside universal free meals, identifying other population-level strategies to reduce obesity among children is necessary to address this public health issue.
As of 2023, several states have implemented their own universal free school meals policies. States such as California, Maine, Colorado, Minnesota and New Mexico have pledged to cover the difference between school meal expenditures and federal reimbursements. As more states adopt their own universal free meals policies, understanding their effects on child health and well-being, as well as barriers and supports to successfully implementing these programs, will be critical.
- Childhood obesity
- Child health
- School meals
- National School Lunch Program
- K-12 education
- Health disparities
- School lunches
- Federal role in K-12 education

Lecturer (Hindi-Urdu)

Initiative Tech Lead, Digital Products COE

Director, Defence and Security

Opportunities with the new CIEHF

School of Social Sciences – Public Policy and International Relations opportunities
This paper is in the following e-collection/theme issue:
Published on 2.4.2024 in Vol 26 (2024)
The Impact of Digital Self-Monitoring of Weight on Improving Diabetes Clinical Outcomes: Quasi-Randomized Study
Authors of this article:

Original Paper
- Yifat Fundoiano-Hershcovitz 1 , PhD ;
- Marilyn D Ritholz 2 , PhD ;
- David L Horwitz 3 , MD, PhD ;
- Ephraim Behar 1 , MSc ;
- Omar Manejwala 1 , MD ;
- Pavel Goldstein 4 , PhD
1 Dario Health, Caesarea, Israel
2 Joslin Diabetes Center, Harvard Medical School, Boston, MA, United States
3 DLH Biomedical Consulting, Las Vegas, NV, United States
4 School of Public Health, University of Haifa, Haifa, Israel
Corresponding Author:
Yifat Fundoiano-Hershcovitz, PhD
Dario Health
Caesarea, 3079821
Phone: 972 525296979
Email: [email protected]
Background: The management of type 2 diabetes (T2D) and obesity, particularly in the context of self-monitoring, remains a critical challenge in health care. As nearly 80% to 90% of patients with T2D have overweight or obesity, there is a compelling need for interventions that can effectively manage both conditions simultaneously. One of the goals in managing chronic conditions is to increase awareness and generate behavioral change to improve outcomes in diabetes and related comorbidities, such as overweight or obesity. There is a lack of real-life evidence to test the impact of self-monitoring of weight on glycemic outcomes and its underlying mechanisms.
Objective: This study aims to assess the efficacy of digital self-monitoring of weight on blood glucose (BG) levels during diabetes management, investigating whether the weight changes may drive glucose fluctuations.
Methods: In this retrospective, real-world quasi-randomized study, 50% of the individuals who regularly used the weight monitoring (WM) feature were propensity score matched with 50% of the users who did not use the weight monitoring feature (NWM) based on demographic and clinical characteristics. All the patients were diagnosed with T2D and tracked their BG levels. We analyzed monthly aggregated data 6 months before and after starting their weight monitoring. A piecewise mixed model was used for analyzing the time trajectories of BG and weight as well as exploring the disaggregation effect of between- and within-patient lagged effects of weight on BG.
Results: The WM group exhibited a significant reduction in BG levels post intervention ( P <.001), whereas the nonmonitoring group showed no significant changes ( P =.59), and both groups showed no differences in BG pattern before the intervention ( P =.59). Furthermore, the WM group achieved a meaningful decrease in BMI ( P <.001). Finally, both within-patient ( P <.001) and between-patient ( P =.008) weight variability was positively associated with BG levels. However, 1-month lagged back BMI was not associated with BG levels ( P =.36).
Conclusions: This study highlights the substantial benefits of self-monitoring of weight in managing BG levels in patients with diabetes, facilitated by a digital health platform, and advocates for the integration of digital self-monitoring tools in chronic disease management. We also provide initial evidence of testing the underlying mechanisms associated with BG management, underscoring the potential role of patient empowerment.
Introduction
People with type 2 diabetes (T2D) face challenging self-management regimens to improve glycemia and decrease morbidity and mortality while often dealing with high costs of care [ 1 ]. Obesity is one of the most common, serious, and costly medical condition in the United States, with a prevalence of 41.9% from 2017 to 2020 [ 2 ]. After a dramatic increase in its prevalence over several decades, obesity has become a major public health crisis in the United States [ 3 ]. Obesity has become one of the leading causes of death, as it is known to be the main risk factor for several noncommunicable diseases, particularly T2D [ 4 ]. It is crucial to take effective and decisive actions to hinder both the rise in the prevalence of obesity and the prevention and treatment of obesity and other obesity-related comorbidities. Approximately 80% to 90% of patients with T2D have overweight or obesity, which imposes a considerable burden on individuals, families, communities, and the health system [ 5 , 6 ].
Obesity and overweight are considered the primary accelerators for the T2D inflammatory component inducing progressive loss of beta cell insulin secretion with coexisting insulin resistance [ 7 - 9 ]. In addition, the expansion of white adipose tissue is related to a changed microenvironment in obesity, which impairs insulin signaling, reduces insulin-stimulated glucose transport activity, and accelerates beta cell dysfunction [ 10 ].
Previous studies have shown the beneficial effect of weight-lowering treatment on diabetes outcomes [ 11 ].
Healthful weight reduction in patients with obesity can improve glucose metabolism [ 12 ]. Weight reduction via carbohydrate-restricted nutritional intervention in patients with preobesity or obesity and prediabetes or T2D may contribute to improvement or remission in diabetes mellitus [ 13 ].
Antiobesity therapies for the treatment of patients with obesity and T2D include those that reduce body weight and improve glucose levels and other metabolic parameters. Considering the prevalence of obesity-related conditions such as adiposopathy and the fact that a significant portion of patients in cardiovascular outcomes trials for T2D had overweight or obesity, there is support for the “treat obesity first” therapeutic approach [ 13 ]. It is recommended in the guidelines for obesity that appropriate 5% to 10% weight loss can achieve significant metabolic improvement [ 14 ]. For the prevention of T2D, even modest weight reduction as little as 5%, can significantly reduce diabetes-associated complications [ 15 , 16 ]. Previous studies have shown that changes in various indexes such as blood lipid, blood glucose (BG), and insulin improved when weight loss reached 15% [ 14 ]. Furthermore, long-term tight weight control resulted in significant glycemic improvement, particularly demonstrated in the overweight population with T2D [ 17 , 18 ].
One of the goals of chronic condition management is to increase awareness and generate behavioral change to improve clinical outcomes. Behavior change for effective self-management was proven to improve health outcomes and quality of life in people living with chronic conditions such as obesity, T2D, and heart disease [ 19 ]. Underlying well-intentioned lifestyle messages is the assumption that if people deem health important, are aware of exercise and nutrition guidelines, and have access to healthy options to maintain proper levels of nutrition, diet, and exercise, then they will make healthier choices [ 20 ]. The American Diabetes Association guidelines state that lifestyle management should be intensive and involve frequent follow-ups [ 21 ].
Despite these recommendations, data from the National Health and Nutrition Examination Survey indicate that only 54.6% of patients reported receiving any diabetes education and only 13.4% had received an educational visit of any kind [ 16 ]. Earlier studies showed that helping participants with goal setting and self-monitoring of behavior, for instance, using a logbook and receiving feedback on the outcome of behavior, was associated with better intervention effects [ 22 ].
Facilitating behavior change involves using a series of strategies aimed at empowering patients, enabling them to take increasing control of their condition. This includes setting clear, achievable, and personalized goals, as well as enhancing self-efficacy [ 23 - 25 ]. The timing of health information and feedback focuses on when health behavior messages are delivered to people with diabetes. As diabetes care visits usually take place every 3 months, there can be a significant gap between these appointments and the daily engagement in desired behaviors. This gap makes it challenging to offer timely behavioral prompts or reinforcement [ 26 ].
In fact, patients’ mindset may modulate health outcomes, including glucose levels, in patients with diabetes [ 27 ]. Indeed, increasing perceived self-monitoring would be expected to result in subsequent health benefits [ 28 ], including glucose control in diabetes [ 29 ]. Individuals possess significant psychological influence over their health [ 30 ].
Currently, traditional health care models are being revamped with digital technologies. Digital platforms have the potential to improve our ability to enhance the delivery of health care for individual patients as well as empower patients to have more control over, and make better-informed decisions about, their health. Treatment optimization through digital health could enhance users’ alertness to their health condition through real-time monitoring, leading to effective treatments that build awareness of their daily health-related behaviors and promote increased engagement with those behaviors [ 31 - 34 ]. Technology-driven solutions can help people with diabetes build awareness of their daily health-related behaviors and promote increased engagement with those behaviors [ 32 - 34 ].
Communication of test results has been shown to be highly desired by people who have overweight, and lifestyle-focused educational messages providing advice, motivational reminders, and support have also been shown to be effective in improving chronic conditions [ 35 ]. Using a mobile platform for self-management purposes could facilitate individuals with chronic conditions in gaining insight into and controlling their BG and weight levels. Self-monitoring is a core component of behavioral obesity treatment; however, it is unknown how digital health has been used for self-monitoring and what engagement rates are achieved in these interventions [ 36 ].
Mobile apps have been shown to improve diabetes outcomes via education and support for adherence to evidence-based recommendations [ 37 - 40 ]. Mobile technology has emerged as a potentially useful platform to facilitate weight management [ 41 ]. Mobile apps for weight management typically offer similar features, including self-monitoring of diet and physical activity. Users can set goals within specified time frames and input data into the app, often receiving reminders or text messages. These apps have shown promising results [ 41 ]. Numerous digital health technologies have been developed to support the self-management of single chronic diseases, primarily diabetes. These technologies provide timely feedback, enhance patient education, and support the behavioral changes necessary for effective weight management. Recent research has indicated that digital self-monitoring tools can significantly influence health behaviors in patients with T2D, leading to better management of their condition [ 42 , 43 ]. However, given the rise in the number of people managing multiple chronic conditions, it is imperative to design and implement digital health technologies to deal with the additional complexities of multiple chronic conditions, such as the management of multiple symptoms and self-management tasks, avoiding further burden or inconvenience to the user [ 44 - 46 ]. Integrating the management of multiple conditions onto a single platform, where users can monitor their measurements and relevant lifestyle parameters, interact with all their data, share their data, and receive educational support, could help to minimize the known burden of multimorbidity self-management [ 47 - 49 ].
However, there is limited research on platforms that have been implemented to tackle multimorbidity or evaluated over longitudinal periods [ 45 ]. Specifically, the current literature is missing rigorous real-life studies to test the role of a simple self-monitoring of weight and diabetes management platform to better understand the direct association between weight monitoring and glycemic outcomes. Mainly, data are lacking on whether more frequent self-monitoring of those 2 conditions (weight and glycemia) has any impact on body weight and glycemic control in real-world clinical practice among patients with T2D and obesity [ 50 ]. In addition, many of these exclusively weight loss programs are time consuming and costly [ 51 ].
Our study seeks to address this gap by exploring the efficacy of digital self-monitoring of weight in managing BG levels in patients with T2D who are also managing their weight. We used a retrospective analysis of a home-use digital platform containing a diabetes BG meter and weight monitoring system with full longitudinal data capture using a supportive mobile platform among people with T2D and overweight levels. We followed users for 6 months before and 6 months after using the app for self-monitoring of weight and compared them with a matched control group that never used weight monitoring on the platform. We hypothesized that self-monitoring of weight would result in a significant improvement in BG levels. Moreover, weight monitoring (WM) will be associated with a reduction in weight levels. We also hypothesized a linkage between the changes in weight levels and the reduction in BG levels.
This study used the Dario Health digital therapeutics solution for chronic conditions to support the self-management of BG and weight levels. The platform combines an innovative meter with a phone app that is available for both Android and iOS devices. The glucose meter consists of a small pocket-sized holder for strips, a lancet, and the meter. The meter is removed from the holder and plugged directly into a cell phone, effectively converting the cell phone into the display screen for the meter. Weight level monitoring data are logged manually into the app on a special data entry screen ( Figure 1 ).
Connecting the BG meter directly to the phone and adding weight levels improves the quality of data collection. Additional information for weight measurement includes an informative color scale of weight ranges reflecting the Centers for Disease Control and Prevention definitions for BMI (kg/m 2 ) interpretation: <18.5 is underweight, 18.5 to 24.9 is healthy weight, 25.0 to 29.9 is overweight, and ≥30.0 is obese [ 52 ]. All information is stored in the users’ logbook in the app “attached” to the specific BG or weight reading. Data are uploaded to the cloud for backup and further analysis. Digital platform functions include interface design elements as well as specific educational content, wording, or digital interventions that affect the users’ choices in the digital environment; these functions provide personal health information and prompt feedback.

The monthly average weight level, which was defined as the means of all of a user’s weight measurements taken over a 30-day interval, was used as the core outcome metric. The monthly average BG level, which was defined as the meaning of all of a user’s BG measurements taken over a 30-day interval, was used as another outcome metric. The mobile platform collected the following medical and sociodemographic information (by self-report) for each user: sex, age, BMI during registration, physical activity level, stress level (0=no stress and 10=very stressed), alcohol consumption (number of drinks per week), smoking (0=never and 3=yes), and added comorbidities (such as high lipids, chronic kidney disease, cardiovascular disease, sleep disorder, cancer, or stress and depression). Socioeconomic status (median household income) was matched by applying zip code data to Census [ 53 ] and app engagement (number of app sessions per month). All data were transferred and stored in compliance with the Health Insurance Portability and Accountability Act requirements using Amazon Web Services database solutions. All data were anonymized before extraction for this study.
Study Population
A retrospective data study was performed on the Dario database on individuals who used the Dario platform between 2017 and 2023. The users purchased the device via a direct-to-consumer channel. The inclusion criteria were as follows: individuals who reported in the Dario app as diagnosed with T2D with a BG level of >140 mg/100 mL and BMI >25 kg/m 2 in their first month on the platform (baseline) and weight monitoring system (WM group) and used the weight monitoring system (WM monitoring). The resulting group of users was matched through the propensity scores procedure with users with similar clinical parameters but who have not been using the weight monitoring (non–weight monitoring; [NWM] group).
Study Design
The aim of our study design was to evaluate the impact of weight monitoring on BG levels. For the WM group, it was crucial to establish a clear start point for weight monitoring to assess its effects accurately. This start point is a defined intervention onset, marking when participants began actively monitoring their weight using the digital platform.
Conversely, for the NWM group, such a start point for “nonintervention” does not inherently exist, as these participants did not engage in weight monitoring. Hence, selecting a random start point for this group was a methodological necessity. This approach ensures that any observed differences in outcomes are attributable to the act of weight monitoring itself, rather than temporal factors or external influences. Therefore, the comparison between the groups hinges on the presence or absence of weight monitoring behavior. Using this approach, we enhanced the internal validity of the study. This allowed us to isolate the effect of weight monitoring from that of other variables and assess its impact on BG levels more accurately.
Propensity Scores: Causal Inference
Propensity score matching was used in this study to address potential confounding factors and enhance the comparability of the WM and NWM groups. The rationale behind using propensity score matching lies in its ability to reduce bias and mimic the randomization process, thereby facilitating causal inference in observational studies [ 54 ].
In originally nonrandomized studies, it is common for treatment assignment (in this case, use of the weight monitoring system) to be influenced by patient characteristics and other confounding variables. These factors may introduce bias and affect the estimation of treatment effects. Propensity score matching offers a systematic approach to account for such biases and create comparable treatment and control groups [ 55 ].
The propensity score, defined as the conditional probability of receiving the treatment given a set of observed covariates, summarizes the individual’s likelihood of being assigned to the WM group. By incorporating a comprehensive set of covariates that are potential confounders, such as age, sex, initial BG and BMI levels, smoking status, alcohol consumption, stress level, comorbidities, median household income, and platform engagement, the propensity score attempts to balance the distribution of these covariates between the WM and NWM groups.
Matching participants based on their propensity scores allows a comparison between similar individuals who only differ in terms of the treatment received. This strategy helps to reduce selection bias and confounding effects, enabling a more valid estimation of the causal effect of weight monitoring on glycemic control.
The use of propensity score matching aligns with the principle of exchangeability, as it creates groups that are comparable in terms of observed characteristics. By achieving a balance on observed covariates, the propensity score matching enhances the internal validity of the study and strengthens the plausibility of causal inference from the observed associations [ 56 ].
In this study, the propensity scores were calculated for each participant using the “matchit()” function from the R package matchit , which followed a nearest-neighbor approach, and the distance metric used was based on logistic regression using a 1:1 ratio between the 2 study groups [ 57 ].
To achieve balanced groups, nearest-neighbor matching with a caliper width of 0.1 SDs of the propensity score was applied. The matching procedure aimed to identify, for each WM user, a corresponding NWM participant with the closest propensity score. Participants without suitable matches were excluded from the analysis. Figure 2 presents the efficacy of the matching procedure for balancing the groups. A caliper width of 0.05 SDs was reached for all the parameters except alcohol consumption which remained within 0.1 SDs.

Ethical Considerations
All data used for the analysis were anonymized before extraction for this study. The study received an exemption from the institutional review board under the Ethical and Independent Review Services, a professional review board, which issued the institutional review board exemption for this study (18032-06#) [ 58 ]. The users who participated in the study were provided with a Terms of Use document mentioning the legally valid consent of the end user for the company to collect and access their information. The use of the app, site, or services shall be deemed to constitute user consent to be legally bound by these Terms and the Privacy Policy. Please refer to the current “Terms-of-use” at the link [ 59 ].
Analytic Approach
Traditionally, a classical linear longitudinal model assumes a single-slope growth pattern for changes in an outcome variable over time. However, empirical data often exhibit more complex patterns that cannot be adequately captured by such a simple model. In our study, we used piecewise-based mixed-effects models to allow for greater flexibility in modeling trajectories over time [ 60 ].
The piecewise model approach offers the advantage of accommodating different linear trends in the data across distinct regions. Specifically, we used a mixed piecewise model to assess differential changes in the WM and NWM groups in the monthly average BG level in 2 segments: before and after weight monitoring use. This approach enabled us to capture the potential changes in BG trajectories associated with the introduction of the monitoring system. Using a statistical model that accounted for curvilinear changes, we were able to test the complex effects and capture the dynamics of the associated BG fluctuations.
For the analysis, the time data were centered around the beginning of the weight monitoring period. We included a 6-month timeframe before and after this point to capture the potential impact of weight monitoring use. In the NWM group, we randomly selected a cutoff point and included data collected during the 6 months before and after the simulated cutoff point. To model the temporal changes in the monthly average weight level between the WM and NWM groups, we fitted a piecewise-based mixed-effects model. The piecewise cutoff point was set at the initiation of weight monitoring, assuming a change in the time-related trajectory of the monthly average BG level between the 2 groups. We incorporated interaction terms between the time trajectories and groups to capture this differential effect. Thus, 2 time parameters (pre and postintervention) were used as covariates, the groups (WM and NWM) were considered as a factor, and the monthly number of BG measurement served as a potential confounding variable. All the tests were 2-tailed and the type 1 error was set to 5%. The model included random intercepts and random slopes for the time trajectory after the piecewise cutoff, accounting for individual variability in BG changes.
In addition, we used mixed model analysis to examine the time trajectory of BMI changes (covariate) for the initial 6 months of weight monitoring in the WM group, controlling for baseline BMI and the number of monthly BMI measures as confounding variables. These models included random intercepts and random slopes of the time trajectory to capture individual variations in weight changes over time. Unstandardized regression weights (B), test statistics ( t ), and associated significance ( P values) were reported.
Finally, the monthly BMI levels were disaggregated to separate within- and between-person variabilities using person-level centering and person-level aggregation [ 61 ]. In addition, a 1-month lagged within-person BMI was calculated. Thereafter, a mixed model was applied to test the 1-month lagged and simultaneous association of monthly within-person BMI changes and between-person BMI with the monthly average BG level. All the model predictors were defined as covariates.
In total, 1932 users were included in the study. The WM group included 50% users, and the NWM group, matched through the propensity scores procedure, included 50% users. The study cohort comprised 51.6% (997/1932) of men, and 60.82% (1175/1932) of the participants had comorbidities. The average age of the participants was 62.8 (SD 12.5) years, with an average BMI of 35.4 (SD 7.3). The median household income for the participants was US $68,200 (SD US $25,100). The distribution of the other parameters is presented in Table 1 by study group.
No differences were found between the WM and NWM groups. The study included individuals with diabetes who monitored their BG levels and weight using the Dario platform.
The distribution of various sample characteristics overall and by WM and NWM groups is presented in Table 1 , and any significant differences were shown.
a WM: weight monitoring.
b NWM: non–weight monitoring.
c BG: blood glucose.
Weight Monitoring Is Associated With BG Levels
The results from the piecewise mixed model analysis indicated a significant interaction between the time trajectory, starting weight monitoring and the group (B=3.02; t =6.03; P <.001) on BG levels ( Table 2 ). Specifically, the WM group demonstrated a significant reduction in the BG levels (B=−2.81; t =−8.88; P <.001), whereas the NWM group did not exhibit a significant time trend (B=0.21; t =0.55; P =.59; Figure 3 ). Before weight monitoring, there was no significant difference observed in BG time trends between the 2 groups (B=0.69; t =1.06; P =.29). Furthermore, we investigated the proportion of users who achieved a BG level reduction in their last month of measurement less than the average BG levels of 154 mg/100 mL, 183 mg/100 mL, and 212 mg/100 mL, equivalent to estimated glycated hemoglobin (HbA 1c ) of 7.0, 8.0, and 9.0, respectively [ 62 ]. Remarkably, of the 966 users examined per group, 45% (435/966) versus 36% (348/966), 71% (686/966) versus 59% (570/966), and 85% (821/966) versus 76% (734/966) of the WM versus NWM individuals demonstrated substantial reductions in HbA 1c levels of <154 mg/100 mL, 183 mg/100 mL, and 212 mg/100 mL, respectively ( P <.001 for all).
a BG: blood glucose.
b σ2 residual variability=843.15; τ00 UID random intercept=2099.24; τ11 UID.time2 random slope of the second slope=53.68; ρ01 UID: covariance between the random intercept and slope=−0.27; intraclass correlation=0.72.
c #BG measurements=number of BG measurements per month.
d time1represents the piecewise slopes before the weight monitoring intervention.
e NWM: non–weight monitoring.
f time2 represents the piecewise slopes after the weight monitoring intervention.

BMI Fluctuations and the Link to BG
During the weight monitoring period ( Table 3 ) of the WM group, a significant decrease in BMI was observed (B=−0.13; t =−9.35; P <.001).
Interestingly, the number of monthly measurements was negatively associated with BMI (B=−0.003; t =−2.22; P =.03). Furthermore, the findings of the lagged analysis disaggregating within- and between-person variabilities shed light on BMI as a potential mechanism driving BG ( Table 4 ). Specifically, the analysis demonstrated that an increase in within-person BMI was associated with elevated BG levels (B=4.67; t =3.47; P <.001). Similarly, an increase in between-person BMI was found to be associated with higher BG levels (B=0.61; t =2.65; P =.008). However, the 1-month lagged back BMI was not associated with BG levels (B=−0.77; t =−0.91; P =.36).
b σ2 residual variability=0.24; τ00 UID random intercept=1.29; τ11 UID.time random slope of the time=0.17; ρ01 UID covariance between the random intercept and slope=−0.25; intraclass correlation=0.93.
c time represents the slope over 6 months after the intervention.
b WM: weight monitoring.
c σ2 residual variability=464.96; τ00 UID random intercept=1684.51; τ11 UID.time random slope of the within-person BMI=325.17; ρ01 UID covariance between the random intercept and slope=−0.01; intraclass correlation=0.80.
Principal Findings
This study examined the ability of people with diabetes to regulate BG levels through simple weight monitoring. It used propensity score matching for the control group and used a piecewise mixed model as a statistical framework to describe the nonlinear behavior in BG levels, comparing 2 user cohorts over time. Our analysis indicated that before the weight monitoring phase, both groups demonstrated flat trajectories in BG levels. However, after starting the use of the self-monitoring of weight, the WM group experienced a significant reduction in BG levels, whereas the NWM group’s BG levels remained flat.
In addition, by disaggregating within- and between-person BMI variabilities, we showed an association between both BMI sources and BG levels, suggesting that general BMI levels and BMI fluctuations can potentially contribute to BG modulation. However, a lagged analysis did not find an association between within-person BMI fluctuations and next-month BG levels, which does not support the claim of BMI as a potential mechanism of BG changes.
This study demonstrates that the use of digital tools for self-monitoring of weight can significantly affect BG levels in patients with T2D. This finding offers a practical approach to enhancing T2D management, especially for the majority of patients who are also dealing with overweight or obesity issues. Given that weight loss has been consistently shown to improve glycemic control in patients with T2D, as highlighted in previous studies [ 12 - 16 , 25 ], our findings reinforce the importance of weight management as an integral part of diabetes care. Self-monitoring can enhance patient awareness and engagement in their health management, leading to better outcomes. This aligns with the growing body of evidence suggesting that patient engagement and empowerment are critical in managing chronic conditions such as T2D [ 34 , 40 , 63 , 64 ].
Self-monitoring is the centerpiece of behavioral weight loss intervention programs. A significant association between self-monitoring and weight loss was consistently reported for various health conditions; however, the level of evidence was weak due to methodological limitations [ 65 ]. The use of self-monitoring in behavioral changes has a strong theoretical foundation. Self-management was defined as “the personal application of behavior-change tactics that produces a desired change in behavior” [ 66 ]. Through self-management interventions, individuals learn to identify occurrences of their own target responding, accurately self-recording the target response, self-evaluating their behavior, and self-delivering reinforcement as a consequence [ 67 ].
Although self-monitoring has been described as the cornerstone of behavioral treatment for weight loss, there is a limited examination conducted in the literature [ 65 ]. More recently, self-weighing has been introduced as a monitoring component. Daily weighing is valuable for individuals trying to lose weight or prevent weight gain [ 68 ]. Consistent with our findings, frequent self-weighing was associated with a lower fat intake, a greater history of dieting to lose weight, and a lower current BMI [ 68 , 69 ].
Previous systematic reviews provided extensive evidence that self-monitoring via digital health, including weight, diet, and physical activity, is associated with superior weight loss [ 36 ]. It was specifically shown how distinct features of a digital therapeutic app have the potential to deliver equitable person-centric care and how digital engagement can play a key role in enhancing a person’s chronic condition self-management [ 63 , 64 , 70 , 71 ].
Self-monitoring has been shown repeatedly to be an important feature of behavioral weight loss digital programs [ 71 ]. Self-monitoring of weight and diet were positively correlated with weight loss, and the more consistently the monitoring occurred, the better the weight loss [ 72 , 73 ]. Self-monitoring is also a core component of behavioral obesity treatment, but there is limited knowledge about the efficacy of digital self-monitoring of weight in diabetes [ 36 ]. We had previously demonstrated how digital engagement and digital blood pressure monitoring may improve diabetes management [ 34 , 74 ]. Prominently, in this study, the WM and NWM groups were not different in their digital engagement. In addition, the median household income distribution of users in both groups was comparable, suggesting that the digital solution is desired and affordable across lower-, middle-, and high-income levels to enhance glycemic and weight loss outcomes. Mobile apps can successfully help patients lose weight and represent a cost-effective and accessible alternative to intensive in-person weight loss programs [ 51 ].
From a psychological perspective, it is assumed that individuals using a digital platform may develop more active roles in managing their health, and self-monitoring affects health in part or in whole via the placebo effect, initiated by mindset modulations [ 75 ]. In the realm of physical exercise, a compelling body of research highlights the remarkable impact of mindset on various health parameters. It has been demonstrated that individuals’ mindsets about stress could profoundly alter their cortisol levels and influence various hormonal and cardiovascular functions when confronted with stressful situations [ 76 ]. Levy et al [ 77 ] conducted a noteworthy study that revealed a significant association between individuals’ mindsets about aging and their cardiovascular function as well as their actual longevity. A notable example of this phenomenon is evident in the study conducted by Crum and Langer [ 28 ], who investigated the effects of mindset on hotel room attendants. These workers, upon adopting the mindset that their daily work constituted a form of beneficial exercise, experienced substantial improvements in several critical health indicators, including weight, BMI, and systolic blood pressure. The potential mechanism may include beliefs and feelings of control people have over their health [ 28 , 78 ]. Collectively, these studies illuminate the potent role of the mindset in shaping various aspects of physical health, providing a background for the potential effect of weight monitoring on BG levels through mindset changes, considering the absence of a quasi-causal association between BMI and BG levels. There is evidence supporting the idea that the placebo effect plays a role in prompting the psychological benefits associated with health-related outcomes [ 79 ]. Treatments are delivered in a context that includes social and physical signals, verbal suggestions, and clinical history. This context is actively interpreted by the brain and can elicit expectations, memories, and emotions, which in turn can influence health-related outcomes in the body [ 79 ]. Considering the absence of a quasi-causal association between BMI and BG levels, one may consider the effect of self-weighing on BG levels to be mediated by perceptional processes, including mindset modulation.
In agreement with previous studies, we found that the WM group, which monitored their weight, also improved their BMI levels over time [ 80 ]. There is strong and consistent evidence that obesity management can delay the progression from prediabetes to T2D and is highly beneficial in treating T2D [ 80 - 83 ]. A significant overlap between T2D and overweight or obesity in etiology and disease mechanisms was broadly investigated. Previous studies have shown a significant improvement in all diabetes-related outcomes, including weight reduction, in patients with T2D and those who have overweight [ 17 ]. Controlling both diseases through weight management requires an intensive multidisciplinary approach [ 84 , 85 ]. As body weight increases, patients become more insulin resistant [ 86 ], which further drives the need for higher doses of antihyperglycemic medications to keep BG levels in the target range, which then may increase weight gain [ 17 ]. It was observed that in obese individuals, adipose tissue releases increased amounts of nonesterified fatty acids, glycerol, hormones, proinflammatory cytokines, and other factors that are involved in the development of insulin resistance. Insulin resistance associated with dysfunction of pancreatic islet beta cells results in the failure to maintain BG levels within the target range [ 86 ]. Losing weight can alleviate many of these issues. While losing weight, the pancreas is better able to keep up with the body’s need for insulin. In some cases, weight loss is enough to restore BG to a normal level, which eliminates diabetes or even lowers the need for insulin therapy or other medications to control diabetes [ 87 ]. However, other important components may also play a role in weight and BG levels, and other laboratory tests may need to be performed by health care providers.
Monitoring several chronic conditions may have the potential to offer a greater means for helping people with diabetes who have overweight or obesity effectively modulate their glycemia and weight than managing each condition separately. The findings of this study suggest the need for further exploration of how digital health platforms can be effectively integrated into routine clinical practice. Future research should focus on how these tools can be optimized for individual patient needs and how they can be incorporated into broader diabetes management programs. In addition, exploring the long-term impacts of such interventions on patient outcomes and health care use will be valuable. We expect that our analytical framework will be useful for examining other chronic conditions and metabolic syndrome outcomes (eg, lipid profile).
Limitations
As in all studies involving retrospective real-world data, groups were not randomly assigned, and treatment protocols were not prescribed. The propensity score matching approach, while comprehensive, introduces potential biases due to selection methods, which may not be fully mitigated. Unobserved confounders, measurement errors, and other limitations inherent to observational studies may still impact the validity of causal inferences. Nevertheless, propensity score matching represents a rigorous analytical technique that is widely accepted and applied in observational studies to approximate the design and control of randomized controlled trials, making it a valuable tool in the pursuit of causal inference. In this study, we relied on self-reported data for measurements, including weight and BMI. Although self-reporting is a common and practical method in many observational and digital health studies, it can be subject to inaccuracies due to factors such as recall bias or the desire to present oneself in a certain light.
In this real-world data analysis, we designed our timescale to capture changes over a 6-month period both before and after the initiation of weight monitoring. Nevertheless, it is worth noting that the research question of interest in this study could potentially be explored at various temporal scales, including daily, weekly, or monthly intervals. Given the practical challenges associated with monitoring daily changes in real-world settings, most studies in this domain tend to emphasize monthly fluctuations. Moreover, while BG levels offer real-time data and are sensitive to immediate changes in diabetes management, they do not provide a comprehensive view of long-term glycemic control. In addition, longer-term weight monitoring can provide a long-term perspective on glycemic control. Monitoring HbA 1c levels over a longer period would provide additional insights into the long-term effects of self-monitoring of weight on glycemic control. However, our study was designed to assess the short-term impacts of digital self-monitoring of weight on BG levels with increased resolution compared to HbA 1c . The 6-month period was chosen as it provides a sufficient window to observe significant changes in BG levels in response to weight management, without extending to long-term effects where other variables might confound the results. In addition, the average BMI of the participants was 35.0 (SD 7.3), which is considered a unique population of obesity. Furthermore, longer-term follow-up with these participants is needed because it is not clear how long this weight loss and glycemic improvement will last and what needs to be added for increased sustainability.
Conclusions
In summary, our study underscored the tangible benefits of self-monitoring of weight in the modulation of BG levels among people with diabetes. By leveraging an innovative analytical framework, we found that self-monitoring of weight led to significant reductions in BG levels in the WM group, despite the lack of a direct causal link between BMI fluctuations and BG changes. Drawing from extensive evidence, both historical and from our study, the act of self-monitoring seems to foster a heightened sense of agency and potentially influence health outcomes through mindset modulations.
From a practical standpoint, these findings reinforce the importance of digital health tools in chronic disease management, especially in the realms of diabetes and obesity. Digital self-monitoring platforms not only offer scalable and affordable solutions but also empower individuals to take a proactive role in their health journey. Moreover, the convergence of digital health tools with robust psychological mechanisms, such as the placebo effect and mindset modulation, paves the way for a holistic approach to health care.
This research may also open the door to a myriad of possibilities. While we have illuminated the potential effects of self-monitoring of weight on diabetes management, similar methods could be deployed to investigate the impact on other chronic conditions and metabolic syndrome outcomes. Furthermore, with advancing technology, more granular, real-time data can be leveraged to delve deeper into the daily or even hourly impacts of such interventions. Future studies should also focus on investigating the mechanisms underlying the comorbidity of diabetes and obesity and their management, identifying, and applying mediation models that drive behavioral change that goes beyond multiple chronic conditions.
In light of the significant overlap between T2D and obesity, there is an imperative need to conceptualize and design multifaceted interventions. Blending digital innovation, behavioral science, and clinical knowledge, we can usher in a new era of person-centric health care that is not only responsive but also preemptive. The journey has just begun, and the road ahead promises transformative potential for patients and health care systems alike.
Conflicts of Interest
YFH, EB, and OM are employees of Dario Health. MDR and DLH serve as Dario Health scientific advisory board members, and PG has received a consulting fee to assist with analyses but otherwise has no conflicts of interest.
- Amante DJ, Harlan DM, Lemon SC, McManus DD, Olaitan OO, Pagoto SL, et al. Evaluation of a diabetes remote monitoring program facilitated by connected glucose meters for patients with poorly controlled type 2 diabetes: randomized crossover trial. JMIR Diabetes. Mar 11, 2021;6(1):e25574. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bryan S, Afful J, Carroll M, Te-Ching C, Orlando D, Fink S, et al. National health and nutrition examination survey 2017–March 2020 prepandemic data files—development of files and prevalence estimates for selected health outcomes. Centers for Disease Control and Prevention. 2021. URL: https://www.cdc.gov/nchs/data/nhsr/nhsr158-508.pdf [accessed 2024-03-16]
- Cawley J, Biener A, Meyerhoefer C, Ding Y, Zvenyach T, Smolarz BG, et al. Direct medical costs of obesity in the United States and the most populous states. J Manag Care Spec Pharm. Mar 2021;27(3):354-366. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leitner DR, Frühbeck G, Yumuk V, Schindler K, Micic D, Woodward E, et al. Obesity and type 2 diabetes: two diseases with a need for combined treatment strategies - EASO can lead the way. Obes Facts. 2017;10(5):483-492. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nianogo RA, Arah OA. Forecasting obesity and type 2 diabetes incidence and burden: the ViLA-obesity simulation model. Front Public Health. 2022;10:818816. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ruze R, Liu T, Zou X, Song J, Chen Y, Xu R, et al. Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Front Endocrinol (Lausanne). 2023;14:1161521. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol. Jul 2020;16(7):349-362. [ CrossRef ] [ Medline ]
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. Jan 2019;42(Suppl 1):S13-S28. [ CrossRef ] [ Medline ]
- Versini M, Jeandel PY, Rosenthal E, Shoenfeld Y. Obesity in autoimmune diseases: not a passive bystander. Autoimmun Rev. Sep 2014;13(9):981-1000. [ CrossRef ] [ Medline ]
- Tuomi T, Santoro N, Caprio S, Cai M, Weng J, Groop L. The many faces of diabetes: a disease with increasing heterogeneity. Lancet. Mar 22, 2014;383(9922):1084-1094. [ CrossRef ] [ Medline ]
- Thom G, Messow CM, Leslie WS, Barnes AC, Brosnahan N, McCombie L, et al. Predictors of type 2 diabetes remission in the Diabetes Remission Clinical Trial (DiRECT). Diabet Med. Aug 2021;38(8):e14395. [ CrossRef ] [ Medline ]
- Bays HE. Why does type 2 diabetes mellitus impair weight reduction in patients with obesity? A review. Obes Pillars. Sep 2023;7:100076. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bays HE, Bindlish S, Clayton TL. Obesity, diabetes mellitus, and cardiometabolic risk: an obesity medicine association (OMA) clinical practice statement (CPS) 2023. Obes Pillars. Mar 2023;5:100056. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kong DX, Xiao Y, Zhang ZX, Liu YB. Study on the correlation between metabolism, insulin sensitivity and progressive weight loss change in type-2 diabetes. Pak J Med Sci. 2020;36(7):1523-1528. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Scheen AJ, Van Gaal LF. Combating the dual burden: therapeutic targeting of common pathways in obesity and type 2 diabetes. Lancet Diabetes Endocrinol. Nov 2014;2(11):911-922. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Apovian CM, Okemah J, O'Neil PM. Body weight considerations in the management of type 2 diabetes. Adv Ther. Jan 2019;36(1):44-58. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hamdy O, Ashrafzadeh S, Mottalib A. Weight management in patients with type 2 diabetes: a multidisciplinary real-world approach. Curr Diab Rep. Jul 17, 2018;18(9):66. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bolignano D, Zoccali C. Effects of weight loss on renal function in obese CKD patients: a systematic review. Nephrol Dial Transplant. Nov 2013;28 Suppl 4:iv82-iv98. [ CrossRef ] [ Medline ]
- Araújo-Soares V, Hankonen N, Presseau J, Rodrigues A, Sniehotta FF. Developing behavior change interventions for self-management in chronic illness: an integrative overview. Eur Psychol. 2019;24(1):7-25. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. Aug 2014;104(8):e25-e31. [ CrossRef ] [ Medline ]
- Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. Dec 2018;41(12):2669-2701. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act. Mar 28, 2017;14(1):42. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Magkos F, Yannakoulia M, Chan JL, Mantzoros CS. Management of the metabolic syndrome and type 2 diabetes through lifestyle modification. Annu Rev Nutr. 2009;29:223-256. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Estabrooks PA, Nelson CC, Xu S, King D, Bayliss EA, Gaglio B, et al. The frequency and behavioral outcomes of goal choices in the self-management of diabetes. Diabetes Educ. 2005;31(3):391-400. [ CrossRef ] [ Medline ]
- Reynolds LR, Anderson JW. Practical office strategies for weight management of the obese diabetic individual. Endocr Pract. 2004;10(2):153-159. [ CrossRef ] [ Medline ]
- Hood KK, Hilliard M, Piatt G, Ievers-Landis CE. Effective strategies for encouraging behavior change in people with diabetes. Diabetes Manag (Lond). 2015;5(6):499-510. [ FREE Full text ] [ Medline ]
- Raffali A, Asraf RM. Fostering growth mindset principles in the prevention of type 2 diabetes through a narrative game. Int J Learn Teach Educ Res. 2023;22(2):244-261. [ FREE Full text ] [ CrossRef ]
- Crum AJ, Langer EJ. Mind-set matters: exercise and the placebo effect. Psychol Sci. Feb 2007;18(2):165-171. [ CrossRef ] [ Medline ]
- Park C, Pagnini F, Reece A, Phillips D, Langer E. Blood sugar level follows perceived time rather than actual time in people with type 2 diabetes. Proc Natl Acad Sci U S A. Jul 19, 2016;113(29):8168-8170. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee KS, Feltner FJ, Bailey AL, Lennie TA, Chung ML, Smalls BL, et al. The relationship between psychological states and health perception in individuals at risk for cardiovascular disease. Psychol Res Behav Manag. 2019;12:317-324. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Awad A, Trenfield SJ, Pollard TD, Ong JJ, Elbadawi M, McCoubrey LE, et al. Connected healthcare: improving patient care using digital health technologies. Adv Drug Deliv Rev. Nov 2021;178:113958. [ CrossRef ] [ Medline ]
- Cahn A, Akirov A, Raz I. Digital health technology and diabetes management. J Diabetes. Jan 2018;10(1):10-17. [ CrossRef ] [ Medline ]
- Han J, King F, Klonoff D, Drincic A, Crosby KP, Robinson T, et al. Digital diabetes congress 2019. J Diabetes Sci Technol. Sep 2019;13(5):979-989. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fundoiano-Hershcovitz Y, Hirsch A, Dar S, Feniger E, Goldstein P. Role of digital engagement in diabetes care beyond measurement: retrospective cohort study. JMIR Diabetes. Feb 18, 2021;6(1):e24030. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chow CK, Redfern J, Hillis GS, Thakkar J, Santo K, Hackett ML, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255-1263. [ CrossRef ] [ Medline ]
- Patel ML, Wakayama LN, Bennett GG. Self-monitoring via digital health in weight loss interventions: a systematic review among adults with overweight or obesity. Obesity (Silver Spring). Mar 2021;29(3):478-499. [ CrossRef ] [ Medline ]
- Michie S, Yardley L, West R, Patrick K, Greaves F. Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. J Med Internet Res. Jun 29, 2017;19(6):e232. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Offringa R, Sheng T, Parks L, Clements M, Kerr D, Greenfield MS. Digital diabetes management application improves glycemic outcomes in people with type 1 and type 2 diabetes. J Diabetes Sci Technol. May 25, 2018;12(3):701-708. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bollyky JB, Melton ST, Xu T, Painter SL, Knox B. The effect of a cellular-enabled glucose meter on glucose control for patients with diabetes: prospective pre-post study. JMIR Diabetes. Oct 07, 2019;4(4):e14799. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Osborn CY, van Ginkel JR, Rodbard D, Heyman M, Marrero DG, Huddleston B, et al. One drop | mobile: an evaluation of hemoglobin A1c improvement linked to app engagement. JMIR Diabetes. Aug 24, 2017;2(2):e21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ghelani DP, Moran LJ, Johnson C, Mousa A, Naderpoor N. Mobile apps for weight management: a review of the latest evidence to inform practice. Front Endocrinol (Lausanne). 2020;11:412. [ FREE Full text ] [ CrossRef ] [ Medline ]
- MacPherson MM, Merry KJ, Locke SR, Jung ME. mHealth prompts within diabetes prevention programs: a scoping review. Mhealth. 2022;8:20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- MacPherson MM, Merry KJ, Locke SR, Jung ME. Effects of mobile health prompts on self-monitoring and exercise behaviors following a diabetes prevention program: secondary analysis from a randomized controlled trial. JMIR Mhealth Uhealth. Sep 05, 2019;7(9):e12956. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. Feb 14, 2013;15(2):e35. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Doyle J, Murphy E, Gavin S, Pascale A, Deparis S, Tommasi P, et al. A digital platform to support self-management of multiple chronic conditions (ProACT): findings in relation to engagement during a one-year proof-of-concept trial. J Med Internet Res. Dec 15, 2021;23(12):e22672. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ancker JS, Witteman HO, Hafeez B, Provencher T, Van de Graaf M, Wei E. "You get reminded you're a sick person": personal data tracking and patients with multiple chronic conditions. J Med Internet Res. Aug 19, 2015;17(8):e202. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Doyle J, Murphy E, Kuiper J, Smith S, Hannigan C, Jacobs A, et al. Managing multimorbidity: identifying design requirements for a digital self-management tool to support older adults with multiple chronic conditions. In: Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 2019. Presented at: CHI '19; May 4-9, 2019;1-14; Glasgow, Scotland. URL: https://dl.acm.org/doi/10.1145/3290605.3300629
- Lim CY, Berry AB, Hartzler A, Hirsch T, Carrell DS, Bermet ZA, et al. Facilitating self-reflection about values and self-care among individuals with chronic conditions. In: Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 2019. Presented at: CHI '19; May 4-9, 2019;1-12; Glasgow, Scotland. URL: https://dl.acm.org/doi/10.1145/3290605.3300885 [ CrossRef ]
- Caldeira C, Gui X, Reynolds TL, Bietz M, Chen Y. Managing healthcare conflicts when living with multiple chronic conditions. Int J Hum Comput Stud. Jan 2021;145:102494. [ FREE Full text ] [ CrossRef ]
- Tomah S, Mahmoud N, Mottalib A, Pober DM, Tasabehji MW, Ashrafzadeh S, et al. Frequency of self-monitoring of blood glucose in relation to weight loss and A1C during intensive multidisciplinary weight management in patients with type 2 diabetes and obesity. BMJ Open Diabetes Res Care. 2019;7(1):e000659. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ufholz K, Werner J. The efficacy of mobile applications for weight loss. Curr Cardiovasc Risk Rep. Mar 23, 2023;17(4):83-90. [ FREE Full text ] [ CrossRef ] [ Medline ]
- About adult BMI. Centers for Disease Control and Prevention. URL: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html [accessed 2022-05-03]
- Measuring America's people, places, and economy. The United States Census Bureau. URL: https://www.census.gov/ [accessed 2024-03-16]
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. May 2011;46(3):399-424. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. Mar 12, 2012;39(1):33-38. [ CrossRef ]
- Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. Feb 01, 2010;25(1):1-21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ho D, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1-28. [ CrossRef ]
- Home page. Ethical & Independent Review Services (E&I). URL: https://eandireview.com/ [accessed 2023-06-13]
- Terms of use. DarioHealth Corp. URL: https://www.dariohealth.com/terms-of-use/ [accessed 2024-03-16]
- Kohli N, Peralta Y, Zopluoglu C, Davison ML. A note on estimating single-class piecewise mixed-effects models with unknown change points. Int J Behav Dev. Feb 15, 2018;42(5):518-524. [ CrossRef ]
- Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. Jan 30, 2015;17(1):e30. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ, et al. A1c-Derived Average Glucose Study Group. Translating the A1C assay into estimated average glucose values. Diabetes Care. Aug 2008;31(8):1473-1478. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open-label, cluster-randomized pilot clinical trial. J Med Internet Res. Jul 11, 2017;19(7):e246. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shan R, Sarkar S, Martin SS. Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetologia. Jun 8, 2019;62(6):877-887. [ CrossRef ] [ Medline ]
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. Jan 2011;111(1):92-102. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cooper JO, Heron TE, Heward WL. Applied Behavior Analysis. 3rd edition. Old Bridge, NJ. Pearson Prentice Hall; 2020.
- Erhard P, Wong T, Barnett M, Falcomata T, Lang R. Self-management skills and applied behavior analysis. In: Matson JL, Sturmey P, editors. Handbook of Autism and Pervasive Developmental Disorder: Assessment, Diagnosis, and Treatment. Cham, Switzerland. Springer; 2022;957-973.
- Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. Dec 2005;30(3):210-216. [ CrossRef ] [ Medline ]
- Patel ML, Hopkins CM, Brooks TL, Bennett GG. Comparing self-monitoring strategies for weight loss in a smartphone app: randomized controlled trial. JMIR Mhealth Uhealth. Feb 28, 2019;7(2):e12209. [ FREE Full text ] [ CrossRef ] [ Medline ]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 1. improving care and promoting health in populations: standards of care in diabetes-2023. Diabetes Care. Jan 01, 2023;46(Supple 1):S10-S18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lin PH, Grambow S, Intille S, Gallis JA, Lazenka T, Bosworth H, et al. The association between engagement and weight loss through personal coaching and cell phone interventions in young adults: randomized controlled trial. JMIR Mhealth Uhealth. Oct 18, 2018;6(10):e10471. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Burke LE, Warziski M, Starrett T, Choo J, Music E, Sereika S, et al. Self-monitoring dietary intake: current and future practices. J Ren Nutr. Jul 2005;15(3):281-290. [ CrossRef ] [ Medline ]
- Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behav Ther. Jun 1993;24(3):377-394. [ CrossRef ]
- Gershoni T, Ritholz MD, Horwitz D, Manejwala O, Donaldson-Pitter T, Fundoiano-Hershcovitz Y. Glycemic management by a digital therapeutic platform across racial/ethnic groups: a retrospective cohort study. Applied Sciences. Dec 29, 2022;13(1):431. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tighe SA, Ball K, Kensing F, Kayser L, Rawstorn JC, Maddison R. Toward a digital platform for the self-management of noncommunicable disease: systematic review of platform-like interventions. J Med Internet Res. Oct 28, 2020;22(10):e16774. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Crum AJ, Salovey P, Achor S. Rethinking stress: the role of mindsets in determining the stress response. J Pers Soc Psychol. Apr 2013;104(4):716-733. [ CrossRef ] [ Medline ]
- Levy BR, Slade MD, Kunkel SR, Kasl SV. Longevity increased by positive self-perceptions of aging. J Pers Soc Psychol. Aug 2002;83(2):261-270. [ CrossRef ] [ Medline ]
- Salvia MG, Ritholz MD, Craigen KL, Quatromoni PA. Women's perceptions of weight stigma and experiences of weight-neutral treatment for binge eating disorder: a qualitative study. EClinicalMedicine. Feb 2023;56:101811. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wager TD, Atlas LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci. Jul 2015;16(7):403-418. [ FREE Full text ] [ CrossRef ] [ Medline ]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. on behalf of the American Diabetes Association. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes-2023. Diabetes Care. Jan 01, 2023;46(Suppl 1):S128-S139. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rothberg AE, McEwen LN, Kraftson AT, Fowler CE, Herman WH. Very-low-energy diet for type 2 diabetes: an underutilized therapy? J Diabetes Complications. 2014;28(4):506-510. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garvey WT, Ryan DH, Bohannon NJ, Kushner RF, Rueger M, Dvorak RV, et al. Weight-loss therapy in type 2 diabetes: effects of phentermine and topiramate extended release. Diabetes Care. Dec 2014;37(12):3309-3316. [ CrossRef ] [ Medline ]
- Davies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjøth TV, et al. NN8022-1922 Study Group. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. Aug 18, 2015;314(7):687-699. [ CrossRef ] [ Medline ]
- Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the comprehensive type 2 diabetes management algorithm - 2018 executive summary. Endocr Pract. Jan 2018;24(1):91-120. [ CrossRef ] [ Medline ]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. on behalf of the American Diabetes Association. 5. Facilitating positive health behaviors and well-being to improve health outcomes: standards of care in diabetes-2023. Diabetes Care. Jan 01, 2023;46(Supple 1):S68-S96. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. Dec 14, 2006;444(7121):840-846. [ CrossRef ] [ Medline ]
- Bishop S. Losing weight can have big impact on those with diabetes. Mayo Clinic News Network. URL: https://newsnetwork.mayoclinic.org/discussion/losing-weight-can-have-big-impact-on-those-with-diabetes/ [accessed 2023-08-06]
Abbreviations
Edited by G Eysenbach, T Leung; submitted 28.11.23; peer-reviewed by Y Ding, T de Azevedo Cardoso; comments to author 02.01.24; revised version received 18.02.24; accepted 22.02.24; published 02.04.24.
©Yifat Fundoiano-Hershcovitz, Marilyn D Ritholz, David L Horwitz, Ephraim Behar, Omar Manejwala, Pavel Goldstein. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 02.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

More Than One Billion People Around the Globe are Facing Obesity
March 26, 2024 · Baton Rouge, LA
Pennington Biomedical’s Dr. Peter Katzmarzyk was among hundreds of researchers who tracked BMI measurements gathered from more than 3,600 population-based studies since 1990
Obesity is now the most common form of malnutrition in most countries, with the rates rising in all categories of men, women, children and adolescents since 1990. Obesity rates in adult men have nearly tripled since 1990, with obesity rates in woman doubling in that time. The rates of obesity in children and adolescents quadrupled in that time frame, as well. As of 2022, nearly 880 million adults and nearly 160 million children were living with obesity.
The prevalence of malnutrition across the globe was shared by the NCD Risk Factor Collaboration, a network of health scientists from around the world who provide and evaluate data on major risk factors for all countries, in collaboration with the World Health Organization. Dr. Peter Katzmarzyk, Associate Executive Director of the Population and Public Health Sciences department of Pennington Biomedical Research Center in Baton Rouge, was an author contributor to this publication.
The network participants reviewed body mass index data from more than 3,600 studies from 1990 to 2022, determining the rates of malnutrition, either from obesity or underweight, for all countries, and the degree to which the data has changed through the years.
“The current rates of obesity appear overwhelming, but the trend has been moving in this direction for more than three decades,” said Dr. Katzmarzyk. “With more than 1 billion people living with obesity, it is important that we do not talk about obesity in a vacuum. We know that obesity can directly lead to comorbidities, including high blood pressure, heart disease, diabetes, cancer, and obstructive sleep apnea. By better understanding the root causes of obesity, we can identify ways to prevent, treat or even reverse its adverse effects.”
Out of the 190-plus countries represented in this study , the United States ranked 10th highest in the world for the prevalence of obesity in men, with an increase in percentage of men from 16.9 percent in 1990 to 41.6 percent in 2022. For women, the obesity rate in 1990 was 21.2 percent, climbing to 43.8 percent in 2022, with ranking 36th highest in the world. For boys, the rate of obesity increased from 11.5 percent in 1990 to 21.7 percent in 2022, ranking the U.S. 26th highest in the world. The rate of obesity for girls in the U.S. ranked 22nd highest in the world, with the rate climbing from 11.6 percent in 1990 to 19.4 percent in 2022.
The results echo the prevalence of obesity on granular levels, as in 2020, 38 percent of adults in Louisiana are facing obesity, according to County Health Rankings and Roadmaps.
“The results of this study resoundingly affirm the value of Pennington Biomedical’s mission,” said Dr. John Kirwan, Executive Director of Pennington Biomedical. “With the prevalence of obesity growing through the decades, we remain steadfast in our commitment to promote metabolic health, eliminate metabolic disease, discover the triggers of obesity and improve the health of all people. I extend my appreciation and applaud the contribution that Dr. Katzmarzyk made to this important global study.”
Over the same period, the rates of children, adolescents and adults being underweight fell on a global scale, with the rate of underweight of men in some African countries falling steeply. Both obesity and underweight are forms of malnutrition, with obesity rates higher than the rates of underweight for boys and girls in two thirds of the world’s countries.
For more information contact:
Joe Coussan, Media Relations Manager, [email protected] , 225-763-3049 or Ernie Ballard, Senior Director of Communications & Marketing, [email protected] , 225-263-2677 .
About the Pennington Biomedical Research Center
The Pennington Biomedical Research Center is at the forefront of medical discovery as it relates to understanding the triggers of obesity, diabetes, cardiovascular disease, cancer and dementia. The Center conducts basic, clinical, and population research, and is a campus of the LSU System. The research enterprise at Pennington Biomedical includes over 530 employees within a network of 44 clinics and research laboratories, and 13 highly specialized core service facilities. Its scientists and physician/scientists are supported by research trainees, lab technicians, nurses, dietitians, and other support personnel. Pennington Biomedical a state-of-the-art research facility on a 222-acre campus in Baton Rouge. For more information, see www.pbrc.edu .
Pennington Biomedical Research Center 6400 Perkins Road Baton Rouge, LA 70808
Centers & Institutes

Metabolic Basis of Disease Center
Institute for Dementia Research & Prevention
Louisiana Clinical & Translational Science Center
Nutrition Obesity Research Center
Metamor Institute
Center for Military Performance & Resilience
Childhood Obesity and Diabetes Research
Human Research Protections Program
Research Kitchen + Recipes
Business Development
LAUNCHED Program
Pennington Biomedical Research Foundation
Our Partners
Obesity Society
American Diabetes Association
Sign Up For Updates
6400 Perkins Rd. Baton Rouge, LA 70808 ph: (225) 763-2500 fax: (225) 763-3022
© Copyright Pennington Biomedical Research Center

- Publication
- Arts & Humanities
- Behavioural Sciences
- Business & Economics
- Earth & Environment
- Education & Training
- Health & Medicine
- Engineering & Technology
- Physical Sciences
- Thought Leaders
- Community Content
- Outreach Leaders
- Our Company
- Our Clients
- Testimonials
- Our Services
- Researcher App
- Podcasts & Video Abstracts
Subscribe To Our Free Publication
By selecting any of the topic options below you are consenting to receive email communications from us about these topics.
- Behavioral Science
- Engineering & Technology
- All The Above
We are able share your email address with third parties (such as Google, Facebook and Twitter) in order to send you promoted content which is tailored to your interests as outlined above. If you are happy for us to contact you in this way, please tick below.
- I consent to receiving promoted content.
- I would like to learn more about Research Outreach's services.
We use MailChimp as our marketing automation platform. By clicking below to submit this form, you acknowledge that the information you provide will be transferred to MailChimp for processing in accordance with their Privacy Policy and Terms .
Obesity and inflammation: A recipe for depression in women
A team led by Dr Julie Pasco, Professor of Epidemiology at Deakin University and Barwon Health, Australia, analysed data from the longitudinal Geelong Osteoporosis Study over 16 years. The researchers discovered that metabolically unhealthy obesity, defined by low-grade inflammation in combination with obesity, puts women at higher risk of developing depression. These novel findings highlight inflammation as both a key factor in this pathology and a potential target to minimise depression risk.
Metabolic disorders and obesity are on the rise worldwide. Shedding light on this topic and the increased risk these conditions carry for depression are Professor Julie Pasco and colleagues at Deakin University and Barwon Health, Australia. Experts in the patterns of such diseases across populations, Pasco and her team have published extensively on musculoskeletal and cardiometabolic diseases and their connection to mental health.

It has been known for some time that obesity is linked to depression and that this relationship is bi-directional. Controlling and treating obesity is therefore key to reducing these co-morbidities. The Geelong Osteoporosis Study, a population-based study beginning in 1993, was originally designed to understand the epidemiology of osteoporosis, but it has also enabled insight into other physical and mental disorders over time. Now, Pasco and team delve into this wealth of data again, this time unmasking a link between metabolically unhealthy obesity and depression.
Metabolic health
Changes to normal metabolism, altering it from its native homeostatic state, affect physiological processes in our cells, organs, and body. Poor metabolic health presents as metabolic syndrome, a mixture of conditions including fat build-up in organs, high blood glucose, high blood pressure, and imbalanced blood lipids. The presence of even one of these conditions indicates metabolic abnormality. Such metabolic abnormalities are a risk factor for cardiovascular disease and are termed cardiometabolic disorders.
Individuals with such disorders have a greater chance of heart attack, stroke, and coronary heart disease (fat build-up in coronary arteries). Globally, the prevalence of cardiometabolic disorders is increasing, with two-thirds residing in low- and middle-income countries. One of the many contributing factors to this is obesity, defined as excessive fat accumulation that can be detrimental to health. This body fat, known as adipose tissue, can act as a reservoir of pro-inflammatory cytokines (signalling molecules that promote inflammation).
Obesity can be divided into different phenotypes based on metabolic health status. This has led to the somewhat controversial terms ‘metabolically healthy obesity’ and ‘metabolically unhealthy obesity’. There are different ways to classify ‘metabolically unhealthy’, with the conditions present in metabolic syndrome often used to define it. However, in a first-of-its-kind study, Pasco and colleagues put the spotlight on obesity-related inflammation as opposed to metabolic syndrome conditions to determine obesity’s role in depression risk.
Inflammation at the heart of the problem
Inflammation is an immune reaction and a broad term indicating a state where pro-inflammatory markers outweigh anti-inflammatory responses. It can occur acutely or chronically, and examples include fighting off a foreign pathogen, auto-immune disorders, and prolonged exposure to irritants or allergies. Conditions such as obesity can promote inflammation due to fat deposits being a potential source of pro-inflammatory cytokines.

Metabolic dysregulation combined with persistent low-grade inflammation is known as immunometabolic dysregulation and in obese individuals constitutes an obesity phenotype. Research is growing on the association between this phenotype and psychiatric disorders. Another type of obesity is sarcopenic obesity, a condition occurring in ageing obese individuals who are often insulin resistant and also have low skeletal muscle mass and strength.
A well-known marker of inflammation is C-Reactive Protein (CRP). Existing evidence implicates circulating CRP, indicative of systemic inflammation, in obesity-related depression. One study found that high CRP levels were linked to worsening depression scores over time in a fifth of obese individuals. More than that, lower CRP levels following gastric bypass surgery complemented weight loss and are associated with improved depression scores. Now, in a well-characterised cohort of women followed for several years, Pasco and researchers demonstrate clear and strong evidence for an association between low-grade inflammation and depression in obese individuals.

The Geelong Osteoporosis Study, a unique epidemiological cohort study, began in the 1990s and has followed women living in Southeast Australia for decades, providing a wealth of data to better understand osteoporosis and risk factors for fragility fractures. The study also collects metabolic and mental disorders data. The study by Pasco and team focuses on a sub-analysis of 808 women followed for an average of 16 years. According to the researchers, one of their study’s strengths rests in the methods used to classify obesity. Measures included the well-known body mass index (BMI), which represents overall body mass adjusted for height, and more specific measures of body fatness wherein fat mass is detected by dual-energy x-ray absorptiometry and expressed as body fat mass adjusted for height (fat mass index) and body fat percentage. In addition, blood tests provided high sensitivity CRP levels as a marker of systemic inflammation. Another strength promoted by the researchers is the use of structured clinical interview methods to identify major depressive disorder (MDD) during follow-up.
Double trouble
Firstly, obesity alone increases MDD risk with rates one and a half times higher in obese women compared to non-obese peers. Similarly, high levels of CRP have also been identified as increasing MDD risk. However, it is a combination of obesity and high inflammation that led to the highest depression rates at follow-up, regardless of whether obesity was defined by BMI, body fat mass index, or body fat percentage. Importantly, this consistent finding was independent of age or any prior history of depression, and it could not be explained by socioeconomic status or sedentary lifestyles of this phenotype. The same findings were noted for women with a high ratio of body fat-to-muscle typically seen in sarcopenic obesity, adding to a mixed body of evidence for this condition. The researchers suggest that to improve our understanding of the confused literature for sarcopenic obesity, both a consensus on the definition is needed as well as better data on muscle quality in the condition. The researchers also note that women with depressive symptoms commonly have poor muscle strength which is a key characteristic of sarcopenia.
Other large cohort studies implicate metabolically unhealthy obesity as a risk factor for depression. The study by Pasco and colleagues supports these findings, stacking up the evidence for a strong link between metabolically unhealthy obesity and depression. The difference is this novel study focused on the harmful obesity type that is accompanied by heightened systemic inflammation which, in tandem, increase the risk of developing subsequent depression. This research provides valuable insight into the complex interplay of factors associated with MDD.
The researchers acknowledge their results may not be applicable to men and other ethnicities – more research is needed to confirm findings in these populations. Despite limitations, this large, well-characterised cohort provides vital insight into the development of depression in obese women.

New treatments for depression that target inflammation in metabolic disorders are needed. Pasco’s study highlights the pro-inflammatory state of obesity as a potential target to decrease depression risk. The team speculate that diet and insulin sensitisers may improve metabolic abnormality, but more therapies should be considered, including behavioural options that reduce inflammation in the body. Critically, this study makes clinicians aware of the psychological associations of metabolically unhealthy obesity related depression and that any successful therapies may have both physical and mental benefits. Now, the causes of this inflammation, obesity, and depression need to be determined to untangle their complex web and reveal therapeutic targets.
Personal Response
You mention in the publication that an extension to your study has the possibility of identifying novel treatments or behavioural modifications targeting metabolic disorders. Can you please elaborate further on this extension with an emphasis on the translational aspect of your work?
This feature article was created with the approval of the research team featured. This is a collaborative production, supported by those featured to aid free of charge, global distribution.
Want to read more articles like this, sign up to our mailing list and read about the topics that matter to you the most., leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The Epidemiology of Obesity: A Big Picture
The epidemic of overweight and obesity presents a major challenge to chronic disease prevention and health across the life course around the world. Fueled by economic growth, industrialization, mechanized transport, urbanization, an increasingly sedentary lifestyle, and a nutritional transition to processed foods and high calorie diets over the last 30 years, many countries have witnessed the prevalence of obesity in its citizens double, and even quadruple. Rising prevalence of childhood obesity, in particular, forebodes a staggering burden of disease in individuals and healthcare systems in the decades to come. A complex, multifactorial disease, with genetic, behavioral, socioeconomic, and environmental origins, obesity raises risk of debilitating morbidity and mortality. Relying primarily on epidemiologic evidence published within the last decade, this non-exhaustive review discusses the extent of the obesity epidemic, its risk factors—known and novel—, sequelae, and economic impact across the globe.
1. Introduction
Obesity is a complex, multifactorial, and largely preventable disease ( 1 ), affecting, along with overweight, over a third of the world’s population today ( 2 , 3 ). If secular trends continue, by 2030 an estimated 38% of the world’s adult population will be overweight and another 20% will be obese ( 4 ). In the USA, the most dire projections based on earlier secular trends point to over 85% of adults being overweight or obese by 2030 ( 5 ). While growth trends in overall obesity in most developed countries seem to have leveled off ( 2 ), morbid obesity in many of these countries continues to climb, including among children. In addition, obesity prevalence in developing countries continues to trend upwards toward US levels.
Obesity is typically defined quite simply as excess body weight for height, but this simple definition belies an etiologically complex phenotype primarily associated with excess adiposity, or body fatness, that can manifest metabolically and not just in terms of body size ( 6 ). Obesity greatly increases risk of chronic disease morbidity—namely disability, depression, type 2 diabetes, cardiovascular disease, certain cancers—and mortality. Childhood obesity results in the same conditions, with premature onset, or with greater likelihood in adulthood ( 6 ). Thus, the economic and psychosocial costs of obesity alone, as well as when coupled with these comorbidities and sequealae, are striking.
In this article, we outline the prevalence and trends of obesity, then review the myriad risk factors to which a preventive eye must be turned, and finally present the costs of obesity in terms of its morbidity, mortality, and economic burden.
2. Classification of Body Weight in Adults
The current most widely used criteria for classifying obesity is the body mass index (BMI; body weight in kilograms, divided by height in meters squared, Table 1 ), which ranges from underweight or wasting (<18.5 kg/m 2 ) to severe or morbid obesity (≥40 kg/m 2 ). In both clinical and research settings, waist circumference, a measure of abdominal adiposity, has become an increasingly important and discriminating measure of overweight/obesity ( 7 ). Abdominal adiposity is thought to be primarily visceral, metabolically active fat surrounding the organs, and is associated with metabolic dysregulation, predisposing individuals to cardiovascular disease and related conditions ( 8 ). Per internationally used guidelines of metabolic syndrome—a cluster of dysmetabolic conditions that predispose individuals to cardiovascular disease of which abdominal adiposity is one component—a waist circumference resulting in increased cardiovascular risk is defined as ≥94 cm in European men, and ≥80 cm in European women, with different cut points recommended in other races and ethnicities (e.g., ≥90 and ≥80 cm in men and women, respectively, in South Asians, Chinese, and Japanese) ( 8 , 9 ).
Common Classifications of Body Weight in Adults and Children
Abbreviations used: BMI, body mass index; IOTF, International Obesity Task Force; SD, standard deviation; WHO, World Health Organization; WH weight-for-height; Z, z score.
3. Classification of Body Weight in Children
In children, body weight classifications ( Table 1 ) differ from those of adults because body composition varies greatly as a child develops, and further varies between boys and girls primarily owing to differences in sexual development and maturation. The World Health Organization (WHO) Child Growth Standards are the most widely currently used classification system of weight and height status for children from birth to 5 years old, based on data from children in six regions across the globe born and raised in optimal conditions ( 10 ). In 2007, the WHO published updated growth references combining the 1977 National Center for Health Statistics (NCHS)/WHO growth reference and the 2006 WHO Child Growth Standards to create the most recent BMI-for-age references for individuals aged 5–19 years ( 11 ). Thus, the latest WHO guidelines are designed to represent relatively seamless standards and references from birth all the way into late adolescence/early adulthood.
In the USA, the Centers for Disease Control and Prevention (CDC) currently use the 2000 CDC growth references based on 1963–1994 US children’s data, to determine age- and sex-specific BMI percentiles for children aged 2–19 years ( 12 ). Overweight is defined in US children as age- and sex-specific BMI ≥85th and <95th percentile, while obesity is ≥95th percentile ( 13 ). Cut points for severe obesity in childhood have been proposed in recognition of the alarming growing prevalence of this extreme condition, defined as the 99th BMI percentile ( 13 ) or 120% of the 95th percentile ( 14 ). For US children <2 years old, the CDC currently uses the 2006 WHO Child Growth Standards, described above ( 15 ).
4. Prevalence and Trends
4.1. adult obesity—us and europe.
The first indications that obesity was taking on epidemic proportions originated in the USA and Europe. With few restrictions on access to or availability of food, the prevalence of overweight and obesity in the USA climbed virtually unmitigated over the last 50 years. Today, those who are overweight (BMI 25–<30 kg/m 2 ) or obese (BMI ≥30 kg/m 2 ) in the USA eclipse two-fold the numbers of those who are normal weight ( 16 ). In US adults, 1960–1994 trends showed that while levels of overweight hovered at approximately 31% over the time period, in contrast, age-adjusted obesity jumped from 13 to 23%, bringing the crude prevalence of overweight or obesity to 55% of the American population ( 17 ). Unfortunately, 1994 did not represent the endpoint of the upward trend, as the following decade saw adult obesity rise from 23 to 32% by 2003–2004 ( 16 ). In the last 10 years, national estimates of obesity seem to indicate that the steady upward trend of obesity in Americans has leveled off at a prevalence of about 35% ( 16 ) ( Figure 1 ), perhaps having reached some “Malthusian” obesity limit. However, certain subpopulations are faring worse than others, as 2011–2012 obesity rates in Hispanics and non-Hispanic blacks were 43 and 48%, respectively, pointing to a disproportionate burden in differing racial/ethnic and/or socioeconomic status (SES) groups. Gender also plays a role, with women being disproportionately affected by extreme obesity (classes 2–3, BMI ≥35 kg/m 2 ) than men, regardless of age or race/ethnicity ( 16 ).

Trends in age-adjusted prevalence of overweight, obesity, and extreme obesity in US adults, aged 20–74 years, 1960–2012. Trends in prevalence of overweight as BMI 25–<30 kg/m 2 (circles), and upward trends in obesity as BMI ≥30 kg/m 2 (squares), and extreme obesity as BMI ≥40 kg/m 2 (diamonds) in adult males (closed points) and females (open points). The figure is based on data from NHES I (1960–1962), NHANES I (1971–1974), NHANES II (1976–1980), NHANES III (1988–1994), and NHANES (1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012). Data derived are derived from Ogden, et al ., and Fryar, et al . ( 16 , 141 ). BMI, body mass index; NHANES, National Health and Nutrition Examination Survey; NHES, National Health Examination Survey.
Meanwhile, in Europe, longitudinal data (1992–1998 to 1998–2005) from participants in five countries involved in the European Prospective Investigation into Cancer and Nutrition (EPIC) study (Italy, the United Kingdom, the Netherlands, Germany, and Denmark), indicate that adult obesity increased modestly from 13 to 17% in that time period ( 18 ). However, were such linear trends were to continue, the overall obesity prevalence in these populations could reach 30% by 2015, paralleling US rates. A more conservative projection suggests a prevalence of just 20% obesity in these populations by 2015, if public awareness and public health measures take hold ( 18 ).
European studies including populations beyond EPIC indicate there is considerable disparity in overweight/obesity between European countries. A systematic review of national and regional surveys conducted between 1990 and 2008 points to obesity rates as low as 4.0 and 6.2% in French men and women, respectively (regional survey, 1994–1996), and as high as 30.0 and 32.0% in Czech men and women, respectively (national survey, 2002–2005) ( 19 ). Regional trends within Europe are apparent, with southern Italy and southern Spain, and Eastern European countries showing higher prevalence of obesity than countries in Western and Northern Europe ( 19 ). As in the USA, these data suggest that socioeconomic disparities and relatively recent/ongoing economic transitions are playing a considerable role in apparent differences across and within countries with respect to obesity risk.
4.2. Child Obesity—USA and Europe
US children may be faring better than their adult counterparts in some ways ( 16 ), potentially offsetting earlier dire predictions of rampant obesity by 2030 ( 5 ). In national surveys, levels of overweight in children, as in adults, seem to have leveled off (or even declined) at approximately 30% of US children aged 2–19 years ( 16 , 20 ). However, this belies a potentially disturbing long-term trend in the rising prevalence of extreme obesity (equivalent to adult class 2 obesity and higher, BMI ≥35 kg/m 2 ). Since 1999–2000, the prevalence of class 2 obesity in children (BMI ≥120% of the 95th percentile) has risen from 3.8 to 5.9% and class 3 obesity (BMI ≥140% of the 95th percentile) has doubled from 0.9 to 2.1%, the latter category jumping 30% since 2009–2010 alone ( 20 ). Again, as in their adult counterparts, certain sub-populations appear to be faring worse than others, notably Hispanic girls and Black boys, in whom overweight, obesity, and class 2 obesity have increased significantly ( 20 ).
Childhood obesity prevalence varies considerably between and within countries as well. Relatively recent estimates based on 2007–2008 data of children aged 6–9-years collected in 12 European countries as a part of the WHO European Childhood Obesity Surveillance Initiative observed overweight/obesity (BMI z score >+1 standard deviation [SD]) prevalence of 19.3–49.0% of boys and 18.4–42.5% of girls, while obesity (BMI z score >+2 SD) affected 6.0–26.6% of boys and 4.6–17.3% of girls. Researchers continued to observe the trend of north-south and west-east gradients evident in adults, with the highest levels of overweight in southern European countries ( 21 ).
4.3. Obesity Beyond North America and Europe
The data discussed above focus on the USA and European countries, many with robust national health surveillance programs. While historical data tends to be scarcer outside of these regions, an alarming picture has emerged over the last decades in low- and middle-income countries around the globe, complicated by rapidly changing socioeconomic environments. While country-specific trends are not discussed in this article, regional and national estimates of long-term changes in child (<20 years old) and adult (>20 years old) overweight and obesity have increased in nearly all countries and regions since 1980 ( Figure 2 ) ( 2 , 3 ). While the USA still may boast the largest absolute numbers of overweight and obese individuals, several other nations exceed the USA in terms of overall prevalence and, moreover, the rate of growth in certain countries is disheartening. For example, the prevalence of overweight and obesity in nationally representative Mexican adults was estimated to be 71.3% overweight/obese, with overweight at 38.8% and obesity at 32.4% ( 22 ). This prevalence represents an increase of 15% since 2000, placing this population among the most rapidly accelerating in terms of obesity prevalence over the last decade. Further, while rates of overweight remained relatively stable since 2000 at approximately 38% overall, extreme obesity (class 3, BMI ≥40 kg/m 2 ) increased by an estimated 76.5% from 2000 to 2012. These trends are also evident in countries outside of the Americas. In China, for example, between 1993 and 2009, overweight (BMI 25 to <27.5 kg/m 2 ) doubled in men (8 to 17%) and increased from 11 to 14% in women. Meanwhile, obesity (BMI ≥27.5 kg/m 2 ) nearly quadrupled in men, from 3 to 11%, and doubled in women, from 5 to 10%. Chinese children are faring as badly as their adult counterparts: overweight/obesity doubled from 6 to 13% in children aged 6–17 years over the same time period, suggesting that the obesity epidemic will continue to deepen in this country ( 23 ).

Prevalence of overweight and obesity in adults aged ≥20 years by global region, 1980–2008. From left to right, each column represents the estimated regional prevalence of overweight and obesity for 1980, 1985, 1990, 1995, 2000, 2005, and 2008. For a given region, a dark gray column indicates the lowest estimated prevalence in the trend, while the highest estimated prevalence is indicated by a black column. As is evident, the vast majority of regions demonstrate the lowest estimated prevalence of overweight and obesity in 1980, and the highest in 2008, demonstrating the global reach of obesity. The scale shows 25, 50, and 100% prevalence columns, for reference. Asterisks denotes high income. Data are sourced from Stevens, et al . ( 3 ).
5. Risk Factors for Obesity
Currently, our greatest gap in knowledge is not regarding the numbers of risk factors, nor in their independent impact on risk, but rather in how they interact with one another—their confluence—to produce today’s aptly if unfortunately named “globesity” epidemic. Obesity arises as the result of an energy imbalance between calories consumed and the calories expended, creating an energy surplus and a state of positive energy balance resulting in excess body weight. This energy imbalance is partially a result of profound social and economic changes at levels well beyond the control of any single individual. These “obesogenic” changes—economic growth, growing availability of abundant, inexpensive, and often nutrient-poor food, industrialization, mechanized transportation, urbanization—have been occurring in high-income countries since the early 20th century, and today these forces are accelerating in low- and middle-income countries. And yet, not all of us living in obesogenic environments experience the same growth in our waistlines. Hereditary factors—genetics, family history, racial/ethnic differences—and our particular socioeconomic and sociocultural milieus have been shown to affect risk of obesity ( Table 2 ) even in ostensibly similar obesogenic environments. So while body weight regulation is and should be viewed as a complex interaction between environmental, socioeconomic, and genetic factors, ultimately, personal behaviors in response to these conditions continue to play a dominant role in preventing obesity. Importantly, apart from genetics, every risk factor discussed below is modifiable .
Risk Factors, Comorbidities, and Sequelae of Obesity
5.1. Genetics of Obesity
To date, over 60 relatively common genetic markers 1 have been implicated in elevated susceptibility to obesity ( 24 , 25 ); however, the 32 most common genetic variants are thought to account for <1.5% of the overall inter-individual variation in BMI ( 24 ). When these 32 “top” genetic hits are combined into a genetic risk of obesity score, those with the highest genetic risk (i.e., carriers of over 38 risk alleles), have just a 2.7 kg/m 2 higher BMI on average than those with a low genetic risk. This translates into about a 15-lb (7-kg) weight difference between two 5’3” (160 cm) individuals with high versus low genetic risk ( 24 ). Although genetics undoubtedly play a role, this relatively small difference in BMI, coupled with the dramatic rise in obesity over the last half century in developed and developing nations alike point to obesity risk factors beyond genetics. A concomitant and rich area of research has therefore evolved investigating gene-environment interaction based on the idea that underlying genetic risk predisposes individuals to particularly adverse (or beneficial) effects of behavioral or environmental exposures such as diet and exercise, a concept scientifically popularized in, for example, the “thrifty gene” hypothesis ( 26 ). In many ways, these types of gene-environment interactions are playing out in population research: for example, a variant in FTO (rs9939609)—the strongest obesity susceptibility locus—increases odds of obesity in risk allele carriers by an estimated 23% per allele; however, this risk is modified by physical activity in adults ( 27 , 28 ) and children ( 29 ), among other factors. Nevertheless, these types of interactions have so far been investigated in relatively few genetic risk loci out of millions, and with just a handful of environmental factors, raising important questions of how to aggregate this complexity for public health and ultimately personalized medicine.
In addition, parental diet, lifestyle, and other exposures have been implicated in subsequent offspring obesity risk, including famine exposure ( 30 ), parental obesity ( 31 – 33 ), smoking ( 34 ), endocrine-disrupting and other chemicals ( 35 , 36 ), and weight gain during gestation and gestational diabetes ( 33 , 37 ). These and other studies point to lasting effects of fetal programming that via differing mechanisms, likely epigenetic, result in substantial repercussions in life course health, with implications across the socioeconomic/food availability spectrum. Careful management of diet and lifestyle in pre- and perinatal periods could exert a considerable impact on the obesity epidemic for generations to come ( 37 ).
5.2. Individual Behaviors
5.2.1. diet.
In the decades preceding the 21st century, the vast majority of research on obesity risk factors focused on individual-level, largely modifiable behaviors. The role of diet and physical activity in mitigating obesity risk and reducing prevalent obesity have received the most attention, and with good reason: 15% of deaths in 2000 in the USA were attributable to excess weight, owing to poor diet and physical inactivity ( 38 ). Caloric intake and expenditure needed for weight maintenance or healthy growth has historically taken center stage ( 39 ), and caloric restriction remains today a primary focus of most popular and clinical weight-management and weight-loss approaches.
Beyond overall caloric intake to regulate body weight, a tremendous amount of research has attempted to resolve the roles of diet quality and dietary patterns, including those specifying combinations of macronutrients ( 40 ). Evidence from clinical trials have almost universally shown that caloric restriction, regardless of dietary pattern, is associated with better weight outcomes ( 40 ). Although the metabolic nuances and relative merits of the differing dietary patterns for various comorbid conditions are still being investigated, the evidence seems to suggest that merely adhering to a diet—nearly irrespective of what type of healthy diet it is—has an impact on weight loss/control ( 41 – 43 ).
For long-term maintenance of healthy weight, evidence from observational cohorts indicate that diets that are considered “healthier” lead to better long-term weight maintenance, or at least mitigate weight gain typically associated with aging through middle age. For example, research in US health professionals pointed to averaged 4-year weight gain throughout middle age as being strongly associated with increasing intake of potato chips and potatoes, sugar-sweetened beverages, and processed and unprocessed red meats, but inversely associated with the intake of vegetables, fruits, whole grains, nuts, and yogurt ( 44 ). Specific food groups, such as sugar-sweetened beverages, have received considerable attention largely because added sugar consumption (primarily as sugar-sweetened beverages) has been rising concomitantly with prevalent obesity ( 45 ). Indeed, the weight of the evidence about the role of sugar-sweetened beverages in obesity ( 46 , 47 ) is a strong impetus for public health interventions and policies, such as limiting advertising on these beverages as in Mexico ( 48 ), attempts to limit beverage sizes permitted for sale as in New York City ( 49 ), taxation, eliminating sale in schools, etc.
5.2.2. Physical Activity, Sedentary Behaviors, and Sleep
Personal behaviors beyond diet (physical activity, sleep, sedentary and screen time, and stress) have also been independently associated with weight change and maintenance in adulthood. Combined with diet, these elements have synergistic and likely cumulative effects on an individual’s ability to maintain or obtain a healthy body weight over the life course. Recently reviewed evidence from randomized trials and observational studies support 2008 US recommendations for weight management ( 50 ), consistently showing that in general, 150–250 minutes per week of moderate intensity activity is required to prevent weight gain, or aid in weight loss when accompanied by dietary restriction ( 51 ). Activity (>250 minutes per week) is associated with weight loss and weight maintenance after weight loss ( 51 ). Leisure-time activities involving sitting, but which are not truly restful behaviors, such as getting <6 or >8 hours of sleep in adults and adolescents ( 44 , 52 – 55 ) or <10–11 hours of sleep in children ( 52 ), television viewing or screen time ( 44 , 56 , 57 ), and other leisure-time sitting ( 58 ) are also associated with weight gain.
5.3. Socioeconomic Risk Factors: Income and Education
Income has had a shifting role in obesity risk over the last century. As late as the mid-20th century, the USA and Europe could link wealth directly with obesity—the wealthier an individual, the more likely to be overweight. Over the last few decades, however, perhaps owing to the abundance of cheap and highly available food, coupled with changing sociocultural norms, this link has flipped. Today, wealth in the USA tends to be inversely correlated with obesity, and it is those who are at or below the level of poverty who appear to have the highest rates of obesity ( 59 ). Indeed, in US cities where the homeless are surveyed, the prevalence of overweight and obesity parallels that of non-homeless populations, contrary to our typical beliefs about thinness accompanying food insecurity or homelessness ( 60 , 61 ).
More broadly, across 11 Organisation for Economic Co-Operation and Development (OECD) countries, SES, whether defined by household income or occupation-based social class, showed an inverse relationship with obesity: women, in particular, had consistently higher prevalence of overweight/obesity the less affluent they were ( 62 ). In men, too, those in low income strata tended to have higher prevalence of obesity, but the gradient for overweight reversed in about half of the countries surveyed. That is, in some countries, poverty was associated with more prevalent overweight than wealth, but in others, lower income was associated with more favorable weight status. The differences between sexes in terms of income status and obesity, in particular the trend reversal in men, may be in part due to low-paying jobs typically involving more physically demanding work performed by men more than by women ( 62 ). Adding complexity to this picture is the role of education: in the 11 OECD countries discussed above, education showed a strong inverse relationship with overweight/obesity, particularly in women, who had consistently higher prevalence of overweight/obesity the less educated they were ( 62 ).
As wealth rises in low- and middle-income countries, it is expected for poverty-obesity patterns to begin more closely mimicking those of high-income countries. Evidence of this transition is already accumulating. In explorations of the role of education and wealth in women and weight status in four middle-income countries (Colombia, Peru, Jordan, and Egypt), authors observed a significant interaction between education and wealth: in women with little or no education, higher income was associated with 9–40% higher odds of obesity, while in those with higher levels of education, the association with income was either not present (Egypt, Peru) or associated with 14–16% lower odds of obesity (Jordan, Colombia) ( 63 ). This suggests that in currently transitioning economies, education may offset the apparently negative effects of increasing purchasing power in emerging obesogenic environments. However, the protective effect of education has yet to be seen in the poorer countries, such as India, Nigeria, and Benin, where both education and wealth were directly associated with increased odds of obesity ( 63 ).This is perhaps unsurprising, as obesity was relatively rare at <6.0% of women in these countries, and >50% of women had little or no education.
The glimmer of hope, then, is that in the context of a paradigm of diseases of affluence, in which the transition to wealth seem to invariably lead to higher obesity and thus greater chronic disease burden, higher education levels may yet offset some of the frightening challenges that lay before us.
5.4. Environmental 2 Risk Factors
5.4.1. the built environment.
Research on the built environment tends to focus on a few measurable characteristics of neighborhoods as they relate to weight status, while holding sociodemographic and other person-level characteristics constant. Such neighborhood characteristics range from more concrete factors (e.g., fast food restaurants, supermarkets, parks, transportation, etc.) to more variably scored factors (e.g., walkability, neighborhood healthiness). Most studies of the built environment have been cross-sectional, tending to focus on one or two characteristics; thus, findings on the relative importance or effects of given characteristics on obesity have been inconsistent ( 66 – 72 ), revealing the fundamental challenge of teasing out whether neighborhood characteristics play a causal role in weight status, or whether health-minded folks inhabit health-friendly areas to begin with (residential selection bias) ( 73 ). However, the emerging picture points to the primacy of diet-related built environments over those associated with physical activity. While presence of neighborhood physical activity or recreational spaces has been associated with increased physical activity levels or energy expenditure ( 71 , 72 ), healthy food environments, characterized by availability of produce or presence of supermarkets over convenience stores or fast food restaurants, play a potentially more important role ( 68 , 70 , 74 , 75 ).
Research on the causality of the built environment as obesity-inducing or health-promoting is critical for municipalities and public health authorities to justify potentially costly improvements to public spaces and/or zoning regulations. There is an unmet need for standardized measures, definitions, and criteria, established residential and occupational geographic radii relevant to health, and research methodologies that can take into account the complexity of something as seemingly simple as a neighborhood.
5.4.2. Environmental “Pathogens”: Viruses, Microbiomes, and Social Networks
Growing evidence from animal and human studies indicates that obesity may be attributable to infection, or that obesity itself may be a contagion. Infectious agents include viruses, the trillions of microbiota inhabiting the human gut, and, of course, obese humans as infectious agents themselves.
Although several viruses have been identified as potentially having a causal role in obesity ( 76 ), Ad-36 is among the most studied, being causally associated with adiposity in animals. Studies in diverse human populations generally support greater Ad-36 viral loads as probably causal of obesity in both children and adults ( 76 – 79 ), with links to other metabolic traits ( 77 , 79 ).
Ground-breaking research in the last decade has emerged on the role of trillions of gut bacteria—the human microbiome—in relation to obesity, energy metabolism, and carbohydrate and lipid digestion, opening promising therapeutic avenues for obesity and disease ( 80 ). Two primary phyla of bacteria differ in their proportions in lean vs. obese populations; these proportions change as obese individuals lose weight and correlate highly with the percentage of body weight lost ( 81 ). Broad and sometimes dramatic changes in microbiome populations have been catalogued following gastric bypass surgery ( 80 ), and in both the short- ( 82 , 83 ) and long-term ( 81 , 83 ) in response to changes in dietary composition ( 80 ). Research in mice indicates that increased adiposity is a transmissible trait via microbiome transplantation ( 84 ), and has prompted similar experimental fecal transplantation research in humans for the promotion of weight loss ( 85 ). In addition, other research has examined the feeding of pre- and probiotics as therapeutic modalities designed to manipulate the gut microbiome; these strategies also show promise for a range of conditions ( 85 ).
Finally, the importance of social networks—real and virtual—in obesity is a fascinating, relatively new area of research that capitalizes on known characteristics of infectious disease transmission. In a landmark 2007 study examining the spread of obesity due to social ties using 32-year prospective data from the Framingham Heart Study, Christakis and Fowler ( 86 ) showed that an individual’s chances of becoming obese increased by 57% if he or she had a friend who became obese in a given 4-year interval. This was a stronger risk ratio than that observed between pairs of adult siblings or even between spouses. Conversely, it may be possible to capitalize on the social contagion of obesity in the reverse direction, that is, in the promotion of healthy weight and behavior. Intervention studies of weight loss often include a social-relational component, although the evidence supporting any single approach or its efficacy is relatively scarce ( 87 ). In theory, a supportive network, community, or coaching relationship is supposed to improve weight loss; despite a lack of strong evidence, it is a key component of many popular commercial (e.g., Weight Watchers), trial/intervention, and online approaches.
6. Costs of Obesity: Co-Morbidities, Mortality, and Economic Burden
Obesity is associated with concomitant or increased risk of nearly every chronic condition, from diabetes, to dyslipidemia, to poor mental health. Its impacts on risk of stroke and cardiovascular disease, certain cancers, and osteoarthritis are significant.
6.1. Overall Mortality
In the year 2000 in the USA, 15% of deaths were attributable to excess weight, owing to poor diet and physical inactivity ( 38 ). Overweight/obesity in middle age shortens life expectancy by an estimated 4–7 years ( 88 ). Many long-term cohort studies, as well as three recent major syntheses of pooled data from established cohorts ( 89 – 91 ), which adequately accounted for history of smoking and chronic disease status, unequivocally show that overweight and obesity over the life course is associated with excess risk of total mortality, death from cardiovascular disease, diabetes, cancer, or accidental death ( 89 – 97 ).
Some studies suggest that excess body weight may be protective against mortality from certain chronic conditions—resulting in a so-called “obesity paradox.” However, most studies that have shown an obesity paradox, or no association between obesity and mortality, have been conducted in groups of older (>65) or elderly patients or in those with chronic conditions, or have inadequately accounted for smoking. Indeed, the role of excess adiposity in old age is unclear. While the protective effects of overweight in specific instances of diseased older populations may be real, these observations are fraught with methodological problems, especially reverse causation, and belie the limitations of generalizing excess adiposity’s supposed benefits to younger populations over the life course, not least because excess body weight leads to higher disease incidence to begin with ( 7 ).
6.2. Diabetes
Excess weight and diabetes are so tightly linked that the American Diabetes Association recommends physicians test for type 2 diabetes and assess risk of future diabetes in asymptomatic people ≥45 years old simply if they are overweight/obese, and regardless of age if they are severely obese ( 98 ). Overweight raises risk of developing type 2 diabetes by a factor of three, and obesity by a factor of seven, compared to normal weight ( 99 ). Excess weight in childhood and in young adulthood, and weight gain through early to mid-adulthood are strong risk factors for diabetes ( 100 – 102 ). While not every overweight/obese individual has diabetes, some 80% of those with diabetes are overweight/obese ( 103 ). Obesity itself raises diabetes risk even in the absence of other metabolic dysregulation (insulin resistance, poor glycemic control, hypertension, dyslipidemia). While metabolically healthy obese individuals are estimated to have half the risk of their metabolically unhealthy counterparts, they still have four times the risk of those who are normal weight and metabolically healthy ( 104 ).
6.3. Heart and Vascular Diseases
Ischemic heart disease and stroke are the leading causes of death in the USA and globally ( 105 ). Excess body weight is a well-known risk factor for heart disease and ischemic stroke, including their typical antecedents—dyslipidemia and hypertension. Recent studies have consistently shown that benign obesity appears to be a myth ( 106 – 108 ); overweight clearly adds to risk of heart disease and stroke beyond its implications for hypertension, dyslipidemia, and dysglycemia.
Given childhood obesity rates, research has lately focused on the role of obesity in early life and subsequent adulthood disease. Obesity in childhood or adolescence has been associated with twofold or higher risk of adult hypertension, coronary heart disease, and stroke ( 100 ). A recent study pooling data from four child cohorts (aged 11 years at baseline with average 23-year follow-up), observed that, compared with individuals who were normal weight in childhood and non-obese as adults, those who were normal weight or overweight but became obese as adults, or who were obese and stayed obese into adulthood, had considerably higher risk of high-risk dyslipidemia, hypertension, and higher carotid intima-media thickness. Notably, those individuals who were overweight/obese as children, but non-obese as adults, had similar risk profiles to those individuals who were never obese, indicating that the potential health effects of childhood obesity can be offset by weight loss prior to or while entering into adulthood ( 109 ).
6.4. Cancer
An estimated 6% of all cancers (4% in men, 7% in women) diagnosed in 2007 were attributable to obesity ( 110 ). Beyond being a major risk factor for diabetes, which itself is a risk factor for most cancers, obesity has long been understood to be associated with increased risk of esophageal, colon, pancreatic, postmenopausal breast, endometrial, and renal cancers ( 111 ). More recently, evidence has accumulated that overweight and/or obesity raise risk of cancers of the gallbladder ( 112 ), liver ( 113 ), ovaries (epithelial) ( 114 ), and advanced cancer of the prostate ( 115 ), as well as leukemia ( 116 ).
6.5. Trauma and Infection
A study in Pennsylvania (USA) trauma centers (2000–2009) showed that in-hospital mortality and risk of major complications of surgery were increased in obese patients as compared to non-obese patients. Severely obese patients had upwards of 30% increased risk of mortality from their trauma than non-obese patients, and double the risk of major complications. Severely obese females also had more than double the risk of developing wound complications, and quadruple the risk of developing decubitus ulcers ( 117 ). A recent meta-analysis of obesity in trauma care concluded that obesity was associated with 45% increased odds of mortality, longer stays in the intensive care unit, and higher rates of complications, and tended to associate with longer durations of mechanical ventilation and longer stays in the hospital overall, compared to non-obese patients, despite equivalent injury severity ( 118 ).
While elevated risk of chronic disease is a seemingly obvious consequence of obesity, increasing attention is being given to increased risk of infection and infectious disease in obesity, including surgical-site, intensive care unit (ICU)-acquired catheter, blood, nosocomial, urinary tract, and cellulitis and other skin infections ( 119 ), community-acquired infections, and poorer recovery outcomes owing to higher risk of influenza, pneumonia, bacteremia, and sepsis ( 119 ). Impaired immunological response may be an underlying mechanism; recent research has demonstrated lower vaccine efficacy and serological response to vaccination in the obese. For example, a recent study estimated an eightfold increase in the odds of non-responsiveness to hepatitis-B vaccination in obese versus normal-weight women ( 120 ).
The consequences of a global obesity epidemic may not merely be greater chronic and infectious disease burden for the obese, but also a greater global burden of infectious disease owing to obesity. Greater infectious disease vigilance may be required in populations with high levels of overweight/obesity, and there is a clear need for better clinical practice guidelines (e.g., use and dosage of antimicrobials, vaccines, other pharmaceuticals) for obese individuals.
6.6. Mental Health
The role of weight in mental health faces causal challenges, but what is clear is that obesity and adiposity are associated with anatomical as well as functional changes in the human brain. Studies in older populations have shown that BMI is inversely correlated with brain volume, and that obese older adults, compared to normal weight counterparts, show atrophy in the frontal lobes, anterior cingulate gyrus, hippocampus, and thalamus ( 121 ). In addition, obesity in children and adolescents (aged >9 years) has been associated with smaller orbitofrontal cortex gray matter volume, along with poorer performance in certain domains of executive function (e.g., inhibitory control) ( 122 ). Being overweight in midlife increases risk of Alzheimer's disease, vascular dementia, or any type of dementia by 35, 33, and 26%, respectively; even higher risk is observed for obesity ( 123 ). Importantly, physical activity, even among overweight individuals, may stave off poor mental functioning: moderately active or highly active adult overweight Finns did not have significantly increased risk of poor mental functioning at a 7-year follow-up compared to those who were normal weight and highly active, but inactive and overweight patients presented a nearly 40% increased risk of poor mental functioning ( 124 ). Thus, exercise may play an important mediating role in the relationship between excess body weight and age-related cognitive decline.
6.7. Economic Burden of Obesity
In the USA, recent estimates indicate that obese men are thought to incur an additional US$1,152 per year in medical spending, particularly due to hospitalizations and prescription drugs, compared to their non-obese counterparts, while obese women incur over double that of obese men, an additional US$3,613 per year in medical spending (year 2005 values). Extrapolating these costs to the national level, authors estimate some US$190 billion per year of healthcare spending, approximately 21% of US healthcare expenditures, is due to treating obesity and obesity-related conditions ( 125 ).
Total hospital costs account for a part of this: another author group studied non-bariatric, non-obstetric hospital procedures for obese patients, finding they were US$648 higher (year 2009 values) per capita than for non-obese patients. The estimated national hospital expenditures for the largest volume surgical procedures was US$160 million higher per year for obese than for their non-obese counterparts ( 126 ).
Employers bear a substantial brunt of obesity-related costs in the USA. Data from the Human Capital Management Services Research Reference Database (2001–2012) on employees and their dependents was used to compare medical, drug, sick leave, short-term disability, and workers’ compensation costs as well as absent days across three BMI strata: <27, ≥27–<30, and ≥30 kg/m 2 . Each of the costs was incrementally higher in ascending BMI categories. For example, total annual costs and total days absent in the highest vs. lowest BMI strata were US$6,313 versus US$4,258 (year 2012 values), and 7.5 versus 4.5 days. In addition, productivity was lowest in the obese group ( 127 ).
Finally, lifetime direct incremental medical costs of obesity in childhood in the USA were estimated to range from US$12,660 to US$19,630 (year 2012 values) for an obese 10-year old compared to a normal-weight 10-year old, if expected weight gain through adulthood among the normal weight child occurs ( 128 ). If normal weight children were to not continue on the typical weight gain trajectory into overweight/obesity, estimated incremental medical costs for today’s 10-year old obese child ranges between US$16,310 and US$39,080. Putting these figures into perspective, multiplying the lifetime medical cost estimate of US$19,000 by the number of obese 10-year-olds today generates a total direct medical cost of obesity of roughly US$14 billion for this 10-year old age group alone. In terms of big picture savings, the upper estimate of US$39,000 per case represents two years of public college tuition for that child ( 128 ).
In Europe, a 2008 review of 13 studies in ten Western European countries estimated the obesity-related healthcare burden had a relatively conservative upper limit of €10.4 billion annually (in Germany, in 1995 € equivalent), and ranging between <0.1 to 0.61% of each country’s gross domestic product (GDP). The review relied on study data from as early as the 1980s in the Netherlands, through 2002 in most of the remaining countries surveyed ( 129 ). A more recent review focused on 19 studies published in 2007–2010 in eight Western European countries (predominantly Germany, Denmark, and the United Kingdom). Excess health care costs of obesity or derivations of excess health care costs by comparisons of mean costs between normal weight and obese individuals in seven of the reviewed studies were between €117 and €1,873 per person (based on the € valuation given in each study year). Excess costs increased particularly due to severe obesity. Approximately 23% of medication costs and 6.9% of out-of-pocket costs were attributable to overweight or obesity. Health economic models estimated that 2.1–4.7% of total health care costs and 2.8% of total hospital costs were due to overweight and obesity. Total (direct and indirect) costs were generally unchanged from the 2008 estimate of the earlier review, accounting for 0.47–0.61% of GDP in these countries ( 130 ).
In the context of the Brazilian Unified Health System (i.e., public hospitals), estimated direct costs of diseases related to overweight/obesity in outpatient and inpatient care based on 2008–2010 data were US$2.1 billion annually (year 2010 values), 68.4% of which was attributable to hospitalizations, and the remainder due to ambulatory procedures ( 131 ). The largest costs of outpatient and inpatient care in both sexes were due to cardiovascular disease (US$747 million) followed by overweight- and obesity-related neoplasms (US$299.8 million), asthma (US$34 million), type 2 diabetes (US$3.7 million), and osteoarthritis (US$3.9 million). Authors estimated that these direct costs were a considerable underestimate of the true burden of overweight/obesity in Brazil, which would include private health care expenditures, as well as indirect costs due to lost productivity, premature death, and home care ( 131 ).
Given the predicted rise in obesity in Brazil, coronary heart disease, stroke, hypertension, cancers, osteoarthritis, and diabetes are projected to at least double by 2050, with concomitant doubling in health care costs, from US$5.8 billion in 2010 to US$10.1 billion per year—totaling US$330 billion over 40 years (year 2010 values). It is estimated that a 5% reduction in mean BMI across the population could save Brazil some US$57 billion over that time frame ( 132 ). A similar analytic approach that substituted Mexican prevalence and trends for the Brazilian ones estimated 2010 costs of obesity at US$806 million (year 2000 values), which were projected to increase to US$1.7 billion by 2050, at which point a mere 1% reduction in BMI prevalence in Mexico could save an estimated US$85 million per year ( 133 ).
Of course, none of these estimates include dollars spent on the weight-loss industry, which is estimated to be over US$60 billion dollars in 2014 in the USA alone ( 134 ), and includes non-prescription drugs and supplements, diet plans, gym memberships, workout videos, and an endless stream of money-making schemes.
7. Touching on Solutions, and Some Conclusions
Obesity is a major contributor to preventable disease and death across the globe, and poses a nearly unprecedented challenge not just to those tasked with addressing it at the public health level, or at the healthcare provider level, but to each of us as individuals, for none of us are immune. Increasing ease of life, owing to reduced physical labor and automated transportation, an increasingly sedentary lifestyle, and liberal access to calorie-dense food, driven by dramatic economic growth in many parts of the world in the last century, have turned a once rare disease of the affluent into one of the most common diseases—increasingly of the poor. That barely one in three people in the USA today are normal weight portends, quite simply, an astounding and frightening future. Significant reductions in public health and healthcare expenditures could occur around the world if we were able to stem the tide of childhood obesity trends, and if young and middle-aged overweight and obese adults lost approximately10% of their body weight, as recommended for a considerably reduced risk of debilitating chronic conditions ( 135 ).
Obesity is complex. Although its risk factors are myriad and compounding, there is an urgent need for deeper understanding of the way risk factors interact with each other, and the potential solutions to the epidemic are as multi-leveled and complex as its causes. There are calls for applying systems-level ( 136 ) and systems epidemiology ( 137 ) approaches to this and related nutrition and metabolic diseases, approaches which attempt to comprehensively address biological, behavioral, and environmental contributors to disease as well as their intricate feedback loops. Additional research on solutions to this epidemic would include, for example, examining the relative cost/benefit to individuals and populations of individual versus systemic policies and/or interventions, concurrently or independently, particularly when individuals and communities must decide between approaches given limited resources, and moreover, with the currently limited evidence in the case of broad industry, agricultural, or public health policies. For example, we could attempt to limit national production and import of sugar-sweetened beverages, tax sugar-sweetened beverages, or restrict fast food restaurant zoning. These largely political acts seem relatively inexpensive, but may have economic impacts in communities and regions beyond what we currently understand. We may push for the increasing medicalization of obesity, including developing an obesity vaccine. While such a “cure” may someday arise, the medicalization of a condition typically improves its treatment rather than its prevention, and prevention is key in the case of obesity. However, preventing and remediating obesity in children and adults—e.g., via health and wellness incorporation into curricula at every educational level from kindergarten through medical school—requires vast resources allocated to educators, as well as earlier diagnosis and treatment of overweight (education, counseling, drug treatment, etc.). Given these resource costs, perhaps greater attention should be given to pregnancy, a condition which is already highly medicalized and which may be an ideal preventive avenue for the provision of nutrition education and intensive monitoring of weight gain, to ensure that children have the most optimal start with respect to their future obesity risk. Clearly, no single approach is optimal, but with limited resources, an evidence base supporting one or more approaches or their combination is needed, as is tenacity and perhaps some audacity by local government and public health authorities in testing some of these approaches within their populations. However, an epidemic of this magnitude needs, quite simply, more resources. One of the reasons why the American Medical Association opted to declare obesity a “disease” was to give obesity the label it needs for greater allocation of resources for research, prevention, and treatment ( 1 ).
Despite the many unknowns, we can be cautiously optimistic about our ability to address the obesity epidemic. Indeed, we have relatively successfully faced similarly daunting public health challenges before: smoking, to name just one. While tobacco can loosely be thought of as a single product, and our food culture is infinitely more complex, as a case study in how to approach obesity, it provides numerous lessons in multi-level solutions to a major health threat in terms of both mitigation and prevention. We began by developing an understanding of smoking’s epidemiological impact and the healthcare costs borne by society, uncovered its biological basis, learned about and applied behavior change, and initiated and carried out vast public health, public policy, political, and economic strategies that ultimately affected whole environments as well as sociocultural norms.
It took over half a century to achieve the immense success we have with regard to smoking in the USA and still we are not yet tobacco-free ( 138 ); other parts of the world continue to wrestle with it to a greater degree. It has only been a couple decades since we first deeply appreciated that obesity was epidemic. We clearly still have a long way to go.
Key Points for Decision Makers
- In 2013, an estimated one in three adults worldwide was overweight or obese, and adult obesity exceeded 50% in several countries around the globe. While the prevalence of adult obesity in the developed world seems to have stabilized, the prevalence of obesity in children and adolescents globally, as well as adults obesity in developing countries, is still increasing. In addition, some developed countries continue to observe increasing prevalence of extreme classes of obesity.
- Overweight and obesity—defined as excess body weight for height—have genetic, behavioral, socioeconomic, and environmental origins.
- Obesity increases risk of major chronic diseases, including heart disease, diabetes, depression, and many cancers, as well as premature death.
- Estimates of annual healthcare costs attributable to obesity are US$190 billion per year in the USA, approximately 21% of US healthcare expenditures.
- Given its complexity, the obesity epidemic requires multilevel and integrated solutions, from individual intervention, to broad food policy, industry, and agriculture initiatives.
Acknowledgements
The authors declare no conflict of interest. AH is supported by an American Diabetes Association Mentor-Based Postdoctoral Fellowship award. FH is supported by NIH grants DK51158, HL60712, P30 DK46200, and U54CA155626. The authors broadly thank the researchers in this field for their consistent and tireless work in illuminating the etiology, sequelae, and solutions to this complex condition.
1 See also http://www.genome.gov/gwastudies/
2 We do not review the impact of food, agriculture, trade, and nutrition policy on obesity in the present paper, but refer interested readers to a recent review ( 64 ). Further, we do not address the body of growing evidence on the role of environmental pollutants–“obesogens”–in obesity, specifically those known as endocrine-disrupting chemicals. We refer readers to recent reviews on the topic ( 35 , 36 , 65 ).
Author Contributions
AH wrote the first draft of the paper. AH and FH contributed to writing, revised, and edited the paper. AH is the final guarantor of this work and takes full responsibility for its contents. Both authors read and approved the final manuscript.

IMAGES
COMMENTS
Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the prevalence of 30.5% during 1999 to 2002. 2 Among those afflicted with ...
The obesity epidemic. The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a).A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2.It is well known that obesity and overweight are a growing problem globally with high rates in ...
N Engl J Med 2023;389:2467-2467. A 25-year-old woman with severe obesity presented with a 1-week history of blurred vision and headaches. Neurologic examination revealed optic-disk swelling in ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
1. Introduction. Obesity is a chronic disease that is increasing in prevalence and is now considered to be a global epidemic. Epidemiologic studies have revealed an association between high body mass index (BMI) and an extensive range of chronic diseases such as Non Alcoholic Fatty Liver (NAFL), cardiovascular disease , , diabetes mellitus , several malignancies , , musculoskeletal diseases ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
Projected State-Specific Prevalence of Adult Obesity and Severe Obesity in 2030. Our projections show that the national prevalence of adult obesity and severe obesity will rise to 48.9% (95% ...
Obesity articles from across Nature Portfolio. Obesity is a condition in which excess fat has accumulated in the body, such that it can have an adverse effect on health. Obesity is defined as a ...
Obesity is the official journal of The Obesity Society and is the premier source of information for increasing knowledge, fostering translational research from basic to population science, and promoting better treatment for people with obesity. Obesity publishes important peer-reviewed research and cutting-edge reviews, commentaries, and public ...
Obesity is excessive accumulation of body fat, that results from the impairment in energy balance mechanisms [ 3, 4 ]. Example of the condition edema can illustrate this point. Edema is not a ...
See the 2020-2030 Strategic Plan for NIH Nutrition Research. The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) external link. , which is a public-private partnership to accelerate progress in reducing childhood obesity. The NHLBI has been providing guidance to physicians on the diagnosis, prevention ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this ...
Obesity affects brain cortex gene expression in an APOE genotype and sex dependent manner. Harshul Pandit. Nahdia S. Jones. G. William Rebeck. Article 07 Mar 2024.
DOI: 10.1056/NEJMe1514957. The prevalence of severe obesity in the United States has increased dramatically, not only among adults but also among children. The increase in childhood severe obesity ...
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the ...
Obesity, mortality and BMI. Obesity, as defined by BMI (Table 1), is associated with an increased risk of all-cause mortality, with CVD and malignancy being the most common causes of death. 5 -8 A meta-analysis of 239 prospective studies involving 10.6 million individuals from Asia, Australia, New Zealand, Europe and North America found that all-cause mortality was lowest between a BMI of 20 ...
Submit your best research and join the community of thought leaders in the fight against obesity. Read more about Obesity.. Obesity editorial staff. Editor-in-Chief: Michael Jensen, MD Associate Editor-In-Chief: Leanne Redman, PhD. Obesity Journal Symposium. Leading papers from the journal are presented at the annual Obesity Journal Symposium at ObesityWeek® each November.
Worldwide adult obesity has more than doubled since 1990, and adolescent obesity has quadrupled. In 2022, 2.5 billion adults (18 years and older) were overweight. Of these, 890 million were living with obesity. In 2022, 43% of adults aged 18 years and over were overweight and 16% were living with obesity. In 2022, 37 million children under the ...
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, "Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55.
Future childhood obesity research should evaluate the best methods for educating primary care providers in providing family-centered care and the optimal approaches to delivering this care. Acknowledgments. The authors would like to thank Dr Tom D. Thacher, Mayo Clinic Department of Family Medicine Research Chair, for support of our work. ...
Pennington Biomedical Research Center ... Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, ...
Obesity is a classified risk factor for several of the world's leading causes of death. In this study, we combined information contained in body mass index (BMI), total percentage body fat (TPBF) and relative fat mass (RFM) to estimate obesity prevalence and examine the risk factors associated with obesity. The study recruited 1027 undergraduate students aged between 16 and 25 years using a ...
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health, increases the risk of long-term medical complications and reduces lifespan. 1 Epidemiologic studies define obesity using the body mass index (BMI; weight/height 2), which can stratify obesity-related health risks at the population level.Obesity is operationally defined as a BMI exceeding 30 kg ...
Obesity often continues into adulthood and is linked to a range of chronic health conditions and premature death. Growing research is showing the benefits of universal free school meals for the ...
Background: The management of type 2 diabetes (T2D) and obesity, particularly in the context of self-monitoring, remains a critical challenge in health care. As nearly 80% to 90% of patients with T2D have overweight or obesity, there is a compelling need for interventions that can effectively manage both conditions simultaneously. One of the goals in managing chronic conditions is to increase ...
Obesity is now the most common form of malnutrition in most countries, with the rates rising in all categories of men, women, children and adolescents since 1990. ... The research enterprise at Pennington Biomedical includes over 530 employees within a network of 44 clinics and research laboratories, and 13 highly specialized core service ...
Introduction. Childhood and adolescent obesity have reached epidemic levels in the United States, affecting the lives of millions of people. In the past 3 decades, the prevalence of childhood obesity has more than doubled in children and tripled in adolescents. 1 The latest data from the National Health and Nutrition Examination Survey show that the prevalence of obesity among US children and ...
Research is growing on the association between this phenotype and psychiatric disorders. Another type of obesity is sarcopenic obesity, a condition occurring in ageing obese individuals who are often insulin resistant and also have low skeletal muscle mass and strength. A well-known marker of inflammation is C-Reactive Protein (CRP).
We also expect obesity drug data from Structure Therapeutics, Eli Lilly, and Amgen. But it's not all obesity: Sage Therapeutics will have readouts in Parkinson's disease, Huntington's ...
2. Classification of Body Weight in Adults. The current most widely used criteria for classifying obesity is the body mass index (BMI; body weight in kilograms, divided by height in meters squared, Table 1), which ranges from underweight or wasting (<18.5 kg/m 2) to severe or morbid obesity (≥40 kg/m 2).In both clinical and research settings, waist circumference, a measure of abdominal ...