An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Breech presentation.
Caron J. Gray ; Meaghan M. Shanahan .
Affiliations
Last Update: November 6, 2022 .
- Continuing Education Activity
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. This activity reviews the cause and pathophysiology of breech presentation and highlights the role of the interprofessional team in its management.
- Describe the pathophysiology of breech presentation.
- Review the physical exam of a patient with a breech presentation.
- Summarize the treatment options for breech presentation.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by breech presentation.
- Introduction
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended). [1] [2] [3]
Clinical conditions associated with breech presentation include those that may increase or decrease fetal motility, or affect the vertical polarity of the uterine cavity. Prematurity, multiple gestations, aneuploidies, congenital anomalies, Mullerian anomalies, uterine leiomyoma, and placental polarity as in placenta previa are most commonly associated with a breech presentation. Also, a previous history of breech presentation at term increases the risk of repeat breech presentation at term in subsequent pregnancies. [4] [5] These are discussed in more detail in the pathophysiology section.
- Epidemiology
Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech.
Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10%, and for a subsequent third pregnancy, it was 27%. Prior cesarean delivery has also been described by some to increase the incidence of breech presentation two-fold.
- Pathophysiology
As mentioned previously, the most common clinical conditions or disease processes that result in the breech presentation are those that affect fetal motility or the vertical polarity of the uterine cavity. [6] [7]
Conditions that change the vertical polarity or the uterine cavity, or affect the ease or ability of the fetus to turn into the vertex presentation in the third trimester include:
- Mullerian anomalies: Septate uterus, bicornuate uterus, and didelphys uterus
- Placentation: Placenta previa as the placenta is occupying the inferior portion of the uterine cavity. Therefore, the presenting part cannot engage
- Uterine leiomyoma: Mainly larger myomas located in the lower uterine segment, often intramural or submucosal, that prevent engagement of the presenting part.
- Prematurity
- Aneuploidies and fetal neuromuscular disorders commonly cause hypotonia of the fetus, inability to move effectively
- Congenital anomalies: Fetal sacrococcygeal teratoma, fetal thyroid goiter
- Polyhydramnios: Fetus is often in unstable lie, unable to engage
- Oligohydramnios: Fetus is unable to turn to vertex due to lack of fluid
- Laxity of the maternal abdominal wall: Uterus falls forward, the fetus is unable to engage in the pelvis.
The risk of cord prolapse varies depending on the type of breech. Incomplete or footling breech carries the highest risk of cord prolapse at 15% to 18%, while complete breech is lower at 4% to 6%, and frank breech is uncommon at 0.5%.
- History and Physical
During the physical exam, using the Leopold maneuvers, palpation of a hard, round, mobile structure at the fundus and the inability to palpate a presenting part in the lower abdomen superior to the pubic bone or the engaged breech in the same area, should raise suspicion of a breech presentation.
During a cervical exam, findings may include the lack of a palpable presenting part, palpation of a lower extremity, usually a foot, or for the engaged breech, palpation of the soft tissue of the fetal buttocks may be noted. If the patient has been laboring, caution is warranted as the soft tissue of the fetal buttocks may be interpreted as caput of the fetal vertex.
Any of these findings should raise suspicion and ultrasound should be performed.
Diagnosis of a breech presentation can be accomplished through abdominal exam using the Leopold maneuvers in combination with the cervical exam. Ultrasound should confirm the diagnosis.
On ultrasound, the fetal lie and presenting part should be visualized and documented. If breech presentation is diagnosed, specific information including the specific type of breech, the degree of flexion of the fetal head, estimated fetal weight, amniotic fluid volume, placental location, and fetal anatomy review (if not already done previously) should be documented.
- Treatment / Management
Expertise in the delivery of the vaginal breech baby is becoming less common due to fewer vaginal breech deliveries being offered throughout the United States and in most industrialized countries. The Term Breech Trial (TBT), a well-designed, multicenter, international, randomized controlled trial published in 2000 compared planned vaginal delivery to planned cesarean delivery for the term breech infant. The investigators reported that delivery by planned cesarean resulted in significantly lower perinatal mortality, neonatal mortality, and serious neonatal morbidity. Also, there was no significant difference in maternal morbidity or mortality between the two groups. Since that time, the rate of term breech infants delivered by planned cesarean has increased dramatically. Follow-up studies to the TBT have been published looking at maternal morbidity and outcomes of the children at two years. Although these reports did not show any significant difference in the risk of death and neurodevelopmental, these studies were felt to be underpowered. [8] [9] [10] [11]
Since the TBT, many authors since have argued that there are still some specific situations that vaginal breech delivery is a potential, safe alternative to planned cesarean. Many smaller retrospective studies have reported no difference in neonatal morbidity or mortality using these specific criteria.
The initial criteria used in these reports were similar: gestational age greater than 37 weeks, frank or complete breech presentation, no fetal anomalies on ultrasound examination, adequate maternal pelvis, and estimated fetal weight between 2500 g and 4000 g. In addition, the protocol presented by one report required documentation of fetal head flexion and adequate amniotic fluid volume, defined as a 3-cm vertical pocket. Oxytocin induction or augmentation was not offered, and strict criteria were established for normal labor progress. CT pelvimetry did determine an adequate maternal pelvis.
Despite debate on both sides, the current recommendation for the breech presentation at term includes offering external cephalic version (ECV) to those patients that meet criteria, and for those whom are not candidates or decline external cephalic version, a planned cesarean section for delivery sometime after 39 weeks.
Regarding the premature breech, gestational age will determine the mode of delivery. Before 26 weeks, there is a lack of quality clinical evidence to guide mode of delivery. One large retrospective cohort study recently concluded that from 28 to 31 6/7 weeks, there is a significant decrease in perinatal morbidity and mortality in a planned cesarean delivery versus intended vaginal delivery, while there is no difference in perinatal morbidity and mortality in gestational age 32 to 36 weeks. Of note, due to lack of recruitment, no prospective clinical trials are examining this issue.
- Differential Diagnosis
- Face and brow presentation
- Fetal anomalies
- Fetal death
- Grand multiparity
- Multiple pregnancies
- Oligohydramnios
- Pelvis Anatomy
- Preterm labor
- Primigravida
- Uterine anomalies
- Pearls and Other Issues
In light of the decrease in planned vaginal breech deliveries, thus the decrease in expertise in managing this clinical scenario, it is prudent that policies requiring simulation and instruction in the delivery technique for vaginal breech birth are established to care for the emergency breech vaginal delivery.
- Enhancing Healthcare Team Outcomes
A breech delivery is usually managed by an obstetrician, labor and delivery nurse, anesthesiologist and a neonatologist. The ultimate decison rests on the obstetrician. To prevent complications, today cesarean sections are performed and experienced with vaginal deliveries of breech presentation is limited. For healthcare workers including the midwife who has no experience with a breech delivery, it is vital to communicate with an obstetrician, otherwise one risks litigation if complications arise during delivery. [12] [13] [14]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gray CJ, Shanahan MM. Breech Presentation. [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. [Z Geburtshilfe Neonatol. 1997] [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. Krause M, Fischer T, Feige A. Z Geburtshilfe Neonatol. 1997 Jul-Aug; 201(4):128-35.
- The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. [Early Hum Dev. 1993] The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. Sival DA, Prechtl HF, Sonder GH, Touwen BC. Early Hum Dev. 1993 Mar; 32(2-3):161-76.
- The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. [PLoS One. 2019] The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. Jennewein L, Allert R, Möllmann CJ, Paul B, Kielland-Kaisen U, Raimann FJ, Brüggmann D, Louwen F. PLoS One. 2019; 14(12):e0225546. Epub 2019 Dec 2.
- Review Breech vaginal delivery at or near term. [Semin Perinatol. 2003] Review Breech vaginal delivery at or near term. Tunde-Byass MO, Hannah ME. Semin Perinatol. 2003 Feb; 27(1):34-45.
- Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. [Gynecol Obstet Fertil Senol. 2...] Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. Mattuizzi A. Gynecol Obstet Fertil Senol. 2020 Jan; 48(1):70-80. Epub 2019 Nov 1.
Recent Activity
- Breech Presentation - StatPearls Breech Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Christine Zink, MD, is a board-certified emergency medicine with expertise in the wilderness and global medicine. She completed her medical training at Weill Cornell Medical College and residency in emergency medicine at New York-Presbyterian Hospital. She utilizes 15-years of clinical experience in her medical writing.
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Fetal Presentation, Position, and Lie (Including Breech Presentation)
, MD, Children's Hospital of Philadelphia
Variations in Fetal Position and Presentation
- 3D Models (0)
- Calculators (0)
- Lab Test (0)

Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).

The fetus has a birth defect Overview of Birth Defects Birth defects, also called congenital anomalies, are physical abnormalities that occur before a baby is born. They are usually obvious within the first year of life. The cause of many birth... read more .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
Sometimes the doctor can turn the fetus to be head first before labor begins by doing a procedure that involves pressing on the pregnant woman’s abdomen and trying to turn the baby around. Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication (such as terbutaline ) during the procedure to prevent contractions.
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.
Drugs Mentioned In This Article

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition

- IN THIS TOPIC
When viewing this topic in a different language, you may notice some differences in the way the content is structured, but it still reflects the latest evidence-based guidance.
Breech presentation
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Breech presentation in pregnancy occurs when a baby presents with the buttocks or feet rather than the head first (cephalic presentation) and is associated with increased morbidity and mortality for both the mother and the baby. [1] Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997. [2] Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002. There is good current evidence regarding effective management of breech presentation in late pregnancy using external cephalic version and/or planned cesarean section.
History and exam
Key diagnostic factors.
- buttocks or feet as the presenting part
- fetal head under costal margin
- fetal heartbeat above the maternal umbilicus
Other diagnostic factors
- subcostal tenderness
- pelvic or bladder pain
Risk factors
- premature fetus
- small for gestational age fetus
- nulliparity
- fetal congenital anomalies
- previous breech delivery
- uterine abnormalities
- abnormal amniotic fluid volume
- placental abnormalities
- female fetus
Diagnostic investigations
1st investigations to order.
- transabdominal/transvaginal ultrasound
Treatment algorithm
<37 weeks' gestation, ≥37 weeks' gestation not in labor, ≥37 weeks' gestation in labor: no imminent delivery, ≥37 weeks' gestation in labor: imminent delivery, contributors, natasha nassar, phd.
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Disclosures
NN has received salary support from Australian National Health and a Medical Research Council Career Development Fellowship; she is an author of a number of references cited in this topic.
Christine L. Roberts, MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
CLR declares that she has no competing interests.
Jonathan Morris, MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
JM declares that he has no competing interests.
Peer reviewers
John w. bachman, md.
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
JWB declares that he has no competing interests.
Rhona Hughes, MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
RH declares that she has no competing interests.
Brian Peat, MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
BP declares that he has no competing interests.

Lelia Duley, MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
LD declares that she has no competing interests.
Justus Hofmeyr, MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
JH is an author of a number of references cited in this topic.
Differentials
- Transverse lie
- Antenatal corticosteroids to reduce neonatal morbidity and mortality
- Caesarean birth
Use of this content is subject to our disclaimer
Help us improve BMJ Best Practice
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
- Help & Feedback
- About epocrates
Breech presentation
Highlights & basics, diagnostic approach, risk factors, history & exam, differential diagnosis.
- Tx Approach
Emerging Tx
Complications.
PATIENT RESOURCES
Patient Instructions
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Quick Reference
Key Factors
buttocks or feet as the presenting part
Fetal head under costal margin, fetal heartbeat above the maternal umbilicus.
Other Factors
subcostal tenderness
Pelvic or bladder pain.
Diagnostics Tests
1st Tests to Order
transabdominal/transvaginal ultrasound
Treatment options.
presumptive
<37 weeks' gestation
specialist evaluation
corticosteroid
magnesium sulfate
≥37 weeks' gestation not in labor
unsuccessful ECV with persistent breech
Classifications
Types of breech presentation
Baby's buttocks lead the way into the birth canal
Hips are flexed, knees are extended, and the feet are in close proximity to the head
65% to 70% of breech babies are in this position.
Baby presents with buttocks first
Both the hips and the knees are flexed; the baby may be sitting cross-legged.
One or both of the baby's feet lie below the breech so that the foot or knee is lowermost in the birth canal
This is rare at term but relatively common with premature fetuses.
Common Vignette
Other Presentations
Epidemiology
33% of births less than 28 weeks' gestation
14% of births at 29 to 32 weeks' gestation
9% of births at 33 to 36 weeks' gestation
6% of births at 37 to 40 weeks' gestation.
Pathophysiology
- Natasha Nassar, PhD
- Christine L. Roberts, MBBS, FAFPHM, DrPH
- Jonathan Morris, MBChB, FRANZCOG, PhD
- John W. Bachman, MD
- Rhona Hughes, MBChB
- Brian Peat, MD
- Lelia Duley, MBChB
- Justus Hofmeyr, MD

Clinical exam
Palpation of the abdomen to determine the position of the baby's head
Palpation of the abdomen to confirm the position of the fetal spine on one side and fetal extremities on the other
Palpation of the area above the symphysis pubis to locate the fetal presenting part
Palpation of the presenting part to confirm presentation, to determine how far the fetus has descended and whether the fetus is engaged.
Ultrasound examination
Premature fetus.
Prematurity is consistently associated with breech presentation. [ 6 ] [ 9 ] This may be due to the smaller size of preterm infants, who are more likely to change their in utero position.
Increasing duration of pregnancy may allow breech-presenting fetuses time to grow, turn spontaneously or by external cephalic version, and remain cephalic-presenting.
Larger fetuses may be forced into a cephalic presentation in late pregnancy due to space or alignment constraints within the uterus.
small for gestational age fetus
Low birth-weight is a risk factor for breech presentation. [ 9 ] [ 11 ] [ 12 ] [ 13 ] [ 14 ] Term breech births are associated with a smaller fetal size for gestational age, highlighting the association with low birth-weight rather than prematurity. [ 6 ]
nulliparity
Women having a first birth have increased rates of breech presentation, probably due to the increased likelihood of smaller fetal size. [ 6 ] [ 9 ]
Relaxation of the uterine wall in multiparous women may reduce the odds of breech birth and contribute to a higher spontaneous or external cephalic version rate. [ 10 ]
fetal congenital anomalies
Congenital anomalies in the fetus may result in a small fetal size or inappropriate fetal growth. [ 9 ] [ 12 ] [ 14 ] [ 15 ]
Anencephaly, hydrocephaly, Down syndrome, and fetal neuromuscular dysfunction are associated with breech presentation, the latter due to its effect on the quality of fetal movements. [ 9 ] [ 14 ]
previous breech delivery
The risk of recurrent breech delivery is 8%, the risk increasing from 4% after one breech delivery to 28% after three. [ 16 ]
The effects of recurrence may be due to recurring specific causal factors, either genetic or environmental in origin.
uterine abnormalities
Women with uterine abnormalities have a high incidence of breech presentation. [ 14 ] [ 17 ] [ 18 ] [ 19 ]
female fetus
Fifty-four percent of breech-presenting fetuses are female. [ 14 ]
abnormal amniotic fluid volume
Both oligohydramnios and polyhydramnios are associated with breech presentation. [ 1 ] [ 12 ] [ 14 ]
Low amniotic fluid volume decreases the likelihood of a fetus turning to a cephalic position; an increased amniotic fluid volume may facilitate frequent change in position.
placental abnormalities
An association between placental implantation in the cornual-fundal region and breech presentation has been reported, although some studies have not found it a risk factor. [ 8 ] [ 20 ] [ 21 ] [ 22 ] [ 10 ] [ 14 ]
The association with placenta previa is also inconsistent. [ 8 ] [ 9 ] [ 22 ] Placenta previa is associated with preterm birth and may be an indirect risk factor.
Pelvic or vaginal examination reveals the buttocks and/or feet, felt as a yielding, irregular mass, as the presenting part. [ 26 ] In cephalic presentation, a hard, round, regular fetal head can be palpated. [ 26 ]
The Leopold maneuver on examination suggests breech position by palpation of the fetal head under the costal margin. [ 26 ]
The baby's heartbeat should be auscultated using a Pinard stethoscope or a hand-held Doppler to indicate the position of the fetus. The fetal heartbeat lies above the maternal umbilicus in breech presentation. [ 1 ]
Tenderness under one or other costal margin as a result of pressure by the harder fetal head.
Pain due to fetal kicks in the maternal pelvis or bladder.
breech position
Visualizes the fetus and reveals its position.
Used to confirm a clinically suspected breech presentation. [ 28 ]
Should be performed by practitioners with appropriate skills in obstetric ultrasound.
Establishes the type of breech presentation by imaging the fetal femurs and their relationship to the distal bones.
Transverse lie
Differentiating Signs/Symptoms
Fetus lies horizontally across the uterus with the shoulder as the presenting part.
Similar predisposing factors such as placenta previa, abnormal amniotic fluid volume, and uterine anomalies, although more common in multiparity. [ 1 ] [ 2 ] [ 29 ]
Differentiating Tests
Clinical examination and fetal auscultation may be indicative.
Ultrasound confirms presentation.
Treatment Approach
Breech presentation <37 weeks' gestation.
The UK Royal College of Obstetricians and Gynaecologists (RCOG) recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ] The American College of Obstetricians and Gynecologists (ACOG) recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
Magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, and concurrent tocolysis. [ 34 ]
Breech presentation from 37 weeks' gestation, before labor
ECV is the initial treatment for a breech presentation at term when the patient is not in labor. It involves turning a fetus presenting by the breech to a cephalic (head-down) presentation to increase the likelihood of vaginal birth. [ 35 ] [ 36 ] Where available, it should be offered to all women in late pregnancy, by an experienced clinician, in hospitals with facilities for emergency delivery, and no contraindications to the procedure. [ 35 ] There is no upper time limit on the appropriate gestation for ECV, with success reported at 42 weeks.
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
The procedure involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
The overall ECV success rate varies but, in a large series, 47% of women following an ECV attempt had a cephalic presentation at birth. [ 35 ] [ 38 ] Various factors influence the success rate. One systematic review found ECV success rates to be 68% overall, with the rate significantly higher for women from African countries (89%) compared with women from non-African countries (62%), and higher among multiparous (78%) than nulliparous women (48%). [ 39 ] Overall, the ECV success rates for nulliparous and multiparous non-African women were 43% and 73%, respectively, while for nulliparous and multiparous African women rates were 79% and 91%, respectively. Another study reported no difference in success rate or rate of cesarean section among women with previous cesarean section undergoing ECV compared with women with previous vaginal birth. However, numbers were small and further studies in this regard are required. [ 40 ]
Women's preference for vaginal delivery is a major contributing factor in their decision for ECV. However, studies suggest women with a breech presentation at term may not receive complete and/or evidence-based information about the benefits and risks of ECV. [ 41 ] [ 42 ] Although up to 60% of women reported ECV to be painful, the majority highlighted the benefits outweigh the risks (71%) and would recommend ECV to their friends or be willing to repeat for themselves (84%). [ 41 ] [ 42 ]
Cardiotocography and ultrasound should be performed before and after the procedure. Tocolysis should be used to facilitate the maneuver, and Rho(D) immune globulin should be administered to women who are Rhesus negative. [ 35 ] Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with ECV in some countries, but not yet available in the US). One Cochrane review of tocolytic beta stimulants demonstrates that these are less likely to be associated with failed ECV, and are effective in increasing cephalic presentation and reducing cesarean section. [ 43 ] There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended. The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48 to 72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. One systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of three, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
Planned cesarean section should be offered as the safest mode of delivery for the baby, even though it carries a small increase in serious immediate maternal complications compared with vaginal birth. [ 24 ] [ 25 ] [ 31 ] In the US, most unsuccessful ECV with persistent breech will be delivered via cesarean section.
A vaginal mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Breech presentation from 37 weeks' gestation, during labor
The first option should be a planned cesarean section.
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ]
Planned cesarean section is safer for babies, but is associated with increased neonatal respiratory distress. The risk is reduced when the section is performed at 39 weeks' gestation. [ 64 ] [ 65 ] [ 66 ] For women undergoing a planned cesarean section, RCOG recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] ACOG does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
Undiagnosed breech in labor generally results in cesarean section after the onset of labor, higher rates of emergency cesarean section associated with the least favorable maternal outcomes, a greater likelihood of cord prolapse, and other poor infant outcomes. [ 23 ] [ 67 ] [ 49 ] [ 68 ] [ 69 ] [ 70 ] [ 71 ]
This mode of delivery may be considered by some clinicians as an option for women who are in labor, particularly when delivery is imminent. Vaginal breech delivery may also be considered, where suitable, when delivery is not imminent, maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Findings from one systematic review of 27 observational studies revealed that the absolute risks of perinatal mortality, fetal neurologic morbidity, birth trauma, 5-minute Apgar score <7, and neonatal asphyxia in the planned vaginal delivery group were low at 0.3%, 0.7%, 0.7%, 2.4%, and 3.3%, respectively. However, the relative risks of perinatal mortality and morbidity were 2- to 5-fold higher in the planned vaginal than in the planned cesarean delivery group. Authors recommend ongoing judicious decision-making for vaginal breech delivery for selected singleton, term breech babies. [ 72 ]
ECV may also be considered an option for women with breech presentation in early labor, when delivery is not imminent, provided that the membranes are intact.
A woman presenting with a breech presentation <37 weeks is an area of clinical controversy. Optimal mode of delivery for preterm breech has not been fully evaluated in clinical trials, and the relative risks for the preterm infant and mother remain unclear. In the absence of good evidence, if diagnosis of breech presentation prior to 37 weeks' gestation is made, prematurity and clinical circumstances should determine management and mode of delivery.
Primary Options
12 mg intramuscularly every 24 hours for 2 doses
6 mg intramuscularly every 12 hours for 4 doses
The UK Royal College of Obstetricians and Gynaecologists recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ]
The American College of Obstetricians and Gynecologists recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
consult specialist for guidance on dose
external cephalic version (ECV)
There is no upper time limit on the appropriate gestation for ECV; it should be offered to all women in late pregnancy by an experienced clinician in hospitals with facilities for emergency delivery and no contraindications to the procedure. [ 35 ] [ 36 ]
ECV involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
Cardiotocography and ultrasound should be performed before and after the procedure.
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. A systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of 3, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
tocolytic agents
see local specialist protocol for dosing guidelines
Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with external cephalic version [ECV] in some countries, but not yet available in the US). They are used to delay or inhibit labor and increase the success rate of ECV. There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended.
The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48-72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
A systematic review found there was no evidence to support the use of nifedipine for tocolysis. [ 73 ]
There is insufficient evidence to evaluate other interventions to help ECV, such as fetal acoustic stimulation in midline fetal spine positions, or epidural or spinal analgesia. [ 43 ]
Rho(D) immune globulin
300 micrograms intramuscularly as a single dose
Nonsensitized Rh-negative women should receive Rho(D) immune globulin. [ 35 ]
The indication for its administration is to prevent rhesus isoimmunization, which may affect subsequent pregnancy outcomes.
Rho(D) immune globulin needs to be given at the time of external cephalic version and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
It is best administered as soon as possible after the procedure, usually within 72 hours.
Dose depends on brand used. Dose given below pertains to most commonly used brands. Consult specialist for further guidance on dose.
elective cesarean section/vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors. In the US, most unsuccessful external cephalic version (ECV) with persistent breech will be delivered via cesarean section.
Cesarean section, at 39 weeks or greater, has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, bleeding, infection, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Vaginal delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women undergoing a planned cesarean section, the UK Royal College of Obstetricians and Gynaecologists recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] The American College of Obstetricians and Gynecologists does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
It is best administered as soon as possible after delivery, usually within 72 hours.
Administration of postpartum Rho (D) immune globulin should not be affected by previous routine prenatal prophylaxis or previous administration for a potentially sensitizing event. [ 74 ]
≥37 weeks' gestation in labor: no imminent delivery
planned cesarean section
For women with breech presentation in labor, planned cesarean section at 39 weeks or greater has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Continuous cardiotocography monitoring should continue until delivery. [ 24 ] [ 25 ]
vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors.
This mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women with persisting breech presentation, planned cesarean section has, however, been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
ECV may also be considered an option for women with breech presentation in early labor, provided that the membranes are intact.
There is no upper time limit on the appropriate gestation for ECV. [ 35 ]
Involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
Relative contraindications include placental abruption, severe preeclampsia/HELLP syndrome, and signs of fetal distress (abnormal cardiotocography and/or abnormal Doppler flow). [ 35 ] [ 36 ]
Rho(D) immune globulin needs to be given at the time of ECV and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
≥37 weeks' gestation in labor: imminent delivery
cesarean section
For women with persistent breech presentation, planned cesarean section has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
This mode of delivery may be considered by some clinicians as an option, particularly when delivery is imminent, maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
It is best administered as soon as possible after the delivery, usually within 72 hours.
External cephalic version before term
Moxibustion, postural management, follow-up overview, perinatal complications.
Compared with cephalic presentation, persistent breech presentation has increased frequency of cord prolapse, abruptio placentae, prelabor rupture of membranes, perinatal mortality, fetal distress (heart rate <100 bpm), preterm delivery, lower fetal weight. [ 10 ] [ 11 ] [ 67 ]
complications of cesarean section
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ] The evidence suggests that using sutures, rather than staples, for wound closure after cesarean section reduces the incidence of wound dehiscence. [ 59 ]
Emergency cesarean section, compared with planned cesarean section, has demonstrated a higher risk of severe obstetric morbidity, intra-operative complications, postoperative complications, infection, blood loss >1500 mL, fever, pain, tiredness, and breast-feeding problems. [ 23 ] [ 48 ] [ 50 ] [ 70 ] [ 81 ]
Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
25. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG committee opinion no. 745: mode of term singleton breech delivery. Obstet Gynecol. 2018 Aug;132(2):e60-3. [Abstract] [Full Text]
26. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
27. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
28. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
29. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
30. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
31. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
32. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
33. American College of Obstetricians and Gynaecologists Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. August 2017 (reaffirmed 2020) [internet publication]. [Full Text]
34. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. Committee opinion no. 455: magnesium sulfate before anticipated preterm birth for neuroprotection. March 2010 (reaffirmed 2020) [internet publication]. [Full Text]
35. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
36. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
37. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
38. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
39. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
40. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
41. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
42. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
43. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
44. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
45. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
46. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
47. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
48. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
49. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
50. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
51. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
52. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
53. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
54. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
55. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
56. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
57. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
58. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
59. National Institute for Health and Care Excellence. Caesarean birth. Mar 2021 [internet publication]. [Full Text]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
68. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
69. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
70. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
71. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
72. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
73. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
74. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
75. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
76. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
77. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
78. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
79. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
80. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
81. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Published by
American College of Obstetricians and Gynecologists
2016 (reaffirmed 2022)
Royal College of Obstetricians and Gynaecologists (UK)
National Institute for Health and Care Excellence (UK)
Topic last updated: 2024-03-05
Natasha Nassar , PhD
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Christine L. Roberts , MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
Jonathan Morris , MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
Peer Reviewers
John W. Bachman , MD
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
Rhona Hughes , MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
Brian Peat , MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
Lelia Duley , MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
Justus Hofmeyr , MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
- Search Please fill out this field.
- Newsletters
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

- Cerebral Palsy
- Erb's Palsy
- Brain Damage
- Delivery Complications
- Prenatal Problems
- Birth Injury Stories

- Breech Position
Not all babies move into the normal head-first presentation before delivery. Instead, a certain percentage of babies do not reposition and end up with their butt and/or feet downwards towards the birth canal with the head up.
This referred to as the "breech" position or breech presentation. Breech position is not normal and consider a pregnancy complication. The occurrence rate of breech position is around 5% or 1 out of every 25 babies in full-term pregnancies. The occurrence rate for breach presentation is significantly higher, however, in preterm pregnancies.
Normally in the last few weeks of a pregnancy the baby will gradually reposition itself in the head down presentation in preparation for birth. Head first is the normal presentation because it is the optimal position to safely and effectively facilitate vaginal delivery. When in the head first position the crown of the baby's skull functions like a spear head which pushes into and through the birth canal.
Breech presentation generally includes any presentation in which the baby's butt or feet are pointing down towards the birth canal. However, there are several different recognized subtypes of breech presentation depending on the specifics and extent of the baby's abnormal position and the positioning of the legs:
- Frank Breech : the butt is still facing down toward the birth canal (same as with complete breech) instead of the legs being bent at the knees and tucked in the fetal position the baby's legs at straight at the knees and facing upwards so that the feet are basically in front of the face. Frank breech is the most common type of breech in full-terms babies and accounts for anywhere from 50-70% of all breech presentations.
- Footling Breech : in a footling breech presentation the baby's feet are actually pointing downward and will enter first into the birth canal ahead of the butt. Footling breech is more common in premature babies. Fooling has the second highest occurrence rate of all breech positions.
- Complete Breech : in complete breech presentation the butt is aimed down towards the birth canal entrance and the baby is in the traditional "fetal" position with knees bent and pulled up to the chest and feet near the butt. Complete breech is rarest of all types of breech presentation. Less than 10% of breech birth are classified as complete breech.
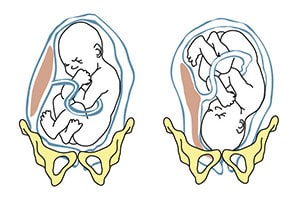
- Pregnancy with twins or multiples
- Mother has had prior pregnancies
- Maternal history of premature delivery
- Too much amniotic fluid ( polyhydramnios )
- Placenta previa
- Abnormally shaped uterus or abnormal uterine growths (fibroids)
The occurrence of any of these complications during pregnancy can significantly increase the chances of breech presentation occurring. However, breech presentation can occur in a normal pregnancy without complications.
Breech presentation is something that gets diagnosed towards the very end of a full term pregnancy. A formal diagnosis of breech presentation is not made until at least the 35 th week of pregnancy because before week 35 it is perfectly normal for a baby to be positioned head-up or sideways. Repositioning is something that the baby is supposed to naturally do on their own in the final few weeks before birth.
Diagnosis of breech presentation will start in a prenatal examination occurring at or sometime after the 35 th week of gestation. The doctor will initially perform a manual abdominal exam to gently feel around and identify the apparent position of the baby's head, butt and feet. If the baby doesn't seem to be in the expected position an ultrasound will usually be done to confirm the diagnosis of breech presentation. If ultrasound imaging is not enough there are also special prenatal X-rays that can be done to give doctors a more accurate image of the baby's presentation.
When a baby is in breech position attempting a vaginal delivery can be very dangerous and most OB/GYNs will automatically plan to deliver the baby via C-section. There are several reasons why vaginal delivery of a breech baby is so hazardous.
For starters, breech presentation makes the basic mechanics of vaginal delivery much more difficult. The baby's head is the largest part of their body so it is the most difficult to push through the birth canal. This is why brachial plexus palsy is the most common injury in a vaginal breech delivery. In a normal, head-first delivery the crown of the baby's head sort of spears its way into and through the birth canal. Getting the head safely through the birth canal in the reverse direction is much more difficult and potentially dangerous.
Another major reason why vaginal delivery from breech position is so hazardous is because there is a much higher risk of a delivery complication called umbilical cord prolapse . Umbilical cord prolapse is one of the most dangerous events that can occur during childbirth. It occurs when the umbilical cord (the baby's lifeline to the mother) drops down into the birth canal in front of the baby (instead of behind like in a normal delivery). When the cord goes first and the baby comes through the birth canal after the umbilical cord gets squeezed and compressed against the walls of the birth canal by the baby's head and body. This can severely restrict or even cut off oxygen supply to the baby and cause major brain injuries or even death from perinatal asphyxia.
Attempting a vaginal delivery when the baby is in breech position can greatly increase the risk of a birth injury. Although there is currently a major push towards doing less C-sections, breech presentation is a situation where a planned C-section is simply the most sensible option. This is particularly true for premature babies that are more fragile.
Further Reading
Athiel, Y., et al. (2022). Association Between Hospitals' Cesarean Delivery Rates For Breech Presentation And Their Success Rates For External Cephalic Version. European Journal of Obstetrics & Gynecology and Reproductive Biology, 270 , 156-163.
This article looked at the association between a hospital’s C-section and external cephalic version rates. The researchers found that the ECV success rates correlated with C-section rates for persistent breech presentations.
Benmessaoud, I., et al. (2022). Analysis of spontaneous labor progression of breech presentation at term. PloS one, 17 (3), e0262002.
This article looked at the labor progression pattern in breech presentation patients and determined whether the breech type or parity affected cervical dilation speed. The researchers found that the labor progression’s first stage in breech presentation involved latent and active phases. They also found that labor progression should be interpreted based on parity and breech type did not seem to influence the cervical dilation rate when adequately managed.
Claire, G., et al. (2022). Neonatal morbidity and mortality for preterm in breech presentation regarding the onset mode of labor. Archives of Gynecology and Obstetrics , 1-10.
This study compared the neonatal mortality and morbidity rates in preterm breech deliveries involving induced labor and spontaneous labor. The researchers found that both groups had similar neonatal mortality and morbidity rates. They concluded that the onset mode of labor did not seem to affect neonatal mortality and morbidity in breech presentation cases.
Coskun, B., et al. (2020). Comparison of Emergency and Elective Cesarean Sections in the Breech Presentation: A Case-Control Study.
This study compared outcomes in breech presentation pregnancies that underwent an emergency C-section and those that underwent an elective C-section. The researchers found that the emergency C-section group had lower Apgar scores and postoperative hemoglobin levels. They also found that cervical dilations of two centimeters and above in emergency C-sections were associated with lower hemoglobin counts, increased blood transfusion needs, and NICU transfers. The researchers concluded that healthcare providers should use caution when considering emergency C-sections and avoid iatrogenic preterm births.
Lallemant, M., et al. (2021). Asymmetric pelvis and term breech presentation: is planned vaginal delivery still a safe option? Archives of Gynecology and Obstetrics, 304 , 919-927.
This study looked at whether planned vaginal deliveries were safe for term breech presentations involving asymmetric pelvises. The researchers found higher vaginal delivery rates in the asymmetric pelvis group compared to the symmetric group. They also found no statistical differences in neonatal and maternal complications. The researchers concluded that breech presentation births were “not an indication for” an elective C-section.
Gunay, T., et al. (2020). Comparison of maternal and fetal complications in pregnant women with breech presentation undergoing spontaneous or induced vaginal delivery, or cesarean delivery. Taiwanese Journal of Obstetrics and Gynecology, 59 (3), 392-397.
This study compared and contrasted complications in spontaneous, induced, or C-section deliveries that involved breech presentation. The researchers found that induced vaginal deliveries had the highest complication rate, while C-sections had the lowest. They concluded that healthcare providers should consider specific delivery types’ risks and benefits when handling breech presentation pregnancies.
Martel-Santiago, C.R., et al. (2020). Delivery in breech presentation: Perinatal outcome and neurodevelopmental evaluation at 18 months of life. European Journal of Obstetrics & Gynecology and Reproductive Biology, 255 , 147-153.
This study compared the outcomes of cephalic and breech deliveries. The researchers found that C-sections involving breech presentations had lower Apgar scores than cephalic presentations. They also found that vaginal concluded that healthcare providers should implement specific protocols in certain breech presentation pregnancies to achieve similar outcomes as cephalic presentation ones.
Toijonen, A.E., et al. (2020). A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case-control study. Archives of Gynecology and Obstetrics, 301 , 393-403.
This study looked at whether breech presentation’s common risks in term labor were present in preterm labor. The researchers found that breech presentation-associated factors in preterm breech deliveries were similar to factors in term pregnancies. By contrast, they found that exceptionally preterm breech births had comparable risks to cephalic presentations.
- Birth Defects
- Cerebral Palsy Birth Injuries
- Infant Brain Damage
- Amniotic Fluid Embolism
- Cephalopelvic Disproportion
- Cervical Dystonia in Infants
- Epidurals and Birth Injuries
- Episiotomy Complications and Side Effects
- Fetal Monitoring During Childbirth
- Forceps Delivery & Birth Injuries
- Fundal Pressure
- Herpes and Infants
- Meconium Aspiration Syndrome
- Most Dangerous Delivery Room Complications
- Newborn Resuscitation and Birth Injuries
- Pitocin and Birth Injuries
- Retained Placenta
- Shoulder Dystocia
- Subconjunctival Hemorrhage
- The History of Childbirth
- Umbilical Cord Prolapse
- Ruptured Uterus
- Vacuum Assisted Delivery and Birth Injuries
- Vaginal Tears
- Help Center

- Privacy Policy
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Please do not include any confidential or sensitive information in a contact form, text message, or voicemail. The contact form sends information by non-encrypted email, which is not secure. Submitting a contact form, sending a text message, making a phone call, or leaving a voicemail does not create an attorney-client relationship.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Breech - series—Types of breech presentation
- Go to slide 1 out of 7
- Go to slide 2 out of 7
- Go to slide 3 out of 7
- Go to slide 4 out of 7
- Go to slide 5 out of 7
- Go to slide 6 out of 7
- Go to slide 7 out of 7
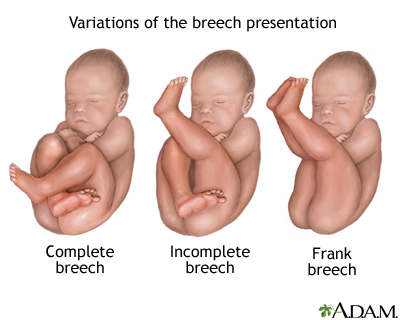
There are three types of breech presentation: complete, incomplete, and frank.
Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
There is also footling breech where one or both feet are presenting.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
Breech Presentation
Affiliations.
- 1 Creighton University School of Medicine
- 2 Creighton University
- PMID: 28846227
- Bookshelf ID: NBK448063
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended).
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Epidemiology
- Pathophysiology
- History and Physical
- Treatment / Management
- Differential Diagnosis
- Pearls and Other Issues
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide

IMAGES
VIDEO
COMMENTS
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Breech presentation, which occurs in approximately 3 percent of fetuses at term, describes the fetus whose presenting part is the buttocks and/or feet. Although most breech fetuses have normal anatomy, this presentation is associated with an increased risk for congenital malformations and mild deformations, torticollis, and developmental ...
Single or double footling presentation: One or both legs are completely extended and present before the buttocks. Types of breech presentations. Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the ...
A breech baby, or breech birth, is when your baby's feet or buttocks are positioned to come out of your vagina first. Your baby's head is up closest to your chest and its bottom is closest to your vagina. Most babies will naturally move so their head is positioned to come out of the vagina first during birth. Breech is common in early ...
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards.
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation.A breech presentation occurs when the fetus's buttocks, feet, or both are in place to come out first during birth. This happens in 3-4% of full-term births.
Types of Breech Presentation Breech babies can present in a variety of ways, including buttocks first, one leg first or both legs first. Frank breech means the buttocks are presenting and the legs are up along the fetal chest. The fetal feet are next to the fetal face.
Almost 90% of breech presentations are born by C/S — no differentiation made between elective and non-elective C/S (3e). Planned VBB success rate of 70% (3d). ... As the feet of a complete breech may be felt below the buttocks [Kotaska A. Menticoglou S. No. 384-management of breech presentation at term. J. Obstet. Gynaecol. Can. 2019; 41: ...
Baby's buttocks lead the way into the birth canal. Hips are flexed, knees are extended, and the feet are in close proximity to the head. 65% to 70% of breech babies are in this position. Complete breech. Baby presents with buttocks first. Both the hips and the knees are flexed; the baby may be sitting cross-legged.
Breech presentation is a type of malpresentation and occurs when the fetal head lies over the uterine fundus and fetal buttocks or feet present over the maternal pelvis (instead of cephalic/head presentation). The incidence in the United Kingdom of breech presentation is 3-4% of all fetuses. 1.
The baby is in a breech position when its buttocks or feet are in place to come out first. There are three types: Frank breech—the baby's buttocks are down and the legs extend straight up in front of the body with the feet up near the head. Complete breech—the baby's buttocks are down with the legs bent at the knees and the feet near ...
Approximately 3-4% of babies end up "upside-down" in breech presentation, with their feet or buttocks near the cervix. Breech presentation is typically diagnosed during a visit to an OB-GYN ...
Overview. Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
The definition of breech presentation is when the buttocks, foot or feet are presenting instead of the head. There are 3 classifications of breech: Frank breech where the hips are flexed and legs extended Complete breech where the hips and knees are flexed and the feet are not below the level of the fetal buttocks
Breech Presentation. With breech presentation, your baby is in a buttocks—or feet-first position. Babies are usually in a head-first position. A breech presentation can make it hard for the baby's head to fit through the birth canal during delivery. This can cause lack of oxygen or nerve damage in your baby.
Complete Breech: in complete breech presentation the butt is aimed down towards the birth canal entrance and the baby is in the traditional "fetal" position with knees bent and pulled up to the chest and feet near the butt. Complete breech is rarest of all types of breech presentation. Less than 10% of breech birth are classified as complete ...
Overview. There are three types of breech presentation: complete, incomplete, and frank. Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal. Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are …
A breech presentation at delivery occurs when the fetus does not turn to a cephalic presentation. ... The relatively larger buttocks dilate the cervix as effectively as the head does in the typical head-down presentation. In contrast, the relative head size of a preterm baby is greater than the fetal buttocks. If the baby is preterm, it may be ...